Abstract
Background/Objectives: Conventional oxygen therapy (COT) is the cornerstone of management for hypoxaemia associated with acute respiratory failure (ARF) in wards. COT implementation guidance is provided in local health guidance documents (LHGDs). This study aimed to identify ward-delivered adult COT implementation LHGDs in Australian health services and assess their content and accuracy. Methods: A scoping review was conducted on 1 May 2022 and updated on 19 December 2023 to identify public health services COT LHGDs. Data were extracted and analysed regarding COT initiation, monitoring, maintenance and weaning, and management of clinical deterioration. Results: Thirty-seven included LHGDs, and eleven referenced the Australian COT guidelines. A definition in the LHGDs for hypoxaemia is that any oxygen saturation (SpO2) or arterial blood gas (ABG) is rare. None required ABG prior to COT initiation. Twenty-nine provided target SpO2 aims for initiation and maintenance. Fifteen did not specify the criteria for clinical review. Nine LHGDs provided guidance on weaning. Conclusions: There was considerable variation in the structure and content of COT LHGDs in Australian health services. Variations and limited guideline concordance of LHGDs may impact the quality and safety of health care. Considerations for future research include the development and implementation of standardised core LHGD recommendations for COT, as well as conducting a national oxygen audit to better measure and benchmark the safety and quality of care.
1. Introduction
Acute respiratory failure (ARF) is characterised by lung impairment leading to insufficient oxygenation (hypoxemia), ventilation (hypercapnia) or both. ARF is a leading cause of hospitalisation with high morbidity and mortality [1,2]. Optimising the management of ARF to improve survival is a key priority for clinicians. Non-invasive respiratory support therapy (NIRS) such as conventional oxygen therapy (COT), high-flow nasal oxygen (HFNO), and non-invasive ventilation (NIV) are important respiratory supports that may be delivered in medical wards to adults with ARF outside of intensive care units and emergency departments [3,4]. Of these supports, conventional oxygen therapy (COT) is the cornerstone of management for hypoxaemia associated with ARF.
COT can be delivered using low-flow nasal cannula or non-rebreather and venturi mask systems that achieve maximum flow rates of 10–15 litres per minute [5]. Often, COT is the preferred initial intervention for ARF over other forms of NIRS, given that it is low-cost, readily available, and non-invasive [6,7]. Nevertheless, appropriate use of COT requires careful prescription with specified target range aims of oxygen saturation for patients with and without hypercapnia, as well as clinical monitoring and review as recommended by professional societies such as the British Thoracic Society (BTS) [8,9]. These clinical practice guidelines recommend that healthcare organisations adopt an implementation approach for COT use, which includes education strategies and local audits to monitor clinical practice and patient outcomes [8,9,10].
However, implementation, adoption, and adherence to national and international clinical practice guidelines are the responsibility of healthcare organisations with well-recognised variations in care [11,12,13,14,15]. A key step in the implementation of COT is the development of local health guidance documents (LHGDs), including policies and procedural protocols informed by clinical practice guidelines, to provide technical information and clinical care standards to clinicians [16,17]. Heterogeneity in content and quality of LHGDs between health services may impact the quality and safety of patient care. Despite the importance of ward-based administration of COT, it is not known to what extent health services have specific LHGDs for COT, if these are informed by clinical practice guidelines, or the accuracy of the included information.
The aim of this study is to identify ward-delivered adult COT implementation LHGDs in Australian health services. Additionally, the study sought to assess their content and how they align with national and international clinical guidelines. We also aimed to develop a standardised minimum core set of information that clinicians require for ward-delivered adult COT implementation. We hypothesised that the structure and fundamental content of the healthcare organisations’ LHGDs would differ greatly.
2. Materials and Methods
A scoping review was conducted to detect and explore public health services’ LHGDs for adult ward-delivered COT implementation for patients with ARF in Australia. This scoping review protocol was registered on the Open Science Framework (https://osf.io/2ghyf) (accessed on 3 September 2024). The search was performed using the PROMPT database (https://prompt.org.au/) (accessed on 3 September 2024), which houses guidance documents online for 110 health services (public and private) in Victoria and New South Wales. This document repository enables participating health services to share LHGDs, aiming to support the provision of safe and high-quality clinical care among organisations, regardless of their available resources, including location and size.
On 1 May 2022, PROMPT was searched with the keywords ‘oxygen therapy’, which detected documents that included these words singularly or as a combination. The document search was updated on 19 December 2023. This search was complemented by incorporating LHGDs from healthcare organisations that did not use PROMPT during the study and were affiliated with the study team.
2.1. Inclusion and Exclusion Criteria
The inclusion criteria for identifying LHGDs were as follows, and documents meeting these criteria were incorporated into this review:
- Documents included local guidance of policy, procedure, protocol or guideline (or a combination);
- The title contained the term ‘oxygen therapy’ or similar;
- The content concentrated on adult ARF ward-delivered COT implementation.
COT LHGDs, which concentrated solely on COT use in paediatric or pregnant populations; oxygen delivery in the home, aged care, palliative care, intensive care, or emergency settings; COT use in ARF due to COVID-19; and HFNO only (without COT) were excluded. All LHGDs that met the inclusion criteria were reviewed, including those from healthcare services with more than one document.
2.2. Screening, Data Extraction, and Analysis
Two independent reviewers (T.T. and M.Z.) conducted title and full-text screening, with differences resolved with additional reviewers (N.S., Y.K., and C.B.) via discussion. Data were extracted using a specifically developed data extraction tool, including key components of (a) indications for COT, (b) COT initiation, monitoring, maintenance and weaning, and (c) overseeing clinical deterioration when using COT therapy and escalation of the care process. Two reviewers (C.B. and T.T.) independently extracted the data and cross-checked it. The full study team resolved any disagreements by discussion. Descriptive statistics using Microsoft Excel (v16.63.1) were used to analyse the data.
3. Results
The initial search of the PROMPT database identified 17,321 documents, with ten additional documents added from Victorian health services not using PROMPT at the time of the study. After title screening, 41 documents underwent full-text review, with 4 documents being ineligible. The remaining 37 documents were included in the final review (Figure 1). No new documents were identified from the updated search in December 2023. However, 12 out of the 37 included documents from the initial search had been updated: 10 had new version identifications or logo amendments without content changes, and 2 had revisions with new information. The most up-to-date versions of LHGDs were included in this study.
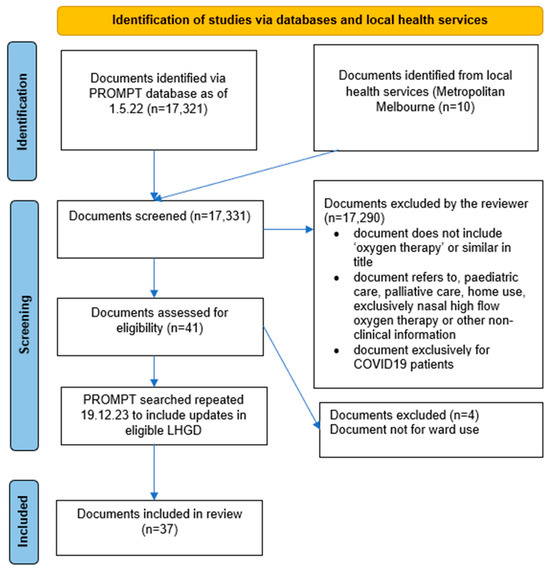
Figure 1.
PRISMA diagram.
3.1. Characteristics of Included Documents
The majority of the LHGDs were from rural health services (n = 21, 56.7%), followed by nine from regional (24.3%) and seven from metropolitan (18.9%) health services. Victorian health services LHGDs were the most represented (n = 36, 97.3%). The document types consisted of local guidelines (n = 17, 46.0%), combined policy and procedures (n = 6, 16.2%), policy (n = 8, 21.6%), and procedures (n = 6, 16.2%). Twelve (29.7%) LHGDs included HFNO recommendations, with others referring to separate HFNO LHGDs (n = 8, 21.6%). Six (16.2%) LHDGs had links to COT use in people with ARF associated with COVID-19. Nurses (n = 32, 86.5%) were the most often specified target audience of LHGDs, followed by doctors (n = 30, 81.1%), physiotherapists (n = 18, 48.6%) or all clinical staff involved in patient care (n = 18, 48.6%) (Supplementary Table S1).
The LHGDs infrequently referenced national and international acute oxygen therapy guidelines. Eleven documents (29.7%) referenced the 2015 Thoracic Society of Australia and New Zealand (TSANZ) Acute Oxygen Guidelines [18]; however, none referenced the revised 2021 TSANZ Acute Oxygen Position Statement [7] or the 2022 European Respiratory Society clinical practice guidelines [19]. The 2008 BTS Guideline for Emergency Oxygen Use in Adults was referred to in six documents (16.2%) [8], with the more recent 2017 BTS Guideline for Emergency Oxygen Use in Adults being referenced less often (n = 4, 10.8%) [9].
3.2. Indications for COT
All LHGDs provided a list of indications for COT, most commonly hypoxaemia (n = 37, 100%), followed by hypercapnic respiratory failure (n = 31, 83.8%), cyanosis (n = 11, 29.7%), and respiratory distress (n = 10, 27.0%) (Table 1). Most LHGDs (n = 23, 62.2%). did not provide a definition for hypoxaemia using one or the other of oxygen saturation (SpO2) or arterial blood gas (ABG) partial pressure of oxygen (PaO2). When definitions of hypoxaemia were specified, just over half (n = 22, 59.5%) stated SpO2 < 92% as a reason to consider COT initiation (Table 1). Pulse oximetry (n = 23, 62.2%) was more frequently recommended for assessment of the presence of hypoxaemia than ABG measurement (n = 13, 35.1%).

Table 1.
Indications for COT.
Less than half the documents included at least one contraindication for COT (n = 18, 48.6%), most commonly cigarette smoking (n = 18, 48.6%), followed by epistaxis (n = 4, 10.8%), base-of-skull fracture (n = 4, 10.8%), and carbon dioxide retention (n = 3, 8.1%). Most (n = 34, 91.9%) did not suggest consideration of goals of care prior to COT initiation. Nearly half of the documents recommended communication with the patients regarding oxygen use (n = 16, 43.2%), but none provided guidance on communication with non-English speakers.
3.3. COT Initiation and Maintenance
No LHGDs required ABG to be performed prior to initiation of COT (Table 2). One document (2.7%) stated that venous blood gases were not appropriate for the assessment of hypoxaemia. Most documents provided target SpO2 ranges for both initiation and ongoing treatments with COT. Recommendations for types and frequency of patient observations varied widely.

Table 2.
Recommendations for implementation and monitoring—COT.
Medical staff were most often described as COT prescribers (n = 21, 56.7%), followed by nurses (n = 14, 37.8%) and physiotherapists (n = 4, 10.8%). The seniority of the medical nurses and physiotherapists who were able to initiate COT was not specified in 12 (32.4%), 22 (59.4%), and 33 (89.2%) of the LHGDs, respectively. No documents recommended the use of a COT prescription chart, yet two-thirds recommended that COT prescriptions include target SpO2 ranges (n = 25), followed by oxygen flow rate (n = 22, 59.4%), oxygen delivery device (n = 21, 56.7%), and frequency of observations (n = 15, 40.5%). Very few LHGDs specified the COT prescription location in the electronic medical record (EMR) (n = 3, 8.1%) or paper-based medical record (n = 3, 8.1%). Thirty-two documents (86.5%) described potential adverse events related to COT use, most commonly hypercapnia (n = 32, 86.5%), followed by cerebral hypoperfusion (n = 6, 16.2%), acute lung injury (n = 5, 13.5%), myocardial infarction (n = 4, 10.8%), and reabsorption atelectasis (n = 4, 10.8%). Guidance on the health professional clinical discipline (i.e., medical, nursing or physiotherapy) responsible for patient reassessment post-COT initiation, including adverse effects, clinical deterioration, or ongoing therapy required, was not specified in all LGHDs, including those that listed more than one clinical discipline such as nurses and doctors.
3.4. Escalation of Care
Maximum litres per minute of oxygen delivery and types of COT devices that could safely be implemented in the medical ward were not provided. Twenty-four (64.9%) documents specified COT devices that can achieve flow rates > 15 L per minute (Supplementary Table S1). Nearly half of the documents stated escalation to other NIRS, including HFNO (n = 15, 40.5%) and NIV (n = 18, 48.6%).
Twenty-two (59.4%) LHGDs contained at least one clinical parameter in COT users that required medical review, such as persistent hypoxaemia on COT despite increasing oxygen flow rate and no improvement in SpO2 while on COT. One document (2.7%) recommended escalation review for utilisation of COT for more than 4 days. Approximately half the documents (n = 19, 51.3%) specified a detection system for care escalation for patients deteriorating despite COT, most commonly the medical emergency criteria (n = 17, 45.9%) followed by the early warning score criteria (n = 2, 5.4%).
3.5. Weaning
Guidance for weaning patients from COT was rarely provided (n = 9, 24.3%). The majority of LHGDs (n = 34, 91.9%) did not specify COT device flow rate targets before commencing weaning. Twenty-nine documents (78.4%) did not provide guidance on which COT device to use (e.g., nasal cannulae or face mask) prior to COT cessation (Table 3). Less than a third of documents (n = 10) provided referral or ongoing clinical review advice for current or potential long-term oxygen therapy users (Supplementary Table S1).

Table 3.
Weaning recommendations for COT.
Following the examination of the LHGDs, including the level of alignment with the current national and international COT recommendations [7,9], we developed a guidance template of essential information for ward-delivered COT implementation in adults with ARF (Table 4). This core information can be used to standardise COT implementation and improve the quality of care in the ward setting.

Table 4.
COT LHGD template.
4. Discussion
This scoping review is the first to investigate LHGDs concerning the implementation of ward-delivered COT to adults with ARF. Key areas of insufficient information included inconsistent definitions of hypoxemia, variable target saturation ranges for COT, no oxygen prescription chart recommendations, limited guidance for COT initiation, maintenance and weaning, and inadequate information for detecting deteriorating patients. Importantly, guidance for treatment escalation to other NIRS (e.g., HFNO or NIV) was often lacking. The small number of LHGDs that included information on HFNO in the same document provided insufficient and varied information regarding initiation, safe monitoring and weaning of HFNO, and none referred to the European Respiratory Society HFNO guidelines [19]. Even fewer COT LHGDs alerted the reader that there were also separate relevant HFNO documents in their organisation. These discrepancies are noteworthy, as they may influence variations in patient care and result in clinician confusion, especially for those who work across multiple health services.
Most LHDGs did not provide a recommended SpO2 or ABG value to define hypoxemia; these parameters are crucial for assessing respiratory status and informing clinical decisions. The TSANZ Acute Oxygen Guidelines recommend initiating COT when people with ARF have SpO2 < 92% (or <88% for people at risk of hypercapnia) [7]. In addition, while the majority of LHGDs provided target SpO2 ranges for patients using COT, there was a lack of consistency with recommendations above and below the evidenced-based recommended SpO2 ranges. Target SpO2 ranges are key to minimising the harm associated with under-oxygenation [20,21] and over-oxygenation [22], yet concerningly, a study by Harper et al. found that patients with prescribed target SpO2 ranges spent significant time below and above these targets [23]. A meta-analysis by Chu et al. showed that oxygen administration above SpO2 94–96% increases in-hospital mortality [24]. Furthermore, there is often a lack of appreciation that too much oxygen can cause harm and that adverse effects occur in those at risk of oxygen-induced hypercapnia [10,25]. Thus, it is vital that LHGDs recommend evidence-based target SpO2 ranges, including stating an upper limit for the range.
National and international acute COT guidelines have recommended written oxygen therapy prescriptions in the medical record and drug chart, including target oxygen saturation range, monitoring, and maintenance (e.g., titration) to achieve treatment aims [7,9]. Despite these recommendations, documentation of oxygen prescriptions is variable and often not guideline-concordant and may contribute to adverse events [26,27,28,29]. Anderson et al. study reports that over-oxygenation occurred in two-thirds of admissions in the setting of high levels of medical record oxygen prescription documentation but with inadequate documentation on prescription charts [30]. No LHDGs recommended the use of a COT prescription chart, and very few specified a documentation location in the medical record. There is no standardised COT prescription chart in Australia, and the national inpatient medication chart is not recommended for COT prescription, as the design elements do not effectively support the safe prescription, administration and monitoring of COT [31]. Notwithstanding, the development and use of a COT prescription chart, integrated into the EMR, is key to improved COT implementation, monitoring, and safe care.
While COT is used routinely in the ward setting for patients with ARF, some will fail COT and early deterioration detection and response is required to consider escalation to alternative NIRS such as HFNO or NIV, which may avoid transfer to higher acuity areas such as intensive care units (ICUs), and improve outcomes [32,33]. The physiological parameter most commonly recommended for monitoring patients on COT was SpO2, with respiratory rate and heart rate infrequently recommended and with considerable variability between LHGDs. However, respiratory rate is an important but under-utilised early indicator of clinical deterioration in medical wards, which can increase many hours before the oxygen saturations fall [34,35]. The frequency and timing of physiological observations were often lacking and also highly variable between LHGDs. The TSANZ and BTS Acute Oxygen Guidelines recommend using a physiological track and trigger system, such as an early warning score, to predict inpatient deterioration and identify at-risk patients [7,9]. Notably, there are many different early warning systems in use in different Australian hospitals [36]. In this study, half of the LHGDs specified a detection system, most commonly the modified early warning score used within the medical emergency team, for rapid care escalation for patients deteriorating despite COT [37,38]. No LHGDs in this study provided guidance as to the upper limit for ward-delivered COT flow, with one document recommending clinical review for those using COT for more than four days.
In this study, most LHGDs did not reference the national or international acute oxygen therapy clinical practice guidelines [7,9,19]. The TSANZ and BTS guidelines for acute oxygen therapy provide key evidenced-based recommendations regarding indications for COT use, monitoring required after initiation, and maintenance and weaning of COT [7,9]. Not drawing on or citing these key guidelines by LHGD authors may have occurred due to a lack of awareness or due to limited time and resources to review and update LHGDs as new guidelines are published [39]. A study by Alonso-Coello et al. found that half of the organisations had no standardised process for assessing whether a guideline is out of date, only a fifth would use external guidelines when updating or developing local guidelines, and two-thirds report that the current review and updating process lacks rigour [39]. Nevertheless, to improve clinical care provision and quality for patients using ward-delivered COT, it is crucial that LHGDs reflect national and international guidelines’ evidence-based recommendations.
The development and implementation of a standardised core LHGD template for ward-delivered COT is a mechanism that could be utilised to tackle LHGD inconsistencies. Such a template could then be adapted according to the local healthcare organisation’s context and service provision. In the United Kingdom, the BTS developed a national oxygen audit tool to support healthcare organisations in monitoring oxygen guideline implementation, and in hospitals that use electronic medical records (EMRs), it is possible to automate key guidance components to monitor oxygen use at the individual and hospital-wide levels [40,41]. This national program evolved to include all NIRS; however, in Australia, there is no similar national approach to audit COT implementation or examine any education provided to clinicians regarding COT.
While this study identified variations in recommendations for ward-delivered COT, it is unknown how the LHGDs are used by clinicians. Previous studies have shown under-utilisation of LHGDs and clinical practice guidelines due to a lack of awareness and preferential use of knowledge and clinical experience [29,42]. Additionally, writing a guideline for oxygen therapy alone will not change clinical practice without active measures (e.g., staff education—senior and junior; doctors, nurses, and physiotherapists, local champions, electronic medical record prompts and links to decision-aid tools, posters on the wall near oxygen source) to ensure effective implementation and behaviour change [29,42,43,44].
It is imperative that future research investigate LHGD awareness and use by clinicians in their daily practice and uncover the elements that hinder or aid their implementation. Additionally, monitoring health services with COT LHGD patient outcomes could illuminate the importance of the adoption of high-quality LHGDs for the safe delivery of COT.
Strengths and Limitations
This is the first study to evaluate acute oxygen LHGDs to ascertain if core recommendations are consistent, based on current evidence, and provide sufficient information to support clinical decisions and application, to our knowledge. A scoping review approach with a clear protocol was utilised in this study. We used the PROMPT database, an LHGD-sharing portal utilised by over 100 health services in the largest states in Australia (by population of over 15 million) and across metropolitan, rural and regional areas [45]. A limitation of this study is that not all health services utilise the PROMPT portal; hence, the identified LHGDs in this study might not be representative of all LHGDs for COT in the ward setting.
5. Conclusions
Considerable variation in the composition and content of LHGDs for ward-delivered COT implementation in Australian public health services has been shown in this novel study. We identified significant variations in the guidance for the initiation, monitoring, and weaning of COT, as well as the mechanism for detecting patient deterioration when using COT. Such variations and limited guideline concordance of LHGDs may impact the quality and safety of health care. Considerations for future research include the development and implementation of standardised core LHGD recommendations for COT and conducting a national oxygen audit to better measure and benchmark the safety and quality of care.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/jcm13185506/s1, Table S1: Further characteristics of included LHGDs.
Author Contributions
Conceptualisation, C.B., Y.H.K. and N.S.; methodology, C.B., Y.H.K. and N.S.; validation, C.B.; formal analysis, C.B.; investigation, C.B.; resources, N.S.; data curation, C.B.; writing—original draft preparation, C.B.; writing—review and editing, C.B., Y.H.K., T.T. and N.S. supervision, N.S.; project administration, C.B. and N.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding. C.B. is supported by the Australian Government Research Training Program Scholarship.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data used are not publicly available to maintain the anonymity of the health services that were included in the study.
Acknowledgments
We would like to thank Muhtasim Rahman Zahin (M.Z.) for their contribution to this study.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Chen, L.; Rackley, C.R. Diagnosis and Epidemiology of Acute Respiratory Failure. Crit. Care Clin. 2024, 40, 221–233. [Google Scholar] [CrossRef] [PubMed]
- Wong, A.-K.I.; Kamaleswaran, R.; Tabaie, A.; Reyna, M.A.; Josef, C.; Robichaux, C.; de Hond, A.A.H.; Steyerberg, E.W.; Holder, A.L.; Nemati, S.; et al. Prediction of Acute Respiratory Failure Requiring Advanced Respiratory Support in Advance of Interventions and Treatment: A Multivariable Prediction Model From Electronic Medical Record Data. Crit. Care Explor. 2021, 3, e0402. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.-C.; Peng, Y.; Dai, B.; Hou, H.-J.; Zhao, H.-W.; Wang, W.; Tan, W. Comparison between high-flow nasal cannula and conventional oxygen therapy in COVID-19 patients: A systematic review and meta-analysis. Ther. Adv. Respir. Dis. 2024, 18, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Roca, O.; Riera, J.; Torres, F.; Masclans, J.R. High-flow oxygen therapy in acute respiratory failure. Respir. Care 2010, 55, 408–413. [Google Scholar]
- Batool, S.; Garg, R. Appropriate Use of Oxygen Delivery Devices. Open Anesthesiol. J. 2017, 11, 35–38. [Google Scholar] [CrossRef]
- Gottlieb, J.; Capetian, P.; Hamsen, U.; Janssens, U.; Karagiannidis, C.; Kluge, S.; Nothacker, M.; Roiter, S.; Volk, T.; Worth, H.; et al. German S3 Guideline: Oxygen Therapy in the Acute Care of Adult Patients. Respiration 2022, 101, 214–252. [Google Scholar] [CrossRef]
- Barnett, A.; Beasley, R.; Buchan, C.; Chien, J.; Farah, C.S.; King, G.; McDonald, C.F.; Miller, B.; Munsif, M.; Psirides, A.; et al. Thoracic Society of Australia and New Zealand Position Statement on Acute Oxygen Use in Adults: ‘Swimming between the flags’. Respirology 2022, 27, 262–276. [Google Scholar] [CrossRef]
- O’Driscoll, B.R.; Howard, L.S.; Davison, A.G. BTS guideline for emergency oxygen use in adult patients. Thorax 2008, 63, vi1–vi68. [Google Scholar] [CrossRef]
- O’Driscoll, B.R.; Howard, L.S.; Earis, J.; Mak, V. BTS guideline for oxygen use in adults in healthcare and emergency settings. Thorax 2017, 72, ii1–ii90. [Google Scholar] [CrossRef]
- Kane, B.; Decalmer, S.; Ronan O’Driscoll, B. Emergency oxygen therapy: From guideline to implementation. Breathe 2013, 9, 246–253. [Google Scholar] [CrossRef]
- Guerra-Farfan, E.; Garcia-Sanchez, Y.; Jornet-Gibert, M.; Nuñez, J.H.; Balaguer-Castro, M.; Madden, K. Clinical practice guidelines: The good, the bad, and the ugly. Injury 2023, 54, S26–S29. [Google Scholar] [CrossRef]
- Pereira, V.C.; Silva, S.N.; Carvalho, V.K.S.; Zanghelini, F.; Barreto, J.O.M. Strategies for the implementation of clinical practice guidelines in public health: An overview of systematic reviews. Health Res. Policy Syst. 2022, 20, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Sutherland, K.; Levesque, J.F. Unwarranted clinical variation in health care: Definitions and proposal of an analytic framework. J. Eval. Clin. Pract. 2020, 26, 687–696. [Google Scholar] [CrossRef] [PubMed]
- Australian Commission on Safety and Quality in Health Care. The Fourth Australian Atlas of Healthcare Variation; Australian Commission on Safety and Quality in Health Care: Canberra, Australia, 2021.
- NHS Right Care. Reducing unwarranted variation to improve health outcomes and value. In The 2nd Atlas of Variation in Risk Factors and Healthcare for Respiratory Disease in England; Public Health England: London, UK, 2019. Available online: https://fingertips.phe.org.uk/static-reports/atlas-of-variation/2ndRespiratoryAtlas_v1.0_20190923.pdf (accessed on 3 September 2024).
- Australian Commission on Safety and Quality in Health Care. National Safety and Quality Health Service Standards Guideline for Hospitals. Available online: https://www.safetyandquality.gov.au/sites/default/files/migrated/National-Safety-and-Quality-Health-Service-Standards-Guide-for-Hospitals.pdf (accessed on 29 June 2024).
- Australian Commission on Safety and Quality in Health Care. Action 1.07: Policies and Procedures. Available online: https://www.safetyandquality.gov.au/standards/nsqhs-standards/clinical-governance-standard/patient-safety-and-quality-systems/action-107#:~:text=Action%201.07%20states,-The%20health%20service&text=Set%20out%2C%20review%2C%20and%20maintain,legislation%2C%20regulation%20and%20jurisdictional%20requirements (accessed on 29 June 2024).
- Beasley, R.; Chien, J.; Douglas, J.; Eastlake, L.; Farah, C.; King, G.; Moore, R.; Pilcher, J.; Richards, M.; Smith, S.; et al. Thoracic Society of Australia and New Zealand oxygen guidelines for acute oxygen use in adults: ‘Swimming between the flags’. Respirology 2015, 20, 1182–1191. [Google Scholar] [CrossRef] [PubMed]
- Oczkowski, S.; Ergan, B.; Bos, L.; Chatwin, M.; Ferrer, M.; Gregoretti, C.; Heunks, L.; Frat, J.-P.; Longhini, F.; Nava, S.; et al. ERS clinical practice guidelines: High-flow nasal cannula in acute respiratory failure. Eur. Respir. J. 2022, 59, 2101574. [Google Scholar] [CrossRef]
- Bowton, D.L.; Scuderi, P.E.; Haponik, E.F. The incidence and effect on outcome of hypoxemia in hospitalized medical patients. Am. J. Med. 1994, 97, 38–46. [Google Scholar] [CrossRef]
- Buist, M.; Bernard, S.; Nguyen, T.V.; Moore, G.; Anderson, J. Association between clinically abnormal observations and subsequent in-hospital mortality: A prospective study. Resuscitation 2004, 62, 137–141. [Google Scholar] [CrossRef]
- Siemieniuk, R.A.C.; Chu, D.K.; Kim, L.H.-Y.; Güell-Rous, M.-R.; Alhazzani, W.; Soccal, P.M.; Karanicolas, P.J.; Farhoumand, P.D.; Siemieniuk, J.L.K.; Satia, I.; et al. Oxygen therapy for acutely ill medical patients: A clinical practice guideline. BMJ 2018, 363, k4169. [Google Scholar] [CrossRef]
- Harper, J.C.P.; Semprini, R.; Kearns, N.A.; Hatter, L.; Bird, G.E.; Braithwaite, I.; Eathorne, A.; Weatherall, M.; Beasley, R. Determination of oxygen saturation compared to a prescribed target range using continuous pulse oximetry in acutely unwell medical patients. BMC Pulm. Med. 2021, 21, 1–9. [Google Scholar] [CrossRef]
- Chu, D.K.; Kim, L.H.; Young, P.J.; Zamiri, N.; Almenawer, S.A.; Jaeschke, R.; Szczeklik, W.; Schünemann, H.J.; Neary, J.D.; Alhazzani, W. Mortality and morbidity in acutely ill adults treated with liberal versus conservative oxygen therapy (IOTA): A systematic review and meta-analysis. Lancet 2018, 391, 1693–1705. [Google Scholar] [CrossRef]
- Sarkar, M.; Madabhavi, I.; Kadakol, N. Oxygen-induced hypercapnia: Physiological mechanisms and clinical implications. Monaldi Arch. Chest Dis. 2022, 93, 2399. [Google Scholar] [CrossRef] [PubMed]
- Deshpande, S.; Datey, N.; Liacos, A.; Joosten, S.A.; Leong, P. Acute oxygen use in hospitalised patients with chronic obstructive pulmonary disease is guideline discordant. Intern. Med. J. 2021, 51, 780–783. [Google Scholar] [CrossRef] [PubMed]
- Kamran, A.; Chia, E.; Tobin, C. Acute oxygen therapy: An audit of prescribing and delivery practices in a tertiary hospital in Perth, Western Australia. Intern. Med. J. 2018, 48, 151–157. [Google Scholar] [CrossRef] [PubMed]
- McDonald, V.; Cousins, J.; Wark, P. Acute oxygen therapy: A review of prescribing and delivery practices. Int. J. Chronic Obstr. Pulm. Dis. 2016, 11, 1067–1075. [Google Scholar] [CrossRef]
- Cousins, J.L.; Wark, P.A.B.; Hiles, S.A.; McDonald, V.M. Understanding Clinicians’ Perceived Barriers and Facilitators to Optimal Use of Acute Oxygen Therapy in Adults. Int. J. Chron. Obs. Pulmon Dis. 2020, 15, 2275–2287. [Google Scholar] [CrossRef]
- Anderson, J.; Hoang, T.; Hay, K.; Tay, G. Evaluation of inpatient oxygen therapy in hypercapnic chronic obstructive pulmonary disease. Intern. Med. J. 2021, 51, 654–659. [Google Scholar] [CrossRef]
- Australian Commission on Safety and Quality in Health Care. NIMC User Guide. National In-patient Medication Chart. Available online: https://www.safetyandquality.gov.au/ (accessed on 3 September 2024).
- Lee, C.C.; Mankodi, D.; Shaharyar, S.; Ravindranathan, S.; Danckers, M.; Herscovici, P.; Moor, M.; Ferrer, G. High flow nasal cannula versus conventional oxygen therapy and non-invasive ventilation in adults with acute hypoxemic respiratory failure: A systematic review. Respir. Med. 2016, 121, 100–108. [Google Scholar] [CrossRef]
- Vincent, J.-L.; Einav, S.; Pearse, R.; Jaber, S.; Kranke, P.; Overdyk, F.J.; Whitaker, D.K.; Gordo, F.; Dahan, A.; Hoeft, A. Improving detection of patient deterioration in the general hospital ward environment. Eur. J. Anaesthesiol. 2018, 35, 325–333. [Google Scholar] [CrossRef]
- Palmer, J.H.; James, S.; Wadsworth, D.; Gordon, C.J.; Craft, J. How registered nurses are measuring respiratory rates in adult acute care health settings: An integrative review. J. Clin. Nurs. 2023, 32, 4515–4527. [Google Scholar] [CrossRef]
- Churpek, M.M.; Adhikari, R.; Edelson, D.P. The value of vital sign trends for detecting clinical deterioration on the wards. Resuscitation 2016, 102, 1–5. [Google Scholar] [CrossRef]
- Le Lagadec, M.D.; Dwyer, T.; Browne, M. The efficacy of twelve early warning systems for potential use in regional medical facilities in Queensland, Australia. Aust. Crit. Care 2020, 33, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Jones, D. The medical emergency team—Current status and future directions: A perspective for acute care physicians. Intern. Med. J. 2023, 53, 888–891. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, L.T.; Grion, C.M.; Matsuo, T.; Anami, E.H.; Kauss, I.A.; Seko, L.; Bonametti, A.M. Impact of delayed admission to intensive care units on mortality of critically ill patients: A cohort study. Crit. Care 2011, 15, R28. [Google Scholar] [CrossRef] [PubMed]
- Alonso-Coello, P.; Martínez García, L.; Carrasco, J.M.; Solà, I.; Qureshi, S.; Burgers, J.S. The updating of clinical practice guidelines: Insights from an international survey. Implement. Sci. 2011, 6, 107. [Google Scholar] [CrossRef] [PubMed]
- O’Driscoll, B.R.; Howard, L.S.; Bucknall, C.; Welham, S.A.; Davison, A.G. British Thoracic Society emergency oxygen audits. Thorax 2011, 66, 734–735. [Google Scholar] [CrossRef]
- O’Driscoll, R.; Bakerly, N.D. Automated audit of hospital oxygen use devised during the COVID-19 pandemic. BMJ Open Respir. Res. 2023, 10, e001866. [Google Scholar] [CrossRef]
- Foley, C. A Study of the Relationship bewteen Hospital Policy and Nursing Practice. Ph.D. Thesis, University of Tasmania, Hobart, Australia, 2020. [Google Scholar]
- Talat, U.; Schmidtke, K.A.; Khanal, S.; Turner, A.M.; Vlaev, I. Can guidelines rein in oxygen use? A retrospective cross-sectional study using routinely collected data. Int. J. Qual. Health Care 2023, 35, 1–7. [Google Scholar] [CrossRef]
- Baker, R.; Camosso-Stefinovic, J.; Gillies, C.; Shaw, E.J.; Cheater, F.; Flottorp, S.; Robertson, N. Tailored interventions to overcome identified barriers to change: Effects on professional practice and health care outcomes. Cochrane Database Syst. Rev. 2010, 3, 1–86. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. National, State and Territory Population, December 2023. Available online: https://population.gov.au/data-and-forecasts/key-data-releases/national-state-and-territory-population-december-2023 (accessed on 29 June 2024).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).