Abstract
Sleep disturbances are strongly associated with mild traumatic brain injury (mTBI) and post-traumatic stress disorder (PTSD). PTSD and mTBI have been linked to alterations in white matter (WM) microstructure, but whether poor sleep quality has a compounding effect on WM remains largely unknown. We evaluated sleep and diffusion magnetic resonance imaging (dMRI) data from 180 male post-9/11 veterans diagnosed with (1) PTSD (n = 38), (2) mTBI (n = 25), (3) comorbid PTSD+mTBI (n = 94), and (4) a control group with neither PTSD nor mTBI (n = 23). We compared sleep quality (Pittsburgh Sleep Quality Index, PSQI) between groups using ANCOVAs and calculated regression and mediation models to assess associations between PTSD, mTBI, sleep quality, and WM. Veterans with PTSD and comorbid PTSD+mTBI reported poorer sleep quality than those with mTBI or no history of PTSD or mTBI (p = 0.012 to <0.001). Poor sleep quality was associated with abnormal WM microstructure in veterans with comorbid PTSD+mTBI (p < 0.001). Most importantly, poor sleep quality fully mediated the association between greater PTSD symptom severity and impaired WM microstructure (p < 0.001). Our findings highlight the significant impact of sleep disturbances on brain health in veterans with PTSD+mTBI, calling for sleep-targeted interventions.
1. Introduction
Approximately 23% of military service members returning from deployment to Iraq and Afghanistan are subsequently diagnosed with post-traumatic stress disorder (PTSD) [], making it one of the most common psychiatric diagnoses in veterans []. Additionally, 12–35% of service members sustain a mild traumatic brain injury (mTBI) [,], which increases the risk of developing or exacerbating PTSD symptom severity [,,]. While poor sleep quality is highly prevalent in veterans in general [], it is particularly important in the context of PTSD and mTBI. In fact, poor sleep quality is a hallmark symptom of PTSD [,], highly prevalent after mTBI [,,], and has been associated with increased symptom severity [] and slower recovery from both PTSD and mTBI []. Alarmingly, sleep quality disturbances may remain present for years after a traumatic experience [], adversely impact quality of life [,], and respond poorly to treatment-as-usual [,]. However, the pathomechanisms underlying the compounding effects of poor sleep quality in those with PTSD and mTBI are not fully understood, impeding the development of proper diagnostic and treatment protocols.
Evidence suggests that sleep is directly linked to brain homeostasis and is essential to preserve the environment the brain requires to function optimally []. Interestingly, sleep seems particularly relevant for white matter health, with animal studies showing that the number of myelin-forming proliferating oligodendrocytes doubles during sleep []. Furthermore, sleep impairments have been related to brain volume loss [,], reduced neurogenesis, and reduced cortical activation [,].
Magnetic resonance imaging (MRI) allows for the in vivo, three-dimensional investigation of brain structure, and thus, provides a vital avenue to study the pathomechanisms underlying poor sleep quality, PTSD, and mTBI in military veterans []. Diffusion-weighted MRI (dMRI) studies revealed white matter (WM) microstructure alterations associated with PTSD [,,,,,,,,,,,,,,,,,], mTBI [,,,,,,], and comorbid PTSD+mTBI [,,,]. Moreover, various studies showed widespread alterations of white matter microstructure in association with poor sleep quality in otherwise healthy individuals. Most studies utilized fractional anisotropy (FA) as a marker of white matter microstructural integrity and tissue organization and found lower FA related to poorer sleep quality in frontal, temporal, parietal, and occipital regions [,,,,,,,,,,]. A few studies have also linked white matter alterations to impaired sleep quality in individuals with PTSD [] and mTBI [,], revealing associations between poor sleep quality and decreased FA in several main white matter fiber tracts. However, the link between sleep quality and WM microstructure in the context of PTSD and mTBI remains largely unknown.
The current study addresses the understudied impact of sleep quality disturbances on brain structure in the context of PTSD and mTBI. We assess the relationship between sleep quality, PTSD, mTBI, and WM microstructure, leveraging a large sample of veterans returning from deployment to Iraq and Afghanistan (N = 180). As highlighted above, earlier studies have consistently demonstrated the impact of PTSD, mTBI, or comorbid PTSD+mTBI on brain structure and function. Therefore, we followed a previous publication [] and examined sleep quality in groups of veterans with PTSD, mTBI, comorbid PTSD+mTBI, or no history of PTSD or mTBI. Next, we assessed the associations between PTSD, mTBI, sleep quality, and WM microstructure in the combined sample and the four groups. Our central hypotheses were that veterans with PTSD, mTBI, or comorbid PTSD+mTBI would experience poorer sleep quality than veterans without a history of PTSD or mTBI. We further hypothesized that PTSD, mTBI, and poorer sleep quality were related to WM microstructure. We subsequently conducted post-hoc mediation analyses based on our primary analyses to examine the interactions between PTSD, mTBI, sleep quality, and WM microstructure.
2. Materials and Methods
2.1. Participants
The Translational Research Center for TBI and Stress Disorders (TRACTS) study is a longitudinal prospective cohort study of Operation Enduring Freedom (OEF)/Operation Iraqi Freedom (OIF) military service members [].
Out of the first 384 consecutively recruited service members at the VA Boston Healthcare System Jamaica Plain Campus, 278 participants underwent an MRI assessment and consented to share their data with investigators outside of TRACTS. Twenty-five cases did not pass the visual neuroimaging data quality control due to excessive motion or scanner artifacts. Additional reasons for the exclusion of participants can be found in Figure S1. The final sample for the current project consisted of 180 participants, which were classified into four groups based on lifetime diagnoses of PTSD and mTBI: PTSD only (n = 38), mTBI only (n = 25), comorbid PTSD+mTBI (n = 94), and no history of PTSD or mTBI (n = 23). We opted for this grouping approach based on previous studies in veteran populations [,]. We used cumulative lifetime diagnoses, as previous studies demonstrate a stronger influence on GM and WM structure when considering lifetime diagnoses [,], suggesting that disorder-related neurobiological effects persist or even increase over time.
2.2. Diagnostic and Clinical Assessment
2.2.1. Assessment of PTSD
Lifetime PTSD diagnosis and current symptom severity were assessed according to the 30-item Clinician-Administered PTSD Scale for DSM-IV (CAPS-IV) []. To assess PTSD symptom severity separate from sleep quality, we removed two items (i.e., difficulty sleeping and recurrent distressing dreams) from the scale and calculated a sleep-corrected PTSD total score, in line with prior work [].
2.2.2. Assessment of mTBI
The Boston Assessment of TBI-Lifetime (BAT-L) [] was administered to diagnose mTBI and to rate the cumulative lifetime mTBI burden. The BAT-L distinguishes mild, moderate, and severe TBIs, where a mild TBI is classified as loss of consciousness not exceeding 30 min and where posttraumatic amnesia or an altered mental status must not exceed 24 h. The BAT-L classifies mild TBI into stages 1–3, where a higher stage refers to greater mTBI severity. Using this assessment tool, a total mTBI burden score was computed from the number and severity of all mTBIs pre-, during, and post-deployment. Pre-deployment mTBIs included mTBIs before enlistment. MTBIs during deployment referred to all deployments if deployed multiple times.
2.2.3. Assessment of Sleep Quality
Current sleep quality was assessed using the Pittsburgh Sleep Quality Index (PSQI) [], an 18-item self-report questionnaire measuring subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medication, and daytime dysfunction on seven subscales. Here, we follow a previously reported and validated approach suggesting that the seven subscales of the PSQI are best represented by three factors: sleep efficiency, perceived sleep quality, and daily disturbances [] (Figure S2).
2.2.4. Assessment of Comorbid Psychiatric Disorders
The non-patient research version of the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I/NP) [] was used to diagnose comorbid lifetime psychiatric disorders.
2.2.5. Assessment of Warzone-Related Stress
Warzone-related stress was assessed using the Deployment Risk & Resilience Inventory-2 (DRRI-2) [].
2.3. Magnetic Resonance Imaging
2.3.1. Image Acquisition
DMRI data were acquired on a 3-Tesla Siemens TIM Trio scanner (Siemens Healthineers, Erlangen, Germany) at the VA Medical Center in Boston using a single-shot echo-planar sequence with a twice-refocused spin-echo pulse. The following sequence parameters were applied: 64 axial slices with no inter-slice gap, 60 gradient directions with a b-value of 700 s/mm2, and 10 additional scans with b = 0 gradients, TR = 10,000 ms, TE = 103 ms, voxel size = 2 × 2 × 2 mm3, and FOV = 256 mm2.
2.3.2. Image Pre-Processing
The dMRI data were processed in several steps using an in-house image processing pipeline (https://github.com/pnlbwh/pnlutil/blob/master/pipeline/README.md, accessed on 1 October 2018). First, the images were axis-aligned, centered, motion-, and eddy current-corrected utilizing the FMRIB Software Library (version 5.1, https://fsl.fmrib.ox.ac.uk/fsl/fslwiki/, accessed on 1 October 2018) [,]. Image quality was checked for artifacts using 3D Slicer (version 4.5, http://www.slicer.org, accessed on 1 October 2018) [], leading to the exclusion of 25 participants (due to severe motion artifact or signal dropout). DMRI brain masks were created using SlicerDMRI [,] and corrected manually where necessary.
2.3.3. WM Fiber Clustering
We conducted WM fiber clustering utilizing an open-source pipeline, whitematteranalysis software (https://github.com/SlicerDMRI/whitematteranalysis, accessed on 1 May 2019), to perform fiber tract parcellation and extraction automatically. The white matter fiber clustering method extracts fiber tracts from the entire brain by grouping tracts based on their anatomical shape and spatial location. This method is significantly improved compared to previous automated fiber tracking methods, which can only extract the main fiber tracts, failing to cover the entire brain’s white matter (i.e., including the cerebellum and superficial tracts). In addition, it was successfully applied in several recent studies [,,,,,,,,,], demonstrating high test-retest reproducibility [] and robustness to anatomical variability [].
First, a two-tensor whole-brain unscented Kalman Filter (UKF) tractography was computed (https://github.com/pnlbwh/ukftractography, accessed on 1 May 2019) [,]. A two-tensor model was chosen to account for crossing fibers [,]. The first tensor is associated with the main direction of a fiber tract, while the second tensor represents crossing fibers. We performed qualitative and quantitative quality checks of the generated tractography data for all subjects using the whitematteranalysis software quality control tool (https://github.com/SlicerDMRI/whitematteranalysis, accessed on 1 May 2019). Previous studies demonstrated that the UKF method is highly consistent [] and more sensitive than single-tensor tractography [,,].
Next, we identified white matter fiber tracts for each subject using the White Matter Analysis (WMA) package for tract parcellation. WMA is based on a neuroanatomist-curated white matter atlas (http://dmri.slicer.org/atlases/, accessed on 1 May 2019) [] and applies machine learning to identify fiber tracts in an individual [,,]. This approach enabled us to substantially reduce the known tractography issue of false-positive tracking, increasing the repeatability of white matter parcellation []. False positive fibers in the atlas have been annotated and marked as to be excluded based on expert neuroanatomical judgment []. For each subject, atlas-based white matter parcellation [,,] was performed, registering the tractography to the atlas space. The similarity between the fibers in the atlas and the fibers of an individual was quantified, used to classify the fibers into a cluster, and finally assigned to the corresponding tract in the atlas.
As highlighted in the introduction, we expected a widespread effect of sleep on WM microstructure [,,,,]. For our primary analyses, we, therefore, opted to merge the entire brain’s fiber tracts into one whole-brain WM variable by appending all WM tracts into one large tract. For supplementary analyses, the main white matter fiber tracts (left/right arcuate fasciculus, cingulum bundle, inferior longitudinal fasciculus, inferior occipito-frontal fasciculus, superior longitudinal fasciculus, uncinate fasciculus, and corpus callosum) were extracted. To ensure there were no individual participants with outlier values, we performed a quantitative quality assessment of the number of fiber streamlines. Moreover, each participant’s whole-brain white matter tracts were visually evaluated, following standardized guidelines [,,,,,]. All data successfully passed the quality check.
2.3.4. Diffusion Parameter Extraction
We used free-water (FW) imaging to obtain a voxel-wise whole-brain free-water corrected fractional anisotropy (FAT) value for each individual. By separating the MRI signal into two compartments [], FW imaging is able to eliminate partial volume with extracellular FW (e.g., caused by CSF contamination, edema, or atrophy) in each voxel. Given the correction for FW, FAT serves as a more accurate marker for cellular WM structure than the conventional FA measure [].
2.4. Statistical Analysis
Statistical analyses were performed using IBM SPSS Statistics 27. We created figures using R 4.0.3, GraphPad Prism 9, Python 3.10.2, and PowerPoint. We applied a hierarchical statistical approach, conducting all analyses in the total sample and if significant in the four groups (PTSD, mTBI, comorbid PTSD+mTBI, no history of PTSD or mTBI; Figure 1). All analyses included age as a covariate and were corrected for multiple comparisons, as detailed in Figure 1.
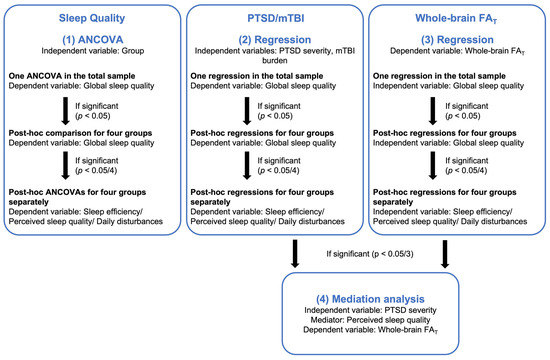
Figure 1.
Hierarchical statistical approach. Note. PTSD, post-traumatic stress disorder; mTBI, mild traumatic brain injury; PSQI, Pittsburgh Sleep Quality Index; FAT, fractional anisotropy tissue. This figure illustrates the hierarchical statistical approach.
2.4.1. Group Differences in Sleep Quality
First, we wanted to examine if sleep quality differed according to veterans‘ histories of PTSD and mTBI. We conducted one ANCOVA, including group (PTSD, mTBI, comorbid PTSD+mTBI, no history of PTSD or mTBI) as the independent variable and global sleep quality as the dependent variable. If the overall ANCOVA was significant (p < 0.05), we performed post-hoc comparisons for the four groups. If the group comparisons for global sleep quality were significant (p < 0.05/4), we post-hoc compared sleep efficiency, perceived sleep quality, and daily disturbances between the four groups.
2.4.2. PTSD, mTBI, and Sleep Quality
Next, we calculated one regression analysis in the total sample, including PTSD symptom severity and mTBI burden as the independent variables and global sleep quality as the dependent variable. In the case of significant associations between PTSD symptom severity, mTBI burden, and global sleep quality (p < 0.05), we repeated the regression analyses within the four groups separately. If the regression model was found significant in one of the groups (p < 0.05/4), we performed three additional regression analyses, including PTSD symptom severity/mTBI burden as the independent variable and sleep efficiency, perceived sleep quality, and daily disturbances as dependent variables respectively.
2.4.3. Sleep Quality and WM Microstructure
Next, we conducted a regression analysis in the total sample, including global sleep quality as the independent variable and whole-brain FAT as the dependent variable. In the case of a significant association (p < 0.05), we repeated the regression analysis within each group. If found significant in one of the groups (p < 0.05/4), we performed three additional regression analyses, including sleep efficiency, perceived sleep quality, and daily disturbances as the independent variables and whole-brain FAT as the dependent variable.
In addition, we computed supplementary analyses with the FAT of the main WM fiber tracts as the dependent variables (Table S3).
2.4.4. Sleep Quality as a Mediator between PTSD Symptom Severity and WM Microstructure
Given the significant associations between PTSD symptom severity and perceived sleep quality and between perceived sleep quality and whole-brain FAT, we performed a post-hoc mediation analysis. Here, we assessed whether perceived sleep quality (mediator) mediated the association between PTSD symptom severity (independent variable) and whole-brain FAT (dependent variable). The model was calculated using the Hayes PROCESS macro [] for SPSS (model 4), which follows a nonparametric bootstrapping procedure based on n = 5000 samples and a 95% CI.
We repeated the mediation analysis controlling for variables that have repeatedly been associated with alterations in brain structure. These included lifetime psychiatric diagnoses (mood [,,,,], anxiety [,,], and substance use disorder [,], Figure S3), warzone-related stress [,,,], body mass index (BMI) [,,,,,], current psychiatric medication use [,,,,,], race (white, non-white) [], and completed years of education [,].
3. Results
For demographic information, please see Table 1 and Table S1. The four groups did not significantly differ in age, the number of deployments, and the total duration of the deployment. Veterans with comorbid PTSD+mTBI were the most severely clinically burdened group, as indicated by the high number of comorbid psychiatric diagnoses, medication use, and the highest rates of military mTBI (mTBIs sustained during deployment or military service) in this group.

Table 1.
Sample characteristics.
3.1. Group Differences in Sleep Quality
We first examined the influence of a diagnosis of PTSD and mTBI on sleep quality using ANCOVAs. Table 2 and Figure S4 display the differences in sleep quality between the groups. The PTSD and comorbid PTSD+mTBI groups demonstrated more significant impairments on the PSQI global sleep quality, sleep efficiency, perceived sleep quality, and daily disturbances scales than those with mTBI or no history of PTSD or mTBI. There were no significant differences in sleep quality between the PTSD and comorbid PTSD+mTBI groups. Moreover, there was no significant difference in sleep quality between veterans with mTBI and veterans without a history of PTSD and mTBI.

Table 2.
Sleep quality group comparisons.
3.2. PTSD, mTBI, and Sleep Quality
The regression analyses revealed a significant association between PTSD symptom severity and poorer global sleep quality in the total sample (β = 0.58, t = 9.15, p < 0.001), whereas there was no significant association between mTBI burden and global sleep quality (β = 0.07, t = 1.07, p = 0.288). Post-hoc analyses demonstrated that in the PTSD, mTBI, and comorbid PTSD+mTBI groups, more severe PTSD symptoms were associated with poorer global sleep quality. Moreover, in the PTSD and comorbid PTSD+mTBI groups, more severe PTSD symptoms were associated with poorer perceived sleep quality and more daily disturbances. In the mTBI group, more severe PTSD symptoms were associated with lower sleep efficiency (Table S2).
3.3. Sleep Quality and WM Microstructure
The regression analyses investigating the association between sleep quality and WM microstructure showed a significant negative association between the PSQI global score and whole-brain FAT in the total sample (β = −0.24, t = −3.35, p = 0.001). Post-hoc analyses revealed a significant association between global sleep quality and whole-brain FAT in the comorbid PTSD+mTBI group (β = −0.39, t = −4.04, f2 = 0.18, p < 0.001). Supplementary analyses of the main WM fiber tracts similarly showed significant associations between global sleep quality and WM FAT in the comorbid PTSD+mTBI group (Table S3). No region-specific pattern was observed, supporting our hypothesis that poor sleep quality may lead to widespread WM alterations. We subsequently assessed the association between the three PSQI sub-scales (sleep efficiency, perceived sleep quality, and daily disturbances) and whole-brain FAT in the comorbid PTSD+mTBI group. Only perceived sleep quality was significantly associated with whole-brain FAT (β = −0.43, t = −3.86, f2 = 0.21, p < 0.001, Table S4, Figure 2).
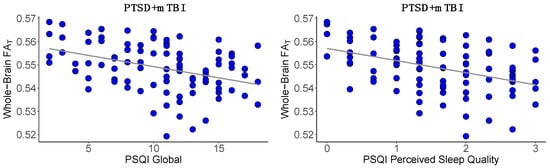
Figure 2.
Association between sleep quality and whole-brain FAT. Note. PSQI, Pittsburgh Sleep Quality Index []; PTSD, post-traumatic stress disorder; mTBI, mild traumatic brain injury; FAT, fractional anisotropy tissue. This figure illustrates the significant negative association between global sleep quality and whole-brain FAT (p < 0.001) and between perceived sleep quality and whole-brain FAT (p < 0.001). Lower scores on the PSQI scales represent better sleep quality.
3.4. Sleep Quality Mediates the Association between PTSD Symptom Severity and WM Microstructure
Given the significant association between PTSD symptom severity and perceived sleep quality and between perceived sleep quality and WM microstructure in the comorbid PTSD+mTBI group, we performed additional mediation analyses to assess whether perceived sleep quality mediates the association between PTSD symptom severity and whole-brain FAT. When not including sleep in our model we observed an effect of PTSD symptom severity on whole-brain FAT (b = −0.00, SE = 0.00, t(91) = −2.88, p = 0.005, Figure 3 path c). When including perceived sleep quality as a mediator, the relationships between PTSD symptom severity and perceived sleep quality (b = 0.02, SE = 0.00, t(91) = 5.55, p < 0.001, Figure 3 path a), perceived sleep quality and whole-brain FAT (b = −0.00, SE = 0.00, t(90) = −3.26, p = 0.002, Figure 3 path b), and the model’s total effect (F(3, 90) = 6.81, R2 = 0.19, p < 0.001) were significant. However, the direct effect of PTSD symptom severity on whole-brain FAT was not statistically significant (b = −0.00, SE = 0.00, t(90) = −0.97, p = 0.331, Figure 3 path c’). The findings indicate that the association between PTSD symptom severity and whole-brain FAT is statistically mediated by perceived sleep quality. When the mediation model included psychiatric comorbidities (anxiety, depression, and substance use disorder), warzone-related stress, BMI, psychiatric medication use, race, and education as additional covariates, results did not change significantly.
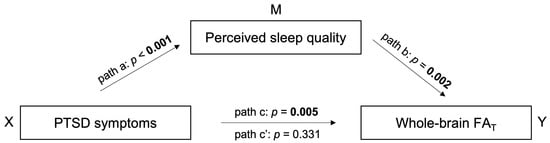
Figure 3.
Mediation model. Note. PTSD, post-traumatic stress disorder; mTBI, mild traumatic brain injury; FAT, fractional anisotropy tissue. This figure illustrates the mediating effect of perceived sleep quality between PTSD symptom severity and whole-brain FAT. Path a refers to the association between X and M. Path b refers to the association between M and Y when taking X into account. Path c represents the total effect of X on Y, including the axb path. Path c’ shows the direct effect of X on Y when M is omitted.
4. Discussion
The current study investigated relationships between PTSD, mTBI, sleep quality, and WM microstructure in veterans. We observed impaired sleep quality in veterans with PTSD and comorbid PTSD+mTBI compared to those with mTBI only or those without a history of PTSD or mTBI. Additionally, global and perceived sleep quality measures were associated with characteristics of WM microstructure in veterans with comorbid PTSD+mTBI. Most importantly, our findings suggest that perceived sleep quality may explain the association between PTSD symptom severity and WM microstructure in veterans with comorbid PTSD+mTBI. Thus, our findings indicate that sleep plays a central role in how psychological trauma affects brain health.
4.1. Group Differences in Sleep Quality
In line with previous investigations [,], we found that individuals with PTSD or comorbid PTSD+mTBI experience poorer global sleep quality, sleep efficiency, perceived sleep quality, and more daily disturbances than individuals with mTBI only or no history of PTSD or mTBI. Contrary to earlier studies [,], we did not see a difference in sleep quality between veterans with mTBI and those without a history of PTSD or mTBI. Given that some of the participating veterans may have sustained their head trauma years ago, an explanation for this finding could be that sleep quality disturbances related to mTBI improved over time. Indeed, only a minority of individuals who sustain mTBI experience ongoing post-concussive symptoms (including sleep quality disturbances) [,,]. On the contrary, recurrent sleep quality disturbances are still prevalent in individuals with remitted PTSD [,]. Therefore, PTSD appears to be an index of poor sleep quality, even without comorbid mTBI.
4.2. PTSD, mTBI, and Sleep Quality
We observed a significant association between greater PTSD symptom severity and worse global sleep quality, sleep efficiency, perceived sleep quality, and daily disturbances in veterans with PTSD, mTBI, and comorbid PTSD+mTBI. Interestingly, there was no significant association between mTBI burden and sleep quality, suggesting that the psychological consequences after a traumatic experience (rather than the physical trauma) are most predictive of sleep quality disturbances. These results highlight an integral role of poor sleep quality in PTSD severity [,], underscoring that traumatic experiences might be the driving force behind sleep quality disturbances in veterans [,].
4.3. Sleep Quality and WM Microstructure
As hypothesized [,,,,], we showed a significant relationship between impaired sleep quality and characteristics of the WM microstructure. We speculate that the observed WM microstructure alterations might be due to impaired myelin repair processes. Previous research demonstrates that sleep initiates myelin deposition and repair [] and is necessary for maintaining WM health. Myelin genesis and repair depend on the sufficient clearance of brain waste products []. The brain’s waste clearance system relies on the glymphatic system which consists of perivascular spaces vital for flushing out accumulated neurotoxins, such as beta-amyloid and tau [,]. Critically, the glymphatic system is most active during sleep []. Thus, we hypothesize that poor sleep quality, as observed in this study, may be related to impaired clearance of neurotoxins, which, in turn, may lead to neurodegenerative processes, including impaired myelination. This hypothesis is supported by the fact that amyloid and tau deposition have previously been linked to WM damage in veterans with comorbid PTSD+mTBI [,].
Notably, the association between impaired sleep quality and abnormal WM microstructure pertained solely to veterans with comorbid PTSD+mTBI. This finding may be ascribed to a statistical power effect as veterans with comorbid PTSD+mTBI made up the largest group. However, even though sleep quality disturbances were not statistically different between the comorbid PTSD+mTBI and PTSD groups, veterans with comorbid PTSD+mTBI presented as the most severely clinically burdened group, as indicated by the high number of comorbid psychiatric diagnoses, medication use, and the highest rates of military mTBI. Previous studies suggest that psychiatric disorders, medication use, and mTBI may increase brain vulnerability [,,,], potentially creating a neural environment that leaves the brain unprotected from the harmful effects of impaired sleep quality. Similarly, poor sleep quality negatively impacts brain structure and function, thus fueling the onset or progression of neuropsychiatric disorders and related brain abnormalities [].
When assessing different aspects of sleep quality (sleep efficiency, perceived sleep quality, and daily disturbances), lower perceived sleep quality was the only significant indicator of alterations in WM microstructure. This finding aligns well with a previous study, reporting an association between overall sleep quality and cortical GM volume that was driven by perceived sleep quality []. Additionally, perceived sleep quality has been shown to be essential for functional outcomes and mental well-being in individuals with PTSD []. Of particular interest is that perceived sleep quality may not correlate with objectively measured sleep quality. Indeed, the phenomenon of paradoxical insomnia—the discrepancy between subjective and objective assessments of sleep []—is a common observation among veterans with sleep disorders [] and PTSD []. Paradoxical insomnia is associated with general distress, ongoing hyperarousal states, and a negative cognitive bias that affects sleep perception [,,,,,]. Importantly, however, perceived sleep quality (rather than the objective assessment of sleep) appears to be reflective of overall mental well-being [,,,].
4.4. Sleep Quality Mediates the Association between PTSD Symptom Severity and WM Microstructure
We observed a relationship between more severe PTSD symptoms and greater WM abnormalities in the comorbid PTSD+mTBI group, which aligns well with several previous studies [,]. Strikingly, when including PTSD symptom severity, perceived sleep quality, and WM in the same statistical model, we found that perceived sleep quality accounted for the relationship between PTSD symptom severity and WM microstructure in veterans with comorbid PTSD+mTBI. This result suggests that poor sleep might be the most impactful symptom in the context of brain structure in individuals with comorbid PTSD+mTBI.
Future research is needed to elucidate the bidirectional interplay between sleep impairments and PTSD symptom severity. It is noteworthy that current first-line treatments for PTSD commonly fail to resolve sleep issues completely, even when other PTSD symptoms remit []. Persistent sleep quality disturbances are, in turn, a risk factor for PTSD [], resulting in adverse bi-directionally reinforcing conditions []. Thus, interventions that reduce disturbed sleep quality may simultaneously improve overall PTSD symptom severity [], given that restorative sleep is needed for fear extinction [,] and facilitates the emotional processing of traumatic events []. Targeting sleep disturbances is often a necessary first step when beginning trauma therapy to support emotional coping mechanisms and cognitive resources needed for a successful outcome []. Sleep-targeted interventions may yield higher acceptance and compliance, as they are less stigmatized than mental health therapies and may encourage more veterans to seek help if needed. Finally, specific training targeted at establishing and maintaining a healthy sleep routine even before deployment may be beneficial in fostering resiliency in veterans.
4.5. Limitations and Future Directions
We acknowledge several study limitations. First, our findings are limited to a male sample of veterans. They may, thus, not be generalizable to the general population of veterans, including women, given that sleep and WM structure may be affected by sex [,]. Second, the unequal sample sizes across groups may have affected statistical power and type I error rates, warranting replications utilizing balanced designs and larger samples. As highlighted above, the comorbid PTSD+mTBI group is the largest group, which might partially drive our findings. However, it is also critical to note that individuals with PTSD+mTBI were the most severely affected by psychiatric symptoms and that our results align with previous studies, suggesting that this group is specifically vulnerable. Third, mTBI diagnosis was based on retrospective self-recall of head injuries without available medical records for verification, potentially distorting reports of mTBI occurrence and severity. Similarly, sleep quality was assessed through self-report only and may not accurately reflect objective sleep quality. Future studies may benefit from employing trained clinicians to diagnose sleep disorders and include objective sleep measures, such as polysomnography, to record sleep quality complaints. Nevertheless, and as discussed above, subjective sleep quality serves as a valuable diagnostic tool indicative of mental and brain health. Furthermore, while we controlled for many potentially confounding variables, such as age, psychiatric comorbidities (anxiety, depression, and substance use disorder), warzone-related stress, BMI, psychiatric medication use, race, and education, we were unable to include other potentially relevant variables, such as caffeine or other stimulant use, exercise, cumulative sleep deficit, previous shift work, or socioeconomic status. Last, while the mediation analysis allowed for an advanced statistical assessment of complex interactions between the studied variables, the cross-sectional design restricts the interpretability of causal relationships. It is probable that some veterans experienced sleep quality disturbances even before deployment and were, thus, more likely to develop neuropsychiatric symptoms and exhibit structural brain alterations [,,,,]. In summary, future longitudinal studies are needed to elucidate the underlying pathomechanism of perceived sleep quality and investigate its relationship with objective sleep quality and brain structure in veterans with PTSD and mTBI.
5. Conclusions
Findings from this study suggest that perceived sleep quality plays a vital role in mental and brain health in veterans. Importantly, our findings suggest that disturbed sleep quality may account for the relationship between PTSD symptom severity and WM microstructure alterations, which we speculate to result from impaired myelin repair processes, given that healthy sleep is required for lipid production and the proliferation of oligodendrocyte precursors, which are essential for myelin genesis and deposition. Furthermore, poor sleep has been linked to inadequate brain waste clearance through the perivascular glymphatic system, and accumulated neurotoxins may trigger neurodegenerative processes, including demyelination. Notably, our study reports a link between white matter alterations and perceived sleep quality. While self-reported sleep quality is a strong indicator of mental well-being, it may not necessarily mirror objectively assessed sleep quality. Future research may benefit from employing both self-reports and device-assessed sleep ratings to gain further insights into sleep disturbances in relation to PTSD and mTBI. Moreover, future research is needed to investigate whether sleep-targeted interventions may benefit overall brain health in the veteran population.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm12052079/s1, Figure S1: Excluded participants and final sample sizes; Figure S2: Assessment of sleep quality; Figure S3: Overlap of diagnoses; Figure S4: Sleep quality group comparisons; Table S1: Sample characteristics: Group comparisons; Table S2: Association between PTSD symptom severity and sleep quality; Table S3: Association between sleep quality and white matter FAT; Table S4: Association between sleep quality and whole-brain FAT.
Author Contributions
Conceptualization, P.R., J.S.-H., M.E.S. and I.K.K.; methodology, P.R. and J.S.-H.; software, F.Z., Y.R., S.B., O.P. and L.J.O.; formal analysis, P.R. and J.S.-H.; investigation, P.R. and J.S.-H.; resources, M.E.S., I.K.K., W.P.M. and R.E.M.; data curation, P.R., E.K., V.J.S., L.F.U. and J.P.G.; writing—original draft preparation, P.R., writing—review and editing, P.R., J.S.-H., E.K., V.J.S., C.L.K., L.F.U., T.L.T.W., J.P.G., F.Z., Y.R., S.B., O.P., C.B.F., D.S., S.R.H., F.H., L.J.O., W.P.M., R.E.M., M.E.S. and I.K.K.; visualization, P.R., J.S.-H., C.L.K. and T.L.T.W.; supervision, M.E.S. and I.K.K.; project administration, C.B.F., D.S., W.P.M. and R.E.M.; funding acquisition, M.E.S., I.K.K., W.P.M., R.E.M. and P.R. All authors have read and agreed to the published version of the manuscript.
Funding
The current research was supported by the Translational Research Center for TBI and Stress Disorders (TRACTS) via a VA Rehabilitation Research and Development National Network Research Center for Traumatic Brain Injury Grant (B3001-C) to R.E.M., VA Merit Award (I01RX000928-01A2) to M.E.S., National Institute of Neurological Disorders and Stroke (NINDS) Awards (R01NS100952) and (R01NS115957) to I.K.K., and a National Institutes of Health Neuroimage Analysis Center grant (NIH P41EB015902) to O.P. We further acknowledge support from the Harvard Medical School Livingston Fellowship Award (J.S.-H.), the BBRF Young investigator grant (J.S.-H., funded by Mary and John Osterhaus and the Brain & Behavior Research Foundation), the Evangelische Studienwerk Villigst (P.R.), and the German Society for Clinical Neurophysiology and Functional Imaging (DGKN) Fellowship (E.K.). The present work is part of the PhD dissertation of P.R.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of the VA Boston Healthcare System (protocol code 2817 and 4/7/2014).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study is available on request from the corresponding author.
Acknowledgments
The authors express special gratitude to the service members participating in this study and the whole TRACTS team for data collection and management.
Conflicts of Interest
E. Kaufmann received speaker honoraria and financial compensation for travel expenses from Medtronic, UCB, Livanova, and Eisai and has participated in clinical trials for Medtronic, UCB and Precisis, all unrelated to the submitted work. Her research is supported by the Medical Clinical Scientist Program (MCSP). Koerte is a professor at Ludwig-Maximilians-Universität Munich (paid position). She serves as European Editor at Journal of Neurotrauma (unpaid position) and as Vice President of the European Neurotrauma Organization (unpaid position). She receives research grant funding from the National Institutes of Health, the European Research Council, the German Ministry for Research and Education. She receives funding for a research study on sport-related concussion from Abbott Inc. The Ludwig-Maximilians-University hospital received donations for her research from the Schatt Foundation and from Mary Ann Liebert Inc. She receives royalties for book chapters published by Thieme Publishers. Her spouse is employee at Siemens and she thus holds stock options at Siemens and Siemens Healthineers. Koerte’s in-kind contributions: PhD students working under her supervision receive scholarships from the Villigst Foundation, the China Scholarship Council collaboration with Ludwig-Maximilians-University Munich, and Fulbright. The other authors disclose no financial or other biomedical interests or potential conflicts of interest.
References
- Fulton, J.J.; Calhoun, P.S.; Wagner, H.R.; Schry, A.R.; Hair, L.P.; Feeling, N.; Elbogen, E.; Beckham, J.C. The Prevalence of Posttraumatic Stress Disorder in Operation Enduring Freedom/Operation Iraqi FreDevelopment of a Clinician-Administered edom (OEF/OIF) Veterans: A Meta-Analysis. J. Anxiety Disord. 2015, 31, 98–107. [Google Scholar] [CrossRef] [PubMed]
- Trivedi, R.B.; Post, E.P.; Sun, H.; Pomerantz, A.; Saxon, A.J.; Piette, J.D.; Maynard, C.; Arnow, B.; Curtis, I.; Fihn, S.D.; et al. Prevalence, Comorbidity, and Prognosis of Mental Health among US Veterans. Am. J. Public Health 2015, 105, 2564–2569. [Google Scholar] [CrossRef] [PubMed]
- Schneiderman, A.I.; Braver, E.R.; Kang, H.K. Understanding Sequelae of Injury Mechanisms and Mild Traumatic Brain Injury Incurred during the Conflicts in Iraq and Afghanistan: Persistent Postconcussive Symptoms and Posttraumatic Stress Disorder. Am. J. Epidemiol. 2008, 167, 1446–1452. [Google Scholar] [CrossRef] [PubMed]
- Lindquist, L.K.; Love, H.C.; Elbogen, E.B. Traumatic Brain Injury in Iraq and Afghanistan Veterans: New Results from a National Random Sample Study. J. Neuropsychiatry Clin. Neurosci. 2017, 29, 254–259. [Google Scholar] [CrossRef]
- Combs, H.L.; Berry, D.T.R.; Pape, T.; Babcock-Parziale, J.; Smith, B.; Schleenbaker, R.; Shandera-Ochsner, A.; Harp, J.P.; High, W.M. The Effects of Mild Traumatic Brain Injury, Post-Traumatic Stress Disorder, and Combined Mild Traumatic Brain Injury/Post-Traumatic Stress Disorder on Returning Veterans. J. Neurotrauma 2015, 32, 956–966. [Google Scholar] [CrossRef]
- Vasterling, J.J.; Aslan, M.; Lee, L.O.; Proctor, S.P.; Ko, J.; Jacob, S.; Concato, J. Longitudinal Associations among Posttraumatic Stress Disorder Symptoms, Traumatic Brain Injury, and Neurocognitive Functioning in Army Soldiers Deployed to the Iraq War. J. Int. Neuropsychol. Soc. 2018, 24, 311–323. [Google Scholar] [CrossRef]
- Lagarde, E.; Salmi, L.-R.; Holm, L.W.; Contrand, B.; Masson, F.; Ribéreau-Gayon, R.; Laborey, M.; Cassidy, J.D. Association of Symptoms Following Mild Traumatic Brain Injury with Posttraumatic Stress Disorder vs. Postconcussion Syndrome. JAMA Psychiatry 2014, 71, 1032–1040. [Google Scholar] [CrossRef]
- Seelig, A.D.; Jacobson, I.G.; Smith, B.; Hooper, T.I.; Boyko, E.J.; Gackstetter, G.D.; Gehrman, P.; Macera, C.A.; Smith, T.C. Sleep Patterns before, during, and after Deployment to Iraq and Afghanistan. Sleep 2010, 33, 1615–1622. [Google Scholar] [CrossRef]
- Germain, A. Sleep Disturbances as the Hallmark of PTSD: Where Are We Now? Am. J. Psychiatry 2013, 170, 372–382. [Google Scholar] [CrossRef]
- Khazaie, H. Sleep Disturbances in Veterans with Chronic War-Induced PTSD. J. Inj. Violence Res. 2016, 8, 99–107. [Google Scholar] [CrossRef]
- Grima, N.; Ponsford, J.; Rajaratnam, S.M.; Mansfield, D.; Pase, M.P. Sleep Disturbances in Traumatic Brain Injury: A Meta-Analysis. J. Clin. Sleep Med. 2016, 12, 419–428. [Google Scholar] [CrossRef] [PubMed]
- Mathias, J.L.; Alvaro, P.K. Prevalence of Sleep Disturbances, Disorders, and Problems Following Traumatic Brain Injury: A Meta-Analysis. Sleep Med. 2012, 13, 898–905. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, K.S.; Kark, S.M.; Gehrman, P.; Bogdanova, Y. Sleep Disturbances, TBI and PTSD: Implications for Treatment and Recovery. Clin. Psychol. Rev. 2015, 40, 195–212. [Google Scholar] [CrossRef] [PubMed]
- Maher, M.J.; Rego, S.A.; Asnis, G.M. Sleep Disturbances in Patients with Post-Traumatic Stress Disorder: Epidemiology, Impact and Approaches to Management. CNS Drugs 2006, 20, 567–590. [Google Scholar] [CrossRef]
- Lavie, P.; Hefez, A.; Halperin, G.; Enoch, D. Long-Term Effects of Traumatic War-Related Events on Sleep. Am. J. Psychiatry 1979, 136, 175–178. [Google Scholar] [CrossRef]
- McCarthy, E.; DeViva, J.C.; Norman, S.B.; Southwick, S.M.; Pietrzak, R.H. Self-Assessed Sleep Quality Partially Mediates the Relationship between PTSD Symptoms and Functioning and Quality of Life in U.S. Veterans: Results from the National Health and Resilience in Veterans Study. Psychol. Trauma Theory Res. Pract. Policy 2019, 11, 869–876. [Google Scholar] [CrossRef]
- Colvonen, P.J.; Ellison, J.; Haller, M.; Norman, S.B. Examining Insomnia and PTSD over Time in Veterans in Residential Treatment for Substance Use Disorders and PTSD. Behav. Sleep Med. 2019, 17, 524–535. [Google Scholar] [CrossRef]
- Spoormaker, V.I.; Montgomery, P. Disturbed Sleep in Post-Traumatic Stress Disorder: Secondary Symptom or Core Feature? Sleep Med. Rev. 2008, 12, 169–184. [Google Scholar] [CrossRef]
- Eugene, A.R.; Masiak, J. The Neuroprotective Aspects of Sleep. MEDtube Sci. 2015, 3, 35–40. [Google Scholar]
- De Vivo, L.; Bellesi, M. The Role of Sleep and Wakefulness in Myelin Plasticity. Glia 2019, 67, 2142–2152. [Google Scholar] [CrossRef]
- Babu Henry Samuel, I.; Pollin, K.U.; Breneman, C.B. Lower Cortical Volume Is Associated with Poor Sleep Quality after Traumatic Brain Injury. Brain Imaging Behav. 2022, 16, 1362–1371. [Google Scholar] [CrossRef] [PubMed]
- Chao, L.L.; Mohlenhoff, B.S.; Weiner, M.W.; Neylan, T.C. Associations between Subjective Sleep Quality and Brain Volume in Gulf War Veterans. Sleep 2014, 37, 445–452. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Cornelissen-Guillaume, G.G.; He, J.; Kastin, A.J.; Harrison, L.M.; Pan, W. Circadian Rhythm of Autophagy Proteins in Hippocampus Is Blunted by Sleep Fragmentation. Chronobiol. Int. 2016, 33, 553–560. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.C.; Gillin, J.C.; Buchsbaum, M.S.; Hershey, T.; Hazlett, E.; Sicotte, N.; Bunney, W.E. The Effect of Sleep Deprivation on Cerebral Glucose Metabolic Rate in Normal Humans Assessed with Positron Emission Tomography. Sleep 1991, 14, 155–162. [Google Scholar] [CrossRef]
- Shenton, M.E.; Hamoda, H.M.; Schneiderman, J.S.; Bouix, S.; Pasternak, O.; Rathi, Y.; Vu, M.-A.; Purohit, M.P.; Helmer, K.; Koerte, I.; et al. A Review of Magnetic Resonance Imaging and Diffusion Tensor Imaging Findings in Mild Traumatic Brain Injury. Brain Imaging Behav. 2012, 6, 137–192. [Google Scholar] [CrossRef]
- Schuff, N.; Zhang, Y.; Zhan, W.; Lenoci, M.; Ching, C.; Boreta, L.; Mueller, S.G.; Wang, Z.; Marmar, C.R.; Weiner, M.W.; et al. Patterns of Altered Cortical Perfusion and Diminished Subcortical Integrity in Posttraumatic Stress Disorder: An MRI Study. Neuroimage 2011, 54, S62–S68. [Google Scholar] [CrossRef]
- Aschbacher, K.; Mellon, S.H.; Wolkowitz, O.M.; Henn-Haase, C.; Yehuda, R.; Flory, J.D.; Bierer, L.M.; Abu-Amara, D.; Marmar, C.R.; Mueller, S.G. Posttraumatic Stress Disorder, Symptoms, and White Matter Abnormalities among Combat-Exposed Veterans. Brain Imaging Behav. 2018, 12, 989–999. [Google Scholar] [CrossRef]
- Ju, Y.; Ou, W.; Su, J.; Averill, C.L.; Liu, J.; Wang, M.; Wang, Z.; Zhang, Y.; Liu, B.; Li, L.; et al. White Matter Microstructural Alterations in Posttraumatic Stress Disorder: An ROI and Whole-Brain Based Meta-Analysis. J. Affect. Disord. 2020, 266, 655–670. [Google Scholar] [CrossRef]
- O’Doherty, D.C.M.; Ryder, W.; Paquola, C.; Tickell, A.; Chan, C.; Hermens, D.F.; Bennett, M.R.; Lagopoulos, J. White Matter Integrity Alterations in Post-Traumatic Stress Disorder. Hum. Brain Mapp. 2018, 39, 1327–1338. [Google Scholar] [CrossRef]
- Siehl, S.; King, J.A.; Burgess, N.; Flor, H.; Nees, F. Structural White Matter Changes in Adults and Children with Posttraumatic Stress Disorder: A Systematic Review and Meta-Analysis. NeuroImage Clin. 2018, 19, 581–598. [Google Scholar] [CrossRef]
- Graziano, R.; Bruce, S.; Paul, R. The Corpus Callosum and PTSD Severity. J. Interpers. Violence 2021, 36, 7480–7494. [Google Scholar] [CrossRef]
- Olson, E.A.; Cui, J.; Fukunaga, R.; Nickerson, L.D.; Rauch, S.L.; Rosso, I.M. Disruption of White Matter Structural Integrity and Connectivity in Posttraumatic Stress Disorder: A TBSS and Tractography Study. Depress. Anxiety 2017, 34, 437–445. [Google Scholar] [CrossRef]
- Averill, C.L.; Averill, L.A.; Wrocklage, K.M.; Scott, J.C.; Akiki, T.J.; Schweinsburg, B.; Southwick, S.M.; Krystal, J.H.; Abdallah, C.G. Altered White Matter Diffusivity of the Cingulum Angular Bundle in Posttraumatic Stress Disorder. Complex Psychiatry 2018, 4, 75–82. [Google Scholar] [CrossRef]
- Koch, S.B.J.; Van Zuiden, M.; Nawijn, L.; Frijling, J.L.; Veltman, D.J.; Olff, M. Decreased Uncinate Fasciculus Tract Integrity in Male and Female Patients with PTSD: A Diffusion Tensor Imaging Study. J. Psychiatry Neurosci. 2017, 42, 331–342. [Google Scholar] [CrossRef]
- McCunn, P.; Richardson, J.D.; Jetly, R.; Dunkley, B. Diffusion Tensor Imaging Reveals White Matter Differences in Military Personnel Exposed to Trauma with and without Post-Traumatic Stress Disorder. Psychiatry Res. 2021, 298, 113797. [Google Scholar] [CrossRef]
- Dennis, E.L.; Disner, S.G.; Fani, N.; Salminen, L.E.; Logue, M.; Clarke, E.K.; Haswell, C.C.; Averill, C.L.; Baugh, L.A.; Bomyea, J.; et al. Altered White Matter Microstructural Organization in Posttraumatic Stress Disorder across 3047 Adults: Results from the PGC-ENIGMA PTSD Consortium. Mol. Psychiatry 2021, 26, 4315–4330. [Google Scholar] [CrossRef]
- Bierer, L.M.; Ivanov, I.; Carpenter, D.M.; Wong, E.W.; Golier, J.A.; Tang, C.Y.; Yehuda, R. White Matter Abnormalities in Gulf War Veterans with Posttraumatic Stress Disorder: A Pilot Study. Psychoneuroendocrinology 2015, 51, 567–576. [Google Scholar] [CrossRef]
- Sanjuan, P.M.; Thoma, R.; Claus, E.D.; Mays, N.; Caprihan, A. Reduced White Matter Integrity in the Cingulum and Anterior Corona Radiata in Posttraumatic Stress Disorder in Male Combat Veterans: A Diffusion Tensor Imaging Study. Psychiatry Res. Neuroimaging 2013, 214, 260–268. [Google Scholar] [CrossRef]
- Kennis, M.; van Rooij, S.J.H.; Tromp, D.P.M.; Fox, A.S.; Rademaker, A.R.; Kahn, R.S.; Kalin, N.H.; Geuze, E. Treatment Outcome-Related White Matter Differences in Veterans with Posttraumatic Stress Disorder. Neuropsychopharmacology 2015, 40, 2434–2442. [Google Scholar] [CrossRef]
- Hedges, D.W.; Thatcher, G.W.; Bennett, P.J.; Sood, S.; Paulson, D.; Creem-Regehr, S.; Brown, B.L.; Allen, S.; Johnson, J.; Froelich, B.; et al. Brain Integrity and Cerebral Atrophy in Vietnam Combat Veterans with and without Posttraumatic Stress Disorder. Neurocase 2007, 13, 402–410. [Google Scholar] [CrossRef]
- Daniels, J.K.; Lamke, J.P.; Gaebler, M.; Walter, H.; Scheel, M. White Matter Integrity and Its Relationship to PTSD and Childhood Trauma—A Systematic Review and Meta-Analysis. Depress. Anxiety 2013, 30, 207–216. [Google Scholar] [CrossRef]
- Abe, O.; Yamasue, H.; Kasai, K.; Yamada, H.; Aoki, S.; Iwanami, A.; Ohtani, T.; Masutani, Y.; Kato, N.; Ohtomo, K. Voxel-Based Diffusion Tensor Analysis Reveals Aberrant Anterior Cingulum Integrity in Posttraumatic Stress Disorder Due to Terrorism. Psychiatry Res. Neuroimaging 2006, 146, 231–242. [Google Scholar] [CrossRef] [PubMed]
- Harnett, N.G.; Goodman, A.M.; Knight, D.C. PTSD-Related Neuroimaging Abnormalities in Brain Function, Structure, and Biochemistry. Exp. Neurol. 2020, 330, 113331. [Google Scholar] [CrossRef] [PubMed]
- Dailey, N.S.; Smith, R.; Bajaj, S.; Alkozei, A.; Gottschlich, M.K.; Raikes, A.C.; Satterfield, B.C.; Killgore, W.D.S. Elevated Aggression and Reduced White Matter Integrity in Mild Traumatic Brain Injury: A DTI Study. Front. Behav. Neurosci. 2018, 12, 118. [Google Scholar] [CrossRef]
- Nakayama, N.; Okumura, A.; Shinoda, J.; Yasokawa, Y.-T.; Miwa, K.; Yoshimura, S.-I. Evidence for White Matter Disruption in Traumatic Brain Injury without Macroscopic Lesions. J. Neurol. Neurosurg. Psychiatry 2006, 77, 850–855. [Google Scholar] [CrossRef]
- Petrie, E.C.; Cross, D.J.; Yarnykh, V.L.; Richards, T.; Martin, N.M.; Pagulayan, K.; Hoff, D.; Hart, K.; Mayer, C.; Tarabochia, M.; et al. Neuroimaging, Behavioral, and Psychological Sequelae of Repetitive Combined Blast/Impact Mild Traumatic Brain Injury in Iraq and Afghanistan War Veterans. J. Neurotrauma 2014, 31, 425–436. [Google Scholar] [CrossRef]
- Rutgers, D.R.; Fillard, P.; Paradot, G.; Tadié, M.; Lasjaunias, P.; Ducreux, D. Diffusion Tensor Imaging Characteristics of the Corpus Callosum in Mild, Moderate, and Severe Traumatic Brain Injury. Am. J. Neuroradiol. 2008, 29, 1730–1735. [Google Scholar] [CrossRef]
- Mu, W.; Catenaccio, E.; Lipton, M.L. Neuroimaging in Blast-Related Mild Traumatic Brain Injury. J. Head Trauma Rehabil. 2017, 32, 55–69. [Google Scholar] [CrossRef]
- Wallace, E.J.; Mathias, J.L.; Ward, L. Diffusion Tensor Imaging Changes Following Mild, Moderate and Severe Adult Traumatic Brain Injury: A Meta-Analysis. Brain Imaging Behav. 2018, 12, 1607–1621. [Google Scholar] [CrossRef]
- Xiong, K.; Zhu, Y.; Zhang, Y.; Yin, Z.; Zhang, J.; Qiu, M.; Zhang, W. White Matter Integrity and Cognition in Mild Traumatic Brain Injury Following Motor Vehicle Accident. Brain Res. 2014, 1591, 86–92. [Google Scholar] [CrossRef]
- Davenport, N.D.; Lamberty, G.J.; Nelson, N.W.; Lim, K.O.; Armstrong, M.T.; Sponheim, S.R. PTSD Confounds Detection of Compromised Cerebral White Matter Integrity in Military Veterans Reporting a History of Mild Traumatic Brain Injury. Brain Inj. 2016, 30, 1491–1500. [Google Scholar] [CrossRef]
- Lepage, C.; Pasternak, O.; Bouix, S.; Shenton, M.E.; Zafonte, R.D.; Coleman, M.J.; McAllister, T.W.; Flashman, L.A.; George, M.S.; Morey, R.A.; et al. White Matter Abnormalities in Mild Traumatic Brain Injury with and without Post-Traumatic Stress Disorder: A Subject-Specific Diffusion Tensor Imaging Study. Brain Imaging Behav. 2017, 12, 870–881. [Google Scholar] [CrossRef] [PubMed]
- Santhanam, P.; Teslovich, T.; Wilson, S.H.; Yeh, P.-H.; Oakes, T.R.; Weaver, L.K. Decreases in White Matter Integrity of Ventro-Limbic Pathway Linked to Post-Traumatic Stress Disorder in Mild Traumatic Brain Injury. J. Neurotrauma 2019, 36, 1093–1098. [Google Scholar] [CrossRef]
- Lopez, K.C.; Leary, J.B.; Pham, D.L.; Chou, Y.-Y.; Dsurney, J.; Chan, L. Brain Volume, Connectivity, and Neuropsychological Performance in Mild Traumatic Brain Injury: The Impact of Post-Traumatic Stress Disorder Symptoms. J. Neurotrauma 2017, 34, 16–22. [Google Scholar] [CrossRef]
- Bresser, T.; Foster-Dingley, J.C.; Wassing, R.; Leerssen, J.; Ramautar, J.R.; Stoffers, D.; Lakbila-Kamal, O.; van den Heuvel, M.; van Someren, E.J.W. Consistent Altered Internal Capsule White Matter Microstructure in Insomnia Disorder. Sleep 2020, 43, zsaa031. [Google Scholar] [CrossRef]
- Sexton, C.E.; Zsoldos, E.; Filippini, N.; Griffanti, L.; Winkler, A.; Mahmood, A.; Allan, C.L.; Topiwala, A.; Kyle, S.D.; Spiegelhalder, K.; et al. Associations between Self-Reported Sleep Quality and White Matter in Community-Dwelling Older Adults: A Prospective Cohort Study. Hum. Brain Mapp. 2017, 38, 5465–5473. [Google Scholar] [CrossRef]
- Khalsa, S.; Hale, J.R.; Goldstone, A.; Wilson, R.S.; Mayhew, S.D.; Bagary, M.; Bagshaw, A.P. Habitual Sleep Durations and Subjective Sleep Quality Predict White Matter Differences in the Human Brain. Neurobiol. Sleep Circadian Rhythm. 2017, 3, 17–25. [Google Scholar] [CrossRef]
- Spiegelhalder, K.; Regen, W.; Prem, M.; Baglioni, C.; Nissen, C.; Feige, B.; Schnell, S.; Kiselev, V.G.; Hennig, J.; Riemann, D. Reduced Anterior Internal Capsule White Matter Integrity in Primary Insomnia. Hum. Brain Mapp. 2014, 35, 3431–3438. [Google Scholar] [CrossRef]
- Li, S.; Tian, J.; Bauer, A.; Huang, R.; Wen, H.; Li, M.; Wang, T.; Xia, L.; Jiang, G. Reduced Integrity of Right Lateralized White Matter in Patients with Primary Insomnia: A Diffusion-Tensor Imaging Study. Radiology 2016, 280, 520–528. [Google Scholar] [CrossRef]
- Kang, J.M.; Joo, S.W.; Son, Y.D.; Kim, H.; Ko, K.P.; Lee, J.S.; Kang, S.G. Low White-Matter Integrity between the Left Thalamus and Inferior Frontal Gyrus in Patients with Insomnia Disorder. J. Psychiatry Neurosci. 2018, 43, 366–374. [Google Scholar] [CrossRef]
- Cai, W.; Zhao, M.; Liu, J.; Liu, B.; Yu, D.; Yuan, K. Right Arcuate Fasciculus and Superior Longitudinal Fasciculus Abnormalities in Primary Insomnia. Brain Imaging Behav. 2019, 13, 1746–1755. [Google Scholar] [CrossRef]
- Kocevska, D.; Tiemeier, H.; Lysen, T.S.; de Groot, M.; Muetzel, R.L.; Van Someren, E.J.W.; Ikram, M.A.; Vernooij, M.W.; Luik, A.I. The Prospective Association of Objectively Measured Sleep and Cerebral White Matter Microstructure in Middle-Aged and Older Persons. Sleep 2019, 42, zsz140. [Google Scholar] [CrossRef]
- Lu, F.-M.; Dai, J.; Couto, T.A.; Liu, C.-H.; Chen, H.; Lu, S.-L.; Tang, L.-R.; Tie, C.-L.; Chen, H.-F.; He, M.-X.; et al. Diffusion Tensor Imaging Tractography Reveals Disrupted White Matter Structural Connectivity Network in Healthy Adults with Insomnia Symptoms. Front. Hum. Neurosci. 2017, 11, 583. [Google Scholar] [CrossRef]
- Grau-Rivera, O.; Operto, G.; Falcón, C.; Sánchez-Benavides, G.; Cacciaglia, R.; Brugulat-Serrat, A.; Gramunt, N.; Salvadó, G.; Suárez-Calvet, M.; Minguillon, C.; et al. Association between Insomnia and Cognitive Performance, Gray Matter Volume, and White Matter Microstructure in Cognitively Unimpaired Adults. Alzheimers Res. Ther. 2020, 12, 4. [Google Scholar] [CrossRef]
- Yaffe, K.; Nasrallah, I.; Hoang, T.D.; Lauderdale, D.S.; Knutson, K.L.; Carnethon, M.R.; Launer, L.J.; Lewis, C.E.; Sidney, S. Sleep Duration and White Matter Quality in Middle-Aged Adults. Sleep 2016, 39, 1743–1747. [Google Scholar] [CrossRef]
- Bottari, S.A.; Lamb, D.G.; Murphy, A.J.; Porges, E.C.; Rieke, J.D.; Harciarek, M.; Datta, S.; Williamson, J.B. Hyperarousal Symptoms and Decreased Right Hemispheric Frontolimbic White Matter Integrity Predict Poorer Sleep Quality in Combat-Exposed Veterans. Brain Inj. 2021, 35, 922–933. [Google Scholar] [CrossRef]
- Fakhran, S.; Yaeger, K.; Alhilali, L. Symptomatic White Matter Changes in Mild Traumatic Brain Injury Resemble Pathologic Features of Early Alzheimer Dementia. Radiology 2013, 269, 249–257. [Google Scholar] [CrossRef]
- Raikes, A.C.; Bajaj, S.; Dailey, N.S.; Smith, R.S.; Alkozei, A.; Satterfield, B.C.; Killgore, W.D.S. Diffusion Tensor Imaging (DTI) Correlates of Self-Reported Sleep Quality and Depression Following Mild Traumatic Brain Injury. Front. Neurol. 2018, 9, 468. [Google Scholar] [CrossRef]
- DeGutis, J.; Chiu, C.; Thai, M.; Esterman, M.; Milberg, W.; McGlinchey, R. Trauma Sequelae Are Uniquely Associated with Components of Self-Reported Sleep Dysfunction in OEF/OIF/OND Veterans. Behav. Sleep Med. 2018, 16, 38–63. [Google Scholar] [CrossRef]
- McGlinchey, R.E.; Milberg, W.P.; Fonda, J.R.; Fortier, C.B. A Methodology for Assessing Deployment Trauma and Its Consequences in OEF/OIF/OND Veterans: The TRACTS Longitudinal Prospective Cohort Study. Int. J. Methods Psychiatr. Res. 2017, 26, e1556. [Google Scholar] [CrossRef]
- Kinzel, P.; Marx, C.E.; Sollmann, N.; Hartl, E.; Guenette, J.P.; Kaufmann, D.; Bouix, S.; Pasternak, O.; Rathi, Y.; Coleman, M.J.; et al. Serum Neurosteroid Levels Are Associated With Cortical Thickness in Individuals Diagnosed with Posttraumatic Stress Disorder and History of Mild Traumatic Brain Injury. Clin. EEG Neurosci. 2020, 51, 285–299. [Google Scholar] [CrossRef] [PubMed]
- Lindemer, E.R.; Salat, D.H.; Leritz, E.C.; McGlinchey, R.E.; Milberg, W.P. Reduced Cortical Thickness with Increased Lifetime Burden of PTSD in OEF/OIF Veterans and the Impact of Comorbid TBI. NeuroImage Clin. 2013, 2, 601–611. [Google Scholar] [CrossRef] [PubMed]
- Blake, D.D.; Weathers, F.W.; Nagy, L.M.; Kaloupek, D.G.; Gusman, F.D.; Charney, D.S.; Keane, T.M. The Development of a Clinician-Administered PTSD Scale. J. Trauma. Stress 1995, 8, 75–90. [Google Scholar] [CrossRef] [PubMed]
- Weathers, F.W.; Bovin, M.J.; Lee, D.J.; Sloan, D.M.; Schnurr, P.P.; Kaloupek, D.G.; Keane, T.M.; Marx, B.P. The Clinician-Administered PTSD Scale for DSM–5 (CAPS-5): Development and Initial Psychometric Evaluation in Military Veterans. Psychol. Assess. 2018, 30, 383–395. [Google Scholar] [CrossRef]
- Fortier, C.B.; Amick, M.M.; Grande, L.; McGlynn, S.; Kenna, A.; Morra, L.; Clark, A.; Milberg, W.P.; McGlinchey, R.E. The Boston Assessment of Traumatic Brain Injury–Lifetime (BAT-L) Semistructured Interview: Evidence of Research Utility and Validity. J. Head Trauma Rehabil. 2014, 29, 89–98. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A New Instrument for Psychiatric Practice and Research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Cole, J.C.; Motivala, S.J.; Buysse, D.J.; Oxman, M.N.; Levin, M.J.; Irwin, M.R. Validation of a 3-Factor Scoring Model for the Pittsburgh Sleep Quality Index in Older Adults. Sleep 2006, 29, 112–116. [Google Scholar] [CrossRef] [PubMed]
- First, M.B.; Gibbon, M.; Spitzer, R.L.; Williams, J.B.W. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I); American Psychiatric Press: Washington, DC, USA, 1997. [Google Scholar]
- Vogt, D.S.; Smith, B.N.; King, L.A.; King, D.W.; Knight, J.A.; Vasterling, J.J. Deployment Risk and Resilience Inventory-2 (DRRI-2): An Updated Tool for Assessing Psychosocial Risk and Resilience Factors among Service Members and Veterans. J. Trauma. Stress 2013, 26, 710–717. [Google Scholar] [CrossRef]
- Greve, D.N.; Fischl, B. Accurate and Robust Brain Image Alignment Using Boundary-Based Registration. Neuroimage 2009, 48, 63–72. [Google Scholar] [CrossRef]
- Jenkinson, M.; Bannister, P.; Brady, M.; Smith, S. Improved Optimization for the Robust and Accurate Linear Registration and Motion Correction of Brain Images. Neuroimage 2002, 17, 825–841. [Google Scholar] [CrossRef]
- Fedorov, A.; Beichel, R.; Kalpathy-Cramer, J.; Finet, J.; Fillion-Robin, J.-C.; Pujol, S.; Bauer, C.; Jennings, D.; Fennessy, F.; Sonka, M.; et al. 3D Slicer as an Image Computing Platform for the Quantitative Imaging Network. Magn. Reson. Imaging 2012, 30, 1323–1341. [Google Scholar] [CrossRef]
- Zhang, F.; Noh, T.; Juvekar, P.; Frisken, S.F.; Rigolo, L.; Norton, I.; Kapur, T.; Pujol, S.; Wells, W.; Yarmarkovich, A.; et al. SlicerDMRI: Diffusion MRI and Tractography Research Software for Brain Cancer Surgery Planning and Visualization. JCO Clin. Cancer Inform. 2020, 299–309. [Google Scholar] [CrossRef]
- Norton, I.; Essayed, W.I.; Zhang, F.; Pujol, S.; Yarmarkovich, A.; Golby, A.J.; Kindlmann, G.; Wasserman, D.; Estepar, R.S.J.; Rathi, Y.; et al. SlicerDMRI: Open Source Diffusion MRI Software for Brain Cancer Research. Cancer Res. 2017, 77, e101–e103. [Google Scholar] [CrossRef]
- Levitt, J.J.; Zhang, F.; Vangel, M.; Nestor, P.G.; Rathi, Y.; Kubicki, M.; Shenton, M.E.; O’Donnell, L.J. The Organization of Frontostriatal Brain Wiring in Healthy Subjects Using a Novel Diffusion Imaging Fiber Cluster Analysis. Cereb. Cortex 2021, 31, 5308–5318. [Google Scholar] [CrossRef]
- Kochsiek, J.; O’Donnell, L.J.; Zhang, F.; Bonke, E.M.; Sollmann, N.; Tripodis, Y.; Wiegand, T.L.T.; Kaufmann, D.; Umminger, L.; Di Biase, M.A.; et al. Exposure to Repetitive Head Impacts Is Associated with Corpus Callosum Microstructure and Plasma Total Tau in Former Professional American Football Players. J. Magn. Reson. Imaging 2021, 54, 1819–1829. [Google Scholar] [CrossRef]
- Irimia, A.; Fan, D.; Chaudhari, N.N.; Ngo, V.; Zhang, F.; Joshi, S.H.; O’Donnell, L.J. Mapping Cerebral Connectivity Changes after Mild Traumatic Brain Injury in Older Adults Using Diffusion Tensor Imaging and Riemannian Matching of Elastic Curves. In Proceedings of the 2020 IEEE 17th International Symposium on Biomedical Imaging (ISBI), Iowa City, IA, USA, 3–7 April 2020; IEEE: Piscataway, NJ, USA, 2020; pp. 1690–1693. [Google Scholar]
- Gong, S.; Zhang, F.; Norton, I.; Essayed, W.I.; Unadkat, P.; Rigolo, L.; Pasternak, O.; Rathi, Y.; Hou, L.; Golby, A.J.; et al. Free Water Modeling of Peritumoral Edema Using Multi-Fiber Tractography: Application to Tracking the Arcuate Fasciculus for Neurosurgical Planning. PLoS ONE 2018, 13, e197056. [Google Scholar] [CrossRef]
- Zekelman, L.R.; Zhang, F.; Makris, N.; He, J.; Chen, Y.; Xue, T.; Liera, D.; Drane, D.L.; Rathi, Y.; Golby, A.J.; et al. White Matter Association Tracts Underlying Language and Theory of Mind: An Investigation of 809 Brains from the Human Connectome Project. Neuroimage 2022, 246, 118739. [Google Scholar] [CrossRef]
- Robles, D.J.; Dharani, A.; Rostowsky, K.A.; Chaudhari, N.N.; Ngo, V.; Zhang, F.; O’Donnell, L.J.; Green, L.; Sheikh-Bahaei, N.; Chui, H.C.; et al. Older Age, Male Sex, and Cerebral Microbleeds Predict White Matter Loss after Traumatic Brain Injury. GeroScience 2022, 44, 83–102. [Google Scholar] [CrossRef]
- Zhang, F.; Karayumak, S.C.; Pieper, S.; O’Donnell, L.J. Consistent White Matter Parcellation in Adolescent Brain Cognitive Development (ABCD). In Proceedings of the Annual Meeting of the International Society for Magnetic Resonance in Medicine (ISMRM), London, UK, 7–12 May 2022; ISMRM: Concord, CA, USA, 2022. [Google Scholar]
- He, H.; Zhang, F.; Pieper, S.; Makris, N.; Rathi, Y.; Wells, W.; O’Donnell, L.J. Model and Predict Age and Sex in Healthy Subjects Using Brain White Matter Features: A Deep Learning Approach. In Proceedings of the 2022 IEEE 19th International Symposium on Biomedical Imaging (ISBI), Kolkata, India, 28–31 March 2022. [Google Scholar] [CrossRef]
- Wang, J.; Zhang, F.; Zhao, C.; Zeng, Q.; He, J.; O’Donnell, L.J.; Feng, Y. Investigation of Local White Matter Abnormality in Parkinson’s Disease by Using an Automatic Fiber Tract Parcellation. Behav. Brain Res. 2020, 394, 112805. [Google Scholar] [CrossRef]
- Sydnor, V.J.; Rivas-Grajales, A.M.; Lyall, A.E.; Zhang, F.; Bouix, S.; Karmacharya, S.; Shenton, M.E.; Westin, C.-F.; Makris, N.; Wassermann, D.; et al. A Comparison of Three Fiber Tract Delineation Methods and Their Impact on White Matter Analysis. Neuroimage 2018, 178, 318–331. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Wu, Y.; Norton, I.; Rathi, Y.; Golby, A.J.; O’Donnell, L.J. Test–Retest Reproducibility of White Matter Parcellation Using Diffusion MRI Tractography Fiber Clustering. Hum. Brain Mapp. 2019, 40, 3041–3057. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, L.J.; Suter, Y.; Rigolo, L.; Kahali, P.; Zhang, F.; Norton, I.; Albi, A.; Olubiyi, O.; Meola, A.; Essayed, W.I.; et al. Automated White Matter Fiber Tract Identification in Patients with Brain Tumors. NeuroImage Clin. 2017, 13, 138–153. [Google Scholar] [CrossRef]
- Lienhard, S.; Malcolm, J.G.; Westin, C.-F.; Rathi, Y. A Full Bi-Tensor Neural Tractography Algorithm Using the Unscented Kalman Filter. EURASIP J. Adv. Signal Process. 2011, 2011, 77. [Google Scholar] [CrossRef]
- Malcolm, J.G.; Shenton, M.E.; Rathi, Y. Filtered Multitensor Tractography. IEEE Trans. Med. Imaging 2010, 29, 1664–1675. [Google Scholar] [CrossRef] [PubMed]
- Vos, S.B.; Viergever, M.A.; Leemans, A. Multi-Fiber Tractography Visualizations for Diffusion MRI Data. PLoS ONE 2013, 8, e81453. [Google Scholar] [CrossRef] [PubMed]
- Farquharson, S.; Tournier, J.-D.; Calamante, F.; Fabinyi, G.; Schneider-Kolsky, M.; Jackson, G.D.; Connelly, A. White Matter Fiber Tractography: Why We Need to Move beyond DTI. J. Neurosurg. 2013, 118, 1367–1377. [Google Scholar] [CrossRef]
- Zhang, F.; Wu, Y.; Norton, I.; Rigolo, L.; Rathi, Y.; Makris, N.; O’Donnell, L.J. An Anatomically Curated Fiber Clustering White Matter Atlas for Consistent White Matter Tract Parcellation across the Lifespan. Neuroimage 2018, 179, 429–447. [Google Scholar] [CrossRef]
- Baumgartner, C.; Michailovich, O.; Levitt, J.; Pasternak, O.; Bouix, S.; Westin, C.-F.; Rathi, Y. A Unified Tractography Framework for Comparing Diffusion Models on Clinical Scans. In Proceedings of the International Conference on Medical Image Computing and Computer Assisted Intervention (MICCAI’12)—Computational Diffusion MRI Workshop, Nice, France, 1–5 October 2012; pp. 27–32. [Google Scholar]
- Chen, Z.; Tie, Y.; Olubiyi, O.; Rigolo, L.; Mehrtash, A.; Norton, I.; Pasternak, O.; Rathi, Y.; Golby, A.J.; O’Donnell, L.J. Reconstruction of the Arcuate Fasciculus for Surgical Planning in the Setting of Peritumoral Edema Using Two-Tensor Unscented Kalman Filter Tractography. NeuroImage Clin. 2015, 7, 815–822. [Google Scholar] [CrossRef]
- Liao, R.; Ning, L.; Chen, Z.; Rigolo, L.; Gong, S.; Pasternak, O.; Golby, A.J.; Rathi, Y.; O’Donnell, L.J. Performance of Unscented Kalman Filter Tractography in Edema: Analysis of the Two-Tensor Model. NeuroImage Clin. 2017, 15, 819–831. [Google Scholar] [CrossRef]
- O’Donnell, L.J.; Wells, W.M.; Golby, A.J.; Westin, C.-F. Unbiased Groupwise Registration of White Matter Tractography. Med. Image Comput. Comput. Assist. Interv. 2012, 15, 123–130. [Google Scholar] [CrossRef]
- O’Donnell, L.J.; Westin, C.F. Automatic Tractography Segmentation Using a High-Dimensional White Matter Atlas. IEEE Trans. Med. Imaging 2007, 26, 1562–1575. [Google Scholar] [CrossRef] [PubMed]
- Maier-Hein, K.H.; Neher, P.F.; Houde, J.-C.; Côté, M.-A.; Garyfallidis, E.; Zhong, J.; Chamberland, M.; Yeh, F.-C.; Lin, Y.-C.; Ji, Q.; et al. The Challenge of Mapping the Human Connectome Based on Diffusion Tractography. Nat. Commun. 2017, 8, 1349. [Google Scholar] [CrossRef] [PubMed]
- Xue, T.; Zhang, F.; Zhang, C.; Chen, Y.; Song, Y.; Makris, N.; Rathi, Y.; Cai, W.; O’Donnell, L.J. Supwma: Consistent and Efficient Tractography Parcellation of Superficial White Matter with Deep Learning. In Proceedings of the 2022 IEEE 19th International Symposium on Biomedical Imaging (ISBI), Kolkata, India, 28–31 March 2022; IEEE: New York, NY, USA; pp. 1–5. [Google Scholar]
- Steinmann, S.; Lyall, A.E.; Langhein, M.; Nägele, F.L.; Rauh, J.; Cetin-Karayumak, S.; Zhang, F.; Mussmann, M.; Billah, T.; Makris, N.; et al. Sex-Related Differences in White Matter Asymmetry and Its Implications for Verbal Working Memory in Psychosis High-Risk State. Front. Psychiatry 2021, 12, 686967. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Cetin Karayumak, S.; Hoffmann, N.; Rathi, Y.; Golby, A.J.; O’Donnell, L.J. Deep White Matter Analysis (DeepWMA): Fast and Consistent Tractography Segmentation. Med. Image Anal. 2020, 65, 101761. [Google Scholar] [CrossRef]
- Hong, Y.; O’Donnell, L.J.; Savadjiev, P.; Zhang, F.; Wassermann, D.; Pasternak, O.; Johnson, H.; Paulsen, J.; Vonsattel, J.P.; Makris, N.; et al. Genetic Load Determines Atrophy in Hand Cortico-Striatal Pathways in Presymptomatic Huntington’s Disease. Hum. Brain Mapp. 2018, 39, 3871–3883. [Google Scholar] [CrossRef]
- Pasternak, O.; Sochen, N.; Gur, Y.; Intrator, N.; Assaf, Y. Free Water Elimination and Mapping from Diffusion MRI. Magn. Reson. Med. 2009, 62, 717–730. [Google Scholar] [CrossRef]
- Metzler-Baddeley, C.; O’Sullivan, M.J.; Bells, S.; Pasternak, O.; Jones, D.K. How and How Not to Correct for CSF-Contamination in Diffusion MRI. Neuroimage 2012, 59, 1394–1403. [Google Scholar] [CrossRef] [PubMed]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis—A Regression-Based Approach; Guilford Press: New York, NY, USA, 2013. [Google Scholar]
- Isaac, L.; Main, K.L.; Soman, S.; Gotlib, I.H.; Furst, A.J.; Kinoshita, L.M.; Fairchild, J.K.; Yesavage, J.A.; Ashford, J.W.; Bayley, P.J.; et al. The Impact of Depression on Veterans with PTSD and Traumatic Brain Injury: A Diffusion Tensor Imaging Study. Biol. Psychol. 2015, 105, 20–28. [Google Scholar] [CrossRef]
- Espinoza Oyarce, D.A.; Shaw, M.E.; Alateeq, K.; Cherbuin, N. Volumetric Brain Differences in Clinical Depression in Association with Anxiety: A Systematic Review with Meta-Analysis. J. Psychiatry Neurosci. 2020, 45, 406–429. [Google Scholar] [CrossRef]
- Davey, D.K.; Jurick, S.M.; Crocker, L.D.; Hoffman, S.N.; Sanderson-Cimino, M.; Tate, D.F.; Velez, C.S.; Delano-Wood, L.; Jak, A.J. White Matter Integrity, Suicidal Ideation, and Cognitive Dysfunction in Combat-Exposed Iraq and Afghanistan Veterans. Psychiatry Res. Neuroimaging 2021, 317, 111389. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.F.; Peng, W.; Sweeney, J.A.; Jia, Z.Y.; Gong, Q.Y. Brain Structure Alterations in Depression: Psychoradiological Evidence. CNS Neurosci. Ther. 2018, 24, 994–1003. [Google Scholar] [CrossRef] [PubMed]
- Van Velzen, L.S.; Kelly, S.; Isaev, D.; Aleman, A.; Aftanas, L.I.; Bauer, J.; Baune, B.T.; Brak, I.V.; Carballedo, A.; Connolly, C.G.; et al. White Matter Disturbances in Major Depressive Disorder: A Coordinated Analysis across 20 International Cohorts in the ENIGMA MDD Working Group. Mol. Psychiatry 2020, 25, 1511–1525. [Google Scholar] [CrossRef]
- Lee, K.S.; Lee, S.H. White Matter-Based Structural Brain Network of Anxiety. Adv. Exp. Med. Biol. 2020, 1191, 61–70. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Zhong, Y.; Ma, Z.; Lu, X.; Zhang, N.; Fox, P.T.; Wang, C. Gray Matter Changes in Panic Disorder: A Voxel-Based Meta-Analysis and Meta-Analytic Connectivity Modeling. Psychiatry Res. Neuroimaging 2018, 282, 82–89. [Google Scholar] [CrossRef]
- Harrewijn, A.; Cardinale, E.M.; Groenewold, N.A.; Bas-Hoogendam, J.M.; Aghajani, M.; Hilbert, K.; Cardoner, N.; Porta-Casteràs, D.; Gosnell, S.; Salas, R.; et al. Cortical and Subcortical Brain Structure in Generalized Anxiety Disorder: Findings from 28 Research Sites in the ENIGMA-Anxiety Working Group. Transl. Psychiatry 2021, 11, 502. [Google Scholar] [CrossRef]
- Pando-Naude, V.; Toxto, S.; Fernandez-Lozano, S.; Parsons, C.E.; Alcauter, S.; Garza-Villarreal, E.A. Gray and White Matter Morphology in Substance Use Disorders: A Neuroimaging Systematic Review and Meta-Analysis. Transl. Psychiatry 2021, 11, 29. [Google Scholar] [CrossRef]
- Navarri, X.; Afzali, M.H.; Lavoie, J.; Sinha, R.; Stein, D.J.; Momenan, R.; Veltman, D.J.; Korucuoglu, O.; Sjoerds, Z.; van Holst, R.J.; et al. How Do Substance Use Disorders Compare to Other Psychiatric Conditions on Structural Brain Abnormalities? A Cross-Disorder Meta-Analytic Comparison Using the ENIGMA Consortium Findings. Hum. Brain Mapp. 2022, 43, 399–413. [Google Scholar] [CrossRef]
- Kuo, J.R.; Kaloupek, D.G.; Woodward, S.H. Amygdala Volume in Combat-Exposed Veterans with and without Posttraumatic Stress Disorder: A Cross-Sectional Study. Arch. Gen. Psychiatry 2012, 69, 1080–1086. [Google Scholar] [CrossRef]
- Aupperle, R.L.; Connolly, C.G.; Stillman, A.N.; May, A.C.; Paulus, M.P. Deployment and Post-Deployment Experiences in OEF/OIF Veterans: Relationship to Gray Matter Volume. PLoS ONE 2013, 8, e75880. [Google Scholar] [CrossRef]
- Clausen, A.N.; Billinger, S.A.; Sisante, J.-F.V.; Suzuki, H.; Aupperle, R.L. Preliminary Evidence for the Impact of Combat Experiences on Gray Matter Volume of the Posterior Insula. Front. Psychol. 2017, 8, 2151. [Google Scholar] [CrossRef] [PubMed]
- Butler, O.; Adolf, J.; Gleich, T.; Willmund, G.; Zimmermann, P.; Lindenberger, U.; Gallinat, J.; Kühn, S. Military Deployment Correlates with Smaller Prefrontal Gray Matter Volume and Psychological Symptoms in a Subclinical Population. Transl. Psychiatry 2017, 7, e1031. [Google Scholar] [CrossRef] [PubMed]
- McWhinney, S.R.; Abé, C.; Alda, M.; Benedetti, F.; Bøen, E.; del Mar Bonnin, C.; Borgers, T.; Brosch, K.; Canales-Rodríguez, E.J.; Cannon, D.M.; et al. Association between Body Mass Index and Subcortical Brain Volumes in Bipolar Disorders–ENIGMA Study in 2735 Individuals. Mol. Psychiatry 2021, 26, 6806–6819. [Google Scholar] [CrossRef] [PubMed]
- Medic, N.; Ziauddeen, H.; Ersche, K.D.; Farooqi, I.S.; Bullmore, E.T.; Nathan, P.J.; Ronan, L.; Fletcher, P.C. Increased Body Mass Index Is Associated with Specific Regional Alterations in Brain Structure. Int. J. Obes. 2016, 40, 1177–1182. [Google Scholar] [CrossRef]
- Steegers, C.; Blok, E.; Lamballais, S.; Jaddoe, V.; Bernardoni, F.; Vernooij, M.; van der Ende, J.; Hillegers, M.; Micali, N.; Ehrlich, S.; et al. The Association between Body Mass Index and Brain Morphology in Children: A Population-Based Study. Brain Struct. Funct. 2021, 226, 787–800. [Google Scholar] [CrossRef]
- Bolzenius, J.D.; Laidlaw, D.H.; Cabeen, R.P.; Conturo, T.E.; McMichael, A.R.; Lane, E.M.; Heaps, J.M.; Salminen, L.E.; Baker, L.M.; Scott, S.E.; et al. Brain Structure and Cognitive Correlates of Body Mass Index in Healthy Older Adults. Behav. Brain Res. 2015, 278, 342–347. [Google Scholar] [CrossRef]
- Gunstad, J.; Paul, R.H.; Cohen, R.A.; Tate, D.F.; Spitznagel, M.B.; Grieve, S.; Gordon, E. Relationship between Body Mass Index and Brain Volume in Healthy Adults. Int. J. Neurosci. 2008, 118, 1582–1593. [Google Scholar] [CrossRef]
- Alosco, M.L.; Stanek, K.M.; Galioto, R.; Korgaonkar, M.S.; Grieve, S.M.; Brickman, A.M.; Spitznagel, M.B.; Gunstad, J. Body Mass Index and Brain Structure in Healthy Children and Adolescents. Int. J. Neurosci. 2014, 124, 49–55. [Google Scholar] [CrossRef]
- Thomaes, K.; Dorrepaal, E.; Draijer, N.; Jansma, E.P.; Veltman, D.J.; van Balkom, A.J. Can Pharmacological and Psychological Treatment Change Brain Structure and Function in PTSD? A Systematic Review. J. Psychiatr. Res. 2014, 50, 1–15. [Google Scholar] [CrossRef]
- Scherk, H.; Falkai, P. Changes in Brain Structure Caused by Neuroleptic Medication. Nervenarzt 2004, 75, 1112–1117. [Google Scholar] [CrossRef]
- Seiger, R.; Gryglewski, G.; Klöbl, M.; Kautzky, A.; Godbersen, G.M.; Rischka, L.; Vanicek, T.; Hienert, M.; Unterholzner, J.; Silberbauer, L.R.; et al. The Influence of Acute SSRI Administration on White Matter Microstructure in Patients Suffering from Major Depressive Disorder and Healthy Controls. Int. J. Neuropsychopharmacol. 2021, 24, 542–550. [Google Scholar] [CrossRef] [PubMed]
- Dusi, N.; Barlati, S.; Vita, A.; Brambilla, P. Brain Structural Effects of Antidepressant Treatment in Major Depression. Curr. Neuropharmacol. 2015, 13, 458–465. [Google Scholar] [CrossRef] [PubMed]
- Vieira, R.; Coelho, A.; Reis, J.; Portugal-Nunes, C.; Magalhães, R.; Ferreira, S.; Moreira, P.S.; Sousa, N.; Bessa, J.M. White Matter Microstructure Alterations Associated with Paroxetine Treatment Response in Major Depression. Front. Behav. Neurosci. 2021, 15, 693109. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Xu, X.; Luo, Q.; Luo, Y.; Chen, Y.; Lui, S.; Wu, M.; Zhu, H.; Kemp, G.J.; Gong, Q. Brain Grey Matter Volume Alterations Associated with Antidepressant Response in Major Depressive Disorder. Sci. Rep. 2017, 7, 10464. [Google Scholar] [CrossRef]
- Fani, N.; Harnett, N.G.; Bradley, B.; Mekawi, Y.; Powers, A.; Stevens, J.S.; Ressler, K.J.; Carter, S.E. Racial Discrimination and White Matter Microstructure in Trauma-Exposed Black Women. Biol. Psychiatry 2022, 91, 254–261. [Google Scholar] [CrossRef]
- Noble, K.G.; Korgaonkar, M.S.; Grieve, S.M.; Brickman, A.M. Higher Education Is an Age-Independent Predictor of White Matter Integrity and Cognitive Control in Late Adolescence. Dev. Sci. 2013, 16, 653–664. [Google Scholar] [CrossRef]
- Tummala, S.; Roy, B.; Park, B.; Kang, D.W.; Woo, M.A.; Harper, R.M.; Kumar, R. Associations between Brain White Matter Integrity and Disease Severity in Obstructive Sleep Apnea. J. Neurosci. Res. 2016, 94, 915–923. [Google Scholar] [CrossRef]
- Balba, N.M.; Elliott, J.E.; Weymann, K.B.; Opel, R.A.; Duke, J.W.; Oken, B.S.; Morasco, B.J.; Heinricher, M.M.; Lim, M.M. Increased Sleep Disturbances and Pain in Veterans with Comorbid Traumatic Brain Injury and Posttraumatic Stress Disorder. J. Clin. Sleep Med. 2018, 14, 1865–1878. [Google Scholar] [CrossRef]
- Martindale, S.L.; Farrell-Carnahan, L.V.; Ulmer, C.S.; Kimbrel, N.A.; McDonald, S.D.; Rowland, J.A. Sleep Quality in Returning Veterans: The Influence of Mild Traumatic Brain Injury. Rehabil. Psychol. 2017, 62, 563–570. [Google Scholar] [CrossRef]
- Selassie, A.W.; Zaloshnja, E.; Langlois, J.A.; Miller, T.; Jones, P.; Steiner, C. Incidence of Long-Term Disability Following Traumatic Brain Injury Hospitalization, United States, 2003. J. Head Trauma Rehabil. 2008, 23, 123–131. [Google Scholar] [CrossRef]
- Cassidy, J.D.; Cancelliere, C.; Carroll, L.J.; Côté, P.; Hincapié, C.A.; Holm, L.W.; Hartvigsen, J.; Donovan, J.; Nygren-De Boussard, C.; Kristman, V.L.; et al. Systematic Review of Self-Reported Prognosis in Adults after Mild Traumatic Brain Injury: Results of the International Collaboration on Mild Traumatic Brain Injury Prognosis. Arch. Phys. Med. Rehabil. 2014, 95, 132–151. [Google Scholar] [CrossRef] [PubMed]
- Gonschorek, A.S.; Schwenkreis, P.; Guthke, T. Psychische Störungen Nach Leichtem Schädel-Hirn-Trauma. Nervenarzt 2016, 87, 567–579. [Google Scholar] [CrossRef] [PubMed]
- Martindale, S.L.; Konst, M.J.; Bateman, J.R.; Arena, A.; Rowland, J.A. The Role of PTSD and TBI in Post-Deployment Sleep Outcomes. Mil. Psychol. 2020, 32, 212–221. [Google Scholar] [CrossRef]
- Jessen, N.A.; Munk, A.S.F.; Lundgaard, I.; Nedergaard, M. The Glymphatic System: A Beginner’s Guide. Neurochem. Res. 2015, 40, 2583–2599. [Google Scholar] [CrossRef]
- Xie, L.; Kang, H.; Xu, Q.; Chen, M.J.; Liao, Y.; Thiyagarajan, M.; O’Donnell, J.; Christensen, D.J.; Nicholson, C.; Iliff, J.J.; et al. Sleep Drives Metabolite Clearance from the Adult Brain. Science 2013, 342, 373–377. [Google Scholar] [CrossRef]
- Piantino, J.; Schwartz, D.L.; Luther, M.; Newgard, C.; Silbert, L.; Raskind, M.; Pagulayan, K.; Kleinhans, N.; Iliff, J.; Peskind, E. Link between Mild Traumatic Brain Injury, Poor Sleep, and Magnetic Resonance Imaging: Visible Perivascular Spaces in Veterans. J. Neurotrauma 2021, 38, 2391–2399. [Google Scholar] [CrossRef]
- Mohamed, A.Z.; Cumming, P.; Nasrallah, F.A.; Department of Defense Alzheimer’s Disease Neuroimaging Initiative. White Matter Alterations Are Associated with Cognitive Dysfunction Decades after Moderate-to-Severe Traumatic Brain Injury and/or Posttraumatic Stress Disorder. Biol. Psychiatry Cogn. Neurosci. Neuroimaging 2021, 6, 1100–1109. [Google Scholar] [CrossRef]
- Wooten, D.W.; Ortiz-Terán, L.; Zubcevik, N.; Zhang, X.; Huang, C.; Sepulcre, J.; Atassi, N.; Johnson, K.A.; Zafonte, R.D.; El Fakhri, G. Multi-Modal Signatures of Tau Pathology, Neuronal Fiber Integrity, and Functional Connectivity in Traumatic Brain Injury. J. Neurotrauma 2019, 36, 3233–3243. [Google Scholar] [CrossRef]
- Santhanam, P.; Wilson, S.H.; Oakes, T.R.; Weaver, L.K. Effects of Mild Traumatic Brain Injury and Post-Traumatic Stress Disorder on Resting-State Default Mode Network Connectivity. Brain Res. 2019, 1711, 77–82. [Google Scholar] [CrossRef]
- Sydnor, V.J.; Bouix, S.; Pasternak, O.; Hartl, E.; Levin-Gleba, L.; Reid, B.; Tripodis, Y.; Guenette, J.P.; Kaufmann, D.; Makris, N.; et al. Mild Traumatic Brain Injury Impacts Associations between Limbic System Microstructure and Post-Traumatic Stress Disorder Symptomatology. NeuroImage Clin. 2020, 26, 102190. [Google Scholar] [CrossRef]
- Rezaie, L.; Fobian, A.D.; McCall, W.V.; Khazaie, H. Paradoxical Insomnia and Subjective–Objective Sleep Discrepancy: A Review. Sleep Med. Rev. 2018, 40, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Mysliwiec, V.; McGraw, L.; Pierce, R.; Smith, P.; Trapp, B.; Roth, B.J. Sleep Disorders and Associated Medical Comorbidities in Active Duty Military Personnel. Sleep 2013, 36, 167–174. [Google Scholar] [CrossRef] [PubMed]
- Ghadami, M.R.; Khaledi-Paveh, B.; Nasoori, M.; Khazaie, H. PTSD-Related Paradoxical Insomnia: An Actigraphic Study among Veterans with Chronic PTSD. J. Inj. Violence Res. 2015, 7, 54–58. [Google Scholar] [CrossRef] [PubMed]
- Werner, K.B.; Griffin, M.G.; Galovski, T.E. Objective and Subjective Measurement of Sleep Disturbance in Female Trauma Survivors with Posttraumatic Stress Disorder. Psychiatry Res. 2016, 240, 234–240. [Google Scholar] [CrossRef]
- Lewis, C.; Lewis, K.; Kitchiner, N.; Isaac, S.; Jones, I.; Bisson, J.I. Sleep Disturbance in Post-Traumatic Stress Disorder (PTSD): A Systematic Review and Meta-Analysis of Actigraphy Studies. Eur. J. Psychotraumatol. 2020, 11, 1767349. [Google Scholar] [CrossRef] [PubMed]
- Kram Mendelsohn, A.; Daffre, C.; Oliver, K.I.; Seo, J.; Lasko, N.B.; Pace-Schott, E.F. 1071 Subjective Measures of Hyperarousal Predict Subjective Longitudinal and Retrospective Measures of Sleep Quality in Individuals Exposed to Trauma. Sleep 2020, 43, A408. [Google Scholar] [CrossRef]
- Parrino, L.; Milioli, G.; De Paolis, F.; Grassi, A.; Terzano, M.G. Paradoxical Insomnia: The Role of CAP and Arousals in Sleep Misperception. Sleep Med. 2009, 10, 1139–1145. [Google Scholar] [CrossRef]
- Johnson, D.A.; Javaheri, S.; Guo, N.; Champion, C.L.; Sims, J.F.; Brock, M.P.; Sims, M.; Patel, S.R.; Williams, D.R.; Wilson, J.G.; et al. Objective Measures of Sleep Apnea and Actigraphy-Based Sleep Characteristics as Correlates of Subjective Sleep Quality in an Epidemiologic Study: The Jackson Heart Sleep Study. Psychosom. Med. 2020, 82, 324–330. [Google Scholar] [CrossRef]
- Moshkani Farahani, D.; Tavallaie, A.; Vahedi, E.; Rezaiemaram, P.; Naderi, Z.; Talaie, A. The Relationship between Perceived Sleep Quality, Polysomnographic Measures and Depressive Symptoms in Chemically-Injured Veterans: A Pilot Study. Iran. J. Psychiatry 2014, 9, 169–174. [Google Scholar]
- Strasshofer, D.R.; Pacella, M.L.; Irish, L.A.; Palmieri, P.A.; Johnson, D.M.; Delahanty, D.L. The Role of Perceived Sleep Quality in the Relationship between PTSD Symptoms and General Mental Health. Ment. Health Prev. 2017, 5, 27–32. [Google Scholar] [CrossRef]
- Fernandez-Mendoza, J.; Calhoun, S.L.; Bixler, E.O.; Karataraki, M.; Liao, D.; Vela-Bueno, A.; Jose Ramos-Platon, M.; Sauder, K.A.; Basta, M.; Vgontzas, A.N. Sleep Misperception and Chronic Insomnia in the General Population: Role of Objective Sleep Duration and Psychological Profiles. Psychosom. Med. 2011, 73, 88–97. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.E.; Campbell-Sills, L.; Kessler, R.C.; Sun, X.; Heeringa, S.G.; Nock, M.K.; Ursano, R.J.; Jain, S.; Stein, M.B. Pre-Deployment Insomnia Is Associated with Post-Deployment Post-Traumatic Stress Disorder and Suicidal Ideation in US Army Soldiers. Sleep 2019, 42, zsy229. [Google Scholar] [CrossRef]
- Pace-Schott, E.F.; Milad, M.R.; Orr, S.P.; Rauch, S.L.; Stickgold, R.; Pitman, R.K. Sleep Promotes Generalization of Extinction of Conditioned Fear. Sleep 2009, 32, 19–26. [Google Scholar] [CrossRef]
- Zuj, D.V.; Palmer, M.A.; Hsu, C.-M.K.; Nicholson, E.L.; Cushing, P.J.; Gray, K.E.; Felmingham, K.L. Impaired Fear Extinction Associated with PTSD Increased with Hours since Waking. Depress. Anxiety 2016, 33, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Walker, M.P.; van der Helm, E. Overnight Therapy? The Role of Sleep in Emotional Brain Processing. Psychol. Bull. 2009, 135, 731–748. [Google Scholar] [CrossRef] [PubMed]
- Merritt, V.C.; Jurick, S.M.; Crocker, L.D.; Sullan, M.J.; Sakamoto, M.S.; Davey, D.K.; Hoffman, S.N.; Keller, A.V.; Jak, A.J. Associations between Multiple Remote Mild TBIs and Objective Neuropsychological Functioning and Subjective Symptoms in Combat-Exposed Veterans. Arch. Clin. Neuropsychol. 2020, 35, 491–505. [Google Scholar] [CrossRef]
- Foster, S.N.; Hansen, S.L.; Capener, D.C.; Matsangas, P.; Mysliwiec, V. Gender Differences in Sleep Disorders in the US Military. Sleep Health 2017, 3, 336–341. [Google Scholar] [CrossRef]
- Seitz, J.; Cetin-Karayumak, S.; Lyall, A.; Pasternak, O.; Baxi, M.; Vangel, M.; Pearlson, G.; Tamminga, C.; Sweeney, J.; Clementz, B.; et al. Investigating Sexual Dimorphism of Human White Matter in a Harmonized, Multisite Diffusion Magnetic Resonance Imaging Study. Cereb. Cortex 2021, 31, 201–212. [Google Scholar] [CrossRef]
- Koffel, E.; Polusny, M.A.; Arbisi, P.A.; Erbes, C.R. Pre-Deployment Daytime and Nighttime Sleep Complaints as Predictors of Post-Deployment PTSD and Depression in National Guard Troops. J. Anxiety Disord. 2013, 27, 512–519. [Google Scholar] [CrossRef]
- Acheson, D.T.; Kwan, B.; Maihofer, A.X.; Risbrough, V.B.; Nievergelt, C.M.; Clark, J.W.; Tu, X.M.; Irwin, M.R.; Baker, D.G. Sleep Disturbance at Pre-Deployment Is a Significant Predictor of Post-Deployment Re-Experiencing Symptoms. Eur. J. Psychotraumatol. 2019, 10, 1679964. [Google Scholar] [CrossRef]
- Van Liempt, S.; Van Zuiden, M.; Westenberg, H.; Super, A.; Vermetten, E. Impact of Impaired Sleep on the Development of PTSD Symptoms in Combat Veterans: A Prospective Longitudinal Cohort Study. Depress. Anxiety 2013, 30, 469–474. [Google Scholar] [CrossRef] [PubMed]
- van den Heuvel, M.P.; Mandl, R.C.W.; Kahn, R.S.; Hulshoff Pol, H.E. Functionally Linked Resting-State Networks Reflect the Underlying Structural Connectivity Architecture of the Human Brain. Hum. Brain Mapp. 2009, 30, 3127–3141. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).