Abstract
Background: Investigating the health-related quality of life (HRQoL) after intensive care unit (ICU) discharge is necessary to identify possible modifiable risk factors. The primary aim of this study was to investigate the HRQoL in COVID-19 critically ill patients one year after ICU discharge. Methods: In this multicenter prospective observational study, COVID-19 patients admitted to nine ICUs from 1 March 2020 to 28 February 2021 in Italy were enrolled. One year after ICU discharge, patients were required to fill in short-form health survey 36 (SF-36) and impact of event-revised (IES-R) questionnaire. A multivariate linear or logistic regression analysis to search for factors associated with a lower HRQoL and post-traumatic stress disorded (PTSD) were carried out, respectively. Results: Among 1003 patients screened, 343 (median age 63 years [57–70]) were enrolled. Mechanical ventilation lasted for a median of 10 days [2–20]. Physical functioning (PF 85 [60–95]), physical role (PR 75 [0–100]), emotional role (RE 100 [33–100]), bodily pain (BP 77.5 [45–100]), social functioning (SF 75 [50–100]), general health (GH 55 [35–72]), vitality (VT 55 [40–70]), mental health (MH 68 [52–84]) and health change (HC 50 [25–75]) describe the SF-36 items. A median physical component summary (PCS) and mental component summary (MCS) scores were 45.9 (36.5–53.5) and 51.7 (48.8–54.3), respectively, considering 50 as the normal value of the healthy general population. In all, 109 patients (31.8%) tested positive for post-traumatic stress disorder, also reporting a significantly worse HRQoL in all SF-36 domains. The female gender, history of cardiovascular disease, liver disease and length of hospital stay negatively affected the HRQoL. Weight at follow-up was a risk factor for PTSD (OR 1.02, p = 0.03). Conclusions: The HRQoL in COVID-19 ARDS (C-ARDS) patients was reduced regarding the PCS, while the median MCS value was slightly above normal. Some risk factors for a lower HRQoL have been identified, the presence of PTSD is one of them. Further research is warranted to better identify the possible factors affecting the HRQoL in C-ARDS.
1. Introduction
Since the beginning of the pandemic, more than half a billion people worldwide have suffered from the novel coronavirus disease (COVID-19) [1].
Patients with severe acute hypoxemic respiratory failure have several risk factors for post-intensive care syndrome (PICS), including prolonged invasive mechanical ventilation, development of intensive care unit (ICU)-acquired weakness, steroids and neuromuscular blocking agent administration, which has been demonstrated to reduce the health-related quality of life (HRQoL) after ICU discharge [2,3,4].
Herridge et al. described a persistently reduced HRQoL that lasted several months to years in patients who suffered from acute respiratory distress syndrome (ARDS) [5]. Other studies confirmed their findings and further demonstrated that critically ill patients who survived ICU discharge presented persistent physical and mental impairment [6,7,8].
However, how the same factors affect COVID-19 ARDS (C-ARDS) patients is still poorly known. Limited resources during the first phase of the pandemic, coupled with ineffective treatments and insufficient evidence of C-ARDS management, may have led to increased mortality and worse recovery from critical COVID-19 illness [9].
Preliminary studies in C-ARDS patients at 3- and 6-month follow-up revealed an impaired HRQoL after ICU discharge [10,11]. Following this period, improvements in physical symptoms and performance have been reported in studies in a relatively small cohort of patients [12]. Thus, the quality of life in C-ARDS survivors at longer follow-up remains poorly investigated.
The primary aim of this study was to evaluate the HRQoL after 1 year of ICU discharge in COVID-19 survivors.
Secondary aims included identifying possible correlations between HRQoL 1 year after ICU discharge and the demographic, medical or clinical data (during hospitalization), screening for post-traumatic stress disorder (PTSD), detecting the risk factors and investigating whether PTSD has an impact on the HRQoL.
2. Materials and Methods
2.1. Study Setting and Design
A prospective multicenter observational study was conducted in nine Italian ICUs, eight academic and one nonacademic, after the Ethics Committee of Friuli Venezia Giulia Region (Udine, Italy), as the coordinating center (CEUR-2021-Os-99), approved the study.
Principal investigators for each location were responsible for obtaining the local ethics committees’ approval and patients’ consent to participate in the study. This was completed following hospital protocols and institutional regulations during the COVID-19 emergency. This study was prospectively registered at ClinicalTrials.gov number: NCT04860687 (registered on 27th April 2021). This work follows the STROBE checklist.
2.2. Patients’ Characteristics
The patients included in the study had a positive COVID-19 assay from either nasal or pharyngeal swabs or lower respiratory tract aspirates, and were admitted to ICU due to acute hypoxemic respiratory failure and survived the ICU stay.
Excluded patients who had known cognitive disorders (medical history positive for dementia, delirium or loss of memory previous to ICU admission), psychological disorders (depression, history of previous PTSD), advanced malignancies (under palliative care), end-stage organ disease at ICU admission (defined as patient requiring chronic hemodialysis, mechanical cardiocirculatory support, palliative care to resolve symptoms related to cardiac disease refractory to all available treatments, long-term oxygen therapy, on a waiting list for solid organ transplantation or with cirrhosis but excluded from liver transplantation) or did not require mechanical ventilatory support during their ICU stay.
2.3. Outcomes
The quality of life after ICU discharge was assessed with the short-form health survey-36 (SF-36), while PTSD was screened with the impact of event scale-revised (IES-R).
The SF-36 is a 36-item patient-reported questionnaire that evaluates the HRQoL. The SF-36 produces eight scaled scores that are the weighted sums of the questions in their section. Each scale is directly transformed into a 0–100 scale on the assumption that each question carries equal weight. The higher the score, the better the quality of life and vice versa.
The domains of the SF-36 are physical functioning (PF), which reflects the extent to which general health limits physical activity; physical role (PR), which expresses how physical health interferes with work or limits activity; bodily pain (BP), which analyzes the intensity of pain and the effect of pain on a patient’s ability to work; general health (GH), a patient’s own evaluation of his or her health or health outlook; vitality (VT), which includes the energy the patient has; social functioning (SF), a measure of how health or emotional problems interfere with social activities; emotional role (RE), an evaluation of the extent to which emotional problems interfere with work or activities; and mental health (MH), a global assessment of general mental health. The SF-36 can be filled in by the patient alone or with the help of relatives. Moreover, it can be administered by phone.
The eight SF-36 domains could be collapsed to create two global components: the physical component summary (PCS) and mental component summary (MCS), according to the method proposed by Ware et al. [13].
The PCS is principally derived from PF, PR and BP, while for the MCS, major determinants are MH, RE and SF. VT and GH are equally determinants of both summary scores. In practical, the PCS reflects the physical wellness, while MCS returns information on the global mental health condition.
They are constructed using a principal component analysis, based on the data of the general population of the US, standardized to obtain a mean of 50 and a standard deviation of 10.
The IES-R is a 22-item questionnaire that measures the subjective distress caused by traumatic events. It is a self-reported scale, with items rated on a 5-point Likert scale ranging from 0 to 4, with a minimum of 0 to a maximum total score of 88. There are also three subscale scores that define intrusion, avoidance and hyperarousal aspects of PTSD. Sum scores equal to or greater than 33 or a mean cutoff value equal to or greater than 1.75 for overall questions indicate the probable presence of PTSD, as described in Supplementary Material S1 [14].
2.4. Data Collection
Local investigators were responsible for screening and determining the patients’ inclusion, specifically considering a 1-year follow-up after ICU discharge. The same investigators also contacted patients to complete the self-reported short-form health survey-36 (SF-36) questionnaire to analyze the HRQoL and IES-R, as a screening tool for PTSD.
Patients were contacted by phone and asked to complete the questionnaires independently or with the help of a relative. Results were delivered either by mail or e-mail depending on individual’s preference. Patients who did not respond after three phone calls were considered unavailable and excluded from the study; those who agreed to participate but did not send the completed questionnaires, despite three reminders, were considered lost to follow-up.
The following demographic data were recorded: age, gender, weight at ICU admission and at follow-up, APACHE II score, lung injury score (LIS score) [15], level of education (lower education: <8 years of school [compulsory school], higher education >8 years of school [high school degree or college degree]), marital status (single, married, separated/divorced, widowed), and employment (jobless, active worker, retired), previous medical history of cardiac, pulmonary, kidney or liver disease, diabetes, time between hospital admission and ICU admission (days), length of ICU stay (LOSICU), length of hospital stay (LOSHOSP), and ward of destination after ICU discharge.
Clinical ICU data included the type of mechanical ventilation (noninvasive vs. invasive), use of steroids and neuromuscular blocking agents and their respective duration, need for renal replacement therapy, duration of mechanical ventilation and the eventual need for tracheostomy.
2.5. Statistical Analysis
Categorical variables were presented as absolute values (percentages) and continuous variables as medians and interquartile ranges [IQRs]. Normality was assessed using the Shapiro–Wilk test. Categorical variables were compared using the chi-square test or Fisher’s exact test, as appropriate. Univariable and multivariable linear regressions were performed to estimate the associations between the SF-36 domains, IES-R and the clinical/demographic variables by calculating β (linear regression coefficient) and 95% confidence intervals (CIs). Univariable and multivariable logistic regressions were performed to explore variables associated with the presence of PTSD by estimating the odds ratios (OR, 95% CI). Multivariable analyses included all significant variables, p < 0.05 from univariable analyses, and considered potential collinearities. Results were adjusted for each hospital center. No imputation was carried out for missing data. Statistical analyses were performed using STATA 17.
2.6. Sample Size
According to Herridge’s study, surviving ARDS patients showed a median PF of 60 (IQR 35–85) 1 year after ICU discharge [5]. Given this value, Wan’s method was used to obtain a mean value of 60 and standard deviation of 37 [16]. A convenience sample size of 340 patients produces a two-sided 95% confidence interval for this mean with a precision of 4%, an α level of 0.05. Physical functioning was chosen because this domain asks respondents to report limitations on 10 mobility activities, such as walking specified distances, carrying groceries, bathing or dressing. This fully reflects the extent to which general health, also in patients experiencing PICS, limits daily life physical activity, with a consequent impact on the HRQoL.
3. Results
In all, 1003 patients with C-ARDS were admitted to the nine participating ICUs from 1 March 2020 to 28 February 2021. The follow-up ended on 9 April 2022 given that the last patient included was discharged from ICU on 9 April 2021. The final statistical analysis included 343 patients who satisfied the inclusion and exclusion criteria, as shown in the study flow chart (Figure 1).
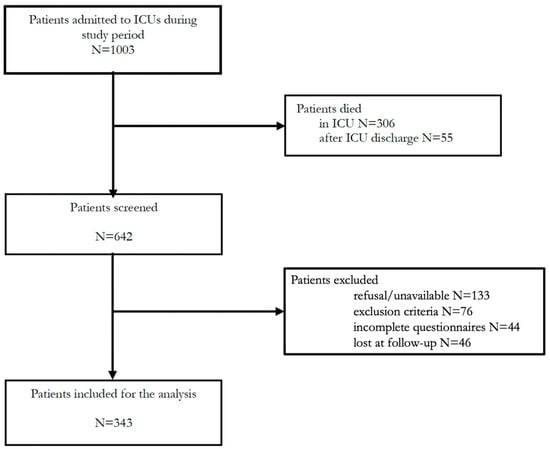
Figure 1.
Study flow chart.
The median age was 63 years. The majority of patients were men (79.3%). They required critical care admission in the absence of previously known pulmonary conditions. Approximately half of the patients had arterial hypertension (42.9%), and 14.2% had diabetes. At 6.1%, COPD was the most represented pulmonary comorbidity. In all, 54% of patients had a high level of education and 79.6% were married or cohabiting at the time of the study. In contrast, 58 (17%) patients lived alone. In all, 159 (46.3%) patients were active workers, and 45.5% were retired (Table 1).

Table 1.
Baseline patients’ characteristics.
Median APACHE II and LIS scores at ICU admission were, respectively, 11 [8–14] and 3 [2.3–3]. In all, 91% of patients required endotracheal intubation and invasive mechanical ventilation (MV) with a median duration of 10 days [2–20]. Neuromuscular blockers were administered to 111 (32.3%) patients for a median of 96 h [IQR 36–160]. In all, 194 (56.5%) patients received steroids for 10 days [7–13]. Some patients (6.7%) needed renal replacement therapy, while 87 (25.4%) were tracheostomized during their ICU stay. Median LOSICU was 13 days [IQR 6–25], and 26.5% of patients were discharged to a high dependency unit (HDU), 24% to pulmonology and 24.1% to a medical ward. Median LOSHOSP was 32 days [IQR 19–47] (Table 2).

Table 2.
Main hospital and ICU data.
The HRQoL at 1-year follow-up of C-ARDS patients is shown in Table 3.

Table 3.
HRQoL according to the SF-36 items and comparison between patients with and without PTSD.
The median physical component score and mental component score were 45.9 (36.5–53.5) and 51.7 (48.8–54.3), respectively, as shown in Figure 2.
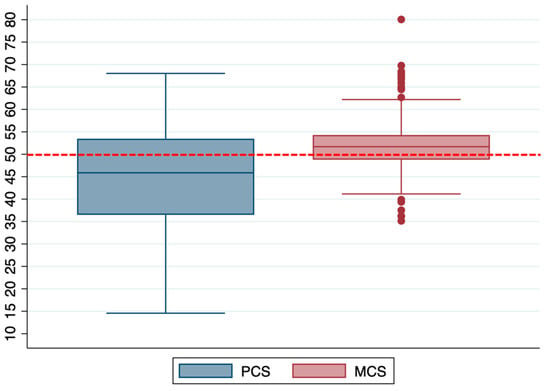
Figure 2.
Distribution of the PCS and MCS in the entire population. Box plot shows median and interquartile ranges, while whiskers represent the outliers. The red dotted line represents the value for the normal population.
In all, 109 (31.8%) tested positive for PTSD, as defined by a IES-R sum score ≥ 33. In this group, the median value for avoidance was 1.9 [IQR 1.1–2.3] and 2.4 [IQR 1.9–2.3] for intrusion, while hyperarousal had a median score of 2 [IQR 1.3–2.7]. The median sum score was 47 [IQR 40–57]. When comparing the HRQoL in COVID-19 survivors, all SF-36 domains scores were significantly higher in the group that did not develop PTSD (Table 3 and Figure 3).
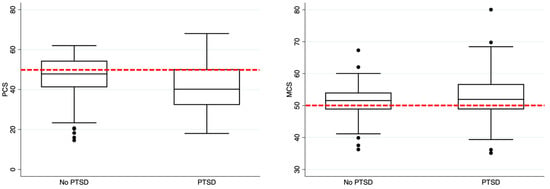
Figure 3.
HRQoL comparison between patients without and with PTSD. In the left part of the figure, it represents the comparison between no PTSD versus PTSD patients regarding the PCS, while in the right part of the figure, the MCS comparison is shown.
The box plot shows the median and interquartile ranges, while the whiskers represent the outliers. The red dotted line represents the value for the normal population.
To explore the possible factors related to the HRQoL, a multivariate linear regression analysis was performed and revealed that the female gender (β = −6.97, p = 0.044), a history of cardiovascular (β = −10.02, p = 0.001), liver disease (β = −17.07, p = 0.036) and LOSHOSP (β = −0.21, p = 0.001), reduced the PF score.
LOSHOSP also influenced the PR score (β = −0.31, p = 0.01). Weight at baseline (β = −0.31, p = 0.017) and a history of pulmonary disease (β = −12.51, p = 0.048) significantly influenced the RE score. The BP was lower in patients with known pulmonary disease (β = −15.76, p < 0.001). A history of cardiovascular and pulmonary disease also reduced the GH score, respectively, at β = −6.04 (p = 0.022) and β = −8.47 (p = 0.017). The female gender was associated with a lower VT score (β = −8.10, p = 0.005). The SF was lower in patients with cardiovascular disease, β = −6.58 (p = 0.035), and with a longer LOSHOSP, β = −0.15 (p = 0.042). Lastly, regarding the SF-36, health change was higher in patients who received NMB during their ICU stay (β = 8.67, p = 0.040). Complete multivariable analyses for each SF-36 domain are provided as Supplementary Material S2.
In addition, the risk factors for lower PCS and MCS scores were investigated, as reported in Supplementary Material S2. LOSHOSP negatively affected the PCS (β = −0.07, p = 0.007).
An evaluation of the possible factors related to PTSD was also performed. Weight at follow-up was found to be a risk factor for PTSD, OR 1.02 [IQR 1.00–1.04], p = 0.03.
Other risk factors for PTSD are reported in Supplementary Material S3.
4. Discussion
This multicenter observational study reports C-ARDS patients’ HRQoL 1 year after ICU discharge including the identification of clinical/demographic factors that correlate with it. The physical component summary was lower than normal. The mental component summary was slightly above the reference value for the normal population.
Risk factors for a lower PF score, which is a major determinant of the PCS, were the female gender, a history of cardiovascular or liver disease and LOSHOSP. The latter factor negatively also affected the PCS. Nearly one out of three patients tested positive for PTSD and had a significantly lower HRQoL.
Eberst et al. found results akin to ours with C-ARDS patients, showing higher HRQoL scores than those in Herridge’s report [17].
In the multicenter study of 118 Dutch C-ARDS survivors, Vlake et al. described comparable results, although the HRQoL was superior to their traditional cohort of critically ill patients [13]. In contrast with our work, Eberst’s was a single center study with a small sample size, and Vlake et al. limited the follow-up to 6 months after ICU discharge.
The literature includes frequent reports of a reduced HRQoL after traditional ARDS due to the physical impairment that sometimes requires years of external support [18,19,20]. This has an impact on patients’ families as well as society. Marti et al., in addition to the HRQoL after 1 year of ICU discharge, investigated the economic costs of traditional ARDS survivors. They advocated further research to optimize resources and improve outcomes because they discovered that patient care had high costs and, in most cases, the HRQoL remained low [21].
There is a substantial difference between traditional ARDS and C-ARDS populations: C-ARDS patients were mainly men, with severe acute pulmonary disease and a high demand for invasive mechanical ventilation (91%), but unlike traditional ARDS, they mainly suffered from acute single organ failure at ICU admission. In fact, considering that sepsis with multi-organ involvement was the main cause of ICU admission for traditional ARDS [17], in COVID-19 critically ill patients with lung damage was the main feature at ICU admission. Then, with the ongoing and massive activation of the immune system, the single organ failure often became a multiple organ dysfunction (MODS-CoV-2) [22,23].
In fact, brain, heart, liver and coagulation disorders have been frequently reported as the consequence of MODS-CoV-2 [24,25,26,27]
Further complications were caused by tight triage since demand for ICU admission increased as infection rates peaked in a context of limited resources [28,29]. This probably resulted in ICU admission being denied for patients with high predicted mortality, favoring better outcomes for those granted ICU admission [30,31,32,33].
We found that the female gender negatively influenced the PF (β = −7.13). This result aligns with a recent study by Huang et al. [11] in which females had persistent symptoms while also confirming findings by Brown et al. in which female ICU survivors, after traditional ARDS, were associated with a lower HRQoL at follow-up [34]. This should translate into the need for strict follow-up after ICU discharge in women who suffered from C-ARDS.
A history of cardiovascular disease was also strongly correlated with a worse PF at follow-up (β = −10.4, p = 0.001). Considering that the most represented cardiovascular disease in this cohort was arterial hypertension, this correlation sheds new light on the role of hypertension in COVID-19 outcomes [35,36].
It is well known that arterial hypertension creates endothelial dysfunction, and numerous studies have also demonstrated that hypertension per se reduces the HRQoL [37]. SARS-CoV-2 infection leads to persistent endothelial dysfunction and thus increases the risk of developing “long COVID” (persistence of physical symptoms) [38,39]. Consequently, we hypothesize that endothelial dysfunction in hypertensive COVID-19 patients could play a major role in the HRQoL reduction.
Duration of hospital stay was related to a lower PF at follow-up (β = −0.22, p = 0.001), and in general with a reduced PCS (β = −0.07, p = 0.007). Long hospital stay is also a well-established risk factor for PICS that could last for months after ICU discharge impairing the quality of life [40].
Nevertheless, prolonged recovery from acute illness often implies longer hospitalization in general and in rehabilitation wards. LOSHOSP in this study was not different from that of other studies involving severe ARDS patients [21].
An interesting finding is that 31.8% of patients screened with IES-R had PTSD. This was tested in C-ARDS patients at long-term follow-up after ICU discharge. Previous coronavirus epidemics, severe acute respiratory syndrome coronavirus and Middle East respiratory syndrome coronavirus, highlighted the increased psychologic distress with PTSD, depression and anxiety [41,42].
A recent metanalysis of non-COVID patients found that 12 months after ICU discharge, 19.8% presented PTSD [43], which is a lower result than this study. However, the first studies on PTSD after C-ARDS seem to confirm that its incidence is about 30% [44,45,46]. Furthermore, the high burden of PTSD might have been the result of the near complete denial in ABCDEF bundles during the peak of contagions [47].
Additional risk factors for PTSD development include social limitations and restrictions, media overpressure, restricted hospital visits and protective clothes and masks that hindered face-to-face interactions between patients and health-care workers [48,49]. Moreover, infectious disease survivors, including those who survived SARS-CoV-2, are exposed to psychological risks due to public fear of the disease and contagiousness that may result in extensive isolation [50]. Curiously, experimental studies found that PTSD could be an expression of endothelial dysfunction after viral infection, a well-represented feature in COVID-19 patients [51].
Given that we reported a significantly better HRQoL in the subgroup of C-ARDS patients without PTSD, a search for PTSD risk factors was performed. A multivariate analysis revealed that a higher weight at follow-up was a risk factor for PTSD (OR 1.02). Similar results were obtained by Tarsitani et al. when they evaluated a mixed cohort of critical and noncritical COVID patients. They advocated further investigations to determine if obesity could be a risk factor for PTSD or vice versa [52] because evidence in non-COVID-19 patients highlighted that PTSD could result in faster weight gain [53]. Therefore, it is possible to speculate that increased weight is probably a consequence of PTSD rather than a risk factor.
The literature has yet to fully assess the risks and protective factors that determine mental health outcomes after COVID-19 [54,55,56,57,58,59]. To the best of our knowledge, no studies have evaluated the impact of employment on the incidence of PTSD after C-ARDS.
There are some limitations to this study that include the absence of the SF-36 and IES-R baseline values. However, the patients were young and presented few comorbidities at baseline, so it is possible to speculate that they should have no reasons for the low SF-36 scores at baseline. In addition, patients with a previous history of cognitive and psychological disorders were excluded.
Some missing patients that did not accept to participate or were lost to follow-up could have had a poor performance status after ICU discharge, limiting their ability to answer the questionnaires. However, we cannot exclude that some of them probably were less sick and felt to be in a good health status that they thought they had nothing to report. It is our opinion that these opposite behaviors may limit the selection bias.
Patients who tested positive for PTSD through the IES-R were not further evaluated with psychiatric consultation, but restricted access to hospitals in the acute phase of the pandemic has limited this evaluation. Our findings reflect the characteristics of our population, hence our results must be taken cautiously.
Finally, patients performed a self-reported questionnaire that could not be collinear with test objectivation, such as a 6-min walking test. In fact, as Latronico et al. suggested, objective tests may reveal functional impairment, regardless of good scores on self-reported questionnaires [60].
5. Conclusions
The HRQoL in C-ARDS patients was reduced in the PCS, while the PCS was quite maintained in the overall population. More than 30% of patients tested positive for PTSD. In this group, the HRQoL was significantly lower than in those not reporting PTSD at follow-up. Continuous and prolonged follow-up of C-ARDS survivors, the HRQoL evaluation and PTSD screening are highly advocated because evidence is still low. It is imperative to obtain better outcomes and a better HRQoL, especially during a pandemic in which a large part of the population required hospitalization.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm12031058/s1, Supplementary Material S1: SF-36 and IES-R “pocket guide”. Supplementary Material S2: Univariable and multivariable analyses to find possible correlations between the SF-36 items and baseline, medical and ICU data. Supplementary Material S3: Univariable and multivariable analyses to find possible correlations between the IES-R items and baseline, medical and ICU data.
Author Contributions
C.D. and L.V. equally contributed and had full access to all of the data in the study and take responsibility for the integrity of the data. M.C., S.M.M. and the Italian Odissea Group, share senior authorship. Concept and design: C.D. and L.V. Acquisition: analysis, or interpretation of data: C.D., L.V., A.C., S.M. (Silvia Mongodi), G.S., M.M., A.B., T.P., S.M. (Sara Miori), A.S., S.L., S.M. (Sandra Magnoni), E.F., E.B., F.L., F.C., F.F., F.B., N.C., A.F., D.B., G.C., E.D.R., S.S., D.L.G., A.C., M.I., F.M., M.G., P.N., E.G.B., A.G., S.M.M. and the Italian Odissea Group. Drafting of the manuscript: C.D., L.V., A.C., P.N., M.C., S.M.M. and the Italian Odissea Group. Critical revision of the manuscript for important intellectual content: C.D., L.V., A.C., E.G.B., P.N., S.M.M. and the Italian Odissea Group. Statistical analysis: M.I. and M.D.M. Administrative: technical, or material support: L.M. (Luca Menga, on behalf of the Italian Odissea Group), I.R. (Ilaria Riccardi, on behalf of the Italian Odissea Group), S.F. (Samuele Ferrari, on behalf of the Italian Odissea Group). Supervision: C.D., L.V., A.C., E.G.B., P.N., M.C., S.M.M. and the Italian Odissea Group. All authors have read and agreed to the published version of the manuscript.
Funding
This research was partially funded by PRIN 2017 n.20178S4EK9 (available at https://prin.mur.gov.it) “Innovative statistical methods in biomedical research on biomarkers: from their identification to their use in clinical practice.” The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Institutional Review Board Statement
The Ethics Committee of Friuli Venezia Giulia Region approved the study (CEUR-2021-Os-99) as the coordinating center. The local ethics committee for each participating center approved the study. The study was conducted in accordance with good clinical practice guidelines and the guiding principles of the Declaration of Helsinki. Written informed consent was obtained from each patient. This study is prospectively registered at ClinicalTrials.gov on 27th April 2021 with number NCT04860687.
Informed Consent Statement
Written informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data are available from the corresponding author upon reasonable request.
Acknowledgments
We are grateful to all intensive care unit physicians, residents, nurses, and personnel from the participating centers, whose sacrifice, efforts, devotion to patients, and passion have made this study possible. The Members of the Italian Odissea Group are listed here: Enrico Boero, Anesthesia and Intensive Care Unit, San Giovanni Bosco Hospital, Turin, Italy; Ilaria Riccardi, Department of Anesthesia and Intensive Care, Health Integrated Agency of Friuli Centrale, Udine, Italy. Francesca Stefani, Department of Anesthesia and Intensive Care, Health Integrated Agency of Friuli Centrale, Udine, Italy. Lolita Fasoli, Department of Pediatrics, Health Integrated Agency of Friuli Centrale, Udine, Italy. Nicolò Sella, Institute of Anesthesia and Intensive Care, Padua University Hospital, Padua, Italy. Matteo Procopio, Anesthesiology, Critical Care and Pain Medicine Division, Department of Medicine and Surgery, University of Parma, Parma, Italy. Vincenzo Patruno, Pulmonology Unit, Academic Hospital of Udine, Health Integrated Agency of Friuli Centrale, Udine, Italy. Andrea Bruni, Anesthesia and Intensive Care Unit, Department of Medical and Surgical Sciences, University Hospital Mater Domini, Magna Graecia University, Catanzaro, Italy. Luca Menga, Department of Anesthesiology and Intensive Care Medicine, Catholic University of The Sacred Heart, Rome, Italy. Department of Anesthesia, Emergency and Intensive Care Medicine, Fondazione Policlinico Universitario A. Gemelli IRCCS, Rome, Italy. Eleonora Squadrani, Anesthesiology and Intensive Care, Department of Translational medicine, Faculty of Medicine and Surgery, University of Ferrara, Italy. Erika Taddei, Department of Surgical, Medical and Molecular Pathology and Critical Care Medicine, University of Pisa, Pisa, Italy. Elena Alberti, Department of Surgical, Medical and Molecular Pathology and Critical Care Medicine, University of Pisa, Pisa, Italy. Samuele Ferrari, Department of Surgical, Medical and Molecular Pathology and Critical Care Medicine, University of Pisa, Pisa, Italy. Lucrezia Zuccarelli, Department of Medicine, University of Udine, Udine, Italy. Rocco Pace, Anesthesia and Intensive Care 1, Santa Chiara Hospital, Trento, Italy. Anita Orlando, Department of Clinical-Surgical, Diagnostic and Pediatric Sciences, Unit of Anesthesia and Intensive Care, University of Pavia, Pavia, Italy. Andrea Bottazzi, Department of Clinical-Surgical, Diagnostic and Pediatric Sciences, Unit of Anesthesia and Intensive Care, University of Pavia, Pavia, Italy. Anna Aliberti, Department of Clinical-Surgical, Diagnostic and Pediatric Sciences, Unit of Anesthesia and Intensive Care, University of Pavia, Pavia, Italy. Annalisa Malara, Department of Clinical-Surgical, Diagnostic and Pediatric Sciences, Unit of Anesthesia and Intensive Care, University of Pavia, Pavia, Italy. Caterina Sonnati, Department of Clinical-Surgical, Diagnostic and Pediatric Sciences, Unit of Anesthesia and Intensive Care, University of Pavia, Pavia, Italy. Daniele Maria Piovera, Department of Clinical-Surgical, Diagnostic and Pediatric Sciences, Unit of Anesthesia and Intensive Care, University of Pavia, Pavia, Italy. Giulia Ceschin, Department of Clinical-Surgical, Diagnostic and Pediatric Sciences, Unit of Anesthesia and Intensive Care, University of Pavia, Pavia, Italy. Maria Antonietta Forte, Department of Clinical-Surgical, Diagnostic and Pediatric Sciences, Unit of Anesthesia and Intensive Care, University of Pavia, Pavia, Italy. Maria Martina Moscariello, Department of Clinical-Surgical, Diagnostic and Pediatric Sciences, Unit of Anesthesia and Intensive Care, University of Pavia, Pavia, Italy. Raffaella Arioli, Department of Clinical-Surgical, Diagnostic and Pediatric Sciences, Unit of Anesthesia and Intensive Care, University of Pavia, Pavia, Italy. Rachele Calabria, Department of Clinical-Surgical, Diagnostic and Pediatric Sciences, Unit of Anesthesia and Intensive Care, University of Pavia, Pavia, Italy. Silvia Bonaiti, Department of Clinical-Surgical, Diagnostic and Pediatric Sciences, Unit of Anesthesia and Intensive Care, University of Pavia, Pavia, Italy.
Conflicts of Interest
F.M. received fees for lectures from GE Healthcare, Hamilton Medical and SEDA SpA outside the present work. S.M. (Silvia Mongodì) received fees for lectures from GE Healthcare outside the present work. A research agreement is active between the University of Pavia and Hamilton Medical. Domenico Luca Grieco DLG has received payments for travel expenses by Getinge and Air Liquide, speaking fees by Intersurgical, GE, Fisher and Paykel and Gilead, and discloses a research grant by GE outside this work. G.C. has received fees for lectures from MSD and Getinge outside this work. M.C. is a consultant of Edwards Lifesciences (Directed Systems Consultancy). The other authors declare no conflict of interest.
Abbreviations
ARDS: acute respiratory distress syndrome; SARS-CoV2: severe acute respiratory syndrome coronavirus 2; PICS: post-intensive care syndrome; HRQoL: health-related quality of life; ICU: intensive care unit; C-ARDS: coronavirus acute respiratory distress syndrome; PTSD: post-traumatic stress disorder; RT-PCR: real time polymerase chain reaction; SF-36: short-form 36; IES-R: impact of event-revised; APACHE II: acute physiologic assessment and chronic health evaluation II; LIS: lung injury score; LOSICU: length of ICU stay; LOSHOSP: length of hospital stay; PF: physical functioning; PR: physical role; RE: emotional role; BP: bodily pain; SF: social functioning; MH: mental health; GH: general health; VT: vitality.
References
- World Health Organization (WHO). Coronavirus COVID-19 Dashboard; World Health Organization: Geneva, Switzerland, 2020; Available online: https://covid19.who.int (accessed on 19 January 2023).
- Hajjar, L.A.; Costa, I.B.S.D.S.; Rizk, S.I.; Biselli, B.; Gomes, B.R.; Bittar, C.S.; de Oliveira, G.Q.; de Almeida, J.P.; Bello, M.V.D.O.; Garzillo, C.; et al. Intensive care management of patients with COVID-19: A practical approach. Ann. Intensiv. Care 2021, 11, 1–17. [Google Scholar] [CrossRef] [PubMed]
- The Recovery Collaborative Group. Dexamethasone in Hospitalized Patients with COVID-19. N. Engl. J. Med. 2021, 384, 693–704. [Google Scholar] [CrossRef] [PubMed]
- Inoue, S.; Hatakeyama, J.; Kondo, Y.; Hifumi, T.; Sakuramoto, H.; Kawasaki, T.; Taito, S.; Nakamura, K.; Unoki, T.; Kawai, Y.; et al. Post-intensive care syndrome: Its pathophysiology, prevention, and future directions. Acute Med. Surg. 2019, 6, 233–246. [Google Scholar] [CrossRef] [PubMed]
- Herridge, M.S.; Cheung, A.M.; Tansey, C.M.; Matte-Martyn, A.; Diaz-Granados, N.; Al-Saidi, F.; Cooper, A.B.; Guest, C.B.; Mazer, C.D.; Mehta, S.; et al. One-Year Outcomes in Survivors of the Acute Respiratory Distress Syndrome. N. Engl. J. Med. 2003, 348, 683–693. [Google Scholar] [CrossRef] [PubMed]
- Hatch, R.; Young, D.; Barber, V.; Griffiths, J.; Harrison, D.A.; Watkinson, P. Anxiety, Depression and Post Traumatic Stress Disorder after critical illness: A UK-wide prospective cohort study. Crit. Care 2018, 22, 1–13. [Google Scholar] [CrossRef]
- Kerckhoffs, M.C.; Kosasi, F.F.L.; Soliman, I.W.; van Delden, J.J.M.; Cremer, O.L.; de Lange, D.W.; Slooter, A.J.C.; Kesecioglu, J.; van Dijk, D. Determinants of self-reported unacceptable outcome of intensive care treatment 1 year after discharge. Intensiv. Care Med. 2019, 45, 806–814. [Google Scholar] [CrossRef]
- Bein, T.; Weber-Carstens, S.; Apfelbacher, C. Long-term outcome after the acute respiratory distress syndrome. Curr. Opin. Crit. Care 2018, 24, 35–40. [Google Scholar] [CrossRef]
- Emanuel, E.J.; Persad, G.; Upshur, R.; Thome, B.; Parker, M.; Glickman, A.; Zhang, C.; Boyle, C.; Smith, M.; Phillips, J.P. Fair Allocation of Scarce Medical Resources in the Time of COVID-19. N. Engl. J. Med. 2020, 382, 2049–2055. [Google Scholar] [CrossRef]
- Gamberini, L.; Mazzoli, C.A.; Sintonen, H.; Colombo, D.; Scaramuzzo, G.; Allegri, D.; Tonetti, T.; Zani, G.; Capozzi, C.; Giampalma, E.; et al. Quality of life of COVID-19 critically ill survivors after ICU discharge: 90 days follow-up. Qual. Life Res. 2021, 30, 2805–2817. [Google Scholar] [CrossRef]
- Huang, C.; Huang, L.; Wang, Y.; Li, X.; Ren, L.; Gu, X.; Kang, L.; Guo, L.; Liu, M.; Zhou, X.; et al. 6-month consequences of COVID-19 in patients discharged from hospital: A cohort study. Lancet 2021, 397, 220–232. [Google Scholar] [CrossRef]
- Vlake, J.H.B.; Van Bommel, J.; Hellemons, M.E.; Wils, E.-J.; Bienvenu, O.J.; Schut, A.F.C.; Klijn, E.; Van Bavel, M.P.; Gommers, D.; Van Genderen, M.E. Psychologic Distress and Quality of Life After ICU Treatment for Coronavirus Disease 2019: A Multicenter, Observational Cohort Study. Crit. Care Explor. 2021, 3, e0497. [Google Scholar] [CrossRef] [PubMed]
- Ware, J.E.; Kosinski, M.; Bayliss, M.S.; McHorney, C.A.; Rogers, W.H.; Raczek, A. Comparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: Summary of results from the Medical Outcomes Study. Med. Care 1995, 33, AS264–AS279. [Google Scholar]
- Weiss, D.S. The Impact of Event Scale: Revised. In Cross-cultural Assessment of Psychological Trauma and PTSD; Wilson, J.P., Tang, C.S., Eds.; Springer: New York, NY, USA, 2007; pp. 219–238. [Google Scholar]
- Murray, J.F.; Matthay, M.A.; Luce, J.M.; Flick, M.R. An Expanded Definition of the Adult Respiratory Distress Syndrome. Am. Rev. Respir. Dis. 1988, 138, 720–723, Erratum in Am. Rev. Respir. Dis. 1989, 139, 1065. [Google Scholar] [CrossRef]
- Wan, X.; Wang, W.; Liu, J.; Tong, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med. Res. Methodol. 2014, 14, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Eberst, G.; Claudé, F.; Laurent, L.; Meurisse, A.; Roux-Claudé, P.; Barnig, C.; Vernerey, D.; Paget-Bailly, S.; Bouiller, K.; Chirouze, C.; et al. Result of one-year, prospective follow-up of intensive care unit survivors after SARS-CoV-2 pneumonia. Ann. Intensiv. Care 2022, 12, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Cheung, A.M.; Tansey, C.M.; Tomlinson, G.; Diaz-Granados, N.; Matté, A.; Barr, A.; Mehta, S.; Mazer, C.D.; Guest, C.B.; Stewart, T.E.; et al. Two-Year Outcomes, Health Care Use, and Costs of Survivors of Acute Respiratory Distress Syndrome. Am. J. Respir. Crit. Care Med. 2006, 174, 538–544. [Google Scholar] [CrossRef]
- Bienvenu, J.; Colantuoni, E.; Mendez-Tellez, P.A.; Shanholtz, C.; Himmelfarb, C.D.; Pronovost, P.J.; Needham, D.M. Cooccurrence of and Remission From General Anxiety, Depression, and Posttraumatic Stress Disorder Symptoms After Acute Lung Injury. Crit. Care Med. 2015, 43, 642–653. [Google Scholar] [CrossRef]
- Herridge, M.S.; Tansey, C.M.; Matté, A.; Tomlinson, G.; Diaz-Granados, N.; Cooper, A.; Guest, C.B.; Mazer, C.D.; Mehta, S.; Stewart, T.E.; et al. Functional Disability 5 Years after Acute Respiratory Distress Syndrome. N. Engl. J. Med. 2011, 364, 1293–1304. [Google Scholar] [CrossRef]
- Marti, J.; Hall, P.; Hamilton, P.; Lamb, S.; McCabe, C.; Lall, R.; Darbyshire, J.; Young, D.; Hulme, C. One-year resource utilisation, costs and quality of life in patients with acute respiratory distress syndrome (ARDS): Secondary analysis of a randomised controlled trial. J. Intensive Care 2016, 4, 56. [Google Scholar] [CrossRef]
- Robba, C.; Battaglini, D.; Pelosi, P.; Rocco, P.R.M. Multiple organ dysfunction in SARS-CoV-2: MODS-CoV-2. Expert Rev. Respir. Med. 2020, 14, 865–868. [Google Scholar] [CrossRef]
- Cui, J.M.; Yuan, B.M.; Li, Y.B.; Li, Z.M.; Yuan, Y. The clinical characters and prognosis of COVID-19 patients with multiple organ dysfunction. Medicine 2021, 100, e27400. [Google Scholar] [CrossRef] [PubMed]
- Deana, C.; Bagatto, D. Severe stroke in patients admitted to intensive care unit after COVID-19 infection: Pictorial essay of a case series. Brain Hemorrhages 2022, 3, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Deana, C.; Vetrugno, L.; Fabris, M.; Curcio, F.; Sozio, E.; Tascini, C.; Bassi, F. Pericardial Cytokine “Storm” in a COVID-19 Patient: The Confirmation of a Hypothesis. Inflammation 2022, 45, 1–5. [Google Scholar] [CrossRef]
- DePace, N.L.; Colombo, J. Long-COVID Syndrome and the Cardiovascular System: A Review of Neurocardiologic Effects on Multiple Systems. Curr. Cardiol. Rep. 2022, 24, 1711–1726. [Google Scholar] [CrossRef]
- Zhao, W.; Li, H.; Li, J.; Xu, B.; Xu, J. The mechanism of multiple organ dysfunction syndrome in patients with COVID-19. J. Med. Virol. 2021, 94, 1886–1892. [Google Scholar] [CrossRef] [PubMed]
- Tyrrell, C.S.B.; Mytton, O.T.; Gentry, S.V.; Thomas-Meyer, M.; Allen, J.L.Y.; Narula, A.A.; McGrath, B.; Lupton, M.; Broadbent, J.; Ahmed, A.; et al. Managing intensive care admissions when there are not enough beds during the COVID-19 pandemic: A systematic review. Thorax 2020, 76, 302–312. [Google Scholar] [CrossRef]
- Deana, C.; Rovida, S.; Orso, D.; Bove, T.; Bassi, F.; De Monte, A.; Vetrugno, L. Learning from the Italian experience during COVID-19 pandemic waves: Be prepared and mind some crucial aspects. Acta Bio-Med. Atenei Parm. 2021, 92, e2021097. [Google Scholar] [CrossRef]
- Dennis, J.M.; McGovern, A.P.M.; Vollmer, S.J.; Mateen, B.A.M. Improving Survival of Critical Care Patients With Coronavirus Disease 2019 in England: A National Cohort Study, March to June 2020. Crit. Care Med. 2021, 49, 209–214. [Google Scholar] [CrossRef]
- Sprung, C.L.; Joynt, G.M.; Christian, M.D.; Truog, R.D.; Rello, J.; Nates, J.L. Adult ICU Triage During the Coronavirus Disease 2019 Pandemic: Who Will Live and Who Will Die? Recommendations to Improve Survival. Crit. Care Med. 2020, 48, 1196–1202. [Google Scholar] [CrossRef]
- Lombardi, Y.; Azoyan, L.; Szychowiak, P.; Bellamine, A.; Lemaitre, G.; Bernaux, M.; Daniel, C.; Leblanc, J.; Riller, Q.; Steichen, O.; et al. External validation of prognostic scores for COVID-19: A multicenter cohort study of patients hospitalized in Greater Paris University Hospitals. Intensiv. Care Med. 2021, 47, 1426–1439. [Google Scholar] [CrossRef]
- Vetrugno, L.; Castaldo, N.; Fantin, A.; Deana, C.; Cortegiani, A.; Longhini, F.; Forfori, F.; Cammarota, G.; Grieco, D.L.; Isola, M.; et al. Ventilatory associated barotrauma in COVID-19 patients: A multicenter observational case control study (COVI-MIX-study). Pulmonology 2022. [CrossRef] [PubMed]
- Brown, S.M.; Wilson, E.; Presson, A.P.; Zhang, C.; Dinglas, V.D.; Greene, T.; Hopkins, R.O.; Needham, D.M. Predictors of 6-month health utility outcomes in survivors of acute respiratory distress syndrome. Thorax 2017, 72, 311–317. [Google Scholar] [CrossRef] [PubMed]
- Guan, W.-J.; Liang, W.-H.; Zhao, Y.; Liang, H.-R.; Chen, Z.-S.; Li, Y.-M.; Liu, X.-Q.; Chen, R.-C.; Tang, C.-L.; Wang, T.; et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: A nationwide analysis. Eur. Respir. J. 2020, 55, 2000547. [Google Scholar] [CrossRef] [PubMed]
- Pranata, R.; Lim, M.A.; Huang, I.; Raharjo, S.B.; Lukito, A.A. Hypertension is associated with increased mortality and severity of disease in COVID-19 pneumonia: A systematic review, meta-analysis and meta-regression. J. Renin-Angiotensin-Aldosterone Syst. 2020, 21, 1470320320926899. [Google Scholar] [CrossRef]
- Trevisol, D.J.; Moreira, L.B.; Kerkhoff, A.; Fuchs, S.C.; Fuchs, F. Health-related quality of life and hypertension: A systematic review and meta-analysis of observational studies. J. Hypertens. 2011, 29, 179–188. [Google Scholar] [CrossRef]
- Charfeddine, S.; Ibn Hadj Amor, H.; Jdidi, J.; Torjmen, S.; Kraiem, S.; Hammami, R.; Bahloul, A.; Kallel, N.; Moussa, N.; Touil, I.; et al. Long COVID 19 Syndrome: Is It Related to Microcirculation and Endothelial Dysfunction? Insights From TUN-EndCOV Study. Front. Cardiovasc. Med. 2021, 8, 1702. [Google Scholar] [CrossRef]
- Prasad, M.; Leon, M.; Lerman, L.O.; Lerman, A. Viral Endothelial Dysfunction: A Unifying Mechanism for COVID-19. Mayo Clin. Proc. 2021, 96, 3099–3108. [Google Scholar] [CrossRef]
- Harvey, M.A.; Davidson, J.E. Postintensive Care Syndrome. Crit. Care Med. 2016, 44, 381–385. [Google Scholar] [CrossRef]
- Rogers, J.P.; Chesney, E.; Oliver, D.; Pollak, T.A.; McGuire, P.; Fusar-Poli, P.; Zandi, M.S.; Lewis, G.; David, A.S. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: A systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry 2020, 7, 611–627. [Google Scholar] [CrossRef]
- Lee, D.T.S.; Wing, Y.K.; Leung, H.C.M.; Sung, J.J.Y.; Ng, Y.K.; Yiu, G.C.; Chen, R.Y.L.; Chiu, H.F.K. Factors Associated with Psychosis among Patients with Severe Acute Respiratory Syndrome: A Case-Control Study. Clin. Infect. Dis. 2004, 39, 1247–1249. [Google Scholar] [CrossRef]
- Righy, C.; Rosa, R.G.; da Silva, R.T.A.; Kochhann, R.; Migliavaca, C.B.; Robinson, C.C.; Teche, S.P.; Teixeira, C.; Bozza, F.A.; Falavigna, M. Prevalence of post-traumatic stress disorder symptoms in adult critical care survivors: A systematic review and meta-analysis. Crit. Care 2019, 23, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Mongodi, S.; Salve, G.; Tavazzi, G.; Politi, P.; Mojoli, F. High prevalence of acute stress disorder and persisting symptoms in ICU survivors after COVID-19. Intensiv. Care Med. 2021, 47, 616. [Google Scholar] [CrossRef] [PubMed]
- Carenzo, L.; Protti, A.; Corte, F.D.; Aceto, R.; Iapichino, G.; Milani, A.; Santini, A.; Chiurazzi, C.; Ferrari, M.; Heffler, E.; et al. Short-term health-related quality of life, physical function and psychological consequences of severe COVID-19. Ann. Intensiv. Care 2021, 11, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Rousseau, A.-F.; Minguet, P.; Colson, C.; Kellens, I.; Chaabane, S.; Delanaye, P.; Cavalier, E.; Chase, J.G.; Lambermont, B.; Misset, B. Post-intensive care syndrome after a critical COVID-19: Cohort study from a Belgian follow-up clinic. Ann. Intensiv. Care 2021, 11, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Deana, C.; Verriello, L.; Pauletto, G.; Corradi, F.; Forfori, F.; Cammarota, G.; Bignami, E.; Vetrugno, L.; Bove, T. Insights into neurological dysfunction of critically ill COVID-19 patients. Trends Anaesth. Crit. Care 2021, 36, 30–38. [Google Scholar] [CrossRef]
- Zante, B.; Erne, K.; Grossenbacher, J.; Camenisch, S.A.; Schefold, J.C.; Jeitziner, M.-M. Symptoms of post-traumatic stress disorder (PTSD) in next of kin during suspension of ICU visits during the COVID-19 pandemic: A prospective observational study. BMC Psychiatry 2021, 21, 1–9. [Google Scholar] [CrossRef]
- Moss, S.J.; Rosgen, B.K.; Lucini, F.; Krewulak, K.D.; Soo, A.; Doig, C.J.; Patten, S.B.; Stelfox, H.T.; Fiest, K.M. Psychiatric Outcomes in ICU Patients With Family Visitation. Chest 2022, 162, 578–587. [Google Scholar] [CrossRef]
- Lettinga, K.D.; Verbon, A.; Nieuwkerk, P.; Jonkers, R.E.; Gersons, B.P.R.; Prins, J.M.; Speelman, P. Health-Related Quality of Life and Posttraumatic Stress Disorder among Survivors of an Outbreak of Legionnaires Disease. Clin. Infect. Dis. 2002, 35, 11–17. [Google Scholar] [CrossRef]
- Sfera, A.; Osorio, C.; Rahman, L.; del Campo, C.M.Z.-M.; Maldonado, J.C.; Jafri, N.; Cummings, M.A.; Maurer, S.; Kozlakidis, Z. PTSD as an Endothelial Disease: Insights From COVID-19. Front. Cell. Neurosci. 2021, 15, 770387. [Google Scholar] [CrossRef]
- Tarsitani, L.; Vassalini, P.; Koukopoulos, A.; Borrazzo, C.; Alessi, F.; Di Nicolantonio, C.; Serra, R.; Alessandri, F.; Ceccarelli, G.; Mastroianni, C.M.; et al. Post-traumatic Stress Disorder Among COVID-19 Survivors at 3-Month Follow-up After Hospital Discharge. J. Gen. Intern. Med. 2021, 36, 1702–1707. [Google Scholar] [CrossRef]
- Kubzansky, L.D.; Bordelois, P.; Jun, H.J.; Roberts, A.; Cerda, M.; Bluestone, N.; Koenen, K. The Weight of Traumatic Stress. JAMA Psychiatry 2014, 71, 44–51. [Google Scholar] [CrossRef] [PubMed]
- Vindegaard, N.; Benros, M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 2020, 89, 531–542. [Google Scholar] [CrossRef] [PubMed]
- Qiu, D.; Li, Y.; Li, L.; He, J.; Ouyang, F.; Xiao, S. Prevalence of post-traumatic stress symptoms among people influenced by coronavirus disease 2019 outbreak: A meta-analysis. Eur. Psychiatry 2021, 64, 1–42. [Google Scholar] [CrossRef] [PubMed]
- Schou, T.M.; Joca, S.; Wegener, G.; Bay-Richter, C. Psychiatric and neuropsychiatric sequelae of COVID-19—A systematic review. Brain Behav. Immun. 2021, 97, 328–348. [Google Scholar] [CrossRef]
- Vahia, I.V.; Jeste, D.V.; Reynolds, C.F. Older Adults and the Mental Health Effects of COVID-19. JAMA 2020, 324, 2253. [Google Scholar] [CrossRef]
- Dmytriw, A.A.; Chibbar, R.; Chen, P.P.Y.; Traynor, M.D.; Kim, D.W.; Bruno, F.P.; Cheung, C.C.; Pareek, A.; Chou, A.C.C.; Graham, J.; et al. Outcomes of acute respiratory distress syndrome in COVID-19 patients compared to the general population: A systematic review and meta-analysis. Expert Rev. Respir. Med. 2021, 15, 1347–1354. [Google Scholar] [CrossRef]
- Fazzini, B.; Battaglini, D.; Carenzo, L.; Pelosi, P.; Cecconi, M.; Puthucheary, Z. Physical and psychological impairment in survivors of acute respiratory distress syndrome: A systematic review and meta-analysis. Br. J. Anaesth. 2022, 129, 801–814. [Google Scholar] [CrossRef]
- Latronico, N.; Peli, E.; Calza, S.; Rodella, F.; Novelli, M.P.; Cella, A.; Marshall, J.; Needham, D.M.; Rasulo, F.A.; Piva, S. Physical, cognitive and mental health outcomes in 1-year survivors of COVID-19-associated ARDS. Thorax 2022, 77, 300–303. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).