Abstract
The aim of our study is to review the current available knowledge regarding preferences and expectations of patients with overactive bladder (OAB). The Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement guidelines were followed for this manuscript’s preparation. Three online databases were searched: PubMed/Medline, Embase, and Scopus, while a combination of the following keywords was used: detrusor overactivity, overactive bladder, urinary incontinence, perspectives, expectations, and preferences. Overall, 1349 studies were retrieved and screened while only 10 studies appeared to be relevant for the scope of this review. Most of the studies were related to preferences about OAB medications (i.e., antimuscarinics); four of them reported patients’ inclinations to alternative treatments in the case of medication therapy failure (i.e., neuromodulation, Botox). No data were found about diagnosis or other aspects of disease management (i.e., surgery, follow-up). Based on these findings, from the patient’s point of view, the ideal medication should be cheap, without risk of cognitive function impairment, and able to reduce daytime urinary frequency and incontinence episodes.
1. Introduction
Overactive bladder (OAB) is defined as urgency, with or without urgency urinary incontinence, usually with increased daytime frequency and nocturia, with no proven infection or other obvious pathology [1]. OAB is a descriptive clinical term, a symptom-based definition, and it is not diagnostic of a specific disease. The pathophysiology of OAB is poorly understood, but probably involves changes at multiple levels of micturition control (i.e., brain, spinal cord, and smooth muscle of the bladder). However, the true aetiology of OAB is still unknown.
Treatment of OAB is very challenging for several reasons. First, about one patient over two with bothersome OAB symptoms consulted a physician and less than a quarter received treatment [2]. Thus, several treatments have been proposed for OAB including lifestyle changes (first line treatment), medical and surgical options. Regarding medical options, several antimuscarinics agents are widely used for OAB symptoms. However, their fair efficacy and side effects often result in a poor adherence. More specifically, adherence rates at one year may be as low as 35% [3]. Surgical options are usually reserved for refractory cases or in presence of OAB related complications. Nonetheless, surgical options need to be accurately tailored to the patient’s bladder condition, overall medical status, physical abilities, and expectations.
Nowadays, patient-centred care and shared decision making (SDM) are generally recognized as the gold standard for medical consultations. SDM is an approach that involves a mutual discussion regarding management or treatment options to identify the best option for the patient in terms of risk-benefit ratio and patient’s preferences. Likewise, from the clinician’s perspective, SDM is a useful way of presenting to patients their health condition. Some authors have suggested that treatment adherence could be improved by enhancing the interaction between physician and patient and cost ‘effectiveness [4,5].
Furthermore, there is an increasing interest to include patients’ preferences into recommendations for diseases management. For instance, the National Institute for Clinical Excellence (NICE) has developed a research project to test various methods of surveying patient preferences. The current guidelines from the European Association of Urology include the participation of patient representatives among the Authors.
With this knowledge in mind, aim of our study was to systematically review the current knowledge on expectations and preferences of patients with OAB.
2. Evidence Acquisition
The Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement guidelines were followed during manuscript preparation of this review. A protocol was developed and approved in the PROSPERO database (CRD: 42022327200).
Literature research was carried out in September 2022 to identify published studies relevant to the scope of this review. Three online databases were searched: in PubMed/Medline, Embase and Scopus while a combination of the following keywords was used: detrusor overactivity, overactive bladder, urinary incontinence, perspectives, expectations, and preferences. The reference lists of all manuscripts reviewed as full text were also screened for eligible studies. Two independent authors (AC, RL) screened the databases and disagreements were resolved upon consensus with a senior author (CDN). PRISMA flow chart is available in Figure 1.
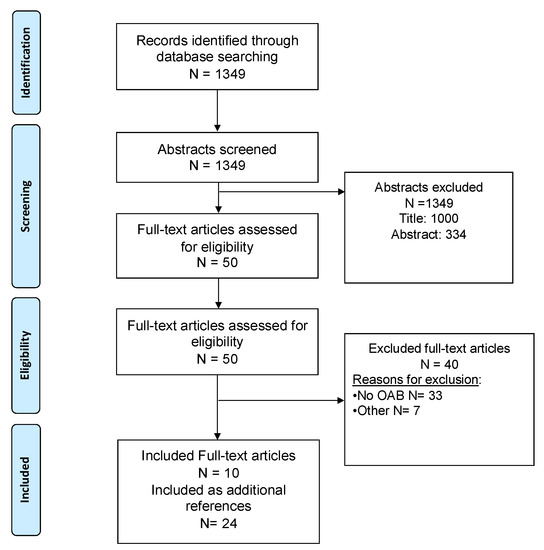
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Flow diagram of studies identified, excluded and included.
Studies were included if published in English and available online while they were excluded if related to children population (age < 18 years), faecal incontinence, post radical prostatectomy incontinence, and if patients’ preferences were not the outcome. This research strategy yielded 1349 papers with potentially relevant title and abstract. However, only ten studies were deemed to be relevant for the purpose of this review (Figure 1) after screening. No previous reviews were found.
Risk of Bias Assessment
The risk of bias of each included study was assessed by two review authors, working independently using the Newcastle-Ottawa scale for observational studies [6].
3. Evidence Synthesis
3.1. How to Evaluate Patients’ Preferences and Expectation?
Several tools are described as possible methods to evaluate and compare patients’ preferences and expectations. Quantitative data were collected using dedicated questionnaires. Overall, seven studies used a discrete choice experiment, two studies used oral interviews, and one study used questionnaires with a utility score.
Regarding DCE, this is a quantitative technique for eliciting individual preferences. It allows researchers to discover how individuals value selected attributes of a programme, product, or service by asking them to state their choice over different hypothetical alternatives [7]. DCE is also known as a conjoint analysis and usually the choice set is composed of two or more competing alternatives which vary in terms of several attributes. In recent years, DCEs have been increasingly used to help understand preferences in the field of health and healthcare. Interestingly, one study [8] used health utility index as an approach to compute the value that patient assigned to some aspects of OAB, including both therapy and symptoms severity [8]. The Utility index was originally developed as a rating scale to measure general health status and health-related quality of life (HRQoL). However, it seems a simple way to assign and compare values between different contexts.
The retrieved studies highlight the absence of validated and standardized tools to assess and measure patient’s preferences and expectations regarding a treatment option or a therapeutic strategy. This limit probably depends on differences in cultural, geographical, society, economic, and national factors [9].
Although there is no world-wide validated tools to assess patients’ preferences and expectations. Previous experiences on the use of DCE in other areas such as the evaluation of environmental goods and services, indicate that we can be optimistic on the utility of this approach. Moreover, Sumedha Chhatre et al. (2021) recently showed that the use of DCE [10] for assessing OAB preferences is feasible and acceptable whereas future research remains required to evaluate its use in different subgroups distinct for sociodemographic and clinical characteristics [11,12,13].
3.2. Patients’ Preferences and Expectations in Medical Treatment
Overall, eight studies addressed the preferences and expectations of OAB patients: four studies were related to the use antimuscarinics, four studies included patients undergoing treatments for OAB unresponsive to antimuscarinics, and one study evaluated the importance of economic burden in patient’s preferences (Table 1).

Table 1.
Studies included in the systematic review.
Amod Athavale et al. (2018) evaluated medical treatment preferences of treatment-naïve individuals with symptoms of OAB [14]. Data from 514 patients were analysed, 68% of them were female, and 66% of the cohort were less than 65 years of age. Most respondents reported moderate/severe OAB (64.2%) and experienced incontinence (79.4%) and/or nocturia (59.1%). A DCE was designed to quantify the strength of preference. This survey showed that treatment-naïve patients assigned a strong preference for drug delivery method, reduction of daytime micturition frequency, and lower costs. More specifically, oral and patches were more desirable than injectable therapies. Furthermore, the study highlighted how physician and patient perspectives may be different. Physicians are mostly focused on efficacy, whereas patients on tolerability [15,16,23].
Overall, patients on AMs present a higher risk of side effects when compared to placebo [17,24] (1.26 times). The study evaluated frailly elderly patients’ perspectives about AEs of AMs treatment. DCE analysis highlighted how much older patients are concerned by cognitive side effects of AMs treatment.
OAB treatment can be expensive for the patient. Harpe et al., in a survey based on 133 OAB patients, investigated medication preferences using a dedicated questionnaire including nine hypothetical scenarios [18]. Briefly, participants were asked to provide an estimate of the likelihood (from 0% to 100%) of medications to control OAB symptoms vs. doing nothing to control symptoms. Insurance coverage was the most important attribute for choosing a treatment, followed by sleep disturbance [18].
3.3. Patients Preferences and Expectations in Minimally Invasive Treatment
Patients nonresponsive to medical treatment may benefit from 3rd line treatment including sacral neuromodulation (SNM), onabotulinum toxin A (Botox®), and/or percutaneous tibial nerve stimulation (PTNS). Hashim Hashim (2015) investigated patient preferences for these treatments and their respective characteristics in a sample of patients with idiopathic OAB in the UK. Among 127 (91%) of patients included in the analysis, most of them (≥80%) were willing to try each of the three treatments: respectively, 57%, 34%, and 9% most preferred PTNS, SNM, and Botox. Furthermore, preferences for the attributes differed from each treatment the patients chose. For instance, patients choosing SNM favoured an implanted device in upper buttock more than those preferring PTNS or Botox. Moreover, it has been recently reported that successful rate of SNM improves when the patient can interact with the device [22] while low side effects followed by the effectiveness on continence and micturition frequency had the greatest impact on patients when a SNM device was implanted [20]. Moreover, Fontaine et al. evaluated 217 patients who failed medical treatment. Nobody opted for ileal conduit. Further, 25% opted for Botox injections, and 25% for SNM. Only 2.5% of patients chose cystoplasty ± Mitrofanoff channel reconstruction.
4. Conclusions
Our review summarizes the current evidence on patients’ preferences and expectations regarding OAB management (Table 2). Unfortunately, few studies investigated this topic using different non-standardized methods.

Table 2.
Patients’ preferences and expectations regarding OAB management.
Patient preferences and expectations should be part of the decision making process in managing benign and malignant disorders [25,26,27,28,29,30]. Recently, Malde et al. summarized patient preferences and expectations in LUTS management and clearly showed how patient and physician perspectives may be completely different and that often patients prefer a less effective treatment but with a minor risk of AEs [31,32,33]. Our findings in a similar topic confirm these results. In OAB patients, medical treatment is a challenge scenario for the physicians considering the low adherence and satisfaction to medications. Several explanations have been proposed, such as lack of efficacy, rate of adverse events, costs, and patients’ awareness on their condition. A better knowledge of patients expectation and preferences could help physicians to better profile OAB patients in order to identify the best treatment for every single patient, to improve patient adherence and compliance and to reduce doctor ‘google’ and doctor shopping [25,34].
With respect to the current evidence, OAB patients prefer an oral treatment which the reduces urgency, frequency, and incontinence episodes, with no effect on cognitive function and covered by insurance. The impact of costs and insurance coverage on patients’ compliance is particularly evident in Europe, where in some countries AMs and beta-3-agonists are not covered and as a consequence patients adherence and compliance is lower when compared to other countries.
The lack of standardized method in the evaluation of patient’s preferences and expectations represents an important bias of this research area. Given the poor evidence on the subject, first of all, it is very important to develop a validated and universal method to assess patients’ preferences and expectations. This approach could lead to a better understanding of patient’s preferences and expectations, better analysis, and identifying possible differences based on social and demographic characteristics. Another unmet need in OAB is that most of the available evidence is based on female population.
Currently, the importance of sharing decisions on treatment with patients has long been recognized and this will lead to consider a “patient-based approach” instead of “one size fits all” strategy.
Author Contributions
Conceptualization, A.C.; literature search, E.M. and G.T.; writing—original draft preparation, A.C., R.L., J.S., C.G., A.N. and B.T.; writing—review & editing, A.N., C.D.N., A.F., and G.G.; supervision, A.T., R.D., A.N. and V.U. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data will be available upon request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Haylen, B.T.; De Ridder, D.; Freeman, R.M.; Swift, S.E.; Berghmans, B.; Lee, J.; Monga, A.; Petri, E.; Rizk, D.E.; Sand, P.K.; et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) Joint Report on the Terminology for Female Pelvic Floor Dysfunction. Int. Urogynecol. J. 2010, 21, 5–26. Available online: https://pubmed.ncbi.nlm.nih.gov/19937315/ (accessed on 5 November 2022). [CrossRef] [PubMed]
- Benner, J.S.; Nichol, M.B.; Rovner, E.S.; Jumadilova, Z.; Alvir, J.; Hussein, M.; Fanning, K.; Trocio, J.N.; Brubaker, L. Patient-Reported Reasons for Discontinuing Overactive Bladder Medication. BJU Int. 2010, 105, 1276–1282. Available online: https://pubmed.ncbi.nlm.nih.gov/19912188/ (accessed on 5 November 2022). [CrossRef] [PubMed]
- Sexton, C.C.; Notte, S.M.; Maroulis, C.; Dmochowski, R.R.; Cardozo, L.; Subramanian, D.; Coyne, K.S. Persistence and Adherence in the Treatment of Overactive Bladder Syndrome with Anticholinergic Therapy: A Systematic Review of the Literature. Int. J. Clin. Pract. 2011, 65, 567–585. Available online: https://pubmed.ncbi.nlm.nih.gov/21489081/ (accessed on 5 November 2022). [CrossRef] [PubMed]
- Kini, V.; Michael Ho, P. Interventions to Improve Medication Adherence: A Review. JAMA 2018, 320, 2461–2473. Available online: https://pubmed.ncbi.nlm.nih.gov/30561486/ (accessed on 5 November 2022). [CrossRef]
- Sahakyan, Y.; Erman, A.; Bhojani, N.; Chughtai, B.; Zorn, K.C.; Sander, B.; Elterman, D.S. Pharmacotherapy vs. Minimally Invasive Therapies as Initial Therapy for Moderate-to-Severe Benign Prostatic Hyperplasia: A Cost-Effectiveness Study. Prostate Cancer Prostatic Dis. 2022, 1–6. Available online: https://www.nature.com/articles/s41391-022-00561-2 (accessed on 28 December 2022).
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomized Studies in Meta-Analysis; Ottawa Hospital Research Institute: Ottawa, ON, Canada, 2011. [Google Scholar]
- Watson, V.; Ryan, M.; Brown, C.T.; Barnett, G.; Ellis, B.W.; Emberton, M. Eliciting Preferences for Drug Treatment of Lower Urinary Tract Symptoms Associated with Benign Prostatic Hyperplasia. J. Urol. 2004, 172, 2321–2325. Available online: https://pubmed.ncbi.nlm.nih.gov/15538258/ (accessed on 5 November 2022). [CrossRef]
- Wu, J.M.; Fulton, R.G.; Amundsen, C.L.; Knight, S.K.; Kuppermann, M. Patient Preferences for Different Severities of and Treatments for Overactive Bladder. Female Pelvic Med. Reconstr. Surg. 2011, 17, 184–189. Available online: https://pubmed.ncbi.nlm.nih.gov/22453849/ (accessed on 5 November 2022). [CrossRef]
- Fourcade, R.-O.; Lacoin, F.; Rouprêt, M.; Slama, A.; Le Fur, C.; Michel, E.; Sitbon, A.; Cotté, F.-E. Outcomes and general health-related quality of life among patients medically treated in general daily practice for lower urinary tract symptoms due to benign prostatic hyperplasia. World J. Urol. 2012, 30, 419–426. [Google Scholar] [CrossRef]
- Chhatre, S.; Newman, D.K.; Wein, A.J.; Jayadevappa, R. Patient Preference Elicitation Instrument, OABCare, to Facilitate Shared Decision-Making in the Care of Overactive Bladder. Neurourol. Urodyn. 2021, 40, 791–801. Available online: https://pubmed.ncbi.nlm.nih.gov/33565118/ (accessed on 5 November 2022). [CrossRef]
- Ryan, M.; Gerard, K. Using Discrete Choice Experiments to Value Health Care Programmes: Current Practice and Future Research Reflections. Appl. Health Econ. Health Policy 2003, 2, 55–64. Available online: https://pubmed.ncbi.nlm.nih.gov/14619274/ (accessed on 5 November 2022).
- Ryan, M.; Scott, D.A.; Donaldson, C. Valuing Health Care Using Willingness to Pay: A Comparison of the Payment Card and Dichotomous Choice Methods. J. Health Econ. 2004, 23, 237–258. Available online: https://pubmed.ncbi.nlm.nih.gov/15019754/ (accessed on 5 November 2022). [CrossRef]
- Bai, F.; Ling, J.; Esoimeme, G.; Yao, L.; Wang, M.; Huang, J.; Shi, A.; Cao, Z.; Chen, Y.; Tian, J.; et al. A Systematic Review of Questionnaires about Patient’s Values and Preferences in Clinical Practice Guidelines. Patient Prefer Adherence 2018, 12, 2309–2323. Available online: https://pubmed.ncbi.nlm.nih.gov/30464419/ (accessed on 5 November 2022). [CrossRef]
- Athavale, A.; Gooch, K.; Walker, D.; Suh, M.; Scaife, J.; Haber, A.; Hadker, N.; Dmochowski, R. A Patient-Reported, Non-Interventional, Cross-Sectional Discrete Choice Experiment to Determine Treatment Attribute Preferences in Treatment-Naïve Overactive Bladder Patients in the US. Patient Prefer Adherence 2018, 12, 2139–2152. Available online: https://pubmed.ncbi.nlm.nih.gov/30349208/ (accessed on 15 October 2022). [CrossRef]
- Heisen, M.; Baeten, S.A.; Verheggen, B.G.; Stoelzel, M.; Hakimi, Z.; Ridder, A.; van Maanen, R.; Stolk, E.A. Patient and Physician Preferences for Oral Pharmacotherapy for Overactive Bladder: Two Discrete Choice Experiments. Curr. Med. Res. Opin. 2016, 32, 787–796. Available online: https://pubmed.ncbi.nlm.nih.gov/26789823/ (accessed on 5 November 2022). [CrossRef]
- Swinburn, P.; Lloyd, A.; Ali, S.; Hashmi, N.; Newal, D.; Najib, H. Preferences for Antimuscarinic Therapy for Overactive Bladder. BJU Int. 2011, 108, 868–873. Available online: https://pubmed.ncbi.nlm.nih.gov/21105989/ (accessed on 5 November 2022). [CrossRef]
- Decalf, V.H.; Huion, A.M.J.; Benoit, D.F.; Denys, M.A.; Petrovic, M.; Everaert, K.C.M.M. Older People’s Preferences for Side Effects Associated with Antimuscarinic Treatments of Overactive Bladder: A Discrete-Choice Experiment. Drugs Aging 2017, 34, 615–623. Available online: https://pubmed.ncbi.nlm.nih.gov/28656509/ (accessed on 15 October 2022). [CrossRef]
- Harpe, S.E.; Szeinbach, S.L.; Caswell, R.J.; Corey, R.; McAuley, J.W. The Relative Importance of Health Related Quality of Life and Prescription Insurance Coverage in the Decision to Pharmacologically Manage Symptoms of Overactive Bladder. J. Urol. 2007, 178, 2532–2536. Available online: https://pubmed.ncbi.nlm.nih.gov/17937937/ (accessed on 15 October 2022). [CrossRef]
- Hashim, H.; Beusterien, K.; Bridges, J.F.P.; Amos, K.; Cardozo, L. Patient Preferences for Treating Refractory Overactive Bladder in the UK. Int. Urol. Nephrol. 2015, 47, 1619–1627. Available online: https://pubmed.ncbi.nlm.nih.gov/26347077/ (accessed on 5 November 2022). [CrossRef]
- Sanders, P.M.H.; Ijzerman, M.J.; Roach, M.J.; Gustafson, K.J. Patient Preferences for Next Generation Neural Prostheses to Restore Bladder Function. Spinal Cord 2011, 49, 113–119. Available online: https://pubmed.ncbi.nlm.nih.gov/20531360/ (accessed on 15 October 2022). [CrossRef]
- Fontaine, C.L.; Rudd, I.; Pakzad, M.; Hamid, R.; Ockrim, J.L.; Greenwell, T.J. Patient Treatment Preferences for Symptomatic Refractory Urodynamic Idiopathic Detrusor Overactivity. Urol. Ann. 2017, 9, 249–252. Available online: https://pubmed.ncbi.nlm.nih.gov/28794591/ (accessed on 5 November 2022).
- Te Dorsthorst, M.; van Balken, M.; Janssen, D.; Heesakkers, J.; Martens, F. Real-Life Patient Experiences of TTNS in the Treatment of Overactive Bladder Syndrome. Ther. Adv. Urol. 2021, 13, 17562872211041470. Available online: https://pubmed.ncbi.nlm.nih.gov/34484428/ (accessed on 5 November 2022). [CrossRef]
- Agarwal, A.; Eryuzlu, L.N.; Cartwright, R.; Thorlund, K.; Tammela, T.L.; Guyatt, G.H.; Auvinen, A.; Tikkinen, K.A. What Is the Most Bothersome Lower Urinary Tract Symptom? Individual- and Population-level Perspectives for Both Men and Women. Eur. Urol. 2014, 65, 1211–1217. [Google Scholar] [CrossRef]
- Vouri, S.M.; Kebodeaux, C.D.; Stranges, P.M.; Teshome, B.F. Adverse Events and Treatment Discontinuations of Antimuscarinics for the Treatment of Overactive Bladder in Older Adults: A Systematic Review and Meta-Analysis. Arch. Gerontol. Geriatr. 2017, 69, 77–96. Available online: http://www.ncbi.nlm.nih.gov/pubmed/27889591 (accessed on 11 November 2018). [CrossRef]
- De Nunzio, C.; Presicce, F.; Lombardo, R.; Trucchi, A.; Bellangino, M.; Tubaro, A.; Moja, E. Patient centred care for the medical treatment of lower urinary tract symptoms in patients with benign prostatic obstruction: A key point to improve patients’ care—A systematic review. BMC Urol. 2018, 18, 62. [Google Scholar] [CrossRef]
- De Nunzio, C.; Presicce, F.; Pirozzi, L.; Castellan, P.; Schips, L.; Cindolo, L.; Lombardo, R.; Tubaro, A. The current indications and the benefits of combining a β3-agonist with an anticholinergic for the treatment of OAB. Curr. Drug Targets 2015, 16, 1198–1206. [Google Scholar] [CrossRef]
- De Nunzio, C.; Nacchia, A.; Cicione, A.; Sica, A.; Baldassarri, V.; Voglino, O.; Mancini, E.; Guarnotta, G.; Trucchi, A.; Tubaro, A. Night Shift Workers Refer Higher Urinary Symptoms with an Impairment Quality of Life: A Single Cohort Study. Minerva Urol. Nefrol. 2021, 73, 831–835. Available online: http://www.ncbi.nlm.nih.gov/pubmed/32284530 (accessed on 21 September 2020).
- De Nunzio, C.; Brucker, B.; Bschleipfer, T.; Cornu, J.N.; Drake, M.J.; Fusco, F.; Gravas, S.; Oelke, M.; Peyronnet, B.; Tutolo, M. Beyond Antimuscarinics: A Review of Pharmacological and Interventional Options for Overactive Bladder Management in Men. Eur. Urol. 2021, 79, 492–504. Available online: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85098970229&doi=10.1016%2Fj.eururo.2020.12.032&partnerID=40&md5=982502be04f61ce7e7a2714be30eabde (accessed on 5 November 2022). [CrossRef]
- De Nunzio, C.; Cicione, A.; Izquierdo, L.; Lombardo, R.; Tema, G.; Lotrecchiano, G.; Minervini, A.; Simone, G.; Cindolo, L.; D’Orta, C.; et al. Multicenter Analysis of Postoperative Complications in Octogenarians After Radical Cystectomy and Ureterocutaneostomy: The Role of the Frailty Index. Clin. Genitourin. Cancer 2019, 17, 402–407. [Google Scholar] [CrossRef]
- Chesnut, G.T.; Tin, A.L.; Fleshner, K.A.; Benfante, N.E.; Vickers, A.J.; Eastham, J.A.; Sjoberg, D.D.; Carlsson, S.V. Estimating Patient Health in Prostate Cancer Treatment Counseling. Prostate Cancer Prostatic Dis. 2021. Available online: https://pubmed.ncbi.nlm.nih.gov/34732855/ (accessed on 5 November 2022).
- Malde, S.; Umbach, R.; Wheeler, J.R.; Lytvyn, L. A Systematic Review of Patients’ Values, Preferences, and Expectations for the Diagnosis and Treatment of Male Lower Urinary Tract Symptoms. Eur. Urol. 2021, 79, 796–809. [Google Scholar] [CrossRef]
- Ornaghi, P.I.; Porreca, A.; Sandri, M.; Sciarra, A.; Falsaperla, M.; Ludovico, G.M.; Cerruto, M.A.; Antonelli, A. Features of Patients Referring to the Outpatient Office Due to Benign Prostatic Hyperplasia: Analysis of a National Prospective Cohort of 5815 Cases. Prostate Cancer Prostatic Dis. 2022, 1–6. Available online: https://www.nature.com/articles/s41391-022-00575-w (accessed on 28 December 2022).
- Huang, J.; Chan, C.-K.; Yee, S.; Deng, Y.; Bai, Y.; Chan, S.C.; Tin, M.S.; Liu, X.; Lok, V.; Zhang, L.; et al. Global Burden and Temporal Trends of Lower Urinary Tract Symptoms: A Systematic Review and Meta-Analysis. Prostate Cancer Prostatic Dis. 2022, 1–8. Available online: https://www.nature.com/articles/s41391-022-00610-w (accessed on 28 December 2022).
- Welliver, C.; Feinstein, L.; Ward, J.B.; Kirkali, Z.; Martinez-Miller, E.E.; Matlaga, B.R.; McVary, K. Poor Clinical Guideline Adherence and Inappropriate Testing for Incident Lower Urinary Tract Symptoms Associated with Benign Prostatic Hyperplasia. Prostate Cancer Prostatic Dis. 2021, 25, 269–273. Available online: https://www.nature.com/articles/s41391-021-00435-z (accessed on 28 December 2022). [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).