Anxiety and Depression Levels in Parents after Counselling for Fetal Heart Disease
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Study Setting
2.2. Variables and Assessment Measures
2.3. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Education and Profession
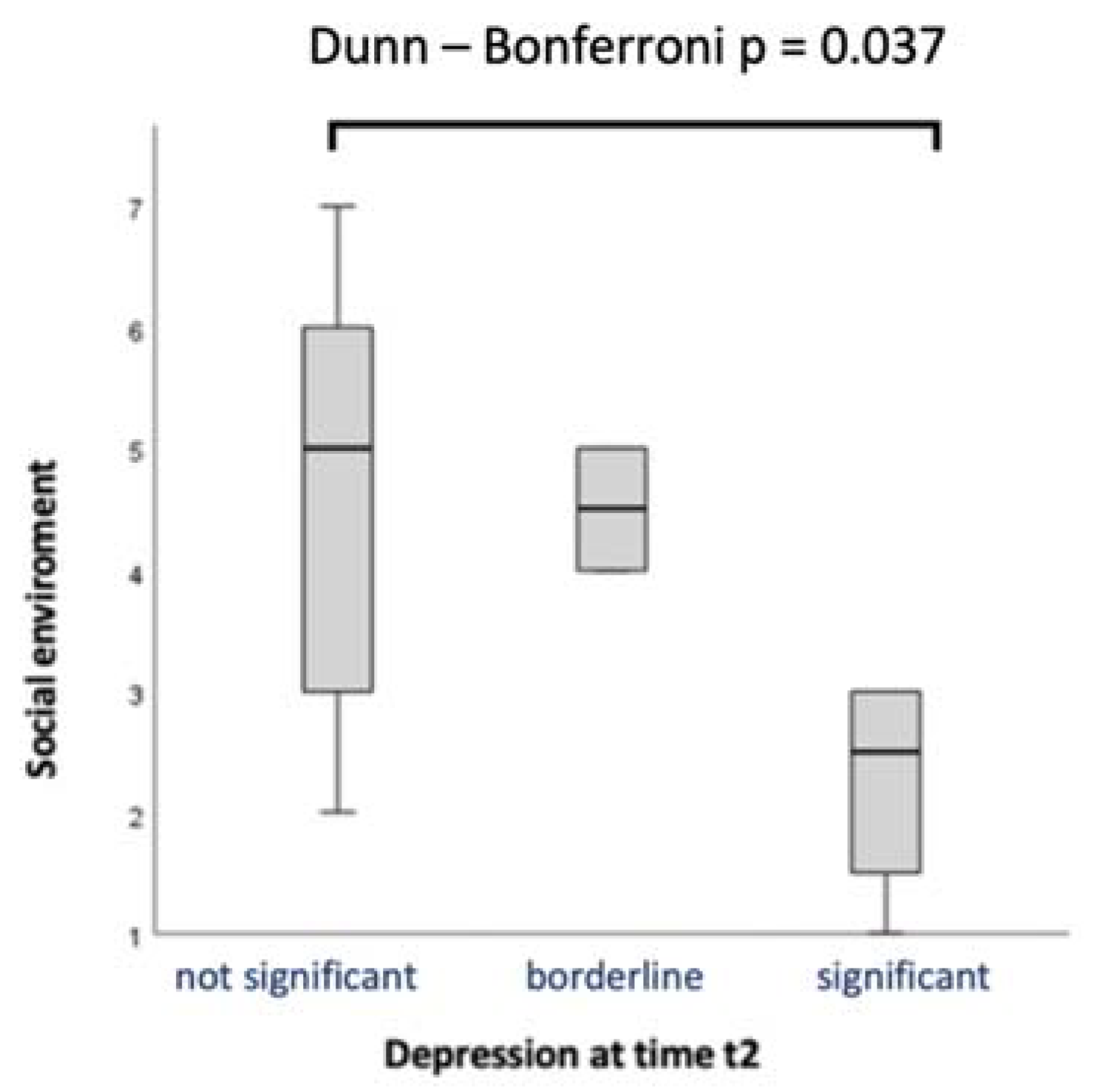
3.3. Family Structure and Social Environment
3.4. Gender Aspects and Pregnancy
3.5. Results of the Hospital Anxiety and Depression Scale
3.6. Differences between Time Points
3.7. Predictors for Mental Stress
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hoffman, J.I.; Kaplan, S. The incidence of congenital heart disease. J. Am. Coll. Cardiol. 2002, 39, 1890–1900. [Google Scholar] [CrossRef] [PubMed]
- Lytzen, R.; Vejlstrup, N.; Bjerre, J.; Bjorn Petersen, O.; Leenskjold, S.; Keith Dodd, J.; Stener Jorgensen, F.; Sondergaard, L. The accuracy of prenatal diagnosis of major congenital heart disease is increasing. J. Obstet. Gynaecol. 2020, 40, 308–315. [Google Scholar] [CrossRef] [PubMed]
- Gardiner, H.M.; Kovacevic, A.; van der Heijden, L.B.; Pfeiffer, P.W.; Franklin, R.C.; Gibbs, J.L.; Averiss, I.E.; Larovere, J.M. Prenatal screening for major congenital heart disease: Assessing performance by combining national cardiac audit with maternity data. Heart 2014, 100, 375–382. [Google Scholar] [CrossRef]
- Jone, P.N.; Schowengerdt, K.O., Jr. Prenatal diagnosis of congenital heart disease. Pediatr. Clin. N. Am. 2009, 56, 709–715. [Google Scholar] [CrossRef]
- Yin, X.; Sun, N.; Jiang, N.; Xu, X.; Gan, Y.; Zhang, J.; Qiu, L.; Yang, C.; Shi, X.; Chang, J.; et al. Prevalence and associated factors of antenatal depression: Systematic reviews and meta-analyses. Clin. Psychol. Rev. 2021, 83, 101932. [Google Scholar] [CrossRef]
- Dennis, C.L.; Falah-Hassani, K.; Shiri, R. Prevalence of antenatal and postnatal anxiety: Systematic review and meta-analysis. Br. J. Psychiatry 2017, 210, 315–323. [Google Scholar] [CrossRef]
- Dagklis, T.; Papazisis, G.; Tsakiridis, I.; Chouliara, F.; Mamopoulos, A.; Rousso, D. Prevalence of antenatal depression and associated factors among pregnant women hospitalized in a high-risk pregnancy unit in Greece. Soc. Psychiatry Psychiatr. Epidemiol. 2016, 51, 1025–1031. [Google Scholar] [CrossRef]
- Woolf-King, S.E.; Anger, A.; Arnold, E.A.; Weiss, S.J.; Teitel, D. Mental Health Among Parents of Children With Critical Congenital Heart Defects: A Systematic Review. J. Am. Heart Assoc. 2017, 6, e004862. [Google Scholar] [CrossRef] [PubMed]
- Sood, E.; Lisanti, A.J.; Woolf-King, S.E.; Wray, J.; Kasparian, N.; Jackson, E.; Gregory, M.R.; Lopez, K.N.; Marino, B.S.; Neely, T.; et al. Parent mental health and family functioning following diagnosis of CHD: A research agenda and recommendations from the Cardiac Neurodevelopmental Outcome Collaborative. Cardiol. Young 2021, 31, 900–914. [Google Scholar] [CrossRef]
- Misri, S.; Kendrick, K.; Oberlander, T.F.; Norris, S.; Tomfohr, L.; Zhang, H.; Grunau, R.E. Antenatal depression and anxiety affect postpartum parenting stress: A longitudinal, prospective study. Can. J. Psychiatry 2010, 55, 222–228. [Google Scholar] [CrossRef]
- Glover, V. Maternal depression, anxiety and stress during pregnancy and child outcome; what needs to be done. Best Pract. Res. Clin. Obstet. Gynaecol. 2014, 28, 25–35. [Google Scholar] [CrossRef] [PubMed]
- Dunkel Schetter, C.; Tanner, L. Anxiety, depression and stress in pregnancy: Implications for mothers, children, research, and practice. Curr. Opin. Psychiatry 2012, 25, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Arya, B.; Glickstein, J.S.; Levasseur, S.M.; Williams, I.A. Parents of children with congenital heart disease prefer more information than cardiologists provide. Congenit. Heart Dis. 2013, 8, 78–85. [Google Scholar] [CrossRef] [PubMed]
- Allan, L.D.; Huggon, I.C. Counselling following a diagnosis of congenital heart disease. Prenat. Diagn. 2004, 24, 1136–1142. [Google Scholar] [CrossRef] [PubMed]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Bjelland, I.; Dahl, A.A.; Haug, T.T.; Neckelmann, D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J. Psychosom. Res. 2002, 52, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Herrmann-Lingen, C.; Buss, U.; Snaith, P. Deutsche Adaptation der Hospital Anxiety and Depression Scale (HADS); von Snaith, R.P., Zigmond, A.S., Eds.; Huber: Bern, Switzerland, 2011. [Google Scholar]
- Lodhi, F.S.; Elsous, A.M.; Irum, S.; Khan, A.A.; Rabbani, U. Psychometric properties of the Urdu version of the Hospital Anxiety and Depression Scale (HADS) among pregnant women in Abbottabad, Pakistan. Gen. Psychiatry 2020, 33, e100276. [Google Scholar] [CrossRef]
- Abiodun, O.A. A validity study of the Hospital Anxiety and Depression Scale in general hospital units and a community sample in Nigeria. Br. J. Psychiatry 1994, 165, 669–672. [Google Scholar] [CrossRef]
- Bjelland, I.; Krokstad, S.; Mykletun, A.; Dahl, A.A.; Tell, G.S.; Tambs, K. Does a higher educational level protect against anxiety and depression? The HUNT study. Soc. Sci. Med. 2008, 66, 1334–1345. [Google Scholar] [CrossRef]
- Lorant, V.; Deliege, D.; Eaton, W.; Robert, A.; Philippot, P.; Ansseau, M. Socioeconomic inequalities in depression: A meta-analysis. Am. J. Epidemiol. 2003, 157, 98–112. [Google Scholar] [CrossRef]
- Miech, R.A.; Shanahan, M.J. Socioeconomic Status and Depression over the Life Course. J. Health Soc. Behav. 2000, 41, 162–176. [Google Scholar] [CrossRef]
- Miech, R.A.; Caspi, A.; Moffitt, T.E.; Wright, B.R.E.; Silva, P.A. Low Socioeconomic Status and Mental Disorders: A Longitudinal Study of Selection and Causation during Young Adulthood. Am. J. Sociol. 1999, 104, 1096–1131. [Google Scholar] [CrossRef]
- van de Loo, K.F.E.; Vlenterie, R.; Nikkels, S.J.; Merkus, P.; Roukema, J.; Verhaak, C.M.; Roeleveld, N.; van Gelder, M. Depression and anxiety during pregnancy: The influence of maternal characteristics. Birth 2018, 45, 478–489. [Google Scholar] [CrossRef]
- Nisar, A.; Yin, J.; Waqas, A.; Bai, X.; Wang, D.; Rahman, A.; Li, X. Prevalence of perinatal depression and its determinants in Mainland China: A systematic review and meta-analysis. J. Affect. Disord. 2020, 277, 1022–1037. [Google Scholar] [CrossRef] [PubMed]
- Christensen, U.; Schmidt, L.; Kriegbaum, M.; Hougaard, C.O.; Holstein, B.E. Coping with unemployment: Does educational attainment make any difference? Scand. J. Public Health 2006, 34, 363–370. [Google Scholar] [CrossRef]
- Niemeyer, H.; Bieda, A.; Michalak, J.; Schneider, S.; Margraf, J. Education and mental health: Do psychosocial resources matter? SSM Popul. Health 2019, 7, 100392. [Google Scholar] [CrossRef]
- Chen, J.; Cross, W.M.; Plummer, V.; Lam, L.; Sun, M.; Qin, C.; Tang, S. The risk factors of antenatal depression: A cross-sectional survey. J. Clin. Nurs. 2019, 28, 3599–3609. [Google Scholar] [CrossRef]
- Gonzalez-Mesa, E.; Kabukcuoglu, K.; Blasco, M.; Korukcu, O.; Ibrahim, N.; Gonzalez-Cazorla, A.; Cazorla, O. Comorbid anxiety and depression (CAD) at early stages of the pregnancy. A multicultural cross-sectional study. J. Affect. Disord. 2020, 270, 85–89. [Google Scholar] [CrossRef]
- Teixeira, C.; Figueiredo, B.; Conde, A.; Pacheco, A.; Costa, R. Anxiety and depression during pregnancy in women and men. J. Affect. Disord. 2009, 119, 142–148. [Google Scholar] [CrossRef]
- Glazier, R.H.; Elgar, F.J.; Goel, V.; Holzapfel, S. Stress, social support, and emotional distress in a community sample of pregnant women. J. Psychosom. Obstet. Gynecol. 2004, 25, 247–255. [Google Scholar] [CrossRef]
- Vignato, J.; Perkhounkova, Y.; McCarthy, A.M.; Segre, L.S. Pain and Depression Symptoms During the Third Trimester of Pregnancy. MCN Am. J. Matern. Child Nurs. 2020, 45, 351–356. [Google Scholar] [CrossRef]
- Lee, A.M.; Lam, S.K.; Sze Mun Lau, S.M.; Chong, C.S.; Chui, H.W.; Fong, D.Y. Prevalence, course, and risk factors for antenatal anxiety and depression. Obstet. Gynecol. 2007, 110, 1102–1112. [Google Scholar] [CrossRef]
- Brittain, K.; Myer, L.; Koen, N.; Koopowitz, S.; Donald, A.K.; Barnett, W.; Zar, H.J.; Stein, D.J. Risk Factors for Antenatal Depression and Associations with Infant Birth Outcomes: Results From a South African Birth Cohort Study. Paediatr. Perinat. Epidemiol. 2015, 29, 505–514. [Google Scholar] [CrossRef]
- Raisanen, S.; Lehto, S.M.; Nielsen, H.S.; Gissler, M.; Kramer, M.R.; Heinonen, S. Risk factors for and perinatal outcomes of major depression during pregnancy: A population-based analysis during 2002–2010 in Finland. BMJ Open 2014, 4, e004883. [Google Scholar] [CrossRef]
- Adewuya, A.O.; Ola, B.A.; Aloba, O.O.; Dada, A.O.; Fasoto, O.O. Prevalence and correlates of depression in late pregnancy among Nigerian women. Depress. Anxiety 2007, 24, 15–21. [Google Scholar] [CrossRef]
- Zeng, Y.; Cui, Y.; Li, J. Prevalence and predictors of antenatal depressive symptoms among Chinese women in their third trimester: A cross-sectional survey. BMC Psychiatry 2015, 15, 66. [Google Scholar] [CrossRef]
- Savory, N.A.; Hannigan, B.; John, R.M.; Sanders, J.; Garay, S.M. Prevalence and predictors of poor mental health among pregnant women in Wales using a cross-sectional survey. Midwifery 2021, 103, 103103. [Google Scholar] [CrossRef]
- Thoits, P.A. Social support as coping assistance. J. Consult. Clin. Psychol. 1986, 54, 416–423. [Google Scholar] [CrossRef]
- Figueiredo, B.; Conde, A. Anxiety and depression in women and men from early pregnancy to 3-months postpartum. Arch. Women’s Ment. Health 2011, 14, 247–255. [Google Scholar] [CrossRef]
- Carlsson, T.; Mattsson, E. Emotional and cognitive experiences during the time of diagnosis and decision-making following a prenatal diagnosis: A qualitative study of males presented with congenital heart defect in the fetus carried by their pregnant partner. BMC Pregnancy Childbirth 2018, 18, 26. [Google Scholar] [CrossRef]
- Noble, R.E. Depression in women. Metabolism 2005, 54, 49–52. [Google Scholar] [CrossRef]
- Huizink, A.C.; Mulder, E.J.; Robles de Medina, P.G.; Visser, G.H.; Buitelaar, J.K. Is pregnancy anxiety a distinctive syndrome? Early Hum. Dev. 2004, 79, 81–91. [Google Scholar] [CrossRef]
- Hoffman, M.F.; Karpyn, A.; Christofferson, J.; Neely, T.; McWhorter, L.G.; Demianczyk, A.C.; James Mslis, R.; Hafer, J.; Kazak, A.E.; Sood, E. Fathers of Children With Congenital Heart Disease: Sources of Stress and Opportunities for Intervention. Pediatr. Crit. Care Med. 2020, 21, e1002–e1009. [Google Scholar] [CrossRef]
- Lin, P.J.; Liu, Y.T.; Huang, C.H.; Huang, S.H.; Chen, C.W. Caring perceptions and experiences of fathers of children with congenital heart disease: A systematic review of qualitative evidence. Int. J. Nurs. Pract. 2021, 27, e12952. [Google Scholar] [CrossRef]
- Sood, E.; Karpyn, A.; Demianczyk, A.C.; Ryan, J.; Delaplane, E.A.; Neely, T.; Frazier, A.H.; Kazak, A.E. Mothers and Fathers Experience Stress of Congenital Heart Disease Differently: Recommendations for Pediatric Critical Care. Pediatr. Crit Care Med. 2018, 19, 626–634. [Google Scholar] [CrossRef] [PubMed]
- Hwang, J.H.; Chae, S.M. Experiences of Fathers of Young Children With Severe Congenital Heart Defects in Korea: A Qualitative Descriptive Study. J. Pediatr. Nurs. 2020, 53, e108–e113. [Google Scholar] [CrossRef] [PubMed]
- Kovacevic, A.; Wacker-Gussmann, A.; Bar, S.; Elsasser, M.; Mohammadi Motlagh, A.; Ostermayer, E.; Oberhoffer-Fritz, R.; Ewert, P.; Gorenflo, M.; Starystach, S. Parents’ Perspectives on Counseling for Fetal Heart Disease: What Matters Most? J. Clin. Med. 2022, 11, 278. [Google Scholar] [CrossRef]
- Kovacevic, A.; Elsasser, M.; Fluhr, H.; Muller, A.; Starystach, S.; Bar, S.; Gorenflo, M. Counseling for fetal heart disease-current standards and best practice. Transl. Pediatr. 2021, 10, 2225–2234. [Google Scholar] [CrossRef]
- Bratt, E.L.; Jarvholm, S.; Ekman-Joelsson, B.M.; Mattson, L.A.; Mellander, M. Parent’s experiences of counselling and their need for support following a prenatal diagnosis of congenital heart disease--a qualitative study in a Swedish context. BMC Pregnancy Childbirth 2015, 15, 171. [Google Scholar] [CrossRef] [PubMed]
- Menahem, S.; Grimwade, J. Counselling strategies in the prenatal diagnosis of major heart abnormality. Heart Lung Circ. 2004, 13, 261–265. [Google Scholar] [CrossRef]
- Lee, C.K. Prenatal Counseling of Fetal Congenital Heart Disease. Curr. Treat. Options Cardiovasc. Med. 2017, 19, 5. [Google Scholar] [CrossRef]
- Gdanska, P.; Drozdowicz-Jastrzebska, E.; Grzechocinska, B.; Radziwon-Zaleska, M.; Wegrzyn, P.; Wielgos, M. Anxiety and depression in women undergoing infertility treatment. Ginekol. Pol. 2017, 88, 109–112. [Google Scholar] [CrossRef] [PubMed]
- Tiller, J.W. Depression and anxiety. Med. J. Aust. 2013, 199, S28–S31. [Google Scholar] [CrossRef] [PubMed]
- Andersson, L.; Sundstrom-Poromaa, I.; Wulff, M.; Astrom, M.; Bixo, M. Depression and anxiety during pregnancy and six months postpartum: A follow-up study. Acta Obstet. Et Gynecol. Scand. 2006, 85, 937–944. [Google Scholar] [CrossRef]
- Middeldorp, C.M.; Cath, D.C.; Van Dyck, R.; Boomsma, D.I. The co-morbidity of anxiety and depression in the perspective of genetic epidemiology. A review of twin and family studies. Psychol Med. 2005, 35, 611–624. [Google Scholar] [CrossRef]
- Boyer, P. Do anxiety and depression have a common pathophysiological mechanism? Acta Psychiatr. Scand. 2000, 24–29. [Google Scholar] [CrossRef]
| Frequency | Percentage (%) | Valid Percentage (%) | Cumulative Percentage (%) | ||
|---|---|---|---|---|---|
| Native language | German | 66 | 85.7 | 85.7 | 85.7 |
| Other | 7 | 9.1 | 9.1 | 94.8 | |
| German and other | 4 | 5.2 | 5.2 | 100 | |
| Country of birth | Germany | 67 | 87.0 | 87.0 | 87.0 |
| Abroad | 10 | 13.0 | 13.0 | 100.0 |
| HADS A (n = 76) | HADS D (n = 76) | HADS A t2 (n = 24) | HADS D t2 (n = 24) | |
|---|---|---|---|---|
| ”Not significant” | 53 (69.7%) | 65 (85.5%) | 15 (62.5%) | 18 (75%) |
| ”Borderline” | 14 (18.4%) | 6 (7.9%) | 3 (12.5%) | 2 (8.3%) |
| ”Significant” | 9 (11.8%) | 5 (6.6%) | 6 (25.0%) | 4 (16.7%) |
| mean (SD) | 5.97 (3.521 | 3.83 (3.446) | 6.38 (4.871) | 24 (100%) |
| Anxiety at t1 | Depression at t1 | ||||||
|---|---|---|---|---|---|---|---|
| Not Significant n (%) | Significant n (%) | p-Value * | Not Significant n (%) | Significant n (%) | p-Value * | ||
| Sex | Female | 23 (51.1%) | 22 (48.9%) | 0.165 | 36 (80%) | 9 (20%) | 0.183 |
| Male | 21 (67.7%) | 10 (32.3%) | 29 (93.5%) | 2 (6.5%) | |||
| Medical assisted pregnancy | No | 39 (60%) | 26 (40%) | 0.511 | 57 (87.7%) | 8 (12.3%) | 0.192 |
| Yes | 5 (45.5%) | 6 (54.5%) | 8 (72.7%) | 3 (27.3%) | |||
| Planned pregnancy | No | 2 (50%) | 2 (50%) | 1.000 | 2 (50%) | 2 (50%) | 0.098 |
| Yes | 42 (58.3%) | 30 (41.7%) | 63 (87.5%) | 9 (12.5%) | |||
| Social environment | No | 0 (0%) | 0 (0%) | --- | 0 (0%) | 0 (0%) | --- |
| Yes | 44 (57.9%) | 32 (42.1%) | 65 (85.5%) | 11 (14.5%) | |||
| Number of children | None | 17 (54.8%) | 14 (45.2%) | 0.813 | 24 (77.4%) | 7 (22.6%) | 0.111 |
| ≥ 1 child | 27 (60%) | 18 (40%) | 41 (91.1%) | 4 (8.9%) | |||
| Surgery | No | 0 (0%) | 2 (100%) | 0.481 | 1 (50%) | 1 (50%) | 0.342 |
| Yes | 13 (52%) | 12 (48%) | 21 (84%) | 4 (16%) | |||
| Occupational field | Other | 35 (68.6%) | 16 (31.4%) | 0.082 | 47 (92.2%) | 4 (7.8%) | 0.355 |
| Health, social affairs, teaching, education | 7 (41.2%) | 10 (58.8%) | 14 (82.4%) | 3 (17.6%) | |||
| Social envirnoment including mother | No | 9 (40.9%) | 13 (59.1%) | 0.700 | 18 (81.8%) | 4 (18.2%) | 0.721 |
| Yes | 35 (66%) | 18 (34%) | 46 (86.8%) | 7 (13.2%) | |||
| Occupation | In education | 0 (0%) | 0 (0%) | 0.087 | 0 (0%) | 0 (0%) | 0.115 |
| Partly employed | 3 (75%) | 1 (25%) | 3 (75%) | 1 (25%) | |||
| Employed | 36 (59%) | 25 (41%) | 54 (88.5%) | 7 (11.5%) | |||
| Self-employed | 3 (100%) | 0 (0%) | 3 (100%) | 0 (0%) | |||
| Unemployed | 0 (0%) | 3 (100%) | 1 (33.3%) | 2 (66.7%) | |||
| Unable to work | 1 (100%) | 0 (0%) | 1 (100%) | 0 (0%) | |||
| Marital status | Married | 28 (54.9%) | 23 (45.1%) | 0.452 | 40 (78.4%) | 11 (21.6%) | 0.013 |
| In a relationship | 16 (66.7%) | 8 (33.3%) | 24 (100%) | 0 (0%) | |||
| Single | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | |||
| Divorced | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | |||
| Widowed | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | |||
| * Fisher‘s test | |||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Erbas, G.S.; Herrmann-Lingen, C.; Ostermayer, E.; Kovacevic, A.; Oberhoffer-Fritz, R.; Ewert, P.; Wacker-Gussmann, A. Anxiety and Depression Levels in Parents after Counselling for Fetal Heart Disease. J. Clin. Med. 2023, 12, 394. https://doi.org/10.3390/jcm12010394
Erbas GS, Herrmann-Lingen C, Ostermayer E, Kovacevic A, Oberhoffer-Fritz R, Ewert P, Wacker-Gussmann A. Anxiety and Depression Levels in Parents after Counselling for Fetal Heart Disease. Journal of Clinical Medicine. 2023; 12(1):394. https://doi.org/10.3390/jcm12010394
Chicago/Turabian StyleErbas, Gizem Seyda, Christoph Herrmann-Lingen, Eva Ostermayer, Alexander Kovacevic, Renate Oberhoffer-Fritz, Peter Ewert, and Annette Wacker-Gussmann. 2023. "Anxiety and Depression Levels in Parents after Counselling for Fetal Heart Disease" Journal of Clinical Medicine 12, no. 1: 394. https://doi.org/10.3390/jcm12010394
APA StyleErbas, G. S., Herrmann-Lingen, C., Ostermayer, E., Kovacevic, A., Oberhoffer-Fritz, R., Ewert, P., & Wacker-Gussmann, A. (2023). Anxiety and Depression Levels in Parents after Counselling for Fetal Heart Disease. Journal of Clinical Medicine, 12(1), 394. https://doi.org/10.3390/jcm12010394






