Abstract
Many variables obtained during cardiopulmonary exercise test (CPET), including O2 uptake (VO2) versus heart rate (HR, O2-pulse) and work rate (VO2/Watt), provide quantitative patterns of responses to exercise when left ventricular dysfunction is an effect of myocardial ischemia (MI). Therefore, CPET offers a unique approach to evaluate exercise-induced MI in the presence of fixed or dynamic coronary arteries stenosis. In this paper, we examined the case of a 74-year-old patient presenting with an ischemic CPET and a normal stress cardiac magnetic resonance (CMR) with dipyridamole. A coronary angiography demonstrated the presence of myocardial bridging (MB), a well-known congenital coronary anomaly that is able to generate MI during exercise (but not in provocative testing using coronary artery vasodilators, such as dipyridamole). Despite the good diagnostic accuracy of the imaging methods (i.e., stress CMR) in MI detection, this case shows that exercise should be the method of choice in elicit ischemia in specific cases, like MB.
1. Introduction
Several variables attained during the Cardiopulmonary Exercise Test (CPET), including O2 uptake relative to heart rate (HR, O2-pulse) and work rate (VO2/Watt), supply quantitative patterns of responses to exercise when left ventricular dysfunction is an effect of myocardial ischemia (MI) [1,2]. Specifically, O2-pulse is a CPET parameter that is calculated from the ratio of oxygen consumption (VO2) to HR. According to Fick’s law, it represents the product of stroke volume (SV) and O2 extraction. Given that this latter parameter (O2 extraction) is generally considered to be constant and predictable [3,4], the O2-pulse changes during a maximal ramp protocol CPET, which may be considered a metabolic surrogate of the SV variations [5,6,7]. Therefore, the development of exercise-induced MI may lead to loss of SV and a plateau (or fall) in O2-pulse during exercise [1]. Even if not highly specific for ischemic coronary arteries stenosis, given that these parameters (i.e., VO2/Watt and O2-pulse) also altered in other settings, such as hypertrophic cardiomyopathy [8] or dynamic mitral regurgitation, they suggest the importance of CPET in evaluating exercise-induced MI [9]. Patients with or without chest pain or dyspnea can show rapid reduction in SV as a pathological response to exercise. Myocardial bridging (MB), a congenital coronary anomaly, is a cluster of myocardial fibers crossing over the epicardial coronary arteries [10]. Although MB may be a casual finding (angiography or autopsy) or a diagnosis made in case of typical angina, patients with no symptoms may also develop MI due to dynamic systolic compression.
We present the case of a 74-year-old patient presenting with a pathological drop in O2-pulse and VO2/Watt slopes during maximal exercise and a normal stress cardiac magnetic resonance (CMR) in order to underline the importance of exercise in eliciting MI in specific cases as well as the central role of CPET in this context.
2. Case Description
A 74-year-old man, who is a sportsman (ski mountaineering) (Figure 1), was symptomatic for atypical chest pain, and underwent a maximal (respiratory exchange ratio at peak (RER) 1.1) ramp protocol CPET, showing metabolic and ECG signs of MI (Figure 2A,B). Baseline CPET data are presented in Table 1. In brief, peak VO2 was 27.7 mL/min/Kg (corresponding to 112% of the predicted VO2), peak O2-pulse was 11.4 mL/bpm (corresponding to 105% of the predicted peak O2-pulse), and maximal HR was 154 bpm (105% of the predicted maximal HR).
Figure 1.
Case presentation. A 74-year-old man with no cardiovascular history who performs high-load physical activity (multiple ski mountaineering trips) was referred for CPET following episodes of atypical chest pain. Abbreviations: CPET = Cardiopulmonary Exercise Testing.
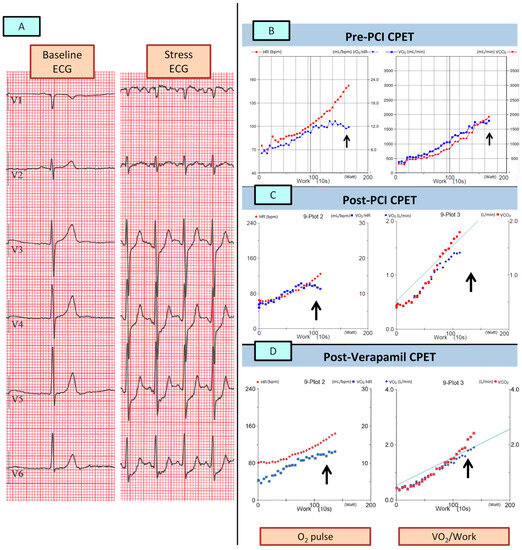
Figure 2.
Serial CPETs. The figure shows the exercise-induced ECG changes (A) and the metabolic changes in both the baseline CPET (B) and in the post-PCI CPET (C) with a clear flattening/downsloping of the O2-pulse and VO2/Work (arrows). Panel (D) shows the normalization of the metabolic behavior after the introduction of Verapamil in the medical therapyAbbreviations: CPET = Cardiopulmonary Exercise Testing; PCI = Percutaneous Coronary Intervention; VO2 = Oxygen Intake.

Table 1.
CPETs data.
A subsequent pharmacological (dipyridamole 0.14 mg/Kg/min for 6 min) stress CMR showed a normal cardiac picture (preserved biventricular function, no valvopathies, and no late-gadolinium enhancement) at rest with no induced MI (Figure 3). In view of the discrepancy between the CPET and the CMR data, a coronary angiography (CA) was performed showing single vessel coronary artery disease (CAD), with a calcified plaque on the medium right coronary artery (RCA) leading to a 70% stenosis (Figure 4A). The RCA stenosis underwent a successful percutaneous coronary intervention (PCI) without complications and with a good final angiographic result. A left descending artery (LDA) MB with a dynamic compression was also observed (Figure 4B). At two months, a follow-up same ramp maximal CPET was performed, still diagnostic for MI (Figure 2C; Table 1). The patient was treated with calcium channel blockers (Verapamil 80 mg t.d.s.), and after 2 months, another CPET was normal (no MI) (Figure 2D; Table 1).
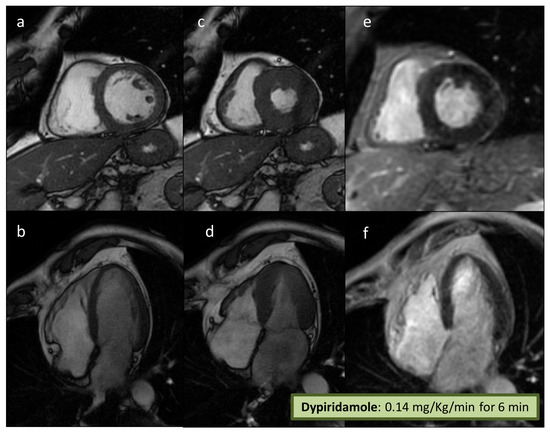
Figure 3.
Stress CMR. A stress CMR was performed to exclude MI, showing normal biventricular volumes and systolic function (a–d). No LGE was detected (e,f), and a normal dynamic response was observed after dypiridamole with no signs of MI. Abbreviations: CMR = Cardiac Magnetic Resonance; MI = Myocardial Ischemia; LGE = Late Gadolinium Enhancement.
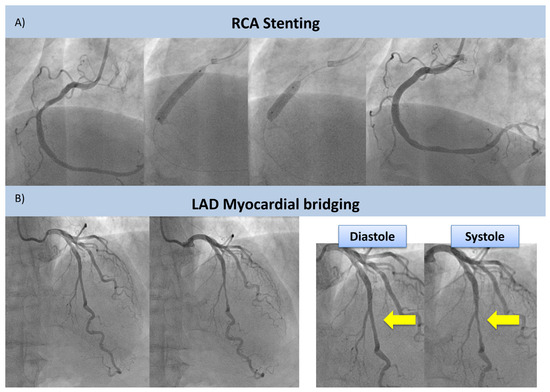
Figure 4.
CA and PCI. CA shows stenosis of the RCA undergoing successful PCI without complications (upper panel, (A)) and the presence of a MB of the LAD (lower panel, (B)). MB is showed by yellow arrows. Abbreviations: CA = Coronary Angiography; RCA = Right Coronary Artery; PCI = Percutaneous Coronary Intervention; MB = Myocardial Bridging; LAD = Left Descending Artery.
3. Discussion
This clinical case report of MB-related MI demonstrates the central role of exercise (and, in particular, its evaluation by CPET) as a provocative test in patients with “dynamic” coronary artery stenosis, such as in case of MB.
Even if stress CMR is an accurate method to assess MI in patients with known or suspected CAD [11], only a few MB patients have been systematically evaluated with this technique. In these subjects, due to a pure “steal-flow” vasodilator effect without a fixed obstruction, the use of dipyridamole during stress testing may result in an underestimation of MI compared with exercise. CPET provides a unique approach to assess MI due to the direct observation of functional changes during strong physiological exercise. In these cases, especially, the use of metabolic variables on top of electrocardiographic changes allows noninvasive estimation of the impact of exercise on SV. In this case, a sudden reduction in O2 pulse during exercise was observed, accompanied by a decrease in VO2/W slope (Figure 2B,C). These findings, more than the absolute values of these parameters (which can be still considered within the normal range), suggest an abrupt reduction in left ventricular SV due to coronary stenosis of a large-caliber coronary artery or, in special cases, due to an increase in the intraventricular dynamic gradient during exercise in HCM [8]. Moreover, in the described case, the appropriateness of myocardial revascularization by PCI of the RCA is doubtful. In fact, despite an uncomplicated PCI with an excellent final result (Figure 3a), the subsequent CPET (Figure 2C) was still diagnostic for inducible ischemia, which is a sign that the treated coronary artery lesion was not responsible for the observed ischemic changes. An approach involving an invasive evaluation of coronary reserve (e.g., with Fractional Flow Reserve (FFR)) could have guided the revascularization procedure––likely avoiding it––and could have helped in the functional evaluation of the LAD MB, as previously described [12,13].
Despite the limitations associated with the use of dipyridamole, the use of CMR in the context of MB may still be of interest, especially in selected cases [14,15], e.g., in HCM-associated forms of MB [16]. In addition, a provocative approach with a positive inotropic drug (e.g., dobutamine) would have likely been effective in eliciting myocardial ischemia. However, the use of dobutamine is made more complex during CMR because it is not always well tolerated by patients [17]. Therefore, in a non-invasive setting, the use of physiological exercise could be proposed as the method of choice in MB patients, and it could eventually be associated with echocardiography or single-photon emission computed tomography.
The absolute values of the metabolic variables obtained during the CPET of this athletic subject merit further discussion. Despite the presence of clear signs of MI, the peak exercise data obtained in the first two CPETs were well within normal limits (peak VO2 27.7 and 22.4 mL/kg/min, corresponding to 112% and 96% of the predicted, respectively, and peak O2-pulse 105% and 114% of the predicted value (Table 1)). However, in accordance with Fick’s law, which clearly demonstrates how VO2 values depend on peripheral extraction (and, therefore, on the level of training) as well as SV, in such a well-trained subject, one would expect even higher peak values. Confirming this, in the CPET performed after initiating medical therapy, despite the theoretical negative inotropic and chronotropic effects of the calcium antagonist, the peak VO2 values during exercise increased to 29.4 mL/kg/min (127% of the peak VO2 predicted) and the O2-pulse values increased to 13 mL/bpm (128% of the predicted values). These data highlight the importance of analyzing metabolic parameters not only in absolute numerical terms but also by evaluating their behavior during exercise through careful observation of the graphs.
4. Conclusions
We described the case of a sporty patient with MB, and, for this patient, a maximal CPET proved superior to stress CMR with dipyridamole in identifying signs of MI. This case highlights the importance of exercise in eliciting ischemia in specific cases.
Author Contributions
Conceptualization M.M. and E.S.; Investigation M.M., D.M., U.A. and E.P.; writing—original draft preparation, M.M., E.S., U.A., I.M. and D.M.; writing—review and editing, M.M., E.P., G.C. and P.A.; visualization, M.M., I.M., P.P. and P.A.; supervision, P.P., G.C. and P.A. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Italian Ministry of Health, Rome, Italy (Ricerca Corrente, Centro Cardiologico Monzino IRCCS).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki. Ethical review and approval were waived for this study due to its nature (single patient observational case report).
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this paper (including the figures).
Data Availability Statement
No database is available due to the nature of the study (single patient observational case report).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Belardinelli, R.; Lacalaprice, F.; Carle, F.; Minnucci, A.; Cianci, G.; Perna, G.; D’Eusanio, G. Exercise-induced myocardial ischaemia detected by cardiopulmonary exercise testing. Eur. Heart J. 2003, 24, 1304–1313. [Google Scholar] [CrossRef] [PubMed]
- Belardinelli, R.; Lacalaprice, F.; Tiano, L.; Muçai, A.; Perna, G.P. Cardiopulmonary exercise testing is more accurate than ECG-stress testing in diagnosing myocardial ischemia in subjects with chest pain. Int. J. Cardiol. 2014, 174, 337–342. [Google Scholar] [CrossRef] [PubMed]
- Stringer, W.W.; Hansen, J.E.; Wasserman, K. Cardiac output estimated noninvasively from oxygen uptake during exercise. J. Appl. Physiol. 1997, 82, 908–912. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, M.J.; Knight, J.D.; Higginbotham, M.B.; Cobb, F.R. Relation between central and peripheral hemodynamics during exercise in patients with chronic heart failure. Muscle blood flow is reduced with maintenance of arterial perfusion pressure. Circulation 1989, 80, 769–781. [Google Scholar] [CrossRef] [PubMed]
- Accalai, E.; Vignati, C.; Salvioni, E.; Pezzuto, B.; Contini, M.; Cadeddu, C.; Meloni, L.; Agostoni, P. Non-invasive estimation of stroke volume during exercise from oxygen in heart failure patients. Eur. J. Prev. Cardiol. 2021, 28, 280–286. [Google Scholar] [CrossRef] [PubMed]
- Bhambhani, Y.; Norris, S.; Bell, G. Prediction of Stroke Volume from Oxygen Pulse Measurements in Untrained and Trained Men. Can. J. Appl. Physiol. 1994, 19, 49–59. [Google Scholar] [CrossRef] [PubMed]
- Crisafulli, A.; Piras, F.; Chiappori, P.; Vitelli, S.; Caria, M.A.; Lobina, A.; Milia, R.; Tocco, F.; Concu, A.; Melis, F. Estimating stroke volume from oxygen pulse during exercise. Physiol. Meas. 2007, 28, 1201–1212. [Google Scholar] [CrossRef] [PubMed]
- Mapelli, M.; Romani, S.; Magrì, D.; Merlo, M.; Cittar, M.; Masè, M.; Muratori, M.; Gallo, G.; Sclafani, M.; Carriere, C.; et al. Exercise oxygen pulse kinetics in patients with hypertrophic cardiomyopathy. Heart 2022, 108, 1629–1636. [Google Scholar] [CrossRef] [PubMed]
- Bussotti, M.; Apostolo, A.; Andreini, D.; Palermo, P.; Contini, M.; Agostoni, P. Cardiopulmonary evidence of exercise-induced silent ischaemia. Eur. J. Prev. Cardiol. 2006, 13, 249–253. [Google Scholar] [CrossRef] [PubMed]
- Danek, B.A.; Kearney, K.; Steinberg, Z.L. Clinically significant myocardial bridging. Heart, 2023; online ahead of print. [Google Scholar] [CrossRef]
- Patel, A.R.; Salerno, M.; Kwong, R.Y.; Singh, A.; Heydari, B.; Kramer, C.M. Stress Cardiac Magnetic Resonance Myocardial Perfusion Imaging: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2021, 78, 1655–1668. [Google Scholar] [CrossRef] [PubMed]
- Pargaonkar, V.S.; Kimura, T.; Kameda, R.; Tanaka, S.; Yamada, R.; Schwartz, J.G.; Perl, L.; Rogers, I.S.; Honda, Y.; Fitzgerald, P.; et al. Invasive assessment of myocardial bridging in patients with angina and no obstructive coronary artery disease. EuroIntervention 2021, 16, 1070–1078. [Google Scholar] [CrossRef] [PubMed]
- Tarantini, G.; Barioli, A.; Fovino, L.N.; Fraccaro, C.; Masiero, G.; Iliceto, S.; Napodano, M. Unmasking Myocardial Bridge–Related Ischemia by Intracoronary Functional Evaluation. Circ. Cardiovasc. Interv. 2018, 11, e006247. [Google Scholar] [CrossRef] [PubMed]
- Kelle, S.; Thouet, T.; Tangcharoen, T.; Fleck, E.; Nagel, E. Anatomical and Functional Evaluation of Myocardial Bridging on the Left Anterior Descending Artery by Cardiovascular Magnetic Resonance Imaging. J. Cardiovasc. Magn. Reson. 2006, 8, 755–757. [Google Scholar] [CrossRef] [PubMed]
- Sternheim, D.; Power, D.A.; Samtani, R.; Kini, A.; Fuster, V.; Sharma, S. Myocardial Bridging: Diagnosis, Functional Assessment, and Management: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2021, 78, 2196–2212. [Google Scholar] [CrossRef] [PubMed]
- Thomson, V.; Botnar, R.; Croisille, P. Usefulness of MRI to Demonstrate the Mechanisms of Myocardial Ischemia in Hypertrophic Cardiomyopathy with Myocardial Bridge. Cardiology 2006, 107, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Mandapaka, S.; Hundley, W.G. Dobutamine cardiovascular magnetic resonance: A review. J. Magn. Reson. Imaging 2006, 24, 499–512. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).