Abstract
Telemedicine can be an effective tool for managing chronic diseases. The disruption in traditional diabetes care resulting from the COVID-19 pandemic led to global interest in telemedicine. With this manuscript, we evaluated the use of telemedicine for the management of diabetes during the pandemic and its impact on glycemic control, focusing on retrospective and prospective studies which included adult, non-pregnant patients with diabetes. We evaluated whether there was an improvement in HbA1c, time in range (TIR), glucose management indicator (GMI), mean glucose values, hypoglycemic episodes, time below range (TBR), or hospitalizations for hypoglycemia/DKA, depending on the available information provided. This review article highlights the benefits of telemedicine during the global state of emergency, which altered the standard of healthcare delivery. Across the studies reported in this review, telemedicine was shown to be an effective tool for the management of diabetes, illustrating its potential to be the new standard of care. Although these improvements may be confounded by potential extraneous factors present during the pandemic, telemedicine was shown to positively impact glycemic control. Overall, this article highlights the benefits of telemedicine on glycemic control during the global state of emergency, which altered the standard of care. With the rollback of COVID-19 restrictions, and a return to the office, this article emphasizes the necessity to study how telemedicine can be best utilized for diabetes management when compared to the traditional standard of care.
1. Introduction
Diabetes is one of the most prevalent diseases worldwide. According to the CDC, from 2001 to 2020, the prevalence of diabetes significantly increased among adults in the United States. Furthermore, the CDC estimated that 37.3 million people, representing 11.3% of the US population, have diabetes [1]. Notably, the global prevalence is expected to rise to 578 million by 2030 [2]. Following COVID-19 pandemic declaration, patients with diabetes were found to be at particularly high risk of intensive care admission (ICU) and mortality from COVID-19 infection, representing a vulnerable population [3,4,5,6]. The advent of the pandemic ushered in a new era in medical care, especially for diabetes, by allowing telehealth to become a key alternative tool that can help modernize care through the use of tools such as continuous glucose monitors, smart pens, and smart phones [7]. The outbreak of the COVID-19 pandemic created an additional challenge in providing care for chronic diseases such as diabetes. Given its highly contagious nature and propensity to spread from one person to another through direct transmission, measures such as social distancing, lockdowns, and travel restrictions were implemented to mitigate virus spread and reduce hospitalizations in different parts of the world, which led countries to adapt different strategies [8]. In the United States, there was a significant drop in in-person outpatient visits, prompting a shift towards the use of telemedicine as a consequence [9]. However, the impact of the pandemic extended beyond the United States and had a major repercussion in care across different countries around the world and medical specialties [10].
Overall, the change in the landscape of medical care posed a challenge to the way healthcare was delivered. Consequently, institutions increasingly utilized virtual clinics and telemedicine interventions to provide appropriate care for patients, including those with diabetes, to protect against COVID-19 infections. Despite the sudden change in care, telemedicine was positively received by patients [11,12]. Telemedicine is defined by the Institute of Medicine as “the use of electronic information and communications technologies to provide and support health care when distance separates the participants” [13]. The Centers for Medicare and Medicaid Services (CMS) describes telemedicine as “the exchange of medical information from one site to another through electronic communication to improve a patient’s health” [14]. Telemedicine can be an effective tool for more than just patients with an established diabetes diagnosis. It can also be used to navigate challenging situations such as insulin pump training through virtual clinics or management of new-onset diabetes, circumstances where in-person care were traditionally deemed necessary [15,16]. Although telemedicine was not broadly used prior to the onset of the pandemic, it swiftly became an instrumental tool for the care of patients with diabetes; that, in conjunction with the use of technology such as continuous glucose monitors (CGM), allowed physicians to provide adequate care and makes telemedicine feasible [17].
The COVID-19 pandemic led to worldwide interest in telemedicine, as evidenced by the multiple publications presented in this paper. In this article, we evaluate the use of telemedicine for the management of diabetes by presenting a comprehensive review of papers that focused on the use of telemedicine on glycemic control in adults after the COVID-19 pandemic declaration.
2. Methods
An electronic search of PubMed was conducted by two independent reviewers (F.S., R.H.) to analyze publications relating to diabetes management, telemedicine, and COVID-19. The search was conducted via PubMed advanced search builder using the following key words: ‘Diabetes telemedicine clinic and COVID-19′, or ‘Glycemic control telemedicine clinic and COVID-19′, or ‘Diabetes management and SARS-CoV lockdown’, or ‘Telemedicine diabetes and lockdown’ or ‘Impact telemedicine and diabetes control lockdown’. The search resulted in a total of 646 articles, which we filtered based on publication date. Using ‘11 March 2020–31 July 2022′, a total of 376 records remained. Two duplicate records were removed, and those that included pediatric patients or pregnant patients were excluded. From the 317 reports that remained, a filter was used to exclude review articles, systematic reviews, and meta-analysis articles. The remaining articles were screened for relevance, study purpose, and outcome measures. Those that did not have glycemic control evaluation as either primary or secondary end points, did not describe the impact of telemedicine on diabetes management during the pandemic, or studied diabetes comorbidities were excluded (Figure 1). This review did not focus on the financial impact of telemedicine.
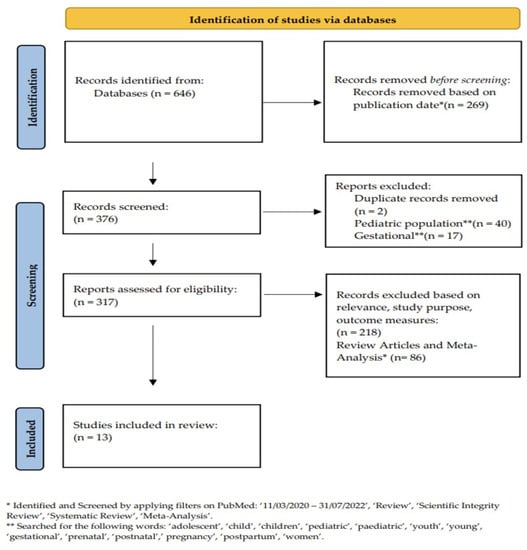
Figure 1.
Database Search.
In the included studies, time in range (TIR), time above range (TAR), glucose management indicator (GMI), mean glucose value, postprandial plasma glucose (PPPG), fasting plasma glucose (FPG), hemoglobin A1c (HbA1c), time below range (TBR), and hypoglycemic events were used as parameters for evaluating glycemic control. Glucose monitoring methods used to monitor patients included continuous glucose monitor (CGM), self-monitoring of blood glucose (SMBG), and flash glucose monitoring (FGM). Additionally, multiple daily insulin injections (MDI), continuous subcutaneous insulin infusion (CSII), and non-insulin hypoglycemic medications (oral hypoglycemic agents and GLP-1 agonists) were among the different glucose treatment methods used in the various studies. (Table 1 and Table 2).

Table 1.
Retrospective studies which examined telemedicine use in patients with DM.

Table 2.
Prospective studies which examined telemedicine use in patients with DM.
3. Results
3.1. Evidence from Retrospective Studies
Among the retrospective studies published (Table 1), three of them assessed patients exclusively with type 1 diabetes (T1D) and included patients who used insulin pumps or MDI as methods of treatment and either CGM or FGM as glycemic monitoring methods [18,19,20].
A study conducted with 30 T1D patients on hybrid closed loop (HCL) insulin pumps [18] evaluated glycemic control through telemedicine across four different time points during the pandemic lockdown period (two weeks before the lockdown, Time 0), during the first two weeks of lockdown (Time 1), last two weeks of lockdown (Time 2), and first two weeks after the lockdown (Time 3) [18]. The study found an improvement in mean glucose value (155 mg/dL in Time 0 vs. 153 mg/dL in Time 3, p = 0.004), a significant improvement in TIR (68.5% in Time 0 vs. 73.5% in Time 3, p = 0.012) without an increase in level 1 (54–69 mg/dL) and level 2 (<54 mg/dL) hypoglycemia. The improvement in TIR was instead associated with a reduction in TAR (Table 1).
Another study by Boscari et al. [19], which enrolled 71 T1D patients managed by either MDI or CSII, analyzed the efficacy of telemedicine by comparing CGM/FGM combined data gathered four weeks before and four weeks after patients attended a telephone visit. This study showed a reduction in GMI from 7.16 to 7.05%, p = 0.002, a reduction in mean glucose value from 161.1 mg/dL to 156.3 mg/dL, p = 0.001, a reduction in TAR (>180 mg/dL) from 33.4 to 30.5%, p = 0.002, with an improvement in TIR (70–180 mg/dL) from 63.6 to 66.4%, p < 0.001. Furthermore, among those managed by CSII, there was a reduction in mean glucose value from 157.9 mg/dL to 152.6 mg/dL, p = 0.003 [19]. No changes were observed in TBR (<70 mg/dL) with 3.0 vs. 3.2% p = 0.6, respectively.
Alharthi et al. [20] evaluated patients with T1D and compared glycemic control from FGM device data in a total of 101 patients who attended a specialized diabetes clinic during the six-week lockdown period 61 patients attended a telemedicine visit (TM) and a total of 40 patients did not [20]. The study showed improvements in average blood glucose from 180 mg/dL to 159 mg/dL, p < 0.01 in those who attended a TM visit vs. 159.5 to 160 mg/dL p = 0.99 in those who did not. An improvement in TIR (70–180 mg/dL) from 46.0% to 55.0%, p < 0.01 vs. 58.0 to 57.0%, p = 0.20, was also observed. The authors also found a reduction in GMI from 7.7 to 7.2%, p = 0.03 vs. 7.3 to 7.2%, p = 0.65 in those who attended a TM visit vs. those who did not attend a TM visit, respectively. Additionally, a reduction in TAR (>180 mg/dL) was noted, without any significant change in TBR (<70 mg/dL) or in hypoglycemic events [20].
Four studies explored the impact of telemedicine on glycemic control in patients with type 2 diabetes (T2D) [21,22,23,24]. These studies monitored glycemic control through SMBG, fasting, or postprandial blood glucose. Unlike the studies mentioned above, none of the subjects used a continuous or flash glucose monitor. In addition, a wide range of medications, such as insulin, GLP-RA, and SGLT2i, were used for glucose control in these studies; insulin pumps in patients with type 2 diabetes were not explored.
Scoccimarro et al. [21] evaluated 269 patients and assessed the difference in HbA1c and body weight between the pre-lockdown and post-lockdown periods (from November 2019 to February 2020 vs. May to June 2020). They found no deterioration in metabolic profile but rather a slight improvement in HbA1cHbA1c% (7.3% ± 3.1% pre-lockdown vs. 7.2% ± 3.2% post-lockdown, p < 0.01) and in weight (83.2 ± 16.8 kg vs. 81.6 ± 16.4, p < 0.01) in the entire cohort.
In another study, Dutta et al. [22] compared glycemic control among a cohort of 96 patients with T2D who were followed for a six-month period through telemedicine or in-person visits [20]. The study found a reduction in HbA1c from baseline 8.7% ± 1.8 to 6.9 ± 1.1 in the telemedicine compared to the in-person group, which had a reduction in HbA1c from baseline 8.6% ± 2.1% to 7.0% ± 1.0%, p = 0.88 at six months follow-up. A reduction in FPG (fasting plasma glucose) and PPPG (post prandial plasma glucose) was noted in both groups as well [22].
The clinical effectiveness of telemedicine vs. a traditional care model was evaluated in 200 patients with uncontrolled T2D (HbA1c > 9%) who attended an outpatient diabetes clinic [23]. The telemedicine arm included patients that attended a virtual clinic between March and June 2020 and the traditional care model included patients who received in-person care between August and November 2020. The telemedicine group had a reduction of 1.82% ± 1.35% (95% Cl = 1.56–2.09, p < 0.001) when compared to the traditional care model, which had a mean reduction of 1.54% ± 1.56% (95% Cl = 1.23–1.85, p < 0.001 [23].
Another study explored the impact of telemedicine on HbA1c in high-risk patients (HbA1c > 8%) with T2D before and after the implementation of a pharmacist-led telehealth service [24]. The study evaluated the change in HbA1c between the pre-COVID-19 group (August 2019–February 2020) and the COVID-19 group (March 2020–October 2020). The study showed an HbA1c reduction of 1.3% in the pre-COVID-19 group vs. 2% in the COVID-19 group at three months follow-up, p = 0.305. An HbA1c reduction of 1.2% in the pre-COVID-19 vs. 2.2% in the COVID-19 group, p = 0.249 at six months follow-up, was also observed [24].
Finally, three retrospective studies enrolled both T1D and T2D patients to analyze the efficacy of telemedicine during the state of emergency [25,26,27]. Of these studies, one evaluated outpatient diabetes care and HbA1c levels during the 2020 pandemic to 2019 by comparing the 13 weeks before (pre-period) and after (post-period) the lockdown period (26 May–24 August 2020) with the same time frame in 2019 [25]. This study found a post-period HbA1c of 7.2% in 2020 and 7.2% in 2019 (p = 0.43) with a change in HbA1c of −0.1 and −0.2 from the pre-period, respectively (p < 0.001). A propensity analysis done between clinic visits vs. telemedicine visits in 2020 showed a reduction in HbA1c from baseline 7.6 to 7.5%, p = 0.023, with a difference reduction of –0.15 in the telemedicine compared with the clinic visit group that showed a reduction of HbA1c from 7.6 to 7.4%, p = 0.023 with a reduction of −0.23, p = 0.019 favoring clinic visit over telemedicine [26]. The second study conducted a multiple regression analysis of patients with T1D and T2D (N = 2727), which showed that following adjustment for sex and type of diabetes, lower pre-BMI, lower pre-HbA1c, younger age, and clinic visit and/or telemedicine visit were associated with a higher chance of achieving an HbA1c < 7% [26]. Lastly, a study conducted by Wong et al. analyzed a cohort of 504 patients with both T1D and T2D) [27]. The study assessed telehealth consultations that took place between 1st April 2020 and 1st September 2020 (Visit A) and compared it to the proportion of patients that attended a face-to-face encounter during the same months in the year 2019 (Visit B) and finally compared it to patients that attended the clinic between April and September 2020 and had been attending the clinic face-to-face for at least 12 months prior to the onset of the pandemic (Visit C). When assessing HbA1c available at all patients, the study found improvements in HbA1c of 7.8% ± 1.6% at Visit A when compared to 8.1 ± 1.4 at Visit B and 8.2 ± 1.7% at visit C (p < 0.001). Patients with T2D also had a lower HbA1c at visit A compared to visit B and visit C. However, in patients with T1D, there was no significant difference in glycemic control between visit A, visit B, and visit C, with an HbA1c of 8.3 ± 1.4%, 8.4 ± 1.7, and 8.4 ± 1.8, respectively [27].
3.2. Evidence from Prospective Studies
Three prospective studies evaluated the effect of telemedicine in improving glycemic control in individuals with T1D and T2D. Two of the three studies enrolled patients with T1D and one enrolled patient with T2D [28,29,30].
A pilot study, which included 166 patients with T1D, aimed to evaluate different glycemic outcomes collected during two virtual visits during the lockdown period [26]. The study considered different methods of insulin delivery and glucose monitoring for its assessment (CSII + CGM, MDI + CGM, and CSII or MDI + SMBG), showing that TIR increased from baseline to follow-up visits in all patients). There was a non-statistically significant improvement in TBR and GMI compared to baseline and statistically significant improvements in TAR and mean daily glucose (Table 2) [28]. Notably, the CSII and MDI+SMBG group displayed better improvements in the TAR from baseline compared to follow-up visits (40.0% ± 18.0% vs. 28.0% ± 15.0%, respectively; p = 0.03), a reduction in mean daily glucose (176± 49 mg/dL vs. 150 ± 25 mg/dL; p = 0.04), and improvement in GMI (7.5% ± 1.1% vs. 6.9% ± 0.6%; p = 0.04), and CV (36.0% ± 8.0% vs. 42.0%± 9.0%; p = 0.04) compared to the other groups. In a subgroup analysis, the authors found a significant improvement in TIR in those with a GMI > 7.5% as compared to those with a GMI < 7.5% [28].
Another study enrolled 87 patients with uncontrolled T1D diabetes (GMI > 9%) and followed patients between March and June 2020 through online visits, conferences, and group sessions [29]. The authors evaluated the number of hospitalizations for DKA and severe hypoglycemia causing loss of consciousness or seizures and, as a secondary endpoint, reduction in GMI. The participant’s outcomes were compared to patient data from patients with HbA1c > 9% in the TID exchange. The study found fewer hospitalizations for DKA in the enrolled patients vs. T1D exchange (2.2 vs. 6.71%), fewer episodes of severe hypoglycemia in telemedicine vs. T1D exchange (1.1% vs. 7%) and change in mean GMI of −0.66% (reduced from 9.91 to 9.25%) during this period [29].
Finally, a study assessed 130 T2D patients with HbA1c > 9% who attended a virtual integrated care clinic over four months during the pandemic. Using Hb1Ac as a marker for glycemic control, this single-arm observational study showed a decrease in pre-intervention HbA1c from 9.98 ± 1.33 to 8.32 ± 1.31 (p < 0.001) post-intervention [30].
4. Discussion
Hyperglycemia, hypoglycemia, or increased glucose variability have been associated with increased morbidity, frequent hospitalizations/emergency department (ED) visits, and higher mortality [31,32,33,34,35]. Achieving better glucose control is important and frequent clinic visits are often required for medication adjustments. In addition, many patients with diabetes have underlying comorbidities that restrict mobility or live in remote/rural areas posing barriers to seeking in-person care. Telemedicine can serve as an alternative method of providing less time consuming and more accessible patient care, it is just a matter of embracing the technological options already available [36]; by doing so, it could allow quicker titration of diabetes medications, improving monitoring and glycemic parameters compliance in medication taking, and improving outcomes [37]. Although telemedicine can be an option, most visits are still performed in-person. Telemedicine can utilize different telecommunication options, among them video conference applications, which have expanded following the COVID-19 declaration. With a growing number of patients using smartphones and having Internet access (more than 85% of the US population using smartphones [38] and 93% having Internet access [39], a figure that is constantly rising), utilizing the Internet to transfer data and perform telemedicine should not be considered a futuristic solution for healthcare delivery, but an option to use at the present time.
Overall, telemedicine proved to be a timely solution in the face of the COVID-19 outbreak, allowing for appropriate glycemic control (Figure 2). The studies reported were conducted across different countries worldwide, showcasing a diverse population. They focused on patients with both type 1 and type 2 diabetes with different treatment modalities (insulin pump, multiple daily insulin injections, oral hypoglycemic agents, GLP-1 agonists) and different glucose monitoring methods (CGM, FGM, SMBG) (Table 1 and Table 2). Notably, the retrospective studies focusing on individuals with T1D showed improvements across various glycemic control measures regardless of the treatment modality [18,19,20]. These studies showed improvements in TIR, reductions in TAR, improvements in mean glucose values, and reductions in HbA1c% and GMI [18,19,20]. In the retrospective studies following patients with T2D, most studies found that the use of telemedicine led to reductions in HbA1c [21,24], with one study showing it to be equally effective as the standard of care model [22]. Similar findings were observed in studies that used mixed population of patients with T1D and T2D, in which telemedicine led to improvements in HbA1c [25,26,27].
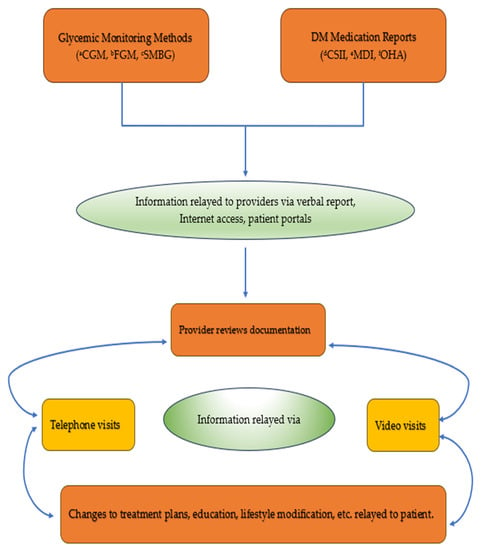
Figure 2.
Use of telemedicine for remote glucose monitoring. a CGM: Continuous Glucose Monitor; b FGM: Flash Glucose Monitor; c SMBG: Self-Monitoring Blood Glucose; d CSII: Continuous Subcutaneous Insulin Infusion; e MDI: Multiple Daily Injection; f OHA: Oral Hypoglycemic Agent.
It is crucial to acknowledge that the heterogenicity of these studies, including variations in outcomes, patient population, sample size, methods of glycemic monitoring, and insulin delivery restricts the clear interpretation of telemedicine’s role on diabetes management. While some prospective studies showed improvements in TIR, mean glucose value, and reductions in TAR [18,19,20], it is important to note that their small sample size could contribute to their results. Additionally, while reductions in HbA1c were noted across all telemedicine groups [21,22,23,24,25,26,27,30], some studies only found slight improvements [21], and another found no statistical significance among the groups [24]. Furthermore, studies focused on T1D patients used CGM devices to monitor glycemic control [18,19,20], potentially confounding the role of telemedicine. Therefore, while the telemedicine groups did show improvements in glycemic control, the use of CGM devices could have contributed to their overall improvement. Nonetheless, the prospective study conducted by Parise et al. [28] highlighted that in all patients with T1D, the telemedicine group showed improvements in TIR regardless of the glucose monitoring method. In addition, lockdown could have allowed patients to have more time to allocate to diabetes care, hence confounding the effect of telemedicine. It should be also noted that that current evidence is based on retrospective-observational studies, as the number of prospective studies which were conducted evaluating the role of telemedicine in patients with diabetes during the COVID-19 era is much smaller. Large randomized clinical trials are needed to evaluate the role of telemedicine in glycemic control in patients with diabetes.
Even with the heterogenicity of these studies, telemedicine showed improvements in diabetes control, across different monitoring methods and treatment modalities, proving effective in diabetes management across various studies; however, even those with similar glycemic control outcomes did not exhibit a clear clink between telemedicine and specific measures. Furthermore, not all articles focused on the impact of hospitalization or events such as DKA or hypoglycemia. We also did not focus on the financial impact of telemedicine, as we deemed that that deserves a separate analysis of its own.
The use of diabetes technology, such as CGM or FGM, has emerged as an important tool for diabetes management. As shown in the studies presented, such technology seems to make diabetes management suitable for telemedicine by allowing a provider to review data remotely. With the development of new integrative information sharing, telemedicine can impact how diabetes is managed in the future. Remote monitoring can lead to improved glycemic measures, and as healthcare becomes more integrative, individuals with diabetes can be closely monitored by their physician. Expanding on these services will further allow those with diabetes to play a more active role in the management of their chronic illness. However, it faces significant hurdles such as cost, patient education, and need of technology training. As mentioned earlier, telemedicine was not widely used prior to the COVID-19 pandemic, but quickly became adopted as an instrument for diabetes care during the initial stages [17]. Our article emphasizes the variability in the current literature regarding the use of telemedicine in diabetes management, highlighting that while telemedicine has been shown to be a safe, valid, and adequate option for managing chronic diseases such as diabetes [17], its precise role is yet to be understood. Furthermore, as restrictions are lifted and life returns to normal, this article seeks to highlight the need for randomized clinical trials that assess telemedicine’s impact beyond the pandemic’s initial phases and how it can be optimized for diabetes management as we move forward from the pandemic.
5. Conclusions
Across different studies reported in this review, telemedicine was shown to be an effective tool for the management of diabetes, illustrating potential to be the new standard of care. Indeed, telemedicine became an invaluable tool during the initial phases of the pandemic and continues to prove crucial in managing chronic diseases. The evolution of technology is set to play a crucial role in future diabetes care. Tools such as continuous glucose monitors, insulin pumps, and smart pens not only have a positive impact on diabetes management but can also allow telemedicine to become standard practice in this group of patients. The heterogenicity and variability in the study results make it apparent that we do not yet fully understand how to best optimize telemedicine for the management of diabetes. Yet, these studies showed that telemedicine can be a promising and safe method of health care delivery in patients with diabetes compared to in-person visits.
Author Contributions
Writing—original draft preparation, F.S. and R.H.; writing—review and editing, F.S., R.H., R.M., N.P. and E.K.S.; supervision, E.K.S., F.S. and R.H. contributed equally to the concept, writing, and draft preparation. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported in part by the VA MERIT award (#1I01CX001825) from the United States (US) Department of Veterans Affairs Clinical Sciences Research and Development Service.
Conflicts of Interest
E.K.S. was partially supported by the VA MERIT award (#1I01CX001825) from the United States (US) Department of Veterans Affairs Clinical Sciences Research and Development Service. E.K.S. has received unrestricted research support from Dexcom and Tandem Diabetes Care (to Baltimore VA Medical Center and to University of Maryland) for the conduction of clinical trials. F.S., R.H., R.M., and N.P. have nothing to disclose.
References
- Centers for Disease Control and Prevention. By the Numbers: Diabetes in America. Available online: https://www.cdc.gov/diabetes/health-equity/diabetes-by-the-numbers.html (accessed on 25 October 2022).
- Saeedi, P.; Petersohn, I.; Salpea, P.; Malanda, B.; Karuranga, S.; Unwin, N.; Colagiuri, S.; Guariguata, L.; Motala, A.A.; Ogurtsova, K.; et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res. Clin. Pract. 2019, 157, 107843. [Google Scholar] [CrossRef] [PubMed]
- Spanakis, E.K.; Yoo, A.; Ajayi, O.N.; Siddiqui, T.; Khan, M.M.; Seliger, S.L.; Klonoff, D.C.; Feng, Z.; Sorkin, J.D. Excess Mortality in COVID-19-Positive Versus COVID-19-Negative Inpatients with Diabetes: A Nationwide Study. Diabetes Care 2021, 44, e169–e170. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef] [PubMed]
- Guan, W.J.; Ni, Z.Y.; Hu, Y.; Liang, W.H.; Ou, C.Q.; He, J.X.; Liu, L.; Shan, H.; Lei, C.L.; Hui, D.S.C.; et al. Clinical Characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients with 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA 2020, 323, 1061–1069. [Google Scholar] [CrossRef] [PubMed]
- Aberer, F.; Hochfellner, D.A.; Mader, J.K. Application of Telemedicine in Diabetes Care: The Time is Now. Diabetes Ther. 2021, 12, 629–639. [Google Scholar] [CrossRef]
- Agarwal, K.M.; Mohapatra, S.; Sharma, P.; Sharma, S.; Bhatia, D.; Mishra, A. Study and overview of the novel corona virus disease (COVID-19). Sens. Int. 2020, 1, 100037. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.Y.; Mehrotra, A.; Huskamp, H.A.; Uscher-Pines, L.; Ganguli, I.; Barnett, M.L. Trends in Outpatient Care Delivery and Telemedicine During the COVID-19 Pandemic in the US. JAMA Intern. Med. 2021, 181, 388–391. [Google Scholar] [CrossRef]
- Dupraz, J.; Le Pogam, M.-A.; Peytremann-Bridevaux, I. Early impact of the COVID-19 pandemic on in-person outpatient care utilisation: A rapid review. BMJ Open 2022, 12, e056086. [Google Scholar] [CrossRef]
- Mann, D.M.; Chen, J.; Chunara, R.; Testa, P.A.; Nov, O. COVID-19 transforms health care through telemedicine: Evidence from the field. J. Am. Med Inform. Assoc. 2020, 27, 1132–1135. [Google Scholar] [CrossRef]
- Scott, S.N.; Fontana, F.Y.; Züger, T.; Laimer, M.; Stettler, C. Use and perception of telemedicine in people with type 1 diabetes during the COVID-19 pandemic—Results of a global survey. Endocrinol. Diabetes Metab. 2020, 4, e00180. [Google Scholar] [CrossRef]
- Telemedicine: A Guide to Assessing Telecommunications in Health Care; Field, M.J. (Ed.) National Academies Press: Washington, DC, USA, 1996. [Google Scholar]
- (CMS) CfMaMS. Medicare Telemedicine Health Care Provider Fact Sheet. 2020. Available online: https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet (accessed on 6 June 2023).
- Garg, S.K.; Rodbard, D.; Hirsch, I.B.; Forlenza, G.P. Managing New-Onset Type 1 Diabetes during the COVID-19 Pandemic: Challenges and Opportunities. Diabetes Technol. Ther. 2020, 22, 431–439. [Google Scholar] [CrossRef]
- Pinsker, J.E.; Singh, H.; Malloy, M.M.; Constantin, A.; Leas, S.; Kriegel, K.; Habif, S. A Virtual Training Program for the Tandem t:slim X2 Insulin Pump: Implementation and Outcomes. Diabetes Technol. Ther. 2021, 23, 467–470. [Google Scholar] [CrossRef] [PubMed]
- de Kreutzenberg, S.V. Telemedicine for the Clinical Management of Diabetes; Implications and Considerations after COVID-19 Experience. High Blood Press. Cardiovasc. Prev. 2022, 29, 319–326. [Google Scholar] [CrossRef] [PubMed]
- Longo, M.; Caruso, P.; Petrizzo, M.; Castaldo, F.; Sarnataro, A.; Gicchino, M.; Bellastella, G.; Esposito, K.; Maiorino, M.I. Glycemic control in people with type 1 diabetes using a hybrid closed loop system and followed by telemedicine during the COVID-19 pandemic in Italy. Diabetes Res. Clin. Pract. 2020, 169, 108440. [Google Scholar] [CrossRef] [PubMed]
- Boscari, F.; Ferretto, S.; Uliana, A.; Avogaro, A.; Bruttomesso, D. Efficacy of telemedicine for persons with type 1 diabetes during Covid19 lockdown. Nutr. Diabetes 2021, 11, 1. [Google Scholar] [CrossRef] [PubMed]
- Alharthi, S.K.; Alyusuf, E.Y.; Alguwaihes, A.M.; Alfadda, A.; Al-Sofiani, M.E. The impact of a prolonged lockdown and use of telemedicine on glycemic control in people with type 1 diabetes during the COVID-19 outbreak in Saudi Arabia. Diabetes Res. Clin. Pract. 2021, 173, 108682. [Google Scholar] [CrossRef]
- Scoccimarro, D.; Giove, G.; Silverii, A.; Dicembrini, I.; Mannucci, E. Effects of home confinement during COVID-19 outbreak on glycemic control in patients with type 2 diabetes receiving telemedicine support. Acta Diabetol. 2021, 59, 281–284. [Google Scholar] [CrossRef]
- Mithal, A.; Dutta, A.; Mahendru, S.; Sharma, R.; Singh, A.; Jain, A.; Jevalikar, G. Video consultation versus in-person clinic visit for glycemic control in type 2 diabetes during COVID-19 pandemic (VIP-CD study). Indian J. Endocrinol. Metab. 2021, 25, 427–431. [Google Scholar] [CrossRef]
- AlMutairi, M.F.; Tourkmani, A.M.; Alrasheedy, A.A.; Alharbi, T.J.; Bin Rsheed, A.M.; Aljehani, M.; AlRuthia, Y. Cost-effectiveness of telemedicine care for patients with uncontrolled type 2 diabetes mellitus during the COVID-19 pandemic in Saudi Arabia. Ther. Adv. Chronic Dis. 2021, 12, 20406223211042542. [Google Scholar] [CrossRef]
- Woodhouse, A.G.; Orvin, C.; Rich, C.; Crosby, J.; Keedy, C.A. Diabetes outcomes before and during telehealth advancements surrounding COVID-19. J. Am. Pharm. Assoc. 2022, 62, 214–217. [Google Scholar] [CrossRef] [PubMed]
- Onishi, Y.; Ichihashi, R.; Yoshida, Y.; Tahara, T.; Kikuchi, T.; Kobori, T.; Kubota, T.; Iwamoto, M.; Hamano, S.; Kasuga, M. Substitution of telemedicine for clinic visit during the COVID-19 pandemic of 2020: Comparison of telemedicine and clinic visit. J. Diabetes Investig. 2022, 13, 1617–1625. [Google Scholar] [CrossRef] [PubMed]
- Onishi, Y.; Yoshida, Y.; Takao, T.; Tahara, T.; Kikuchi, T.; Kobori, T.; Kubota, T.; Shimmei, A.; Iwamoto, M.; Kasuga, M. Diabetes management by either telemedicine or clinic visit improved glycemic control during the coronavirus disease 2019 pandemic state of emergency in Japan. J. Diabetes Investig. 2021, 13, 386–390. [Google Scholar] [CrossRef]
- Wong, V.W.; Wang, A.; Manoharan, M. Utilisation of telehealth for outpatient diabetes management during COVID-19 pandemic: How did the patients fare? Intern. Med. J. 2021, 51, 2021–2026. [Google Scholar] [CrossRef] [PubMed]
- Parise, M.; Tartaglione, L.; Cutruzzolà, A.; Maiorino, M.I.; Esposito, K.; Pitocco, D.; Gnasso, A.; Irace, C. Teleassistance for Patients With Type 1 Diabetes during the COVID-19 Pandemic: Results of a Pilot Study. J. Med. Internet Res. 2021, 23, e24552. [Google Scholar] [CrossRef] [PubMed]
- Zeller, W.P.; DeGraff, R. A novel telemedicine protocol improved outcomes for high-risk patients with type 1 diabetes: A 3-month quality improvement project during the COVID-19 pandemic. J. Clin. Transl. Endocrinol. Case Rep. 2021, 19, 100078. [Google Scholar] [CrossRef] [PubMed]
- Tourkmani, A.M.; Alharbi, T.J.; Rsheed, A.M.B.; Alrasheedy, A.A.; Almadani, W.; Aljuraisi, F.; AlOtaibi, A.F.; AlHarbi, M.; AlAbood, A.F.; Ibn Alshaikh, A.A. The impact of telemedicine on patients with uncontrolled type 2 diabetes mellitus during the COVID-19 pandemic in Saudi Arabia: Findings and implications. J. Telemed. Telecare 2021, 29, 390–398. [Google Scholar] [CrossRef]
- Monnier, L.; Colette, C.; Owens, D.R. Glycemic variability: The third component of the dysglycemia in diabetes. Is it important? How to measure it? J. Diabetes Sci. Technol. 2008, 2, 1094–1100. [Google Scholar] [CrossRef]
- Diabetes Control and Complications Trial Research Group; Nathan, D.M.; Genuth, S.; Lachin, J.; Cleary, P.; Crofford, O.; Davis, M.; Rand, L.; Siebert, C. The Effect of Intensive Treatment of Diabetes on the Development and Progression of Long-Term Complications in Insulin-Dependent Diabetes Mellitus. N. Engl. J. Med. 1993, 329, 977–986. [Google Scholar] [CrossRef]
- UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998, 352, 837–853. [Google Scholar] [CrossRef]
- Lee, A.K.; Warren, B.; Lee, C.J.; McEvoy, J.W.; Matsushita, K.; Huang, E.S.; Sharrett, A.R.; Coresh, J.; Selvin, E. The Association of Severe Hypoglycemia With Incident Cardiovascular Events and Mortality in Adults With Type 2 Diabetes. Diabetes Care 2017, 41, 104–111. [Google Scholar] [CrossRef] [PubMed]
- Holman, N.; Hillson, R.; Young, R.J. Excess mortality during hospital stays among patients with recorded diabetes compared with those without diabetes. Diabet. Med. 2013, 30, 1393–1402. [Google Scholar] [CrossRef] [PubMed]
- Duffy, S.; Lee, T.H. In-Person Health Care as Option B. N. Engl. J. Med. 2018, 378, 104–106. [Google Scholar] [CrossRef] [PubMed]
- Mushcab, H.; Kernohan, W.G.; Wallace, J.; Martin, S. Web-Based Remote Monitoring Systems for Self-Managing Type 2 Diabetes: A Systematic Review. Diabetes Technol. Ther. 2015, 17, 498–509. [Google Scholar] [CrossRef]
- Mobile Fact Sheet. 2021. Available online: https://www.pewresearch.org/internet/fact-sheet/mobile/ (accessed on 6 June 2023).
- Internet/Broadband Fact Sheet. 2021. Available online: https://www.pewresearch.org/internet/fact-sheet/internet-broadband/ (accessed on 6 June 2023).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).