Abstract
This randomized comparative study was conducted to investigate the outcomes of patellar resurfacing with a medialized dome or an anatomical type in patients receiving primary unilateral posterior-stabilized TKA. Between March 2019 and January 2021, 98 knees were randomly assigned to receive patellar resurfacing by a medialized dome type (group D, 49 knees) or an anatomic type (group A, 49 knees). The primary outcome was the Knee Injury and Osteoarthritis Outcome Score. The secondary outcomes were the Western Ontario and McMaster Universities Osteoarthritis Index, Feller’s patella score, the Kujala anterior knee pain score, knee joint range of motion (ROM), and postoperative complications, including periprosthetic patellar fracture, patellar tilt angle, and lateral patellar shift. Patient-reported outcomes were not significantly different between the two groups. The ROM of the knee joint was significantly better in group A at six months after surgery (p = 0.021). No complications such as patellar fractures were observed. The anatomic type of patellar component showed a significant improvement of the patellar tilt angle after surgery compared with the medialized dome type of component. However, there were no significant differences in patient-reported clinical outcomes between the two groups during the follow-up period of 12 months.
1. Introduction
Various designs of patellar components have been used in total knee arthroplasty (TKA), including dome, medialized dome, oval, and anatomical types [1,2,3]. They vary from implant to implant or even within the same implant, and most are made of ultra-high molecular weight polyethylene [4,5]. To our knowledge, medialized dome-type components have been most commonly used because of their ease of operation due to the absence of an axis of rotation for patellar tracking [1,4].
With the recent development of TKA design, an anatomic type of patellar component, with the theoretical advantages of optimizing the conformity of the patello-femoral (P-F) joint, promoting native patellar tracking, and improving quadriceps function, has been developed [6,7,8,9]. It has been suggested that P-F symptoms can be reduced by optimizing kinematics [2,5,10].
To our knowledge, some studies related to P-F kinematics according to patellar component design have been reported [5,7,8]. However, even if a patellar component with this advanced design has the theoretical advantages of kinematics, there has been a paucity of literature regarding whether it leads to clinically improved patient-reported outcomes.
Therefore, the purpose of this randomized comparative study was to investigate the outcomes of patellar resurfacing with a medialized dome or an anatomical type in patients receiving primary unilateral posterior-stabilized TKA. We hypothesized that, although the anatomical type of patellar component had kinematic advantages, it would not affect patient-reported outcomes.
2. Materials and Methods
2.1. Participants
This prospective comparative study was ethically approved by the institutional review board of our hospital before gathering the patient data. Informed consent was obtained from all patients for study enrollment. From March 2019 to January 2021, 103 knees that underwent unilateral primary TKA with patellar resurfacing using a medialized dome type or an anatomic type were screened. Indications for patellar resurfacing were as follows: patients with progressed patellofemoral osteoarthritis (OA) according to the Iwano classification system (stage III–IV) [11], with a resultant thickness greater than 12 mm after patellar resection, considering the native patellar thickness [12]. We enrolled patients with a 12-month follow-up after the index operation for the study. We excluded five knees for the following reasons: rheumatoid arthritis in two, previous arthroscopic surgery around the knee in two, and post-traumatic OA in one. Finally, 98 knees fully meeting the inclusion criteria were randomly assigned either to the group with a medialized dome type (group D, 49 knees) or to the group with an anatomic type (group A, 49 knees). All patients completed the 12-month follow-up (Figure 1).
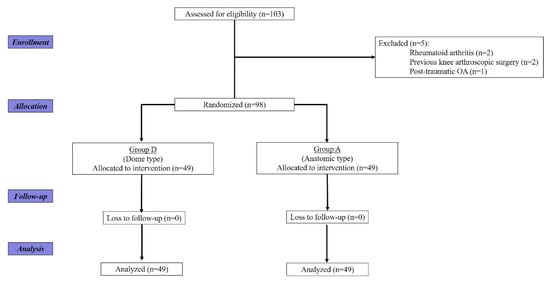
Figure 1.
Consolidated Standards of Reporting Trials (CONSORT) flow diagram for enrolled patients.
2.2. Surgical Techniques
All operations were performed by the same surgeon (G.B.K.) in our hospital using the modified gap-balancing technique, which can balance the extension gap before the flexion gap with posterior-stabilized (PS) gradually reducing radius femoral implants (Attune® TKA System, Depuy Synthes Inc., Warsaw, IN, USA) [13,14]. A medial parapatellar arthrotomy with a midline incision was performed. Femur sizing was performed using an anterior reference system in all the cases. The rotation of the tibial component was set by considering several reference points, including the medial one-third of the tibial tuberosity, anterior tibial cortex, and floating technique. All prostheses were used with cement. Fixed-bearing antioxidant polyethylene inserts were used in all cases.
The patellar components in the Attune® TKA System are composed of a medialized dome-type or an anatomic-type patellar component (Figure 2) [5].

Figure 2.
Anteroposterior and lateral views of two types of patellar components. (a) Medialized dome type and (b) anatomic type.
The thickness of the patella was measured using a vernier caliper before cutting in all patients. The amount of resection was decided using a cutting jig of either 7.5 mm or 9.5 mm, depending on the native patellar thickness, which corresponded to the thickness of the patellar component to be used. In the medialized dome-type components, cutting was set regardless of the axis of patellar tracking, whereas in the anatomic type, the longitudinal axis of the patella was set to be parallel to the tibial component in order to precisely match the rotational axis of the patellar tracking (Figure 3).
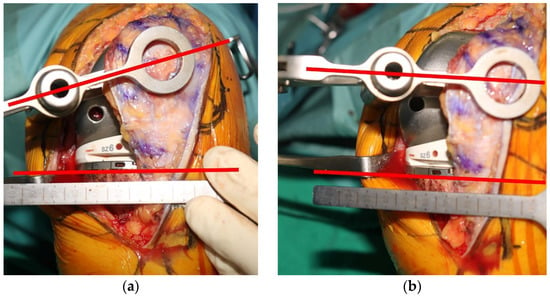
Figure 3.
Determining method of the tracking axis of anatomic-type patellar components. (a) If the longitudinal axis of the patella is not parallel to the tibial component, the tracking axis is considered inappropriate, and (b) if it is parallel, it is considered appropriate.
The size of the component was determined to provide maximum coverage of the articular surface. After resection, the resultant thickness was measured using a vernier caliper. Moreover, patelloplasty, including the removal of marginal osteophytes, and circumferential denervation using electrocautery were performed. Intraoperative patellar tracking was checked throughout the knee motion with the no thumb technique [15].
2.3. Postoperative Protocols
A closed suction drain was inserted and was removed 24 h after surgery. All patients performed the same perioperative pain-control protocol, including a multimodal drug regimen, postoperative patient-controlled analgesia, and an intraoperative periarticular injection. Active and passive postoperative range of motion (ROM) exercises were started on the day of surgery. If the acute pain subsided, partial weight-bearing with a crutch was allowed on the first postoperative day. Full weight-bearing was permitted 3 weeks after surgery.
2.4. Outcome Assessments
Demographic characteristics were investigated before surgery. All patients were regularly followed up at six weeks, and at three, six, and 12 months after index surgery. Patient-reported clinical evaluations were performed using the Knee Injury and Osteoarthritis Outcome Score (KOOS) [16], the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) [17], Feller’s patella score [18], the Kujala anterior knee pain (AKP) score [19], the ROM of the knee joint (including flexion contracture and further flexion), and postoperative complications including periprosthetic patellar fracture. Clinical outcomes were assessed at regular follow-ups by an independent observer in an outpatient clinic.
Radiographic images were retrieved using a picture-archiving and communication system (PACS; IMPAX, Agfa Healthcare, Mortsel, Belgium), and radiographic measurements were performed at regular follow-ups by another independent observer of the operative team. Radiographic evaluations included the patellar tilt angle and the lateral patellar shift on a Merchant view radiograph. The patellar tilt angle was set as the angle between the line crossing the widest portion of the patella and the line passing through the most anterior surface of both femoral condyles [20,21].
The primary outcome was KOOS. The secondary outcomes were: (1) WOMAC; (2) Feller’s patella score; (3) Kujala AKP score; (4) knee joint ROM; (5) postoperative complications including periprosthetic patellar fracture; (6) patellar tilt angle; and (7) lateral patellar shift.
2.5. Statistical Analysis
A power analysis (G* power software, version 3.1.9) was performed to calculate the number of patients needed in each group to identify the significant differences in clinical outcomes. We designed the study with a power of 90% at a two-sided significant level of 7%, which indicated that 44 knees were necessary in each group. Finally, considering an anticipated dropout rate of 10%, a total of 98 knees were required.
Statistical evaluation was performed using IBM SPSS software version 23 (IBM Corp., Armonk, NY, USA), and continuous data were expressed as means with SDs. All dependent variables were tested for normality of distribution and equality of variances using the Kolmogorov–Smirnov test and analyzed using parametric or non-parametric tests based on normality. An independent samples t-test (parametric) and a Mann–Whitney U-test (non-parametric) were performed to assess the differences in clinical and radiographic variables between the two groups. Fisher’s exact test was used to compare the ratios between the groups. For all tests, the statistical significance was set at p < 0.05.
3. Results
This A total of 98 knees were recruited into the study, 49 of which received patellar resurfacing using a medialized dome-type patellar component (group D), and 49 of which received with an anatomic-type patellar component (group A). There was no significant difference in the baseline characteristics between the two groups (Table 1).

Table 1.
Baseline patient characteristics for the medialized dome type (group D) and anatomic type (group A).
Patient-reported outcomes were significantly improved in both groups at 12 months after surgery (p < 0.001). All clinical outcomes were not significantly different between the two groups at each time period (Table 2, Table 3 and Table 4).

Table 2.
Mean Knee Injury and Osteoarthritis Outcome Score (KOOS) for group with the medialized dome type (group D) and group with anatomic type (group A).

Table 3.
Mean Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) for group with the medialized dome type (group D) and group with anatomic type (group A).

Table 4.
Mean Feller’s patella score and mean Kujala anterior knee pain score for group with the medialized dome type (group D) and group with anatomic type (group A).
Further flexion of the knee joint was significantly better in group A at six months after surgery (p = 0.021), but not at 12 months after surgery (Table 5).

Table 5.
Mean ROM of the knee joint for group with the medialized dome type (group D) and group with anatomic type (group A).
No complications such as patellar fractures were observed during the follow-up period.
The preoperative patellar tilt angle and lateral patellar shift did not differ significantly between the groups. However, postoperative patellar tilt angle was significantly improved in group A compared with group D and was consistent during the follow-up period (p < 0.001) (Figure 4).
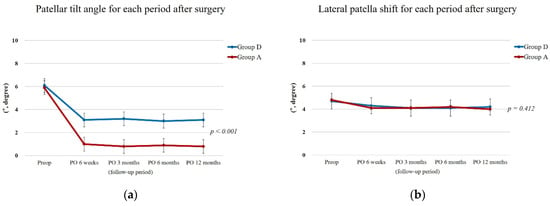
Figure 4.
Radiographic outcomes for each period after surgery. (a) Patellar tilt angle. (b) Lateral patella shift. Postoperative patellar tilt angle was significantly improved in group A compared with group D. (An independent sample t-test was used to assess the differences in clinical and radiographic variables between the two groups. p value < 0.05 was considered statistically significant).
4. Discussion
This randomized prospective comparative study showed that, although the anatomic-type patellar component showed significant radiological improvement after surgery, it did not lead to significant clinical improvements in Asian people.
Since the anatomic patellar component has a highly conforming geometry in the trochlear of the femoral component by implementing more anatomic patellar bone with a medialized apex, sagittal plane kinematics and quadriceps performance can be improved by optimizing native PFJ tracking. These factors were also reflected in the radiological outcomes of this study, suggesting that the postoperative patellar tilt angle was significantly improved. A study that revealed differences in patellar kinematics according to patellar component design reported that patellar tilt was reduced in the anatomic-type patellar component for each angle of the knee flexion [7]. This can be attributed to the fact that the dome-type component has a larger medial and lateral contact area compared with that of the anatomic type [9]. However, despite these kinematic advantages, since anatomic-type patellar components are usually more sensitive to mal-positioning such as rotational error [4], effort is needed to accurately align the tracking axis (Figure 3). If the central ridge of the anatomical-type component is not rotationally aligned with the femoral trochlea, adverse effects such as polyethylene wear or increased force in the extensor mechanism may occur. On the other hand, in the case of the medialized dome type, it can be implemented regardless of the rotational axis for patellar tracking.
Some studies related to the kinematic effects of different patellar component design reported that the anatomic type of patellar component had greater PF joint flexion angle with reduced contact force during activities [7,8,9,22]. This was also demonstrated in the results of this study, in which knee ROM was significantly improved in group A up to 6 months after surgery. However, there was no statistically significant difference in knee ROM at 12 months after surgery, which seems to have reduced the difference between the two groups as the pain subsides, the swelling of the surrounding tissue decreases, and the muscle power improves.
Moreover, the patient-reported clinical outcomes of the current study did not differ between the two groups. Theoretical kinematic advantages due to subtle changes in patellar component design did not lead to a significant improvement in short-term clinical outcomes. In the future, it is necessary to evaluate patient-reported outcomes over a longer term.
Despite the informative results, there are limitations meriting discussion. First, this study had a relatively short-term follow-up. Accordingly, significant differences may have been missed, and we could not confirm that the results of this study guarantee mid- to long-term outcomes. Another limitation of this study was the small sample size. The sample size of this study was determined by the effect size based on the KOOS score of previous similar studies. Therefore, a randomized controlled trial with a large sample and longer-term follow-up is needed. Third, since this study was conducted with only a specific type of implant (fixed-bearing PS implant), the results of this study cannot be representative of all TKA implants. The outcomes may vary for other implants or manufacturers with different kinematics. Lastly, a female predominance was observed in this study. Thus, the same outcomes may not apply to populations with different sex ratios. This trend has been characteristic of the Asian population [23,24].
Nevertheless, the strengths of this study are as follows: first, to our knowledge, this is the first prospective study to report the outcomes of a medialized dome-type and an anatomic-type patellar component in Asian people; secondly, patients were randomly assigned, and a variety of patient-reported clinical assessments were performed. Therefore, the patient-reported outcomes can be considered sufficiently reliable.
5. Conclusions
In conclusion, the anatomic type of patellar component showed a significant improvement of the patellar tilt angle after surgery compared with the medialized dome type of component. However, there were no significant differences in patient-reported clinical outcomes between the two groups during short-term follow-up.
Author Contributions
Conceptualization, G.B.K.; methodology, G.B.K. and O.-J.S.; formal analysis, G.B.K.; resources, G.B.K.; data curation, G.B.K.; writing—original draft preparation, G.B.K.; writing—review and editing, G.B.K. and O.-J.S.; visualization, G.B.K.; supervision, O.-J.S.; project administration, G.B.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (2021R1A6A1A03040177).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of the Yeungnam University Medical Center (Protocol No. 2019-03-003-001).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patients to publish this paper.
Data Availability Statement
Data supporting the reported findings are available from the corresponding author upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Brilhault, J.; Ries, M.D. Measuring patellar height using the lateral active flexion radiograph: Effect of total knee implant design. Knee 2010, 17, 148–151. [Google Scholar] [CrossRef] [PubMed]
- Yoshii, I.; Whiteside, L.A.; Anouchi, Y.S. The effect of patellar button placement and femoral component design on patellar tracking in total knee arthroplasty. Clin. Orthop. Relat. Res. 1992, 275, 211–219. [Google Scholar] [CrossRef]
- Maniar, R.N.; Bhatnagar, N.; Bidwai, R.; Dhiman, A.; Chanda, D.; Sanghavi, N. Comparison of patellofemoral outcomes between attune and pfc sigma designs: A prospective matched-pair analysis. Clin. Orthop. Surg. 2022, 14, 96–104. [Google Scholar] [CrossRef]
- Schindier, O.S. Basic kinematics and biomechanics of the patellofemoral joint. Part 2: The patella in total knee arthroplasty. Acta. Orthop. Belg. 2012, 78, 11. [Google Scholar]
- Smith, L.A.; LaCour, M.T.; Dennis, D.A.; Komistek, R.D. Anatomic vs. dome patella: Is there a difference between fixed-vs mobile-bearing posterior-stabilized total knee arthroplasties? J. Arthroplast. 2021, 36, 3773–3780. [Google Scholar] [CrossRef]
- White, P.B.; Sharma, M.; Siddiqi, A.; Satalich, J.R.; Ranawat, A.S.; Ranawat, C.S. Role of anatomical patella replacement on anterior knee pain. J. Arthroplast. 2019, 34, 887–892. [Google Scholar] [CrossRef]
- Mochizuki, T.; Yano, K.; Ikari, K.; Hiroshima, R.; Okazaki, K. Effect on patellar kinematics of the different patellar component designs in total knee arthroplasty: Intraoperative measurement of dome type versus anatomic type. Eur. J. Orthop. Surg. Traumatol. 2020, 30, 419–424. [Google Scholar] [CrossRef]
- Ali, A.A.; Mannen, E.M.; Rullkoetter, P.J.; Shelburne, K.B. In vivo comparison of medialized dome and anatomic patellofemoral geometries using subject-specific computational modeling. J. Orthop. Res. 2018, 36, 1910–1918. [Google Scholar] [CrossRef]
- Fitzpatrick, C.K.; Baldwin, M.A.; Clary, C.W.; Wright, A.; Laz, P.J.; Rullkoetter, P.J. Identifying alignment parameters affecting implanted patellofemoral mechanics. J. Orthop. Res. 2012, 30, 1167–1175. [Google Scholar] [CrossRef]
- Frye, B.M.; Floyd, M.W.; Pham, D.C.; Feldman, J.J.; Hamlin, B.R. Effect of femoral component design on patellofemoral crepitance and patella clunk syndrome after posterior-stabilized total knee arthroplasty. J. Arthroplast. 2012, 27, 1166–1170. [Google Scholar] [CrossRef]
- Iwano, T.; Kurosawa, H.; Tokuyama, H.; Hoshikawa, Y. Roentgenographic and clinical findings of patellofemoral osteoarthrosis. With special reference to its relationship to femorotibial osteoarthrosis and etiologic factors. Clin. Orthop. Relat. Res. 1990, 252, 190–197. [Google Scholar] [CrossRef]
- Ortiguera, C.J.; Berry, D.J. Patellar fracture after total knee arthroplasty. J. Bone Jt. Surg. Am. 2002, 84, 532–540. [Google Scholar] [CrossRef] [PubMed]
- Daines, B.K.; Dennis, D.A. Gap balancing vs. Measured resection technique in total knee arthroplasty. Clin. Orthop. Surg. 2014, 6, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Moro-oka, T.-A.; Shiraishi, H.; Iwamoto, Y.; Banks, S.A. Modified gap-balancing technique in total knee arthroplasty: Evaluation of the post-operative coronal laxity. Knee Surg. Sports Traumatol. Arthrosc. 2010, 18, 375–380. [Google Scholar] [CrossRef]
- Scott, R.D. Prosthetic replacement of the patellofemoral joint. Orthop. Clin. N. Am. 1979, 10, 129–137. [Google Scholar] [CrossRef]
- Roos, E.M.; Toksvig-Larsen, S. Knee injury and osteoarthritis outcome score (koos)–validation and comparison to the womac in total knee replacement. Health Qual Life Outcomes 2003, 1, 17. [Google Scholar] [CrossRef] [Green Version]
- Bellamy, N.; Buchanan, W.W.; Goldsmith, C.H.; Campbell, J.; Stitt, L.W. Validation study of womac: A health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J. Rheumatol. 1988, 15, 1833–1840. [Google Scholar]
- Feller, J.A.; Bartlett, R.J.; Lang, D.M. Patellar resurfacing versus retention in total knee arthroplasty. J. Bone Jt. Surg. Br. 1996, 78, 226–228. [Google Scholar] [CrossRef]
- Kujala, U.M.; Jaakkola, L.H.; Koskinen, S.K.; Taimela, S.; Hurme, M.; Nelimarkka, O. Scoring of patellofemoral disorders. Arthroscopy 1993, 9, 159–163. [Google Scholar] [CrossRef]
- Laurin, C.; Dussault, R.; Levesque, H. The tangential x-ray investigation of the patellofemoral joint: X-ray technique, diagnostic criteria and their interpretation. Clin. Orthop. Relat. Res. 1979, 144, 16–26. [Google Scholar] [CrossRef]
- Bito, H.; Takeuchi, R.; Kumagai, K.; Aratake, M.; Saito, I.; Hayashi, R.; Sasaki, Y.; Saito, T. Opening wedge high tibial osteotomy affects both the lateral patellar tilt and patellar height. Knee Surg. Sports Traumatol. Arthrosc. 2010, 18, 955–960. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.; Koo, J.; Moon, S.W.; Yang, Y.; Son, J. Long-term follow-up of patellar nonresurfacing in total knee arthroplasty. Clin. Orthop. Surg. 2020, 12, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Vina, E.R.; Kwoh, C.K. Epidemiology of osteoarthritis: Literature update. Curr. Opin. Rheumatol. 2018, 30, 160. [Google Scholar] [CrossRef] [PubMed]
- Koh, I.J.; Kim, M.W.; Kim, J.H.; Han, S.Y.; In, Y. Trends in high tibial osteotomy and knee arthroplasty utilizations and demographics in korea from 2009 to 2013. J. Arthroplast. 2015, 30, 939–944. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).