Abstract
(1) Context: The management of acute coronary syndrome (ACS) is based on a rapid diagnosis. The aim of this study was to focus on the ACS symptoms differences according to gender, in order to contribute to the improvement of knowledge regarding the clinical presentation in women. (2) Methods: We searched for relevant literature in two electronic databases, and analyzed the symptom presentation for patients with suspected ACS. Fifteen prospective studies were included, with a total sample size of 10,730. (3) Results: During a suspected ACS, women present more dyspnea, arm pain, nausea and vomiting, fatigue, palpitations and pain at the shoulder than men, with RR (95%CI) of 1.13 [1.10; 1.17], 1.30 [1.05; 1.59], 1,40 [1.26; 1.56], 1.08 [1.01; 1.16], 1.67 [1.49; 1.86], 1.78 [1.02; 3.13], respectively. They are older by (95%CI) 4.15 [2.28; 6.03] years compared to men. The results are consistent in the analysis of the ACS confirmed subgroup. (4) Conclusions: We have shown that there is a gender-based symptomatic difference and a female presentation for ACS. The “typical” or “atypical” semiology of ACS symptoms should no longer be used.
1. Introduction
Acute coronary syndrome (ACS) is one of the leading causes of death worldwide. It is responsible for 7.4 million deaths annually, particularly in developed countries [1,2]. The management of ACS is based on a rapid diagnosis in order to lead the patient to an adequate place of support and to provide him the right treatment [3,4]. The faster the diagnosis, the lower the risk of death or complications. If the final diagnosis of ACS is based on clinical signs of myocardial ischemia, such as chest pain, electrocardiographic signs (ST-Elevation Myocardial Infarction, STEMI; or Non-ST-Elevation Myocardial Infarction, NSTEMI), and on cardiac biomarkers, such as increased troponine [3], its semiology is very heterogeneous. Thus, while it is clear that chest pain is the main symptom, other symptoms such as dyspnea, digestive disorders and fatigue are described as “atypical” [5]. This “atypical” designation has been called into question for several years, and today it is rather thought that the symptomatology depends on the patient’s gender [5].
Lately, several authors were interested in the ACS differences between men and women [6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23]. First of all, physiopathologically, men and women are not exposed to cardiovascular risk factors in the same way. In fact, estrogen provides some cardioprotection, but exposure to tobacco is more harmful in women than in men [24]. The clinical presentation is also reported to be different, men being described as presenting classic symptoms such as chest pain, whereas women can present more heterogeneous symptoms close to the form historically described as “atypical” [25,26]. Women tend not to receive treatment or to receive sub-optimal treatment for ACS due to the late recognition of the acute event [27].
In this context, the main goal of our systematic review of the literature with a meta-analysis was to focus on the ACS symptoms differences according to gender in order to contribute to the improvement in knowledge regarding the clinical presentation in women.
2. Materials and Methods
2.1. Study Design
We carried out a systematic review of the literature and then a meta-analysis of these studies using the “Preferred Reporting Items for Systematic Reviews and Meta-analyzes” (PRISMA) methodology [28]. We searched two databases, PubMed and COCHRANE, with the aim of studying the articles published between 1 January 2010 and 4 February 2021. We included analyses focused on the clinical symptoms of ACS according to gender (the search equations are available in Figure 1). All prospective, retrospective, observational and interventional studies were included. The exclusion criteria were the unavailability of the entire text (only abstract available despite an extensive search on other existing databases), the absence of information on the suspected or retained diagnosis of ACS, the absence of any distinction between men and women, the absence of a description of symptoms and case reports. We excluded all studies that did not meet at least one quality criterion described below. Studies published in a language other than French or English were also excluded.
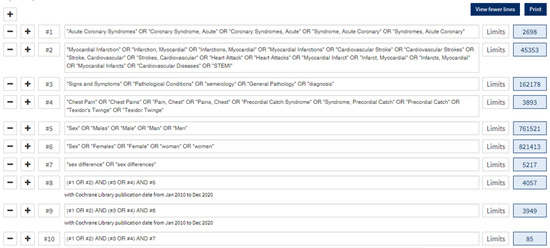
Figure 1.
Research equation from Cochrane.
Two co-authors (M.C. and L.A.V.) independently assessed the studies for eligibility. Differences were resolved by consensus.
2.2. Data Collection and Processing
Two coauthors (M.C. and L.A.V.) independently extracted data from the included full-text citations with a report form validated by N.P. The following information was abstracted: the last name of the first author, publication year, country where the study was performed, study design, total participants in the study, numbers of male and female participants, mean age of each sex, number of patients and percentage of symptoms of ACS (chest pain, dyspnea, arm pain, sweating, nausea and vomiting, fatigue, palpitations, shoulder pain, abdominal and epigastric pain). Data were collected with Excel® (Microsoft Corporation, Richmond, VA, USA).
2.3. Quality Assessment
We used an adapted version of the Newcastle Ottawa Scale [29]. We awarded 4 stars for the “selection” yardstick to studies that used random or consecutive selection of their patients. For the “comparability” yardstick, we awarded 2 stars to studies that adjusted their results with multiple covariates. Finally, the independent analysis of symptoms allowed the attribution of one star for the “outcomes” yardstick.
2.4. Statistical Analysis
The outcomes measured in studies of sex differences in the symptom presentation of patients with suspected or confirmed acute coronary syndrome were binary covariates. For these binary outcomes, the risk ratio was used to measure sex’s effect on the symptom presentation. The overall estimate was taken from a fixed effects or a random effects model for heterogeneity testing using a standard chi-square statistic. A subgroup analysis of patients with a diagnosis of ACS confirmed by the authors was performed. All analyses were conducted using R software version 4.0.2. A value of p < 0.05 was considered significant for main effect and heterogeneity tests.
Heterogeneity was first taken into account by running a random effects model when necessary. Then, a metaregression with the region was carried out to analyze its effect on the logarithm of the relative risk.
3. Results
3.1. Characteristics of Included Studies
We obtained 5403 results on the “men” equations, 4981 results on the “women” equations and 346 results on the “comparison” equations, for a total of 10,730 articles. After an initial screening of the titles of the articles and then the abstracts, followed by a review of the full texts and the application of the inclusion and exclusion criteria, 96 studies were selected. After removing duplicate articles, and excluding studies that did not contain data that could be used in a meta-analysis (non-individual statistics, meta-analysis), 15 studies were approved (Figure 2) for the meta-analysis studies, including all prospective studies.
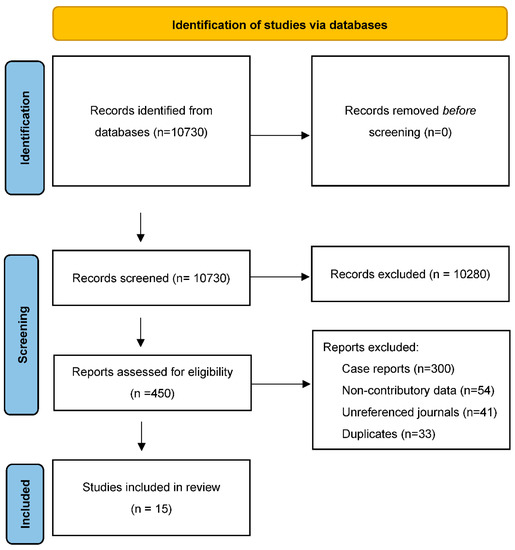
Figure 2.
Flowchart.
Baseline characteristics of the 15 included studies are summarized in Table 1. Heterogeneity was first taken into account by running a random effects model.

Table 1.
Summaries of included studies.
3.2. Patients’ Characteristics
Our study included 1,213,709 patients: 711,149 men (58.59%) and 502,560 women (41.41%). The “confirmed ACS” subgroup represented 1,195,524 patients, including 494,641 women. Patients included in the studies were admitted to emergency departments for chest pain, ACS suggestive symptoms according to the receiving physicians [10,12,16,17,18,20,21] or ACS suspicion from troponin measurement [11,13], or were hospitalized for ACS [9,14,15,19,22,23].
3.3. Symptoms
During an ACS, women are more likely to have dyspnea than men (RR (95%CI): 1.13 [1.10; 1.17]), arm pain in either arm (RR (95%CI): 1.30 [1.05; 1.59]), nausea and vomiting (RR (95%CI): 1.40 [1.26; 1.5]) and fatigue (RR (95%CI): 1.08 [1.01; 1.16]) (Table 2 and Figure 3). They are also more likely to present with palpitations (RR (95%CI): 1.67 [1.49; 1.86]) and pain in the shoulder (RR (95%CI): 1.78 [1.02; 3.13]) (Table 2 and Figure 3). Finally, the women were older by 4.15 years compared to men (95%CI): 4.15 [2.28; 6.03]) (Table 2 and Figure 3).

Table 2.
Results of the meta-analysis. RR of getting the symptom if a woman.
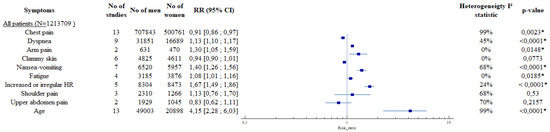
Figure 3.
Results of the meta-analysis, forest plots. Legend: * = p < 0.005.
The results are consistent in the analysis of the ACS confirmed subgroup. All results are available in Table 2, Figure 3 and Figure 4 and in Figures S1–S18.
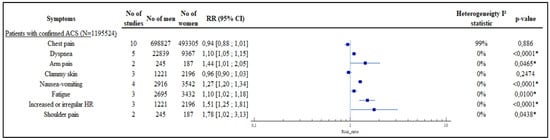
Figure 4.
Results of the meta-analysis, subgroup of confirmed ACS, forest plots. Legend: * = p < 0.005.
There was an effect of the region on the logarithm of the relative risk only for nausea-vomiting, increased or irregular heart rate and shoulder pain with all patients.
4. Discussion
Our systematic review of the literature, with meta-analysis, on a large volume of patients, confirmed that the clinical presentation of ACS in women is different from that of men, and may include pain in the upper limbs, palpitations, dyspnea, nausea and vomiting or simply fatigue. Women are also older during their first attack on average. To our knowledge, this is the first meta-analysis on the subject. We included 15 prospective studies, using RR calculations and a subgroup study with confirmed ACS. Indeed, previous literature reviews lacked precision due to the missing standardization in data collection [30,31]. The standardization proposed by the ESC in the definition of ACS makes it possible to limit bias in the inclusion of studies [3]. Given the large number of studies on ACS, it was also important to produce a strong synthesis using the robust method of meta-analysis. Our meta-analysis was based on multiple databases, minimizing the possibility that evidence-based studies were missing from the analysis. The heterogeneity between the studies was taken into account with a random effects model when necessary. The studies analyzed took place in several countries, with different health systems, making it possible to include populations from the United States, Europe and Asia (including the Arabian Peninsula). Nevertheless, our main strengths have been to include a significant number of patients (over one million), thanks to the analysis of high quality studies. Indeed, all the studies were prospective and therefore did not rely on a posteriori collection of the symptoms of ACS presented by the patients. Data collection was standardized in each of the studies by systematic collection by the investigators [6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23]. Carrying out the analysis of the “Confirmed ACS” subgroup allowed us to analyze the symptoms even better.
Our results are consistent with those of the meta-analysis by Van Oosterhoutand et al., who also studied presentation differences between males and females [32]. This study, although exhaustive, was limited to people with confirmed ACS and did not compare the gender differences in symptom presentation in people with suspected ACS. The classic symptomatology of ACS, which is chest pain, as known by the general public and taught in medical universities, has a strong gender bias [5,33,34]. ACS in women takes a less classic shape, and these symptoms are poorly known by the medical profession [35]. This notion has been emerging for several years. Thereby, De Von et al. proposed to stop using the terminology “typical” and “atypical” or to specify to which reference group it applies [6]. In this way, our study also supports this position, and all recent data should be widely disseminated so that these terms “typical” and “atypical” disappear completely from semiology. Prevention campaigns intended for the general public are also beginning to describe the different clinical symptoms between men and women [36]. These differences in clinical presentation could be linked to different pathophysiology. It is now known that some forms of ACS are more frequent in women, such as ACS type 2, which is based on an inadequacy in myocardial oxygen caused by insufficient intake, without acute coronary injury; and myocardial infarction with non-obstructive coronary arteries (MINOCA), whose pathophysiology has not been clearly elucidated [3].
Unfortunately, all of the studies on ACS in our meta-analysis did not specify the pathophysiology of the latter, which may therefore be predominant in women. Cohorts underlining the mechanisms of ACS could help to clarify the link between the clinical presentation and the gender of the patient and the kind of ACS.
There was an effect of the region on the logarithm of the relative risk only for nausea-vomiting, increased or irregular heart rate and shoulder pain with all patients. There is sometimes significant heterogeneity in some symptoms, which is why the models used were random effects. The meta-regression showed that the heterogeneity could be partly explained by the region, but other factors are also possibly responsible.
Limitations
Our study had several limitations. First, not all territories were covered, especially not low-income countries, thereby limiting the generalization of our results to middle- or high-income countries. Secondly, our equations excluded unpublished studies in English and French. Some studies, published in other languages, may potentially find different results. Thirdly, some symptoms were lacking in precision—for example, the lateralization of pain for pain in the arm or shoulder. All the selected studies reported the symptom of chest pain; however, it was not possible to analyze this symptom for two studies because chest pain was divided into several locations (retrosternal, laterothoracic, etc.) and we could not determine how many patients had chest pain. Then some symptoms, such as confusion and headache, which were mentioned in some studies, could not be included in our meta-analysis due to a lack of data.
5. Conclusions
Women with ACS are at greater risk of developing clinical symptoms such as dyspnea, arm pain, nausea, vomiting, fatigue and palpitations than men. In light of this knowledge, the notion of “typical” or “atypical” ACS symptoms should no longer exist. More than half of the victims of ACS are women, so it is now more than necessary to give this knowledge to health students, health professionals and the general public.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm11051319/s1.
Author Contributions
M.C. and L.A.V. independently assessed the studies for eligibility and extracted data from the included full text citations with a report form validated by N.P. F.L. carried out the statistical analysis. M.C., L.A.V., F.B., L.C., P.L.B. and C.G.-J. revised all the work. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
There was no dedicated funding for this work. All authors thank Gilles Garatti for his help in correcting the English and Tahar Chouihed for his wise advice at the time of M.C.’s thesis defense that concerned this study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- World Health Organization. Cardiovascular Diseases. 2017. Available online: https://www.who.int/fr/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed on 4 August 2021).
- World Health Organization. The Top 10 Causes of Death. Available online: https://www.who.int/fr/news-room/fact-sheets/detail/the-top-10-causes-of-death (accessed on 4 August 2021).
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D.; Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction. Fourth Universal Definition of Myocardial Infarction (2018). Circulation 2018, 138, e618–e651. [Google Scholar] [CrossRef] [PubMed]
- Collet, J.P.; Thiele, H.; Barbato, E.; Barthélémy, O.; Bauersachs, J.; Bhatt, D.L.; Dendale, P.; Dorobantu, M.; Edvardsen, T.; Folliguet, T.; et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur. Heart J. 2021, 42, 1289–1367. [Google Scholar] [CrossRef]
- DeVon, H.A.; Mirzaei, S.; Zègre-Hemsey, J. Typical and Atypical Symptoms of Acute Coronary Syndrome: Time to Retire the Terms? J. Am. Heart Assoc. 2020, 9, e015539. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-S.; Kim, Y.-J.; Shin, D.-G.; Jeong, J.-O.; Ahn, Y.-K.; Chung, W.-S.; Seung, K.-B.; Kim, C.-J.; Cho, M.-C.; Jang, Y.-S.; et al. Gender Differences in Clinical Features and In-hospital Outcomes in ST-segment Elevation Acute Myocardial Infarction: From the Korean Acute Myocardial Infarction Registry (KAMIR) Study. Clin. Cardiol. 2010, 33, E1–E6. [Google Scholar] [CrossRef] [PubMed]
- Butala, N.M.; Desai, M.M.; Linnander, E.L.; Wong, Y.R.; Mikhail, D.G.; Ott, L.S.; Spertus, J.A.; Bradley, E.H.; Aaty, A.A.; Abdelfattah, A.; et al. Gender Differences in Presentation, Management, and In-Hospital Outcomes for Patients with AMI in a Lower-Middle Income Country: Evidence from Egypt. PLoS ONE 2011, 6, e25904. [Google Scholar] [CrossRef] [PubMed]
- Lichtman, J.H.; Leifheit-Limson, E.C.; Watanabe, E.; Allen, N.B.; Garavalia, B.; Garavalia, L.S.; Spertus, J.A.; Krumholz, H.M.; Curry, L.A. Symptom Recognition and Healthcare Experiences of Young Women With Acute Myocardial Infarction. Circ. Cardiovasc. Qual. Outcomes 2015, 8, S31–S38. [Google Scholar] [CrossRef] [PubMed]
- Bjerking, L.H.; Hansen, K.W.; Madsen, M.; Jensen, J.S.; Madsen, J.K.; Sørensen, R.; Galatius, S. Use of diagnostic coronary angiography in women and men presenting with acute myocardial infarction: A matched cohort study. BMC Cardiovasc. Disord. 2016, 16, 120. [Google Scholar] [CrossRef]
- Canto, J.G.; Rogers, W.J.; Goldberg, R.J.; Peterson, E.D.; Wenger, N.K.; Vaccarino, V.; Kiefe, C.I.; Frederick, P.; Sopko, G.; Zheng, Z.-J.; et al. Association of Age and Sex with Myocardial Infarction Symptom Presentation and In-Hospital Mortality. JAMA J. Am. Med. Assoc. 2012, 307, 813–822. [Google Scholar] [CrossRef]
- Devon, H.A.; Rosenfeld, A.; Steffen, A.D.; Daya, M. Sensitivity, specificity, and sex differences in symptoms reported on the 13-item acute coronary syndrome checklist. J. Am. Heart Assoc. 2014, 3, e000586. [Google Scholar] [CrossRef]
- Ferry, A.V.; Anand, A.; Strachan, F.E.; Mooney, L.; Stewart, S.D.; Marshall, L.; Chapman, A.; Lee, K.K.; Jones, S.; Orme, K.; et al. Presenting Symptoms in Men and Women Diagnosed with Myocardial Infarction Using Sex-Specific Criteria. J. Am. Heart Assoc. 2019, 8, e012307. [Google Scholar] [CrossRef]
- Rubini Gimenez, M.; Reiter, M.; Twerenbold, R.; Reichlin, T.; Wildi, K.; Haaf, P.; Wicki, K.; Zellweger, C.; Hoeller, R.; Moehring, B.; et al. Sex-specific chest pain characteristics in the early diagnosis of acute myocardial infarction. JAMA Intern. Med. 2014, 174, 241–249. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.K.; Ferry, A.V.; Anand, A.; Strachan, F.E.; Chapman, A.; Kimenai, D.M.; Meex, S.J.; Berry, C.; Findlay, I.; Reid, A.; et al. Sex-Specific Thresholds of High-Sensitivity Troponin in Patients with Suspected Acute Coronary Syndrome. J. Am. Coll. Cardiol. 2019, 74, 2032–2043. [Google Scholar] [CrossRef] [PubMed]
- Lichtman, J.H.; Leifheit, E.C.; Safdar, B.; Bao, H.; Krumholz, H.M.; Lorenze, N.P.; Daneshvar, M.; Spertus, J.A.; D’Onofrio, G. Sex Differences in the Presentation and Perception of Symptoms Among Young Patients with Myocardial Infarction: Evidence from the VIRGO Study (Variation in Recovery: Role of Gender on Outcomes of Young AMI Patients). Circulation 2018, 137, 781–790. [Google Scholar] [CrossRef] [PubMed]
- Nanna, M.G.; Hajduk, A.; Krumholz, H.M.; Murphy, T.E.; Dreyer, R.P.; Alexander, K.P.; Mary Geda, M.; Tsang, S.; Welty, F.K.; Safdar, B.; et al. Sex-Based Differences in Presentation, Treatment, and Complications among Older Adults Hospitalized for Acute Myocardial Infarction: The SILVER-AMI Study. Circ. Cardiovasc. Qual. Outcomes 2019, 12, e005691. [Google Scholar] [CrossRef]
- Patel, A.; Vishwanathan, S.; Nair, T.; Bahuleyan, C.G.; Jayaprakash, V.L.; Baldridge, A.S.; Huffman, M.; Prabhakaran, D.; Mohanan, P.P. Sex Differences in the Presentation, Diagnosis, and Management of Acute Coronary Syndromes: Findings from the Kerala-India ACS Registry. Glob. Heart 2015, 10, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Pelter, M.M.; Riegel, B.; McKinley, S.; Moser, D.K.; Doering, L.V.; Meischke, H.; Davidson, P.; Baker, H.; Yang, W.; Dracup, K. Are there symptom differences in patients with coronary artery disease presenting to the ED ultimately diagnosed with or without ACS? Am. J. Emerg. Med. 2012, 30, 1822–1828. [Google Scholar] [CrossRef]
- Shah, A.; Griffiths, M.; Lee, K.K.; McAllister, D.; Hunter, A.L.; Ferry, A.V.; Cruikshank, A.; Reid, A.; Stoddart, M.; Strachan, F.; et al. High sensitivity cardiac troponin and the under-diagnosis of myocardial infarction in women: Prospective cohort study. BMJ 2015, 350, g7873. [Google Scholar] [CrossRef]
- Shehab, A.; Bhagavathula, A.S.; Alhabib, K.F.; Ullah, A.; Suwaidi, J.A.; Almahmeed, W.; AlFaleh, H.; Zubaid, M. Age-Related Sex Differences in Clinical Presentation, Management, and Outcomes in ST-Segment-Elevation Myocardial Infarction: Pooled Analysis of 15 532 Patients From 7 Arabian Gulf Registries. J. Am. Heart Assoc. 2020, 9, e013880. [Google Scholar] [CrossRef] [PubMed]
- Sörensen, N.A.; Neumann, J.T.; Ojeda, F.; Schäfer, S.; Magnussen, C.; Keller, T.; Lackner, K.J.; Zeller, T.; Karakas, M.; Münzel, T.; et al. Relations of Sex to Diagnosis and Outcomes in Acute Coronary Syndrome. J. Am. Heart Assoc. 2018, 7, e007297. [Google Scholar] [CrossRef]
- van der Meer, M.G.; Backus, B.E.; van der Graaf, Y.; Cramer, M.J.; Appelman, Y.; Doevendans, P.A.; Six, A.J.; Nathoe, H.M. The diagnostic value of clinical symptoms in women and men presenting with chest pain at the emergency department, a prospective cohort study. PLoS ONE 2015, 10, e0116431. [Google Scholar] [CrossRef]
- You, B.; Zhu, B.; Su, X.; Liu, F.; Wang, B. Gender Differences among Elderly Patients with Primary Percutaneous Coronary Intervention. Aging Dis. 2018, 9, 852–860. [Google Scholar] [CrossRef] [PubMed]
- Perrino, C.; Ferdinandy, P.; Bøtker, H.E.; Brundel, B.J.J.M.; Collins, P.; Davidson, S.M.; den Ruijter, H.M.; Engel, F.B.; Gerdts, E.; Girao, H.; et al. Improving translational research in sex-specific effects of comorbidities and risk factors in ischaemic heart disease and cardioprotection: Position paper and recommendations of the ESC Working Group on Cellular Biology of the Heart. Cardiovasc Res. 2021, 117, 367–385. [Google Scholar] [CrossRef]
- Canto, J.G.; Goldberg, R.J.; Hand, M.M.; Bonow, R.O.; Sopko, G.; Pepine, C.J.; Long, T. Symptom presentation of women with acute coronary syndromes: Myth vs reality. Arch. Intern. Med. 2007, 167, 2405–2413. [Google Scholar] [CrossRef] [PubMed]
- Arslanian-Engoren, C.; Patel, A.; Fang, J.; Armstrong, D.; Kline-Rogers, E.; Duvernoy, C.S.; Eagle, K.A. Symptoms of Men and Women Presenting With Acute Coronary Syndromes. Am. J. Cardiol. 2006, 98, 1177–1181. [Google Scholar] [CrossRef]
- Jneid, H.; Fonarow, G.; Cannon, C.P.; Hernandez, A.F.; Palacios, I.F.; Maree, A.; Wells, Q.; Bozkurt, B.; LaBresh, K.A.; Liang, L.; et al. Sex Differences in Medical Care and Early Death After Acute Myocardial Infarction. Circulation 2008, 118, 2803–2810. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Wells, G.A. The Ottawa Hospital Research Institute. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 26 August 2021).
- Dey, S.; Flather, M.D.; Devlin, G.; Brieger, D.; Gurfinkel, E.P.; Steg, P.G.; Fitzgerald, G.; Jackson, E.A.; Eagle, K.A.; Global Registry of Acute Coronary Events Investigators. Sex-related differences in the presentation, treatment and outcomes among patients with acute coronary syndromes: The Global Registry of Acute Coronary Events. Heart 2009, 95, 20–26. [Google Scholar] [CrossRef] [PubMed]
- Kirchberger, I.; Heier, M.; Kuch, B.; Wende, R.; Meisinger, C. Sex Differences in Patient-Reported Symptoms Associated with Myocardial Infarction (from the Population-Based MONICA/KORA Myocardial Infarction Registry). Am. J. Cardiol. 2011, 107, 1585–1589. [Google Scholar] [CrossRef]
- van Oosterhout, R.E.M.; de Boer, A.R.; Maas, A.H.E.M.; Rutten, F.H.; Bots, M.L.; Peters, S.A.E. Sex Differences in Symptom Presentation in Acute Coronary Syndromes: A Systematic Review and Meta-analysis. J. Am. Heart Assoc. 2020, 9, e014733. [Google Scholar] [CrossRef]
- Connaitre les Numéros D’urgence. Available online: https://www.gouvernement.fr/risques/connaitre-les-numeros-d-urgence (accessed on 5 August 2021).
- Harvard Medical School. Chest Pain. Available online: https://www.health.harvard.edu/decision_guide/chest-pain#yesiamexperiencingonormoreofthesesymptoms (accessed on 5 August 2021).
- Birnbach, B.; Höpner, J.U.; Mikolajczyk, R. Cardiac symptom attribution and knowledge of the symptoms of acute myocardial infarction: A systematic review. BMC Cardiovasc. Disord. 2020, 20, 445. [Google Scholar] [CrossRef]
- Fédération Française de Cardiologie. Rétrospective de Nos Campagnes Vidéo. Available online: https://fedecardio.org/nous-connaitre/retrospective-publicitaire/ (accessed on 5 August 2021).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).