Abstract
Despite its positive influence on physical and mental wellbeing, running is associated with a high incidence of musculoskeletal injury. Potential modifiable risk factors for running-related injury have been identified, including running biomechanics. Gait retraining is used to address these biomechanical risk factors in injured runners. While recent systematic reviews of biomechanical risk factors for running-related injury and gait retraining have been conducted, there is a lack of information surrounding the translation of gait retraining for injured runners into clinical settings. Gait retraining studies in patients with patellofemoral pain syndrome have shown a decrease in pain and increase in functionality through increasing cadence, decreasing hip adduction, transitioning to a non-rearfoot strike pattern, increasing forward trunk lean, or a combination of some of these techniques. This literature suggests that gait retraining could be applied to the treatment of other injuries in runners, although there is limited evidence to support this specific to other running-related injuries. Components of successful gait retraining to treat injured runners with running-related injuries are presented.
1. Background
The sport of running has positive effects on both physical [1] and mental [2] wellbeing. Unfortunately, runners experience a high rate of running-related injuries (RRIs). While reports of incidence rate vary depending on the population, up to 79% of recreational runners suffer a RRI each year [3]. In addition, RRIs have a high rate of recurrence. For example, female youth runners with a history of bone stress injury (BSI) have a 5 times elevated risk of sustaining a subsequent BSI [4]. Similar rates of injury reoccurrence were found in high school cross country runners [5].
Prior research has characterized risk factors for RRI. Of those that are modifiable, risk factors include neuromuscular, kinetic, kinematic, and spatiotemporal variables. While muscle weakness and imbalance may contribute to RRIs [6], strengthening alone may be insufficient for modifying biomechanical abnormalities that contribute to RRI [7]. Several variables related to running mechanics are thought to be related to injury and are frequent targets of intervention, including hip adduction [8,9], trunk lean [10,11], vertical loading rates [12,13,14,15,16,17,18], and step rate [19,20,21,22].
Gait retraining has been described as a method to change running biomechanics contributing to a given RRI [23]. Gait retraining using external feedback was first described in patients following stroke [24]. It used concepts of motor learning for both acquisition and transfer phases and resulted in sustained improvements in hemiparetic gait. These concepts have since been applied to the management of RRIs by addressing a variety of aspects related to gait mechanics. Gait retraining typically involves the use of devices to measure the targeted biomechanical variable and provide external visual, verbal, or auditory cues to facilitate change. These external cues are described as biofeedback, and a faded biofeedback design refers to gradual reduction in external cues to promote learning of a new desired movement pattern without further feedback [24].
For gait retraining to be effective, biomechanical risk factors associated with RRI must be properly identified, and, if possible, addressed appropriately during treatment. The results of a recent systematic review and meta-analysis, which evaluated different forms of gait retraining [23], suggest that the literature surrounding gait retraining is occasionally inconsistent and largely inconclusive. There is need for a more easily digestible guide for clinicians seeking to implement gait retraining in the treatment of injured runners. The purpose of this narrative review is to provide a practical overview of what is known on biomechanical risk factors for RRI, gait retraining strategies to alter these risk factors, and provide clinical practical application of this knowledge.
2. Methods
This narrative review included studies related to the following topics: (I) Biomechanical risk factors for RRI, and (II) Gait retraining for runners with RRI. No restrictions were placed on language, publication date, participant age, gender, and duration of symptoms or stage of disease. Articles were excluded if: (I) running was not the primary focus of the study; (II) there was not a clear description of the gait retraining protocol used; (III) feedback was not removed after gait retraining to determine if gait adjustments could be maintained; (IV) the protocol did not use multiple sessions to allow for motor learning to occur. Additionally, studies that were not presented as a full manuscript (i.e., abstracts) were excluded. PubMed and EMBASE were the databases used. The date of the last search was 30 June 2022. Subject headings, synonyms, relevant terms, and variant spellings of three concepts (running biomechanics; gait retraining; running-related injuries) were used for the searches on each database. This strategy was used for each database with the appropriate truncation. All references were imported into Mendeley Reference Manager (Version 2.65.0), and duplicates were removed. The screening of eligible studies was performed in two steps: (I) screening the titles and abstracts, and (II) screening the full texts. List of references of the retrieved studies were searched to identify additional publications. Eligibility assessment was performed by two reviewers (LWG and MB). Disagreements were resolved by discussion between the two review authors. If no agreement could be reached, a final arbitration was performed by a third independent reviewer (AST). Relevant information was organized using the following topics: (I) Biomechanical risk factors for RRI; (II) Gait retraining overview; (III) Interventions characterizing gait retraining variables; (IV) Clinical application of gait retraining; (V) Limitation of current gait retraining strategies.
3. Biomechanical Risk Factors for Running-Related Injury (RRI)
Two recent systematic reviews of prospective studies have examined potential biomechanical risk factors for RRI [25,26]. Both reviews concluded that there was not strong evidence for a single biomechanical variable as a risk factor for all RRIs. The lack of an association between biomechanical variables and grouped RRI indicates the importance of investigating injury-specific biomechanical risk factors for RRI.
A recent systemic review examined biomechanical risk factors for several common RRIs including hamstring tendinopathy, patellofemoral pain syndrome (PFPS), patellar tendinopathy, iliotibial band syndrome, medial tibial stress syndrome, tibial stress fractures, Achilles tendinopathy, and plantar fasciitis [27]. Criteria for inclusion of a biomechanical risk factor in the study was a significant difference from a control group in one prospective study or two retrospective studies [27]. Levels of evidence for biomechanical risk factors for specific RRIs varied from conflicting evidence to moderate evidence.
The strongest evidence supported decreased braking impulse [28,29] and increased ground contact time [28,29] for PFPS, increased duration of rearfoot eversion angle [30,31] and increased contralateral pelvic drop angle [30,32] for medial tibial stress syndrome, and increased average [33,34] and instantaneous loading rate [33,35] of vertical ground reaction force for plantar fasciitis. Each biomechanical variable was observed to have moderate evidence as risk factors for specific RRIs. More limited evidence was found for biomechanical risk factors for Achilles tendinopathy and tibial stress fractures, and very limited evidence was found for iliotibial band syndrome. No biomechanical variables met the study criteria for inclusion for patellar tendinopathy and hamstring tendinopathy. Definitions of potential biomechanical risk factors can be found below in Table 1.

Table 1.
Definitions of key biomechanical variables.
4. Gait Retraining Overview
A narrative review published in 2020 evaluated the use of gait retraining as an intervention for PFPS [37]. The review included mostly case series or studies that did not contain a control group. Most biomechanical interventions included in the review, specifically decreasing hip adduction, increasing trunk lean, transitioning from a rearfoot strike (RFS) to a forefoot strike pattern, and increasing cadence, resulted in a reduction of pain [37]. The review also concluded that greater gait retraining session volume and a faded feedback design resulted in better outcomes compared to studies without a faded feedback design.
While a previous systematic review conducted in 2015 found foot strike manipulation had the greatest effect on kinematic measures and live feedback of tibial acceleration had the greatest effect on kinetic measures [38], a more recent systematic review and meta-analysis of gait retraining by Doyle et al. [23], which included only randomized controlled trials, concluded that the best evidence for gait retraining for runners supported step rate-based gait retraining. Though it achieved only moderate evidence, step rate-based gait retraining was shown to increase step rate, decrease stride length, decrease peak hip adduction (HADD) during stance, increase footstrike angle at initial contact and decrease VALR and VILR. Moderate evidence was also found for the ability of tibial acceleration based gait retraining to lower VILR.
While some gait retraining studies have reported a decrease in pain and improvement in functional outcomes in patients that underwent gait retraining, an insufficient number of studies reported pain measurements or clinical outcomes compared to a control group for inclusion in the systematic review and meta-analysis for conclusions regarding the effectiveness of gait retraining on patient pain or clinical outcomes to be made [23]. A summary of gait retraining studies and their effect on various clinical and biomechanical outcome variables can be seen in Table 2.

Table 2.
Overview of Gait Retraining Studies.
5. Interventions Characterizing Gait Retraining Variables
Biomechanical targets of gait retraining studies (shown above in Table 2) include degree of hip adduction [8,9], step rate [19,20,21], tibial acceleration [12,14,15,16,17,18,39,45], footstrike pattern [41,42,43,44] and trunk lean [10]. The outcome measures of each study varied and included pain and functionality in injured runners, joint angles, and measures of loading rates (such as VALR and VILR) in healthy runners.
While the literature supporting hip adduction as a risk factor for PFPS is inconsistent [27], two studies have reported beneficial outcomes related to reduced hip adduction in runners with PFPS [8,9]. One study used a real time display generated by motion capture technology to display hip adduction [8], while the other study used visual feedback with a full-length mirror [9]. Both studies reported decreases in pain and increases in functionality, exceeding the minimal clinically important difference, at the end of the trial and at a 1- or 3-month follow-up.
Increases in step rate by 5% or 10% have been shown to lower COM vertical excursion, decrease breaking impulse and transition runners towards a more anterior footstrike pattern [36]. Three gait retraining studies have shown that step rate can be altered through gait retraining outside of a laboratory setting, including while runners continue with their training [20,21,50]. Willy et al. [20] found that this increase in step rate was also associated with a decrease in VALR, VILR and HADD [20]. A decrease in pain and increase in functionality was seen at the 6-month follow-up in runners that underwent gait retraining to increase their step rate by 10% [11]. The changes in step rate seen after gait retraining may not be constant at faster speeds, however [50]. One prospective study found no difference in KOS-ADLS scores between runners who received education on load management and underwent gait retraining based on step rate compared to those who only received education on load management [19]. A possible side effect of step rate-based gait retraining is calf muscle soreness. In one study, 43% of participants mentioned calf muscle soreness [49]. However, this did not affect running volume.
Tibial acceleration is a common variable of interest in gait retraining studies as a surrogate measure of loading rate. While a variety of techniques can be used to decrease tibial acceleration, some studies have found that runners are capable of lowering their tibial accelerations with visual feedback combined with instruction to land “softly” and “quietly” [14,39,41]. A study that used visual feedback of accelerometer data for gait retraining found significant reductions in tibial acceleration, VIP, VALR and VILR at post-training compared to pre-training [14]. Tibial acceleration, VIP, VALR and VILR all remained significantly reduced at 1-month, 6-month, and 12-month follow-ups.
Transitioning from a rearfoot strike to a forefoot strike has been shown to decrease loading rates while running [41]. Improvements in clinical outcomes that reach minimal clinically important difference in patients with PFPS that switch to a forefoot strike have been reported in a case series study [11]. These improvements remained at a 6-month follow-up. One randomized controlled trial found a significant reduction in pain in runners with PFPS that underwent gait retraining while the control group did not experience any significant changes in pain. However, subjects that underwent gait retraining reported calf soreness while undergoing gait retraining. Twenty-five percent of participants from the retraining group also reported ankle soreness at the 1-month follow-up when running more than 4 miles in a single session [42]. Chan et al. also found that runners who transitioned to a midfoot striking pattern did not display significantly different load rates compared to rearfoot strikers [43].
While fewer studies involving trunk lean were found, improvements in functional outcomes and decreases in pain were reported immediately upon the completion of gait retraining and at a 6-month follow-up [11]. Changes in functionality between pre-training and post-training reached minimal clinically important difference. These changes were similar to the changes seen in the treatment group that transitioned to a forefoot strike pattern.
6. Clinical Application of Gait Retraining
Sports injuries are complex and result from a combination of intrinsic and extrinsic factors [51]. Although biomechanics play a role in RRIs [27], it is important to highlight that a multifactorial perspective is required, and clinicians must identify the non-linear interactions between biomechanics and other aspects that may be related to injuries [51]. Gait retraining expands upon traditional approaches of addressing impairments in strength and flexibility to address abnormal biomechanics and motor control and should be considered as an aspect of a multimodal approach.
Most research on gait retraining strategies identified in this review (Table 2) focus on changing lower extremity mechanics to address knee pain. In PFPS, best evidence guidelines include exercises to improve hip and knee strength [52]. In the basics of the preliminary strengthening phase, the patient can also be considered in the cognitive stages of learning, using different exercises to gain intrinsic awareness of these muscles, and using visual cues to gain greater proprioceptive awareness. The treatment program then progresses to the associative stages of learning as tasks become more challenging. At this point, the participant should not only improve strength based on exercise prescription but improve ability to modify their alignment in a variety of tasks.
After addressing the pre-gait guidelines for management of PFPS, patients may further benefit by participating in gait retraining programs. Changes in pain and function up to six months were seen in runners with hip adduction greater than 20° that received visual feedback and were cued to “run with your knees apart with your kneecaps pointing straight ahead” [8,9], in runners with trunk flexion of 11° that were asked to “run with an increase in flexed trunk posture” [11], in runners with step rate between 160 to 170 steps/minute that were cued via an audio metronome set at 7.5–10% above their baseline step rate [11,19,49], and in runners that adopted a forefoot strike pattern using visual feedback and cues such as “run on your toes” and/or “run on the balls of your feet” [11,42].
The programs can be done using 8–12 sessions completed over 2–4 weeks (average of 2–3 gait retraining sessions per week). In this design, the feedback is provided continually in the first week and then is gradually removed in the second week. Run time progressively increases from 15 to 30 min [8,9,11,41,42]. This faded feedback program prevents dependency on external feedback and generates long-term retention [24]. Various other gait retraining programs have been proposed for patients with PFPS [19,49,53]. These include programs using five sessions over eight weeks [19], ten sessions over six weeks [49], and or only one session of ten minutes followed by four weeks of self-administration and monitoring increased step rate [53]. Each has shown improvements in symptoms and function and thus may be considered as an alternative to the above gait retraining prescription. Considerations for type of gait retraining intervention need to account for multiple factors including type of injury being treated, injury duration, time in season, and level of competition, with the goal of developing a long-term strategy to reduce risk for new or recurrent RRI.
Gait retraining implementation must consider the role of muscle strength and fatiguability, as different strategies will have different demands of the neuromotor system. An increase in trunk flexion is associated with greater peak hip extension moment [54], and transition to a forefoot strike is associated with greater peak ankle plantarflexion moment [55]. Strengthening the calf muscles may reduce the incidence of calf soreness that was reported for the step rate [49] and forefoot strike strategies [42]. Similarly, strengthening hip extensor muscles may facilitate a better transition to a gait with increased trunk lean [56]. Further, a combination of gait retraining strategies may be used to achieve the goals of the retraining program. Previous studies based on increasing step rate instructed patients to land softly [49] or to land softly and adopt a non-rearfoot strike pattern if necessary [19].
Regardless of the benefits for injured runners, very limited evidence supports the use of gait retraining for healthy runners. Athletes with VALR greater than 70 BW/s that received visual feedback and were instructed to “run softer” presented a 62% lower occurrence of RRIs in a year [57]. Only one retrospective study provided evidence that RFS runners present higher rates of prior RRIs than non-rearfoot strikers [58] and conversely another cross-sectional study found that a non-RFS was associated with calf muscle injuries and Achilles tendinopathy. Since no prospective studies have been performed, the transition to a forefoot strike in healthy runners cannot be uniformly recommended using evidence-based treatment [59,60]. Finally, limited evidence shows that the transition to a forefoot strike does not change running economy at fast speeds and limited-to-moderate evidence shows a decrease in running economy at low-medium speeds in recreational runners [59]. Therefore, changing the foot strike pattern to improve the running economy is not recommended. The potential of the other strategies to reduce the likelihood of RRIs and improve performance was not assessed.
While gait retraining has largely been studied for those with PFPS; limited work has been conducted on addressing biomechanical risk factors in non-PFPS RRI. Examples of gait retraining strategies that may be applied to runners presenting with various injuries are illustrated in Figure 1 and Figure 2. It is important to note that gait retraining has only been used to treat runners with PFPS and chronic exertional compartment syndrome (CECS). Studies examining the effect of gait retraining on pain and functionality in many common running injuries do not currently exist, so specific recommendations for using gait retraining in injured runners with injuries other than PFPS and CECS cannot be made. Figure 1 and Figure 2 serve only to provide examples on how a clinician may treat an injured runner using gait retraining based on literature surrounding gait retraining studies and risk factors for specific RRIs such as medial tibial stress syndrome [30,32], tibial stress fractures [61,62], iliotibial band syndrome [63,64], PFPS [28,29,32,42,65,66,67], CECS [46] and plantar fasciitis [33,34,35].
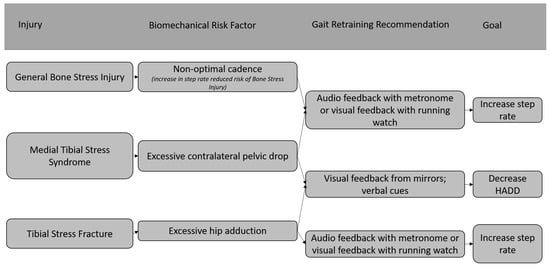
Figure 1.
Examples of using gait retraining to treat bone related RRIs [22,30,32,61,62].
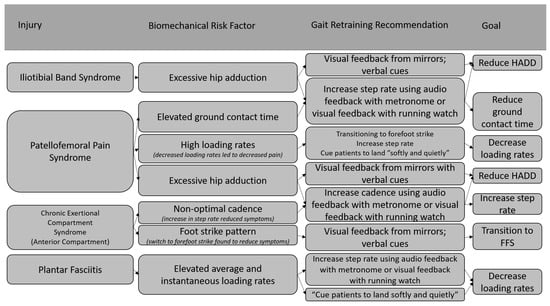
Figure 2.
Examples of using gait retraining to treat other specific RRIs [28,29,32,33,34,35,42,46,63,64,65,66,67].
7. Limitations of Current Gait Retraining Strategies
Most studies characterizing gait retraining require participants to limit their running to gait retraining sessions in a laboratory setting [12,14]. This may discourage injured runners with an upcoming race, or those unwilling to take extended time away from running, from undergoing gait retraining. Studies that have allowed participants to continue with their own training schedules outside of gait retraining have found that runners can benefit from performing gait retraining while still participating in training outside of the laboratory [10,16,44]. Gait retraining completed outside of a laboratory setting while still continuing typical training has been observed to significantly reduce footstrike angle and increase step rate [50]. While this study did not report any negative outcomes for participants, RRI risk should be considered when allowing runners to continue with training while completing gait retraining, accounting for time for soft tissue and bone adaptations. Since this study only examined step rate manipulation, adjusting other variables may be less feasible outside of the clinical setting.
Despite the success found in gait retraining strategies employed in many of the studies examined in this review, a study conducted by Esculier et al. [19] found that education of proper training loads and education combined with gait retraining resulted in similar decreases in knee pain in runners with PFPS. Notably the session duration and frequency was lower than standard gait retraining programs and did not use a faded feedback design [8,9,11,14,18,41,42,47]. This discrepancy in results highlights that not all gait retraining protocols are equally effective, and that it is important to identify factors that may aid in the success of a gait retraining protocol.
Presently, it is unknown if gait retraining effectiveness is influenced by severity of injury. For example, improvement in pain and functionality in patients with PFPS following gait retraining only included participants that reported a pain level below a 7 out of 10 on a visual analog scale [42]. A separate investigation on gait retraining instructed PFPS patients to run only when their pain level was below a 2 out of 10 on the visual analog scale [19]. Thus, patients who report severe pain while running may benefit from undergoing other forms of treatment before beginning gait retraining.
There exists a clear gap in the literature surrounding gait retraining in terms of randomized controlled trials. Only two randomized controlled gait retraining studies have examined the effects of gait retraining as a form of injury treatment [19,42]. Both trials examined knee pain as an outcome measure and the two studies found contrasting results. While one study found a significant reduction in knee pain in the group that underwent gait retraining [42], the other study found there was no difference in knee pain in those who had undergone gait retraining and education compared to those who had underwent education alone [19]. Other studies using gait retraining did not record patient pain levels or did not include a control group. No randomized controlled trials have examined the effect of gait retraining on pain and functionality in RRIs other than PFPS. Further investigation into the effects of gait retraining as treatment for specific injuries may reveal that gait retraining is not equally effective for all types of RRIs. Identifying specific injuries that gait retraining is more effective in treating could increase the value of gait retraining as a rehabilitation tool for RRIs.
Only two studies included in this review reported adverse effects [42,49]. Both studies cited soreness of the calves that did not affect the ability of subjects to complete their training. One study reported ankle soreness at a 1-month follow-up after gait retraining. The time to achieve strength and tissue adaption must be individualized to reduce risk for RRI and gait retraining should be progressed gradually. More studies investigating potential adverse effects of gait retraining are needed before gait retraining can be fully recommended as a treatment strategy in injured runners.
8. Conclusions
While biomechanical risk factors are variable across RRIs, gait retraining may be used to modify potentially faulty running mechanics. An individualized and diagnosis-specific approach is important to address specific risk factors for the injured runner. Running mechanics can be modified using different forms of biofeedback and should use a faded feedback design for motor learning. Future studies, ideally in a randomized clinical study design, may clarify how different forms of gait retraining may be used, alone or in combination, to treat and prevent RRI.
Author Contributions
Conceptualization, L.W.G., M.M.B., A.S.T., L.W. and J.P.; formal analysis, L.W.G. and M.M.B.; writing—original draft preparation, L.W.G., M.M.B., J.P. and L.W.; writing—review and editing, J.R.d.S.J., B.H., C.D.J., L.K.S., M.J.R., K.H. and A.S.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
All authors have no disclosures related to this work. José Roberto de Souza Junior is a Fulbright visiting research student at the Spaulding National Running Center. Bryan Heiderscheit is a paid consultant to Biocore, has ownership interest in Science of Running Medicine LLC, is an advisory board member for Springbok Analytics and has received research funding (paid to institution) from the National Football League, National Basketball Association and GE Healthcare. Adam Tenforde serves as Senior editor for PM&R Journal. He gives professional talks such as grand rounds and medical conference plenary lectures and receives honoraria from conference organizers. He has participated in research funded by Arnold P. Gold Foundation (physician and patient care disparities), Football Player Health Study at Harvard (health in American-Style Football players), American Medical Society for Sports Medicine (bone density research), Uniform Health Service and Enovis (Achilles tendinopathy). He is a paid consultant for State Farm Insurance and Strava.
References
- Lee, D.C.; Pate, R.R.; Lavie, C.J.; Sui, X.; Church, T.S.; Blair, S.N. Leisure-time running reduces all-cause and cardiovascular mortality risk. J. Am. Coll. Cardiol. 2014, 64, 472–481. [Google Scholar] [CrossRef] [PubMed]
- Oswald, F.; Campbell, J.; Williamson, C.; Richards, J.; Kelly, P. A scoping review of the relationship between running and mental health. Int. J. Environ. Res. Public Health 2020, 17, 8059. [Google Scholar] [CrossRef] [PubMed]
- Lun, V.; Meeuwisse, W.H.; Stergiou, P.; Stefanyshyn, D. Relation between running injury and static lower limb alignment in recreational runners. Br. J. Sports Med. 2004, 38, 576–580. [Google Scholar] [CrossRef] [PubMed]
- Kelsey, J.L.; Bachrach, L.K.; Procter-Gray, E.; Nieves, J.; Greendale, G.A.; Sowers, M.; Brown, B.W.; Matheson, K.A.; Crawford, S.L.; Cobb, K.L. Risk factors for stress fracture among young female cross-country runners. Med. Sci. Sports Exerc. 2007, 39, 1457–1463. [Google Scholar] [CrossRef] [PubMed]
- Rauh, M.J.; Margherita, A.J.; Rice, S.G.; Koepsell, T.D.; Rivara, F.P. High School Cross Country Running Injuries: A Longitudinal Study. J. Clin. Sport Med. 2000, 10, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Mucha, M.D.; Caldwell, W.; Schlueter, E.L.; Walters, C.; Hassen, A. Hip abductor strength and lower extremity running related injury in distance runners: A systematic review. J. Sci. Med. Sport 2017, 20, 349–355. [Google Scholar] [CrossRef]
- Willy, R.W.; Davis, I.S. The effect of a hip-strengthening program on mechanics during running and during a single-leg squat. J. Orthop. Sports Phys. Ther. 2011, 41, 625–632. [Google Scholar] [CrossRef]
- Noehren, B.; Scholz, J.; Davis, I. The effect of real-time gait retraining on hip kinematics, pain and function in subjects with patellofemoral pain syndrome. Br. J. Sports Med. 2011, 45, 691–696. [Google Scholar] [CrossRef]
- Willy, R.W.; Scholz, J.P.; Davis, I.S. Mirror gait retraining for the treatment of patellofemoral pain in female runners. Clin. Biomech. 2012, 27, 1045–1051. [Google Scholar] [CrossRef]
- Teng, H.-L.; Dilauro, A.; Weeks, C.; Odell, C.; Kincaid, H.; VanDine, B.; Wu, W.F. Short-term effects of a trunk modification program on patellofemoral joint stress in asymptomatic runners. Phys. Ther. Sport 2020, 44, 107–113. [Google Scholar] [CrossRef]
- Dos Santos, A.F.; Nakagawa, T.H.; Lessi, G.C.; Luz, B.C.; Matsuo, H.T.; Nakashima, G.Y.; Maciel, C.D.; Serrão, F.V. Effects of three gait retraining techniques in runners with patellofemoral pain. Phys. Ther. Sport 2019, 36, 92–100. [Google Scholar] [CrossRef] [PubMed]
- Crowell, H.P.; Davis, I.S. Gait retraining to reduce lower extremity loading in runners. Clin. Biomech. 2011, 26, 78–83. [Google Scholar] [CrossRef] [PubMed]
- Clansey, A.C.; Hanlon, M.; Wallace, E.S.; Nevill, A.; Lake, M.J. Influence of Tibial shock feedback training on impact loading and running economy. Med. Sci. Sports Exerc. 2014, 46, 973–981. [Google Scholar] [CrossRef] [PubMed]
- Bowser, B.J.; Fellin, R.; Milner, C.E.; Pohl, M.B.; Davis, I.S. Reducing impact loading in runners: A one-year follow-up. Med. Sci. Sports Exerc. 2018, 50, 2500–2506. [Google Scholar] [CrossRef] [PubMed]
- Ching, E.; An, W.W.-K.; Au, I.P.H.; Zhang, J.H.; Chan, Z.Y.; Shum, G.; Cheung, R.T. Impact Loading during Distracted Running before and after Auditory Gait Retraining. Int. J. Sports Med. 2018, 39, 1075–1080. [Google Scholar] [CrossRef]
- Zhang, J.H.; Chan, Z.Y.S.; Au, I.P.H.; An, W.W.; Cheung, R.T.H. Can runners maintain a newly learned gait pattern outside a laboratory environment following gait retraining? Gait Posture 2019, 69, 8–12. [Google Scholar] [CrossRef]
- Zhang, J.H.; Chan, Z.Y.-S.; Au, I.P.-H.; An, W.W.; Shull, P.B.; Cheung, R.T.-H. Transfer Learning Effects of Biofeedback Running Retraining in Untrained Conditions. Med. Sci. Sports Exerc. 2019, 51, 1904–1908. [Google Scholar] [CrossRef]
- Sheerin, K.R.; Reid, D.; Taylor, D.; Besier, T.F. The effectiveness of real-time haptic feedback gait retraining for reducing resultant tibial acceleration with runners. Phys. Ther. Sport 2020, 43, 173–180. [Google Scholar] [CrossRef]
- Esculier, J.-F.; Bouyer, L.J.; Dubois, B.; Fremont, P.; Moore, L.; McFadyen, B.; Roy, J.-S. Is combining gait retraining or an exercise programme with education better than education alone in treating runners with patellofemoral pain? A randomised clinical trial. Br. J. Sports Med. 2018, 52, 659–666. [Google Scholar] [CrossRef]
- Willy, R.W.; Buchenic, L.; Rogacki, K.; Ackerman, J.; Schmidt, A.; Willson, J.D. In-field gait retraining and mobile monitoring to address running biomechanics associated with tibial stress fracture. Scand. J. Med. Sci. Sports 2016, 26, 197–205. [Google Scholar] [CrossRef]
- Baumgartner, J.; Gusmer, R.; Hollman, J.; Finnoff, J.T. Increased stride-rate in runners following an independent retraining program: A randomized controlled trial. Scand. J. Med. Sci. Sports 2019, 29, 1789–1796. [Google Scholar] [CrossRef] [PubMed]
- Kliethermes, S.A.; Stiffler-Joachim, M.R.; Wille, C.M.; Sanfilippo, J.L.; Zavala, P.; Heiderscheit, B.C. Lower step rate is associated with a higher risk of bone stress injury: A prospective study of collegiate cross country runners. Br. J. Sports Med. 2021, 55, 851–856. [Google Scholar] [CrossRef] [PubMed]
- Doyle, E.; Doyle, T.L.A.; Bonacci, J.; Fuller, J.T. The Effectiveness of Gait Retraining on Running Kinematics, Kinetics, Performance, Pain, and Injury in Distance Runners: A Systematic Review with Meta-analysis. J. Orthop. Sports Phys. Ther. 2022, 52, 192–206. [Google Scholar] [CrossRef] [PubMed]
- Winstein, C.J.; Gardner, E.R.; McNeal, D.R.; Barto, P.S.; Nicholson, D.E. Standing balance training: Effect on balance and locomotion in hemiparetic adults. Arch. Phys. Med. Rehabil. 1989, 70, 755–762. [Google Scholar]
- Vannatta, C.N.; Heinert, B.L.; Kernozek, T.W. Biomechanical risk factors for running-related injury differ by sample population: A systematic review and meta-analysis. Clin. Biomech. 2020, 75, 104991. [Google Scholar] [CrossRef]
- Ceyssens, L.; Vanelderen, R.; Barton, C.; Malliaras, P.; Dingenen, B. Biomechanical Risk Factors Associated with Running-Related Injuries: A Systematic Review. Sports Med. 2019, 49, 1095–1115. [Google Scholar] [CrossRef]
- Willwacher, S.; Kurz, M.; Robbin, J.; Thelen, M.; Hamill, J.; Kelly, L.; Mai, P. Running-Related Biomechanical Risk Factors for Overuse Injuries in Distance Runners: A Systematic Review Considering Injury Specificity and the Potentials for Future Research. Sports Med. 2022, 52, 1863–1877. [Google Scholar] [CrossRef]
- Duffey, M.J.; Martin, D.F.; Cannon, D.W.; Craven, T.; Messier, S.P. Etiologic factors associated with anterior knee pain in distance runners. Med. Sci. Sports Exerc. 2000, 32, 1825–1832. [Google Scholar] [CrossRef]
- Messier, S.P.; Davis, S.E.; Curl, W.W.; Lowery, R.B.; Pack, R.J. Etiological factors associated with patellofemoral pain in runners. Med. Sci. Sports Exerc. 1991, 23, 1008–1015. [Google Scholar] [CrossRef]
- Becker, J.; Nakajima, M.; Wu, W.F.W. Factors Contributing to Medial Tibial Stress Syndrome in Runners: A Prospective Study. Med. Sci. Sports Exerc. 2018, 50, 2092–2100. [Google Scholar] [CrossRef]
- Becker, J.; James, S.; Wayner, R.; Osternig, L.; Chou, L. Biomechanical Factors Associated With Achilles Tendinopathy and Medial Tibial Stress Syndrome in Runners. Am. J. Sports Med. 2017, 45, 2614–2621. [Google Scholar] [CrossRef] [PubMed]
- Bramah, C.; Preece, S.J.; Gill, N.; Herrington, L. Is There a Pathological Gait Associated with Common Soft Tissue Running Injuries? Am. J. Sports Med. 2018, 46, 3023–3031. [Google Scholar] [CrossRef] [PubMed]
- Johnson, C.D.; Tenforde, A.S.; Outerleys, J.; Reilly, J.; Davis, I.S. Impact-Related Ground Reaction Forces Are More Strongly Associated With Some Running Injuries Than Others. Am. J. Sports Med. 2020, 48, 3072–3080. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, A.P.; João, S.M.A.; Dinato, R.C.; Tessutti, V.D.; Sacco, I.C.N. Dynamic patterns of forces and loading rate in runners with unilateral plantar fasciitis: A cross-sectional study. PLoS ONE 2015, 10, e0136971. [Google Scholar] [CrossRef] [PubMed]
- Pohl, M.B.; Hamill, J.; Davis, I.S. Biomechanical and Anatomic Factors Associated with a History of Plantar Fasciitis in Female Runners. Clin. J. Sport Med. 2009, 19, 372–376. [Google Scholar] [CrossRef] [PubMed]
- Heiderscheit, B.C.; Chumanov, E.S.; Michalski, M.P.; Wille, C.M.; Ryan, M.B. Effects of step rate manipulation on joint mechanics during running. Med. Sci. Sports Exerc. 2011, 43, 296–302. [Google Scholar] [CrossRef]
- Davis, I.S.; Tenforde, A.S.; Neal, B.S.; Roper, J.L.; Willy, R.W. Gait Retraining as an Intervention for Patellofemoral Pain. Curr. Rev. Musculoskelet. Med. 2020, 13, 103–114. [Google Scholar] [CrossRef] [PubMed]
- Napier, C.; Cochrane, C.K.; Taunton, J.E.; Hunt, M.A. Gait modifications to change lower extremity gait biomechanics in runners: A systematic review. Br. J. Sports Med. 2015, 49, 1382–1388. [Google Scholar] [CrossRef]
- Cheung, R.T.H.; An, W.W.; Au, I.P.H.; Zhang, J.H.; Chan, Z.Y.S.; MacPhail, A.J. Control of impact loading during distracted running before and after gait retraining in runners. J. Sports Sci. 2018, 36, 1497–1501. [Google Scholar] [CrossRef]
- Neto, W.C.d.; Lopes, A.D.; Ribeiro, A.P. Gait Retraining with Visual Biofeedback Reduces Rearfoot Pressure and Foot Pronation in Recreational Runners. J. Sport Rehabil. 2022, 31, 165–173. [Google Scholar] [CrossRef]
- Cheung, R.T.H.; Davis, I.S. Landing pattern modification to improve patellofemoral pain in runners: A case series. J. Orthop. Sports Phys. Ther. 2011, 41, 914–919. [Google Scholar] [CrossRef] [PubMed]
- Roper, J.L.; Harding, E.M.; Doerfler, D.; Dexter, J.G.; Kravitz, L.; Dufek, J.S.; Mermier, C.M. The effects of gait retraining in runners with patellofemoral pain: A randomized trial. Clin. Biomech. 2016, 35, 14–22. [Google Scholar] [CrossRef] [PubMed]
- Chan, Z.Y.S.; Zhang, J.H.; Ferber, R.; Shum, G.; Cheung, R.T.H. The effects of midfoot strike gait retraining on impact loading and joint stiffness. Phys. Ther. Sport 2020, 42, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Zhang, X.; Luo, Z.; Wang, X.; Ye, D.; Fu, W. Alterations in running biomechanics after 12 week gait retraining with minimalist shoes. Int. J. Environ. Res. Public Health 2020, 17, 818. [Google Scholar] [CrossRef] [PubMed]
- Chan, P.P.K.; Chan, Z.Y.S.; Au, I.P.H.; Lam, B.M.F.; Lam, W.K.; Cheung, R.T.H. Biomechanical effects following footstrike pattern modification using wearable sensors. J. Sci. Med. Sport 2021, 24, 30–35. [Google Scholar] [CrossRef]
- Helmhout, P.H.; Diebal, A.R.; van der Kaaden, L.; Harts, C.C.; Beutler, A.; Zimmermann, W.O. The effectiveness of a 6-week intervention program aimed at modifying running style in patients with chronic exertional compartment syndrome: Results from a series of case studies. Orthop. J. Sports Med. 2015, 3, 2325967115575691. [Google Scholar] [CrossRef]
- Futrell, E.E.; Gross, K.D.; Reisman, D.; Mullineaux, D.R.; Davis, I.S. Transition to forefoot strike reduces load rates more effectively than altered cadence. J. Sport Health Sci. 2020, 9, 248–257. [Google Scholar] [CrossRef]
- Miller, E.M.; Crowell, M.S.; Morris, J.B.; Mason, J.S.; Zifchock, R.; Goss, D.L. Gait Retraining Improves Running Impact Loading and Function in Previously Injured U.S. Military Cadets: A Pilot Study. Mil. Med. 2021, 186, E1077–E1087. [Google Scholar] [CrossRef]
- Bonacci, J.; Hall, M.; Saunders, N.; Vicenzino, B. Gait retraining versus foot orthoses for patellofemoral pain: A pilot randomised clinical trial. J. Sci. Med. Sport 2018, 21, 457–461. [Google Scholar] [CrossRef]
- Molina-Molina, A.; Latorre-Román, P.Á.; Mercado-Palomino, E.; Delgado-García, G.; Richards, J.; Soto-Hermoso, V.M. The effect of two retraining programs, barefoot running vs increasing cadence, on kinematic parameters: A randomized controlled trial. Scand. J. Med. Sci. Sports 2022, 32, 533–542. [Google Scholar] [CrossRef]
- Bittencourt, N.F.N.; Meeuwisse, W.H.; Mendonça, L.D.; Nettel-Aguirre, A.; Ocarino, J.M.; Fonseca, S.T. Complex systems approach for sports injuries: Moving from risk factor identification to injury pattern recognition-Narrative review and new concept. Br. J. Sports Med. 2016, 50, 1309–1314. [Google Scholar] [CrossRef] [PubMed]
- Willy, R.W.; Hoglund, L.T.; Barton, C.J.; Bolgla, L.A.; Scalzitti, D.A.; Logerstedt, D.S.; Lynch, A.D.; Snyder-Mackler, L.; McDonough, C.M. Patellofemoral pain clinical practice guidelines linked to the international classification of functioning, disability and health from the academy of orthopaedic physical therapy of the American physical therapy association. J. Orthop. Sports Phys. Ther. 2019, 49, CPG1–CPG95. [Google Scholar] [CrossRef] [PubMed]
- Bramah, C.; Preece, S.J.; Gill, N.; Herrington, L. A 10% Increase in Step Rate Improves Running Kinematics and Clinical Outcomes in Runners With Patellofemoral Pain at 4 Weeks and 3 Months. Am. J. Sports Med. 2019, 47, 3406–3413. [Google Scholar] [CrossRef] [PubMed]
- Warrener, A.; Tamai, R.; Lieberman, D.E. The effect of trunk flexion angle on lower limb mechanics during running. Hum. Mov. Sci. 2021, 78, 102817. [Google Scholar] [CrossRef]
- Xu, Y.; Yuan, P.; Wang, R.; Wang, D.; Liu, J.; Zhou, H. Effects of Foot Strike Techniques on Running Biomechanics: A Systematic Review and Meta-analysis. Sports Health 2021, 13, 71–77. [Google Scholar] [CrossRef]
- Teng, H.L.; Powers, C.M. Hip-extensor strength, trunk posture, and use of the knee-extensor muscles during running. J. Athl. Train. 2016, 51, 519–524. [Google Scholar] [CrossRef]
- Chan, Z.Y.; Zhang, J.H.; Au, I.P.; An, W.W.; Shum, G.L.; Ng, G.Y.; Cheung, R.T.H. Gait Retraining for the Reduction of Injury Occurrence in Novice Distance Runners: 1-Year Follow-up of a Randomized Controlled Trial. Am. J. Sports Med. 2018, 46, 388–395. [Google Scholar] [CrossRef]
- Daoud, A.I.; Geissler, G.J.; Wang, F.; Saretsky, J.; Daoud, Y.A.; Lieberman, D.E. Foot strike and injury rates in endurance runners: A retrospective study. Med. Sci. Sports Exerc. 2012, 44, 1325–1334. [Google Scholar] [CrossRef]
- Anderson, L.M.; Bonanno, D.R.; Hart, H.F.; Barton, C.J. What are the Benefits and Risks Associated with Changing Foot Strike Pattern During Running? A Systematic Review and Meta-analysis of Injury, Running Economy, and Biomechanics. Sports Med. 2020, 50, 885–917. [Google Scholar] [CrossRef]
- Hoenig, T.; Rolvien, T.; Hollander, K. Footstrike patterns in runners: Concepts, classifications, techniques, and implications for running-related injuries. Dtsch. Z. Sportmed. 2020, 71, 55–61. [Google Scholar] [CrossRef]
- Pohl, M.B.; Mullineaux, D.R.; Milner, C.E.; Hamill, J.; Davis, I.S. Biomechanical predictors of retrospective tibial stress fractures in runners. J. Biomech. 2008, 41, 1160–1165. [Google Scholar] [CrossRef] [PubMed]
- Milner, C.E.; Hamill, J.; Davis, I.S. Distinct hip and rearfoot kinematics in female runners with a history of tibial stress fracture. J. Orthop. Sports Phys. Ther. 2010, 40, 59–66. [Google Scholar] [CrossRef] [PubMed]
- Ferber, R.; Noehren, B.; Hamill, J.; Davis, I. Competitive female runners with a history of iliotibial band syndrome demonstrate atypical hip and knee kinematics. J. Orthop. Sports Phys. Ther. 2010, 40, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Noehren, B.; Davis, I.; Hamill, J. ASB Clinical Biomechanics Award Winner 2006. Prospective study of the biomechanical factors associated with iliotibial band syndrome. Clin. Biomech. 2007, 22, 951–956. [Google Scholar] [CrossRef]
- Noehren, B.; Pohl, M.B.; Sanchez, Z.; Cunningham, T.; Lattermann, C. Proximal and distal kinematics in female runners with patellofemoral pain. Clin. Biomech. 2012, 27, 366–371. [Google Scholar] [CrossRef]
- Neal, B.S.; Barton, C.J.; Birn-jeffery, A.; Morrissey, D. Increased hip adduction during running is associated with patellofemoral pain and differs between males and females: A case-control study. J. Biomech. 2019, 91, 133–139. [Google Scholar] [CrossRef]
- Noehren, B.; Hamill, J.; Davis, I. Prospective Evidence for a Hip Etiology in Patellofemoral Pain. Med. Sci. Sports Exerc. 2013, 45, 1120–1124. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).