Abstract
Background/Objectives: Persistent human papillomavirus (HPV) infection can lead to malignancies of the cervix, vulva, vagina, penis, anus, and oropharynx. The increasing incidence of HPV-related head and neck cancers has raised concerns regarding potential occupational exposure and transmission risks among healthcare workers. This study aimed to systematically evaluate the evidence on occupational HPV transmission in healthcare settings. Methods: A systematic review of the literature was conducted using three electronic databases (PubMed, Scopus, and Web of Science) from inception to August 2025, following PRISMA 2020 guidelines. A total of 34 studies met the inclusion criteria and were included in the review. Expert opinions and practical recommendations from members of the European Society of Gynaecological Oncology (ESGO) Prevention Committee were included to support interpretation of the results. Results: The available literature on occupational HPV transmission was limited, with a paucity of high-quality studies. Nevertheless, existing data suggest a potential occupational risk, particularly during aerosol or smoke-generating procedures performed for cervical intraepithelial neoplasia or cervical cancer. Several studies reported the detection of HPV DNA in surgical smoke or on instruments used during such procedures, indicating possible exposure among healthcare workers. Conclusions: Although current evidence is insufficient to definitively classify HPV infection as an occupational disease, available data indicate a potential exposure risk for healthcare workers involved in HPV-related procedures. Preventive measures, like personal protective equipment, should be emphasized. HPV vaccination has been recommended by some professional societies for healthcare workers performing gynecological procedures, though further research is needed to evaluate vaccine efficacy beyond the standard age range and its cost-effectiveness in this context.
1. Introduction
Human papillomavirus (HPV) is recognized as the most common sexually transmitted infection worldwide [1]. Following transmission, HPV infection typically clears spontaneously in most individuals, but oncogenic HPV infections can persist and lead to cancer. HPV can primarily cause cancers in the cervix, vulva, vagina, penis, anus, and oropharyngeal regions [2]. Outside the anogenital area, HPV-associated cancers are most detected in the head and neck region. The frequency of HPV-associated head and neck squamous cell cancers is increasing, both in the United States (US) and in Europe [3,4]. HPV now accounts for 71% and 51% of all oropharyngeal squamous cell carcinomas (OPSCCs) in the US and United Kingdom (UK), respectively. HPV Type 16 is responsible for more than 80% of HPV-related cancers [4,5].
Despite the fact that the oncogenesis of HPV-related OPSCC resembles the molecular biology of other HPV-associated malignancies, the difficulty in identifying pre-invasive lesions prevents the implementation of screening programmes [2]. Low-risk HPV infections are also implicated in the etiology of laryngeal papillomatosis in the oropharyngeal and laryngo-bronchial regions, which cause significant morbidity [6].
During the treatment of HPV-associated lesions, surgical smoke is generated. Cases of OPSCCs and laryngeal papillomatosis have been reported among healthcare workers, in which transmission through surgical smoke was suggested as a possible etiologic factor. However, evidence regarding the risk of HPV transmission via surgical smoke remains inconclusive. In addition, the potential for HPV contamination through examination instruments or clinical environments has not been clearly established.
HPV is traditionally associated with mucosal transmission; however, increasing evidence suggests that healthcare workers may also encounter HPV through nonsexual occupational exposure routes, particularly during aerosol or smoke-generating procedures.
In this study, we aimed to summarize the available literature investigating occupational HPV exposure and transmission among healthcare workers.
2. Materials and Methods
This study was conducted in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. A systematic literature search was conducted by three independent researchers.
Search Strategy
The search was performed in September 2025 (including studies published up to August 2025) from inception to present in three databases (PubMed/MEDLINE, Web of Science, and Scopus). Our research keywords were selected to address the question: “Is there an occupational risk of HPV transmission for healthcare workers?”. The occupational exposure concept was operationalized using terms such as “healthcare workers,” “health workers,” “doctor,” “nurse,” “gynaecologist,” “dermatologist,” and “occupational,” each combined with “human papillomavirus.” The complete and reproducible search strategies for all databases, including exact search terms and Boolean operators, are provided in Supplementary File S1. References of the identified studies were also hand-searched to identify additional relevant articles. Only English-language publications were included.
Studies, case reports, surveys, and cross-sectional studies that provided data on occupational HPV exposure among healthcare workers were eligible for inclusion. Additionally, survey-based studies assessing healthcare workers’ knowledge and awareness of occupational HPV transmission risk were also considered. After removing duplicates, all retrieved records were screened by titles and abstracts for relevance. Full-text versions of potentially eligible studies were then reviewed.
Following completion of the systematic literature review and data synthesis, the findings were shared with selected members of the European Society of Gynaecological Oncology (ESGO) Prevention Committee for expert opinion and practical considerations. Experts were selected based on their clinical and academic expertise in gynecologic oncology and HPV-related disease prevention.
3. Results
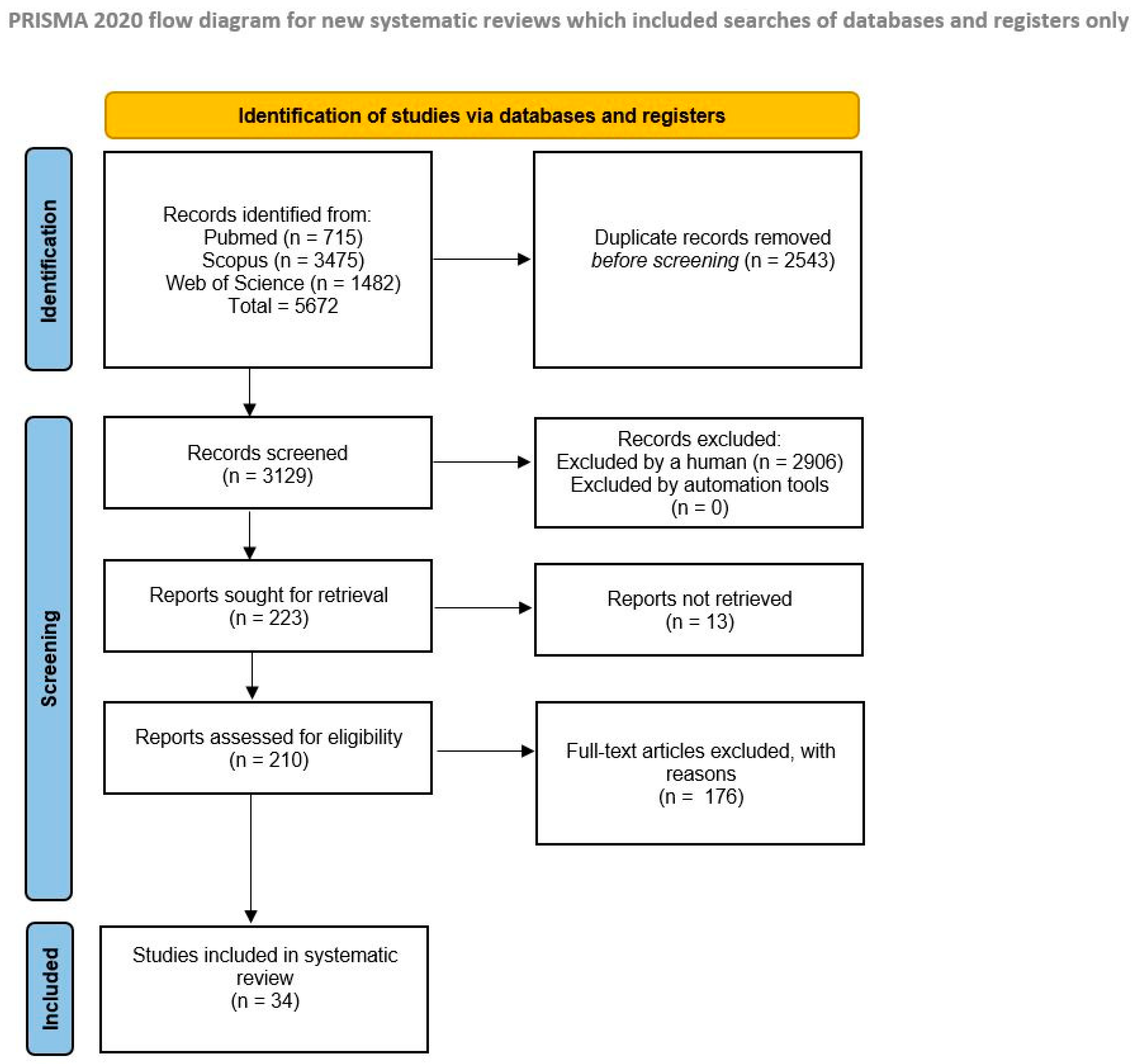
The search detected 715 articles in PubMed, 3475 in Scopus, and 1482 in Web of Science. One additional relevant case report not indexed in these databases was added manually. After screening and eligibility assessment, a total of 34 articles met the inclusion criteria (Figure 1). Most studies investigated the risk of HPV transmission during surgical procedures involving HPV-related lesions.
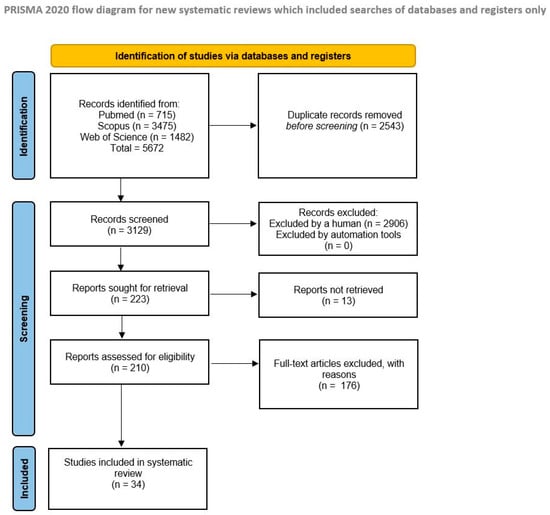
Figure 1.
PRISMA flow diagram of the review process.
The final list of included studies was presented to selected members of the ESGO Prevention Committee for expert discussion. A complete list of included studies is presented in Table 1.

Table 1.
Summary of studies.
Most studies have investigated the presence of HPV DNA in the surgical smoke generated during the treatment of HPV-associated lesions. In eight studies, HPV DNA was detected either in the surgical smoke collected during procedures or on equipment exposed to the smoke [7,8,9,12,14,20,21,26]. Swabs taken from healthcare workers exposed to smoke during treatment were also analyzed for contamination. In three studies, HPV DNA was found on swabs taken from healthcare workers (including physicians, surgeons, nurses and anaesthesiology staff) from different anatomical sites, such as the oral mucosa, nasolabial fold, nasal cavity and conjunctiva, and on PPE. These findings were suggested as potential evidence of occupational exposure [13,22,25]. Animal studies have also been conducted to investigate the infectious potential of occupational exposure. Garden et al. demonstrated that smoke produced by CO2 laser ablation of bovine papillomaviruses (BPV) positive cutaneous fibropapillomas, when applied to the skin of healthy calves, resulted in the development of BPV DNA-positive lesions in all three animals [17]. In another study by Best et al., lesions associated with mouse papillomavirus (MusPV) in mice were treated by sharp excision, KTP laser and coblation. The resulting smoke and sample solutions were applied to mucosally abraded mouse tails, and wart development was observed in all cases [23]. Three studies examined the risk of HPV transmission to healthcare workers through non-aerosol routes. One study investigating HPV DNA contamination on examination equipment (glove box, lamp of a gynaecological chair, gel tubes for ultrasound, colposcope and speculum) found that colposcopes had the highest risk of contamination (OR: 3.02, 95% CI 0.86 to 10.57) [27]. The study demonstrated that HPV contamination could occur despite routine cleaning of gynecological equipment. A prevalence study investigating the incidence of warts among healthcare workers treating HPV-related lesions found that the lesions typically occurred on the hands, highlighting the potential for direct contact transmission [38]. The literature also includes six cases (four case reports) of individuals diagnosed with HPV-related diseases with exposure to surgical smoke during the treatment of HPV-associated lesions [30,31,32,33]. In a case report, laryngeal papillomatosis occurring in healthcare personnel was defined as an occupational disease based on the opinion of a virology institute expert [32]. The risk of aerosol transmission is not limited to procedures that use energy modalities alone. In recent years, studies have suggested that practices such as endotracheal aspiration, intubation–extubation, bronchoscopy, manual ventilation, cardiopulmonary resuscitation, tracheostomy procedures, and high-flow oxygen therapies generate aerosols [41,42].
There are also studies in the literature that do not support the occupational HPV exposure among healthcare workers treating HPV-related diseases. We identified seven studies in which HPV DNA was not detected in the surgical smoke or on equipment used in the treatment of HPV-associated lesions. These studies concluded that the risk of occupational exposure was either absent or minimal [11,15,16,18,19,28,29]. In a 2020 study by Subbarayan et al., no HPV DNA was detected in the smoke produced from the cauterization of mouse tails injected with DNA plasmids. The same study also failed to detect HPV DNA on PPE or robotic arms used during robotic oropharyngeal cancer surgeries [24]. There are also observational studies with control groups addressing this issue. In a survey conducted by Kofoed et al. involving 287 participants, although the swabs from healthcare workers who performed treatments on HPV-related lesions showed higher HPV positivity, the difference was not statistically significant compared to the control group [40]. Similarly, in a study by Gloster et al. involving 570 surgeons, no significant difference was found in the prevalence of warts between those who performed CO2 laser treatments and those who did not perform CO2 laser treatments (5.4% vs 4.9%; p: 0.56) [39]. There was also no significant difference in PPE use (e.g., gloves, masks, smoke extraction) between the warts and non-warts groups.
In four questionnaire-based studies, the perceptions of healthcare workers involved in the treatment of HPV-related lesions regarding the risk of occupational HPV exposure were evaluated. In the study conducted by Leahy et al., which included 75 healthcare professionals treating cutaneous lesions, 36.8% of participants acknowledged the risk of HPV infection through surgical smoke, and 76.8% reported concern about potential occupational exposure [34]. In another study by Al-Dawsari et al., 55.7% of healthcare workers reported developing warts following dermatologic procedures [35]. Afsar et al. assessed both awareness of the risk of occupational exposure and attitudes towards HPV vaccination among healthcare workers [36]. In this study, 84% of participants were aware of the risk of occupational HPV exposure and expressed willingness to receive the HPV vaccine if available. In a survey by Mercier et al., it was found that while many participants expressed concern about occupational exposure to HPV, they had not received sufficient education on the risk [37]. Notably, approximately one-third of adult vaccinations reported in the study were motivated by concerns over occupational HPV exposure. All four surveys demonstrated that health care workers were concerned about potential infection while treating HPV-related lesions.
4. Discussion
According to the Protocol of 2002 to the Occupational Safety and Health Convention, 1981, the term “occupational disease” covers any disease contracted as a result of exposure to risk factors arising from work activity. In the identification of an occupational disease, two fundamental elements are discernible: firstly, the causal relationship between exposure in a specific working environment or work activity and a specific disease; and secondly, an incidence rate among exposed workers that is higher than that in the general population [43]. This framework raises the question of whether HPV infection should be considered an occupational disease. Sexual transmission is the most well-known and documented mode of HPV infection. However, fomites, non-sexual contacts such as mouth-to-finger or skin contact, contribute to HPV transmission [44]. It is possible for the patient to infect themselves through fomites or fingers (oral infection and auto-inoculation). Vertical transmission from mother to the baby through different routes has been demonstrated [45]. Studies examining HPV transmission in gynaecological examination areas have documented HPV contamination in instruments used [27,46]. Traditional disinfection methods may not be effective in eliminating HPV transmission in medical equipment and devices [44]. Resistance shown by HPV to commonly used chemicals such as glutaraldehyde or alcohol supports evidence of transmission from fomites and surfaces. All of these findings can support the existence of nosocomial infection risk for HPV, in particular, in healthcare facilities where sterilization with high-temperature or high-pressure autoclaves is not employed [46].
Transmission of HPV infection via aerosol and non-aerosol is a currently debated issue. Certain clinical procedures appear to confer a higher occupational risk of HPV exposure, particularly those that generate surgical smoke or aerosols. Procedures such as electrocautery, laser ablation, LEEP, and other energy-based interventions used in the treatment of HPV-related lesions have been frequently associated with the detection of HPV DNA in surgical plumes. These risks are especially relevant for healthcare professionals in gynecology, otolaryngology, dermatology, and head and neck surgery, where prolonged or repeated exposure to smoke-generating techniques is common. During procedures performed for HPV treatment, surgical smoke contains various toxic materials, both biological and non-biological, and poses a risk of HPV transmission through aerosols [7,12,13,14,17,18,19,20,21,22,23,25,26]. Additionally, the risk of occupational HPV transmission during excisional and ablative procedures was comprehensively evaluated in the systematic review and meta-analysis in 2021, which demonstrated detectable HPV DNA in surgical smoke and documented variable exposure risk for healthcare workers [6]. Measures to be taken to protect against surgical smoke, which is potentially infectious, can reduce HPV exposure (such as proper aspiration during electro-surgical procedures generating smoke, use of N95 masks) [8,9,13,14,17,19,22,23,25]. However, there are studies in the literature that do not support the transmission of HPV through surgical smoke [15,16,24]. Differences in HPV DNA detection techniques, sampling methods, and analytical sensitivity may partly explain the heterogeneity of results across studies.
Case reports have documented instances of laryngeal papillomatosis, tonsillar cancer, oropharyngeal cancer and tongue carcinoma linked to HPV occupational exposure [30,31,32,33]. Although case reports cannot establish a causal relationship, they should be considered as important signals that may indicate potential occupational risk. Several studies in the literature indicate that healthcare workers are concerned about the risk of occupational HPV exposure [34,35,36,37]. However, these studies also demonstrate that healthcare workers generally lack sufficient knowledge regarding preventive strategies for occupational HPV exposure [37]. Despite the presence of many identified and estimated modes of transmission, a professional risk definition for healthcare workers has not been made for HPV infections [47]. Healthcare workers have not yet been included in high-risk groups for HPV infection, even though not only gynaecologists but also many other healthcare groups may be at risk of HPV transmission [48].
Despite existing concerns and reports of HPV-related disease cases, there are still obstacles to defining HPV infection as an occupational disease. Comprehensive studies on the incidence of HPV infection among healthcare workers need to be conducted to investigate whether there is a significant difference compared to the general population. Additionally, determining the actual source and route of transmission in a healthcare worker with HPV infection poses another challenge. The limitations of screening and follow-up programs for HPV infection and related diseases further complicate the issue. Currently, healthcare workers undergo periodic screenings for certain infectious agents depending on the centres in which they work, but there are no applicable periodic screening programs for HPV (except for cervical diseases at present). While more evidence may be needed, based on the available literature, necessary precautions should still be taken regarding the risk of HPV transmission among healthcare workers. Possible measures to reduce occupational HPV exposure among healthcare workers are summarized in Table 2.

Table 2.
Occupational preventive measures against HPV exposure in healthcare workers.
4.1. Role of HPV Vaccines
The HPV types prevented by the 9-valent vaccination account for approximately 90% of HPV-attributable cancers worldwide [49]. In 2020, the U.S. Food and Drug Administration approved GARDASIL-9 (Merck & Co., Rahway, NJ, USA) for boys and men for the prevention of anal, oropharyngeal, and other head and neck cancers caused by HPV types 16, 18, 31, 33, 45, 52, and 58. International randomized controlled trials conducted with female adolescents and women aged 15 to 26 have demonstrated a vaccine efficacy of at least 96% in preventing cervical precancers (cervical intraepithelial neoplasia grade ≥ 2 or adenocarcinoma in situ) caused by the specific HPV types targeted by the vaccine. [50] Trials of the quadrivalent vaccine demonstrated 100% efficacy in preventing anogenital warts [51,52].
Although cervical cancer screening programmes are widely implemented, vaccination remains the only effective strategy for preventing other HPV-related diseases, such as head and neck cancers, for which routine screening is far less effective and cannot be recommended [53,54,55]. However, there is still a lack of robust, literature-based evidence of a significant reduction in oral HPV 16–18 infections after bivalent vaccination, particularly in males [56].
The American Society for Colposcopy and Cervical Pathology (ASCCP) has recommended that healthcare professionals responsible for gynecological procedures, such as the excision or ablation of lesions associated with HPV, should receive the HPV vaccine. This recommendation extends to healthcare workers engaged in gynecological operations, including nurses, physicians, nurse practitioners, dermatologists, anesthetists, otolaryngologists, family practice, gynecologic oncology, pulmonologists, critical care medicine, and health technicians, who are also at risk and could benefit from expanding vaccination guidelines [57]. The American College of Obstetrics and Gynecologists reports that it concurs with ASCCP’s recommendation, despite the lack of sufficient data supporting the efficacy or cost-effectiveness of the vaccine [47]. The British Association of Dermatologists recommends using HPV smoke aspirators, PPE, further occupational health research, and professional training to prevent disease transmission via smoke plumes, including HPV aerosolization during procedures but did not mention vaccination [58]. In a December 2022 statement, the World Health Organization (WHO) stated that vaccination recommendations for healthcare workers are the same as for the general population [59]. The WHO does not categorise HPV vaccines as recommended for healthcare workers [60]. The National Institute for Occupational Safety and Health has established recommendations for locations where medical procedures generating smoke are performed [61]. In recent years, numerous articles have highlighted the need to evaluate HPV vaccination and the use of PPE for healthcare workers due to potential occupational exposure [47,62,63,64,65,66].
Several studies have investigated HPV vaccination rates among healthcare workers in recent years. The results of these studies showed that vaccination rates varied, ranging from 7% to 41% [36,67,68,69,70,71]. A study evaluating the vaccination habits of medical students found that 32% were fully vaccinated, while 15% were partially vaccinated [72]. Cost or limited availability have been found to be some of the main reasons cited for not getting vaccinated [67,71].
However, population-level vaccine effectiveness appears lower with increasing age [73]. Although the vaccine is approved for individuals up to 45 years of age, it is less effective after the age of 26, which highlights the importance of early vaccination [74]. Therefore, HPV vaccination should ideally be administered as early as possible during a healthcare professional’s career, particularly before the onset of occupational exposure. In fact, vaccinating future healthcare workers who are at risk of exposure to HPV early in their training (e.g., during the first years of medical school or nursing school) may present an important opportunity. Additionally, catch-up vaccination or educational programs within medical schools could help increase HPV vaccine uptake among those who missed it during adolescence.
However, vaccination may still be considered later in life for healthcare workers with ongoing or anticipated occupational risk. In the context of procedures associated with aerosol or surgical smoke generation, HPV vaccination may offer potential occupational benefit and should be discussed irrespective of age, following appropriate individual counseling.
Importantly, the reduced population-level effectiveness of HPV vaccination in older individuals primarily reflects prior HPV exposure rather than diminished vaccine-induced immune responses [75].
Although HPV vaccines have demonstrated an excellent overall safety profile, careful monitoring for adverse reactions following initial doses remains essential [75]. This is particularly important when vaccination is offered outside standard age-based programs.
Healthcare institutions and healthcare leaders may have a unique opportunity to improve HPV vaccine uptake by integrating vaccination into existing occupational vaccination programs, such as seasonal influenza or Hepatitis B vaccination campaigns. Targeting healthcare workers under the age of 46 during routinely scheduled institutional immunization sessions could represent a practical and cost-effective strategy to increase coverage among individuals at potential occupational risk.
We found there was a lack of large-scale observational studies examining the incidence of HPV related diseases in healthcare workers versus the general population. Such studies are of course still subject to bias but would inform both the strength of the association and the types of occupational exposure most likely to result in HPV-related disease.
4.2. Strengths and Limitations
To our knowledge, this systematic review provides one of the most comprehensive overviews of HPV-related occupational exposure, incorporating both recent evidence and healthcare professionals’ perspectives on risk perception and preventive practices. We combine this systematic review with expert opinion from across Europe. The review captures both supporting and opposing evidence for HPV occupational transmission, incorporating studies from diverse medical disciplines. Recommendations regarding PPE, smoke evacuation, and vaccination are concrete and actionable.
The article has some limitations. Firstly, most studies supporting the association between HPV transmission to healthcare workers and treatment procedures are either animal studies or involve a small number of participants. The risk of bias in the literature is therefore high. The authors acknowledge the limited evidence base, highlighting methodological constraints and a lack of large prospective studies. While the survey results show awareness and concern among healthcare workers, they cannot establish risk causality as perceived risk (including psychological issues) is different from biological risk. Further limitation is the slow progression of HPV infection, which obscured the identification of the incident HPV infection as an occupational exposure.
Interpretation of occupational HPV exposure is also inherently limited by the high background prevalence of HPV in the general population and by the fact that routine screening is restricted to cervical disease. These factors make it difficult to distinguish occupational acquisition from prior or non-occupational exposure.
5. Conclusions
Lesions related to HPV infections are frequently treated, and healthcare workers are at risk of HPV transmission during these procedures. Moreover, the evidence suggests that some interventions and procedures on individuals with HPV virus carriers, even in cases where HPV-related disease treatment is not performed, have the risk of transmission through contact or aerosol. While the evidence base was limited, the likelihood of this risk should prompt the consideration of HPV infection in healthcare workers as an occupational disease, and this designation should be confirmed with high-quality prospective studies. We recommend consideration of implementing the following preventive strategies due to the potential occupational risk of HPV infection: well-equipped intervention areas/operation rooms (containing smoke evacuators or room suction systems), PPE to reduce the probability of disease (surgical mask, gloves, etc.) and administration of HPV vaccines in populations with proven effectiveness.
Research priorities should include not only seroprevalence studies but also prospective cohort studies focusing on HPV-related disease outcomes among occupationally exposed healthcare workers, along with molecular studies assessing HPV DNA in surgical smoke using standardized detection methods and cost-benefit analyses of extending HPV vaccination to healthcare workers.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/vaccines14020148/s1, File S1: The keywords used in the literature search and the search results.
Author Contributions
Conceptualization, M.G. (Murat Gültekin) and M.K.; methodology, M.G. (Murat Gültekin). and M.K.; software, B.E.T. and B.L.-C.; validation, H.V.E. and B.E.T.; formal analysis, H.V.E., B.E.T. and B.L.-C.; investigation, H.V.E., B.E.T., L.B.E. and B.L.-C.; resources, B.L.-C. and H.V.E.; data curation, H.V.E., B.E.T., L.B.E. and S.J.B.; writing—original draft preparation, H.V.E., B.E.T., L.B.E. and S.J.B.; writing—review and editing, L.B.E., S.J.B., M.P., I.Z., M.G. (Mihaela Grigore), E.J., M.K. and M.G. (Murat Gültekin); visualization, H.V.E., B.E.T., L.B.E. and S.J.B.; supervision, M.K., M.P., E.J., M.G. (Mihaela Grigore), I.Z. and M.G. (Murat Gültekin); project administration, M.K. and M.G. (Murat Gültekin).; funding acquisition, M.G. (Murat Gültekin). All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study did not require ethical approval.
Informed Consent Statement
This study did not involve humans.
Data Availability Statement
The data supporting the findings of this systematic review are included within the article and its Supplementary Materials. All analyzed data were derived from previously published studies cited in the reference list.
Acknowledgments
The authors would like to thank Zuzana Santamaria, Project Manager of the ESGO Prevention Committee.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| ESGO | European Society of Gynaecological Oncology |
| HPV | Human Papillomavirus |
| US | United States |
| UK | United Kingdom |
| OPSCCs | Oropharyngeal squamous cell carcinomas |
| CO2 | Carbon dioxide |
| CIN | Cervical intraepithelial neoplasia |
| LEEP | Loop electrosurgical excision procedure |
| PPE | Personal protective equipment |
| HSIL | High-Grade Squamous Intraepithelial Lesion |
| SCC | Squamous Cell Carcinoma |
| ASCCP | American Society for Colposcopy and Cervical Pathology |
| BPV | Bovine papillomaviruses |
| WHO | World Health Organization |
References
- Roman, B.R.; Aragones, A. Epidemiology and incidence of HPV-related cancers of the head and neck. J. Surg. Oncol. 2021, 124, 920–922. [Google Scholar] [CrossRef]
- Ghebre, R.; Berry-Lawhorn, J.M.; D’Souza, G. State of the Science: Screening, Surveillance, and Epidemiology of HPV-Related Malignancies. Am. Soc. Clin. Oncol. Educ. Book 2021, 41, 377–388. [Google Scholar] [CrossRef]
- St Laurent, J.; Luckett, R.; Feldman, S. HPV vaccination and the effects on rates of HPV-related cancers. Curr. Probl. Cancer 2018, 42, 493–506. [Google Scholar] [CrossRef]
- Lechner, M.; Liu, J.; Masterson, L.; Fenton, T.R. HPV-associated oropharyngeal cancer: Epidemiology, molecular biology and clinical management. Nat. Rev. Clin. Oncol. 2022, 19, 306–327. [Google Scholar] [CrossRef]
- Herrero, R.; Castellsagué, X.; Pawlita, M.; Lissowska, J.; Kee, F.; Balaram, P.; Rajkumar, T.; Sridhar, H.; Rose, B.; Pintos, J.; et al. Human papillomavirus and oral cancer: The International Agency for Research on Cancer multicenter study. J. Natl. Cancer Inst. 2003, 95, 1772–1783. [Google Scholar] [CrossRef]
- Palma, S.; Gnambs, T.; Crevenna, R.; Jordakieva, G. Airborne human papillomavirus (HPV) transmission risk during ablation procedures: A systematic review and meta-analysis. Environ. Res. 2021, 192, 110437. [Google Scholar] [CrossRef]
- Garden, J.M.; O’Banion, M.K.; Shelnitz, L.S.; Pinski, K.S.; Bakus, A.D.; Reichmann, M.E.; Sundberg, J.P. Papillomavirus in the vapor of carbon dioxide laser-treated verrucae. JAMA 1988, 259, 1199–1202. [Google Scholar] [CrossRef]
- Sawchuk, W.S.; Weber, P.J.; Lowy, D.R.; Dzubow, L.M. Infectious papillomavirus in the vapor of warts treated with carbon dioxide laser or electrocoagulation: Detection and protection. J. Am. Acad. Dermatol. 1989, 21, 41–49. [Google Scholar] [CrossRef] [PubMed]
- Ferenczy, A.; Bergeron, C.; Richart, R.M. Human papillomavirus DNA in CO2 laser-generated plume of smoke and its consequences to the surgeon. Obstet. Gynecol. 1990, 75, 114–118. [Google Scholar] [CrossRef] [PubMed]
- Wisniewski, P.; Warhol, M.; Rando, R.; Sedlacek, T.; Kemp, J.; Fisher, J. Studies on the transmission of viral disease via the CO2 laser plume and ejecta. J. Reprod. Med. 1990, 35, 1117–1123. [Google Scholar] [PubMed]
- Abramson, A.L.; DiLorenzo, T.P.; Steinberg, B.M. Is papillomavirus detectable in the plume of laser-treated laryngeal papilloma? Arch. Otolaryngol.–Head Neck Surg. 1990, 116, 604–607. [Google Scholar] [CrossRef]
- Kashima, H.K.; Kessis, T.; Mounts, P.; Shah, K. Polymerase chain reaction identification of human papillomavirus DNA in CO2 laser plume from recurrent respiratory papillomatosis. Otolaryngol.—Head Neck Surg. 1991, 104, 191–195. [Google Scholar] [CrossRef]
- Bergbrant, I.M.; Samuelsson, L.; Olofsson, S.; Jonassen, F.; Ricksten, A. Polymerase chain reaction for monitoring human papillomavirus contamination of medical personnel during treatment of genital warts with CO2 laser and electrocoagulation. Acta Derm.-Venereol. 1994, 74, 393–395. [Google Scholar] [CrossRef]
- Sood, A.K.; Bahrani-Mostafavi, Z.; Stoerker, J.; Stone, I.K. Human papillomavirus DNA in LEEP plume. Infect. Dis. Obstet. Gynecol. 1994, 14 2, 167–170. [Google Scholar] [CrossRef] [PubMed]
- Kunachak, S.; Sithisarn, P.; Kulapaditharom, B. Are laryngeal papilloma virus-infected cells viable in the plume derived from a continuous mode carbon dioxide laser, and are they infectious? A preliminary report on one laser mode. J. Laryngol. Otol. 1996, 110, 1031–1033. [Google Scholar] [CrossRef]
- Hughes, P.S.; Hughes, A.P. Absence of human papillomavirus DNA in the plume of erbium: YAG laser–treated warts. J. Am. Acad. Dermatol. 1998, 38, 426–428. [Google Scholar] [CrossRef]
- Garden, J.M.; O’Banion, M.K.; Bakus, A.D.; Olson, C. Viral disease transmitted by laser-generated plume (aerosol). Arch. Dermatol 2002, 138, 1303–1307. [Google Scholar] [CrossRef]
- Weyandt, G.H.; Tollmann, F.; Kristen, P.; Weissbrich, B. Low risk of contamination with human papilloma virus during treatment of condylomata acuminata with multilayer argon plasma coagulation and CO2 laser ablation. Arch. Dermatol. Res. 2011, 303, 141–144. [Google Scholar] [CrossRef] [PubMed]
- Ilmarinen, T.; Auvinen, E.; Hiltunen-Back, E.; Ranki, A.; Aaltonen, L.M.; Pitkäranta, A. Transmission of human papillomavirus DNA from patient to surgical masks, gloves and oral mucosa of medical personnel during treatment of laryngeal papillomas and genital warts. Eur. Arch. Oto-Rhino-Laryngol 2012, 269, 2367–2371. [Google Scholar] [CrossRef] [PubMed]
- Akbarov, I.; Tok, A.; Wieland, U.; Engelmann, U.; Wille, S. 624 HPV-contamination of laser smoke during laser treatment of condylomata acuminata. Eur. Urol. Suppl. 2013, 12, e624. [Google Scholar] [CrossRef]
- Neumann, K.; Cavalar, M.; Rody, A.; Friemert, L.; Beyer, D.A. Is surgical plume developing during routine LEEPs contaminated with high-risk HPV? A pilot series of experiments. Arch. Gynecol. Obstet. 2018, 297, 421–424. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Q.; Hu, X.; Zhou, J.; Zhao, M.; Zhu, X.; Zhu, X. Human papillomavirus DNA in surgical smoke during cervical loop electrosurgical excision procedures and its impact on the surgeon. Cancer Manag. Res. 2019, 11, 3643–3654. [Google Scholar] [CrossRef]
- Best, S.R.; Esquivel, D.; Mellinger-Pilgrim, R.; Roden, R.B.S.; Pitman, M.J. Infectivity of murine papillomavirus in the surgical byproducts of treated tail warts. Laryngoscope 2020, 130, 712–717. [Google Scholar] [CrossRef]
- Subbarayan, R.S.; Shew, M.; Enders, J.; Bur, A.M.; Thomas, S.M. Occupational exposure of oropharyngeal human papillomavirus amongst otolaryngologists. Laryngoscope 2020, 130, 2366–2371. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.; Zhou, Q.; Yu, J.; Wang, J.; Tu, Q.; Zhu, X. Prevalence of HPV infections in surgical smoke exposed gynecologists. Int. Arch. Occup. Environ. Health 2021, 94, 107–115. [Google Scholar] [CrossRef]
- Yan, L.; Liu, Y.; Zhang, J.; Chen, X.; Li, J.; Zhu, X. In vivo and in vitro study of the potential hazards of surgical smoke during cervical cancer treatment with an ultrasonic scalpel. Gynecol. Oncol. 2022, 164, 587–595. [Google Scholar] [CrossRef]
- Gallay, C.; Miranda, E.; Schaefer, S.; Catarino, R.; Jacot-Guillarmod, M.; Menoud, P.A.; Guerry, F.; Achtari, C.; Sahli, R.; Vassilakos, P.; et al. Human papillomavirus (HPV) contamination of gynaecological equipment. Sex. Transm. Infect. 2016, 92, 19–23. [Google Scholar] [CrossRef] [PubMed]
- Dodhia, S.; Baxter, P.C.; Ye, F.; Pitman, M.J. Investigation of the presence of HPV on KTP laser fibers following KTP laser treatment of papilloma. Laryngoscope 2018, 128, 926–928. [Google Scholar] [CrossRef]
- Lucet, J.C.; Heard, I.; Roueli, A.; Lafourcade, A.; Mandelbrot, L.; Estellat, C.; Dommergues, M.; PREEV Study Group. Transvaginal ultrasound probes are human papillomavirus-free following low-level disinfection: Cross-sectional multicenter survey. Ultrasound Obstet. Gynecol. 2019, 54, 688–695. [Google Scholar] [CrossRef]
- Rioux, M.; Garland, A.; Webster, D.; Reardon, E. HPV positive tonsillar cancer in two laser surgeons: Case reports. J. Otolaryngol.-Head Neck Surg. 2013, 42, 54. [Google Scholar] [CrossRef]
- Hallmo, P.; Naess, O. Laryngeal papillomatosis with human papillomavirus DNA contracted by a laser surgeon. Eur. Arch. Oto-Rhino-Laryngol 1991, 248, 425–427. [Google Scholar] [CrossRef]
- Calero, L.; Brusis, T. Laryngeal papillomatosis—First recognition in Germany as an occupational disease in an operating room nurse. Laryngorhinootologie 2003, 82, 790–793. [Google Scholar]
- Parker, J.; Clark, J. HPV positive oropharyngeal cancer in two gynaecologists exposed to electrosurgical smoke plume. Obstet. Gynecol. Cases Rev. 2021, 8, 205. [Google Scholar]
- Leahy, M.; Harrington, R.; Laing, M. Risk of HPV infection among dermatologists: Are we prepared? J. Eur. Acad. Dermatol. Venereol. 2023, 38, E24–E25. [Google Scholar] [CrossRef]
- Al-Dawsari, N.A.; Hafez, S.M.; Hafez, D.M.; Al-Tawfiq, J. Self-Precautions among Dermatologists Managing HPV-Related Infections: Awareness and Current Practice of Dermatologists Practicing in Saudi Arabia. Skinmed 2021, 19, 274–279. [Google Scholar] [PubMed]
- Afsar, S.; Hossain, M.; Islam, M.; Simmonds, H.; Stillwell, A.A.; Butler, K.A. Human papillomavirus and occupational exposure: The need for vaccine provision for healthcare providers. Hum. Vaccines Immunother. 2024, 20, 2342622. [Google Scholar] [CrossRef] [PubMed]
- Mercier, A.M.; Allison, M.K. Occupational Exposure to Aerosolized Human Papillomavirus: Assessing and Addressing Perceptions of and Barriers to Vaccination of at-Risk Health Care Workers. J. Public Health Manag. Pract. 2024, 30, 681–687. [Google Scholar] [CrossRef]
- Lobraico, R.V.; Schifano, M.J.; Brader, K.R. A retrospective study on the hazards of the carbon dioxide laser plume. J. Laser Appl. 1988, 1, 6–8. [Google Scholar] [CrossRef]
- Gloster, H.M.; Roenigk, R.K., Jr. Risk of acquiring human papillomavirus from the plume produced by the carbon dioxide laser in the treatment of warts. J. Am. Acad. Dermatol. 1995, 32, 436–441. [Google Scholar] [CrossRef]
- Kofoed, K.; Norrbom, C.; Forslund, O.; Møller, C.; Frøding, L.P.; Pedersen, A.E.; Markauskas, A.; Blomberg, M.; Baumgartner-Nielsen, J.; Madsen, J.; et al. Low prevalence of oral and nasal human papillomavirus in employees performing CO2-laser evaporation of genital warts or loop electrode excision procedure of cervical dysplasia. Acta Derm.-Venereol. 2015, 95, 173–176. [Google Scholar] [CrossRef]
- Jackson, T.; Deibert, D.; Wyatt, G.; Durand-Moreau, Q.; Adisesh, A.; Khunti, K.; Khunti, S.; Smith, S.; Chan, X.H.S.; Ross, L.; et al. Classification of aerosol-generating procedures: A rapid systematic review. BMJ Open Respir. Res. 2020, 7, e000730. [Google Scholar] [CrossRef]
- Thamboo, A.; Lea, J.; Sommer, D.D.; Sowerby, L.; Abdalkhani, A.; Diamond, C.; Ham, J.; Heffernan, A.; Long, M.C.; Phulka, J.; et al. Clinical evidence based review and recommendations of aerosol generating medical procedures in otolaryngology—Head and neck surgery during the COVID-19 pandemic. J. Otolaryngol.-Head Neck Surg. 2020, 49, 28. [Google Scholar] [CrossRef] [PubMed]
- International Labour Organization. List of Occupational Diseases (Revised 2010); International Labour Office: Geneva, Switzerland, 2010. [Google Scholar]
- Petca, A.; Borislavschi, A.; Zvanca, M.E.; Petca, R.C.; Sandru, F.; Dumitrascu, M.C. Non-sexual HPV transmission and role of vaccination for a better future (Review). Exp. Ther. Med. 2020, 20, 186. [Google Scholar] [CrossRef] [PubMed]
- Khayargoli, P.; Niyibizi, J.; Mayrand, M.H.; Audibert, F.; Monnier, P.; Brassard, P.; Laporte, L.; Lacaille, J.; Zahreddine, M.; Bédard, M.-J.; et al. Human Papillomavirus Transmission and Persistence in Pregnant Women and Neonates. JAMA Pediatr. 2023, 177, 684–692. [Google Scholar] [CrossRef]
- Ryndock, E.J.; Meyers, C. A risk for non-sexual transmission of human papillomavirus? Expert Rev. Anti-Infect. Ther. 2014, 12, 1165–1170. [Google Scholar] [CrossRef]
- Harrison, R.; Huh, W. Occupational Exposure to Human Papillomavirus and Vaccination for Health Care Workers. Obstet. Gynecol. 2020, 136, 663–665. [Google Scholar] [CrossRef]
- Martínez-Gómez, X.; Curran, A.; Campins, M.; Alemany, L.; Rodrigo-Pendás, J.Á.; Borruel, N.; Castellsagué, X.; Díaz-De-Heredia, C.; Moraga-Llop, F.A.; del Pino, M.; et al. Multidisciplinary, evidence-based consensus guidelines for human papillomavirus (HPV) vaccination in high-risk populations, Spain, 2016. Euro Surveill. 2019, 24, 1700857. [Google Scholar] [CrossRef]
- de Martel, C.; Plummer, M.; Vignat, J.; Franceschi, S. Worldwide burden of cancer attributable to HPV by site, country and HPV type. Int. J. Cancer 2017, 141, 664–670. [Google Scholar] [CrossRef]
- Paavonen, J.; Naud, P.; Salmerón, J.; Wheeler, C.M.; Chow, S.N.; Apter, D.; Kitchener, H.; Castellsague, X.; Teixeira, J.C.; Skinner, S.R.; et al. Efficacy of human papillomavirus (HPV)-16/18 AS04-adjuvanted vaccine against cervical infection and precancer caused by oncogenic HPV types (PATRICIA): Final analysis of a double-blind, randomised study in young women. Lancet 2009, 374, 301–314. [Google Scholar] [CrossRef] [PubMed]
- Schiller, J.T.; Castellsagué, X.; Garland, S.M. A review of clinical trials of human papillomavirus prophylactic vaccines. Vaccine 2012, 30, F123–F138. [Google Scholar] [CrossRef]
- Garland, S.M.; Hernandez-Avila, M.; Wheeler, C.M.; Perez, G.; Harper, D.M.; Leodolter, S.; Tang, G.W.; Ferris, D.G.; Steben, M.; Bryan, J.; et al. Quadrivalent vaccine against human papillomavirus to prevent anogenital diseases. N. Engl. J. Med. 2007, 356, 1928–1943. [Google Scholar] [CrossRef]
- Macilwraith, P.; Malsem, E.; Dushyanthen, S. The effectiveness of HPV vaccination on the incidence of oropharyngeal cancers in men: A review. Infect. Agents Cancer 2023, 18, 24. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, K.J.; Jakobsen, K.K.; Jensen, J.S.; Grønhøj, C.; Von Buchwald, C. The Effect of Prophylactic HPV Vaccines on Oral and Oropharyngeal HPV Infection-A Systematic Review. Viruses 2021, 13, 1339. [Google Scholar] [CrossRef]
- Takes, R.P.; Wierzbicka, M.; D’Souza, G.; Jackowska, J.; Silver, C.E.; Rodrigo, J.P.; Dikkers, F.G.; Olsen, K.D.; Rinaldo, A.; Brakenhoff, R.H.; et al. HPV vaccination to prevent oropharyngeal carcinoma: What can be learned from anogenital vaccination programs? Oral Oncol. 2015, 51, 1057–1060. [Google Scholar] [CrossRef]
- Herrero, R.; Quint, W.; Hildesheim, A.; Gonzalez, P.; Struijk, L.; Katki, H.A.; Porras, C.; Schiffman, M.; Rodriguez, A.C.; Solomon, D.; et al. Reduced prevalence of oral human papillomavirus (HPV) 4 years after bivalent HPV vaccination in a randomized clinical trial in Costa Rica. PLoS ONE 2013, 8, e68329. [Google Scholar] [CrossRef]
- American Society for Colposcopy and Cervical Pathology (ASCCP). HPV Vaccination. ASCCP. Available online: https://portal.asccp.org/hpv-vaccination (accessed on 1 September 2025).
- Dermatologists Warn of Risks to Medics from HPV, COVID, and Other Viruses in Surgical Smoke. 2021. Available online: https://www.bad.org.uk/dermatologists-warn-of-risks-to-medics-from-hpv-covid-and-other-viruses-in-surgical-smoke (accessed on 1 September 2025).
- Organisation Mondiale de la Santé; World Health Organization. Human papillomavirus vaccines: WHO position paper (2022 update)–Vaccins contre les papillomavirus humains: Note de synthèse de l’OMS (mise à jour de 2022). Wkly. Epidemiol. Rec. = Relev. épidémiologique Hebd. 2022, 97, 645–672. [Google Scholar]
- Summary of WHO Position Papers—Immunization of Health Care Workers 2024. Available online: https://www.who.int/publications/m/item/table-4-summary-of-who-position-papers-immunization-of-health-care-workers (accessed on 2 September 2025).
- Moss, C.E. Control of smoke from laser/electric surgical procedures. Appl. Occup. Environ. Hyg. 1999, 14, 71. [Google Scholar] [CrossRef]
- Boitano, T.K.L.; Ketch, P.W.; Scarinci, I.C.; Huh, W.K. An Update on Human Papillomavirus Vaccination in the United States. Obstet. Gynecol. 2023, 141, 324–330. [Google Scholar] [CrossRef]
- Shemtob, L.; Asanati, K.; Jayasekera, P. Should healthcare workers with occupational exposure to HPV be vaccinated? Occup. Med. 2023, 73, 115–116. [Google Scholar] [CrossRef] [PubMed]
- Webb, W.M.; Covey, A.E. Risk of Occupational HPV Exposure Among Medical Trainees: A Call for HPV Vaccination. Kans. J. Med. 2023, 64 16, 143. [Google Scholar] [CrossRef] [PubMed]
- Dunne, E.F.; Markowitz, L.E.; Taylor, L.D.; Unger, E.R.; Wheeler, C.M. Human papilloma virions in the laboratory. J. Clin. Virol. 2014, 61, 196–198. [Google Scholar] [CrossRef]
- Bourgeois, J.; Ross, L. Vaccinating Providers for HPV Due to Transmission Risk in Ablative Dermatology Procedures. J. Clin. Aesthetic Dermatol. 2023, 16, 26–27. [Google Scholar]
- Yakşi, N.; Topaktaş, B. Knowledge Beliefs and Barriers of Healthcare Workers about Human Papilloma Virus (HPV) and HPV Vaccination. Acıbadem Üniversitesi Sağlık Bilim. Derg. 2023, 14, 183–189. [Google Scholar] [CrossRef]
- Shao, X.; Lu, X.; Zhou, W.; Huang, W.; Lu, Y. HPV Vaccination Behavior, Vaccine Preference, and Health Beliefs in Chinese Female Health Care Workers: A Nationwide Cross-Sectional Study. Vaccines 2023, 11, 1367. [Google Scholar] [CrossRef] [PubMed]
- AlShamlan, N.A.; AlOmar, R.S. HPV Vaccine Uptake, Willingness to Receive, and Causes of Vaccine Hesitancy: A National Study Conducted in Saudi Arabia Among Female Healthcare Professionals. Int. J. Women’s Health 2024, 16, 463–474. [Google Scholar] [CrossRef] [PubMed]
- Shakurnia, A.; Salehpoor, F.; Ghafourian, M.; Nashibi, R. Knowledge and attitudes toward HPV, cervical cancer and HPV vaccine among healthcare providers in Ahvaz, Southwest Iran. Infect Agent Cancer 2025, 20, 44. [Google Scholar] [CrossRef]
- Mishra, A.; Kushwaha, P.; Sud, S.S. Awareness and Acceptance of HPV Vaccine Among Healthcare Workers of Rural Haryana: A Cross-Sectional Study. J. Neonatal Surg. 2025, 14, 527–531. [Google Scholar]
- Daniel, C.L.; McLendon, L.; Green, C.L.; Anderson, K.J.; Pierce, J.Y.; Perkins, A.; Beasley, M. HPV and HPV Vaccination Knowledge and Attitudes Among Medical Students in Alabama. J. Cancer Educ. 2021, 36, 168–177. [Google Scholar] [CrossRef]
- Drolet, M.; Bénard, É.; Pérez, N.; Brisson, M. Population-level impact and herd effects following the introduction of human papillomavirus vaccination programmes: Updated systematic review and meta-analysis. Lancet 2019, 394, 497–509. [Google Scholar] [CrossRef]
- Arbyn, M.; Xu, L.; Simoens, C.; Martin-Hirsch, P.P. Prophylactic vaccination against human papillomaviruses to prevent cervical cancer and its precursors. Cochrane Database Syst. Rev. 2018, 5, Cd009069. [Google Scholar] [CrossRef]
- Kamolratanakul, S.; Pitisuttithum, P. Human Papillomavirus Vaccine Efficacy and Effectiveness against Cancer. Vaccines 2021, 9, 1413. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.