Abstract
The human papillomavirus (HPV) vaccine was initially approved for a three-dose regimen. Due to resource limitations, budget constraints, low acceptance, and poor adherence, global vaccination coverage is only 15%. A single-dose regimen could simplify logistics, reduce costs, and improve accessibility. However, its clinical effectiveness remains debatable. This review systematically searched PubMed, Embase, and Cochrane Library, including 42 clinical studies, to assess the effectiveness of a single-dose HPV vaccination for preventing HPV infections, cervical abnormalities, and genital warts. We summarized the effectiveness of bivalent, quadrivalent, and nonavalent vaccines across different age groups and buffer periods, and analyzed the factors contributing to the inconsistency of results. The review also provides insights into designing robust future research to inform single-dose HPV vaccination policies and guidelines, highlighting the need for further research to refine vaccination strategies.
1. Introduction
Human papillomavirus (HPV) infection is the most prevalent sexually transmitted infection globally, with an estimated 80% lifetime exposure risk [1]. Over 40 types of HPV can infect the genital regions, oral cavity, and throat in both men and women. Fifteen genotypes of HPV are linked to cervical cancer, and at least one type is associated with cancers of the vulva, vagina, penis, anus, and certain head and neck regions—specifically the oropharynx [2,3]. Recombinant prophylactic vaccines containing virus-like particles of HPV have been approved for human use, providing prevention against HPV infections, cervical abnormalities, genital warts, and anal intraepithelial neoplasia [2,4]. Despite these benefits, global vaccination coverage remains low at approximately 15% due to limited resources, budget constraints, low acceptance, and poor adherence to the HPV vaccine [5]. A single-dose regimen could simplify vaccine administration, lower costs, and increase accessibility compared to multi-dose schedules, and especially benefits low- and middle-income countries (LMICs), where 85% of cervical cancer deaths occur [6,7]. Thus, reliable and quantitative evidence on the effectiveness of a single-dose HPV vaccination is essential to guide decision-making.
While earlier studies have examined the efficacy of a single-dose HPV vaccination compared to two- and three-dose ones, the single-dose HPV vaccination schedule is still debatable [8,9,10]. Previous reviews on the clinical efficacy of the single-dose HPV vaccination have been limited by the inclusion of an incomplete range of studies, leading to insufficient reporting of clinical outcomes. In addition, these reviews did not explore the effectiveness of bivalent, quadrivalent, and nonavalent vaccines separately [8,9,11]. This called for a thorough analysis to evaluate and compare the clinical efficacy of single-dose regimen for each HPV vaccine variant. Our review included all eligible clinical studies, regardless of study design, aiming to assess the clinical effectiveness of a one-dose bivalent HPV vaccination (Cervarix®, Cecolin® or Walrinvax®), quadrivalent HPV vaccination (Gardasil®), or nonavalent HPV vaccination (Cervarix®) [12] on HPV infection, cervical cytological and histological abnormalities, and genital warts in both men and women.
2. Methods
2.1. Search Strategy and Study Selection
To ensure a comprehensive search of the existing literature on the clinical effectiveness of the single-dose HPV vaccination, we searched PubMed, Embase, and Cochrane Library to identify eligible studies published before May 2024. Our search terms comprised (“papillomavirus vaccine”, or “papillomavirus vaccination”, “HPV vaccine”, “HPV vaccination”) AND (“vaccine effectiveness”, “infection”, “HPV”, “cervical abnormality”, “cervical neoplasm”, “cervical neoplasia”, “cervical intraepithelial neoplasia”, “HPV related disease”, “condyloma”, “genital wart”, “anogenital wart”, “anal intraepithelial neoplasia”) AND (“single-dose”, “one-dose”, “two-dose”, “three-dose”, “dose”), and detailed search strategies are given in Table S1. Moreover, we cross-referenced the references in the included studies to guarantee thorough coverage in the online search.
Studies were eligible for inclusion if they fulfilled the following criteria: (1) The study reported the clinical effectiveness of the HPV vaccination against HPV infection, cervical abnormalities, genital warts, and anal intraepithelial neoplasia. (2) The study compared the clinical effectiveness between the group receiving a one-dose HPV vaccine and the group not receiving an HPV vaccine, or between the group receiving a one-dose HPV vaccine and the group receiving a multiple-dose HPV vaccine. Studies were excluded if: (1) The study did not investigate the role of the prophylactic HPV vaccination. (2) The study solely explored the cost-effectiveness of vaccination. (3) The article type was a conference abstract or letter without original research data, or a review. (4) No full text could be found.
2.2. Data Extraction
Two authors (W.B. and X.H.) independently extracted the main study characteristics using standardized forms. Discrepancies were resolved by a third author (Z.L.). The main study characteristics included endpoint, vaccine, author, year, country, study design, gender, number of the population in each group, participant age, follow-up duration, case definition, assignment of dose number, buffer periods, sensitivity analyses by age group/buffer, adjustment, and outcome.
2.3. Data Synthesis
Data reported in the publications were synthesized narratively. The primary outcome was the effectiveness of HPV vaccination by comparing the HPV-related endpoints between individuals vaccinated with different numbers of doses (one vs. none, two vs. none, three vs. none). The vaccines analyzed included a bivalent HPV vaccine (Cervarix®, Cecolin®, or Walrinvax®), a quadrivalent HPV vaccine (Gardasil®), and a nonavalent HPV vaccine (Gardasil ®). Results were presented as crude or adjusted risk ratios (RR), hazard ratios (HR), incidence rate ratios (IRR), prevalence ratios (PR), or odds ratios (OR).
We decided not to use meta-analysis due to significant heterogeneity among the eligible studies: (1) The research encompassed both database-based investigations and clinical trials. The differences in their study topics, data sources, and methodological choices were substantial. (2) The study designs varied, including cohort studies, cross-sectional studies, and case-control studies. (3) The control groups exhibited inconsistency, as numerous studies compared non-vaccinated groups with 1-, 2-, and 3-dose vaccine groups, while other studies only compared groups receiving varying dosages. (4) Participants’ characteristics differed significantly, such as age at vaccination, sexual history, HPV infection status, and smoking status. (5) Clinical outcomes were measured at different follow-up times, leading to inconsistent evaluation time points for vaccine efficacy. (6) The results were reported in various formats, with some studies providing detailed numbers of patients, and others reporting only RR/HR/IRR/PR/OR. These distinctions between studies affected the consistency and comparability of the results, preventing standardization across studies. Therefore, we summarized the key information from each study in Table 1 and Tables S2–S4, and used forest plots to integrate useful data.
3. Results
3.1. Study Characteristics
A total of 5388 articles were initially identified. After a thorough screening process, 124 articles underwent full-text review, and 42 clinical studies published between 2011 and 2023 were included in the final analysis (Figure 1) [11,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53]. Among these, 14 studies investigated the clinical effectiveness of the bivalent HPV vaccine, 29 studies focused on the quadrivalent HPV vaccine, and only two studies examined the efficacy of the nonavalent HPV vaccine. Regarding study populations, only one study on the quadrivalent vaccine included both men and women, and another study on the quadrivalent vaccine included males only, while the remaining studies included females only. The clinical outcomes assessed included cervical HPV infections, oral HPV infections, cervical cytological and histological abnormalities, and genital warts.
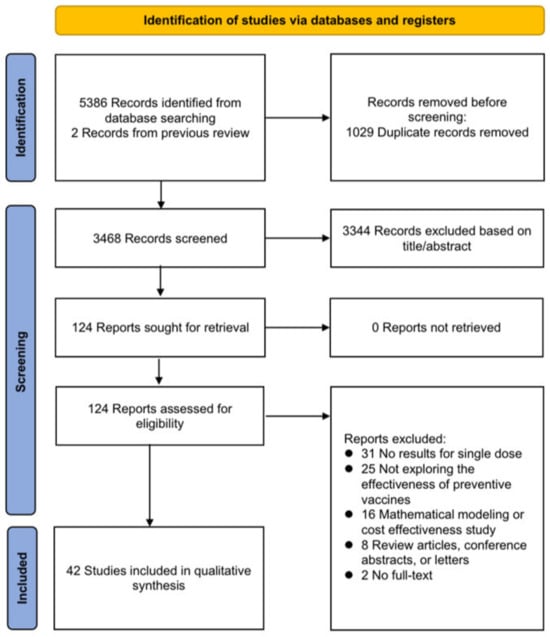
Figure 1.
Flow diagram of study selection process.

Table 1.
Characteristics of studies that evaluated HPV vaccine effectiveness by number of doses.
Table 1.
Characteristics of studies that evaluated HPV vaccine effectiveness by number of doses.
| Endpoint/ Vaccine/Author | Country | Study Design | Gender | Number of Population in Each Group | Participant Age | Follow-Up Duration | Case Definition | Assignment of Dose Number | Buffer Periods (Months) | Sensitivity Analyses by Age Group /Buffer | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Vaccination | Outcome | ||||||||||
| Cervical HPV infection | |||||||||||
| Bivalent vaccine | |||||||||||
| Kreimer 2011 [21] | Costa Rica | Post-hoc analysis of RCT (CVT) | Women | 0: 3578 1: 196 2 (months 0, 1 /0, 6): 422 3 (months 0, 1, 6): 2957 | 18–25 | 18–29 | 4 years | Persistent infection for 6/12 months: HPV 16/18 | Final status | 6 | ——a |
| Kavanagh 2014 [17] | Scotland | Cross-sectional study using screening registry data | Women | 0: 3418 1: 55 2: 106 3: 1100 | 12–13 | 20–21 | —— | (1) HPV 16/18 (2) HPV 31/33/45 (3) HPV35/39/51/52/56/58/59 (4) Any HPV type | Final status | 0 | —— |
| Kreimer 2015 [21] | Costa Rica | Retrospective cohort study (Combined CVT and PATRICIA data) | Women | 1: case: 292 control: 251 2 (months 0, 1/0, 6): case: 611 control: 574 3 (months 0, 1, 6): case: 11,110 control: 11,217 | 15–25 | 15–29 | 4 years | Incident and persistent infection for 6/12 months: (1) HPV 16/18 (2) HPV 31/33/45 | Final status | 6 | —— |
| Cuschieri 2016 [22] | Scotland | Cross-sectional study using screening registry data | women | 0: 3619 1: 177 2: 300 3: 1853 | 15–17 | 20–21 | —— | (1) HPV 16/18 (2) HPV 31/33/45 | Final status | 0 | —— |
| Kavanagh 2017 [27] | Scotland | Cross-sectional study using screening registry data | women | 0: 4008 1: 223 2: 391 3: 3962 | 12–≥18 | 20–21 | —— | (1) HPV 16/18 (2) HPV 31/33/45 (3) HPV35/39/51/52/56/58/59 (4) Any HPV type | Final status | 0 | —— |
| Safaeian 2018 [32] | Costa Rica | Post-hoc analysis of RCT (CVT) | Women | 0: 2382 1: 134 2 (months 0, 1): 193 2 (months 0, 6): 79 3 (months 0, 1, 6): 2043 | 18–25 | 18–32 | 7 years | Year 7 prevalent HPV infection (an infection detected at year 7): (1) HPV 16/18 (2) HPV 31/33/45 (3) HPV 35/39/51/52/56/58/59 (4) Non-carcinogenic HPV | Final status | 12 | —— |
| Kreimer 2020 [43] | Costa Rica | Post-hoc analysis of RCT (CVT) | Women | 0: 1783 1: 112 2 (months 0, 6): 62 3 (months 0, 1, 6): 1365 | 18–25 | 18–37 | 12 years | Incident HPV infection (an infection detected at year 11 but not detected at the year or prevalent HPV infection (an infection detected at years 9 and 11: (1) HPV 16/18 (2) HPV 35/39/51/52/56/58/59 (3) Non-carcinogenic HPV | Final status | 0 | —— |
| Barnabas 2022 [50] | Kenya | Randomized controlled trial | Women | 0: 473 1: 489 | 15–20 | 15–22 | 18 months | Persistent HPV for ≥4 months: HPV 16/18 | Final status | 3, 6 | Buffer |
| Barnabas 2023 [51] | Kenya | Randomized controlled trial | Women | 0: 473 1: 489 | 15–20 | 15–23 | 3 years | Persistent HPV for ≥4 months: HPV 16/18 | Final status | 3, 6 | Buffer |
| Quadrivalent vaccine | |||||||||||
| Sankaranarayanan 2016 [25] | India | Prospective cohort study | Women | 1: 870 2 (days 1, 60): 717 2 (days 1, ≥180): 526 3 (days 1, 60, ≥180): 536 | 10–18 | 10–22 | 4 years | Incident and persistent infection for ≥12 months: (1) HPV 16 (2) HPV 18 (3) HPV 16/18 (4) HPV 6/11 (5) HPV 6/11/16/18 (6) HPV 31/33/35 (7) HPV 6/11/16/18/31/33/35 | Final status | 0 | —— |
| Sankaranarayanan 2018 [33] | India | Prospective cohort study | Women | 0: 1141 1: 604 2 (days 1, 60): 608 2 (days 1, ≥180): 818 3 (days 1, 60, ≥180): 959 | 10–18 | 10–25 | 7 years | Persistent infection for ≥12 months: (1) HPV 16/18 (2) HPV 31/33/35 (3) Non-vaccine targeted HPV | Final status | 0 | —— |
| Sonawane 2019 [39] | United States | Cross-sectional study of a nationally representative sample | Women | 0: 1004 1: 106 2: 126 3: 384 | ≤26 | 18–26 | —— | (1) HPV 6/11/16/18 (2) HPV 31/33/45 (3) HPV 35/39/51/55/56/58/59/68 | Final status | 0 | —— |
| Markowitz 2020 [44] | United States | Cross-sectional study of women enrolled in an integrated health-care delivery system | Women | 0: 1052 1: 303 2: 304 3: 2610 | ≤29 | 20–29 | —— | (1) HPV 6/11/16/18 (2) Non-4vHPV (3) HPV 16/18/31/33/35/39/45/51 /52/56/58/59/66/68 (4) HPV 31/33/45 | Final status | 1 | Age group |
| Batmunkh 2020 [41] | Mongolia | Retrospective cohort study | Women | 0: 357 1: 118 | 11–17 | 16–26 | 6 years | (1) HPV 16 (2) HPV 18 (3) HPV 16/18 (4) Any HPV (5) HPV 35/39/51/52/56/58/59/68 (6) HPV 16 + other type/18 + other type/16 + 18 + other type | Final status | 0 | —— |
| Basu 2021 [49] | India | Prospective cohort study | Women | 0: 1479 1: 2858 2: 2166 3: 2019 | 10–18 | 10–28 | 10 years | Incident and persistent infections for ≥10 months: (1) HPV 16/18 (2) HPV 6/11/16/18 (3) HPV 31/33/35 (4) Any HPV | Final status | 1 | —— |
| Reyburn 2023 [53] | Fiji | Retrospective cohort study | Women | 0: 376 1: 158 2: 99 3: 189 | 15–23 | 15–34 | 6–11 years | (1) HPV 16/18/31/33/35/39/45 /51/52/56/58/59/66/68; (2) HPV 16/18 (3) HPV 6/11 (4) HPV 31/33/35/39/45/51/52 /56/58/59/66/68 (5) HPV 6/11/16/18/31/33/45/52/58 (6) HPV 6/11/31/33/45/52/58 | Final status | 0 | —— |
| Nonavalent vaccine | |||||||||||
| Barnabas 2022 [50] | Kenya | Randomized controlled trial | Women | 0: 473 1: 496 | 15–20 | 15–22 | 18 months | Persistent HPV infection for ≥4 months: (1) HPV 16/18 (2) HPV 16/18/31/33/45/52/58 | Final status | 3, 6 | Buffer |
| Barnabas 2023 [51] | Kenya | Randomized controlled trial | Women | 0: 473 1: 496 | 15–20 | 15–23 | 3 years | Persistent HPV infection for ≥4 months: (1) HPV 16/18 (2) HPV 16/18/31/33/45/52/58 (3) HPV 31/33/45 | Final status | 3, 6 | Buffer |
| Penile, scrotal, or anal HPV infection in men | |||||||||||
| Quadrivalent vaccine | |||||||||||
| Widdice 2019 [40] | United States | Cross-sectional study | Men | 0: 471 1: 58 2: 37 3: 143 | Attained vaccine in 2013–2014: 16.2 (mean); attained vaccine in 2016–2017: 15.1 (mean) | 13–26 | —— | HPV 6/11/16/18 | Final status | 0 | —— |
| Oral HPV infection in women | |||||||||||
| Quadrivalent vaccine | |||||||||||
| Gheit 2023 [52] | India | Retrospective cohort study | Women | 0: 179 1: 204 2 (days 1 and 60): 101 3 (days 1 and 180): 190 3:(days 1, 60, and 180): 323 | 10–18 | 18–25 | —— | (1) HPV 16 (2) HPV 18 (3) HPV 16/18 (4) HPV 6/11/16/18 (5) Non-HPV 6/11/16/18 (6) Any HPV | Final status | 0 | —— |
| Cervical abnormalities | |||||||||||
| Bivalent vaccine | |||||||||||
| Pollock 2014 [18] | Scotland | Retrospective cohort study using linked national registry data | Women | 0: 76,114 1: 1315 2: 2725 3: 25,898 | 15–>18 | 20–21 | —— | Histology: (1) CIN3 (2) CIN2 (3) CIN1 | Final status | 0 | —— |
| Cameron 2017 [26] | Scotland | Retrospective cohort study using linked national registry data | Women | 0: 75,683 1: 2258 2: 4462 3: 55,303 | 14–>18 | 20–21 | —— | Histology: (1) CIN3 (2) CIN2 (3) CIN1 | Final status | 0 | —— |
| Palmer 2019 [38] | Scotland | Retrospective cohort study using linked national registry data | Women | 0: 64,026 1: 2051 2: 4135 3: 68,480 | 12–>18 | 20 | —— | Histology: (1) CIN3+ (2) CIN2 (3) CIN1 Cytology: (1) high grade dyskaryosis/HSIL-H borderline/ASCUS (2) moderate dyskaryosis/HSIL-M (3) low grade dyskaryosis/LSIL (4) borderline/ASCUS | Final status | 0 | —— |
| Martellucci 2021 [47] | Italy | Retrospective cohort study using administrative data | Women | 0: 7394 1: 212 2: 83 3: 96 | 14–>30 | 17–32 | —— | Cytology: (1) HSIL (2) LSIL | Final status | 1, 6, 12 | Buffer |
| Quadrivalent vaccine | |||||||||||
| Gertig 2013 [14] | Australia | Retrospective cohort study using linked data from registries | Women | 0: 14,085 1: 1422 2: 2268 3: 21,151 | 12–19 | 12–21 | —— | Histology: (1) CIN3/AIS (2) CIN2+/AIS (3) CIN2 (4) CIN1 Cytology: (1) High grade (possible HSIL, HSIL, HSIL with possible microinvasion/invasion, squamous cell carcinoma, possible high-grade endocervical glandular lesion, AIS, AIS with possible microinvasion/invasion and adenocarcinoma) (2) Low grade (possible LSIL, LSIL and atypical endocervical cells of uncertain significance) | Time-dependent; final status | 0 | —— |
| Crowe 2014 [15] | Australia | Case-control study using linked data from registries | Women | 0: 60,282 1: 10,879 2: 12,073 3: 25,119 | 12–26 | 11–31 | —— | Histology: (1) CIN2+/AIS (2) Other cases (either a low-grade abnormality at histology or an abnormal cytology result that was not confirmed by histology) | Final status | 0, 1, 6, 12 | Age group, buffer |
| Brotherton 2015 [11] | Australia | Retrospective cohort study using linked regional data registries | Women | 0: 133,055 1: 20,659 2: 27,500 3: 108,264 | 12–26 | 12–30 | —— | Histology: (1) CIN3/AIS, (2) CIN2+ (3) CIN2 Cytology: (1)high grade (possible HSIL, HSIL, HSIL with possible microinvasion/invasion, squamous cell carcinoma, possible high-grade endocervical glandular lesion, AIS, AIS with possible microinvasion/invasion and adenocarcinoma) (2) low grade (possible LSIL, LSIL) | Final status | 0, 1, 6, 12, 24 | Age group, buffer |
| Hofstetter 2016 [23] | United States | Retrospective cohort study using medical center records | Women | 0: 1632 1: 695 2: 604 3: 1196 | 11–20 | 11–27 | —— | Cytology: Any abnormal (atypical squamous cells of undetermined significance, atypical glandular cells, atypical squamous cells cannot exclude a high-grade squamous intraepithelial lesion, low-grade squamous intraepithelial lesion, and high-grade squamous intraepithelial lesion) | Final status | 1 | Age group |
| Kim 2016 [24] | Canada | Nested case-control study using linked data from registries | Women | 0: 5712 1: 327 2: 490 ≥3: 3675 | 10–15 | 18–21 | —— | Cytology: (1) High grade (ASC-H or HSIL) (2) Low grade (ASC-US or LSIL) (3) Abnormal (ASC-US, LSIL, ASC-H or HSIL) | Final status | 0 | —— |
| Silverberg 2018 [34] | United States | Nested case-control study of women enrolled in an integrated health-care delivery system | Women | 0: 23,293 1: 756 2: 554 ≥3: 1527 | 14–26 | 18–34 | —— | Histology: (1) CIN3+ (2) CIN2+ | Final status | 6 | —— |
| Dehlendorff 2018 [30] | Denmark & Sweden | Retrospective cohort study using linked national registry data | Women | 0: 2,091,579 1: NA 2: NA 3: NA | 13–29 | 13–30 | —— | Histology: CIN2+ | Time- dependent | 0 | Age group |
| Brotherton 2019 [37] | Australia | Retrospective cohort study using linked regional data registries | Women | 0: 48,845 1: 8618 2: 18,190 3: 174,995 | ≤13–22 | 15–22 | —— | Histology: (1) CIN3/AIS + histopathology (2) CIN2+/AIS | Final status | 0, 12, 24 | Buffer |
| Verdoodt 2020 [46] | Denmark | Retrospective cohort study using linked national registry data | Women | 0: 374,327 1: 10,480 2: 30,259 3: 174,532 | 12–16 | 17–25 | —— | Histology: (1) CIN3+ (2) CIN2+ | Time- dependent | 0, 6 in secondary analysis | Age group |
| Johns 2020 [42] | United States | Case-control study using medical records data | Women | 0: 2731 1: 136 2: 108 3: 325 | 12–26 | 18–39 | —— | Histology: CIN2+ | Final status | 1, 12, 24, 36 | Buffer |
| Rodriguez 2020 [45] | United States | Retrospective matched cohort study using health insurance claims database | Women | 0: 66,541 1: 13,630 2: 14,088 ≥3: 38,823 | 9–26 | 9–31 | —— | Histology: CIN2/3 Cytology: high-grade (HSIL/ASC-H) | Final status | 12 | Age group, dose interval, history and results of pap test |
| Genital warts | |||||||||||
| Bivalent vaccine | |||||||||||
| Navarro- Illana 2017 [28] | Spain | Retrospective cohort study using national health registries | Women | 0: 607,006 1: 18,142 2: 31,420 3: 153,296 | 14 | 14–19 | —— | Genital warts (ICD9-CM code 078.11) | Time- dependent | 0 | —— |
| Quadrivalent vaccine | |||||||||||
| Herweijer 2014 [16] | Sweden | Retrospective cohort study using population-based health registries | Women | 0: 1,045,157 1: 115,197 2: 107,338 3: 89,836 | 10–19 | 10–24 | —— | Genital warts (ICD-10 code A63.0 or podophyllotoxin/imiquimod prescription) | Time- dependent | 0–12 | Age group |
| Blomberg 2015 [19] | Denmark | Retrospective cohort study using national health registries | Women | 0: 188,956 1: 55,666 2: 93,519 3: 212,549 | 12–27 | 12–27 | —— | Genital warts (ICD-10 code A63.0 or podophyllotoxin prescription) | Time- dependent | 1 | —— |
| Dominiak- Felden 2015 [30] | Belgium | Retrospective cohort study using sick-fund/insurance reimbursement database | Women | 0: 63,180 1: 4020 2: 3587 3: 35,792 | 10–22 | 16–22 | —— | Genital warts (reimbursement of imiquimod) | Time- dependent | 1 | —— |
| Perkins 2017 [29] | United States | Retrospective cohort study using commercial claims database | Women | 0: 201,933 1: 30,438 2: 36,583 3: 118,962 | 9–25 | 9–25 | —— | Genital warts (ICD-9 and CPT codes and prescriptions) | Final status | 0 | —— |
| Navarro- Illana 2017 [28] | Spain | Retrospective cohort study using national health registries | Women | 0: 607,006 1: 18,142 2: 31,420 3: 153,296 | 14 | 14–19 | —— | Genital warts (ICD-9-CM code 078.11) | Time- dependent | 0 | —— |
| Hariri 2018 [31] | United States | Retrospective cohort study in integrated health-care delivery systems | Women | 0: 31,563 1: 5864 2: 5459 3: 21,631 | 16–17 (mean) | 11–28 | —— | Genital warts (ICD-9 code 078.10, 078.11, 078.19, specialty of diagnosing provider, and sexually transmitted infection tests ordered) | Final status | 6 from last dose 12 from first dose | Buffer |
| Zeybek 2018 [36] | United States | Matched retrospective cohort study using health insurance claims databases | Men and women | 0: 286,963 1: 54,280 2: 55,632 3: 177,051 | 9–26 | 10–31 | 5 years | Genital warts (ICD-9-CM or 10 code 078.11 or A63.0) | Final status | 3 from the last dose | Age group |
| Willows 2018 [54] | Canada | Matched retrospective cohort study using linked vaccine registry and claims and population-based databases | Women | 0: 94,327 1: 3521 2: 6666 3: 21,277 | 9–26 | 10–33 | —— | Genital warts (ICD-9-CM or 10 code 078.11 or A63.0 and related procedure code) | Final status | 0 | Age group |
| Baandrup 2021 [48] | Denmark | Retrospective cohort study using population-based health national registries | Women | 0: 1,904,895 1: 235,653 2: 460,978 3: 1,934,589 (person-yrs) | 12–30 | 12–30 | —— | Genital warts (ICD-10 code A63.0 or podophyllotoxin prescription) | Time- dependent | 1 | Age group, maternal educational level |
| Reyburn 2023 [53] | Fiji | Retrospective cohort study | Women | 0: 376 1: 158 2: 99 3: 189 | 15–23 | 15–34 | 6–11 years | Genital warts (confirmed by the midwife and antenatal clinic obstetric doctor) | Final status | 0 | —— |
Abbreviations: HPV, human papillomavirus; CIN, cervical intraepithelial neoplasia; AIS, adenocarcinoma in situ; HSIL, high-grade squamous intraepithelial lesions (HSIL-M = mild dyskaryosis; HSIL-H = high grade dyskaryosis); LSIL, low-grade squamous intraepithelial lesions; ASC-H, atypical squamous cells, cannot exclude HSIL; ASC-US, atypical squamous cells of undetermined significance; ICD-9-CM, international classification of diseases, 9th revision, clinical modification; CPT, current procedural terminology. a Articles did not have sensitivity analyses by age group/buffer.
3.2. Cervical HPV Infection in Women
3.2.1. Bivalent Vaccine
The HPV 16/18 infection in the one-dose group was evaluated in nine studies. According to three trials from a single piece of research, the one-dose bivalent vaccine offered comparable protection against HPV 16/18 infection to the two- and three-dose regimens across follow-up periods of 4, 7, and 12 years [21,32,43]. Besides, the effectiveness of the single-dose vaccination in preventing persistent HPV 16/18 infections for at least 4 months [50,51], 6 months [13,21], and 12 months [13,21] was similar to that of two and three doses. Nevertheless, three studies reported that a single dose was less beneficial than two and three doses [17,22,27]. Notably, Barbanas et al.’s studies evaluated the vaccine’s effectiveness by applying varying buffer periods and suggested that the effectiveness of a single dose increased with a 6-month buffer period compared to 3 months [50,51].
Six studies evaluated the single-dose bivalent vaccination’s effectiveness against HPV 31/33/45 infections, but only that of Safaeian et al. showed similar protection for one, two, and three doses [32]. Four studies assessed the vaccine’s impact on high-risk HPV (hrHPV) 35/39/51/52/56/58/59, finding no significant prevention effectiveness, regardless of the number of doses [17,27,32,43].
3.2.2. Quadrivalent Vaccine
Four studies concluded that a single dose was highly effective against HPV16/18 infection [25,41,49,53]. Three studies comparing the effectiveness of 1, 2, and 3 doses against 10 months and ≥12 months of persistent HPV16/18 infection also found similar protection across all doses [25,33,49].
Four studies evaluated the vaccine’s efficacy against HPV 6/11/16/18, indicating similar protection for 1, 2, and 3 doses [25,39,44,49]. One study noted higher effectiveness among women who received the first dose at age ≤ 18 than those >18, regardless of the number of doses [44].
The effectiveness of quadrivalent vaccine against HPV31/33/45 varied across five studies [25,33,39,44,49]. Only one study reported lower HPV31/33/45 infection rates in the one-dose group compared to unvaccinated individuals, similar to the two- and three-dose groups. Three studies indicated no protection against HPV31/33/45 with one dose [25,39,44], and two studies based on the same clinical study showed that one-dose quadrivalent vaccination could not protect against persistent HPV 31/33/45 infection over 12 months during the 4-year and 7-year follow-ups [25,33].
Two studies provided data on all hrHPV (16/18/31/33/35/39/45/51/52/56/58/59/66/68) [44,53], and one study provided data on non-vaccine hrHPV (31/33/35/39/45/51/52/56/58/59/66/68) [53]. They all showed that one-, two-, and three-dose quadrivalent vaccinations did not reduce the hrHPV infection rate.
3.2.3. Nonavalent Vaccine
Two manuscripts based on the same study explored the effectiveness of a nonavalent vaccine on HPV infection, and both analyzed the vaccine effectiveness with different buffer periods [50,51].
The efficacy of the single-dose nonavalent HPV vaccination was high among persistent HPV 16/18 and persistent HPV 16/18/31/33/45/52/58 for at least 4 months in 18-month [50] and 3-year [51] follow-up periods, and high among persistent HPV31/33/45 for at least 4 months in a 3-year follow-up duration [51], exhibiting strong defenses against vaccine-specific HPV infection. Both of these publications showed that the efficacy of a single dose appeared to rise with buffer periods of six months as opposed to three months.
In conclusion, the one-dose bivalent vaccination was able to prevent HPV16/18 infections, although some research suggested that two or three doses of bivalent vaccination were more effective (Figure 2). One-dose quadrivalent and nonavalent HPV vaccinations showed comparable protection against vaccine-specific HPV types to two- and three-dose regimens, with the effectiveness rising with younger age groups and longer buffer periods (Figure 2 and Figure 3). Comparing single-dose bivalent or quadrivalent HPV vaccinations to two and three doses, single-dose vaccination demonstrated less cross-protection against hrHPV (Figure 4).
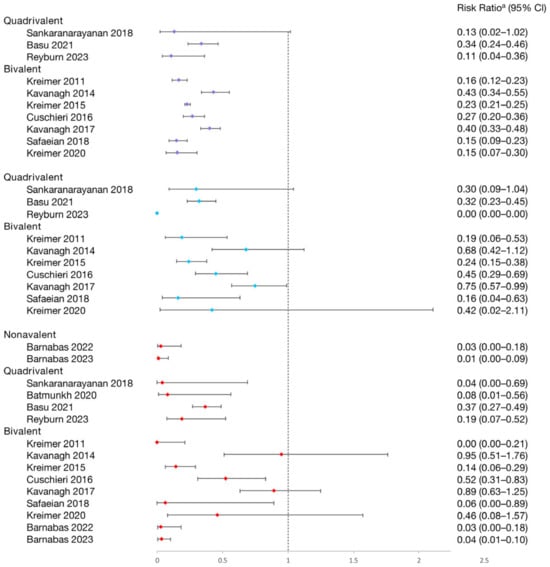
Figure 2.
Effectiveness of varying doses of bivalent, quadrivalent, and nonavalent HPV vaccines in protecting women against HPV 16/18 infection [13,17,21,22,27,32,33,43,49,50,51,53]. Purple square: 3 dose vs. 0 dose; blue square: 2 doses vs. 0 dose; red square: 1 dose vs. 0 dose. a The risk ratio encompasses various measures depending on the study, including risk ratio, hazard ratio, prevalence ratio, or odds ratio. The risk ratio for Sankaranarayanan 2018 and Safaeian 2018 was not provided in the original texts and was calculated based on sample sizes. Other risk ratios in the figure were extracted directly from the original articles. If the original articles did not include available data for all age groups, they were excluded from this figure.
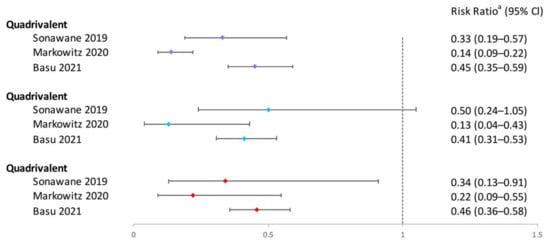
Figure 3.
Effectiveness of varying doses of quadrivalent HPV vaccine in protecting women against HPV 6/11/16/18 infection. Purple square: 3 dose vs. 0 dose; blue square: 2 doses vs. 0 dose; red square: 1 dose vs. 0 dose [39,44,49]. a The risk ratio encompasses various measures depending on the study, including risk ratio, prevalence ratio, or hazard ratio. The risk ratio for Sonawane 2019 was not provided in the original texts and was calculated based on sample sizes. Other risk ratios in the figure were extracted directly from the original articles. If the original articles did not include available data for all age groups, they were excluded from this figure.
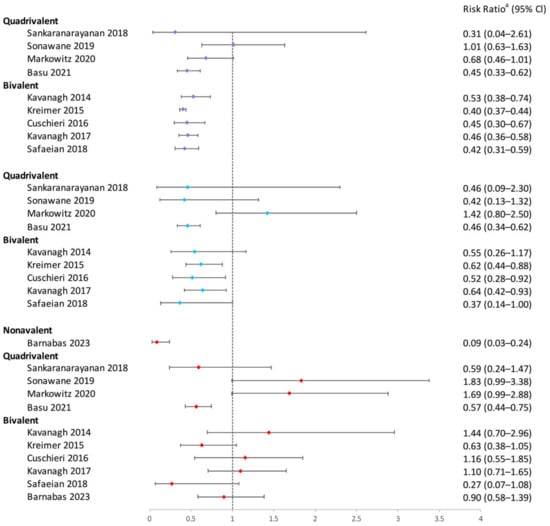
Figure 4.
Effectiveness of varying doses of bivalent, quadrivalent, and nonavalent HPV vaccines in protecting women against HPV 31/33/35 infection. Purple square: 3 dose vs. 0 dose; blue square: 2 doses vs. 0 dose; red square: 1 dose vs. 0 dose [17,21,22,27,32,33,39,40,49,51]. a The risk ratio encompasses various measures depending on the study, including risk ratio, prevalence ratio, hazard ratio, or odds ratio. The risk ratio for Sankaranarayanan 2018, Sonawane 2019, and Safaeian 2018 was not provided in the original texts and was calculated based on sample sizes. Other risk ratios in the figure were extracted directly from the original articles. If the original articles did not include available data for all age groups, they were excluded from this figure.
3.3. Other HPV Infection
3.3.1. Penile, Scrotal, or Anal HPV Infection in Men
Among young men who had previously engaged in sexual activity, a cross-sectional study examined the efficacy of the quadrivalent vaccine [40]. The results showed no statistically significant differences in vaccine-type HPV infection rates between those receiving 0, 1, 2, or ≥3 doses.
3.3.2. Oral HPV Infection in Women
A retrospective cohort study aimed to investigate whether married female participants could avoid oral HPV infection by taking the quadrivalent vaccine [52]. The findings implied that vaccine-type and non-vaccine-type oral HPV infection might be avoided with two- or three-dose HPV vaccination, but not with a one-dose one.
3.4. Cervical Histological and Cytological Abnormalities in Women
3.4.1. Bivalent Vaccine
Four studies assessed the effectiveness of the bivalent vaccine in reducing cervical histological abnormalities. Two studies showed no significant effectiveness for one or two doses on reducing atypical squamous cells of undetermined significance (ASC-US), low-grade squamous intraepithelial lesions (LSIL), high-grade squamous intraepithelial lesions (HSIL), cervical intraepithelial neoplasia 1 (CIN1), CIN2+, and CIN3+, with only three doses being effective except for LSIL [18,38]. Cameron et al. [26] found that the one-dose quadrivalent vaccine could reduce CIN1, CIN2, and CIN 3, but the effect was weaker than with two or three doses. Only Martellucci et al. found reductions in LSIL for at least one dose, similar to two and three doses, with effectiveness confirmed across buffer periods [47].
3.4.2. Quadrivalent Vaccine
Data on the prevention of cervical histological and cytological abnormalities with a single dose of quadrivalent vaccine have been reported in 11 studies [11,14,15,23,24,30,34,37,42,45,46]. The effectiveness of a quadrivalent vaccine against CIN3+,CIN2+, high-grade (HG) abnormalities, and cytological low-grade (LG) abnormalities all varied across different studies. Some found that one-, two-, and three-dose vaccinations provided similar protection [45,46], and some noted that single-dose effectiveness was slightly weaker than two- and three-dose regimens [15,24,30,37,42], while other studies reported that a single dose was not effective [34].
In studies that support the effectiveness of single-dose immunization, five studies evaluated the effectiveness by using varying age groups [11,15,30,45,46]. Two studies reported that the quadrivalent vaccine had better effectiveness on younger age groups. Verdoodt et al. found a lower CIN3+ rate in women aged under 23, compared to those aged 23 and older [46]. Dehlendorff et al. reported that CIN2+ risk decreased in women aged 13–16 and 17–19, but that it could not decrease in women aged 20–29 [30]. Notably, three studies found the quadrivalent vaccine was less effective in not only older women, but also in young girls. Crowe et al. found the vaccine effective against CIN2+ among women vaccinated at ages 15–18 and 19–22, but not among those aged 11–13 and 23–27 [15]. Rodriguez et al. found a similar reduction in HG abnormalities for women aged 15–19, but no effectiveness in those under 15 or over 20 [45]. Brotherton et al. observed a decrease in HG abnormalities in women vaccinated at ages 17–23, but no decrease for women aged ≤ 16 [11].
In studies suggesting the efficacy of single-dose vaccination, the impact of different buffer intervals on vaccine efficacy was examined in four studies [11,15,37,42]. They all discovered that extended buffer intervals increased vaccination efficacy.
To sum up, single-dose bivalent HPV vaccinations showed limited effectiveness in reducing cervical abnormalities compared to three-dose ones; single-dose quadrivalent HPV vaccines demonstrated varying efficacy in preventing cervical abnormalities, while two and three doses of vaccination generally provided more consistent protection (Figure 5, Figure 6, Figure 7 and Figure 8). Better effectiveness of bivalent and quadrivalent HPV vaccines could be found in studies with longer buffer periods.
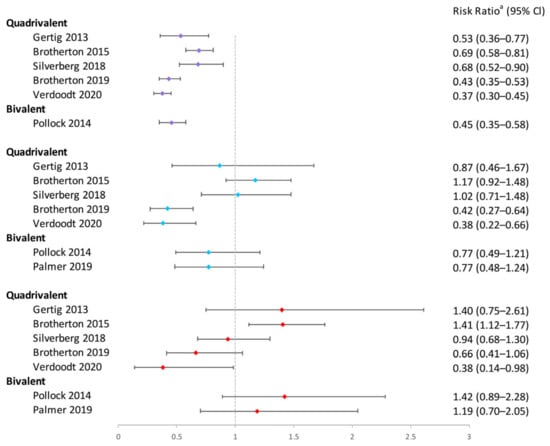
Figure 5.
Effectiveness of varying doses of bivalent and quadrivalent HPV vaccines in protecting women against CIN3+ [11,14,18,34,37,38,46]. Purple square: 3 doses vs. 0 dose; blue square: 2 doses vs. 0 dose; red square: 1 dose vs. 0 dose. a The risk ratio encompasses various measures depending on the study, including hazard ratio, risk ratio, incidence rate ratio, or odds ratio. The risk ratio in the figure was extracted directly from the original articles. If the original articles did not include available data for all age groups, they were excluded from this figure.
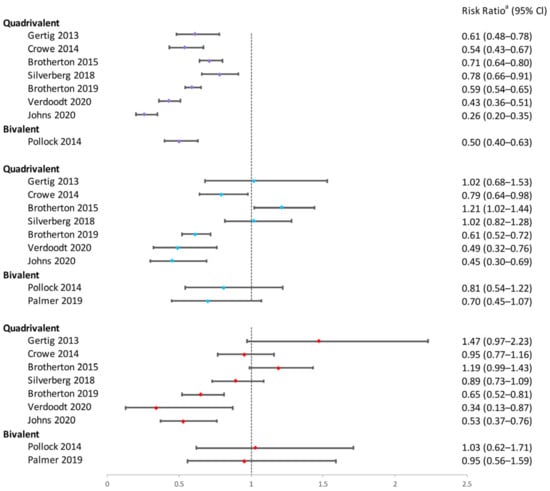
Figure 6.
Effectiveness of varying doses of bivalent and quadrivalent HPV vaccines in protecting women against CIN2+. Purple square: 3 doses vs. 0 dose; blue square: 2 doses vs. 0 dose; red square: 1 dose vs. 0 dose [11,14,15,18,34,37,38,42,46]. a The risk ratio encompasses various measures depending on the study, including hazard ratio, odds ratio, risk ratio, or incidence rate ratio. The risk ratio in the figure was extracted directly from the original articles. If the original articles did not include available data for all age groups, they were excluded from this figure.
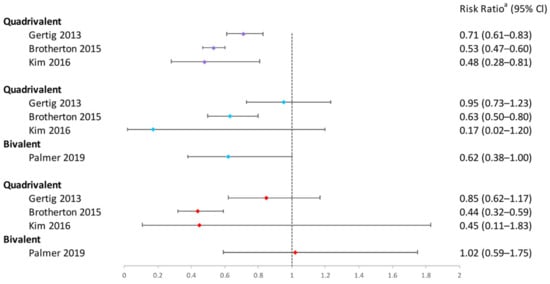
Figure 7.
Effectiveness of varying doses of bivalent and quadrivalent HPV vaccines in protecting women against cytological high-grade abnormalities [11,14,24,38]. Purple square: 3 doses vs. 0 dose; blue square: 2 doses vs. 0 dose; red square: 1 dose vs. 0 dose. a The risk ratio encompasses various measures depending on the study, including hazard ratio or odds ratio. The risk ratio in the figure was extracted directly from the original articles. If the original articles did not include available data for all age groups, they were excluded from this figure.
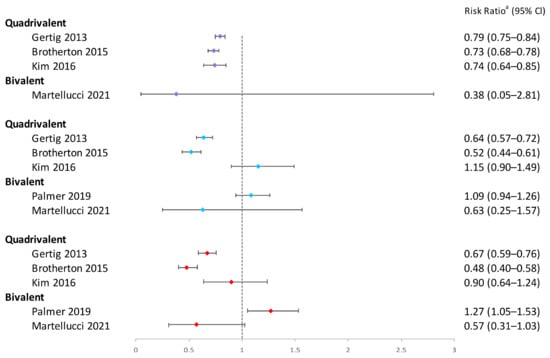
Figure 8.
Effectiveness of varying doses of bivalent and quadrivalent HPV vaccines in protecting women against cytological low-grade abnormalities [11,14,24,38,47]. Purple square: 3 doses vs. 0 dose; blue square: 2 doses vs. 0 dose; red square: 1 dose vs. 0 dose. a The risk ratio encompasses various measures depending on the study, including hazard ratio or odds ratio. The risk ratio in the figure was extracted directly from the original articles. If the original articles did not include available data for all age groups, they were excluded from this figure.
3.5. Genital Warts in Women and Men
Ten studies examined the association between a one-dose quadrivalent HPV vaccination and the first occurrence of condyloma [16,19,20,28,29,31,35,36,48,53]. Eight studies indicated the greatest reduction in condyloma risk with three doses and the least with one dose [16,19,20,28,29,31,35,48]. Notably, the outcomes of a retrospective cohort study involving young pregnant women and a follow-up of a duration of 6–11 years contradicted the previously mentioned research findings [53]. However, the 95% confidence intervals for the aPR crossed the null value because of the limited case numbers.
The vaccine effectiveness was analyzed with various age groups in four studies [16,35,36,48]. Three studies demonstrated that younger age groups had lower genital wart rates [16,36,48,54]. It is noteworthy that Zeybek et al. found similar effectiveness for one, two, and three doses in preventing genital warts among 15–19-year-olds, but weaker effectiveness for those under 15, and no reduction in warts for women aged ≥ 20 [36].
The vaccine effectiveness was analyzed with different buffer periods only in Hariri et al.‘s study. According to their sensitivity analysis, longer buffer durations for all dose groups were associated with higher vaccine effectiveness [31].
To sum up, when compared to two or three doses, the single-dose quadrivalent HPV vaccination is less efficient at preventing genital warts (Figure 9). Longer buffer times and lower age could help increase the efficacy of the quadrivalent HPV vaccine. In addition, there was just one trial that examined the prevention of genital warts with a bivalent HPV vaccine, and the findings indicated that there was no protection against the disease, regardless of the dosage administered [28].
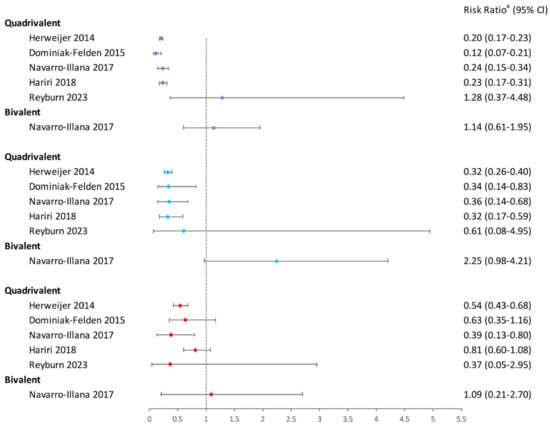
Figure 9.
Effectiveness of varying doses of bivalent and quadrivalent HPV vaccines in preventing women against genital warts [16,20,28,31,53]. Purple square: 3 doses vs. 0 dose; blue square: 2 doses vs. 0 dose; red square: 1 dose vs. 0 dose. a The risk ratio encompasses various measures depending on the study, including incidence rate ratio, risk ratio, hazard ratio, or prevalence ratio. The risk ratio in the figure was extracted directly from the original articles. If the original articles did not include available data for all age groups, they were excluded from this figure.
4. Discussion
Public health policies prioritize enhancing the effectiveness of vaccination, maximizing coverage in target populations, addressing vaccine supply shortages, and facilitating cost-effective vaccine delivery [54]. Administering a single dose of the HPV vaccine offers significant advantages over the traditional three-dose regimen, including potentially higher uptake, fewer side effects, better cost-effectiveness, and more simplified logistics. It is crucial to have robust and quantitative data on the efficacy of a single-dose HPV vaccination. Our review provided robust evidence suggesting that one, two, or three doses of quadrivalent and nonavalent HPV vaccinations offered similar protective effectiveness against vaccine-type HPV infection. One dose of a bivalent vaccination could prevent HPV16/18 infections, although some studies indicated it was less effective than two or three doses. There was ongoing debate regarding the prevention of cervical abnormalities with one-dose bivalent or quadrivalent vaccinations. Additionally, two or three doses of a quadrivalent vaccination were more beneficial than one dose for preventing genital warts. Notably, the efficacy of the HPV vaccine declined with increasing age and extending the buffer period.
HPV16 and HPV18 are the most prevalent types found in cervical cancer patients, accounting for approximately 71% of cervical cancer worldwide [55]. There was continuous discussion regarding the HPV16/18 infection rate among participants receiving one, two, or three doses of the HPV vaccine. A review of clinical trials specifically designed to randomize participants to receive a single dose of the HPV vaccine found no significant difference in HPV16/18 infection rates between the one-, two-, and three-dose groups [9]. However, a meta-analysis concluded that the risk of HPV16/18 infection was slightly higher in the one-dose group compared to those receiving multiple doses [11]. Based on a more thorough literature analysis, we found that a single dosage of quadrivalent and nonavalent vaccinations was just as efficient at preventing HPV16/18 infection as two and three doses. Further research is needed to evaluate the efficacy of a single dose of bivalent vaccination.
In addition to HPV16 and HPV18, quadrivalent and nonavalent vaccines target HPV6 and HPV11, which cause over 90% of genital warts [56]. Similar to two and three doses, single doses of both 4-valent and 9-valent vaccines could effectively prevent HPV 6 and 11 infections. Nonavalent vaccines also target hrHPV 31, 33, 45, 52, and 58, which are responsible for up to 90% of additional cervical cancer globally [55,57]. Our findings suggest that the efficacy of bivalent or quadrivalent vaccines in preventing hrHPV infections was limited, regardless of the dosage, while a single dose of nonavalent vaccination could offer similar protection against HPV16/18/31/33/45/52/58 as two and three doses. This evidence underscored the importance of the 9-valent HPV vaccine in mitigating hrHPV infection [58,59].
Invasive cervical cancer, preceded by a long phase of precancerous lesions, is a leading cause of cancer-related deaths among women in LMIC [60]. Without treatment, more than 20% of CIN2/3 lesions progress to carcinoma in situ or cancer [61]. A meta-analysis found that a one-dose HPV vaccination had a similar impact on preventing HSIL, ASC-H, or CIN2/3 as multiple doses, although study heterogeneity was high [11]. However, a review summarized that only some recently published studies had reported that effectiveness with three, two and one doses was similar [8]. Our review found variability in bivalent and quadrivalent vaccines’ roles in preventing CIN3+, CIN2+, HG, and LG lesions across studies. Furthermore, while a single dose of quadrivalent vaccination could prevent genital warts, its effectiveness was weaker than that of two or three doses. These results highlight the requirement for more doses.
Current evidence indicates that vaccinating younger individuals is more effective. This is because younger participants are more likely to be sexually inactive, reducing the likelihood of pre-existing HPV infections at the time of vaccination, and the immune response to the HPV vaccine is robust in HPV-naive cohorts [62]. In several studies [30,45,48], women vaccinated at age ≥ 19 or 20 showed no significant difference in the risk of histologically confirmed HG lesions compared to unvaccinated women, likely due to pre-vaccination exposure to hrHPV. However, in some studies [11,15,36,45], for girls vaccinated before age 16, there was no significant difference in the risk of cytologically or histologically cervical abnormalities compared to unvaccinated girls, possibly due to the lack of ability to study this outcome in such a young group where events were rare.
Our research and previous studies indicated that the effectiveness of HPV vaccination increased with longer buffer periods. The possible reason is that partially vaccinated women were often older than fully vaccinated women, making them more likely to have pre-vaccination HPV infections [24,45,46]. Many studies lacked baseline information on HPV DNA status, HPV serology, or sensitive indicators of previous HPV exposure [14,15,20,24,28,29,30,31,35,36,46,48], potentially causing the effectiveness of one- and two-dose vaccinations to be underestimated. Buffer periods, which delay case counting, help address this issue by increasing the likelihood that detected outcomes are due to post-vaccination infections.
Our study is distinguished from prior reviews by incorporating all eligible studies on single-dose HPV vaccinations, exploring the effectiveness of bivalent, quadrivalent, and nonavalent vaccines, and analyzing various clinical outcomes, including cervical and oral vaccine-type HPV infections, non-vaccine-type hrHPV infections, both cytological and histological cervical abnormalities, as well as genital warts.
Several factors might contribute to any remaining inconsistency in our analysis: (1) Some studies that used information from commercial claim databases and population-based health registries might have incorrectly classified people’s vaccination statuses and baseline characteristics if they received care for a disease outside of their insurance or health plan, or if they did not take part in disease screening and treatment. (2) Many studies did not have accurate data regarding sexual behavior and baseline HPV infection status. (3) Regarding unmeasured or missing characteristics, women may have varied among research and groups (i.e., with respect to risk behaviors or smoking status). (4) The variability in the design, implementation, and reporting quality of the included studies may introduce study quality bias, leading to systematic errors. (5) Some non-English articles may not be published in the searched databases, leading to language bias in the review.
However, our analysis has inherent limitations: (1) Due to the limited number of studies on nonavalent vaccines, we could not fully analyze the clinical efficacy of a single dose of the 9-valent vaccine. (2) Many studies lacked data on comorbidities in the study populations prior to vaccination, preventing an analysis of the vaccine effectiveness on specific populations at higher risk of HPV infection and precancerous lesions, such as HIV patients, cancer patients, and organ transplant recipients [63]. (3) Few studies investigated the protective effectiveness of the HPV vaccine against oral HPV infections, male genital HPV infections, and male genital warts, limiting our ability to thoroughly explore the vaccine effectiveness.
Consequently, more pragmatic studies with rigorous designs are warranted to ascertain the single-dose cost-effectiveness of HPV vaccines. Several key considerations merit attention: (1) To ensure accurate assessment of single-dose HPV vaccines’ effectiveness in different populations, researchers should transparently document and report detailed baseline information, such as HPV DNA status, HPV serology, sexual history, smoking status, and comorbidities. In addition, they can use multivariable analysis to account for potential differences among study populations and use multiple imputation to reduce the impact of missing data on study results. (2) Design studies specifically targeting nonavalent vaccines and high-risk populations (such as HIV patients, cancer patients, and organ transplant recipients). (3) Conduct longitudinal studies to track the effectiveness of single-dose HPV vaccines on multiple clinical outcomes in men and women, and report outcomes according to age subgroup. (4) To enhance the quality of study design, implementation, and reporting, as well as to lower the risk of systematic mistakes, adopt internationally recognized standards and guidelines, such as Strengthening the Reporting of Observational studies in Epidemiology and Consolidated Standards of Reporting Trials.
5. Conclusions
In summary, by incorporating a wide range of studies with robust evidence, our review supports the hypothesis that a single dose of quadrivalent and nonavalent HPV vaccines may be as effective as two or three doses in preventing vaccine-type HPV infections. However, the effectiveness of single-dose quadrivalent vaccination in preventing genital warts is weaker compared to two or three doses. To optimize the effectiveness of the HPV vaccine, it is advised to be given it at a younger age.
Further rigorous studies are needed to provide reliable evidence for single-dose HPV vaccination policies and guidelines. These studies should transparently document baseline information, conduct longitudinal tracking of the effectiveness of HPV vaccines on various clinical outcomes across different age groups, and appropriately use buffer intervals to mitigate bias while assessing vaccine effectiveness. Such research is essential to better understand the relationship between the number of vaccine doses and cross-protection against HPV, cervical cancer risk, and other clinical outcomes.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/vaccines12090956/s1, Table S1: search strategy in different databases; Table S2: clinical effectiveness of bivalent HPV vaccine by number of doses; Table S3: clinical effectiveness of quadrivalent HPV vaccine by number of doses; Table S4: clinical effectiveness of nonavalent HPV vaccine by number of doses.
Author Contributions
Conceptualization, W.B., X.H., Y.H., R.L., and Z.L.; investigation, W.B., X.H., Y.H., and R.L; writing—original draft, W.B., X.H., Y.H., and R.L.; formal analysis, W.B., X.H., Y.H., R.L., and Z.L.; writing—review and editing, W.B., X.H., Y.H., R.L., and Z.L.; funding acquisition, Z.L. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by the Medical Science and Technology Project of Sichuan Provincial Health Commission (grant number 2023NSFSC0743).
Institutional Review Board Statement
This article does not contain any studies with human participants performed by the author. All research was conducted in an ethical and responsible manner.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data are available in the articles included in this review.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Villa, L.L.; Richtmann, R. HPV vaccination programs in LMIC: Is it time to optimize schedules and recommendations? J. Pediatr. (Rio J.) 2023, 99 (Suppl. S1), S57–S61. [Google Scholar] [CrossRef]
- Kamolratanakul, S.; Pitisuttithum, P. Human Papillomavirus Vaccine Efficacy and Effectiveness against Cancer. Vaccines 2021, 9, 1413. [Google Scholar] [CrossRef]
- Cutts, F.T.; Franceschi, S.; Goldie, S.; Castellsague, X.; de Sanjose, S.; Garnett, G.; Edmunds, W.J.; Claeys, P.; Goldenthal, K.L.; Harper, D.M.; et al. Human papillomavirus and HPV vaccines: A review. Bull. World Health Organ. 2007, 85, 719–726. [Google Scholar] [CrossRef]
- Pinto, L.A.; Dillner, J.; Beddows, S.; Unger, E.R. Immunogenicity of HPV prophylactic vaccines: Serology assays and their use in HPV vaccine evaluation and development. Vaccine 2018, 36 Pt A, 4792–4799. [Google Scholar] [CrossRef]
- Larkin, H.D. Studies Find Single Dose of HPV Vaccines May Be Effective. JAMA 2022, 328, 1896. [Google Scholar] [CrossRef]
- Randall, T.C.; Ghebre, R. Challenges in Prevention and Care Delivery for Women with Cervical Cancer in Sub-Saharan Africa. Front. Oncol. 2016, 6, 160. [Google Scholar] [CrossRef]
- Donken, R.; Bogaards, J.A.; van der Klis, F.R.M.; Meijer, C.J.L.M.; de Melker, H.E. An exploration of individual- and population-level impact of the 2-dose HPV vaccination schedule in pre-adolescent girls. Hum. Vaccin. Immunother. 2016, 12, 1381–1393. [Google Scholar] [CrossRef][Green Version]
- Markowitz, L.E.; Drolet, M.; Lewis, R.M.; Lemieux-Mellouki, P.; Pérez, N.; Jit, M.; Brotherton, J.M.; Ogilvie, G.; Kreimer, A.R.; Brisson, M. Human papillomavirus vaccine effectiveness by number of doses: Updated systematic review of data from national immunization programs. Vaccine 2022, 40, 5413–5432. [Google Scholar] [CrossRef]
- Whitworth, H.S.; Gallagher, K.E.; Howard, N.; Mounier-Jack, S.; Mbwanji, G.; Kreimer, A.R.; Basu, P.; Kelly, H.; Drolet, M.; Brisson, M.; et al. Efficacy and immunogenicity of a single dose of human papillomavirus vaccine compared to no vaccination or standard three and two-dose vaccination regimens: A systematic review of evidence from clinical trials. Vaccine 2020, 38, 1302–1314. [Google Scholar] [CrossRef]
- Quang, C.; Chung, A.W.; Frazer, I.H.; Toh, Z.Q.; Licciardi, P.V. Single-dose HPV vaccine immunity: Is there a role for non-neutralizing antibodies? Trends Immunol. 2022, 43, 815–825. [Google Scholar] [CrossRef] [PubMed]
- Brotherton, J.M.; Malloy, M.; Budd, A.C.; Saville, M.; Drennan, K.T.; Gertig, D.M. Effectiveness of less than three doses of quadrivalent human papillomavirus vaccine against cervical intraepithelial neoplasia when administered using a standard dose spacing schedule: Observational cohort of young women in Australia. Papillomavirus Res. 2015, 1, 59–73. [Google Scholar] [CrossRef]
- You, T.; Zhao, X.; Hu, S.; Gao, M.; Liu, Y.; Zhang, Y.; Qiao, Y.; Jit, M.; Zhao, F. Optimal allocation strategies for HPV vaccination introduction and expansion in China accommodated to different supply and dose schedule scenarios: A modelling study. EClinicalMedicine 2023, 56, 101789. [Google Scholar] [CrossRef]
- Kreimer, A.R.; Rodriguez, A.C.; Hildesheim, A.; Herrero, R.; Porras, C.; Schiffman, M.; González, P.; Solomon, D.; Jiménez, S.; Schiller, J.T.; et al. Proof-of-principle evaluation of the efficacy of fewer than three doses of a bivalent HPV16/18 vaccine. J. Natl. Cancer Inst. 2011, 103, 1444–1451. [Google Scholar] [CrossRef]
- Gertig, D.M.; Brotherton, J.M.; Budd, A.C.; Drennan, K.; Chappell, G.; Saville, A.M. Impact of a population-based HPV vaccination program on cervical abnormalities: A data linkage study. BMC Med. 2013, 11, 227. [Google Scholar] [CrossRef]
- Crowe, E.; Pandeya, N.; Brotherton, J.M.L.; Dobson, A.J.; Kisely, S.; Lambert, S.B.; Whiteman, D.C. Effectiveness of quadrivalent human papillomavirus vaccine for the prevention of cervical abnormalities: Case-control study nested within a population based screening programme in Australia. BMJ 2014, 348, g1458. [Google Scholar] [CrossRef]
- Herweijer, E.; Leval, A.; Ploner, A.; Eloranta, S.; Simard, J.F.; Dillner, J.; Netterlid, E.; Sparén, P.; Arnheim-Dahlström, L. Association of varying number of doses of quadrivalent human papillomavirus vaccine with incidence of condyloma. JAMA 2014, 311, 597–603. [Google Scholar] [CrossRef]
- Kavanagh, K.; Pollock, K.G.J.; Potts, A.; Love, J.; Cuschieri, K.; Cubie, H.; Robertson, C.; Donaghy, M. Introduction and sustained high coverage of the HPV bivalent vaccine leads to a reduction in prevalence of HPV 16/18 and closely related HPV types. Br. J. Cancer 2014, 110, 2804–2811. [Google Scholar] [CrossRef] [PubMed]
- Pollock, K.G.J.; Kavanagh, K.; Potts, A.; Love, J.; Cuschieri, K.; Cubie, H.; Robertson, C.; Cruickshank, M.; Palmer, T.J.; Nicoll, S.; et al. Reduction of low- and high-grade cervical abnormalities associated with high uptake of the HPV bivalent vaccine in Scotland. Br. J. Cancer 2014, 111, 1824–1830. [Google Scholar] [CrossRef]
- Blomberg, M.; Dehlendorff, C.; Sand, C.; Kjaer, S.K. Dose-Related Differences in Effectiveness of Human Papillomavirus Vaccination against Genital Warts: A Nationwide Study of 550,000 Young Girls. Clin. Infect. Dis. 2015, 61, 676–682. [Google Scholar] [CrossRef]
- Dominiak-Felden, G.; Gobbo, C.; Simondon, F. Evaluating the Early Benefit of Quadrivalent HPV Vaccine on Genital Warts in Belgium: A Cohort Study. PLoS ONE 2015, 10, e0132404. [Google Scholar] [CrossRef] [PubMed]
- Kreimer, A.R.; Struyf, F.; Del Rosario-Raymundo, M.R.; Hildesheim, A.; Skinner, S.R.; Wacholder, S.; Garland, S.M.; Herrero, R.; David, M.-P.; Wheeler, C.M. Efficacy of fewer than three doses of an HPV-16/18 AS04-adjuvanted vaccine: Combined analysis of data from the Costa Rica Vaccine and PATRICIA Trials. Lancet Oncol. 2015, 16, 775–786. [Google Scholar] [CrossRef]
- Cuschieri, K.; Kavanagh, K.; Moore, C.; Bhatia, R.; Love, J.; Pollock, K.G. Impact of partial bivalent HPV vaccination on vaccine-type infection: A population-based analysis. Br. J. Cancer 2016, 114, 1261–1264. [Google Scholar] [CrossRef]
- Hofstetter, A.M.; Ompad, D.C.; Stockwell, M.S.; Rosenthal, S.L.; Soren, K. Human Papillomavirus Vaccination and Cervical Cytology Outcomes Among Urban Low-Income Minority Females. JAMA Pediatr. 2016, 170, 445–452. [Google Scholar] [CrossRef]
- Kim, J.; Bell, C.; Sun, M.; Kliewer, G.; Xu, L.; McInerney, M.; Svenson, L.W.; Yang, H. Effect of human papillomavirus vaccination on cervical cancer screening in Alberta. CMAJ 2016, 188, E281–E288. [Google Scholar] [CrossRef]
- Sankaranarayanan, R.; Prabhu, P.R.; Pawlita, M.; Gheit, T.; Bhatla, N.; Muwonge, R.; Nene, B.M.; Esmy, P.O.; Joshi, S.; Poli, U.R.R.; et al. Immunogenicity and HPV infection after one, two, and three doses of quadrivalent HPV vaccine in girls in India: A multicentre prospective cohort study. Lancet Oncol. 2016, 17, 67–77. [Google Scholar] [CrossRef]
- Cameron, R.L.; Kavanagh, K.; Watt, D.C.; Robertson, C.; Cuschieri, K.; Ahmed, S.; Pollock, K.G. The impact of bivalent HPV vaccine on cervical intraepithelial neoplasia by deprivation in Scotland: Reducing the gap. J. Epidemiol. Community Health 2017, 71, 954–960. [Google Scholar] [CrossRef]
- Kavanagh, K.; Pollock, K.G.; Cuschieri, K.; Palmer, T.; Cameron, R.L.; Watt, C.; Bhatia, R.; Moore, C.; Cubie, H.; Cruickshank, M.; et al. Changes in the prevalence of human papillomavirus following a national bivalent human papillomavirus vaccination programme in Scotland: A 7-year cross-sectional study. Lancet Infect. Dis. 2017, 17, 1293–1302. [Google Scholar] [CrossRef]
- Navarro-Illana, E.; López-Lacort, M.; Navarro-Illana, P.; Vilata, J.J.; Diez-Domingo, J. Effectiveness of HPV vaccines against genital warts in women from Valencia, Spain. Vaccine 2017, 35, 3342–3346. [Google Scholar] [CrossRef]
- Perkins, R.B.; Lin, M.; Wallington, S.F.; Hanchate, A. Impact of Number of Human Papillomavirus Vaccine Doses on Genital Warts Diagnoses Among a National Cohort of U.S. Adolescents. Sex. Transm. Dis. 2017, 44, 365–370. [Google Scholar] [CrossRef]
- Dehlendorff, C.; Sparén, P.; Baldur-Felskov, B.; Herweijer, E.; Arnheim-Dahlström, L.; Ploner, A.; Uhnoo, I.; Kjaer, S.K. Effectiveness of varying number of doses and timing between doses of quadrivalent HPV vaccine against severe cervical lesions. Vaccine 2018, 36, 6373–6378. [Google Scholar] [CrossRef]
- Hariri, S.; Schuler, M.S.; Naleway, A.L.; Daley, M.F.; Weinmann, S.; Crane, B.; Newcomer, S.R.; Tolsma, D.; Markowitz, L.E. Human Papillomavirus Vaccine Effectiveness Against Incident Genital Warts Among Female Health-Plan Enrollees, United States. Am. J. Epidemiol. 2018, 187, 298–305. [Google Scholar] [CrossRef]
- Safaeian, M.; Sampson, J.N.; Pan, Y.; Porras, C.; Kemp, T.J.; Herrero, R.; Quint, W.; van Doorn, L.J.; Schussler, J.; Lowy, D.R.; et al. Durability of Protection Afforded by Fewer Doses of the HPV16/18 Vaccine: The CVT Trial. J. Natl. Cancer Inst. 2018, 110, 205–212. [Google Scholar] [CrossRef]
- Sankaranarayanan, R.; Joshi, S.; Muwonge, R.; Esmy, P.O.; Basu, P.; Prabhu, P.; Bhatla, N.; Nene, B.M.; Shaw, J.; Poli, U.R.R.; et al. Can a single dose of human papillomavirus (HPV) vaccine prevent cervical cancer? Early findings from an Indian study. Vaccine 2018, 36 Pt A, 4783–4791. [Google Scholar] [CrossRef]
- Silverberg, M.J.; Leyden, W.A.; Lam, J.O.; Gregorich, S.E.; Huchko, M.J.; Kulasingam, S.; Kuppermann, M.; Smith-McCune, K.K.; Sawaya, G.F. Effectiveness of catch-up human papillomavirus vaccination on incident cervical neoplasia in a US health-care setting: A population-based case-control study. Lancet Child. Adolesc. Health 2018, 2, 707–714. [Google Scholar] [CrossRef]
- Willows, K.M.; Bozat-Emre, S.; Righolt, C.H.; Kliewer, E.V.; Mahmud, S.M.M. Early Evidence of the Effectiveness of the Human Papillomavirus Vaccination Program Against Anogenital Warts in Manitoba, Canada: A Registry Cohort Study. Sex. Transm. Dis. 2018, 45, 254–259. [Google Scholar] [CrossRef]
- Zeybek, B.; Lin, Y.-L.; Kuo, Y.-F.; Rodriguez, A.M. The Impact of Varying Numbers of Quadrivalent Human Papillomavirus Vaccine Doses on Anogenital Warts in the United States: A Database Study. J. Low. Genit. Tract. Dis. 2018, 22, 189–194. [Google Scholar] [CrossRef]
- Brotherton, J.M.; Budd, A.; Rompotis, C.; Bartlett, N.; Malloy, M.J.; Andersen, R.L.; Coulter, K.A.; Couvee, P.W.; Steel, N.; Ward, G.H.; et al. Is one dose of human papillomavirus vaccine as effective as three?: A national cohort analysis. Papillomavirus Res. 2019, 8, 100177. [Google Scholar] [CrossRef]
- Palmer, T.; Wallace, L.; Pollock, K.G.; Cuschieri, K.; Robertson, C.; Kavanagh, K.; Cruickshank, M. Prevalence of cervical disease at age 20 after immunisation with bivalent HPV vaccine at age 12–13 in Scotland: Retrospective population study. BMJ 2019, 365, l1161. [Google Scholar] [CrossRef]
- Sonawane, K.; Nyitray, A.G.; Nemutlu, G.S.; Swartz, M.D.; Chhatwal, J.; Deshmukh, A.A. Prevalence of Human Papillomavirus Infection by Number of Vaccine Doses Among US Women. JAMA Netw. Open 2019, 2, e1918571. [Google Scholar] [CrossRef] [PubMed]
- Widdice, L.E.; Bernstein, D.I.; Franco, E.L.; Ding, L.; Brown, D.R.; Ermel, A.C.; Higgins, L.; Kahn, J.A. Decline in vaccine-type human papillomavirus prevalence in young men from a Midwest metropolitan area of the United States over the six years after vaccine introduction. Vaccine 2019, 37, 6832–6841. [Google Scholar] [CrossRef]
- Batmunkh, T.; Dalmau, M.T.; Munkhsaikhan, M.-E.; Khorolsuren, T.; Namjil, N.; Surenjav, U.; Toh, Z.Q.; Licciardi, P.V.; Russell, F.M.; Garland, S.M.; et al. A single dose of quadrivalent human papillomavirus (HPV) vaccine is immunogenic and reduces HPV detection rates in young women in Mongolia, six years after vaccination. Vaccine 2020, 38, 4316–4324. [Google Scholar] [CrossRef]
- Jones, M.L.J.; Gargano, J.W.; Powell, M.; Park, I.U.; Niccolai, L.M.; Bennett, N.M.; Griffin, M.R.; Querec, T.; Unger, E.R.; Markowitz, L.E.; et al. Effectiveness of 1, 2, and 3 Doses of Human Papillomavirus Vaccine Against High-Grade Cervical Lesions Positive for Human Papillomavirus 16 or 18. Am. J. Epidemiol. 2020, 189, 265–276. [Google Scholar] [CrossRef] [PubMed]
- Kreimer, A.R.; Sampson, J.N.; Porras, C.; Schiller, J.T.; Kemp, T.; Herrero, R.; Wagner, S.; Boland, J.; Schussler, J.; Lowy, D.R.; et al. Evaluation of Durability of a Single Dose of the Bivalent HPV Vaccine: The CVT Trial. J. Natl. Cancer Inst. 2020, 112, 1038–1046. [Google Scholar] [CrossRef]
- Markowitz, L.E.; Naleway, A.L.; Klein, N.P.; Lewis, R.M.; Crane, B.; Querec, T.D.; Hsiao, A.; Aukes, L.; Timbol, J.; Weinmann, S.; et al. Human Papillomavirus Vaccine Effectiveness Against HPV Infection: Evaluation of One, Two, and Three Doses. J. Infect. Dis. 2020, 221, 910–918. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, A.M.; Zeybek, B.; Vaughn, M.; Westra, J.; Kaul, S.; Montealegre, J.R.; Lin, Y.; Kuo, Y. Comparison of the long-term impact and clinical outcomes of fewer doses and standard doses of human papillomavirus vaccine in the United States: A database study. Cancer 2020, 126, 1656–1667. [Google Scholar] [CrossRef]
- Verdoodt, F.; Dehlendorff, C.; Kjaer, S.K. Dose-related Effectiveness of Quadrivalent Human Papillomavirus Vaccine against Cervical Intraepithelial Neoplasia: A Danish Nationwide Cohort Study. Clin. Infect. Dis. 2020, 70, 608–614. [Google Scholar] [CrossRef]
- Martellucci, C.A.; Nomura, S.; Yoneoka, D.; Ueda, P.; Brotherton, J.; Canfell, K.; Palmer, M.; Manzoli, L.; Rossi, P.G.; De Togni, A.; et al. Human papillomavirus vaccine effectiveness within a cervical cancer screening programme: Cohort study. BJOG Int. J. Obstet. Gynaecol. 2021, 128, 532–539. [Google Scholar] [CrossRef]
- Baandrup, L.; Dehlendorff, C.; Kjaer, S.K. One-Dose Human Papillomavirus Vaccination and the Risk of Genital Warts: A Danish Nationwide Population-based Study. Clin. Infect. Dis. 2021, 73, e3220–e3226. [Google Scholar] [CrossRef] [PubMed]
- Basu, P.; Malvi, S.G.; Joshi, S.; Bhatla, N.; Muwonge, R.; Lucas, E.; Verma, Y.; Esmy, P.O.; Poli, U.R.R.; Shah, A.; et al. Vaccine efficacy against persistent human papillomavirus (HPV) 16/18 infection at 10 years after one, two, and three doses of quadrivalent HPV vaccine in girls in India: A multicentre, prospective, cohort study. Lancet Oncol. 2021, 22, 1518–1529. [Google Scholar] [CrossRef]
- Barnabas, R.V.; Brown, E.R.; Onono, M.A.; Bukusi, E.A.; Njoroge, B.; Winer, R.L.; Galloway, D.A.; Pinder, L.F.; Donnell, D.; Wakhungu, I.; et al. Efficacy of single-dose HPV vaccination among young African women. NEJM Evid. 2022, 1, EVIDoa2100056. [Google Scholar] [CrossRef]
- Barnabas, R.V.; Brown, E.R.; Onono, M.A.; Bukusi, E.A.; Njoroge, B.; Winer, R.L.; Galloway, D.A.; Pinder, L.F.; Donnell, D.; Wakhungu, I.N.; et al. Durability of single-dose HPV vaccination in young Kenyan women: Randomized controlled trial 3-year results. Nat. Med. 2023, 29, 3224–3232. [Google Scholar] [CrossRef]
- Gheit, T.; Muwonge, R.; Lucas, E.; Galati, L.; Anantharaman, D.; McKay-Chopin, S.; Malvi, S.G.; Jayant, K.; Joshi, S.; Esmy, P.O.; et al. Impact of HPV vaccination on HPV-related oral infections. Oral. Oncol. 2023, 136, 106244. [Google Scholar] [CrossRef]
- Reyburn, R.; Tuivaga, E.; Ratu, T.; Young, S.; Garland, S.M.; Murray, G.; Cornall, A.; Tabrizi, S.; Nguyen, C.D.; Jenkins, K.; et al. A single dose of quadrivalent HPV vaccine is highly effective against HPV genotypes 16 and 18 detection in young pregnant women eight years following vaccination: An retrospective cohort study in Fiji. Lancet Reg. Health West. Pac. 2023, 37, 100798. [Google Scholar] [CrossRef]
- Kamani, M.O.; Kyrgiou, M.; Joura, E.; Zapardiel, I.; Grigore, M.; Arbyn, M.; Preti, M.; Planchamp, F.; Gultekin, M. ESGO Prevention Committee opinion: Is a single dose of HPV vaccine good enough? Int. J. Gynecol. Cancer 2023, 33, 462–464. [Google Scholar] [CrossRef]
- Serrano, B.; Alemany, L.; Tous, S.; Bruni, L.; Clifford, G.M.; Weiss, T.; Bosch, F.X.; de Sanjosé, S. Potential impact of a nine-valent vaccine in human papillomavirus related cervical disease. Infect. Agent. Cancer 2012, 7, 38. [Google Scholar] [CrossRef]
- Baandrup, L.; Blomberg, M.; Dehlendorff, C.M.; Sand, C.M.; Andersen, K.K.M.; Kjaer, S.K.M. Significant decrease in the incidence of genital warts in young Danish women after implementation of a national human papillomavirus vaccination program. Sex. Transm. Dis. 2013, 40, 130–135. [Google Scholar] [CrossRef] [PubMed]
- de Sanjose, S.; Quint, W.G.V.; Alemany, L.; Geraets, D.T.; Klaustermeier, J.E.; Lloveras, B.; Tous, S.; Felix, A.; Bravo, L.E.; Shin, H.-R.; et al. Human papillomavirus genotype attribution in invasive cervical cancer: A retrospective cross-sectional worldwide study. Lancet Oncol. 2010, 11, 1048–1056. [Google Scholar] [CrossRef]
- Sangwa-Lugoma, G.; Ramanakumar, A.V.; Mahmud, S.; Liaras, J.; Kayembe, P.K.; Tozin, R.R.; Lorincz, A.; Franco, E.L. Prevalence and determinants of high-risk human papillomavirus infection in women from a sub-Saharan African community. Sex. Transm. Dis. 2011, 38, 308–315. [Google Scholar] [CrossRef]
- FRIDA Study Group; Rudolph, S.E.; Lorincz, A.; Wheeler, C.M.; Gravitt, P.; Lazcano-Ponce, E.; Torres-Ibarra, L.; León-Maldonado, L.; Ramírez, P.; Rivera, B.; et al. Population-based prevalence of cervical infection with human papillomavirus genotypes 16 and 18 and other high risk types in Tlaxcala, Mexico. BMC Infect. Dis. 2016, 16, 461. [Google Scholar] [CrossRef]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Syrjänen, K.J. Spontaneous evolution of intraepithelial lesions according to the grade and type of the implicated human papillomavirus (HPV). Eur. J. Obstet. Gynecol. Reprod. Biol. 1996, 65, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Mariani, L.; Venuti, A. HPV vaccine: An overview of immune response, clinical protection, and new approaches for the future. J. Transl. Med. 2010, 8, 105. [Google Scholar] [CrossRef]
- Ellerbrock, T.V.; Chiasson, M.A.; Bush, T.J.; Sun, X.-W.; Sawo, D.; Brudney, K.; Wright, J.T.C. Incidence of cervical squamous intraepithelial lesions in HIV-infected women. JAMA 2000, 283, 1031–1037. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).