Abstract
High-density lipoprotein (HDL) metabolism depends on several key factors, including ATP-binding cassette (ABC) transporters such as ABCA1 and ABCG1. These transporters are essential for maintaining cholesterol homeostasis by mediating the efflux of cellular lipids and promoting HDL formation and maturation. Dysfunction in these pathways compromises HDL biogenesis, leading to lipid accumulation in macrophages and peripheral cells. Together with oxidized low-density lipoproteins (LDLs), these alterations promote foam cell formation, atherosclerotic plaque development, and the progression of cardiovascular and metabolic diseases. Oxidative stress plays a central role in disturbing lipid balance and impairing ABC transporter activity. Unlike previous reviews that have mainly summarized mechanisms of oxidative regulation, this work integrates recent molecular findings to propose a unifying framework in which oxidative stress sequentially disrupts ABCA1 and ABCG1 function, thereby altering HDL metabolism. Moreover, it highlights emerging pharmacological strategies aimed at restoring cholesterol homeostasis and mitigating oxidative damage, contributing to the prevention of cardiovascular and metabolic disorders.
1. Introduction
Lipids constitute one of the principal structural and functional components of living organisms. Beyond being a fundamental source of metabolic energy, they play essential roles in cell membrane architecture, molecular signaling, and the regulation of energy metabolism [1,2,3]. Under physiological conditions, the balance between lipid synthesis, transport, and degradation is essential to maintaining metabolic homeostasis and preventing the onset of chronic diseases. However, this delicate equilibrium can be disrupted by several factors, among which oxidative stress stands out, as it compromises both the structural integrity of lipids and their metabolic regulation [4,5,6,7].
Lipid transport is mediated by lipoproteins that enable hydrophobic molecules, such as triacylglycerols and cholesterol, to circulate in the aqueous environment of plasma [8,9]. These lipoproteins, chylomicrons (CMs), very-low-density lipoproteins (VLDLs), low-density lipoproteins (LDLs), and high-density lipoproteins (HDLs), ensure the proper delivery of lipids to peripheral tissues and the clearance of excess cholesterol to the liver through the process known as reverse cholesterol transport (RCT) [10,11,12,13,14,15,16,17]. Apolipoproteins, including ApoA-I, ApoB-100, and ApoE, are essential structural and functional components of lipoproteins [18,19]. They facilitate lipid binding, mediate recognition by cellular receptors, and modulate the activity of enzymes involved in lipoprotein metabolism, thereby ensuring efficient lipid transport and metabolic regulation [12,20,21]. Among these lipoproteins, HDL particles play a particularly protective role by facilitating cholesterol efflux from peripheral cells, thereby preventing foam cell formation and the progression of atherosclerosis [22,23,24,25,26].
Lipoprotein metabolism involves a complex network of apolipoproteins, enzymes, and transporters that regulate lipid uptake, efflux, and transformation at the cellular level [8,13]. There, the ATP-binding cassette (ABC) transporters, particularly ABCA1 and ABCG1, are crucial for mediating cholesterol efflux and phospholipid transfer to HDL particles, thereby enabling their formation and maturation [27,28]. Dysfunction of these transporters, whether caused by genetic variations or environmental factors, impairs RCT and promotes intracellular cholesterol accumulation, especially in macrophages, leading to foam cell formation and the development of cardiovascular diseases such as atherosclerosis [28,29], in which oxidative stress plays a central role. Oxidative stress is defined as an imbalance between the generation of reactive oxygen species (ROS) and the organism’s antioxidant defense systems [4,5]. Due to cellular metabolism, ROS are generated from different compartments such as mitochondria, peroxisomes, endoplasmic reticulum, cytosolic enzymatic systems, and exogenous factors [30].
Excessive ROS not only induce lipid peroxidation and structural cellular damage but also modify the ABCA1 and ABCG1 transporters, reducing their interaction with apolipoproteins and consequently their efficiency in mediating cholesterol efflux [31,32]. In this way, oxidative stress links lipid metabolism with inflammation and vascular dysfunction, representing a key pathogenic axis in the progression of metabolic and cardiovascular diseases [33,34,35,36,37,38].
A comprehensive understanding of the interplay between lipid metabolism, cholesterol transport, and the oxidative modulation of ABCA1 and ABCG1 transporters thus provides an essential framework for elucidating novel therapeutic strategies aimed at preventing and treating atherosclerosis and related metabolic disorders [28,29].
This article aims to explain the relationship between oxidative stress and lipid homeostasis, showing how ROS damage to the ABCA1 and ABCG1 transporters disrupt RCT, thereby contributing to the development and progression of atherosclerosis and other metabolic disorders. Furthermore, it discusses current and emerging therapeutic strategies focused on restoring lipid balance and preventing disease progression.
2. ABC Transporters
ABC transporters constitute one of the largest and most diverse protein superfamilies in living beings: they are essential for their role as primary active transporters [39]. They use the energy generated by ATP hydrolysis to move molecules across biological membranes, thus serving for the translocation of various substrates, including vitamins, steroids, lipids, ions, peptides, proteins, polysaccharides, and xenobiotics [40,41,42]. Currently, 48 ABC transporters have been identified in humans, which have been classified into 7 subfamilies: A, B, C, D, E, F, and G [40]. The importance of this protein family lies in its functional variety and its implications in various pathologies, including cystic fibrosis, cancer, adrenoleukodystrophy, retinal degeneration, and cholesterol transport defects [42,43,44].
In general, human ABC transporters are located at the plasma membrane and export substrates from the cytoplasm. However, some are in peroxisomes, lysosomes, photoreceptor discs, and mitochondria [45,46].
According to their structure, ABC transporters can be organized in two ways: as a complete transporter formed by a monomer, which is the case of ABCA1, or as a semi-transporter formed by dimers (homodimers or heterodimers), which is the case of ABCG1 [40,47,48]. These transporters possess ATP-binding and hydrolysis sites, known as nucleotide-binding domains (NBDs), and are highly conserved [49]. NBDs contain the consensus sequences Walker A (phosphate-binding) and Walker B (ATP-binding and hydrolysis) [47,50]. They also contain transmembrane domains (TMDs), each comprising several hydrophobic α-helices, which are involved in substrate recognition and translocation across the lipid membrane [51].
ABC transporters participate in numerous cellular processes such as the maintenance of osmotic homeostasis (ABCC7) [52], antigen processing (ABCB2/3) [39], cell proliferation (ABCC1, ABCG2, ABCB6) [44,53,54], the immune response (ABCB2/3) [55] and the efflux of cholesterol and lipids (ABCA1 and ABCG1) [56,57].
ABCA1 and ABCG1 act primarily as translocators of sterols and lipids from plasma membranes to lipoproteins, particularly HDLs [57]. They are ubiquitously expressed, although there is higher expression in some cells or tissues (Table 1) [40,58]. The function of these two transporters is vital, because they prevent the accumulation of lipids in macrophages, hepatocytes, enterocytes, endothelial cells and vascular smooth muscle cells [56,57,58,59,60,61,62,63]. ABCA1 is composed of 2261 amino acid residues that form six domains: two TMDs consisting of six transmembrane helices each; two NBDs in the cytoplasm, which serve to couple ATP hydrolysis to translocase activity, and two large extracellular domains (ECDs) that are involved in protein–protein interactions, essential for ApoA-I binding and regulatory functions (Figure 1) [59,64].
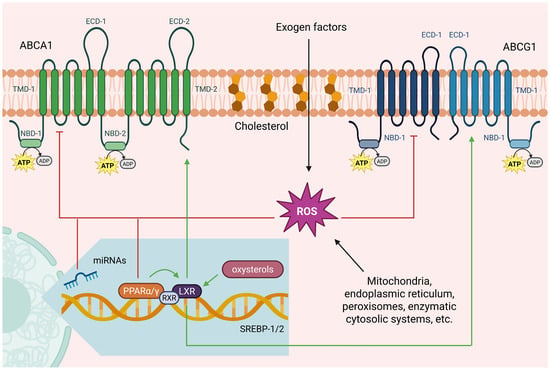
Figure 1.
Structure and regulation of ABCA1 and ABCG1. ABCA1 is a complete transporter composed of a single polypeptide containing two ATP-binding sites (NBDs), two transmembrane domains (TMDs) each with six α-helices, and two extracellular domains (ECDs) that are essential for ApoA-I binding. In contrast, ABCG1 is a semi-transporter that functions as a dimer. Each monomer consists of one NBD, one TMD, and one ECD. These transporters are finely regulated. Their function is inhibited by ROS produced through various intracellular and extracellular sources. While their expression is induced via nuclear hormone receptors such as the liver X receptor (LXR), the retinoid X receptor (RXR) and the peroxisome proliferator-activated receptors alpha and gamma (PPARα and PPARγ), and it is inhibited by microRNAs located in the intronic regions of genes encoding sterol regulatory element binding factors 1 and 2 (SREBF1 and SREBF2). Created in BioRender. Matuz Mares, D. (2025) https://BioRender.com/5kwwntp.
On the other hand, ABCG1 can be composed of 666 or 678 amino acids, depending on alternative splicing, leading to the formation of two isoforms: ABCG1 (−12) and ABCG1(+12), respectively [47]. It has only one NBD and a TMD with six transmembrane helices, which dimerize to form a functionally active transporter (Figure 1) [48].
Mutations in the abca1 gene have been reported to cause the autosomal recessive genetic disorder called Tangier disease [65], in which patients show very low serum HDL levels, increasing the risk of atherosclerosis (Table 1). No pathogenic alterations in the abcg1 gene have been identified in humans. Although in murine models, in which the abcg1 gene has been eliminated and they are fed with a diet high in fat and cholesterol, show accumulation of lipids in hepatocytes and macrophages [66]. In humans, alterations in the function of both transporters are related to the development of various diseases, as mentioned in Table 1.

Table 1.
Characteristics of ABCA1 and ABCG1 transporters.
Table 1.
Characteristics of ABCA1 and ABCG1 transporters.
| Transporter | ABCA1 | ABCG1 |
|---|---|---|
| Type of transporter | Full transporter [40,48] | Half transporter |
| Molecular Mass | 254 kDa [40] | 75.69 kDa [40] |
| Tissue expressed | Ubiquitous, highly expressed in hepatocytes, macrophages, and smooth muscle cells [67,68] | High expression levels in macrophages, lymphocytes, epithelial cells, endothelial cells, vascular smooth muscle cells, liver, and intestine, brain and placenta [60,62,69,70,71] |
| Cell localization | Plasma membrane, endosome, peroxisomes, mitochondria, endoplasmic reticulum, or lamellar bodies [40] | Plasma membrane, endosomes, peroxisomes, mitochondria, endoplasmic reticulum, Golgi apparatus, lamellar bodies and endocytic vesicles [40,72] |
| Function | HDL biogenesis, cholesterol efflux, insulin secretion, microvesicle formation in platelets, glucose uptake in skeletal muscle, apolipoprotein ApoE secretion, and lipidation in astrocytes [67] | Transport of cholesterol, phosphatidylcholine, sphingomyelin, oxysterol and participates in RCT [47,63,73] |
| Human Genetic disease | Tangier disease [65] | There are no reports [40] |
| Associated diseases | Dyslipidemia, atherosclerosis, inflammation, coronary heart disease, type 2 diabetes, thrombosis, neurological disorders, age-related macular degeneration, glaucoma, viral infections, and cancer progression [32,67,74,75] | Atherosclerosis, inflammation, Alzheimer’s disease (AD), type 2 diabetes, cancer, immune disorders, obesity, and age-related macular degeneration [47,60,63,71] |
The expression of these transporters is an activation cascade involving different elements. It begins with the activation of some nuclear hormone receptors, such as liver X receptor (LXR) and retinoid X receptor (RXR) [25,48,76], which in turn are activated by fatty acids and oxysterols. (Figure 1). Fatty acids positively stimulate peroxisome proliferator-activated receptors alpha and gamma (PPARα and PPARγ) [77,78], while oxysterols act directly on nuclear receptors LXR and RXR [79,80]. These same transporters are negatively regulated through microRNAs (miRNAs/miR) such as miR-33a and miR-33b [81], which are located in intronic regions of sterol regulatory element binding factor 1 and 2 (SREBF1 and SREBF2) genes, which control cholesterol synthesis [82]. Finally, at the post-translational level, both transporters are degraded by the calpain and proteasome pathways in macrophages [48,83,84].
3. HDL Metabolism
The HDL metabolism starts with the synthesis and secretion of ApoA-I by hepatocytes and enterocytes, the main structural apolipoprotein of HDL [22]. Free ApoA-I in plasma interacts specifically with the ABCA1 transporter on the membrane of peripheral cells, particularly macrophages and endothelial cells, initiating the assembly of HDL (Figure 2) [85]. ABCA1 utilizes the energy from ATP hydrolysis to translocate phospholipids (primarily phosphatidylcholine) and unesterified cholesterol from the cell membrane to ApoA-I, thereby generating small discoidal HDL particles known as pre-β1-HDL. Instead, ABCG1 facilitates the efflux of cholesterol and phospholipids to pre-β1-HDL, forming a bigger particle [19,48]. Seemingly, ABCG1 is more efficient in transferring lipids to pre-β1-HDL, whereas ABCA1 primarily loads lipids onto lipid-free ApoA-I [86]. This indicates that, unlike ABCA1, ABCG1 does not initiate HDL biogenesis de novo, but acts at a later stage of the HDL cycle, promoting their lipid enrichment [25].
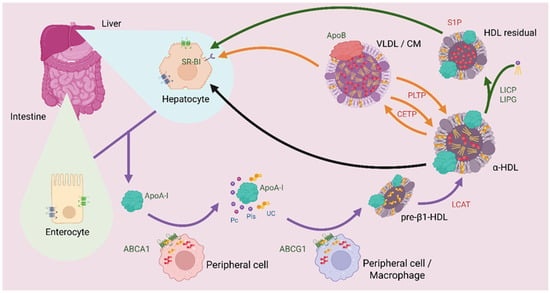
Figure 2.
HDL metabolism. Purple arrows illustrate the process of HDL formation and maturation. It begins with the release of ApoA-I from hepatocytes or enterocytes. ApoA-I circulates through the bloodstream to peripheral cells expressing the ABCA1 transporter, where it acquires phosphatidylcholine (PC), unesterified cholesterol (UC), and phospholipids (PLs). Subsequently, pre-β1-HDL interacts with macrophages or other peripheral tissues expressing ABCG1, where it again acquires PC, UC, and PLs to form a larger particle. Then, LCAT esterifies cholesterol, transforming pre-β1-HDL into α-HDL, the mature form of HDL. The black arrow represents the reverse cholesterol transport (RCT) pathway, in which α-HDL returns cholesterol to hepatocytes through recognition by the scavenger receptor class B type 1 (SR-B1) to allow cholesterol metabolism. The orange arrows indicate a possible fate of α-HDL, in which cholesteryl ester transfer protein (CETP) and phospholipid transfer protein (PLTP) exchange cholesteryl esters and triacylglycerols among very-low-density lipoproteins (VLDL), chylomicrons (CM), and α-HDL. This enables VLDL and CM to deliver more cholesterol to peripheral tissues, while α-HDL returns triacylglycerols to the liver. The green arrows represent another remodeling pathway of α-HDL, in which interaction with hepatic lipase (LIPC) and endothelial lipase (LIPG), which are in the bloodstream, reduces the triacylglycerol content of α-HDL, generating HDL residual enriched in sphingosine-1-phosphate (S1P) that are subsequently returned to hepatocytes for metabolism. Created in BioRender. Matuz Mares, D. (2025) https://BioRender.com/fpnzf7i.
Newly formed pre-β1-HDL undergoes a maturation process through the sequential action of multiple plasma factors (Figure 2): Lecithin cholesterol acyltransferase enzyme (LCAT), activated by ApoA-I, esterifies the captured cholesterol using a fatty acid from phosphatidylcholine, generating cholesterol esters that accumulate in the hydrophobic core of the particle and transforming its morphology from discoidal to spherical (α-HDL) [87].
α-HDL circulate in plasma, where they undergo continuous remodeling via three principal pathways (Figure 2): (1) cholesteryl ester transfer protein (CETP) and phospholipid transfer protein (PLTP) mediate the exchange of cholesteryl esters for triacylglycerides and phospholipids with triacylglycerol-rich lipoproteins (VLDL and CM); (2) Hepatic lipase (LIPC) and Endothelial lipase (LIPG) selectively hydrolyze triacylglycerides and phospholipids to modify α-HDL composition; and (3) the Scavenger Receptor Class B type I (SR-BI) in hepatocytes mediates the selective uptake of cholesteryl esters without degrading the entire particle [88,89]. This last mechanism represents the final stage of RCT, where cholesterol is returned to the liver for biliary excretion or metabolic reuse [22].
Additional to its role in RCT, ABCG1 contributes to cholesterol synthesis by regulating sterol regulatory element-binding protein 2 (SREBP-2), which activates the expression of genes such as β-hydroxy β-methylglutaryl-CoA (HMG-CoA), HMG-CoA reductase (HMGR), HMG-CoA synthase (HMGS), squalene synthase (Sqs), farnesyl diphosphate synthase (Fpps), the low-density lipoprotein receptor (LDLR), and other genes involved in cholesterol synthesis and transport, including insulin-induced gene 1 protein (INSIG1) and StAR-related lipid transfer protein 4 (StarD4) [90].
4. Alterations in HDL Metabolism
The transporters involved in cholesterol efflux systems are particularly vulnerable to the prooxidant microenvironment characteristic of conditions such as atherosclerosis, diabetes, and metabolic syndrome. For example, a study in vivo in murine blood cells has demonstrated that NOX enzymes (NOX 2/4), are a major contributor to ROS production, leading to the downregulation of transporters such as ABCA1 and ABCG1, and induce the accumulation of oxidized LDL, especially in areas susceptible to atherosclerosis [91,92,93]. Additionally, ABCG1 expression was downregulated in human umbilical cord cells exposed to a prooxidant microenvironment, leading to an increase in the activity of NADPH oxidase (particularly NOX4) and reduced the levels of Nuclear factor erythroid 2 (Nrf2), a key regulator of antioxidant defense genes [63].
In addition, the decreased formation of new HDL particles and alterations of existing HDL reduce the efficiency of RCT by decreasing ABCA1 activity, compromising the initial formation of pre-β1-HDL particles, which serve as the primary acceptors of cholesterol from peripheral tissues (Figure 3). When this rate limiting step is impaired, intracellular accumulation of unesterified cholesterol occurs, particularly in macrophages within the arterial intima, promoting foam cell formation [94]. Also, when α-HDL are in an oxidative environment undergo structural modifications that render them dysfunctional: oxidation of methionine residues in ApoA-I (particularly Met148 and Met158). This compromises its ability to activate the enzyme LCAT, which is essential for cholesterol esterification and HDL maturation [95,96]. Furthermore, oxidized HDL exhibits an increased affinity for CETP, promoting the transfer of oxidized lipids to LDL. This phenomenon creates a vicious cycle, as LDL modified through this process becomes more susceptible to further oxidation and more atherogenic [91,97].
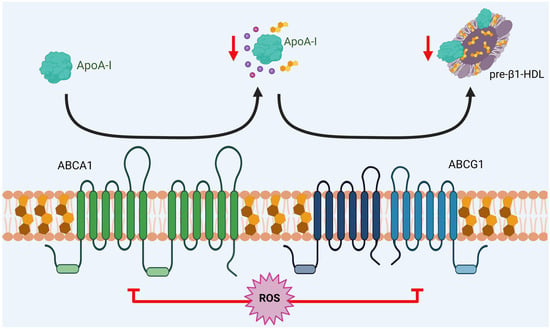
Figure 3.
Dysfunction of HDL metabolism. The generation of ROS reduces the function of ABCA1 and ABCG1 transporters, leading to a decrease in ApoA-I lipidation and producing a similar effect on the formation of pre-β1-HDL and α-HDL (mature HDL) particles. This reduction leads to impaired reverse cholesterol transport (RCT). Created in BioRender. Matuz Mares, D. (2025) https://BioRender.com/efnkqlg.
Also, when the LDL are oxidized, they are not efficiently recognized by the conventional LDLR, but they are preferentially taken up by Scavenger Receptor Class A type I (SR-A1) and Platelet glycoprotein 4 (CD36) on macrophages, a process that is not subject to negative feedback regulation by intracellular cholesterol [19,94]. This dysregulated uptake leads to accelerated foam cell formation, the core of the atherosclerotic plaque. Furthermore, systemic oxidative stress reduces LDLR expression in hepatocytes through epigenetic mechanisms, particularly via ROS induced methylation of its promoter [98,99,100].
Instead, some studies have underscored the critical role of cysteine residues in the functional regulation of transporter proteins. In the case of ABCA1, in vitro models have demonstrated that most of the cysteine residues require palmitoylation, involving the covalent attachment of palmitic acid, to ensure proper activity. Accordingly, mutations at residues Cys3, Cys23, Cys1100, and Cys1111 abolish palmitoylation at these sites and consequently result in a 40–60% reduction in the cholesterol efflux capacity of the transporter. In the case of ABCG1, studies in human cells have shown that mutations at Cys26, Cys248, Cys298, Cys390, Cys397, and Cys402 markedly impair its palmitoylation. Nevertheless, a significant decrease in cholesterol efflux has been experimentally confirmed only for mutations at Cys298 and Cys402 [101,102].
Advances in the understanding of modifications in these transporters offers a promising therapeutic approach for pharmacological targets that may contribute to the prevention and clinical management of cardiovascular diseases, as further discussed in the subsequent section.
5. Potential Treatments
As the activity of ABC transporters is essential for lipid homeostasis, their deregulation can cause multiple lipid-metabolism diseases, such as Tangier disease, sitosterolemia, atherosclerosis, metabolic syndrome, obesity, stroke, type 2 diabetes, and Alzheimer’s disease [29,103].
The conventional approaches to treating them include the use of drugs or traditional compounds that regulate the expression and stability of the ABCA1 and ABCG1 transporters [103], reducing lipid accumulation, avoiding atherosclerotic plaque formation, and increasing cholesterol efflux [104]. In Table 2, a comparison of the potential or available therapies is shown.

Table 2.
Potential or available treatment for ABCA1 and ABCG1 transporter-related diseases.
Table 2.
Potential or available treatment for ABCA1 and ABCG1 transporter-related diseases.
| Compound | Status | Nature | Target | Effect | Mechanism | Model System | Adverse Effects | Reference |
|---|---|---|---|---|---|---|---|---|
| Antagomir | Preclinic | Synthetic | ABCA1 & ABCG1 | ↑ | ↓ miR-23a-5p | ApoE−/− mice | ND | [105] |
| Cilostazol | Clinic | Synthetic | ABCA1 | ↑ | ↑ LXR/ABCA1/SREBP-1 | Human hepatoma cell line HepG2 | ND | [106] |
| CoQ | Preclinic | Natural | ABCG1 | ↑ | ↑ Activator protein-1, ↑ miR-378 | C57BL/6J mouse peritoneal macrophages, J774. A1, THP-1, HEK293 cells & ApoE−/− mice | No found | [107] |
| Diosgenin | Preclinic | Natural | ABCA1 | ↑ | ↓ miR-19b, | THP-1 macrophages/MPM-derived foam cells & ApoE−/− mice | ND | [108] |
| Dihydrogen | Clinic | Synthetic | ABCA1 | ↑ | ND | Potential metabolic syndrome patients | No found | [109] |
| Hydrogen sulfide | Preclinic | Synthetic | ABCA1 | ↑ | ↑ Peroxisome proliferator-activated receptor α (PPARα) translocation | Human hepatoma cell line HepG2 & ApoE−/− mice | ND | [110] |
| Paeonol | Preclinic | Natural | ABCA1 | ↑ | ↓ Calpain-related pathway, ↓ CD36 (platelet glycoprotein-4), ↑ Heme oxygenase-1 | RAW264.7 macrophages & ApoE−/− mice | ND | [104] |
| Qingre Sanjie Formula | Preclinic | Natural | ABCA1 | ↑ | ↑ LXRα/ABCG5/G8 pathway | ApoE−/− mice | No found | [111] |
| Statins (Atorvastatin & pitavastatin) | Clinic | Synthetic | ABCA1 | ↓ | ↓ Protein kinase B phosphorylation, ↑ miR-33 levels | RAW264.7 cells & bone marrow-derived macrophages | Risk of hyperglycemia and new-onset diabetes | [112] |
| Triptolide | Preclinic | Natural | ABCA1 | ↑ | May mediate expression through LPS/TLR4/GPS2 pathway | Male Sprague Dawley rats | ND | [113] |
↑: upregulation, ↓: downregulation, ND: not determined.
Apart from ABCA1 and ABCG1, other components of the pathway can be targeted to increase the HDL levels; however, most of them cause several side effects, for example, LXR antagonist (LXR-623) administration is related to liver steatosis and neurological problems [114], and administration of external ApoA-1 with hepatotoxicity [115]. Nevertheless, the use of CETP inhibitors (such as anacetrapib and dalcetrapib) has been shown to increase HDL cholesterol levels without adverse effects, providing a safe option for patients with dyslipidemia [116,117]. The same occurs when Ezetimibe, an inhibitor of the Niemann-Pick-C1 protein (NPC1L1), is administered; the HDL cholesterol increases and LDL cholesterol and triglycerides levels decrease without adverse effects [118].
Moreover, the use of combination treatments without adverse effects has been reported. The work by Ma et al. (2018) indicates that when metformin is administered with T0901317 (a selective LXR inhibitor), their inhibitory effect on atherosclerosis is enhanced [119]. A similar effect occurs when niacin (vitamin B3) is applied together with statins [120].
In addition, a synthetic ApoE peptide called EpK, reduces the development of atherosclerosis by binding to HDL in ApoE-deficient mice [121]. When EpK is linked to methionine sulfoxide reductase A (MsrA), a hepatic protein with anti-atherosclerotic properties, its effect is enhanced due to the improvement of the redox status and inflammatory profile of dysfunctional HDL, promoting hepatic cholesterol uptake and excretion. EpK-MsrA also exhibited anti-inflammatory and modulatory effects on key HDL-associated proteins, including ApoA-I, paraoxonase 1 (PON1), and LCAT, leading to a further reduction in atherosclerotic burden [35].
On the other hand, an emerging strategy is the use of miRNAs in the regulation of ABCA1 and ABCG1 transporters expression [122]. miRNAs are small non-coding RNAs that control gene expression due to the binding of 3′UTR regions of mRNAs [123]. Many miRNAs have been reported to modulate lipoprotein metabolism. In Table 3, a compilation of these compounds and their effect on transporter gene expression is shown. For further information, we refer the reader to Rozhkova et al. (2021) [25] and Goedeke et al. (2014) [124].

Table 3.
Effect of miRNAs on the expression levels of ABCA1 and ABCG1 transporters.
Furthermore, some natural antioxidant compounds have been used as a promising treatment for atherosclerosis: Auricularia heimuer, better known as heimuer, with its anti-inflammatory, hypolipidemic, and antioxidant effects, demonstrates regulating lipid levels, gut microbiota, body weight, and alleviating aortic lesions in atherosclerosis induced in a high-fat diet ApoE−/− mice [125]. Curcumin, normally consumed for its anti-inflammatory properties, also modulates gut microbiota with anti-obesity and anti-hyperlipidemic effects that contribute to the prevention atherosclerosis progression [126]. Resveratrol attenuates the progression of atherosclerosis by inhibiting the oxidative modification of LDL cholesterol and demonstrates multifaceted anti-atherosclerotic effects [127]. Oleuropein, extracted from olive leaves, significantly attenuated the atherosclerosis progression and enhanced plaque stability. It is demonstrated that this compound suppresses ferroptosis by upregulating GPX4/xCT (Phospholipid hydroperoxide glutathione peroxidase 4/Cystine/glutamate transporter) level and enhances Nrf2 activation and nuclear translocation [128]. Finally, brown marine algae-derived polysaccharides, such as fucoidan, alginate, laminarin, carrageenan, and chitosan, exert anti-inflammatory, antioxidant, lipid-regulating, antithrombotic, and endothelial-protective effects, relevant to the pathogenesis of atherosclerotic cardiovascular disease, but their oral bioavailability and structural diversity are challenges to overcome for using them for preventing and treatment of atherosclerotic cardiovascular disease [129].
One of the main challenges of current therapies, regardless of their chemical nature, lies in the adverse side effects on the body. However, the development of nanomaterials offers a promising option to overcome these limitations [130]. For example, a nanofibrous hydrogel encapsulating D-Nap-GFFY-T0901317, an LXR agonist, has been shown to inhibit atherosclerosis without inducing hepatic lipogenesis, representing a novel and potentially effective strategy for the treatment of atherosclerosis [131].
6. Limitations and Perspectives
ABCA1 and ABCG1 transporters are potential pharmacological targets for the prevention and treatment of atherosclerosis. However, safe, effective clinical therapies without serious side effects are not yet available. Therefore, it is necessary to develop molecules that specifically activate ABCA1 and ABCG1 through genetic regulation.
To date, attempts to induce ABCA1 and ABCG1 expression by modulating LXR have been unsuccessful due to adverse effects. For example, administration of LXR-623 (an LXR antagonist) that increases mature HDL levels may cause hepatic steatosis and neurological problems [114]. Consequently, current research focuses on engineering drugs that can target ABCA1 and ABCG1 expression through transcriptional regulation, such as the PPAR-α-based therapies [110]. One potential strategy is to combine both compounds to enhance their effect on atherosclerosis. LXR agonists induce ABCA1 and ABCG1 expression, while PPAR stimulation suppresses triacylglycerol levels by increasing β-oxidation and LIPC enzyme activity, thereby avoiding potential serious side effects [77,78].
Another approach is the development of compounds that specifically increase the activity of ABCA1 and ABCG1 or prevent their protein degradation. For example, the administration of a recombinant HDL-like particle (designated ETC-216), containing ApoA-I, resulted in a 4.2% decrease from baseline in coronary atheroma volume measured by intravascular ultrasound [132].
On the other hand, numerous reports describe several natural products present in foods, as well as synthetic small molecules, that could activate the expression of ABCA1 and ABCG1. Still, most of them are in the preclinical stage (see Table 2), so greater effort is needed to implement them in the clinic.
Furthermore, the origin of ABCA1 and ABCG1 dysfunction lies in the cysteine mutation experiments [101,102]; these residues may serve as susceptible targets for oxidation, given their high reactivity under prooxidant conditions. This could account for the reduced activity of ABCA1 and ABCG1, clarifying the pathophysiology of atherosclerosis and potential therapeutic targets.
The next critical step in understanding the pathophysiology of atherosclerosis involves characterizing the precise structural and functional consequences of oxidative stress on ABCA1 and ABCG1. Given the complexity and range of potential modifications, bioinformatic tools can generate high-resolution structural models, predict the dynamic effects of cysteine oxidation at the atomic level, and identify new susceptible residues. Additionally, the genetic and epigenetic regulation of ABCA1 and ABCG1 expressions represent a promising approach to restore HDL function, potentially with a lower risk of systemic adverse effects than direct pharmacological interventions. Finally, integrating these computational insights with in vitro functional assays could facilitate the development of compounds that enhance antioxidant defenses or stabilize transporter activity, which represents a future direction for reducing atherosclerotic damage and the burden of cardiovascular disease.
7. Conclusions
The present work aimed to provide a concise overview of HDL metabolism, emphasizing the key roles of the ABCA1 and ABCG1 transporters and their correct function, which is currently of greater relevance due to increasing scientific evidence supporting the notion that oxidative stress promotes their dysfunction, thus contributing to the development of cardiovascular diseases such as atherosclerosis. However, the precise molecular mechanisms underlying this impairment remain unclear, and based on the data available to date, ABCA1 and ABCG1 could be good candidates as pharmacological targets to induce proper RCT function. Safer and more effective clinical treatments are needed to reduce side effects in patients with atherosclerosis or related conditions characterized by low circulating HDL levels.
Author Contributions
Conceptualization, K.D.L.-M., M.M.V.-L. and D.M.-M.; funding acquisition none, writing—original draft preparation, K.D.L.-M., M.V.-C., M.M.V.-L., D.U.-R. and D.M.-M.; writing—review, K.D.L.-M., M.V.-C., M.M.V.-L., D.U.-R. and D.M.-M.; editing, K.D.L.-M., M.M.V.-L., M.V.-C., D.U.-R. and D.M.-M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Acknowledgments
We thank Héctor Vázquez-Meza for his editorial collaboration and valuable contributions to the improvement of this manuscript.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| HDLs | High-density lipoproteins |
| ABC | ATP-binding cassette |
| LDLs | Low-density lipoproteins |
| CMs | Chylomicrons |
| VLDL | Very-low-density lipoprotein |
| RCT | Reverse cholesterol transport |
| ROS | Reactive oxygen species |
| NBDs | Nucleotide-binding domains |
| TMDs | Transmembrane domains |
| ECDs | Extracellular domains |
| LXR | Liver X receptor |
| RXR | Retinoid X receptor |
| PPAR α and γ | Peroxisome proliferator-activated receptors alpha and gamma |
| SREBF1 | Sterol regulatory element binding factors 1 |
| SREBF2 | Sterol regulatory element binding factors 2 |
| AD | Alzheimer’s disease |
| miRNAs/miR | MicroRNAs |
| LCAT | Lecithin cholesterol acyltransferase |
| PC | Phosphatidylcholine |
| UC | Unesterified cholesterol |
| PLs | Phospholipids |
| SR-B1 | Scavenger receptor class B type 1 |
| CETP | Cholesteryl ester transfer protein |
| PLTP | Phospholipid transfer protein |
| LIPC | Hepatic lipase |
| LIPG | Endothelial lipase |
| SREBP-2 | Sterol regulatory element-binding protein 2 |
| HMG-CoA | β-hydroxy β-methylglutaryl-CoA |
| HMGR | HMG-CoA reductase |
| HMGS | HMG-CoA synthase |
| Sqs | Squalene synthase |
| Fpps | Farnesyl diphosphate synthase |
| LDLR | Low-density lipoprotein receptor |
| INSIG1 | Insulin-induced gene 1 protein S |
| StarD4 | StAR-related lipid transfer protein 4 |
| Nrf2 | Nuclear factor erythroid 2 |
| SR-A1 | Scavenger Receptor Class A type 1 |
| CD36 | Platelet glycoprotein 4 |
| NPC1L1 | Niemann-Pick-C1 protein |
| MsrA | Methionine sulfoxide reductase A |
| PON1 | Paraoxonase 1 |
| GPX4/xCT | Phospholipid hydroperoxide glutathione peroxidase 4/Cystine/glutamate transporter |
References
- Avery, S.V. Molecular targets of oxidative stress. Biochem. J. 2011, 434, 201–210. [Google Scholar] [CrossRef]
- Iqbal, J.; Hussain, M.M. Intestinal lipid absorption. Am. J. Physiol. Endocrinol. Metab. 2009, 296, E1183–E1194. [Google Scholar] [CrossRef]
- Liu, Z.; Ren, Z.; Zhang, J.; Chuang, C.C.; Kandaswamy, E.; Zhou, T.; Zuo, L. Role of ROS and Nutritional Antioxidants in Human Diseases. Front. Physiol. 2018, 9, 477. [Google Scholar] [CrossRef] [PubMed]
- Alonso-Pineiro, J.A.; Gonzalez-Rovira, A.; Sanchez-Gomar, I.; Moreno, J.A.; Duran-Ruiz, M.C. Nrf2 and Heme Oxygenase-1 Involvement in Atherosclerosis Related Oxidative Stress. Antioxidants 2021, 10, 1463. [Google Scholar] [CrossRef] [PubMed]
- Loboda, A.; Damulewicz, M.; Pyza, E.; Jozkowicz, A.; Dulak, J. Role of Nrf2/HO-1 system in development, oxidative stress response and diseases: An evolutionarily conserved mechanism. Cell. Mol. Life Sci. 2016, 73, 3221–3247. [Google Scholar] [CrossRef] [PubMed]
- Matuz-Mares, D.; Gonzalez-Andrade, M.; Araiza-Villanueva, M.G.; Vilchis-Landeros, M.M.; Vazquez-Meza, H. Mitochondrial Calcium: Effects of Its Imbalance in Disease. Antioxidants 2022, 11, 801. [Google Scholar] [CrossRef]
- Schieber, M.; Chandel, N.S. ROS function in redox signaling and oxidative stress. Curr. Biol. 2014, 24, R453–R462. [Google Scholar] [CrossRef]
- Álvarez-López, H.; Ruiz-Gastélum, E.; Díaz-Aragón, A. Conociendo los mecanismos básicos del metabolismo de los lípidos. Cardiovasc. Metab. Sci. 2021, 32, 147–152. [Google Scholar] [CrossRef]
- Havel, R.J.; Eder, H.A.; Bragdon, J.H. The distribution and chemical composition of ultracentrifugally separated lipoproteins in human serum. J. Clin. Investig. 1955, 34, 1345–1353. [Google Scholar] [CrossRef]
- Ansell, B.J.; Navab, M.; Hama, S.; Kamranpour, N.; Fonarow, G.; Hough, G.; Rahmani, S.; Mottahedeh, R.; Dave, R.; Reddy, S.T.; et al. Inflammatory/antiinflammatory properties of high-density lipoprotein distinguish patients from control subjects better than high-density lipoprotein cholesterol levels and are favorably affected by simvastatin treatment. Circulation 2003, 108, 2751–2756. [Google Scholar] [CrossRef]
- Chapman, M.J. Animal lipoproteins: Chemistry, structure, and comparative aspects. J. Lipid Res. 1980, 21, 789–853. [Google Scholar] [CrossRef]
- Franczyk, B.; Rysz, J.; Lawinski, J.; Rysz-Gorzynska, M.; Gluba-Brzozka, A. Is a High HDL-Cholesterol Level Always Beneficial? Biomedicines 2021, 9, 1083. [Google Scholar] [CrossRef]
- Ginsberg, H.N. Lipoprotein physiology and its relationship to atherogenesis. Endocrinol. Metab. Clin. N. Am. 1990, 19, 211–228. [Google Scholar] [CrossRef]
- Jonas, A.P.; Michael, C. Lipoprotein structure. In Biochemistry of Lipids, Lipoproteins and Membranes, 5th ed.; Ennis, E., Vance, J.E.V., Eds.; Elsevier: Amsterdam, The Netherlands, 2008; pp. 485–506. [Google Scholar]
- Khosravi, M.; Hosseini-Fard, R.; Najafi, M. Circulating low density lipoprotein (LDL). Horm. Mol. Biol. Clin. Investig. 2018, 35, 20180024. [Google Scholar] [CrossRef] [PubMed]
- Kindel, T.; Lee, D.M.; Tso, P. The mechanism of the formation and secretion of chylomicrons. Atheroscler. Suppl. 2010, 11, 11–16. [Google Scholar] [CrossRef] [PubMed]
- van Zwol, W.; van de Sluis, B.; Ginsberg, H.N.; Kuivenhoven, J.A. VLDL Biogenesis and Secretion: It Takes a Village. Circ. Res. 2024, 134, 226–244. [Google Scholar] [CrossRef]
- Errico, T.L.; Chen, X.; Martin Campos, J.M.; Julve, J.; Escola-Gil, J.C.; Blanco-Vaca, F. Basic mechanisms: Structure, function and metabolism of plasma lipoproteins. Clin. Investig. Arterioscler. 2013, 25, 98–103. [Google Scholar] [CrossRef]
- Hernández Puga, G.; Laguna Maldonado, K.D.; Reyes Galindo, M.; Moreno Piña, J.R.; Matuz Mares, D. Lipoproteínas de Alta Densidad y Riesgo Cardiovascular. Rev. Educ. Bioquíim. 2019, 4, 93–99. [Google Scholar]
- Chen, J.; Fang, Z.; Luo, Q.; Wang, X.; Warda, M.; Das, A.; Oldoni, F.; Luo, F. Unlocking the mysteries of VLDL: Exploring its production, intracellular trafficking, and metabolism as therapeutic targets. Lipids Health Dis. 2024, 23, 14. [Google Scholar] [CrossRef]
- Olofsson, S.O.; Asp, L.; Boren, J. The assembly and secretion of apolipoprotein B-containing lipoproteins. Curr. Opin. Lipidol. 1999, 10, 341–346. [Google Scholar] [CrossRef]
- Jomard, A.; Osto, E. High Density Lipoproteins: Metabolism, Function, and Therapeutic Potential. Front. Cardiovasc. Med. 2020, 7, 39. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.Y.; Parks, J.S. ATP-binding cassette transporter AI and its role in HDL formation. Curr. Opin. Lipidol. 2005, 16, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Phillips, M.C. Molecular mechanisms of cellular cholesterol efflux. J. Biol. Chem. 2014, 289, 24020–24029. [Google Scholar] [CrossRef] [PubMed]
- Rozhkova, A.V.; Dmitrieva, V.G.; Nosova, E.V.; Dergunov, A.D.; Limborska, S.A.; Dergunova, L.V. Genomic Variants and Multilevel Regulation of ABCA1, ABCG1, and SCARB1 Expression in Atherogenesis. J. Cardiovasc. Dev. Dis. 2021, 8, 170. [Google Scholar] [CrossRef]
- Zannis, V.I.; Kurnit, D.M.; Breslow, J.L. Hepatic apo-A-I and apo-E and intestinal apo-A-I are synthesized in precursor isoprotein forms by organ cultures of human fetal tissues. J. Biol. Chem. 1982, 257, 536–544. [Google Scholar] [CrossRef]
- Guerin, M. Reverse Cholesterol Transport in HDL Metabolism. In The HDL Handbook; Academic Press: Cambridge, MA, USA, 2017. [Google Scholar]
- Voloshyna, I.; Reiss, A.B. The ABC transporters in lipid flux and atherosclerosis. Prog. Lipid Res. 2011, 50, 213–224. [Google Scholar] [CrossRef]
- Schumacher, T.; Benndorf, R.A. ABC Transport Proteins in Cardiovascular Disease—A Brief Summary. Molecules 2017, 22, 589. [Google Scholar] [CrossRef]
- Vilchis-Landeros, M.M.; Vazquez-Meza, H.; Vazquez-Carrada, M.; Uribe-Ramirez, D.; Matuz-Mares, D. Antioxidant Enzymes and Their Potential Use in Breast Cancer Treatment. Int. J. Mol. Sci. 2024, 25, 5675. [Google Scholar] [CrossRef]
- Chen, M.; Li, W.; Wang, N.; Zhu, Y.; Wang, X. ROS and NF-kappaB but not LXR mediate IL-1beta signaling for the downregulation of ATP-binding cassette transporter A1. Am. J. Physiol. Cell Physiol. 2007, 292, C1493–C1501. [Google Scholar] [CrossRef]
- Wang, J.; Xiao, Q.; Wang, L.; Wang, Y.; Wang, D.; Ding, H. Role of ABCA1 in Cardiovascular Disease. J. Pers. Med. 2022, 12, 1010. [Google Scholar] [CrossRef]
- An, Y.; Xu, B.T.; Wan, S.R.; Ma, X.M.; Long, Y.; Xu, Y.; Jiang, Z.Z. The role of oxidative stress in diabetes mellitus-induced vascular endothelial dysfunction. Cardiovasc. Diabetol. 2023, 22, 237. [Google Scholar] [CrossRef] [PubMed]
- Giacco, F.; Brownlee, M. Oxidative stress and diabetic complications. Circ. Res. 2010, 107, 1058–1070. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Pu, J.X.; Yang, X.; Liu, M.C.; Zhang, P.; Cao, J.; Du, F.; Wu, D.F.; Lu, Z.B.; Yu, H. ApoE Mimetic Peptide-MsrA Fusion Protein Restores HDL Function and Ameliorates Atherosclerosis via Circulatory Redox Remodeling in SR-BI Deficient Mice. FASEB J. 2025, 39, e70999. [Google Scholar] [CrossRef] [PubMed]
- Matuz-Mares, D.; Riveros-Rosas, H.; Vilchis-Landeros, M.M.; Vazquez-Meza, H. Glutathione Participation in the Prevention of Cardiovascular Diseases. Antioxidants 2021, 10, 1220. [Google Scholar] [CrossRef]
- Panth, N.; Paudel, K.R.; Parajuli, K. Reactive Oxygen Species: A Key Hallmark of Cardiovascular Disease. Adv. Med. 2016, 2016, 9152732. [Google Scholar] [CrossRef]
- Ranneh, Y.; Ali, F.; Akim, A.M.; Hamid, H.A.; Khazaai, H.; Fadel, A. Crosstalk between reactive oxygen species and pro-inflammatory markers in developing various chronic diseases: A review. Appl. Biol. Chem. 2017, 60, 327–338. [Google Scholar] [CrossRef]
- Seyffer, F.; Tampe, R. ABC transporters in adaptive immunity. Biochim. Biophys. Acta 2015, 1850, 449–460. [Google Scholar] [CrossRef]
- Alam, A.; Locher, K.P. Structure and Mechanism of Human ABC Transporters. Annu. Rev. Biophys. 2023, 52, 275–300. [Google Scholar] [CrossRef]
- Falguieres, T. ABC Transporters in Human Diseases: Future Directions and Therapeutic Perspectives. Int. J. Mol. Sci. 2022, 23, 4250. [Google Scholar] [CrossRef]
- Thomas, C.; Tampe, R. Structural and Mechanistic Principles of ABC Transporters. Annu. Rev. Biochem. 2020, 89, 605–636. [Google Scholar] [CrossRef]
- Dean, M.; Moitra, K.; Allikmets, R. The human ATP-binding cassette (ABC) transporter superfamily. Hum. Mutat. 2022, 43, 1162–1182. [Google Scholar] [CrossRef]
- Duvivier, L.; Gerard, L.; Diaz, A.; Gillet, J.P. Linking ABC transporters to the hallmarks of cancer. Trends Cancer 2024, 10, 124–134. [Google Scholar] [CrossRef]
- Stefan, K.Y.; Leck, L.Y.W.; Namasivayam, V.; Bascuñana, P.; Huang, M.L.H.; Riss, P.J.; Pahnke, J.; Jansson, P.J.; Stefan, S.M. Vesicular ATP-binding cassette transporters in human disease: Relevant aspects of their organization for future drug development. Future Drug Discov. 2020, 4, FDD51. [Google Scholar] [CrossRef]
- Szakacs, G.; Abele, R. An inventory of lysosomal ABC transporters. FEBS Lett. 2020, 594, 3965–3985. [Google Scholar] [CrossRef]
- Kotlyarov, S.; Kotlyarova, A. Biological Functions and Clinical Significance of the ABCG1 Transporter. Biology 2024, 14, 8. [Google Scholar] [CrossRef] [PubMed]
- Matsuo, M. ABCA1 and ABCG1 as potential therapeutic targets for the prevention of atherosclerosis. J. Pharmacol. Sci. 2022, 148, 197–203. [Google Scholar] [CrossRef] [PubMed]
- Liu, X. ABC Family Transporters. Adv. Exp. Med. Biol. 2019, 1141, 13–100. [Google Scholar] [CrossRef] [PubMed]
- Beis, K. Structural basis for the mechanism of ABC transporters. Biochem. Soc. Trans. 2015, 43, 889–893. [Google Scholar] [CrossRef]
- Vasiliou, V.; Vasiliou, K.; Nebert, D.W. Human ATP-binding cassette (ABC) transporter family. Hum. Genom. 2009, 3, 281–290. [Google Scholar] [CrossRef]
- Nguyen, J.P.; Kim, Y.; Cao, Q.; Hirota, J.A. Interactions between ABCC4/MRP4 and ABCC7/CFTR in human airway epithelial cells in lung health and disease. Int. J. Biochem. Cell Biol. 2021, 133, 105936. [Google Scholar] [CrossRef]
- Chen, Z.; Liu, F.; Ren, Q.; Zhao, Q.; Ren, H.; Lu, S.; Zhang, L.; Han, Z. Suppression of ABCG2 inhibits cancer cell proliferation. Int. J. Cancer 2010, 126, 841–851. [Google Scholar] [CrossRef]
- Polireddy, K.; Chavan, H.; Abdulkarim, B.A.; Krishnamurthy, P. Functional significance of the ATP-binding cassette transporter B6 in hepatocellular carcinoma. Mol. Oncol. 2011, 5, 410–425. [Google Scholar] [CrossRef] [PubMed]
- Mantel, I.; Sadiq, B.A.; Blander, J.M. Spotlight on TAP and its vital role in antigen presentation and cross-presentation. Mol. Immunol. 2022, 142, 105–119. [Google Scholar] [CrossRef] [PubMed]
- Feingold, K.R. Introduction to Lipids and Lipoproteins. In Endotext; Feingold, K.R., Ahmed, S.F., Anawalt, B., Blackman, M.R., Boyce, A., Chrousos, G., Corpas, E., de Herder, W.W., Dhatariya, K., Dungan, K., et al., Eds.; MDText.com, Inc.: South Dartmouth, MA, USA, 2000. [Google Scholar]
- Mineo, C.; Shaul, P.W. Regulation of signal transduction by HDL. J. Lipid Res. 2013, 54, 2315–2324. [Google Scholar] [CrossRef] [PubMed]
- Kerr, I.D.; Hutchison, E.; Gerard, L.; Aleidi, S.M.; Gelissen, I.C. Mammalian ABCG-transporters, sterols and lipids: To bind perchance to transport? Biochim. Biophys. Acta Mol. Cell Biol. Lipids 2021, 1866, 158860. [Google Scholar] [CrossRef]
- Choi, H.Y.; Choi, S.; Iatan, I.; Ruel, I.; Genest, J. Biomedical Advances in ABCA1 Transporter: From Bench to Bedside. Biomedicines 2023, 11, 561. [Google Scholar] [CrossRef]
- Dahik, V.D.; Kc, P.; Materne, C.; Reydellet, C.; Lhomme, M.; Cruciani-Guglielmacci, C.; Denom, J.; Bun, E.; Ponnaiah, M.; Deknuydt, F.; et al. ABCG1 orchestrates adipose tissue macrophage plasticity and insulin resistance in obesity by rewiring saturated fatty acid pools. Sci. Transl. Med. 2024, 16, eadi6682. [Google Scholar] [CrossRef]
- Wang, H.J.; Wang, J.H.; Xu, X.N.; Zhao, X.S.; Liu, W. ABCG1 is Expressed in an LXR-Independent Manner in Patients with Type 2 Diabetes Mellitus. Curr. Mol. Med. 2023, 23, 815–824. [Google Scholar] [CrossRef]
- Wang, N.; Yvan-Charvet, L.; Lutjohann, D.; Mulder, M.; Vanmierlo, T.; Kim, T.W.; Tall, A.R. ATP-binding cassette transporters G1 and G4 mediate cholesterol and desmosterol efflux to HDL and regulate sterol accumulation in the brain. FASEB J. 2008, 22, 1073–1082. [Google Scholar] [CrossRef]
- Xue, J.; Fan, J.; Li, Y.; Wu, W.; Yan, Q.; Zheng, Q. ABCG1 Attenuates Oxidative Stress Induced by H(2)O(2) through the Inhibition of NADPH Oxidase and the Upregulation of Nrf2-Mediated Antioxidant Defense in Endothelial Cells. Anal. Cell. Pathol. 2020, 2020, 2095645. [Google Scholar] [CrossRef]
- Sunidhi, S.; Sacher, S.; Atul; Garg, P.; Ray, A. Elucidating the Structural Features of ABCA1 in its Heterogeneous Membrane Environment. Front. Mol. Biosci. 2021, 8, 803078. [Google Scholar] [CrossRef] [PubMed]
- Rust, S.; Rosier, M.; Funke, H.; Real, J.; Amoura, Z.; Piette, J.C.; Deleuze, J.F.; Brewer, H.B.; Duverger, N.; Denefle, P.; et al. Tangier disease is caused by mutations in the gene encoding ATP-binding cassette transporter 1. Nat. Genet. 1999, 22, 352–355. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, M.A.; Barrera, G.C.; Nakamura, K.; Baldan, A.; Tarr, P.; Fishbein, M.C.; Frank, J.; Francone, O.L.; Edwards, P.A. ABCG1 has a critical role in mediating cholesterol efflux to HDL and preventing cellular lipid accumulation. Cell Metab. 2005, 1, 121–131. [Google Scholar] [CrossRef] [PubMed]
- Jacobo-Albavera, L.; Dominguez-Perez, M.; Medina-Leyte, D.J.; Gonzalez-Garrido, A.; Villarreal-Molina, T. The Role of the ATP-Binding Cassette A1 (ABCA1) in Human Disease. Int. J. Mol. Sci. 2021, 22, 1593. [Google Scholar] [CrossRef]
- Wang, Y.; Guo, M.; Tang, C.K. History and Development of ABCA1. Curr. Probl. Cardiol. 2024, 49, 102036. [Google Scholar] [CrossRef]
- Kober, A.C.; Manavalan, A.P.C.; Tam-Amersdorfer, C.; Holmer, A.; Saeed, A.; Fanaee-Danesh, E.; Zandl, M.; Albrecher, N.M.; Bjorkhem, I.; Kostner, G.M.; et al. Implications of cerebrovascular ATP-binding cassette transporter G1 (ABCG1) and apolipoprotein M in cholesterol transport at the blood-brain barrier. Biochim. Biophys. Acta Mol. Cell Biol. Lipids 2017, 1862, 573–588. [Google Scholar] [CrossRef]
- Stefulj, J.; Panzenboeck, U.; Becker, T.; Hirschmugl, B.; Schweinzer, C.; Lang, I.; Marsche, G.; Sadjak, A.; Lang, U.; Desoye, G.; et al. Human endothelial cells of the placental barrier efficiently deliver cholesterol to the fetal circulation via ABCA1 and ABCG1. Circ. Res. 2009, 104, 600–608. [Google Scholar] [CrossRef]
- Zeng, G.G.; Lei, Q.; Jiang, W.L.; Zhang, X.X.; Nie, L.; Gong, X.; Zheng, K. A new perspective on the current and future development potential of ABCG1. Curr. Probl. Cardiol. 2024, 49, 102161. [Google Scholar] [CrossRef]
- Rezaei, F.; Farhat, D.; Gursu, G.; Samnani, S.; Lee, J.Y. Snapshots of ABCG1 and ABCG5/G8: A Sterol’s Journey to Cross the Cellular Membranes. Int. J. Mol. Sci. 2022, 24, 484. [Google Scholar] [CrossRef]
- Kobayashi, A.; Takanezawa, Y.; Hirata, T.; Shimizu, Y.; Misasa, K.; Kioka, N.; Arai, H.; Ueda, K.; Matsuo, M. Efflux of sphingomyelin, cholesterol, and phosphatidylcholine by ABCG1. J. Lipid Res. 2006, 47, 1791–1802. [Google Scholar] [CrossRef]
- Paseban, T.; Alavi, M.S.; Etemad, L.; Roohbakhsh, A. The role of the ATP-Binding Cassette A1 (ABCA1) in neurological disorders: A mechanistic review. Expert Opin. Ther. Targets 2023, 27, 531–552. [Google Scholar] [CrossRef]
- Wu, K.; Zou, L.; Lei, X.; Yang, X. Roles of ABCA1 in cancer. Oncol. Lett. 2022, 24, 349. [Google Scholar] [CrossRef]
- Lewandowski, C.T.; Laham, M.S.; Thatcher, G.R.J. Remembering your A, B, C’s: Alzheimer’s disease and ABCA1. Acta Pharm. Sin. B 2022, 12, 995–1018. [Google Scholar] [CrossRef]
- Akiyama, T.E.; Sakai, S.; Lambert, G.; Nicol, C.J.; Matsusue, K.; Pimprale, S.; Lee, Y.H.; Ricote, M.; Glass, C.K.; Brewer, H.B., Jr.; et al. Conditional disruption of the peroxisome proliferator-activated receptor gamma gene in mice results in lowered expression of ABCA1, ABCG1, and apoE in macrophages and reduced cholesterol efflux. Mol. Cell. Biol. 2002, 22, 2607–2619. [Google Scholar] [CrossRef] [PubMed]
- Ozasa, H.; Ayaori, M.; Iizuka, M.; Terao, Y.; Uto-Kondo, H.; Yakushiji, E.; Takiguchi, S.; Nakaya, K.; Hisada, T.; Uehara, Y.; et al. Pioglitazone enhances cholesterol efflux from macrophages by increasing ABCA1/ABCG1 expressions via PPARgamma/LXRalpha pathway: Findings from in vitro and ex vivo studies. Atherosclerosis 2011, 219, 141–150. [Google Scholar] [CrossRef] [PubMed]
- Abildayeva, K.; Jansen, P.J.; Hirsch-Reinshagen, V.; Bloks, V.W.; Bakker, A.H.; Ramaekers, F.C.; de Vente, J.; Groen, A.K.; Wellington, C.L.; Kuipers, F.; et al. 24(S)-hydroxycholesterol participates in a liver X receptor-controlled pathway in astrocytes that regulates apolipoprotein E-mediated cholesterol efflux. J. Biol. Chem. 2006, 281, 12799–12808. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Wei, Z.; Ma, X.; Yang, X.; Chen, Y.; Sun, L.; Ma, C.; Miao, Q.R.; Hajjar, D.P.; Han, J.; et al. 25-Hydroxycholesterol activates the expression of cholesterol 25-hydroxylase in an LXR-dependent mechanism. J. Lipid Res. 2018, 59, 439–451. [Google Scholar] [CrossRef]
- Aryal, B.; Singh, A.K.; Rotllan, N.; Price, N.; Fernandez-Hernando, C. MicroRNAs and lipid metabolism. Curr. Opin. Lipidol. 2017, 28, 273–280. [Google Scholar] [CrossRef]
- Najafi-Shoushtari, S.H.; Kristo, F.; Li, Y.; Shioda, T.; Cohen, D.E.; Gerszten, R.E.; Naar, A.M. MicroRNA-33 and the SREBP host genes cooperate to control cholesterol homeostasis. Science 2010, 328, 1566–1569. [Google Scholar] [CrossRef]
- Hori, N.; Hayashi, H.; Sugiyama, Y. Calpain-mediated cleavage negatively regulates the expression level of ABCG1. Atherosclerosis 2011, 215, 383–391. [Google Scholar] [CrossRef]
- Ogura, M.; Ayaori, M.; Terao, Y.; Hisada, T.; Iizuka, M.; Takiguchi, S.; Uto-Kondo, H.; Yakushiji, E.; Nakaya, K.; Sasaki, M.; et al. Proteasomal inhibition promotes ATP-binding cassette transporter A1 (ABCA1) and ABCG1 expression and cholesterol efflux from macrophages in vitro and in vivo. Arterioscler. Thromb. Vasc. Biol. 2011, 31, 1980–1987. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Zhao, Z.W.; Zeng, P.H.; Zhou, Y.J.; Yin, W.J. Molecular mechanisms for ABCA1-mediated cholesterol efflux. Cell Cycle 2022, 21, 1121–1139. [Google Scholar] [CrossRef] [PubMed]
- Dergunov, A.D.; Baserova, V.B. Different Pathways of Cellular Cholesterol Efflux. Cell Biochem. Biophys. 2022, 80, 471–481. [Google Scholar] [CrossRef] [PubMed]
- Laurenzi, T.; Parravicini, C.; Palazzolo, L.; Guerrini, U.; Gianazza, E.; Calabresi, L.; Eberini, I. rHDL modeling and the anchoring mechanism of LCAT activation. J. Lipid Res. 2021, 62, 100006. [Google Scholar] [CrossRef]
- Singh, S.A.; Andraski, A.B.; Higashi, H.; Lee, L.H.; Ramsaroop, A.; Sacks, F.M.; Aikawa, M. Metabolism of PLTP, CETP, and LCAT on multiple HDL sizes using the Orbitrap Fusion Lumos. JCI Insight 2021, 6, e143526. [Google Scholar] [CrossRef]
- von Eckardstein, A.; Nordestgaard, B.G.; Remaley, A.T.; Catapano, A.L. High-density lipoprotein revisited: Biological functions and clinical relevance. Eur. Heart J. 2023, 44, 1394–1407. [Google Scholar] [CrossRef]
- Chandrasekaran, P.; Weiskirchen, R. The Role of SCAP/SREBP as Central Regulators of Lipid Metabolism in Hepatic Steatosis. Int. J. Mol. Sci. 2024, 25, 1109. [Google Scholar] [CrossRef]
- Huang, L.; Fan, B.; Ma, A.; Shaul, P.W.; Zhu, H. Inhibition of ABCA1 protein degradation promotes HDL cholesterol efflux capacity and RCT and reduces atherosclerosis in mice. J. Lipid Res. 2015, 56, 986–997. [Google Scholar] [CrossRef]
- Wang, B.; Chen, R.; Yin, T.; Li, Y.; Xi, Z.; Li, B.; Chu, X.M. Fucoidan: A marine-derived polysaccharide with therapeutic potential in atherosclerotic cardiovascular diseases: A review. Int. J. Biol. Macromol. 2025, 321, 146055. [Google Scholar] [CrossRef]
- Zhang, Z.; Guo, J. Deciphering Oxidative Stress in Cardiovascular Disease Progression: A Blueprint for Mechanistic Understanding and Therapeutic Innovation. Antioxidants 2024, 14, 38. [Google Scholar] [CrossRef]
- Jebari-Benslaiman, S.; Galicia-Garcia, U.; Larrea-Sebal, A.; Olaetxea, J.R.; Alloza, I.; Vandenbroeck, K.; Benito-Vicente, A.; Martin, C. Pathophysiology of Atherosclerosis. Int. J. Mol. Sci. 2022, 23, 3346. [Google Scholar] [CrossRef] [PubMed]
- Casula, M.; Colpani, O.; Xie, S.; Catapano, A.L.; Baragetti, A. HDL in Atherosclerotic Cardiovascular Disease: In Search of a Role. Cells 2021, 10, 1869. [Google Scholar] [CrossRef] [PubMed]
- Vaisar, T.; Pennathur, S.; Green, P.S.; Gharib, S.A.; Hoofnagle, A.N.; Cheung, M.C.; Byun, J.; Vuletic, S.; Kassim, S.; Singh, P.; et al. Shotgun proteomics implicates protease inhibition and complement activation in the antiinflammatory properties of HDL. J. Clin. Investig. 2007, 117, 746–756. [Google Scholar] [CrossRef] [PubMed]
- Habash, N.; Abdul-Rasheed, O.; Salman, M. The Association of Single Nucleotide Polymorphism rs5883 in The CETP Gene with Oxidized-LDL Level in Coronary Atherosclerosis Patients: CETP gene and Coronary Atherosclerosis. Iraqi J. Cancer Med. Genet. 2023, 16, 93–99. [Google Scholar] [CrossRef]
- Libby, P. The changing landscape of atherosclerosis. Nature 2021, 592, 524–533. [Google Scholar] [CrossRef]
- Munno, M.; Mallia, A.; Greco, A.; Modafferi, G.; Banfi, C.; Eligini, S. Radical Oxygen Species, Oxidized Low-Density Lipoproteins, and Lectin-like Oxidized Low-Density Lipoprotein Receptor 1: A Vicious Circle in Atherosclerotic Process. Antioxidants 2024, 13, 583. [Google Scholar] [CrossRef]
- Packard, C.J.; Demant, T.; Stewart, J.P.; Bedford, D.; Caslake, M.J.; Schwertfeger, G.; Bedynek, A.; Shepherd, J.; Seidel, D. Apolipoprotein B metabolism and the distribution of VLDL and LDL subfractions. J. Lipid Res. 2000, 41, 305–318. [Google Scholar] [CrossRef]
- Gu, H.M.; Li, G.; Gao, X.; Berthiaume, L.G.; Zhang, D.W. Characterization of palmitoylation of ATP binding cassette transporter G1: Effect on protein trafficking and function. Biochim. Biophys. Acta 2013, 1831, 1067–1078. [Google Scholar] [CrossRef]
- Singaraja, R.R.; Kang, M.H.; Vaid, K.; Sanders, S.S.; Vilas, G.L.; Arstikaitis, P.; Coutinho, J.; Drisdel, R.C.; El-Husseini Ael, D.; Green, W.N.; et al. Palmitoylation of ATP-binding cassette transporter A1 is essential for its trafficking and function. Circ. Res. 2009, 105, 138–147. [Google Scholar] [CrossRef]
- Ye, Z.; Lu, Y.; Wu, T. The impact of ATP-binding cassette transporters on metabolic diseases. Nutr. Metab. 2020, 17, 61. [Google Scholar] [CrossRef]
- Li, X.; Zhou, Y.; Yu, C.; Yang, H.; Zhang, C.; Ye, Y.; Xiao, S. Paeonol suppresses lipid accumulation in macrophages via upregulation of the ATP—binding cassette transporter A1 and downregulation of the cluster of differentiation 36. Int. J. Oncol. 2015, 46, 764–774. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Ye, Z.M.; Chen, S.; Luo, X.Y.; Chen, S.L.; Mao, L.; Li, Y.; Jin, H.; Yu, C.; Xiang, F.X.; et al. MicroRNA-23a-5p promotes atherosclerotic plaque progression and vulnerability by repressing ATP-binding cassette transporter A1/G1 in macrophages. J. Mol. Cell. Cardiol. 2018, 123, 139–149. [Google Scholar] [CrossRef] [PubMed]
- Jeon, B.H.; Lee, Y.H.; Yun, M.R.; Kim, S.H.; Lee, B.W.; Kang, E.S.; Lee, H.C.; Cha, B.S. Increased expression of ATP-binding cassette transporter A1 (ABCA1) as a possible mechanism for the protective effect of cilostazol against hepatic steatosis. Metabolism 2015, 64, 1444–1453. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Yan, X.; Xia, M.; Yang, Y.; Li, D.; Li, X.; Song, F.; Ling, W. Coenzyme Q10 promotes macrophage cholesterol efflux by regulation of the activator protein-1/miR-378/ATP-binding cassette transporter G1-signaling pathway. Arterioscler. Thromb. Vasc. Biol. 2014, 34, 1860–1870. [Google Scholar] [CrossRef]
- Lv, Y.C.; Yang, J.; Yao, F.; Xie, W.; Tang, Y.Y.; Ouyang, X.P.; He, P.P.; Tan, Y.L.; Li, L.; Zhang, M.; et al. Diosgenin inhibits atherosclerosis via suppressing the MiR-19b-induced downregulation of ATP-binding cassette transporter A1. Atherosclerosis 2015, 240, 80–89. [Google Scholar] [CrossRef]
- Song, G.; Lin, Q.; Zhao, H.; Liu, M.; Ye, F.; Sun, Y.; Yu, Y.; Guo, S.; Jiao, P.; Wu, Y.; et al. Hydrogen Activates ATP-Binding Cassette Transporter A1-Dependent Efflux Ex Vivo and Improves High-Density Lipoprotein Function in Patients With Hypercholesterolemia: A Double-Blinded, Randomized, and Placebo-Controlled Trial. J. Clin. Endocrinol. Metab. 2015, 100, 2724–2733. [Google Scholar] [CrossRef]
- Li, D.; Xiong, Q.; Peng, J.; Hu, B.; Li, W.; Zhu, Y.; Shen, X. Hydrogen Sulfide Up-Regulates the Expression of ATP-Binding Cassette Transporter A1 via Promoting Nuclear Translocation of PPARalpha. Int. J. Mol. Sci. 2016, 17, 635. [Google Scholar] [CrossRef]
- Li, X.; Huang, X.; Song, K.; Liu, J.; Jin, Y.; Li, T.; Zhang, L.; Zhang, H. Qingre Sanjie Formula alleviates atherosclerosis by promoting LXR-alpha/ABCG5/G8-mediated reverse cholesterol transport and bile acid synthesis. Phytomedicine 2025, 142, 156691. [Google Scholar] [CrossRef]
- Chen, W.M.; Sheu, W.H.; Tseng, P.C.; Lee, T.S.; Lee, W.J.; Chang, P.J.; Chiang, A.N. Modulation of microRNA Expression in Subjects with Metabolic Syndrome and Decrease of Cholesterol Efflux from Macrophages via microRNA-33-Mediated Attenuation of ATP-Binding Cassette Transporter A1 Expression by Statins. PLoS ONE 2016, 11, e0154672. [Google Scholar] [CrossRef]
- Chen, J.; Gao, J.; Yang, J.; Zhang, Y.; Wang, L. Effect of triptolide on the regulation of ATP—binding cassette transporter A1 expression in lipopolysaccharide—induced acute lung injury of rats. Mol. Med. Rep. 2014, 10, 3015–3020. [Google Scholar] [CrossRef][Green Version]
- Katz, A.; Udata, C.; Ott, E.; Hickey, L.; Burczynski, M.E.; Burghart, P.; Vesterqvist, O.; Meng, X. Safety, pharmacokinetics, and pharmacodynamics of single doses of LXR-623, a novel liver X-receptor agonist, in healthy participants. J. Clin. Pharmacol. 2009, 49, 643–649. [Google Scholar] [CrossRef]
- Tardif, J.C.; Gregoire, J.; L’Allier, P.L.; Ibrahim, R.; Lesperance, J.; Heinonen, T.M.; Kouz, S.; Berry, C.; Basser, R.; Lavoie, M.A.; et al. Effects of reconstituted high-density lipoprotein infusions on coronary atherosclerosis: A randomized controlled trial. JAMA 2007, 297, 1675–1682. [Google Scholar] [CrossRef]
- Bloomfield, D.; Carlson, G.L.; Sapre, A.; Tribble, D.; McKenney, J.M.; Littlejohn, T.W., 3rd; Sisk, C.M.; Mitchel, Y.; Pasternak, R.C. Efficacy and safety of the cholesteryl ester transfer protein inhibitor anacetrapib as monotherapy and coadministered with atorvastatin in dyslipidemic patients. Am. Heart J. 2009, 157, 352–360.e2. [Google Scholar] [CrossRef] [PubMed]
- Stein, E.A.; Stroes, E.S.; Steiner, G.; Buckley, B.M.; Capponi, A.M.; Burgess, T.; Niesor, E.J.; Kallend, D.; Kastelein, J.J. Safety and tolerability of dalcetrapib. Am. J. Cardiol. 2009, 104, 82–91. [Google Scholar] [CrossRef] [PubMed]
- Moriarty, P.M.; Thompson, P.D.; Cannon, C.P.; Guyton, J.R.; Bergeron, J.; Zieve, F.J.; Bruckert, E.; Jacobson, T.A.; Kopecky, S.L.; Baccara-Dinet, M.T.; et al. Efficacy and safety of alirocumab vs ezetimibe in statin-intolerant patients, with a statin rechallenge arm: The ODYSSEY ALTERNATIVE randomized trial. J. Clin. Lipidol. 2015, 9, 758–769. [Google Scholar] [CrossRef] [PubMed]
- Ma, C.; Zhang, W.; Yang, X.; Liu, Y.; Liu, L.; Feng, K.; Zhang, X.; Yang, S.; Sun, L.; Yu, M.; et al. Functional interplay between liver X receptor and AMP-activated protein kinase alpha inhibits atherosclerosis in apolipoprotein E-deficient mice—A new anti-atherogenic strategy. Br. J. Pharmacol. 2018, 175, 1486–1503. [Google Scholar] [CrossRef]
- Fitzgerald, M.L.; Mujawar, Z.; Tamehiro, N. ABC transporters, atherosclerosis and inflammation. Atherosclerosis 2010, 211, 361–370. [Google Scholar] [CrossRef]
- Cao, J.; Xu, Y.; Shang, L.; Liu, H.-M.; Du, F.; Yu, H. Effect of The Apolipoprotein E Mimetic Peptide EpK on Atherosclerosis in apoE(−/−) Mice. Prog. Biochem. Biophys. 2015, 42, 833–842. [Google Scholar] [CrossRef]
- O’Brien, J.; Hayder, H.; Zayed, Y.; Peng, C. Overview of MicroRNA Biogenesis, Mechanisms of Actions, and Circulation. Front. Endocrinol. 2018, 9, 402. [Google Scholar] [CrossRef]
- Ono, K.; Horie, T.; Nishino, T.; Baba, O.; Kuwabara, Y.; Kimura, T. MicroRNAs and High-Density Lipoprotein Cholesterol Metabolism. Int. Heart J. 2015, 56, 365–371. [Google Scholar] [CrossRef]
- Goedeke, L.; Aranda, J.F.; Fernandez-Hernando, C. microRNA regulation of lipoprotein metabolism. Curr. Opin. Lipidol. 2014, 25, 282–288. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Ma, S.; Hu, Y.; Ling, J.; Wang, Z.; Wang, J.; Chen, J.; Zhang, Y. Auricularia heimuer Ameliorates Oxidative Stress and Inflammation to Inhibit Atherosclerosis Development in ApoE(−/−) Mice. Nutrients 2025, 17, 2799. [Google Scholar] [CrossRef] [PubMed]
- Feng, J. Role of curcumin in altering gut microbiota for anti-obesity and anti-hyperlipidemic effects. Front. Microbiol. 2025, 16, 1625098. [Google Scholar] [CrossRef] [PubMed]
- Ekawa, K.; Marumo, M.; Wakabayashi, I. Antithrombotic Action of Resveratrol: Particularly Regarding Inhibition of Platelet Aggregation. Yakugaku Zasshi 2025, 145, 765–776. [Google Scholar] [CrossRef]
- Zhu, X.; Chen, Y.; Xu, B.; Mou, J.; Wang, M.; Gu, Q.; Sun, Q.; Li, M.; Zhao, C.; Zeng, M.; et al. Targeting KEAP1/NRF2 interaction with oleuropein ameliorates atherosclerosis by inhibiting macrophage ferroptosis. Free Radic. Biol. Med. 2025, 240, 566–582. [Google Scholar] [CrossRef]
- Jim, E.L.; Jim, E.L.; Surya, R.; Permatasari, H.K.; Nurkolis, F. Marine-Derived Polymers-Polysaccharides as Promising Natural Therapeutics for Atherosclerotic Cardiovascular Disease. Mar. Drugs 2025, 23, 325. [Google Scholar] [CrossRef]
- Duan, Y.; Gong, K.; Xu, S.; Zhang, F.; Meng, X.; Han, J. Regulation of cholesterol homeostasis in health and diseases: From mechanisms to targeted therapeutics. Signal Transduct. Target. Ther. 2022, 7, 265. [Google Scholar] [CrossRef]
- Ma, C.; Feng, K.; Yang, X.; Yang, Z.; Wang, Z.; Shang, Y.; Fan, G.; Liu, L.; Yang, S.; Li, X.; et al. Targeting macrophage liver X receptors by hydrogel-encapsulated T0901317 reduces atherosclerosis without effect on hepatic lipogenesis. Br. J. Pharmacol. 2021, 178, 1620–1638. [Google Scholar] [CrossRef]
- Ouimet, M.; Barrett, T.J.; Fisher, E.A. HDL and Reverse Cholesterol Transport. Circ. Res. 2019, 124, 1505–1518. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).