Oxidative Stress and Inflammatory Status in COVID-19 Outpatients: A Health Center-Based Analytical Cross-Sectional Study
Abstract
:1. Introduction
2. Methods and Materials
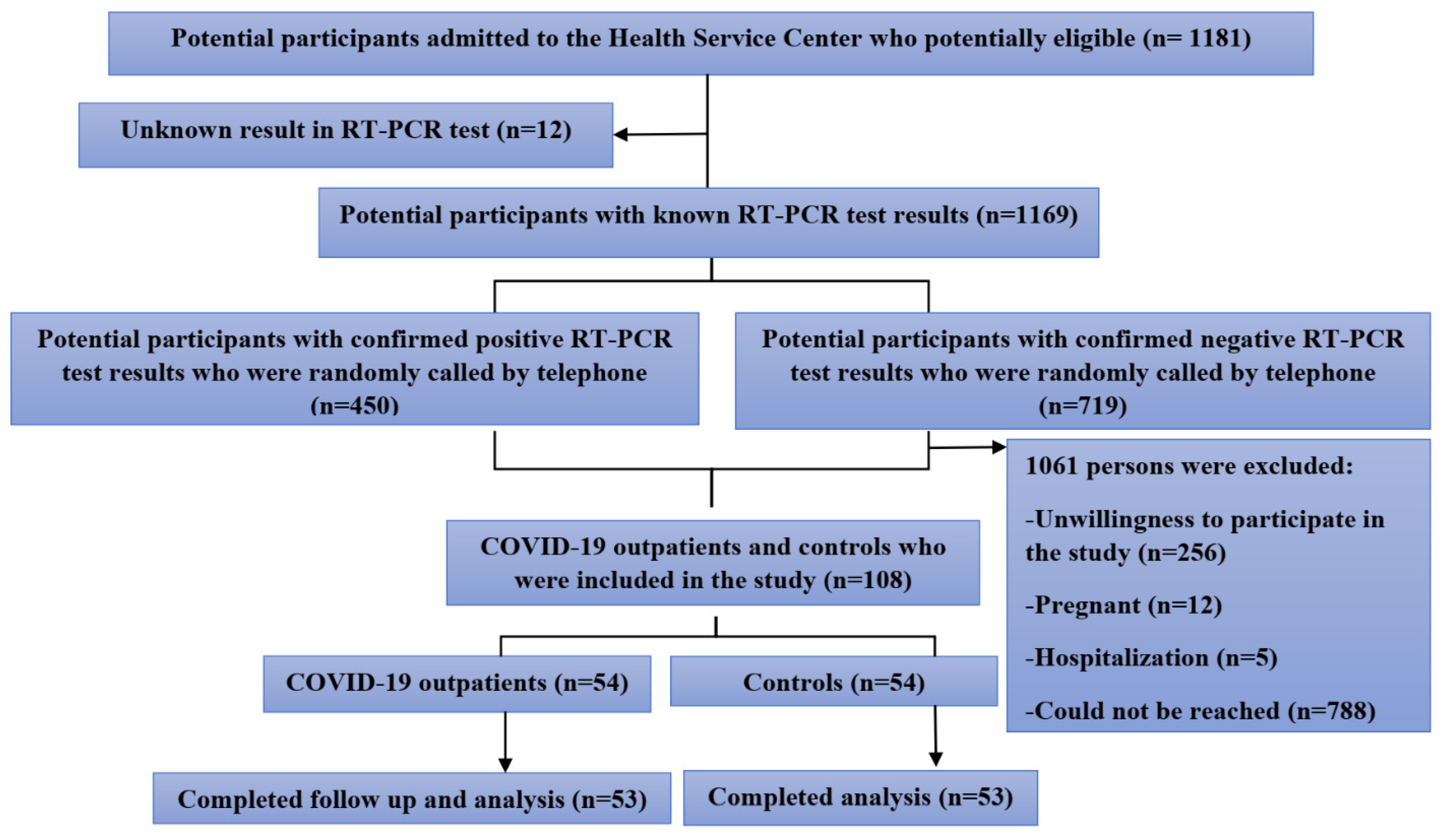
2.1. Participants
2.2. Study Design
2.3. Anthropometric Measurements
2.4. Blood Sampling
2.5. Assessment of Oxidative Stress Markers
2.5.1. Measurement of SAA
2.5.2. Measurement of TAC
2.5.3. SOD Assay Method
2.5.4. GPx Assay Method
2.6. Primary and Secondary Outcome Measures and Confounders
2.7. Statistical Analysis
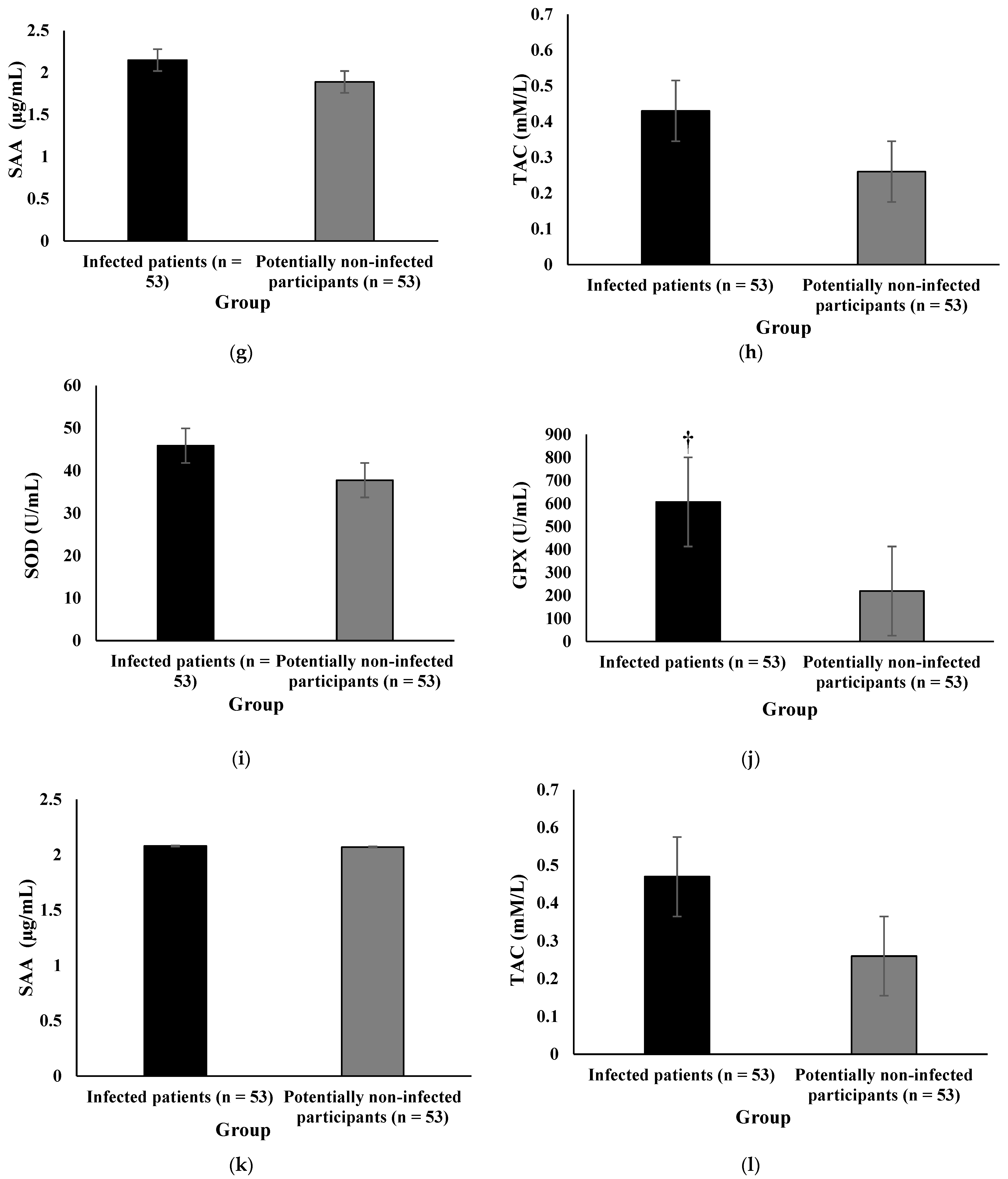
3. Results
Patient Characteristics
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhou, T.; Liu, Q.; Yang, Z.; Liao, J.; Yang, K.; Bai, W.; Lu, X.; Zhang, W. Preliminary prediction of the basic reproduction number of the Wuhan novel coronavirus 2019-nCoV. J. Evid. Based Med. 2020, 13, 3–7. [Google Scholar] [CrossRef]
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Ji, P.; Zhu, J.; Zhong, Z.; Li, H.; Pang, J.; Li, B.; Zhang, J. Association of elevated inflammatory markers and severe COVID-19: A me-ta-analysis. Medicine 2020, 99, e23315. [Google Scholar] [CrossRef] [PubMed]
- Del Valle, D.M.; Kim-Schulze, S.; Huang, H.H.; Beckmann, N.D.; Nirenberg, S.; Wang, B.; Lavin, Y.; Swartz, T.H.; Madduri, D.; Stock, A.; et al. An inflammatory cytokine signature predicts COVID-19 severity and survival. Nat. Med. 2020, 26, 1636–1643. [Google Scholar] [CrossRef]
- Zeng, F.; Huang, Y.; Guo, Y.; Yin, M.; Chen, X.; Xiao, L.; Deng, G. Association of inflammatory markers with the severity of COVID-19: A meta-analysis. Int. J. Infect. Dis. 2020, 96, 467–474. [Google Scholar] [CrossRef] [PubMed]
- Hariyanto, T.I.; Japar, K.V.; Kwenandar, F.; Damay, V.; Siregar, J.I.; Lugito, N.P.H.; Tjiang, M.M.; Kurniawan, A. Inflammatory and hematologic markers as predictors of severe outcomes in COVID-19 infection: A systematic review and meta-analysis. Am. J. Emerg. Med. 2020, 41, 110–119. [Google Scholar] [CrossRef] [PubMed]
- Lin, Z.; Long, F.; Yang, Y.; Chen, X.; Xu, L.; Yang, M. Serum ferritin as an independent risk factor for severity in COVID-19 patients. J. Infect. 2020, 81, 647–679. [Google Scholar] [CrossRef] [PubMed]
- Yip, T.T.; Chan, J.W.; Cho, W.C.; Yip, T.T.; Wang, Z.; Kwan, T.L.; Law, S.C.; Tsang, D.N.; Chan, J.K.; Lee, K.-C.; et al. Protein chip array profiling analysis in patients with severe acute respiratory syndrome identified serum amyloid a protein as a biomarker potentially useful in monitoring the extent of pneumonia. Clin. Chem. 2005, 51, 47–55. [Google Scholar] [CrossRef] [Green Version]
- Gómez-Ambrosi, J.; Salvador, J.; Rotellar, F.; Silva, C.; Catalán, V.; Rodríguez, A.; Gil, M.J.; Frühbeck, G. Increased Serum Amyloid A Concentrations in Morbid Obesity Decrease after Gastric Bypass. Obes. Surg. 2006, 16, 262–269. [Google Scholar] [CrossRef]
- Cheng, K.B.; Wei, M.; Shen, H.; Wu, C.; Chen, D.; Xiong, W. Clinical characteristics of 463 patients with common and severe type coronavirus disease. Shanghai Med. J. 2020, 1, 1–15. (In Chinese) [Google Scholar]
- Xiang, T.X.L.J.; Liu, J.; Xu, F.; Cheng, N.; Liu, Y.; Qian, K.J. Analysis of clinical characteristics of 49 patients with Novel Coronavirus Pneumonia in Jiangxi province. Chin. J. Respir. Crit. Care Med. 2020, 19, 1–7. (In Chinese) [Google Scholar]
- Zhang, J.; Dong, X.; Cao, Y.; Yuan, Y.; Yang, Y.; Yan, Y.; Akdis, C.A.; Gao, Y. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy 2020, 75, 1730–1741. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Liu, H.G.; Liu, W.; Liu, J.; Liu, K.; Shang, J.; Deng, Y.; Wei, S. Analysis of clinical features of 29 patients with 2019 novel coronavirus pneumonia. Zhonghua Jie He He Hu Xi Za Zhi 2020, 43, 203–208. [Google Scholar] [PubMed]
- Rael, L.T.; Bar-Or, R.; Salottolo, K.; Mains, C.W.; Slone, D.S.; Offner, P.J.; Bar-Or, D. Injury severity and serum amyloid A correlate with plasma oxidation-reduction potential in multi-trauma patients: A retrospective analysis. Scand. J. Trauma Resusc. Emerg. Med. 2009, 17, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suresh, D.R.; Annam, V.; Pratibha, K.; Prasad, B.V.M. Total antioxidant capacity-a novel early bio-chemical marker of oxidative stress in HIV infected individuals. J. Biomed. Sci. 2009, 16, 61–64. [Google Scholar] [CrossRef] [Green Version]
- Hussain, T.; Tan, B.; Yin, Y.; Blachier, F.; Tossou, M.C.; Rahu, N. Oxidative Stress and Inflammation: What Polyphenols Can Do for Us? Oxidative Med. Cell Longev. 2016, 2016, 7432797. [Google Scholar] [CrossRef] [Green Version]
- Nediani, C.; Giovannelli, L. Oxidative Stress and Inflammation as Targets for Novel Preventive and Therapeutic Approches in Non Communicable Diseases. Antioxidants 2020, 9, 290. [Google Scholar] [CrossRef] [Green Version]
- Bolukbas, C.; Bolukbas, F.F.; Horoz, M.; Aslan, M.; Celik, H.; Erel, O. Increased oxidative stress associated with the severity of the liver disease in various forms of hepatitis B virus infection. BMC Infect. Dis. 2005, 5, 95. [Google Scholar] [CrossRef] [Green Version]
- Cecchini, R.; Cecchini, A.L. SARS-CoV-2 infection pathogenesis is related to oxidative stress as a response to aggression. Med. Hypotheses 2020, 143, 110102. [Google Scholar] [CrossRef]
- Naghashpour, M.; Ghiassian, H.; Mobarak, S.; Adelipour, M.; Piri, M.; Seyedtabib, M.; Golabi, S. Profiling serum levels of glutathione reductase and interleukin-10 in positive and negative-PCR COVID-19 outpatients: A comparative study from southwestern Iran. J. Med. Virol. 2021, 94, 1457–1464. [Google Scholar] [CrossRef]
- Pandey, K.B.; Rizvi, S.I. Markers of Oxidative Stress in Erythrocytes and Plasma During Aging in Humans. Oxidative Med. Cell. Longev. 2010, 3, 2–12. [Google Scholar] [CrossRef] [PubMed]
- Heer, C.D.; Davis, A.B.; Riffe, D.B.; Wagner, B.A.; Falls, K.C.; Allen, B.G.; Buettner, G.R.; Beardsley, R.A.; Riley, D.P.; Spitz, D.R. Superoxide Dismutase Mimetic GC4419 Enhances the Oxidation of Pharmacological Ascorbate and Its Anticancer Effects in an H2O2-Dependent Manner. Antioxidants 2018, 7, 18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cemek, M.; Caksen, H.; Bayiroğlu, F.; Cemek, F.; DeDe, S.; Bayıroğlu, F. Oxidative stress and enzymic–non-enzymic antioxidant responses in children with acute pneumonia. Cell Biochem. Funct. 2006, 24, 269–273. [Google Scholar] [CrossRef] [PubMed]
- Mehri, F.; Rahbar, A.H.; Ghane, E.T.; Souri, B.; Esfahani, M. The comparison of oxidative markers between COVID-19 patients and healthy subjects. Arch Med Res. 2021, 52, 843–849. [Google Scholar] [CrossRef]
- Tan, B.L.; Norhaizan, M.E.; Liew, W.-P.-P.; Rahman, H.S. Antioxidant and Oxidative Stress: A Mutual Interplay in Age-Related Diseases. Front. Pharmacol. 2018, 9, 1162. [Google Scholar] [CrossRef] [Green Version]
- Liguori, I.; Russo, G.; Curcio, F.; Bulli, G.; Aran, L.; Della-Morte, D.; Gargiulo, G.; Testa, G.; Cacciatore, F.; Bonaduce, D.; et al. Oxidative stress, aging, and diseases. Clin. Interv. Aging. 2018, 13, 757–772. [Google Scholar] [CrossRef] [Green Version]
- Sofic, E.; Rustembegovic, A.; Kroyer, G.; Cao, G. Serum antioxidant capacity in neurological, psychiatric, renal diseases and cardiomyopathy. J. Neural Transm. 2002, 109, 711–719. [Google Scholar] [CrossRef]
- Bruha, R.; Vítek, L.; Marecek, Z.; Pospisilova, L.; Nevsimalova, S.; Martasek, P.; Petrtyl, J.; Urbánek, P.; Jiraskova, A.; Malíková, I.; et al. Decreased serum antioxidant capacity in patients with Wilson disease is associated with neurological symptoms. J. Inherit. Metab. Dis. 2011, 35, 541–548. [Google Scholar] [CrossRef]
- Hadžović-Džuvo, A.; Lepara, O.; Valjevac, A.; Avdagić, N.; Hasić, S.; Kiseljaković, E.; Ibragić, S.; Alajbegović, A. Serum total antioxidant capacity in patients with multiple sclerosis. Bosn. J. Basic Med. Sci. 2011, 11, 33–36. [Google Scholar] [CrossRef] [Green Version]
- Nieto, F.J.; Iribarren, C.; Gross, M.D.; Comstock, G.W.; Cutler, R.G. Uric acid and serum antioxidant capacity: A reaction to athero-sclerosis? Atherosclerosis 2000, 148, 131–139. [Google Scholar] [CrossRef]
- Abbasi, M.D.M.; Hedayati, M.; Mottaghi, M.; Pourvali, K.; Azizi, F. The relationship between MnSOD Val16Ala gene polymorphism and the level of serum total antioxidant capacity with the risk of chronic kidney disease in type 2 diabetic patients: A nested case-control study in the Tehran lipid glucose study. Nutr. Metab. Volume. 2018, 15, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Çakırca, G.; Çakırca, T.D.; Üstünel, M.; Torun, A.; Koyuncu, I. Thiol level and total oxidant/antioxidant status in patients with COVID-19 infection. Ir. J. Med. Sci. 2021, 1971, 1–6. [Google Scholar] [CrossRef]
- Karkhanei, B.; Ghane, E.T.; Mehri, F. Evaluation of oxidative stress level: Total antioxidant capacity, total oxidant status and glutathione activity in patients with COVID-19. New Microbes New Infect. 2021, 42, 100897. [Google Scholar] [CrossRef] [PubMed]
- COVID-19 (Coronavirus Disease): People with Certain Medical Conditions. Available online: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html (accessed on 7 December 2020).
- McIntosh, K. COVID-19: Clinical Features: Wolters Kluwer; 2021. Available online: https://www.uptodate.com/contents/covid-19-clinical-features#H2858229650 (accessed on 4 February 2022).
- Sethuram, R.; Bai, D.; Abu-Soud, H.M. Potential Role of Zinc in the COVID-19 Disease Process and its Probable Impact on Reproduction. Reprod. Sci. 2021, 1–6. [Google Scholar] [CrossRef]
- Pham-Huy, L.A.; He, H.; Pham-Huy, C. Free Radicals, Antioxidants in Disease and Health. Int. J. Biomed. Sci. 2008, 4, 89. [Google Scholar] [PubMed]
- Gong, J.; Dong, H.; Xia, Q.S.; Huang, Z.Y.; Wang, D.K.; Zhao, Y.; Liu, W.; Tu, S.; Zhang, M.; Wang, Q.; et al. Correlation analysis between disease severity and inflamma-tion-related parameters in patients with COVID-19: A retrospective study. BMC Infect Dis. 2020, 20, 963. [Google Scholar] [CrossRef]
- Qin, C.; Zhou, L.; Hu, Z.; Zhang, S.; Yang, S.; Tao, Y.; Xie, C.; Ma, K.; Shang, K.; Wang, W.; et al. Dysregulation of Immune Response in Patients With Coronavirus 2019 (COVID-19) in Wuhan, China. Clin. Infect. Dis. 2020, 71, 762–768. [Google Scholar] [CrossRef]
- Cai, X.; Ahmad, G.; Hossain, F.; Liu, Y.; Wang, X.; Dennis, J.; Freedman, B.; Witting, P.K. High-Density Lipoprotein (HDL) Inhibits Serum Amyloid A (SAA)-Induced Vascular and Renal Dysfunctions in Apolipoprotein E-Deficient Mice. Int. J. Mol. Sci. 2020, 21, 1316. [Google Scholar] [CrossRef] [Green Version]
- Heinrich, P.C.; Behrmann, I.; Müller-Newen, G.; Schaper, F.; Graeve, L. Interleukin-6-type cytokine signalling through the gp130/Jak/STAT pathway. Biochem. J. 1998, 334, 297–314. [Google Scholar] [CrossRef] [Green Version]
- Heinrich, P.C.; Castell, J.V.; Andus, T. Interleukin-6 and the acute phase response. Biochem. J. 1990, 265, 621–636. [Google Scholar] [CrossRef]
- Jain, S.; Gautam, V.; Naseem, S. Acute-phase proteins: As diagnostic tool. J. Pharm. Bioallied Sci. 2011, 3, 118–127. [Google Scholar] [CrossRef]
- Lannergård, A.; Larsson, A.; Kragsbjerg, P.; Friman, G. Correlations between serum amyloid A protein and C-reactive protein in infectious diseases. Scand. J. Clin. Lab. Investig. 2003, 63, 267–272. [Google Scholar] [CrossRef]
- Jung, S.Y.; Park, M.-C.; Park, Y.-B.; Lee, S.-K. Serum Amyloid A as a Useful Indicator of Disease Activity in Patients with Ankylosing Spondylitis. Yonsei Med. J. 2007, 48, 218–224. [Google Scholar] [CrossRef] [Green Version]
- Kermali, M.; Khalsa, R.K.; Pillai, K.; Ismail, Z.; Harky, A. The role of biomarkers in diagnosis of COVID-19-A systematic review. Life Sci. 2020, 254, 117788. [Google Scholar] [CrossRef]
- Meng, Z.; Guo, S.; Zhou, Y.; Li, M.; Wang, M.; Ying, B. Applications of laboratory findings in the prevention, diagnosis, treatment, and monitoring of COVID-19. Signal Transduct. Target. Ther. 2021, 6, 1–26. [Google Scholar] [CrossRef]
- Camini, F.C.; Da Silva Caetano, C.C.; Almeida, L.T.; De Brito Magalhães, C.L. Implications of oxidative stress on viral pathogenesis. Arch. Virol. 2016, 162, 907–917. [Google Scholar] [CrossRef]
- Giugliano, D.; Ceriello, A.; Esposito, K. The Effects of Diet on Inflammation: Emphasis on the Metabolic Syndrome. J. Am. Coll. Cardiol. 2006, 48, 677–685. [Google Scholar] [CrossRef] [Green Version]
- Golabi, S.; Adelipour, M.; Mobarak, S.; Piri, M.; Seyedtabib, M.; Bagheri, R.; Suzuki, K.; Ashtary-Larky, D.; Maghsoudi, F.; Naghashpour, M. The Association between Vitamin D and Zinc Status and the Progression of Clinical Symptoms among Outpatients Infected with SARS-CoV-2 and Potentially Non-Infected Participants: A Cross-Sectional Study. Nutrients 2021, 13, 3368. [Google Scholar] [CrossRef]
- Qu, R.; Ling, Y.; Zhang, Y.H.; Wei, L.Y.; Chen, X.; Li, X.M.; Liu, X.; Liu, H.; Guo, Z.; Ren, H.; et al. Platelet-to-lymphocyte ratio is associated with prognosis in patients with coronavirus disease-19. J. Med. Virol. 2020, 92, 1533–1541. [Google Scholar] [CrossRef]
- The Role of Spike-ACE2 Interaction in Pulmonary Blood Pressure Regulation. FAIRDOM Hub. 2020. Available online: https://fairdomhub.org/models/709 (accessed on 27 May 2020).
- Mardani, R.; Ahmadi Vasmehjani, A.; Zali, F.; Gholami, A.; Mousavi Nasab, S.D.; Kaghazian, H.; Kaviani, M.; Ahmadi, N. Laboratory Parameters in Detection of COVID-19 Patients with Positive RT-PCR; a Diagnostic Accuracy Study. Arch. Acad. Emerg. Med. 2020, 8, e43. [Google Scholar]
- Iddir, M.; Brito, A.; Dingeo, G.; Del Campo, S.S.F.; Samouda, H.; La Frano, M.R.; Bohn, T. Strengthening the Immune System and Reducing Inflammation and Oxidative Stress through Diet and Nutrition: Considerations during the COVID-19 Crisis. Nutrients 2020, 12, 1562. [Google Scholar] [CrossRef] [PubMed]


| Characteristics | COVID-19 Outpatients (n = 53) | Controls (n = 53) | p-Value | |
|---|---|---|---|---|
| Age (year) | 41 ± 12.9 | 40 ± 13.4 | 0.609 | |
| <50 | 40 (18.4%) | 42 (79.2%) | ||
| 50–64 | 9 (17.6%) | 9 (17.0%) | 0.995 | |
| ≥65 | 2 (3.9%) | 2 (3.8%) | ||
| Sex | ||||
| Female | 17 (32.1%) | 15 (28.3%) | ||
| Male | 36 (67.9%) | 38 (71.7%) | 0.416 | |
| Married status | ||||
| Single | 12 (22.6%) | 12 (22.6%) | 0.592 | |
| Married | 41 (77.4%) | 41 (77.4%) | ||
| Education levels | ||||
| Illiterate | 2 (3.8%) | 1 (1.9%) | 0.754 | |
| Less than high school | 15 (28.8%) | 19 (36.8%) | ||
| High school | 13 (25%) | 10 (19.2%) | ||
| College education | 22 (42.3%) | 22 (42.3%) | ||
| Cigarette smoking | ||||
| No | 40 (75.5%) | 45 (84.9%) | 0.165 | |
| Yes | 13 (24.5%) | 8 (15.1%) | ||
| RR (number/min) | 14.1 ± 1.62 | 13 ± 1.9 | 0.001 | |
| PR (number/min) | 90.71 ± 18 | 87.23 ± 13.3 | 0.271 | |
| SpO2 (%) | 96.9 ± 1.35 | 97.4 ± 1.23 | 0.032 | |
| Duration of infection (day) | 6.5 ± 2 | - | ||
| BMI (kg/m2) | 27.1 ± 4.7 | 27.5 ± 4.3 | 0.663 | |
| CRP | ||||
| Negative | 37 (69.8%) | 48 (90.6%) | 0.007 | |
| Positive | 16 (30.2%) | 5 (9.4%) | ||
| WBC, 10 × 3/µL | 6 ± 1.3 | 6.8 ± 2 | 0.014 | |
| RBC, 10 × 3/µL | 4.8 ± 0.6 | 4.6 ± 0.5 | 0.021 | |
| HGB, g/dL | 14 ± 1.4 | 13.2 ± 1.6 | 0.007 | |
| HCT, % | 41 ± 4.1 | 38.7 ± 4.1 | 0.005 | |
| MCV, fL | 85.1 ± 6.7 | 85 ± 6.8 | 0.939 | |
| MCH, pg | 29.3 ± 2.5 | 29 ± 2.8 | 0.593 | |
| MCHC, g/dL | 34.4 ± 0.8 | 34.1 ± 1.3 | 0.114 | |
| RDW, % | 13.1 ± 1 | 13.5 ± 1.1 | 0.109 | |
| MPV, % | 9.8 ± 1.1 | 9.2 ± 0.9 | 0.004 | |
| PDW, % | 16.9 ± 0.5 | 17.1 ± 1.6 | 0.398 | |
| Platelets | 250.1 ± 72.2 | 236.6 ± 64.8 | 0.312 | |
| NEU, % | 52.9 ± 8.5 | 52.2 ± 9.4 | 0.657 | |
| LYM, % | 42.4 ± 8.8 | 43.3 ± 9.2 | 0.612 | |
| MNC, % | 3.7 ± 1.2 | 3.4 ± 1.3 | 0.285 | |
| EOS, % | 1.4 ± 0.6 | 1.5 ± 0.6 | 0.574 | |
| Comorbidities | COVID-19 Outpatients (n = 53) | Controls (n = 53) | p-Value | |
|---|---|---|---|---|
| Hypertension, n (%) | ||||
| Yes | 10 (18.9) | 5 (9.4) | ||
| No | 43 (81.1) | 48 (90.6) | 0.164 | |
| Type 2 diabetes mellitus, n (%) | ||||
| Yes | 6 (11.3) | 4 (7.5) | ||
| No | 47 (88.7) | 49 (92.5) | 0.506 | |
| Obesity, n (%) | ||||
| Yes | 13 (24.5) | 21 (39.6) | ||
| No | 40 (75.5) | 32 (60.4) | 0.096 | |
| Malnutrition, n (%) | ||||
| Yes | 1 (1.9) | 0 (0.00) | ||
| No | 52 (98.1) | 53 (100) | 0.096 | |
| Asthma and allergy, n (%) | ||||
| Yes | 6 (11.3) | 5 (9.4) | ||
| No | 47 (88.7) | 48 (90.6) | 0.500 | |
| Cancer, n (%) | ||||
| Yes | 2 (3.8) | 0 (0.00) | ||
| No | 51 (96.2) | 53 (100) | 0.462 | |
| Chronic pulmonary disease, n (%) | ||||
| Yes | 2 (3.8) | 0 (0.00) | ||
| No | 51 (96.2) | 53 (100) | 0.153 | |
| Chronic neurological disease, n (%) | ||||
| Yes | 2 (3.8) | 1 (1.9) | ||
| No | 50 (96.2) | 52 (98.1) | 0.547 | |
| Chronic hematological disease, n (%) | ||||
| Yes | 2 (3.8) | 0 (0) | ||
| No | 51 (96.2) | 52 (100) | 0.157 | |
| Liver disease, n (%) | ||||
| Yes | 5 (9.4) | 3 (5.7) | ||
| No | 48 (90.6) | 50 (94.3) | 0.462 | |
| Renal disease, n (%) | ||||
| Yes | 3 (5.7) | 4 (7.5) | ||
| No | 50 (94.3) | 49 (92.5) | 0.696 | |
| Chronic heart disease, n (%) | ||||
| Yes | 4 (7.5) | 2 (3.8) | ||
| No | 49 (92.5) | 50 (96.2) | 0.414 | |
| HIV, n (%) | ||||
| Yes | 2 (3.8) | 0 (0.00) | ||
| No | 51 (96.2) | 53 (100) | 0.153 | |
| Rheumatoid arthritis (RA) n (%) | ||||
| Yes | 1 (1.9) | 1 (1.9) | ||
| No | 52 (98.1) | 52 (98.1) | 1.00 | |
| Other diseases * | ||||
| Yes | 8 (15.1) | 16 (30.2) | ||
| No | 45 (84.9) | 37 (69.8) | 0.063 | |
| Parameters | Mild and Asymptomatic | Moderate | p-Value |
|---|---|---|---|
| SOD (U/mL) | 47.12 ± 16 | 49.74 ± 11.84 | 0.523 |
| GPX (U/mL) | 533.85 ± 436.38 | 616.18 ± 395.59 | 0.541 |
| SAA (µg/mL) | 1.99 ± 0.39 | 2.21 ± 0.53 | 0.227 |
| TAC (mM/L) | 0.46 ± 0.34 | 0.32 ± 0.37 | 0.232 |
| Symptom Categories | |||||
|---|---|---|---|---|---|
| Parameters | General | Pulmonary | Gastrointestinal | Neurologic | |
| Age (year) | 0.99 (0.96–1.03) | 0.96 (0.90–1.02) | 0.96 (0.91–1.01) | 0.97 (0.93–1.00) | |
| Sex | |||||
| Female | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | |
| Male | 0.73 (0.34–1.56) | 1.51 (0.48–4.73) | 0.81 (0.42–1.56) | 0.40 (0.17–0.94) * | |
| Married status | |||||
| Single | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | |
| Married | 2.13 (0.49–9.26) | 0.82 (0.22–3.00) | 4.48 (1.28–15.67) * | 1.53 (0.39–5.95) | |
| Education levels | |||||
| Illiterate | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | |
| Less than high school | 0.81 (0.16–4.12) | 0.06 (0.005–0.66) * | 0.26 (0.04–1.50) | 0.10 (0.02–0.62) * | |
| High school | 0.66 (0.12–3.73) | 0.22 (0.02–2.78) | 0.29 (0.03–2.90) | 0.22 (0.04–1.08) | |
| College education | 1.01 (0.22–4.73) | 0.07 (0.006–0.98) * | 0.66 (0.10–4.42) | 0.29 (0.07–1.26) | |
| SOD | 0.97 (0.94–1.00) | 1.00 (0.95–1.06) | 0.99 (0.96–1.02) | 1.00 (0.97–1.03) | |
| GPx | 1.00 (0.999–1.00) | 1.00 (1.00–1.001) | 1.00 (0.999–1.00) | 1.00 (0.999–1.001) | |
| SAA | 0.27 (0.07–1.06) | 2.31 (0.68–7.90) | 0.44 (0.13–1.47) | 0.37(0.11–1.17) | |
| TAC | 0.53 (0.08–3.68) | 1.41 (0.25–7.99) | 2.41 (0.48–12.22) | 0.55 (0.09–3.40) | |
| BMI (kg/m2) | 1.07 (0.99–1.15) | 0.96 (0.87–1.05) | 1.07 (0.98–1.18) | 1.11 (1.01–1.21) * | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Golabi, S.; Ghasemi, S.; Adelipour, M.; Bagheri, R.; Suzuki, K.; Wong, A.; Seyedtabib, M.; Naghashpour, M. Oxidative Stress and Inflammatory Status in COVID-19 Outpatients: A Health Center-Based Analytical Cross-Sectional Study. Antioxidants 2022, 11, 606. https://doi.org/10.3390/antiox11040606
Golabi S, Ghasemi S, Adelipour M, Bagheri R, Suzuki K, Wong A, Seyedtabib M, Naghashpour M. Oxidative Stress and Inflammatory Status in COVID-19 Outpatients: A Health Center-Based Analytical Cross-Sectional Study. Antioxidants. 2022; 11(4):606. https://doi.org/10.3390/antiox11040606
Chicago/Turabian StyleGolabi, Sahar, Sheyda Ghasemi, Maryam Adelipour, Reza Bagheri, Katsuhiko Suzuki, Alexei Wong, Maryam Seyedtabib, and Mahshid Naghashpour. 2022. "Oxidative Stress and Inflammatory Status in COVID-19 Outpatients: A Health Center-Based Analytical Cross-Sectional Study" Antioxidants 11, no. 4: 606. https://doi.org/10.3390/antiox11040606
APA StyleGolabi, S., Ghasemi, S., Adelipour, M., Bagheri, R., Suzuki, K., Wong, A., Seyedtabib, M., & Naghashpour, M. (2022). Oxidative Stress and Inflammatory Status in COVID-19 Outpatients: A Health Center-Based Analytical Cross-Sectional Study. Antioxidants, 11(4), 606. https://doi.org/10.3390/antiox11040606








