Abstract
Threat activation or deactivation in the brain–body is associated with learned nocebo or placebo somatic effects induced by fake invasive medical–surgical procedures. Some functional somatic disorders (FSDs) originate as acute nocebo somatic effects and can become 30–50% of chronic somatic presentations to primary care physicians. Patients with FSD overutilize medical–surgical services, despite the lack of identified pathophysiology, and are at risk for morbidity from unintentional iatrogenic injury. The Conditioned Response Model (CRM) of learning postulates three innate mechanisms, modulated by trait hypnotizability, which drive placebo and nocebo somatic effects and FSD. The High Risk Model of Threat Perception (HRMTP) postulates 10 psychosocial risk factors that modulate threat perception, driving placebo and nocebo somatic effects and biologically embedded FSD. Psychosocial factors and the trait of high and low hypnotizability modulate threat and are postulated to reduce heart rate variability (HRV), inducing autonomic nervous system (ANS) dysregulation. Reduced HRV was found in a large (N = 6,891) sample of patients with FSD. A total of 50% of patients with FSD with chronic pain (n = 224) without identified pathophysiology had a Paradoxical Increase in hand Temperature (PTI) during experimental threat induction. The HRMTP predicts that PTI associated with ANS dysregulation is associated with the risk factor Adverse Childhood Experiences (ACEs). This ACE prediction was independently confirmed. Learning predicts that threat activation by unconscious neutral stimuli (CS) can amplify nocebo and FSD and can negate placebo effects in clinician–patient relationships. Identifying psychosocial risk factors that modulate threat perception enables the diagnosis of FSD by inclusion and not simply by excluding pathophysiology.
1. Introduction
The analysis of life and survival, even down to the level of the immune system, is about “identifying and neutralizing threats from other species” [1]. Immune mechanisms operate behaviorally through threat avoidance by associative Pavlovian learning [2,3]. Threat (HPAA) learning appears to be mediated by unconscious automatic amygdala brain circuits, but fear learning is apparently mediated by neocortical circuits [4]. Acute threat in humans [5,6,7,8] is apparently mediated automatically and unconsciously by the sympathetic division of the autonomic nervous system (ANS) through cortisol. Associative emotional learning of threat activation or deactivation in the brain and body, manifested as clinical nocebo and placebo somatic effects, are postulated to be associated with the modulation of the hormones of the neuroendocrine system, specifically cortisol and the immune system [6,7,9,10,11,12,13]. High and low cortisol secretion implicates the hypothalamic–pituitary–adrenal axis (HPAA) and pro- and anti-inflammatory cytokines [6,9,14,15,16,17].
This article is primarily a selective review of 1) Placebo, 2) Nocebo and 3) Functional Somatic Disorders (FSD) focusing primarily on two theoretical models (Conditioned Response Model of Learning-CRM and the High Risk Model of Threat Perception-HRMTP) which integrate the acquisition, extinction and modulation by 10 psychosocial risk factors, of the above 3 clinical phenomena in terms of autonomically (ANS) mediated human emotional learning.
Reduced heart rate variability (HRV) or low parasympathetic activity is an independent risk factor associated with a 2-year risk of sudden death [18,19,20]. Reduced HRV is also associated with functional somatic disorders (FSDs) in Denmark, with a large sample (n = 6891) of patients [21]. The High Risk Model of Threat Perception—HRMTP [22,23,24,25,26,27,28,29,30,31,32,33,34] postulates that trait high and low hypnotizability, but not moderate hypnotizability (68% of the general population), is a risk factor for (1) sympathetic hyperreactivity and delayed parasympathetic recovery and eventually for (2) dysregulation of the autonomic nervous system and PTI [35,36,37]. Jorgensen & Zachariae [23] using normal healthy college students tested the above hypotheses with HRV and EDR (electrodermal) data and experimentally induced cognitive and emotional threat and found that there was an apparent potential for sympathetic hyperreactivity and delayed parasympathetic recovery and a potential for ANS dysregulation in trait high and low, but not moderate, hypnotizability. Jorgensen and Zachariae’s [23] data (Figure 3 and Figure 4) appeared to confirm the HRMTP hypothesis of reduced HRV in trait high and low hypnotizability but not moderate trait hypnotizability. Jorgensen & Zachariae [23] also appeared to confirm the hypothesis of a distinct quadratic relationship between trait hypnotizability and threat perception, postulated by the HRMTP [24,27,30,31,32,33].
Greenleaf et al. [22] also found a quadratic relationship between trait hypnotizability and threat of surgical incision in coronary bypass surgery patients, modulating their blood pressure in the ICU, and reported their outcome data in terms of blood pressure medication utilization and speed of recovery and discharge from the ICU and hospital. Perlstrom and Wickramasekera [38] also found a quadratic relationship between trait hypnotizability and EEG-defined primary insomnia and threat perception (High Neuroticism), without identified pathophysiology. Younger et al. [34], also using healthy college students and psychometric–behavioral measures of somatic symptoms, confirmed a dose–response or linear relationship between trait hypnotizability and somatic symptoms but not the predicted quadratic model of ANS hyperreactivity and eventual ANS dysregulation [29,30,31,33,35,36]. The Jorgensen & Zachariae [23] study and Greenleaf et al. [22] used the predicted ANS measures of threat perception [24,27,33], whereas the Younger et al. [34] study used only behavioral measures of threat perception. Two large major meta-analyses of the efficacy of trait hypnotizability–suggestibility in reducing threat in experimental [39] pain (n = 3632) and clinical [40] pain (in 42 studies) found a linear relationship between these two predicted variables. A linear relationship between trait hypnotizability and threat perception in somatic symptom modulation was found by multiple other clinical and meta-analytic studies [41]. For example, the following studies found a linear relationship between trait hypnotizability–suggestibility and clinical or experimental threat perception in the following somatic symptoms: anticipatory nausea and vomiting [42,43], chronic tension headache [44], Conversion Disorder [45], moderate obesity [46], surgical candidates with morbid obesity [47], somatization [48], chronic pain [49], primary care somatization patients [50] and acute stress disorder [51].
George Engel [52], in a salient paper in Science, proposed a new medical model, but he did not specify or operationalize the psychosocial factors of his model. Nor did he specify the mechanisms of learning [53,54] through which threat perception and activation of the HPAA could be modulated by psychosocial risk factors to induce stress-related somatic symptoms (SRSSs), without identified pathophysiology [24,25,26,27,28,29,30,31,32,33] or, as labeled today, functional somatic disorders—FSDs [55]. Threat perception (HPAA) pierces the skin, invades the brain and body and is correlated with somatic symptoms [6,7,56,57] which are postulated to be modulated by ten semi-orthogonal empirically established psychosocial risk factors specified by the High Risk Model of Threat Perception (HRMTP) [24,25,26,27,28,29,30,31,32,33]. HPAA activation is correlatively linked to chronic SRSS or somatization [24,30,33,58,59]. Activation or deactivation of threat (HPAA) perception by fake invasive medical–surgical procedures [5,60] drive learned placebo and nocebo somatic effects and may contribute to chronic functional somatic disorders (FSDs) without identified pathophysiology [30,32,33]. Placebo and nocebo somatic effects and functional somatic disorders are postulated to be modulated by learned threat perception, which is modulated by the Predisposing, Triggering and Buffering psychosocial risk factors of the HRMTP [27,30,32,33]. Threat perception is a link through the associative (CS-US) and other learning of placebo and nocebo somatic effects and functional somatic disorders [33,53,54,61,62] from mental to physical health [24,30,31,35,36,55].
The primary Predisposing risk factor, trait hypnotizability–suggestibility, of the HRMTP is postulated to modulate invasive threat perception (HPAA), somatic symptoms and experimental and clinical pain perception [22,23,24,33,34,35,36,37,40,63,64,65,66,67]. Acute and chronic threat perception is postulated to be associated with both hyper- and hypoactivation of the HPAA and this variability is modulated by several factors, like the type of stressor, the type of personality and the timing of the stressor [68]. Threat and acute pain activates the hypothalamic–pituitary–adrenal axis (HPAA) to secrete cortisol, and variability in chronic cortisol secretion is predicted by the HRMTP to contribute to dysregulation of the autonomic nervous system and paradoxical temperature increase—PTI—in chronic pain [6,7,17,35,36,37] and can induce other stress-related somatic symptoms (SRSSs) [17,24,27,30,31,33,36,37] or FSDs [55].
Reduced heart rate variability (HRV), consistent with sympathetic (SNS) predominance, was found in a large-scale study in Denmark of people with FSD (N = 6891) and also was found in several previous meta-analyses of HRV and FSD [21]. This recent sympathetic predominance finding in a large FSD sample is consistent with the HRMTP’s prediction of sympathetic hyperreactivity and delayed parasympathetic recovery in the primary Predisposing risk factor trait high hypnotizability in FSD or SRSS [22,23,31,33,35,36,64].
Trait low hypnotizability appears related to incongruence in measures of ANS reactivity and emotional hypoactivation of the HPAA [23] on conscious verbal report measures but not on direct ANS measures of threat perception [27,69,70,71]. Trait low hypnotizability is apparently related to trait High Alexithymia, defined as “without words for feelings” [72,73]. High Alexithymia is negatively correlated with trait high hypnotizability [72,74,75]. Threat perception in FSD appears associated with incongruent emotional anomalies in vagally modulated gut disorders specified by Porges [76] like IBS and specifically with affective agnosia [72,75,76,77,78,79].
Hence, the HRMTP predicts that chronic hyper- or hypoactivation of threat (HPAA) and emotional anomalies like affective agnosia [78], as clinically observed in many chronic pain patients with trait high or low hypnotizability–suggestibility and FSD, will eventually induce dysregulation of the ANS [30,35,36,37,79,80,81]. Normal organ function, termed homeostasis, is apparently disrupted during allostasis or adaptation to chronic threat through change [6,7]. Allostasis requires reciprocal interactions between the ANS and the immune systems [7,82]. Chronic threat perception is apparently associated with dysregulation of the ANS and PTI during adaptation to chronic threat, termed allostasis [7,82].
2. Is Paradoxical Skin Temperature Increase (PTI) During Threat Perception in Chronic Pain Linked to Dysregulation of the ANS?
We now review the first empirical confirmation [37] of HRMTP’s prediction of dysregulation of the autonomic nervous system (ANS), during experimental threat induction in patients (N = 224) with FSD with chronic pain (persistent for >6 months without positive response to conventional medical–surgical therapy) and without identified pathophysiology [30,37]. In an electrically shielded and temperature-controlled psychophysiology lab, an experimentally induced emotional–cognitive threat state, measured with the electrodermal response—SCL—a correlate of state negative affect [83,84,85,86], was induced by a simple timed mental arithmetic stress test. A subset of this group of 224 FSD adult chronic pain patients (mean age = 38.05 years, SD = 11.92 years, men = 83 and women = 141) responded to emotional–cognitive threat with a paradoxical left-hand temperature increase (PTI) during threat induction. This PTI was observed in 49.4% of male patients and 42.6% of female patients during the standardized experimental emotional threat induction procedure, validated by their increased Skin Conductance Level (SCL) during their increased left-hand temperature response. Concurrently, we also monitored several other parameters of peripheral physiological function (BVP, HR, frontalis EMG, etc.) that responded normally. This paradoxical left-hand temperature ANS response to threat (HPAA) induction appears restricted to the peripheral vascular hand temperature of these chronic FSD pain patients. A validity check of their SCL, which is primarily sympathetically innervated [84,87], and other physiological measures found normal SNS activation during (1) baseline, (2) threat induction (HPAA) and (3) return to baseline. The PTI was also unrelated to regression to the mean as indicated by data analysis and the Blomqvist [88] statistical test. The PTI is postulated to be a specific peripheral vascular response and an apparent objective marker of a predicted dysregulated ANS response to chronic threat perception [31,36,37] related to an apparent anomalous peripheral increase in vagal tone during threat perception.
The PTI response to threat perception may be an automatic unconscious protective–dissociative response [89] mediated partly by the interaction of trait (1) hypnotizability–suggestibility and (2) trait High Neuroticism [30,90] of the HRMTP. In the medical literature, this anomalous phenomena of PTI has been previously observed and is called “idiopathic flushing” [91,92,93] and PTI has been observed even after sympathetic blockade [92] and also during “panic attacks.” The HRMTP predicts and has found the PTI response in patients with chronic threat-related somatic symptoms (SRSSs) like chronic pain, IBS and morbid obesity in candidates for GI surgery [28,37,47,90]. The HRMTP predicts that PTI will be observed in FSD [55] and specifically those FSDs with the Triggering risk factor Adverse Childhood Experiences (ACEs) or other “biologically embedded body memories” [6,57] of adversity [94] or trauma blocked from consciousness [28,29,31,36,37,90,95].
An independent PhD dissertation [96], using our experimental threat induction procedure [37] with experimental (n = 20) and control (n = 20) groups, replicated the PTI observation. The study found that PTI occurred significantly (p = 0.0266) more frequently in the Adverse Childhood Experiences risk factor group (abused sample) than in the non-abused sample. This PTI response can be inexpensively tested in a psychophysiology lab and confirmed or falsified with an FSD sample of chronic pain patients with a history of Adverse Childhood Experiences.
3. The HRMTP Modulates Functional Somatic Disorders and Placebo and Nocebo Somatic Effects
“Sometimes it is more important to know what kind of patient has a disease than what kind of disease the patient has.”—Sir William Osler
The HRMTP seeks to operationalize Osler’s intuition that sometimes the interaction of the psychosocial features of a patient, with the threat (HPAA) activating invasive clinical investigation (US-UR) of the patient in a medical–surgical context [53,54,61], may account for more variance in the measurement of clinical outcome than the identified pathophysiology of their disease. In the biomedical model, illness and somatic symptoms are driven primarily by identified pathophysiology. The HRMTP postulates that the penetration of the skin, brain and body by threat perception (HPAA), in the increasingly invasive medical–surgical context, is modulated by 10 semi-orthogonal empirically established psychosocial risk factors (modulating human emotionality) that are postulated to modulate ANS reactivity. These 10 psychosocial risk factors fall into three categories, Predisposing, Triggering and Buffering risk factors, and these risk factors can interact with chronicity in the same patient to generate morbidity and mortality.
The HRMTP’s Buffering or protective psychosocial factors include the following: 1. high social support (S.S.), 2. High Approach and Low Avoidance Coping Skills (CS) and 3. high trait positive affectivity (P.A.). If perceived social support is low, there is an increased risk of patient progression of morbidity or mortality even in stress-related organic diseases, like cancer and cardiovascular disease [97,98,99]. Smith et al. [100] have proposed multiple mechanistic causal pathways between psychosocial variables (e.g., social support) and biological variables.
These 10 psychosocial risk factors are postulated to modulate threat perception in placebo and nocebo somatic effects and FSD in patients. The primary Predisposing risk factor trait hypnotizability–suggestibility can interact with threat perception in a top-down and bottom-up manner to generate somatic placebo effects [101,102,103,104,105,106], somatic nocebo effects [106,107,108,109] and functional somatic disorders [23,30,34,38,41,44,45] in patients and healthy people (Figure 1).
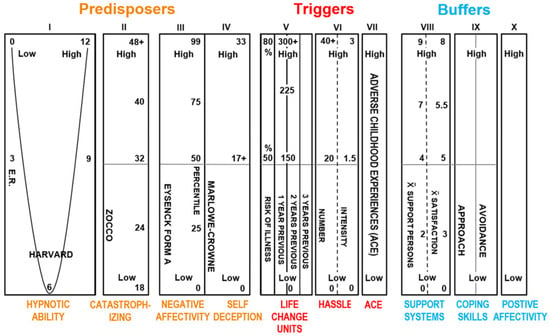
Figure 1.
Profile of the HRMTP. The Predisposes can be amplified by the Triggers, and the Buffers theoretically attenuate the Predisposes and Triggers [23,24,31,33,34,36,38,44,45,47,48,49,50,64,69,70].
- A. Predisposing Risk Factors Modulating Threat and Pain Perception
- 1.
- Trait hypnotizability–suggestibility [65,66,67,71,110], related trait Absorption [111] and trait Alexithymia [27,72,75,78] are three closely related personality trait factors that are postulated by the HRMTP to be psychosocial personality mechanisms modulating (1) ANS reactivity during threat (HPAA) and pain perception, (2) the generation of somatic placebo and nocebo effects and (3) FSD [55]. Specifically, it is postulated [24,26,27,33] that these three related personality traits, (1) hypnotizability–suggestibility, (2) Absorption and (3) Alexithymia, despite varied labels, all empirically converge to modulate human threat perception (HPAA) and pain perception and to modulate FSD [55].
- 2.
- High learned catastrophizing [24,28,30,112,113,114,115,116,117] is explicit or implicit verbal responses to threat that reliably amplifies threat and pain perception and is measured by verbal report psychometric scales [27,114] and also apparently manifests in EEG effective connectivity measures [113]. Amygdala functional connectivity in fMRI data mediates the association between catastrophizing and threat-safety learning in chronic pain in youth [16].
- 3.
- High trait Neuroticism or Negative Affectivity (NA) [24,30,36,38,86,112,118,119] is a predisposition to amplified threat perception, independent of objective negative events. Trait or state NA can be measured with psychometric measures [86] or by the electrodermal response—EDR [36,38,83], and state NA appears associated with the default mode network (DMN) in chronic low back pain [85]. Nocebo effects are linked to high NA as a risk factor [116]. High NA is robustly related experimentally, even to the common cold ([120], NEJM) and medical illness with identified pathophysiology [121].
- 4.
- High trait Self-Deception (SD) is a trait tendency to interpret negative events or threats positively [30,33,112]. SD is measured with a High Marlowe Crowne score [122,123] or another psychometric measure of social desirability. High SD is a >17 score on the Marlowe Crowne psychometric scale and is a measure of repressed threat perception unrelated to the complex Weinberger hypothesis [122,124].
- B. Triggering Risk Factors Modulating Threat or Pain Perception
- 1.
- Life Change Units or stressful life events (SLEs) have been empirically linked to the experimentally induced common cold ([120], NEJM) and to morbidity and mortality [30,33,94,125,126,127,128] and are measured by several psychometric scales [126].
- 2.
- The density and intensity of Daily Hassles: Accumulation of Daily Hassles inducing threat in some people activates the hypothalamic–pituitary–adrenal axis and can be associated with mortality and morbidity [24,30,33,129]. Hassles are measured with several psychometric scales of known reliability and validity.
- 3.
- High adverse childhood experiences (ACEs) are biologically embedded and strongly linked in adulthood to depression, smoking, substance abuse, severe obesity, heart disease, cancer, chronic lung disease and reduced life span [6,7,33,57,130,131,132] and are measured by several psychometric scales.
- C. Buffering Risk Factors Modulating Threat or Pain Perception
- 1.
- High social support [24,26,30,33,99,100,133] is measured by several verbal report psychometric scales and is reliably correlated with many physical diseases, including cardiovascular and cancer diseases, in replicated studies of morbidity and mortality mediated by threat (HPAA) and other neuroendocrine measures.
- 2.
- Approach and Avoidance Coping Skills [133,134,135] are measured by Approach and Avoidance psychometric scales [136] and are related to amplified Approach Coping Skills in positive mental and physical health outcomes [133]. Two-factor learning theory [27] predicts that avoidance behavior [137] is associated with many mental disorders and avoidance coping is postulated to be associated with FSD, specifically chronic pain [27,32,138]. Approach coping and placebo effects are associated with “safety cues” and fear extinction [27,139] and reduced somatization and reduced FSD.
- 3.
- High positive affectivity [30,140,141,142] is measured with several psychometric verbal report scales and is reliably related to positive mental and physical clinical health outcomes [140]. High positive affectivity appears to buffer nocebo effects [141]. Two studies [141,142] recently confirmed the HRMTP’s prediction that experimentally induced trait or state positive affectivity would buffer or reduce nocebo effects.
The replicated empirical support for each of the above 10 postulated risk factors is too extensive to review here and is reviewed elsewhere [6,23,24,26,27,28,30,32,33,35,36,57,72,86,123,133,140,143]. The review of the supporting evidence for the HRMTP is restricted to trait hypnotizability–suggestibility, the primary Predisposing risk factor and its two related traits, Absorption and Alexithymia.
4. Primary Predisposing Risk Factor Trait Hypnotizability–Suggestibility Modulates Threat Perception (HPAA) and the Expression of Other Predisposing, Triggering and Buffering Risk Factors
The psychophysiological expression of the Triggering risk factors, adverse childhood experiences (ACEs) and adult stressful life events (SLEs), and the Buffering risk factors (e.g., social support, trait high positive affectivity, etc.) are predicted by the HRMTP to be expressed and modulated by the primary Predisposing risk factor, trait hypnotizability–suggestibility [30,65,110]. Trait high and low hypnotizability–suggestibility, but not moderate trait hypnotizability (approximately 70% of the general population), appears to quadratically modulate ANS sympathetic threat (HPAA) reactivity (e.g., blood pressure lability, EDR and HRV) during invasive cardiac bypass surgical incision in patients [22] and to experimentally induced distinct patterns of ANS reactivity, measured by heart rate variability (HRV) and electrodermal skin conductance (EDR), to emotional–cognitive threat induction in normal college students [23,64]. It is postulated that personality trait (a) high hypnotizability–suggestibility is associated with ANS Hyper-responsiveness and (b) trait low hypnotizability with emotional–cognitive incongruencies [26,27,69,70] and ANS Hypo-responsiveness to threat and pain perception.
4.1. Predisposing Risk Factor Trait Hypnotizaiblity and Blood Pressure Reactivity in the ICU from Cadiac Bypass Surgery
The rate of recovery and healing from the threat (HPAA) of cardiac bypass surgery was examined in 32 patients of high, medium and low trait hypnotizability in the ICU and hospital after all patients had received one session of hypnotherapy, delivered by a hypnotherapist blinded to the patients’ measured hypnotizability [22]. It was found that both high (HH) and low (LH), but not moderate, hypnotizability was linked to delayed recovery and healing in the ICU and delayed hospital discharge from the threat (HPAA activation) by surgical incision (UCS-UCR) during coronary bypass surgery. High hypnotizable (HH) patients had more labile blood pressure in the ICU and required more medication, compared to the medium and low hypnotizable patients (p < 0.05). But high hypnotizable (HH) patients in the ICU through one session with a hypnotherapist appeared to reduce or abolish their perception of threat (HPAA) and healed rapidly in the ICU and were discharged early from the hospital. But low hypnotizables (LHs) who also had one session with the hypnotherapist (blinded to their trait hypnotizability) had delayed recovery from the surgery and were discharged later (mean = 5 days) from the hospital than the HH patients. Moderate trait hypnotizability patients, as predicted by the HRMTP, stabilized more quickly in the intensive care unit (ICU) than those who were high or low (p < 0.05) in trait hypnotizability. Measured trait hypnotizability was associated with the following recovery sequence from surgery: moderates, highs and lows. The above finding is consistent with a meta-analysis of 20 controlled studies of 1624 patients that found a large weighted effect size (D = 1.20; VarD = 0.83) and concluded that surgical patients in adjunctive hypnosis therapy had a better outcome than 89% of patients in control conditions [144]. The magnitude of this clinical efficacy finding in Montogomery et al. [144] was probably due to the confounding of the placebo effect (CS-CR) of hypnotherapy with the active ingredient trait hypnotizability (US-UR). The above [22] study supports the HRMTP precise prediction of quadratic modulation of human threat perception by trait hypnotizability.
4.2. Predisposing Risk Factor High and Low Hypnotizability Is Associated with Distinct Patterns of ANS Reactivity to Threat Induction
Jorgensen and Zachariae [23] in Denmark examined ANS reactivity to cognitive and emotional threat (HPAA) in low, medium and high trait hypnotizability in healthy college students. This research tested predictions derived from the HRMTP regarding high, medium and low trait hypnotizability and ANS reactivity. Hypnotizability was measured 9 months prior to the ANS reactivity threat (HPAA) testing, and hypnotizability was never mentioned as relevant to the ANS threat (HPAA) testing conducted in a location and institution different from where the hypnotizability of the 71 healthy students (low H = 13, medium = 44 and high H = 14) was tested. This experimental context manipulation was performed to negate controversial hypothesized context effects [145] between the independent (trait hypnotizability) and dependent variables (ANS reactivity) in this study.
The investigators experimentally induced cognitive–emotional threat (HPAA) and measured the sympathetic and parasympathetic system (ANS) reactivity (EDA, ECG, HRV-HF-LF and BP) in 71 healthy college students, measured by a verbal report of stress, peripheral hand skin temperature, the electrodermal response—EDR—(mainly sympathetically innervated [84]) and high-frequency (HF) heart rate variability [146,147]. It is postulated that quadratically, trait a) high hypnotizability is associated with Hyper-responsiveness and B) trait low hypnotizability with Hypo-responsiveness of the neuroendocrine stress response axes (HPAA) and elevated or decreased sympathetic or parasympathetic basal tone. Electrodermal activity (EDA) was used as a measure of sympathetic activity and the high-frequency (HF) spectral component of heart rate variability as a measure of parasympathetic activity. High hypnotizables exhibited greater EDA at baseline and slower EDA recovery following both cognitive and emotional threat induction (HPAA) tasks than did medium and low hypnotizables (p = 0.003). “Medium hypnotizables responded with greater decreases in normalized HF power than did highs and lows during the emotional threat task. The results suggest diminished EDA variability in High hypnotizables and the potential for HF power as an indicator of autonomic dysregulation in Low and High hypnotizables, compared to mediums. In general, our results provide support for the hypothesis of differences in autonomic regulation between Low, Medium and High hypnotizable subjects, as predicted by the HRMTP. Our results could thus be interpreted as an indication of autonomic dysregulation in both Low and High hypnotizables, compared to medium hypnotizables, as predicted by the HRMTP” [23]. The above finding of potential ANS dysregulation in trait high and low hypnotizables is consistent with the prediction from the HRMTP [24,30,33,35,36,37,47,90].
4.3. Primary Predisposing Risk Factor Trait Hypnotizability–Suggestibility, Definition and Parameters
Trait high hypnotizability (HH) can be defined as the innate ability (US-UR) to modulate in a dose–response or linear manner human perception, cognition, memory, mood [65,110,148,149,150,151] and ANS physiology [152,153], with a reduced sense of personal agency or with the perception of “involuntariness” [154] in response to standardized verbal suggestions [65,110]. Trait high hypnotizability–suggestibility is also postulated to modulate automaticity in adaptive or maladaptive human learning [27,71,155,156,157,158,159,160] (Figure 2).
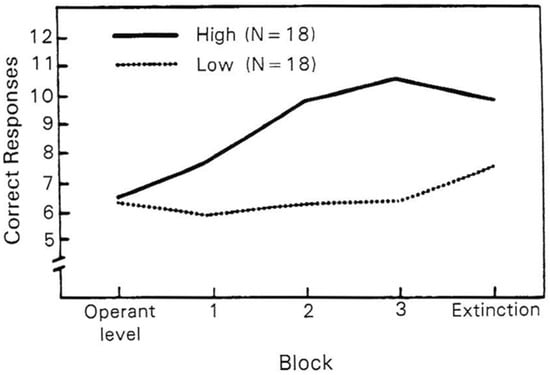
Figure 2.
Verbal conditioning as a function of hypnotic susceptibility (Harvard). From “Hypnotic Susceptibility and Verbal Conditioning,” [27,156]. Reprinted from Wickramasekera, 1988 [27].
Cognitive expectancy [110] appears to be an essential but not sufficient condition for high hypnotizability as empirically shown by skeptics of trait hypnotizability Spanos et al., 1989 [161], and Benham et al., 2006 [162]. Benham et al. [162,163] state, “There was an abundance of variance in hypnotic performance unexplained by the direct and indirect influence of expectation and compatible with the presence of an underlying cognitive ability” (p. 342). Horton & Crawford [164] apparently found that increased anterior corpus callosum size is positively correlated with trait high hypnotizability (HH). Hypnotic induction is associated with decreased activity in the anterior default mode network (DMN) only in trait high hypnotizable (HH) subjects [165] and naloxone does not block the mechanism of hypnotic analgesia in trait HH subjects [166]. HHs can modulate EEG-validated REM and slow-wave sleep in response to posthypnotic verbal suggestion [167,168].
Traits hypnotizability and suggestibility are highly correlated (r = 0.67–0.82) trait measures of personality with or without a hypnotic induction ritual [65,169,170]. Trait hypnotizability is measured with standardized behavioral tests like the Harvard Group scale or the Stanford scales, Forms A, B and C (Form C is the gold standard measure). Trait hypnotizability is stable and has high (r = 0.71) reliability over 15–25 years [171] and appears in behavioral data to be partly genetically based in monozygotic and dizygotic twins [172,173], but in genetic data there is still controversy [174]. Trait hypnotizability is orthogonal to the other Big Five trait factors in human personality [175]. In the general population and also cross cultures, trait hypnotizability appears to be normally distributed [176]. But trait hypnotizability is apparently not normally distributed in psychopathology [30,34,38,51,177,178] but appears quadratically distributed in somatization, functional somatic disorders or stress-related somatic symptoms—SRSSs [22,27,30,32,33,37,38].
Trait hypnotizability–suggestibility, through a verbal suggestion mechanism, was found to robustly reduce both experimental and clinical pain perception in a linear or dose–response manner. Suggestions for the reduction in threatening clinical [40] and experimental pain [39] are modulated by the trait hypnotizability–suggestibility, as evidenced in two large meta-analyses of 42 controlled clinical pain studies and 85 controlled experimental pain studies. Trait hypnotizability–suggestibility is associated in clinical pain reduction with a mean weighted effect size of r = 0.53 (p < 0.001). Trait hypnotizability is associated in experimental pain with a 42% pain reduction in high hypnotizable (HH) and a 29% pain reduction in moderate hypnotizability and negligible pain reduction in low hypnotizable (LH) people.
The above finding is also consistent with a meta-analysis of 20 controlled studies of 1624 patients that found a large significant weighted effect size (D = 1.20) and concluded that surgical patients in adjunctive hypnosis therapy had a better outcome than 89% of patients in control conditions [144]. Rosendahl et al. [179] conducted a meta-analysis and concluded that effect sizes (medium to large) were largest for pain in threatening invasive medical–surgical procedures and children/adolescents. The magnitude of this clinical efficacy finding in the Montogomery et al. [144] study and the Rosendahl et al. study [179] was apparently due to the confounding of the placebo effect (CS-US) of hypnotherapy with the unmeasured active ingredient trait (US-UR) hypnotizability–suggestibility in the above two studies [33,53,54,61]. Innate trait high and moderate hypnotizability–suggestibility (US-UR) has a reliable placebo effect mobilized by verbal hypnotic induction rituals that should be clinically leveraged.
Recently, Landry et al. [180], and in a personal communication (2024), proposed that the most predictive neural feature identifying high vs. low hypnotizability in normal people was the aperiodic exponent of the EEG power spectrum measured at the anterior part of the frontal lobe at baseline and outside of hypnosis verbal rituals [181]. This suggests that trait hypnotizability may be a latent innate neural trait (US-UR), prior to any verbal hypnotic interventions. Previously, baseline EEG theta was found to discriminate between HH and LH normal people at baseline [71,182,183]. Significant gene–trait interactions have been studied in relation to attention and dopamine-related COMPT [174]. Cortade et al. [184] in a genetic study found that 89.5% of the individuals having the optimal COMT diplotypes had moderate to high hypnotizability (measurement with the Hypnotic Induction Profile, >3), based on a brief low-cost saliva test indicating a potential to identify a subset of primarily female patients (p < 0.001) (a relatively small number of men in this study) who may benefit from medical–surgical hypnosis interventions. Incidentally, the COMT amplifies stress reactivity through cortisol and the HPAA [185] and this is consistent with prediction from the HRMTP.
4.4. ANS Reactivity and Functional Somatic Disorders (FSDs)
A study (Figure 3) of 118 adult FSD patients presenting with chronic pain and chronic somatic symptoms found that trait high hypnotizability (Harvard test) modulated experimentally induced threat or negative affect, measured by their electrodermal skin level (SCL), in a linear or dose–response manner as hypothesized by the HRMTP. This hypothesized interaction of hypnotic ability and negative affect found that larger increases in the SCL during cognitive threat were significantly related to higher levels of trait hypnotizability (p = 0.0065). In addition, individuals with trait high hypnotizability retained higher levels of SCL (delayed recovery from threat or stress) than individuals with low hypnotic ability (p = 0.0065) after cognitive stress. ANS-mediated gastric acid secretion [152] and ANS-mediated pain symptoms [153] have been shown to be modulated by trait hypnotizability–suggestibility. Also, trait hypnotizability apparently modulates muscular contraction or “tension headache” and vascular headache—Migraine [27,44,160], Conversion Disorder [45], moderate obesity [46], morbid obesity [47] and the severity of somatic complaints [34].
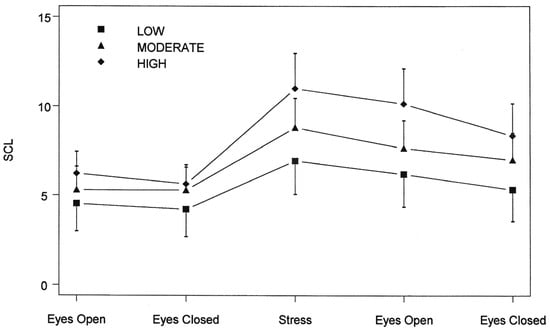
Figure 3.
Hypnotic ability, SCL means and 95% confidence intervals (Wickramasekera et al., 1996 [36]).
High and low hypnotizability is robustly (p < 0.001) and quadratically associated with FSD in patients (n = 83) with chronic pain and multiple other somatic symptoms in a medical school Behavioral Medicine Clinic and psychophysiology laboratory [30]. This study of chronic FSD patients was conducted on a consecutive series of 83 adult patients (male and female) presenting chronic pain and multiple chronic somatic symptoms (FSDs) without identified pathophysiology (investigated–tested previously by multiple medical specialists and subspecialists) who were compared to a healthy matched (mean age 40 years) community sample (N = 78) of male (N = 38) and female (N = 40) adults who were high, low and moderate in hypnotizability as defined by the Harvard Group test. The patient sample with somatic symptoms predicted by the HRMTP was quadratically distributed on trait hypnotizability and was significantly different from the normal distribution of high, low and moderate hypnotizability from the matched community control group (p < 0.001). Trait low hypnotizability was significantly (p < 0.003) more often associated with the presentation of somatic symptoms (pain, IBS, etc.) rather than psychological symptoms (anxiety, phobias and depression).
In two medical school sleep disorder clinics, EEG-defined primary insomnia, with pathophysiology (apnea) and psychopathology (depression) excluded, was quadratically and robustly (p < 0.0001) associated with trait high and low hypnotizability [38]. In high (HH) people, EEG-defined slow-wave sleep (SWS) was increased 81% by posthypnotic suggestion, and time spent awake was reduced by 67% [168]. In an early sleep laboratory study, REM sleep was modulated by posthypnotic suggestion only in trait high hypnotizable normal subjects [167].
In a meta-analysis [41] of functional neurological disorders, trait high suggestibility was significantly (p < 0.001) associated with FND in a meta-analysis (FND: n = 316; control: n = 360) of FND patients. A systematic review [186] of 35 studies (N = 1584 patients) of the efficacy of hypnosis and suggestion for functional neurological disorders (FNDs) reported a surprising 87% clinal efficacy rate but did not measure or control for the patient-measured innate trait hypnotizability–suggestibility, which is the implicated innate active ingredient (US-UR) in hypnotherapy [33,53,54,61,71]. Somatic complaint severity in normal college students (n = 45) was positively correlated (r = 0.452; p < 0.002) with high hypnotizability (Waterloo–Stanford, Form C) as predicted by the HRMTP [34].
An unpublished PhD dissertation study [187] by an MD student of pulmonary function and HRMTP risk factors, in the hypnotherapy of moderate to moderately severe asthma patients, found that two risk factors of the HRMTP predicted the magnitude of symptom and medication reduction in these patients. Wagman [187] found that risk factors, 1. high hypnotizability (defined by both Harvard, p < 0.0001, and Stanford Form C, p < 0.0001 measures) and 2. High Self-Deception (p < 0.01) (Marlowe Crowne score >17) significantly (p < 0.001) predicted, with pulmonary measurement, the magnitude of medication reduction for these moderate to moderately severe asthma patients.
5. Can Automaticity and Reduced Sense of Self Agency in High Hypnotizable (HH) Patients Exponentially Amplify Threat Perception?
Amplified responsivity to suggestions in HH but not LH is based on evidence from the cognitive gold standard Stroop test [158,188,189,190] of automaticity in human information processing and cerebral EEG event-related potential-ERP data [157,191]. HHs appear to acquire and retain simple information very rapidly, and this automaticity in HH people’s information processing is not simply verbal but also extends down to the non-conscious perceptual level as indicated by ERP data ([157], personal communications) and is associated with greater cognitive flexibility in HH rather than in LH people in response to simple verbal instructions implicating the anterior cingulate cortex [110,159,190].
Automaticity is defined as processing information effortlessly, rapidly and involuntarily [192]. In a seminal experimental study, Raz et al. [158] showed that only in trait high hypnotizable (HH) people, with or without a hypnotic induction, can a posthypnotic suggestion that words are meaningless or an alien language block normal automatic word recognition in proficient English readers using the gold standard Stroop experimental procedure [188,190]. The use of verbal suggestion to reliably alter the meaning of a noxious sensory stimulus (e.g., surgical pain) has been used for over 100 years in clinical and experimental hypnotic analgesia [27,63] and in numerous controlled meta-analytic studies with significant (D = 1.20) adjunctive hypnotherapy for invasive medical diagnostic or surgical procedures [144,179].
The HRMTP postulates that when HHs are threatened (HPAA) by invasive physical or psychosocial procedures (e.g., some clinical interviews), they may perceive cognitive-behavioral and motor alterations as occurring automatically and outside their voluntary control [157,190] and with a reduced sense of personal agency [154,193,194]. This perception in trait high hypnotizables of a reduced sense of agency [154] over one’s own mind and body can amplify threat perception (HPAA). This is particularly so in HH patients during interactions with other Predisposing risk factors, like (1) high verbal catastrophizing and (2) High trait Negative Affectivity ruminations on past memories of grief–loss and adversity [27,90].
5.1. Trait Hypnotizability–Suggestibility and Related Trait Absorption (TAS) Modulate Learned Placebo and Nocebo Effects and Functional Somatic Disorders
Trait high hypnotizability–suggestibility and trait High Absorption are highly correlated, particularly in the high range of both trait Absorption and trait hypnotizability [195,196]. In a randomized double-blind placebo-controlled crossover study [103] of 117 Multiple Sclerosis patients, it was found that placebo responders scored significantly higher (p < 0.01) on trait Absorption than placebo non-responders, and discriminant analysis found that 80% of placebo responders were accurately identified (p < 0.0004) (Figure 4).
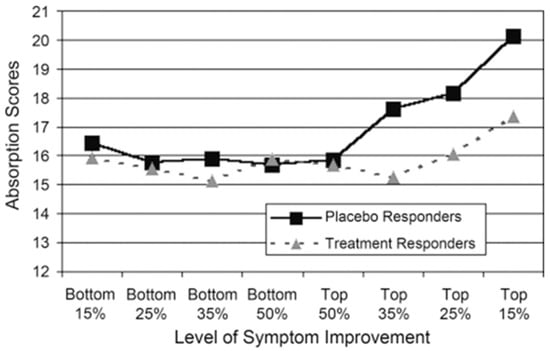
Figure 4.
Absorption scores of placebo responders and treatment responders at increasing levels of symptom improvement (n = 16–56) [103].
Trait hypnotizability–suggestibility is postulated [53,54,61,197] to modulate (1) verbal suggestion learning [39,40] and (2) associative (CS-US) learning of placebo effects [101,102,104,105] and nocebo effects [106,107,108,109].
Huber et al. [104] report an fMRI study of trait hypnotizability (Stanford scale, Form A) modulating brain activity linked to experimental placebo analgesia in brain-imaging data but not in behavioral data. In fact, they did not use a formal hypnotic induction procedure in this study because hypnotizability–suggestibility are highly (r = 0.67–0.87) correlated [170]. Also, this study acknowledged it was deficient in high hypnotizable subjects [104], and like Voudouris et al. [198], they covertly reduced the intensity of the pain stimulus. However, their study found that high hypnotizability (HH) was linked to increased analgesia after a placebo conditioning procedure and that this effect is mediated by decreased functional connectivity of the DLPFC with the anterior cingulate.
5.2. Trait Absorption (TAS) and Functional Somatic Disorders
My associates, I and others have used both the Harvard behavioral test of hypnotizability–suggestibility and also the psychometric Tellegen Absorption scale (TAS) [111] as a surrogate measure of hypnotizability–suggestibility in time-limited medical–surgical settings. Trait Absorption (TAS) can be defined as a person’s predisposition to become deeply attentionally engrossed in a sensory or imaginative experience [111]. TAS is a brief psychometric noninvasive test of hypnotizability–suggestibility, whereas the invasive Harvard test can be associated with an invasive 5–10% incidence of somatic side effects, particularly in clinical samples [27,199].
Trait Absorption (TAS) is a stable psychometric personality trait closely related to behavioral hypnotizability, despite the discrepant label trait Absorption [111,196,200]. The TAS measurement can be made in 15–20 min, unlike the Harvard and Stanford behavioral performance measures of trait hypnotizability that require specialized administration skills and require 1.5 to 2.5 h for testing and scoring. Controversially [145,201], personality traits hypnotizability–suggestibility and trait Absorption were claimed to be only contextually correlated [145], but spectral analysis of easy and challenging test suggestions of hypnotizability find that high hypnotizability and High Absorption are robustly correlated [196]. And in fact it was stated that “Absorption may be a reasonably good predictor of the responses to the difficult cognitive suggestions,” [196] and Balthazard & Woody [195] found Absorption related to the hardest hypnotic tasks (hallucinations and cognitive distortions) and a measure of “true” hypnotic responsiveness.
The TAS is stable and partly genetically based in behavioral data in monozygotic and dizygotic twins reared apart and together [202]. A heuristic and empirically supported distinction made by Tellegen [111]; personal communication, 1992) postulates that High Absorption (HA) people have an experiential or respondent (Pavlovian) mental set for human learning and Low Absorption (LA) people have an operant or instrumental (Skinner) mental set towards learning. This theoretical distinction appears supported by preliminary experimental and clinical studies in normal and clinical FSD samples [48,49,118,203,204,205].
TAS is significantly (p < 0.001) related to a wide range of phenomena, from morbid obesity surgical candidates [47] to ANS-mediated anticipatory nausea and vomiting both in and outside the chemotherapy context [42,43] and to risk factors for musical performance anxiety [112]. For example, High patient Absorption (TAS) is significantly (p ≤ 0.001) associated with anticipatory nausea and vomiting (CR) in chemotherapy patients [42] at the sight or smell of chemotherapy nursing staff (CS) both in and outside (e.g., grocery store) the clinical context of infusion and even in High TAS patients (N = 72) remotely approaching the clinical context (CS-US) of chemotherapy (US) infusion. This early correlational evidence of associative learning (CS-US) of neutral person-CS (e.g., nurses), place-CS (clinics and hospitals) and aversive invasive procedures (US-UR) associated with chemotherapy (CS-US) infusion ([53,54,206], NEJM) automatically and unconsciously eliciting anticipatory nausea and vomiting in High TAS patients has been replicated [43]. Trait Absorption (TAS) is associated (p < 0.01) with specific patterns of ANS reactivity (e.g., HRV and EDR) to cognitive experimental threat induction in normal college students [64]. Low TAS is robustly (p < 0.001) associated with morbid obesity in candidates for GI bypass surgery [47] and with High and Low TAS in functional somatic disorders (FSDs) in a primary care medical school clinic [27,50]. Also, it is associated with chronic pain in FSD patients in a private practice pain clinic [49] and is correlated with the magnitude of somatic symptom distress in a university Behavioral Medicine Clinic [48]. Vaitl et al. [207] reported a significant positive relationship between TAS and baroreflex sensitivity. This modulation of cardiovascular baroreflex sensitivity by TAS has apparently been independently replicated twice [208]. It appears that the TAS measures at least a cognitive–affective trait that modulates human sensory experiences and may be related to anomalous sensory experiences across cultures and somatic symptoms [209]. High TAS appears to be associated with somatic symptoms in clinical and normal samples during threat (HPAA) perception, induced by invasive physical and psychosocial procedures [42,43,48,49,50,64]. In the thermal grill illusion test, amplified pain perception was associated with two HRMTP risk factors, Absorption and Neuroticism [203].
5.3. Predisposing Risk Factor Trait High Alexithymia Is Correlated Negatively with Low Hypnotizability and During Threat-Induced Functional Somatic Disorders
Trait High Alexithymia literally means “without words for feelings” [210] and is empirically linked to emotional dysfunction [81,143] and is also apparently linked to affective agnosia [78,80]. A seminal study by Frankel, Apfel-Savitz, Nemiah & Sifneos [72] reported an inverse correlation between two tests of trait hypnotizability (the Harvard test and the Hypnotic Induction Profile test of [211]) and an early measure of Alexithymia in a clinical (n = 32) sample, replicated three times with the same patients. This early inverse correlation between two measures of hypnotizability and Alexithymia was replicated by [74,75] with a larger normal sample (n = 286) and the present TAS-20 psychometric test of Alexithymia. Költő and Banyai [75] reported an inverse and more specifically a nonlinear or quadratic relationship between the Harvard and the TAS-20 scores.
Alexithymia is measured today with the Toronto Alexithymia scale (TAS-20), a psychometric scale which has high reliability and good construct validity [81,143]). High Alexithymia or High TAS-20 is associated with both functional and organic somatic symptoms [73] and with both a deficit in emotional processing and a surplus in emotional reactivity [73]. These claims about High Alexithymia and emotionality appear problematic. The TAS-20 uses verbal report measures of beliefs to measure three factors in Alexithymia: 1. deficits in identifying feelings, 2. deficits in describing feelings to other people and 3. a constricted imagination-fantasy process and externally oriented thinking (EOT). High Alexithymia appears empirically related to emotional dysregulation and insecure attachment to primary caregivers in childhood [81]. The above three personality features appear congruent with low hypnotizability [212].
A large mail survey using the TAS-20 and the Danish twin Registry (N = 8785) found that genetic factors have a similar impact on all three factors of Alexithymia [213]. Alexithymia (low hypnotizability) is strongly to moderately correlated with FSD or somatization [78,81,143,214,215,216]. The functional somatic symptom and High Alexithymia link appears to hold even in multiple brain-imaging studies [80,214].
Affective agnosia [78], a separate but related construct, is measured with the Levels of Emotional Awareness Scale—LEAS—and is a performance-based measure of a deficit or absence of the ability to experience feelings [78]. The above two test measures of the emotional domain correlate poorly [78]. Van Der Velde et al. [214], in a brain-imaging study, reported that High Alexithymia is associated with (1) stronger activation of the anterior cingulate cortex (ACC) during emotion processing, (2) lower activation in the emotional attention system and (3) reduced activation in areas of cognitive emotional processing. A meta-analysis of 258 patients found a significant association between Alexithymia and the risk of delay in visits to the ER even during acute myocardial infarction [217]. High Alexithymia is also reliably associated with a lack of response to psychotherapy [27,78,81]. FSD patients presenting IBS and High in Alexithymia (negatively correlated with low hypnotizability) respond to invasive rectal distention in a brain-imaging study with strong physiological reactivity in the brain’s insula but a reduced subjective verbal report of pain sensitivity [79,214]. The magnitude of this incongruence between verbal report and direct physiological measures is predicted by the HRMTP to be larger during high stressful stimulation vs. low stressful stimulation [26,27,69,70].
Less is known empirically about trait low hypnotizability (LH) per se, except for a propensity to reduced cognitive flexibility and reduced automatic or involuntary imagery as is apparently associated with HH [218]. According to the HRMTP, low hypnotizable people (on the Harvard and Stanford scales) are postulated to show an incongruence between a) verbal report measures of threat and pain perception and b) direct physiological measures of pain and threat perception (EDR, frontalis EMG, BVP, HRV, BP, etc.). In low hypnotizable (LH) normal people, this postulated incongruence between verbal report measures vs. direct physiological measures (EMG, EDR and BP) of threat perception was empirically first confirmed by Pomerantz & Wickramasekera (1992) [70] and in Pomerantz’s (1986) [69] dissertation. As previously reported, traits hypnotizability and Alexithymia are negatively correlated in normal and clinical samples [75,177]. Many years later, Gastroenterologists Kano and Fukodo [216], using fMRI technology and the TAS-20 Alexithymia scale, appear to confirm this early Pomerantz and Wickramasekera [70] report with the blunt words, “The neural mechanism of Alexithymia is therefore activated more on a” physiologic, motor-expressive level and less in the cognitive-experiential domain of the emotional response system.” This incongruence between objective physiological measures and indirect verbal subjective report measures of pain during high threat perception (rectal distention) appear to link High Alexithymia [219] and low behaviorally (Harvard scale) measured hypnotizability [70]. It appears from the above review that all three traits (hypnotizability–suggestibility, Absorption and Alexithymia), despite discrepant labels, empirically converge to predispose people to FSD as postulated by the HRMTP [27,30,33].
6. Is Pavlovian Learning of Biologically Embedded Threat Perception Modulated by the Predisposing, Triggering and Buffering Risk Factors of the HRMTP?
“Stress is a state of mind, involving both the brain and body as well as their interactions; … it also reflects stable epigenetic modifications in development that set lifelong patterns of physiological reactivity and behavior through biological embedding of early environments interacting with cumulative change from experiences over the lifespan.”(McEwen, 2012, PNAS, p. 17180 [6])
Clinical threat learning [27,33,53,54,61] is postulated to be mediated by unconscious automatic emotional amygdala circuits [4,220] that precede laboratory-induced conscious cognitive expectancies and appraisal [221]. Jensen et al. [222,223,224] showed through associative learning and brain-imaging data that masked or unconscious neutral stimuli (CS) can automatically elicit placebo and nocebo responses and analgesic and hyperalgesic pain responses through unconscious neural mechanisms [224]. Hence, fMRI [222,223] and now behavioral data from Poland [225] show that placebo and nocebo effects can operate automatically and unconsciously, if triggered by the context effects of associative neutral stimuli (CS) of persons and places [33,53,54,61,226,227]. Biologically embedded body memories of unconscious learned threats (CS-US) in childhood [6,14,56,57] may be elicited by the HRMTP’s Triggering risk factors, adverse childhood experiences (ACEs) and/or stressful life experiences (SLEs) in adults [6,14,29,31,36,38,56,57,228].
These mechanisms of biological embedding include altered neuroendocrine stress regulation, chronic intermittent activation of the HPAA and apparent ANS dysregulation [35,37,94] and stable altered gene expression in methyl groups [14,228,229]. It is postulated based on strong correlative data but still incompletely understood causal epigenetic mechanisms (e.g., heterochromatin and Euchromatin) that threat perception learning sets lifelong patterns of physiological reactivity and behavior through biological embedding of the early childhood environment, interacting with cumulative change through associative and other mechanisms of learning over the life span [6,7,29,37,56,228]. Biologically embedded risk factors like ACEs and stressful life events (SLEs) in adults appear to operate automatically and unconsciously if triggered by present neutral stimuli (CS) of nocebo experiences and are apparently based on stable changes in DNA methylation trajectories [6,56,228].
7. Are Predisposing Risk Factors Linked to Triggering Risk Factors of the HRMTP?
Brennan et al. [132] empirically showed that the HRMTP’s Predisposing risk factor (1) High trait Negative Affectivity links (p < 0.001) to Triggering risk factors (2) adverse childhood experiences (ACEs) and (3) adult stressful life events. These three risk factors of the HRMTP are postulated to be elicited by neutral CS unconsciously and automatically and linked through associative learning of threat perception [53,54,61,222,223,224,225] to present or adult nocebo effects and FSD [29,36]. In a groundbreaking nocebo effect study, apparently implicating epigenetics, Benedetti et al. [60] found that the rate and magnitude of nocebo somatic effects induced by suggested threat (HPAA) learning in 378 heathy adults, through an inert or “fake placebo oxygen” inhalation procedure, correlated with maternal plasma cortisol measured during the first, second and third trimester of maternal pregnancy. In these healthy adults, it was found that suggested high adverse event reports of somatic symptoms, in response to fake oxygen inhalation, including headache, chest pain, abdominal pain and objective cough, and plasma cortisol responses were positively correlated with intrauterine maternal plasma cortisol. If replicated, this correlational finding about maternal cortisol levels in the intrauterine milieu modulating nocebo hyperalgesia in high adverse event reports in adulthood [60] is consistent with the HRMTP’s hypothesis of unconscious and automatic biologically embedded threat [14] elicited by neutral CS (fake oxygen inhalation) Triggering biologically embedded risk factors like (1) adverse childhood events (ACEs) and (2) stressful life events in adults (SLEs) modulating present nocebo effects and FSD in adults.
Respiratory Heart Rate Variability [19] Learning Activates and Modulates the Vagal Brake in Emotional Learning
It is known that relative to neutral (CS) sensory stimuli, attention and perceptual thresholds are biased towards stimuli that convey threat HPAA (UCS) to survival [230], and attentional salience appears critical in placebo and nocebo effects [231]. Placebo and nocebo somatic effects are learned hopeful or threatening patient emotional responses induced by invasive fake (inert, neutral or CS) medical procedures. Behavioral and neuroimaging data indicate both additive and interactive modulation of trait and state emotional-affect in the top-down central nervous system (CNS) modulation of human attention [232]. The HRMTP [30,31,33] postulates that unconscious and automatically Triggered feelings of (1) safety–hope or (2) threat–fear drive clinical placebo and nocebo learning experiences and FSD.
The HRMTP and Polyvagal theory [76,233,234,235] appears consistent with the primacy of human emotions of safety (placebo) and threat (nocebo) in human learning [30,53,61,236] in clinical situations, implicating hormonal changes [9] modulating human emotional behavior [135,236,237]. Polyvagal theory [76,233] proposes that unconscious neural evaluation (“neuroception”) of risk and safety reflexively triggers shifts in ANS states without requiring conscious awareness or cognitive appraisal [221,238]. Polyvagal theory also appears consistent with the biological embedding of threatening adverse childhood experiences [6,14]. Polyvagal theory [76,233] postulates that social connectedness and trust are a core biological imperative for human survival, since human survival particularly in the health care domain is dependent on trusted others (parents and doctors) and is wired into our genetics and is expressed through the life span from the moment of birth [233,234,235], mediated by the new ventral vagal complex [76,233]. There is apparently some controversy about the neuroanatomical basis of Polyvagal theory [239,240].
Polyvagal theory proposes that trusting social engagements are mediated through the ventral vagal complex and this complex has been empirically linked to trait high hypnotizability [241]. High-frequency (HF) heart rate variability (HRV) measures are related to vagal modulation of heart rate [146]. In a sample of normal nursing students, there was a strong relationship between measured (Harvard scale) trait hypnotizability and both cardiac vagal tone (r = 0.45) and baseline heart rate (r = −0.47) in the students [241]. These two variables were strongly interrelated (r = −0.78). Thus, individuals with a lower heart rate and greater cardiac vagal tone were higher in trait hypnotizability. Blood pressure variables were not related to trait hypnotizability. Multiple regression analyses indicated that approximately 40% of the individual difference variance in hypnotizability was accounted for by baseline cardiac vagal tone and heart rate reactivity during experimentally manipulated mood states [151] in the students. Heart-rate variability (HRV) also appears to be a quantitative measure of subjective self-reported hypnotic depth (SRHD) with normal people [242] measured for trait hypnotizability with the brief clinical Hypnotic Induction Profile [243]. This small study (n = 10) found a significant linear relationship between SRHD and the high frequency (HF) component of HRV.
High-frequency heart rate variability (HF-HRV) biofeedback training delivered in a threatening context (a medical clinic) may temporarily reduce threat perception (HPAA) of the clinic through associative learning and amplify safety perception of the clinic and the patient’s emotional self-regulation [243,244,245,246]. HF-HRV biofeedback training [245] can be particularly effective with people of low and moderate trait hypnotizability (approximately 85% of the general population) if delivered in conjunction with warmth and empathy [61,71,247] to increase their objective vagal tone, reduce SNS activation and increase their verbal–cognitive receptivity to therapeutic verbal suggestion [33,61,71,151,241]. Oscillations in heart rate [248], an aspect of heart rate variability (HRV), show robust associations with psychological health [245,249,250] despite some neuroanatomical controversy related to Polyvagal theory [235,239,240,246].
Neural oscillations may interact directly with slower physiological rhythms, like heart rate and respiration [244]. Mather & Thayer [244] proposed that associations between HRV and psychological health may reflect a causal influence of cardiac rhythms on neural activity. Granger causality analyses indicate stronger heart-to-brain than brain-to-heart effects in all frequency bands except gamma [248] as originally proposed by Sir William Harvey in 1628 [27]. The above finding appears consistent with the reciprocal and bottom-up physiological regulation hypothesis [27,237] and the primacy of human emotions in placebo (safety and hope) and nocebo (threat–fear) clinical emotional learning [27,61,71,135,236,237].
8. Frequency of Functional Somatic Disorders in Primary Care Medicine and the Risk of Unintentional Iatrogenic Injury in the Invasive Medical–Surgical Hospital Context
“Pain syndrome patients, in their desperate search for the elusive cure, often chase “windmills” and convince their doctors to perform a myriad of invasive tests, and procedures. As a result of their pain behaviors, many experience iatrogenic complications, suffering and disability.”—G.M. Aronoff, MD Editor, Clinical Journal of Pain, 1(1) 1985 [251].
Patients presenting with acute somatic nocebo effects [29] or chronic stress-related somatic symptoms (SRSSs) without identified pathophysiology [26,28,30,31,32] or FSD [55] are approximately 30–50% of all presentations in primary care medicine [35,55,58,252,253]. Patients with chronic pain are known to overutilize medical diagnostic and surgical services to sometimes legitimize and be socially reinforced (empathy) and supported in their chronic disability and demands [27,59,138,253,254].
Two Subsets of Patients at Risk for Unintentional Iatrogenic Injury
According to the HRMTP there appear to be at least two subsets of patients with chronic pain and somatic symptoms at risk of overutilizing medical–surgical services.
The first subset at risk, despite discrepant descriptive labels, are trait high hypnotizability–suggestibility and related trait High Absorption patients, with ANS sympathetic hyperactivity to threat [21,22,23,34]. This first subset of FSD patients, if low on Alexithymia and therapy-compliant, is receptive and responsive to multiple forms of structured psychosocial therapy like CBT, EMDR, psychophysiological–biofeedback therapy [27,36,197] and pain reprocessing therapy [255] and have moderate to high efficacy rates in private and public pain clinics.
The second subset of FSD patients at risk for overutilizing medical–surgical services are postulated to be low on trait suggestibility–hypnotizability, Low on trait Absorption [111] and High on trait Alexithymia. According to the HRMTP, low hypnotizable people (on the Harvard and Stanford scales) are postulated to show emotional anomalies, such as an incongruence between (a) verbal report measures of threat and pain perception and (b) direct objective physiological measures of pain and threat perception (e.g., EDR, frontalis EMG, BVP, HRV, BP, etc.). The magnitude of this incongruence between verbal report and direct physiological measures is predicted by the HRMTP to be larger during high stressful stimulation vs. low stressful stimulation [26,27,69,70]. This second subset is associated with incongruities in ANS reactivity and perhaps affective agnosia [78,80], chronic somatic symptoms and ANS dysregulation [22,30,47,77,78,79,80,81,143,214,216]. This second subset is postulated by the HRMTP to be very likely insisting specifically on medical–surgical resolution of their pain or distressing somatic symptoms, even without pathophysiological findings [253,254,256]. These patients are postulated to be cognitively–affectively locked into a biomedical model [52] of their chronic pain or somatic symptoms. This low hypnotizability and High Alexithymia subset of FSD patients are cognitively–emotionally rigid and have a high dropout rate from conventional psychotherapy [27,73,81].
The diagnosis of FSD by inclusion of psychosocial risk factors (HRMTP) may reduce the risk of unintentional iatrogenic injury to patients with FSD, who are insisting on medical–surgical resolution of their chronic and distressing somatic symptoms [27,138,253,254]. Unintentional iatrogenic injury appears to be a leading cause of mortality in the USA [257,258,259,260]. A report in 2000 from the Institute of Medicine, National Academy of Sciences [257] found that 98,000 patients die in any given year from unintentional medical errors that occur in hospitals, which is more than died from motor vehicle accidents or breast cancer in 2000. Ten years later, Landrigan et al. in the NEJM [258], in a retrospective study of a stratified random sample of 10 hospitals in North Carolina from 2002 to 2007, found that multivariate analyses of hospital harms identified by internal reviewers showed no significant changes in the overall rate of harms per 1000 patient days from the earlier study [256]. Makary & Daniel [259], in a controversial paper in the British Medical Journal, reported that medical errors were the third leading cause of death in the USA. A recent apparent update on Medical Error Reduction and Prevention reports that medical errors are still a leading cause of death in the US [260]. It is likely that some unknown percentage of these patients may be FSD. In this busy context of technologically sophisticated medical care and scientific information compassionately applied, learned medical skills and science [7,261] battle the constraints of natural disease and death daily.
In the early years of biofeedback therapy [61,160], it was empirically established that there was little or no correlation between experimental alterations in ANS or CNS physiological signals (EMG, EEG, EDR and peripheral Blood Volume Pulse) and the efficacy of clinical outcomes [27,61,197,262,263,264]. It was clear that non-specific factors or placebo effects accounted for the bulk of the variance in the reduction in autonomically mediated clinical somatic symptoms. Hence, it was imperative to specify the learning mechanisms of placebo somatic effects [2,53,54,226] to identify the psychosocial risk factors modulating placebo and nocebo somatic effects and somatization or FSD. A promising and successful early effort to reduce chronic pain and recruit non-specific suggestibility effects was demonstrated by Ronald Melzack & Campbell Perry in an early salient paper in Experimental Neurology [265] and elsewhere [71,266,267].
9. The Conditioned Response Model (CRM) of Emotional Learning of Placebo and Nocebo Somatic Effects and FSD
It is postulated that primitive mechanisms of threat–fear (nocebo) and safety–hope (placebo) perception are associated with the emotional learning, implicated in the context of invasively learned fake placebo and nocebo somatic effects [10,12,53,54,61,197].
“Wickramasekera was the first to propose a broad and coherent theoretical account of placebo effects as conditional reflexes” [225]. Kirsch [221,268] challenged this view and proposed that response expectancy was a determinant of experience and behavior and Placebo effects and Colloca & Miller [269] accepted the expectancy model but expanded it to include conditioned stimuli and the psychosocial context. But expectancies are by definition conscious events and there is a large and growing body of empirical data establishing, under different labels (Classical conditioning, Nonconscious activation of placebo effects, Hidden conditioning, subliminal or low intensity sensory stimuli) providing evidence that unconscious and automatic mechanisms establish placebo and nocebo effects [222,224].
Mechanisms
- Positive or negative verbal suggestion is postulated by the CRM to induce placebo or nocebo somatic effects and FSD, and all invasive verbal suggestion is postulated to be modulated by the innately effective (US-UR) psychosocial active ingredient trait hypnotizability–suggestibility [33,35,36,53,54,61,154,267,270]. Two large meta-analyses found that trait hypnotizability–suggestibility modulates, in a dose–response or linear manner, the efficacy of verbal suggestions to reduce clinical and experimental threat and pain perception [39,40].
- Interpersonal delivery of rapport through accurate verbal Empathy and Warmth, are innately effective (US-UR) psychosocial active stimuli to induce and modulate placebo and nocebo somatic effects and FSD. Empirically, empathy and warmth can modulate anxiety, threat and pain perception [27,264,271,272,273,274,275,276]. It also appears that empathy is modulated by trait hypnotizability-suggestibility [247].
- Pavlovian (CS-US) and other learning (operant, cognitive, observational, evaluative conditioning) is postulated to be modulated by trait Hypnotizability-Suggestibility [101,102,103,104,105,106,109,277].
Predictions:
- The CRM predicts that the identification and application of innately effective [53,54,61,197] psychosocially active stimuli (US-UR), in the context of increasingly invasive [278] and threatening medical–surgical procedures (US-UR) on patients, can amplify the magnitude of future placebo effects in clinical trials [61,197,278,279,280,281,282,283].
- Associative learning can, through neutral stimuli (CS), automatically and unconsciously [222,223] trigger activation or deactivation of previously learned (e. g., adverse childhood experiences and traumatic major life changes like the injury or death of a parent) and biologically embedded nocebo effects [6,7,28,29,31,35,37,54,56,228] through epigenetic mechanisms, like heterochromatin and Euchromatin [284,285,286].
- Trait hypnotizability–suggestibility is postulated to be an innately effective (US-UR) modulator of empathy learning [247], verbal suggestion learning and associative learning of placebo somatic effects [101,102,103,104,105,106], nocebo somatic effects [106,107,108,109] and functional somatic disorders [23,30,33,34,41,44,45].
- It is predicted by the CRM and HRMTP that chronic anomalies and incongruities [27,69,70,71] in emotional perception and emotional learning and ANS reactivity in trait low hypnotizability–suggestibility and High Alexithymia can reduce HRV [19] and increase risk of ANS dysregulation [28,30,31,35,36,79,80,81] as postulated in chronic threat and pain perception associated with allostasis and biological embedding [6,7,82].
- It is predicted that trait high hypnotizability (HH) amplifies threat perception, and that HH is a risk factor for FSD, unless the patient’s HH is mobilized specifically by verbal hypnotherapy or non-specifically by psychosocial therapies, like pain reprocessing therapy, CBT, EMDR, or biofeedback therapy.
10. Clinical vs. Experimental Contexts
Recent studies suggest that experimental placebo effects may be unstable across contexts (experimental vs. clinical) but that clinical placebo effects as in chronic pain patients can be predicted by genetics, brain properties and language use [11]. Clinical associative emotional learning (CS-US) experiences are postulated by the Conditioned Response Model (CRM) of the placebo and nocebo somatic effects to be modulated by trait high hypnotizability–suggestibility [53,54,61], especially in interaction with the Triggering risk factors like adverse childhood experiences (ACEs) of the HRMTP. Placebo effects and pain perception can be significantly different in clinical vs. experimental pain situations because of the time- and place-constrained nature of experimental pain vs. the ongoing aversive nature of clinical pain. Nocebo threat learning frequently occurs in previous failed clinical experience contexts [226,227,287].
11. The Psychophysiology of the Clinician–Patient Relationship and Associative Emotional Learning Modulated by Trait Hypnotizability–Suggestibility and Social Support
The efficacy of the psychophysiology of healing, is postulated to be modulated by innately effective biological (US-UR) and psychosocial stimuli like empathy, warmth and the trait hypnotizability of persons as evidenced by behavioral and psychophysiological measures [9,264,272,273,274,276,288,289] and specifically linked to High Empathy and to trait High Hypnotizability [247]. Empathy and warmth were operationalized for measurement with psychometric scales [279] and now appear to be innately effective psycho-social stimuli (US-UR) for mental and somatic healing [27,276,290]. Social support [97,99,100,291] empathy and warmth are now increasingly supported by neural brain imaging data and operationalized by the specificity of perceived “interpersonal trust” [272,273,274,289]. An fMRI study found significant reduction in the neural systems supporting emotional and behavioral threat responses when women held their husband’s hand. Neural threat responses varied as a function of marital quality and were specific to the husband and but not a stranger [292]. Social support decreased pain-related skin conductance responses (EDR’s) in both women and men and social support reduced threat activation in neural data (fMRI) indicated by reduced nociceptive signals [274]. Doctor-patient warmth and empathy reduced nocebo effects and amplified placebo effects in a fake oxytocin nocebo and placebo study of 84 people [271]. In HH people, verbal suggestions reduce conflict in the brain and is associated with reduced anterior cingulate cortex activation (fMRI measure) but not in trait Low Hypnotizable (LH) people [189,293]. Theoretically, the Conditioned Response Model of associative emotional learning predicts that low empathy and low warmth [271] can negatively modulate the neutral stimuli (CS) of a doctor and an invasive medical procedure in a clinical context [33,53,54,61]. Neutral stimuli (CS) can elicit unconscious and automatic associative threat activation and nocebo effects [222,223,224] from any Predisposing (high catastrophizing) and Triggering (adverse childhood experiences) risk factors of the HRMTP in a specific patient.
Psychosocial active ingredients or innately effective stimuli (US-UR) like physician delivered (1) high empathy and (2) high warmth [271,276] in interaction with (3) High hypnotizability in the patient, can reduce or abolish a patient’s pain and threat perception [27,39,40]. These innately effective psychosocially active ingredients (US-UR) can be mobilized to amplify the efficacy of verbal suggestion to reduce nocebo somatic effects and to increase placebo effects [103,104,271] and to reduce threat perception that drives Functional Somatic Disorders [23,30,33,34,41,44,45].
International survey data of health care professionals (without measurement of trait hypnotizability) indicates that verbal hypnotic procedures [294] can amplify the efficacy of doctor-patient rapport induction procedures particularly in GI disorders [295].
12. General Predictions from the CRM and the HRMTP
- The CRM predicted that as new innate specific active biological ingredients (US-UR), including psychosocial active ingredients (e.g., trait hypnotizability, empathy and warmth) for “healing” are isolated, paradoxically the placebo response can get stronger in future randomized placebo-controlled gold standard clinical trials [53,54,61]. This early prediction of amplified placebo effects in future clinical trials [53,54,61] appears to be supported today by the high reported correlation (r = 0.73) between placebo effects and pharmacological effects in recent clinical randomized controlled trials [281] predicted by Wickramasekera in 1980 and 1985. The increased magnitude of placebo effects in US clinical trials of pain and especially of neuropathic pain [282,296] support the CRM prediction. The progressive mean increases in placebo effects (40%) in Irritable Bowel Syndrome—IBS [297] are also supportive of the CRM prediction. The recent review of treatment effects in pharmacological randomized controlled clinical trials of five diseases [281] stated that the placebo effect is the “major driver of treatment effects in clinical trials that alone explains 69% of the variance” [281]. This review [281] of the efficacy of 150 pharmacological randomized controlled clinical trials found that 72% of the variance in treatment effects could be attributed to placebo effects or context effects.
- The HRMTP predicts that, in FSD patients with chronic pain, intermittent threat perception can drive dysregulation of the ANS and PTI. This prediction was apparently confirmed by the association of experimental threat induction and Paradoxical Increase in hand Temperature (PTI) in approximately 50% of 224 of chronic pain patients of both genders. This PTI was first experimentally demonstrated by Wickramasekera et al. [37] and replicated independently in a PhD dissertation [96].
- The HRMTP predicts that the primary Predisposing risk factors (a) trait hypnotizability–suggestibility, if it implicates threat learning, interacting with other HRMTP risk factors (e.g., high catastrophizing, high ACEs and low social support) can maladaptively amplify threat perception in an exponential manner and launch a progressive trajectory of severe morbidity, if not mortality.
- Acute nocebo effects may be the maternity ward of FSD [30,33,54]. Acute nocebo effects can become chronic FSD resistant to specific medical–surgical therapy.
13. Conclusions
Replicated clinical and even experimental studies in the last 50 years are supportive of the Conditioned Response Model’s [33,53,54] three mechanisms of emotional learning of clinical placebo and nocebo effects and FSD.
The High Risk Model of Threat Perception [24,30,33] predicts that the Predisposing, Triggering and Buffering psychosocial risk factors that modulate threat (HPAA) perception will also modulate the learning of placebo, nocebo and functional somatic disorders (FSDs). Recent independent reviews [5,231,298] appear to confirm these predictions.
Funding
This research received no external funding.
Acknowledgments
I am grateful for the towering integrity and the anchoring security of my loving wife Judy for her support, her encouragement and her patience during the many days and years I have spent thinking, reading and writing on these topics, even after she became ill and died during the pandemic of 2020–2021 when incidentally I was invited by -the chair to speak on this topic at the 2021 SIPS conference. I want to thank Mark Zinn for his kindness, patience and IT assistance with this paper.
Conflicts of Interest
The author declares no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| HRMTP | High Risk Model of Threat Perception |
| CRM | Conditioned Response Model |
| FSD | Functional Somatic Disorder |
| HPAA | Hypothalamus–Pituitary–Adrenal Axis |
| ANS | Autonomic Nervous System |
| PTI | Paradoxical Hand Temperature Increase |
| SRSSs | Stress-Related Somatic Symptoms |
| US | Unconditioned Stimulus |
| UCR | Unconditioned Response |
| CS | Conditioned Stimulus |
| CR | Conditioned Response |
References
- Nicholson, L.B. The Immune System. Essays Biochem. 2016, 60, 275–301. [Google Scholar] [CrossRef]
- Ader, R. Conditioned Immunopharmacological Effects in Animals: Implications for a Conditioning Model of Pharmacotherapy. In Placebo: Theory, Research, and Mechanisms; White, L., Tursky, B., Schwartz, G.E., Eds.; Guilford Press: New York, NY, USA, 1985; pp. 306–323. [Google Scholar]
- Hadamitzky, M.; Lückemann, L.; Pacheco-López, G.; Schedlowski, M. Pavlovian Conditioning of Immunological and Neuroendocrine Functions. Physiol. Rev. 2020, 100, 357–405. [Google Scholar] [CrossRef] [PubMed]
- LeDoux, J.E. Coming to Terms with Fear. Proc. Natl. Acad. Sci. USA 2014, 111, 2871–2878. [Google Scholar] [CrossRef] [PubMed]
- Fiorio, M.; Braga, M.; Marotta, A.; Villa-Sánchez, B.; Edwards, M.J.; Tinazzi, M.; Barbiani, D. Functional Neurological Disorder and Placebo and Nocebo Effects: Shared Mechanisms. Nat. Rev. Neurol. 2022, 18, 624–635. [Google Scholar] [CrossRef] [PubMed]
- McEwen, B.S. Brain on Stress: How the Social Environment Gets under the Skin. Proc. Natl. Acad. Sci. USA 2012, 109, 17180–17185. [Google Scholar] [CrossRef] [PubMed]
- McEwen, B.S. Chapter 5—Central Role of the Brain in Stress and Adaptation: Allostasis, Biological Embedding, and Cumulative Change. In Stress: Concepts, Cognition, Emotion, and Behavior; Fink, G., Ed.; Academic Press: San Diego, CA, USA, 2016; pp. 39–55. ISBN 978-0-12-800951-2. [Google Scholar]
- Smith, S.M.; Vale, W.W. The Role of the Hypothalamic-Pituitary-Adrenal Axis in Neuroendocrine Responses to Stress. Dialogues Clin. Neurosci. 2006, 8, 383–395. [Google Scholar] [CrossRef]
- Benedetti, F.; Pollo, A.; Lopiano, L.; Lanotte, M.; Vighetti, S.; Rainero, I. Conscious Expectation and Unconscious Conditioning in Analgesic, Motor, and Hormonal Placebo/Nocebo Responses. J. Neurosci. 2003, 23, 4315–4323. [Google Scholar] [CrossRef]
- Botvinik-Nezer, R.; Petre, B.; Ceko, M.; Lindquist, M.A.; Friedman, N.P.; Wager, T.D. Placebo Treatment Affects Brain Systems Related to Affective and Cognitive Processes, but Not Nociceptive Pain. Nat. Commun. 2024, 15, 6017. [Google Scholar] [CrossRef]
- Branco, P.; Vachon-Presseau, E.; Hall, K.T.; Wager, T.D.; Vania Apkarian, A. C2.1Predictability of Placebo Responses and Their Clinical Implications. In Placebo Effects Through the Lens of Translational Research; Colloca, L., Noel, J., Franklin, P.D., Seneviratne, C., Eds.; Oxford University Press: Oxford, UK, 2023. [Google Scholar]
- Colloca, L. Emotional Modulation of Placebo Analgesia. Pain 2014, 155, 651. [Google Scholar] [CrossRef]
- Colloca, L.; Raghuraman, N.; Wang, Y.; Akintola, T.; Brawn-Cinani, B.; Colloca, G.; Kier, C.; Varshney, A.; Murthi, S. Virtual Reality: Physiological and Behavioral Mechanisms to Increase Individual Pain Tolerance Limits. Pain 2020, 161, 2010–2021. [Google Scholar] [CrossRef]
- Berens, A.E.; Jensen, S.K.G.; Nelson, C.A. Biological Embedding of Childhood Adversity: From Physiological Mechanisms to Clinical Implications. BMC Med. 2017, 15, 135. [Google Scholar] [CrossRef]
- Timmers, I.; Quaedflieg, C.W.E.M.; Hsu, C.; Heathcote, L.C.; Rovnaghi, C.R.; Simons, L.E. The Interaction between Stress and Chronic Pain through the Lens of Threat Learning. Neurosci. Biobehav. Rev. 2019, 107, 641–655. [Google Scholar] [CrossRef]
- Timmers, I.; López-Solà, M.; Heathcote, L.C.; Heirich, M.; Rush, G.Q.; Shear, D.; Borsook, D.; Simons, L.E. Amygdala Functional Connectivity Mediates the Association between Catastrophizing and Threat-Safety Learning in Youth with Chronic Pain. Pain 2022, 163, 719–728. [Google Scholar] [CrossRef] [PubMed]
- Woda, A.; Picard, P.; Dutheil, F. Dysfunctional Stress Responses in Chronic Pain. Psychoneuroendocrinology 2016, 71, 127–135. [Google Scholar] [CrossRef]
- Algra, A.; Tijssen, J.G.; Roelandt, J.R.; Pool, J.; Lubsen, J. Heart Rate Variability from 24-Hour Electrocardiography and the 2-Year Risk for Sudden Death. Circulation 1993, 88, 180–185. [Google Scholar] [CrossRef] [PubMed]
- Menuet, C.; Ben-Tal, A.; Linossier, A.; Allen, A.M.; Machado, B.H.; Moraes, D.J.A.; Farmer, D.G.S.; Paterson, D.J.; Mendelowitz, D.; Lakatta, E.G.; et al. Redefining Respiratory Sinus Arrhythmia as Respiratory Heart Rate Variability: An International Expert Recommendation for Terminological Clarity. Nat. Rev. Cardiol. 2025, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Shanks, J.; Abukar, Y.; Lever, N.A.; Pachen, M.; LeGrice, I.J.; Crossman, D.J.; Nogaret, A.; Paton, J.F.R.; Ramchandra, R. Reverse Re-Modelling Chronic Heart Failure by Reinstating Heart Rate Variability. Basic Res. Cardiol. 2022, 117, 4. [Google Scholar] [CrossRef]
- Jorgensen, T.; Dantoft, T.M.; Petersen, M.W.; Gormsen, L.; Winter-Jensen, M.; Fink, P.; Linneberg, A.; Benros, M.E.; Eplov, L.F.; Bjerregaard, A.A.; et al. Is Reduced Heart Rate Variability Associated with Functional Somatic Disorders? A Cross-Sectional Population-Based Study; DanFunD. BMJ Open 2024, 14, e073909. [Google Scholar] [CrossRef]
- Greenleaf, M.; Fisher, S.; Miaskowski, C.; DuHamel, K. Hypnotizability and Recovery from Cardiac Surgery. Am. J. Clin. Hypn. 1992, 35, 119–128. [Google Scholar] [CrossRef]
- Jorgensen, M.M.; Zachariae, R. Autonomic Reactivity to Cognitive and Emotional Stress of Low, Medium, and High Hypnotizable Healthy Subjects: Testing Predictions from the High Risk Model of Threat Perception. Int. J. Clin. Exp. Hypn. 2002, 50, 248–275. [Google Scholar] [CrossRef]
- Wickramasekera, I. A Model of the Patient at High Risk for Chronic Stress Related Disorders: Do Beliefs Have Biological Consequences? In Proceedings of the Annual Convention of the Biofeedback Society of America, San Diego, CA, USA, 23–27 February 1979; Biofeedback Society of America: Wheat Ridge, CO, USA, 1979. [Google Scholar]
- Wickramasekera, I. A Model of People at High Risk to Develop Chronic Stress-Related Symptoms. In Stress and Tension Control; McGuigan, F.J., Ed.; Plenum: New York, NY, USA, 1984. [Google Scholar]
- Wickramasekera, I. Risk Factors That Lead to the Development of Chronic Stress Related Symptoms. Advances 1986, 4, 9–35. [Google Scholar]
- Wickramasekera, I. Clinical Behavioral Medicine: Some Concepts and Procedures; Plenum: New York, NY, USA, 1988. [Google Scholar]
- Wickramasekera, I. Assessment and Treatment of Somatization Disorders: The High-Risk Model of Threat Perception. In Handbook of Clinical Hypnosis; Lynn, S., Rhue, J., Kirsh, I., Eds.; American Psychological Association: Washington, DC, USA, 1993. [Google Scholar]
- Wickramasekera, I. Somatic to Psychological Symptoms and Information Transfer from Implicit to Explicit Memory: A Controlled Study with Predictions from the High Risk Model of Threat Perception. Dissociation Prog. Dissociative Disord. 1994, 7, 153–166. [Google Scholar]
- Wickramasekera, I. Somatization. Concepts, Data, and Predictions from the High Risk Model of Threat Perception. J. Nerv. Ment. Dis. 1995, 183, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Wickramasekera, I. Secrets Kept from the Mind but Not the Body or Behavior: The Unsolved Problems of Identifying and Treating Somatization and Psychophysiological Disease. Adv. Mind-Body Med. 1998, 14, 81–98. [Google Scholar]
- Wickramasekera, I. The High Risk Model of Threat Perception and Trojan Horse Role Induction: Somatization and Psychophysiological Disease. In Handbook of Mind-Body Medicine for Primary Care; Moss, D., McGrady, A., Davies, T., Wickramasekera, I., Eds.; Sage: Thousand Oaks, CA, USA, 2003; pp. 19–42. [Google Scholar]
- Wickramasekera, I. Specific Predictions from the Conditioned Response Model (CR) of the Placebo and Empirical Data Consistent with These Specific Predictions. In Proceedings of the 3rd International Conference of the Society for Interdisciplinary Placebo Studies, Baltimore, MD, USA, 26–28 May 2021. [Google Scholar]
- Younger, J.W.; Rossetti, G.C.; Borckardt, J.J.; Smith, A.R.; Tasso, A.F.; Nash, M.R. Hypnotizability and Somatic Complaints: A Gender-Specific Phenomenon. Int. J. Clin. Exp. Hypn. 2007, 55, 1–13. [Google Scholar] [CrossRef]
- Wickramasekera, I.; Davies, T.E.; Davies, S.M. Applied Psychophysiology: A Bridge between the Biomedical Model and the Biopsychosocial Model in Family Medicine. Prof. Psychol. Res. Pract. 1996, 27, 221–233. [Google Scholar] [CrossRef]
- Wickramasekera, I.; Pope, A.T.; Kolm, P. On the Interaction of Hypnotizability and Negative Affect in Chronic Pain. Implications for the Somatization of Trauma. J. Nerv. Ment. Dis. 1996, 184, 628–635. [Google Scholar] [CrossRef]
- Wickramasekera, I.; Kolm, P.; Pope, A.; Turner, M. Observation of a Paradoxical Temperature Increase during Cognitive Stress in Some Chronic Pain Patients. Appl. Psychophysiol. Biofeedback 1998, 23, 233–241. [Google Scholar] [CrossRef]
- Perlstrom, J.R.; Wickramasekera, I. Insomnia, Hypnotic Ability, Negative Affectivity, and the High Risk Model of Threat Perception. J. Nerv. Ment. Dis. 1998, 186, 437–440. [Google Scholar] [CrossRef]
- Thompson, T.; Terhune, D.B.; Oram, C.; Sharangparni, J.; Rouf, R.; Solmi, M.; Veronese, N.; Stubbs, B. The Effectiveness of Hypnosis for Pain Relief: A Systematic Review and Meta-Analysis of 85 Controlled Experimental Trials. Neurosci. Biobehav. Rev. 2019, 99, 298–310. [Google Scholar] [CrossRef]
- Milling, L.S.; Valentine, K.E.; LoStimolo, L.M.; Nett, A.M.; McCarley, H.S. Hypnosis and the Alleviation of Clinical Pain: A Comprehensive Meta-Analysis. Int. J. Clin. Exp. Hypn. 2021, 69, 297–322. [Google Scholar] [CrossRef]
- Wieder, L.; Brown, R.; Thompson, T.; Terhune, D.B. Suggestibility in Functional Neurological Disorder: A Meta-Analysis. J. Neurol. Neurosurg. Psychiatry 2021, 92, 150–157. [Google Scholar] [CrossRef]
- Challis, G.B.; Stam, H.J. A Longitudinal Study of the Development of Anticipatory Nausea and Vomiting in Cancer Chemotherapy Patients: The Role of Absorption and Autonomic Perception. Health Psychol. 1992, 11, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Zachariae, R.; Paulsen, K.; Mehlsen, M.; Jensen, A.B.; Johansson, A.; von der Maase, H. Anticipatory Nausea: The Role of Individual Differences Related to Sensory Perception and Autonomic Reactivity. Ann. Behav. Med. 2007, 33, 69–79. [Google Scholar] [CrossRef]
- Spinhoven, P.; ter Kuile, M.M. Treatment Outcome Expectancies and Hypnotic Susceptibility as Moderators of Pain Reduction in Patients with Chronic Tension-Type Headache. Int. J. Clin. Exp. Hypn. 2000, 48, 290–305. [Google Scholar] [CrossRef] [PubMed]
- Roelofs, K.; Hoogduin, K.A.L.; Keijsers, G.P.J.; Näring, G.W.B.; Moene, F.C.; Sandijck, P. Hypnotic Susceptibility in Patients with Conversion Disorder. J. Abnorm. Psychol. 2002, 111, 390–395. [Google Scholar] [CrossRef] [PubMed]
- Andersen, M.S. Hypnotizability as a Factor in the Hypnotic Treatment of Obesity. Int. J. Clin. Exp. Hypn. 1985, 33, 150–159. [Google Scholar] [CrossRef]
- Wickramasekera, I.; Price, D.C. Morbid Obesity, Absorption, Neuroticism, and the High Risk Model of Threat Perception. Am. J. Clin. Hypn. 1997, 39, 291–301. [Google Scholar] [CrossRef]
- Gick, M.; Mcleod, C.; Hulihan, D. Absorption, Social Desirability, and Symptoms in a Behavioral Medicine Population. J. Nerv. Ment. Dis. 1997, 185, 454–458. [Google Scholar] [CrossRef]
- Kermit, K.; Devine, D.A.; Tatman, S.M. High Risk Model of Threat Perception in Chronic Pain Patients: Implications for Primary Care and Chronic Pain Programs. J. Nerv. Ment. Dis. 2000, 188, 577–582. [Google Scholar] [CrossRef]
- McGrady, A.V.; Andrasik, F.; Davies, T.; Striefel, S.; Wickramasekera, I.; Baskin, S.M.; Penzien, D.B.; Tietjen, G. Psychophysiologic Therapy for Chronic Headache in Primary Care. Prim. Care Companion J. Clin. Psychiatry 1999, 1, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Bryant, R.A.; Guthrie, R.M.; Moulds, M.L. Hypnotizability in Acute Stress Disorder. Am. J. Psychiatry 2001, 158, 600–604. [Google Scholar] [CrossRef] [PubMed]
- Engel, G.L. The Need for a New Medical Model: A Challenge for Biomedicine. Science 1977, 196, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Wickramasekera, I. A Conditioned Response Model of the Placebo Effect Predictions from the Model. Biofeedback Self Regul. 1980, 5, 5–18. [Google Scholar] [CrossRef]
- Wickramasekera, I. A Conditioned Response Model of the Placebo Effect: Predictions from the Model. In Placebo: Theory, Research, and Mechanisms; White, L., Tursky, B., Schwartz, G.E., Eds.; Guilford Press: New York, NY, USA, 1985; pp. 255–287. [Google Scholar]
- Burton, C.; Fink, P.; Henningsen, P.; Löwe, B.; Rief, W. EURONET-SOMA Group Functional Somatic Disorders: Discussion Paper for a New Common Classification for Research and Clinical Use. BMC Med. 2020, 18, 34. [Google Scholar] [CrossRef]
- Aristizabal, M.J.; Anreiter, I.; Halldorsdottir, T.; Odgers, C.L.; McDade, T.W.; Goldenberg, A.; Mostafavi, S.; Kobor, M.S.; Binder, E.B.; Sokolowski, M.B.; et al. Biological Embedding of Experience: A Primer on Epigenetics. Proc. Natl. Acad. Sci. USA 2020, 117, 23261–23269. [Google Scholar] [CrossRef]
- Schury, K.; Kolassa, I.-T. Biological Memory of Childhood Maltreatment: Current Knowledge and Recommendations for Future Research. Ann. N. Y. Acad. Sci. 2012, 1262, 93–100. [Google Scholar] [CrossRef]
- Haller, H.; Cramer, H.; Lauche, R.; Dobos, G. Somatoform Disorders and Medically Unexplained Symptoms in Primary Care. Dtsch. Arztebl. Int. 2015, 112, 279–287. [Google Scholar] [CrossRef]
- Husain, M.; Chalder, T. Medically Unexplained Symptoms: Assessment and Management. Clin. Med. 2021, 21, 13–18. [Google Scholar] [CrossRef]
- Benedetti, F.; Amanzio, M.; Giovannelli, F.; Craigs-Brackhahn, K.; Arduino, C.; Shaibani, A. Are Nocebo Effects in Adulthood Linked to Prenatal Maternal Cortisol Levels? Clin. Neuropsychiatry 2022, 19, 298–306. [Google Scholar] [CrossRef]
- Wickramasekera, I. How Does Biofeedback Reduce Clinical Symptoms and Do Memories and Beliefs Have Biological Consequences? Toward a Model of Mind-Body Healing. Appl. Psychophysiol. Biofeedback 1999, 24, 91–105. [Google Scholar] [CrossRef] [PubMed]
- Wickramasekera, I. Adjunctive Hypnotherapy. In Essentials of Complementary and Alternative Medicine; Jonas, W.B., Levin, J.S., Eds.; Williams & Wilkins: Philadelphia, PA, USA, 1999; pp. 426–443. ISBN 978-0-683-30674-3. [Google Scholar]
- Hilgard, E.R.; Hilgard, J.R. Hypnosis in the Relief of Pain, 1st ed.; William Kaufmann, Inc.: Los Altos, CA, USA, 1975; ISBN 978-0-913232-16-3. [Google Scholar]
- Zachariae, R.; Jørgensen, M.M.; Bjerring, P.; Svendsen, G. Autonomic and Psychological Responses to an Acute Psychological Stressor and Relaxation: The Influence of Hypnotizability and Absorption. Int. J. Clin. Exp. Hypn. 2000, 48, 388–403. [Google Scholar] [CrossRef] [PubMed]
- Terhune, D.B.; Cleeremans, A.; Raz, A.; Lynn, S.J. Hypnosis and Top-down Regulation of Consciousness. Neurosci. Biobehav. Rev. 2017, 81, 59–74. [Google Scholar] [CrossRef] [PubMed]
- Derbyshire, S.W.G.; Whalley, M.G.; Stenger, V.A.; Oakley, D.A. Cerebral Activation during Hypnotically Induced and Imagined Pain. NeuroImage 2004, 23, 392–401. [Google Scholar] [CrossRef]
- Derbyshire, S.W.G.; Whalley, M.G.; Oakley, D.A. Fibromyalgia Pain and Its Modulation by Hypnotic and Non-Hypnotic Suggestion: An fMRI Analysis. Eur. J. Pain 2009, 13, 542–550. [Google Scholar] [CrossRef]
- Miller, G.E.; Chen, E.; Zhou, E.S. If It Goes up, Must It Come down? Chronic Stress and the Hypothalamic-Pituitary-Adrenocortical Axis in Humans. Psychol. Bull. 2007, 133, 25–45. [Google Scholar] [CrossRef]
- Pomerantz, B. Stress and Relaxation Effects in High and Low Hypnotizables: Physiological and Subjective Measures. Doctoral Dissertation, Virginia Consortium for Professional Psychology, Norfolk, VA, USA, 1986. [Google Scholar]
- Pomerantz, B.; Wickramasekera, I. High and Low Trait Hypnotizability and Their Psychophysiological Correlates Under High and Low Stress. Washington, DC, USA, 1992. [Google Scholar]
- Wickramasekera, I. On Attempts to Modify Hypnotic Susceptibility: Some Psychophysiological Procedures and Promising Directions. Ann. N. Y. Acad. Sci. 1977, 296, 143–153. [Google Scholar] [CrossRef]
- Frankel, F.H.; Apfel-Savitz, R.; Nemiah, J.C.; Sifneos, P.E. The Relationship between Hypnotizability and Alexithymia. Psychother. Psychosom. 1977, 28, 172–178. [Google Scholar] [CrossRef]
- Luminet, O.; Nielson, K.A. Alexithymia: Toward an Experimental, Processual Affective Science with Effective Interventions. Annu. Rev. Psychol. 2025, 76, 741–769. [Google Scholar] [CrossRef]
- Költő, A. Hypnotic Susceptibility and Mentalization Skills in the Context of Parental Behavior. Ph.D. Thesis, ELTE Eötvös Loránd University, Budapest, Hungary, 2015. [Google Scholar]
- Költő, A.; Banyai, E. Hypnotizability and Alexithymia: Preliminary Findings; Targu Mures, Romania, 2014. Available online: https://real.mtak.hu/37714/1/mental.15.2014.004.pdf (accessed on 23 August 2025).
- Porges, S.W. Polyvagal Theory: A Science of Safety. Front. Integr. Neurosci. 2022, 16, 871227. [Google Scholar] [CrossRef]
- Kano, M.; Yoshizawa, M.; Kono, K.; Muratsubaki, T.; Morishita, J.; Van Oudenhove, L.; Yagihashi, M.; Mugikura, S.; Dupont, P.; Takase, K.; et al. Parasympathetic Activity Correlates with Subjective and Brain Responses to Rectal Distension in Healthy Subjects but Not in Non-Constipated Patients with Irritable Bowel Syndrome. Sci. Rep. 2019, 9, 7358. [Google Scholar] [CrossRef]
- Lane, R.D.; Solms, M.; Weihs, K.L.; Hishaw, A.; Smith, R. Affective Agnosia: A Core Affective Processing Deficit in the Alexithymia Spectrum. Biopsychosoc. Med. 2020, 14, 20. [Google Scholar] [CrossRef]
- Kano, M.; Endo, Y.; Fukudo, S. Association Between Alexithymia and Functional Gastrointestinal Disorders. Front. Psychol. 2018, 9, 599. [Google Scholar] [CrossRef]
- Lane, R.D. Alexithymia 3.0: Reimagining Alexithymia from a Medical Perspective. Biopsychosoc. Med. 2020, 14, 21. [Google Scholar] [CrossRef]
- Taylor, G.J.; Porcelli, P.; Bagby, R.M. Alexithymia: A Defense of the Original Conceptualization of the Construct and a Critique of the Attention-Appraisal Model. Clin. Neuropsychiatry 2024, 21, 329–357. [Google Scholar] [CrossRef]
- Benarroch, E. Autonomic Nervous System and Neuroimmune Interactions. Neurology 2019, 92, 377–385. [Google Scholar] [CrossRef] [PubMed]
- Norris, C.J.; Larsen, J.T.; Cacioppo, J.T. Neuroticism Is Associated with Larger and More Prolonged Electrodermal Responses to Emotionally Evocative Pictures. Psychophysiology 2007, 44, 823–826. [Google Scholar] [CrossRef]
- Dawson, M.E.; Schell, A.M.; Filion, D.L. The Electrodermal System. In Handbook of Psychophysiology, 4th ed.; Cambridge handbooks in psychology; Cambridge University Press: New York, NY, USA, 2017; pp. 217–243. ISBN 978-1-107-05852-1. [Google Scholar]
- Letzen, J.E.; Robinson, M.E. Negative Mood Influences Default Mode Network Functional Connectivity in Chronic Low Back Pain Patients: Implications for Functional Neuroimaging Biomarkers. Pain 2017, 158, 48–57. [Google Scholar] [CrossRef]
- Watson, D. Neuroticism/Negative Affectivity. In The Cambridge Handbook of Anxiety and Related Disorders; Cambridge University Press: New York, NY, USA, 2019; pp. 91–120. ISBN 978-1-107-19306-2. [Google Scholar]
- Boucsein, W. Electrodermal Activity; Plenum: New York, NY, USA, 1992. [Google Scholar]
- Blomqvist, N. On the Relation between Change and Initial Value. J. Am. Stat. Assoc. 1977, 72, 746–749. [Google Scholar] [CrossRef]
- Hilgard, E.R. Divided Consciousness: Multiple Controls in Human Thought and Action, 2nd ed.; Wiley-Interscience: New York, NY, USA, 1986. [Google Scholar]
- Wickramasekera, I. Invited Presentation—On the Interaction of Two Orthogonal Risk Factors: 1) Hypnotic Ability, 2) Negative Affectivity (Threat Perception-HPAA) for Psychophysiological Dysregulation (Sympathetic and Parasympathetic) in Somatization-Nocebo Phenomena. In Proceedings of the Suggestion and Suggestibility Theory in Research, Rome, Italy, 1994; Available online: https://www.meg-stiftung.de/index.php/de/component/phocadownload/category/1-artikel?download=239:16-wickramasekera-2000-4-hyint-245-252&Itemid=216 (accessed on 17 October 2021).
- Aldrich, L.B.; Moattari, A.R.; Vinik, A.I. Distinguishing Features of Idiopathic Flushing and Carcinoid Syndrome. Arch. Intern. Med. 1988, 148, 2614–2618. [Google Scholar] [CrossRef]
- Halperin, J.L.; Cohen, R.A.; Coffman, J.D. Digital Vasodilatation during Mental Stress in Patients with Raynaud’s Disease. Cardiovasc. Res. 1983, 17, 671–677. [Google Scholar] [CrossRef] [PubMed]
- Cooke, J.P.; Creager, M.A.; Osmundson, P.J.; Shepherd, J.T. Sex Differences in Control of Cutaneous Blood Flow. Circulation 1990, 82, 1607–1615. [Google Scholar] [CrossRef] [PubMed]
- Madison, A.A.; Andridge, R.; Shrout, M.R.; Renna, M.E.; Bennett, J.M.; Jaremka, L.M.; Fagundes, C.P.; Belury, M.A.; Malarkey, W.B.; Kiecolt-Glaser, J.K. Frequent Interpersonal Stress and Inflammatory Reactivity Predict Depressive-Symptom Increases: Two Tests of the Social-Signal-Transduction Theory of Depression. Psychol. Sci. 2022, 33, 152–164. [Google Scholar] [CrossRef] [PubMed]
- Wickramasekera, I.; Wickramasekera, I., II. A Case Study: Electromyographic Correlates in the Hypnotic Recall of a Repressed Memory. J. Trauma Dissociation 1997, 10, 11–20. [Google Scholar]
- McCarthy, R.E. An Investigation of Paradoxical Temperature Increase During Cognitve Stress in an Abused Population. Doctoral Dissertation, Saybrook Graduate School and Research Center, San Francisco, CA, USA, 2003. [Google Scholar]
- House, J.S.; Landis, K.R.; Umberson, D. Social Relationships and Health. Science 1988, 241, 540–545. [Google Scholar] [CrossRef]
- Smith, P.J.; Merwin, R.M. The Role of Exercise in Management of Mental Health Disorders: An Integrative Review. Annu. Rev. Med. 2021, 72, 45–62. [Google Scholar] [CrossRef]
- Holt-Lunstad, J.; Steptoe, A. Social Isolation: An Underappreciated Determinant of Physical Health. Curr. Opin. Psychol. 2021, 43, 232–237. [Google Scholar] [CrossRef]
- Smith, R.; Weihs, K.L.; Alkozei, A.; Killgore, W.D.S.; Lane, R.D. An Embodied Neurocomputational Framework for Organically Integrating Biopsychosocial Processes: An Application to the Role of Social Support in Health and Disease. Psychosom. Med. 2019, 81, 125–145. [Google Scholar] [CrossRef]
- De Pascalis, V.; Chiaradia, C.; Carotenuto, E. The Contribution of Suggestibility and Expectation to Placebo Analgesia Phenomenon in an Experimental Setting. Pain 2002, 96, 393–402. [Google Scholar] [CrossRef]
- De Pascalis, V.; Scacchia, P. Hypnotizability and Placebo Analgesia in Waking and Hypnosis as Modulators of Auditory Startle Responses in Healthy Women: An ERP Study. PLoS ONE 2016, 11, e0159135. [Google Scholar] [CrossRef][Green Version]
- Owens, J.E.; Menard, M. The Quantification of Placebo Effects Within a General Model of Health Care Outcomes. J. Altern. Complement. Med. 2011, 17, 817–821. [Google Scholar] [CrossRef] [PubMed]
- Huber, A.; Lui, F.; Porro, C.A. Hypnotic Susceptibility Modulates Brain Activity Related to Experimental Placebo Analgesia. Pain 2013, 154, 1509–1518. [Google Scholar] [CrossRef] [PubMed]
- Parsons, R.D.; Bergmann, S.; Wiech, K.; Terhune, D.B. Direct Verbal Suggestibility as a Predictor of Placebo Hypoalgesia Responsiveness. Psychosom. Med. 2021, 83, 1041–1049. [Google Scholar] [CrossRef] [PubMed]
- Corsi, N.; Colloca, L. Placebo and Nocebo Effects: The Advantage of Measuring Expectations and Psychological Factors. Front. Psychol. 2017, 8, 308. [Google Scholar] [CrossRef]
- Winter, D.; Braw, Y. Effects of Diagnosis Threat on Cognitive Complaints after COVID-19. Health Psychol. 2023, 42, 335–342. [Google Scholar] [CrossRef]
- Khan, A.Y.; Baade, L.; Ablah, E.; McNerney, V.; Golewale, M.H.; Liow, K. Can Hypnosis Differentiate Epileptic from Nonepileptic Events in the Video/EEG Monitoring Unit? Data from a Pilot Study. Epilepsy Behav. 2009, 15, 314–317. [Google Scholar] [CrossRef]
- Stein, M.V.; Heller, M.; Hughes, N.; Marr, D.; Brake, B.; Chapman, S.; James Rubin, G.; Terhune, D.B. Moderators of Nocebo Effects in Controlled Experiments: A Multi-Level Meta-Analysis. Neurosci. Biobehav. Rev. 2025, 172, 106042. [Google Scholar] [CrossRef]
- Lynn, S.J.; Laurence, J.-R.; Kirsch, I. Hypnosis, Suggestion, and Suggestibility: An Integrative Model. Am. J. Clin. Hypn. 2015, 57, 314–329. [Google Scholar] [CrossRef]
- Tellegen, A. Practicing the Two Disciplines for Relaxation and Enlightenment: Comment on “Role of the Feedback Signal in Electromyograph Biofeedback: The Relevance of Attention” by Qualls and Sheehan. J. Exp. Psychol. Gen. 1981, 110, 217–231. [Google Scholar] [CrossRef]
- Zinn, M.L.; McCain, C.; Zinn, M. Musical Performance Anxiety and the High-Risk Model of Threat Perception. Med. Probl. Perform. Artist. 2000, 15, 65–71. [Google Scholar] [CrossRef]
- Ferdek, M.A.; Adamczyk, A.K.; van Rijn, C.M.; Oosterman, J.M.; Wyczesany, M. Pain Catastrophizing Is Associated with Altered EEG Effective Connectivity during Pain-related Mental Imagery. Acta Neurobiol. Exp. 2019, 79, 53–72. [Google Scholar]
- Quartana, P.J.; Campbell, C.M.; Edwards, R.R. Pain Catastrophizing: A Critical Review. Expert. Rev. Neurother. 2009, 9, 745–758. [Google Scholar] [CrossRef]
- Darnall, B.D.; Colloca, L. Chapter Six—Optimizing Placebo and Minimizing Nocebo to Reduce Pain, Catastrophizing, and Opioid Use: A Review of the Science and an Evidence-Informed Clinical Toolkit. In International Review of Neurobiology; Colloca, L., Ed.; Neurobiology of the Placebo Effect Part II; Academic Press: Cambridge, MA, USA, 2018; Volume 139, pp. 129–157. [Google Scholar]
- Grosso, F.; Barbiani, D.; Cavalera, C.; Volpato, E.; Pagnini, F. Risk Factors Associated with Nocebo Effects: A Review of Reviews. Brain Behav. Immun. Health 2024, 38, 100800. [Google Scholar] [CrossRef]
- Sarter, L.; Heider, J.; Kirchner, L.; Schenkel, S.; Witthöft, M.; Rief, W.; Kleinstäuber, M. Cognitive and Emotional Variables Predicting Treatment Outcome of Cognitive Behavior Therapies for Patients with Medically Unexplained Symptoms: A Meta-Analysis. J. Psychosom. Res. 2021, 146, 110486. [Google Scholar] [CrossRef]
- Van Den Houte, M.; Bogaerts, K.; Van Diest, I.; De Bie, J.; Persoons, P.; Van Oudenhove, L.; Van den Bergh, O. Inducing Somatic Symptoms in Functional Syndrome Patients: Effects of Manipulating State Negative Affect. Psychosom. Med. 2017, 79, 1000–1007. [Google Scholar] [CrossRef] [PubMed]
- Bogaerts, K.; Van Den Houte, M.; Jongen, D.; Ly, H.G.; Coppens, E.; Schruers, K.; Van Diest, I.; Jan, T.; Van Wambeke, P.; Petre, B.; et al. Brain Mediators of Negative Affect-Induced Physical Symptom Reporting in Patients with Functional Somatic Syndromes. Transl. Psychiatry 2023, 13, 285. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Tyrrell, D.A.J.; Smith, A.P. Psychological Stress and Susceptibility to the Common Cold. N. Engl. J. Med. 1991, 325, 606–612. [Google Scholar] [CrossRef] [PubMed]
- Lane, R.D. Neural Substrates of Implicit and Explicit Emotional Processes: A Unifying Framework for Psychosomatic Medicine. Psychosom. Med. 2008, 70, 214–231. [Google Scholar] [CrossRef]
- McCrae, R.R.; Costa, P.T. Social Desirability Scales: More Substance than Style. J. Consult. Clin. Psychol. 1983, 51, 882–888. [Google Scholar] [CrossRef]
- Williams, M.M.; Rogers, R.; Sharf, A.J.; Ross, C.A. Faking Good: An Investigation of Social Desirability and Defensiveness in an Inpatient Sample With Personality Disorder Traits. J. Pers. Assess. 2019, 101, 253–263. [Google Scholar] [CrossRef]
- Weinberger, D.A. The Construct Validity of the Repressive Coping Style. In Repression and Dissociation: Implications for Personality Theory, Psychopathology, and Health; The John D. and Catherine T. MacArthur Foundation series on mental health and development; The University of Chicago Press: Chicago, IL, USA, 1995; pp. 337–386. ISBN 978-0-226-76105-3. [Google Scholar]
- Slavich, G.M.; Irwin, M.R. From Stress to Inflammation and Major Depressive Disorder: A Social Signal Transduction Theory of Depression. Psychol. Bull. 2014, 140, 774–815. [Google Scholar] [CrossRef]
- Cohen, S.; Murphy, M.L.M.; Prather, A.A. Ten Surprising Facts About Stressful Life Events and Disease Risk. Annu. Rev. Psychol. 2019, 70, 577–597. [Google Scholar] [CrossRef] [PubMed]
- Muscatell, K.A.; Dedovic, K.; Slavich, G.M.; Jarcho, M.R.; Breen, E.C.; Bower, J.E.; Irwin, M.R.; Eisenberger, N.I. Greater Amygdala Activity and Dorsomedial Prefrontal-Amygdala Coupling Are Associated with Enhanced Inflammatory Responses to Stress. Brain Behav. Immun. 2015, 43, 46–53. [Google Scholar] [CrossRef] [PubMed]
- Nilaweera, D.; Gurvich, C.; Freak-Poli, R.; Woods, R.L.; Owen, A.; McNeil, J.; Nelson, M.; Stocks, N.; Ryan, J. The Association between Adverse Events in Later Life and Mortality in Older Individuals. Compr. Psychoneuroendocrinol. 2023, 16, 100210. [Google Scholar] [CrossRef] [PubMed]
- Jeong, Y.-J.; Aldwin, C.M.; Igarashi, H.; Spiro, A. Do Hassles and Uplifts Trajectories Predict Mortality? Longitudinal Findings from the VA Normative Aging Study. J. Behav. Med. 2016, 39, 408–419. [Google Scholar] [CrossRef]
- Felitti, V.J.; Anda, R.F.; Nordenberg, D.; Williamson, D.F.; Spitz, A.M.; Edwards, V.; Koss, M.P.; Marks, J.S. Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults. The Adverse Childhood Experiences (ACE) Study. Am. J. Prev. Med. 1998, 14, 245–258. [Google Scholar] [CrossRef]
- Bourassa, K.J.; Moffitt, T.E.; Harrington, H.; Houts, R.; Poulton, R.; Ramrakha, S.; Caspi, A. Lower Cardiovascular Reactivity Is Associated With More Childhood Adversity and Poorer Midlife Health: Replicated Findings From the Dunedin and MIDUS Cohorts. Clin. Psychol. Sci. 2021, 9, 961–978. [Google Scholar] [CrossRef]
- Brennan, G.M.; Moffitt, T.E.; Bourassa, K.; Harrington, H.; Hogan, S.; Houts, R.M.; Poulton, R.; Ramrakha, S.; Caspi, A. The Continuity of Adversity: Negative Emotionality Links Early Life Adversity With Adult Stressful Life Events. Clin. Psychol. Sci. 2024, 12, 1111–1126. [Google Scholar] [CrossRef]
- Smith, R.; Kirlic, N.; Stewart, J.L.; Touthang, J.; Kuplicki, R.; McDermott, T.J.; Taylor, S.; Khalsa, S.S.; Paulus, M.P.; Aupperle, R.L. Long-Term Stability of Computational Parameters during Approach-Avoidance Conflict in a Transdiagnostic Psychiatric Patient Sample. Sci. Rep. 2021, 11, 11783. [Google Scholar] [CrossRef]
- Roth, S.; Cohen, L.J. Approach, Avoidance, and Coping with Stress. Am. Psychol. 1986, 41, 813–819. [Google Scholar] [CrossRef]
- Livermore, J.J.A.; Klaassen, F.H.; Bramson, B.; Hulsman, A.M.; Meijer, S.W.; Held, L.; Klumpers, F.; de Voogd, L.D.; Roelofs, K. Approach-Avoidance Decisions Under Threat: The Role of Autonomic Psychophysiological States. Front. Neurosci. 2021, 15, 353. [Google Scholar] [CrossRef] [PubMed]
- Moos, R.H. Coping Responses Inventory: CRI from Adults. Professional Manual; Psychological Assessment Resources: Odessa, TX, USA, 1993. [Google Scholar]
- Krypotos, A.-M.; Effting, M.; Kindt, M.; Beckers, T. Avoidance Learning: A Review of Theoretical Models and Recent Developments. Front. Behav. Neurosci. 2015, 9, 189. [Google Scholar] [CrossRef] [PubMed]
- Fordyce, W. Behavioral Methods for Chronic Pain and Illness; C.V. Mosby, Company: St. Louis, MO, USA, 1976. [Google Scholar]
- Meyer, H.C.; Odriozola, P.; Cohodes, E.M.; Mandell, J.D.; Li, A.; Yang, R.; Hall, B.S.; Haberman, J.T.; Zacharek, S.J.; Liston, C.; et al. Ventral Hippocampus Interacts with Prelimbic Cortex during Inhibition of Threat Response via Learned Safety in Both Mice and Humans. Proc. Natl. Acad. Sci. USA 2019, 116, 26970–26979. [Google Scholar] [CrossRef]
- Watson, D.; Naragon, K. Positive Affectivity: The Disposition to Experience Positive Emotional States. In Oxford Handbook of Positive Psychology, 2nd ed.; Oxford library of psychology; Oxford University Press: New York, NY, USA, 2009; pp. 207–215. ISBN 978-0-19-518724-3. [Google Scholar]
- Geers, A.L.; Close, S.; Caplandies, F.C.; Vogel, C.L.; Murray, A.B.; Pertiwi, Y.; Handley, I.M.; Vase, L. Testing a Positive-Affect Induction to Reduce Verbally Induced Nocebo Hyperalgesia in an Experimental Pain Paradigm. Pain 2019, 160, 2290–2297. [Google Scholar] [CrossRef]
- Geers, A.L.; Faasse, K.; Guevarra, D.A.; Clemens, K.S.; Helfer, S.G.; Colagiuri, B. Affect and Emotions in Placebo and Nocebo Effects: What Do We Know so Far? Social. Personal. Psychol. Compass 2021, 15, e12575. [Google Scholar] [CrossRef]
- Bagby, R.M.; Parker, J.D.; Taylor, G.J. The Twenty-Item Toronto Alexithymia Scale--I. Item Selection and Cross-Validation of the Factor Structure. J. Psychosom. Res. 1994, 38, 23–32. [Google Scholar] [CrossRef]
- Montgomery, G.H.; David, D.; Winkel, G.; Silverstein, J.H.; Bovbjerg, D.H. The Effectiveness of Adjunctive Hypnosis with Surgical Patients: A Meta-Analysis. Anesth. Analg. 2002, 94, 1639–1645. [Google Scholar] [CrossRef]
- Council, J.R.; Kirsch, I.; Hafner, L.P. Expectancy versus Absorption in the Prediction of Hypnotic Responding. J. Personal. Social. Psychol. 1986, 50, 182–189. [Google Scholar] [CrossRef]
- Berntson, G.G.; Thomas Bigger, J., Jr.; Eckberg, D.L.; Grossman, P.; Kaufmann, P.G.; Malik, M.; Nagaraja, H.N.; Porges, S.W.; Saul, J.P.; Stone, P.H.; et al. Heart Rate Variability: Origins, Methods, and Interpretive Caveats. Psychophysiology 1997, 34, 623–648. [Google Scholar] [CrossRef]
- European Society of Cardiology and the North American Society of Pacing and Electrophysiology Heart Rate Variability: Standards of Measurement, Physiological Interpretation and Clinical Use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Circulation 1996, 93, 1043–1065. [Google Scholar]
- Barber, T.X. Hypnosis: A Scientific Approach; Van Nostrand Reinhold: New York, NY, USA, 1969. [Google Scholar]
- Hilgard, E.R. Hypnotic Susceptibility; Hypnotic susceptibility; Harcourt, Brace & World: Oxford, UK, 1965. [Google Scholar]
- Kihlstrom, J.F. The Cognitive Unconscious. Science 1987, 237, 1445–1452. [Google Scholar] [CrossRef] [PubMed]
- Velten, E. A Laboratory Task for Induction of Mood States. Behav. Res. Ther. 1968, 6, 473–482. [Google Scholar] [CrossRef]
- Klein, K.B.; Spiegel, D. Modulation of Gastric Acid Secretion by Hypnosis. Gastroenterology 1989, 96, 1383–1387. [Google Scholar] [CrossRef]
- De Benedittis, G. Hypnotic Modulation of Autonomic Nervous System (ANS) Activity. Brain Sci. 2024, 14, 249. [Google Scholar] [CrossRef]
- Terhune, D.B.; Hedman, L.R.A. Metacognition of Agency Is Reduced in High Hypnotic Suggestibility. Cognition 2017, 168, 176–181. [Google Scholar] [CrossRef]
- Das, J.P. Conditioning and Hypnosis. J. Exp. Psychol. 1958, 56, 110–113. [Google Scholar] [CrossRef]
- King, D.R.; McDonald, R.D. Hypnotic Susceptibility and Verbal Conditioning. Int. J. Clin. Exp. Hypn. 1976, 24, 29–37. [Google Scholar] [CrossRef]
- Laurence, J. Hypnotisability and Automaticity from a Synergistic Perspective? Montreal, QC, Canada, 2018. [Google Scholar]
- Raz, A.; Shapiro, T.; Fan, J.; Posner, M.I. Hypnotic Suggestion and the Modulation of Stroop Interference. Arch. Gen. Psychiatry 2002, 59, 1155–1161. [Google Scholar] [CrossRef]
- Lifshitz, M.; Cusumano, E.; Raz, A. Hypnosis as Neurophenomenology. Front. Human. Neurosci. 2013, 7, 469. [Google Scholar] [CrossRef]
- Wickramasekera, I. (Ed.) Biofeedback, Behavior Therapy and Hypnosis: Potentiating the Verbal Control of Behavior for Clinicians; Nelson-Hall: Oxford, UK, 1976; pp. xv, 591. [Google Scholar]
- Spanos, N.P.; Perlini, A.H.; Robertson, L.A. Hypnosis, Suggestion, and Placebo in the Reduction of Experimental Pain. J. Abnorm. Psychol. 1989, 98, 285–293. [Google Scholar] [CrossRef] [PubMed]
- Benham, G.; Woody, E.Z.; Wilson, K.S.; Nash, M.R. Expect the Unexpected: Ability, Attitude, and Responsiveness to Hypnosis. J. Personal. Social. Psychol. 2006, 91, 342–350. [Google Scholar] [CrossRef] [PubMed]
- Jensen, M.P.; Karoly, P. Motivation and Expectancy Factors in Symptom Perception: A Laboratory Study of the Placebo Effect. Psychosom Med. 1991, 53, 144–152. [Google Scholar] [CrossRef] [PubMed]
- Horton, J.E.; Crawford, H.J. Neruophysiological and Genetic Determinants of High Hypnotizability. In The Highly Hypnotizable Person: Theoretical, Experimental and Clinical Issues; Heap, M., Brown, R.J., Oakley, D.A., Eds.; Routledge: London, UK, 2004; pp. 133–151. ISBN 978-0-203-48782-2. [Google Scholar]
- McGeown, W.J.; Mazzoni, G.; Venneri, A.; Kirsch, I. Hypnotic Induction Decreases Anterior Default Mode Activity. Conscious. Cogn. 2009, 18, 848–855. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, A.; Hilgard, E.R. Failure of the Opiate Antagonist Naloxone to Modify Hypnotic Analgesia. Proc. Natl. Acad. Sci. USA 1975, 72, 2041–2043. [Google Scholar] [CrossRef]
- Stoyva, J.M. Posthypnotically Suggested Dreams and the Sleep Cycle. Arch. General. Psychiatry 1965, 12, 287–294. [Google Scholar] [CrossRef]
- Cordi, M.J.; Rossier, L.; Rasch, B. Hypnotic Suggestions given before Nighttime Sleep Extend Slow-Wave Sleep as Compared to a Control Text in Highly Hypnotizable Subjects. Int. J. Clin. Exp. Hypn. 2020, 68, 105–129. [Google Scholar] [CrossRef]
- Hilgard, E.R.; Tart, C.T. Responsiveness to Suggestions Following Waking and Imagination Instructions and Following Induction of Hypnosis. J. Abnorm. Psychol. 1966, 71, 196–208. [Google Scholar] [CrossRef]
- Kirsch, I.; Braffman, W. Imaginative Suggestibility and Hypnotizability. Curr. Dir. Psychol. Sci. 2001, 10, 57–61. [Google Scholar] [CrossRef]
- Piccione, C.; Hilgard, E.R.; Zimbardo, P.G. On the Degree of Stability of Measured Hypnotizability over a 25-Year Period. J. Pers. Soc. Psychol. 1989, 56, 289–295. [Google Scholar] [CrossRef]
- Morgan, A.H. The Heritability of Hypnotic Susceptibility in Twins. J. Abnorm. Psychol. 1973, 82, 55–61. [Google Scholar] [CrossRef]
- Morgan, A.H.; Hilgard, E.R.; Davert, E.C. The Heritability of Hypnotic Susceptibility of Twins: A Preliminary Report. Behav. Genet. 1970, 1, 213–224. [Google Scholar] [CrossRef]
- Rominger, C.; Weiss, E.M.; Nagl, S.; Niederstätter, H.; Parson, W.; Papousek, I. Carriers of the COMT Met/Met Allele Have Higher Degrees of Hypnotizability, Provided That They Have Good Attentional Control: A Case of Gene-Trait Interaction. Int. J. Clin. Exp. Hypn. 2014, 62, 455–482. [Google Scholar] [CrossRef]
- Nordenstrom, B.K.; Council James, R.; and Meier, B.P. The “Big Five” and Hypnotic Suggestibility. Int. J. Clin. Exp. Hypn. 2002, 50, 276–281. [Google Scholar] [CrossRef]
- Bates, B.L. Individual Differences in Response to Hypnosis. In Handbook of Clinical Hypnosis; American Psychological Association: Washington, DC, USA, 1993; pp. 23–54. ISBN 978-1-55798-440-1. [Google Scholar]
- Frankel, F.H.; Orne, M.T. Hypnotizability and Phobic Behavior. Arch. Gen. Psychiatry 1976, 33, 1259–1261. [Google Scholar] [CrossRef]
- Pettinati, H.M.; Kogan, L.G.; Evans, F.J.; Wade, J.H.; Horne, R.L.; Staats, J.M. Hypnotizability of Psychiatric Inpatients According to Two Different Scales. Am. J. Psychiatry 1990, 147, 69–75. [Google Scholar] [CrossRef] [PubMed]
- Rosendahl, J.; Alldredge, C.T.; Haddenhorst, A. Meta-Analytic Evidence on the Efficacy of Hypnosis for Mental and Somatic Health Issues: A 20-Year Perspective. Front. Psychol. 2024, 14, 1330238. [Google Scholar] [CrossRef] [PubMed]
- Landry, M.; Castanheira, J.d.S.; Boisvert, C.; Rousseaux, F.; Sackur, J.; Raz, A.; Richebé, P.; Ogez, D.; Rainville, P.; Jerbi, K. Aperiodic Activity as a Central Neural Feature of Hypnotic Susceptibility Outside of Hypnosis. bioRxiv 2024. bioRxiv:2023.11.16.567097. [Google Scholar]
- De Pascalis, V. Brain Functional Correlates of Resting Hypnosis and Hypnotizability: A Review. Brain Sci. 2024, 14, 115. [Google Scholar] [CrossRef]
- Graffin, N.F.; Ray, W.J.; Lundy, R. EEG Concomitants of Hypnosis and Hypnotic Susceptibility. J. Abnorm. Psychol. 1995, 104, 123–131. [Google Scholar] [CrossRef]
- Sabourin, M.E.; Cutcomb, S.D.; Crawford, H.J.; Pribram, K. EEG Correlates of Hypnotic Susceptibility and Hypnotic Trance: Spectral Analysis and Coherence. Int. J. Psychophysiol. 1990, 10, 125–142. [Google Scholar] [CrossRef]
- Cortade, D.L.; Markovits, J.; Spiegel, D.; Wang, S.X. Point-of-Care Testing of Enzyme Polymorphisms for Predicting Hypnotizability and Postoperative Pain. J. Mol. Diagn. 2023, 25, 197–210. [Google Scholar] [CrossRef] [PubMed]
- Slade, G.D.; Sanders, A.E.; Ohrbach, R.; Bair, E.; Maixner, W.; Greenspan, J.D.; Fillingim, R.B.; Smith, S.; Diatchenko, L. COMT Diplotype Amplifies Effect of Stress on Risk of Temporomandibular Pain. J. Dent. Res. 2015, 94, 1187–1195. [Google Scholar] [CrossRef]
- Connors, M.H.; Quinto, L.; Deeley, Q.; Halligan, P.W.; Oakley, D.A.; Kanaan, R.A. Hypnosis and Suggestion as Interventions for Functional Neurological Disorder: A Systematic Review. Gen. Hosp. Psychiatry 2024, 86, 92–102. [Google Scholar] [CrossRef] [PubMed]
- Wagaman, M.J. Physiological and Psychological Effects of Various Hypnotic Suggestions with Asthma Patients. Ph.D. Dissertation, The Union Institute, Cincinnati, OH, USA, 2000. [Google Scholar]
- MacLeod, C.M. Hypnosis and the Control of Attention: Where to from Here? Conscious. Cogn. An. Int. J. 2011, 20, 321–324. [Google Scholar] [CrossRef] [PubMed]
- Raz, A.; Fan, J.; Posner, M.I. Hypnotic Suggestion Reduces Conflict in the Human Brain. Proc. Natl. Acad. Sci. USA 2005, 102, 9978–9983. [Google Scholar] [CrossRef]
- Raz, A.; Kirsch, I.; Pollard, J.; Nitkin-Kaner, Y. Suggestion Reduces the Stroop Effect. Psychol. Sci. 2006, 17, 91–95. [Google Scholar] [CrossRef]
- Dixon, M.; Brunet, A.; Laurence, J.-R. Hypnotizability and Automaticity: Toward a Parallel Distributed Processing Model of Hypnotic Responding. J. Abnorm. Psychol. 1990, 99, 336–343. [Google Scholar] [CrossRef]
- Shiffrin, R.M.; Schneider, W. Controlled and Automatic Human Information Processing: II. Perceptual Learning, Automatic Attending and a General Theory. Psychol. Rev. 1977, 84, 127–190. [Google Scholar] [CrossRef]
- Weitzenhoffer, A.M. When Is an “Instruction” an “Instruction”? Int. J. Clin. Exp. Hypn. 1974, 22, 258–269. [Google Scholar] [CrossRef]
- Bowers, K.S. Do the Stanford Scales Tap the “Classic Suggestion Effect”? Int. J. Clin. Exp. Hypn. 1981, 29, 42–53. [Google Scholar] [CrossRef]
- Balthazard, C.; Woody, E. The Spectral Analysis of Hypnotic Performance with Respect to Absorption. Int. J. Exp. Clin. Hypn. 1992, 40, 21–43. [Google Scholar] [CrossRef]
- Kirsch, I.; Council, J.R. Situational and Personality Correlates of Hypnotic Responsiveness. In Contemporary Hypnosis Research; The Guilford Press: New York, NY, USA, 1992; pp. 267–291. ISBN 978-0-89862-893-7. [Google Scholar]
- Wickramasekera, I. The Placebo Effect and Its Use in Biofeedback Therapy. In Handbook of Mind-Body Medicine for Primary Care; Moss, D., McGrady, A., Davies, T., Wickramasekera, I., Eds.; Sage: Thousand Oaks, CA, USA, 2003; pp. 69–82. [Google Scholar]
- Voudouris, N.J.; Peck, C.L.; Coleman, G. Conditioned Placebo Responses. J. Pers. Soc. Psychol. 1985, 48, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Gruzelier, J. New and Rediscovered Insights about the Nature of Hynotizability: Exceptional Ability and Vulnerability. Contemp. Hypn. Integr. Ther. 2011, 28, 116–135. [Google Scholar]
- Lifshitz, M.; Aubert Bonn, N.; Fischer, A.; Kashem, I.F.; Raz, A. Using Suggestion to Modulate Automatic Processes: From Stroop to McGurk and Beyond. Cortex 2013, 49, 463–473. [Google Scholar] [CrossRef] [PubMed]
- Barnier, A.J.; McConkey, K.M. Absorption, Hypnotizability and Context: Non-Hypnotic Contexts Are Not All the Same. Contemp. Hypn. 1999, 16, 1–8. [Google Scholar] [CrossRef]
- Tellegen, A.; Lykken, D.T.; Bouchard, T.J.; Wilcox, K.J.; Segal, N.L.; Rich, S. Personality Similarity in Twins Reared Apart and Together. J. Pers. Soc. Psychol. 1988, 54, 1031–1039. [Google Scholar] [CrossRef]
- Bräscher, A.-K.; Sütterlin, S.; Scheuren, R.; Van den Bergh, O.; Witthöft, M. Somatic Symptom Perception From a Predictive Processing Perspective: An Empirical Test Using the Thermal Grill Illusion. Psychosom. Med. 2020, 82, 708–714. [Google Scholar] [CrossRef]
- Qualls, P.J.; Sheehan, P.W. Imagery Encouragement, Absorption Capacity, and Relaxation during Electromyograph Biofeedback. J. Personal. Soc. Psychol. 1981, 41, 370–379. [Google Scholar] [CrossRef]
- Zillmer, E.; Wickramasekera, I. Biofeedback and Hypnotizability: Initial Treatment Considerations. Clin. Biofeedback Health 1987, 10, 51057. [Google Scholar]
- Morrow, G.R.; Morrell, C. Behavioral Treatment for the Anticipatory Nausea and Vomiting Induced by Cancer Chemotherapy. N. Engl. J. Med. 1982, 307, 1476–1480. [Google Scholar] [CrossRef]
- Vaitl, D.; Ott, U. Altered States of Consciousness Induced by Psychophysiological Techniques. Mind Matter 2005, 3, 9–30. [Google Scholar]
- Jamieson, G.A. The Modified Tellegen Absorption Scale: A Clearer Window on the Structure and Meaning of Absorption. Aust. J. Clin. Exp. Hypn. 2005, 33, 119–139. [Google Scholar]
- Lifshitz, M.; Sacchet, M.D.; Huntenburg, J.M.; Thiery, T.; Fan, Y.; Gärtner, M.; Grimm, S.; Winnebeck, E.; Fissler, M.; Schroeter, T.A.; et al. Mindfulness-Based Therapy Regulates Brain Connectivity in Major Depression. PPS 2019, 88, 375–377. [Google Scholar] [CrossRef] [PubMed]
- Sifneos, P.E. The Prevalence of “alexithymic” Characteristics in Psychosomatic Patients. Psychother. Psychosom. 1973, 22, 255–262. [Google Scholar] [CrossRef]
- Spiegel, H.; Spiegel, D. Trance and Treatment: Clinical Uses of Hypnosis; American Psychiatric Publishing: Washington, DC, USA, 2008; ISBN 978-1-58562-727-1. [Google Scholar]
- Heap, M.; Brown, R.J.; Oakley, D.A. (Eds.) The Highly Hypnotizable Person: Theoretical, Experimental and Clinical Issues; Routledge: London, UK, 2004; ISBN 978-0-203-48782-2. [Google Scholar]
- Jørgensen, M.M.; Zachariae, R.; Skytthe, A.; Kyvik, K. Genetic and Environmental Factors in Alexithymia: A Population-Based Study of 8785 Danish Twin Pairs. Psychother. Psychosom. 2007, 76, 369–375. [Google Scholar] [CrossRef] [PubMed]
- van der Velde, J.; Servaas, M.N.; Goerlich, K.S.; Bruggeman, R.; Horton, P.; Costafreda, S.G.; Aleman, A. Neural Correlates of Alexithymia: A Meta-Analysis of Emotion Processing Studies. Neurosci. Biobehav. Rev. 2013, 37, 1774–1785. [Google Scholar] [CrossRef] [PubMed]
- Kano, M.; Muratsubaki, T.; Yagihashi, M.; Morishita, J.; Mugikura, S.; Dupont, P.; Takase, K.; Kanazawa, M.; Van Oudenhove, L.; Fukudo, S. Insula Activity to Visceral Stimulation and Endocrine Stress Responses as Associated with Alexithymia in Patients With Irritable Bowel Syndrome. Psychosom. Med. 2020, 82, 29. [Google Scholar] [CrossRef]
- Kano, M.; Fukudo, S. The Alexithymic Brain: The Neural Pathways Linking Alexithymia to Physical Disorders. Biopsychosoc. Med. 2013, 7, 1. [Google Scholar] [CrossRef]
- Preti, A.; Sancassiani, F.; Cadoni, F.; Carta, M.G. Alexithymia Affects Pre-Hospital Delay of Patients with Acute Myocardial Infarction: Meta-Analysis of Existing Studies. Clin. Pract. Epidemiol. Ment. Health 2013, 9, 69–73. [Google Scholar] [CrossRef]
- Terhune, D.B.; Oakley, D.A. Hypnosis and Imagination. In The Cambridge Handbook of the Imagination; Cambridge University Press: New York, NY, USA, 2020; pp. 711–727. ISBN 978-1-108-45342-4. [Google Scholar]
- Kano, M.; Oudenhove, L.V.; Dupont, P.; Wager, T.D.; Fukudo, S. Imaging Brain Mechanisms of Functional Somatic Syndromes: Potential as a Biomarker? Tohoku J. Exp. Med. 2020, 250, 137–152. [Google Scholar] [CrossRef]
- LeDoux, J. The Emotional Brain, Fear, and the Amygdala. Cell Mol. Neurobiol. 2003, 23, 727–738. [Google Scholar] [CrossRef] [PubMed]
- Montgomery, G.H.; Kirsch, I. Classical Conditioning and the Placebo Effect. Pain 1997, 72, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Jensen, K.B.; Kaptchuk, T.J.; Kirsch, I.; Raicek, J.; Lindstrom, K.M.; Berna, C.; Gollub, R.L.; Ingvar, M.; Kong, J. Nonconscious Activation of Placebo and Nocebo Pain Responses. Proc. Natl. Acad. Sci. USA 2012, 109, 15959–15964. [Google Scholar] [CrossRef] [PubMed]
- Jensen, M.P.; Adachi, T.; Hakimian, S. Brain Oscillations, Hypnosis, and Hypnotizability. Am. J. Clin. Hypn. 2015, 57, 230–253. [Google Scholar] [CrossRef]
- Jensen, K.B.; Kaptchuk, T.J.; Chen, X.; Kirsch, I.; Ingvar, M.; Gollub, R.L.; Kong, J. A Neural Mechanism for Nonconscious Activation of Conditioned Placebo and Nocebo Responses. Cereb. Cortex 2015, 25, 3903–3910. [Google Scholar] [CrossRef]
- Bąbel, P. Classical Conditioning as a Distinct Mechanism of Placebo Effects. Front. Psychiatry 2019, 10, 449. [Google Scholar] [CrossRef]
- Colloca, L.; Barsky, A.J. Placebo and Nocebo Effects. N. Engl. J. Med. 2020, 382, 554–561. [Google Scholar] [CrossRef]
- Colloca, L. The Nocebo Effect. Annu. Rev. Pharmacol. Toxicol. 2023, 64, 171–190. [Google Scholar] [CrossRef]
- Martins, J.; Czamara, D.; Sauer, S.; Rex-Haffner, M.; Dittrich, K.; Dörr, P.; de Punder, K.; Overfeld, J.; Knop, A.; Dammering, F.; et al. Childhood Adversity Correlates with Stable Changes in DNA Methylation Trajectories in Children and Converges with Epigenetic Signatures of Prenatal Stress. Neurobiol. Stress 2021, 15, 100336. [Google Scholar] [CrossRef]
- Raffington, L. Utilizing Epigenetics to Study the Shared Nature of Development and Biological Aging across the Lifespan. Npj Sci. Learn. 2024, 9, 24. [Google Scholar] [CrossRef]
- Schmidt, L.J.; Belopolsky, A.V.; Theeuwes, J. The Time Course of Attentional Bias to Cues of Threat and Safety. Cogn. Emot. 2017, 31, 845–857. [Google Scholar] [CrossRef]
- Barbiani, D.; Camerone, E.M.; Grosso, F.; Geers, A.L.; Pagnini, F. The Role of Attention in Placebo and Nocebo Effects. Ann. Behav. Med. 2024, 58, 635–644. [Google Scholar] [CrossRef] [PubMed]
- Hur, J.; Miller, G.A.; McDavitt, J.R.B.; Spielberg, J.M.; Crocker, L.D.; Infantolino, Z.P.; Towers, D.N.; Warren, S.L.; Heller, W. Interactive Effects of Trait and State Affect on Top-down Control of Attention. Soc. Cogn. Affect. Neurosci. 2015, 10, 1128–1136. [Google Scholar] [CrossRef] [PubMed]
- Porges, S.W. Vagal Tone: A Physiologic Marker of Stress Vulnerability. Pediatrics 1992, 90, 498–504. [Google Scholar] [CrossRef]
- Porges, S.W. The Polyvagal Perspective. Biol. Psychol. 2007, 74, 116–143. [Google Scholar] [CrossRef] [PubMed]
- Porges, S.W. The Polyvagal Theory: New Insights into Adaptive Reactions of the Autonomic Nervous System. Cleve Clin. J. Med. 2009, 76, S86–S90. [Google Scholar] [CrossRef]
- Zajonc, R.B. On the Primacy of Affect. Am. Psychol. 1984, 39, 117–123. [Google Scholar] [CrossRef]
- Cromwell, H.C.; Panksepp, J. Rethinking the Cognitive Revolution from a Neural Perspective: How Overuse/Misuse of the Term ‘Cognition’ and the Neglect of Affective Controls in Behavioral Neuroscience Could Be Delaying Progress in Understanding the BrainMind. Neurosci. Biobehav. Rev. 2011, 35, 2026–2035. [Google Scholar] [CrossRef]
- Folkman, S. Personal Control and Stress and Coping Processes: A Theoretical Analysis. J. Pers. Soc. Psychol. 1984, 46, 839–852. [Google Scholar] [CrossRef]
- Neuhuber, W.L.; Berthoud, H.-R. Functional Anatomy of the Vagus System: How Does the Polyvagal Theory Comply? Biol. Psychol. 2022, 174, 108425. [Google Scholar] [CrossRef]
- Grossman, P. Fundamental Challenges and Likely Refutations of the Five Basic Premises of the Polyvagal Theory. Biol. Psychol. 2023, 180, 108589. [Google Scholar] [CrossRef]
- Harris, R.M.; Porges, S.W.; Carpenter, M.E.; Vincenz, L.M. Hypnotic Susceptibility, Mood State, and Cardiovascular Reactivity. Am. J. Clin. Hypn. 1993, 36, 15–25. [Google Scholar] [CrossRef]
- Diamond, S.G.; Davis, O.C.; Howe, R.D. Heart-Rate Variability as a Quantitative Measure of Hypnotic Depth. Int. J. Clin. Exp. Hypn. 2008, 56, 1–18. [Google Scholar] [CrossRef]
- Stern, D.B.; Spiegel, H.; Nee, J.C. The Hypnotic Induction Profile: Normative Observations, Reliability and Validity. Am. J. Clin. Hypn. 1978, 21, 109–133. [Google Scholar] [CrossRef]
- Mather, M.; Thayer, J. How Heart Rate Variability Affects Emotion Regulation Brain Networks. Curr. Opin. Behav. Sci. 2018, 19, 98–104. [Google Scholar] [CrossRef] [PubMed]
- Goessl, V.C.; Curtiss, J.E.; Hofmann, S.G. The Effect of Heart Rate Variability Biofeedback Training on Stress and Anxiety: A Meta-Analysis. Psychol. Med. 2017, 47, 2578–2586. [Google Scholar] [CrossRef] [PubMed]
- Kolacz, J.; Porges, S.W. Chronic Diffuse Pain and Functional Gastrointestinal Disorders After Traumatic Stress: Pathophysiology Through a Polyvagal Perspective. Front. Med. 2018, 5, 145. [Google Scholar] [CrossRef] [PubMed]
- Wickramasekera II, I.E.; Szlyk, J.P. Could Empathy Be a Predictor of Hypnotic Ability? Int. J. Clin. Exp. Hypn. 2003, 51, 390–399. [Google Scholar] [CrossRef]
- Sargent, K.S.; Martinez, E.L.; Reed, A.C.; Guha, A.; Bartholomew, M.E.; Diehl, C.K.; Chang, C.S.; Salama, S.; Popov, T.; Thayer, J.F.; et al. Oscillatory Coupling Between Neural and Cardiac Rhythms. Psychol. Sci. 2024, 35, 517–528. [Google Scholar] [CrossRef]
- Friedman, B.H.; Thayer, J.F. Autonomic Balance Revisited: Panic Anxiety and Heart Rate Variability. J. Psychosom. Res. 1998, 44, 133–151. [Google Scholar] [CrossRef]
- Thayer, J.F.; Lane, R.D. A Model of Neurovisceral Integration in Emotion Regulation and Dysregulation. J. Affect. Disord. 2000, 61, 201–216. [Google Scholar] [CrossRef]
- Aronoff, G.M. Editorial. Clin. J. Pain 1985, 1, 1–3. Available online: https://journals.lww.com/clinicalpain/citation/1985/01010/editorial.1.aspx (accessed on 23 August 2025). [CrossRef]
- Henningsen, P.; Zipfel, S.; Sattel, H.; Creed, F. Management of Functional Somatic Syndromes and Bodily Distress. Psychother. Psychosom. 2018, 87, 12–31. [Google Scholar] [CrossRef] [PubMed]
- Schneider, A.; Donnachie, E.; Zipfel, S.; Enck, P. Patients With Somatoform Disorders Are Prone to Expensive and Potentially Harmful Medical Procedures—Results of a Retrospective Cohort Study Over 15 Years. Dtsch. Arztebl. Int. 2021, 118, 425–431. [Google Scholar] [CrossRef] [PubMed]
- Jonas, W.B.; Crawford, C.; Colloca, L.; Kriston, L.; Linde, K.; Moseley, B.; Meissner, K. Are Invasive Procedures Effective for Chronic Pain? A Systematic Review. Pain Med. 2019, 20, 1281–1293. [Google Scholar] [CrossRef] [PubMed]
- Ashar, Y.K.; Gordon, A.; Schubiner, H.; Uipi, C.; Knight, K.; Anderson, Z.; Carlisle, J.; Polisky, L.; Geuter, S.; Flood, T.F.; et al. Effect of Pain Reprocessing Therapy vs Placebo and Usual Care for Patients With Chronic Back Pain: A Randomized Clinical Trial. JAMA Psychiatry 2022, 79, 13–23. [Google Scholar] [CrossRef]
- Sullivan, M.D.; Ballantyne, J.C. Randomised Trial Reveals Opioids Relieve Acute Back Pain No Better than Placebo. Lancet 2023, 402, 267–269. [Google Scholar] [CrossRef]
- Kohn, L.T.; Corrigan, J.M.; Donaldson, M.S. To Err Is Human: Building a Safer Health System; Institute of Medicine (US) Committee on Quality of Health Care in America, Ed.; National Academies Press (US): Washington, DC, USA, 2000; ISBN 978-0-309-06837-6. [Google Scholar]
- Landrigan, C.P.; Parry, G.J.; Bones, C.B.; Hackbarth, A.D.; Goldmann, D.A.; Sharek, P.J. Temporal Trends in Rates of Patient Harm Resulting from Medical Care. N. Engl. J. Med. 2010, 363, 2124–2134. [Google Scholar] [CrossRef]
- Makary, M.A.; Daniel, M. Medical Error—The Third Leading Cause of Death in the US. BMJ 2016, 353, i2139. [Google Scholar] [CrossRef]
- Rodziewicz, T.L.; Houseman, B.; Vaqar, S.; Hipskind, J.E. Medical Error Reduction and Prevention. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- McEwen, B.S.; Bowles, N.P.; Gray, J.D.; Hill, M.N.; Hunter, R.G.; Karatsoreos, I.N.; Nasca, C. Mechanisms of Stress in the Brain. Nat. Neurosci. 2015, 18, 1353–1363. [Google Scholar] [CrossRef]
- Andrasik, F.; Holroyd, K.A. A Test of Specific and Nonspecific Effects in the Biofeedback Treatment of Tension Headache. J. Consult. Clin. Psychol. 1980, 48, 575–586. [Google Scholar] [CrossRef]
- Cohen, H.D.; Graham, C.; Fotopoulos, S.S.; Cook, M.R. A Double-Blind Methodology for Biofeedback Research. Psychophysiology 1977, 14, 603–608. [Google Scholar] [CrossRef] [PubMed]
- Taub, E.; School, P.J. Some Methodological Considerations in Thermal Biofeedback Training. Behav. Res. Methods Instrum. 1978, 10, 617–622. [Google Scholar] [CrossRef]
- Melzack, R.; Perry, C. Self-Regulation of Pain: The Use of Alpha-Feedback and Hypnotic Training for the Control of Chronic Pain. Exp. Neurol. 1975, 46, 452–469. [Google Scholar] [CrossRef]
- Wickramasekera, I. Temperature Feedback for the Control of Migraine. J. Behav. Ther. Exp. Psychiatry 1973, 4, 343–345. [Google Scholar] [CrossRef]
- Wickramasekera, I. The Placebo Effect and Medical Instruments in Biofeedback. J. Clin. Eng. 1977, 2, 227–230. [Google Scholar] [CrossRef]
- Kirsch, I. Response Expectancy as a Determinant of Experience and Behavior. Am. Psychologist. 1985, 40, 1189–1202. [Google Scholar] [CrossRef]
- Colloca, L.; Miller, F.G. How Placebo Responses Are Formed: A Learning Perspective. Philos. Trans. Biol. Sci. 2011, 366, 1859–1869. [Google Scholar] [CrossRef]
- Landry, M.; Lifshitz, M.; Raz, A. Brain Correlates of Hypnosis: A Systematic Review and Meta-Analytic Exploration. Neurosci. Biobehav. Rev. 2017, 81, 75–98. [Google Scholar] [CrossRef]
- Barnes, K.; Wang, R.; Faasse, K. Practitioner Warmth and Empathy Attenuates the Nocebo Effect and Enhances the Placebo Effect. Appl. Psychol. Health Well-Being 2024, 16, 421–441. [Google Scholar] [CrossRef]
- Ellingsen, D.-M.; Isenburg, K.; Jung, C.; Lee, J.; Gerber, J.; Mawla, I.; Sclocco, R.; Grahl, A.; Anzolin, A.; Edwards, R.R.; et al. Brain-to-Brain Mechanisms Underlying Pain Empathy and Social Modulation of Pain in the Patient-Clinician Interaction. Proc. Natl. Acad. Sci. USA 2023, 120, e2212910120. [Google Scholar] [CrossRef]
- Mulej Bratec, S.; Bertram, T.; Starke, G.; Brandl, F.; Xie, X.; Sorg, C. Your Presence Soothes Me: A Neural Process Model of Aversive Emotion Regulation via Social Buffering. Social Cogn. Affect. Neurosci. 2020, 15, 561–570. [Google Scholar] [CrossRef] [PubMed]
- Reddan, M.C.; Young, H.; Falkner, J.; López-Solà, M.; Wager, T.D. Touch and Social Support Influence Interpersonal Synchrony and Pain. Soc. Cogn. Affect. Neurosci. 2020, 15, 1064–1075. [Google Scholar] [CrossRef] [PubMed]
- Traux, C.B.; Carkhuff, R.R. The Measurement of Interpersonal Sensitivity: The Jacobson Empathy Scale and the Carkhuff-Truax Empathy Scale. 1967. [Google Scholar]
- Wampold, B.E. Healing in a Social Context: The Importance of Clinician and Patient Relationship. Front. Pain Res. 2021, 2, 21. [Google Scholar] [CrossRef] [PubMed]
- Nitzan, U.; Chalamish, Y.; Krieger, I.; Erez, H.B.; Braw, Y.; Lichtenberg, P. Suggestibility as a Predictor of Response to Antidepressants: A Preliminary Prospective Trial. J. Affect. Disord. 2015, 185, 8–11. [Google Scholar] [CrossRef]
- Beecher, H.K. Increased Stress and Effectiveness of Placebos and “Active” Drugs. Science 1960, 132, 91–92. [Google Scholar] [CrossRef]
- Bräscher, A.-K.; Witthöft, M.; Becker, S. The Underestimated Significance of Conditioning in Placebo Hypoalgesia and Nocebo Hyperalgesia. Pain Res. Manag. 2018, 2018, 6841985. [Google Scholar] [CrossRef]
- Cusin, C.; Colloca, L. Treatment-Resistant Depression—Resistant to Placebos as Well? JAMA Netw. Open 2021, 4, e2127952. [Google Scholar] [CrossRef]
- Schmidt, S.; Loef, M.; Ostermann, T.; Walach, H. Treatment Effects in Pharmacological Clinical Randomized Controlled Trials Are Mainly Due to Placebo. J. Clin. Epidemiol. 2024, 179, 111658. [Google Scholar] [CrossRef]
- Tuttle, A.; Tohyama, S.; Ramsay, T.; Kimmelman, J.; Schweinhardt, P.; Bennett, G.; Mogil, J. Increasing Placebo Responses over Time in U.S. Clinical Trials of Neuropathic Pain. Pain 2015, 156, 2616–2626. [Google Scholar] [CrossRef]
- Vase, L.; Petersen, G.L.; Lund, K. Placebo Effects in Idiopathic and Neuropathic Pain Conditions. In Handbook of Experimental Pharmacology; Springer: Berlin/Heidelberg, Germany, 2014; Volume 225, pp. 121–136. [Google Scholar] [CrossRef]
- Bowers, M.E.; Yehuda, R. Intergenerational Transmission of Stress in Humans. Neuropsychopharmacology 2016, 41, 232–244. [Google Scholar] [CrossRef] [PubMed]
- Carone, B.R.; Fauquier, L.; Habib, N.; Shea, J.M.; Hart, C.E.; Li, R.; Bock, C.; Li, C.; Gu, H.; Zamore, P.D.; et al. Paternally Induced Transgenerational Environmental Reprogramming of Metabolic Gene Expression in Mammals. Cell 2010, 143, 1084–1096. [Google Scholar] [CrossRef] [PubMed]
- Jablonka, E.; Raz, G. Transgenerational Epigenetic Inheritance: Prevalence, Mechanisms, and Implications for the Study of Heredity and Evolution. Q. Rev. Biol. 2009, 84, 131–176. [Google Scholar] [CrossRef]
- Colloca, L. The Placebo Effect in Pain Therapies. Annu. Rev. Pharmacol. Toxicol. 2019, 59, 191–211. [Google Scholar] [CrossRef]
- Truax, C.B.; Carkhuff, R.R. Toward Effective Counseling and Psychotherapy: Training and Practice; Aldine Publishing Co.: Hawthorne, NY, USA, 1967; pp. xiv, 416. [Google Scholar]
- Anderson, S.R.; Gianola, M.; Medina, N.A.; Perry, J.M.; Wager, T.D.; Losin, E.A.R. Doctor Trustworthiness Influences Pain and Its Neural Correlates in Virtual Medical Interactions. Cereb. Cortex 2023, 33, 3421–3436. [Google Scholar] [CrossRef]
- Wickramasekera, I. Desensitization, Re-Sensitization and Desensitization Again: A Preliminary Study. J. Behav. Ther. Exp. Psychiatry 1970, 1, 257–262. [Google Scholar] [CrossRef]
- Wilson, S.J.; Woody, A.; Padin, A.C.; Lin, J.; Malarkey, W.B.; Kiecolt-Glaser, J.K. Loneliness and Telomere Length: Immune and Parasympathetic Function in Associations With Accelerated Aging. Ann. Behav. Med. 2019, 53, 541–550. [Google Scholar] [CrossRef]
- Coan, J.A.; Schaefer, H.S.; Davidson, R.J. Lending a Hand: Social Regulation of the Neural Response to Threat. Psychol. Sci. 2006, 17, 1032–1039. [Google Scholar] [CrossRef]
- Rainville, P.; Streff, A.; Chen, J.-I.; Houzé, B.; Desmarteaux, C.; Piché, M. Hypnotic Automaticity in the Brain at Rest: An Arterial Spin Labelling Study. Int. J. Clin. Exp. Hypn. 2019, 67, 512–542. [Google Scholar] [CrossRef]
- Palsson, O.S.; Kekecs, Z.; De Benedittis, G.; Moss, D.; Elkins, G.R.; Terhune, D.B.; Varga, K.; Shenefelt, P.D.; Whorwell, P.J. Current Practices, Experiences, and Views in Clinical Hypnosis: Findings of an International Survey. Int. J. Clin. Exp. Hypn. 2023, 71, 92–114. [Google Scholar] [CrossRef]
- Palsson, O.S.; Ballou, S. Hypnosis and Cognitive Behavioral Therapies for the Management of Gastrointestinal Disorders. Curr. Gastroenterol. Rep. 2020, 22, 31. [Google Scholar] [CrossRef]
- Vase, L.; Petersen, G.L.; Riley, J.L.; Price, D.D. Factors Contributing to Large Analgesic Effects in Placebo Mechanism Studies Conducted between 2002 and 2007. Pain 2009, 145, 36–44. [Google Scholar] [CrossRef] [PubMed]
- Enck, P.; Klosterhalfen, S. Placebo Responses and Placebo Effects in Functional Gastrointestinal Disorders. Front. Psychiatry 2020, 11, 797. [Google Scholar] [CrossRef]
- Pagnini, F.; Barbiani, D.; Grosso, F.; Cavalera, C.; Volpato, E.; Minazzi, G.A.; Poletti, V.; Riva, G.; Phillips, D. Enacting the Mind/Body Connection: The Role of Self-Induced Placebo Mechanisms. Humanit. Soc. Sci. Commun. 2024, 11, 977. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).