Predicting Fear Extinction in Posttraumatic Stress Disorder
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedures
2.2.1. Clinical Interviews
2.2.2. Self-Report Measures
Trauma-Exposure and PTSD Symptom Questionnaires
Dissociation Questionnaires
Depression Questionnaires
Fear and Anxiety Questionnaires
Sleep and Resilience Questionnaires
2.2.3. Laboratory Paradigms
Dark-Enhanced Startle
Fear Conditioning
2.2.4. Physiological Data Acquisition and Processing
Startle
Skin Conductance
Cardiography
2.2.5. Statistical Analyses
Outcome Variables
Predictor Variables
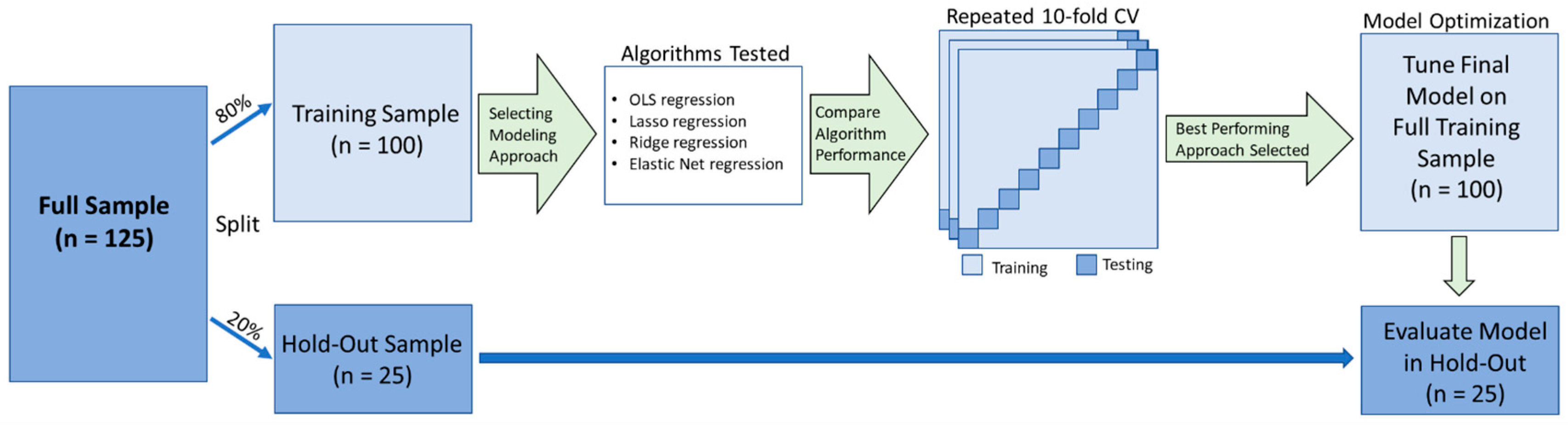
Analysis Pipeline
Comparing Predictive Models
Examining Specific Predictor Variables
Post Hoc Analyses
3. Results
3.1. Model Fit Comparisons
3.1.1. Early Extinction
3.1.2. Late Extinction
3.2. Predictors
3.2.1. Early Extinction
3.2.2. Late Extinction
3.3. Post Hoc Analyses
Early Extinction
4. Discussion
4.1. Modeling Approaches
4.2. Predictor Variables
4.3. Methodological Considerations
4.4. Limitations and Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Variable | UN BF | UN 0.05 | Lasso | ENR | MV Lasso BF | MV Lasso 0.05 | MV ENR BF | MV ENR 0.05 |
|---|---|---|---|---|---|---|---|---|
| CAPS Avoidance | X | X | ||||||
| CAPS Hyperarousal | X | X | X | X | X | |||
| White, Non-Hispanic | X | |||||||
| Sex (Female) | X | X | X | |||||
| PCL Total | X | X | ||||||
| LEC Experienced + Witnessed | X | |||||||
| CTQ Emotional Abuse | X | |||||||
| CTQ Emotional Neglect | X | |||||||
| CTQ Physical Neglect | X | X | X | |||||
| DES Total | X | X | ||||||
| DES Absorption | X | |||||||
| DES Depersonalization | X | X | X | X | X | |||
| ASI Total | X | X | ||||||
| STAI Trait Total | X | |||||||
| BDI Total | X | |||||||
| PSQI Total | X | X | X | |||||
| Baseline Startle | X | X | X | X | ||||
| Dark-Enhanced Startle | X | X | X | X | X | X | X | X |
| FPS to CS+, Acq block 1 | X | X | X | X | X | |||
| FPS to CS+, Acq block 2 | X | X | X | X | ||||
| FPS to CS+, Acq block 3 | X | X | X | X | X | |||
| FPS to CS−, Acq block 1 | X | |||||||
| FPS to CS−, Acq block 2 | X | X | X | X | ||||
| FPS to CS−, Acq block 3 | X | X | X | X | ||||
| HR, Dark-Enhanced Startle | X | |||||||
| HR, Acq | X | |||||||
| RSA, Baseline | X | X |
| Variable | UN BF | UN 0.05 | Lasso | ENR | MV Lasso BF | MV Lasso 0.05 | MV ENR BF | MV ENR 0.05 |
|---|---|---|---|---|---|---|---|---|
| CAPS Intrusion | X | X | ||||||
| CAPS Avoidance | X | X | X | X | ||||
| CAPS Hyperarousal | X | X | ||||||
| Age | X | X | ||||||
| White, Non-Hispanic | X | |||||||
| LEC Experienced + Witnessed | X | X | ||||||
| CTQ total score | X | |||||||
| CTQ Emotional Neglect | X | X | ||||||
| CTQ Physical Neglect | X | X | X | |||||
| BDI Total | X | X | ||||||
| PSQI Total | X | X | ||||||
| FSS Total | X | |||||||
| Baseline Startle | X | X | X | X | X | X | ||
| Dark-Enhanced Startle | X | X | X | |||||
| FPS to CS+, Acq block 2 | X | X | X | X | X | |||
| FPS to CS+, Acq block 3 | X | X | ||||||
| FPS to CS−, Acq block 1 | X | X | X | |||||
| FPS to CS−, Acq block 2 | X | X | X | |||||
| FPS to CS−, Acq block 3 | X | X | X | X | X | |||
| Heart Rate, Acq | X | |||||||
| RSA, Dark-Enhanced Startle | X | X | ||||||
| SCR Difference score (CS+-CS−) Acq block 2 | X | X |
References
- Ressler, K.J.; Berretta, S.; Bolshakov, V.Y.; Rosso, I.M.; Meloni, E.G.; Rauch, S.L.; Carlezon, W.A., Jr. Post-traumatic stress disorder: Clinical and translational neuroscience from cells to circuits. Nat. Rev. Neuro. 2022, 18, 273–288. [Google Scholar] [CrossRef]
- Rauch, S.A.M.; Eftekhari, A.; Ruzek, J.I. Review of exposure therapy: A gold standard for PTSD treatment. J. Rehabil. Res. Dev. 2012, 49, 679–687. [Google Scholar] [PubMed]
- Norrholm, S.D.; Jovanovic, T.; Gerardi, M.; Breazeale, K.G.; Price, M.; Davis, M.; Duncan, E.; Ressler, K.J.; Bradley, B.; Rizzo, A.; et al. Baseline psychophysiological and cortisol reactivity as a predictor of PTSD treatment outcome in virtual reality exposure therapy. Behav. Res. Ther. 2016, 82, 28–37. [Google Scholar]
- Kirlic, N.; Kuplicki, R.; Touthang, J.; Cohen, Z.P.; Stewart, J.L.; Paulus, M.P.; Aupperle, R.L. Behavioral and neural responses during fear conditioning and extinction in a large transdiagnostic sample. NeuroImage Clin. 2022, 35, 103060. [Google Scholar] [PubMed]
- Wangelin, B.C.; Tuerk, P.W. Taking the pulse of prolonged exposure therapy: Physiological reactivity to trauma imagery as an objective measure of treatment response. Depress. Anxiety 2015, 32, 927–934. [Google Scholar] [CrossRef] [PubMed]
- Lonsdorf, T.B.; Merz, C.J. More than just noise: Inter-individual differences in fear acquisition, extinction and return of fear in humans—Biological, experiential, temperamental factors, and methodological pitfalls. Neurosci. Biobehav. Rev. 2017, 80, 703–728. [Google Scholar] [PubMed]
- Pöhlchen, D.; Leuchs, L.; Binder, F.P.; Blaskovich, B.; Nantawisarakul, T.; Topalidis, P.; Brückl, T.M.; Norrholm, S.D.; Jovanovic, T.; BeCOME Working Group; et al. No robust differences in fear conditioning between patients with fear-related disorders and healthy controls. Behav. Res. Ther. 2020, 129, 103610. [Google Scholar] [CrossRef]
- Wen, Z.; Fried, J.; Pace-Schott, E.F.; Lazar, S.W.; Milad, M.R. Revisiting sex differences in the acquisition and extinction of threat conditioning in humans. Learn. Mem. 2022, 29, 274–282. [Google Scholar] [CrossRef]
- Lewis, M.W.; Bradford, D.E.; Pace-Schott, E.F.; Rauch, S.L.; Rosso, I.M. Multiverse analyses of fear acquisition and extinction retention in posttraumatic stress disorder. Psychophysiology 2023, 60, e14265. [Google Scholar] [PubMed]
- Sjouwerman, R.; Scharfenort, R.; Lonsdorf, T.B. Individual differences in fear acquisition: Multivariate analyses of different emotional negativity scales, physiological responding, subjective measures, and neural activation. Sci. Rep. 2020, 10, 15283. [Google Scholar]
- Webb, C.A.; Cohen, Z.D.; Beard, C.; Forgeard, M.; Peckham, A.D.; Björgvinsson, T. Personalized prognostic prediction of treatment outcome for depressed patients in a naturalistic psychiatric hospital setting: A comparison of machine learning approaches. J. Consult. Clin. Psychol. 2020, 88, 25–38. [Google Scholar] [PubMed]
- Greenwood, C.J.; Youssef, G.J.; Letcher, P.; Macdonald, J.A.; Hagg, L.J.; Sanson, A.; Mcintosh, J.; Hutchinson, D.M.; Toumbourou, J.W.; Fuller-Tyszkiewicz, M.; et al. A comparison of penalised regression methods for informing the selection of predictive markers. PLoS ONE 2020, 15, e0242730. [Google Scholar] [CrossRef] [PubMed]
- Studerus, E.; Vizeli, P.; Harder, S.; Ley, L.; Liechti, M.E. Prediction of MDMA response in healthy humans: A pooled analysis of placebo-controlled studies. J. Psychopharmacol. 2021, 35, 556–565. [Google Scholar] [CrossRef] [PubMed]
- van Rooij, S.J.H.; Stevens, J.S.; Ely, T.D.; Hinrichs, R.; Michopoulos, V.; Winters, S.J.; Ogbonmwan, Y.E.; Shin, J.; Nugent, N.R.; Hudak, L.A.; et al. The role of the hippocampus in predicting future posttraumatic stress disorder symptoms in recently traumatized civilians. Biol. Psychiatry 2018, 84, 106–115. [Google Scholar]
- Zuj, D.V.; Palmer, M.A.; Lommen, M.J.J.; Felmingham, K.L. The centrality of fear extinction in linking risk factors to PTSD: A narrative review. Neurosci. Biobehav. Rev. 2016, 69, 15–35. [Google Scholar] [CrossRef]
- Norrholm, S.D.; Jovanovic, T.; Olin, I.W.; Sands, L.A.; Karapanou, I.; Bradley, B.; Ressler, K.J. Fear extinction in traumatized civilians with posttraumatic stress disorder: Relation to symptom severity. Biol. Psychiatry 2011, 69, 556–563. [Google Scholar] [PubMed]
- Orcutt, H.K.; Hannan, S.M.; Seligowski, A.V.; Jovanovic, T.; Norrholm, S.D.; Ressler, K.J.; McCanne, T. Fear-potentiated startle and fear extinction in a sample of undergraduate women exposed to a campus mass shooting. Front. Psychol. 2016, 7, 2031. [Google Scholar] [CrossRef]
- Galatzer-Levy, I.R.; Andero, R.; Sawamura, T.; Jovanovic, T.; Papini, S.; Ressler, K.J.; Norrholm, S.D. A cross species study of heterogeneity in fear extinction learning in relation to FKBP5 variation and expression: Implications for the acute treatment of posttraumatic stress disorder. Neuropharmacology 2017, 116, 188–195. [Google Scholar] [CrossRef]
- Norrholm, S.D.; Glover, E.M.; Stevens, J.S.; Fani, N.; Galatzer-Levy, I.R.; Bradley, B.; Ressler, K.J.; Jovanovic, T. Fear load: The psychophysiological over-expression of fear as an intermediate phenotype associated with trauma reactions. Int. J. Psychophysiol. 2015, 98, 270–275. [Google Scholar] [CrossRef]
- Richards, A.; Inslicht, S.S.; Yack, L.M.; Metzler, T.J.; Russell Huie, J.; Straus, L.D.; Dukes, C.; Hubachek, S.Q.; Felmingham, K.L.; Mathalon, D.H.; et al. The relationship of fear-potentiated startle and polysomnography-measured sleep in trauma-exposed men and women with and without PTSD: Testing REM sleep effects and exploring the roles of an integrative measure of sleep, PTSD symptoms, and biological Sex. Sleep 2022, 45, zsab271. [Google Scholar] [CrossRef]
- Galatzer-Levy, I.R.; Bryant, R.A. 636,120 Ways to have posttraumatic stress disorder. Perspect. Psychol. Sci. 2013, 8, 651–662. [Google Scholar] [CrossRef] [PubMed]
- Zoellner, L.A.; Pruitt, L.D.; Farach, F.J.; Jun, J.J. Understanding heterogeneity in PTSD: Fear, dysphoria, and distress. Depress. Anxiety 2014, 31, 97–106. [Google Scholar] [CrossRef] [PubMed]
- Lonsdorf, T.B.; Gerlicher, A.; Klingelhöfer-Jens, M.; Krypotos, A.-M. Multiverse analyses in fear conditioning research. Behav. Res. Ther. 2022, 153, 104072. [Google Scholar] [CrossRef] [PubMed]
- Pappens, M.; Schroijen, M.; Sütterlin, S.; Smets, E.; den Bergh, O.V.; Thayer, J.F.; Diest, I.V. Resting heart rate variability predicts safety learning and fear extinction in an interoceptive fear conditioning paradigm. PLoS ONE 2014, 9, e105054. [Google Scholar] [CrossRef] [PubMed]
- Bottary, R.; Seo, J.; Daffre, C.; Gazecki, S.; Moore, K.N.; Kopotiyenko, K.; Dominguez, J.P.; Gannon, K.; Lasko, N.B.; Roth, B.; et al. Fear extinction memory is negatively associated with REM sleep in insomnia disorder. Sleep 2020, 43, zsaa007. [Google Scholar] [CrossRef]
- Pace-Schott, E.F.; Germain, A.; Milad, M.R. Effects of sleep on memory for conditioned fear and fear extinction. Psychol. Bull. 2015, 141, 835–857. [Google Scholar] [CrossRef]
- Pace-Schott, E.F.; Seo, J.; Bottary, R. The influence of sleep on fear extinction in trauma-related disorders. Neurobiol. Stress 2023, 22, 100500. [Google Scholar] [CrossRef]
- Schenker, M.T.; Ince, S.; Ney, L.J.; Hsu, C.-M.K.; Zuj, D.V.; Jordan, A.S.; Nicholas, C.L.; Felmingham, K.L. Sex differences in the effect of subjective sleep on fear conditioning, extinction learning, and extinction recall in individuals with a range of PTSD symptom severity. Behav. Res. Ther. 2022, 159, 104222. [Google Scholar] [CrossRef]
- Marusak, H.A.; Hehr, A.; Bhogal, A.; Peters, C.; Iadipaolo, A.; Rabinak, C.A. Alterations in fear extinction neural circuitry and fear-related behavior linked to trauma exposure in children. Behav. Brain. Res. 2021, 398, 112958. [Google Scholar] [CrossRef]
- Jenness, J.L.; Miller, A.B.; Rosen, M.L.; McLaughlin, K.A. Extinction learning as a potential mechanism linking high vagal tone with lower PTSD symptoms among abused youth. J. Abnorm. Child Psychol. 2019, 47, 659–670. [Google Scholar] [CrossRef]
- Hermann, A.; Küpper, Y.; Schmitz, A.; Walter, B.; Vaitl, D.; Hennig, J.; Stark, R.; Tabbert, K. Functional gene polymorphisms in the serotonin system and traumatic life events modulate the neural basis of fear acquisition and extinction. PLoS ONE 2012, 7, e44352. [Google Scholar] [CrossRef]
- Kuhn, M.; Höger, N.; Feige, B.; Blechert, J.; Normann, C.; Nissen, C. Fear extinction as a model for synaptic plasticity in major depressive disorder. PLoS ONE 2014, 9, e115280. [Google Scholar] [CrossRef] [PubMed]
- Rainer, C.; Nasrouei, S.; Tschofen, S.; Bliem, H.R.; Wilhelm, F.H.; Marksteiner, J. Fear acquisition and extinction in elderly patients with depression. J. Affect. Disord. 2020, 276, 197–204. [Google Scholar] [CrossRef]
- Wendt, J.; Neubert, J.; Koenig, J.; Thayer, J.F.; Hamm, A.O. Resting heart rate variability is associated with inhibition of conditioned fear. Psychophysiology 2015, 52, 1161–1166. [Google Scholar] [CrossRef]
- Seligowski, A.V.; Lee, D.J.; Miron, L.R.; Orcutt, H.K.; Jovanovic, T.; Norrholm, S.D. Prospective associations between emotion dysregulation and fear-potentiated startle: The moderating effect of respiratory sinus arrhythmia. Front. Psychol. 2016, 7, 652. [Google Scholar] [CrossRef] [PubMed]
- Giesbrecht, T.; Smeets, T.; Merckelbach, H.; Jelicic, M. Depersonalization experiences in undergraduates are related to heightened stress cortisol responses. J. Nerv. Ment. Dis. 2007, 195, 282–287. [Google Scholar] [CrossRef] [PubMed]
- Seligowski, A.V.; Lebois, L.A.M.; Hill, S.B.; Kahhale, I.; Wolff, J.D.; Jovanovic, T.; Winternitz, S.R.; Kaufman, M.L.; Ressler, K.J. Autonomic responses to fear conditioning among women with PTSD and dissociation. Depress. Anxiety 2019, 36, 625–634. [Google Scholar] [CrossRef]
- van Rooij, S.J.H.; Ravi, M.; Ely, T.D.; Michopoulos, V.; Winters, S.J.; Shin, J.; Marin, M.-F.; Milad, M.R.; Rothbaum, B.O.; Ressler, K.J.; et al. Hippocampal activation during contextual fear inhibition related to resilience in the early aftermath of trauma. Behav. Brain Res. 2021, 408, 113282. [Google Scholar] [CrossRef]
- Rakesh, G.; Morey, R.A.; Zannas, A.S.; Malik, Z.; Marx, C.E.; Clausen, A.N.; Kritzer, M.D.; Szabo, S.T. Resilience as a translational endpoint in the treatment of PTSD. Mol. Psychiatry 2019, 24, 1268–1283. [Google Scholar] [CrossRef]
- DePierro, J.M.; D’Andrea, W.; Frewen, P. Anhedonia in trauma related disorders: The good, the bad, and the shut-down. In Anhedonia: A Comprehensive Handbook Volume II: Neuropsychiatric and Physical Disorders; Ritsner, M.S., Ed.; Springer: Dordrecht, The Netherlands, 2014; pp. 175–189. [Google Scholar]
- Olson, E.A.; Kaiser, R.H.; Pizzagalli, D.A.; Rauch, S.L.; Rosso, I.M. Anhedonia in trauma-exposed individuals: Functional connectivity and decision-making correlates. Biol. Psychiatry Cogn. Neurosci. Neuroimaging 2018, 3, 959–967. [Google Scholar] [CrossRef]
- Walker, R.S.W. The Function of Conditioned Fear in Reward Propensity: Evidence for Interrelated Approach-Avoid Systems. Ph.D. Thesis, University of Washington, Seattle, WA, USA, 2017. [Google Scholar]
- Lewis, M.W.; Jones, R.T.; Davis, M.T. Exploring the impact of trauma type and extent of exposure on posttraumatic alterations in 5-HT1A expression. Transl. Psychiatry 2020, 10, 237. [Google Scholar] [CrossRef] [PubMed]
- Stenson, A.F.; van Rooij, S.J.H.; Carter, S.E.; Powers, A.; Jovanovic, T. A legacy of fear: Physiological evidence for intergenerational effects of trauma exposure on fear and safety signal learning among African Americans. Behav. Brain Res. 2021, 402, 113017. [Google Scholar] [CrossRef] [PubMed]
- Hunt, C.; Cooper, S.E.; Hartnell, M.P.; Lissek, S. Anxiety sensitivity and intolerance of uncertainty facilitate associations between generalized Pavlovian fear and maladaptive avoidance decisions. J. Abnorm. Psychol. 2019, 128, 315–326. [Google Scholar] [CrossRef]
- Lebeaut, A.; Tran, J.K.; Vujanovic, A.A. Posttraumatic stress, alcohol use severity, and alcohol use motives among firefighters: The role of anxiety sensitivity. Addict. Behav. 2020, 106, 106353. [Google Scholar] [CrossRef]
- Scharff, A.; Ortiz, S.N.; Forrest, L.N.; Smith, A.R. Comparing the clinical presentation of eating disorder patients with and without trauma history and/or comorbid PTSD. Eat. Disord. 2021, 29, 88–102. [Google Scholar] [CrossRef] [PubMed]
- Taylor, S.; Koch, W.J.; McNally, R.J. How does anxiety sensitivity vary across the anxiety disorders? J. Anxiety Disord. 1992, 6, 249–259. [Google Scholar] [CrossRef]
- Taylor, S. Anxiety sensitivity and its implications for understanding and treating PTSD. J. Cogn. Psychother. 2003, 17, 179–186. [Google Scholar] [CrossRef]
- Carpenter, J.K.; Bragdon, L.; Pineles, S.L. Conditioned physiological reactivity and PTSD symptoms across the menstrual cycle: Anxiety sensitivity as a moderator. Psychol. Trauma Theory Res. Pract. Policy 2022, 14, 453–461. [Google Scholar] [CrossRef] [PubMed]
- Overstreet, C.; Brown, E.; Berenz, E.C.; Brown, R.C.; Hawn, S.; McDonald, S.; Pickett, T.; Danielson, C.K.; Thomas, S.; Amstadter, A. Anxiety sensitivity and distress tolerance typologies and relations to posttraumatic stress disorder: A cluster analytic approach. Mil. Psychol. 2018, 30, 547–556. [Google Scholar] [CrossRef]
- Vaidyanathan, U.; Patrick, C.J.; Bernat, E.M. Startle reflex potentiation during aversive picture viewing as an indicator of trait fear. Psychophysiology 2009, 46, 75–85. [Google Scholar] [CrossRef]
- Kredlow, A.M.; Orr, S.P.; Otto, M.W. Who is studied in de novo fear conditioning paradigms? An examination of demographic and stimulus characteristics predicting fear learning. Int. J. Psychophysiol. 2018, 130, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Morris, M.C.; Hellman, N.; Abelson, J.L.; Rao, U. Cortisol, heart rate, and blood pressure as early markers of PTSD risk: A systematic review and meta-analysis. Clin. Psychol. Rev. 2016, 49, 79–91. [Google Scholar] [CrossRef] [PubMed]
- Schiweck, C.; Piette, D.; Berckmans, D.; Claes, S.; Vrieze, E. Heart rate and high frequency heart rate variability during stress as biomarker for clinical depression. A systematic review. Psychol. Med. 2019, 49, 200–211. [Google Scholar] [CrossRef] [PubMed]
- Russo, A.S.; Parsons, R.G. Acoustic startle response in rats predicts inter-individual variation in fear extinction. Neurobiol. Learn. Mem. 2017, 139, 157–164. [Google Scholar] [CrossRef]
- Bradford, D.E.; Kaye, J.T.; Curtin, J.J. Not just noise: Individual differences in general startle reactivity predict startle response to uncertain and certain threat. Psychophysiology 2014, 51, 407–411. [Google Scholar] [CrossRef]
- Kamkwalala, A.; Norrholm, S.D.; Poole, J.M.; Brown, A.; Donley, S.; Duncan, E.; Bradley, B.; Ressler, K.J.; Jovanovic, T. Dark-enhanced startle responses and heart rate variability in a traumatized civilian sample: Putative sex-specific correlates of posttraumatic stress disorder. Psychosom. Med. 2012, 74, 153–159. [Google Scholar] [CrossRef]
- Fani, N.; Tone, E.B.; Phifer, J.; Norrholm, S.D.; Bradley, B.; Ressler, K.J.; Kamkwalala, A.; Jovanovic, T. Attention bias toward threat is associated with exaggerated fear expression and impaired extinction in PTSD. Psychol. Med. 2012, 42, 533–543. [Google Scholar] [CrossRef]
- Jovanovic, T. How the neurocircuitry and genetics of fear inhibition may inform our understanding of PTSD. Am. J. Psychiatry 2010, 167, 648–662. [Google Scholar] [CrossRef]
- Burger, A.M.; Verkuil, B.; Van Diest, I.; Van der Does, W.; Thayer, J.F.; Brosschot, J.F. The effects of transcutaneous vagus nerve stimulation on conditioned fear extinction in humans. Neurobiol. Learn. Mem. 2016, 132, 49–56. [Google Scholar] [CrossRef]
- Shvil, E.; Rusch, H.L.; Sullivan, G.M.; Neria, Y. Neural, psychophysiological, and behavioral markers of fear processing in PTSD: A review of the literature. Curr. Psychiatry Rep. 2013, 15, 358. [Google Scholar] [CrossRef]
- Friedman, J.; Hastie, T.; Tibshirani, R. Regularization paths for generalized linear models via coordinate descent. J. Stat. Softw. 2010, 33, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Privé, F.; Aschard, H.; Blum, M.G.B. Efficient implementation of penalized regression for genetic risk prediction. Genetics 2019, 212, 65–74. [Google Scholar] [CrossRef] [PubMed]
- Ambler, G.; Seaman, S.; Omar, R.Z. An evaluation of penalised survival methods for developing prognostic models with rare events. Stat. Med. 2012, 31, 1150–1161. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Liang, C.; Ma, F. Forecasting stock market volatility with a large number of predictors: New evidence from the MS-MIDAS-LASSO model. Ann. Oper. Res. 2022, 1–40. [Google Scholar] [CrossRef]
- Pavlou, M.; Ambler, G.; Seaman, S.R.; Guttmann, O.; Elliott, P.; King, M.; Omar, R.Z. How to develop a more accurate risk prediction model when there are few events. BMJ 2015, 351, h3868. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.; Kim, K.; Kim, Y.J.; Lee, J.-K.; Cho, Y.S.; Lee, J.-Y.; Han, B.-G.; Kim, H.; Ott, J.; Park, T. Joint identification of multiple genetic variants via elastic-net variable selection in a genome-wide association analysis. Ann. Hum. Genet. 2010, 74, 416–428. [Google Scholar] [CrossRef]
- Ghosh, D.; Zhu, Y.; Coffman, D.L. Penalized regression procedures for variable selection in the potential outcomes framework. Stat. Med. 2015, 34, 1645–1658. [Google Scholar] [CrossRef]
- Tibshirani, R. The lasso method for variable selection in the cox model. Stat. Med. 1997, 16, 385–395. [Google Scholar] [CrossRef]
- Walter, S.; Tiemeier, H. Variable selection: Current practice in epidemiological studies. Eur. J. Epidemiol. 2009, 24, 733–736. [Google Scholar] [CrossRef]
- Glover, E.M.; Phifer, J.E.; Crain, D.F.; Norrholm, S.D.; Davis, M.; Bradley, B.; Ressler, K.J.; Jovanovic, T. Tools for translational neuroscience: PTSD is associated with heightened fear responses using acoustic startle but not skin conductance measures. Depress. Anxiety 2011, 28, 1058–1066. [Google Scholar] [CrossRef]
- Lonsdorf, T.B.; Menz, M.M.; Andreatta, M.; Fullana, M.A.; Golkar, A.; Haaker, J.; Heitland, I.; Hermann, A.; Kuhn, M.; Kruse, O.; et al. Don’t fear “fear conditioning”: Methodological considerations for the design and analysis of studies on human fear acquisition, extinction, and return of fear. Neurosci. Biobehav. Rev. 2017, 77, 247–285. [Google Scholar] [CrossRef] [PubMed]
- Weathers, F.W.; Bovin, M.J.; Lee, D.J.; Sloan, D.M.; Schnurr, P.P.; Kaloupek, D.G.; Keane, T.M.; Marx, B.P. The Clinician-Administered PTSD Scale for DSM–5 (CAPS-5): Development and initial psychometric evaluation in military veterans. Psychol. Assess. 2018, 30, 383–395. [Google Scholar] [CrossRef] [PubMed]
- Lecrubier, Y.; Sheehan, D.; Weiller, E.; Amorim, P.; Bonora, I.; Harnett Sheehan, K.; Janavs, J.; Dunbar, G. The Mini International Neuropsychiatric Interview (MINI). A short diagnostic structured interview: Reliability and validity according to the CIDI. Eur. Psychiatry 1997, 12, 224–231. [Google Scholar] [CrossRef]
- Weathers, F.W.; Blake, D.D.; Schnurr, P.P.; Kaloupek, D.G.; Marx, B.P.; Keane, T.M. The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5). 2013. Available online: www.ptsd.va.gov (accessed on 5 March 2023).
- Bernstein, D.P.; Fink, L.; Handelsman, L.; Foote, J. Childhood Trauma Questionnaire; APA PsycTests; APA: Washington, DC, USA, 1994. [Google Scholar]
- Gray, M.J.; Litz, B.T.; Hsu, J.L.; Lombardo, T.W. Psychometric properties of the Life Events Checklist. Assessment 2004, 11, 330–341. [Google Scholar] [CrossRef] [PubMed]
- Blevins, C.A.; Weathers, F.W.; Witte, T.K. Dissociation and posttraumatic stress disorder: A latent profile analysis. J. Trauma. Stress 2014, 27, 388–396. [Google Scholar] [CrossRef] [PubMed]
- Carlson, E.B.; Putnam, F.W. An update on the Dissociative Experiences Scale. Dissociation Prog. Dissociative Disord. 1993, 6, 16–27. [Google Scholar]
- Briere, J.; Weathers, F.W.; Runtz, M. Is dissociation a multidimensional construct? Data from the Multiscale Dissociation Inventory. J. Trauma. Stress 2005, 18, 221–231. [Google Scholar] [CrossRef]
- Beck, A.T.; Steer, R.A.; Brown, G. Beck Depression Inventory-II (BDI-II); APA PsycTests; APA: Washington, DC, USA, 1996. [Google Scholar]
- Snaith, R.P.; Hamilton, M.; Morley, S.; Humayan, A.; Hargreaves, D.; Trigwell, P. A scale for the assessment of hedonic tone the Snaith-Hamilton Pleasure Scale. Br. J. Psychiatry 1995, 167, 99–103. [Google Scholar] [CrossRef]
- Spielberger, C.D. State-Trait Anxiety Inventory for Adults; APA PsycTests; APA: Washington, DC, USA, 1983. [Google Scholar]
- Geer, J.H. The development of a scale to measure fear. Behav. Res. Ther. 1965, 3, 45–53. [Google Scholar] [CrossRef]
- Taylor, S.; Zvolensky, M.J.; Cox, B.J.; Deacon, B.; Heimberg, R.G.; Ledley, D.R.; Abramowitz, J.S.; Holaway, R.M.; Sandin, B.; Stewart, S.H.; et al. Robust dimensions of anxiety sensitivity: Development and initial validation of the Anxiety Sensitivity Index-3. Psychol. Assess. 2007, 19, 176–188. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Campbell-Sills, L.; Stein, M.B. Psychometric analysis and refinement of the Connor–Davidson Resilience Scale (CD-RISC): Validation of a 10-item measure of resilience. J. Trauma. Stress 2007, 20, 1019–1028. [Google Scholar] [CrossRef]
- Blumenthal, T.D.; Cuthbert, B.N.; Filion, D.L.; Hackley, S.; Lipp, O.V.; Van Boxtel, A. Committee report: Guidelines for human startle eyeblink electromyographic studies. Psychophysiology 2005, 42, 1–15. [Google Scholar] [CrossRef]
- Boucsein, W.; Fowles, D.C.; Grimnes, S.; Ben-Shakhar, G.; Roth, W.T.; Dawson, M.E.; Filion, D.L. Publication Recommendations for Electrodermal Measurements. Psychophysiology 2012, 49, 1017–1034. [Google Scholar]
- Morgan, E. All about ECG Part 4: Basic Artifact Correction. In MindWare Technologies Support; MindWare Technologies Ltd.: Westerville, OH, USA, 2016. [Google Scholar]
- Stekhoven, D.J.; Buehlmann, P. MissForest-nonparametric missing value imputation for mixed-type data. Bioinform 2012, 28, 112–118. [Google Scholar] [CrossRef]
- R Core Team, R. The R Project for Statistical Computing. Available online: https://www.r-project.org/ (accessed on 12 February 2023).
- Friedman, J.; Hastie, T.; Tibshirani, R.; Narasimhan, B.; Tay, K.; Simon, N.; Qian, J.; Yang, J. Glmnet. In Lasso and Elastic-Net Regularized Generalized Linear Models; 2023; Available online: https://glmnet.stanford.edu/ (accessed on 12 February 2023).
- Kuhn, M. The Caret Package. 2019. Available online: https://topepo.github.io/caret/ (accessed on 12 February 2023).
- Chicco, D.; Warrens, M.J.; Jurman, G. The coefficient of determination R-squared is more informative than SMAPE, MAE, MAPE, MSE and RMSE in regression analysis evaluation. Peer J. Comput. Sci. 2021, 7, e623. [Google Scholar] [CrossRef]
- Rubin, M. When to adjust alpha during multiple testing: A consideration of disjunction, conjunction, and individual testing. Synthese 2021, 199, 10969–11000. [Google Scholar] [CrossRef]
- Bennett, C.M.; Wolford, G.L.; Miller, M.B. The principled control of false positives in neuroimaging. Soc. Cogn. Affect. Neurosci. 2009, 4, 417–422. [Google Scholar] [CrossRef]
- Cramer, A.O.J.; van Ravenzwaaij, D.; Matzke, D.; Steingroever, H.; Wetzels, R.; Grasman, R.P.P.P.; Waldorp, L.J.; Wagenmakers, E.-J. Hidden multiplicity in exploratory multiway ANOVA: Prevalence and remedies. Psychon. Bull. Rev. 2016, 23, 640–647. [Google Scholar] [CrossRef]
- Streiner, D.L. Best (but oft-forgotten) practices: The multiple problems of multiplicity—Whether and how to correct for many statistical tests. Am. J. Clin. 2015, 102, 721–728. [Google Scholar] [CrossRef]
- Parker, R.A.; Weir, C.J. Non-adjustment for multiple testing in multi-arm trials of distinct treatments: Rationale and justification. Clin. Trials 2020, 17, 562–566. [Google Scholar] [CrossRef] [PubMed]
- Wason, J.M.S.; Stecher, L.; Mander, A.P. Correcting for multiple-testing in multi-arm trials: Is it necessary and is it done? Trials 2014, 15, 364. [Google Scholar] [CrossRef] [PubMed]
- Tutzauer, F. On the sensible application of familywise alpha adjustment. Hum. Commun. Res. 2003, 29, 455–463. [Google Scholar] [CrossRef]
- Bender, R.; Lange, S. Adjusting for multiple testing—When and how? J. Clin. Epidemiol. 2001, 54, 343–349. [Google Scholar] [CrossRef] [PubMed]
- Blevins, C.A.; Weathers, F.W.; Davis, M.T.; Witte, T.K.; Domino, J.L. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. J. Trauma. Stress 2015, 28, 489–498. [Google Scholar] [CrossRef] [PubMed]
- Mohri, M.; Rostamizadeh, A.; Talwalkar, A. Foundations of Machine Learning, 2nd ed.; MIT Press: Cambridge, MA, USA, 2018. [Google Scholar]
- Morriss, J.; van Reekum, C.M. I feel safe when I know: Contingency instruction promotes threat extinction in high intolerance of uncertainty individuals. Behav. Res. Ther. 2019, 116, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Potential Threat (“Anxiety”). Available online: https://www.nimh.nih.gov/research/research-funded-by-nimh/rdoc/constructs/potential-threat-anxiety (accessed on 6 March 2023).
- Kozak, M.J.; Cuthbert, B.N. The NIMH Research Domain Criteria initiative: Background, issues, and pragmatics. Psychophysiology 2016, 53, 286–297. [Google Scholar] [CrossRef]
- Cuthbert, B.N. Research Domain Criteria (RDoC): Progress and potential. Curr. Dir. Psychol. Sci. 2022, 31, 107–114. [Google Scholar] [CrossRef]
- Acute Threat (“Fear”). Available online: https://www.nimh.nih.gov/research/research-funded-by-nimh/rdoc/constructs/acute-threat-fear (accessed on 6 March 2023).
- Michelini, G.; Palumbo, I.M.; DeYoung, C.G.; Latzman, R.D.; Kotov, R. Linking RDoC and HiTOP: A new interface for advancing psychiatric nosology and neuroscience. Clin. Psychol. Rev. 2021, 86, 102025. [Google Scholar] [CrossRef] [PubMed]
- Resick, P.A.; Suvak, M.K.; Johnides, B.D.; Mitchell, K.S.; Iverson, K.M. The impact of dissociation on PTSD treatment with cognitive processing therapy. Depress. Anxiety 2012, 29, 718–730. [Google Scholar] [CrossRef]
- Powers, A.; Dixon, H.D.; Conneely, K.; Gluck, R.; Munoz, A.; Rochat, C.; Mendoza, H.; Hartzell, G.; Ressler, K.J.; Bradley, B.; et al. The differential effects of PTSD, MDD, and dissociation on CRP in trauma-exposed women. Compr. Psychiatry 2019, 93, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Powers, A.; Mekawi, Y.; Fickenwirth, M.; Nugent, N.R.; Dixon, H.D.; Minton, S.; Kim, Y.J.; Gluck, R.; Carter, S.; Fani, N.; et al. Emotion dysregulation and dissociation contribute to decreased heart rate variability to an acute psychosocial stressor in trauma-exposed Black women. J. Psychiatr. Res. 2021, 142, 125–131. [Google Scholar] [CrossRef]
- Powers, A.; Cross, D.; Fani, N.; Bradley, B. PTSD, emotion dysregulation, and dissociative symptoms in a highly traumatized sample. J. Psychiatr. Res. 2015, 61, 174–179. [Google Scholar] [CrossRef] [PubMed]
- Norrholm, S.D.; Jovanovic, T. Tailoring therapeutic strategies for treating posttraumatic stress disorder symptom clusters. Neuropsychiatr. Dis. Treat. 2010, 6, 517–532. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, M.; Gerlicher, A.M.V.; Lonsdorf, T.B. Navigating the manyverse of skin conductance response quantification approaches—A direct comparison of trough-to-peak, baseline correction, and model-based approaches in Ledalab and PsPM. Psychophysiology 2022, 59, e14058. [Google Scholar] [CrossRef]
- Sjouwerman, R.; Illius, S.; Kuhn, M.; Lonsdorf, T.B. A data multiverse analysis investigating non-model based SCR quantification approaches. Psychophysiology 2022, 59, e14130. [Google Scholar] [CrossRef]
- Button, K.S.; Ioannidis, J.P.A.; Mokrysz, C.; Nosek, B.A.; Flint, J.; Robinson, E.S.J.; Munafò, M.R. Power failure: Why small sample size undermines the reliability of neuroscience. Nat. Rev. Neurosci. 2013, 14, 365–376. [Google Scholar] [CrossRef]
- Baldwin, S.A. Improving the rigor of psychophysiology research. Int. J. Psychophysiol. 2017, 111, 5–16. [Google Scholar] [CrossRef]
- Vinograd, M.; Stout, D.M.; Risbrough, V.B. Anhedonia in posttraumatic stress disorder: Prevalence, phenotypes, and neural circuitry. In Anhedonia: Preclinical, Translational, and Clinical Integration; Pizzagalli, D.A., Ed.; Current Topics in Behavioral Neurosciences; Springer International Publishing: Cham, Switzerland, 2022; pp. 185–199. ISBN 978-3-031-09683-9. [Google Scholar]
- Beauchaine, T.P.; Thayer, J.F. Heart rate variability as a transdiagnostic biomarker of psychopathology. Int. J. Psychophysiol. 2015, 98, 338–350. [Google Scholar] [CrossRef]
- Van Calster, B.; van Smeden, M.; De Cock, B.; Steyerberg, E.W. Regression shrinkage methods for clinical prediction models do not guarantee improved performance: Simulation study. Stat. Methods Med. Res. 2020, 29, 3166–3178. [Google Scholar] [CrossRef]
- VanderWeele, T.J.; Mathur, M.B. Some desirable properties of the Bonferroni correction: Is the Bonferroni correction really so bad? Am. J. Epidemiol. 2019, 188, 617–618. [Google Scholar] [CrossRef]
- Lee, D.J.; Weathers, F.W.; Thompson-Hollands, J.; Sloan, D.M.; Marx, B.P. Concordance in PTSD symptom change between DSM-5 versions of the Clinician-Administered PTSD Scale (CAPS-5) and PTSD Checklist (PCL-5). Psychol. Assess. 2022, 34, 604–609. [Google Scholar] [CrossRef]
- Cross, D.; Fani, N.; Powers, A.; Bradley, B. Neurobiological development in the context of childhood trauma. Clin. Psychol. Sci. Pract. 2017, 24, 111–124. [Google Scholar] [CrossRef]
- Heim, C.; Nemeroff, C.B. The role of childhood trauma in the neurobiology of mood and anxiety disorders: Preclinical and clinical Studies. Biol. Psychiatry 2001, 49, 1023–1039. [Google Scholar] [CrossRef]
- Herringa, R.J. Trauma, PTSD, and the developing brain. Curr. Psychiatry Rep. 2017, 19, 69. [Google Scholar] [CrossRef]
- Nemeroff, C.B. Neurobiological Consequences of Childhood Trauma. J. Clin. Psychiatry 2004, 65 (Suppl. S1), 18–28. [Google Scholar]
- Bosch, J.; Mackintosh, M.-A.; Wells, S.Y.; Wickramasinghe, I.; Glassman, L.H.; Morland, L.A. PTSD treatment response and quality of life in women with childhood trauma histories. Psychol. Trauma Theory Res. Pract. Policy 2020, 12, 55–63. [Google Scholar] [CrossRef]
- McLaughlin, K.A.; Lambert, H.K. Child trauma exposure and psychopathology: Mechanisms of risk and resilience. Curr. Opin. Psychol. 2017, 14, 29–34. [Google Scholar] [CrossRef]
- Charak, R.; de Jong, J.T.V.M.; Berckmoes, L.H.; Ndayisaba, H.; Reis, R. Assessing the factor structure of the Childhood Trauma Questionnaire, and cumulative effect of abuse and neglect on mental health among adolescents in conflict-affected Burundi. Child Abuse Negl. 2017, 72, 383–392. [Google Scholar] [CrossRef]
- Cheng, Y.-C.; Kuo, P.-H. Reliability and factor structure of the Chinese version of Childhood Trauma Questionnaire-Short Form in patients with substance use disorder. Taiwanese J. Psychiatry 2018, 32, 52–62. [Google Scholar]
- Scher, C.D.; Stein, M.B.; Asmundson, G.J.; McCreary, D.R.; Forde, D.R. The Childhood Trauma Questionnaire in a community sample: Psychometric properties and normative data. J. Trauma. Stress 2001, 14, 843–857. [Google Scholar] [CrossRef]
- Spinhoven, P.; Penninx, B.W.; Hickendorff, M.; van Hemert, A.M.; Bernstein, D.P.; Elzinga, B.M. Childhood Trauma Questionnaire: Factor structure, measurement invariance, and validity across emotional disorders. Psychol. Assess. 2014, 26, 717–729. [Google Scholar] [CrossRef]
- May, C.L.; Wisco, B.E. Defining Trauma: How level of exposure and proximity affect risk for posttraumatic stress disorder. Psychol. Trauma Theory Res. Pract. Policy 2016, 8, 233–240. [Google Scholar] [CrossRef]
- Olson, E.A.; Overbey, T.A.; Ostrand, C.G.; Pizzagalli, D.A.; Rauch, S.L.; Rosso, I.M. Childhood maltreatment experiences are associated with altered diffusion in occipito-temporal white matter Pathways. Brain Behav. 2019, 10, e01485. [Google Scholar] [CrossRef]
- Weis, C.N.; Webb, E.K.; Stevens, S.K.; Larson, C.L.; deRoon-Cassini, T.A. Scoring the Life Events Checklist: Comparison of three scoring methods. Psychol. Trauma Theory Res. Pract. Policy 2022, 14, 714–720. [Google Scholar] [CrossRef]
- Rosso, I.M.; Silveri, M.M.; Olson, E.A.; Eric Jensen, J.; Ren, B. Regional specificity and clinical correlates of cortical GABA alterations in posttraumatic stress disorder. Neuropsychopharmacology 2022, 47, 1055–1062. [Google Scholar] [CrossRef]
- Pugach, C.P.; Nomamiukor, F.O.; Gay, N.G.; Wisco, B.E. Temporal stability of self-reported trauma exposure on the Life Events Checklist for DSM-5. J. Trauma. Stress 2021, 34, 248–256. [Google Scholar] [CrossRef] [PubMed]
- Dorahy, M.J.; van der Hart, O. DSM–5′s Posttraumatic stress disorder with dissociative symptoms: Challenges and future directions. J. Trauma Dissociation 2015, 16, 7–28. [Google Scholar] [CrossRef]
- Lanius, R.A.; Vermetten, E.; Loewenstein, R.J.; Brand, B.; Schmahl, C.; Bremner, J.D.; Spiegel, D. Emotion modulation in PTSD: Clinical and neurobiological evidence for a dissociative subtype. Am. J. Psychiatry 2010, 167, 640–647. [Google Scholar] [CrossRef]
- Lanius, R.A.; Brand, B.; Vermetten, E.; Frewen, P.A.; Spiegel, D. The dissociative subtype of posttraumatic stress disorder: Rationale, clinical and neurobiological evidence, and implications. Depress. Anxiety 2012, 29, 701–708. [Google Scholar] [CrossRef]
- Schiavone, F.L.; Frewen, P.; McKinnon, M.; Lanius, R.A. The dissociative subtype of PTSD: An update of the literature. PTSD Research Quarterly. 2018, 29, 2–13. [Google Scholar]
- Lyssenko, L.; Schmahl, C.; Bockhacker, L.; Vonderlin, R.; Bohus, M.; Kleindienst, N. Dissociation in psychiatric disorders: A meta-analysis of studies using the Dissociative Experiences Scale. Am. J. Psychiatry 2018, 175, 37–46. [Google Scholar] [CrossRef]
- Carlson, E.B.; Rosser-Hogan, R. Trauma experiences, Posttraumatic Stress, dissociation, and depression in Cambodian refugees. Am. J. Psychiatry 1991, 148, 1548–1551. [Google Scholar] [PubMed]
- Ross, C.A.; Ellason, J.W.; Anderson, G. A factor analysis of the Dissociative Experiences Scale (DES) in dissociative identity disorder. Dissociation Prog. Dissociative Disord. 1995, 8, 229–235. [Google Scholar]
- Stockdale, G.D.; Gridley, B.E.; Balogh, D.W.; Holtgraves, T. Confirmatory factor analysis of single- and multiple-factor competing models of the dissociative experiences scale in a nonclinical sample. Assessment 2002, 9, 94–106. [Google Scholar] [CrossRef]
- Patel, H.; O’Connor, C.; Andrews, K.; Amlung, M.; Lanius, R.; McKinnon, M.C. Dissociative symptomatology mediates the relation between posttraumatic stress disorder severity and alcohol-related problems. Alcohol Clin. Exp. Res. 2022, 46, 289–299. [Google Scholar] [CrossRef]
- Strunk, K.K.; Lane, F.C. The Beck Depression Inventory, Second Edition (BDI-II): A cross-sample structural analysis. Meas. Eval. Couns. Dev. 2016, 0748175616664010. [Google Scholar] [CrossRef]
- Kline, A.C.; Cooper, A.A.; Rytwinski, N.K.; Feeny, N.C. The effect of concurrent depression on PTSD outcomes in trauma-focused psychotherapy: A meta-analysis of randomized controlled trials. Behav. Ther. 2021, 52, 250–266. [Google Scholar] [CrossRef]
- Brouwer, D.; Meijer, R.R.; Zevalkink, J. On the factor structure of the Beck Depression Inventory-II: G Is the Key. Psychol. Assess. 2013, 25, 136–145. [Google Scholar] [CrossRef] [PubMed]
- Faro, A.; Pereira, C.R. Factor structure and gender invariance of the Beck Depression Inventory–Second Edition (BDI-II) in a community-dwelling sample of adults. Health Psychol. Behav. Med. 2020, 8, 16–31. [Google Scholar] [CrossRef] [PubMed]
- Keller, F.; Kirschbaum-Lesch, I.; Straub, J. Factor structure and measurement invariance across gender of the Beck Depression Inventory-II in adolescent psychiatric patients. Front. Psychiatry 2020, 11, 527559. [Google Scholar] [CrossRef] [PubMed]
- McElroy, E.; Casey, P.; Adamson, G.; Filippopoulos, P.; Shevlin, M. A comprehensive analysis of the factor structure of the Beck Depression Inventory-II in a sample of outpatients with adjustment disorder and depressive episode. Ir. J. Psychol. Med. 2018, 35, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Young, K.S.; Bookheimer, S.Y.; Nusslock, R.; Zinbarg, R.E.; Damme, K.S.F.; Chat, I.K.-Y.; Kelley, N.J.; Vinograd, M.; Perez, M.; Chen, K.; et al. Dysregulation of threat neurocircuitry during fear extinction: The role of anhedonia. Neuropsychopharmacology 2021, 46, 1650–1657. [Google Scholar] [CrossRef]
- Jakši, N.; Brajkovic, L.; Ivezic, E.; Topic, R.; Jakovljevic, M. The role of personality traits in posttraumatic stress disorder (PTSD). Psychiatr. Danub. 2012, 24, 256–266. [Google Scholar]
- Rooney, E.A.; Hallauer, C.J.; Xie, H.; Shih, C.-H.; Rapport, D.; Elhai, J.D.; Wang, X. Longitudinal PTSD symptom trajectories: Relative contributions of state anxiety, depression, and emotion dysregulation. J. Affect. Disord. 2022, 308, 281–288. [Google Scholar] [CrossRef]
- Asmundson, G.J.G.; Stapleton, J.A. Associations between dimensions of anxiety sensitivity and PTSD symptom clusters in active-duty police officers. Cogn. Behav. Ther. 2008, 37, 66–75. [Google Scholar] [CrossRef]
- Marshall, G.N.; Miles, J.N.V.; Stewart, S.H. Anxiety sensitivity and PTSD symptom severity are reciprocally related: Evidence from a longitudinal study of physical trauma survivors. J. Abnorm. Psychol. 2010, 119, 143–150. [Google Scholar] [CrossRef]
- Simpson, T.; Jakupcak, M.; Luterek, J.A. Fear and avoidance of internal experiences among patients with substance use disorders and PTSD: The centrality of anxiety sensitivity. J. Trauma. Stress 2006, 19, 481–491. [Google Scholar] [PubMed]
- Gutner, C.A.; Nillni, Y.I.; Suvak, M.; Wiltsey-Stirman, S.; Resick, P.A. Longitudinal course of anxiety sensitivity and PTSD symptoms in cognitive-behavioral therapies for PTSD. J. Anxiety Disord. 2013, 27, 728–734. [Google Scholar] [CrossRef][Green Version]
- Manzar, M.D.; BaHammam, A.S.; Hameed, U.A.; Spence, D.W.; Pandi-Perumal, S.R.; Moscovitch, A.; Streiner, D.L. Dimensionality of the pittsburgh sleep quality index: A systematic review. Health Qual. Life Outcomes 2018, 16, 89. [Google Scholar] [CrossRef] [PubMed]
| Variable | Mean ± SD or N (%) | Missing (%) |
|---|---|---|
| Age, years | 29.48 ± 8.27 | 0 (0) |
| Sex, female | 96 (77) | 0 (0) |
| Race/Ethnicity | 0 (0) | |
| Asian | 13 (10) | |
| Black | 10 (8) | |
| Hispanic non-white | 12 (10) | |
| Other | 2 (2) | |
| white | 88 (70) | |
| CAPS Total | 29.10 ± 10.59 | 0 (0) |
| Intrusion (Cluster B) | 7.79 ± 3.14 | 0 (0) |
| Avoidance (Cluster C) | 3.48 ± 1.75 | 0 (0) |
| Negative Cognitions (Cluster D) | 10.73 ± 5.15 | 0 (0) |
| Hyperarousal (Cluster E) | 7.47 ± 3.72 | 0 (0) |
| PCL-5 Total | 39.73 ± 13.65 | 0 (0) |
| CD-RISC Total | 25.01 ± 6.99 | 3 (2.4) |
| STAI Trait Total | 49.56 ± 10.95 | 4 (3.2) |
| STAI State Total | 38.77 ± 10.35 | 4 (3.2) |
| SHAPS Total | 27.73 ± 7.05 | 3 (2.4) |
| PSQI Total | 8.19 ± 3.78 | 5 (4) |
| LEC Experienced + Witnessed | 7.36 ± 4.06 | 0 |
| LEC Experienced | 4.48 ± 2.03 | 0 |
| CTQ Total | 58.44 ± 19.44 | 2 (1.6) |
| Sexual Abuse | 10.89 ± 6.41 | 1 (0.8) |
| Physical Neglect | 9.25 ± 4.07 | 1 (0.8) |
| Physical Abuse | 9.41 ± 4.94 | 2 (1.6) |
| Emotional Neglect | 14.41 ± 5.217 | 1 (0.8) |
| Emotional Abuse | 14.51 ± 5.73 | 2 (1.6) |
| FSS Total | 162.66 ± 38.36 | 3 (2.4) |
| ASI Total | 25.56 ± 12.56 | 2 (1.6) |
| BDI Total | 21.16 ± 10.14 | 0 (0) |
| DES Total | 17.23 ± 10.72 | 3 (2.4) |
| Depersonalization and Derealization | 10.04 ± 13.53 | 3 (2.4) |
| Amnesia and Dissociation | 7.41 ± 7.22 | 3 (2.4) |
| DES Absorption and Imagination | 25.51 ± 15.2 | 3 (2.4) |
| Predictors | |
|---|---|
| Clinical Measures | Demographics |
| CAPS for DSM-5 total score (α = 0.87) | Age ^^ |
| CAPS Intrusion (Cluster B) score (α = 0.68) ^^ | Race (white, non-Hispanic) *^ |
| CAPS Avoidance (Cluster C) score (α = 0.61) **^^^^ | Sex (Female) *** |
| CAPS Negative Cognitions (Cluster D) score (α = 0.72) | |
| CAPS Hyperarousal (Cluster E) score (α = 0.63) *****^^ | |
| Self-Report Measures | Psychophysiological Measures |
| PTSD Checklist for DSM-5 Total Score (α = 0.90) ** | Baseline Startle (rSB = 0.96) ****^^^^^^ |
| LEC. Experienced + Witnessed (α = 0.76) *^^ | Dark-Enhanced Startle (rSB = 0.74) ********^^^ |
| LEC Experienced (α = 0.62) | FPS to CS+, Acq block 1 (rSB = 0.79) ***** |
| CTQ total score (α = 0.86) ^ | FPS to CS+, Acq block 2 (rSB = 0.81) ****^^^^^ |
| CTQ Emotional Abuse subscale score (α = 0.89) * | FPS to CS+, Acq block 3 (rSB = 0.75) *****^^ |
| CTQ Emotional Neglect subscale score (α = 0.92) *^^ | FPS to CS−, Acq block 1 (rSB = 0.71) *^^^ |
| CTQ Physical Abuse subscale score (α = 0.87) | FPS to CS−, Acq block 2 (rSB = 0.78) ****^^^ |
| CTQ Physical Neglect subscale score (α = 0.80) ***^^^ | FPS to CS−, Acq block 3 (rSB = 0.67) ****^^^^^ |
| CTQ Sexual Abuse subscale score (α = 0.92) | HR, Baseline (rSB = 0.98) |
| DES total score (α = 0.90) ** | HR, Dark-Enhanced Startle (rSB = 0.98) * |
| DES Absorption subscale score (α = 0.81) * | HR, Dark blocks Dark-Enhanced Startle (rSB = 0.98) |
| DES Amnesia subscale score (α = 0.67) | HR, Light blocks Dark-Enhanced Startle (rSB = 0.98) |
| DES Depersonalization subscale score (α = 0.82) ***** | HR, Acq (rSB = 0.99) *^ |
| Anxiety Sensitivity Index total score (α = 0.88) ** | HRV, Baseline (rSB = 0.94) ** |
| STAI, State Anxiety score (α = 0.93) | HRV, Dark-Enhanced Startle (rSB = 0.96) ^^ |
| STAI, Trait Anxiety score (α = 0.92) * | HRV, Dark blocks Dark-Enhanced Startle (rSB = 0.92) |
| BDI total score (α = 0.89) *^^ | HRV, Light blocks Dark-Enhanced Startle (rSB = 0.91) |
| PSQI total score (α = 0.73) ***^^ | HRV, Acq (rSB = 0.99) |
| CDRISC total score (α = 0.85) | SCR Difference score, Acq block 1 (rSB = 0.71) |
| Fear Survey Schedule total score (α = 0.93) ^ | SCR Difference score, Acq block 2 (rSB = 0.65) ^^ |
| Snaith–Hamilton Pleasure Scale total score (α = 0.89) | SCR Difference score, Acq block 3 (rSB = 0.58) |
| Outcome Measures | |
| FPS to CS+, Early Extinction (rSB = 0.82) | FPS to CS+, Late Extinction (rSB = 0.73) |
| (A) Cross-Validated Training Sample | |||
| Algorithm | MSE | MAE | R2 |
| OLS Linear Regression | 2454.13 | 39.08 | 0.32 |
| Ridge Regression | 1301.99 | 28.02 | 0.49 |
| Lasso Regression | 1325.76 | 28.31 | 0.48 |
| Elastic Net Regression | 1296.41 | 28.30 | 0.50 |
| (B) Holdout Sample | |||
| Algorithm | MSE | MAE | R2 |
| OLS Linear Regression | 3947.74 | 49.80 | −0.29 |
| Ridge Regression | 799.81 | 22.50 | 0.53 |
| Lasso Regression | 794.48 | 21.92 | 0.54 |
| Elastic Net Regression | 726.91 | 21.29 | 0.57 |
| (A) Cross-Validated Training Sample | |||
| Algorithm | MSE | MAE | R2 |
| OLS Linear Regression | 2114.49 | 37.74 | 0.14 |
| Ridge Regression | 987.29 | 24.05 | 0.29 |
| Lasso Regression | 1000.88 | 24.82 | 0.28 |
| Elastic Net Regression | 966.55 | 23.60 | 0.29 |
| (B) Holdout Sample | |||
| Algorithm | MSE | MAE | R2 |
| OLS Linear Regression | 4747.17 | 48.26 | −0.61 |
| Ridge Regression | 2153.86 | 32.49 | 0.25 |
| Lasso Regression | 2037.19 | 32.18 | 0.29 |
| Elastic Net Regression | 2087.37 | 32.33 | 0.28 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lewis, M.W.; Webb, C.A.; Kuhn, M.; Akman, E.; Jobson, S.A.; Rosso, I.M. Predicting Fear Extinction in Posttraumatic Stress Disorder. Brain Sci. 2023, 13, 1131. https://doi.org/10.3390/brainsci13081131
Lewis MW, Webb CA, Kuhn M, Akman E, Jobson SA, Rosso IM. Predicting Fear Extinction in Posttraumatic Stress Disorder. Brain Sciences. 2023; 13(8):1131. https://doi.org/10.3390/brainsci13081131
Chicago/Turabian StyleLewis, Michael W., Christian A. Webb, Manuel Kuhn, Eylül Akman, Sydney A. Jobson, and Isabelle M. Rosso. 2023. "Predicting Fear Extinction in Posttraumatic Stress Disorder" Brain Sciences 13, no. 8: 1131. https://doi.org/10.3390/brainsci13081131
APA StyleLewis, M. W., Webb, C. A., Kuhn, M., Akman, E., Jobson, S. A., & Rosso, I. M. (2023). Predicting Fear Extinction in Posttraumatic Stress Disorder. Brain Sciences, 13(8), 1131. https://doi.org/10.3390/brainsci13081131







