Mental Well-Being of Nursing Staff and Destructive Role of COVID-19 Fear and Perceived Stress
Abstract
1. Introduction
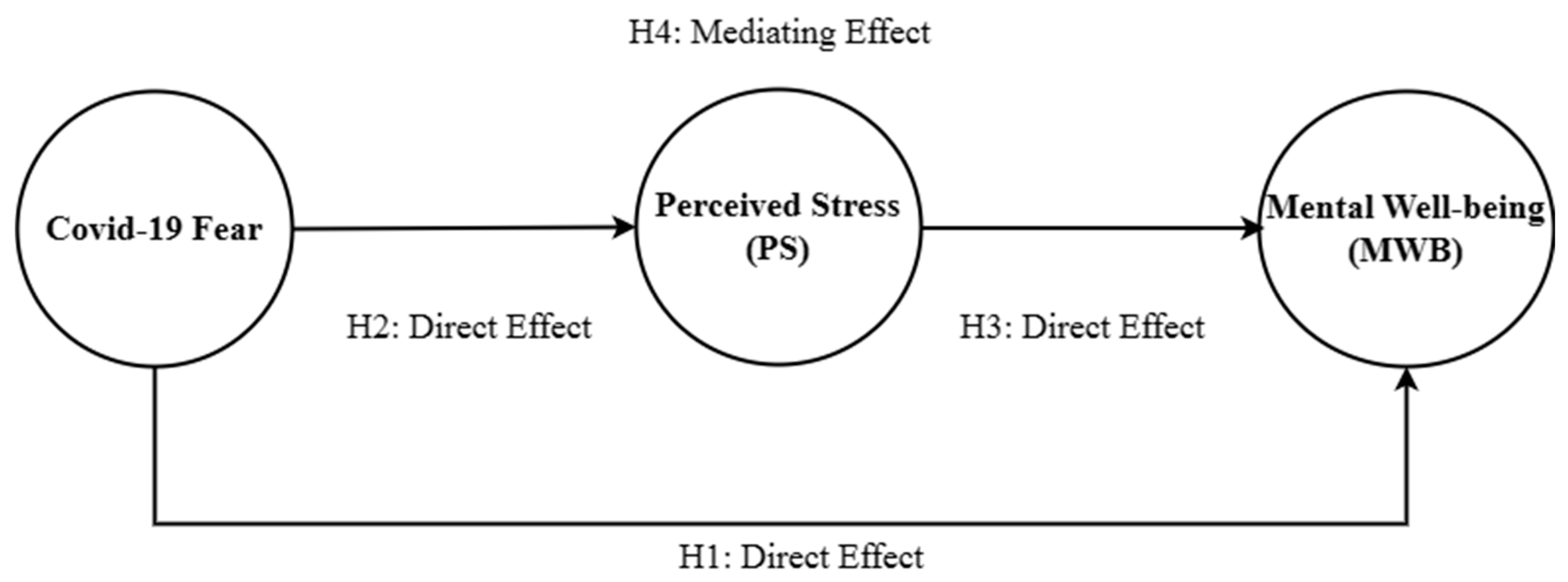
2. Literature Review
2.1. COVID-19 Fear and MWB
2.2. COVID-19 Fear and PS
2.3. Mediating Role of PS
3. Methodology
3.1. Context and Sample
3.2. Study Measures
3.3. Statistical Techniques and Analysis
4. Results
4.1. Reliability and Validity Analysis
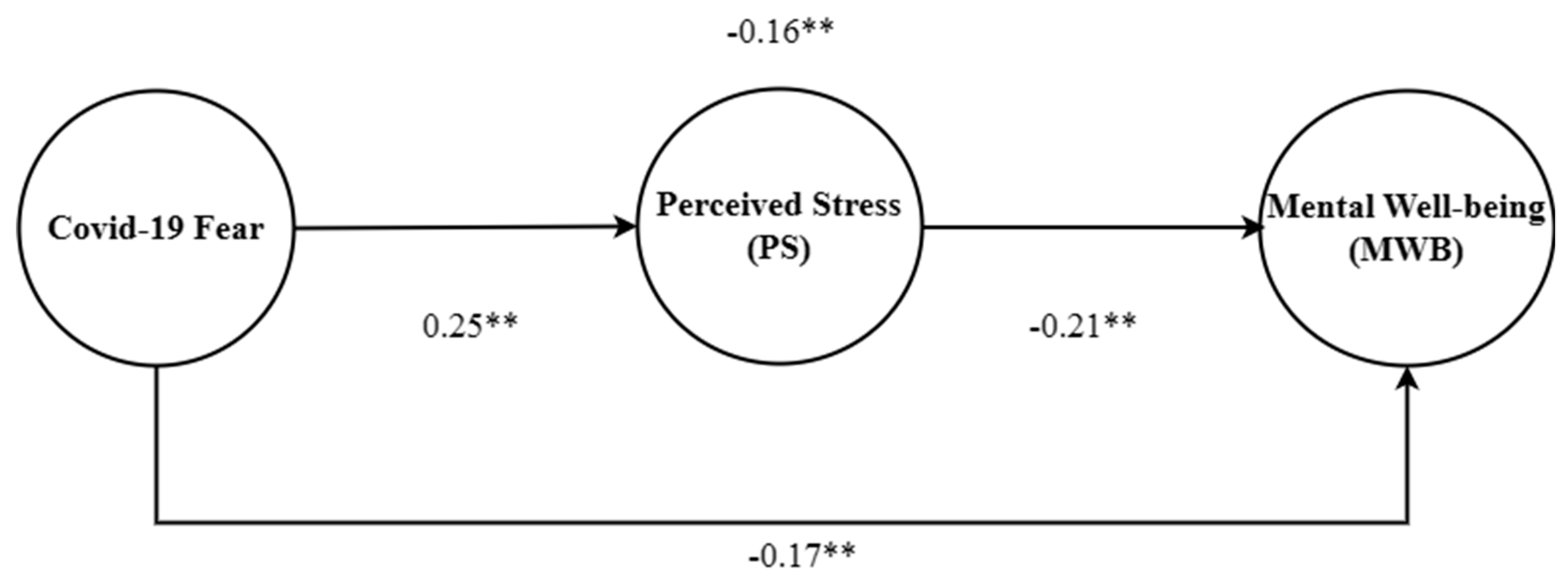
4.2. Hypothesis Testing
5. Discussion
5.1. Theoretical Contribution
5.2. Practical Implications
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Study measures
- COVID-19 Fear
- I am afraid of Coronavirus-19 contamination
- I fill uncomfortable thinking on the coronavirus-19 hazard
- When I am thinking about coronavirus-19 my body lose control
- I become anxious and nervous when I am watching news about coronavirus-19
- I am afraid of high risk to die by coronavirus-19 disease
- I am worried and my slip is affected by the fear of coronavirus-19 contamination
- When I think about getting coronavirus-19 I am devastated
- Perceived Stress
- risk of contagion
- condition of social isolation?
- relationships with your relatives
- relationships with your colleagues
- relationships with your health care professionals
- performance experience
- your love and sexual life and social isolation
- Mental well-being
- Felling optimistic about the future
- Felling useful
- Feeling relaxed
- Interested in other people
- Energy to spare
- Dealing with problem well
- Thinking clearly
- Feeling good about myself
- Feeling close to other people
- Feeling confident
- Able to make up my own mind about things
- Feeling loved
- Interested in new things
- Felling cheerful
References
- Nurunnabi, M.; Almusharraf, N.; Aldeghaither, D. Mental health and well-being during the COVID-19 pandemic in higher education: Evidence from G20 countries. J. Public Health Res. 2020, 9, jphr-2020. [Google Scholar] [CrossRef]
- Sahu, P. Closure of universities due to coronavirus disease 2019 (COVID-19): Impact on education and mental health of students and academic staff. Cureus 2020, 12, 34–45. [Google Scholar] [CrossRef]
- Simou, E.; Koutsogeorgou, E. Effects of the economic crisis on health and healthcare in Greece in the literature from 2009 to 2013: A systematic review. Health Policy 2014, 115, 111–119. [Google Scholar] [CrossRef] [PubMed]
- Ciotti, M.; Ciccozzi, M.; Terrinoni, A.; Jiang, W.C.; Wang, C.B.; Bernardini, S. The COVID-19 pandemic. Crit. Rev. Clin. Lab. Sci. 2020, 57, 365–388. [Google Scholar] [CrossRef] [PubMed]
- Dong, L.; Bouey, J. Public mental health crisis during COVID-19 pandemic, China. Emerg. Infect. Dis. 2020, 26, 1616. [Google Scholar] [CrossRef] [PubMed]
- Lopez, V.; Anderson, J.; West, S.; Cleary, M. Does the COVID-19 pandemic further impact nursing shortages? Issues Ment. Health Nurs. 2022, 43, 293–295. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Intrator, O.; Bowblis, J.R. Shortages of staff in nursing homes during the COVID-19 pandemic: What are the driving factors? J. Am. Med. Dir. Assoc. 2020, 21, 1371–1377. [Google Scholar] [CrossRef] [PubMed]
- Hong, Y.; Cai, G.; Mo, Z.; Gao, W.; Xu, L.; Jiang, Y.; Jiang, J. The impact of COVID-19 on tourist satisfaction with BB in Zhejiang, China: An importance–performance analysis. Int. J. Environ. Res. Public Health 2020, 17, 3747. [Google Scholar] [CrossRef]
- Ip, Y.; Iqbal, W.; Du, L.; Akhtar, N. Assessing the impact of green finance and urbanization on the tourism industry—An empirical study in China. Environ. Sci. Pollut. Res. 2023, 30, 3576–3592. [Google Scholar] [CrossRef]
- Li, M.; Hamawandy, N.M.; Wahid, F.; Rjoub, H.; Bao, Z. Renewable energy resources investment and green finance: Evidence from China. Resour. Policy 2021, 74, 102402. [Google Scholar] [CrossRef]
- Holton, S.; Wynter, K.; Trueman, M.; Bruce, S.; Sweeney, S.; Crowe, S.; Dabscheck, A.; Eleftheriou, P.; Booth, S.; Hitch, D.; et al. Psychological well-being of Australian hospital clinical staff during the COVID-19 pandemic. Aust. Health Rev. 2020, 45, 297–305. [Google Scholar] [CrossRef]
- Chen, Q.; Liang, M.; Li, Y.; Guo, J.; Fei, D.; Wang, L.; He, L.; Sheng, C.; Cai, Y.; Li, X.; et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry 2020, 7, e15–e16. [Google Scholar] [CrossRef] [PubMed]
- Haravuori, H.; Junttila, K.; Haapa, T.; Tuisku, K.; Kujala, A.; Rosenström, T.; Suvisaari, J.; Pukkala, E.; Laukkala, T.; Jylhä, P. Personnel well-being in the Helsinki university hospital during the COVID-19 pandemic—A prospective cohort study. Int. J. Environ. Res. Public Health 2020, 17, 7905. [Google Scholar] [CrossRef]
- Siddique, R.F.; Ahmed, O.; Hossain, K.N. Relationship between the fear of COVID-19 disease and sleep quality: The mediating role of stress. Heliyon 2021, 7, e07033. [Google Scholar] [CrossRef] [PubMed]
- Yousaf, Z.; Nassani, A.A.; Haffar, M. Destructive role of COVID-19 fear on nurses performance: Mediating role of stress. Nurs. Rep. 2021, 11, 955–964. [Google Scholar] [CrossRef] [PubMed]
- Krok, D.; Zarzycka, B.; Telka, E. Risk of contracting COVID-19, personal resources and subjective well-being among healthcare workers: The mediating role of stress and meaning-making. J. Clin. Med. 2021, 10, 132. [Google Scholar] [CrossRef]
- Abbas, S.; Al-Abrrow, H.; Abdullah, H.O.; Alnoor, A.; Khattak, Z.Z.; Khaw, K.W. Encountering COVID-19 and perceived stress and the role of a health climate among medical workers. Curr. Psychol. 2021, 41, 9109–9122. [Google Scholar] [CrossRef]
- Gritsenko, V.; Skugarevsky, O.; Konstantinov, V.; Khamenka, N.; Marinova, T.; Reznik, A.; Isralowitz, R. COVID 19 fear, stress, anxiety, and substance use among Russian and Belarusian university students. Int. J. Ment. Health Addict. 2021, 19, 2362–2368. [Google Scholar] [CrossRef]
- Bakioğlu, F.; Korkmaz, O.; Ercan, H. Fear of COVID-19 and positivity: Mediating role of intolerance of uncertainty, depression, anxiety, and stress. Int. J. Ment. Health Addict. 2021, 19, 2369–2382. [Google Scholar] [CrossRef]
- Zhang, Y.; Mavoa, S.; Zhao, J.; Raphael, D.; Smith, M. The association between green space and adolescents’ mental well-being: A systematic review. Int. J. Environ. Res. Public Health 2020, 17, 6640. [Google Scholar] [CrossRef]
- Tokac, U.; Razon, S. Nursing professionals’ mental well-being and workplace impairment during the COVID-19 crisis: A Network analysis. J. Nurs. Manag. 2021, 29, 1653–1659. [Google Scholar] [CrossRef]
- Cvenkel, N. Mental Health and Well-Being in the Workplace. In Well-Being in the Workplace: Governance and Sustainability Insights to Promote Workplace Health; Springer Nature: Prince George, BC, Canada, 2020; pp. 159–189. [Google Scholar]
- Gray, P.; Senabe, S.; Naicker, N.; Kgalamono, S.; Yassi, A.; Spiegel, J.M. Workplace-based organizational interventions promoting mental health and happiness among healthcare workers: A realist review. Int. J. Environ. Res. Public Health 2019, 16, 4396. [Google Scholar] [CrossRef]
- Bidnurmath, A.S.; Rao, C.R.; Shetty, A.; Kamath, A.; Shetty, L. Epidemiological determinants of mental well-being and quality of life among homemakers with hypertension: A cross-sectional analysis. Indian J. Community Med. Off. Publ. Indian Assoc. Prev. Soc. Med. 2020, 45, 448. [Google Scholar]
- Antolini, F.; Grassini, L. Economic growth and mental well-being in Italian regions. Electron. J. Appl. Stat. Anal. 2020, 13, 498–518. [Google Scholar]
- Cleary, M.; Schafer, C.; McLean, L.; Visentin, D.C. Mental health and well-being in the health workplace. Issues Ment. Health Nurs. 2020, 41, 172–175. [Google Scholar] [CrossRef] [PubMed]
- Diener, E.; Biswas-Diener, R. Will money increase subjective well-being? Soc. Indic. Res. 2002, 57, 119–169. [Google Scholar] [CrossRef]
- Tarkar, P. Impact of COVID-19 pandemic on education system. Int. J. Adv. Sci. Technol. 2020, 29, 3812–3814. [Google Scholar]
- Goetzel, R.Z.; Roemer, E.C.; Holingue, C.; Fallin, M.D.; McCleary, K.; Eaton, W.; Agnew, J.; Azocar, F.; Ballard, D.; Bartlett, J.; et al. Mental health in the workplace: A call to action proceedings from the mental health in the workplace: Public health summit. J. Occup. Environ. Med. 2018, 60, 322. [Google Scholar] [CrossRef]
- Abdin, S.; Welch, R.K.; Byron-Daniel, J.; Meyrick, J. The effectiveness of physical activity interventions in improving well-being across office-based workplace settings: A systematic review. Public Health 2018, 160, 70–76. [Google Scholar] [CrossRef]
- Chaudhury, S.; Samudra, M. COVID-19 lockdown: Psychological effects. Med. J. Dr. DY Patil Univ. 2020, 13, 580–584. [Google Scholar] [CrossRef]
- Escudero-Castillo, I.; Mato-Díaz, F.J.; Rodriguez-Alvarez, A. Furloughs, teleworking and other work situations during the COVID-19 lockdown: Impact on mental well-being. Int. J. Environ. Res. Public Health 2021, 18, 2898. [Google Scholar] [CrossRef]
- Evanoff, B.A.; Strickland, J.R.; Dale, A.M.; Hayibor, L.; Page, E.; Duncan, J.G.; Kannampallil, T.; Gray, D.L. Work-related and personal factors associated with mental well-being during the COVID-19 response: Survey of health care and other workers. J. Med. Internet Res. 2020, 22, e21366. [Google Scholar] [CrossRef] [PubMed]
- Vanhaecht, K.; Seys, D.; Bruyneel, L.; Cox, B.; Kaesemans, G.; Cloet, M.; Van Den Broeck, K.; Cools, O.; De Witte, A.; Lowet, K.; et al. COVID-19 is having a destructive impact on health-care workers’ mental well-being. Int. J. Qual. Health Care 2021, 33, 158–176. [Google Scholar] [CrossRef] [PubMed]
- Petrie, K.; Smallwood, N.; Pascoe, A.; Willis, K. Mental health symptoms and workplace challenges among Australian paramedics during the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2022, 19, 1004. [Google Scholar] [CrossRef] [PubMed]
- Pennington, C.R.; Bates, E.A.; Kaye, L.K.; Bolam, L.T. Transitioning in higher education: An exploration of psychological and contextual factors affecting student satisfaction. J. Furth. High. Educ. 2018, 42, 596–607. [Google Scholar] [CrossRef]
- Gorgenyi-Hegyes, E.; Nathan, R.J.; Fekete-Farkas, M. Workplace health promotion, employee wellbeing and loyalty during COVID-19 Pandemic—Large scale empirical evidence from Hungary. Economies 2021, 9, 55. [Google Scholar] [CrossRef]
- Turale, S.; Meechamnan, C.; Kunaviktikul, W. Challenging times: Ethics, nursing and the COVID-19 pandemic. Int. Nurs. Rev. 2020, 67, 164–167. [Google Scholar] [CrossRef]
- Buheji, M.; Buhaid, N. Nursing human factor during COVID-19 pandemic. Int. J. Nurs. Sci. 2020, 10, 12–24. [Google Scholar] [CrossRef]
- Fofana, N.K.; Latif, F.; Sarfraz, S.; Bashir, M.F.; Komal, B. Fear and agony of the pandemic leading to stress and mental illness: An emerging crisis in the novel coronavirus (COVID-19) outbreak. Psychiatry Res. 2020, 291, 113230. [Google Scholar] [CrossRef]
- Allan, J.; Lawless, N. Stress caused by on-line collaboration in e-learning: A developing model. Educ. Train. 2003, 45, 564–572. [Google Scholar] [CrossRef]
- Foster, K.; Roche, M.; Giandinoto, J.A.; Furness, T. Workplace stressors, psychological well-being, resilience, and caring behaviours of mental health nurses: A descriptive correlational study. Int. J. Ment. Health Nurs. 2020, 29, 56–68. [Google Scholar] [CrossRef] [PubMed]
- Pfefferbaum, B.; North, C.S. Mental health and the COVID-19 pandemic. N. Engl. J. Med. 2020, 383, 510–512. [Google Scholar] [CrossRef] [PubMed]
- Cooper, C.L.; Baglioni Jr, A.J. A structural model approach toward the development of a theory of the link between stress and mental health. Br. J. Med. Psychol. 1988, 61, 87–102. [Google Scholar] [CrossRef]
- Holman, D.; Johnson, S.; O’Connor, E. Stress management interventions: Improving subjective psychological well-being in the workplace. In Handbook of Well-Being; DEF Publishers: Salt Lake City, UT, USA, 2018; Volume 2. [Google Scholar]
- Havaei, F.; Ma, A.; Staempfli, S.; MacPhee, M. Nurses’ workplace conditions impacting their mental health during COVID-19: A cross-sectional survey study. Healthcare 2021, 9, 84. [Google Scholar] [CrossRef] [PubMed]
- Labrague, L.J.; de Los Santos, J.A.A. Fear of COVID-19, psychological distress, work satisfaction and turnover intention among frontline nurses. J. Nurs. Manag. 2021, 29, 395–403. [Google Scholar] [CrossRef] [PubMed]
- Byrom, N.C.; Dinu, L.; Kirkman, A.; Hughes, G. Predicting stress and mental wellbeing among doctoral researchers. J. Ment. Health 2022, 31, 783–791. [Google Scholar] [CrossRef]
- Robinson, L.E.; Valido, A.; Drescher, A.; Woolweaver, A.B.; Espelage, D.L.; LoMurray, S.; Long, A.C.J.; Wright, A.A.; Dailey, M.M. Teachers, stress, and the COVID-19 pandemic: A qualitative analysis. Sch. Ment. Health 2023, 15, 78–89. [Google Scholar] [CrossRef]
- Ozamiz-Etxebarria, N.; Idoiaga Mondragon, N.; Bueno-Notivol, J.; Pérez-Moreno, M.; Santabárbara, J. Prevalence of anxiety, depression, and stress among teachers during the COVID-19 pandemic: A rapid systematic review with meta-analysis. Brain Sci. 2021, 11, 1172. [Google Scholar] [CrossRef]
- Shen, P.; Slater, P. The Effect of Occupational Stress and Coping Strategies on Mental Health and Emotional Well-Being among University Academic Staff during the COVID-19 Outbreak. Int. Educ. Stud. 2021, 14, 82–95. [Google Scholar] [CrossRef]
- Capone, V.; Borrelli, R.; Marino, L.; Schettino, G. Mental well-being and job satisfaction of hospital physicians during COVID-19: Relationships with efficacy beliefs, organizational support, and organizational non-technical skills. Int. J. Environ. Res. Public Health 2022, 19, 3734. [Google Scholar] [CrossRef]
- Ahorsu, D.K.; Lin, C.Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The fear of COVID-19 scale: Development and initial validation. Int. J. Ment. Health Addict. 2020, 20, 1537–1545. [Google Scholar] [CrossRef] [PubMed]
- Foa, E.B.; Ehlers, A.; Clark, D.M.; Tolin, D.F.; Orsillo, S.M. The posttraumatic cognitions inventory (PTCI): Development and validation. Psychol. Assess. 1999, 11, 303. [Google Scholar] [CrossRef]
- Zurlo, M.C.; Cattaneo Della Volta, M.F.; Vallone, F. COVID-19 student stress questionnaire: Development and validation of a questionnaire to evaluate students’ stressors related to the coronavirus pandemic lockdown. Front. Psychol. 2020, 11, 576758. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; Springer Publishing Company: NewYork, NY, USA, 1984. [Google Scholar]
| Construct | Method | Authors | Number of Items |
|---|---|---|---|
| COVID-19 Fear | Adapted | [53] | 7 items |
| MWB | Adapted | [54] | 20 items |
| PS | Adapted | [55,56] | 7 items |
| Items | Cronbach’s Alpha | Factor Loading | Composite Reliability | AVE | |
|---|---|---|---|---|---|
| COVID-19 Fear | 7 | 0.79 | 0.73–0.91 | 0.82 | 0.68 |
| MWB | 20 | 0.76 | 0.70–0.88 | 0.80 | 0.71 |
| PS | 7 | 0.81 | 0.76–0.90 | 0.84 | 0.73 |
| Constructs | Mean | SD | Gender | Age | Experience | Education | COVID-19 Fear | PS | MWB |
|---|---|---|---|---|---|---|---|---|---|
| Gender | 0.87 | 0.84 | 1 | ||||||
| Respondent age | 34 | --- | 0.09 | 1 | |||||
| Work experience | 2.6 | 0.84 | 0.08 | 0.03 | 1 | ||||
| Education level | 2.4 | 0.91 | 0.06 | 0.05 | 0.04 | 1 | |||
| COVID-19 fear | 3.8 | 0.93 | 0.09 | 0.12 | 0.08 | 0.07 | 1 | ||
| PS | 3.5 | 0.91 | 0.05 | 0.09 | 0.04 | 0.05 | 0.32 ** | 1 | |
| MWB | 3.6 | 0.90 | 0.08 | 0.03 | 0.04 | 0.09 | −0.25 ** | −0.23 ** | 1 |
| Paths | Estimates | Standard Error | C.R (t-Value) |
|---|---|---|---|
| COVID-19 fear → MWB | −0.17 | 0.063 | 2.698 ** |
| COVID-19 fear → PS | 0.25 | 0.057 | 4.385 ** |
| PS → MWB | −0.21 | 0.059 | 3.559 ** |
| Specification | Estimate | LL | UL |
|---|---|---|---|
| Standardized direct impact | |||
| COVID-19 fear → MWB | −0.17 | −0.05 | 0.27 |
| COVID-19 fear → PS | 0.25 ** | 0.39 | 0.58 |
| PS → MWB | −0.21 ** | 0.19 | 0.50 |
| Standardized indirect effects | |||
| COVID-19 fear → PS → MWB | −0.16 ** | 0.07 | 0.27 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Binsaeed, R.H.; Grigorescu, A.; Patru, C.L.; Yousaf, Z.; Nassani, A.A.; Patru, L. Mental Well-Being of Nursing Staff and Destructive Role of COVID-19 Fear and Perceived Stress. Brain Sci. 2023, 13, 1047. https://doi.org/10.3390/brainsci13071047
Binsaeed RH, Grigorescu A, Patru CL, Yousaf Z, Nassani AA, Patru L. Mental Well-Being of Nursing Staff and Destructive Role of COVID-19 Fear and Perceived Stress. Brain Sciences. 2023; 13(7):1047. https://doi.org/10.3390/brainsci13071047
Chicago/Turabian StyleBinsaeed, Rima H., Adriana Grigorescu, Ciprian Laurentiu Patru, Zahid Yousaf, Abdelmohsen A. Nassani, and Larisa Patru (Grigorie). 2023. "Mental Well-Being of Nursing Staff and Destructive Role of COVID-19 Fear and Perceived Stress" Brain Sciences 13, no. 7: 1047. https://doi.org/10.3390/brainsci13071047
APA StyleBinsaeed, R. H., Grigorescu, A., Patru, C. L., Yousaf, Z., Nassani, A. A., & Patru, L. (2023). Mental Well-Being of Nursing Staff and Destructive Role of COVID-19 Fear and Perceived Stress. Brain Sciences, 13(7), 1047. https://doi.org/10.3390/brainsci13071047








