Dietary Intake of Flavonoids Associated with Sleep Problems: An Analysis of Data from the National Health and Nutrition Examination Survey, 2007–2010
Abstract
1. Introduction
2. Materials and Methods
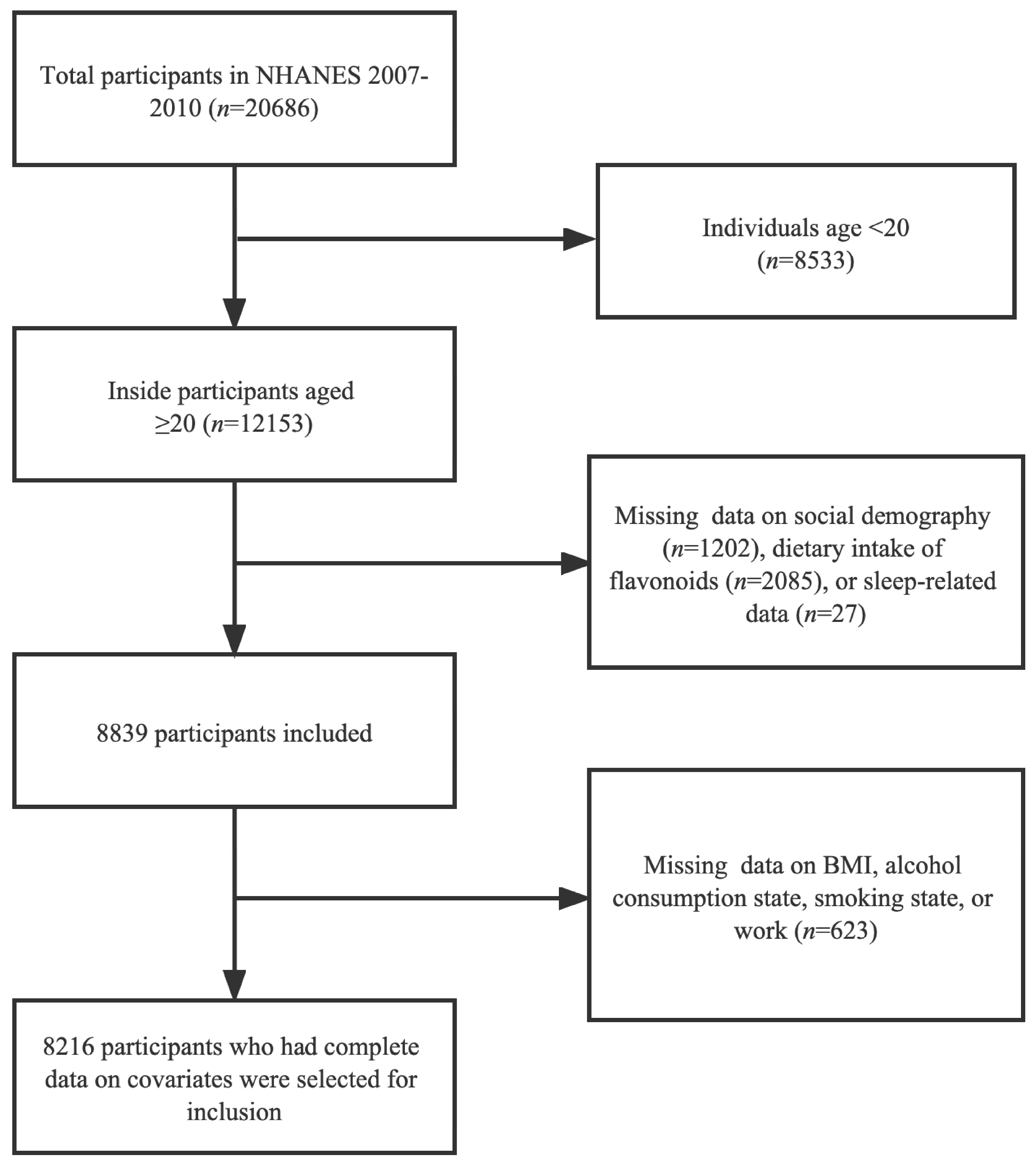
2.1. Study Population
2.2. The Intake of Flavonoids
2.3. Sleep Problems
2.4. Covariates
2.5. Statistical Analysis
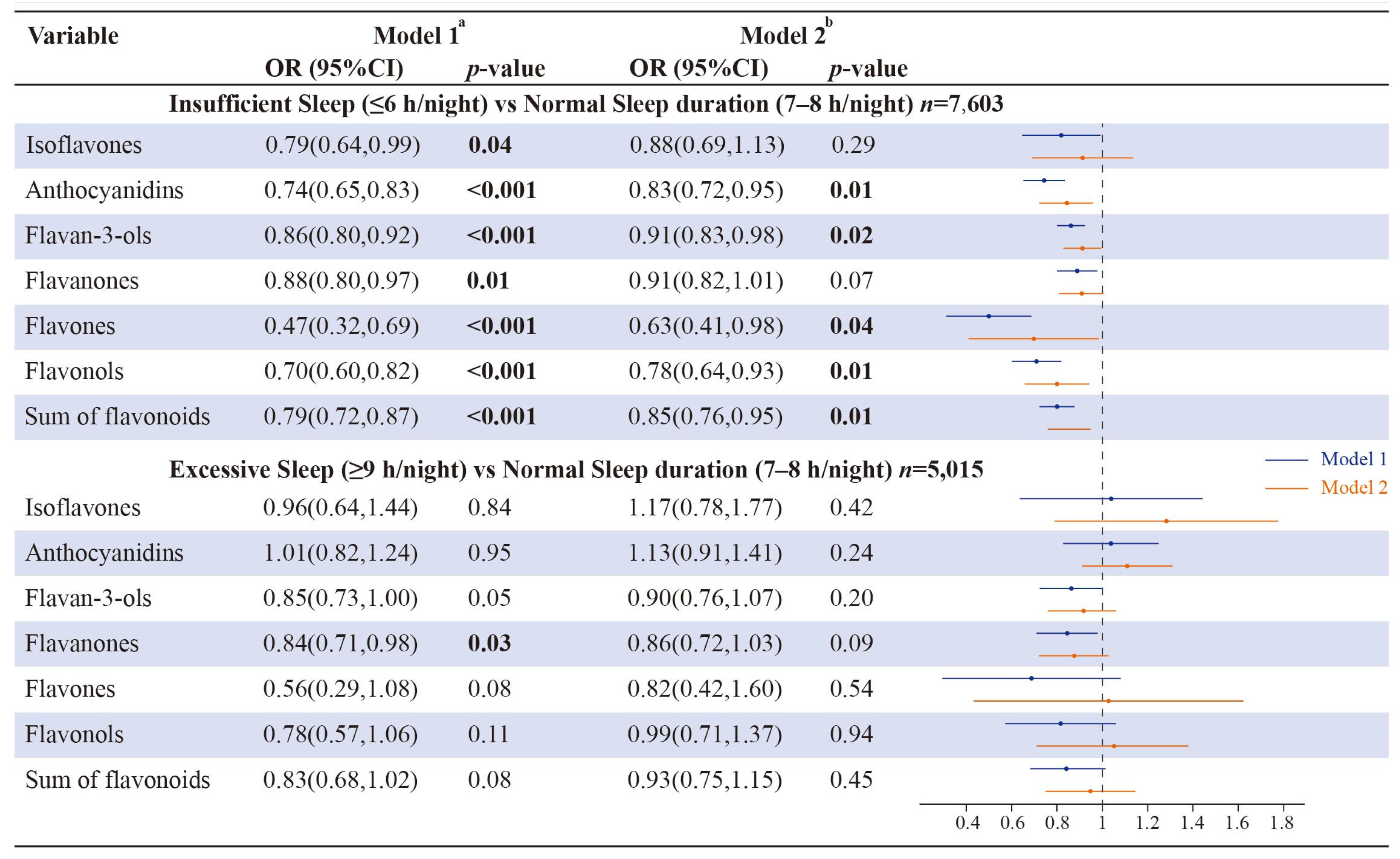
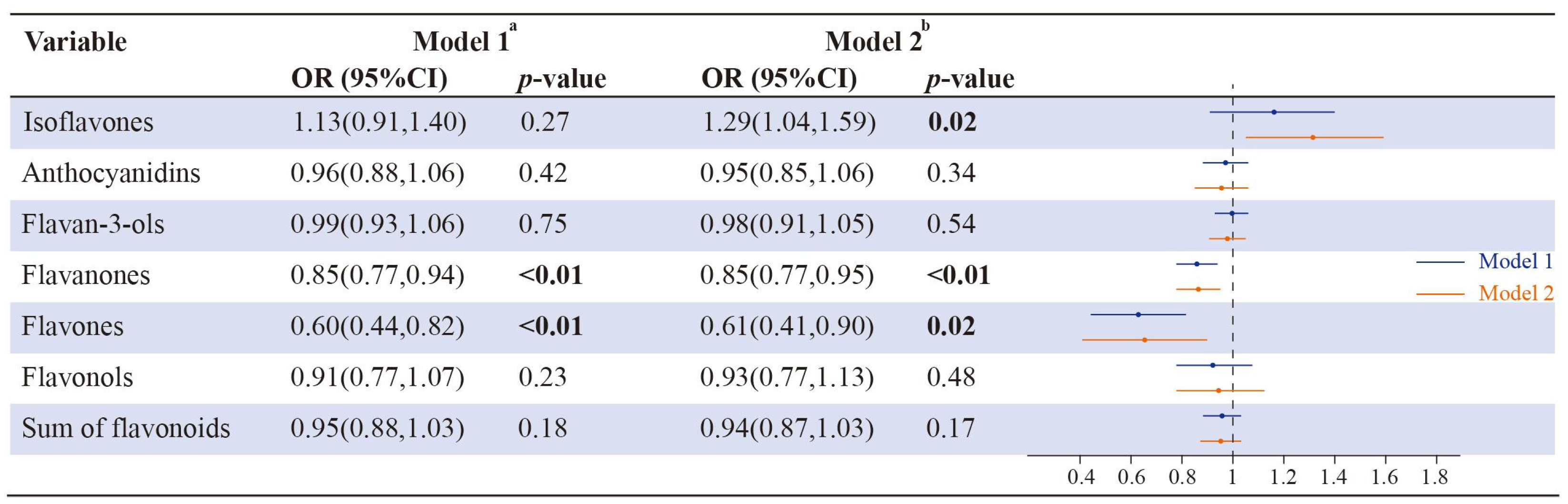
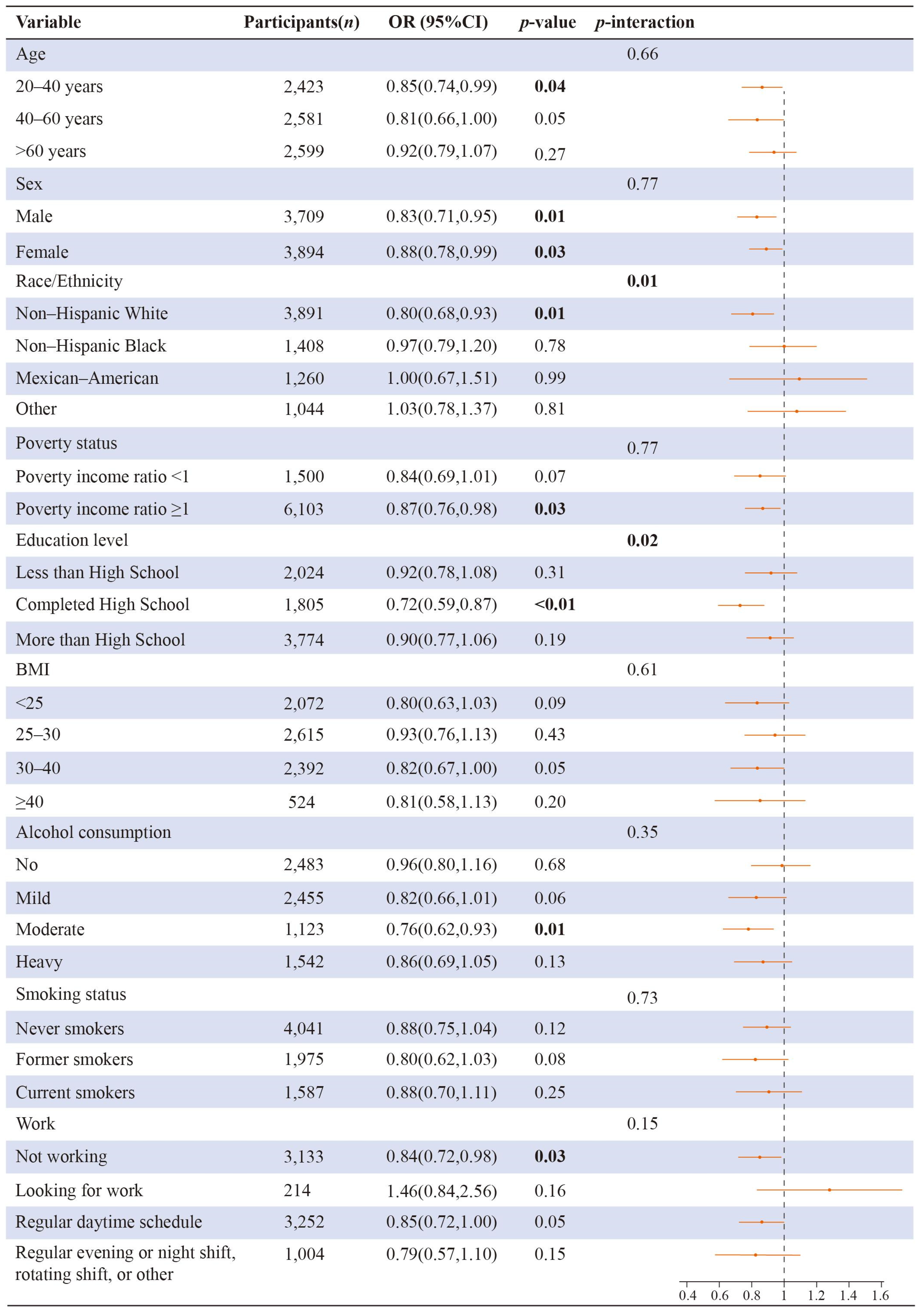
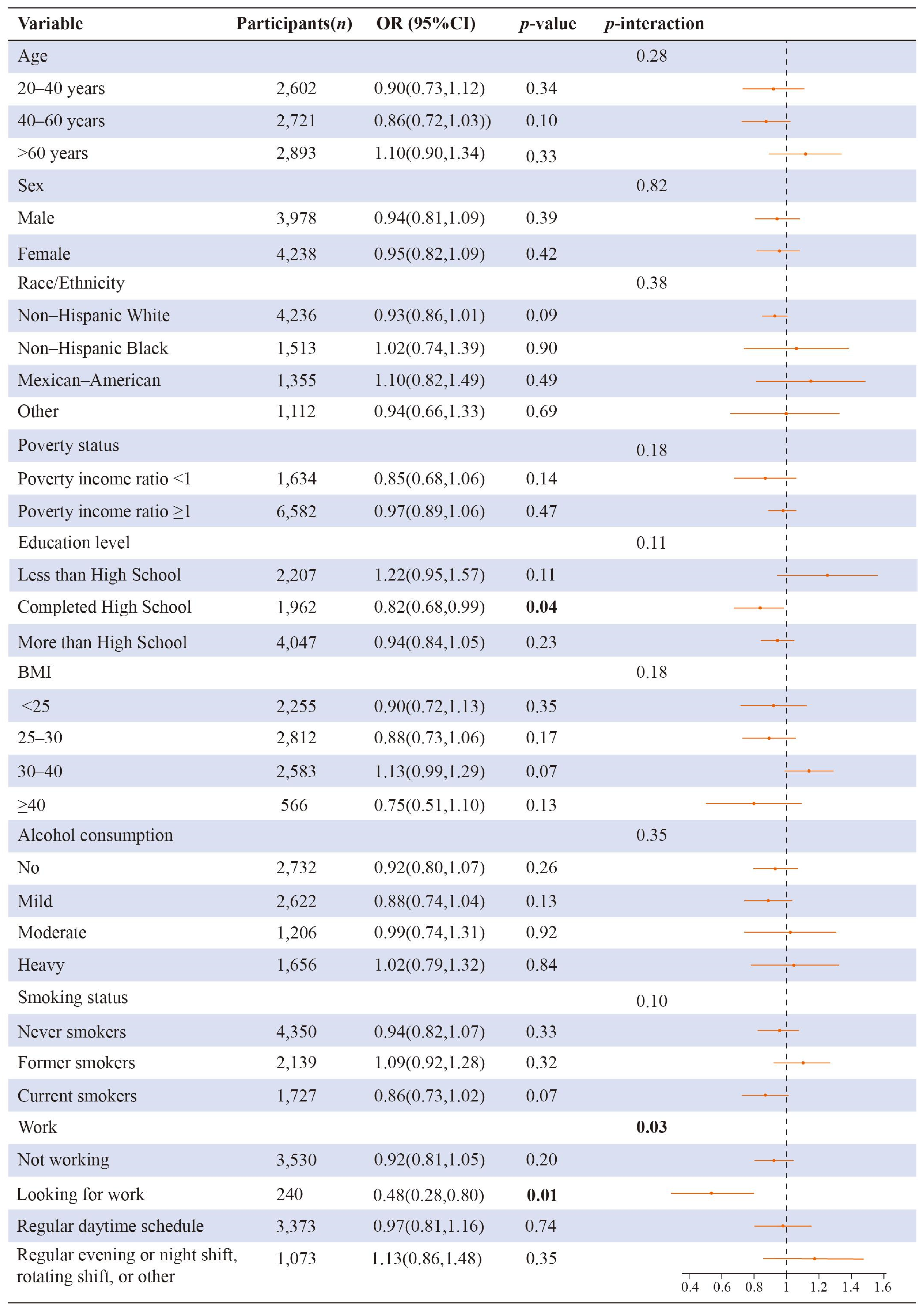
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Milena, K.P.; Latreille, V. Sleep Disorders. Am. J. Med. 2019, 132, 292–299. [Google Scholar] [CrossRef]
- Albqoor, M.A.; Shaheen, A.M. Sleep quality, sleep latency, and sleep duration: A national comparative study of university students in Jordan. Sleep Breath 2021, 25, 1147–1154. [Google Scholar] [CrossRef]
- Grandner, M.A. Sleep, Health, and Society. Sleep Med. Clin. 2017, 12, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Ford, E.S.; Cunningham, T.J.; Croft, J.B. Trends in Self-Reported Sleep Duration among US Adults from 1985 to 2012. Sleep 2015, 38, 829–832. [Google Scholar] [CrossRef]
- Carskadon, M.A.; Barker, D.H. Editorial Perspective: Adolescents’ fragile sleep-shining light on a time of risk to mental health. J. Child Psychol. Psychiatry 2020, 61, 1058–1060. [Google Scholar] [CrossRef]
- Sateia, M.J. International classification of sleep disorders-third edition: Highlights and modifications. Chest 2014, 146, 1387–1394. [Google Scholar] [CrossRef]
- Moloney, M.E.; Ciciurkaite, G.; Brown, R.L. The medicalization of sleeplessness: Results of U.S. office visit outcomes, 2008–2015. SSM Popul. Health 2019, 8, 100388. [Google Scholar] [CrossRef]
- Watson, N.F.; Badr, M.S.; Belenky, G.; Bliwise, D.L.; Buxton, O.M.; Buysse, D.; Dinges, D.F.; Gangwisch, J.; Grandner, M.A.; Kushida, C.; et al. Recommended Amount of Sleep for a Healthy Adult: A Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep 2015, 38, 843–844. [Google Scholar] [CrossRef]
- Levenson, J.C.; Shensa, A.; Sidani, J.E.; Colditz, J.B.; Primack, B.A. The association between social media use and sleep disturbance among young adults. Prev. Med. 2016, 85, 36–41. [Google Scholar] [CrossRef]
- Shankar, A.; Charumathi, S.; Kalidindi, S. Sleep duration and self-rated health: The national health interview survey 2008. Sleep 2011, 34, 1173–1177. [Google Scholar] [CrossRef]
- Cappuccio, F.P.; Miller, M.A. Sleep and Cardio-Metabolic Disease. Curr. Cardiol. Rep. 2017, 19, 110. [Google Scholar] [CrossRef]
- Park, S.; Lee, S.; Kim, Y.; Lee, Y.; Kang, M.W.; Kim, K.; Kim, Y.C.; Han, S.S.; Lee, H.; Lee, J.P.; et al. Short or Long Sleep Duration and CKD: A Mendelian Randomization Study. J. Am. Soc. Nephrol. 2020, 31, 2937–2947. [Google Scholar] [CrossRef]
- Li, C.; Shang, S. Relationship between Sleep and Hypertension: Findings from the NHANES (2007–2014). Int. J. Environ. Res. Public Health 2021, 18, 7867. [Google Scholar] [CrossRef]
- Reutrakul, S.; Van Cauter, E. Sleep influences on obesity, insulin resistance, and risk of type 2 diabetes. Metabolism 2018, 84, 56–66. [Google Scholar] [CrossRef]
- Guo, R.; Shi, A.M.; Deng, L.; Li, L.; Wang, L.C.; Oteng, A.B.; Wei, M.P.; Zhao, Z.H.; Hooiveld, G.; Zhang, C.; et al. Flavonoid-Like Components of Peanut Stem and Leaf Extract Promote Sleep by Decreasing Neuronal Excitability. Mol. Nutr. Food Res. 2022, 66, e2100210. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.; Taylor, A.W.; Zhen, S.; Adams, R.; Appleton, S.; Shi, Z. Soy Isoflavone Intake and Sleep Parameters over 5 Years among Chinese Adults: Longitudinal Analysis from the Jiangsu Nutrition Study. J. Acad. Nutr. Diet. 2017, 117, 536–544.e2. [Google Scholar] [CrossRef]
- Hachul, H.; Brandao, L.C.; D’Almeida, V.; Bittencourt, L.R.; Baracat, E.C.; Tufik, S. Isoflavones decrease insomnia in postmenopause. Menopause 2011, 18, 178–184. [Google Scholar] [CrossRef]
- Singh, B.; Kumar, A.; Malik, A.K. Flavonoids biosynthesis in plants and its further analysis by capillary electrophoresis. Electrophoresis 2017, 38, 820–832. [Google Scholar] [CrossRef] [PubMed]
- Panche, A.N.; Diwan, A.D.; Chandra, S.R. Flavonoids: An overview. J. Nutr. Sci. 2016, 5, e47. [Google Scholar] [CrossRef]
- Maleki, S.J.; Crespo, J.F.; Cabanillas, B. Anti-inflammatory effects of flavonoids. Food Chem. 2019, 299, 125124. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.Y.; Li, Q.; Bi, K.S. Bioactive flavonoids in medicinal plants: Structure, activity and biological fate. Asian J. Pharm. Sci. 2018, 13, 12–23. [Google Scholar] [CrossRef] [PubMed]
- Kicinska, A.; Jarmuszkiewicz, W. Flavonoids and Mitochondria: Activation of Cytoprotective Pathways? Molecules 2020, 25, 3060. [Google Scholar] [CrossRef] [PubMed]
- Chahar, M.K.; Sharma, N.; Dobhal, M.P.; Joshi, Y.C. Flavonoids: A versatile source of anticancer drugs. Pharmacogn. Rev. 2011, 5, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Ren, W.; Qiao, Z.; Wang, H.; Zhu, L.; Zhang, L. Flavonoids: Promising anticancer agents. Med. Res. Rev. 2003, 23, 519–534. [Google Scholar] [CrossRef]
- Yi, Y.S. Regulatory Roles of Flavonoids on Inflammasome Activation during Inflammatory Responses. Mol. Nutr. Food Res. 2018, 62, e1800147. [Google Scholar] [CrossRef]
- Hu, Q.; Liu, Z.; Guo, Y.; Lu, S.; Du, H.; Cao, Y. Antioxidant capacity of flavonoids from Folium Artemisiae Argyi and the molecular mechanism in Caenorhabditis elegans. J. Ethnopharmacol. 2021, 279, 114398. [Google Scholar] [CrossRef]
- Cho, N.; Lee, K.Y.; Huh, J.; Choi, J.H.; Yang, H.; Jeong, E.J.; Kim, H.P.; Sung, S.H. Cognitive-enhancing effects of Rhus verniciflua bark extract and its active flavonoids with neuroprotective and anti-inflammatory activities. Food Chem. Toxicol. 2013, 58, 355–361. [Google Scholar] [CrossRef]
- Ebrahimpour, S.; Zakeri, M.; Esmaeili, A. Crosstalk between obesity, diabetes, and Alzheimer’s disease: Introducing quercetin as an effective triple herbal medicine. Ageing Res. Rev. 2020, 62, 101095. [Google Scholar] [CrossRef]
- Wang, L.; Lee, I.M.; Zhang, S.M.; Blumberg, J.B.; Buring, J.E.; Sesso, H.D. Dietary intake of selected flavonols, flavones, and flavonoid-rich foods and risk of cancer in middle-aged and older women. Am. J. Clin. Nutr. 2009, 89, 905–912. [Google Scholar] [CrossRef]
- Nakajima, A.; Ohizumi, Y. Potential Benefits of Nobiletin, A Citrus Flavonoid, against Alzheimer’s Disease and Parkinson’s Disease. Int. J. Mol. Sci. 2019, 20, 3380. [Google Scholar] [CrossRef]
- Inanami, O.; Watanabe, Y.; Syuto, B.; Nakano, M.; Tsuji, M.; Kuwabara, M. Oral administration of (-)catechin protects against ischemia-reperfusion-induced neuronal death in the gerbil. Free Radic. Res. 1998, 29, 359–365. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.; Smith, J.V.; Paramasivam, V.; Burdick, A.; Curry, K.J.; Buford, J.P.; Khan, I.; Netzer, W.J.; Xu, H.; Butko, P. Inhibition of amyloid-beta aggregation and caspase-3 activation by the Ginkgo biloba extract EGb761. Proc. Natl. Acad. Sci. USA 2002, 99, 12197–12202. [Google Scholar] [CrossRef]
- World Health Organization. Obesity: Preventing and Anaging the Global Epidemic. Report of a WHO Consultation; WHO Obesity Technical Report Series; World Health Organization: Geneva, Switzerland, 2000; Volume 894, pp. i–xii, 1–253.
- Scinicariello, F.; Buser, M.C.; Feroe, A.G.; Attanasio, R. Antimony and sleep-related disorders: NHANES 2005–2008. Environ. Res. 2017, 156, 247–252. [Google Scholar] [CrossRef] [PubMed]
- Wasowski, C.; Marder, M. Flavonoids as GABAA receptor ligands: The whole story? J. Exp. Pharmacol. 2012, 4, 9–24. [Google Scholar] [CrossRef]
- Kim, T.H.; Custodio, R.J.; Cheong, J.H.; Kim, H.J.; Jung, Y.S. Sleep Promoting Effect of Luteolin in Mice via Adenosine A1 and A2A Receptors. Biomol. Ther. 2019, 27, 584–590. [Google Scholar] [CrossRef]
- Li, X.; Tang, Z.; Fei, D.; Liu, Y.; Zhang, M.; Liu, S. Evaluation of the sedative and hypnotic effects of astragalin isolated from Eucommia ulmoides leaves in mice. Nat. Prod. Res. 2017, 31, 2072–2076. [Google Scholar] [CrossRef]
- Xiao, H.B.; Wang, Y.S.; Liang, L.; Lu, X.; Sun, Z.L. Procyanidin B2 from lotus seedpod regulate NO/ADMA/DDAH pathway to treat insomnia in rats. Fundam. Clin. Pharmacol. 2019, 33, 549–557. [Google Scholar] [CrossRef]
- Olonode, E.T.; Aderibigbe, A.O.; Adeoluwa, O.A.; Eduviere, A.T.; Ben-Azu, B. Morin hydrate mitigates rapid eye movement sleep deprivation-induced neurobehavioural impairments and loss of viable neurons in the hippocampus of mice. Behav. Brain Res. 2019, 356, 518–525. [Google Scholar] [CrossRef]
- Wickwire, E.M.; Collop, N.A. Insomnia and sleep-related breathing disorders. Chest 2010, 137, 1449–1463. [Google Scholar] [CrossRef]
- Ford, D.E.; Kamerow, D.B. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA 1989, 262, 1479–1484. [Google Scholar] [CrossRef] [PubMed]
- Zick, S.M.; Wright, B.D.; Sen, A.; Arnedt, J.T. Preliminary examination of the efficacy and safety of a standardized chamomile extract for chronic primary insomnia: A randomized placebo-controlled pilot study. BMC Complement. Altern. Med. 2011, 11, 78. [Google Scholar] [CrossRef] [PubMed]
- Dalgard, O.S.; Mykletun, A.; Rognerud, M.; Johansen, R.; Zahl, P.H. Education, sense of mastery and mental health: Results from a nation wide health monitoring study in Norway. BMC Psychiatry 2007, 7, 20. [Google Scholar] [CrossRef] [PubMed]
- Wright, K.P.; Drake, A.L.; Frey, D.J.; Fleshner, M.; Desouza, C.A.; Gronfier, C.; Czeisler, C.A. Influence of sleep deprivation and circadian misalignment on cortisol, inflammatory markers, and cytokine balance. Brain Behav. Immun. 2015, 47, 24–34. [Google Scholar] [CrossRef] [PubMed]
- Irwin, M.R.; Witarama, T.; Caudill, M.; Olmstead, R.; Breen, E.C. Sleep loss activates cellular inflammation and signal transducer and activator of transcription (STAT) family proteins in humans. Brain Behav. Immun. 2015, 47, 86–92. [Google Scholar] [CrossRef]
- Atrooz, F.; Salim, S. Sleep deprivation, oxidative stress and inflammation. Adv. Protein Chem. Struct. Biol. 2020, 119, 309–336. [Google Scholar] [CrossRef]
- Villafuerte, G.; Miguel-Puga, A.; Murillo Rodríguez, E.; Machado, S.; Manjarrez, E.; Arias-Carrión, O. Sleep Deprivation and Oxidative Stress in Animal Models: A Systematic Review. Oxidative Med. Cell. Longev. 2015, 2015, 234952. [Google Scholar] [CrossRef]
- Aziz, N.; Kim, M.Y.; Cho, J.Y. Anti-inflammatory effects of luteolin: A review of in vitro, in vivo, and in silico studies. J. Ethnopharmacol. 2018, 225, 342–358. [Google Scholar] [CrossRef]
- Parhiz, H.; Roohbakhsh, A.; Soltani, F.; Rezaee, R.; Iranshahi, M. Antioxidant and anti-inflammatory properties of the citrus flavonoids hesperidin and hesperetin: An updated review of their molecular mechanisms and experimental models. Phytother. Res. 2015, 29, 323–331. [Google Scholar] [CrossRef]
- Matenchuk, B.A.; Mandhane, P.J.; Kozyrskyj, A.L. Sleep, circadian rhythm, and gut microbiota. Sleep Med. Rev. 2020, 53, 101340. [Google Scholar] [CrossRef]
- Khan, M.S.; Ikram, M.; Park, J.S.; Park, T.J.; Kim, M.O. Gut Microbiota, Its Role in Induction of Alzheimer’s Disease Pathology, and Possible Therapeutic Interventions: Special Focus on Anthocyanins. Cells 2020, 9, 853. [Google Scholar] [CrossRef]
- Shrestha, S.; Park, J.H.; Lee, D.Y.; Cho, J.G.; Cho, S.; Yang, H.J.; Yong, H.I.; Yoon, M.S.; Han, D.S.; Baek, N.I. Rhus parviflora and its biflavonoid constituent, rhusflavone, induce sleep through the positive allosteric modulation of GABA(A)-benzodiazepine receptors. J. Ethnopharmacol. 2012, 142, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Youdim, K.A.; Dobbie, M.S.; Kuhnle, G.; Proteggente, A.R.; Abbott, N.J.; Rice-Evans, C. Interaction between flavonoids and the blood-brain barrier: In vitro studies. J. Neurochem. 2003, 85, 180–192. [Google Scholar] [CrossRef] [PubMed]
- Youdim, K.A.; Qaiser, M.Z.; Begley, D.J.; Rice-Evans, C.A.; Abbott, N.J. Flavonoid permeability across an in situ model of the blood-brain barrier. Free Radic. Biol. Med. 2004, 36, 592–604. [Google Scholar] [CrossRef] [PubMed]
| Variable | Mean (SE) or n (Weighted Percentage) |
|---|---|
| Age (years) | 46.82 (0.38) |
| BMI (kg/m2) | 28.87 (0.12) |
| Sleep duration (hours) | 6.89 (0.03) |
| Isoflavones (mg) | 1.71 (0.15) |
| Anthocyanidins (mg) | 14.30 (0.92) |
| Flavan-3-ols | 169.72 (9.39) |
| Flavanones (mg) | 13.38 (0.60) |
| Flavones (mg) | 0.99 (0.06) |
| Flavonols (mg) | 18.12 (0.52) |
| Sum of flavonoids (mg) | 218.22 (9.97) |
| Sex | |
| Female | 4238 (51.58) |
| Male | 3978 (48.42) |
| Race/Ethnicity | |
| Non-Hispanic White | 4236 (51.56) |
| Non-Hispanic Black | 1513 (18.42) |
| Mexican-American | 1355 (16.49) |
| Other | 1112 (13.53) |
| Poverty status | |
| Poverty income ratio <1 | 1634 (19.89) |
| Poverty income ratio ≥1 | 6582 (80.11) |
| Education level | |
| Less than High School | 2207 (26.86) |
| Completed High School | 1962 (23.88) |
| More than High School | 4047 (49.26) |
| Alcohol consumption | |
| No | 2732 (33.25) |
| Mild | 2622 (31.91) |
| Moderate | 1206 (14.68) |
| Heavy | 1656 (20.16) |
| Smoking status | |
| Never smokers | 4350 (52.95) |
| Former smokers | 2139 (26.03) |
| Current smokers | 1727 (21.02) |
| Work | |
| Not working | 3530 (42.96) |
| Looking for work | 240 (2.92) |
| Regular daytime schedule | 3226 (39.26) |
| Regular evening or night shift, rotating shift, or other | 1220 (14.85) |
| Sleep disorders | |
| Yes | 2174 (26.46) |
| No | 6042 (73.54) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, L.; Gui, J.; Ding, R.; Yang, X.; Yang, J.; Luo, H.; Huang, D.; Han, Z.; Jiang, L. Dietary Intake of Flavonoids Associated with Sleep Problems: An Analysis of Data from the National Health and Nutrition Examination Survey, 2007–2010. Brain Sci. 2023, 13, 873. https://doi.org/10.3390/brainsci13060873
Wang L, Gui J, Ding R, Yang X, Yang J, Luo H, Huang D, Han Z, Jiang L. Dietary Intake of Flavonoids Associated with Sleep Problems: An Analysis of Data from the National Health and Nutrition Examination Survey, 2007–2010. Brain Sciences. 2023; 13(6):873. https://doi.org/10.3390/brainsci13060873
Chicago/Turabian StyleWang, Lingman, Jianxiong Gui, Ran Ding, Xiaoyue Yang, Jiaxin Yang, Hanyu Luo, Dishu Huang, Ziyao Han, and Li Jiang. 2023. "Dietary Intake of Flavonoids Associated with Sleep Problems: An Analysis of Data from the National Health and Nutrition Examination Survey, 2007–2010" Brain Sciences 13, no. 6: 873. https://doi.org/10.3390/brainsci13060873
APA StyleWang, L., Gui, J., Ding, R., Yang, X., Yang, J., Luo, H., Huang, D., Han, Z., & Jiang, L. (2023). Dietary Intake of Flavonoids Associated with Sleep Problems: An Analysis of Data from the National Health and Nutrition Examination Survey, 2007–2010. Brain Sciences, 13(6), 873. https://doi.org/10.3390/brainsci13060873




