Abstract
On 11 March 2020, a national lockdown was imposed by the Italian government to contain the spread of COVID19 disease. This is an observational longitudinal study conducted at Fondazione Stella Maris (FSM), Italy to investigate lockdown-related emotional and behavioural changes in paediatric neuropsychiatric population. Families having children (1.5–18 years) with neuropsychiatric disorders referred to FSM have been contacted and proposed to fulfil two online questionnaires (General questionnaire and Child Behaviour Check List (CBCL)) to (i) compare (paired two-sample t-tests) the CBCL scores during lockdown with previous ones, and (ii) investigate the influence (multiple linear regression models) of variables such as age, diagnosis grouping (neurological, neurodevelopmental, emotional, and behavioural disorders) and financial hardship. One hundred and forty-one parents fulfilled the questionnaires. Anxiety and somatic problems increased in 1.5–5 years subpopulation, while obsessive-compulsive, post-traumatic and thought problems increased in 6–18 years subpopulation. In the regression models, younger age in the 1.5–5 years subpopulation resulted as “protective” while financial hardship experienced by families during lockdown was related to psychiatric symptoms increasing in the 6–18 years subpopulation. Some considerations, based on first clinical impressions, are provided in text together with comments in relation to previous and emerging literature on the topic.
1. Introduction
In order to contain the spread of SARS-CoV-2 disease, defined as a global pandemic by the World Health Organization (WHO), on 11 March 2020 a national quarantine was imposed by the Italian government until 3rd June. Recent research has shown that these lockdown measures, despite being mandatory to contain the spread of the infectious disease, have had a negative psychological impact on the general population and mental effects have been reported [1]. Previous studies reporting on the effects of quarantine in past epidemics and pandemics such as SARS, Ebola, the 2009 and 2010 H1N1 flu, Middle Eastern respiratory syndrome and equine influenza pandemics, were carried out in adult individuals [2,3,4,5,6,7,8,9,10,11], on healthcare workers [12,13,14,15], in school communities [16,17], on people who had been in contact with infected individuals [18,19], and on adult workers [20,21,22,23]. In these studies, mood deflection and an increase in depression and anxiety are the most frequently reported psychopathological features in the general adult population, while post-traumatic stress disorder (PTSD) was reported in health workers. Less is known about the effects of quarantine and isolation in the children and adolescents. Sprang and Silman 2013 [24] investigated the psychological effects after a pandemic disaster (H1N1, SARS) in children and their parents reporting that the disease containment measures can be harmful for a significant portion of children and their parents. Criteria for PTSD were found in 30% of isolated or quarantined children based on parental reports, and 25% of quarantined or isolated parents, based on self-report measures. Studies on the psychological and psychiatric effects of traumatic events on children and adolescents, such as earthquakes [25], tsunami [26], wars [27], and traumatic life events [28] have been carried out. The assessment measures were the Child Behaviour Checklist (CBCL) and the Youth Self Report (YSR), both worldwide [26,27,28] and in Italy, where these tools were used to evaluate the psychiatric symptoms in children exposed to the earthquake in L’Aquila [25].
Recent studies support the negative psychological impact of the COVID-19 epidemic quarantine on the adult population in China [29]. COVID-19 peritraumatic stress disorder was associated with gender, age, education, occupation and region of respondents. Indeed, females showed significantly higher psychological distress than males, and individuals between 18–30 years and over 60 years presented the highest levels of COVID-19 peritraumatic stress disorder. Moreover, those with a higher level of formal education were more distressed. However, there is little data available on the psychological consequences of lockdown in the paediatric population. In a recent article [30], the authors suggest the deleterious psychological impact of absence of school activity in healthy children and adolescents. Furthermore, the study interestingly showed an association between a greater expression of symptoms and a home delivery birth. Moreover, the eating dimension has been reported as altered in the young adult population of undergraduate students in a recent study [31]. Specifically, the authors report that the level of confinement-related stress increased the risk of problematic eating behaviours among students, especially in those presenting with eating-related concerns. To date, there are not available studies exploring the changes in the psychiatric symptoms in Italian children and adolescents referred for neurological and/or psychiatric disorders. The main aim of this study is to evaluate the possible changes in emotional and/or behavioural symptoms in patients referred to University Hospital IRCCS Fondazione Stella Maris (FSM) in relation to the COVID-19 lockdown (in terms of isolation, change of daily routine, interruption of school attendance and accessibility to health care). This evaluation was conducted by comparing the CBCL [32] assessment scores pre- and during lockdown in patients, ranging in age from 1.5–18 years old, who had presented with a complex neurological and psychiatric diagnosis, meaning with “complex” the high rate of comorbidities in the referred population. Second, the potential influence of variables such as age, diagnosis grouping, financial hardship have been investigated. These data were collected through a General Questionnaire developed in collaboration with the European Academy of Childhood Disability (EACD).
2. Materials and Methods
2.1. Study Design
This observational longitudinal study was conducted by a group of residents in the Department of Child Neurology and Psychiatry in the University of Pisa (Italy), settled in the Foundation Stella Maris (FSM), under the supervision of the Director of the School (RB). FSM is a Research and Care Institute admitting every year more than 3000 children and adolescents for diagnosis and treatment of neurological and psychiatric disorders. Moreover, it hosts the University residency program in Child Neurology and Psychiatry. The referring population is characterised by complex developmental problems, including psychiatric and neurological diseases with frequent comorbidities within and across the diagnostic categories.
In order to detect the potential emotional and behavioural changes in this population, the CBCL tool was uploaded on a devoted online platform (“REDCap”, Research Electronic Data Capture, Vanderbilt University, Nashville, TN, USA). The additional General Questionnaire set-up in collaboration with EACD was distributed to collect further environmental data.
The inclusion criteria for the study were as follows; (i) age under 18 years; (ii) presence of a neuropsychiatric disorder assessed in FSM by a multidisciplinary team (neurologist and psychiatrist, psychologist, speech therapist, educational therapist, and child therapist) and through the administration of standardised measures such as K-SADS-PL [33], ADOS-2 [34], ADI-R [35], CBCL [32] etc.; and (iii) availability of CBCL scores obtained before the lockdown between September 2019 and February 2020.
The families that matched the inclusion criteria were contacted by the residents by telephone and informed about the study. Those who were willing and keen to participate received instructions by e mail to complete the two questionnaires. Follow-up contacts with families in the enrolment-window were made and families who asked for help in the completion of the forms were assisted by phone. Recruitment lasted two weeks (from the 20 April to the 4 May), while lockdown was stopped by the Government on the 18 May). The study was approved by the Tuscany Paediatric Ethics Committee (N. 95/20- 20.04.2020).
2.2. Measures
2.2.1. The General Questionnaire
The General Questionnaire was completed anonymously by the enrolled families. The same questionnaire was distributed in a further European study—“EACD COVID-19 Survey-Families”—which was conducted in parallel and promoted by the same association to evaluate the impact of the COVID-19 emergency on all European families with children or adolescents with neuropsychiatric disorders. Different aspects of the daily life of young patients and their families during the lockdown were investigated (EACD COVID-19 SURVEYS—INITIAL REPORT (2020) http://edu.eacd.org/eacd-covid-19-surveys-initial-report).
2.2.2. Child Behaviour Check List (CBCL)
The Child Behaviour Check List 1.5–5 (CBCL 1.5–5) is a parent-report used to analyse behavioural symptoms in pre-schoolers. It presents 100 items describing the presence and the frequency of a specific behaviour through a three-point Likert scale (0, not true; 1, sometimes true; 2, very true). The CBCL 1.5–5 consists of 3 summary scales, 7 syndrome scales, 5 DSM-Oriented Scales, and 1 Stress Scale. The first are represented by Internalising, Externalising and Total Problems, the second by Emotionally Reactive, Anxious/Depressed, Somatic Complaints, Withdrawn, Sleep Problems, Attention Problems, and Aggressive Behaviour, the third by Affective Problems, Anxiety Problems, Pervasive Developmental Problems, Attention Deficit/Hyperactive Problems and Oppositional Defiant Problems.
The Child Behaviour Check List 6–18 is a 113-item parent report is used to assess child and adolescent psychopathology. Similarly, to the CBCL1.5–5, each item is rated on a three-point Likert scale. The items are categorised in 8 syndrome scales (anxious/depressed, withdrawn/depressed, somatic complaints, social problems, thought problems, attention problems, rule-breaking behaviour, and aggressive behaviour), 6 DSM-Oriented scales (Affective Problems, Anxiety Problems, Somatic Problems, Attention Deficit/Hyperactivity Problems, Oppositional Defiant Problems Conduct Problems), and 3 scales Scored Using T Scores for ASEBA Standard (Sluggish Cognitive Tempo, Obsessive-Compulsive Problems, Post-traumatic Stress Problems). The Syndrome Scale items are also classified in three summary scales: Internalising Problems, Externalising Problems and Total Problems.
In both CBCL (½–5 and 6–18) the score is considered clinically significant when the T-score is 63 or above for summary scales and 70 or above for syndrome, DSM-Oriented Scales and scales scored using T Scores for ASEBA Standard, while it is in the border clinical range when the value is between 60 and 63 for summary scales and between 65 and 70 for syndrome, DSM-Oriented Scales and scales Scored Using T Scores for ASEBA Standard. Values under 60 for the summary scales or under 65 for other scales are considered not clinically significant.
2.3. The Online Platform: REDCap
When the Italian Government recommended the public to isolate themselves at home and minimise face-to-face interactions, potential respondents were contacted by phone and invited to complete questionnaires in Italian. The survey was uploaded and shared on the REDCap online platform and the link to the electronic survey was distributed by means of invitations via e-mails. The survey included an introductory section describing the background and the aims of the study and information ethics for participants that could be downloaded at any time. All parents provided electronic informed consent. During the informed consent process, participants were informed that all data would be used for research purposes only. Respondents were also able to withdraw participation and abandon the survey at any stage before the submission process.
2.4. Statistical Methods
In order to extrapolate the emotional and behavioural changes, measures of T-Scores for the subscales included in the CBCL at two time-points (pre- and during lockdown) were obtained and compared through paired two-sample t-tests, whose use is justified through the central limit theorem.
To further investigate the differences between pre- and during lockdown T-Scores and break down the different sources of variability, we adopted a multiple linear regression model in which the difference in T-Scores (pre- and during) was used as response variable.
The covariates considered in the models are the weekly average hours of treatment pre-lockdown declared by the respondent, the age in years of the patient, the parents’ financial hardship during the lockdown period, and three not mutually exclusive diagnosis groupings: “Neurological Disorders”, “Emotional and Behavioural Disorders”, and “Neurodevelopmental Disorders”. In particular, in the present study the Neurological Disorder grouping includes patients presenting with cerebral palsy and epilepsy; The “Emotional and Behavioural Disorders” grouping includes patients presenting with generalised anxiety, mood disorders, obsessive compulsive and feeding disorders; finally, the Neurodevelopmental Disorders (NDD) grouping includes patients presenting with autism spectrum disorder, attention deficit and hyperactivity disorder, motor coordination disorder, intellectual disability, language/learning disorder. Due to the complex diagnosis of the patients enrolled in the study, a patient could simultaneously belong to one, two or three groupings. More specifically, the models were composed as follows,
μdiff = β0 + β1 p1 + β2 p2 + β3 p3 + βh hours + βa age + βf financial
In this model, the response μdiff is the difference in a specific T-Score among the CBCL subscale scores before and after COVID-19 hit; p1, p2 and p3 are, respectively, “Neurological Disorders”, “Emotional and Behavioural Disorders”, and “Neurodevelopmental Disorders”; hours indicates the weekly average hours of treatment pre-lockdown declared by the respondent; age is the age (in years) of the patient; financial is a binary variable stating whether the family of the patient indicated that they experienced financial hardship during the lockdown period. Covariates p1, p2, p3, and age were obtained having studied the diagnoses in the IRCCS FSM clinical database. Covariates hours and financial were obtained from the EACD Questionnaire.
Sixteen differences in CBCL T-Scores were investigated as response variables for the 1.5–5 age group, while twenty differences were analysed for the 6–18 age group. Since the response is always calculated “pre- vs. during”, a negative difference indicates an increase in T-Score. Given this, covariates for which the effect has a negative sign are associated with an increase in T-Score and thus a worsening in the patient’s conditions, while the opposite is true for positive coefficients.
In the following section, coefficients and results with p-value lower than the conventional threshold for statistical significance of 0.05 will be underlined. Moreover, for an explorative purpose due to the size of the sample with regards to the magnitude of the measured effects, and due to the nature of the sample itself, results with p < 0.1 will also be highlighted.
3. Results
3.1. Enrollment and Population Description
Seven-hundred families were contacted by the residents of the School of Developmental Neuropsychiatry, University of Pisa. Six-hundred-and-twenty-one families filled out 75% of the EACD questionnaire, but only 494 completed the measures. Among these, 205 started the CBCL questionnaire according to the age of the patient and 201 completed it.
Only the fully compiled CBCL questionnaires were considered for the statistical comparison. Among the 201 CBCL questionnaires completed, 156 patients had had a previous CBCL assessment in our Institute in the previous six months, but 15 of these changed the CBCL questionnaire according to the age range. Consequently, the present paper includes the results of 141 subjects that filled in CBCL questionnaires useful for the comparison with those available in pre-lockdown. More specifically, 61 were completed by the parents of patients ranging in age from 1.5 to 5 years and 80 by parents of patients from 6 to 18 years old (Figure 1). As EACD questionnaire has been delivered also via Web, 47 families on our platform have completed EACD and CBLC questionnaires, but cannot be enrolled in this longitudinal study since they are not FSM patients and have not a previous CBCL assessment. These data will be used for other ongoing studies.
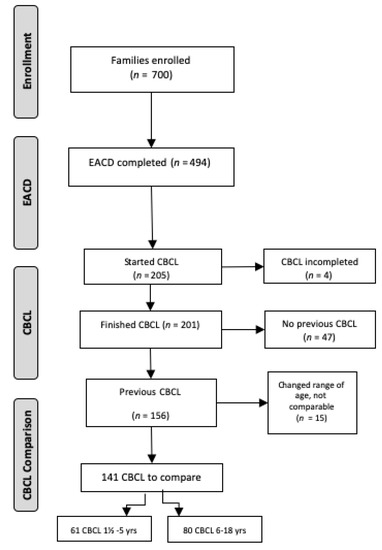
Figure 1.
Patients Recruitment Flowchart. Abbreviations: EACD = European Academy of Childhood Disability; CBCL = Child Behaviour Checklist.
The sample 1.5–5 was composed of 8 females and 53 males. Forty-eight subjects presented overlaps in the three diagnosis groupings: 1 patient presented both Neurological and Emotional and Behavioural Disorders, 3 presented Neurological and Neurodevelopmental Disorders, and 30 presented both Neurodevelopmental and Emotional and Behavioural Disorders. Two patients presented Neurological Disorders and 25 presented with Neurodevelopmental Disorders. None of the children in this sample presented only Emotional and Behavioural Disorders (Figure 2a) or the co-occurrence of the all the three groups.
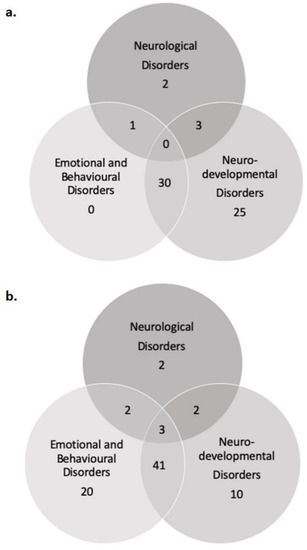
Figure 2.
The distribution of patients is here shown across Diagnosis grouping for (a) CBCL—1.5/5 and (b) CBCL—6/18.
Sixteen females and 64 males constituted the 6–18 sample. Overlapping in diagnosis groupings emerged in 48 patients: 2 patients presented Neurological Disorders and Emotional and Behavioural Disorders, 2 patients presented Neurological and Neurodevelopmental Disorders, 41 presented Neurodevelopmental and Emotional and Behavioural Disorders. Three patients fit in all three groupings. Two patients presented Neurological Disorders, 20 presented Emotional and Behavioural Disorders and 10 patients presented Neurodevelopmental Disorders (Figure 2b).
3.2. Pre- vs. During Lockdown Comparisons
The means of the CBCL subscales T-Scores of all the patients were compared using t-tests. For the population aged 1.5–5, significant negative differences (that is a worsening in the clinical features) were observed in the Syndrome Scale Score in the Somatic Complaints (p < 0.1) and in the DSM-Oriented Anxiety Scale (p < 0.05). For the CBCL 6–18 questionnaire, a significant negative difference (that is a worsening) was observed in the Syndrome Scale Score Thought problems (p < 0.05) as well as in the Obsessive scale (p < 0.05) and the PTSD scale (p < 0.1). All the other CBCL domains in both forms did not show significant differences. A descriptive graphical representation of the significant T-Scores is given in Figure 3a,b.
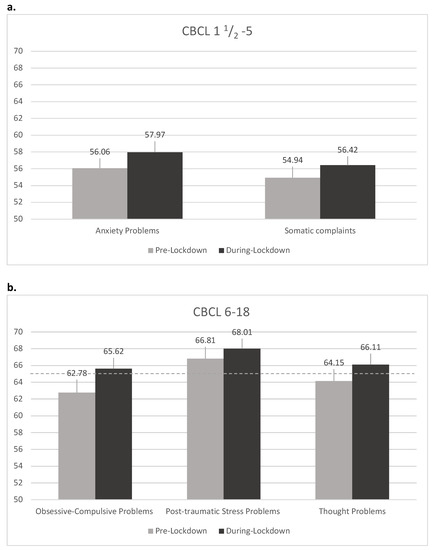
Figure 3.
Student’s t–test results: (a) CBCL 1.5–5 years subpopulation. Graphical representation of the means in significantly different pre- and during lockdown T-Scores in the CBCL 1.5–5. The segment on top of each bar represents the upper half of the 90% confidence interval, while the dashed line indicates the clinical score for the subscales; (b) CBCL 6–18 years subpopulation. Graphical representation of the means in significantly different pre- and during lockdown T-Scores in the CBCL 6–18. The segment on top of each bar represents the upper half of the 90% confidence interval, while the dashed line indicates the clinical score for the subscales.
The results obtained from the fitting of the multiple linear regression models, as in (1) in the statistical analysis section, are showed in Table 1 and Table 2, respectively, for CBCL 1.5–5 and CBCL 6–18. A detailed interpretation of the results can be found in the discussion section.

Table 1.
Regression models results (1.5–5 years).

Table 2.
Regression models results (6–18 years).
4. Discussion
To the best of our knowledge, this is the first study exploring emotional and behavioural changes during the COVID-19 lockdown in an Italian paediatric population with neurological and psychiatric disorders, using the CBCL as assessment measure. During the lockdown, the clinical activity of IRCCS Fondazione Stella Maris was strongly limited due to the emergency situation, but the residents immediately sought to guarantee via telephone contact whenever required. The quasi overnight change in the work routine created a unique opportunity to study the effects of this worldwide situation could have on children with neurological and/or psychiatric disorders.
It is known that lockdown is a potentially traumatic experience due to separation from relatives and friends, loss of freedom, uncertainty over disease status, and boredom. It can determine dramatic effects in the general population (as reviewed in [1]), while the consequences could even be worse in those families with severe concerns about the health of their children. As recently reviewed in [36], the COVID-19 outbreak was a particularly challenging time in terms of psychiatric symptoms occurrence, somatic symptoms, sleep disturbances for children and adolescents with special needs or disabilities, and low socioeconomic status [36].
Results from the current study shed light on difficulties experienced in our neuropsychiatric population, exploring the changes reported by their parents during this extreme social experience, by comparing pre-lockdown and during lockdown CBCL scores.
It is important to highlight that the population involved in the study is potentially more vulnerable than other neuropsychiatric patients as they present with complex comorbid diagnosis and are referred to the largest Developmental Neuropsychiatric Institute in Italy (FSM).
Despite these difficult conditions, the parents’ willingness to participate to the study and to explore behavioural and/or emotional changes during the lockdown was commendable and greatly appreciated, although some parents had difficulty completing the questionnaires as it was time-consuming. Moreover, the stressful situation experienced by families in terms of isolation, the closure of schools, worries over health and finances, loss of grandparents’ support, need to quickly adapt to “smart-working” at home, and ban on going outdoors to reach open spaces compounded the situation.
Furthermore, it is important to underline that the experience of specific worries about their child’s mental health increases the parents’ risk of depression, ruminative thought, anxiety, or other types of psychological distress, as reported in parents of children with autism spectrum disorders by [37]. Regarding families with children with autism spectrum disorders, stressful COVID-19-related consequences have also been recently reported by Colizzi and colleagues, using an online survey [38]. Despite the non-completion of the questionnaires by some parents, our research has managed to study a heterogeneous and complex population, ranging in age from 2 to 18 years, with neurological and psychiatric issues.
As far as the pre-school subgroup is concerned, significant worsening was found in the Syndrome Scale Score in the Somatic Complaints (p < 0.1) and in the DSM-Oriented Anxiety Scale (p < 0.05). This is not surprising, considering previous research that correlated anxiety disorders with somatisation in the pre-schooler population [39]. However, to the best of our knowledge, no data in this age population was analysed in COVID-19 studies, even if an increase in anxiety symptoms was reported in older children in several recent studies [40,41]. These results should be considered in a broader perspective, taking into account the relationship between the child and his/her caregiver and the child’s symptoms, as younger children are more vulnerable to maternal mental illness. As highlighted by the National Research Council and Institute of Medicine Committee (2009) [42], parental depression has been consistently found to be associated to early signs of “difficult” temperament in children, insecure attachment, emotional dysregulation, reduced cognitive and academic performances, cognitive vulnerability to depression, poor interpersonal functioning, and psychobiological dysfunction.
Besides, young children could be more sensitive to the spill over stress contagion as highlighted by [43] referring to COVID-19: the stress of increased work demands or financial burdens are likely to “spill over” into parents’ responsibilities as caregivers, and compromise their ability to provide sensitive and responsive care. Furthermore, the stress that children might experience as a result of changes in routine, such as being at home rather than at school, may “spill over” into how they interact with their siblings and parents. In a recent study carried out during the lockdown [44], both caregivers for children and adults with intellectual disabilities presented major levels of defeat/entrapment, anxiety, and depression which could affect the child–parent relationship.
As far as the schoolers subgroup is concerned (6–18 CBCL questionnaire), a significant negative difference was observed in the Syndrome Scale Score Thought problems, (p < 0.05), in the Obsessive scale (p < 0.05) and the PTSD scale (p < 0.1), thus meaning a clinical worsening during lockdown.
In a comprehensive review of studies conducted in children and adolescents during the COVID-19 lockdown [36], anxiety and depression were reported in most of the studies, while another study [45], exploring mental health in the community, reported a general intensification of the psychopathology, specifically in 2% of their population. Regarding the increase of Obsessive-Compulsive symptoms, this is in line with a previous study [46], which reported in children and adolescents during COVID-19 pandemic a worsening of obsessive compulsive disorder (OCD), namely in terms of contamination obsessions and cleaning/washing compulsions, using Children’s Yale-Brown Obsessive Compulsive (CY-BOCS [47]) and Clinical Global Impression-Severity Scale. It is of note that levels of Sensitivity and Specificity of Obsessive-Compulsive Scale from the CBCL were previously analysed and the results were found to be fairly high, demonstrating high diagnostic power according to favourable Positive-Predicted-value and Negative-Predictive-Value. A worsening in PTSD symptoms after COVID-19 hit has also been reported in a sample of young Chinese people with no neuropsychiatric issues [48]. The validity and factor structure of the CBCL-derived measures of trauma symptoms (PTSD) are supported in the literature, and the scale is useful to study trauma symptomatology in a sample of neglected children.
As far as the results of the regression models in this study, it has been investigated the effect on the changes between pre- and during lockdown scores in the CBCL scales of the variables financial hardship, age, weekly average hours of treatment pre-lockdown, and the previously defined diagnostic groupings. Considering the sub-population aged 1.5–5 years, even though some statistically significant effects show up in different regressions, no specific patterns seem to emerge in the comparison between the different diagnostic categories.
Almost all effects for the control variable age are negative, showing a tendency for the younger children in the 1.5–5 sample that could be interpreted as a better reaction to the lockdown. More sporadically within the Emotional and Behavioural grouping the dimension of “stress problems” and “pervasive developmental problems” appear significantly worsened (Table 1); not surprisingly, this finding could be related in this group to the coexistence of the Emotional and Behavioural disorder with Neurodevelopmental disorder (Figure 2a).
On the other hand, “anxiety problems” resulted increased in Neurological disorders grouping, possibly due to the familiar distress for the management of the organic issues (Table 1).
Regarding the sub-population aged 6–18 years, all estimated effects for “Emotional and Behavioural Disorders” have a positive sign, six of them (in the regressions for Internalising, Externalising, Total Problems, Affective, DSM ADHD and Attention difference in T-Scores) being statistically significant. This surprisingly suggests that there was tendency for a better reaction to the lockdown in these patients compared to those patients who do not present psychiatric problems (namely patients with neurological and/or neurodevelopmental disorders), controlling for all other factors. Note that, on average, patients with Emotional and Behavioural Disorders had higher starting T-Scores than the other patients in our sample, and thus a reduction in T-Scores for those patients could be interpreted as a regression of the scores of those patients towards the mean. Based on first clinical impressions, it can be speculated that this “protective effect” of having psychopathological diagnosis may be linked to the reduction of environmental requests during the lockdown situation. For example, the interruption of school and switch to online didactics could impact positively in the attention dimension [49]. Furthermore, due to the low exposure to competition and comparison with pairs, externalising and affective problems could have been reduced.
In addition, the results of the 6–18 CBCLs also show that financial hardship experienced by the family significantly worsened the following CBCL subscales; Total Problems, specifically Internalising Problems, the PTSD scale, the Obsessive-compulsive scale, and, in the Syndrome Scale Scores, the Withdrawn and Somatic problems subscales. This finding is in line with previous evidence [50], indicating that economic disadvantages were significantly associated with children’s internalising and externalising problems. Furthermore, a recent narrative review paper, focused on the COVID-19 pandemic burden on child and adolescent mental health [51], particularly underlined the string impact of financial losses. To our knowledge our results show scientific evidence regarding the crucial role of financial issues in managing a stressful family situation, especially in families with children and adolescents presenting with complex neuro-psychiatric problems, particularly regarding internalising problems.
Sporadically, it also appears that oppositional defiant dimension present high score during lockdown time when compared to Neurodevelopmental Disorders grouping, probably due to the loss of outdoor opportunities and the great amount of restrictions.
In the current study there are some limitations which are worthy of discussion, namely a possible selection bias. Indeed, only 201 out of the 700 families firstly contacted fully completed the two questionnaires. The limited number of participants that completed the CBCL could be due to the difficulties the families had understanding the online platform, where some instructions were written in English (an Italian translation was not possible for the software restrictions), and to the difficulty of completing a one hour questionnaire online. In addition, some families, who were contacted several times and were asked to complete the questionnaires, reported great difficulty in managing stressful home situation (e.g., taking care of children and adolescents on their own, working long hours at home). Moreover, the relatively low response rate could be a potential source of bias, since the parents that were able to fill out the whole questionnaire could be representative of a specific subpopulation with more facilities (for example open spaces, grandparents living with the families). Nonetheless, the results seem to be interesting for their internal validity. Gender bias represents another potential factor that has to be considered thus in literature the “sex biological variable” has been argued in neuropsychiatric field (e.g., [52]). In the current sample, the great majority of patients are male, and the small sample size does not allow to disentangle gender effect of pandemic-related symptoms changes.
In the missed 62 patients, due to the unavailability of pre-lockdown CBCLs or changes in the age group of patients over time, a longitudinal comparison was not possible. The sample size is thus certainly small compared to the size firstly estimated, and partially hindered the statistical significance of the results, albeit still sufficient for some preliminary analyses. A follow-up project to detect the medium-long term mental health consequences is ongoing. Furthermore, considering the importance of interaction between genetic and epigenetic factors in neuropsychiatric etiology, it would be interesting in future work to correlate available baseline genetic CNVs to pandemic-related symptoms augmentation, in order to investigate vulnerability and resilience.
5. Conclusions
This study represents a first step in the ongoing discussion regarding the emotional and behavioural consequences in a population with complex neurological and psychiatric disorders during such a uniquely stressful pandemic event. The present results are informative, both in preparation for a re-assessment of the clinical population after this period of isolation, as well as in the eventuality of a second wave of the pandemic, which may lead to a second lockdown.
Author Contributions
Conceptualization, E.C., T.B., S.B., E.B., B.B., S.D.V., F.F., C.F., M.G., G.M. (Gemma Marinella), C.M., J.M., G.P., A.S., G.S. (Gianluca Sesso), V.S., G.T., I.T., A.M., and R.B.; Formal analysis, G.S. (Giuseppina Sgandurra) and G.D.N.; Methodology, T.B., S.B., E.B., B.B., S.D.V., F.F., C.F., M.G., G.M., C.M., J.M., G.P., A.S., G.S. (Gianluca Sesso), V.S., G.T., I.T., A.M., and R.B.; Software, E.C., C.F., J.M., G.S. (Gianluca Sesso), and I.T.; Supervision, E.C., G.S. (Giuseppina Sgandurra), G.C., G.M. (Gabriele Masi), F.M., and R.B.; Writing—original draft, T.B., S.B., E.B., B.B., S.D.V., F.F., C.F., M.G., G.M. (Gemma Marinella), C.M., J.M., G.P., A.S., G.S. (Gianluca Sesso), V.S., G.T., and I.T.; Writing—review and editing, E.C., A.M., and R.B. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by RC (Ricerca Corrente) 2000 of Italian Ministry of Health and funds 5 for thousand IRCCS FSM.
Acknowledgments
Special thanks to Paola Vitagliano, Roberta Scalise, and Roberta Marotta for their collaboration during the contact calls to the families and to Ailish Kynam for the English Language Revision.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Blendon, R.J.; Benson, J.M.; DesRoches, C.M.; Raleigh, E.; Taylor-Clark, K. The public’s response to severe acute respiratory syndrome in Toronto and the United States. Clin. Infect. Dis. 2004, 38, 925–931. [Google Scholar] [CrossRef] [PubMed]
- Caleo, G.; Duncombe, J.; Jephcott, F.; Lokuge, K.; Mills, C.; Looijen, E.; Theoharaki, F.; Kremer, R.; Kleijer, K.; Squire, J.; et al. The factors affecting household transmission dynamics and community compliance with Ebola control measures: A mixed-methods study in a rural village in Sierra Leone. BMC Public Health 2018, 18. [Google Scholar] [CrossRef] [PubMed]
- Cava, M.A.; Fay, K.E.; Beanlands, H.J.; McCay, E.A.; Wignall, R. The experience of quarantine for individuals affected by SARS in Toronto. Public Health Nurs. 2005, 22, 398–406. [Google Scholar] [CrossRef] [PubMed]
- DiGiovanni, C.; Conley, J.; Chiu, D.; Zaborski, J. Factors influencing compliance with quarantine in Toronto during the 2003 SARS outbreak. Biosecur. Bioterror. 2004, 2, 265–272. [Google Scholar] [CrossRef]
- Hawryluck, L.; Gold, W.L.; Robinson, S.; Pogorski, S.; Galea, S.; Styra, R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg. Infect. Dis. 2004, 10, 1206–1212. [Google Scholar] [CrossRef]
- Jeong, H.; Yim, H.W.; Song, Y.J.; Ki, M.; Min, J.A.; Cho, J.; Chae, J.H. Mental health status of people isolated due to Middle East Respiratory Syndrome. Epidemiol. Health 2016, 38, e2016048. [Google Scholar] [CrossRef]
- Lee, S.; Chan, L.Y.Y.; Chau, A.M.Y.; Kwok, K.P.S.; Kleinman, A. The experience of SARS-related stigma at Amoy Gardens. Soc. Sci. Med. 2005, 61, 2038–2046. [Google Scholar] [CrossRef]
- Pellecchia, U.; Crestani, R.; Decroo, T.; Van Den Bergh, R.; Al-Kourdi, Y. Social consequences of ebola containment measures in Liberia. PLoS ONE 2015, 10. [Google Scholar] [CrossRef]
- Wilken, J.A.; Pordell, P.; Goode, B.; Jarteh, R.; Miller, Z.; Saygar, B.G.; Maximore, L.; Borbor, W.M.; Carmue, M.; Walker, G.W.; et al. Knowledge, attitudes, and practices among members of households actively monitored or quarantined to prevent transmission of ebola virus disease-margibi county, liberia: February-march 2015. Prehosp. Disaster Med. 2017, 32, 673–678. [Google Scholar] [CrossRef]
- Yoon, M.K.; Kim, S.Y.; Ko, H.S.; Lee, M.S. System effectiveness of detection, brief intervention and refer to treatment for the people with post-traumatic emotional distress by MERS: A case report of community-based proactive intervention in South Korea. Int. J. Ment. Health Syst. 2016, 10. [Google Scholar] [CrossRef] [PubMed]
- Bai, Y.M.; Lin, C.C.; Lin, C.Y.; Chen, J.Y.; Chue, C.M.; Chou, P. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr. Serv. 2004, 55, 1055–1057. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Kakade, M.; Fuller, C.J.; Fan, B.; Fang, Y.; Kong, J.; Guan, Z.; Wu, P. Depression after exposure to stressful events: Lessons learned from the severe acute respiratory syndrome epidemic. Compr. Psychiatry 2012, 53, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Marjanovic, Z.; Greenglass, E.R.; Coffey, S. The relevance of psychosocial variables and working conditions in predicting nurses’ coping strategies during the SARS crisis: An online questionnaire survey. Int. J. Nurs. Stud. 2007, 44, 991–998. [Google Scholar] [CrossRef]
- Wu, P.; Liu, X.; Fang, Y.; Fan, B.; Fuller, C.J.; Guan, Z.; Yao, Z.; Kong, J.; Lu, J.; Litvak, I.J. Alcohol abuse/dependence symptoms among hospital employees exposed to a SARS outbreak. Alcohol Alcohol. 2008, 43, 706–712. [Google Scholar] [CrossRef]
- Braunack-Mayer, A.; Tooher, R.; Collins, J.E.; Street, J.M.; Marshall, H. Understanding the school community’s response to school closures during the H1N1 2009 influenza pandemic. BMC Public Health 2013, 13. [Google Scholar] [CrossRef]
- Wang, Y.; Xu, B.; Zhao, G.; Cao, R.; He, X.; Fu, S. Is quarantine related to immediate negative psychological consequences during the 2009 H1N1 epidemic? Gen. Hosp. Psychiatry 2011, 33, 75–77. [Google Scholar] [CrossRef]
- Desclaux, A.; Badji, D.; Ndione, A.G.; Sow, K. Accepted monitoring or endured quarantine? Ebola contacts’ perceptions in Senegal. Soc. Sci. Med. 2017, 178, 38–45. [Google Scholar] [CrossRef]
- Reynolds, D.L.; Garay, J.R.; Deamond, S.L.; Moran, M.K.; Gold, W.; Styra, R. Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiol. Infect. 2008, 136, 997–1007. [Google Scholar] [CrossRef]
- Mihashi, M.; Otsubo, Y.; Yinjuan, X.; Nagatomi, K.; Hoshiko, M.; Ishitake, T. Predictive Factors of Psychological Disorder Development During Recovery Following SARS Outbreak. Health Psychol. 2009, 28, 91–100. [Google Scholar] [CrossRef]
- Robertson, E.; Hershenfield, K.; Grace, S.L.; Stewart, D.E. The psychosocial effects of being quarantined following exposure to SARS: A qualitative study of Toronto health care workers. Can. J. Psychiatry 2004, 49, 403–407. [Google Scholar] [CrossRef] [PubMed]
- Taylor, M.R.; Agho, K.E.; Stevens, G.J.; Raphael, B. Factors influencing psychological distress during a disease epidemic: Data from Australia’s first outbreak of equine influenza. BMC Public Health 2008, 8. [Google Scholar] [CrossRef] [PubMed]
- Wester, M.; Giesecke, J. Ebola and healthcare worker stigma. Scand. J. Public Health 2019, 47, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Sprang, G.; Silman, M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Med. Public Health Prep. 2013, 7, 105–110. [Google Scholar] [CrossRef]
- Feo, P.; Di Gioia, S.; Carloni, E.; Vitiello, B.; Tozzi, A.E.; Vicari, S. Prevalence of psychiatric symptoms in children and adolescents one year after the 2009 L’Aquila earthquake. BMC Psychiatry 2014, 14. [Google Scholar] [CrossRef]
- Vijayakumar, L.; Kannan, G.K.; Daniel, S.J. Mental health status in children exposed to tsunami. Int. Rev. Psychiatry 2006, 18, 507–513. [Google Scholar] [CrossRef]
- Sourander, A. Behavior problems and traumatic events of unaccompanied refugee minors. Child Abus. Negl. 1998, 22, 719–727. [Google Scholar] [CrossRef]
- Mclaughlin, K.A.; Fairbank, J.A.; Gruber, M.J.; Jones, R.T.; Lakoma, M.D.; Pfefferbaum, B.; Sampson, N.A.; Kessler, R.C. Serious Emotional Disturbance Among Youths Exposed to Hurricane Katrina 2 Years Postdisaster. J. Am. Acad. Child Adolesc. Psychiatry 2009, 48, 1069–1078. [Google Scholar] [CrossRef]
- Qiu, J.; Shen, B.; Zhao, M.; Wang, Z.; Xie, B.; Xu, Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen. Psychiatry 2020, 33, e100213. [Google Scholar] [CrossRef]
- Wang, Y.; Zhao, X.; Feng, Q.; Liu, L.; Yao, Y.; Shi, J. Psychological assistance during the coronavirus disease 2019 outbreak in China. J. Health Psychol. 2020, 733–737. [Google Scholar] [CrossRef]
- Flaudias, V.; Iceta, S.; Zerhouni, O.; Rodgers, R.F.; Billieux, J.; Llorca, P.M.; Boudesseul, J.; Chazeron, I.D.E.; Romo, L.; Maurage, P.; et al. COVID-19 pandemic lockdown and problematic eating behaviors in a student population. J. Behav. Addict. 2020, 9, 826–835. [Google Scholar] [CrossRef] [PubMed]
- Achenbach, T.; Rescorla, L. Manual for the ASEBA School-Age Forms and Profiles: An Integrated System of Multi-Informant Assessment; University of Vermont, Research Center for Children, Youth, & Families: Burlington, VT, USA, 2001. [Google Scholar]
- Kaufman, J.; Birmaher, B.; Brent, D.; Rao, U.; Flynn, C.; Moreci, P.; Williamson, D.; Ryan, N. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. J. Am. Acad. Child Adolesc. Psychiatry 1997, 36, 980–988. [Google Scholar] [CrossRef] [PubMed]
- Lord, C.; Rutter, M.; DiLavore, P.; Risi, S.; Gotham, K.; Bishop, S. Autism Diagnostic Observation Schedule (ADOS-2), 2nd ed.; WWW Document; Los Angeles West. Psychol. Corp: New York, NY, USA, 2012; Available online: https://www.wpspublish.com/ados-2-autism-diagnostic-observation-schedule-second-edition (accessed on 22 February 2020).
- Rutter, M.; LeCouteur, A.; Lord, C. Autism Diagnostic Interview-Revised (ADI-R); WPS: Torrance, CA, USA, 2012. [Google Scholar]
- Racine, N.; Cooke, J.E.; Eirich, R.; Korczak, D.J.; McArthur, B.A.; Madigan, S. Child and adolescent mental illness during COVID-19: A rapid review. Psychiatry Res. 2020, 292. [Google Scholar] [CrossRef] [PubMed]
- Bitsika, V.; Sharpley, C.F.; Andronicos, N.M.; Agnew, L.L. Prevalence, structure and correlates of anxiety-depression in boys with an autism spectrum disorder. Res. Dev. Disabil. 2016, 49–50, 302–311. [Google Scholar] [CrossRef] [PubMed]
- Colizzi, M.; Bortoletto, R.; Silvestri, M.; Mondini, F.; Puttini, E.; Cainelli, C.; Gaudino, R.; Ruggeri, M.; Zoccante, L. Medically unexplained symptoms in the times of Covid-19 pandemic: A case-report. Brain, Behav. Immun. Health 2020, 100073. [Google Scholar] [CrossRef] [PubMed]
- Serra Giacobo, R.; Jané, M.C.; Bonillo, A.; Ballespí, S.; Díaz-Regañon, N. Somatic symptoms, severe mood dysregulation, and aggressiveness in preschool children. Eur. J. Pediatr. 2012, 171, 111–119. [Google Scholar] [CrossRef] [PubMed]
- Xie, X.; Xue, Q.; Zhou, Y.; Zhu, K.; Liu, Q.; Zhang, J.; Song, R. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatr. 2020, 174, 898–900. [Google Scholar] [CrossRef]
- Zhou, S.J.; Zhang, L.G.; Wang, L.L.; Guo, Z.C.; Wang, J.Q.; Chen, J.C.; Liu, M.; Chen, X.; Chen, J.X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psychiatry 2020, 29, 749–758. [Google Scholar] [CrossRef]
- England, M.J.; Sim, L.J. Depression in Parents, Parenting, and Children: Opportunities to Improve Identification, Treatment, and Prevention; National Academies Press: Washingon, DC, USA, 2009; ISBN 0309121787. [Google Scholar]
- Liu, N.; Zhang, F.; Wei, C.; Jia, Y.; Shang, Z.; Sun, L.; Wu, L.; Sun, Z.; Zhou, Y.; Wang, Y.; et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: Gender differences matter. Psychiatry Res. 2020, 287, 112921. [Google Scholar] [CrossRef]
- Willner, P.; Rose, J.; Stenfert Kroese, B.; Murphy, G.H.; Langdon, P.E.; Clifford, C.; Hutchings, H.; Watkins, A.; Hiles, S.; Cooper, V. Effect of the COVID-19 pandemic on the mental health of carers of people with intellectual disabilities. J. Appl. Res. Intellect. Disabil. 2020. [Google Scholar] [CrossRef]
- Sockalingam, S.; Leung, S.E.; Cassin, S.E. The Impact of COVID-19 on Bariatric Surgery: Re-Defining Psychosocial Care. Obesity (Silver Spring) 2020. [Google Scholar] [CrossRef]
- Tanir, Y.; Karayagmurlu, A.; Kaya, İ.; Kaynar, T.B.; Türkmen, G.; Dambasan, B.N.; Meral, Y.; Coşkun, M. Exacerbation of obsessive compulsive disorder symptoms in children and adolescents during COVID-19 pandemic. Psychiatry Res. 2020, 293. [Google Scholar] [CrossRef] [PubMed]
- Scahill, L.; Riddle, M.A.; McSwiggin-Hardin, M.; Ort, S.I.; King, R.A.; Goodman, W.K.; Cicchetti, D.; Leckman, J.F. Children’s Yale-Brown Obsessive Compulsive Scale: Reliability and validity. J. Am. Acad. Child Adolesc. Psychiatry 1997, 36, 844–852. [Google Scholar] [CrossRef] [PubMed]
- Liang, L.; Ren, H.; Cao, R.; Hu, Y.; Qin, Z.; Li, C.; Mei, S. The Effect of COVID-19 on Youth Mental Health. Psychiatr. Q. 2020. [Google Scholar] [CrossRef] [PubMed]
- Bobo, E.; Lin, L.; Acquaviva, E.; Caci, H.; Franc, N.; Gamon, L.; Picot, M.C.; Pupier, F.; Speranza, M.; Falissard, B.; et al. How do children and adolescents with Attention Deficit Hyperactivity Disorder (ADHD) experience lockdown during the COVID-19 outbreak? Encephale 2020, 46, S85–S92. [Google Scholar] [CrossRef]
- Reising, M.M.; Watson, K.H.; Hardcastle, E.J.; Merchant, M.J.; Roberts, L.; Forehand, R.; Compas, B.E. Parental Depression and Economic Disadvantage: The Role of Parenting in Associations with Internalizing and Externalizing Symptoms in Children and Adolescents. J. Child Fam. Stud. 2013, 22, 335–343. [Google Scholar] [CrossRef]
- Fegert, J.M.; Vitiello, B.; Plener, P.L.; Clemens, V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: A narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc. Psychiatry Ment. Health 2020, 14. [Google Scholar] [CrossRef]
- Joel, D.; McCarthy, M.M. Incorporating Sex As a Biological Variable in Neuropsychiatric Research: Where Are We Now and Where Should We Be? Neuropsychopharmacology 2017, 42, 1–7. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).