Abstract
The development of robotic devices for rehabilitation is a fast-growing field. Nowadays, thanks to novel technologies that have improved robots’ capabilities and offered more cost-effective solutions, robotic devices are increasingly being employed during clinical practice, with the goal of boosting patients’ recovery. Robotic rehabilitation is also widely used in the context of neurological disorders, where it is often provided in a variety of different fashions, depending on the specific function to be restored. Indeed, the effect of robot-aided neurorehabilitation can be maximized when used in combination with a proper training regimen (based on motor control paradigms) or with non-invasive brain machine interfaces. Therapy-induced changes in neural activity and behavioral performance, which may suggest underlying changes in neural plasticity, can be quantified by multimodal assessments of both sensorimotor performance and brain/muscular activity pre/post or during intervention. Here, we provide an overview of the most common robotic devices for upper and lower limb rehabilitation and we describe the aforementioned neurorehabilitation scenarios. We also review assessment techniques for the evaluation of robotic therapy. Additional exploitation of these research areas will highlight the crucial contribution of rehabilitation robotics for promoting recovery and answering questions about reorganization of brain functions in response to disease.
1. Introduction
Motor and sensory loss or dysfunction, caused by brain injuries or neurological disorders, severely affects the quality of life and may culminate in the inability to perform simple activities of daily living. Unfortunately, such sensorimotor impairments are very common among neurological patients: More than two-thirds of all stroke patients have affected upper limbs [1] and approximately 50% of them suffer from a chronic reduction in arm function [2]. These impairments can also affect the lower limb, compromising, with different degrees of severity, the sensorimotor strategies used by the brain during gait and balance control. In order to understand how to recover from these pathological conditions, it is necessary to highlight how the patient behavior is affected by a specific impairment. For example, proprioceptive impairments affect movement planning and inter-limb coordination [3,4]; paresis affects movements in accuracy, temporal efficiency, and efficacy [5]; and abnormal muscle tone turns into a lack of movement smoothness and intra-limb coordination [6].
In the last decades, innovative robotic technologies have been developed in order to effectively help clinicians during the neurorehabilitation process. The term “robotic technology” in this application domain refers to any mechatronic device with a certain degree of intelligence that can physically intervene on the behavior of the patient, optimizing and speeding up his/her sensorimotor recovery. The two key capabilities of these robots are: (1) Assessing the human sensorimotor function; and (2) re-training the human brain in order to improve the patient’s quality of life. However, most of the studies in this field have been focused more on the development of the devices, whereas less effort was made on maximizing their efficacy for promoting recovery. The main challenge consists of designing effective training modalities, supported by appropriate control strategies. Thus, each robotic device supports a pre-defined training modality depending on the low-level control strategy implemented and also on the residual abilities of each patient. Usually, most of the rehabilitation devices implement a passive training modality (robot-driven, position control strategy), where the robot imposes the trajectories, and an active training modality (patient-driven), where the robot modulates its trajectory in response to the subject’s intention to move [7,8]. However, among all the different training modalities, the most relevant is the assistive one. Assistive controllers help participants to move their impaired limbs according to the desired postures during grasping, reaching, or walking, reflecting the strategy adopted by conventional physical and occupational therapy (active assistive training mode). Specifically, among the assistive strategies, the assistance-as-needed is widely employed because it reduces the patient risk of relying only on the robot to accomplish the rehabilitative task. Indeed, over-assistance could decrease the level of participation and, as a consequence, also the chance to induce neuroplastic changes [9]. This is called the “slacking” effect, and can be formally defined as a reduction of voluntary movement control when the patient undergoes repetitive passive mobilization of the limbs [10]. In addition to the assistance-as-needed strategy, to avoid the slacking effect, challenge-based controllers are used to make tasks more difficult or stimulating. Among them, there are controllers that provide resistance to the participant’s limb movements during exercise (active resistive) [11,12]. Another challenge-based approach is the constraint-induced strategy. The main idea of this strategy is to “force use” the impaired limb, constraining the unimpaired limb/joint. This requires specific patterns of force generation to avoid compensatory movements and ensure the right postures [13]. Corrective strategies have the same aim: Through the creation of virtual haptic channels for the end-effector or the joints of the exoskeleton (tunneling), users are allowed to move only in delimited tunnels. Once they go out from the correct path, adopting compensatory movements, they are forced to go back into the channel [14,15]. Moreover, error enhancement strategies that amplify movement errors have been proposed since kinematic errors generated during movement are a fundamental neural signal that drives motor adaptation [16,17] (for a detailed review of the available control strategies and their implications, see Marchal-Crespo et al. [18]).
In order to improve the potentiality of neurorehabilitation, it is then crucial to combine robotic therapy with other disciplines, such as computational neuroscience, motor learning and control, and bio-signal processing, among others. Based on the previous considerations, here, we highlight recent findings in different fields that could be (or are already) applied to robotic neurorehabilitation. In the first section, we present an overview of state-of-the-art robotic devices for the upper and lower limb, with two specific case studies. The second section exploits complementing knowledge of other domains, focusing on rehabilitative training and assessment of behavioral and neural changes induced by robotic therapy. We conclude by providing a general perspective on the research in the robotic neurorehabilitation field for the near future, illustrating the limitations of current systems and perspectives for further improvement.
2. An Overview of Robotic Devices for Neurorehabilitation
Robotic devices for neurorehabilitation can be classified into two main categories based on the different types of physical human–robot interaction: end-effector devices and exoskeletons.
End-effector-based systems are robotic devices provided with a specific interface that mechanically constrains the distal part of the human limb (e.g., the human wrist). These systems do not control the whole kinematic chain and the human limb is free to completely adapt either to external disturbances or to movements applied by the end-effector robot. In this type of device, it is thus only possible to directly control the distal body segment that is attached to the end-effector; further information about forces and/or positions of the remaining parts of the human limb can be obtained indirectly.
Exoskeletons, on the contrary, exactly reproduce the kinematics of the human limb and support its movements through the control of the position and the orientation of each joint. The devices are designed with the specific purpose of coupling and aligning the mechanical joints to the human ones. As an example, in the context of upper limb robotics, the devices are linked to the limb either at the level of the arm and/or at the forearm. In addition, the range of motion (ROM) and the number of the actuated joints are appropriately chosen to optimize the control. Therefore, by using the exoskeleton, the patient’s movements are more supervised but at the cost of a higher complexity for the control of the degrees of freedom (DOFs).
In the following section, an overview of the available robotic devices for the upper and lower limb is provided, including a detailed description of two newly developed systems treated as case studies.
2.1. Robotic Neurorehabilitation for the Upper Limb
Various robotic systems for the upper limb have been developed, and protocols based on task-oriented repetitive movements have been proposed to improve ROM [19,20], muscle strength [21], movement coordination [22], and to promote motor learning [23].
Depending on the type and severity of the motor dysfunction and related impairment, one type of device could be more effective than the other. Specifically, if the residual sensorimotor functionalities of the patient are extremely low, exoskeletons could be more appropriate to apply forces to each joint [24]. Moreover, end-effector devices could be more effective to deliver complex patterns of forces (e.g., based on assistance-as-needed strategies) able to exploit the redundancy of the human body, thus speeding up sensorimotor recovery [25].
One of the first end-effector robots developed for upper limb rehabilitation, the MIT Manus [26], belongs to the laboratories of the Massachusetts Institute of Technology (MIT) and was designed for the shoulder and elbow joints. Other interesting examples are the ARM (Assisted Rehabilitation and Measurement) Guide [27] (a counterbalanced robot that does not load the arm and mechanically assist the reaching movement), the GENTLE/s (Robotic assistance in neuro and motor rehabilitation) [28], the Italian NeReBot (Neurorehabilitation Robot) [29], and the ACT3D (Arm Coordination Training Robot), specifically used to quantitatively measure abnormal joint torque coupling in chronic stroke [30]. Additionally, the Mirror Image Motion Enabler [31] and the Bi-Manu-Track [32] are two examples of upper limb robotic devices designed to implement bimanual training protocols. A summary of the most common upper limb end-effector robots and their main features is provided in Table 1.

Table 1.
Main features of the most common upper limbs end-effector rehabilitation robots.
Regarding the use of exoskeletons in the neurorehabilitation of the upper limb, interesting attempts have been proposed: SUEFUL [49], ARMin III [50], CADEN (Cable-Actuated Dextrous Exoskeleton for Neurorehabilitation) [51], and RUPERT (Robotic Upper Extremity Repetitive Trainer) [52].
It is worth mentioning that the exoskeletons currently developed differ in terms of mechanical structure. In detail, regarding the upper limb, most of them do not provide actuation for all the degrees of freedom (see [53] for a complete review), as they are only equipped with motors for the movements of the shoulder (L-Exos [54], the Pneu-Wrex [55]) and elbow joints, while additional actuation for the wrist is not available. On the contrary, the prototype, UL-EXO7 [51], and the commercial exoskeleton, ARMEO Power, developed from the ARMinIII [50], also provide forces on the wrist and forearm.
The design of the exoskeleton for the hand is indeed more difficult. Yet, remarkable examples, such as the Manovo Power (eventually integrated in the ARMEO Power (Hocoma, Switzerland)) and the IntelliArm exoskeleton [56], exist. Those devices are actuated to train hand opening and closing in reach and grasp movements or fingers’ passive stretching. Table 2 summarizes the exoskeletons for the upper limb.

Table 2.
Main features of the most common upper limbs exoskeletons.
Another interesting classification of exoskeleton and end-effector devices relates to their actuation system. Available possibilities are actuation by a motor, actuation by pneumatic muscle, and non-motorized actuation (such as hydraulic or springs) [53].
In the first category, i.e., actuated by an electric motor, are the exoskeletons, L-Exos [54], UL-Exo7 [62], GENTLE/G [66], REHAROB [67], and Armeo Power (Hocoma, Switzerland), and the end-effector systems, InMotion ARM, In Motion WRIST (Bionik), MIT-MANUS [33], and Braccio di Ferro [43]. Conversely, the exoskeletons, Pneu-Wrex [55] and BONES [65], are based on pneumatic muscles. Finally, the T-Wrex [68] and its commercial version, ARMEO Spring (Hocoma, Switzerland), only provide gravity support to the whole arm with no robotic actuation [69].
Upper limb exoskeletons for rehabilitation have been developed only recently compared to the end-effector devices. This is due to different reasons [70]: (i) The complex interaction between the mechanical structure of the exoskeletons and the different joints of the human body; (ii) the complex control schemes to be adopted to deal with back-drivability and transparency; and (iii) the need to promote sensorimotor recovery of the patient not passively moving their joints but using assistive training modalities able to respond to any pathological movement [71].
The low-level implementation of these assistive training modalities is more challenging in exoskeletons than in end-effector devices. In particular, with the goal to exploit exoskeletons to also improve inter-joint coordination in the neurological population [72], several innovative control schemes have been designed. Starting from the common control schemes implemented in end-effector devices and exoskeletons, there is closed-loop feedback control with feedforward components. This scheme permits the correction of patients’ performance errors and compensates for the weight, inertia, and friction of the device mechanisms. To obtain the error signal of the feedback loop, the ability to sense some kinematic variable (positions, velocities) or interaction forces and then compare them with a pre-determined reference trajectory is needed [58]. Instead, the feedforward components can be computed by the robot-model or can be learnt with iterative techniques [52]. This control strategy is more commonly implemented in exoskeletons using position information to close the loop [73,74]. Assistive strategies are also implemented by exploiting the interaction control framework [75]. In particular, most of the end-effector devices adopt impedance control schemes while exoskeletons adopt admittance control schemes. In the first case, the controllers use position feedback in order to regulate the mechanical impedance of the robot (a non-linear generalization of the mechanical stiffness). The second case is the opposite: The controllers use force feedback in order to regulate the position of the specific joints (based on a model of the system). Exoskeletons usually implement admittance control schemes due to the usual lack of back-drivability of their mechanisms.
In recent years, more complex schemes have been developed for upper limb exoskeletons: Sliding mode controllers [76] or controllers triggered by the intention detection of the patient computed by electrophysiological measurements (i.e., surface electromyography (sEMG) [77,78] and electroencephalography (EEG) [79]). All the aforementioned methods are based on the comparison of an error signal with a reference trajectory. With the end-effector devices, this trajectory can be easily computed or designed while with exoskeletons there are many issues to be solved. As already said, exoskeletons are potentially used to restore patient inter-joint coordination by properly tuning the different robot joint trajectories; however, the relation between recovery and exoskeleton trajectories is still unclear. The design of appropriate reference trajectories for each joint is a real challenge. Some methods have recently been proposed: (1) Reproduction of previously recorded trajectories performed by healthy subjects [80]; and (2) use of previously recorded pathological involuntary joint torques translated in the joint kinematics domain [81].
In order to have a more complete idea of a robot for upper limb neurorehabilitation, in the following paragraph, we briefly introduce a new robot developed in our laboratories, as a case study.
End-Effector Device for Wrist Rehabilitation: WristBot
WristBot is an end-effector robotic device designed for the wrist neurorehabilitation of patients with neurological or orthopedic disabilities (Figure 1). It was developed in the Motor Learning, Assistive and Rehabilitation Robotics laboratory of the Italian Institute of Technology (IIT). The robot allows movements along the three wrist articulations, with a range of motion similar to a typical human subject: ±62° in flexion/extension, 45°/40° in radial/ulnar deviation, and ±60° for pronation/supination movements [82]. It is provided with four brushless motors that allow guidance and assistance of wrist movements in the three above-mentioned planes, with a maximum torque of 1.53 Nm in flexion/extension, 1.63 Nm in radial/ulnar deviation, and 2.77 Nm in pronation/supination movements. In addition, these motors are chosen in such a way as to provide an accurate haptic rendering and compensate for the weight and inertia of the device, thus allowing free smooth movements.
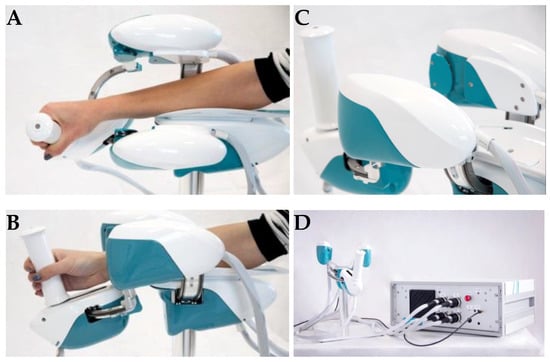
Figure 1.
Lateral view of WristBot during combined movements in the flexion–extension and pronation–supination DOFs (degrees of freedom) (A) and movements in the radial–ulnar deviation DOF (B); posterior–lateral view of the handle of WristBot (C) and a frontal view of the device connected to the case, with the integrated PC and electronic control unit (D).
Angular rotations on the three axes are acquired by means of high-resolution incremental encoders with a maximum error of 0.17°, thus making WristBot an optimal tool to assess the rehabilitative process in an objective and precise way. Another peculiarity of the WristBot is the possibility to provide assistive or perturbative forces that automatically adapt to the level of disability and performances of the patient. An intuitive graphical user interface (GUI) allows the therapist to choose the desired exercises and to set a wide range of parameters to continuously tailor the therapy to the patient’s needs. As for the interaction with patients, they are requested to hold the handle of the WristBot to perform wrist movements and execute the task presented on a monitor. In fact, a virtual reality environment is integrated into the system in order to provide stimulating visual feedback and engaging interaction.
The main advantages of the WristBot are its programmability and multi-functionality, which allow for a highly personalized therapy. In addition, the quantitative functional assessment provided by the device constitutes a valuable tool to support clinicians in the choice of the optimal therapy.
2.2. Robotic Neurorehabilitation for the Lower Limb
As for the upper limb, robotic devices for lower limb neurorehabilitation can also differ in terms of mechanical design (i.e., end-effector devices vs. exoskeletons), mechanism of actuation, training modality, number of degrees of freedom, and control architecture [7,83].
End-effector robots (see Table 3) are grouped in “footplate-based”, such as the Gait Trainer GTI [84], Haptic Walker [85], and G-EO Systems (EO, from latin: I walk) [86] robots, where the patient’s feet are firmly strapped onto platforms that are able to simulate the different gait cycles [87], and in “platform-based” robots, such as Hunova [88] (Movendo Technology, Genova, Italy) and Rutgers Ankle [89]. These robots are characterized by a fixed platform that does not simulate the walking pattern [90], but instead applies a controlled motion to the joints, specifically focusing on the ankle. One of the first examples of a footplate-based robot was the GTI [84], which allows partial or complete assistance support to both stance and swing phases of gait, depending on the subject’s residual abilities. The Haptic Walker, developed by the same research group of GTI, represents its improvement. Therefore, it allows for complex exercises, such as up and down stair-climbing or walking on rough surfaces, and it even simulates sliding or stumbling events [87]. G-EO Systems is similar to the Haptic Walker, but with reduced dimensions and with some precautions to comply for use in a clinical setting. Concerning “platform-based” end-effector robots, the recent Hunova platform has been developed, starting from the ARBOT device [91]. Hunova consists of two robotic platforms, one at the foot level and one at the seat level, allowing for rehabilitative exercises in both seated and upright mono and bipodalic conditions. It integrates force sensors to regulate the interaction with the patient and a wireless inertial sensor placed on the body of the subject, which allows detection of compensatory trunk movements and gives sensory feedback during exercise. Hunova can target rehabilitation of the lower limbs, from ankle to knee and hip, the pelvis, and trunk, by providing a large variety of training modalities, including the assistive resistive one [92].

Table 3.
Main features of the most common lower limb end-effector rehabilitation robots.
On the other hand, exoskeletons (see Table 4) are classified as “treadmill-based”, like Lokomat [99] (Hocoma, Volketswil, Switzerland), LokoHelp [100] (Woodway, Waukesha, WI, USA), LOPES [101], and ALEX [102], and as devices that directly allow for “overground walking”, such as Ekso [103] (Ekso Bionics, Richmond, VA, USA), HAL (Cyberdyne, Tsukuba, Japan), Rewalk [104] (Rewalk Robotics, Marlborough, MA, USA), and Indego Therapy [105] (Parker Hannifin, Macedonia, OH, USA). In this category, new emerging devices include EXOATLET [106] (Exoatlet, Moscow, Russia), PhoeniX (SuitX, Berkeley, CA, USA), for which limited information is currently available, and REX (REX Bionics, London, UK). In addition, some of these exoskeletons, such as Lokomat and REX, have been employed to develop brain machine interfaces (BMIs) (for a review, see [107]). Then, albeit still in progress, the development of self-balancing exoskeletons might allow for arm swing, which is an important feature during locomotion (no crutches or other external supports are required). Treadmill-based exoskeletons have been designed for use in a static configuration inside a rehabilitation structure, while the lightweight overground-walking exoskeletons have been developed to promote functional recovery of locomotion in a natural setting. Moreover, they have also been developed with the intention of using them in continuous contact with the patient, in order to allow, with a long term-perspective, home-based rehabilitation. For further differences between treadmill-based and overground-walking exoskeletons, the reader may refer to a previous review [108]. It is important to note that, among their differences, the overground-walking exoskeletons allow for more adequate control over step initiation than treadmill-based exoskeletons do.

Table 4.
Main features of the most common lower limbs exoskeletons.
The number of DOFs changes depending on the lower limb rehabilitation robot that is considered. Indeed, most of the current systems have two DOFs (per each leg) obtained by the flexion–extension of the knee and hip joints. As an example, the Lokomat, Rewalk, Ekso, and Indego Therapy exoskeletons actuate these two DOFs. Instead, the treadmill-based exoskeleton, ALEX, actuates seven DOFs (three for the trunk, two for the hip flexion/extension and abduction/adduction, one for the knee flexion/extension, and one for the ankle dorsi/plantar flexion). In terms of actuation mechanism, the choice generally falls on electric motors, but an exception does exist when switching to other applications, such as human performance augmentation, as in the case of the BLEEX exoskeleton [109], intended for military use, which is equipped with hydraulic linear actuators.
Likewise the upper limb, lower limbs robots use control strategies that take into account motor control paradigms useful for the acquisition or re-learning of motor skills [110,111]. In this perspective, an interesting example of a control strategy is the “cooperative patient control” that implies an active involvement of the patient during walking [112]. In this case, the robot imposes a previously defined physiological trajectory, but, at the same time, it allows the patient to move without temporal constraints. Thus, the subject can perform each step at his own pace while exploring their own motor strategy. This motor command exploration is crucial for the brain to promote motor learning [113]. Therefore, the level of effort and the exploitation of variability [114] are enhanced during the protocol with respect to passive mobilization of the legs, where trajectories are imposed (i.e., position control). The LokoMat supports the cooperative control strategy. Finally, another interesting control strategy in the field of locomotor rehabilitation is to employ surface electromyography to control the level of assistance [115] after the readout of the patient’s intention to perform a movement, like knee flexion [116] (implemented in the HAL exosuit).
As for the upper limb robots, in the following section, we shortly present a case study of an exoskeleton for robotic neurorehabilitation of the lower limbs, developed in our laboratories at the Italian Institute of Technology (IIT) in collaboration with the National Institute for Insurance against Accidents at Work (INAIL).
Modular Exoskeleton for Gait Assistance: Twin
The Twin exoskeleton was born thanks to the collaboration between IIT and INAIL and is currently employed in a clinical trial on spinal cord injury (SCI) subjects [83,134]. Figure 2 depicts the exoskeleton layout. It is composed by: (i) Three structural elements, including the pelvis (one), femur, and tibia (two per each leg); (ii) by four motors for the hip and knee actuation; (iii) by ergonomic interfaces (braces) of the femur, tibia, and trunk; (iv) by two foot/ankle orthosis; and (v) by a control central unit that contains an inertial measurement unit (IMU), located on the pelvis structural element. Each of the braces, links, and orthosis are available with different sizes in order to fit different subjects’ anthropometries. The motherboard installed in the control unit is able to send/receive commands and measurements to/from the actuators and it is located in the back part of the exoskeleton.

Figure 2.
Fronto-lateral view of the Twin exoskeleton (A), lateral view (B) with a particular focus on the hip joint (motor and electromechanical interface), fronto-lateral view (C) of the pelvis module highlighting the pelvis structural element and the backpack containing the battery, and posterior view (D). Written informed consent was obtained from the subject depicted in the panels.
A custom-made battery pack is located next to the motherboard and it guarantees up to five hours of continuous operation. There are two electric motors per each leg (hip and knee) and they allow for joints’ flexion/extension in the sagittal plane. As a result, Twin’s actuated DOFs are two per leg, the hips and the knees. The total number of DOFs is three per leg, if we consider the ankle that, however, is passive. Twin’s main feature is its complete modularity that allows the device to be assembled and disassembled easily and quickly. Eight electromechanical connectors make it possible to achieve this goal. These connectors realize a dual function: They can both bear the structural mechanical load and serve as an electrical interface between the different parts of the exoskeleton. This facilitates and decreases the time to don and doff Twin.
Currently, a position control has been implemented to assist subjects with complete Spinal Cord Injury (SCI). The IMU installed in the central control unit estimates the pitch and roll angles of the trunk. As soon as the trunk exceeds a certain degree of tilt angle in the sagittal plane (this value depends on the patient’s degree of impairment and it is set by the operator in agreement with the therapist), the motors automatically perform a step. Thus, by detecting trunk inclination, it is possible to determine the patient’s intention to move. Furthermore, it is possible to set other variables, such as the step length, the clearance that is the maximum distance between the foot trajectory during the swing phase and the ground, and the duration of the gait cycle. A mobile GUI allows all these parameters to be set and monitors the events in real-time. During Twin-aided locomotion assistance, the use of crutches is required. Moreover, another Twin functionality supports the patient’s sitting/standing up movement. In this case, the exoskeleton fully performs the movement, meaning that the patient’s intention to move is not read as in the walking scenario. A remote command from the GUI sends the trigger to start sitting or standing up. In this operative modality, different parameters are used with respect to the walking modality. Indeed, there is the possibility to set: The inclination value of the trunk during the phase of sitting/standing up, the total duration of the sitting/standing up procedure, and the pause between the two events. In the current state, Twin is undergoing further modifications in the control strategy for neurorehabilitation applications that will target stroke survivors.
3. Current Trends of Robot-Aided Neurorehabilitation
In the previous section, we provided an overview of the current rehabilitation devices, exploiting two recent case studies. We now present a description of the different settings in which robotic devices can be employed.
Robotic training plays a key role in neurorehabilitation. Indeed, it is possible to program the devices to implement different training possibilities, based on motor learning paradigms and/or on brain control. Furthermore, robots are not only able to provide highly reproducible, repeatable, and accurate movements (as imposed by forces and torques), but they can also accurately and precisely read out information about movement performance.
Moreover, we stress the fact that often the behavioral outcome of a rehabilitation treatment is inadequate to obtain a clear picture of the underlying complex mechanism of neuroplastic changes accompanying the recovery, and we thus present a multimodal framework of assessment. In this context, modern neuroimaging techniques play an important role in order to characterize the neural correlates of neurorehabilitation. Taken together, these evidences effectively validate the use of robotic devices for neurorehabilitation and pave the way for the development of novel robotic-based solutions aimed at boosting the therapeutic efficacy of treatment.
3.1. Rehabilitative Training
In order to maximize the use of rehabilitation robots for patients’ care, an appropriate rehabilitation training protocol must be carefully designed. To accomplish this goal, in the last decades, a huge amount of studies have been devoted to pursuing a complete understanding of the different processes in which humans learn (or re-learn) a motor skill. We describe these mechanisms in the next section, starting from the fundamental concepts of variability exploitation in motor learning and motor learning by action observation, passing through the description of the interplay between motor and sensory learning.
We also address the question of how the recovery process can be measured, predicted, and modeled, presenting a computational framework as a solution. Next, we discuss the strategies used by the brain to accomplish a task and we describe recent studies on the brain’s capability to self-select its own motor control strategy. Finally, we present examples of collaborative exercises to engage the patient in acquiring the optimal sensorimotor control strategy in a given task.
We then review recent works in which robotic rehabilitation is combined with BCI systems and discuss the opportunity offered by a brain-controlled therapy.
3.1.1. Advances in Motor Control for Robotic Neurorehabilitation
Understanding how the brain controls movements and which are the applied mechanisms to learn new skills is fundamental to plan an effective robot-based therapy, aimed at the promotion of sensorimotor recovery. In this framework, the design of the most appropriate and effective control strategy (i.e., the most sophisticated assistance) plays a crucial role, and can be achieved by exploiting and properly applying the latest findings in human neuroscience.
Many studies in the field of human physiology, biomechanics, and motor control have developed key theories that attempt to provide a complete understanding on how we plan and generate movements.
The first neuroscientific result to exploit sensorimotor neurorehabilitation relates to how motor variability plays a crucial role in promoting motor learning. While originally variability was seen as a “noise” that the brain had to reduce during learning [138], current studies have started to understand its value in the acquisition of motor skills (i.e., a higher exploration of the dynamical manifold of the environment). Specifically, Wu et al. [113] demonstrated how variability before learning a task is associated with faster rates of adaptation in both error-based and reinforcement tasks. Other studies tried to go further, separating variability on the basis of its effect on task performance [139] and, more recently, different amounts of variability have emerged as differently affecting the learning process, if applied in different spaces (task space vs. null space) of the dynamical manifold [140].
All these results suggest that the design of robotic rehabilitation protocols that introduce variability in the task during the training phase (see, as an example, the patient cooperative control strategy that is described above) may facilitate learning and thus sensorimotor recovery.
The second neuroscientific hint that is worth considering is related to action observation. It has been extensively demonstrated that visual feedback received from the observation of an action performed by another person contributes to improving motor learning [141]. Mattar and Gribble [142] revealed that when subjects observe a video of an individual performing reaching movements in a challenging environment and then perform the task by themselves, their performances in terms of learning are higher than those of individuals who did not observe any video. As a possible explanation, the authors suggested that action observation could be related to the acquisition of a neural representation of the dynamics of the task, as further discussed and also supported by other experiments [143,144]. It is therefore reasonable to believe that the integration of action observation phases in robotic neurorehabilitation programs may lead to more consistent improvements.
Based on these findings, action observation and passive proprioceptive training have been performed together, introducing here an additional point to discuss: The role of proprioceptive learning (or more generally, sensory learning) in the recovery process. Sensory learning is closely related to motor learning in the way in which motor learning shapes sensory networks in the brain and sensory learning changes motor areas [145,146]. In particular, sensory learning results in changes to motor networks in the brain and is also associated with plasticity in sensory systems that is determined by afferent inputs from the periphery and cortical projections from motor areas. Limited to proprioception, the idea to use robots to improve the recovery of this sensory channel has been extensively tested [145,146], in addition with supplementary vibro-tactile feedback [147].
Despite all the above-mentioned findings, we still do not have any information about the mechanisms adopted by the brain in the sensorimotor recovery process. New tools that can be applied to address this issue are models that belong to the field of computational neurorehabilitation. The computational neurorehabilitation paradigm [148] consists of mathematically modelling the mechanisms underlying the rehabilitation process, with the aim of understanding the biological details of recovery and of optimizing the individual treatment of patients. Each model is characterized by three features: (1) It uses, as an input, a quantitative description of the sensorimotor activity obtained by simulations or by the interaction with robots; (2) it is based on the description of computational mechanisms of activity-dependent plasticity; and (3) it produces, as an output, quantitative values of functional outcomes. Some examples of these models have been developed [10,149,150] and even if they are limited to specific cases, it could be possible to apply them in conjunction with robotic neurorehabilitation to tailor the treatment to the patient.
Despite all these considerations, we must take into account the possibility of the brain to autonomously choose a specific motor control strategy in order to perform a task. For example, when learning to stabilize unstable tools [151], either a strategy that relies more on feedback control [152] or one that is based on stiffness control [153] can be chosen. Therefore, understanding and modelling the strategies and the switching mechanisms between them may give us the possibility to predict more effectively the behavioral consequences of the application of a specific assistance. In this framework, if we could integrate models of sensorimotor control during robotic neurorehabilitation, we might have robots that are fully adaptable to the level of impairment of the patient and able to change their behavior accordingly to the patient’s intention.
The last aspect that is worth considering is the recent trend of training patients and/or therapists together, in groups or at least in couples (i.e., dyads). This synergy can be collaborative and/or competitive with a double goal: In the case of two patients training with the robot jointly, it brings improvement in the efficacy of the treatment through maximization of their motivation [154,155]; in the case of a therapist who performs a training jointly with a patient, it brings to an improvement of the generalization capabilities of the patient [156,157].
3.1.2. Robotic Neurorehabilitation Coupled to Brain Computer Interfaces
BCIs were originally conceived as non-invasive devices enabling communication, while their invasive counterpart, often defined as brain machine interfaces (BMIs), were aimed at providing some level of motor control in completely paralyzed or severely impaired people [158,159]. Given their ability to change and shape neural plasticity [160], more recently, BCIs and BMIs have been employed in neurorehabilitation of motor-impaired individuals, often in combination with other therapeutic approaches, including end-effector devices or exoskeletons [161].
As an example, in a recent study, the group of Millan showed that the use of functional electrical stimulation (FES) based on a BCI was able to induce significant functional recovery in stroke patients, and that such recovery was retained 6 to 12 months after the end of therapy [162]. In this study, decoding of movement intention by the BCI triggered activation of hand muscles through FES, and the authors showed that motor recovery came along with significant cortical reorganization.
In another study, the group of Contreras-Vidal investigated human treadmill walking with and without BCI control of a walking avatar and through source localization analysis of the EEG data, they showed that the use of the BCI involved a major cortical activation with respect to the case without the BCI, thus suggesting the potential benefit of a BCI-based therapy for promoting cortical engagement during rehabilitation therapy [163].
Recently, the groups of Ramos-Murguialday and Carmena developed a novel ‘hybrid’ BMI in which intracortical signals and EMG were used to control a multi-DOF upper limb robotic exoskeleton in a severely impaired chronic stroke patient and showed that rehabilitation with this system was able to induce significant motor recovery, which was retained 6 months afterwards [164].
These examples show that BCIs and BMIs can be successfully exploited to augment the outcome of a neurorehabilitation intervention: Indeed, these systems propose that the assistance follows the user’s motor intention, with the consequence being that stronger cortical changes are induced. These evidences pave the way for new combined and personalized interventions, where closed loop decoding of brain activity plays a key role for maximizing the sensorimotor recovery.
3.2. Multimodal Assessment of Recovery
The development of the robotic devices treated in this work is pivotal not only for therapy administration but also to accomplish another objective for the neuroscientific, medical, and rehabilitation engineering communities: The quantitative assessment of sensorimotor performance. Therefore, in addition to the kinematic and kinetic monitoring during gait, balance, or upper limb control, it is also necessary to assess the outcomes and the potential long-term retention of a neurorehabilitation protocol. As reported by Maggioni et al. [165], providing a reliable assessment of the sensorimotor components is important in order to optimize the patient’s chance of recovery. Despite this well-established evidence, these quantitative assessments by means of robotic devices are not continuously performed during clinical practice. Hence, the increased accuracy given by objective measurements of the performance is discarded in favor of objective clinical scales that are biased by the experience and the ability of the clinicians, leading to results that lack reliable measurement of the patient’s impairment. Moreover, subtle sensory and motor abnormalities are hardly detected by clinical measurements. In this framework, rehabilitation robotics are also able to improve the clinical evaluation, at least by placing the quantitative assessment side by side with the standard clinical evaluations.
Then, many of the neurorehabilitation studies that employed emerging robotic solutions did not account for a complete characterization of brain activity. Some studies exist [166,167,168], but further efforts are required [166] to characterize the neural basis of the sensorimotor function recovery driven by novel robotic devices. An unmet interest is understanding how the structural and functional properties of the brain are sculpted by the rehabilitation program. In fact, characterizing the brain reorganization, together with an adequate assessment of the behavioral performance, might help in a quantification of the recovery processes driven by the robot, in terms of both the ability to restore movements and to restitute pre-disease onset brain function [148]. Modern non-invasive neuroimaging techniques strike in, giving the possibility to assess brain activity changes pre/post and during the administration of robot-aided rehabilitation protocol.
In the next sections, we first describe current assessment procedures based on clinical scales, and we then address: (i) The quantitative assessment of sensorimotor performance; and (ii) neural and muscular correlates of sensorimotor performance.
3.2.1. Clinical Scales
The current clinical procedure to assess movement abnormalities is mostly represented by qualitative evaluations performed by human operators using clinical scales. The administration of these scales consists of proposing a series of tasks, tests, and questionnaires to the patients and observing their performance in order to assign a score proportional to the performance.
Developed clinical scales can be divided into those measuring motor performance and those assessing sensory functions. Among the former group, the most widely adopted are: the Quality of Upper Extremity Skills Test (QUEST) to evaluate movement patterns and hand function [169], the Modified Ashworth Scale (MAS) to measure the upper limb degree of spasticity based on the muscle resistance to passive stretches [170], the Fugl–Meyer Assessment (FMA) to quantitatively measure sensorimotor impairments [171], the Melbourne Assessment of Unilateral Upper Limb Function (MAUULF) to assess the quality of the movements [172], and finally the Box and Block Test (BBT) to evaluate gross manual dexterity [173]. Besides, the clinical rating scales validated and mostly used to measure sensory functions are the Nottingham Sensory Assessment [174] or the Rivermead Assessment of Somatosensory Performance [175] and the Joint Position Matching (JPM) test [176] to measure position sense acuity, the threshold to detection of passive motion (TTDPM) [177] for the testing of kinesthesia, and the tuning fork test to measure vibration sense [178].
All the afore-mentioned sensory clinical scales are applied also to the lower limbs. Other scales used for the lower limb are the five times sit to stand test [179], the timed up and go test (TUG) [180], the two minutes walking test, and ten meters walking test [181]. To test balance control ability during quiet standing, the most common clinical scales are the Romberg test [182] and the Berg balance scale [183]. Despite such scales being widely adopted and recognized worldwide, and despite them actually providing important measures about patients’ sensorimotor function, they are mostly qualitative and have low resolution. For this reason, they may be subjective and hardly repeatable and therefore not suitable to provide accurate and reliable measures. Current limitations for the application of these tests lie within the scarce presence of objective measurement technology in many clinical settings. The commonly used tools, such as hand-held goniometers, are known to lack sensitivity and reliability.
Given the low resolution of such scales, most of the patients get an intermediate score, which does not fully characterize their condition; furthermore, improvements that are below the scale resolution remain invisible, resulting in the same score over a long period of time [184]. Another disadvantage is that many operators consider the administration of these scales too complex and time-consuming [185]. This is not only a matter of comfort, but it also reflects on the reliability of the assessment. Finally, since many assessments can take a long time to complete, clinicians tend to delay treatment in favor of a heavy assessment, despite evidence on the importance of timing and early rehabilitation [186].
3.2.2. Quantitative Assessment of the Sensorimotor Performance
Recent advancements in haptic interfaces designed for sensorimotor rehabilitation provided the starting point for an innovative robot-aided assessment. In fact, such a technology is provided with high temporal and spatial resolution measurement systems that allow precise and continuous measurement of the positions, velocities, and forces of the joints and obtain kinematic and kinetic parameters from them [187,188]. These features of robotic technologies for rehabilitation allow the collection of large normative data sets through a reliable procedure that yields objective, reliable data at a high resolution. Recent contributions highlight the efficacy of robotic devices in providing meaningful information on sensorimotor functions for neurological subjects [189]. These measurements are objective and repeatable and can be used to provide patients and therapists with immediate measures of sensory and motor performance. Reducing the time to evaluate improvement or deterioration may offer new opportunities for designing therapeutic programs and ultimately for increasing the efficiency of patients’ care.
It is worth highlighting how robotic devices can instantaneously measure subjects’ performance during the whole treatment process, providing online indirect movement evaluation, making the assessment transparent to the patient, and reducing/eliminating the administration time as they can offer therapists and patients immediate feedback. Real-time scoring can not only greatly reduce the amount of time required for evaluations of patients’ motor improvements, but it is also becoming a key need for new robot-aided neurorehabilitation scenarios.
Recently, new ways have emerged to even assess energy consumption and psychological states by coupling robot sensors and external devices. Energy consumption, for example, is really relevant during walking and, in order to minimize it, humans are able to change the step length, arm swing, and cadence [190]. It is well known that neurological diseases affecting gait increase energy expenditure up to 70% with respect to healthy conditions [191]. This issue has been quantitatively assessed using indirect calorimetry while patients were walking wearing an exoskeleton [192]. Moreover, new assessment methods that use modelling and only robot sensing capabilities are under development [193]. Regarding the possibility to assess psychological states, there are many studies in the human–robot interaction field [194,195,196]. In particular, the assessment of these states could be crucial to quantitatively monitoring the level of engagement and motivation of the patients. This can be done using external devices to measure heart rate variability, breathing frequency, skin conductance response, and skin temperature and correlating these measures with kinematic and dynamic information coming from the robot [197].
To conclude, robotic devices designed for neurorehabilitation might improve the quality of quantitative assessment, which is also essential to better understand and infer the rehabilitation treatment effect on sensorimotor function. Robotic measurements can potentially outperform human-administered clinical scales and are only limited by the performance of the robot sensors.
3.2.3. Neural and Muscular Correlates of the Sensorimotor Performance
Sensorimotor performance can also be assessed through brain and/or muscle activity recordings. In fact, given the complexity of the brain’s functional reorganization [25] in response to central nervous system diseases, it is pivotal to study brain activity at high temporal (in the order of milliseconds) and good spatial (in the order of 1 cm or less) scales [198]. Thus, combining these two scales might increase the chance of understanding the recovery process. Achieving both these resolutions is nowadays possible thanks to the combination of high density electroencephalography (hdEEG) recordings and source imaging techniques that recently allowed reliable reconstruction of the brain’s resting-state networks [199] and even measurement of electrophysiological sub-cortical activity [200]. Furthermore, hdEEG (or EEG) is attractive because it is inexpensive and portable compared to other non-invasive neuroimaging techniques, such as magnetoencephalography (MEG) or functional and structural magnetic resonance imaging (MRI). In addition, it is possible to use EEG during task performance in an ecological environment. This framework allows exploration of the brain’s functional changes and monitoring of brain activity in response to rehabilitation tasks [201,202,203], potentially shedding light on specific brain–behavior relationships.
In addition to the investigation of task-related activity, it is interesting to estimate the functional connectivity (FC) both during tasks and/or the resting state. FC represents a significant statistical relationship between separate brain areas and any imbalance occurring in FC properties, as modeled by graph-based metrics, might underlie neuropathological processes and insults occurring in the cerebral organization [204,205,206,207]. Moreover, FC during spontaneous oscillatory activity, as measured by other techniques, such as resting state functional MRI, changes after proprioceptive training with a robotic manipulandum [208]. Furthermore, FC predicts the behavioral outcomes of rehabilitation protocols [209] as well as the recovery of motor function [168,207] in stroke subjects and also correlates with the level of clinical disability in early relapsing-remitting multiple sclerosis subjects [210]. As for the EEG, FC measurements follow spontaneous recovery [204], are related to motor deficits in stroke [211] and multiple sclerosis [206], and predict learning rate [212,213] in healthy subjects. Taken together, all these evidences suggest that an evaluation of the FC pre- and post-rehabilitation is a valuable tool to evaluate the effectiveness of the rehabilitation protocol administered with a newly developed robotic device [168]. There are other reasons supporting the use of the resting state paradigm. First, the resting state is compliant even for those subjects who suffer from very high degrees of physical impairment [214] that may cause a dramatic decrease of the signal to noise ratio. Second, it is not sensitive to task-related parameters and it is very well-suited to exploration of the potential long-term retention of the protocol [208]. Third, movement-related artifacts occurring during task performance might be very detrimental, also in healthy and minimally impaired subjects.
The amount of sensorimotor recovery can also be assessed by making use of other electrophysiological measurements, such as sEMG. Indeed, many diseases affecting the human sensorimotor system are associated with abnormal patterns of muscle activation [215,216], and thus motor recovery could be directly measured by EMG patterns [217]. In this context, muscular activity is usually decomposed into invariant modules of spatial and/or temporal activation [218]. Abnormal muscle synergies with respect to their healthy counterparts can, for example, be informative of compensatory strategies, which typically reflect the nature of the deficit and the level of impairment [219].
So far, multi-domain evaluations (behavioral, muscular, and neural correlates) have not performed continuously, and in our opinion, an elegant robotic solution should be accompanied by validation studies of how the rehabilitation robot impacts the patients’ life, by assessing, at the same time, the neural and behavioral correlates’ changes and their interplay [167,220]. Hence, combining these assessments might increase the sensitivity to better understand the recovery of the sensorimotor functions, to individuate potential maladaptive compensatory strategies, to plan customized therapeutic intervention, and to monitor disease progression more accurately. These studies could potentially open new insights about brain function and about the effectiveness of a particular rehabilitation program and device in facing the neurological disease under examination. As an example, in the field of gait rehabilitation for subjects affected by multiple sclerosis, the effectiveness of robot-assisted training for locomotor function recovery is still debated [221]. However, with the multimodal framework showed here, further understanding might be achieved.
Finally, as recently reported [25], the neurophysiological and clinical factors that influence the recovery of sensorimotor function should drive the robotics rehabilitation process. In this context, the combination of these multi-modal approaches seems an encouraging scenario to exploit and better understand these crucial factors. For example, electrophysiological recordings from human muscles might serve as control signals for robotic rehabilitation devices, thus assigning EMG the double role of shaping the amount of rehabilitation intervention and of biofeedback of the performed movement [217].
4. Further Considerations and Conclusions
Despite a great number of remarkable robots for neurorehabilitation being developed in the last decades, there is still room for improvement. We think that future studies should focus on the investigation of more suitable control algorithms and on the design of new mechatronic structures. However, this is not an easy task, especially for exoskeletons. Exoskeletons have to deal with a high mechanical complexity [222]: They should be lightweight, portable, efficient, compliant, and, at the same time, they must safely support the patient even when severe impairments, such as complete SCI are present. Addressing these challenging requirements may dramatically impact on the costs and, in order to contain the expenses during the design of a device, it is fundamental to have in mind the specific impairment the device is being conceived for to select only the most important developmental priorities.
A possible suggestion for the research in this field is the design of effective robotic control strategies to optimize and speed up sensorimotor recovery. Sensorimotor performance and recovery might be fully assessed through the further development of robotic scales and the integration of the measures with biosignals. We thus suggest that in the future, novel and/or composite indicators should exploit computational tools based on different multimodal strategies of assessment. Such an expansion of knowledge has led to recognition of the importance of a deeper investigation of neural correlates of rehabilitation. On the one hand, this improves the comprehension of human physiology and motor control. On the other hand, it allows advancement of the understanding of how to help the brain recover from an injury and thus of how to develop the best devices to enhance motor recovery and elicit neuroplasticity. Possible limitations could be due to the effective adoption of these sophisticated techniques in the clinical setting.
Quantitative assessment of sensorimotor recovery might be crucial to shape robotic neurorehabilitation training. In the training phase, we expect a revolution in the delivery of assistance. In particular, protocols could take into account the structure of motor variability and the effect of observation of others’ actions during the treatment. We could also exploit robots to perform sensorimotor rehabilitation, thus focusing not only on motor aspects but also on sensory ones. This could be done also by the addition of other feedback in the process (vibro-tactile, acoustic, among others).
Moreover, in the era of big data and artificial intelligence, computational models can be developed to understand the recovery mechanisms, predict the use of different motor control strategies, and eventually tailor the treatment to the patient.
As a concluding remark, we highlight that in order to be effective, a rehabilitation intervention must be valued by the patient. It is indeed fundamental to take into account the end-user’s perspective when designing a particular tool to aid a given dysfunction. Such a synergistic effort will surely translate into a valid treatment.
Author Contributions
All authors contributed to the writing—original draft preparation.
Funding
This research was partially funded by Istituto Nazionale per l’Assicurazione contro gli Infortuni sul Lavoro (INAIL).
Acknowledgments
The authors would like to thank Giulio Cerruti and Maria Laura D’Angelo for their valuable help in the discussion about lower limbs exoskeletons. The authors also thank Samuel Stedman for carefully proofreading the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Hatem, S.M.; Saussez, G.; della Faille, M.; Prist, V.; Zhang, X.; Dispa, D.; Bleyenheuft, Y. Rehabilitation of motor function after stroke: A multiple systematic review focused on techniques to stimulate upper extremity recovery. Front. Hum. Neurosci. 2016, 10, 442. [Google Scholar] [CrossRef] [PubMed]
- Broeks, J.G.; Lankhorst, G.J.; Rumping, K.; Prevo, A.J.H. The long-term outcome of arm function after stroke: Results of a follow-up study. Disabil. Rehabil. 1999, 21, 357–364. [Google Scholar] [CrossRef] [PubMed]
- Coderre, A.M.; Zeid, A.A.; Dukelow, S.P.; Demmer, M.J.; Moore, K.D.; Demers, M.J.; Bretzke, H.; Herter, T.M.; Glasgow, J.I.; Norman, K.E. Assessment of upper-limb sensorimotor function of subacute stroke patients using visually guided reaching. Neurorehabil. Neural Repair 2010, 24, 528–541. [Google Scholar] [CrossRef] [PubMed]
- Winward, C.E.; Halligan, P.W.; Wade, D.T. Current practice and clinical relevance of somatosensory assessment after stroke. Clin. Rehabil. 1999, 13, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Lang, C.E.; Bland, M.D.; Bailey, R.R.; Schaefer, S.Y.; Birkenmeier, R.L. Assessment of upper extremity impairment, function, and activity after stroke: Foundations for clinical decision making. J. Hand Ther. 2013, 26, 104–115. [Google Scholar] [CrossRef] [PubMed]
- Lang, C.E.; Beebe, J.A. Relating movement control at 9 upper extremity segments to loss of hand function in people with chronic hemiparesis. Neurorehabil. Neural Repair 2007, 21, 279–291. [Google Scholar] [CrossRef] [PubMed]
- Meng, W.; Liu, Q.; Zhou, Z.; Ai, Q.; Sheng, B.; Xie, S. Recent development of mechanisms and control strategies for robot-assisted lower limb rehabilitation. Mechatronics 2015, 31, 132–145. [Google Scholar] [CrossRef]
- Zhang, X.; Yue, Z.; Wang, J. Robotics in Lower-Limb Rehabilitation after Stroke. Behav. Neurol. 2017, 2017, 13. [Google Scholar] [CrossRef] [PubMed]
- Wolbrecht, E.T.; Chan, V.; Le, V.; Cramer, S.C.; Reinkensmeyer, D.J.; Bobrow, J.E. Real-time computer modeling of weakness following stroke optimizes robotic assistance for movement therapy. In Proceedings of the 2007 3rd International IEEE/EMBS Conference on Neural Engineering, Kohala Coast, HI, USA, 2–5 May 2007; pp. 152–158. [Google Scholar]
- Casadio, M.; Sanguineti, V. Learning, retention, and slacking: A model of the dynamics of recovery in robot therapy. IEEE Trans. Neural Syst. Rehabil. Eng. 2012, 20, 286–296. [Google Scholar] [CrossRef] [PubMed]
- Lambercy, O.; Dovat, L.; Gassert, R.; Burdet, E.; Teo, C.L.; Milner, T. A haptic knob for rehabilitation of hand function. IEEE Trans. Neural Syst. Rehabil. Eng. 2007, 15, 356–366. [Google Scholar] [CrossRef] [PubMed]
- Stienen, A.H.A.; Hekman, E.E.G.; Van der Helm, F.C.T.; Prange, G.B.; Jannink, M.J.A.; Aalsma, A.M.M.; Van der Kooij, H. Dampace: Dynamic force-coordination trainer for the upper extremities. In Proceedings of the 2007 IEEE 10th International Conference on Rehabilitation Robotics, Noordwijk, The Netherlands, 13–15 June 2007. [Google Scholar]
- Johnson, M.J.; Van der Loos, H.F.M.; Burgar, C.G.; Shor, P.; Leifer, L.J. Design and evaluation of Driver’s SEAT: A car steering simulation environment for upper limb stroke therapy. Robotica 2003, 21, 13–23. [Google Scholar] [CrossRef]
- Proietti, T.; Crocher, V.; Roby-Brami, A.; Jarrasse, N. Upper-Limb Robotic Exoskeletons for Neurorehabilitation: A Review on Control Strategies. IEEE Rev. Biomed. Eng. 2016, 9, 4–14. [Google Scholar] [CrossRef] [PubMed]
- Guidali, M.; Duschau-Wicke, A.; Broggi, S.; Klamroth-Marganska, V.; Nef, T.; Riener, R. A robotic system to train activities of daily living in a virtual environment. Med. Biol. Eng. Comput. 2011, 49, 1213–1223. [Google Scholar] [CrossRef] [PubMed]
- Abdollahi, F.; Lazarro, E.D.C.; Listenberger, M.; Kenyon, R.V.; Kovic, M.; Bogey, R.A.; Hedeker, D.; Jovanovic, B.D.; Patton, J.L. Error Augmentation Enhancing Arm Recovery in Individuals With Chronic Stroke: A Randomized Crossover Design. Neurorehabil. Neural Repair 2014, 28, 120–128. [Google Scholar] [CrossRef] [PubMed]
- Patton, J.L.; Stoykov, M.E.; Kovic, M.; Mussa-Ivaldi, F.A. Evaluation of robotic training forces that either enhance or reduce error in chronic hemiparetic stroke survivors. Exp. Brain Res. 2006, 168, 368–383. [Google Scholar] [CrossRef] [PubMed]
- Marchal-Crespo, L.; Reinkensmeyer, D.J. Review of control strategies for robotic movement training after neurologic injury. J. NeuroEng. Rehabil. 2009, 6, 20. [Google Scholar] [CrossRef]
- Posteraro, F.; Mazzoleni, S.; Aliboni, S.; Cesqui, B.; Battaglia, A.; Dario, P.; Micera, S. Robot-mediated therapy for paretic upper limb of chronic patients following neurological injury. J. Rehabil. Med. 2009, 41, 976–980. [Google Scholar] [CrossRef]
- Squeri, V.; Masia, L.; Giannoni, P.; Sandini, G.; Morasso, P. Wrist rehabilitation in chronic stroke patients by means of adaptive, progressive robot-aided therapy. IEEE Trans. Neural Syst. Rehabil. Eng. 2013, 22, 312–325. [Google Scholar] [CrossRef]
- Lum, P.S.; Burgar, C.G.; Shor, P.C.; Majmundar, M.; Van der Loos, M. Robot-assisted movement training compared with conventional therapy techniques for the rehabilitation of upper-limb motor function after stroke. Arch. Phys. Med. Rehabil. 2002, 83, 952–959. [Google Scholar] [CrossRef]
- Riener, R.; Nef, T.; Colombo, G. Robot-aided neurorehabilitation of the upper extremities. Med. Biol. Eng. Comput. 2005, 43, 2–10. [Google Scholar] [CrossRef]
- Shadmehr, R.; Mussa-Ivaldi, F.A. Adaptive representation of dynamics during learning of a motor task. J. Neurosci. 1994, 14, 3208–3224. [Google Scholar] [CrossRef] [PubMed]
- Klamroth-Marganska, V.; Blanco, J.; Campen, K.; Curt, A.; Dietz, V.; Ettlin, T.; Felder, M.; Fellinghauer, B.; Guidali, M.; Kollmar, A.; et al. Three-dimensional, task-specific robot therapy of the arm after stroke: A multicentre, parallel-group randomised trial. Lancet Neurol. 2014, 13, 159–166. [Google Scholar] [CrossRef]
- Gassert, R.; Dietz, V. Rehabilitation robots for the treatment of sensorimotor deficits: A neurophysiological perspective. J. NeuroEng. Rehabil. 2018, 15, 46. [Google Scholar] [CrossRef] [PubMed]
- Krebs, H.I.; Ferraro, M.; Buerger, S.P.; Newbery, M.J.; Makiyama, A.; Sandmann, M.; Lynch, D.; Volpe, B.T.; Hogan, N. Rehabilitation robotics: Pilot trial of a spatial extension for MIT-Manus. J. NeuroEng. Rehabil. 2004, 1, 5. [Google Scholar] [CrossRef] [PubMed]
- Reinkensmeyer, D.J.; Kahn, L.E.; Averbuch, M.; McKenna-Cole, A.; Schmit, B.D.; Rymer, W.Z. Understanding and treating arm movement impairment after chronic brain injury: Progress with the ARM guide. J. Rehabil. Res. Dev. 2000, 37, 653–662. [Google Scholar] [PubMed]
- Coote, S.; Murphy, B.; Harwin, W.; Stokes, E. The effect of the GENTLE/s robot-mediated therapy system on arm function after stroke. Clin. Rehabil. 2008, 22, 395–405. [Google Scholar] [CrossRef]
- Rosati, G.; Gallina, P.; Masiero, S. Design, implementation and clinical tests of a wire-based robot for neurorehabilitation. IEEE Trans. Neural Syst. Rehabil. Eng. 2007, 15, 560–569. [Google Scholar] [CrossRef] [PubMed]
- Ellis, M.D.; Sukal-Moulton, T.M.; Dewald, J.P. Impairment-based 3-D robotic intervention improves upper extremity work area in chronic stroke: Targeting abnormal joint torque coupling with progressive shoulder abduction loading. IEEE Trans. Robot. 2009, 25, 549–555. [Google Scholar] [CrossRef]
- Lum, P.S.; Burgar, C.G.; Van der Loos, M.; Shor, P.C. MIME robotic device for upper-limb neurorehabilitation in subacute stroke subjects: A follow-up study. J. Rehabil. Res. Dev. 2006, 43, 631. [Google Scholar] [CrossRef]
- Hesse, S.; Schulte-Tigges, G.; Konrad, M.; Bardeleben, A.; Werner, C. Robot-assisted arm trainer for the passive and active practice of bilateral forearm and wrist movements in hemiparetic subjects. Arch. Phys. Med. Rehabil. 2003, 84, 915–920. [Google Scholar] [CrossRef]
- Hogan, N.; Krebs, H.I.; Charnnarong, J.; Srikrishna, P.; Sharon, A. MIT-MANUS: A workstation for manual therapy and training. I. In Proceedings of the IEEE International Workshop on Robot and Human Communication, Okyo, Japan, 12 June 1992; pp. 161–165. [Google Scholar]
- Frascarelli, F.; Masia, L.; Di Rosa, G.; Cappa, P.; Petrarca, M.; Castelli, E.; Krebs, H. The impact of robotic rehabilitation in children with acquired or congenital movement disorders. Eur. J. Phys. Rehabil. Med. 2009, 45, 135–141. [Google Scholar] [PubMed]
- Fasoli, S.E.; Fragala-Pinkham, M.; Hughes, R.; Hogan, N.; Stein, J.; Krebs, H.I. Upper limb robot-assisted therapy: A new option for children with hemiplegia. Technol. Disabil. 2010, 22, 193–198. [Google Scholar] [CrossRef]
- Hidler, J.; Nichols, D.; Pelliccio, M.; Brady, K. Advances in the understanding and treatment of stroke impairment using robotic devices. Top. Stroke Rehabil. 2005, 12, 22–35. [Google Scholar] [CrossRef] [PubMed]
- Kahn, L.E.; Zygman, M.L.; Rymer, W.Z.; Reinkensmeyer, D.J. Robot-assisted reaching exercise promotes arm movement recovery in chronic hemiparetic stroke: A randomized controlled pilot study. J. NeuroEng. Rehabil. 2006, 3, 12. [Google Scholar] [CrossRef] [PubMed]
- Amirabdollahian, F.; Loureiro, R.; Gradwell, E.; Collin, C.; Harwin, W.; Johnson, G. Multivariate analysis of the Fugl-Meyer outcome measures assessing the effectiveness of GENTLE/S robot-mediated stroke therapy. J. NeuroEng. Rehabil. 2007, 4, 4. [Google Scholar] [CrossRef]
- van der Linde, R.Q.; Lammertse, P. HapticMaster–a generic force controlled robot for human interaction. Ind. Robot. Int. J. 2003, 30, 515–524. [Google Scholar] [CrossRef]
- Masiero, S.; Poli, P.; Armani, M.; Ferlini, G.; Rizzello, R.; Rosati, G. Robotic upper limb rehabilitation after acute stroke by NeReBot: Evaluation of treatment costs. BioMed Res. Int. 2014, 2014, 5. [Google Scholar]
- Sukal, T.M.; Ellis, M.D.; Dewald, J.P. Shoulder abduction-induced reductions in reaching work area following hemiparetic stroke: Neuroscientific implications. Exp. Brain Res. 2007, 183, 215–223. [Google Scholar] [CrossRef]
- Lum, P.S.; Burgar, C.G.; Shor, P.C. Evidence for improved muscle activation patterns after retraining of reaching movements with the MIME robotic system in subjects with post-stroke hemiparesis. IEEE Trans. Neural Syst. Rehabil. Eng. 2004, 12, 186–194. [Google Scholar] [CrossRef]
- Casadio, M.; Sanguineti, V.; Morasso, P.G.; Arrichiello, V. Braccio di Ferro: A new haptic workstation for neuromotor rehabilitation. Technol. Health Care 2006, 14, 123–142. [Google Scholar]
- Squeri, V.; Vergaro, E.; Brichetto, G.; Casadio, M.; Morasso, P.G.; Solaro, C.; Sanguineti, V. Adaptive robot training in the rehabilitation of incoordination in Multiple Sclerosis: A pilot study. In Proceedings of the 2007 IEEE 10th International Conference on Rehabilitation Robotics, Noordwijk, The Netherlands, 13–15 June 2007; pp. 364–370. [Google Scholar]
- De Santis, D.; Zenzeri, J.; Casadio, M.; Masia, L.; Riva, A.; Morasso, P.; Squeri, V. Robot-assisted training of the kinesthetic sense: Enhancing proprioception after stroke. Front. Hum. Neurosci. 2015, 8, 1037. [Google Scholar] [CrossRef] [PubMed]
- Masia, L.; Casadio, M.; Giannoni, P.; Sandini, G.; Morasso, P. Performance adaptive training control strategy for recovering wrist movements in stroke patients: A preliminary, feasibility study. J. NeuroEng. Rehabil. 2009, 6, 44. [Google Scholar] [CrossRef] [PubMed]
- Marini, F.; Hughes, C.M.L.; Squeri, V.; Doglio, L.; Moretti, P.; Morasso, P.; Masia, L. Robotic wrist training after stroke: Adaptive modulation of assistance in pediatric rehabilitation. Robot. Auton. Syst. 2017, 91, 169–178. [Google Scholar] [CrossRef]
- Marini, F.; Cappello, L.; Squeri, V.; Morasso, P.; Moretti, P.; Riva, A.; Doglio, L.; Masia, L. Online Modulation of Assistance in Robot Aided Wrist Rehabilitation A Pilot Study on a Subject Affected by Dystonia. In Proceedings of the 2014 IEEE Haptics Symposium (HAPTICS), Houston, TX, USA, 23–26 February 2014; pp. 153–158. [Google Scholar]
- Gopura, R.A.R.C.; Kiguchi, K.; Li, Y. SUEFUL-7: A 7DOF upper-limb exoskeleton robot with muscle-model-oriented EMG-based control. In Proceedings of the 2009 IEEE/RSJ International Conference on Intelligent Robots and Systems, St. Louis, MO, USA, 10–15 October 2009; pp. 1126–1131. [Google Scholar]
- Nef, T.; Guidali, M.; Riener, R. ARMin III–arm therapy exoskeleton with an ergonomic shoulder actuation. Appl. Bionics Biomech. 2009, 6, 127–142. [Google Scholar] [CrossRef]
- Perry, J.C.; Rosen, J.; Burns, S. Upper-limb powered exoskeleton design. IEEE/ASME Trans. Mechatron. 2007, 12, 408–417. [Google Scholar] [CrossRef]
- Balasubramanian, S.; Wei, R.; Perez, M.; Shepard, B.; Koeneman, E.; Koeneman, J.; He, J. RUPERT: An exoskeleton robot for assisting rehabilitation of arm functions. In Proceedings of the 2008 Virtual Rehabilitation, Vancouver, BC, Canada, 25–27 August 2008; pp. 163–167. [Google Scholar]
- Rehmat, N.; Zuo, J.; Meng, W.; Liu, Q.; Xie, S.Q.; Liang, H. Upper limb rehabilitation using robotic exoskeleton systems: A systematic review. Int. J. Intell. Robot. Appl. 2018, 2, 283–295. [Google Scholar] [CrossRef]
- Frisoli, A.; Rocchi, F.; Marcheschi, S.; Dettori, A.; Salsedo, F.; Bergamasco, M. A new force-feedback arm exoskeleton for haptic interaction in virtual environments. In Proceedings of the 1st Joint Eurohaptics Conference and Symposium on Haptic Interfaces for Virtual Environment and Teleoperator Systems World Haptics Conference, Pisa, Italy, 18–20 March 2005; pp. 195–201. [Google Scholar]
- Reinkensmeyer, D.J.; Wolbrecht, E.T.; Chan, V.; Chou, C.; Cramer, S.C.; Bobrow, J.E. Comparison of 3D, assist-as-needed robotic arm/hand movement training provided with Pneu-WREX to conventional table top therapy following chronic stroke. Am. J. Phys. Med. Rehabil. Assoc. Acad. Physiatr. 2012, 91, S232. [Google Scholar] [CrossRef]
- Ren, Y.; Park, H.-S.; Zhang, L.-Q. Developing a whole-arm exoskeleton robot with hand opening and closing mechanism for upper limb stroke rehabilitation. In Proceedings of the 2009 IEEE International Conference on Rehabilitation Robotics, Kyoto, Japan, 23–26 June 2009; pp. 761–765. [Google Scholar]
- Nef, T.; Mihelj, M.; Kiefer, G.; Perndl, C.; Muller, R.; Riener, R. ARMin-Exoskeleton for arm therapy in stroke patients. In Proceedings of the 2007 IEEE 10th international conference on rehabilitation robotics, Noordwijk, The Netherlands, 13–15 June 2007; pp. 68–74. [Google Scholar]
- Nef, T.; Mihelj, M.; Riener, R. ARMin: A robot for patient-cooperative arm therapy. Med. Biol. Eng. Comput. 2007, 45, 887–900. [Google Scholar] [CrossRef]
- Huang, J.; Tu, X.; He, J. Design and evaluation of the RUPERT wearable upper extremity exoskeleton robot for clinical and in-home therapies. IEEE Trans. Syst. Man Cybern. Syst. 2015, 46, 926–935. [Google Scholar] [CrossRef]
- Frisoli, A.; Chisari, C.; Sotgiu, E.; Procopio, C.; Fontana, M.; Rossi, B.; Bergamasco, M. Rehabilitation training and evaluation with the L-EXOS in chronic stroke. In Proceedings of the International Conference on Smart Homes and Health Telematics, Singapore, 10–12 July 2018; pp. 242–245. [Google Scholar]
- Byl, N.N.; Abrams, G.M.; Pitsch, E.; Fedulow, I.; Kim, H.; Simkins, M.; Nagarajan, S.; Rosen, J. Chronic stroke survivors achieve comparable outcomes following virtual task specific repetitive training guided by a wearable robotic orthosis (UL-EXO7) and actual task specific repetitive training guided by a physical therapist. J. Hand Ther. 2013, 26, 343–352. [Google Scholar] [CrossRef]
- Kim, H.; Miller, L.M.; Fedulow, I.; Simkins, M.; Abrams, G.M.; Byl, N.; Rosen, J. Kinematic data analysis for post-stroke patients following bilateral versus unilateral rehabilitation with an upper limb wearable robotic system. IEEE Trans. Neural Syst. Rehabil. Eng. 2012, 21, 153–164. [Google Scholar] [CrossRef] [PubMed]
- Wolbrecht, E.T.; Leavitt, J.; Reinkensmeyer, D.J.; Bobrow, J.E. Control of a pneumatic orthosis for upper extremity stroke rehabilitation. In Proceedings of the 2006 International Conference of the IEEE Engineering in Medicine and Biology Society, New York, NY, USA, 30 August–3 September 2006; pp. 2687–2693. [Google Scholar]
- Park, H.-S.; Ren, Y.; Zhang, L.-Q. IntelliArm: An exoskeleton for diagnosis and treatment of patients with neurological impairments. In Proceedings of the 2008 2nd IEEE RAS & EMBS International Conference on Biomedical Robotics and Biomechatronics, Scottsdale, AZ, USA, 19–22 October 2008; pp. 109–114. [Google Scholar]
- Milot, M.-H.; Spencer, S.J.; Chan, V.; Allington, J.P.; Klein, J.; Chou, C.; Bobrow, J.E.; Cramer, S.C.; Reinkensmeyer, D.J. A crossover pilot study evaluating the functional outcomes of two different types of robotic movement training in chronic stroke survivors using the arm exoskeleton BONES. J. NeuroEng. Rehabil. 2013, 10, 112. [Google Scholar] [CrossRef] [PubMed]
- Loureiro, R.C.; Harwin, W.S. Reach & grasp therapy: Design and control of a 9-DOF robotic neuro-rehabilitation system. In Proceedings of the 2007 IEEE 10th International Conference on Rehabilitation Robotics, Noordwijk, The Netherlands, 13–15 June 2007; pp. 757–763. [Google Scholar]
- Fazekas, G.; Horvath, M.; Troznai, T.; Toth, A. Robot-mediated upper limb physiotherapy for patients with spastic hemiparesis: A preliminary study. J. Rehabil. Med. 2007, 39, 580–582. [Google Scholar] [CrossRef] [PubMed]
- Housman, S.J.; Le, V.; Rahman, T.; Sanchez, R.J.; Reinkensmeyer, D.J. Arm-training with T-WREX after chronic stroke: Preliminary results of a randomized controlled trial. In Proceedings of the 2007 IEEE 10th International Conference on Rehabilitation Robotics, Noordwijk, The Netherlands, 13–15 June 2007; pp. 562–568. [Google Scholar]
- Colomer, C.; Baldovi, A.; Torromé, S.; Navarro, M.; Moliner, B.; Ferri, J.; Noé, E. Efficacy of Armeo® Spring during the chronic phase of stroke. Study in mild to moderate cases of hemiparesis. Neurologia 2013, 28, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Jarrasse, N.; Proietti, T.; Crocher, V.; Robertson, J.; Sahbani, A.; Morel, G.; Roby-Brami, A. Robotic exoskeletons: A perspective for the rehabilitation of arm coordination in stroke patients. Front. Hum. Neurosci 2014, 8, 947. [Google Scholar] [CrossRef] [PubMed]
- Maclean, N.; Pound, P.; Wolfe, C.; Rudd, A. Qualitative analysis of stroke patients’ motivation for rehabilitation. BMJ 2000, 321, 1051–1054. [Google Scholar] [CrossRef]
- Fazekas, G.; Tavaszi, I. The future role of robots in neuro-rehabilitation. Expert Rev. Neurother. 2019, 19, 471–473. [Google Scholar] [CrossRef]
- Morales, R.; Badesa, F.J.; Garcia-Aracil, N.; Sabater, J.M.; Perez-Vidal, C. Pneumatic robotic systems for upper limb rehabilitation. Med. Biol. Eng. Comput. 2011, 49, 1145–1156. [Google Scholar] [CrossRef]
- Song, Z.B.; Guo, S.X.; Pang, M.Y.; Zhang, S.Y.; Xiao, N.; Gao, B.F.; Shi, L.W. Implementation of Resistance Training Using an Upper-Limb Exoskeleton Rehabilitation Device for Elbow Joint. J. Med. Biol. Eng. 2014, 34, 188–196. [Google Scholar] [CrossRef]
- Hogan, N. Impedance Control—An Approach to Manipulation 1. Theory. J. Dyn. Syst. Meas. Control 1985, 107, 1–7. [Google Scholar] [CrossRef]
- Rahman, M.H.; Saad, M.; Kenne, J.P.; Archambault, P.S. Control of an Exoskeleton Robot Arm with Sliding Mode Exponential Reaching Law. Int. J. Control Autom. 2013, 11, 92–104. [Google Scholar] [CrossRef]
- Kiguchi, K.; Quan, Q. Muscle-Model-Oriented EMG-Based Control of an Upper-Limb Power-Assist Exoskeleton with a Neuro-Fuzzy Modifier. In Proceedings of the 2008 IEEE International Conference on Fuzzy Systems, Hong Kong, China, 1–6 June 2008; pp. 1181–1186. [Google Scholar]
- Buchanan, T.S.; Lloyd, D.G.; Manal, K.; Besier, T.F. Neuromusculoskeletal modeling: Estimation of muscle forces and joint moments and movements from measurements of neural command. J. Appl. Biomech. 2004, 20, 367–395. [Google Scholar] [CrossRef] [PubMed]
- Blank, A.; O’Malley, M.K.; Francisco, G.E.; Contreras-Vidal, J.L. A Pre-Clinical Framework for Neural Control of a Therapeutic Upper-Limb Exoskeleton. In Proceedings of the 2013 6th International IEEE/EMBS Conference on Neural Engineering (NER), San Diego, CA, USA, 6–8 November 2013; pp. 1159–1162. [Google Scholar]
- Lauretti, C.; Cordella, F.; Ciancio, A.L.; Trigili, E.; Catalan, J.M.; Badesa, F.J.; Crea, S.; Pagliara, S.M.; Sterzi, S.; Vitiello, N. Learning by demonstration for motion planning of upper-limb exoskeletons. Front. Neurorobot. 2018, 12, 5. [Google Scholar] [CrossRef] [PubMed]
- Guidali, M.; Schmiedeskamp, M.; Klamroth, V.; Riener, R. Assessment and training of synergies with an arm rehabilitation robot. In Proceedings of the 2009 IEEE 11th International Conference on Rehabilitation Robotics, Kyoto, Japan, 23–26 June 2009; pp. 899–903. [Google Scholar]
- Masia, L.; Casadio, M.; Sandini, G.; Morasso, P. Eye-hand coordination during dynamic visuomotor rotations. PLoS ONE 2009, 4, e7004. [Google Scholar] [CrossRef] [PubMed]
- Semprini, M.; Laffranchi, M.; Sanguineti, V.; Avanzino, L.; De Icco, R.; De Michieli, L.; Chiappalone, M. Technological approaches for neurorehabilitation: From robotic devices to brain stimulation and beyond. Front. Neurol. 2018, 9, 212. [Google Scholar] [CrossRef] [PubMed]
- Hesse, S.; Uhlenbrock, D. A mechanized gait trainer for restoration of gait. J. Rehabil. Res. Dev. 2000, 37, 701–708. [Google Scholar]
- Schmidt, H.; Hesse, S.; Bernhardt, R.; Krüger, J. HapticWalker—A novel haptic foot device. ACM Trans. Appl. Percept. 2005, 2, 166–180. [Google Scholar] [CrossRef]
- Hesse, S.; Waldner, A.; Tomelleri, C. Innovative gait robot for the repetitive practice of floor walking and stair climbing up and down in stroke patients. J. NeuroEng. Rehabil. 2010, 7, 30. [Google Scholar] [CrossRef]
- Schmidt, H.; Werner, C.; Bernhardt, R.; Hesse, S.; Krüger, J. Gait rehabilitation machines based on programmable footplates. J. NeuroEng. Rehabil. 2007, 4, 2. [Google Scholar] [CrossRef]
- Squeri, V.; De Luca, A.; Cella, A.; Vallone, F.; Siri, G.; Zigoura, E.; Giorgeschi, A.; Tavella, E.; Puntoni, M.; Avella, M. Robotic evaluation of fall risk in older people: Results on trunk parameters in static and dynamic balance conditions by hunova robot. Ann. Phys. Rehabil. Med. 2018, 61, e339. [Google Scholar] [CrossRef]
- Girone, M.; Burdea, G.; Bouzit, M.; Popescu, V.; Deutsch, J.E. A Stewart platform-based system for ankle telerehabilitation. Auton. Robot. 2001, 10, 203–212. [Google Scholar] [CrossRef]
- Zhang, M.; Davies, T.C.; Xie, S. Effectiveness of robot-assisted therapy on ankle rehabilitation–a systematic review. J. NeuroEng. Rehabil. 2013, 10, 30. [Google Scholar] [CrossRef]
- Saglia, J.A.; Tsagarakis, N.G.; Dai, J.S.; Caldwell, D.G. A high-performance redundantly actuated parallel mechanism for ankle rehabilitation. Int. J. Robot. Res. 2009, 28, 1216–1227. [Google Scholar] [CrossRef]
- Saglia, J.A.; De Luca, A.; Squeri, V.; Ciaccia, L.; Sanfilippo, C.; Ungaro, S.; De Michieli, L. Design, Development and Clinical Results of a Novel Total-Body Rehabilitation Robot: Hunova®. In Proceedings of the 2019 IEEE 16th International Conference on Rehabilitation Robotics (ICORR), Toronto, ON, Canada, 24–28 June 2019; pp. 417–422. [Google Scholar]
- Werner, C.; Von Frankenberg, S.; Treig, T.; Konrad, M.; Hesse, S. Treadmill training with partial body weight support and an electromechanical gait trainer for restoration of gait in subacute stroke patients: A randomized crossover study. Stroke 2002, 33, 2895–2901. [Google Scholar] [CrossRef]
- Mehrholz, J.; Pohl, M. Electromechanical-assisted gait training after stroke: A systematic review comparing end-effector and exoskeleton devices. J. Rehabil. Med. 2012, 44, 193–199. [Google Scholar] [CrossRef]
- Gandolfi, M.; Geroin, C.; Picelli, A.; Munari, D.; Waldner, A.; Tamburin, S.; Marchioretto, F.; Smania, N. Robot-assisted vs. sensory integration training in treating gait and balance dysfunctions in patients with multiple sclerosis: A randomized controlled trial. Front. Hum. Neurosci. 2014, 8, 318. [Google Scholar] [CrossRef]
- Picelli, A.; Melotti, C.; Origano, F.; Waldner, A.; Fiaschi, A.; Santilli, V.; Smania, N. Robot-assisted gait training in patients with Parkinson disease: A randomized controlled trial. Neurorehabil. Neural Repair 2012, 26, 353–361. [Google Scholar] [CrossRef]
- Smania, N.; Bonetti, P.; Gandolfi, M.; Cosentino, A.; Waldner, A.; Hesse, S.; Werner, C.; Bisoffi, G.; Geroin, C.; Munari, D. Improved gait after repetitive locomotor training in children with cerebral palsy. Am. J. Phys. Med. Rehabil 2011, 90, 137–149. [Google Scholar] [CrossRef]
- Taglione, E.; Catitti, P.; D’Angelo, M.; Squeri, V.; Saglia, J.; Sanfilippo, C.; De Michieli, L. Proprioceptive and motor training using the high performance robotic device hunova: Protocol of a randomized, controlled trial in patients with lower limb post-traumatic conditions. Ann. Phys. Rehabil. Med. 2018, 61, e497–e498. [Google Scholar] [CrossRef]
- Jezernik, S.; Colombo, G.; Keller, T.; Frueh, H.; Morari, M. Robotic orthosis lokomat: A rehabilitation and research tool. Neuromodul. Technol. Neural Interface 2003, 6, 108–115. [Google Scholar] [CrossRef]
- Freivogel, S.; Mehrholz, J.; Husak-Sotomayor, T.; Schmalohr, D. Gait training with the newly developed ‘LokoHelp’-system is feasible for non-ambulatory patients after stroke, spinal cord and brain injury. A feasibility study. Brain Inj. 2008, 22, 625–632. [Google Scholar] [CrossRef]
- Veneman, J.F.; Kruidhof, R.; Hekman, E.E.; Ekkelenkamp, R.; Van Asseldonk, E.H.; Van Der Kooij, H. Design and evaluation of the LOPES exoskeleton robot for interactive gait rehabilitation. IEEE Trans. Neural Syst. Rehabil. Eng. 2007, 15, 379–386. [Google Scholar] [CrossRef]
- Banala, S.K.; Agrawal, S.K.; Scholz, J.P. Active Leg Exoskeleton (ALEX) for Gait Rehabilitation of Motor-Impaired Patients. In Proceedings of the 2007 IEEE 10th International Conference on Rehabilitation Robotics, Noordwijk, The Netherlands, 13–15 June 2007; pp. 401–407. [Google Scholar]
- Kolakowsky-Hayner, S.A.; Crew, J.; Moran, S.; Shah, A. Safety and feasibility of using the EksoTM bionic exoskeleton to aid ambulation after spinal cord injury. J. Spine 2013, 4. [Google Scholar] [CrossRef]
- Zeilig, G.; Weingarden, H.; Zwecker, M.; Dudkiewicz, I.; Bloch, A.; Esquenazi, A. Safety and tolerance of the ReWalk™ exoskeleton suit for ambulation by people with complete spinal cord injury: A pilot study. J. Spinal Cord Med. 2012, 35, 96–101. [Google Scholar] [CrossRef]
- Farris, R.J.; Quintero, H.A.; Murray, S.A.; Ha, K.H.; Hartigan, C.; Goldfarb, M. A preliminary assessment of legged mobility provided by a lower limb exoskeleton for persons with paraplegia. IEEE Trans. Neural Syst. Rehabil. Eng. 2013, 22, 482–490. [Google Scholar] [CrossRef]
- Kotov, S.; Lijdvoy, V.; Sekirin, A.; Petrushanskaya, K.; Pismennaya, E. The efficacy of the exoskeleton ExoAtlet to restore walking in patients with multiple sclerosis. Zhurnal Nevrol. Psikhiatrii Im. SS Korsakova 2017, 117, 41–47. [Google Scholar] [CrossRef]
- He, Y.; Eguren, D.; Azorín, J.M.; Grossman, R.G.; Luu, T.P.; Contreras-Vidal, J.L. Brain–machine interfaces for controlling lower-limb powered robotic systems. J. Neural Eng. 2018, 15, 021004. [Google Scholar] [CrossRef]
- Louie, D.R.; Eng, J.J. Powered robotic exoskeletons in post-stroke rehabilitation of gait: A scoping review. J. NeuroEng. Rehabil. 2016, 13, 53. [Google Scholar] [CrossRef]
- Kazerooni, H.; Steger, R.; Huang, L. Hybrid control of the Berkeley lower extremity exoskeleton (BLEEX). Int. J. Robot. Res. 2006, 25, 561–573. [Google Scholar] [CrossRef]
- Bastian, A.J. Understanding sensorimotor adaptation and learning for rehabilitation. Curr. Opin. Neurol. 2008, 21, 628. [Google Scholar] [CrossRef]
- Huang, V.S.; Krakauer, J.W. Robotic neurorehabilitation: A computational motor learning perspective. J. NeuroEng. Rehabil. 2009, 6, 5. [Google Scholar] [CrossRef]
- Duschau-Wicke, A.; von Zitzewitz, J.; Caprez, A.; Lunenburger, L.; Riener, R. Path control: A method for patient-cooperative robot-aided gait rehabilitation. IEEE Trans. Neural Syst. Rehabil. Eng. 2009, 18, 38–48. [Google Scholar] [CrossRef]
- Wu, H.G.; Miyamoto, Y.R.; Castro, L.N.G.; Ölveczky, B.P.; Smith, M.A. Temporal structure of motor variability is dynamically regulated and predicts motor learning ability. Nat. Neurosci. 2014, 17, 312. [Google Scholar] [CrossRef]
- Duschau-Wicke, A.; Caprez, A.; Riener, R. Patient-cooperative control increases active participation of individuals with SCI during robot-aided gait training. J. NeuroEng. Rehabil. 2010, 7, 43. [Google Scholar] [CrossRef]
- Grazi, L.; Crea, S.; Parri, A.; Molino Lova, R.; Micera, S.; Vitiello, N. Gastrocnemius myoelectric control of a robotic hip exoskeleton can reduce the user’s lower-limb muscle activities at push off. Front. Neurosci. 2018, 12, 71. [Google Scholar] [CrossRef]
- Kawamoto, H.; Taal, S.; Niniss, H.; Hayashi, T.; Kamibayashi, K.; Eguchi, K.; Sankai, Y. Voluntary motion support control of Robot Suit HAL triggered by bioelectrical signal for hemiplegia. In Proceedings of the 2010 Annual International Conference of the IEEE Engineering in Medicine and Biology, Buenos Aires, Argentina, 31 August–4 September 2010; pp. 462–466. [Google Scholar]
- Westlake, K.P.; Patten, C. Pilot study of Lokomat versus manual-assisted treadmill training for locomotor recovery post-stroke. J. NeuroEng. Rehabil. 2009, 6, 18. [Google Scholar] [CrossRef]
- Nam, K.Y.; Kim, H.J.; Kwon, B.S.; Park, J.-W.; Lee, H.J.; Yoo, A. Robot-assisted gait training (Lokomat) improves walking function and activity in people with spinal cord injury: A systematic review. J. NeuroEng. Rehabil. 2017, 14, 24. [Google Scholar] [CrossRef]
- Lo, A.C.; Chang, V.C.; Gianfrancesco, M.A.; Friedman, J.H.; Patterson, T.S.; Benedicto, D.F. Reduction of freezing of gait in Parkinson’s disease by repetitive robot-assisted treadmill training: A pilot study. J. NeuroEng. Rehabil. 2010, 7, 51. [Google Scholar] [CrossRef]
- Lo, A.C.; Triche, E.W. Improving gait in multiple sclerosis using robot-assisted, body weight supported treadmill training. Neurorehabil. Neural Repair 2008, 22, 661–671. [Google Scholar] [CrossRef]
- Borggraefe, I.; Schaefer, J.S.; Klaiber, M.; Dabrowski, E.; Ammann-Reiffer, C.; Knecht, B.; Berweck, S.; Heinen, F.; Meyer-Heim, A. Robotic-assisted treadmill therapy improves walking and standing performance in children and adolescents with cerebral palsy. Eur. J. Paediatr. Neurol. 2010, 14, 496–502. [Google Scholar] [CrossRef]
- Esquenazi, A.; Lee, S.; Wikoff, A.; Packel, A.; Toczylowski, T.; Feeley, J. A Comparison of Locomotor Therapy Interventions: Partial-Body Weight− Supported Treadmill, Lokomat, and G-EO Training in People With Traumatic Brain Injury. PMR 2017, 9, 839–846. [Google Scholar] [CrossRef]
- Van Asseldonk, E.H.; van der Kooij, H. Robot-aided gait training with LOPES. In Neurorehabilitation Technology; Springer: Berlin, Germany, 2016; pp. 461–481. [Google Scholar]
- Fleerkotte, B.M.; Koopman, B.; Buurke, J.H.; van Asseldonk, E.H.; van der Kooij, H.; Rietman, J.S. The effect of impedance-controlled robotic gait training on walking ability and quality in individuals with chronic incomplete spinal cord injury: An explorative study. J. NeuroEng. Rehabil. 2014, 11, 26. [Google Scholar] [CrossRef]
- Banala, S.K.; Kim, S.H.; Agrawal, S.K.; Scholz, J.P. Robot assisted gait training with active leg exoskeleton (ALEX). In Proceedings of the 2008 2nd IEEE RAS & EMBS International Conference on Biomedical Robotics and Biomechatronics, Scottsdale, AZ, USA, 19–22 October 2008; pp. 653–658. [Google Scholar]
- Baunsgaard, C.B.; Nissen, U.V.; Brust, A.K.; Frotzler, A.; Ribeill, C.; Kalke, Y.-B.; León, N.; Gómez, B.; Samuelsson, K.; Antepohl, W. Gait training after spinal cord injury: Safety, feasibility and gait function following 8 weeks of training with the exoskeletons from Ekso Bionics. Spinal Cord 2018, 56, 106. [Google Scholar] [CrossRef]
- Calabrò, R.S.; Naro, A.; Russo, M.; Bramanti, P.; Carioti, L.; Balletta, T.; Buda, A.; Manuli, A.; Filoni, S.; Bramanti, A. Shaping neuroplasticity by using powered exoskeletons in patients with stroke: A randomized clinical trial. J. NeuroEng. Rehabil. 2018, 15, 35. [Google Scholar] [CrossRef]
- Molteni, F.; Gasperini, G.; Gaffuri, M.; Colombo, M.; Giovanzana, C.; Lorenzon, C.; Farina, N.; Cannaviello, G.; Scarano, S.; Proserpio, D. Wearable robotic exoskeleton for overground gait training in sub-acute and chronic hemiparetic stroke patients: Preliminary results. Eur. J. Phys. Rehabil. Med. 2017, 53, 676–684. [Google Scholar]
- Benson, I.; Hart, K.; Tussler, D.; van Middendorp, J.J. Lower-limb exoskeletons for individuals with chronic spinal cord injury: Findings from a feasibility study. Clin. Rehabil. 2016, 30, 73–84. [Google Scholar] [CrossRef]
- Esquenazi, A.; Talaty, M.; Packel, A.; Saulino, M. The ReWalk powered exoskeleton to restore ambulatory function to individuals with thoracic-level motor-complete spinal cord injury. Am. J. Phys. Rehabil. Med. 2012, 91, 911–921. [Google Scholar] [CrossRef]
- Kozlowski, A.J.; Fabian, M.; Lad, D.; Delgado, A.D. Feasibility and safety of a powered exoskeleton for assisted walking for persons with multiple sclerosis: A single-group preliminary study. Arch. Phys. Med. Rehabil. 2017, 98, 1300–1307. [Google Scholar] [CrossRef]
- Hartigan, C.; Kandilakis, C.; Dalley, S.; Clausen, M.; Wilson, E.; Morrison, S.; Etheridge, S.; Farris, R. Mobility outcomes following five training sessions with a powered exoskeleton. Top. Spinal Cord Inj. Rehabil. 2015, 21, 93–99. [Google Scholar] [CrossRef]
- Murray, S.A.; Ha, K.H.; Goldfarb, M. An assistive controller for a lower-limb exoskeleton for rehabilitation after stroke, and preliminary assessment thereof. In Proceedings of the 2014 36th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Chicago, IL, USA, 26–30 August 2014; pp. 4083–4086. [Google Scholar]
- Laffranchi, M.; Semprini, M.; Manzan, E.; Cerruti, G.; Vassallo, C.; De Giuseppe, S.; Maludrottu, S.; Succi, A.; Chiappalone, M.; Gruppioni, E.; et al. A Novel Lower Limb Exoskeleton and new Neurorehabilitation-based Application Scenarios. In Proceedings of the 40th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC’18), Honolulu, HI, USA, 17–21 July 2018. [Google Scholar]
- Nilsson, A.; Vreede, K.S.; Häglund, V.; Kawamoto, H.; Sankai, Y.; Borg, J. Gait training early after stroke with a new exoskeleton–the hybrid assistive limb: A study of safety and feasibility. J. NeuroEng. Rehabil. 2014, 11, 92. [Google Scholar] [CrossRef]
- Wall, A.; Borg, J.; Palmcrantz, S. Clinical application of the Hybrid Assistive Limb (HAL) for gait training—A systematic review. Front. Syst. Neurosci. 2015, 9, 48. [Google Scholar] [CrossRef]
- Kubota, S.; Nakata, Y.; Eguchi, K.; Kawamoto, H.; Kamibayashi, K.; Sakane, M.; Sankai, Y.; Ochiai, N. Feasibility of rehabilitation training with a newly developed wearable robot for patients with limited mobility. Arch. Phys. Med. Rehabil. 2013, 94, 1080–1087. [Google Scholar] [CrossRef]
- Fitts, P.M.; Peterson, J.R. Information capacity of discrete motor responses. J. Exp. Psychol. 1964, 67, 103. [Google Scholar] [CrossRef]
- Ranganathan, R.; Newell, K.M. Changing up the routine: Intervention-induced variability in motor learning. Exerc. Sport Sci. Rev. 2013, 41, 64–70. [Google Scholar] [CrossRef]
- Cardis, M.; Casadio, M.; Ranganathan, R. High variability impairs motor learning regardless of whether it affects task performance. J. Neurophysiol. 2017, 119, 39–48. [Google Scholar] [CrossRef]
- Stefan, K.; Cohen, L.G.; Duque, J.; Mazzocchio, R.; Celnik, P.; Sawaki, L.; Ungerleider, L.; Classen, J. Formation of a motor memory by action observation. J. Neurosci. 2005, 25, 9339–9346. [Google Scholar] [CrossRef]
- Mattar, A.A.; Gribble, P.L. Motor learning by observing. Neuron 2005, 46, 153–160. [Google Scholar] [CrossRef]
- Hayes, S.J.; Elliott, D.; Bennett, S.J. General motor representations are developed during action-observation. Exp. Brain Res. 2010, 204, 199–206. [Google Scholar] [CrossRef]
- Hodges, N.J.; Williams, A.M.; Hayes, S.J.; Breslin, G. What is modelled during observational learning? J. Sports Sci. 2007, 25, 531–545. [Google Scholar] [CrossRef]
- Cuppone, A.V.; Semprini, M.; Konczak, J. Consolidation of human somatosensory memory during motor learning. Behav. Brain Res. 2018, 347, 184–192. [Google Scholar] [CrossRef]
- Ostry, D.J.; Gribble, P.L. Sensory plasticity in human motor learning. Trends Neurosci. 2016, 39, 114–123. [Google Scholar] [CrossRef]
- Cuppone, A.V.; Squeri, V.; Semprini, M.; Masia, L.; Konczak, J. Robot-assisted proprioceptive training with added vibro-tactile feedback enhances somatosensory and motor performance. PLoS ONE 2016, 11, e0164511. [Google Scholar] [CrossRef]
- Reinkensmeyer, D.J.; Burdet, E.; Casadio, M.; Krakauer, J.W.; Kwakkel, G.; Lang, C.E.; Swinnen, S.P.; Ward, N.S.; Schweighofer, N. Computational neurorehabilitation: Modeling plasticity and learning to predict recovery. J. NeuroEng. Rehabil. 2016, 13, 42. [Google Scholar] [CrossRef]
- Han, C.E.; Arbib, M.A.; Schweighofer, N. Stroke rehabilitation reaches a threshold. PLoS Comput. Biol. 2008, 4, e1000133. [Google Scholar] [CrossRef]
- Reinkensmeyer, D.J.; Guigon, E.; Maier, M.A. A computational model of use-dependent motor recovery following a stroke: Optimizing corticospinal activations via reinforcement learning can explain residual capacity and other strength recovery dynamics. Neural Netw. 2012, 29, 60–69. [Google Scholar] [CrossRef][Green Version]
- Zenzeri, J.; De Santis, D.; Morasso, P. Strategy switching in the stabilization of unstable dynamics. PLoS ONE 2014, 9, e99087. [Google Scholar] [CrossRef]
- Loram, I.D.; Lakie, M.; Gawthrop, P.J. Visual control of stable and unstable loads: What is the feedback delay and extent of linear time-invariant control? J. Physiol. 2009, 587, 1343–1365. [Google Scholar] [CrossRef]
- Burdet, E.; Osu, R.; Franklin, D.W.; Milner, T.E.; Kawato, M. The central nervous system stabilizes unstable dynamics by learning optimal impedance. Nature 2001, 414, 446. [Google Scholar] [CrossRef]
- Goršič, M.; Cikajlo, I.; Novak, D. Competitive and cooperative arm rehabilitation games played by a patient and unimpaired person: Effects on motivation and exercise intensity. J. NeuroEng. Rehabil. 2017, 14, 23. [Google Scholar] [CrossRef]
- Novak, D.; Nagle, A.; Keller, U.; Riener, R. Increasing motivation in robot-aided arm rehabilitation with competitive and cooperative gameplay. J. NeuroEng. Rehabil. 2014, 11, 64. [Google Scholar] [CrossRef]
- Galofaro, E.; Morasso, P.; Zenzeri, J. Improving motor skill transfer during dyadic robot training through the modulation of the expert role. In Proceedings of the 2017 International Conference on Rehabilitation Robotics (ICORR), London, UK, 17-20 July 2017; pp. 78–83. [Google Scholar]
- Avila Mireles, E.J.; Zenzeri, J.; Squeri, V.; Morasso, P.; De Santis, D. Skill learning and skill transfer mediated by cooperative haptic interaction. IEEE Trans. Neural Syst. Rehabil. Eng. 2017, 25, 832–843. [Google Scholar] [CrossRef]
- Birbaumer, N. Breaking the silence: Brain–computer interfaces (BCI) for communication and motor control. Psychophysiology 2006, 43, 517–532. [Google Scholar] [CrossRef]
- Wolpaw, J.R.; Birbaumer, N.; McFarland, D.J.; Pfurtscheller, G.; Vaughan, T.M. Brain–computer interfaces for communication and control. Clin. Neurophysiol. 2002, 113, 767–791. [Google Scholar] [CrossRef]
- Ganguly, K.; Carmena, J.M. Emergence of a stable cortical map for neuroprosthetic control. PLoS Biol. 2009, 7, e1000153. [Google Scholar] [CrossRef]
- Venkatakrishnan, A.; Francisco, G.E.; Contreras-Vidal, J.L. Applications of brain–machine interface systems in stroke recovery and rehabilitation. Curr. Phys. Med. Rehabil. Rep. 2014, 2, 93–105. [Google Scholar] [CrossRef]
- Biasiucci, A.; Leeb, R.; Iturrate, I.; Perdikis, S.; Al-Khodairy, A.; Corbet, T.; Schnider, A.; Schmidlin, T.; Zhang, H.; Bassolino, M. Brain-actuated functional electrical stimulation elicits lasting arm motor recovery after stroke. Nat. Commun. 2018, 9, 2421. [Google Scholar] [CrossRef]
- Luu, T.P.; Nakagome, S.; He, Y.; Contreras-Vidal, J.L. Real-time EEG-based brain-computer interface to a virtual avatar enhances cortical involvement in human treadmill walking. Sci. Rep. 2017, 7, 8895. [Google Scholar] [CrossRef]
- Ramos-Murguialday, A.; Khanna, P.; Sarasola-sanz, A.; Irastorza-Landa, N.; Klein, J.; Jung, J.H.; Garzo, A.; Santisteban, L.; Chueca, C.; Lopez-larraz, E.; et al. A novel implantable hybrid brain-machine-interface (BMI) for motor rehabilitation in stroke patients. In Proceedings of the 2019 9th International IEEE/EMBS Conference on Neural Engineering (NER), San Francisco, CA, USA, 20–23 March 2019. [Google Scholar]
- Maggioni, S.; Melendez-Calderon, A.; van Asseldonk, E.; Klamroth-Marganska, V.; Lünenburger, L.; Riener, R.; van der Kooij, H. Robot-aided assessment of lower extremity functions: A review. J. NeuroEng. Rehabil. 2016, 13, 72. [Google Scholar] [CrossRef]
- Cerasa, A.; Pignolo, L.; Gramigna, V.; Serra, S.; Olivadese, G.; Roccca, F.; Perrotta, P.; Dolce, G.; Quattrone, A.; Tonin, P. Exoskeleton-robot assisted therapy in stroke patients: A lesion mapping study. Front. Neuroinform. 2018, 12, 44. [Google Scholar] [CrossRef]
- Sczesny-Kaiser, M.; Höffken, O.; Lissek, S.; Lenz, M.; Schlaffke, L.; Nicolas, V.; Meindl, R.; Aach, M.; Sankai, Y.; Schildhauer, T.A. Neurorehabilitation in chronic paraplegic patients with the HAL® exoskeleton–preliminary electrophysiological and fMRI data of a pilot study. In Converging Clinical and Engineering Research on Neurorehabilitation; Springer: Berlin, Germany, 2013; pp. 611–615. [Google Scholar]
- Várkuti, B.; Guan, C.; Pan, Y.; Phua, K.S.; Ang, K.K.; Kuah, C.W.K.; Chua, K.; Ang, B.T.; Birbaumer, N.; Sitaram, R. Resting state changes in functional connectivity correlate with movement recovery for BCI and robot-assisted upper-extremity training after stroke. Neurorehabil. Neural Repair 2013, 27, 53–62. [Google Scholar] [CrossRef]
- DeMatteo, C.; Law, M.; Russell, D.; Pollock, N.; Rosenbaum, P.; Walter, S. The reliability and validity of the Quality of Upper Extremity Skills Test. Phys. Occup. Ther. Pediatr. 1993, 13, 1–18. [Google Scholar] [CrossRef]
- Bohannon, R.W.; Smith, M.B. Interrater Reliability of a Modified Ashworth Scale of Muscle Spasticity. Phys. Ther. 1987, 67, 206–207. [Google Scholar] [CrossRef]
- Duncan, P.W.; Propst, M.; Nelson, S.G. Reliability of the Fugl-Meyer Assessment of Sensorimotor Recovery Following Cerebrovascular Accident. Phys. Ther. 1983, 63, 1606–1610. [Google Scholar] [CrossRef]
- Randall, M.; Carlin, J.B.; Chondros, P.; Reddihough, D. Reliability of the Melbourne Assessment of Unilateral Upper Limb Function. Dev. Med. Child Neurol. 2001, 43, 761–767. [Google Scholar] [CrossRef]
- Mathiowetz, V.; Volland, G.; Kashman, N.; Weber, K. Adult norms for the Box and Block Test of manual dexterity. Am. J. Occup. Ther. 1985, 39, 386–391. [Google Scholar] [CrossRef]
- Lincoln, N.; Jackson, J.; Adams, S. Reliability and revision of the Nottingham Sensory Assessment for stroke patients. Physiotherapy 1998, 84, 358–365. [Google Scholar] [CrossRef]
- Winward, C.E.; Halligan, P.W.; Wade, D.T. The Rivermead Assessment of Somatosensory Performance (RASP): Standardization and reliability data. Clin. Rehabil. 2002, 16, 523–533. [Google Scholar] [CrossRef]
- Lephart, S.M.; Warner, J.J.; Borsa, P.A.; Fu, F.H. Proprioception of the shoulder joint in healthy, unstable, and surgically repaired shoulders. J. Shoulder Elb. Surg. 1994, 3, 371–380. [Google Scholar] [CrossRef]
- Lephart, S.M.; Kocher, M.S.; Fu, F.H.; Borsa, P.A.; Harner, C.D. Proprioception following anterior cruciate ligament reconstruction. J. Sport Rehabil. 1992, 1, 188–196. [Google Scholar] [CrossRef]
- Gilman, S. Joint position sense and vibration sense: Anatomical organisation and assessment. J. Neurol. Neurosurg. Psychiatry 2002, 73, 473–477. [Google Scholar] [CrossRef]
- Mong, Y.; Teo, T.W.; Ng, S.S. 5-repetition sit-to-stand test in subjects with chronic stroke: Reliability and validity. Arch. Phys. Med. Rehabil. 2010, 91, 407–413. [Google Scholar] [CrossRef]
- Podsiadlo, D.; Richardson, S. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar]
- Watson, M.J. Refining the ten-metre walking test for use with neurologically impaired people. Physiotherapy 2002, 88, 386–397. [Google Scholar] [CrossRef]
- Lanska, D.J.; Goetz, C.G. Romberg’s sign: Development, adoption, and adaptation in the 19th century. Neurology 2000, 55, 1201–1206. [Google Scholar] [CrossRef]
- Blum, L.; Korner-Bitensky, N. Usefulness of the Berg Balance Scale in stroke rehabilitation: A systematic review. Phys. Ther. 2008, 88, 559–566. [Google Scholar] [CrossRef]
- Barnes, M.P.; Dobkin, B.H.; Bogousslavsky, J. Recovery after Stroke; Cambridge University Press: Cambridge, UK, 2005. [Google Scholar]
- Maulden, S.A.; Gassaway, J.; Horn, S.D.; Smout, R.J.; DeJong, G. Timing of initiation of rehabilitation after stroke. Arch. Phys. Med. Rehabil. 2005, 86, 34–40. [Google Scholar] [CrossRef]
- Feigenson, J.S.; McDowell, F.H.; Meese, P.; McCarthy, M.L.; Greenberg, S.D. Factors influencing outcome and length of stay in a stroke rehabilitation unit. Part 1. Analysis of 248 unscreened patients--medical and functional prognostic indicators. Stroke 1977, 8, 651–656. [Google Scholar] [CrossRef]
- Dukelow, S.P.; Herter, T.M.; Moore, K.D.; Demers, M.J.; Glasgow, J.I.; Bagg, S.D.; Norman, K.E.; Scott, S.H. Quantitative assessment of limb position sense following stroke. Neurorehabil. Neural Repair 2010, 24, 178–187. [Google Scholar] [CrossRef]
- Lunenburger, L.; Colombo, G.; Riener, R.; Dietz, V. Clinical assessments performed during robotic rehabilitation by the gait training robot Lokomat. In Proceedings of the 9th International Conference on Rehabilitation Robotics (ICORR 2005), Chicago, IL, USA, 28 June–1 July 2005; pp. 345–348. [Google Scholar]
- Debert, C.T.; Herter, T.M.; Scott, S.H.; Dukelow, S. Robotic assessment of sensorimotor deficits after traumatic brain injury. J. Neurol. Phys. Ther. 2012, 36, 58–67. [Google Scholar] [CrossRef]
- Zarrugh, M.Y.; Todd, F.N.; Ralston, H.J. Optimization of energy expenditure during level walking. Eur. J. Appl. Physiol. Occup. Physiol. 1974, 33, 293–306. [Google Scholar] [CrossRef]
- Waters, R.L.; Mulroy, S. The energy expenditure of normal and pathologic gait. Gait Posture 1999, 9, 207–231. [Google Scholar] [CrossRef]
- Quinlivan, B.T.; Lee, S.; Malcolm, P.; Rossi, D.M.; Grimmer, M.; Siviy, C.; Karavas, N.; Wagner, D.; Asbeck, A.; Galiana, I.; et al. Assistance magnitude versus metabolic cost reductions for a tethered multiarticular soft exosuit. Sci. Robot. 2017, 2, eaah4416. [Google Scholar] [CrossRef]
- Gordon, D.F.N.; Henderson, G.; Vijayakumar, S. Effectively Quantifying the Performance of Lower-Limb Exoskeletons Over a Range of Walking Conditions. Front. Robot. AI 2018, 5. [Google Scholar] [CrossRef]
- Rich, C.; Ponsler, B.; Holroyd, A.; Sidner, C.L. Recognizing Engagement in Human-Robot Interaction. In Proceedings of the 5th ACM/IEEE International Conference on Human-Robot Interaction (HRI), Osaka, Japan, 2–5 March 2010; pp. 375–382. [Google Scholar]
- Sandini, G.; Mohan, V.; Sciutti, A.; Morasso, P. Social Cognition for Human-Robot Symbiosis-Challenges and Building Blocks. Front. Neurorobot. 2018, 12, 34. [Google Scholar] [CrossRef]
- Drejing, K.; Thill, S.; Hemeren, P. Engagement: A Traceable Motivational Concept in Human-Robot Interaction. In Proceedings of the 2015 International Conference on Affective Computing and Intelligent Interaction (ACII), Xi’an, China, 21–24 September 2015; pp. 956–961. [Google Scholar]
- Cornforth, D.J.; Koenig, A.; Riener, R.; August, K.; Khandoker, A.H.; Karmakar, C.; Palaniswami, M.; Jelinek, H.F. The role of serious games in robot exoskeleton-assisted rehabilitation of stroke patients. In Serious Games Analytics; Springer: Cham, Switzerland, 2015; pp. 233–254. [Google Scholar]
- He, B.; Sohrabpour, A.; Brown, E.; Liu, Z. Electrophysiological source imaging: A noninvasive window to brain dynamics. Annu. Rev. Biomed. Eng. 2018, 20, 171–196. [Google Scholar] [CrossRef]
- Liu, Q.; Farahibozorg, S.; Porcaro, C.; Wenderoth, N.; Mantini, D. Detecting large-scale networks in the human brain using high-density electroencephalography. Hum. Brain Mapp. 2017, 38, 4631–4643. [Google Scholar] [CrossRef]
- Seeber, M.; Cantonas, L.-M.; Hoevels, M.; Sesia, T.; Visser-Vandewalle, V.; Michel, C.M. Subcortical electrophysiological activity is detectable with high-density EEG source imaging. Nat. Commun. 2019, 10, 753. [Google Scholar] [CrossRef]
- Comani, S.; Velluto, L.; Schinaia, L.; Cerroni, G.; Serio, A.; Buzzelli, S.; Sorbi, S.; Guarnieri, B. Monitoring neuro-motor recovery from stroke with high-resolution EEG, robotics and virtual reality: A proof of concept. IEEE Trans. Neural Syst. Rehabil. Eng. 2015, 23, 1106–1116. [Google Scholar] [CrossRef]
- Formaggio, E.; Masiero, S.; Bosco, A.; Izzi, F.; Piccione, F.; Del Felice, A. Quantitative EEG evaluation during robot-assisted foot movement. IEEE Trans. Neural Syst. Rehabil. Eng. 2016, 25, 1633–1640. [Google Scholar] [CrossRef]
- Gandolfi, M.; Formaggio, E.; Geroin, C.; Storti, S.F.; Boscolo Galazzo, I.; Bortolami, M.; Saltuari, L.; Picelli, A.; Waldner, A.; Manganotti, P. Quantification of upper limb motor recovery and EEG power changes after robot-assisted bilateral arm training in chronic stroke patients: A prospective pilot study. Neural Plast. 2018, 2018, 8105480. [Google Scholar] [CrossRef]
- Caliandro, P.; Vecchio, F.; Miraglia, F.; Reale, G.; Della Marca, G.; La Torre, G.; Lacidogna, G.; Iacovelli, C.; Padua, L.; Bramanti, P. Small-world characteristics of cortical connectivity changes in acute stroke. Neurorehabil. Neural Repair 2017, 31, 81–94. [Google Scholar] [CrossRef]
- Fornito, A.; Zalesky, A.; Breakspear, M. The connectomics of brain disorders. Nat. Rev. Neurosci. 2015, 16, 159. [Google Scholar] [CrossRef]
- Lenne, B.; Blanc, J.-L.; Nandrino, J.-L.; Gallois, P.; Hautecæur, P.; Pezard, L. Decrease of mutual information in brain electrical activity of patients with relapsing-remitting multiple sclerosis. Behav. Neurol. 2013, 27, 201–212. [Google Scholar] [CrossRef]
- Wang, L.; Yu, C.; Chen, H.; Qin, W.; He, Y.; Fan, F.; Zhang, Y.; Wang, M.; Li, K.; Zang, Y. Dynamic functional reorganization of the motor execution network after stroke. Brain 2010, 133, 1224–1238. [Google Scholar] [CrossRef]
- Vahdat, S.; Darainy, M.; Thiel, A.; Ostry, D.J. A single session of robot-controlled proprioceptive training modulates functional connectivity of sensory motor networks and improves reaching accuracy in chronic stroke. Neurorehabil. Neural Repair 2019, 33, 70–81. [Google Scholar] [CrossRef]
- Carter, A.R.; Shulman, G.L.; Corbetta, M. Why use a connectivity-based approach to study stroke and recovery of function? Neuroimage 2012, 62, 2271–2280. [Google Scholar] [CrossRef]
- Faivre, A.; Rico, A.; Zaaraoui, W.; Crespy, L.; Reuter, F.; Wybrecht, D.; Soulier, E.; Malikova, I.; Confort-Gouny, S.; Cozzone, P.J. Assessing brain connectivity at rest is clinically relevant in early multiple sclerosis. Mult. Scler. J. 2012, 18, 1251–1258. [Google Scholar] [CrossRef]
- Wu, J.; Quinlan, E.B.; Dodakian, L.; McKenzie, A.; Kathuria, N.; Zhou, R.J.; Augsburger, R.; See, J.; Le, V.H.; Srinivasan, R. Connectivity measures are robust biomarkers of cortical function and plasticity after stroke. Brain 2015, 138, 2359–2369. [Google Scholar] [CrossRef]
- Faiman, I.; Pizzamiglio, S.; Turner, D.L. Resting-state functional connectivity predicts the ability to adapt arm reaching in a robot-mediated force field. Neuroimage 2018, 174, 494–503. [Google Scholar] [CrossRef]
- Meyer, T.; Peters, J.; Zander, T.O.; Schölkopf, B.; Grosse-Wentrup, M. Predicting motor learning performance from electroencephalographic data. J. NeuroEng. Rehabil. 2014, 11, 24. [Google Scholar] [CrossRef]
- Cole, D.M.; Smith, S.M.; Beckmann, C.F. Advances and pitfalls in the analysis and interpretation of resting-state FMRI data. Front. Syst. Neurosci. 2010, 4, 8. [Google Scholar] [CrossRef]
- Cesqui, B.; Tropea, P.; Micera, S.; Krebs, H.I. EMG-based pattern recognition approach in post stroke robot-aided rehabilitation: A feasibility study. J. NeuroEng. Rehabil. 2013, 10, 75. [Google Scholar] [CrossRef]
- Cheung, V.C.; Turolla, A.; Agostini, M.; Silvoni, S.; Bennis, C.; Kasi, P.; Paganoni, S.; Bonato, P.; Bizzi, E. Muscle synergy patterns as physiological markers of motor cortical damage. Proc. Natl. Acad. Sci. USA 2012, 109, 14652–14656. [Google Scholar] [CrossRef]
- Semprini, M.; Cuppone, A.V.; Delis, I.; Squeri, V.; Panzeri, S.; Konczak, J. Biofeedback signals for robotic rehabilitation: Assessment of wrist muscle activation patterns in healthy humans. IEEE Trans. Neural Syst. Rehabil. Eng. 2016, 25, 883–892. [Google Scholar] [CrossRef]
- Delis, I.; Panzeri, S.; Pozzo, T.; Berret, B. A unifying model of concurrent spatial and temporal modularity in muscle activity. J. Neurophysiol. 2013, 111, 675–693. [Google Scholar] [CrossRef]
- Liu, W.; Waller, S.M.; Kepple, T.; Whitall, J. Compensatory arm reaching strategies after stroke: Induced position analysis. J. Rehabil. Res. Dev. 2013, 50, 71. [Google Scholar] [CrossRef]
- Belfatto, A.; Scano, A.; Chiavenna, A.; Mastropietro, A.; Mrakic-Sposta, S.; Pittaccio, S.; Molinari Tosatti, L.; Molteni, F.; Rizzo, G. A Multiparameter Approach to Evaluate Post-Stroke Patients: An Application on Robotic Rehabilitation. Appl. Sci. 2018, 8, 2248. [Google Scholar] [CrossRef]
- Lamers, I.; Feys, P.; Swinnen, E. Robot-assisted rehabilitation in multiple sclerosis: Overview of approaches, clinical outcomes, and perspectives. In Rehabilitation Robotics; Elsevier: Amsterdam, The Netherlands, 2018; pp. 253–266. [Google Scholar]
- Young, A.J.; Ferris, D.P. State of the art and future directions for lower limb robotic exoskeletons. IEEE Trans. Neural Syst. Rehabil. Eng. 2016, 25, 171–182. [Google Scholar] [CrossRef]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).