Simplified Diagnosis of Mandibular Asymmetry in Panoramic Radiographs Through Digital Processing and Its Prospective Integration with Artificial Intelligence: A Pilot Study
Abstract
1. Introduction
2. Materials and Methods
- (1)
- Extraction of anatomical coordinates: A computer vision algorithm was implemented to automatically identify the anatomical points of interest marked in red on the digital panoramic radiographs. To do this, the OpenCV library was used, working in the HSV color space to isolate the pixels of this hue. Subsequently, morphological operations were applied to eliminate noise, and the relevant contours were located. The centers of mass of these contours were recorded as (X, Y) coordinates of the anatomical points, and the results were exported to a CSV file for further analysis.
- (2)
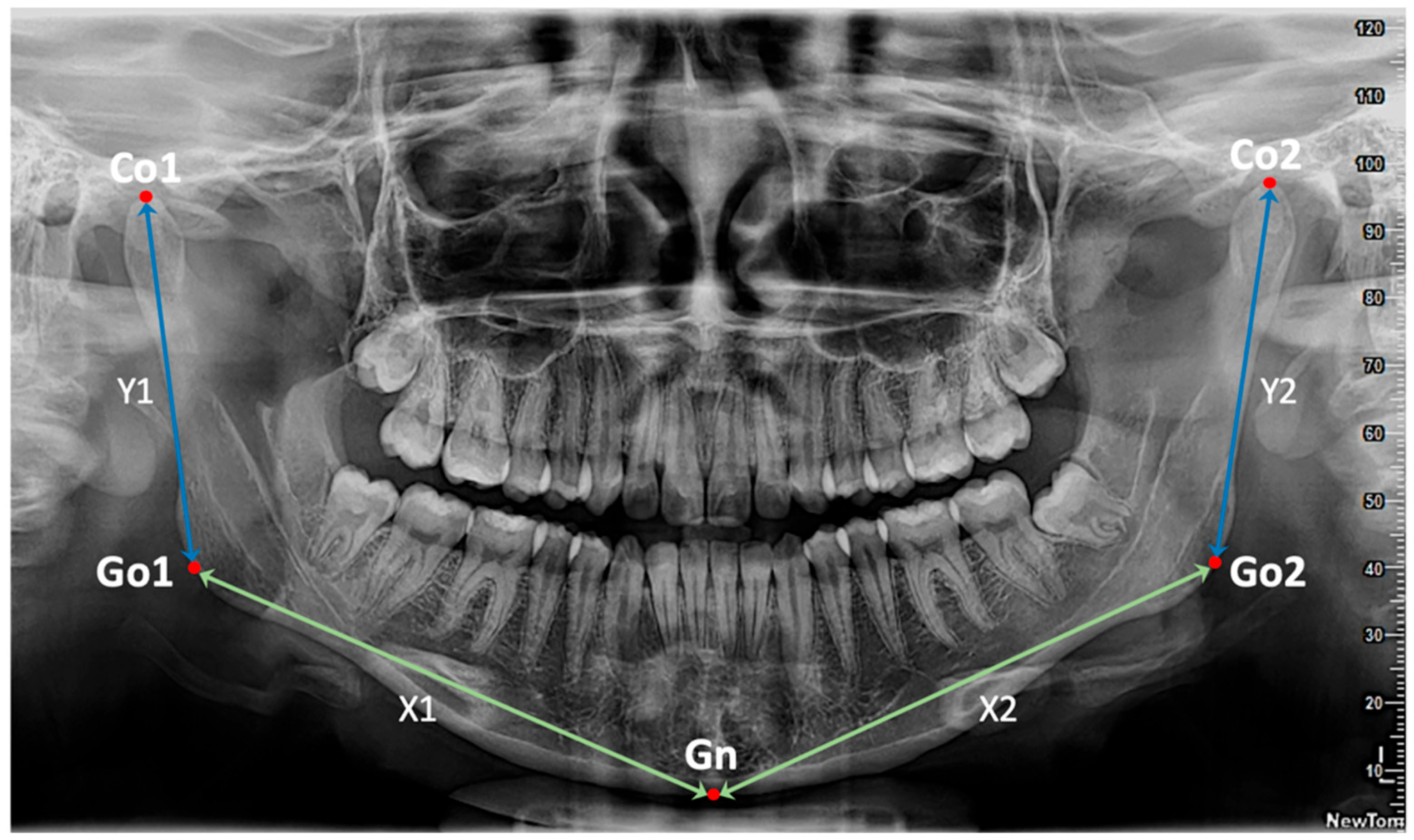
- Conversion and calculation of distances: the obtained coordinates were processed from the 5 anatomical landmarks (Co1, Go1, Gn, Go2, Co2) and representative linear measurements were extracted for the calculation of the 4 key Euclidean distances defined as, X1: distance between Go1 and Gn (right half of the mandibular body); X2: distance between Gn and Go2 (left half of the mandibular body); Y1: distance between Co1 and Go1 (right mandibular ramus); Y2: distance between Go2 and Co2 (left mandibular ramus). All obtained distances were converted from pixels to millimeters using a conversion factor specific to the analyzed images (0.10585 mm/pixel) (Figure 1).
- (3)
- Storage and analysis of results: The coordinate and distance data were organized in Excel spreadsheets using Pandas, which allowed for comparative descriptive analyses between the right and left sides of the mandible, evaluating the presence and magnitude of asymmetry in each radiographic image.
| Stage | Description |
|---|---|
| Stage 1: Extraction of anatomical coordinates | Detection of anatomical landmarks from panoramic radiographs using HSV masking; noise removal with morphological operations; contour filtering and centroid computation (X,Y). |
| Stage 2: Conversion & Distance Calculation | Conversion of pixel values to millimeters (scale factor 0.10585 mm/pixel); calculation of Euclidean distances (X1, X2, Y1, Y2); computation of differences (DIF X1–X2, DIF Y1–Y2); classification of asymmetry severity (≤3 mm, 3–6 mm, >6 mm). |
| Stage 3: Storage & Statistical Analysis | Storage of results in CSV/XLSX format; descriptive statistics; normality testing (Shapiro–Wilk); inferential statistics (paired t-test, Wilcoxon signed-rank test, Mann–Whitney U test). |
3. Results
- Right side (X1): mean of 73.94 mm (range: 67.93 to 81.64 mm).
- Left side (X2): mean of 73.79 mm (range: 66.82 to 80.86 mm).
- Right side (X1): range 66.81 to 105.86 mm.
- Left side (X2): range 70.87 to 106.47 mm.
- Right side (Y1): values ranged from 44.25 to 55.11 mm.
- Left side (Y2): values ranged from 43.73 to 55.44 mm.
- Normality was confirmed by the Shapiro–Wilk test (Y1, p = 0.597; Y2, p = 0.238), and no significant difference between sides was found using a paired t-test (p = 0.058).
- Right side (Y1): ranged from 46.30 to 82.31 mm.
- Left side (Y2): ranged from 45.20 to 74.79 mm.
- For DIF X1–X2: Shapiro–Wilk test showed normality for X1 (p = 0.480), but not for X2 (p = 0.005); the Mann–Whitney U test yielded a non-significant result (p = 0.074).
- For DIF Y1–Y2: normality was borderline or not met (Y1, p = 0.060; Y2, p = 0.033); the Mann–Whitney U test also indicated no significant difference (p = 0.233).
4. Discussion
5. Conclusions
- Successfully process radiographs from three different devices, suggesting adaptability to diverse image sources.
- Consistently calculate key anatomical distances (Co-Go and Go-Gn) bilaterally.
- Classify asymmetries according to severity in millimeters.
- Automatic detection of anatomical landmarks through convolutional neural networks.
- Multicenter validation with larger samples.
- Integration with radiological image management systems (PACS).
- Development of population-specific normative values.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cohen, M. Perspectives on craniofacial asymmetry. III. Common and/or well-known causes of asymmetry. Int. J. Oral Maxillofac. Surg. 1995, 24, 127–133. [Google Scholar] [CrossRef]
- Solem, R.; Ruellas, A.; Miller, A.; Kelly, K.; Ricks-Oddie, J.; Cevidanes, L. Congenital and acquired mandibular asymmetry: Mapping growth and remodeling in 3 dimensions. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 238–251. [Google Scholar] [CrossRef]
- Kumar, V.; Udupa, H. Mandibular asymmetry: Case discussion and literature review. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2019, 127, 39–40. [Google Scholar] [CrossRef]
- Edward, C.; Loy, C.; Richard, J. Classification and management of mandibular asymmetry. Am. J. Surg. 1960, 100, 825–834. [Google Scholar] [CrossRef] [PubMed]
- Leung, M.; Leung, Y. Three-dimensional evaluation of mandibular asymmetry: A new classification and three-dimensional cephalometric analysis. Int. J. Oral. Maxillofac. Surg. 2018, 47, 1043–1051. [Google Scholar] [CrossRef]
- Pinto, S.; Arriola, L. Prevalence of mandibular, condylar and ramus asymmetry in panoramic radiographs of adult individuals. A cross-sectional study. J. Clin. Exp. Dent. 2024, 16, e1332–e1338. [Google Scholar] [CrossRef] [PubMed]
- Evangelista, K.; Teodoro, A.; Bianchi, J.; Soares, L.; de Oliveira-Ruellas, A.; Garcia-Silva, M.; Valladares-Neto, J. Prevalence of mandibular asymmetry in different skeletal sagittal patterns: A systematic review. Angle Orthod. 2021, 92, 118–126. [Google Scholar] [CrossRef]
- Damstra, J.; Fourie, Z.; Ren, Y. Evaluation and comparison of postero-anterior cephalograms and cone-beam computed tomography images for the detection of mandibular asymmetry. Eur. J. Orthod. 2013, 35, 45–50. [Google Scholar] [CrossRef]
- Edler, R.; Wertheim, D.; Greenhill, D. Comparison of radiographic and photographic measurement of mandibular asymmetry. Am. J. Orthod. Dentofac. Orthop. 2003, 123, 167–174. [Google Scholar] [CrossRef]
- Van Elslande, D.; Russett, S.; Major, P.; Flores-Mir, C. Mandibular asymmetry diagnosis with panoramic imaging. Am. J. Orthod. Dentofac. Orthop. 2008, 134, 183–192. [Google Scholar] [CrossRef]
- La Rosa, S.; Leonardi, R.; Ronsivalle, V.; Cicciù, M.; Lo Giudice, A. Radiographic and diagnostic approaches for mandibular asymmetries in orthodontic practice: A narrative review. J. Clin. Pediatr. Dent. 2024, 48, 1–15. [Google Scholar] [CrossRef]
- Molteni, R. The way we were (and how we got here): Fifty years of technology changes in dental and maxillofacial radiology. Dentomaxillofac. Radiol. 2021, 50, 20200133. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Baan, F.; Bruggink, R.; Bronkhorst, E.; Liao, Y.; Ongkosuwito, E. Three-dimensional characterization of mandibular asymmetry in craniofacial microsomia. Clin. Oral Investig. 2020, 24, 4363–4372. [Google Scholar] [CrossRef]
- Mangal, U.; Han, A.; Huisoo, K.; Jung, Y.; Lee, K.; Yu, H.; Hwang, J.; Choi, S. Tomographic similarity scan with a computed modified absolute mandibular midsagittal plane for precise and objective localization of mandibular asymmetry. Comput. Biol. Med. 2021, 134, 104465. [Google Scholar] [CrossRef]
- Fan, Y.; Zhang, Y.; Chen, G.; He, W.; Song, G.; Matthews, H.; Claes, P.; Pei, Y.; Zha, H.; Penington, A.; et al. Automated assessment of mandibular shape asymmetry in 3 dimensions. Am. J. Orthod. Dentofac. Orthop. 2022, 161, 698–707. [Google Scholar] [CrossRef]
- Martins, L.; Brasil, D.; Forner, L.; Viccari, C.; Haiter-Neto, F.; Freitas, D.; Oliveira, M. Does dose optimisation in digital panoramic radiography affect diagnostic performance? Clin. Oral Investig. 2021, 25, 637–643. [Google Scholar] [CrossRef]
- Habets, L.L.; Bezuur, J.N.; Naeiji, M.; Hansson, T.L. The Orthopantomogram, an aid in diagnosis of temporomandibular joint problems. II. The vertical symmetry. J. Oral Rehabil. 1988, 15, 465–471. [Google Scholar] [CrossRef]
- Kjellberg, H.; Ekestubbe, A.; Kiliaridis, S.; Thilander, B. Condylar height on panoramic radiographs: A methodologic study with a clinical application. Acta Odontol. Scand. 1994, 52, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Niu, J.; Cheng, J.; Chen, Y.; Xie, Y.; Liu, H.; Lin, Y. Automated Assessment of Mandibular Asymmetry in Panoramic Radiography. In Proceedings of the IEEE 5th International Conference on Pattern Recognition and Machine Learning (PRML), Chongqing, China, 19–21 July 2024; pp. 421–428. [Google Scholar]
- Qu, W.; Qiu, Z.; Lam, K.C.; Sakaran, K.G.; Chen, H.; Lin, Y. Artificial intelligence-assisted identification and assessment of mandibular asymmetry on panoramic radiography. Am. J. Orthod. Dentofac. Orthop. 2025, 168, 14–23.e2. [Google Scholar] [CrossRef] [PubMed]
- Schwendicke, F.; Golla, T.; Dreher, M.; Krois, J. Convolutional neural networks for dental image diagnostics: A scoping review. J. Dent. 2019, 91, 103226. [Google Scholar] [CrossRef]
- Khanagar, S.; Al-Ehaideb, A.; Vishwanathaiah, S.; Maganur, P.; Patil, S.; Naik, S.; Baeshen, H.; Sarode, S. Scope and performance of artificial intelligence technology in orthodontic diagnosis, treatment planning, and clinical decision-making: A systematic review. J. Dent. Sci. 2020, 16, 482–492. [Google Scholar] [CrossRef]
- Bichu, Y.M.; Hansa, I.; Bichu, A.Y.; Premjani, P.; Flores-Mir, C.; Vaid, N.R. Applications of artificial intelligence and machine learning in orthodontics: A scoping review. Prog. Orthod. 2021, 22, 18. [Google Scholar] [CrossRef]
- Moore-Jansen, P.H.; Ousley, S.D.; Jantz, R.L. Data Collection Procedures for Forensic Skeletal Material; University of Tennessee: Knoxville, TN, USA, 1994. [Google Scholar]
- Azhari, A.; Pramatika, B.; Epsilawati, L. Differences between male and female mandibular length growth according to panoramic radiograph. Maj. Kedokt. Gigi Indones. 2019, 1, 43. [Google Scholar] [CrossRef][Green Version]
- Faryal, A.; Shaikh, A. Reliability of orthopantomogram in comparison to lateral cephalogram for linear mandibular measurements. J. Ayub Med. Coll. Abbottabad JAMC 2022, 34, 957–963. [Google Scholar] [CrossRef]
- Alfaro, C.; Ayala, R.; Barrientos, S.; Rodríguez, A. Mandibular Asymmetries Prevalence in Panoramic Radiographies in a Bogotá Colombia Population. Int. J. Morphol. 2016, 34, 1203–1206. [Google Scholar] [CrossRef]
- Lemos, A.; Katz, C.; Heimer, M.; Rosenblatt, A. Mandibular asymmetry: A proposal of radiographic analysis with public domain software. Dent. Press J. Orthod. 2014, 19, 52–58. [Google Scholar] [CrossRef]
- Al-Gunaid, T.H. Sex-related variation in the dimensions of the mandibular ramus and its relationship with lower third molar impaction. J. Taibah Univ. Med. Sci. 2020, 15, 298–304. [Google Scholar] [CrossRef]
- Mostafa, R.; El-Fotouh, M. Mandibular morphometric analysis for sex assessment: A retrospective radiographic study. J. Indian Acad. Oral Med. Radiol. 2020, 32, 266–270. [Google Scholar] [CrossRef]
- Kaur, R.; Pallagatti, S.; Aggarwal, A.; Mittal, P.G.; Singh, M.; Patel, M.L. Mandibular ramus as a strong expressor of sex determinations: A digital radiographic study. J. Pharm. Bioallied Sci. 2021, 13, 421–424. [Google Scholar] [CrossRef] [PubMed]
- Fekonja, A.; Čretnik, A. Gender and age differences in mandibular ramus and body measurements: A radiographic study. J. Hard Tissue Biol. 2022, 31, 9–14. [Google Scholar] [CrossRef]
- Stăncioiu, A.; Motofelea, A.; Hușanu, A.; Vasica, L.; Nagib, R.; Popa, A.; Szuhanek, C. Associations of digital measurements: Analysis of orthopantomography versus lateral cephalograms for evaluation of facial asymmetry. J. Clin. Med. 2025, 14, 1296. [Google Scholar] [CrossRef]
- Pereira, J.G.D.; Lima, K.F.; Da Silva, R.H.A. Mandibular measurements for sex and age estimation in Brazilian sampling. Acta Stomatol. Croat. 2020, 54, 294–301. [Google Scholar] [CrossRef] [PubMed]
- Cappella, A.; Gibelli, D.; Vitale, A.; Zago, M.; Dolci, C.; Sforza, C.; Cattaneo, C. Preliminary study on sexual dimorphism of metric traits of cranium and mandible in a modern Italian skeletal population and review of population literature. Leg. Med. 2020, 44, 101695. [Google Scholar] [CrossRef]
- Bento, M.I.C.; Crosato, E.M.; Santiago, B.M.; Soriano, E.P.; Carvalho, M.V.D.; Rabello, P.M.; Francesquini Júnior, L.; Almeida, A.C.; Campello, R.I.C. Quantitative analysis of the mandible for sex estimation. Res. Soc. Dev. 2021, 10, e45910414284. [Google Scholar] [CrossRef]
- Jena, A.K.; Singh, S.P.; Utreja, A. Effects of sagittal maxillary growth hypoplasia severity on mandibular asymmetry in unilateral cleft lip and palate subjects. Angle Orthod. 2011, 81, 872–877. [Google Scholar] [CrossRef]
- Ferro, F.; Spinella, P.; Lama, N. Transverse maxillary arch form and mandibular asymmetry in patients with posterior unilateral crossbite. Am. J. Orthod. Dentofac. Orthop. 2011, 140, 828–838. [Google Scholar] [CrossRef]
- Abad-Santamaría, L.; López-de-Andrés, A.; Jiménez-Trujillo, I.; Ruíz, C.; Romero, M. Effect of unilateral posterior crossbite and unilateral cleft lip and palate on vertical mandibular asymmetry. Ir. J. Med. Sci. 2014, 183, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Lim, Y.S.; Chung, D.H.; Lee, J.W.; Lee, S.M. Reliability and validity of mandibular posterior vertical asymmetry index in panoramic radiography compared with cone-beam computed tomography. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 558–567. [Google Scholar] [CrossRef]
- Bal, B.; Dikbas, I.; Malkondu, O.; Oral, K. Radiological study on mandibular ramus asymmetry in young population. Folia Morphol. 2018, 77, 724–729. [Google Scholar] [CrossRef]
- Hlatcu, A.; Galan, E.; Milicescu, S.; Teodorescu, E.; Ionescu, E. An evaluation of the ramus mandibular asymmetry on panoramic radiography. Appl. Sci. 2023, 13, 7645. [Google Scholar] [CrossRef]
- Laster, W.S.; Ludlow, J.B.; Bailey, L.J.; Hershey, H.G. Accuracy of measurements of mandibular anatomy and prediction of asymmetry in panoramic radiographic images. Dentomaxillofac. Radiol. 2005, 34, 343–349. [Google Scholar] [CrossRef] [PubMed]
- Fuentes, R.; Arellano-Villalón, M.; Soto-Faúndez, N.; Dias, F.; Navarro, P.; Arias, A. Condylar and mandibular symmetry indexes through digital panoramic radiographs in a sample of Chilean patients. Int. J. Morphol. 2018, 36, 854–858. [Google Scholar] [CrossRef]
- Klenke, D.; Quast, A.; Prelog, M.; Holl-Wieden, A.; Riekert, M.; Stellzig-Eisenhauer, A.; Meyer-Marcotty, P. TMJ pathomorphology in patients with JIA: Radiographic parameters for early diagnosis. Head Face Med. 2018, 14, 15. [Google Scholar] [CrossRef]
- La Rosa, J.; Restrepo, M.; Torres, E.; Rodríguez, M. Asimetría mandibular en radiografías de niños no sindrómicos con y sin hendidura labio palatina en Bucaramanga, Colombia. Rev. Estomatol. Hered. 2021, 31, 73–80. [Google Scholar] [CrossRef]
- Severt, T.R.; Proffit, W.R. The prevalence of facial asymmetry in the dentofacial deformities population. Am. J. Orthod. Dentofac. Orthop. 1997, 112, 170–177. [Google Scholar]
- Thiesen, G.; Gribel, B.F.; Freitas, M.P.M.; Oliver, D.R.; Kim, K.B. Mandibular asymmetries and associated factors in orthodontic and orthognathic surgery patients. Angle Orthod. 2018, 88, 545–551. [Google Scholar] [CrossRef] [PubMed]
- Pertek, H.; Kamaşak, M.; Kotan, S.; Hatipoğlu, F.P.; Hatipoğlu, Ö.; Köse, T.E. Comparison of mandibular morphometric parameters in digital panoramic radiography in gender determination using machine learning. Oral Radiol. 2024, 40, 415–423. [Google Scholar] [CrossRef]
- Wang, H.; Wang, Y.; Du, Y.; Liu, B. Artificial intelligence applications in facial asymmetry diagnosis: A systematic review. J. Dent. Res. 2020, 99, 1345–1353. [Google Scholar]
- Leon, A.C.; Davis, L.L.; Kraemer, H.C. The role and interpretation of pilot studies in clinical research. J. Psychiatr. Res. 2011, 45, 626–629. [Google Scholar] [CrossRef]
- Lancaster, G.A.; Dodd, S.; Williamson, P.R. Design and analysis of pilot studies: Recommendations for good practice. J. Eval. Clin. Pract. 2004, 10, 307e12. [Google Scholar] [CrossRef] [PubMed]
- Sim, J.; Lewis, M. The size of a pilot study for a clinical trial should be calculated in relation to considerations of precision and efficiency. J. Clin. Epidemiol. 2012, 65, 301–308. [Google Scholar] [CrossRef] [PubMed]


| Asymmetry (mm) | Women DIF X1–X2n (%) | Women DIF Y1–Y2n (%) | Men DIF X1–X2n (%) | Men DIF Y1–Y2n (%) | Total DIF X1–X2n (%) | Total DIF Y1–Y2n (%) | Total n (%) |
|---|---|---|---|---|---|---|---|
| ≤3 (Mild) | 10 (33.3%) | 9 (30.0%) | 6 (20.0%) | 9 (30.0%) | 16 (26.7%) | 18 (30.0%) | 34 (56.7%) |
| (3, 6] (Moderate) | 3 (10.0%) | 4 (13.3%) | 5 (16.7%) | 3 (10.0%) | 8 (13.3%) | 7 (11.7%) | 15 (25.0%) |
| >6 (Severe) | 2 (6.7%) | 2 (6.7%) | 4 (13.3%) | 3 (10.0%) | 6 (10.0%) | 5 (8.3%) | 11 (18.3%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Agurto-Sanhueza, P.; Roco, K.; Navarro, P.; Neyem, A.; Sumonte, N.I.; Ottone, N.E. Simplified Diagnosis of Mandibular Asymmetry in Panoramic Radiographs Through Digital Processing and Its Prospective Integration with Artificial Intelligence: A Pilot Study. Appl. Sci. 2025, 15, 10802. https://doi.org/10.3390/app151910802
Agurto-Sanhueza P, Roco K, Navarro P, Neyem A, Sumonte NI, Ottone NE. Simplified Diagnosis of Mandibular Asymmetry in Panoramic Radiographs Through Digital Processing and Its Prospective Integration with Artificial Intelligence: A Pilot Study. Applied Sciences. 2025; 15(19):10802. https://doi.org/10.3390/app151910802
Chicago/Turabian StyleAgurto-Sanhueza, Paulina, Karla Roco, Pablo Navarro, Andrés Neyem, Nicolás I. Sumonte, and Nicolás E. Ottone. 2025. "Simplified Diagnosis of Mandibular Asymmetry in Panoramic Radiographs Through Digital Processing and Its Prospective Integration with Artificial Intelligence: A Pilot Study" Applied Sciences 15, no. 19: 10802. https://doi.org/10.3390/app151910802
APA StyleAgurto-Sanhueza, P., Roco, K., Navarro, P., Neyem, A., Sumonte, N. I., & Ottone, N. E. (2025). Simplified Diagnosis of Mandibular Asymmetry in Panoramic Radiographs Through Digital Processing and Its Prospective Integration with Artificial Intelligence: A Pilot Study. Applied Sciences, 15(19), 10802. https://doi.org/10.3390/app151910802






