Abstract
Background: Rheumatoid Arthritis (RA) is a systemic and chronic autoimmune disease with inflammation at the synovial joints. The purposes of this study were to evaluate the correlation between serological variables and temporomandibular disorders (TMDs) in patients diagnosed with RA, evaluated through diagnostic criteria for temporomandibular disorders (DC/TMD), and to check the influence of comorbidities on the different TMD signs and symptoms, or any serological variables. Methods: This observational cohort research study included seventeen patients affected by RA. The comorbidities and some variables from the initial serological analyses were collected from the clinical rheumatological charts. Then, the presence of any of the following TMD signs/symptoms, temporal myalgia, temporomandibular joint arthralgia, click or crepitus, was evaluated through the symptom questionnaire of the DC/TMD during clinical evaluation following the DC/TMD examination form. Results: Rheumatoid factor (RF), anticitrullinated protein antibodies (ACPA), and anti-nuclear antibody (ANA) positivity were present in 82.4%, 52.9%, and 41.2% of patients, respectively. Indicators of tissue inflammation were evaluated with median values of 21 mm/h for erythrocyte sedimentation rate (ESR) and 0.50 mg/dL for C-reactive protein (CRP). The RA patients presented comorbidities such as hypertension in 70.6% and diabetes in 23.5%. Negative ACPA had a significant association with myalgia (p = 0.03), and positive ANA was significantly associated with crepitus (p = 0.05). Conclusion: ANA and ACPA evaluation can be considered predictive serological tests associated with specific TMDs. Conversely, no influence of any comorbidities was found between different TMD signs and symptoms, or any serological variables.
1. Introduction
Rheumatoid Arthritis (RA) is a systemic and chronic autoimmune disease with persistent inflammation at the synovial joints causing morphological deformities and pain. It is one of the most common autoimmune diseases, affecting 1–1.5% of the population worldwide with a higher incidence in females. The onset can occur at any age, but peaks between 30 and 50 years [1,2,3,4,5,6]. The most important epidemiological study in Italy was conducted on almost five million Italian people aged ≥18 years. In the Italian population, Rossini et al. found an RA prevalence and incidence of 0.41% and 35/100,000, respectively, without apparent differences between northern and southern regions or urban and rural areas [7].
The etiopathogenesis is quite unknown, and is influenced by both genetic and environmental factors [8,9,10,11]. Specifically, it is largely accepted that several factors are involved in a genetically predisposed substrate. Different studies state that heritability is around 65% [7]. Genes inside the HLA locus, especially HLA-DRB1, represent just under half of the genetic component of susceptibility, as well as being associated with greater disease severity. From a gender viewpoint, females are two to three times more likely to acquire RA than males. It has been hypothesized that this is partially caused by the stimulatory effects of estrogen on the immune system. There are conflicting opinions in the literature regarding pregnancy and the risk of developing RA, although in general a trend towards a protective effect has been demonstrated [3]. Among the risk factors implicated in the development of RA are smoking, obesity, and periodontal disease; the gut microbiome and infections were also involved. Smoking represents an important risk due to the presence of anti-citrullinated protein antibodies (ACPA), which are fundamental diagnostic and prognostic markers in RA; the risk is further increased in the occurrence of specific HLA-DRB1 alleles. This depends mainly on the immunomodulatory effects of smoking, comprising a decrease in the phagocytic and antibacterial functions of alveolar macrophages, changes in cytokine production, and oxidative stress.
Aside from its effect on susceptibility, cigarette smoking can also be considered a risk factor for a greater severity of the disease. While the etiological factors are conflicting, large epidemiological studies state that obesity may be related to a modest spread in the risk of developing RA. Additional studies have shown that obesity is usually associated with worse subjective measures of disease activity, which may be mystified by osteoarthritis, disability, and chronic pain [3].
Autoimmunity and general systemic and joint inflammatory burden drive the destructive development of the disease [1]. According to several authors, the alterations associated with the pathology may derive from chronic inflammation and an autoimmune reaction caused by an external or endogenous pathogen acting on a genetic substratum. The pathogenesis concerns synovial proliferation over the surface of the cartilage, producing a tumor-like mass (pannus) that destroys the articular cartilage and the adjacent bone tissue, causing inflammation that affects the peripheral joints, in particular diarthrosis, often symmetrically [9]. The disease is polyarticular, and most commonly affects the hands, feet, wrists, elbows, shoulders, cervical spine, and knees. The lumbar spine is spared. Extra-articular manifestations (EAMs) may involve the eyes, lungs, heart, nervous system, kidneys, and blood vessels [12]. The EAMs of RA may appear at any time after disease onset, and the presence of these signs is related to amplified mortality. Particularly, multi-organ involvement in RA is more common in patients with severe, active disease and those with positive rheumatoid factor (RF)/anti-CCP Abs and/or positive HLA-DR4. EAMs include the involvement of the skin, eyes, heart, lungs, renal, nervous, and gastrointestinal systems, with tendons, ligaments, and fascia. Consequently, it is essential to recognize EAM because the management is frequently aimed at controlling the underlying RA disease [2].
Among the most frequent manifestations are keratoconjunctivitis, the inflammation of the cornea and conjunctiva, which manifests itself as burning, itchy eyes, pressure behind the eye, or a feeling of grittiness in the eye. Among the less frequent but more destructive processes is scleritis, which is characterized by a very painful inflammation of the sclera. Pleuro-pulmonary involvement is common in RA, and pleural effusions may be found on routine chest X-rays.
Patients with pleural effusions may not have symptoms and may not need any therapy, as effusions usually resolve spontaneously or with the management of the joint disease.
Lung nodules also may be reported in patients with RA. They usually appear in patients with long-standing RA pathology and patients with concomitant subcutaneous rheumatoid nodules. The prognosis of rheumatoid pulmonary nodules is commonly good, but monitoring for potential neoplasms is necessary, especially in those subjects who have a history of smoking [1,2,3]. Male patients, subjects who are older at the onset of the disease, and those with more severe disease show a greater risk of developing ILD.
Considering the systemic inflammatory nature of RA, the main cardiac manifestation in these patients is atherosclerosis. Several studies have found increased cardiovascular morbidity in patients with RA; compared to age- and sex-matched controls, patients with RA present an increased risk of cardiovascular death, ischemic heart disease, and heart failure. Osteoporosis in RA occurs from an interaction of factors, comprising systemic and local inflammation, patient immobilization caused by joint damage and pain, and the associated treatment with glucocorticoids.
Hematologic anomalies are usual in RA, and bone marrow suppression may result from both pathological processes and drug therapy. Clinically, this may present as anemia, leukopenia, neutropenia, eosinophilia, thrombocytopenia, or thrombocytosis. Anemia of long-term disease is the most frequent anomaly, which may present concurrently with iron deficiency anemia and will tend to improve with good disease control. Mononeuritis multiplex is an asymmetric sensory and/or motor peripheral neuropathy that destroys at least two separate, apparently random, nerve areas. Mononeuritis multiplex is usual in diabetes but may also be seen in vasculitis, like RA [2].
Regarding the diagnostic criteria, there are three key factors indicating probable RA according to the more updated classification (ACR/EULAR 2010 Classification) [13]: symmetrical arthritis of small joints (swelling and morning joint stiffness), symptoms lasting longer than 6 weeks, elevated concentrations of C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR), presence of anticitrullinated protein antibodies (ACPA), rheumatoid factor (RF) (when its titer is three times increased), or anti-nuclear antibody (ANA) [6,14,15,16,17,18].
However, currently, there are no single pathognomonic laboratory or imaging findings that definitively diagnose this disease [19]. Although structural changes, which can be visualized by conventional X-rays or other imaging techniques, best distinguish RA from other arthritic disorders, joint damage is rarely apparent in the very early stages of disease, but rather accumulates consistently over time [1]. Therefore, RA diagnosis is also, and above all, clinical, based on the pattern of the following physical symptoms, i.e., swollen joints, redness at affected joints, joint stiffness in the morning, low-grade fever, fatigue, and loss of appetite [19].
The early diagnosis and treatment of RA have extensively shown a strong potential for the improvement of disease outcomes. Established evidence supports the impact of early interventions in terms of early disease activity control, leading to a lower rate of radiographic progression and development of disability. Early diagnosis and treatment are associated with better outcomes in terms of survival, which is mainly dependent on the early suppression of disease activity and prevention of functional impairment. Therefore, the model of care, including early diagnosis, is consistently regarded as a standard of care according to current international RA guidelines. Some recent research showed that quality of care in the population is suboptimal, even in efficient healthcare systems, due to delays in referral and diagnosis [20]. It has been recognized that early therapeutic intervention improves clinical outcomes and reduces the increase in joint damage and disability. Certainly, treating patients at a stage at which the evolution of joint destruction can still be prevented would be ideal [1].
The joints are primarily involved but there are other extra-articular manifestations, such as rheumatoid nodules, pulmonary involvement or vasculitis, and systemic comorbidities [8,9,10,11]. Specifically, RA may severely affect the normal functions of temporomandibular joints (TMJs) in a wide range of the population, reported to be from 4.7% to 88% of adults [6]. The involvement of the TMJ follows the same destructive path occurring in other joints, directly correlated with the severity and duration of the RA. In the initial phase, there may be synovial hyperemia, lymphocyte infiltration, fibrinoid degeneration, and granulation tissue until joint degeneration. From that point on, there may be the formation of scarring and fibrous adhesion [21]. The disease may lead to severe TMJ disabilities including arthralgia, limited mandibular movements with related functions, difficulty in eating, morning stiffness during mouth opening upon waking, weakness of the masticatory muscles with decreased bite force, and joint noises [21].
TMJ radiographic records may only show abnormalities in the integrity of the bone cortex, bone erosions, asymmetry and flattening of the condyles, and joint space narrowing. Moreover, these TMJ signs and symptoms are often underestimated or, worse, ignored, so the diagnosis of TMJ involvement comes too late to prevent permanent damage. The monitoring of this joint should be considered to prevent irreversible issues [22,23].
As abovementioned, RF and ACPA are common, reliable, and regularly used methods of RA assessment [6,14,15,16,17,18]. If these indices correlate with temporomandibular disorders (TMDs) [24,25,26,27] in RA patients, then they can be used as potential predictors of TMJ affection in RA patients.
In the literature, only two clinical trials evaluated the TMD prevalence and the serological tests in RA patients [6,28]. The ACPA showed a significant correlation with the development of clinical TMDs. There is still no evidence of the presence of a direct association between serological tests and TMDs.
The primary objectives of this study were to evaluate, in patients diagnosed with RA, the possible correlation between serological variables and the main TMD signs and symptoms evaluated through the diagnostic criteria for temporomandibular disorders (DC/TMD). The secondary objective was to check the possible influence of any comorbidities with the different TMD signs and symptoms, or any serological variables.
2. Materials and Methods
The research was conducted in accordance with the revised Helsinki Declaration, and it was approved by the Ethics Board Committee of the University of Campania Luigi Vanvitelli, Italy (Prot N° 309), before starting the data collection. All subjects had signed informed consent for the use of personal information in the study.
This prospective observational cohort study was conducted on consecutive patients referred by the Rheumatological Unit to the Orthodontic Program of the University of Campania Luigi Vanvitelli, in Naples, Italy, from January 2019 to December 2022. The inclusion criteria were (1) age higher than 25 years old; (2) a confirmed diagnosis of RA according to the 2010 ACR/EULAR criteria [14]; (3) regular follow-up by a rheumatologist; and (4) complete serological and clinical records. Patients were excluded if they had incomplete medical records, congenital or acquired facial anomalies, a history of facial fractures, previous maxillofacial surgery, or previous orthodontic treatment during the permanent dentition, i.e., previous treatment with occlusal splints for treating TMDs.
Starting from a total of 28 selected subjects, 8 were excluded for missing data, and 3 were discarded for previous treatment with splints. Thus, a total of 17 patients were included in the final analysis after the collection of the previous primary data reported in the clinical charts.
Information on the variables from the serological analyses and the comorbidities of the RA were collected by the rheumatologists and reported in the clinical charts during the initial consultations, as secondary data. Specifically, the ESR (mm/h, and +/−), C-reactive protein (mg/dL, and +/−), RF (+/−), ACPA (+/−), and ANA (+/−) were evaluated.
More in detail, the ESR normal values are 0–15 mm/h in men and 0–20 mm/h in women; therefore, the values outside these ranges were considered positive. For the C-reactive protein parameter, its value is considered positive when exceeding 1 mg/dL. RF are autoantibodies that bind to epitopes within the constant region (Fc) of immunoglobulin type G (IgG). Different assays are used to detect RF. Hemagglutination tests are currently considered to be obsolete and have been replaced by more or less automated immunoassays. [29] Regarding ACPA detection, different generations of tests are currently available. Initially, ACPA was detected by ELISA using citrullinated recombinant rat filaggrin. Subsequently, the sensitivity of ACPA tests was enhanced without compromising specificity by using synthetic cyclic citrullinated peptides (CCP), most commonly version 2 (CCP2) [22]. In Europe, the anti-CCP2 test is the most commonly used test, manufactured and distributed by different companies and assay formats [29].
The presence of any of the main TMD signs and symptoms, specifically, myalgia in the temporal area, TMJ arthralgia, click, or crepitus, was evaluated through the validated Italian version of the DC/TMD [https://ubwp.buffalo.edu/rdc-tmdinternational/tmd-assessmentdiagnosis/dc-tmd-translations/ (accessed on October 2023) during the subsequent clinical evaluations performed in the Unit of Orthodontics by specialists in orthodontics and orofacial pain.
In particular, records about the abovementioned TMJ signs and symptoms were derived from the “Symptom Questionnaire” of the updated DC/TMD examination forms [27], focusing on the assessment of referred pain, headache, joint noises, and eventual previous locking of the jaws (Figure 1).
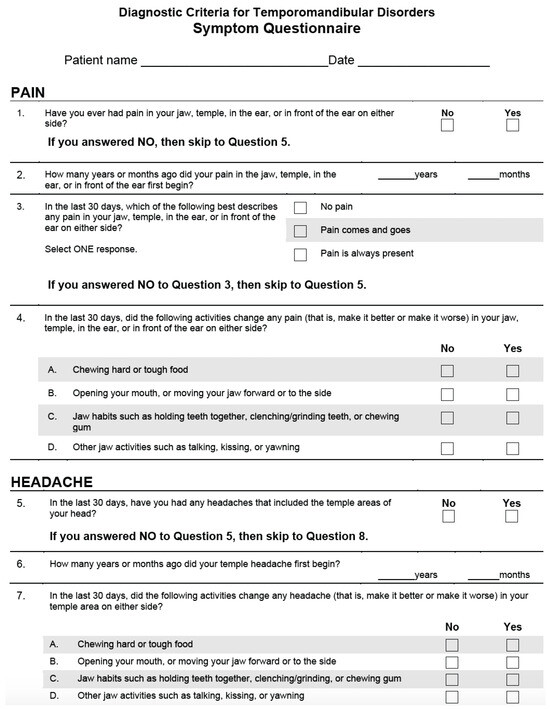
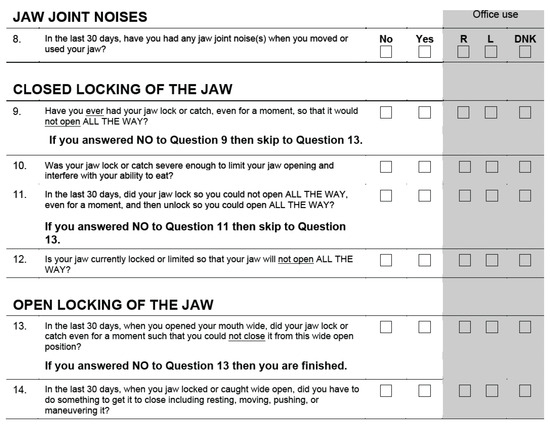
Figure 1.
DC/TMD—Symptom Questionnaire.
All data were shared in an online Excel sheet between the specialists of the two Units in order to check the eventual unavailable information in every patient.
Other information on historical and family anamnesis was excluded, being unrelated to the purposes of this research study.
Statistical Methods
Continuous variables were reported as either the means and standard deviation or median and interquartile ranges (IQRs) according to their distribution, as assessed by the Shapiro–Wilk normality test. Categorical variables were reported as absolute frequencies and percentages. Differences in baseline characteristics of patients affected and unaffected were tested using a Student’s t-test or Wilcoxon test (according to their distribution) for continuous and a Pearson chi-squared test or Fisher’s exact test for categorical variables. Moreover, the group differences analyses were performed to estimate the effect of serological variables on the temporomandibular disorders (absence/presence). All the statistical tests with p-values equal to or smaller than 0.05 were considered statistically significant. The analyses were conducted using the R statistical package (version 3.5.3, R Core Team, Foundation for Statistical Computing, Vienna, Austria).
3. Results
The study included 17 patients (15 females and 2 males) with RA, with a median age of 48 years. RF, ACPA, and ANA positivity were present in 82.4%, 52.9%, and 41.2% of patients, respectively. Indicators of tissue inflammation were evaluated with median values of 21 mm/h for ESR and 0.50 mg/dL for CRP.
The RA patients presented comorbidities such as hypertension in 70.6%, diabetes in 23.5%, lung disease in 7.6%, and atherosclerosis in 11.8%; only one patient showed, in addition, hepatic steatosis and hyperuricemia (Table 1).

Table 1.
Descriptive statistics on variables included in the research.
As seen in Table 2, negative ACPA had a significant association with myalgia (p = 0.03). No other statistical significance was found between myalgia and the other variables. Moreover, 12 patients reported myalgia (females 91.7% and males 8.3%). Among these patients, the ESR median value was 23 mm/h, while RF positivity was present in 75% of patients.

Table 2.
Association between possible predictor variables and myalgia.
Some of the possible predictor variables and TMJ outcomes, specifically arthralgia and click, showed no significant association. The arthralgia was referred by 90.9% of females and 9.1% of males. The median ESR value was 21 mm/h, while the CRP median value was 0.50 mg/dL in patients who reported arthralgia (Table 3).

Table 3.
Association between possible predictor variables and arthralgia.
The click was observed in eight patients (87.7% females and 12.5% male). Patients with no click presented median values of ESR and CRP of about 19 mm/h and 1 mg/dL, respectively. Furthermore, seven patients with no click and seven patients with click were RF-positive (Table 4).

Table 4.
Association between possible predictor variables and click.
In Table 5, it can be seen that only three RA patients presented a crepitus, but they were all RF-positive. The statistical significance was demonstrated between crepitus and ANA positivity (p = 0.05). Both ACPA and ANA were related to clinical TMDs (myalgia and crepitus). Negative ACPA had a significant association with myalgia (p = 0.03), and positive ANA was significantly associated with crepitus (p = 0.05).

Table 5.
Association between possible predictor variables and crepitus.
4. Discussion
The percentage of women affected by RA in the study sample was higher than males (about 88% vs. 11%), and this is in agreement with the worldwide female gender prevalence of rheumatological conditions reported in the recent literature [28,29,30].
The relationship between different serological factors and TMJ involvement in adults affected by RA has already been demonstrated in previous publications [6,28]. Specifically, authors evaluated the association of some serological tests with the prevalence of TMJ disorders assessed by the first research diagnostic criteria (RDC)/TMD axes [28] and with the radiographic TMJ changes. Youssef et al. [6] showed that on CBCT evaluations, the ACPA can be a good indicator of changes in condylar measurements, mainly in the case of highly destructive disease of the TMJ. Conversely, RF level was considered a poor predictor of condylar size or osteoarthritic changes in RA patients. Recent research showed that RA patients, mainly females, follow an individual skeletal growth pattern evaluated using bidimensional radiological examinations, which are not affected by inflammatory parameters, even if they show joint anatomical asymmetry [31,32].
Regarding the serological parameters, Van Hoovel et al. stated that there is some evidence that specificity in RA classification can be improved by refining the serological weight scoring, taking into account the nature of the antibody (RF versus ACPA), their levels, and the occurrence of combined RF/ACPA positivity. There is now increasing awareness that efforts should be undertaken to harmonize the interpretation of RF and ACPA test results in order to further improve the classifications and diagnosis of RA [29].
The current research evaluated, for the first time in patients affected by the RA systemic disease, the presence of signs and symptoms of TMDs, assessed through the updated DC/TMD, [24] and the putative correlation with some of the RA diagnostic factors revealed by the following serological tests: ESR, CRP, RF, ACPA, and ANA.
The assessment of the DC/TMD in this study was carried out by only one examiner to avoid any performance bias. A statistically significant association was found between a negative ACPA and the presence of pain related to the masticatory muscles. This outcome was similar to the previous research in which 80% of TMDs were described as pain in the orofacial region. Similarly, Mortazavi et al. showed a significant correlation between the clinically evaluated presence of TMDs in RA patients and the CRP (57.69%), ACPA (94.23%), and RF (86.53%) serological levels [28].
Moreover, in our study, RF has been found to be positive in more than 80% of patients with RA. The comorbidities more correlated with RA in our sample were hypertension (70%), and also diabetes (23.5%). However, there is no evidence of the possible correlation of any comorbidities with either TMDs or serological tests; thus, no prediction can be made about this point.
In conclusion, ACPA and RF were confirmed to be related to clinical TMDs, and this is important evidence for clinicians within the multidisciplinary diagnostic path in patients affected with RA. Specifically, myalgia is correlated with ACPA negativity, and this parameter should be disseminated among rheumatologists in order to refer RA patients with these characteristics to an orofacial pain specialist for the possible early diagnosis and management of TMD. In this regard, it is important to underline the results of recent research on the cranial structure and condylar asymmetry checked on panoramic X-rays. In patients with RA, compared to a healthy adult control group, the condyles showed a bilateral asymmetry in RA patients due to the high turnover of this joint reacting to severe systemic inflammation [33]. So, it is pivotal to diagnose TMJ early and monitor it in conditions of arthritis, not only assessing the signs and symptoms revealed by patients but also evaluating predictors through additional serological and instrumental exams.
The strength of this research protocol is that we have found some predictive factors for TMDs in patients affected by RA using the updated DC/TMD.
A limitation is the small sample size which consisted of consecutive patients diagnosed with RA in a single university hospital over a specific range of years. However, this should just be the beginning of a future multicentric study that will include several centers using a similar methodology of research.
Thus, future studies are ongoing to validate the serological variables with the presence of myalgia and crepitus involving a wider sample size of patients affected by RA, comparing them with a similar control group.
5. Conclusions
In patients diagnosed with RA, a significant correlation between TMD symptoms was evaluated through DC/TMD. Specifically, myalgia of the masticatory muscles is related to ACPA negativity, whereas the presence of crepitus is correlated with ANA positivity. Thus, within the limitations of the study, ANA and ACPA evaluation can be considered as predictive serological tests associated with specific TMJ disorders. Conversely, no influence of any comorbidities was found between different TMD signs and symptoms, or any serological variables.
Author Contributions
Conceptualization, V.G.; methodology, L.N.; investigation, G.C.; data curation, M.F.; writing—original draft preparation, R.P.R.; writing—review and editing, F.d.; supervision, A.J. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of the University of Campania Luigi Vanvitelli, Naples, Italy (Protocol code 309).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data supporting the reported results are available from the corresponding authors.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Aletaha, D.; Neogi, T.; Silman, A.J.; Funovits, J.; Felson, D.T.; Bingham, C.O.; Birnbaum, N.S.; Burmester, G.R.; Bykerk, V.P.; Cohen, M.D.; et al. 2010 rheumatoid arthritis classification criteria: An American College of Rheumatology/European League against rheumatism collaborative initiative. Arthritis Rheum. 2010, 62, 2569–2581. [Google Scholar] [CrossRef] [PubMed]
- Littlejohn, E.A.; Monrad, S.U. Early diagnosis and treatment of rheumatoid arthritis. Prim. Care 2018, 45, 237–255. [Google Scholar] [CrossRef] [PubMed]
- Aletaha, D. Management of rheumatoid arthritis: What happens and what does not happen in real life. Rheumatol. Int. 2016, 36, 167–168. [Google Scholar] [CrossRef]
- Fiehn, C.; Krüger, K. Management of rheumatoid arthritis. Internist 2016, 57, 1042–1051. [Google Scholar] [CrossRef] [PubMed]
- Hamburger, J. Orofacial manifestations in patients with inflammatory rheumatic diseases. Best Pract. Res. Clin. Rheumatol. 2016, 30, 826–850. [Google Scholar] [CrossRef] [PubMed]
- Youssef Mohamed, M.M.; Dahaba, M.M.; Farid, M.M.; Ali Elsayed, A.M. Radiographic changes in TMJ in relation to serology and disease activity in RA patients. Dentomaxillofac. Radiol. 2020, 49, 20190186. [Google Scholar] [CrossRef]
- Rossini, M.; Rossi, E.; Bernardi, D.; Viapiana, O.; Gatti, D.; Idolazzi, L.; Caimmi, C.; Derosa, M.; Adami, S. Prevalence and incidence of rheumatoid arthritis in Italy. Rheumatol. Int. 2014, 34, 659–664. [Google Scholar] [CrossRef]
- Wasserman, A.M. Diagnosis and management of rheumatoid arthritis. Am. Fam. Physician 2011, 84, 1245–1252. [Google Scholar]
- Smolen, J.S.; Aletaha, D.; Barton, A.; Burmester, G.R.; Emery, P.; Firestein, G.S.; Kavanaugh, A.; McInnes, I.B.; Solomon, D.H.; Strand, V.; et al. Rheumatoid arthritis. Nat. Rev. Dis. Primers. 2018, 4, 18001. [Google Scholar] [CrossRef]
- Smolen, J.S.; Landewé, R.B.M.; Bergstra, S.A.; Kerschbaumer, A.; Sepriano, A.; Aletaha, D.; Caporali, R.; Edwards, C.J.; Hyrich, K.L.; Pope, J.E.; et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2022 update. Ann. Rheum. Dis. 2023, 82, 3–18. [Google Scholar] [CrossRef]
- Rodríguez-Carrio, J.; Cavalli, G.; Gwinnutt, J.; Wieczorek, M.; Guillemin, F.; Verstappen, S.M.M. Developing a framework for the implementation of recommendations for lifestyle factors for people with RMDs across Europe: Assessment of current materials and implementation needs. RMD. Open. 2023, 9, e003443. [Google Scholar] [CrossRef] [PubMed]
- Sidebottom, A.J.; Salha, R. Management of the temporomandibular joint in rheumatoid disorders. Br. J. Oral Maxillofac. Surg. 2013, 51, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Angelotti, F.; Parma, A.; Cafaro, G.; Capecchi, R.; Alunno, A.; Puxeddu, I. One year in review 2017: Pathogenesis of rheumatoid arthritis. Clin. Exp. Rheumatol. 2017, 35, 368–378. [Google Scholar] [PubMed]
- Kay, J.; Upchurch, K.S. ACR/EULAR 2010 rheumatoid arthritis classification criteria. Rheumatology 2012, 51 (Suppl. S6), vi5–vi9. [Google Scholar] [CrossRef]
- Bykerk, V.P.; Massarotti, E.M. The new ACR/EULAR remission criteria: Rationale for developing new criteria for remission. Rheumatology 2012, 51 (Suppl. S6), vi16–vi20. [Google Scholar] [CrossRef]
- Conigliaro, P.; Triggianese, P.; Chimenti, M.S.; Lucchetti, R.; Kroegler, B.; Perricone, R. Serological markers associated with disease activity in patients with rheumatoid arthritis treated with rituximab. J. Int. Med. Res. 2016, 44 (Suppl. S1), 53–57. [Google Scholar] [CrossRef]
- Abdelhafiz, D.; Baker, T.; Glascow, D.A.; Abdelhafiz, A. Biomarkers for the diagnosis and treatment of rheumatoid arthritis—A systematic review. Postgrad. Med. 2023, 135, 214–223. [Google Scholar] [CrossRef]
- Motta, F.; Bizzaro, N.; Giavarina, D.; Franceschini, F.; Infantino, M.; Palterer, B.; Sebastiani, G.D.; Selmi, C. Rheumatoid factor isotypes in rheumatoid arthritis diagnosis and prognosis: A systematic review and meta-analysis. RMD Open 2023, 9, e002817. [Google Scholar] [CrossRef]
- Hodkinson, B.; Meyer, P.W.A.; Musenge, E.; Ally, M.M.T.; Wadee, A.A.; Anderson, R.; Tikly, M. The diagnostic utility of the anti-CCP antibody test is no better than rheumatoid factor in South Africans with early rheumatoid arthritis. Clin. Rheumatol. 2010, 29, 615–618. [Google Scholar] [CrossRef]
- Zanetti, A.; Scirè, C.A.; Argnani, L.; Carrara, G.; Zambon, A.; Italian Society for Rheumatology. Can the adherence to quality of care indicators for early rheumatoid arthritis in clinical practice reduce risk of hospitalisation? Retrospective cohort study based on the Record Linkage of Rheumatic Disease study of the Italian Society for Rheumatology. BMJ Open 2020, 10, e038295. [Google Scholar] [CrossRef]
- Sparks, J.A. Rheumatoid Arthritis. Ann. Intern. Med. 2019, 170, ITC1–ITC16. [Google Scholar] [CrossRef]
- Pantoja, L.L.Q.; de Toledo, I.P.; Pupo, Y.M.; Porporatti, A.L.; De Luca Canto, G.; Zwir, L.F.; Guerra, E.N.S. Prevalence of degenerative joint disease of the temporomandibular joint: A systematic review. Clin. Oral. Investig. 2019, 23, 2475–2488. [Google Scholar] [CrossRef]
- Cordeiro, P.C.; Guimaraes, J.P.; de Souza, V.A.; Dias, I.M.; Silva, J.N.; Devito, K.L.; Bonato, L.L. Temporomandibular joint involvement in rheumatoid arthritis patients: Association between clinical and tomographic data. Acta Odontol. Latinoam. 2016, 29, 123–129. [Google Scholar]
- Mupparapu, M.; Oak, S.; Chang, Y.C.; Alavi, A. Conventional and functional imaging in the evaluation of temporomandibular joint rheumatoid arthritis: A systematic review. Quintessence Int. 2019, 50, 742–753. [Google Scholar]
- Byun, S.H.; Min, C.; Choi, H.G.; Hong, S.J. Increased risk of temporomandibular joint disorder in patients with rheumatoid arthritis: A longitudinal follow-up study. J. Clin. Med. 2020, 9, 3005. [Google Scholar] [CrossRef] [PubMed]
- Piancino, M.G.; Rotolo, R.; Cannavale, R.; Cuomo, G.; Masini, F.; Dalmasso, P.; D’Apuzzo, F.; Perillo, L.; Nucci, L. Cranial structure and condylar asymmetry of adult patients with rheumatoid arthritis. BMC Oral Health 2023, 23, 269. [Google Scholar] [CrossRef] [PubMed]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group. J. Oral Facial Pain Headache 2014, 28, 6–27. [Google Scholar] [CrossRef]
- Mortazavi, N.; Babaei, M.; Babaee, N.; Kazemi, H.H.; Mortazavi, R.; Mostafazadeh, A. Evaluation of the Prevalence of Temporomandibular Joint Involvement in Rheumatoid Arthritis Using Research Diagnostic Criteria for Temporomandibular Disorders. J. Dent. 2018, 15, 332–338. [Google Scholar] [CrossRef]
- Van Hoovels, L.; Studenic, P.; Sieghart, D.; Steiner, G.; Bossuyt, X.; Rönnelid, J. Impact of autoimmune serology test results on RA classification and diagnosis. J. Transl. Autoimmun. 2022, 5, 100142. [Google Scholar] [CrossRef] [PubMed]
- Rotolo, R.P.; d’Apuzzo, F.; Femiano, F.; Nucci, L.; Minervini, G.; Grassia, V. Comparison between ultrasound and magnetic resonance imaging of the temporomandibular joint in juvenile idiopathic arthritis: A systematic review. J. Oral. Rehabil. 2023, 50, 1082–1092. [Google Scholar] [CrossRef]
- Montinaro, F.; Nucci, L.; d’Apuzzo, F.; Perillo, L.; Chiarenza, M.C.; Grassia, V. Oral nonsteroidal anti-inflammatory drugs as treatment of joint and muscle pain in temporomandibular disorders: A systematic review. Cranio 2022, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Nowell, W.B.; Barnes, E.L.; Venkatachalam, S.; Kappelman, M.D.; Curtis, J.R.; Merkel, P.A.; Shaw, D.G.; Larson, K.; Greisz, J.; George, M.D. Racial and Ethnic Distribution of Rheumatic Diseases in Health Systems of the National Patient-Centered Clinical Research Network. J. Rheumatol. 2023. Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Tortarolo, A.; Rotolo, R.; Nucci, L.; Tepedino, M.; Crincoli, V.; Piancino, M.G. Condylar Asymmetry in Children with Unilateral Posterior Crossbite Malocclusion: A Comparative Cross-Sectional Study. Children 2022, 11, 1772. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).