Abstract
Background: Anomalous Aortic Origin of a Coronary Artery (AAOCA) is a congenital condition that can lead to ischemia and sudden cardiac death. Current diagnostic tools are unable to fully quantify the pathological behavior that occurs mainly with physical effort. Methods: Patients’ computed tomography scans and centerline-based geometric quantities were used to develop three-dimensional computer-aided design models of the main anatomical variants of AAOCA. Blood pressure ranging from rest to extreme effort was simulated through structural finite element analyses, and the pressurized geometries were analyzed to evaluate coronary lumen cross-sectional areas and variations at the different loading conditions. Results: We simulated 39 subjects, demonstrating the ability to reproduce accurately the patient-specific anatomy of different AAOCA variants and capture pathological behaviors. AAOCAs with intramural courses showed compression along the proximal segment with a caliber reduction ranging from 0.14% to 18.87% at different pressure levels. The percentage of proximal narrowing relative to the distal segment was greater than any other type of anomalous course and exceeded 50% with simulated exertion. Conclusions: The present study proposes a computational pipeline to investigate conditions not reproducible in clinical practice, providing information to support decision-making in the management of AAOCA patients.
1. Introduction
Anomalous Aortic Origin of a Coronary Artery (AAOCA) is a congenital condition in which any of the main epicardial coronary vessels may have an ectopic origin from the aorta, such as the opposite sinus of the Valsalva [1]. The anomalous origin leads to an anomalous course because coronary arteries need to reach their myocardial distribution territory. So, the AAOCA course can be classified as one of five subtypes that, in order of prevalence, are: retroaortic, interarterial, subpulmonic, prepulmonic, or retrocardiac [2]. The interarterial course can be associated with an intramural segment, i.e., the proximal coronary runs within the aortic wall. This anatomical feature is generally considered among the major risk factors for myocardial ischemia and sudden cardiac death (SCD) [3,4], especially for young competitive athletes [5,6] who undergo intense physical activity. Data from observational studies are extremely heterogeneous, making it difficult to estimate the prevalence of the pathology in the general population, but AAOCA is believed to affect at least one in one thousand individuals [7], and it has been identified as the second most common cardiovascular cause of SCD (17%) in young people engaged in competitive sports [8]. The pathophysiological mechanism seems to be related to a compression of the intramural segment [9,10], but it cannot be determined or quantified during a physical effort. In detail, the entrapped intramural segment, which already shows hemodynamically unfavorable anatomy at baseline, may be subjected to a dynamic lateral compression (mimicking a stenosis) that increases with exertion due to a greater aortic expansion. This dynamic proximal compression of the coronary may lead to a reduction of oxygenated blood supply to the heart during effort that can trigger adverse events such as SCD [4]. Clinical evaluations are based on anatomical assessment and myocardial functional testing [11]. Diagnosis and morphological evaluation are routinely performed with computed tomography angiography (CTA), which allows the definition of anomalous coronary anatomical features. Functional myocardial evaluation is performed with an exercise stress test, cardiac MRI, or myocardial scintigraphy, which showed poor ability to detect inducible myocardial ischemia in AAOCA [12,13]. Cardiac catheterization with fractional flow reserve (FFR) and intravascular ultrasound (IVUS) may help with risk stratification, but they are invasive procedures and not always conclusive. CTA acquisitions or the evaluation of hemodynamic indexes are usually performed at rest, which does not allow for the assessment and demonstration of the pathogenetic mechanism of the intramural segment compression under effort.
In this context, computational simulations can help understand the pathophysiological mechanism of AAOCA, exploring conditions that can trigger ischemia and SCD and that could not be studied in the clinical setting without jeopardizing patient safety. In our previous studies, we have presented an idealized structural parametric model of the aortic root and AAOCA with intramural course, using values obtained from literature [10] or from measurements taken on CTA scans [9], to evaluate the deformations of the arterial wall and thus the morphological changes of the lumen during simulated effort conditions. In both cases, the reconstructed geometry was oversimplified, modeling the coronary lumen as a round pipe and neglecting the typical elliptic shape of the intramural segment. These works focused on a single anatomical variant, and a direct application of their methodologies to all forms of anomalous coronary arteries is not possible, as is the extension of their results.
In this paper, we propose a patient-specific computational pipeline to overcome the limitations of our previous studies, extending the AAOCA modeling and simulation to the main subtypes under a wider range of simulated physical conditions. Our aim is to assess, by means of finite element analysis (FEA), whether there are differences in behavior between healthy and anomalous coronaries and between different forms of anomalous coronaries with and without intramural segments. We extract routine parameters that are used in clinical practice to evaluate the severity of the AAOCA. Therefore, we retrieved the degree of narrowing and the locations of the phenomenon, which are indicators that may support decision-making in the management and treatment of AAOCA patients.
2. Materials and Methods
The present AAOCA patient-specific modeling and simulation workflow, depicted in Figure 1, can be outlined in three main steps:
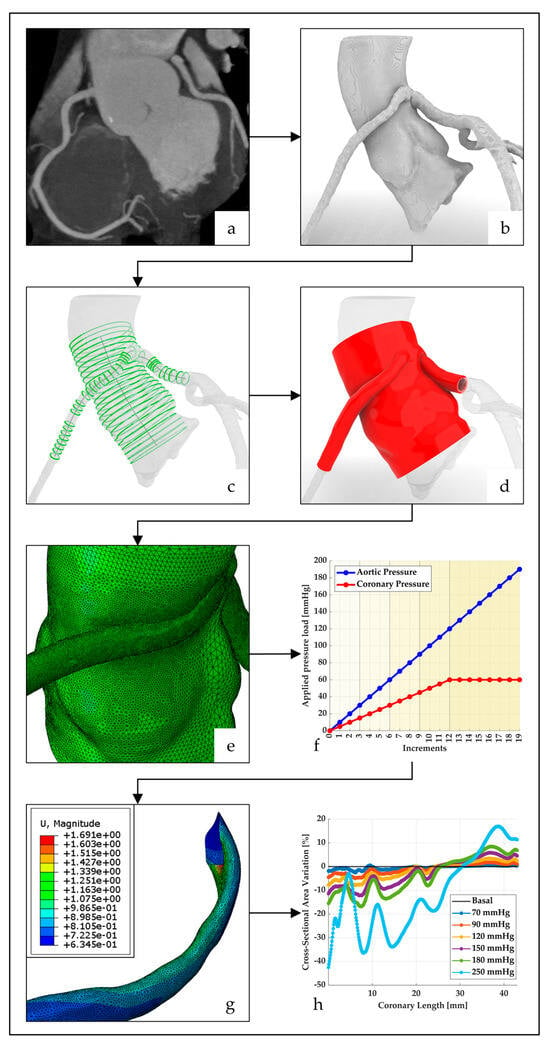
Figure 1.
AAOCA patient-specific modeling and simulation workflow. (a) Coronary CTA sequence; (b) STL reconstruction of the aorta with coronary arteries; (c) Centerline-based geometric quantities computation, slicing of the STL reconstruction and extraction of the profile curves; (d) CAD model of the aortic root with proximal segments of healthy and anomalous coronary artery; (e) Tetrahedral mesh with local refinements; (f) Plot of applied pressures with vertical dashed black lines delimiting the different loading regimes: resting diastole, resting systole, low-medium effort, medium-high effort, extreme effort; (g) extraction of the coronary luminal surface in its deformed configuration (legend: magnitude of nodal displacements); (h) enlargement/narrowing along the coronary vessel, with reference to the undeformed configuration, at six different simulated pressure levels. Simulated pressure = basal pressure (i.e., 60 mmHg) + applied load.
2.1. Study Population
Computed Tomography Angiography (CTA) images of patients with AAOCA referred to the IRCCS Policlinico San Donato (Italy) between 2013 and 2022 were retrospectively retrieved from the institutional database and evaluated using RadiAnt DICOM Viewer version 2022.1.1 (Medixant). The selection of the study population was conducted to include all the main types of anomalous courses while, at the same time, keeping the sample size balanced between anomalies with and without an intramural segment and between right coronary arteries (RCA) and left coronary arteries (LCA). No patients with concomitant major cardiac pathologies or atherosclerosis of the proximal coronary arteries were included in this study. CTA scans of poor quality were excluded. Diastolic sequences with a slice thickness of at least 1 mm and without severe image artifacts were considered suitable for segmentation and three-dimensional (3D) reconstruction. The patients’ images were de-identified before further processing.
2.2. Patient-Specific Model and Simulation: From CTA to CAD Model
The aortic and coronary lumens were segmented from the diastolic sequence of the selected coronary CTA scans using Mimics Medical v.24 software (Materialise, Leuven, Belgium). The segmented anatomies were exported as unstructured triangulated surfaces (STL reconstructions) for further processing via a script in VMTK v1.4 software (Orobix, Bergamo, Italy). First, the surfaces representing the lumen of the aorta and coronary arteries were smoothed with a Taubin filter and clipped. The clipping operation was performed manually through cutting planes using the following anatomical landmarks: the first main bifurcation for the LCA, the left ventricular outflow tract (LVOT), the sinotubular junction for the aorta, and a distal secondary branch for the RCA. Then, the modified STL reconstructions were remeshed and eventually extended in the direction normal to the boundaries under the assumption that some improvements are required to avoid issues during centerline computation [14]. Centerline-based geometric quantities, such as cross-sectional areas, Frenet-Serret frames, and minimum and maximum diameters, were extracted for a length of 5 cm (otherwise for the maximum length available) and used for the computer-aided design (CAD) modeling step. The 3D patient-specific CAD model was generated through Grasshopper, a visual programming language and environment integrated within the software Rhinoceros v6.35 (McNeel and Associates, Seattle, WA, USA). The STL reconstruction of the aortic root was sliced with cross-sectional planes perpendicular to its centerline to obtain the contour curves of the lumen. The polylines thus obtained were rebuilt as Non-Uniform Rational B-Splines (NURBS) curves and interpolated, generating the CAD model of the inner surface of the aortic root. The points that formed the luminal profile curves were radially shifted to define the boundaries of the outer surface of the aortic root. The magnitude of radial displacements, i.e., the arterial wall thickness, was uniformly set to 3 mm, according to the literature [15,16]. Regarding the coronary artery model, the inner surface was obtained by interpolating elliptical sections perpendicular to the centerline, whose positions, maximum, and minimum diameter values were previously retrieved. Sections at the level of secondary branches were excluded, and the coronary wall thickness was uniformly set to 0.9 mm [17]. The intersection between the aorta and the coronary model was granted by duplicating the coronary section closest to the ostium and iteratively moving it toward the nearest point of the aortic centerline until it was completely inside the aortic lumen. Finally, Boolean operations led to the 3D geometric model of the aortic root together with the proximal segments of the coronary arteries.
2.3. Geometric Model Accuracy
The geometric model’s accuracy was evaluated by computing the signed shortest distance of each point on the inner surface of the geometric model from the STL reconstruction. The distance was considered positive for points outside the inner surface of the geometric model and negative otherwise. No smoothing strategies have been adopted on the STL reconstructions, taken as references for the comparison.
2.4. Simulation Settings and Analysis
Structural FEAs were carried out by the commercial finite element package Abaqus/Standard 2019 (Dassault Systemès, Providence, RI, USA). A neo-Hookean model was used for the wall of the aorta and coronary arteries, while the constitutive properties of the fluid domain were not taken into account and prescribed pressure loads were uniformly applied to the inner surface of the solid domain. The hyperelastic parameters were set by assuming an elastic modulus E = 1.5 MPa, a Poisson ratio ν = 0.49, and a density of 1.2 g/cm3 [18]. These material properties correspond to the C10 and D1coefficients of the neo-Hookean model, 0.2517 MPa and 0.08 MPa−1, respectively. The models were discretized using hybrid 4-node tetrahedral elements (C3D4H) with an approximate global size of 1 mm to include at least three elements within the aortic wall. According to a preliminary mesh convergence analysis, local mesh refinements with an element size of 0.3 mm were applied in the coronary regions and in the intramural tract if they were present. Static analyses were performed considering that the 3D geometric model, derived from the medical images, resembles the patient’s anatomy in diastole. Since the diastolic pressure value was not available for all subjects, this was assumed for the entire study population to be equal to the 5th percentile of the arterial pressure range for healthy subjects [19], matching the mean age of our patient cohort. Incremental loads were then applied to simulate blood pressure between this basal value (i.e., 60 mmHg) and 250 mmHg. The specified range completely covers the interval of arterial pressure variation for healthy subjects at rest and during physical exercise. It is worth noting that prestress modeling was not included in the present work, so the initial configuration was unloaded and corresponded to diastolic pressure, which is assumed to be the same for both the aorta and coronary arteries. As a result, a pressure load of 190 mmHg was uniformly applied to the aortic lumen with increments of 10 mmHg. At the same time, the pressure load imposed on the inner surface of the coronaries was increased linearly, with a step of 5 mmHg, up to a value of 60 mmHg and then kept constant, while the aortic lumen persisted to be further loaded until 190 mmHg, as shown in Figure 1f, to reach a simulated pressure of 250 mmHg. This behavior is consistent with the normalization of the coronary perfusion response to exercise [20]. Boundary conditions were set according to our previous studies [9,10]: the proximal and distal cross-sections of the aortic root were constrained longitudinally and circumferentially, allowing only displacements in the radial direction. Spring elements of type spring1 were added to the free extremity of the coronary arteries, acting orthogonally to the plane of the distal cross-section and with a rigidity of 1 MPa, to simulate the constraint due to the myocardium.
2.5. Post-Processing of Simulation Results
The deformed configuration of the coronary lumen was processed for each defined pressure increment. The cross-sectional areas of the vessel were calculated from the ostium along the entire length of the coronary arteries, every 0.1 mm, and used to assess potential enlargement/narrowing with reference to the undeformed configuration. The anomalous coronaries were divided into three zones to better localize the phenomenon: the ostial zone (OST), from the origin up to a length of 1.5 mm; the intramural or middle zone (MID), from the end of the ostial zone to the end of the intramural segment; and the distal zone (DIS), from the end of the intramural zone to the end of the coronary model. In the case of AAOCA without an intramural course, the length of the middle zone was considered equal to the average length of the intramural segments. Measurement of intramural tract lengths was performed on the 3D CAD models in their basal configuration. Healthy coronaries were divided into two zones: the ostial zone, defined as above, and the distal zone, from the end of the ostial zone to the end of the coronary model. Each of the segments defined above was characterized by taking the median luminal area (MLA) variation, defined as the median of the percentage variations of the luminal cross-sectional areas over the corresponding length. These variations were computed with reference to the undeformed basal configuration [i.e., (deformed area − basal area)/basal area × 100]. Furthermore, we assessed the clinical relevance of luminal cross-sectional area reduction by measuring the percentage of proximal course narrowing with respect to the distal segment [i.e., (distal area − proximal area)/distal area × 100] [21]. Positive values denote the degree of proximal stenosis, while negative values indicate no reduction in lumen caliber, i.e., the proximal segment has a greater cross-sectional area than the distal segment.
2.6. Statistical Analysis
Categorical variables were reported as numbers and frequencies. Considering non-normal distributions assessed using the Anderson-Darling test and data visualization, continuous variables were expressed as median and interquartile range (IQR), unless otherwise specified. Two-by-two comparisons of MLA variations between homologous segments within right and left coronary arteries were made by Mann-Whitney U tests to assess whether there are differences in behavior between healthy and anomalous coronaries and between anomalous coronaries with and without intramural course. The Bonferroni correction method was applied to adjust the p-values resulting from these pairwise comparisons. p-values were two-tailed, and a p < 0.05 was considered statistically significant. To complement the statistical hypothesis test and capture the magnitude of the phenomenon, we reported the effect size between two homologous segments as the median difference and bootstrapped the 95% confidence interval (CI).
3. Results
3.1. Study Population
The study population consisted of 39 subjects with AAOCA, retrospectively selected from patients referred to IRCCS Policlinico San Donato (Italy) between 2013 and 2022. The study cohort was composed of 27 males (69%) and 12 females (31%), with a median age of 35 (38) years. We divided the population into left and right coronary artery anomalies, further grouping them according to the type of proximal course. Table 1 summarizes the different types of coronary arteries in the study population.

Table 1.
Coronary arteries in the patient cohort (n = 39).
Non-anomalous LCAs and RCAs, hereinafter called healthy, were collected from patients with right and left AAOCA, respectively. Twenty patients had an anomalous LCA, of which seven were intramural, five were retroaortic, five were subpulmonary, and three were prepulmonary. Notably, one subject presented with two different anomalies: an intramural left anterior descending coronary artery and a retroaortic left circumflex coronary artery. Eighteen patients had an anomalous RCA with an interarterial course, including eleven with and seven without an intramural segment. No retrocardiac course was observed. The CTA images of the selected subjects had an average slice thickness of 0.65 mm (in a range of 0.5 to 1 mm) and an average pixel spacing of 0.35 mm (in a range of 0.23 to 0.53 mm).
3.2. Geometric Model Accuracy
The results of our geometric modeling method for the four types of anomalous coronary courses are shown in Figure 2, superimposed on the respective STL reconstructions obtained by segmenting the CTA images.
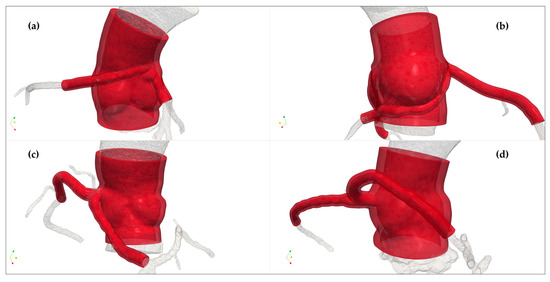
Figure 2.
Three-dimensional patient-specific CAD models of the aortic root with healthy and anomalous coronary arteries differentiated by the type of course: (a) interarterial/intramural; (b) retroaortic; (c) subpulmonary; (d) prepulmonary. In each panel, the arterial wall model is shown in red and the STL lumen reconstruction in transparency.
Figure 3 depicts the signed distance of each point on the inner surface of the geometric model from the STL lumen reconstruction, taken as a reference. Overall, the pointwise distance ranges from −4.42 mm to 4.06 mm, with the greatest differences located at the extremities of the models, where surface processing operations slightly altered the local geometry of the raw STL files. The median of the pointwise distances is 0.06 mm, and 90% of the values are between −0.26 (5th percentile) and 0.44 mm (95th percentile), i.e., within the in-plane resolution range and below the out-of-plane resolution of CTA scans.
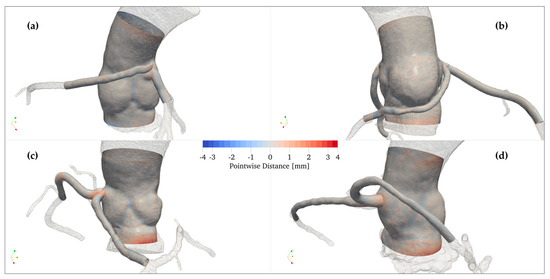
Figure 3.
Pointwise distance between the STL reconstruction (ground truth) and the luminal surface of the geometric model in each type of anomalous course: (a) interarterial/intramural; (b) retroaortic; (c) subpulmonary; (d) prepulmonary. Colors are displayed as a function of distance. Positive values, in red, indicate that the STL reconstruction, shown in transparency, is outside the lumen model.
3.3. Variations in Coronary Cross-Sectional Area
Median luminal area variations of coronary vessels at the ostial, middle, and distal zones, with each increase in simulated pressure, are shown in Figure 4 for each type of course. Enlargement or narrowing was computed with reference to the undeformed configuration at a basal pressure of 60 mmHg. Table 2, Table 3, Table 4, Table 5, Table 6 and Table 7 present MLA variations with IQR and p-values resulting from pairwise comparisons. The effect size of such comparisons, expressed as median difference and 95% CI, is provided in the Appendix A (Table A1, Table A2, Table A3, Table A4, Table A5 and Table A6). Values are reported, for convenience, only for five levels of pressure that can be considered the lower and upper limits of blood pressure under different regimens: resting diastole, resting systole, medium-high effort, and extreme effort. For the sake of completeness, we also reported results regarding the prepulmonary course, but because of the small sample size (n = 3), statistical analysis was not performed.
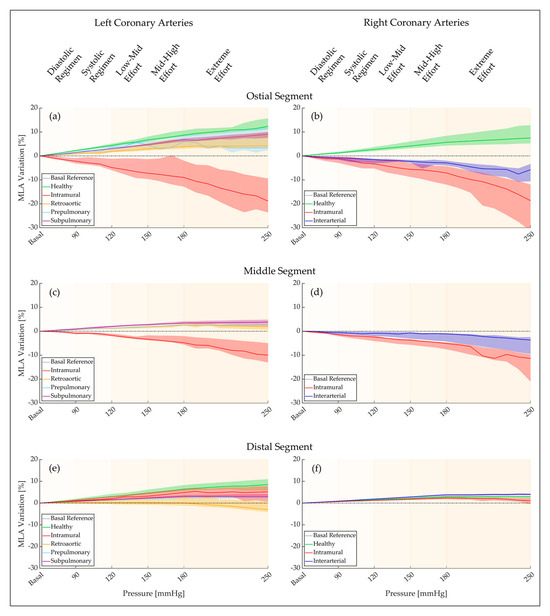
Figure 4.
Median luminal area variations of coronary vessels at increasing simulated blood pressure: (a) ostial segment of the LCAs; (b) ostial segment of the RCAs; (c) middle tract of the LCAs; (d) middle tract of the RCAs; (e) distal segment of the LCAs; (f) distal segment of the RCAs. MLA variations are shown in green for healthy coronaries, red for AAOCAs with intramural course, light blue for AAOCAs with prepulmonary course, yellow for AAOCAs with retroaortic course, purple for AAOCAs with subpulmonary course, blue for AAOCAs with interarterial course, and no intramural tract. The black dashed horizontal line represents null changes in the MLA with respect to the reference sections in basal conditions.
3.3.1. LCA Ostial Segment
MLA variations in the ostial segment of LCAs are presented in Table 2 for healthy, intramural, prepulmonary, subpulmonary, and retroaortic courses. Figure 4a shows that AAOCA with intramural courses is the only variant experiencing luminal narrowing. AAOCAs with intramural course differ significantly from healthy coronaries under any simulated pressure condition (p = 0.006 at 70 mmHg, p < 0.001 in all other cases) and from AAOCAs with subpulmonary course (p = 0.016), except for 70 mmHg. There are no statistically significant differences between intramural and retroaortic courses other than the one observed at 250 mmHg (p = 0.013). Healthy coronary arteries have significant differences from AAOCAs with retroaortic course at all simulated pressure levels and from AAOCAs with subpulmonary course, except for 70 mmHg. The median differences in MLA variations show that all AAOCAs have less expansion than healthy coronaries and that the greatest discrepancies occur for AAOCAs with intramural courses (Table A1).

Table 2.
Median luminal area variation of the ostial segment in left coronary arteries.
Table 2.
Median luminal area variation of the ostial segment in left coronary arteries.
| LCA OST | Simulated Pressure [mmHg] | |||||
|---|---|---|---|---|---|---|
| Course | 70 | 90 | 120 | 180 | 250 | |
| MLA Variation [%] | HC | 0.76 (0.21) | 2.24 (0.62) | 4.37 (1.41) | 8.71 (2.54) | 12.38 (4.59) |
| IM | −0.76 (1.57) | −2.23 (2.31) | −4.88 (4.8) | −9 (10.84) | −18.87 (14.19) | |
| PP | 0.31 (0.31) | 1.38 (0.93) | 3.53 (2.02) | 5.95 (4.57) | 3.36 (9.71) | |
| SP | 0.5 (0.15) | 1.4 (0.25) | 2.95 (0.36) | 6.79 (1.34) | 9.05 (2.52) | |
| RA | 0.3 (0.34) | 0.91 (0.49) | 1.89 (1.22) | 3.85 (3.69) | 4.24 (6.34) | |
| p-value | IM vs. HC | 0.006 | <0.001 | <0.001 | <0.001 | <0.001 |
| IM vs. SP | 1.000 | 0.016 | 0.016 | 0.016 | 0.016 | |
| IM vs. RA | 1.000 | 0.200 | 0.080 | 0.080 | 0.013 | |
| SP vs. HC | 0.099 | 0.027 | 0.022 | 0.022 | 0.033 | |
| RA vs. HC | 0.005 | 0.003 | 0.004 | 0.006 | 0.028 | |
HC: healthy coronary; IM: intramural; PP: prepulmonary; SP: subpulmonary; RA: retroaortic.
3.3.2. LCA Middle Segment
MLA variations in the middle segment of LCAs are presented in Table 3 for intramural, prepulmonary, subpulmonary, and retroaortic courses. Figure 4c shows that AAOCA with intramural courses is the only variant subject to a reduction in luminal area. AAOCAs with intramural course differ significantly from AAOCAs with subpulmonary and retroaortic course (p = 0.009, p = 0.004, respectively) under any simulated pressure condition, except for 70 mmHg. The median differences in MLA variations show that AAOCAs with intramural courses enlarge less than the other types of anomalous courses (Table A2).

Table 3.
Median luminal area variation of the middle segment in left coronary arteries.
Table 3.
Median luminal area variation of the middle segment in left coronary arteries.
| LCA MID | Simulated Pressure [mmHg] | |||||
|---|---|---|---|---|---|---|
| Course | 70 | 90 | 120 | 180 | 250 | |
| MLA Variation [%] | IM | −0.14 (0.3) | −0.81 (0.8) | −1.8 (1.01) | −4.8 (3.55) | −9.98 (8.09) |
| PP | 0.18 (0.09) | 0.63 (0.15) | 1.25 (0.4) | 2.58 (0.66) | 2.46 (0.63) | |
| SP | 0.29 (0.21) | 0.88 (0.47) | 2.01 (0.62) | 3.43 (1.03) | 3.85 (2.2) | |
| RA | 0.2 (0.14) | 0.65 (0.28) | 1.21 (0.57) | 2.63 (1.13) | 1.96 (2.05) | |
| p-value | IM vs. SP | 0.112 | 0.009 | 0.009 | 0.009 | 0.009 |
| IM vs. RA | 0.076 | 0.004 | 0.004 | 0.004 | 0.004 | |
IM: intramural; PP: prepulmonary; SP: subpulmonary; RA: retroaortic.
3.3.3. LCA Distal Segment
MLA variations in the distal segment of LCAs are presented in Table 4 for healthy, intramural, prepulmonary, subpulmonary, and retroaortic courses. Figure 4e shows that AAOCA with a retroaortic course undergoes luminal narrowing for high values of simulated blood pressure. There are no significant differences between AAOCAs with intramural courses and AAOCAs without intramural courses. Healthy coronary arteries differ significantly from AAOCAs with a retroaortic course under simulated pressure conditions. The median differences in MLA variations show that the greatest discrepancies occur when comparing healthy coronaries and AAOCAs with retroaortic courses (Table A3).

Table 4.
Median luminal area variation of the distal segment in left coronary arteries.
Table 4.
Median luminal area variation of the distal segment in left coronary arteries.
| LCA DIS | Simulated Pressure [mmHg] | |||||
|---|---|---|---|---|---|---|
| Course | 70 | 90 | 120 | 180 | 250 | |
| MLA Variation [%] | HC | 0.49 (0.17) | 1.36 (0.67) | 2.99 (1.63) | 6.41 (2.66) | 8.52 (5.2) |
| IM | 0.42 (0.31) | 1.03 (1.21) | 2.08 (1.81) | 4.86 (3.55) | 5.15 (7.12) | |
| PP | 0.21 (0.07) | 0.6 (0.25) | 1.19 (0.42) | 2.4 (0.84) | 2.38 (0.77) | |
| SP | 0.27 (0.05) | 0.78 (0.29) | 1.62 (0.44) | 3.02 (1.03) | 2.9 (1.46) | |
| RA | 0.12 (0.21) | 0.23 (0.92) | 0.33 (1.91) | 0.08 (4.26) | −2.94 (4.93) | |
| p-value | IM vs. HC | 1.000 | 1.000 | 0.400 | 0.320 | 0.286 |
| IM vs. SP | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | |
| IM vs. RA | 0.813 | 0.426 | 0.200 | 0.293 | 0.127 | |
| SP vs. HC | 0.139 | 0.069 | 0.058 | 0.050 | 0.058 | |
| RA vs. HC | 0.005 | 0.006 | 0.005 | 0.014 | 0.002 | |
HC: healthy coronary; IM: intramural; PP: prepulmonary; SP: subpulmonary; RA: retroaortic.
3.3.4. RCA Ostial Segment
MLA variations in the ostial segment of RCAs are presented in Table 5 for healthy, intramural, and interarterial courses. Figure 4b shows that both AAOCAs with intramural courses and AAOCAs with interarterial courses are subject to a reduction in luminal area. The comparison between these two types of courses is not statistically significant, while both differ significantly from healthy coronary arteries (p < 0.001) under any simulated blood pressure conditions. The median differences in MLA variations show that the greatest discrepancies occur when comparing healthy coronaries and AAOCAs with intramural courses (Table A4).

Table 5.
Median luminal area variation of the ostial segment in right coronary arteries.
Table 5.
Median luminal area variation of the ostial segment in right coronary arteries.
| RCA OST | Simulated Pressure [mmHg] | |||||
|---|---|---|---|---|---|---|
| Course | 70 | 90 | 120 | 180 | 250 | |
| MLA Variation [%] | HC | 0.55 (0.35) | 1.25 (0.88) | 2.69 (1.77) | 5.68 (4.07) | 7.49 (7.66) |
| IM | −0.59 (1.14) | −1.19 (2.62) | −3.34 (3.42) | −7.11 (7.67) | −18.69 (19.32) | |
| IA | −0.37 (0.61) | −0.81 (1.08) | −1.54 (1.89) | −2.9 (2.04) | −5.75 (7.28) | |
| p-value | IM vs. HC | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| IM vs. IA | 1.000 | 1.000 | 0.378 | 0.256 | 0.167 | |
| IA vs. HC | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |
HC: healthy coronary; IM: intramural; IA: interarterial.
3.3.5. RCA Middle Segment
MLA variations in the middle segment of RCAs are presented in Table 6 for intramural and interarterial courses. Figure 4d shows that both AAOCAs with intramural courses and AAOCAs with interarterial courses experience luminal narrowing. The comparison between these two types of courses is statistically significant under any simulated pressure condition, except for 70 mmHg.

Table 6.
Median luminal area variation of the middle segment in right coronary arteries.
Table 6.
Median luminal area variation of the middle segment in right coronary arteries.
| RCA MID | Simulated Pressure [mmHg] | |||||
|---|---|---|---|---|---|---|
| Course | 70 | 90 | 120 | 180 | 250 | |
| MLA Variation [%] | IM | −0.41 (0.58) | −1.46 (1.06) | −2.46 (2.34) | −5.13 (2.91) | −11.36 (11.38) |
| IA | 0.01 (0.35) | −0.53 (1.2) | −0.8 (1.69) | −1.11 (3.39) | −3.67 (7.04) | |
| p-value | IM vs. IA | 0.285 | 0.020 | 0.027 | 0.006 | 0.002 |
IM: intramural; IA: interarterial.
3.3.6. RCA Distal Segment
MLA variations in the ostial segment of RCAs are presented in Table 7 for healthy, intramural, and interarterial courses. Figure 4f shows that both healthy coronaries and AAOCAs are not subject to luminal narrowing. There are no significant differences other than the one observed by comparing AAOCAs with intramural courses and healthy coronaries at 250 mmHg (p = 0.013). The median differences in MLA variations show that AAOCAs with intramural courses have less expansion than the other course types (Table A6).

Table 7.
Median luminal area variation of the distal segment in right coronary arteries.
Table 7.
Median luminal area variation of the distal segment in right coronary arteries.
| RCA DIS | Simulated Pressure [mmHg] | |||||
|---|---|---|---|---|---|---|
| Course | 70 | 90 | 120 | 180 | 250 | |
| MLA Variation [%] | HC | 0.24 (0.07) | 0.72 (0.23) | 1.44 (0.35) | 2.92 (0.8) | 2.91 (0.71) |
| IM | 0.23 (0.13) | 0.65 (0.22) | 1.24 (0.4) | 2.32 (0.97) | 1.1 (2.89) | |
| IA | 0.29 (0.1) | 0.91 (0.19) | 1.87 (0.46) | 3.85 (0.68) | 3.98 (0.76) | |
| p-value | IM vs. HC | 0.919 | 0.528 | 0.623 | 0.175 | 0.018 |
| IM vs. IA | 0.625 | 0.050 | 0.068 | 0.068 | 0.068 | |
| IA vs. HC | 1.000 | 0.076 | 0.231 | 0.203 | 0.263 | |
HC: healthy coronary; IM: intramural; IA: interarterial.
In addition, the comparison between left AAOCAs with intramural courses and right AAOCAs with intramural courses does not show any statistically significant differences.
3.4. Proximal to Distal Narrowing
The MLAs of the ostial, middle, and distal zones of healthy and anomalous coronary arteries are summarized as median and IQR in Table A7 for the LCAs and in Table A8 for the RCAs. Table 8 and Table 9 report the percentage of proximal course narrowing in relation to the distal segment for each different type of anomalous course in the LCAs and RCAs, respectively. We recall that negative values indicate the absence of proximal stenosis, i.e., the proximal segment has a greater MLA than the distal segment. The prepulmonary and retroaortic courses do not exhibit proximal narrowing. The subpulmonary course has a reduction of the MLA both at the ostial and middle levels compared with the distal reference, which ranges from 16% to 19% under all simulated pressure conditions. The intramural course in LCAs shows ostial and middle stenosis of 25% and 48% in basal condition, increasing to 48% and 56%, respectively, with a simulated pressure of 250 mmHg. The interarterial course has a reduction of the MLA in the ostial and middle zones compared with the distal reference, which never exceeds a value of 30%. The intramural course in RCAs presents ostial and middle stenosis of 42% and 44% in basal condition, increasing to 59% and 50%, respectively, with a simulated pressure of 250 mmHg.

Table 8.
LCA. Proximal to distal narrowing [%].

Table 9.
RCA: Proximal to distal narrowing [%].
4. Discussion
The present study proposes a patient-specific computational pipeline for modeling and simulation of the different AAOCA variants. We used structural FEAs to simulate blood pressure regimens ranging from rest to extreme effort, and we analyzed the pressurized geometries to evaluate enlargement or narrowing along the coronary vessels at the different loading conditions. Then, we compared homologous segments to assess differences in behavior between healthy and anomalous coronaries and between anomalous coronaries with and without intramural courses. Furthermore, we derived the percentage of proximal course narrowing in relation to the distal segment at rest and under effort. Our results showed that the method herein described is able to accurately reproduce the patient-specific anatomy, regardless of the type of anomaly, ensuring that the computational domain used in the structural simulations reliably reflects the aortic root and coronary arteries of the patients under investigation. The structural simulation results revealed that AAOCAs with interarterial and intramural courses have segment-specific compression along their entire proximal length that increases with increasing physical effort and that is not observed in the other types of anomalous courses. The presence of the intramural tract further magnifies the narrowing effect, in accordance with the literature that recognizes the intramural segment as a high-risk anatomical feature since it may impede blood flow to the myocardium and cause ischemia and SCD [3,4,5,6,7,8]. AAOCAs with a subpulmonary course enlarge their caliber along the entire vessel length, but they expand less than the healthy coronaries at the ostium. AAOCAs with a retroaortic course, compared with healthy coronary arteries, show less expansion of the cross-sectional area at the ostial and distal segments, with slight distal narrowing at higher values of aortic pressure. The smaller ostial expansion of these two anomalous courses could find an explanation considering that, since the coronary vessel passes obliquely through the aortic wall for a short distance (Figure 2b,c), its ability to expand could be compromised near the origin [22]. The distal narrowing of the retroaortic course, instead, might be an effect due to the LVOT expansion.
The percentage of proximal course narrowing in relation to the distal segment is commonly adopted to evaluate the severity of fixed stenosis, and in cases of a value above 50%, revascularization of the proximal vessel may be considered [21]. We found that the subpulmonary and interarterial courses presented mild stenosis in the proximal segment, suggesting that these anomalies should be brought to clinical attention, but only AAOCAs with intramural courses reached a critical narrowing with an indication for surgical treatment. The percentage of stenosis was measured using MLAs, so it is representative of the entire length of the proximal segment, which is another anatomical feature that plays a key role in the pathology [3,21]. Notably, our analysis showed that the severity of stenosis increases from diastole to systole, even in resting conditions, confirming the importance of a dynamic evaluation of the intramural course during the whole cardiac cycle [23]; moreover, the proximal to distal narrowing became more relevant under effort conditions. These findings highlight the necessity to characterize the AAOCAs, particularly the AAOCA with an intramural course, not only at rest but also under a range of physical conditions. Our work directly addresses this necessity, using patient-specific structural FEAs to investigate conditions that cannot be reproduced in clinical practice and providing information to support decision-making in the management and treatment of AAOCA patients. Diagnosis and anatomical evaluation of AAOCAs, routinely performed with coronary CTA at rest, could be supplemented with the assessment of intramural segment compression under simulated exertion. Analysis of the luminal cross-sectional areas at different pressure levels may reveal a dynamic stenosis [21] that becomes significant only during effort conditions, the threat of which could be underestimated by relying exclusively on conventional assessment of lumen morphology. The approach presented in this paper has the potential to increase the diagnostic information that can be extracted from CTA scans about anomalous coronary arteries, especially for patients with milder versions of high-risk anatomic features. Thus, the indication for further non-invasive or invasive diagnostic investigations to evaluate the hemodynamic relevance of the anomalous vessel and, consequently, a possible indication for surgery might be suggested in the first place by a patient-specific structural simulation based on coronary CTA imaging.
Limitation. The prediction of our model should be validated with clinical data, but the specific validation scenario is complex to achieve. On the one hand, dobutamine can induce physical adaptations that typically occur under effort conditions (increased stroke volume, heart rate, and blood pressure) and may highlight the mechanism of lateral compression by aortic expansion. On the other hand, a low heart rate is necessary during CTA acquisition to optimize image quality and interpretability [24], and IVUS imaging with dobutamine infusion is an invasive procedure, not feasible in every patient, technically challenging, and with a non-negligible risk [22]. Furthermore, extreme pressure regimes that can be simulated with computational tools cannot be reproduced in a clinical environment without endangering patients with AAOCAs. For these reasons, there is currently no study that has validated AAOCA models, especially the lateral compression of the intramural segment, against invasive measurements (i.e., IVUS) [25]. This is a limitation that needs to be addressed in future work to take a step toward the application of computational models of the AAOCA in clinical practice.
The geometric model described in this paper does not consider the patient-specific thickness of the aortic and coronary arterial walls. Regarding the material model, the assumption of a neo-Hookean formulation does not take into account the highly nonlinear and anisotropic behavior of the aorta and coronary arteries. Moreover, the present study considered a stress-free configuration of the modelized vessels as a starting point, disregarding the diastolic pressure. Then, incremental loads were applied to simulate blood pressure ranging from rest to extreme effort, assuming that the geometry is built to resemble the patient’s anatomy at the diastolic phase of the cardiac cycle. In order to accurately model the stress distribution and the corresponding deformation of the aortic and coronary walls, further development of the study should target these approximations by implementing strategies to model pre-stress [26,27], incorporating a more complex constitutive model [28], and assigning patient-specific arterial wall thickness retrieved from other imaging modalities.
5. Conclusions
The modeling and simulation workflow presented in this paper demonstrated the ability to accurately reproduce the patient-specific anatomy of any AAOCA variant and capture pathological behaviors in accordance with clinical hypotheses. Our pipeline, based on patient-specific structural FEAs, could serve as a computational tool capable of complementing current diagnostic procedures by investigating effort conditions that cannot be reproduced in clinical practice, retrieving the degree of narrowing and the critical locations of the phenomenon, and supporting decision-making in the management and treatment of AAOCAs without any risk to patient safety.
Author Contributions
Conceptualization, A.R., M.L.R. and M.C.; methodology, A.R., M.L.R. and M.C.; formal analysis, A.R.; investigation, A.R.; resources, F.S.; software, A.R. and S.A.; writing—original draft preparation, A.R.; writing—review and editing, A.R., M.L.R. and M.C.; visualization, S.A., V.C. and A.F.P.; supervision, M.C.; project administration, M.L.R. and M.C. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by IRCCS Policlinico San Donato, a clinical research hospital partially funded by the Italian Ministry of Health.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the IRCCS Policlinico San Donato review board (protocol number: 63/int/2019). All subjects gave their informed consent for inclusion before they participated in the study.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Acknowledgments
The authors thank Giovanni Maria Formato for the preliminary activity on this study.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A

Table A1.
Median luminal area variation of the ostial segment in left coronary arteries.
Table A1.
Median luminal area variation of the ostial segment in left coronary arteries.
| LCA OST | Simulated Pressure [mmHg] | |||||
|---|---|---|---|---|---|---|
| Course | 70 | 90 | 120 | 180 | 250 | |
| MLA Variation [%] | HC | 0.76 (0.21) | 2.24 (0.62) | 4.37 (1.41) | 8.71 (2.54) | 12.38 (4.59) |
| IM | −0.76 (1.57) | −2.23 (2.31) | −4.88 (4.8) | −9 (10.84) | −18.87 (14.19) | |
| PP | 0.31 (0.31) | 1.38 (0.93) | 3.53 (2.02) | 5.95 (4.57) | 3.36 (9.71) | |
| SP | 0.5 (0.15) | 1.4 (0.25) | 2.95 (0.36) | 6.79 (1.34) | 9.05 (2.52) | |
| RA | 0.3 (0.34) | 0.91 (0.49) | 1.89 (1.22) | 3.85 (3.69) | 4.24 (6.34) | |
| p-value | IM vs. HC | 0.006 | <0.001 | <0.001 | <0.001 | <0.001 |
| IM vs. SP | 1.000 | 0.016 | 0.016 | 0.016 | 0.016 | |
| IM vs. RA | 1.000 | 0.200 | 0.080 | 0.080 | 0.013 | |
| SP vs. HC | 0.099 | 0.027 | 0.022 | 0.022 | 0.033 | |
| RA vs. HC | 0.005 | 0.003 | 0.004 | 0.006 | 0.028 | |
| Effect Size [%] | IM vs. HC | −1.5 [−2.2, −0.2] | −4.5 [−5.6, −2] | −9.2 [−10.8, −4] | −17.7 [−22.6, −8] | −31.3 [−46.2, −25.2] |
| IM vs. SP | −1.3 [−2, 0.1] | −3.6 [−4.7, −1.1] | −7.8 [−9.2, −2.7] | −15.8 [−20.9, −6] | −27.9 [−38, −18.5] | |
| IM vs. RA | −1.1 [−1.7, 0.2] | −3.1 [−4.3, −0.8] | −6.8 [−8.7, −1.7] | −12.8 [−19, −3.1] | −23.1 [−34.2, −11.5] | |
| SP vs. HC | −0.3 [−0.4, −0.1] | −0.8 [−1.2, −0.5] | −1.4 [−2.2, −0.9] | −1.9 [−3.3, −1] | −3.3 [−6, −0.9] | |
| RA vs. HC | −0.5 [−0.9, −0.3] | −1.3 [−1.9, −0.8] | −2.5 [−3.6, −1.3] | −4.9 [−6.8, −1] | −8.1 [−11.8, −1.4] | |
HC: healthy coronary; IM: intramural; PP: prepulmonary; SP: subpulmonary; RA: retroaortic.

Table A2.
Median luminal area variation of the middle segment in left coronary arteries.
Table A2.
Median luminal area variation of the middle segment in left coronary arteries.
| LCA MID | Simulated Pressure [mmHg] | |||||
|---|---|---|---|---|---|---|
| Course | 70 | 90 | 120 | 180 | 250 | |
| MLA Variation [%] | IM | −0.14 (0.3) | −0.81 (0.8) | −1.8 (1.01) | −4.8 (3.55) | −9.98 (8.09) |
| PP | 0.18 (0.09) | 0.63 (0.15) | 1.25 (0.4) | 2.58 (0.66) | 2.46 (0.63) | |
| SP | 0.29 (0.21) | 0.88 (0.47) | 2.01 (0.62) | 3.43 (1.03) | 3.85 (2.2) | |
| RA | 0.2 (0.14) | 0.65 (0.28) | 1.21 (0.57) | 2.63 (1.13) | 1.96 (2.05) | |
| p-value | IM vs. SP | 0.112 | 0.009 | 0.009 | 0.009 | 0.009 |
| IM vs. RA | 0.076 | 0.004 | 0.004 | 0.004 | 0.004 | |
| Effect Size [%] | IM vs. SP | −0.4 [−0.8, −0.2] | −1.7 [−2.6, −1.2] | −3.8 [−5.9, −2.9] | −8.2 [−9.7, −5.2] | −13.8 [−18.2, −8.2] |
| IM vs. RA | −0.3 [−0.8, 0.2] | −1.5 [−3.4, −1.1] | −3 [−5.1, −2.1] | −7.4 [−9.6, −4.4] | −11.9 [−15.8, −6.3] | |
IM: intramural; PP: prepulmonary; SP: subpulmonary; RA: retroaortic.

Table A3.
Median luminal area variation of the distal segment in left coronary arteries.
Table A3.
Median luminal area variation of the distal segment in left coronary arteries.
| LCA DIS | Simulated Pressure [mmHg] | |||||
|---|---|---|---|---|---|---|
| Course | 70 | 90 | 120 | 180 | 250 | |
| MLA Variation [%] | HC | 0.49 (0.17) | 1.36 (0.67) | 2.99 (1.63) | 6.41 (2.66) | 8.52 (5.2) |
| IM | 0.42 (0.31) | 1.03 (1.21) | 2.08 (1.81) | 4.86 (3.55) | 5.15 (7.12) | |
| PP | 0.21 (0.07) | 0.6 (0.25) | 1.19 (0.42) | 2.4 (0.84) | 2.38 (0.77) | |
| SP | 0.27 (0.05) | 0.78 (0.29) | 1.62 (0.44) | 3.02 (1.03) | 2.9 (1.46) | |
| RA | 0.12 (0.21) | 0.23 (0.92) | 0.33 (1.91) | 0.08 (4.26) | −2.94 (4.93) | |
| p-value | IM vs. HC | 1.000 | 1.000 | 0.400 | 0.320 | 0.286 |
| IM vs. SP | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | |
| IM vs. RA | 0.813 | 0.426 | 0.200 | 0.293 | 0.127 | |
| SP vs. HC | 0.139 | 0.069 | 0.058 | 0.050 | 0.058 | |
| RA vs. HC | 0.005 | 0.006 | 0.005 | 0.014 | 0.002 | |
| Effect Size [%] | IM vs. HC | −0.1 [−0.4, 0.1] | −0.3 [−1.1, 0.8] | −0.9 [−2.1, 0.9] | −1.6 [−4.1, 0.8] | −3.4 [−9.7, 0.7] |
| IM vs. SP | 0.1 [−0.1, 0.3] | 0.3 [−0.3, 1.4] | 0.5 [−0.6, 1.9] | 1.8 [−0.7, 4.1] | 2.3 [−4, 5.6] | |
| IM vs. RA | 0.3 [0, 0.6] | 0.8 [−0.1, 2.1] | 1.8 [0.3, 3.8] | 4.8 [0.3, 8.5] | 8.1 [2, 15.1] | |
| SP vs. HC | −0.2 [−0.3, −0.1] | −0.6 [−1.1, −0.1] | −1.4 [−2.2, −0.8] | −3.4 [−5.4, −2.3] | −5.6 [−8.3, −3.6] | |
| RA vs. HC | −0.4 [−0.6, −0.1] | −1.1 [−2, −0.5] | −2.7 [−3.9, −1.3] | −6.3 [−8.9, −1.6] | −11.5 [−16.8, −6.9] | |
HC: healthy coronary; IM: intramural; PP: prepulmonary; SP: subpulmonary; RA: retroaortic.

Table A4.
Median luminal area variation of the ostial segment in right coronary arteries.
Table A4.
Median luminal area variation of the ostial segment in right coronary arteries.
| RCA OST | Simulated Pressure [mmHg] | |||||
|---|---|---|---|---|---|---|
| Course | 70 | 90 | 120 | 180 | 250 | |
| MLA Variation [%] | HC | 0.55 (0.35) | 1.25 (0.88) | 2.69 (1.77) | 5.68 (4.07) | 7.49 (7.66) |
| IM | −0.59 (1.14) | −1.19 (2.62) | −3.34 (3.42) | −7.11 (7.67) | −18.69 (19.32) | |
| IA | −0.37 (0.61) | −0.81 (1.08) | −1.54 (1.89) | −2.9 (2.04) | −5.75 (7.28) | |
| p-value | IM vs. HC | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| IM vs. IA | 1.000 | 1.000 | 0.378 | 0.256 | 0.167 | |
| IA vs. HC | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |
| Effect Size [%] | IM vs. HC | −1.1 [−1.8, −0.5] | −2.4 [−4.2, −1.4] | −6 [−7.9, −3.5] | −12.8 [−17.7, −8.5] | −26.2 [−39.4, −17.6] |
| IM vs. IA | −0.2 [−1.1, 0.6] | −0.4 [−2.4, 1.1] | −1.8 [−4, 0.6] | −4.2 [−8, 2.3] | −12.9 [−27.4, −2.8] | |
| IA vs. HC | −0.9 [−1.6, −0.6] | −2.1 [−3.5, −1.5] | −4.2 [−5.7, −2.4] | −8.6 [−12, −6.5] | −13.2 [−18.9, −7] | |
HC: healthy coronary; IM: intramural; IA: interarterial.

Table A5.
Median luminal area variation of the middle segment in right coronary arteries.
Table A5.
Median luminal area variation of the middle segment in right coronary arteries.
| RCA MID | Simulated Pressure [mmHg] | |||||
|---|---|---|---|---|---|---|
| Course | 70 | 90 | 120 | 180 | 250 | |
| MLA Variation [%] | IM | −0.41 (0.58) | −1.46 (1.06) | −2.46 (2.34) | −5.13 (2.91) | −11.36 (11.38) |
| IA | 0.01 (0.35) | −0.53 (1.2) | −0.8 (1.69) | −1.11 (3.39) | −3.67 (7.04) | |
| p-value | IM vs. IA | 0.285 | 0.020 | 0.027 | 0.006 | 0.002 |
| Effect Size [%] | IM vs. IA | −0.4 [−0.9, 0] | −0.9 [−2, 0.1] | −1.7 [−3.8, −0.1] | −4 [−6.8, −0.4] | −7.7 [−19.7, −1.1] |
IM: intramural; IA: interarterial.

Table A6.
Median luminal area variation of the distal segment in right coronary arteries.
Table A6.
Median luminal area variation of the distal segment in right coronary arteries.
| RCA DIS | Simulated Pressure [mmHg] | |||||
|---|---|---|---|---|---|---|
| Course | 70 | 90 | 120 | 180 | 250 | |
| MLA Variation [%] | HC | 0.24 (0.07) | 0.72 (0.23) | 1.44 (0.35) | 2.92 (0.8) | 2.91 (0.71) |
| IM | 0.23 (0.13) | 0.65 (0.22) | 1.24 (0.4) | 2.32 (0.97) | 1.1 (2.89) | |
| IA | 0.29 (0.1) | 0.91 (0.19) | 1.87 (0.46) | 3.85 (0.68) | 3.98 (0.76) | |
| p-value | IM vs. HC | 0.919 | 0.528 | 0.623 | 0.175 | 0.018 |
| IM vs. IA | 0.625 | 0.050 | 0.068 | 0.068 | 0.068 | |
| IA vs. HC | 1.000 | 0.076 | 0.231 | 0.203 | 0.263 | |
| Effect Size [%] | IM vs. HC | 0 [−0.1, 0.4] | −0.1 [−0.2, 0.7] | −0.2 [−0.6, 0] | −0.6 [−1.3, 0.1] | −1.8 [−3.9, −0.9] |
| IM vs. IA | −0.1 [−0.2, 0.1] | −0.3 [−0.4, 0] | −0.6 [−1.1, −0.3] | −1.5 [−2.2, −0.8] | −2.9 [−5, −1.4] | |
| IA vs. HC | 0 [0, 0.6] | 0.2 [0, 0.5] | 0.4 [0, 0.8] | 0.9 [0.3, 1.5] | 1.1 [−0.6, 1.7] | |
HC: healthy coronary; IM: intramural; IA: interarterial.

Table A7.
Median luminal area in left coronary arteries.
Table A7.
Median luminal area in left coronary arteries.
| LCA | Simulated Pressure [mmHg] | |||||
|---|---|---|---|---|---|---|
| Course | Basal | 90 | 120 | 180 | 250 | |
| OST MLA [mm2] | HC | 14.27 | 14.60 | 14.90 | 15.49 | 16.41 |
| IM | 9.79 | 9.75 | 9.55 | 8.87 | 7.17 | |
| PP | 8.36 | 8.48 | 8.66 | 8.86 | 8.54 | |
| SP | 5.94 | 6.01 | 6.09 | 6.27 | 6.38 | |
| RA | 5.89 | 5.98 | 6.08 | 6.29 | 6.41 | |
| MID MLA [mm2] | IM | 6.78 | 6.73 | 6.66 | 6.50 | 6.07 |
| PP | 5.60 | 5.66 | 5.72 | 5.84 | 5.87 | |
| SP | 6.14 | 6.19 | 6.24 | 6.35 | 6.37 | |
| RA | 5.37 | 5.38 | 5.39 | 5.46 | 5.36 | |
| DIS MLA [mm2] | HC | 11.55 | 11.71 | 11.87 | 12.26 | 12.48 |
| IM | 13.05 | 13.18 | 13.31 | 13.71 | 13.82 | |
| PP | 2.77 | 2.78 | 2.80 | 2.83 | 2.83 | |
| SP | 7.37 | 7.41 | 7.47 | 7.60 | 7.63 | |
| RA | 4.41 | 4.38 | 4.36 | 4.31 | 4.18 | |
HC: healthy coronary; IM: intramural; PP: prepulmonary; SP: subpulmonary; RA: retroaortic.

Table A8.
Median luminal area in right coronary arteries.
Table A8.
Median luminal area in right coronary arteries.
| RCA | Simulated Pressure [mmHg] | |||||
|---|---|---|---|---|---|---|
| Course | Basal | 90 | 120 | 180 | 250 | |
| OST MLA [mm2] | HC | 9.30 | 9.44 | 9.61 | 10.00 | 10.34 |
| IM | 5.31 | 5.09 | 4.99 | 4.57 | 3.67 | |
| IA | 5.94 | 5.87 | 5.80 | 5.74 | 5.28 | |
| MID MLA [mm2] | IM | 5.13 | 5.05 | 4.98 | 4.78 | 4.40 |
| IA | 6.86 | 6.81 | 6.78 | 6.67 | 6.44 | |
| DIS MLA [mm2] | HC | 7.95 | 8.01 | 8.06 | 8.18 | 8.19 |
| IM | 9.15 | 9.19 | 9.22 | 9.25 | 8.88 | |
| IA | 7.17 | 7.22 | 7.27 | 7.37 | 7.39 | |
HC: healthy coronary; IM: intramural; IA: interarterial.
References
- Angelini, P. Coronary Artery Anomalies: An Entity in Search of an Identity. Circulation 2007, 115, 1296–1305. [Google Scholar] [CrossRef]
- Cheezum, M.K.; Ghoshhajra, B.; Bittencourt, M.S.; Hulten, E.A.; Bhatt, A.; Mousavi, N.; Shah, N.R.; Valente, A.M.; Rybicki, F.J.; Steigner, M.; et al. Anomalous Origin of the Coronary Artery Arising from the Opposite Sinus: Prevalence and Outcomes in Patients Undergoing Coronary CTA. Eur. Heart J.-Cardiovasc. Imaging 2017, 18, 224–235. [Google Scholar] [CrossRef] [PubMed]
- Jegatheeswaran, A.; Devlin, P.J.; McCrindle, B.W.; Williams, W.G.; Jacobs, M.L.; Blackstone, E.H.; DeCampli, W.M.; Caldarone, C.A.; Gaynor, J.W.; Kirklin, J.K.; et al. Features Associated with Myocardial Ischemia in Anomalous Aortic Origin of a Coronary Artery: A Congenital Heart Surgeons’ Society Study. J. Thorac. Cardiovasc. Surg. 2019, 158, 822–834.e3. [Google Scholar] [CrossRef] [PubMed]
- Angelini, P.; Uribe, C. Critical Update and Discussion of the Prevalence, Nature, Mechanisms of Action, and Treatment Options in Potentially Serious Coronary Anomalies. Trends Cardiovasc. Med. 2022, S1050173822000743. [Google Scholar] [CrossRef]
- Maron, B.J. Sudden Death in Young Competitive Athletes: Clinical, Demographic, and Pathological Profiles. JAMA 1996, 276, 199. [Google Scholar] [CrossRef] [PubMed]
- Basso, C.; Maron, B.J.; Corrado, D.; Thiene, G. Clinical Profile of Congenital Coronary Artery Anomalies with Origin from the Wrong Aortic Sinus Leading to Sudden Death in Young Competitive Athletes. J. Am. Coll. Cardiol. 2000, 35, 1493–1501. [Google Scholar] [CrossRef]
- Gentile, F.; Castiglione, V.; De Caterina, R. Coronary Artery Anomalies. Circulation 2021, 144, 983–996. [Google Scholar] [CrossRef]
- Maron, B.J.; Doerer, J.J.; Haas, T.S.; Tierney, D.M.; Mueller, F.O. Sudden Deaths in Young Competitive Athletes: Analysis of 1866 Deaths in the United States, 1980–2006. Circulation 2009, 119, 1085–1092. [Google Scholar] [CrossRef]
- Lo Rito, M.; Romarowski, R.M.; Rosato, A.; Pica, S.; Secchi, F.; Giamberti, A.; Auricchio, F.; Frigiola, A.; Conti, M. Anomalous Aortic Origin of Coronary Artery Biomechanical Modeling: Toward Clinical Application. J. Thorac. Cardiovasc. Surg. 2021, 161, 191–201.e1. [Google Scholar] [CrossRef]
- Formato, G.M.; Lo Rito, M.; Auricchio, F.; Frigiola, A.; Conti, M. Aortic Expansion Induces Lumen Narrowing in Anomalous Coronary Arteries: A Parametric Structural Finite Element Analysis. J. Biomech. Eng. 2018, 140, 111008. [Google Scholar] [CrossRef]
- Agrawal, H.; Lamari-Fisher, A.; Hasbani, K.; Philip, S.; Fraser, C.D.; Mery, C.M. Decision Making in Anomalous Aortic Origin of a Coronary Artery. Expert Rev. Cardiovasc. Ther. 2023, 21, 177–191. [Google Scholar] [CrossRef] [PubMed]
- Qasim, A.; Doan, T.T.; Dan Pham, T.; Reaves-O’Neal, D.; Sachdeva, S.; Mery, C.M.; Binsalamah, Z.; Molossi, S. Is Exercise Stress Testing Useful for Risk Stratification in Anomalous Aortic Origin of a Coronary Artery? Semin. Thorac. Cardiovasc. Surg. 2022, S1043067922002088. [Google Scholar] [CrossRef] [PubMed]
- Doan, T.T.; Sachdeva, S.; Bonilla-Ramirez, C.; Reaves-O’Neal, D.L.; Masand, P.; Mery, C.M.; Binsalamah, Z.; Heinle, J.H.; Molossi, S. Ischemia in Anomalous Aortic Origin of a Right Coronary Artery: Large Pediatric Cohort Medium-Term Outcomes. Circ. Cardiovasc. Interv. 2023, 16, 147–156. [Google Scholar] [CrossRef] [PubMed]
- Antiga, L.; Piccinelli, M.; Botti, L.; Ene-Iordache, B.; Remuzzi, A.; Steinman, D.A. An Image-Based Modeling Framework for Patient-Specific Computational Hemodynamics. Med. Biol. Eng. Comput. 2008, 46, 1097. [Google Scholar] [CrossRef] [PubMed]
- Muraru, D.; Maffessanti, F.; Kocabay, G.; Peluso, D.; Bianco, L.D.; Piasentini, E.; Jose, S.P.; Iliceto, S.; Badano, L.P. Ascending Aorta Diameters Measured by Echocardiography Using Both Leading Edge-to-Leading Edge and Inner Edge-to-Inner Edge Conventions in Healthy Volunteers. Eur. Heart J.-Cardiovasc. Imaging 2014, 15, 415–422. [Google Scholar] [CrossRef]
- De Kerchove, L.; Jashari, R.; Boodhwani, M.; Duy, K.T.; Lengelé, B.; Gianello, P.; Nezhad, Z.M.; Astarci, P.; Noirhomme, P.; El Khoury, G. Surgical Anatomy of the Aortic Root: Implication for Valve-Sparing Reimplantation and Aortic Valve Annuloplasty. J. Thorac. Cardiovasc. Surg. 2015, 149, 425–433. [Google Scholar] [CrossRef]
- Yoshitani, H.; Takeuchi, M.; Ogawa, K.; Otsuji, Y. Comparison of Usefulness of the Wall Thickness of the Left Anterior Descending Coronary Artery, Determined by Transthoracic Echocardiography, and Carotid Intima-Media Thickness in Predicting Multivessel Coronary Artery Disease. J. Echocardiogr. 2009, 7, 2–8. [Google Scholar] [CrossRef]
- Jiang, M.X.; Khan, M.O.; Ghobrial, J.; Rogers, I.S.; Pettersson, G.B.; Blackstone, E.H.; Marsden, A.L. Patient-Specific Fluid–Structure Simulations of Anomalous Aortic Origin of Right Coronary Arteries. JTCVS Tech. 2022, 13, 144–162. [Google Scholar] [CrossRef]
- Sabbahi, A.; Arena, R.; Kaminsky, L.A.; Myers, J.; Phillips, S.A. Peak Blood Pressure Responses During Maximum Cardiopulmonary Exercise Testing: Reference Standards From FRIEND (Fitness Registry and the Importance of Exercise: A National Database). Hypertension 2018, 71, 229–236. [Google Scholar] [CrossRef]
- Cook, C.M.; Ahmad, Y.; Howard, J.P.; Shun-Shin, M.J.; Sethi, A.; Clesham, G.J.; Tang, K.H.; Nijjer, S.S.; Kelly, P.A.; Davies, J.R.; et al. Impact of Percutaneous Revascularization on Exercise Hemodynamics in Patients with Stable Coronary Disease. J. Am. Coll. Cardiol. 2018, 72, 970–983. [Google Scholar] [CrossRef]
- Bigler, M.R.; Ashraf, A.; Seiler, C.; Praz, F.; Ueki, Y.; Windecker, S.; Kadner, A.; Räber, L.; Gräni, C. Hemodynamic Relevance of Anomalous Coronary Arteries Originating From the Opposite Sinus of Valsalva-In Search of the Evidence. Front. Cardiovasc. Med. 2021, 7, 591326. [Google Scholar] [CrossRef]
- Bigler, M.R.; Kadner, A.; Räber, L.; Ashraf, A.; Windecker, S.; Siepe, M.; Padalino, M.A.; Gräni, C. Therapeutic Management of Anomalous Coronary Arteries Originating From the Opposite Sinus of Valsalva: Current Evidence, Proposed Approach, and the Unknowing. JAHA 2022, 11, e027098. [Google Scholar] [CrossRef]
- Formato, G.M.; Agnifili, M.L.; Arzuffi, L.; Rosato, A.; Ceserani, V.; Zuniga Olaya, K.G.; Secchi, F.; Deamici, M.; Conti, M.; Auricchio, F.; et al. Morphological Changes of Anomalous Coronary Arteries From the Aorta During the Cardiac Cycle Assessed by IVUS in Resting Conditions. Circ. Cardiovasc. Interv. 2023, 16, e012636. [Google Scholar] [CrossRef]
- Stocker, T.J.; Leipsic, J.; Chen, M.Y.; Achenbach, S.; Knuuti, J.; Newby, D.; Hausleiter, J. Influence of Heart Rate on Image Quality and Radiation Dose Exposure in Coronary CT Angiography. Radiology 2021, 300, 701–703. [Google Scholar] [CrossRef]
- Stark, A.W.; Giannopoulos, A.A.; Pugachev, A.; Shiri, I.; Haeberlin, A.; Räber, L.; Obrist, D.; Gräni, C. Application of Patient-Specific Computational Fluid Dynamics in Anomalous Aortic Origin of Coronary Artery: A Systematic Review. JCDD 2023, 10, 384. [Google Scholar] [CrossRef]
- Votta, E.; Presicce, M.; Della Corte, A.; Dellegrottaglie, S.; Bancone, C.; Sturla, F.; Redaelli, A. A Novel Approach to the Quantification of Aortic Root in Vivo Structural Mechanics: Numerical Modelling of Aortic Root in Vivo Structural Mechanics. Int. J. Numer. Meth. Biomed. Engng. 2017, 33, e2849. [Google Scholar] [CrossRef]
- Bols, J.; Degroote, J.; Trachet, B.; Verhegghe, B.; Segers, P.; Vierendeels, J. A Computational Method to Assess the in Vivo Stresses and Unloaded Configuration of Patient-Specific Blood Vessels. J. Comput. Appl. Math. 2013, 246, 10–17. [Google Scholar] [CrossRef]
- Holzapfel, G.A.; Sommer, G.; Gasser, C.T.; Regitnig, P. Determination of Layer-Specific Mechanical Properties of Human Coronary Arteries with Nonatherosclerotic Intimal Thickening and Related Constitutive Modeling. Am. J. Physiol.-Heart Circ. Physiol. 2005, 289, H2048–H2058. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).