Abstract
A structural and organizational redesign of the dental care system is necessary today due to current trends in the demographic process and the accompanying changes in the population’s healthcare needs. The purpose of this article is to review the literature, analyzing those trends that today represent useful tools for the oral health of pediatric patients, with particular reference to teledentistry and all the supports it uses to reach remote territories or patients who, for various reasons, cannot have access to dental care. An independent literature search was conducted in three electronic databases: PubMed/MEDLINE, Google Scholar, and the COCHRANE library. Thirty-one articles were considered. Reported findings highlight that teledentistry has been used in pediatrics to educate and promote oral health and to provide remote diagnosis and monitoring through mobile health applications, smartphone cameras and apps, intraoral cameras, websites and search engines, and telephonic communications. Specifically, teledentistry has been beneficial in providing dental care in remote locations with difficult access to pediatric dentists, conducting remote diagnostic and screening programs, monitoring patients between appointments, promoting children’s oral health through dental education, and providing behavioral counseling prior to office visits. Future research should further investigate the long-term use, additional applications, and cost-effectiveness of teledentistry in children.
1. Introduction
The continuing evolution of demographic dynamics and the concomitant change in the health needs of the population, with a growing proportion of elderly people and chronic diseases require a redesign of the structure and organization of the network of health services [1,2].
Technological innovation and the COVID-19 pandemic have contributed to highlighting the need to reorganize the healthcare system, especially by supporting the shift in the focus of healthcare from the hospital to the community through innovative models of care that focus on the digitalization of health dynamics [3,4]. Health and social service delivery modalities enabled by telemedicine and teledentistry are important and help ensure equitable access to care in remote areas [5].
Teledentistry is an area of telemedicine dedicated explicitly to dentistry. It has emerged from combining dentistry and digital and telecommunication technology and involves exchanging clinical information and images over remote distances for dental consultation and treatment planning [6].
The United States Army introduced the teledentistry concept in 1994 as part of the Total Dental Access project [7]. Since then, several authors have conducted studies that have led to the worldwide dissemination of these methods.
The most used methods are classified as synchronous (real-time) and asynchronous (store-and-forward). The synchronous mode provides for real-time interaction between the user, the patient, the dental assistant, or the doctor through technological support that guarantees audiovisual communication. In asynchronous support, health information is collected at a specific time and later shared with the doctor. This practice allows for the exchange of information and materials collected with other specialists [8].
In addition, the advancement of modern technologies has led to the development of mobile health applications (m-Health app) supported by mobile devices, such as mobile phones, personal digital assistants (PDAs), or wireless devices for remote monitoring, with the ability to interact directly with the patient using telecommunication technologies, such as 4G and 5G or the Global Positioning System (GPS) [9]. The recent pandemic of COVID-19 and the resulting need for social distancing has encouraged the use of technology to provide dental care to patients. TD has allowed specialists to perform remote monitoring, minimizing face-to-face contact [10].
Several studies have shown that this method of remote monitoring can also be used in daily clinical practice to reduce the time and cost of regular checkups, to determine the level of oral hygiene and oral cavity health of patients, to provide rapid and accessible screening, and to provide a means for patients to be monitored in the clinic, which has various benefits for many patients, including people who live far from residential areas and have little opportunity to reach hospitals or private practices, patients with special needs, sick syndromic patients, and people living in socioeconomically disadvantaged conditions [11,12,13,14].
Therefore, this narrative review primarily aims to review the literature, analyzing the trends that today represent useful tools to provide for the oral health of pediatric patients, with particular reference to teledentistry and all the supports it uses to reach remote territories or patients who, for various reasons, cannot have access to dental care. Second, this paper has set the goal of evaluating and identifying the potential criticalities, future challenges, and perspectives that the introduction of this method may have in the daily activities of the dentist.
2. Materials and Methods
2.1. Search Strategy and Study Selection
A literature search was performed independently by two reviewers (G.S., M.P.) in three electronic databases—PubMed/MEDLINE, Google Scholar, and the COCHRANE library—and gray literature, combining the following keywords with Boolean operators: “teledentistry”, “telemedicine”, “remote consultation”, “remote screening”, “dentistry”, “teleconsultation”, “pediatric dentistry”, “pedodontics”, “telediagnosis”, and “pediatric dentistry”.
Citations obtained through the literature search were recorded, duplicates were eliminated using EndNote, and titles and abstracts were independently reviewed by three reviewers (M.P., G.S., A.B.).
Available full texts that met the inclusion and exclusion criteria listed below were also independently reviewed for potentially eligible studies. Any disagreements between reviewers were resolved by discussion and consensus.
The inclusion criteria were as follows:
- Studies published in a peer-reviewed journal
- Source: studies published in the English language from January 1996 to 1 February 2023
- Study design: controlled (randomized or non-randomized) assessment studies
- Study population: pediatric patients with no gender restrictions
- Study intervention: remote screening, tele-assistance, telemonitoring, tele-education, and telediagnosis by digital support
- Study outcomes: reported outcomes of teledentistry intervention(s).
The exclusion criteria were as follows:
- Source: studies published before 1996 or not published in a peer review journal
- Study intervention: indication for treatment not specified
- Study outcomes: not reported outcomes of teledentistry interventions.
No attempt was made to contact the authors for missing information or unavailability of the full text. In case of discrepancies, the evaluation of the majority was taken into account (two out of three reviewers).
References were exported and managed using Mendeley Reference Manager software.
2.2. Data Collection
Data on the source of the article, teledentistry application(s), study type, population, methods, outcomes, and results were extracted and qualitatively synthesized by two independent reviewers (G.S., M.P.) from each study included in the present narrative review.
3. Results
3.1. Study Selection
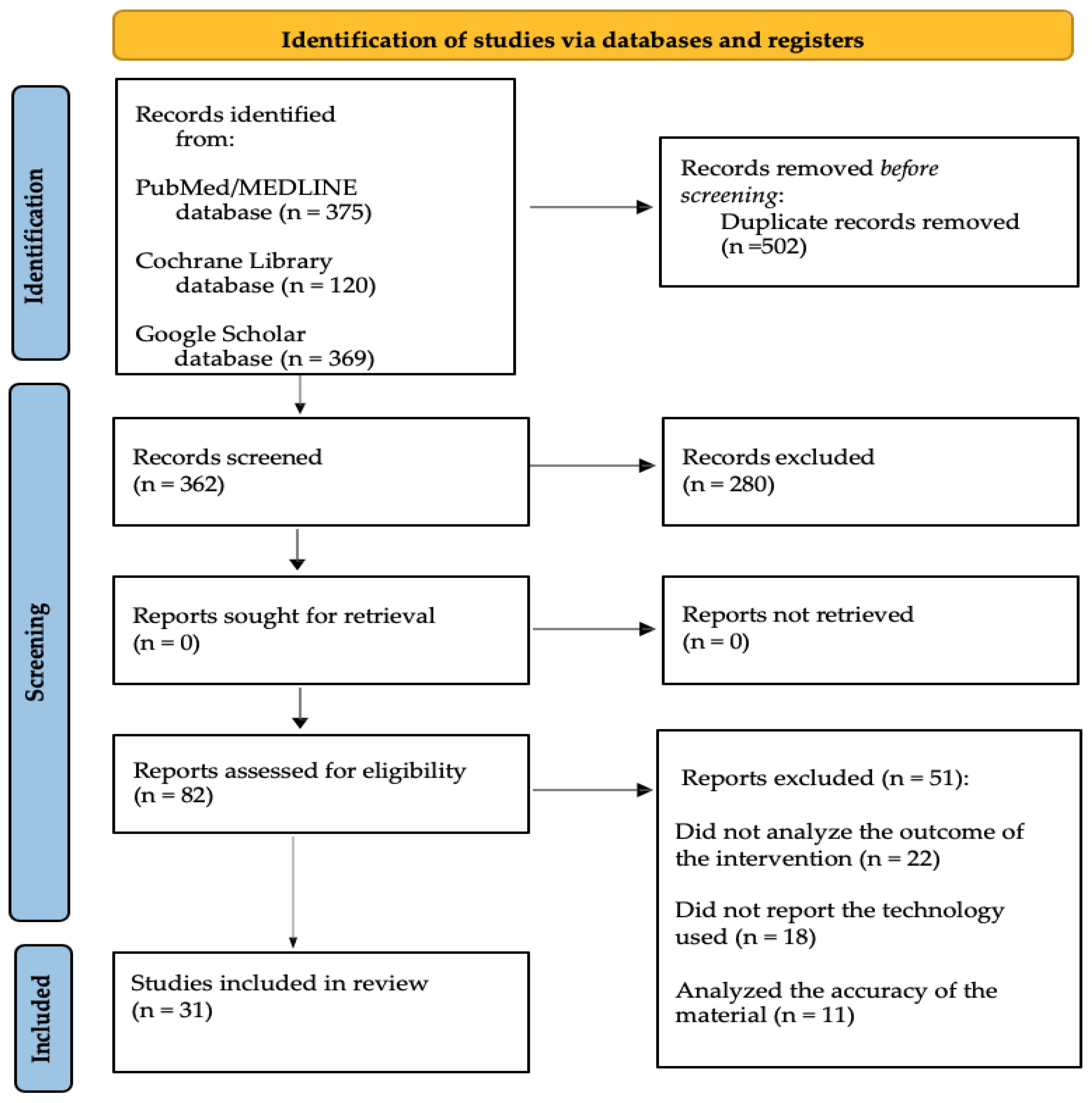
A total of 864 records were retrieved from PubMed/MEDLINE (375 articles), Google Scholar (369 articles), and the COCHRANE library (120 articles). Of these, 502 were excluded because duplicates or full texts were unavailable. Of the remaining 362 records, 280 were not relevant, and 82 full texts were screened; 51 entries were also excluded because the evaluation of the full texts did not reveal study outcomes or intervention methods. Finally, 31 articles were included in the qualitative analysis.
The flowchart for study selection is shown in Figure 1.
Figure 1.
Study selection flowchart.
3.2. Data Collection
Data extracted and collected from the included articles are detailed in Table 1 and organized according to the following parameters: authors, year, country, type of technology used, purpose, methods, and conclusion(s)/outcome(s).

Table 1.
Summary of studies included in this review, with data collected and organized according to the following parameters: authors, year, country, type of technology used, purpose, design, conclusion(s)/outcome(s).
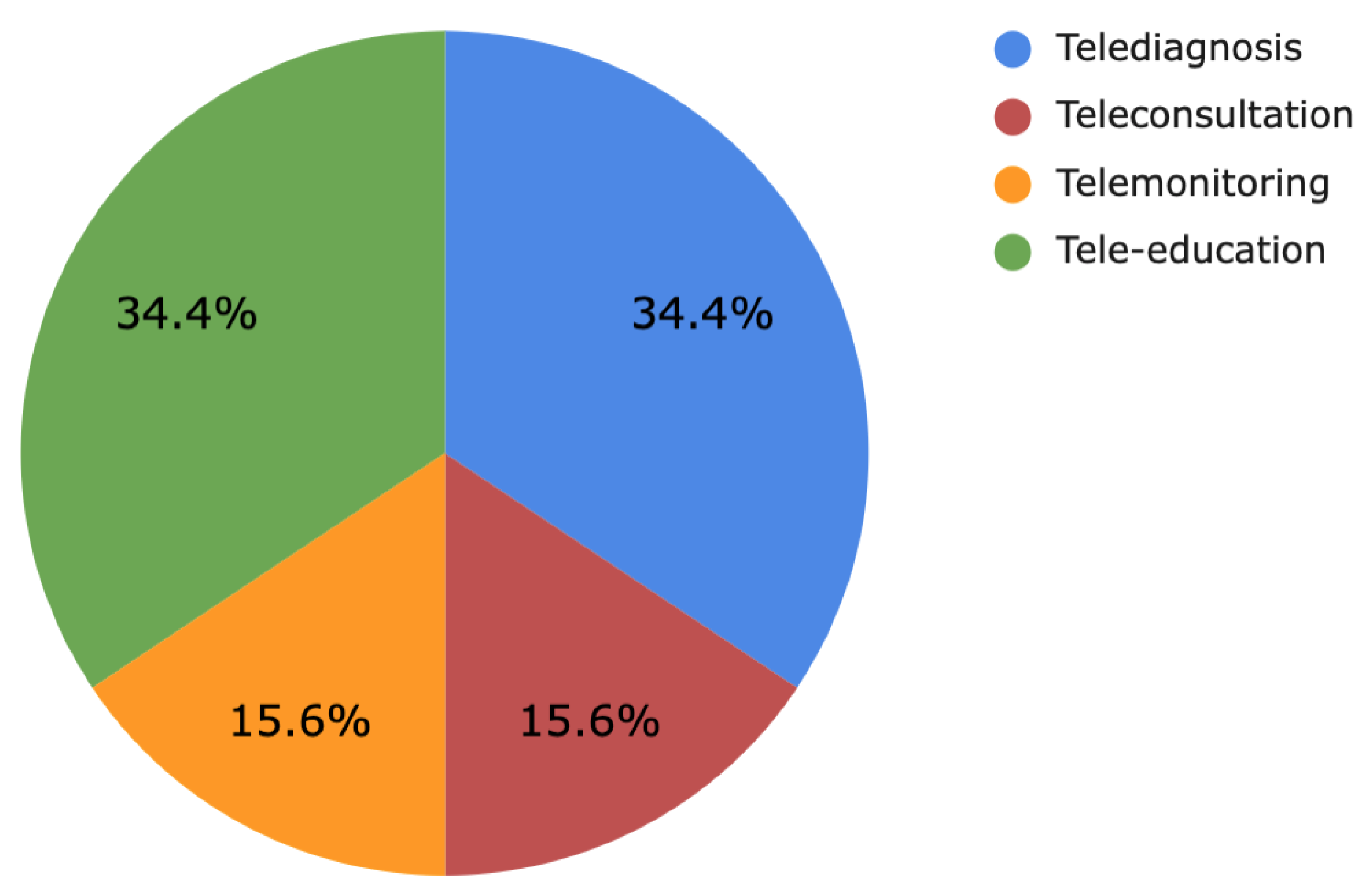
The analyzed studies were then subdivided according to the type of teledentistry application(s) assessed (Figure 2). Eleven studies assessed the use of telediagnosis in children, while n = 11 studies evaluated tele-education, n = 5 telemonitoring, and n = 5 teleconsultation, respectively.
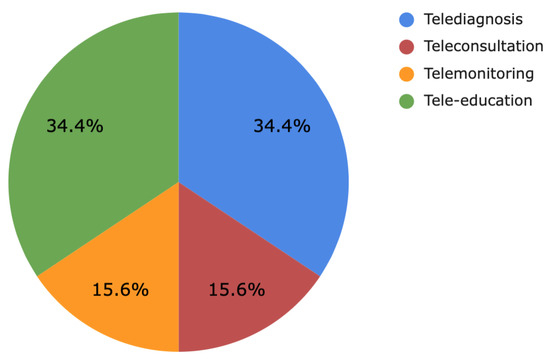
Figure 2.
Subdivision of the studies according to teledentistry applications.
The study by Shao et al. [23] was placed into two categories respectively: telemonitoring and tele-education, on the basis of their dual objectives.
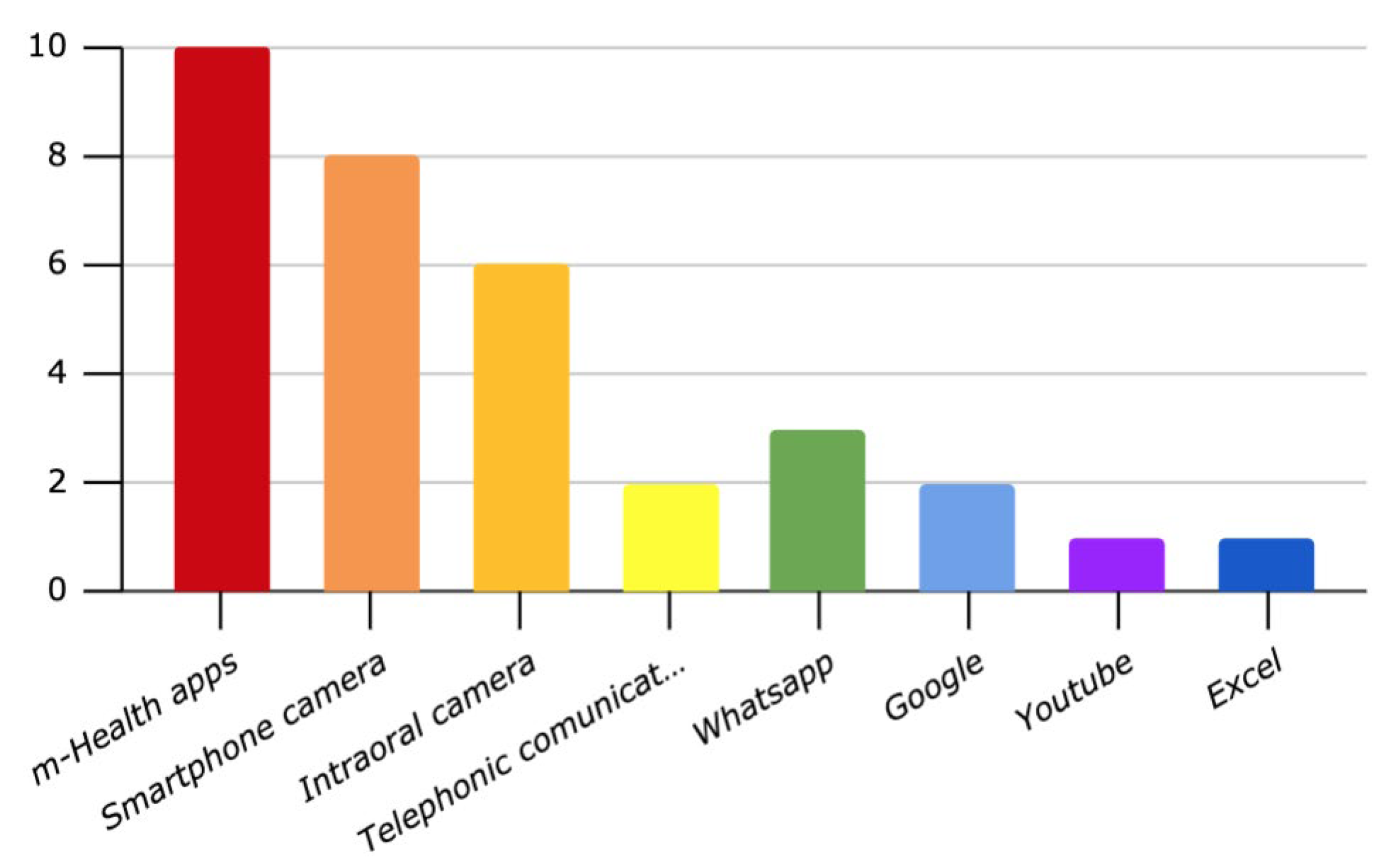
In addition, the studies were divided according to the digital support used (Figure 3) for teledentistry applications in pedodontic patients: 10 studies used mobile health applications; 8, smartphone cameras; 6, intraoral cameras; 3, WhatsApp; 2, the Google platform; 2, telephone communication; 1, YouTube; and 1, Excel. Mobile health applications were most commonly used for oral health education and promotion in pediatric patients. Smartphone cameras and intraoral cameras were the most commonly used tools for remote diagnosis.
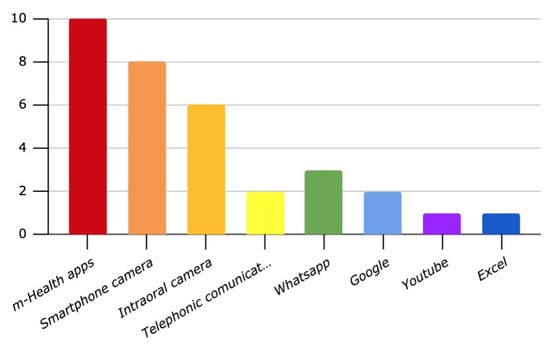
Figure 3.
Classification of studies according to the digital methodology applied.
4. Discussion
There is an evident propensity in the literature to support the usefulness and reliability of teledentistry applications, but it must be considered that many of the studies examined provide only preliminary results and only report the reliability and reproducibility of the short-term use of these services. In addition, several studies have included the participation of family members, health professionals, and dentists whose skills, experience, and knowledge are inevitably different and heterogeneous.
The literature review shows that teledentistry, especially in pediatric patient care, has several applications, such as telediagnosis, tele-education, telemonitoring, and teleconsultation [46]. Teledentistry has brought several advantages during the COVID-19 pandemic by limiting contacts and respecting the safety measures imposed by distancing. At the same time, it has prevented the exposure of dental staff and dentists thanks to the use of different tools, such as mobile phones, webcams, intraoral cameras, and dental applications [47].
Several studies have reported dentists’ and patients’ satisfaction in managing dental and/or orthodontic emergencies with the reduction of in-office appointments. These studies also reported dentists’ and patients’ satisfaction with the fact that dental monitoring did not affect treatment outcomes [48,49]. Therefore, our objective was to review the literature regarding the use of teledentistry, the most widespread applications, and the most commonly used technologies to address the oral health needs of pediatric patients.
The literature review revealed that teledentistry could be helpful in educating and promoting children’s oral health, diagnosing and monitoring pediatric dental patients in remote areas with limited access to dental care, and serving as a behavioral guide for pediatric patients [22].
The present study found that among the technologies used, m-Health apps were widely used for behavioral education, oral health promotion, and reducing anxiety before an in-person appointment among pediatric patients [31,32]. The smartphone and intraoral cameras were mainly used for diagnosing and monitoring young patients and for studies comparing the results of remote diagnosis with traditional clinical examination.
Oral health education and promotion programs using mobile technologies, the internet, and mobile health applications have attracted public attention and reached a large population. Several authors believe that children are proficient in using digital technologies and use them more intensively than adults [27,31].
Therefore, the use of internet- and mobile-based applications increases patient awareness and knowledge to promote oral hygiene, provides an effective communication tool for parents and the community in remote areas, and could address the shortage of qualified public health dental professionals specializing in the management of pediatric patients [36]. m-Health apps used for patient education should be based on accepted behavior change techniques and provide instructions on how to perform a task, include prompts, and reward the user for achieving the goal [37,38]. According to the analyzed data, the most frequently used features in the m-Health app developed for children’s oral health should include educational multimedia and game-based stories. Animation-based educational programs and picture books are mainly used to teach brushing and familiarize with the dental environment and procedures, as children are highly influenced by animations and pictures. In contrast, adult self-care applications are mostly focused on reminders, timers, sensors, online counseling, and SMS.
In the study proposed by Soler et al., adolescents reported that the game was entertaining and educational; it helped them learn new aspects of oral health and had the potential to change their oral health habits [16].
Patil et al. concluded that this method can reduce anxiety about dental treatment and improve patients’ behavior during subsequent face-to-face visits [31]. Following these findings, Patel et al. reported that the use of social media for social, emotional, or experiential support in chronic disease, particularly through Facebook and blogs, appeared to improve patient care [2].
Another application of teledentistry studied by several authors is the ability to diagnose and monitor using digital devices, such as smartphones, digital cameras, intraoral cameras, webcams, and computer monitors [21,40]. Remote diagnosis involves the use of images of the patient to diagnose and monitor any oral pathology. Through this approach, it is possible to prioritize patients in need of urgent treatment through remote diagnosis, while ensuring access to pediatric dentistry specialists, who in many cases are difficult to find in the region, thus eliminating the need for the patient to travel to a specialized dental consultation, especially for individuals who have difficulty accessing medical treatment due to geographic or socioeconomic reasons [33,45,50].
From the physician’s perspective, the advantage is that he or she can share the captured images with other specialists, which allows the general dentist and/or the specialist dentist to develop an appropriate multidisciplinary treatment plan. This telehealth network approach allows doctors with different expertise to be digitally connected to discuss diagnoses and multidisciplinary treatment plans that lead to the resolution of the most complex clinical cases.
Kohara et al. reported that this method was reliable in diagnosing large carious lesions but less effective in diagnosing initial carious lesions [33]. de Almeida Geraldino et al. also reported that remote diagnosis was comparable to conventional in-person examination [30].
Kopycka-Kedzierawski et al. showed that remote diagnosis was as effective as conventional on-site examination in early caries detection in young children [15]. Kopycka-Kedzierawski et al. performed a study testing the efficacy of teleodontology for caries screening in preschool children at high risk for early childhood caries, and the authors concluded that teledentistry was shown to be effective in screening for carious lesions [22]. According to these results, Amavel et al. reported that remote diagnosis of oral problems in pediatric patients through photographs was a valuable resource [17]. Kopycka-Kedzierawski et al. in another study, argued that an intraoral camera was a viable and potentially cost-effective alternative to visual oral examination for caries screening in preschool children attending childcare centers [19].
Among the most analyzed aspects is orthodontic telemonitoring. The Italian Society of Orthodontics (SIDO) during the COVID-19 pandemic published the recommended guidelines for the management of orthodontic patients. In these guidelines, a first approach was recommended through virtual assistance by photographic documentation or a video call with digital support, in order to be able to distinguish through a triage the cases in which a face-to-face visit was necessary from those situations that could be managed remotely according with the restrictions of the pandemic [50]. For these reasons, several authors suggested that orthodontic emergencies should be addressed with a gradual approach [48]. It should be emphasized that orthodontic emergencies are unpredictable problems caused by mostly orthodontic appliances causing pain or discomfort, requiring urgent dental care [49]. Compared with other dental problems, orthodontic problems are less severe and often do not require in-office treatment. Many of these problems can be easily solved at home, which reduces stress for patients’ families and saves time for both patients and dentists. Despite these benefits and the positive impact of orthodontic monitoring during the pandemic, which has produced encouraging results for both dentists and patients, some procedures require direct access to the mouth and hands-on intervention by the clinician that cannot be performed via telemedicine [49]. These procedures include initial orthodontic examination, data collection, bonding and detaching of orthodontic brackets, bands, and clear aligner attachments, interproximal reduction (stripping), enameloplasty/occlusal adjustment, and cutting, bending, and changing wires [51].
In addition, several authors have reported some limitations related to remote support, including the insufficient quality of the photos, the problems related to the insufficient internet support, and/or the learning curve required for the correct functioning of the device or applications, which affect both the dental staff and the patient and his/her family members [52].
What Does the Future Hold?
Continuative applications of teledentistry in pediatric dental practice have begun to emerge. These include teleconsultation, telediagnosis, tele-education, and telehealth networks, which could be systematically integrated for the maintenance of pediatric oral health. However, some aspects must be addressed to ensure these methods become part of dentists’ daily routines. Indeed, aspects related to the privacy and protection of sensitive data of patients and to data protection obligations of a health facility working using telemedicine and teledentistry are diverse and correspond to the sensitivity of the particular data to be processed [53]. For these reasons, staff should request only the data necessary to provide the health service and implement technical and organizational measures to prevent alteration or loss of data and ensure their security throughout the service process. Time limits for data retention or deletion should be established, along with a simple process that identifies ways to address patient needs promptly and clearly. In addition, the cost of compensating healthcare professionals for providing these services should be addressed. Certainly, strategies must be adopted to equip structures with specialized equipment, hardware, and adequate internet coverage to support these procedures to limit the socioeconomic and territorial exclusion dynamics that exist today in many areas; it should be considered that especially in rural or underdeveloped areas, an internet connection is also an obstacle. Communication that is not stable and clear between the patient and the dentist can lead to wasted time, misunderstanding, or misdiagnosis. It may be appropriate to make centers with software, trained staff, and good internet coverage available to patients in rural areas so that they can conveniently connect [54].
The next generation of dentists will have new tools including information networks and simulations, such as learning platforms that deliver virtual content, which will enable the remote transfer of skills. It will be very important to acquire the ability to think and work with these technologies at all levels of education. This will lead to the growth and projection of specialists toward digital health, which will inevitably lead to an adaptation of curricula and training of future dentists [55]. For this reason, it might be desirable to include specific knowledge regarding the possible uses of teledentistry and the skills required for its informed use in the university curriculum of dental students [56].
As a prerequisite for the transition from an experimental method to a structured method in relation to the widespread use of these services, harmonization of telemedicine, as well as teledentistry, guidelines and application models are required.
Despite the initial positive impact, further research is needed to assess effectiveness, cost-benefit, and long-term outcomes.
However, tele-assistance should be seen as an opportunity for dentists and new generations to project the profession into the future. Today, more and more patients are searching online for information about their health, leading to uncertainty, confusion, and scare tactics. Teledentistry services could strengthen the trust relationship between the patient and the dentist. In many cases, the studies examined provide only preliminary results and consider only teledentistry’s feasibility and short-term use.
Due to the limited conclusive evidence, heterogeneity of the methods used by the authors, the interventions, and the outcomes evaluated in the studies reviewed, the generalizability of the results is limited. Well-designed studies evaluating teledentistry and its effectiveness, cost-effectiveness, and long-term use are needed.
5. Conclusions
The present narrative review found a growing body of evidence supporting the effectiveness of teledentistry, particularly in pediatric dentistry.
The positive results suggest that this technological advance in dentistry can significantly help reduce the gap between the supply and demand of pediatric dentistry specialists in locations where dental services are limited. In addition, teledentistry can help ensure long-term oral healthcare for the pediatric population and overcome disparities in access to specialty care. However, it is necessary to consider that these services need to have an adequate internet connection, clear policies and regulations, trained staff, and modern technology, the costs of which could be prohibitive, especially if not supported by governments with funds and subsidies.
Future studies are needed to evaluate the reliability and effectiveness of teledentistry applications and the optimal digital methodology that should be used beyond cost-effectiveness and long-term use.
Author Contributions
Conceptualization, M.P. and R.S.; methodology, A.B.; software, G.S.; validation, M.P., D.M. and R.S.; formal analysis, D.M.; investigation, M.P.; resources, D.M.; data curation, A.B.; writing—original draft preparation, A.B.; writing—review and editing, M.P.; visualization, G.S.; supervision, A.A.; project administration, G.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Giraudeau, N. Teledentistry and COVID-19: Be Mindful of Bogus “Good” Ideas! Inquiry 2021, 58, 469580211015050. [Google Scholar] [CrossRef] [PubMed]
- Patel, R.; Chang, T.; Greysen, S.R.; Chopra, V. Social media use in chronic disease: A systematic review and novel taxonomy. Am. J. Med. 2015, 128, 1335.e50. [Google Scholar] [CrossRef]
- Spirito, F.; Amato, A.; Scelza, G.; Pisano, M.; Caponio, V.C.A.; Martina, S. Education during the COVID-19 pandemic: The perception of Italian dental and medical students. Minerva Dent. Oral Sci. 2022, 71, 277–286. [Google Scholar] [CrossRef]
- Chen, J.W.; Hobdell, M.H.; Dunn, K.; Johnson, K.A.; Zang, J. Teledentistry and its use in dental education. J. Am. Dent. Assoc. 2003, 134, 342–346. [Google Scholar] [CrossRef] [PubMed]
- Sanchez Dils, E.; Lefebvre, C.; Abeyta, K. Teledentistry in the United States: A new horizon of dental care. Int. J. Dent. Hyg. 2004, 2, 161–164. [Google Scholar] [CrossRef]
- Sood, S.; Mbarika, V.; Jugoo, S.; Dookhy, R.; Doarn, C.R.; Prakash, N.; Merrell, R.C. What is telemedicine? A collection of 104 peer-reviewed perspectives and theoretical underpinnings. Telemed. J. e-Health 2007, 13, 573–590. [Google Scholar] [CrossRef]
- Vandre, R.H.; VKudryk, L.; Fay, C.R.; Edwards, J.C.; Jones, T.K. US Army teledentistry. In Proceedings of the National Forum: Military Telemedicine On-Line Today Research, Practice, and Opportunities, McLean, VA, USA, 27–29 March 1995; pp. 53–56. [Google Scholar] [CrossRef]
- Marya, C.M.; Swati, S.; Nagpal, R.; Kataria, S.; Taneja, P. Dental informatics: Integrating technology into dentistry. Austin Dent. Sci. 2020, 5, e1025. [Google Scholar]
- Campos, L.F.; Cavalcante, J.P.; Machado, D.P.; Marçal, E.; Silva, P.G.; Rolim, J.P. Development and evaluation of a mobile oral health application for preschoolers. Telemed. J. e-Health 2019, 25, 492.e8. [Google Scholar] [CrossRef] [PubMed]
- Meng, L.; Hua, F.; Bian, Z. Coronavirus disease 2019 (COVID-19): Emerging and future challenges for dental and oral medicine. J. Dent. Res. 2020, 99, 481–487. [Google Scholar] [CrossRef]
- Howell, S.E.I.; Fukuoka, B. Teledentistry for Patient-centered Screening and Assessment. Dent. Clin. N. Am. 2022, 66, 195–208. [Google Scholar] [CrossRef]
- Di Spirito, F. Integrating P4 Medicine in Teledentistry and M-Health in Oral, Dental, and Periodontal Care. J. Pers. Med. 2023, 13, 111. [Google Scholar] [CrossRef] [PubMed]
- Pisano, M.; Sangiovanni, G.; D’Ambrosio, F.; Romano, A.; Di Spirito, F. Oral Care in Patient with Long Arm Deletion Syndrome of Chromosome 18: A Narrative Review and Case Presentation. Am. J. Case Rep. 2022, 23, e936142. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Kim, J.H.; Rogowski, L.; Al Shami, S.; Howell, S.E.I. Implementation of teledentistry for orthodontic practices. J. World Fed. Orthod. 2021, 10, 9–13. [Google Scholar] [CrossRef] [PubMed]
- Kopycka-Kedzierawski, D.T.; Bell, C.H.; Billings, R.J. Prevalence of dental caries in Early Head Start children as diagnosed using teledentistry. Pediatr. Dent. 2008, 30, 329–333. [Google Scholar] [PubMed]
- Soler, C.; Zacarías, A.; Lucero, A. Molarcropolis: A mobile persuasive game to raise oral health and dental hygiene awareness. In Proceedings of the International Conference on Advances in Computer Entertainment Technology (ACE ‘09). Association for Computing Machinery, New York, NY, USA, 29–31 October 2009; pp. 388–391. [Google Scholar] [CrossRef]
- Amável, R.; Cruz-Correia, R.; Frias-Bulhosa, J. Remote diagnosis of children dental problems based on non-invasive photographs—A valid proceeding? Stud. Health Technol. Inform. 2009, 150, 458–462. [Google Scholar]
- Lienert, N.; Zitzmann, N.U.; Filippi, A.; Weiger, R.; Krastl, G. Teledental consultations related to trauma in a Swiss telemedical center: A retrospective survey. Dent. Traumatol. 2010, 26, 223–227. [Google Scholar] [CrossRef]
- Kopycka-Kedzierawski, D.T.; Billings, R.J. Prevalence of dental caries and dental care utilisation in preschool urban children enrolled in a comparative-effectiveness study. Eur. Arch. Paediatr. Dent. 2011, 12, 133–138. [Google Scholar] [CrossRef]
- Levine, J.; Wolf, R.L.; Chinn, C.; Edelstein, B.L. MySmileBuddy: An iPad-based interactive program to assess dietary risk for early childhood caries. J. Acad. Nutr. Diet. 2012, 112, 1539–1542. [Google Scholar] [CrossRef]
- Torres-Pereira, C.C.; Morosini Ide, A.; Possebon, R.S.; Giovanini, A.F.; Bortoluzzi, M.C.; Leão, J.C.; Piazzetta, C.M. Teledentistry: Distant diagnosis of oral disease using e-mails. Telemed. J. e-Health 2013, 19, 117–121. [Google Scholar] [CrossRef]
- Kopycka-Kedzierawski, D.T.; Billings, R.J. Comparative effectiveness study to assess two examination modalities used to detect dental caries in preschool urban children. Telemed. J. e-Health 2013, 19, 834–840. [Google Scholar] [CrossRef]
- Shao, K.; Huang, J.; Song, H.; Li, R.; Wu, J. DAYA. A System for Monitoring and Enhancing Children’s Oral Hygiene. In CHI’14 Extended Abstracts on Human Factors in Computing Systems; ACM Digital Library: New York, NY, USA, 2014. [Google Scholar]
- Mariño, R.; Ghanim, A. Teledentistry: A systematic review of the literature. J. Telemed. Telecare 2013, 19, 179–183. [Google Scholar] [CrossRef] [PubMed]
- Underwood, B.; Birdsall, J.; Kay, E. The use of a mobile app to motivate evidence-based oral hygiene behaviour. Br. Dent. J. 2015, 219, E2. [Google Scholar] [CrossRef]
- Zotti, F.; Pietrobelli, A.; Malchiodi, L.; Nocini, P.F.; Albanese, M. Apps for oral hygiene in children 4 to 7 years: Fun and effectiveness. J. Clin. Exp. Dent. 2019, 11, e795–e801. [Google Scholar] [CrossRef] [PubMed]
- McLaren, S.W.; Kopycka-Kedzierawski, D.T. Compliance with dental treatment recommendations by rural pediatric patients after a live-video teledentistry consultation: A preliminary report. J. Telemed. Telecare 2016, 22, 198–202. [Google Scholar] [CrossRef] [PubMed]
- Purohit, B.M.; Singh, A.; Dwivedi, A. Utilization of teledentistry as a tool to screen for dental caries among 12-year-old school children in a rural region of India. J. Public Health Dent. 2017, 77, 174–180. [Google Scholar] [CrossRef] [PubMed]
- Estai, M.; Kanagasingam, Y.; Huang, B.; Shiikha, J.; Kruger, E.; Bunt, S.; Tennant, M. Comparison of a Smartphone-Based Photographic Method with Face-to-Face Caries Assessment: A Mobile Teledentistry Model. Telemed. J. e-Health 2017, 23, 435–440. [Google Scholar] [CrossRef]
- De Almeida Geraldino, R.; Rezende, L.V.M.L.; da-Silva, C.Q.; Almeida, J.C.F. Remote diagnosis of traumatic dental injuries using digital photographs captured via mobile phone. Dent. Traumatol. 2017, 33, 350–357. [Google Scholar] [CrossRef]
- Patil, V.H.; Vaid, K.; Gokhale, N.S.; Shah, P.; Mundada, M.; Hugar, S.M. Evaluation of effectiveness of dental apps in management of child behaviour: A pilot study. Int. J. Pedod. Rehabil. 2017, 2, 14–18. [Google Scholar]
- Meshki, R.; Basir, L.; Alidadi, F.; Behbudi, A.; Rakhshan, V. Effects of Pretreatment Exposure to Dental Practice Using a Smartphone Dental Simulation Game on Children’s Pain and Anxiety: A Preliminary Double-Blind Randomized Clinical Trial. J. Dent. 2018, 15, 250–258. [Google Scholar]
- Kohara, E.K.; Abdala, C.G.; Novaes, T.F.; Braga, M.M.; Haddad, A.E.; Mendes, F.M. Is it feasible to use smartphone images to perform telediagnosis of different stages of occlusal caries lesions? PLoS ONE 2018, 13, e0202116. [Google Scholar] [CrossRef]
- Kale, S.; Kakodkar, P.; Shetiya, S.H. Assessment of mother’s ability in caries diagnosis, utilizing the smartphone photographic method. J. Indian Soc. Pedod. Prev. Dent. 2019, 37, 360–364. [Google Scholar] [CrossRef] [PubMed]
- Elicherla, S.R.; Bandi, S.; Nuvvula, S.; Challa, R.S.; Saikiran, K.V.; Priyanka, V.J. Comparative evaluation of the effectiveness of a mobile app (Little Lovely Dentist) and the tell-show-do technique in the management of dental anxiety and fear: A randomized controlled trial. J. Dent. Anesth. Pain Med. 2019, 19, 369–378. [Google Scholar] [CrossRef] [PubMed]
- Radhakrishna, S.; Srinivasan, I.; Setty, J.V.; DR, M.K.; Melwani, A.; Hegde, K.M. Comparison of three behavior modification techniques for management of anxious children aged 4–8 years. J. Dent. Anesth. Pain Med. 2019, 19, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Lotto, M.; Strieder, A.P.; Ayala Aguirre, P.E.; Oliveira, T.M.; Andrade Moreira Machado, M.A.; Rios, D.; Cruvinel, T. Parental-oriented educational mobile messages to aid in the control of early childhood caries in low socioeconomic children: A randomized controlled trial. J. Dent. 2020, 101, 103456. [Google Scholar] [CrossRef] [PubMed]
- Asokan, S.; Geetha Priya, P.R.; Natchiyar, S.N.; Elamathe, M. Effectiveness of distraction techniques in the management of anxious children—A randomized controlled pilot trial. J. Indian Soc. Pedod. Prev. Dent. 2020, 38, 407–412. [Google Scholar] [CrossRef] [PubMed]
- Simsek, H.; Buyuk, S.K.; Cetinkaya, E. YouTube™ as a source of information on oral habits. J. Indian Soc. Pedod. Prev. Dent. 2020, 38, 115–118. [Google Scholar] [CrossRef]
- AlShaya, M.S.; Assery, M.K.; Pani, S.C. Reliability of mobile phone teledentistry in dental diagnosis and treatment planning in mixed dentition. J. Telemed. Telecare 2020, 26, 45–52. [Google Scholar] [CrossRef]
- Wallace, C.K.; Schofield, C.E.; Burbridge, L.A.L.; O’Donnell, K.L. Role of teledentistry in pediatric dentistry. Br. Dent. J. 2021, 1–6. [Google Scholar] [CrossRef]
- Sanghvi, R.; Barrow, S.; Hullah, E.; De Souza, M.; Cook, R.; Siddik, D. Pediatric dental-oral medicine clinic: Management during COVID-19. J. Oral Med. Oral Surg. 2021, 27, 18. [Google Scholar] [CrossRef]
- Damoiselet, C.; Veynachter, T.; Jager, S.; Baudet, A.; Hernandez, M.; Clément, C. Teledentistry and management protocol in a pediatric dental department during the first COVID-19 lockdown. Arch. Pediatr. 2023, 30, 20–24. [Google Scholar] [CrossRef]
- Varkey, I.M.; Ghule, K.D.; Mathew, R.; Desai, J.; Gomes, S.; Mudaliar, A.; Bhori, M.; Tungare, K.; Gharat, A. Assessment of attitudes and practices regarding oral healthcare during the COVID-19 pandemic among the parents of children aged 4–7 years. Dent. Med. Probl. 2022, 59, 365–372. [Google Scholar] [CrossRef] [PubMed]
- AlShaya, M.; Farsi, D.; Farsi, N.; Farsi, N. The accuracy of teledentistry in caries detection in children—A diagnostic study. Digit. Health 2022, 8, 20552076221109075. [Google Scholar] [CrossRef] [PubMed]
- Di Spirito, F.; Amato, A.; Di Palo, M.P.; Ferraro, G.A.; Baroni, A.; Serpico, R.; Contaldo, M. COVID-19 Related Information on Pediatric Dental Care including the Use of Teledentistry: A Narrative Review. Children 2022, 9, 1942. [Google Scholar] [CrossRef] [PubMed]
- Menhadji, P.; Patel, R.; Asimakopoulou, K.; Quinn, B.; Khoshkhounejad, G.; Pasha, P.; Garcia Sanchez, R.; Ide, M.; Kalsi, P.; Nibali, L. Patients’ and dentists’ perceptions of tele-dentistry at the time of COVID-19. A questionnaire-based study. J. Dent. 2021, 113, 103782. [Google Scholar] [CrossRef]
- Dalessandri, D.; Sangalli, L.; Tonni, I.; Laffranchi, L.; Bonetti, S.; Visconti, L.; Signoroni, A.; Paganelli, C. Attitude towards Telemonitoring in Orthodontists and Orthodontic Patients. Dent. J. 2021, 9, 47. [Google Scholar] [CrossRef]
- Maspero, C.; Abate, A.; Cavagnetto, D.; El Morsi, M.; Fama, A.; Farronato, M. Available Technologies, Applications and Benefits of Teleorthodontics. A Literature Review and Possible Applications during the COVID-19 Pandemic. J. Clin. Med. 2020, 9, 1891. [Google Scholar] [CrossRef]
- Di Spirito, F.; Caggiano, M.; di Palo, M.P.; Contaldo, M.; D’Ambrosio, F.; Martina, S.; Amato, A. Oral Lesions in Pediatric Subjects: SARS-CoV-2 Infection and COVID-19 Vaccination. Appl. Sci. 2022, 12, 8995. [Google Scholar] [CrossRef]
- Saccomanno, S.; Quinzi, V.; Sarhan, S.; Laganà, D.; Marzo, G. Perspectives of teleorthodontics in the COVID-19 emergency and as a future tool in daily practice. Eur. J. Paediatr. Dent. 2020, 21, 157.e62. [Google Scholar]
- Giraudeau, N.; Bauer, M.; Tramini, P.; Inquimbert, C.; Toupenay, S. A national teledentistry study on the knowledge, attitudes, training and practices of private dentists. Digit. Health 2022, 8, 20552076221085069. [Google Scholar] [CrossRef]
- Fornaini, C.; Rocca, J.P. Relevance of Teledentistry: Brief Report and Future Perspectives. Front. Dent. 2022, 19, 25. [Google Scholar] [CrossRef]
- Patel, E.; Mascarenhas, A.; Ahmed, S.; Stirt, D.; Brady, I.; Perera, R.; Noël, J. Evaluating the ability of students to learn and utilize a novel telepresence platform, Proximie. J. Robot. Surg. 2022, 16, 973–979. [Google Scholar] [CrossRef] [PubMed]
- Petcu, R.; Kimble, C.; Ologeanu-Taddei, R.; Bourdon, I.; Giraudeau, N. Assessing patient’s perception of oral teleconsultation. Int. J. Technol. Assess Health Care 2017, 33, 147–154. [Google Scholar] [CrossRef] [PubMed]
- El Tantawi, M.; Lam, W.Y.; Giraudeau, N.; Virtanen, J.I.; Matanhire, C.; Chifamba, T.; Sabbah, W.; Gomaa, N.; Al-Maweri, S.A.; Uribe, S.E.; et al. Teledentistry from research to practice: A tale of nineteen countries. Front. Oral Health 2023, 4, 1188557. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).