Abstract
In the last years, both medicine and dentistry have come across a revolution represented by the introduction of more and more digital technologies for both diagnostic and therapeutic purposes. Additive manufacturing is a relatively new technology consisting of a computer-aided design and computer-aided manufacturing (CAD/CAM) workflow, which allows the substitution of many materials with digital data. This process requires three fundamental steps represented by the digitalization of an item through a scanner, the editing of the data acquired using a software, and the manufacturing technology to transform the digital data into a final product, respectively. This narrative review aims to discuss the recent introduction in dentistry of the abovementioned digital workflow. The main advantages and disadvantages of the process will be discussed, along with a brief description of the possible applications on orthodontics.
1. Introduction
In recent years, the introduction of digital technologies in dentistry has represented a significant breakthrough. In particular, intra-oral scanning is becoming a more and more developed technique with a progressive substitution of the traditional dental impressions [1]. These systems showed good precision [2] and excellent patient feedback [3]. Despite digital dental models allowing the diagnosis, treatment planning and simulation of the results at the end of the therapy, they cannot directly reproduce physical models and appliances. To do so, this 3D workflow needs a computer-aided design and manufacturing (CAD-CAM) process, which consists of the elaboration of the digital data, previously acquired with the intra-oral scanner, and the production of a precise 3D physical model [4]. The rise of additive manufacturing, also known as 3D printing, dates to the 1980s, despite its introduction in dentistry being much more recent, because of the initial high cost, as well as its low speed and accuracy. In the meanwhile, an increasing number of printable biomaterials have been developed, thus significantly contributing to almost every field of dentistry [5,6]. To date, several studies have been conducted to evaluate the mechanical properties of 3D-printed materials, such as microhardness, but no extensive literature specifically exists for dental materials [7,8].
In orthodontics, as in other fields of dentistry, five different printing technologies are now available, that is, fused deposition modeling/fused filament fabrication (FDM/FFF), stereolithography (SLA), digital light processing (DLP), selective laser sintering/melting (SLS/SLM) and electron beam melting (EBM), Binder Jetting (BJ) and Material Jetting (MJ) [1,9,10,11,12,13,14,15].
As previously said, 3D printing almost covers every specialty of dentistry, including orthodontics [16,17,18,19,20,21]. A bibliometric analysis using Scopus and PubMed Databases has been conducted using the following MeSH terms: TITLE-ABS-KEY (printing AND three-dimensional AND dentistry) and (printing AND three-dimensional AND orthodontics). The bibliometric research was conducted in January 2021, so data for this year are ongoing. In the last two decades, an increase in the publication of indexed literature about dental 3D printing applications has been noted for both keywords (Figure 1).
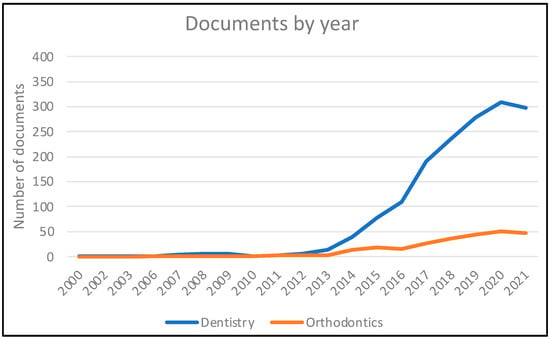
Figure 1.
Bibliometric analysis with Scopus and PubMed Database considering years from 2003 to 2021 (data for the latter year are ongoing).
As regards orthodontics, articles account for 90.87% of the total documents, while reviews constitute 9.13% of the total. As there is a scarcity of clinical trials of 3D-printed appliances, many narrative reviews have been published until now. Articles, instead, are mainly case reports and in vitro/laboratory studies. Scopus and PubMed search engines have been used to perform the present narrative review. All relevant articles are supposed to have been included.
Focusing on the latter, the applicability of the digital workflow regards both dental casts and direct appliances. The present article aims to perform a narrative description of the digital workflow, especially focusing on orthodontics and the applications of the process in this field.
2. Three Dimensional Printing Technologies
The general term “3D Printing” or “Additive Manufacturing” encompasses different technologies, which differ in the way each layer is deposited and processed and in the type of material used. The first classification of 3D printing technologies was proposed in 2009 by the “ASTM Committee F42 on Additive Manufacturing Technologies” established the same year. Beside the classification, the Committee also proposed the term Additive Manufacturing instead of Rapid Prototyping, at that time considered a synonym of 3D printing, thus suggesting a more inclusive application of 3D printing technologies [22]. As it concerns orthodontics, according to the literature the most common technologies are stereolithography (SLA), digital light processing (DLP), fused deposition modeling (FDM)/fused filament fabrication (FFF), selective laser sintering (SLS)/melting (SLM) and electron beam melting (EBM), Binder Jetting (BJ) and Material Jetting (MJ). The main characteristics of each technology are described below.
2.1. Stereolithography (SLA) and Digital Light Processing (DLP)
Stereolithography (SLA) is based on the use of a photocurable liquid resin as a printing material (photopolymer) [23]. Its working process consists of a layer-by-layer model printing starting from liquid resins exposed either to the photopolymerizing action of an ultraviolet laser source (SLA) or a visible light projector (DLP). The former modality requires a progressive movement of the laser across the layer, whereas the former guarantees the curing of an entire resin layer thus resulting in a faster process. In this way, the cross-linking of the polymer and its hardening are promoted by the laser beam, that belongs to the ultraviolet wavelength. A necessary step following SLA/DLP printing is represented by the post-processing of the printed model to avoid its shrinkage and distortions. Accordingly, an alcohol solution removes all the uncured resin, subsequently heat and ultraviolet light are required to harden the model, generally put inside an illumination chamber [6,14,17].
Digital light processing (DLP) is a 3D printing technology that is quite similar to SLA, since a photopolymer is used as a printing material [23]. In particular, the latter is cured with a digital micromirror device (DMD). Different from SLA, the curing light is projected on the entire layer, while the former technique is based on a spot laser beam. This difference results in a faster procedure for DLP [24].
2.2. Fused Deposition Modeling/Fused Filament Fabrication (FDM/FFF)
Fused deposition modeling (equivalent to the not trademarked term “fused filament fabrication”—FFF) consists of the formation of solid objects using a thermoplastic material [23]. This one is heated until reaching a melting temperature and then released through extrusion heads by the printer in a specific pattern, thus forming a single layer of an object [17]. Therefore, the material is released layer-by-layer and these strata are fused together when the entire structure solidifies. Beside supports removal, no further procedures are usually required on the material itself to improve mechanical properties [18].
2.3. Selective Laser Sintering (SLS)/Melting (SLM) and Electron Beam Melting (EBM)
Selective laser sintering/melting (SLS/SLM) aims to print 3D objects using powder materials (e.g., polyamides, polycaprolactone, hydroxyapatite, stainless steel, titanium, and Co/Cr) [23]. This powder is heated above the glass transition or melting temperature using a high energy CO2 beam, thus sintering/melting the particles together in a specific pattern. The curing of the powder proceeds according to a layer-by-layer step, until the entire material is printed. The post-printing processing consists of the removal of the excess powder particles for plastic materials [6], while it is far more challenging for metals, for which specific post-processing is required to remove support structures (sawing, CNC machining etc.).
Electron beam melting (EBM) technology is based on the use of metal powder (stainless steel, titanium, etc.) as a printing material as well. In this case, the powder is submitted to sintering by a computer-controlled electron beam in a vacuum (differently from SLS which uses a laser beam) [17].
2.4. Binder Jetting (BJ)
Binder Jetting (BJ) is a technique aimed at realizing objects by adding a pattern of binding liquid on a powder substrate [23]. The structure results from the reaction between the liquid and the powder, then the phase transformation is promoted by ultraviolet curing, chemical or thermal reaction, or dehydration [17,25].
2.5. Material Jetting (MJ)
An evolution of SLA technology is represented by Material Jetting (MJ), which employs a liquid photopolymer as a printing material. This latter is extruded by a series of small nozzles on a building platform and then cured with UV light. Supportive structures are realized with layers of photopolymeric material as well. Then, supporting materials can be easily removed at the end of the printing process. Different from SLA, objects printed with Material Jetting printers are cured at their maximum rate, thus not requiring an additional post-curing procedure [23].
2.6. Main Features
SLM technologies are commonly the most expensive due to the high cost of the base material (fine metal powder) and to the presence of one or more high power laser sources in the machine. MJ technology is also commonly expensive, especially in terms of the material’s cost. FFF machines are the cheapest both in terms of machine and material cost. They are also capable of processing the widest range of materials (thermoplastic polymers). On the other hand, FFF machines feature the lowest printing quality. BJ, MJ and some SLM machines working with polymers can feature full color resolution, offering great advantages in terms of anatomical modeling. BJ, SLS and some SLM working with polymers can avoid the use of support structures to be removed after the printing, thanks to their functioning principles structure [15].
The application of the aforementioned technologies varies according to their technical features (e.g., minimum detail resolution, accuracy, speed of production) and to the materials’ specifications (e.g., level of biocompatibility, mechanical properties) [16]. Table 1 shows the most relevant 3D-printable materials, their applications in dentistry and the major features related to their use [15,16,26,27,28,29,30,31,32,33,34].

Table 1.
Groups of materials printable with the different 3D-printing technologies, their applications in dentistry, and major features.
3. The Digital Workflow
The steps of the “partial” digital workflow can be divided into the following five sequential steps: acquisition of the intra-oral scan, elaboration of the digital model, 3D printing, post-printing processing, and, finally, production of the model [1].
3.1. Intra-Oral Scanning
The purpose of this step is the acquisition of the morphology of the teeth and the adjacent soft tissues using an intraoral scanner (Figure 2). The image acquired must be exported as a standard tessellation language (STL) file in order to be available for the subsequent digital elaboration [1].
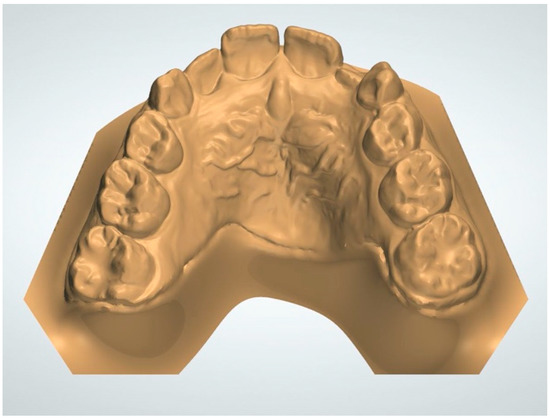
Figure 2.
Dental model acquired through intra-oral scanning.
3.2. Elaboration of the Digital Model
The model acquired in digital format results in an open surface. Accordingly, it is not adequate for the subsequent printing. Before this phase, the digital model requires a “solidification” (consisting of the filling of the hollow spaces) or a thickening of its borders [1]. It is important to notice that the base of the digital model is not required to be as deep as that of the analogic one. Different current software is available for the digital model preparation.
3.3. 3D Printing
Once the digital model has been processed, the subsequent step is to produce a 3D object, reproducing, with the highest possible definition, the model acquired and elaborated. Nowadays, 3D printing for clinical uses is generally based on stereolithography and digital light processing (SLA/DLP), due to its high accuracy. More and more companies are developing new 3D printers with specific characteristics. Generally, the most important factors which distinguish each respective printer are the following: the surface area of the build platform size, the number of models printable per cycle, the printing resolution and speed, the variety of printable resins, the ease of use, and, inevitably, the cost [1].
3.4. Post-Printing Processing
This phase is extremely dependent on the 3D printing process, the material used and the printer manufacturer’s indications. In particular, the post-printing process is required only for SLA technology but not for the other technologies. Generally, the model is washed for 10 min in isopropyl alcohol (IPA) 95% to remove the uncured resin [1]. Despite IPA being volatile, models must be air- or blow-dried to remove any residual of this compound. Subsequently, the model needs to be cured. Despite it is due to gradually harden when exposed to light, the model is generally exposed to UV light and heat. This assures a uniform polymerization in quick times. From now on, models are available to be handled without gloves [1].
3.5. Production of the Appliance
This stage consists of replication of traditional techniques for the production of orthodontic retainers and aligners, where a vacuum or pressure forming machine is employed to form the thermoplastic material exactly around the model. The main advantage of 3D printed models compared to the conventional plaster ones is represented by the fact that they are much less fragile and thus can be easily stored. Additionally, in case the working model is not available anymore, the entire process can be repeated with the final production of a new one starting from the original digital file. [1]
As regards the major applications of 3D printing, the production of working models represents a common application in the different specific fields of dentistry. Considering orthodontics, other applications are represented by the production of orthodontic retainers, activators, sleep apnea appliances, bites, customized lingual orthodontic brackets, Herbst appliance, occlusal splints, surgical templates for orthodontic miniscrews and miniplates placement. Other specific applications are related, for example, to prosthodontics (e.g., production of crown and bridge dentures, complete dentures, removable partial denture frameworks, etc.), oral implantology (e.g., production of custom trays and surgical guides for implants’ positioning) and oral/maxillofacial surgery (e.g., for the production of occlusal splints, surgical implants, prostheses) [23,35].
Case reports showed that appliances fabricated using CAD/CAM technology perform, clinically, like conventional orthodontic appliances [36,37].
Figure 3 and Figure 4 show a Rapid Palatal Expander (RPE) produced using a digital workflow encompassing the 3D printing.
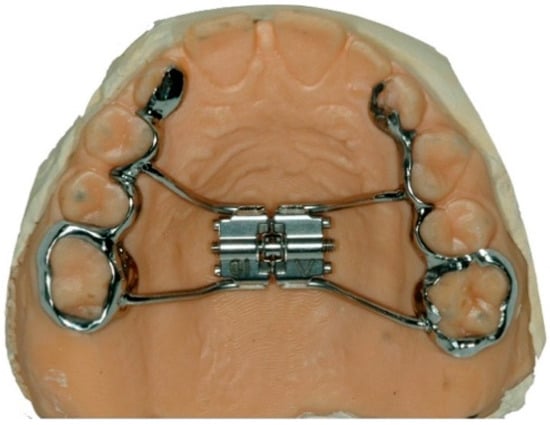
Figure 3.
RPE welded to laser melting bands on a plaster model.
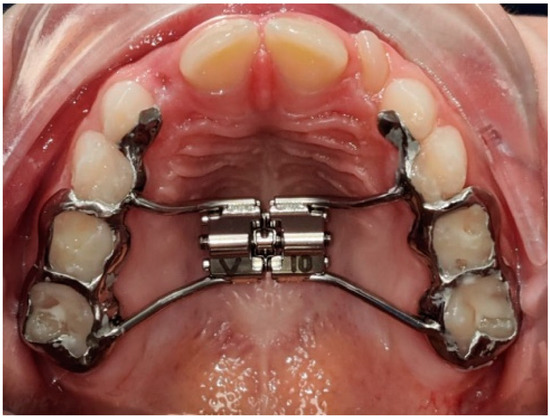
Figure 4.
Clinical image of a cemented RPE.
Figure 5 and Figure 6 respectively show the radiological planning for the placement of orthodontic miniscrews and the relative 3D printed surgical guide.
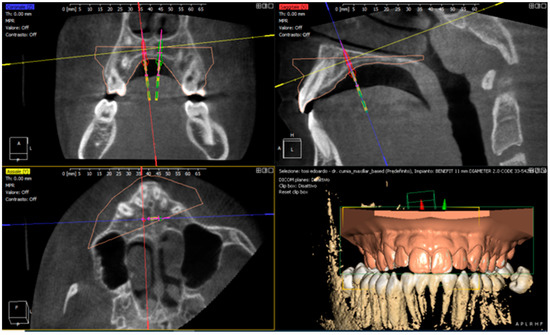
Figure 5.
Three dimensional (3D) planning of a surgical guide for the placement of orthodontic miniscrews.

Figure 6.
Three dimensional (3D) printed surgical guide for the placement of orthodontic miniscrews.
4. Advantages and Disadvantages of 3D Printing
Every technique, both traditional and innovative, is generally characterized by specific advantages and disadvantages which respectively promote and contrast the diffusion of the technique in question. Here is a summary of the pros and cons generally recognized for 3D printing [1,4,31,32,33,34,38,39,40,41,42,43,44].
4.1. Advantages
The advantages of the digital workflow and 3D printing are:
- -
- Accuracy: while traditional models might undergo technical errors and distortions, 3D-printed models might be more accurate as they involve less steps and no manual labor.
- -
- Comfort to the patient: the scanning process might be more comfortable for the patients than the traditional impression technique.
- -
- Reduction of the times: due to the absence of analogic impressions, clinicians can directly send digital STL files to technicians, resulting in a digital workflow much more rapid compared to the traditional one.
- -
- Management of defects: during the elaboration of the digital model acquired, eventual scan defects can be solved guaranteeing a correct progression towards the printing of a reliable product.
- -
- Reduction of environmental costs: considering that traditional dental impressions are avoided by substituting them with STL file, the digital workflow inevitably reduces the numbers of materials which would require to be specifically disposed of. Accordingly, environmental costs are significantly reduced.
4.2. Disadvantages
The disadvantages of the digital workflow and 3D printing are:
- -
- Costs: the expense for the purchase of the 3D printing and hardware are significantly higher compared to the analogic workflow.
- -
- Longer learning curve: specific training is required for clinicians to familiarize themselves with the use of intraoral scanners to acquire a correct scanning guaranteeing a correct result of the entire process.
- -
- The necessity of referral to specific technical laboratories: only laboratories with the available technologies required can be considered by clinicians working with a digital workflow.
- -
- Health risk: specific procedures must be followed when handling uncured resins and cleaning solvents to avoid skin irritations caused by these materials. However, further aspects should be evaluated as regards the eventual toxicity of 3D-printed resins. In particular, monomer resins are recognized as toxic, despite their polymeric form generally are not.
5. Conclusions and Future Perspectives
The present review aims to highlight the potentiality of the digital workflow in dentistry, encompassing the use of 3D printing. In recent years, many more clinicians are facing a revolution in their clinical activity with a reduction that has gone through a significant change with a progressive transition from analogic towards digital dentistry. This requires an important familiarization with software and technologies for both dentists and dental technicians. Several advantages are linked to 3D printing, such as accuracy, patient comfort, shorter times and the reduction of environmental costs. Conversely, some disadvantages are still related to this technology (e.g., costs, longer learning curve, the necessity of referral to specific technical laboratories, and health risk), therefore further research should be performed to improve these shortcomings.
Based on this consideration, the digital workflow will likely go through a further expansion from a clinical point, and this not only in orthodontics but in almost every field of dentistry. Accordingly, future research should be conducted focusing on the mechanical properties of 3D-printed materials, to select the best-performing material for the specific application and further expanding the range of dental appliances that can be 3D printed for clinical use. In particular, in vitro tests should be carried out to compare both the microhardness and flexural strength of conventional materials and the respective 3D-printed version.
Author Contributions
Conceptualization, P.G., M.F.S. and A.S.; methodology, M.F.S. and A.S.; software, A.S.; validation, M.F.S., P.C., S.M.; formal analysis, A.S.; investigation, S.G. and M.P.; resources, M.A.M. and D.B.; data curation, A.S.; writing—original draft preparation, S.G. and M.P.; writing—review and editing, A.S., P.C., S.M.; visualization, P.G. and M.A.M.; supervision, P.G.; project administration, P.G. and M.F.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Cousley, R.R. Introducing 3D printing in your orthodontic practice. J. Orthod. 2020, 47, 265–272. [Google Scholar] [CrossRef] [PubMed]
- Aragón, M.L.; Pontes, L.F.; Bichara, L.M.; Flores-Mir, C.; Normando, D. Validity and reliability of intraoral scanners compared to conventional gypsum models measurements: A systematic review. Eur. J. Orthod. 2016, 38, 429–434. [Google Scholar] [CrossRef]
- Sfondrini, M.F.; Gandini, P.; Malfatto, M.; Di Corato, F.; Trovati, F.; Scribante, A. Computerized Casts for Orthodontic Purpose Using Powder-Free Intraoral Scanners: Accuracy, Execution Time, and Patient Feedback. BioMed Res. Int. 2018, 2018, 4103232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, G.B.; Currier, G.F.; Kadioglu, O.; Kierl, J.P. Accuracy of 3-dimensional printed dental models reconstructed from digital intraoral impressions. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 733–739. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beuer, F.; Schweiger, J.; Edelhoff, D. Digital dentistry: An overview of recent develompents for CAD/CAM generated restorations. Br. Dent. J. 2008, 204, 505–511. [Google Scholar] [CrossRef]
- Ligon, S.C.; Liska, R.; Stampfl, J.; Gurr, M.; Mülhaupt, R. Polymers for 3D Printing and Customized Additive Manufacturing. Chem. Rev. 2017, 117, 10212–10290. [Google Scholar] [CrossRef] [Green Version]
- Vidakis, N.; Petousis, M.; Maniadi, A.; Koudoumas, E.; Kenanakis, G.; Romanitan, C.; Tutunaru, O.; Suchea, M.; Kechagias, J. The Mechanical and Physical Properties of 3D-Printed Materials Composed of ABS-ZnO Nanocomposites and ABS-ZnO Microcomposites. Micromachines 2020, 11, 615. [Google Scholar] [CrossRef]
- Skorski, M.; Esenther, J.; Ahmed, Z.; Miller, A.; Hartings, M. The chemical, mechanical, and physical properties of 3D printed materials composed of TiO2 -ABS nanocomposites. Sci. Technol. Adv. Mater. 2016, 17, 89–97. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dodziuk, H. Applications of 3D printing in healthcare. Kardiochir. Torakochir. Pol. 2016, 13, 283–293. [Google Scholar] [CrossRef]
- Richert, R.; Goujat, A.; Venet, L.; Viguie, G.; Viennot, S.; Robinson, P.; Farges, J.C.; Fages, M.; Ducret, M. Intraoral Scanner Technologies: A Review to Make a Successful Impression. J. Healthc. Eng. 2017, 2017, 8427595. [Google Scholar] [CrossRef]
- Bhargav, A.; Sanjairaj, V.; Rosa, V.; Feng, L.W.; Fuh Yh, J. Applications of additive manufacturing in dentistry: A review. J. Biomed. Mater. Res. B Appl. Biomater. 2018, 106, 2058–2064. [Google Scholar] [CrossRef]
- Liaw, C.Y.; Guvendiren, M. Current and emerging applications of 3D printing in medicine. Biofabrication 2017, 9, 024102. [Google Scholar] [CrossRef]
- Tack, P.; Victor, J.; Gemmel, P.; Annemans, L. 3D-printing techniques in a medical setting: A systematic literature review. Biomed. Eng. Online 2016, 15, 115. [Google Scholar] [CrossRef] [Green Version]
- Alhnan, M.A.; Okwuosa, T.C.; Sadia, M.; Wan, K.W.; Ahmed, W.; Arafat, B. Emergence of 3D Printed Dosage Forms: Opportunities and Challenges. Pharm. Res. 2016, 33, 1817–1832. [Google Scholar] [CrossRef] [PubMed]
- Kessler, A.; Hickel, R.; Reymus, M. 3D Printing in Dentistry-State of the Art. Oper. Dent. 2020, 45, 30–40. [Google Scholar] [CrossRef]
- Tappa, K.; Jammalamadaka, U. Novel biomaterials used in medical 3D printing techniques. J. Funct. Biomater. 2018, 9, 17. [Google Scholar] [CrossRef] [Green Version]
- Chia, H.N.; Wu, B.M. Recent advances in 3D printing of biomaterials. J. Biol. Eng. 2015, 9, 4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, Q.; Leu, M.C.; Schmitt, S.M. Rapid prototyping in dentistry: Technology and application. Int. J. Adv. Manuf. Technol. 2005, 29, 317–335. [Google Scholar] [CrossRef]
- Barazanchi, A.; Li, K.C.; Al-Almeh, B.; Lyons, K.; Waddell, J.N. Additive technology: Update on current materials and applications in dentistry. J. Prosthod. 2017, 26, 156–163. [Google Scholar] [CrossRef] [PubMed]
- Fleming, P.S.; Marinho, V.; Johal, A. Orthodontic measurements on digital study models compared with plaster models: A systematic review. Orthod. Craniofac. Res. 2011, 14, 1–16. [Google Scholar] [CrossRef]
- Al Mortadi, N.; Eggbeer, D.; Lewis, J.; Williams, R.J. CAD/CAM/AM applications in the manufacture of dental appliances. Am. J. Orthod. Dentofac. Orthop. 2012, 142, 727–733. [Google Scholar] [CrossRef] [PubMed]
- ASTM Standard F2792; Standard Terminology for Additive Manufacturing Technologies; ASTM F2792—10e1; ASTM International: West Conshohocken, PA, USA, 2012.
- Bartkowiak, T.; Walkowiak-Sliziuk, A. 3D printing technology in orthodontics–review of current applications. J. Stomatol. 2018, 71, 356–364. [Google Scholar] [CrossRef]
- Osman, R.B.; Alharbi, N.; Wismeijer, D. Build angle: Does it influence the accuracy of 3D-printed dental restorations using digital light-processing technology. Int. J. Prosthodont. 2017, 30, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Taneva, E.; Kusnoto, B.; Evans, C.A. 3D scanning, imaging, and printing in orthodontics. Issues Contemp. Orthod. 2015, 147–188. [Google Scholar]
- Gad, M.M.; Fouda, S.M.; Abualsaud, R.; Alshahrani, F.A.; Al-Thobity, A.M.; Khan, S.Q.; Akhtar, S.; Ateeq, I.S.; Helal, M.A.; Al-Harbi, F.A. Strength and Surface Properties of a 3D-Printed Denture Base Polymer. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2021. [Google Scholar] [CrossRef]
- Al-Qahtani, A.S.; Tulbah, H.I.; Binhasan, M.; Abbasi, M.S.; Ahmed, N.; Shabib, S.; Farooq, I.; Aldahian, N.; Nisar, S.S.; Tanveer, S.A.; et al. Surface Properties of Polymer Resins Fabricated with Subtractive and Additive Manufacturing Techniques. Polymers 2021, 13, 4077. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; Shim, J.S.; Lee, D.; Shin, S.H.; Nam, N.E.; Park, K.H.; Shim, J.S.; Kim, J.E. Effects of Post-Curing Time on the Mechanical and Color Properties of Three-Dimensional Printed Crown and Bridge Materials. Polymers 2020, 12, 2762. [Google Scholar] [CrossRef]
- Bayarsaikhan, E.; Lim, J.H.; Shin, S.H.; Park, K.H.; Park, Y.B.; Lee, J.H.; Kim, J.E. Effects of Postcuring Temperature on the Mechanical Properties and Biocompatibility of Three-Dimensional Printed Dental Resin Material. Polymers 2021, 13, 1180. [Google Scholar] [CrossRef]
- Berli, C.; Thieringer, F.M.; Sharma, N.; Müller, J.A.; Dedem, P.; Fischer, J.; Rohr, N. Comparing the mechanical properties of pressed, milled, and 3D-printed resins for occlusal devices. J. Prosthet. Dent. 2020, 124, 780–786. [Google Scholar] [CrossRef]
- Fayyaz Ahamed, S.; Mohnish Kumar, S.; Vijaya Kumar, R.K.; Apros Kanna, A.S.; Indrapriyadharshini, K. Cytotoxic evaluation of directly 3D printed aligners and Invisalign. Eur. J. Mol. Clin. Med. 2020, 7, 1129–1140. [Google Scholar]
- Colombo, M.; Gallo, S.; Poggio, C.; Ricaldone, V.; Arciola, C.R.; Scribante, A. New Resin-Based Bulk-Fill Composites: In Vitro Evaluation of Micro-Hardness and Depth of Cure as Infection Risk Indexes. Materials 2020, 13, 1308. [Google Scholar] [CrossRef] [Green Version]
- Moharamzadeh, K.; Van Noort, R.; Brook, I.M.; Scutt, A.M. Cytotoxicity of resin monomers on human gingival fibroblasts and HaCaT keratinocytes. Dent. Mater. 2007, 23, 40–44. [Google Scholar] [CrossRef]
- Gupta, S.K.; Saxena, P.; Pant, V.A.; Pant, A.B. Release and toxicity of dental resin composite. Toxicol. Int. 2012, 19, 225–234. [Google Scholar] [PubMed] [Green Version]
- Tian, Y.; Chen, C.; Xu, X.; Wang, J.; Hou, X.; Li, K.; Lu, X.; Shi, H.; Lee, E.S.; Jiang, H.B. A Review of 3D Printing in Dentistry: Technologies, Affecting Factors, and Applications. Scanning 2021, 2021, 9950131. [Google Scholar] [CrossRef] [PubMed]
- Graf, S.; Cornelis, M.A.; Hauber Gameiro, G.; Cattaneo, P.M. Computer-aided design and manufacture of hyrax devices: Can we really go digital? Am. J. Orthod. Dentofac. Orthop. 2017, 152, 870–874. [Google Scholar] [CrossRef] [Green Version]
- Graf, S.; Vasudavan, S.; Wilmes, B. CAD-CAM design and 3-dimensional printing of mini-implant retained orthodontic appliances. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 877–882. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neumeister, A.; Schultz, L.; Glodecki, C. Investigations on the accuracy of 3D-printed drill guides for dental implantology. Int. J. Comput. Dent. 2017, 20, 35–51. [Google Scholar]
- Osman, R.B.; van der Veen, A.J.; Huiberts, D.; Wismeijer, D.; Alharbi, N. 3D-printing zirconia implants; a dream or a reality? An in-vitro study evaluating the dimensional accuracy, surface topography and mechanical properties of printed zirconia implant and discs. J. Mech. Behav. Biomed. Mater. 2017, 75, 521–528. [Google Scholar] [CrossRef]
- Camardella, L.T.; de Vasconcellos Vilella, O.; Breuning, H. Accuracy of printed dental models made with 2 prototype technologies and different designs of model bases. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 1178–1187. [Google Scholar] [CrossRef] [Green Version]
- Favero, C.S.; English, J.D.; Cozad, B.E.; Wirthlin, J.O.; Short, M.M.; Kasper, F.K. Effect of print layer height and printer type on the accuracy of 3-dimensional printed orthodontic models. Am. J. Orthod. Dentofac. Orthop. 2017, 152, 557–565. [Google Scholar] [CrossRef] [Green Version]
- Hazeveld, A.; Huddleston Slater, J.J.; Ren, Y. Accuracy and reproducibility of dental replica models reconstructed by different rapid prototyping techniques. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 108–115. [Google Scholar] [CrossRef] [PubMed]
- Sherman, S.L.; Kadioglu, O.; Currier, G.F.; Kierl, J.P.; Li, J. Accuracy of digital light processing printing of 3-dimensional dental models. Am. J. Orthod. Dentofac. Orthop. 2020, 157, 422–428. [Google Scholar] [CrossRef] [PubMed]
- Canzi, P.; Magnetto, M.; Marconi, S.; Morbini, P.; Mauramati, S.; Aprile, F.; Avato, I.; Auricchio, F.; Benazzo, M. New frontiers and emerging applications of 3D printing in ENT surgery: A systematic review of the literature. Acta Otorhinolaryngol. Ital. 2018, 38, 286–303. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
