Featured Application
The study aimed to demonstrate the abilities and potential usefulness of the method for determining the spinous processes line of vertebrae in spinal deformities by combining X-rays and 3D surface topography (3D ST) scans to enhance visualization of the whole scoliotic spine.
Abstract
Scoliosis is a three-dimensional trunk and spinal deformity. Patient evaluation is essential for the decision-making process and determines the selection of specific and adequate treatment. The diagnosis requires a radiological evaluation that exposes patients to radiation. This exposure reaches hazardous levels when numerous, repetitive radiographic studies are required for diagnostics, monitoring, and treatment. Technological improvements in radiographic devices have significantly reduced radiation exposure, but the risk for patients remains. Optical three-dimensional surface topography (3D ST) measurement systems that use surface topography (ST) to screen, diagnose, and monitor scoliosis are safer alternatives to radiography. The study aimed to show that the combination of plain X-ray and 3D ST scans allows for an approximate presentation of the vertebral column spinous processes line in space to determine the shape of the spine’s deformity in scoliosis patients. Twelve patients diagnosed with scoliosis, aged 13.1 ± 4.5 years (range: 9 to 20 years) (mean: Cobb angle 17.8°, SD: ±9.5°) were enrolled in the study. Patients were diagnosed using full-spine X-ray and whole torso 3D ST. The novel three-dimensional assessment of the spinous process lines by merging 3D ST and X-ray data in patients with scoliosis was implemented. The method’s expected uncertainty is less than 5 mm, which is better than the norm for a standard measurement tool. The presented accuracy level is considered adequate; the proposed solution is accurate enough to monitor the changes in the shape of scoliosis’s spinous processes line. The proposed method allows for a relatively precise calculation of the spinous process lines based on a three-dimensional point cloud obtained with a four-directional, three-dimensional structured light diagnostic system and a single X-ray image. The method may help reduce patients’ total radiation exposure and avoid one X-ray in the sagittal projection if biplanar radiograms are required for reconstructing the three-dimensional line of the spinous processes line.
1. Introduction
Scoliosis produces three-dimensional trunk and spinal deformity. Patient evaluation is an essential point in the decision-making process and determines specific and adequate treatment. The diagnosis requires radiological evaluation of elements such as the Cobb angle, axial rotation, curve pattern classifications, and sagittal configuration to describe scoliosis’s three-dimensional nature. Scoliosis is usually diagnosed using radiography, which operates with a particular radiation dose [1,2]. Plain radiography is usually insufficient to show the three-dimensional shape of the vertebral column.
Expense and radiation dose are reported as the main disadvantages of radiographic methods. Considering the elevated radiation exposure for scoliotic patients who require a periodic radiographic examination, a combined method is proposed for assessing the vertebral column shape expressed by the line of spinous processes. There is a growing awareness of the disadvantages of radiographs. Methods are being sought to reduce the patient’s exposure to X-rays. Reducing the radiation dose by even a single exposure is worth investigating. Several studies have shown the oncogenic effects of radiation exposure. Nash et al. [3] estimated that the increase in risk due to X-ray radiation ranges from 3.4 to 15 per million if teenage patients with scoliosis are subjected to an average of 22 radiographs over three years. Ronckers et al. [4,5] found that cancer mortality was 8% higher than expected in patients who had repeated radiographs for scoliosis, and there was a four-fold greater relative risk of breast cancer in female patients with spinal disorders. Women receiving 50 or more radiographs within 30 years may have a 4.1 higher mortality ratio from breast cancer [6]. Simony et al. [7] found a 4.3% higher rate of overall cancer in this Adolescent Idiopathic Scoliosis (AIS) Danish cohort than in the national population. That risk is five times higher when compared to the age-matched population. Endometrial and breast cancer were most the frequent types of cancer found in this study group.
Computed tomography, magnetic resonance imaging and, recently, slot-scanning three-dimensional X-ray imaging (EOS) enable three-dimensional spinal reconstructions. Despite the technological improvements in radiographic devices that reduce the radiation dose significantly, the risk is still not eliminated for patients. The risk may be reduced with the modern microdose biplanar radiographic system [8,9,10,11,12,13,14,15,16].
Until 2004, the only alternative to conventional X-ray devices was computed tomography. A year later, Dubousset and Charpak [17], together with colleagues, proposed a new device in which they used a gaseous X-ray detector invented and awarded with Nobel Prize by Charpak [18,19]. This approach reduces the dose of radiation required to obtain a 2D image of the skeleton by 8–10 times compared to the classic X-ray image. In the case of 3D ST reconstruction of the spine, when the reference technique is computed tomography, the reduction was 800–1000 times [16,20,21,22,23,24]. A 3D ST spine model in the EOS system is not calculated automatically; it must indicate a set of reference points [25]. Radiation-free examination using ultrasound dedicated to detecting scoliosis up to approximately a 30°Cobb angle [24] usually lasts longer. The EOS system has recently become a recommended diagnostic system due to the microdose of radiation [10,12,15,22,23]. Possible imperfections may occur [26] when an examined patient cannot stand or sit steadily during image acquisition [27]. Only an EOS imager may significantly lower radiation exposure. However, the EOS system cannot be considered a standard, and it is not the equipment used in every radiology department. Mahboub-Ahari et al. mentioned that one of the limitations of the EOS system [28] is that it cannot be considered cost-effective. Its use is also limited while examining children and pregnant women [29]. The costs incurred for the purchase of the expensive system may be justified with public health needs.
Therefore, efforts to reduce the frequency of radiographic examinations should be taken, including developing a method that reduces the need for X-ray to estimate the spinous processes line for patients with scoliosis. A hypothesis was made that it is possible to determine the spine’s three-dimensional spinous processes line from one X-ray and a point cloud. This study describes a method that allows approximating the results of 3D ST and radiological examinations, but using the spinous processes as a reference point due to their closest location to the posterior surface mapped with 3D ST. The use of the uniplanar full spine radiogram combined with the proposed method may deliver additional information during clinical decision making.
This study presents the method of three-dimensional assessment of the spinous process lines by merging 3D ST and X-ray data in patients with scoliosis.
2. Materials and Methods
Diagnostic images of twelve patients (11 girls and one boy) with an age of 13.1 y ± 4.5 y (range 4–20 y) and diagnosed with scoliosis (mean Cobb angle 17.8° ± 9.5°, range 12–39°) were used in the study. Additionally, the thirteenth patient, a 15-year-old girl, 62.2° Cobb angle, was analyzed to present the method’s abilities only due to the 3D ST methodology’s limitations. Institutional review board approval was obtained (KB 22/2012) for the study. All patients provided written, informed consent to participate in the study. The inclusion criterion was a diagnosis of AIS. Post-traumatic, adult, degenerative scoliosis cases were excluded from this study. The analysis included cases that qualified for conservative treatment and that were classified according to Rigo [30]. Scoliosis type A1 was found in four cases, and there two cases each of types A2, C1, C2, and E1. The thirteenth patient was classified B1 by the Rigo classification. However, this case qualified for surgery.
The novel approach was introduced to merge the two-dimensional radiograph with the surface topography (ST) cloud points. The merge of an X-ray image and the point clouds generated by a 3D ST optical scanner was conducted using a vertical calibration line and the reference values. The spinous process line from the radiograph was then projected onto the ST cloud point, and a spline was fitted. The 3D ST data were acquired using a prototype custom-made structured light illumination (SLI) 3D scanner developed for the project entitled “A three-dimensional computer system for designing the functional evaluation of orthopedic equipment in patients with disorders of statics and kinematics of the body in the course of civilization diseases of the musculoskeletal system”. The 3D ST optical system methodology used in this study has been presented in previous studies (Figure 1) [31,32,33].
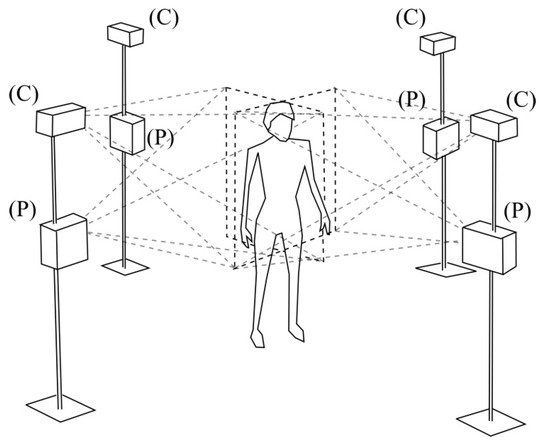
Figure 1.
Four-directional optical measurement system scheme. C—camera, P—projector.
Each scanner acquired information about a partial shape of a patient’s body, which could be captured from its position. The relative position transformation of each scanner was determined during the calibration process. The calibration enables directional data. Naturally, the measurement process consisted of the patient’s body illumination with a sequence of a projected fringe patterns (P). The color of the fringes of neighboring scanners was different. Contralateral scanners emitted the same color of the fringes. Blue and red colors were used because of their ability to be easily distinguished by optical filters mounted on the cameras (Figure 2).
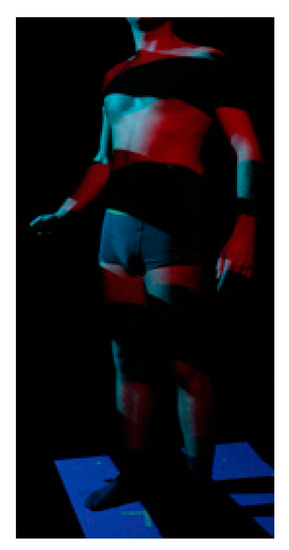
Figure 2.
A patient’s body being illuminated with a sequence of a projected color fringe patterns.
Subsequent projected fringe patterns were captured by the cameras. Projectors and cameras were synchronized to each other to deliver temporarily coherent data. The shape of the patient’s body was calculated for each directional system separately from the sequence of registered images of distorted fringes. Finally, data from all cameras were combined. The merging method combined data from the radiogram and the calculation of the spinous processes line.
The 3D ST system was composed of four unidirectional optical scanners. The scanners’ main components and the structured light method used in the study are described in previous studies [31].
The measurement volume was 1500 × 1400 × 1000 mm. A homogeneous cloud of 100,000 points represented the average 3D ST patient’s body image. The ST diagnostic system could capture the 3D ST full torso image in 1.4 s to make it possible to keep a still standing position, even for younger children and older patients.
2.1. Data Merging
The plain X-ray full standing image data and the 3D ST optical scanning data were obtained in their coordinate systems (Figure 2.). The X-ray image was placed in the xyz coordinate system, while the optical system cloud of points and the best fit data were located in a different coordinate system, denoted by x’y’z’. Data alignment was required before merging. The software was designed to align the 2D X-ray image and the cloud of points acquired by the optical scanner. The reference coordinate system (RCS) of the X-ray image was based on the patient’s body orientation.
The following formula was used to transform the X-ray image from the RCS into global coordinates.
S(x), S(y), and S(z) are positions of the image in the x, y, and z axes, respectively. Positions are relative to the origin of the RCS. The variables X(x), X(y), X(z), Y(x), Y(y), and Y(z) represent the row (X) and column (Y) directions of cosines of the image. The Δi and Δj are the columns and rows of pixel resolutions according to the Digital Imaging and Communications in Medicine (DICOM) standard; i and j represent the column and row indices of the model in the image plane; and P(x), P(y), and P(z) represent the positions of the voxels represented by the indices i and j in the world coordinates. All variables (S(x), S(y), S(z), X(x), X(y), X(z), Y(x), Y(y), Y(z), Δi, and Δj) present information that can be obtained from a DICOM file providing data recorded by an X-ray device during a study. S(x), S(y), and S(z) denote the offset of the image stored in the DICOM document relative to the origin of the device’s coordinate system, in which the image was stored. The standard coordinate system for radiographic data and 3D ST data is a static X-ray image, denoted as xyz. All transformations are related to the point cloud oriented in the x’y’z’ coordinate system. Data merging orients and changes the position of the point cloud. In the present study, S(z) was positioned in the center of the coordinate system and was always set to zero. The presented parameters define the position of the image of the patient’s body while in a standing position. The optical scanning system’s coordinate system depends on a calibration plane’s position and orientation during the calibration process. Proper calibration of the optics and patient settings ensures that the collected data are arranged according to radiological data, making them easy to combine.
Calibration and proper patient positioning guarantee that the data collected by the optical system are in the coordinate system corresponding to the frontal mode of the RCS with anatomical axes directed as right, anterior, and superior (RAS). The measurement data match an auxiliary coordinate system defined by the axes x’, y’, and z’, as the patient cannot stand directly in line with the optical measurement system’s axes. Presented computations use the xyz coordinate system to merge two independently performed exams (X-ray and 3D ST).
The patient was advised to stand with fingers on the clavicles during the optical measurement and X-ray radiography. The X-ray data were placed in the xy plane. The patient’s posture during 3D ST image acquisition was seen along the z’-axis. While both positions may look similar superficially, they may not be identical, and therefore, data alignment was required. If the X-ray image is considered the baseline, its position and orientation should remain unchanged, and the position and orientation of the 3D ST data are modified. The orientation of the cloud of points representing the surface of the patient’s body must be identified. The best-fit plane of the cloud of points concerning the xyz coordinate system was computed using the least-squares method [34]. A plane fit algorithm can be simplified if the patient is assumed to be oriented vertically along the z-axis. With this assumption, the orientation of the normal vector of the sagittal plane passing through the patient’s body was slightly tilted on the z-axis. The normal vector to the torso surface at point P was determined by fitting the plane to points adjacent in a radius of 10mm to point P. The results of finding the best-fit plane were sufficient to calculate the total error function E defined for the z coordinate only. For the plane defined as , the error function is given by the following equation:
The error is minimal when The point where this condition is fulfilled can be found by solving a set of linear equations. The equations are given in matrix form as follows:
The angles from the normal to the best-fit plane and the vector in which , and denote versors of the xyz coordinate system are calculated using the formula:
The change in orientation is relative to the mass center of the 3D ST data. The mass center of the cloud of points is given by:
The PMC and PIC are vectors between the origin of the xyz coordinate system and PMC and PIC points, respectively. The complete transformation matrix for the cloud of points is a combination of subsequent translation T and rotation R operations.
After translation of the cloud by the vector −PMC to the xyz coordinate system’s origin point, the subsequent rotations around x and z are performed at −Θ(x) and −Θ(x) angles, respectively. The cloud is translated by vector PMC(y) to its original position on the y-axis and then by vector PIC(x) in the x-axis to the PIC point, which coincides with the PMC point in this axis (Figure 3).
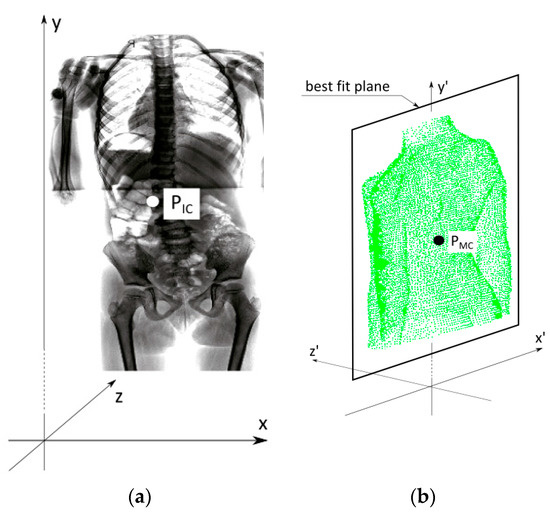
Figure 3.
Coordinate systems of an X-ray image and the cloud of points before alignment. (a) The radiogram is incorporated into the xyz coordinate system. PIC—the central point of the image. (b) The three-dimensional surface topography (3D ST) image from the structured light imaging system. PMC—the point of the center of gravity of the cloud of points.
The automatic adjustment described above allows approximate superimposition of the data from the two systems. The superimposition’s accuracy is evaluated visually by the specialist, who can see the X-ray image’s location inside the partially transparent cloud of points. The 3D ST modeling program allows the merged image to be rotated, shifted, and zoomed, allowing close inspection of the image from any angle. The X-ray image is placed in the correct location within the cloud of points, representing the patient’s trunk’s surface using the specialist’s expert knowledge and experience. If the superimposition is not precise enough, the image merge operator can manually adjust the radiogram’s 3D ST data. This process is repeated until proper superimposition is achieved. The 3D ST scanner image data and radiography data may obscure each other. The size of the points and the cloud of points’ opacity can be modified to improve the combined view. The result, using 100% opacity and 1 mm point size, is documented in Figure 4a. The merged data can be directly used for medical evaluation or used for further processing.
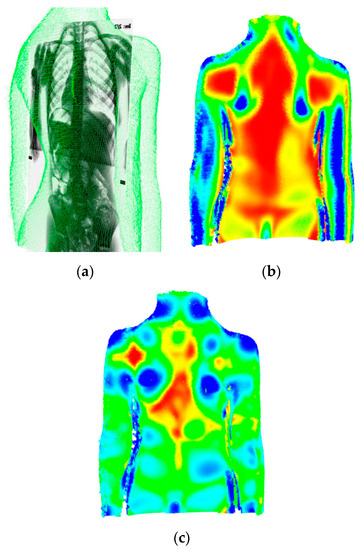
Figure 4.
Visualization of data obtained from the 3D ST scanning system. The composition of a cloud of points with a radiogram image (a). Gaussian curvature (b) and mean curvature (c) calculated for the cloud of points.
2.2. Data Analysis
The representations of the spinous processes’ superficial prominences indicating the spinous processes line are usually searched [31,35,36,37,38] to calculate the vertebral bodies’ locations. Therefore, the merged data points’ colors can be modified to better visualize the surface’s curvature and increase the image’s readability [39]. The physician can select the range of curvature values and stretch the image to full scale to visualize different colors and modes (Figure 4b,c). This approach simplifies the spinous processes line’s location solely based on the cloud of points.
Predicting the vertebral column shape using the 3D ST cloud of points alone can be difficult. The proposed new method for estimating the spinous processes line location projected on the cloud of points obtained by the 3D ST uses the mutually adjusted X-ray image and the 3D ST data. In the same way used to determine the spinous processes line, the X-ray image is manually marked using points representing the spine’s middle line. These points are then projected perpendicularly from the X-ray image plane onto the cloud of points (Figure 5a,b).
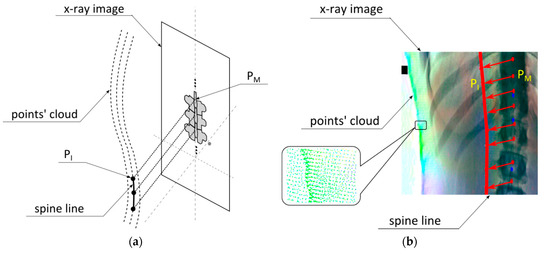
Figure 5.
The projection for assigning the middle line of spine markers from an X-ray image onto an adjusted image of the cloud of points. (a) The presentation of the concept of merging a 3D ST structured light image with the radiogram. PM—a single marked point, PI—the projection of the point PM onto the point cloud (b) An example of merging in a real case.
All cloud points are considered to be in a spherical area D in which the line intersects the cloud for each projected line. The radius of this area is 2 mm. The intersection point position is calculated as the average position of all dots located in the area. When PM is considered as a single marked point, and P is regarded as a point in the cloud, the distance d between the line passing through the point PM and the point P is calculated using the following equation:
The distance is calculated only for because only points on the posterior side of the trunk remain in the scope of our interest. Based on these points, a point of intersection, PI, is calculated. Positions in the x- and y-axes are the same for the points PM and PI. The z-axis position for PI is calculated as an average of the position of points in area D in the z-axis. The weight in the weighted mean is inversely related to the distance in axes x and y between the PM point and the analyzed point P.
Finally, a spline line [40] fits the points and is displayed on top of the cloud of points (Figure 4b). In the presented application, the vtkContourWidget was used to calculate a spline on the dots’ base [41].
2.3. Comparison of the Results
The reference spline calculated from the baseline of the cloud of points alone and the second spline, which was computed by the merged method, were indirectly compared. For comparison, both splines were intersected by a set of equidistant cutting planes parallel to the xz plane, and thus, two sets of points were produced. The distance between the two subsequent cutting planes was 1 mm. For each pair of cutting planes, a distance between the points was calculated to determine the line’s deviation from the reference line.
2.4. Statistical Analysis
The correlation analysis between the spinous line calculated directly from the cloud of points and the spinous line calculated by the presented method was done independently for the sagittal (x-axis) and frontal (z-axis) planes. The Spearman’s correlation was calculated at the 0.95 confidence level. The p-value was considered significant at 0.05. The calculations were made in the R version 4.0.3 using the built-in “stats” package.
3. Results
The method was tested on 12 scoliosis cases. The first case, a 16-year-old male with mild single curve thoracolumbar scoliosis, was used to verify the method’s accuracy. The superimposed spinous processes lines were determined by the acquired 3D ST data (Figure 6). In the biplanar view, the spinous processes line is located in the frontal view (the xy plane in Figure 3) as shown in Figure 6a; the sagittal view is shown in Figure 6b.
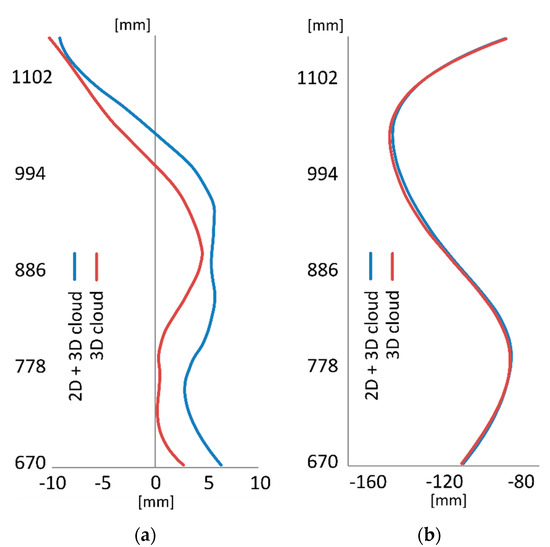
Figure 6.
The graph showing the spinous processes line calculated using the developed methodology (X-ray and 3D ST scanning) and data obtained based on the 3D ST data analyses alone. Frontal (a) and sagittal (b) views. The ordinate and abscissa values are presented using different scales to visualize the abscissa axis data better.
The spinous processes line is shown in the sagittal view (the yz plane in Figure 3). The distribution of the deviation without the decomposition on the x- and z-axes is shown in Figure 7a and is shown with the decomposition in Figure 7b.
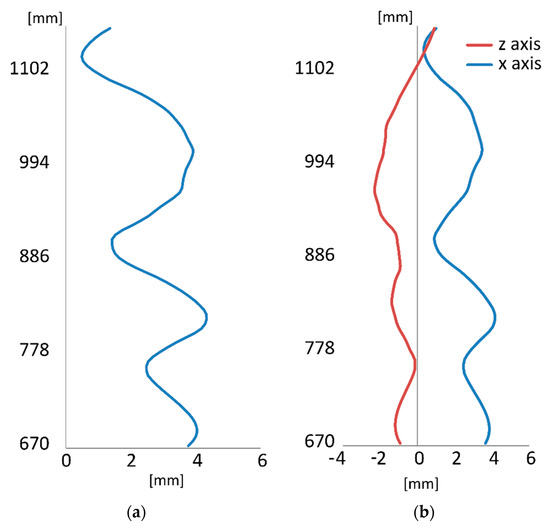
Figure 7.
Distribution of differences in distances between points belonging to the reference and subject spinous processes lines (a) and the x- and z-axes (b). The ordinate and abscissa values are presented using different scales to visualize the abscissa axis data better.
The mean deviation between the points of the lines was 2.84 mm. The maximal deviation was 4.34 mm. Because the spinous processes line is usually analyzed in two perpendicular planes (frontal and sagittal), the values of the deviations for the individual axes are crucial, as illustrated in Figure 7b. The mean deviations in the x- and z-axes were 2.54 mm and 1.01 mm, respectively, and the maximal deviations in the x- and z-axes were 4.17 mm and 2.40 mm, respectively, in the presented cases. The results for all twelve patients (PT1–PT12) in the study are presented in Table 1.

Table 1.
Maximal and mean deviations of the results taken as total value and decompositions on the x- and z-axes [mm].
The maximal deviation between the lines’ points was found in the patient (PT5), who had a maximal deviation of 18.9 mm. In most cases, the x-axis component was more deviated than the z-axis component. The mean deviation was 4.41 mm, and values for individual patients and axes are presented in Table 1. The group’s maximal deviations in the x-axis and z-axis were 18.67 mm and 9.19 mm, respectively.
The method developed here was intended for use in cases where it is impossible to calculate the spinous processes line using data only from the cloud of points obtained using 3D ST scanning. The cloud of points merged with the X-ray image is visible only in the case of scoliosis with a Cobb angle above 50° as presented in Figure 8. Specialists placed the markers on the 3D ST model in the frontal view (denoted by red dots in Figure 8a) in positions relative to spinal bones visible on the X-ray image. The presumed spinous processes line was calculated in the 3D ST real image of cases using the skin markers just above the spinous processes (Figure 8) to show the superimposition of the cloud of points and the X-ray image in the frontal (Figure 8a) and the sagittal (Figure 8b) views. The line is also presented without superimposition with the cloud of points in Figure 8c,d.
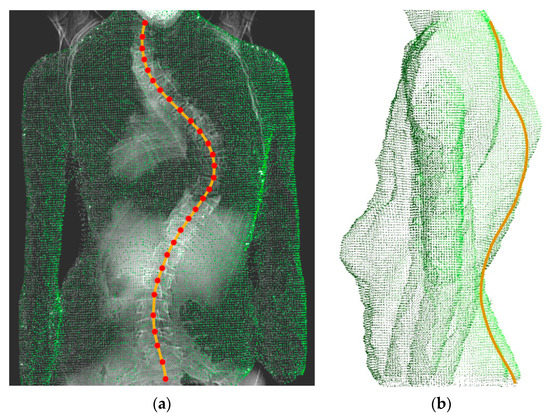
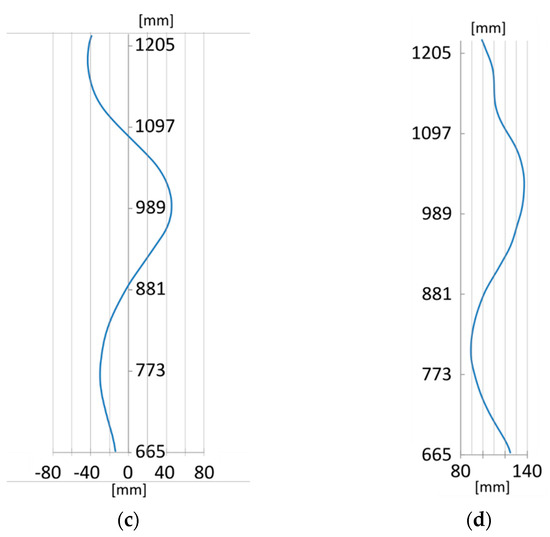
Figure 8.
The calculated spinous processes line projected onto the 3D ST data: the frontal (a) and the close-to-sagittal (b) views; the direct 2D visualization of the spinous processes line: the frontal (c) and sagittal (d) views.
Spearman’s rank correlation coefficients (ρs) for the coronal and sagittal planes calculated for the analyzed cases were in the range of 0.41–0.99, and 0.65–0.99, respectively (p-value < 0.03). The mean correlation for the frontal plane was 0.88; median 0.95; SD = 0.18. The mean correlation for the sagittal plane was 0.92, median 0.96, and SD = 0.11. The obtained results confirm a strong correlation between the lines obtained from both compared methods.
4. Discussion
Studies using 3D ST have often been used to find a measurement method that produces results parallel to the Cobb angle measured by conventional radiography [37,42,43,44,45,46,47,48,49,50,51,52]. Typically, the results of this approach are less than moderately accurate due to the different measures. The 6th SOSORT consensus paper indicated the Cobb angle could be seen neither as the unique nor the only decisive parameter in managing patients with idiopathic scoliosis [48].
The Cobb angle is measured for straight lines drawn for 3D objects—the sum of the absorptions of the vertebral bodies’ endplates visible on X-rays. The authors described a method that approximates 3D ST and radiological examination results but uses the spinous processes as a reference due to their closest location to the posterior surface mapped with 3D ST. As a spinal deformity, scoliosis is typically diagnosed using radiography, which operates with a particular radiation dose [1]. The novel three-dimensional evaluation of the spine using structured light has been proposed to supplement the radiogram to obtain a more accurate and reliable image and fulfill radiation dose reduction attempts [2,7,19,22,26,44]. The method of automatic measurement of anatomical landmarks (prominent skeletal structures) on the human back surface was used to calculate back shape indices from surface measurements [31,53]. The method described in this article allows finding the well correlated three-dimensional spinous processes line in mild to moderate scoliosis patients. Calculation and visualization of the spinous processes line may be useful for physicians, therapists, and patients (and parents for children and adolescents) to visualize the deformity. The range of reliable measurements was anticipated for patients with a Cobb angle smaller than 50° [44]. The curvature may be obscured to some extent by scapulae, as described by Drerup and Hierholzer. The approach presented in this study for scoliosis cases utilizes the combined data from 3D ST optical scans and X-rays.
As a result, contactless optical 3D ST systems are more frequently recommended to estimate spinous processes’ curvature and the spine line’s trajectory. Moiré topography [54], structured-light-projection-based systems [55,56], laser scanning, and videorasterstereography [31,51,57,58,59,60,61,62,63,64,65,66,67,68] are used for three-dimensional evaluation of the spine and full torso. The use of 3D ST also allows analysis of scoliotic deformity, chest deformities including funnel chest, posture, the kyphotic angle of the spine, and back shape, and the detection of stimulated back muscle contractions. Automatic localization of anatomical landmarks on the dorsal surface was proposed by Drerup and Hierholzer in 1987 [39] using calculations from rasterstereographic surface measurements and was continued by other researchers [34,42,45,69,70,71]. The surface curvature drawn from the image is related to the previously described anatomical osteologic prominencies [31,53]. The method allows for finding the 3D spinous processes line in patients with mild to moderate scoliosis. Calculation and visualization of the spinous processes line may help physicians, therapists, patients, and their parents visualize the deformity. The method described in this paper may be suitable for progressed scoliosis cases where other 3D ST methods are uncertain. The method was tested in one patient with a Cobb angle >50°. A single example may not demonstrate that the method is fully operational as it was only shown to work for larger curves by testing in one case. It is anticipated that future inventions will focus on providing 3D ST information of the vertebral column line based on X-ray devices already available in clinics [23]. An MRI scan is usually taken for spinal cord involvement or preoperative planning [19]. Ng and Bettany-Saltikov reviewed diagnostic methods and emphasized that scoliosis measurements should not focus only on Cobb angles best calculations because several methods may deliver equally accurate parameters [19]. The analysis of the human torso’s shape was also applied before and after scoliosis surgery [25,27,72]. The approach presented in this study utilizes the combined data from 3D ST optical scans and X-rays. X-ray imaging of the vertebral column remains crucial for scoliosis case diagnosis. The combination of 3D ST and radiography minimizes the number of required X-rays to one where two X-rays are usually needed. Only simultaneous biplanar radiographic devices with dedicated software (sterEOS software) can create three-dimensional representations of the whole spine [73]. Two perpendicular X-ray images obtained sequentially require extensive computer processing to produce similar results.
Moreover, it may be difficult for the patient to stand in the same body position during both radiographs in two different projections. The proposed solution combines a single posterior-anterior (PA) X-ray image with the information provided by a 3D ST optical system. Combining a plain radiogram and the 3D ST image seems more efficient because four-directional full 3D ST scanning produces significantly more information than unidirectional ST [45,70,71] without repeated exposure to ionizing radiation [74,75,76]. The task to reduce the lifetime risk of cancer from spinal radiographs among people with adolescent idiopathic scoliosis remains essential. Techniques using 3D ST optical scanning may improve patient safety.
The presented method is designed for predicting the spinous processes line and approximating the degree of scoliotic deformity. The method, however, assumes no vertebral torsion, and calculations are given only for rotation. There are few techniques for detecting the spinous processes line because most of the rough ST methods result in scoliometer measurements [63] or use particular indices to determine deformity [38]. Appropriate indices should be able to distinguish between different types of surface deformities [38]. Automatic detection of scoliosis by a computer using Moiré topographic images results in correct recognition in 95 % of cases [77]. Stokes et al. [78] found that a high degree of variability exists between spine scoliosis (Cobb angle) and trunk asymmetry with the back ST’s axial rotation. The method’s accuracy primarily depends on the quality of the X-ray image’s mutual adjustment with the cloud of points obtained using 3D ST optical scanning. The ideal result would be produced using a single device capable of simultaneous X-ray image acquisition and 3D ST optical scanning. In the present study, a single case presented a lower correlation of 0.41. In this case, the reason for the less accurate correlation was technical in nature and was due to the shorter length of the radiograph available for merging of the X-ray and 3D ST. The above would ensure that the data collected by both methods measure the patient in the same posture and would render post hoc alignment unnecessary. Less accurate results are obtained when the data alignment is based on markers placed on the patient’s body visible in both the X-ray image and the 3D ST data scan. Several 3D ST systems need markers on the patient’s back to identify bony landmarks or measure their contour. Stickers [36,79] or markers placed on landmarks of the back, including the spinous processes, are frequently used to identify the “spine line” [80] and follow the scoliosis curve [81] of examined patients. The use of too many markers during the evaluation may lead to skewing the 3D ST data superimposition over the X-ray image, even in simple cases.
This study was performed using previously existing data based on the markerless method. To our knowledge, only Formetric 3D ST [82] and 3DMADMAC/3D Orthoscreen [53] require no markers.
Performing the adjustment of images in the merging procedure in the method may affect the results’ reliability. When considering the case of significant decompensation of scoliosis, the obtained X-ray image could show the patient’s body’s asymmetrical alignment to the y-axis. The projection of the patient’s center of gravity on the x-axis may not be approximately at the center of the coordinate system but some distance from it. Therefore, after performing the translation , the cloud of points will be shifted concerning the image. In the worst scenario, the patient’s positioning during the X-ray is significantly different from the positioning during the 3D ST measurement. In this case, even manual adjustment of the data will be impossible, and the method will fail.
The small difference in the patient’s body’s slope in the xy plane between X-ray and 3D ST measurements will slightly deform the calculated line’s shape. Small gradients characterize the curvature of the back in humans. Therefore, a slight shift of the computed points’ position on the dorsum’s surface causes deformation in the shape of the line in the order of a few millimeters. Smaller rotations of the patient’s body of less than 45° in the xz plane are acceptable and can be compensated by rotation . More extensive rotations are unacceptable because the simplified approach used to calculate the best-fit plane fails. The inclination of the patient’s body in the yz plane can be compensated by rotation . It is unlikely that the inclination angle will be greater than 45° when the patient stands freely without any support. The position of the center of the mass of the cloud of points PMC depends on the shape of the cloud. The cloud of points should represent only the patient’s trunk, as the head and legs, and any asymmetrical areas without points, can change the position of PMC and influence the result of the best-fit plane calculation.
The average difference of 5 mm makes the method unsuitable for surgery planning. In this field, spatial radiological imaging methods, such as computed tomography, will probably remain unrivaled for a long time. The study aimed to develop a method that will visualize the vertebrae’s spinous processes with a good approximation based on a single radiological image, thus supporting the diagnosis. The spine line’s orthogonal projection from the X-ray image onto a point cloud was used in the proposed method.
There are several limitations to this study. First, it uses a single anteroposterior X-ray view of the spine. Therefore, the effectiveness of reducing exposure to X-rays is not entirely convincing. The effectiveness may be 50% only when biplanar radiograms are needed. Second, the study analyses were based on the cases with a relatively small Cobb angle. The authors do not discuss the method’s final effectiveness in patients with greater curvatures who are eligible for surgery. Similarly, the study results were not compared to patients with a high BMI, nor was scoliosis classification made in accordance with Lenke [83] (main thoracic, double thoracic, double major, triple major, single structural, or thoracolumbar/lumbar-main thoracic double curves).
Third, accurate geometric data on the X-ray examination performance should be known and taken into account, such as the X-ray lamp’s position in relation to the detector and the X-ray radiation course during exposure. The exact design parameters of the X-ray apparatus would have to be known. Moreover, it should be ensured that the examined person adopts the same body position during the 3D scanning as during the X-ray examination.
Regardless of this, during the 3D measurement, one can palpate characteristic points, such as those clearly visible on X-rays and easily palpable, such as the shoulder process, the C7 spinous process, the lower angles of the scapula, and the L4 spinous process. It is possible to register images accurately using well-marked characteristic points. The described method’s expected accuracy is approximately ±5 mm, which is a higher inaccuracy level than for a typical measurement tool. However, this level of accuracy is sufficient for monitoring the progress of scoliosis. Furthermore, the method is adequate if the physician requires only a rough estimate of the spinous processes line. In the future, this process may be partially automated, for example, by applying an algorithm for the detection of spinal curves from a postero-anterior view (PA) radiograph [29].
The presented method probably does not provide the level of accuracy necessary for planning spine surgery. However, the excellent correlation results for scoliosis with smaller angles justify its use to monitor the course of treatment of deformities. The spinous processes’ three-dimensional line can be well drawn by combining the PA X-ray and the 3D ST cloud point for scoliosis with larger Cobb angles.
5. Conclusions
The presented method’s clinical application can broaden the scope of applying a 3D ST scanner for scoliosis detection and 3D imaging to improve case analysis. The proposed method allows for calculating the spinous processes based on a four-directional 3D ST point cloud and a single X-ray image. The method is intended for use in patients with spinal deformities, for whom it is difficult to determine the line of the spinous processes only on the point cloud. This method may benefit a patient who requires two orthogonal X-rays of the spine to detect the spinous processes. Combining data from an optical scanner with a frontal radiograph can reduce the need for a sagittal X-ray in scoliosis cases when information about the spine line’s approximate shape is needed. The approximate shape of the spine line can be determined based on the frontal radiograph and the point cloud describing the shape of the examined person’s upper body surface for scoliosis cases with Cobb angles that qualify for conservative treatment. The final effectiveness of the method in patients with greater curvatures was not validated. Obtaining a confirming result in the study of a single case of more extensive scoliosis qualifying for surgery suggests an optimistic premise that the method may be useful in cases where the use of optical methods has been limited thus far. Further research should be devoted to analyzing a larger group of scoliosis cases with a larger Cobb angle.
Author Contributions
Conceptualization, S.P. and W.G.; methodology, S.P. and W.G.; software, S.P.; validation, S.P. and W.G.; formal analysis, S.P. and W.G.; investigation, S.P. and W.G.; resources, S.P. and W.G.; data curation, S.P. and W.G.; writing—original draft preparation, S.P.; writing—review and editing, S.P. and W.G.; visualization, S.P. and W.G.; supervision, S.P. and W.G.; project administration, W.G.; funding acquisition, S.P. and W.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by project NR13-0109-10 /2011, funded by the National Center for Research and Development and partially by the statutory financial support of the Ministry of Scientific Research and Higher Education for the Institute of Micromechanics and Photonics, Warsaw University of Technology. The APC was funded by the Warsaw University of Technology.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of the Medical University of Warsaw for the project entitled "A three-dimensional computer system for designing the functional evaluation of orthopedic equipment in patients with disorders of statics and kinematics of the body in the course of civilization diseases of the musculoskeletal system” (Protocol code KB 22/2012; date of approval Jan 17, 2012).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgments
Authors are thankful to Professor Robert Sitnik for his remarks after reading the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Wall, B.F.; Hart, D. Revised radiation doses for typical X-ray examinations. Report on a recent review of doses to patients from medical X-ray examinations in the UK by NRPB. National Radiological Protection Board. Br. J. Radiol. 1997, 70, 437–439. [Google Scholar] [CrossRef] [PubMed]
- Larson, A.N.; Schueler, B.A.; Dubousset, J. Radiation in Spine Deformity: State-of-the-Art Reviews. Spine Deform. 2019, 7, 386–394. [Google Scholar] [CrossRef] [PubMed]
- Nash, C.L., Jr.; Gregg, E.C.; Brown, R.H.; Pillai, K. Risks of exposure to X-rays in patients undergoing long-term treatment for scoliosis. J. Bone Jt. Surg. Am. Vol. 1979, 61, 371–374. [Google Scholar] [CrossRef]
- Ronckers, C.M.; Land, C.E.; Miller, J.S.; Stovall, M.; Lonstein, J.E.; Doody, M.M. Cancer mortality among women frequently exposed to radiographic examinations for spinal disorders. Radiat. Res. 2010, 174, 83–90. [Google Scholar] [CrossRef]
- Ronckers, C.M.; Doody, M.M.; Lonstein, J.E.; Stovall, M.; Land, C.E. Multiple diagnostic X-rays for spine deformities and risk of breast cancer. Cancer Epidemiol. Biomark. Prev. 2008, 17, 605–613. [Google Scholar] [CrossRef]
- Ardran, G.M.; Coates, R.; Dickson, R.A.; Dixon-Brown, A.; Harding, F.M. Assessment of scoliosis in children: Low dose radiographic technique. Br. J. Radiol. 1980, 53, 146–147. [Google Scholar] [CrossRef]
- Simony, A.; Hansen, E.J.; Christensen, S.B.; Carreon, L.Y.; Andersen, M.O. Incidence of cancer in adolescent idiopathic scoliosis patients treated 25 years previously. Eur. Spine J. 2016, 25, 3366–3370. [Google Scholar] [CrossRef]
- Novosad, J.; Eng, B.; Cheriet, F.; Delorme, S.; Poirier, S.; Beausejour, M.; Labelle, H. Self-calibration of biplanar radiographs for a retrospective comparative study of the 3D correction of adolescent idiopathic scoliosis. Stud. Health Technol. Inform. 2002, 91, 272–275. [Google Scholar]
- Legaye, J.; Saunier, P.; Dumas, R.; Vallee, C. Correction for patient sway in radiographic biplanar imaging for three-dimensional reconstruction of the spine: In vitro study of a new method. Acta Radiol. 2009, 50, 781–790. [Google Scholar] [CrossRef] [PubMed]
- Ilharreborde, B.; Steffen, J.S.; Nectoux, E.; Vital, J.M.; Mazda, K.; Skalli, W.; Obeid, I. Angle measurement reproducibility using EOS three-dimensional reconstructions in adolescent idiopathic scoliosis treated by posterior instrumentation. Spine 2011, 36, E1306–E1313. [Google Scholar] [CrossRef] [PubMed]
- Glaser, D.A.; Doan, J.; Newton, P.O. Comparison of 3-dimensional spinal reconstruction accuracy: Biplanar radiographs with EOS versus computed tomography. Spine 2012, 37, 1391–1397. [Google Scholar] [CrossRef] [PubMed]
- Ilharreborde, B.; Dubousset, J.; Skalli, W.; Mazda, K. Spinal penetration index assessment in adolescent idiopathic scoliosis using EOS low-dose biplanar stereoradiography. Eur. Spine J. 2013, 22, 2438–2444. [Google Scholar] [CrossRef] [PubMed]
- Courvoisier, A.; Drevelle, X.; Vialle, R.; Dubousset, J.; Skalli, W. 3D analysis of brace treatment in idiopathic scoliosis. Eur. Spine J. 2013, 22, 2449–2455. [Google Scholar] [CrossRef] [PubMed]
- Ilharreborde, B.; Vidal, C.; Skalli, W.; Mazda, K. Sagittal alignment of the cervical spine in adolescent idiopathic scoliosis treated by posteromedial translation. Eur. Spine J. 2013, 22, 330–337. [Google Scholar] [CrossRef][Green Version]
- Amzallag-Bellenger, E.; Uyttenhove, F.; Nectoux, E.; Moraux, A.; Bigot, J.; Herbaux, B.; Boutry, N. Idiopathic scoliosis in children and adolescents: Assessment with a biplanar X-ray device. Insights Imaging 2014, 5, 571–583. [Google Scholar] [CrossRef]
- Ilharreborde, B.; Ferrero, E.; Alison, M.; Mazda, K. EOS microdose protocol for the radiological follow-up of adolescent idiopathic scoliosis. Eur. Spine J. 2016, 25, 526–531. [Google Scholar] [CrossRef]
- Dubousset, J.; Charpak, G.; Dorion, I.; Skalli, W.; Lavaste, F.; Deguise, J.; Kalifa, G.; Ferey, S. A new 2D and 3D imaging approach to musculoskeletal physiology and pathology with low-dose radiation and the standing position: The EOS system. Bull. Acad. Natl. Med. 2005, 189, 287–297, discussion 297–300. [Google Scholar]
- Hoan, N.N.; Majewski, S.; Charpak, G.; Policarpo, A.J. An efficient, gaseous detector with good low-energy resolution for (less than or equal to 50 keV) imaging. J. Nucl. Med. 1979, 20, 335–340. [Google Scholar]
- Ng, S.Y.; Bettany-Saltikov, J. Imaging in the Diagnosis and Monitoring of Children with Idiopathic Scoliosis. Open Orthop. J. 2017, 11, 1500–1520. [Google Scholar] [CrossRef]
- Pedersen, P.H.; Vergari, C.; Alzakri, A.; Vialle, R.; Skalli, W. A reduced micro-dose protocol for 3D reconstruction of the spine in children with scoliosis: Results of a phantom-based and clinically validated study using stereo-radiography. Eur. Radiol. 2019, 29, 1874–1881. [Google Scholar] [CrossRef]
- Hui, S.C.; Pialasse, J.P.; Wong, J.Y.; Lam, T.P.; Ng, B.K.; Cheng, J.C.; Chu, W.C. Radiation dose of digital radiography (DR) versus micro-dose X-ray (EOS) on patients with adolescent idiopathic scoliosis: 2016 SOSORT-IRSSD “John Sevastic Award” Winner in Imaging Research. Scoliosis Spinal Disord. 2016, 11, 46. [Google Scholar] [CrossRef] [PubMed]
- Luo, T.D.; Stans, A.A.; Schueler, B.A.; Larson, A.N. Cumulative Radiation Exposure With EOS Imaging Compared With Standard Spine Radiographs. Spine Deform. 2015, 3, 144–150. [Google Scholar] [CrossRef]
- McKenna, C.; Wade, R.; Faria, R.; Yang, H.; Stirk, L.; Gummerson, N.; Sculpher, M.; Woolacott, N. EOS 2D/3D X-ray imaging system: A systematic review and economic evaluation. Health Technol. Assess. 2012, 16, 1–188. [Google Scholar] [CrossRef] [PubMed]
- Brink, R.C.; Wijdicks, S.P.J.; Tromp, I.N.; Schlosser, T.P.C.; Kruyt, M.C.; Beek, F.J.A.; Castelein, R.M. A reliability and validity study for different coronal angles using ultrasound imaging in adolescent idiopathic scoliosis. Spine J. 2018, 18, 979–985. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, O.; Lombaert, H.; Parent, S.; Labelle, H.; Cheriet, F. Spectral Shape Analysis of Human Torsos: Application to the Evaluation of Scoliosis Surgery Outcome. IEEE J. Biomed. Health Inform. 2018, 22, 1552–1560. [Google Scholar] [CrossRef]
- Melhem, E.; Assi, A.; El Rachkidi, R.; Ghanem, I. EOS((R)) biplanar X-ray imaging: Concept, developments, benefits, and limitations. J. Child. Orthop. 2016, 10, 1–14. [Google Scholar] [CrossRef]
- Assi, K.C.; Grenier, S.; Parent, S.; Labelle, H.; Cheriet, F. A physically based trunk soft tissue modeling for scoliosis surgery planning systems. Comput. Med Imaging Graph. 2015, 40, 217–228. [Google Scholar] [CrossRef][Green Version]
- Mahboub-Ahari, A.; Hajebrahimi, S.; Yusefi, M.; Velayati, A. EOS imaging versus current radiography: A health technology assessment study. Med J. Islamic Repub. Iran 2016, 30, 331. [Google Scholar]
- Duong, L.; Cheriet, F.; Labelle, H. Automatic detection of scoliotic curves in posteroanterior radiographs. IEEE Trans. Biomed. Eng. 2010, 57, 1143–1151. [Google Scholar] [CrossRef]
- Rigo, M.D.; Villagrasa, M.; Gallo, D. A specific scoliosis classification correlating with brace treatment: Description and reliability. Scoliosis 2010, 5, 1. [Google Scholar] [CrossRef]
- Michonski, J.; Glinkowski, W.; Witkowski, M.; Sitnik, R. Automatic recognition of surface landmarks of anatomical structures of back and posture. J. Biomed. Opt. 2012, 17, 056015. [Google Scholar] [CrossRef] [PubMed]
- Glinkowski, W.M.; Tomasik, P.; Walesiak, K.; Gluszak, M.; Krawczak, K.; Michonski, J.; Czyzewska, A.; Zukowska, A.; Sitnik, R.; Wielgos, M. Posture and low back pain during pregnancy-3D study. Ginekol. Pol. 2016, 87, 575–580. [Google Scholar] [CrossRef] [PubMed]
- Michonski, J.; Walesiak, K.; Pakula, A.; Glinkowski, W.; Sitnik, R. Monitoring of spine curvatures and posture during pregnancy using surface topography-case study and suggestion of method. Scoliosis Spinal Disord. 2016, 11, 31. [Google Scholar] [CrossRef] [PubMed]
- Firth, N.C.; Brown, N.; Blagg, J. Plane of best fit: A novel method to characterize the three-dimensionality of molecules. J. Chem. Inf. Modeling 2012, 52, 2516–2525. [Google Scholar] [CrossRef]
- Shannon, T.M. Development of an apparatus to evaluate Adolescent Idiopathic Scoliosis by dynamic surface topography. Stud. Health Technol. Inform. 2008, 140, 121–127. [Google Scholar]
- Berryman, F.; Pynsent, P.; Fairbank, J.; Disney, S. A new system for measuring three-dimensional back shape in scoliosis. Eur. Spine J. 2008, 17, 663–672. [Google Scholar] [CrossRef]
- Drerup, B. Rasterstereographic measurement of scoliotic deformity. Scoliosis 2014, 9, 22. [Google Scholar] [CrossRef]
- Patias, P.; Grivas, T.B.; Kaspiris, A.; Aggouris, C.; Drakoutos, E. A review of the trunk surface metrics used as Scoliosis and other deformities evaluation indices. Scoliosis 2010, 5, 12. [Google Scholar] [CrossRef]
- Drerup, B.; Hierholzer, E. Automatic localization of anatomical landmarks on the back surface and construction of a body-fixed coordinate system. J. Biomech. 1987, 20, 961–970. [Google Scholar] [CrossRef]
- Barsky, B.A.; Bartels, R.H.; Beatty, J.C. An Introduction to Splines for Use in Computer Graphics and Geometric Modeling. Available online: https://books.google.pl/books?hl=en&lr=&id=9bQ0f8sYqaAC&oi=fnd&pg=PA1&dq=Bartels,+R.H.%3B+Beatty,+J.C.%3B+Barsky,+B.A.:+An+Introduction+to+Splines+for+Use+in+Computer+Graphics+%26+Geometric+Modeling.+Morgan+Kaufmann+Publishers+1987.&ots=yEiSx4797R&sig=d5EPvK6pgAaLFRWWAZPmmtxrrQE&redir_esc=y#v=onepage&q&f=false (accessed on 20 November 2020).
- The Visualization Toolkit Open Source Project on Open HUB, Online. Available online: https://www.openhub.net/p/vtk (accessed on 20 November 2020).
- Lotfi, N.; Chauhan, G.S.; Gardner, A.; Berryman, F.; Pynsent, P. The relationship between measures of spinal deformity and measures of thoracic trunk rotation. J. Spine Surg. 2020, 6, 555–561. [Google Scholar] [CrossRef]
- Ghaneei, M.; Komeili, A.; Li, Y.; Parent, E.C.; Adeeb, S. 3D Markerless asymmetry analysis in the management of adolescent idiopathic scoliosis. BMC Musculoskelet. Disord. 2018, 19, 385. [Google Scholar] [CrossRef] [PubMed]
- Knott, P.; Sturm, P.; Lonner, B.; Cahill, P.; Betsch, M.; McCarthy, R.; Kelly, M.; Lenke, L.; Betz, R. Multicenter Comparison of 3D Spinal Measurements Using Surface Topography With Those From Conventional Radiography. Spine Deform. 2016, 4, 98–103. [Google Scholar] [CrossRef] [PubMed]
- Komeili, A.; Westover, L.; Parent, E.C.; El-Rich, M.; Adeeb, S. Monitoring for idiopathic scoliosis curve progression using surface topography asymmetry analysis of the torso in adolescents. Spine J. 2015, 15, 743–751. [Google Scholar] [CrossRef] [PubMed]
- Fortin, C.; Feldman, D.E.; Cheriet, F.; Labelle, H. Validity of a quantitative clinical measurement tool of trunk posture in idiopathic scoliosis. Spine 2010, 35, E988–E994. [Google Scholar] [CrossRef]
- Parent, E.C.; Damaraju, S.; Hill, D.L.; Lou, E.; Smetaniuk, D. Identifying the best surface topography parameters for detecting idiopathic scoliosis curve progression. Stud. Health Technol. Inform. 2010, 158, 78–82. [Google Scholar]
- Kotwicki, T.; Negrini, S.; Grivas, T.B.; Rigo, M.; Maruyama, T.; Durmala, J.; Zaina, F.; Members of the international Society on Scoliosis, O.; Rehabilitation, T. Methodology of evaluation of morphology of the spine and the trunk in idiopathic scoliosis and other spinal deformities-6th SOSORT consensus paper. Scoliosis 2009, 4, 26. [Google Scholar] [CrossRef]
- Goldberg, C.J.; Grove, D.; Moore, D.P.; Fogarty, E.E.; Dowling, F.E. Surface topography and vectors: A new measure for the three dimensional quantification of scoliotic deformity. Stud. Health Technol. Inform. 2006, 123, 449–455. [Google Scholar]
- Goldberg, C.J.; Kaliszer, M.; Moore, D.P.; Fogarty, E.E.; Dowling, F.E. Surface topography, Cobb angles, and cosmetic change in scoliosis. Spine 2001, 26, E55–E63. [Google Scholar] [CrossRef]
- Ono, T. Trunk deformity in scoliosis studied by surface measurement. Nihon Seikeigeka Gakkai Zasshi 1995, 69, 915–926. [Google Scholar]
- Dawson, E.G.; Kropf, M.A.; Purcell, G.; Kabo, J.M.; Kanim, L.E.; Burt, C. Optoelectronic evaluation of trunk deformity in scoliosis. Spine 1993, 18, 326–331. [Google Scholar] [CrossRef]
- Glinkowski, W.; Michonski, J.; Glinkowska, B.; Zukowska, A.; Sitnik, R.; Gorecki, A. Telediagnostic 3D school screening of back curvatures and posture using structured light method-pilot study. Stud. Health Technol. Inform. 2012, 176, 291–294. [Google Scholar] [PubMed]
- Takasaki, H. Moire topography. Appl. Opt. 1970, 9, 1467–1472. [Google Scholar] [CrossRef] [PubMed]
- Buendia, M.; Salvador, R.; Cibrian, R.; Laguia, M.; Sotoca, J.M. Determination of the object surface function by structured light: Application to the study of spinal deformities. Phys. Med. Biol. 1999, 44, 75–86. [Google Scholar] [CrossRef] [PubMed]
- Sitnik, R. Four-dimensional measurement by a single-frame structured light method. Appl. Opt. 2009, 48, 3344–3354. [Google Scholar] [CrossRef]
- Drerup, B. The measurement of the kyphotic angle by contact free registration of back-shape (author’s transl). Zeitschrift fur Orthopadie und ihre Grenzgebiete 1982, 120, 64–70. [Google Scholar] [CrossRef]
- Andonian, A.T. Detection of stimulated back muscle contractions by moire topography. J. Biomech. 1984, 17, 653–661. [Google Scholar] [CrossRef]
- Horst, M.; Albrecht, D.; Drerup, B. Objective determination of the shape of the anterior chest wall using moire topography. Method and development of dimension-free indices for the evaluation of funnel chest. Zeitschrift fur Orthopadie und ihre Grenzgebiete 1985, 123, 357–364. [Google Scholar] [CrossRef]
- Ashizawa, K.; Kuki, T.; Kusumoto, A.; Tsutsumi, E.; Kato, S. Approximate surface development of the left side half-trunk by a free-formed model. Am. J. Phys. Anthropol. 1988, 76, 165–173. [Google Scholar] [CrossRef]
- Stokes, I.A.; Moreland, M.S. Concordance of back surface asymmetry and spine shape in idiopathic scoliosis. Spine 1989, 14, 73–78. [Google Scholar] [CrossRef]
- Batouche, M.; Benlamri, R.; Kholladi, M.K. A computer vision system for diagnosing scoliosis using moire images. Comput. Biol. Med. 1996, 26, 339–353. [Google Scholar] [CrossRef]
- Wong, H.K.; Balasubramaniam, P.; Rajan, U.; Chng, S.Y. Direct spinal curvature digitization in scoliosis screening--a comparative study with Moire contourgraphy. J. Spinal Disord. 1997, 10, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.C.; Thometz, J.G.; Lyon, R.M.; McGrady, L. Effects of trunk position on back surface-contour measured by raster stereophotography. Am. J. Orthop. 2002, 31, 402–406. [Google Scholar] [PubMed]
- Hill, D.L.; Berg, D.C.; Raso, V.J.; Lou, E.; Durdle, N.G.; Mahood, J.K.; Moreau, M.J. Evaluation of a laser scanner for surface topography. Stud. Health Technol. Inform. 2002, 88, 90–94. [Google Scholar] [PubMed]
- Jacobi, U.; Chen, M.; Frankowski, G.; Sinkgraven, R.; Hund, M.; Rzany, B.; Sterry, W.; Lademann, J. In vivo determination of skin surface topography using an optical 3D device. Skin Res. Technol. 2004, 10, 207–214. [Google Scholar] [CrossRef] [PubMed]
- Minguez, M.F.; Buendia, M.; Cibrian, R.M.; Salvador, R.; Laguia, M.; Martin, A.; Gomar, F. Quantifier variables of the back surface deformity obtained with a noninvasive structured light method: Evaluation of their usefulness in idiopathic scoliosis diagnosis. Eur. Spine J. 2007, 16, 73–82. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zubovic, A.; Davies, N.; Berryman, F.; Pynsent, P.; Quraishi, N.; Lavy, C.; Bowden, G.; Wilson-Macdonald, J.; Fairbank, J. New method of Scoliosis Deformity Assessment: ISIS2 System. Stud. Health Technol. Inform. 2008, 140, 157–160. [Google Scholar] [CrossRef]
- Ghaneei, M.; Ekyalimpa, R.; Westover, L.; Parent, E.C.; Adeeb, S. Customized k-nearest neighbourhood analysis in the management of adolescent idiopathic scoliosis using 3D markerless asymmetry analysis. Comput. Methods Biomech. Biomed. Eng. 2019, 1–10. [Google Scholar] [CrossRef]
- Komeili, A.; Westover, L.; Parent, E.C.; El-Rich, M.; Adeeb, S. Correlation Between a Novel Surface Topography Asymmetry Analysis and Radiographic Data in Scoliosis. Spine Deform. 2015, 3, 303–311. [Google Scholar] [CrossRef]
- Komeili, A.; Westover, L.M.; Parent, E.C.; Moreau, M.; El-Rich, M.; Adeeb, S. Surface topography asymmetry maps categorizing external deformity in scoliosis. Spine J. 2014, 14, 973–983 e972. [Google Scholar] [CrossRef]
- Glinkowski, W.; Sitnik, R.; Witkowski, M.; Kocon, H.; Bolewicki, P.; Gorecki, A. Method of pectus excavatum measurement based on structured light technique. J Biomed Opt 2009, 14, 044041. [Google Scholar] [CrossRef]
- Newton, P.O.; Osborn, E.J.; Bastrom, T.P.; Doan, J.D.; Reighard, F.G. The 3D Sagittal Profile of Thoracic Versus Lumbar Major Curves in Adolescent Idiopathic Scoliosis. Spine Deform. 2019, 7, 60–65. [Google Scholar] [CrossRef] [PubMed]
- Boice, J.D., Jr. Carcinogenesis—A synopsis of human experience with external exposure in medicine. Health Phys. 1988, 55, 621–630. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, D.A.; Lonstein, J.E.; Morin, M.M.; Visscher, W.; Harris, B.S., 3rd; Boice, J.D., Jr. Breast cancer in women with scoliosis exposed to multiple diagnostic x rays. J. Natl. Cancer Inst. 1989, 81, 1307–1312. [Google Scholar] [CrossRef] [PubMed]
- Boice, J.D., Jr. Radiation and breast carcinogenesis. Med Pediatric Oncol. 2001, 36, 508–513. [Google Scholar] [CrossRef]
- Kim, H.S.; Ishikawa, S.; Ohtsuka, Y.; Shimizu, H.; Shinomiya, T.; Viergever, M.A. Automatic scoliosis detection based on local centroids evaluation on moire topographic images of human backs. IEEE Trans. Med. Imaging 2001, 20, 1314–1320. [Google Scholar] [CrossRef]
- Stokes, I.A. Three-dimensional terminology of spinal deformity. A report presented to the Scoliosis Research Society by the Scoliosis Research Society Working Group on 3-D terminology of spinal deformity. Spine 1994, 19, 236–248. [Google Scholar] [CrossRef]
- Berryman, F.; Pynsent, P.; Fairbank, J. Measuring the rib hump in scoliosis with ISIS2. Stud. Health Technol. Inform. 2008, 140, 65–67. [Google Scholar]
- McArdle, F.J.; Griffiths, C.J.; Macdonald, A.M.; Gibson, M.J. Monitoring the thoracic sagittal curvature in kyphoscoliosis with surface topography: A trend analysis of 57 patients. Stud. Health Technol. Inform. 2002, 91, 199–203. [Google Scholar]
- Klos, S.S.; Liu, X.C.; Lyon, R.M.; Tassone, J.C.; Thometz, J.G. Reliability of a functional classification system in the monitoring of patients with idiopathic scoliosis. Spine 2007, 32, 1662–1666. [Google Scholar] [CrossRef]
- Betsch, M.; Wild, M.; Rath, B.; Tingart, M.; Schulze, A.; Quack, V. Radiation-free diagnosis of scoliosis: An overview of the surface and spine topography. Orthopade 2015, 44, 845–851. [Google Scholar] [CrossRef]
- Lenke, L.G.; Edwards, C.C., 2nd; Bridwell, K.H. The Lenke classification of adolescent idiopathic scoliosis: How it organizes curve patterns as a template to perform selective fusions of the spine. Spine 2003, 28, S199–S207. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).