Abstract
There is evidence of a relationship between motor and cognitive development. The literature has shown that of all the motor skills, fine motor skills are those that contribute most to mathematical performance in preschool children. As this is a sensitive period in the development of motor skills, low levels of physical activity in this period can compromise their development and contribute to weight gain and obesity. The aim of this study was therefore to analyze the relationship between mathematical and motor skills, physical activity levels, and obesity. The sample consisted of 62 preschool children (32 males) with an average age of 4.63 ± 0.81. The Weschler preschool and primary scale of intelligence—revised arithmetic test was used to assess mathematical skills. The tests to assess fine motor skills were the “Adapted Threading Beads Test” and the “Adapted Visuomotor Integration Test”. The movement assessment battery for children-2, band 1, “Aiming & Catching”, and “Balance” tests were used to assess gross motor skills. Levels of physical activity were assessed using the “Preschool-age physical activity questionnaire” and obesity using the body mass index. The results indicated that only the fine motor skills of visuomotor integration were included in the multiple linear regression model (F < 0.001; r = 0.464; R2 = 0.215; p < 0.001), with the exclusion of gross motor skills, physical activity levels, and obesity levels. Thus, it was concluded that mathematical skills were only directly and significantly influenced by visuomotor integration. However, visuomotor integration was positively and significantly associated with gross motor skills (r = 0.269; p < 0.05) and not with levels of physical activity and obesity. Thus, gross motor skills could contribute to improving visuomotor integration directly and consequently mathematical skills indirectly. The results of this study suggest that the implementation of structured physical activity programs can contribute to mathematical performance.
1. Introduction
The early childhood period is a critical phase in the physical, cognitive, social, and emotional development of a child [1]. During this period, there is a significant and intense reorganization of the central nervous system [2,3,4], which is strongly influenced by the child’s environmental context [3,5]. It is a time of great opportunities but also of significant vulnerability to negative influences [2].
During this period, the majority of a child’s time is spent in family and educational environments [6,7]. Therefore, in addition to the family, schools have the responsibility to promote the holistic development of children in their early school years [6,7,8].
The literature has shown that in early childhood, a child’s physical, cognitive, social, and emotional development is influenced by motor development [9,10,11]. It is during this period, before the age of six, that significant motor skill development occurs [12,13].
From a developmental system’s perspective, children’s motor skills are influenced by the complex interplay of biological, social, and environmental factors [14,15]. As a result, there are various theories of development, and numerous authors have explored the relationships between cognitive and motor development [16].
Currently, there is a clear connection between the brain areas involved in motor skills (primarily the cerebellum) and cognitive skills (primarily the prefrontal cortex) [17,18,19]. The development of both skills occurs simultaneously and rapidly in the early years of life [18,20,21]. In this regard, motor skills acquired early in life are related to cognitive abilities from childhood [22] to adulthood [10,23].
Recent studies have shown that motor skills influence academic performance in the early years [24,25,26,27,28,29,30,31] and are described as one of the criteria for school readiness [32]. However, motor skills do not develop naturally, they need to be learned, practiced, and assimilated [33,34,35]. Therefore, in early childhood, there appears to be a close relationship between motor skill development and physical activity (PA) [36,37]. A more active child may have better motor skills [31,38,39,40], with a reduced risk of obesity [36,41,42]. On the other hand, the presence of obesity contributes to physical inactivity and consequently may lead to underdeveloped motor skills [36,43,44]. In this sense, well-developed motor skills in early childhood facilitate children’s engagement in PA [36,45,46,47,48,49] and, as a result, contribute to the prevention of obesity [36,42].
Motor skills refer to the underlying internal pathways responsible for moving the body through space, as well as the cognitive processes that give rise to these movements [50,51]. Traditionally, they are categorized into two main groups (Figure 1): gross motor skills (GMSs) and fine motor skills (FMSs) [52,53,54,55,56].
GMSs primarily involve movements generated by large muscle groups. They encompass locomotor skills, which entail body movements in space (such as walking, running, jumping, and sliding), postural or balance skills, which relate to the ability to maintain a controlled position or posture during a task (dynamic balance—maintaining position during activities that involve movement; or static balance—maintaining position in stationary tasks), and manipulative skills used to control objects through actions with hands or feet (e.g., grasping, striking, absorbing, lifting, etc.). These manipulative skills can be categorized as either propulsive (sending objects) or receptive (receiving objects) [57,58,59,60,61].
FMSs are characterized by movements performed by small muscle groups. The literature often subdivides fine motor skills into two categories. One is fine motor coordination (FMC), related to eye–hand coordination, also known as non-graphomotor ability, which involves manual dexterity, speed, and precision in tasks such as inserting, moving, and handling small objects with the fingers [62,63].
Another category of fine motor skills is visual–motor integration, known as visuomotor integration (VMI) or visuospatial integration, which relates to the organization of small hand and finger movements through the processing of visual and spatial stimuli, with a strong emphasis on synchronized movements between the hand and the eye. These tasks typically include activities like writing, drawing, copying shapes, letters, or other visual stimuli and can be referred to as graphomotor skills [62,63].
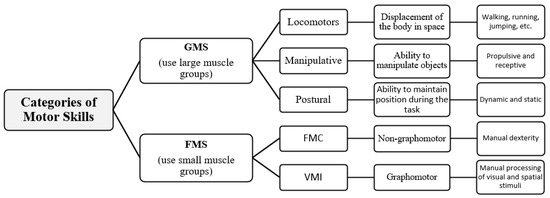
Figure 1.
Summary of motor skills categories (adapted from Flores et al. [64]).
Since the development of motor skills in early childhood contributes to a greater involvement of children in the practice of PA, it is important to characterize and classify this concept.
PA is characterized by all voluntary bodily movements performed by skeletal muscles that require energy expenditure [65]. PA can be classified into structured PA (formal PA conducted under the guidance and direct instruction of an expert) and unstructured PA (informal PA performed spontaneously and freely by children through play activities). Structured PA aims to improve motor skills or specific physical fitness, while unstructured PA is more associated with recreational activities [66].
Regarding the frequency and intensity of PA, the World Health Organization (WHO) recommends that preschool children engage in at least 180 min of PA per day, of which 60 min should be of moderate to vigorous intensity (MVPA) [67].
Prolonged periods of low PA in children can lead to weight gain [67,68,69]. The primary mechanism leading to weight gain is an imbalance between energy consumption and energy expenditure [70].
The WHO [71] defines obesity as the abnormal or excessive accumulation of body fat that poses a risk to an individual’s health. Fat accumulation results from increased energy intake exceeding the energy expenditure, leading to a positive energy balance [72]. Energy consumption can be explained using the metabolic equivalent (MET). One MET (4.2 KJ) corresponds to 1 Kcal/kg body weight/hour, which is approximately equal to the resting metabolic rate [73]. When sitting (sedentary PA-SPA), only 1 to 1.5 METs are used; light PA (LPA) consumes between 1.5 and 3 METs; moderate PA consumes 3 to 6 METs; and vigorous PA consumes more than 6 METs [73,74]. In this context, low levels of PA are associated with obesity development in children and adolescents [75].
The literature has demonstrated the effects of motor skills and PA on cognitive and academic skills, showing a positive relationship between these skills in preschoolers [31,76,77,78,79,80,81]. On the other hand, it has been shown that obesity can compromise children’s participation in PA and negatively influence motor skills [36,43,44] and cognitive skills [82]. In this regard, early childhood motor skills can be the foundation for a more active lifestyle [83,84], as studies have demonstrated a positive association between motor skills and higher levels of PA [40,83,85], resulting in reduced obesity [36,42]. Therefore, higher levels of PA in early childhood are positively associated with many aspects of health, such as reduced obesity [86,87], development of motor skills [40,83,85], and cognitive skills [88,89,90].
Cognitive and academic skill performance primarily emphasizes two curriculum areas, literacy and mathematical performance [91,92]. These two areas are considered prerequisites for success in other disciplines and consequently for academic success [93]. Mathematics plays a prominent role in the school curriculum, and its development is considered a fundamental cognitive attribute. Successful early mathematical learning not only provides a structure for future learning [94] but also serves as an indicator of future academic and professional success [95].
Although the literature is more consistent in supporting a greater influence of FMSs on mathematical performance [29,64,96], some studies support positive and significant associations of GMSs on mathematical performance in preschool children [22,26,97]. In addition to motor skills, there is strong evidence that PA in young children is positively related to cognitive development [98] and specifically mathematical performance [99,100]. On the other hand, it seems that increased obesity leads to decreased PA [36,41], which contributes to a decrease in GMSs [38,39,40,101,102].
In view of the above, given that preschool age is a sensitive period for the development of motor skills and that low levels of PA in this period can compromise their development and contribute to weight gain and obesity, the following objectives were outlined: (1) to analyze the prevalence of difficulties shown by the children in mathematical skills, motor skills, compliance with weekly PA recommendations, and obesity levels, comparing the results with those in the literature, with the aim of justifying the fit or bias of the study variables; (2) to study the associations between all the variables with the aim of analyzing the direct relationships between them; (3) to analyze the direct influence of motor skills, PA levels, and obesity on mathematical skills.
2. Materials and Methods
2.1. Sample
All 115 children attending the preschool at the Vilela School Cluster (Paredes, Porto, Portugal) were invited to participate in the study. However, 5 children were excluded because they were unable to complete the assessments, and another 5 were excluded because they were born prematurely. Typically, among such children, the most common issues are related to both FMSs and GMSs [103,104], which negatively impact their academic performance [105,106].
Of the remaining 105 eligible children, 12 were absent for the FMS assessment, 7 were absent for the math skills assessment, 2 were absent for both assessments, 4 were part of a pilot study (preliminary validation of motor tests for assessing FMS), 10 children did not submit the questionnaire to assess their levels of PA, and 12 children had incomplete or improperly filled-out questionnaires. Thus, the final sample consisted of 62 children (32 males), with an average age of 4.63 ± 0.81 years, distributed across 5 classes (JIV1 to JIV5). In terms of age distribution, the 5-year-old age range predominated (33 children) (Table 1).

Table 1.
Students’ number distribution by age group, means and standard deviations.
2.2. Instruments
2.2.1. Diagnosis of Math Skills
The Weschler preschool and primary scale of intelligence—revised (WPPSI-R) [107] was revised and adapted for the Portuguese population [108], and given the objectives and characteristics of the study, it was the most appropriate scale and therefore the one used to diagnose mathematical skills. Given the scarcity of instruments for assessing math skills in preschool children in our country, this scale was chosen because it has been validated for the population in question, is the most widely used in national research at this level, does not require much training, and is easy to apply [108].
The WPPSI-R consists of two subtests, the achievement and the verbal. For this study, only the arithmetic test from the verbal subtest was used. This test assesses quantitative concepts, counting and problems, which are presented orally to the child. This test has 23 items divided into 3 parts: (i) quantitative skills, picture items (items 1 to 7); (ii) numerical skills, counting items (items 8 to 11); (iii) problem-solving skills, verbal items (items 12 to 23). The test should start at item 1. Although there is no time limit for the child to respond, after 15 s for items 1 to 11 and 30 s for items 12 to 23, a score of zero should be given, and the test should move on to the next item. One point should be awarded for each correct response (maximum score of 23 points), and the test should be stopped after 5 failures. Raw scores are converted into standardized scores, yielding a profile. Standardized scores range from 1 to 19, with a mean value of 10 and a standard deviation of 3 [107,108]. The classification assigned to the test based on standardized scores is as follows: 1–4, very inferior; 5–7, inferior; 8–12, average; 13–16, superior; 17–19, very superior.
2.2.2. Diagnosis of Fine Motor Skills
To assess FMSs, two tests were used. To exclusively evaluate FMC, the adapted threading beads test (TBT-AD) was employed, and to assess visuomotor integration (VMI), the adapted visuomotor integration test (VMI-AD) was used [109]. These two tests were adapted to allow educators to assess FMSs by simultaneously administering them to the entire class, their students, in a classroom setting, within a short time frame, using minimal materials, and with straightforward interpretation of the results obtained from the administration [109].
- Adapted Threading Beads Test (TBT-AD)
This test was adapted from the threading beads test in band 1 of the movement assessment battery for children-2 (MABC-2) [110] to allow it to be administered simultaneously in the classroom by educators to preschool pupils [109]. To this end, adaptations were made to the materials used and the application procedures. The main adaptation concerned the administration procedures, since the original test was only designed for the individual assessment of children [110]. In this way, the time spent on the assessment depends on the number of children being assessed, and when educators administer the test individually, they focus their attention on the child being assessed and may neglect others. Thus, the original test quantifies the time (in seconds) it takes to string a total of cubes on a string (6 cubes for 3- and 4-year-olds and 12 cubes for 5- and 6-year-olds) [110], while the adapted test quantifies the number of cubes strung on the string within specific time periods for each age group [109]. Thus, the following times have been proposed for TBT-AD according to age (years:months): 3:0–3:5, 26 s; 3:6–3:11, 23 s; 4:0–4:5, 21 s; 4:6–4:11, 17 s; 5 to 6:11, 24 s [109]. Based on the number of cubes strung on the string, a cut-off point was proposed to identify children without FMC disorders. Children aged 3:0–4:11 should thread at least 2 cubes, with the exception of children aged 4:0–4:5, who should thread 3 cubes. Children aged 5:0–5:11 must stick at least 5 cubes, and children aged 6:0–6:11 must stick at least 6 cubes [109]. However, depending on the age of the child and the number of cubes strung, a classification has been proposed for FVC: 0—severe disorder; 1—moderate disorder; 2—average; 3—good; 4—very good [109]. The degree of reliability of TBT-AD was analyzed using the intra-observer test–retest method, using intraclass correlation coefficients (ICCs) to assess its temporal stability. When the classroom group was assessed simultaneously, it obtained an ICC of 0.957 and individually an ICC of 0.924. This result indicates that TBT-AD has an excellent level of reliability, which allows it to be used for simultaneous administration in classroom groups, since its results remained stable in all evaluations, both group and individual [109]. With regard to predictive criterion validity, although TBT-AD was valid for explaining the results of the WPPSI-R arithmetic test (F = 6.949; p = 0.010; R2 = 7.8%), its correlation with this test was low (r = 0.280) [109].
- Adapted Visuomotor Integration Test (VMI-AD)
This test was adapted from the reduced version of the Beery-Buktenica developmental test of visuomotor integration (VMI), which is suitable for preschool children [111]. Like the original test, the aim of the adapted visuomotor integration test (VMI-AD) is to accurately copy 15 geometric shapes. The main adaptation is related to the number of sheets used to administer the test, i.e., the original test consists of 7 sheets [111] and the VMI-AD test uses just one A4 sheet folded in half lengthways to form 4 pages, where the first page presents the test instructions and the following pages, 2, 3 and 4, present the 15 figures to copy (5 figures per page) [109]. The test lasts approximately 10 min; however, if a child has not completed it, the examiner should allow them to finish. One point is awarded for each shape copied correctly, for a total of 15 points. If the child fails to copy three consecutive shapes, the grading must end. In this regard, based on the standard score obtained, a performance profile was assigned: 40–67 points, very low; 68–82, low; 83–117, average; 118–132, high; 133–160, very high [111]. Based on the classification, the following points were assigned: zero points for very low performance; 1 point for low performance; 2 points for average performance; 3 points for high performance; 4 points for very high performance.
The degree of reliability of VMI-AD was analyzed using the intra-observer test–retest method with ICCs to assess its temporal stability. When the classroom group was assessed simultaneously, it achieved an ICC of 0.958, and individually, it achieved an ICC of 0.961. This result indicates that VMI-AD exhibits an excellent level of reliability, allowing it to be used for simultaneous classroom group administration, as its results remained stable across all assessments, both in group and individual settings [109]. With regard to predictive criterion validity, VMI-AD was valid for explaining the results of the WPPSI-R arithmetic test (score: F = 15.986; p < 0.001; classification: F = 12.300; p = 0.001), exerting an influence of 16.3% (score: R2 = 0.163) and 13.0% (classification: R2 = 0.130). These values showed a medium effect [112] and the value of the correlations a moderate effect [113].
- Scoring and Classification of Fine Motor Skills
To calculate the score for FMSs, the standard scores of FMC and VMI were summed. To classify FMSs, the classifications of FMC and VMI were also summed, and the mean was calculated, rounded to the nearest decimal place. The following classification was assigned: 0 points, severe impairment; 1 point, moderate impairment; 2 points, average performance; 3 points, good FMSs; 4 points, excellent FMSs.
2.2.3. Diagnosis of Gross Motor Skills
The GMSs were assessed using the MABC-2 [110], justified by the fact that this instrument is the most widely used to identify children with developmental coordination disorder [114,115,116,117]. Additionally, most of children’s learning occurs through manual exploration (manipulative, receptive, and propulsive skills), and balance (static and dynamic) is present in virtually all motor tests and tasks [110], while ball skills involve an important cultural aspect as they are part of children’s games and activities [118].
This instrument is divided into three bands: ages 3 to 6 years (band 1), 7 to 10 years (band 2), and 11 to 16 years (band 3). In this study, band 1 was used, including only the tests that assess manual ball skills (2 tests, aiming and catching) and balance (3 tests, 1 static and 2 dynamic). During the tests, the following behaviors should be recorded in addition to the task scores: “F” if the child does not perform the task correctly; “I” if the task is inappropriate for the child; “R” if the child refuses to perform the task.
The results were recorded on the “Age Range 1 Form (3–6 years)”. To obtain the scores for ball skills, the results of the “Bean Bag Catch and Throw” tests were summed and the respective standard scores, as proposed by the authors [110], were assigned. To obtain the scores for balance skills, the standard scores for unipedal balance (static) (preferred and non-preferred leg) were first summed and divided by 2 (average). Then, the standard scores for the 3 tests (unipedal balance–static, tiptoe walking, and jumping on mats—dynamic balance) were summed, and the respective standard score was assigned. According to the authors of the MABC-2 [110], the motor classification is as follows: red zone (motor disorder), standard score and percentile ≤ 5; yellow zone (risk of motor disorder), standard score between 6 and 7 and percentile between 6 and 15; green zone (no motor disorder), standard score > 7 and percentile ≥ 16.
- Manual Ball Skills (Aiming and Catching)
- Bean Bag Catch (Aiming and Catching 1)
Materials: bean bag and 2 mats; setup: a distance of 1.8 m between the mats. The examiner stands on one mat, and the child stands on the other mat facing the examiner; task: the examiner throws the bean bag to reach the level of the child’s outstretched hands (approximately between the waist and shoulders); trials: 10 attempts. Do not count if the examiner’s throw is poorly executed. If the child fails an attempt, the examiner should correct the error; record: number of attempts correctly executed.
- Throwing the Bean Bag (Aiming and Catching 2)
Materials: bean bag and 2 floor mats (1 is the target); setup: 1.8 m distance between the mats; task: the child stands on the solid-color mat and throws the bean bag, trying to hit any part of the blue mat (the target); trials: 10 attempts. Number of attempts correctly executed without stepping off the mat while throwing noted.
- Balance Skills (Balance)
- Unipedal Balance (Static)
Materials: 1 mat and 1 stopwatch; setup: unobstructed space. Place the mat on the floor; task: the child must remain on one leg with their arms free on the mat for up to 30 s. If balance is maintained for 30 s, a second attempt is not required. No assistance can be given during the test; record: number of seconds, up to 30, that the child maintains balance without moving the supporting foot, touching the ground with the free foot, wrapping the free leg around the supporting leg, or gripping the free leg.
- Tiptoe Walking (Dynamic)
Materials: colored tape; setup: mark a 4.5 m line on the ground with colored tape. The examiner should observe the child’s feet from the side to check if the heels touch the ground during the task; task: start the task with the child’s toe at the beginning of the line. Walk along the line with the heels raised without stepping off the line; trials: 2 attempts. If the child completes 15 steps without any mistakes, a second attempt is not needed. No assistance can be given during the test. Record: record the number of consecutive correct steps (maximum of 15). The child must not land outside the next mat or on the same mat, display an extreme loss of balance upon landing, touch the ground with their hands, or jump more than once on a mat.
- Jumping on Mats (Dynamic)
Materials: 6 floor mats (3 solid-yellow, 2 solid-blue, and 1 target mat); setup: position the six mats side by side in a row, with the long sides touching and the colors alternating; task: the child starts with feet together on the first mat and jumps from mat to mat to the last one; trials: 2 attempts. If the child makes five continuous jumps without errors, a second attempt is not necessary. No assistance can be given during the test. Record: number of consecutive correct jumps (maximum of 5).
2.2.4. Obesity Diagnosis
The body mass index (BMI) was the selected anthropometric indicator for assessing body composition, as it is the most widely used and accepted international predictor as an indirect measure of adiposity in children [119]. To perform this, the following variables needed to be collected: age, sex, height, and weight.
The BMI was calculated according to the formula: weight (kg)/[height (m)]2. The children’s age and sex were provided by the educators based on enrolment records.
Height was measured using a “Seca 213—Precision for health” stadiometer, with the child standing vertically, feet together, and arms extended alongside the body, with the head positioned so that the Frankfurt plane was parallel to the ground [120]. The measurement was recorded to the nearest millimeter (0.1 cm).
To assess weight, a Tanita digital scale (BC-730) was used. These materials were provided by the Instituto Superior de Ciências Educativas do Douro (ISCE Douro, Penafiel, Portugal), and the measurement was recorded to the nearest decigram (0.1 kg). The assessment of weight and height was consistently conducted under the same conditions and with the same equipment. The children were measured and weighed barefoot and wearing as little clothing as possible.
Both the European Childhood Obesity Group [121] and the International Pediatric Association [122] recommend using the cutoff points defined by the WHO for children from 0 to 5 years [123] and those aged 5 to 19 years [124] to standardize protocols and improve the quality of comparisons between different studies for the purpose of enhancing the quality of research and surveillance of the issue.
Thus, for the classification of BMI, percentiles for age were considered according to the criteria and cutoff points defined by the WHO [123,125,126]: underweight, percentile ≤ 5; normal weight, percentile between 5 and 85; pre-obesity, percentile > 85 and < 97; obesity, percentile ≥ 97.
2.2.5. Physical Activity Assessment
To assess the children’s PA levels, the most commonly used objective methods include accelerometers, pedometers, and heart rate monitors. However, the use of these instruments is associated with several issues: the inability to assess aquatic activities, the absence of consensus regarding data cleaning and processing, and accelerometer cutoff points. Additionally, these instruments are relatively expensive for use in large populations [127]. In this context, subjective methods include tools like PA diaries and PA recall questionnaires, which are more practical and economically feasible for researchers to employ in large population studies [128,129].
Therefore, considering the nature and context of this study, the children’s PA level was assessed using the preschool-age physical activity questionnaire (Pre-PAQ) [130], the Portuguese version translated by Sancho [131]. This questionnaire represents a significant contribution for researchers to assess habitual PA and sedentary behavior over 3 days (1 weekday and 2 weekend days) in preschool-aged children [130]. Weekend days were included because activity routines at home tend to differ more on weekends than on weekdays [132,133]). The Pre-PAQ is a reliable and valid measurement tool for assessing various levels of PA in preschool-aged children [130,131,134,135].
The psychometric properties of the Portuguese version of the Pre-PAQ indicate that reliability values range from 0.402 to 0.938, demonstrating acceptable reliability for the translated version [131]. The Portuguese version of the Pre-PAQ [131] consists of 37 questions (Q1 to Q37). Considering the aim of this study, to collect information on children’s sedentary behaviors and PA, only questions Q32, Q36, and Q39 were selected. These questions include a list of typical preschool activities with “Yes” or “No” responses, and if “Yes”, the time the child spent on that activity.
Regarding question Q32, its purpose was to identify whether the child engages in any structured PA (physical education at school, swimming, dancing, soccer, ballet, etc.) inside and/or outside of kindergarten, specifying the activities and the time spent on them. Question Q36, focusing on the previous weekday (Monday to Friday), identified the types of activities the child engaged in, along with the time spent on each. Finally, question Q39, considering the previous weekend (Saturday and Sunday), identified the types of activities the child participated in, along with the time spent on each.
Question Q32 is related to the child’s participation in structured PA and the time spent on them. Questions Q36 and Q39 are related to the types of activities and the time spent on them by the child on a weekday (yesterday) and on the weekend, respectively. These questions encompass 22 types of activities. According to Cox et al. [136], the activities performed by children are categorized as follows: 1, 2, 3, 4, and 5, stationary/sedentary activities (SPAs); 6, 11, 15, 16, and 21, slow/light activities (LPAs); 7, 8, 9, 10, 12, 13, 14, 17, 18, 19, 20, and 22, moderate to vigorous activities (MVPAs).
Regarding time and intensity, the guidelines from the WHO [137] were followed, recommending at least an average of 60 min of moderate to vigorous PA daily.
2.3. Procedures
To collect all the data, the research project was first presented to the Director of the Agrupamento de Escolas de Vilela (Paredes, Porto, Portugal) and submitted for approval by the Pedagogical Council. After obtaining consent from the School Group, permission was sought from parents for their child’s participation in the research. Parents were informed about the study’s objectives, nature, methods, and all the tests the child would undergo, with an assurance that the collected data would remain confidential and used solely for research purposes. The informed, voluntary, and clear consent form for participation in the study was provided in writing and signed by parents before the research activities began.
The tests for evaluating FMSs and math skills were administered by a single investigator (intra-observer) to each of the classes simultaneously during the morning of 16 March 2023, following the respective protocols [109].
Regarding the WPPSI-R, it was individually administered in a designated space (following the protocol of the test) between 20 March and 24 March 2023, during the morning. The test administrator received instructions from a psychologist who is an expert in the field.
For the assessments of GMSs and BMI, these were conducted by students majoring in Sports Science at ISCE Douro between March 20 and March 24, in the morning. These students were instructed in February 2023 with theoretical presentations of the test protocols and subsequent practical experimentation.
Regarding the children’s PA data, the educators handed the Pre-PAQ to the respective guardians for completion between March 27 and March 31. Questionnaires with incomplete, incorrect, or missing data were excluded.
All procedures were in accordance with the Declaration of Helsinki for research involving human subjects.
For the analysis of results, in the initial phase, considering the classifications of the study variables, the children’s prevalence was described regarding: (1) performance on the WPPSI-R; (2) performance of FMSs (FMC and VMI); (3) performance of GMSs (ball skills and balance); (4) participation in structured PA and adherence to weekly PA recommendations; (5) the prevalence of obesity, considering the BMI classification.
In the second phase, the relationship between the study variables and their direct or indirect influence on the performance in the WPPSI-R test was analyzed.
2.4. Data Analysis
Descriptive statistics were employed to calculate the sample distribution, mean as a measure of central tendency, standard deviation as a measure of dispersion, and frequencies to describe the prevalence in the distributions of study variables, specifically performance on the WPPSI-R test, motor skills (FMSs—TBT-AD and VMI-AD; GMSs—MABC-2, aiming and catching, and balance), PA (structured PA and the number of days meeting weekly PA recommendations), and BMI classification.
Pearson’s correlation coefficient (r) was used to analyze the correlations between the study variables, and the following classifications were proposed: trivial (r ≤ 0.1), small (r = 0.1–0.3), moderate (r = 0.3–0.5), large (r = 0.5–0.7), very large (r = 0.7–0.9), and almost perfect (r ≥ 0.9) [113].
To analyze the influence of motor skills, PA, and BMI classification on mathematical performance, multivariate analysis was performed using the stepwise multiple linear regression (MLR) method. MLR examines how multiple independent variables relate to a dependent variable [138]. The MLR model can accurately suggest the relationships between variables and indicate the best effect of independent variables on the dependent variable (regression equation) [139]. This method is commonly used in educational research to measure the effects of explanatory variables on performance [140]. The F-test was used to assess the linearity of variable inclusion in the MLR model. The R test (Pearson) was used to examine the association between the variables for inclusion in the MLR model. The following classifications were proposed to investigate the influence between the variables (R2): values equal to 2% small effect; 13% medium effect; 26% as a large effect [112]. The standardized regression coefficients (β) and the non-standardized regression coefficients were used to analyze the influence that each variable represents in the MLR model. A significance level of p < 0.05 was set. The SPSS program, version 26.0, was used for the statistical analysis.
3. Results
3.1. Included Variables’ Prevalence
Regarding mathematical performance (Table 2), the majority of children did not exhibit difficulties in the arithmetic test of the WPPSI-R (75.8%). However, it was observed that 24.2% (15 children) displayed below-average performance, with only 17.7% (11 children) performing above average.

Table 2.
Distribution of the prevalence classification in the performance of the WPPSI-R arithmetic test.
Table 3 presents the prevalence related to FMSs, where no students were observed to have significant difficulties or perform very well. Approximately 11.3% of students demonstrated some difficulties in their performance. Thus, the vast majority exhibited moderate performance (67.7%). Concerning the TBT-AD test performance, it is notable that none of the children exhibited severe disorders in their FMC. However, none achieved a very high performance, and a substantial number of children showed moderate disorders in their FMC (33.9%). In the VMI-AD test, similarly, none of the children demonstrated very high performance. Nevertheless, three children (4.8%) displayed very low performance, and 15 children displayed low performance (24.2%). These data reveal that approximately 34% of children have difficulties in their FMSs and 29% in their VMI.

Table 3.
Distribution of the prevalence classification of children regarding FMS performance.
Regarding GMSs, only six children (9.7%) showed a risk of motor disorder. In both ball skills (aiming and catching) and balance (static, dynamic, and total), the vast majority of children did not exhibit a risk of motor disorder (aiming and catching = 87.1%—54 children; balance static = 88.7%—55 children; balance dynamic and total = 91.9%—57 children). It was in the balance (dynamic and total) domain where the lowest number of children at risk was observed (4 children—6.5%) or with a motor disorder (1 child—1.6%). However, it is worth noting that six children (9.7%) showed motor disorder in ball skills and were at risk of motor disorder in balance static (9.7%) (Table 4).

Table 4.
Distribution of the classification of the prevalence of children regarding the performance of GMSs.
Regarding PA (Table 5), the majority of children participate in structured PA (45 children—72.6%), with the practice of one structured PA session per week being prevalent (46.8%). However, in terms of meeting the weekly PA recommendations, only 27 children (43.5%) met the recommendations for daily intensity (a minimum of 60 min of MVPAs). Concerning PA intensity, the greatest amount of time was spent on SPAs (M = 328.95 ± 155.23) and the least on LPAs (M = 131.93 ± 96.39). The time spent on SPAs was significantly higher than the time spent on LPAs (p < 0.001) and similar to the time spent on MVPAs (p = 0.254).

Table 5.
Practice of physical activity.
As for BMI, its mean was 16.37 ± 2.22 (minimum = 11.12; maximum = 24.5), and the percentile mean was 59.62 ± 32.16 (minimum = 0.1; maximum = 99.8). Despite the majority (39 children—62.9%) being classified as having normal weight, it was observed that 9 (14.5%) children were in the pre-obese category and 9 others had obesity (Table 6).

Table 6.
Mean and standard deviation of BMI and associated percentile and distribution of classification relative to BMI classification.
3.2. Association between All Variables and Their Influence on Mathematical Skills
In the associations between all variables (Table 7) and concerning the performance in the WPPSI-R, only a significant moderate positive association was observed between the VMI-AD test (r = 0.464; p < 0.01) and the FMSs (r = 0.454; p < 0.01). The FMS result was obtained by summing the TBT-AD and VMI-AD tests. In this regard, the association of FMSs with the WPPSI-R was primarily influenced by the VMI-AD test, as the TBT-AD test exhibited a trivial negative association with the WPPSI-R (r = −0.045; p > 0.05). Moreover, the associations of the WPPSI-R with all other tests were trivial or small.

Table 7.
Association between all study variables.
Regarding the result of FMSs, despite the positive influence of the TBT-AD test, this association was small and not significant (r = 0.177; p > 0.05). Thus, the outcome of FMSs was primarily influenced by the results of the VMI-AD test (r = 0.975; p < 0.001).
An important observation is that an increase in SPAs exhibited a significant negative association with the TBT-AD test performance (r = −0.267; p < 0.05) and a positive but not significant association with the VMI-AD test performance (r = 0.217; p > 0.05). Therefore, SPAs showed a positive association with the VMI-AD test and a negative association with the TBT-AD test.
Concerning the association between FMSs and GMSs, a small positive but non-significant association was found between these motor skills (r = 0.224; p > 0.05). However, this result was justified only by the VMI-AD test, as a significant positive association was observed only between this test and GMSs (r = 0.269; p < 0.05), but not with all GMS tests (VMI-AD—aiming and catching: r = 0.185; p > 0.05; VMI-AD—static balance: r = 0.121; p > 0.05; VMI-AD—dynamic balance: r = 0.160; p > 0.05; VMI-AD—total balance: r = 0.213; p > 0.05). On the other hand, the TBT-AD test showed small negative associations with GMSs (r = −0.186; p > 0.05), particularly with the aiming and catching test (r = −0.199; p > 0.05) and dynamic balance (r = −0.108; p > 0.05), and trivial associations with static balance (r = 0.057; p > 0.05) and total balance (r = −0.072; p > 0.05). These results suggest that the association between FMSs and GMSs was primarily influenced by the VMI-AD test.
Regarding GMSs, contrary to FMSs, all tests evaluating these skills contributed significantly to this association (aiming and catching: r = 0.765; p < 0.01; static balance: r = 0.450; p < 0.01; dynamic balance: r = 0.579; p < 0.01; total balance: r = 0.716; p < 0.01), with a similar contribution of aiming and catching and balance to GMS development. PA levels also had a small association with GMS, mainly SPAs (r = 0.252; p < 0.05) and LPAs (r = 0.204; p > 0.05), and not MVPAs (r = −0.110; p > 0.05). Additionally, an increase in BMI classification contributed slightly to decreased GMSs, as an increase in BMI classification had a negative association with GMSs (r = −0.216; p > 0.05) and their respective tests (aiming and catching: r = −0.188; p > 0.05; static balance: r = −0.050; p > 0.05; dynamic balance: r = −0.022; p > 0.05; total balance: r = −0.130; p > 0.05).
Regarding PA, children engaged in structured PA were significantly more likely to meet the weekly PA recommendations for a greater number of days (r = 0.272; p < 0.05). A significant association was also found between structured PA and PA levels, particularly with SPAs (r = 0.259; p < 0.05) and MVPAs (r = 0.193; p > 0.05), but not with LPAs (r = −0.171; p > 0.05). The association of structured PA with BMI classification was trivial (r = −0.030; p > 0.05). Concerning the days when children met the weekly PA recommendations, an increase was significantly associated with greater MVPAs (r = 0.764; p < 0.01) and not with SPAs (r = 0.181; p > 0.05) or AFL (r = 0.068; p > 0.05).
As for the increase in BMI classification, it had trivial and non-significant associations with other study variables, except for a slight and non-significant decrease in GMSs (r = −0.216; p > 0.05), negatively associated with all its components.
After analyzing the association between all variables, this study aimed to find the best multiple linear regression (MLR) model to explain the results of the WPPSI-R arithmetic test. Therefore, a multivariate analysis was conducted through MLR using the stepwise method to determine which independent variables of the study could directly or indirectly influence performance in the WPPSI-R arithmetic test.
Table 8 presents a summary of the MLR model to determine which independent variables should be included in the model, considering the WPPSI-R arithmetic test as the dependent variable. Table 9 shows the respective standardized regression coefficients (β) and unstandardized regression coefficients (Beta).

Table 8.
Summary of the MRLM according to the score obtained on the WPPSI-R (dependent variable).

Table 9.
Table of MLR coefficients selected by the stepwise method.
Based on the analysis of Table 8 and Table 9, it was observed that MLR selected only one model, including only the VMI-AD test. This test was the only one that demonstrated linearity in the F-test (F = 16.447; p < 0.001), showing a moderate positive association with the WPPSI-R (Beta = 0.464; T = 4.055; p < 0.001) and influencing it by 21.5% (R2 = 0.215). These results suggest that VMI-AD test scores can be used to explain the results of the WPPSI-R arithmetic test since, according to Polit and Beck’s criteria [112], these values are considered moderate (>13%) and close to a large effect size (≥26%).
The values recorded with MLR between R2-R2(Adj) were too high (0.013; 1.3%) to allow generalization to the population, since the values for the effect should be less than or equal to 0.004 (0.4%) of the variance.
Table 10 lists the tests that were excluded from MLR because they did not demonstrate significance for the effect (p > 0.05).

Table 10.
Tests excluded from MLR.
These results indicate that the CMF, GMSs, PA, and BMI classification did not directly influence math skills. Therefore, since the VMI-AD test was the only one to have a direct influence on the WPPSI-R arithmetic test, we sought to analyze whether any of the studied variables could indirectly influence the WPPSI-R arithmetic test through their influence on the VMI-AD test. For this purpose, we used the VMI-AD test as the dependent variable in MLR. The results showed that none of the variables were included in the model. These data suggested that FMC, GMSs, PA, and BMI classification did not directly influence VMI-AD. Thus, the WPPSI-R arithmetic test was indirectly influenced by FMC, GMSs, PA, and BMI classification.
4. Discussion
The main objective of this study was to study the relationships between math performance, motor skills, PA, and BMI classification. In view of the objective, it was considered important, in the first phase, to describe the prevalence of the difficulties shown by the children, in order to characterize the sample and compare the results with those in the literature to check if any variables could bias the study. Subsequently, to answer the main objective of the study, the associations between all the variables and their influence on mathematical performance were analyzed.
4.1. Prevalence Analysis
In terms of prevalence, regarding math performance, there was a prevalence of 24.2% of preschool children who showed difficulties in completing the WPPSI-R arithmetic test. The literature has shown very heterogeneous results regarding the mathematical difficulties experienced by preschool children [141], suggesting that these difficulties can vary between 10 and 30% [142,143]. The results of this study are in line with the literature, suggesting early diagnosis of mathematical skills, since the mathematical skills that children acquire in preschool are important for developing a conceptual understanding of math, predicting their performance up to eighth grade [144], and are a strong indicator of future academic and professional success [95].
Regarding FMSs, there was a prevalence of 11.3% of children with difficulties in these skills. As with the prevalence of math difficulties, the literature is also inconsistent regarding the prevalence of preschool children with FMS disorders [53,145]. Studies have demonstrated a variability in the prevalence of FMS disorders between 20% [146] and 25% [147]. However, other studies have found a lower prevalence, between 9.7% [148] and 11.7% [149]. Once again, the results of the present study are in line with the literature, where international research has shown that many preschool children have revealed difficulties in performing age-appropriate fine motor tasks [148,150]. Since low levels of performance in FMSs are associated with difficulties in learning mathematics [151], there is an urgent need to identify delays in these skills in order to design early intervention programs.
Regarding GMSs, 9.7% of children showed difficulties in performing these motor skills. This result corroborated with that found in the literature, since the studies indicated that the majority of children scored within or above the satisfactory classification for GMSs. An example of this was recorded in the studies carried out by Cook et al. [152] and Draper et al. [153,154], where more than 85% of the children showed no difficulties in GMSs. GMSs are fundamental to the development of social skills [155,156] and influence children’s PA levels and health [157,158]; as for FMSs, it is important to diagnose GMSs early in preschoolers.
Regarding PA, the majority of children participated in structured PA (72.6%); however, only 43.5% fulfilled the weekly PA recommendations. These data suggest that although children performed structured PA, this was not enough to meet the recommendations proposed for PA intensity, that is, at least 60 min of MVPAs daily [137].
Regarding BMI classification, a prevalence of 14.5% of children with pre-obesity and 14.5% with obesity (pre-obesity + obesity = 29%) was recorded. In 2021/2022, in Portugal, the prevalence of childhood pre-obesity was 18.4% and obesity 13.5% (pre-obesity + obesity = 31.9%) [159]. Therefore, the prevalence of pre-obesity and obesity recorded in this study does not differ much from that studied at the national level, with a variance of only 2.9%. It has been documented that pre-obese and obese children engage less in PA [160], contributing to negative outcomes in physical fitness [161], health [162] and motor skills [101,102] and can lead to impaired cognitive development [82]. Furthermore, parents and educators tend to be less likely to encourage obese children to practice PA based on perceptions that children with this typology will have limited physical abilities, which may contribute to triggering a cycle of PA avoidance [160]. As a response to these consequences, obesity prevention should be a priority in the preschool years, as these are essential for establishing an intervention on eating behavior and PA [163,164,165].
After analyzing and discussing the prevalence of the variables included here, it was found that the characteristics of the children in this study were within the values found in the literature, which leads to the conclusion that the characteristics of the children in these variables contributed to reducing a possible bias in this study.
4.2. Associations between Study Variables and Their Influence on Mathematical Performance
After studying the relationship between the prevalence of the study variables and those in the literature, the aim was to analyze the associations between all the variables and their direct and indirect influence on mathematical performance.
In the study on the association between the variables, in relation to FMSs, these were mainly influenced by VMI (VMI-AD, r = 0.975; p < 0.01) with a small contribution from FMC (TBT-AD, r = 0.177; p > 0.05), with no association between VMI skills and FMC. Although VMI and FMC contributed to FMS performance, VMI made a significantly higher contribution than FMC. When studying the relationship between VMI and FMC, no association was found between these specific motor skills. However, studies have demonstrated an interrelationship between VMI and FMC [166], where bead threading tasks have been associated with shape copying tasks [167], with FMC being a precursor to VMI [168]. Unlike FMSs, GMSs were strongly influenced by all the tests that make it up (aiming and catching r = 0.765; balance r = 0.716). However, among the GMS tests, the association was trivial (aiming and catching and balance: r = 0.099). Thus, the propulsive and repulsive manual skills assessed by the aiming and catching tests do not contribute to balance and vice versa.
Regarding the association between FMSs and GMSs, there was a small positive association between these motor skills (r = 0.224; p > 0.05). However, this result was influenced by VMI, since there was only one positive and significant association between GMSs and VMI (r = 0.269; p < 0.05). This result suggests that GMSs can positively influence FMSs by significantly increasing VMI skills. Although the literature shows a moderate positive relationship between FMSs and GMSs during child development, from r = 0.30 [169] to r = 0.60 [170], this is not consensual. Some studies have shown a moderate positive correlation between these skills in preschool children [53,171,172,173], and other studies have disagreed with the correlation [174,175,176]. These results can be justified, on one hand, by the fact that these studies assessed motor skills during short periods of age using very heterogeneous tasks [177] and, on the other hand, by the fact that motor skills do not follow linear developmental trajectories [178]. It has also been mentioned that in the same motor action it is difficult to clearly differentiate the involvement of each of the motor skills (GMSs and FMSs), since they coexist and are fundamental for the efficient performance of the task [178,179]. Regarding the association between the practice of structured PA and PA intensity with GMSs and FMSs, the associations found were small or trivial. It is worth highlighting the fact that SPAs had a small significant negative influence on FMC (TBT-AD, r = −0.267; p < 0.05) and a non-significant positive influence on VMI (VMI-AD, r = 0.217; p > 0.05). GMSs also had a small significant contribution from SPAs (r = 0.252; p < 0.05) and non-significant from LPAs (r = 0.204; p > 0.05). MVPAs did not contribute to the increase in either GMSs or FMSs. Thus, these results suggest that structured PA alone was not enough to influence motor skills and that it was SPAs that exerted the greatest influence, mainly through a decrease in FMC and a small increase in VMI and GMSs. In fact, most of the tasks associated with the development of VMI are graphomotor tasks that mainly require SPA. On the other hand, activities for the development of FMC require speed and precision (non-graphomotor) and may require an increase in PA intensity [180,181,182,183]. In the study carried out by Roth et al. [184], they concluded that SPA contributed to a decrease in motor skills. This decrease could be explained by the amount of time children spend watching TV or using their mobile phones or tablets [185,186]. It has also been reported that extensive tablet use affects FMC and VMI [187,188]. Although digital technologies can support self-directed learning in young children, they have negative consequences for the development of FMSs [189].
Although researchers agree that children in the first years of life should be very active through structured and unstructured PA [190,191], the results show that not all forms or configurations of PA are equally effective in promoting motor skills [84]. Motor skills, such as locomotion or object manipulation, are not acquired innately as children grow up [192]; they should be learned and practiced [34,35] through structured programs during early childhood to facilitate its acquisition [33]. However, many kindergartens focus their work mainly on academic content, reducing children’s opportunities to develop motor skills in these environments [155,193]. Since structured PA is considered more efficient for the development of GMSs and FMSs compared to unstructured PA [194,195,196], there is an urgent need to implement structured PA programs to prevent difficulties in motor skills [197,198,199]. During early childhood, children with difficulties in motor skills have a lower perception of their skills and consequently have more difficulties in engaging in more challenging PA [48], participate less in playing [200], and have more problems with their peers, potentially becoming victims of exclusion [201]. In this sense, despite the importance of the early development of motor skills in children, it has been neglected in educational practices [82], resulting in a growing increase in these difficulties in recent years [202,203]. Therefore, more important than the intensity of PA, it seems that structured PA is the most important prerequisite for the development of motor skills in early childhood.
Regarding the association between BMI, PA, and motor skills, it was found that the fact that children performed structured PA on a weekly basis and different levels of PA were not enough to influence BMI classification. Similarly, motor skills were not influenced by BMI classification either, with only a small, non-significant decrease in GMSs (r = −0.216; p > 0.05). Therefore, the results suggest that children’s adherence to the practice of structured PA, as well as the intensity of PA, had no effect on reducing overweight or obesity. This result can be explained by the fact that some parents enroll their children in structured PA when they reach levels of obesity above expectations. Supporting these results, studies concluded that being less physically active was associated with thinness, and not with overweight or obesity, and time spent in MVPAs was positively associated with BMI [204,205]. However, other studies have shown an inverse relationship between PA and BMI where overweight and obesity were associated with lower PA levels [206,207]. Regarding motor skills, the results indicated that the increase in BMI score did not influence performance of FMSs (FMS: r = 0.050; p > 0.05; FMC: r = 0.096; p > 0.05; VMI: r = −0.029; p > 0.05) and only contributed to a small decrease in GMSs (GMS: r = −0.216; p > 0.05; aiming and catching: r = −0.188; p > 0.05; balance: r = −0.130; p > 0.05). A similar result was recorded in the study carried out by Kakebeeke et al. [208] on 476 preschool children (3.9 ± 0.7 years). The authors concluded that body composition measurements (BMI, skin folds, and abdominal perimeter) were not related to FMSs and found only a small decrease in GMSs and only in children with a high percentage of fat mass.
Exclusively in relation to the association between obesity and FMS, the results in the literature do not suggest any association between FMSs, obesity, and BMI in preschool children [209]. Regarding the relationship between obesity and GMSs, the literature has shown that children who are overweight or obese have more difficulty in some GMSs, such as jumping, running, and balancing [210,211]. Other studies concluded that GMSs were not associated with childhood overweight and obesity [212,213,214]. However, a study carried out on obese children, following the intervention of a structured PA program, showed a reduction in average body weight and an increase in the performance of GMSs [215]. Other studies concluded that obesity leads to a decrease in PA [41] and contributes to a decrease in GMSs [38,39,40,102] and physical fitness and a consequent decrease in participation in structured PA programs, contributing to an increase in obesity [36]. In this sense, we are facing a vicious cycle of physical inactivity that promotes a decrease in motor skills and an increase in obesity, with all the associated risks.
One of the main aims of this research was to study the influence of FMSs, GMSs, PA, and BMI on mathematical performance assessed by the WPPSI-R. The results showed that only the VMI-AD test was positively and significantly associated with the WPPSI-R arithmetic test (Beta = 0.464; T = 4.055; p < 0.001), influencing it by 21.5 per cent (R2 = 0.215). Thus, the VMI-AD test can be used to explain the results of the WPPSI-R arithmetic test, with values close to a large effect (R > 0.26) [112]. By placing the VMI-AD test as the dependent variable in the MLR model, no variables were included in the model, suggesting that FMC, GMSs, PA, and BMI classification did not directly influence VMI-AD and therefore were not indirect predictors of the results of the WPPSI-R math test. These results support recent systematic reviews, which concluded that VMI was the specific motor skill that was most consistently positively and significantly associated with math performance [29,64]. Regarding the role played by PA in academic performance, a recent systematic review found no clear consensus on the effects of PA on academic results in early childhood [216]. However, some studies reinforce the idea that PA with high coordination demands improves higher cognitive processes, particularly executive function, contributing to children’s school learning [217,218], and that aerobic training with low coordination demands has no influence on academic performance [219,220,221]. Regarding GMSs, although some authors suggest significant associations between GMSs and math [22,26,97], the literature is inconsistent and insufficient to report the relationship between the specific GMS components and math performance in preschoolers [29,64,193,222]. Despite the inconsistency of the results, these skills should be part of the kindergarten teacher’s work, since this educational period should contribute to children’s all-round development [222]. Furthermore, preschool children involved in a structured, cognitively challenging GMS program could contribute to the improvement of mathematical skills through the direct effect exerted on the improvement of FMSs [223].
Regarding FMSs, its importance for school readiness has been suggested (Grissmer et al., 2010 [52]). In a systematic review carried out by Flores et al. [64], one of the objectives was to identify the specific motor skills that would most influence mathematical performance in preschool children with typical development; the authors concluded that both FMS and VMI were predictors of mathematical performance, with an advantage for VMI skills, which showed more robust and consistent results. However, children with better FMC may be better at manipulating objects, such as pencils or notebooks, which allows them to direct additional attentional resources to new learning, particularly VMI [224]. Thus, a child with a good FMC when performing an academic task may impose a lower cognitive load compared to a child who still has FMC difficulties [225,226].
After analyzing the associations and influences of the variables on mathematical performance, this study suggests that mathematical performance was not influenced by FMC, GMSs, PA, and BMI, and only VMI skills directly contributed to increasing mathematical performance in preschool children with typical development. However, since VMI skills were positively and significantly associated with GMSs (r = 0.269; p < 0.05), it seems that these skills could contribute to improving VMI skills. Thus, math skills are directly influenced by VMI, and since GMSs were positively and significantly associated with VMI, they could directly contribute to increasing VMI and thus indirectly math skills.
The direct and indirect relationships and influences presented in this study between motor skills, PA, and obesity on mathematical performance demonstrate that new policies should support kindergartens with the implementation of intervention programs at this level.
5. Conclusions
Understanding which specific competencies are related to the mathematical performance of preschool children has significant implications for the implementation of educational programs at this level to prevent gaps in subsequent years.
This study demonstrated that only VMI directly, positively, and significantly influenced the mathematical performance of typically developing preschool children. However, FMSs and GMSs may indirectly contribute to mathematical performance, as evidenced by their associations with VMI.
Typically, motor skills are not highly valued at this educational level, primarily due to the common misconception that children naturally develop motor skills during their developmental process. In this context, our results suggest the implementation of structured programs to develop VMI and thus enhance mathematical performance.
Limitations
This study has several limitations that need to be considered. Firstly, it is essential to highlight that the sample was not representative of the population. This situation is primarily justified by the high number of assessments and data collection at different time points. Consequently, some children who were not eligible for the study either missed some assessments or did not provide necessary information for the research, leading to their exclusion. Another limitation is related to the instruments used, especially the tests for assessing FMSs. This was the first time these tests were used, and there were no existing data in the literature to discuss the results obtained here. More studies using the TBT-AD and VMI-AD are needed to increase the consistency of the conclusions.
Another limitation is associated with the acquisition of data on PA because, given the nature of the study, the type, frequency, and intensity of PA were obtained subjectively using the Pre-PAQ. It would likely be beneficial for this and future studies to include objective assessments of certain physical abilities in children. Regarding data collection on obesity levels, although BMI is the most commonly used measure for classifying overweight and obesity, other measures can be used in the preschool age, such as skinfold measurements or waist-to-hip ratio [188].
In future similar studies, it would be valuable to consider the socioeconomic status of the children, as preschool children in poverty are at a higher risk for lower performance in primary school and lower high school completion rates. Besides socioeconomic status, research has shown that children living with only one parent tend to be more physically active and spend more time playing outdoors. Future research may also consider this aspect.
Author Contributions
Conceptualization, P.F. (Pedro Flore) and P.F. (Pedro Forte); methodology, P.F. (Pedro Flore); software, P.F. (Pedro Flore); validation, E.C., I.M.-C. and P.F. (Pedro Forte); formal analysis, P.F. (Pedro Flore); investigation, P.F. (Pedro Flore); resources, P.F. (Pedro Flore); data curation, P.F. (Pedro Flore); writing—original draft preparation, P.F. (Pedro Flore); writing—review and editing, E.C., I.M.-C. and P.F. (Pedro Forte).; visualization, E.C., I.M.-C. and P.F. (Pedro Forte).; supervision, E.C., I.M.-C. and P.F. (Pedro Forte); project administration, P.F. (Pedro Flore); Funding Acquisition, P.F. (Pedro Forte) All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the FCT—Portuguese Foundation for Science and Technology: UIDB/DTP/04045/2020.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of the Higher Institute of Educational Sciences of the Douro (protocol code: P.M.F:10.2021, date of approval: 28 October 2021).
Informed Consent Statement
Informed consent statements were obtained from all parents and/or legal guardians of the subjects involved in the current investigation.
Data Availability Statement
Data are available upon request from the corresponding author.
Acknowledgments
The authors would like to thank Agrupamento de Escolas de Vilela, Paredes, especially all the teachers, students, and parents involved in this research.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Australian Research Alliance for Children and Youth. Early Childhood and Long Term Development: The Importance of the Early Years; Australian Research Alliance for Children and Youth: Perth, Australia, 2006. [Google Scholar]
- Anderson, L.M.; Shinn, C.; Fullilove, M.T.; Scrimshaw, S.C.; Fielding, J.E.; Normand, J.; Carande-Kulis, V.G.; Task Force on Community Preventive Services. The effectiveness of early childhood development programs: A systematic review. Am. J. Prev. Med. 2003, 24, 32–46. [Google Scholar] [CrossRef] [PubMed]
- Johnston, M.V. Plasticity in the developing brain: Implications for rehabilitation. Dev. Disabil. Res. Rev. 2009, 15, 94–101. [Google Scholar] [CrossRef] [PubMed]
- Dean, D.C., III; O’Muircheartaigh, J.; Dirks, H.; Waskiewicz, N.; Walker, L.; Doernberg, E.; Piryatinsky, I.; Deoni, S.C. Characterizing longitudinal white matter development during early childhood. Brain Struct. Funct. 2015, 220, 1921–1933. [Google Scholar] [CrossRef] [PubMed]
- Falbo, B.C.P.; Andrade, R.D.; Furtado, M.C.C.; Mello, D.F. Estímulo ao desenvolvimento infantil: Produção do conhecimento em enfermagem. Rev. Bras. Enferm. 2012, 65, 148–154. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Stich, H.L.; Baune, B.T.; Caniato, R.N.; Mikolajczyk, R.T.; Krämer, A. Individual development of preschool children-prevalences and determinants of delays in Germany: A cross-sectional study in Southern Bavaria. BMC Pediatr. 2012, 12, 188. [Google Scholar] [CrossRef] [PubMed]
- Bernal, R.; Fernández, C. Subsidized childcare and child development in Colombia: Effects of Hogares Comunitarios de Bien estar as a function of timing and length of exposure. Soc. Sci. Med. 2013, 97, 241–249. [Google Scholar] [CrossRef] [PubMed]
- Bronfenbrenner, U. A Ecologia do Desenvolvimento Humano: Experimentos Naturais e Planejados; Artes Médicas: Porto Alegre, Brazil, 1996. [Google Scholar]
- Sigurdsson, E.; Van Os, J.; Fombonne, E. Are impaired childhood motor skills a risk factor for adolescent anxiety? Results from the 1958 UK birth cohort and the National Child Development Study. Am. J. Psychiatr. 2002, 159, 1044–1046. [Google Scholar] [CrossRef]
- Murray, G.K.; Veijola, J.; Moilanen, K.; Miettunen, J.; Glahn, D.C.; Cannon, T.D.; Jones, P.B.; Isohanni, M. Infant motor development is associated with adult cognitive categorisation in a longitudinal birth cohort study. J. Child Psychol. Psychiatry 2006, 47, 25–29. [Google Scholar] [CrossRef]
- Piek, J.P.; Dawson, L.; Smith, L.M.; Gasson, N. The role of early fine and gross motor development on later motor and cognitive ability. Hum. Mov. Sci. 2008, 27, 668–681. [Google Scholar] [CrossRef]
- Gallahue, D.L.; Ozmun, J.C. Understanding Motor Development: Infants, Children, Adolescents, Adults; McGraw-Hill: New York, NY, USA, 2002. [Google Scholar]
- Gerber, R.J.; Wilks, T.; Erdie-Lalena, C. Developmental milestones: Motordevelopment. Pediatr. Rev. 2010, 31, 267–276. [Google Scholar] [CrossRef]
- Caçola, P.M.; Gabbard, C.; Montebelo, M.I.; Santos, D.C. Further development and validation of the affordances in the home environment for motor development–infant scale (AHEMD-IS). Phys. Ther. 2015, 95, 901–923. [Google Scholar] [CrossRef] [PubMed]
- Valadi, S.; Gabbard, C. The effect of affordances in the home environment on children’s fine-and gross motor skills. Early Child Dev. Care 2020, 190, 1225–1232. [Google Scholar] [CrossRef]
- Frick, A.; Möhring, W. A matter of balance: Motor control is related to children’s spatial and proportional reasoning skills. Front. Psychol. 2016, 6, 2049. [Google Scholar] [CrossRef] [PubMed]
- Diamond, A. Interrelated and interdependent. Dev. Sci. 2007, 10, 152–158. [Google Scholar] [CrossRef] [PubMed]
- Leisman, G.; Moustafa, A.A.; Shafir, T. Thinking, walking, talking: Integratory motor and cognitive brain function. Front. Public Health 2016, 4, 94. [Google Scholar] [CrossRef] [PubMed]
- Jung, J.Y.; Cloutman, L.L.; Binney, R.J.; Lambon-Ralph, M.A. The structural connectivity of higher order association cortices reflects human functional brain networks. Cortex 2017, 97, 221–239. [Google Scholar] [CrossRef] [PubMed]
- Ahnert, J.; Schneider, W.; Bös, K. Developmental changes and individual stability of motor abilities from the preschool period to young adulthood. In Human Development from Early Childhood to Early Adulthood: Findings from a 20-Year Longitudinal Study; Schneider, W., Bullock, M., Eds.; Psychology Press: New York, NY, USA, 2009; pp. 35–62. [Google Scholar]
- Haartsen, R.; Jones, E.J.H.; Johnson, M.H. Human brain development over the early years. Curr. Opin. Behav. Sci. 2016, 10, 149–154. [Google Scholar] [CrossRef]
- Son, S.H.; Meisels, S.J. The relationship of young children’s motor skills to later reading and math achievement. Merrill-Palmer Q. 2006, 52, 755–778. [Google Scholar] [CrossRef]
- Kuh, D.; Hardy, R.; Butterworth, S.; Okell, L.; Richards, M.; Wadsworth, M.; Cooper, C.; Sayer, A.A. Developmental origins of midlife physical performance: Evidence from a British birth cohort. Am. J. Epidemiol. 2006, 164, 110–121. [Google Scholar] [CrossRef]
- Alvarez-Bueno, C.; Pesce, C.; Cavero-Redondo, I.; Sánchez-López, M.; Garrido Miguel, M.; Martínez-Vizcaíno, V. Academic achievement and physical activity: A meta-analysis. Pediatrics 2017, 140, e20171498. [Google Scholar] [CrossRef]
- Carson, V.; Hunter, S.; Kuzik, N.; Wiebe, S.A.; Spence, J.C.; Friedman, A.; Tremblay, M.S.; Slater, L.; Hinkley, T. Systematic review of physical activity and cognitive development in early childhood. J. Sci. Med. Sport 2016, 19, 573–578. [Google Scholar] [CrossRef] [PubMed]
- de Waal, E. Fundamental movement skills and academic performance of 5- to 6-year-old Preschoolers. Early Child. Educ. J. 2019, 47, 455–464. [Google Scholar] [CrossRef]
- Duncan, M.; Cunningham, A.; Eyre, E. A combined movement and story-telling intervention enhances motor competence and language ability in pre-schoolers to a greater extent than movement or story-telling alone. Eur. Phys. Educ. Rev. 2019, 25, 221–235. [Google Scholar] [CrossRef]
- Haapala, E.A.; Lintu, N.; Väistö, J.; Tompuri, T.; Soininen, S.; Viitasalo, A.; Eloranta, A.M.; Venäläinen, T.; Sääkslahti, A.; Laitinen, T.; et al. Longitudinal associations of fitness, motor competence, and adiposity with cognition. Med. Sci. Sports Exerc. 2019, 51, 465–471. [Google Scholar] [CrossRef] [PubMed]
- Macdonald, K.; Milne, N.; Orr, R.; Pope, R. Relationships between motor proficiency and academic performance in mathematics and reading in school-aged children and adolescents: A systematic review. Int. J. Environ. Res. Public. Health 2018, 15, 1603. [Google Scholar] [CrossRef]
- Malambo, C.; Nová, A.; Clark, C.; Musálek, M. Associations between fundamental movement skills, physical fitness, motor competency, physical activity, and executive functions in pre-school age children: A systematic review. Children 2022, 9, 1059. [Google Scholar] [CrossRef] [PubMed]
- Zeng, N.; Ayyub, M.; Sun, H.; Wen, X.; Xiang, P.; Gao, Z. Effects of physical activity on motor skills and cognitive development in early childhood: A systematic review. BioMed Res. Int. 2017, 2017, 2760716. [Google Scholar] [CrossRef] [PubMed]
- Jones, D.; Innerd, A.; Giles, E.L.; Azevedo, L.B.D. The association between physical activity, motor skills and school readiness in 4–5-year-old children in the northeast of England. Int. J. Environ. Res. Public Health 2021, 18, 11931. [Google Scholar] [CrossRef]
- Logan, S.W.; Robinson, L.E.; Wilson, A.E.; Lucas, W.A. Getting the fundamentals of movement: A meta-analysis of the effectiveness of motor skill interventions in children. Child Care Health Dev. 2012, 38, 305–315. [Google Scholar] [CrossRef]
- Pic, M.; Navarro-Adelantado, V.; Jonsson, G.K. Detection of ludic patterns in two triadic motor games and differences in decision complexity. Front. Psychol. 2018, 8, 2259. [Google Scholar] [CrossRef]
- Pic, M.; Navarro-Adelantado, V.; Jonsson, G.K. Gender differences in strategic behavior in a triadic persecution motor game identified through an observational methodology. Front. Psychol. 2020, 11, 109. [Google Scholar] [CrossRef] [PubMed]
- Stodden, D.F.; Goodway, J.D.; Langendorfer, S.J.; Roberton, M.A.; Rudisill, M.E.; Garcia, C.; Garcia, L.E. A Developmental Perspective on the Role of Motor Skill Competence in Physical Activity: An Emergent Relationship. Quest 2008, 60, 290–306. [Google Scholar] [CrossRef]
- Jones, D.; Innerd, A.; Giles, E.L.; Azevedo, L.B.D. Association between fundamental motor skills and physical activity in the early years: A systematic review and meta-analysis. J. Sport Health Sci. 2020, 9, 542–552. [Google Scholar] [CrossRef] [PubMed]
- Goodway, J.D.; Branta, C.F. Influence of a motor skill intervention on fundamental motor skill development of disadvantaged preschool children. Res. Q. Exerc. Sport 2003, 74, 36–46. [Google Scholar] [CrossRef] [PubMed]
- Wrotniak, B.H.; Epstein, L.H.; Dorn, J.M.; Jones, K.E.; Kondilis, V.A. The relationship between motor proficiency and physical activity in children. Pediatrics 2006, 118, e1758–e1765. [Google Scholar] [CrossRef] [PubMed]
- Williams, H.G.; Pfeiffer, K.A.; O’Neill, J.R.; Dowda, M.; McIver, K.L.; Brown, W.H.; Pate, R.R. Motor skill performance and physical activity in preschool children. Obesity 2008, 16, 1421–1426. [Google Scholar] [CrossRef]
- Metcalf, B.S.; Hosking, J.; Jeffer, A.N.; Voss, L.D.; Henley, W.; Wilkin, T.J. Fatness leads to inactivity, but inactivity does not lead to fatness: A longitudinal study in children (EarlyBird 45). Arch. Dis. Child. 2011, 96, 942–947. [Google Scholar] [CrossRef]
- Song, H.Q.; Lau, P.W.C.; Wang, J.J. Investigation of the motor skills assessments of typically developing preschool children in China. BMC Pediatr. 2022, 22, 84. [Google Scholar] [CrossRef]
- Hume, C.; Okely, A.; Bagley, S.; Telford, A.; Booth, M.; Crawford, D.; Salmon, J. Does weight status influence associations between children’s fundamental movement skills and physical activity? Res. Q. Exerc. Sport 2008, 79, 158–165. [Google Scholar] [CrossRef]
- D’Hondt, E.; Deforche, B.; De Bourdeaudhuij, I.; Lenoir, M. Relationship between motor skill and body mass index in 5- to 10-year old children. Adapt. Phys. Activ. Q. 2009, 26, 21–37. [Google Scholar] [CrossRef]
- Barnett, L.M.; van Beurden, E.; Morgan, P.J.; Brooks, L.O.; Beard, J.R. Childhood motor skill proficiency as a predictor of adolescent physical activity. J. Adolesc. Health 2009, 44, 252–259. [Google Scholar] [CrossRef] [PubMed]
- Lopes, V.P.; Rodrigues, L.P.; Maia, J.A.R.; Malina, R.M. Motor coordination as predictor of physical activity in childhood. Scand. J. Med. Sci. Sports 2011, 21, 663–669. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.; Li, Y.; Song, H.; Yong, L.; Luo, L.; Zhang, Z.; Song, N. Assessment of Validity of children’s movement skill quotient (CMSQ) based on the physical education classroom environment. BioMed Res. Int. 2020, 2020, 8938763. [Google Scholar] [CrossRef] [PubMed]
- De Niet, M.; Platvoet, S.W.J.; Hoeboer, J.J.A.A.M.; DeWitte, A.M.H.; De Vries, S.I.; Pion, J. Agreement between the KTK3+ test and the athletic skills track for classifying the fundamental movement skills proficiency of 6- to 12-year-old children. Front. Educ. 2021, 6, 571018. [Google Scholar] [CrossRef]
- Moghaddaszadeh, A.; Belcastro, A.N. Guided active play promotes physical activity and improves fundamental motor skills for school-aged children. J. Sports Sci. Med. 2021, 20, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Burton, A.W.; Rodgerson, R.W. New Perspectives on the Assessment of Movement Skills and Motor Abilities. Adapt. Phys. Activ. Q. 2001, 18, 347–365. [Google Scholar] [CrossRef]
- Matheis, M.; Estabillo, J.A. Assessment of fine and gross motor skills in children. In Handbook of Childhood Psychopathology and Developmental Disabilities Assessment; Matson, J.L., Ed.; Autism and Child Psychopathology Series; Springer: Cham, Switzerland, 2018; pp. 467–484. [Google Scholar] [CrossRef]
- Grissmer, D.; Grimm, K.J.; Aiyer, S.M.; Murrah, W.M.; Steele, J.S. Fine motor skills and early comprehension of the world: Two new school readiness indicators. Dev. Psychol. 2010, 46, 1008–1017. [Google Scholar] [CrossRef]
- Oberer, N.; Gashaj, V.; Roebers, C.M. Motor skills in kindergarten: Internal structure, cognitive correlates and relationships to background variables. Hum. Mov. Sci. 2017, 52, 170–180. [Google Scholar] [CrossRef]
- Gonzalez, S.L.; Alvarez, V.; Nelson, E.L. Do gross and fine motor skills differentially contribute to language outcomes? A systematic review. Front. Psychol. 2019, 10, 2670. [Google Scholar] [CrossRef]
- Goodway, J.; Ozmun, J.; Gallahue, D. Understanding Motor Development: Infants, Children, Adolescents, Adults, 8th ed.; Jones & Bartlett Learning: Burlington, MA, USA, 2019. [Google Scholar]
- Meylia, K.N.; Siswati, T.; Paramashanti, B.A.; Hati, F.S. Fine motor, gross motor, and social independence skills among stunted and non-stunted children. Early Child Dev. Care 2020, 192, 95–102. [Google Scholar] [CrossRef]
- Lopes, L.; Santos, R.; Pereira, B.; Lopes, V.P. Associations between gross motor coordination and academic achievement in elementary school children. Hum. Mov. Sci. 2013, 32, 9–20. [Google Scholar] [CrossRef] [PubMed]
- Magistro, D.; Bardaglio, G.; Rabaglietti, E. Gross motor skills and academic achievement in typically developing children: The mediating effect of ADHD related behaviours. Cogn. Brain Behav. 2015, 19, 149–163. [Google Scholar]
- Kokstejn, J.; Musálek, M.; Tufano, J.J. Are sex differences in fundamental motor skills uniform throughout the entire preschool period? PLoS ONE 2017, 12, e0176556. [Google Scholar] [CrossRef] [PubMed]
- Haywood, K.M.; Getchell, N. Life Span Motor Development, 7th ed.; Human Kinetics: Champaign, IL, USA, 2019. [Google Scholar]
- Bolger, L.E.; Bolger, L.A.; O’Neill, C.; Coughlan, E.; O’Brien, W.; Lacey, S.; Burns, C.; Bardid, F. Global levels of fundamental motor skills in children: A systematic review. J. Sports Sci. 2020, 39, 717–753. [Google Scholar] [CrossRef] [PubMed]
- Davis, J.L.; Matthews, R.N. Review of NEPSY-second edition (NEPSY-II). J. Psychoeduc. Assess. 2010, 28, 175–182. [Google Scholar] [CrossRef]
- Suggate, S.; Pufke, E.; Stoeger, H. Do fine motor skills contribute to early reading development? J. Res. Read. 2018, 41, 1–19. [Google Scholar] [CrossRef]
- Flores, P.; Coelho, E.; Mourão-Carvalhal, M.I.; Forte, P. Association between motor and math skills in preschool children with typical development: Systematic review. Front. Psychol. 2023, 14, 1105391. [Google Scholar] [CrossRef]
- Caspersen, C.J.; Powell, K.E.; Christenson, G.M. Physical activity, exercise, and physical fitness: Definitions and distinctions for health-related research. Public Health Rep. 1985, 100, 126–131. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1424733/ (accessed on 25 September 2023).
- Coutinho, P.; Mesquita, I.; Davids, K.; Fonseca, A.M.; Côté, J. How structured and unstructured sport activities aid the development of expertise in volleyball players. Psychol. Sport Exerc. 2016, 25, 51–59. [Google Scholar] [CrossRef]
- World Health Organization. Guidelines on Physical Activity, Sedentary Behaviour and Sleep for Children under 5 Years of Age; World Health Organization: Geneva, Switzerland, 2019; Available online: https://www.who.int/publications/i/item/9789241550536 (accessed on 25 September 2023).
- Timmons, B.W.; LeBlanc, A.G.; Carson, V.; Connor Gorber, S.; Dillman, C.; Janssen, I.; Kho, M.E.; Spence, J.C.; Stearns, J.A.; Tremblay, M.S. Systematic review of physical activity and health in the early years (aged 0–4 years). Appl. Physiol. Nutr. Metab. 2012, 37, 773–792. [Google Scholar] [CrossRef]
- Graf, C.; Beneke, R.; Bloch, W.; Bucksch, J.; Dordel, S.; Eiser, S.; Ferrari, N.; Koch, B.; Krug, S.; Lawrenz, W.; et al. Vorschläge zur Förderung der körperlichen Aktivität von Kindern und Jugendlichen in Deutschland. Monatsschr. Kinderheilkd. 2013, 161, 439–446. [Google Scholar] [CrossRef]
- Huber, G. Generation S. Mod. Ernähr. Heute 2013, 1, 1–6. [Google Scholar]
- World Health Organization. Obesity. 2017. Available online: https://www.who.int/health-topics/obesity (accessed on 25 September 2023).
- Schwartz, M.; Seeley, R.; Zeltser, L.; Drewnowski, A.; Ravussin, E.; Redman, L.; Leibel, R.A. Obesity Pathogenesis: An Endocrine Society Scientific Statement. Endocr. Rev. 2017, 38, 267–296. [Google Scholar] [CrossRef] [PubMed]
- Ainsworth, B.E.; Haskell, W.L.; Whitt, M.C.; Irwin, M.; Swartz, A.M.; Strath, S.J.; O’Brien, W.L.; Bassett, D.R.; Schmitz, K.H.; Emplaincourt, P.O.; et al. Compendium of physical activities: An update of activity codes and MET intensities. Med. Sci. Sports Exerc. 2000, 32, 498–504. [Google Scholar] [CrossRef] [PubMed]
- Bucksch, J.; Dreger, S. Sitzendes Verhalten als Risikofaktor im Kindes-und Jugendalter. Prävention Und Gesundheitsförderung 2014, 9, 39–46. [Google Scholar] [CrossRef]
- Pate, R.; O’Neill, J.R.; Liese, A.D.; Janz, K.F.; Granberg, E.M.; Colabianchi, N.; Harsha, D.W.; Condrasky, M.M.; O’Neil, P.M.; Lau, E.Y.; et al. Factors associated with development of excessive fatness in children and adolescents: A review of prospective studies. Obes. Rev. 2013, 14, 645–658. [Google Scholar] [CrossRef] [PubMed]
- Planinšec, J. Relations between motor and cognitive dimensions of preschool girls and boys. Percept. Mot. Skills 2002, 94, 415–423. [Google Scholar] [CrossRef] [PubMed]
- Burger, K. How does early childhood care and education affect cognitive development? An international review of the effects of early interventions for children from different social backgrounds. Early Child Res. Q. 2010, 25, 140–165. [Google Scholar] [CrossRef]
- Carson, V.; Lee, E.Y.; Hewitt, L.; Jennings, C.; Hunter, S.; Kuzik, N.; Stearns, J.A.; Unrau, S.P.; Poitras, V.J.; Gray, C.; et al. Systematic review of the relationships between physical activity and health indicators in the early years (0–4 years). BMC Public Health 2017, 17, 854. [Google Scholar] [CrossRef]
- Rasmussen, M.; Laumann, K. The academic and psychological benefits of exercise in healthy children and adolescents. Eur. J. Psychol. Educ. 2013, 28, 945–962. [Google Scholar] [CrossRef]
- Tonge, K.L.; Jones, R.A.; Okely, A.D. Correlates of children’s objectively measured physical activity and sedentary behavior in early childhood education and care services: A systematic review. Prev. Med. 2016, 89, 129–139. [Google Scholar] [CrossRef] [PubMed]
- Figueroa, R.; An, R. Motor skill competence and physical activity in preschoolers: A review. Matern. Child Health J. 2017, 21, 136–146. [Google Scholar] [CrossRef] [PubMed]
- Lopes, V.P.; Stodden, D.F.; Bianchi, M.M.; Maia, J.A.; Rodrigues, L.P. Correlation between BMI and motor coordination in children. J. Sci. Med. Sport 2012, 15, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Lubans, D.R.; Morgan, P.J.; Cliff, D.P.; Barnett, L.M.; Okely, A.D. Fundamental movement skills in children and adolescents. Sports Med. 2010, 40, 1019–1035. [Google Scholar] [CrossRef] [PubMed]
- Robinson, L.E.; Stodden, D.F.; Barnett, L.M.; Lopes, V.P.; Logan, S.W.; Rodrigues, L.P.; D’Hondt, E. Motor competence and its effect on positive developmental trajectories of health. Sports Med. 2015, 45, 1273–1284. [Google Scholar] [CrossRef] [PubMed]
- Fisher, A.; Reilly, J.J.; Kelly, L.A.; Montgomery, C.; Williamson, A.; Paton, J.Y.; Grant, S. Fundamental movement skills and habitual physical activity in young children. Med. Sci. Sports Exerc. 2005, 37, 684–688. [Google Scholar] [CrossRef] [PubMed]
- Biddle, S.J.; Asare, M. Physical activity and mental health in children and adolescents: A review of reviews. Br. J. Sports Med. 2011, 45, 886–895. [Google Scholar] [CrossRef]
- Janssen, I.; LeBlanc, A.G. Systematic Review of the Health Benefits of Physical Activity and Fitness in School-Aged Children and Youth. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 40. Available online: http://www.ijbnpa.org/content/7/1/40 (accessed on 25 September 2023). [CrossRef]
- Ahn, J.V.; Sera, F.; Cummins, S.; Flouri, E. Associations between objectively measured physical activity and later mental health outcomes in children: Findings from the UK Millennium Cohort Study. J. Epidemiol. Community Health 2018, 72, 94–100. [Google Scholar] [CrossRef]
- Donnelly, J.E.; Hillman, C.H.; Castelli, D.; Etnier, J.L.; Lee, S.; Tomporowski, P.; Lambourne, K.; Szabo-Reed, A.N. Physical activity, fitness, cognitive function, and academic achievement in children: A systematic review. Med. Sci. Sports Exerc. 2016, 48, 1197–1222. [Google Scholar] [CrossRef]
- McNeill, J.; Howard, S.J.; Vella, S.A.; Santos, R.; Cliff, D.P. Physical activity and modified organized sport among preschool children: Associations with cognitive and psychosocial health. Ment. Health Phys. Act. 2018, 15, 45–52. [Google Scholar] [CrossRef]
- Ribner, A.D.; Willoughby, M.T.; Blair, C.B.; The Family Life Project Key Investigators. Executive function buffers the association between early math and later academic skills. Front. Psychol. 2017, 8, 869. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, V.R.; Ribeiro, M.L.S.; Melo, T.; de Tarso Maciel-Pinheiro, P.; Guimarães, T.T.; Araújo, N.B.; Ribeiro, S.; Deslandes, A.C. Motor coordination correlates with academic achievement and cognitive function in children. Front. Psychol. 2016, 7, 318. [Google Scholar] [CrossRef] [PubMed]
- Organization for Economic Cooperation and Development (OECD). Preliminary Reflections and Research on Knowledge, Skills, Attitudes and Values Necessary for 2030; Organization for Economic Cooperation and Development (OECD): Paris, France, 2016. [Google Scholar]
- Duncan, G.J.; Dowsett, C.J.; Claessens, A.; Magnuson, K.; Huston, A.C.; Klebanov, P.; Pagani, L.S.; Feinstein, L.; Engel, M.; Brooks-Gunn, J.; et al. School readiness sand later achievement. Dev. Psychol. 2007, 43, 1428–1446. [Google Scholar] [CrossRef] [PubMed]
- Parsons, S.; Bynner, J. Does Numeracy Matter More? National Research and Development Centre for Adult Literacy and Numeracy: London, UK, 2005. [Google Scholar]
- van der Fels, I.M.; Te Wierike, S.C.; Hartman, E.; Elferink-Gemser, M.T.; Smith, J.; Visscher, C. The relationship between motor skills and cognitive skills in 4–16 year old typically developing children: A systematic review. J. Sci. Med. Sport 2015, 18, 697–703. [Google Scholar] [CrossRef] [PubMed]
- Pagani, L.S.; Fitzpatrick, C.; Archambault, I.; Janosz, M. School readiness and later achievement: A French-Canadian replication and extension. Dev. Psychol. 2010, 46, 984–994. [Google Scholar] [CrossRef] [PubMed]
- Sibley, B.A.; Etnier, J.L. The relationship between physical activity and cognition in children: A meta-analysis. Pediatr. Exerc. Sci. 2003, 15, 243–256. [Google Scholar] [CrossRef]
- Fedewa, A.L.; Ahn, S. The effects of physical activity and physical fitness on children’s achievement and cognitive outcomes. Res. Q. Exerc. Sport 2011, 82, 521–535. [Google Scholar] [CrossRef]
- Singh, A.S.; Saliasi, E.; van den Berg, V.; Uijtdewilligen, L.; de Groot, R.H.M.; Jolles, J.; Andersen, L.B.; Bailey, R.; Chang, Y.-K.; Diamond, A.; et al. Effects of physical activity interventions on cognitive and academic performance in children and adolescents: A novel combination of a systematic review and recommendations from an expert panel. Br. J. Sports Med. 2019, 53, 640–647. [Google Scholar] [CrossRef]
- Cliff, D.P.; Okely, A.D.; Morgan, P.J.; Jones, R.A.; Steele, J.R.; Baur, L.A. Proficiency Deficiency: Mastery of Fundamental Movement Skills and Skill Components in Overweight and Obese Children. Obesity 2012, 20, 1024–1033. [Google Scholar] [CrossRef]
- Poulsen, A.A.; Desha, L.; Ziviani, J.; Griffiths, L.; Heaslop, A.; Khan, A.; Leong, G.M. Fundamental movement skills and self-concept of children who are overweight. Int. J. Pediatr. Obes. 2011, 6, e464–e471. [Google Scholar] [CrossRef] [PubMed]
- de Kieviet, J.F.; Piek, J.P.; Aarnoudse-Moens, C.S.; Oosterlaan, J. Motor Development in Very Preterm and Very Low-Birth-Weight Children from Birth to Adolescence: A Meta-analysis. JAMA J. Am. Med. Assoc. 2009, 302, 2235–2242. [Google Scholar] [CrossRef] [PubMed]
- Williams, J.; Lee, K.J.; Anderson, P.J. Prevalence of motor-skill impairment in preterm children who do not develop cerebral palsy: A systematic review . Dev. Med. Child Neurol. 2010, 52, 232–237. [Google Scholar] [CrossRef]
- Feder, K.P.; Majnemer, A. Handwriting development, competency, and intervention. Dev. Med. Child Neurol. 2007, 49, 312–317. [Google Scholar] [CrossRef]
- Edwards, J.; Berube, M.; Erlandson, K.; Haug, S.; Johnstone, H.; Meagher, M.; Sarkodee-Adoo, S.; Zwicker, J. Developmental Coordination Disorder in scholl-aged children born very preterm and/or at very low birth weight: A systematic review. J. Dev. Behav. Pediatr. 2011, 32, 678–687. [Google Scholar] [CrossRef]
- Weschler, D. WPPSI-R Manual; The Psychological Corporation: San Antonio, TX, USA, 1989. [Google Scholar]
- Wechsler, D. Escala de Inteligência de Weschler para a Idade Pré-Escolar e Primária—Edição Revista; Seabra-Santos, M.J.; Simões, M.R.; Ferreira, A.M.R.E.C., Translators; CEGOC-TEA: Lisbon, Portugal, 2003. [Google Scholar]
- Flores, P.; Coelho, E.; Mourão-Carvalhal, M.I.; Forte, P.M. Preliminary Adaptation of Motor Tests to Evaluate Fine Motor Skills Associated with Mathematical Skills in Preschoolers. Eur. J. Investig. Health Psychol. Educ. 2023, 13, 1330–1361. [Google Scholar] [CrossRef]
- Henderson, S.; Sugden, E.; Barnett, A. Movement Evaluation Battery for Children, 2nd ed.; Pearson: London, UK, 2007. [Google Scholar]
- Beery, K.E.; Beery, N.A. The Beery-Buktenica Developmental Test of Visual-Motor Integration, 6th ed.; Pearson: London, UK, 2010. [Google Scholar]
- Polit, D.; Beck, C. The content validity index: Are you know what’s being reported? Critique and recommendations. Res. Nurs. Health 2006, 29, 489–497. [Google Scholar] [CrossRef]
- Hopkins, W.G.; Marshall, S.W.; Batterham, A.M.; Hanin, J. Progressive Statistics for Studies in Sports Medicine and Exercise Science. Med. Sci. Sports Exerc. 2009, 41, 3–12. [Google Scholar] [CrossRef]
- Jaikaew, R.; Satiansukpong, N. Movement Assessment Battery for Children-Second Edition (MABC2): Cross-cultural validity, content validity, and interrater reliability Fin Thai children. Occup. Ther. Int. 2019, 2019, 4086594. [Google Scholar] [CrossRef]
- Caçola, P.; Lage, G. Developmental Coordination Disorder (DCD): An overview of the condition and research evidence. Motriz Rev. Educ. Fís. 2019, 25, e101923. [Google Scholar] [CrossRef]
- Caçola, P. Movement difficulties affect children’s learning: Na overview of Developmental Coordination Disorder (DCD). Learn. Disabil. 2014, 2, 98–106. [Google Scholar] [CrossRef]
- Kirby, A.; Sugden, D.A. Children with developmental coordination disorders. J. R. Soc. Med. 2007, 100, 182–186. [Google Scholar] [CrossRef] [PubMed]
- Smits-Engelsman, B.; Niemeijer, A.; Waelvelde, H. Is the movement assessment battery for children-2nd edition a reliable instrument to measure motor performance in 3 year old children? Res. Dev. Disabil. 2011, 32, 1370–1377. [Google Scholar] [CrossRef] [PubMed]
- Rolland-Cachera, M.F. Childhood obesity: Current definitions and recommendations for their use. Int. J. Pediatr. Obes. 2011, 6, 325–331. [Google Scholar] [CrossRef] [PubMed]
- Lohman, T.G.; Roche, A.E.; Martorell, R. Anthropometric Standardization Reference Manual; Human Kinetics Books: Champaign, IL, USA, 1988. [Google Scholar]
- European Childhood Obesity Group. Endorsement of the New WHO Growth Standards for Infants and Young Children; European Childhood Obesity Group (ECOG): Brussels, Belgium, 2009. [Google Scholar]
- International Pediatric Association. International Pediatric Association Endorsement: The New WHO Growth Standards for Infants and Young Children; International Pediatric Association (IPA): Geneva, Switzerland, 2006. [Google Scholar]
- WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr. 2006, 95, 76–85. [Google Scholar] [CrossRef] [PubMed]
- de Onis, M.; Onyango, A.W.; Borghi, E.; Siyam, A.; Nishida, C.; Siekmann, J. Development of a WHO growth reference for school-aged children and adolescents. Bull. World Health Organ. 2007, 85, 660–667. [Google Scholar] [CrossRef] [PubMed]
- Cole, T.J.; Lobstein, T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatr. Obes. 2012, 7, 284–294. [Google Scholar] [CrossRef] [PubMed]
- de Onis, M.; Lobstein, T. Defining obesity risk status in the general childhood population: Which cut-offs should we use? Int. J. Pediatr. Obes. 2010, 5, 458–460. [Google Scholar] [CrossRef]
- Sylvia, L.G.; Bernstein, E.E.; Hubbard, J.L.; Keating, L.; Anderson, E.J. A practical guide to measuring physical activity. J. Acad. Nutr. Diet. 2014, 114, 199–208. [Google Scholar] [CrossRef]
- Ainsworth, B.; Cahalin, L.; Buman, M.; Ross, R. The current state of physical activity assessment tools. Prog. Cardiovasc. Dis. 2015, 57, 387–395. [Google Scholar] [CrossRef]
- Tudor-Locke, C.E.; Myers, A.M. Challenges and opportunities for measuring physical activity in sedentary adults. Sports Med. 2001, 31, 91–100. [Google Scholar] [CrossRef] [PubMed]
- Dwyer, G.M.; Hardy, L.L.; Peat, J.K.; Louise, A.; Baur, L.A. The validity and reliability of a home environment preschool-age physical activity questionnaire (Pre-PAQ). Int. J. Behav. Nutr. Phys. Act. 2011, 8, 86. Available online: http://www.ijbnpa.org/content/8/1/86 (accessed on 14 September 2023). [CrossRef] [PubMed]
- Sancho, T.S.d.J. Healthy Eating and Physical Activity Intervention in Preschool Children to Prevent Obesity: A Randomized Controlled Trial. Ph.D. Thesis, Faculdade de Desporto da Universidade do Porto, Porto, Portugal, 2014. [Google Scholar]
- Burdette, H.L.; Whitaker, R.C. A national study of neighborhood safety, outdoor play, television viewing, and obesity in preschool children. Pediatrics 2005, 116, 657–662. [Google Scholar] [CrossRef] [PubMed]
- Tucker, P.; Gilliland, J. The effect of season and weather on physical activity: A systematic review. Public Health 2007, 121, 909–922. [Google Scholar] [CrossRef] [PubMed]
- Vollmer, R.L.; Adamsons, K.; Gorin, A.; Foster, J.S.; Mobley, A.R. Investigating the Relationship of Body Mass Index, Diet Quality, and Physical Activity Level between Fathers and Their Preschool-Aged Children. J. Acad. Nutr. Diet. 2015, 115, 919–926. [Google Scholar] [CrossRef]
- Skouteris, H.; Hill, B.; McCabe, M.; Swinburn, B.; Busija, L. A parent-based intervention to promote healthy eating and active behaviours in pre-school children: Evaluation of the MEND 2-4 randomized controlled trial. Pediatr. Obes. 2016, 11, 4–10. [Google Scholar] [CrossRef] [PubMed]
- Cox, R.; Skouterls, H.; Rutherford, l.; Fuller-Tyszklewlcz, M. Television viewing, television content, food intake, physical activity and body mass index: A cross-sectional study of preschool children aged 2-6 years. Health Promot. J. Aust. 2012, 23, 58–62. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guidelines on Physical Activity and Sedentary Behaviour. Geneva. 2020. Available online: https://www.who.int/publications/i/item/9789240015111 (accessed on 14 September 2023).
- Montgomery, D.C.; Peck, E.A.; Vining, G.G. Introduction to Linear Regression Analysis, 5th ed.; JohnWiley & Sons: Hoboken, NJ, USA, 2012. [Google Scholar]
- Holmes, W.H.; Rinaman, W.C. Multiple linear regression. In Statistical Literacy for Clinical Practitioners; Springer International Publishing: New York, NY, USA, 2015; pp. 367–396. [Google Scholar]
- Fariña, P.; San Martín, E.; Preiss, D.D.; Claro, M.; Jara, I. Measuring the relation between computer use and reading literacy in the presence of endogeneity. Comput. Educ. 2015, 80, 176–186. [Google Scholar] [CrossRef]
- Morgan, P.; Farkas, G.; Wu, Q. Five-Year Growth Trajectories of Kindergarten Children with Learning Difficulties in Mathematics. J. Learn. Disabil. 2009, 42, 306–321. [Google Scholar] [CrossRef]
- Chong, S.L.; Siegel, L. Stability of computational deficits in math learning disability from second through fifth grades. Dev. Neuropsychol. 2008, 33, 300–317. [Google Scholar] [CrossRef]
- Fuchs, L.S.; Fuchs, D.; Prentice, K. Responsiveness to mathematical problem-solving instruction: Comparing students at risk of mathematics disability with and without risk of reading disability. J. Learn. Disabil. 2004, 37, 293–306. [Google Scholar] [CrossRef] [PubMed]
- Claesens, A.; Engel, M. How important is where you start? Early mathematics knowledge and later school success. Teach. Coll. Rec. 2013, 115, 1–29. [Google Scholar] [CrossRef]
- Pitchford, N.J.; Papini, C.; Outhwaite, L.A.; Guillford, A. Fine motor skills predict maths ability better than they predict reading ability in the early primary school years. Front. Psychol. 2016, 7, 783. [Google Scholar] [CrossRef] [PubMed]
- Handel, A.J.; Lozoff, B.; Breiilh, J.; Harlow, S.D. Sociodemographic and nutritional correlates of neurobehavioral development- A study of young children in a rural region of Ecuador. Rev. Panam. Salud Publica 2007, 21, 292–300. [Google Scholar] [CrossRef] [PubMed]
- Strooband, K.; de Rosnay, M.; Okely, A. Prevalence and risk factors of pre-schoolers’ fine motor delay within vulnerable Australian communities. J. Paediatr. Child Health 2020, 57, 114–120. [Google Scholar] [CrossRef] [PubMed]
- Bello, A.I.; Quartey, J.N.; Appiah, L.A. Screening for developmental delay among children attending a rural community welfare clinic in Ghana. BMC Pediatr. 2013, 13, 119. [Google Scholar] [CrossRef] [PubMed]
- Troude, P.; Squires, J.; L’Helias, L.F.; Bouyer, J.; de La Rochebrochard, E. Ages and Stages Questionnaires: Feasibility of postal surveys for child follow-up. Early Hum. Dev. 2011, 87, 671–676. [Google Scholar] [CrossRef] [PubMed]
- Goyen, T.; Lui, K. Longitudinal motor development of apparently normal high-risk infants at 18 months, 3 and 5 years. Early Hum. Dev. 2002, 70, 103–115. [Google Scholar] [CrossRef]
- Coetzee, D.; Gerber, B. Difference between visual-motor integration status of typically developed learners and learners with learning-related problems. S. Afr. J. Res. Sport Phys. Educ. Recreat. 2018, 40, 41–52. [Google Scholar]
- Cook, C.J.; Howard, S.J.; Scerif, G.; Twine, R.; Kahn, K.; Norris, S.A.; Draper, C.E. Associations of physical activity and gross motor skills with executive function in preschool children from low-income South African settings. Dev. Sci. 2019, 22, e12820. [Google Scholar] [CrossRef]
- Draper, C.E.; Achmat, M.; Forbes, J.; Lambert, E.V. Impact of a community-based programme for motor development on gross motor skills and cognitive function in preschool children from disadvantaged settings. Early Child Dev. Care 2012, 182, 137–152. [Google Scholar] [CrossRef]
- Draper, C.E.; Tomaz, S.A.; Stone, M.; Hinkley, T.; Jones, R.A.; Louw, J.; Twine, R.; Kahn, K.; Norris, S.A. Developing intervention strategies to optimise body composition in early childhood in South Africa. BioMed Res. Int. 2017, 2017, 5283457. [Google Scholar] [CrossRef] [PubMed]
- Cameron, C.E.; Cottone, E.; Murrah, W.M.; Grissmer, D. How ae motor skills linked to Children’s school performance and academic achievement? Child Dev. Perspect. 2016, 10, 93–98. [Google Scholar] [CrossRef]
- Ommundsen, Y.; Gundersen, K.A.; Mjaavatn, P.E. Fourth graders’ social standing with peers: A prospective study on the role of first grade physical activity, weight status, and motor proficiency. Scand. J. Educ. Res. 2010, 54, 377–394. [Google Scholar] [CrossRef]
- Hamilton, M.; Liu, T. The effects of an intervention on the gross and fine motor skills of Hispanic Pre-K children from low ses backgrounds. Early Child. Educ. J. 2018, 46, 223–230. [Google Scholar] [CrossRef]
- Logan, S.W.; Webster, E.K.; Getchell, N.; Pfeiffer, K.A.; Robinson, L.E. Relationship between fundamental motor skill competence and physical activity during childhood and adolescence: A systematic review. Kinesiol. Rev. 2015, 4, 416–426. [Google Scholar] [CrossRef]
- Rito, A.; Mendes, S.; Faria, M.C.; Carvalho, R.; Santos, T.; Cardoso, S.; Feliciano, E.; Silvério, R.; Sancho, T.S.; Dinis, A.; et al. Childhood Obesity Surveillance Initiative: COSI Portugal; Instituto Nacional de Saúde Doutor Ricardo Jorge IP: Lisbon, Portugal, 2022; ISBN 978-989-8794-92-5. [Google Scholar]
- Li, W.; Rukavina, P. A review on coping mechanisms against obesity bias in physical activity/education settings. Obes. Rev. 2009, 10, 87–95. [Google Scholar] [CrossRef]
- Gale, C.R.; Batty, G.D.; Cooper, C.; Deary, I.J. Psychomotor coordination and intelligence in childhood and health in adulthood-testing the system integrity hypothesis. Psychosom. Med. 2009, 71, 675–681. [Google Scholar] [CrossRef]
- Osika, W.; Montgomery, S.M. Physical control and coordination in childhood and adult obesity: Longitudinal Birth Cohort Study. BMJ 2008, 337, a699. [Google Scholar] [CrossRef]
- Avila, C.; Holloway, A.C.; Hahn, M.K.; Morrison, K.M.; Restivo, M.; Anglin, R.; Taylor, V.H. An overview of links between obesity and mental health. Curr. Obes. Rep. 2015, 4, 303–310. [Google Scholar] [CrossRef]
- Gmeiner, M.S.; Warschburger, P. Psychotherapie bei juvenile Adipositas: Gerechtfertigt und sinnvoll? Psychotherapeut 2021, 66, 16–22. [Google Scholar] [CrossRef]
- Lanigan, J.; Barber, S.; Singhal, A. Prevention of obesity in preschool children. Proc. Nutr. Soc. 2010, 69, 204–210. [Google Scholar] [CrossRef] [PubMed]
- Carlson, A.G.; Rowe, E.W.; Curby, T.W. Disentangling fine motor skills’ relation to academic achievement: The differential impact of visual-spatial integration and visual motor coordination. J. Genet. Psychol. 2013, 174, 514–533. [Google Scholar] [CrossRef] [PubMed]
- Maurer, M.N.; Roebers, C.M. New insights into visual-motor integration exploring process measures during copying shapes. Psychol. Sport Exerc. 2021, 55, 101954. [Google Scholar] [CrossRef]
- Kim, H.; Murrah, W.M.; Cameron, C.E.; Brock, L.L.; Cottone, E.A.; Grissmer, D. Psychometric properties of the teacher-reported Motor Skills Rating Scale. J. Psychoeduc. Assess. 2015, 33, 640–651. [Google Scholar] [CrossRef]
- Webster, E.K.; Martin, C.K.; Staiano, A.E. Fundamental Motor Skills, Screen-Time, and Physical Activity in Preschoolers. J. Sport Health Sci. 2019, 8, 114–121. [Google Scholar] [CrossRef]
- Lipkin, P.H. Motor Development and Dysfunction. In Developmental-Behavioral Pediatrics, 4th ed.; Saunders: Philadelphia, PA, USA, 2009; pp. 643–652. [Google Scholar] [CrossRef]
- Cameron, C.E.; Brock, L.L.; Murrah, W.M.; Bell, L.H.; Worzalla, S.L.; Grissmer, D.; Morrison, F.J. Fine Motor Skills and Executive Function Both Contribute to Kindergarten Achievement. Child Dev. 2012, 83, 1229–1244. [Google Scholar] [CrossRef]
- Dayem, T.S.A.E.; Salem, E.E.; Hadidy, E.I.E. Correlation between Gross Motor Activities and Hand Writing Skills in Elementary School Children. Trends Appl. Sci. Res. 2015, 10, 259–269. [Google Scholar] [CrossRef][Green Version]
- Maurer, M.N.; Roebers, C.M. Towards a better understanding of the association between motor skills and executive functions in 5-to 6-year-olds: The impact of motor task difficulty. Hum. Mov. Sci. 2019, 66, 607–620. [Google Scholar] [CrossRef]
- Tortella, P.; Haga, M.; Loras, H.; Sigmundsson, H.; Fumagalli, G. Motor Skill Development in Italian Pre-School Children Induced by Structured Activities in a Specific Playground. PLoS ONE 2016, 11, e0160244. [Google Scholar] [CrossRef]
- Amaro, N.; Coelho, L.; Cruz, J.; Matos, R.; Morouço, P. Correlation between Fine and Gross Motor Coordination in Children. Rev. Saúde Públ. Leiria 2014, 48, 273. [Google Scholar]
- Suggate, S.; Stoeger, H.; Fischer, U. Finger-based numerical skills link fine motor skills to numerical development in preschoolers. Percept. Mot. Ski. 2017, 124, 1085–1106. [Google Scholar] [CrossRef] [PubMed]
- Sorgente, V.; Cohen, E.J.; Bravi, R.; Minciacchi, D. Crosstalk between Gross and Fine Motor Domains during Late Childhood: The Influence of Gross Motor Training on Fine Motor Performances in Primary School Children. Int. J. Environ. Res. Public Health 2021, 18, 11387. [Google Scholar] [CrossRef] [PubMed]
- Flatters, I.; Mushtaq, F.; Hill, L.J.B.; Rossiter, A.; Jarrett-Peet, K.; Culmer, P.; Holt, R.; Wilkie, R.M.; Mon-Williams, M. Children’s Head Movements and Postural Stability as a Function of Task. Exp. Brain Res. 2014, 232, 1953–1970. [Google Scholar] [CrossRef] [PubMed]
- Payne, V.G.; Isaacs, L.D. Human Motor Development: A Lifespan Approach; McGraw-Hill: New York, NY, USA, 2012. [Google Scholar]
- Wang, X.Q.; Chen, H.X.; Ma, H.J.; Guo, X.R.; Cui, X.H. Investigation on gross motor development of preschool children and analysis of influencing factors. Chin. J. Child Health Care 2015, 23, 188–191. [Google Scholar]
- Zhang, Y.; Cai, G.L.; Zhao, C.Q.; Wang, C.X.; Wang, D.D. Research progress of children’s motor development from the perspective of human motor development. Sichuan Sports Sci. 2019, 38, 37–39. [Google Scholar] [CrossRef]
- Fang, Y.; Wang, J.; Zhang, Y.; Qin, J. The relationship of motor coordination, visual perception, and executive function to the development of 4-6-year-old Chinese preschoolers’ visual motor integration skills. BioMed Res. Int. 2017, 62, 42–54. [Google Scholar] [CrossRef]
- Wassenberg, R.; Feron, F.J.; Kessels, A.G.; Hendriksen, J.G.; Kalff, A.C.; Kroes, M.; Hurks, P.P.; Beeren, M.; Jolles, J.; Vles, J.S. Relation between cognitive and motor performance in 5- to 6-year-old children- results from a large-scale cross-sectional study. Child. Dev. 2005, 76, 1092–1103. [Google Scholar] [CrossRef]
- Roth, K.; Ruf, K.; Obinger, M.; Mauer, S.; Ahnert, J.; Schneider, W.; Graf, C.; Hebestreit, H. Is there a secular decline in motor skills in preschool children? Scand. J. Med. Sci. Sports 2010, 20, 670–678. [Google Scholar] [CrossRef]
- Hinkley, T.; Salmon, J.; Okely, A.D.; Crawford, D.; Hesketh, K. Preschoolers’ physical activity, screen time, and compliance with recommendations. Med. Sci. Sports Exerc. 2012, 44, 458–465. [Google Scholar] [CrossRef]
- Jylänki, P.; Mbay, T.; Hakkarainen, A.; Arja Sääkslahti, A.; Aunio, P. The effects of motor skill and physical activity interventions on preschoolers’ cognitive and academic skills: A systematic review. Prev. Med. 2022, 155, 106948. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.Y. Differences between Preschool Children Using Tablets and Non-Tablets in Visual Perception and Fine Motor Skills. Hong Kong J. Occup. Ther. 2019, 32, 118–126. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.Y.; Cherng, R.J.; Chen, Y.J. Effect of Touch Screen Tablet Use on Fine Motor Development of Young Children. Phys. Occup. Ther. Pediatr. 2017, 37, 457–467. [Google Scholar] [CrossRef] [PubMed]
- Morris, T.H.; Rohs, M. The Potential for Digital Technology to Support Self-Directed Learning in Formal Education of Children: A Scoping Review. Interact. Learn. Environ. 2023, 31, 1974–1987. [Google Scholar] [CrossRef]
- Stevens, J.; Murray, D.M.; Baggett, C.D.; Elder, J.P.; Lohman, T.G.; Lytle, L.A.; Pate, R.R.; Pratt, C.A.; Treuth, M.S.; Webber, L.S.; et al. Objectively assessed associations between physical activity and body composition in middle-school girls: The Trial of Activity for Adolescent Girls. Am. J. Epidemiol. 2007, 166, 1298–1305. [Google Scholar] [CrossRef] [PubMed]
- Ward, D.S.; Vaughn, A.; McWilliams, C.; Hales, D. Interventions for increasing physical activity at child care. Med. Sci. Sports Exerc. 2010, 42, 526–534. [Google Scholar] [CrossRef]
- Clark, J.E. From the beginning: A developmental perspective on movement and mobility. Quest 2005, 57, 37–45. [Google Scholar] [CrossRef]
- Macdonald, K.; Milne, N.; Orr, R.; Pope, R. Associations between motor proficiency and academic performance in mathematics and reading in year 1 school children: A cross-sectional study. BMC Pediatr. 2020, 20, 69. [Google Scholar] [CrossRef]
- Gagen, L.M.; Getchell, N. Using ‘constraints’ to design developmentally appropriate movement activities for early childhood education. Early Child. Educ. J. 2006, 34, 227–232. [Google Scholar] [CrossRef]
- Dapp, L.C.; Roebers, C.M. The mediating role of self-concept between sports-related physical activity and mathematical achievement in fourth graders. Int. J. Environ. Res. Public Health 2019, 16, 2658. [Google Scholar] [CrossRef]
- Dapp, L.C.; Gashaj, V.; Roebers, C.M. Physical activity and motor skills in children: A differentiated approach. Psychol. Sport Exerc. 2021, 54, 101916. [Google Scholar] [CrossRef]
- Cueto, S.; Prieto, J.; Nistal, P.; Abelairas-Gómez, C.; Barcala, R.; López, S. Teachers’ perceptions of preschool children’s psychomotor development in Spain. Percept. Mot. Skills 2017, 124, 725–739. [Google Scholar] [CrossRef] [PubMed]
- Geertsen, S.S.; Thomas, R.; Larsen, M.N.; Dahn, I.M.; Andersen, J.K.; Krause-Jensen, M.; Korup, V.; Nielsen, C.M.; Wienecke, J.; Ritz, C.; et al. Motor skills and exercise capacity are associated with objective measures of cognitive functions and academic performance in preadolescent children. PLoS ONE 2016, 11, e0161960. [Google Scholar] [CrossRef] [PubMed]
- Tsangaridou, N. Early childhood teachers’ views about teaching physical education: Challenges and recommendations. Phys. Educ. Sport Pedagogy 2017, 22, 283–300. [Google Scholar] [CrossRef]
- Bar-Haim, Y.; Bart, O. Motor function and social participation in kindergarten children. Soc. Dev. 2006, 15, 296–310. [Google Scholar] [CrossRef]
- Øksendal, E.; Brandlistuen, R.E.; Wolke, D.; Helland, S.S.; Holte, A.; Wang, M.V. Associations between language difficulties, peer victimization, and bully perpetration from 3 through 8 years of age: Results from a population-based study. J. Speech Lang. Hear. Res. 2021, 64, 2698–2714. [Google Scholar] [CrossRef] [PubMed]
- Escolano-Pérez, E.; Sánchez-López, C.R.; Herrero-Nivela, M.L. Early Environmental and Biological Influences on Preschool Motor Skills: Implications for Early Childhood Care and Education. Front. Psychol. 2021, 12, 725832. [Google Scholar] [CrossRef]
- Honrubia-Montesinos, C.; Gil-Madrona, P.; Losada-Puente, L. Motor development among spanish preschool children. Children 2021, 8, 41. [Google Scholar] [CrossRef]
- Draper, C.E.; Tomaz, S.A.; Jones, R.A.; Hinkley, T.; Twine, R.; Kahn, K.; Norris, S.A. Cross-sectional associations of physical activity and gross motor proficiency with adiposity in South African children of pre-school age. Public Health Nutr. 2018, 22, 614–623. [Google Scholar] [CrossRef]
- Jones, S.; Hendricks, S.; Draper, C.E. Assessment of physical activity and sedentary behavior at preschools in Cape Town, South Africa. Child Obes. 2014, 10, 501–510. [Google Scholar] [CrossRef]
- te Velde, S.J.; van Nassau, F.; Uijtdewilligen, L.; van Stralen, M.M.; Cardon, G.; De Craemer, M.; Manios, Y.; Brug, J.; Chinapaw, M.J.; ToyBox-Study Group. Energy balance-related behaviours associated with overweight and obesity in preschool children: A systematic review of prospective studies. Obes. Rev. 2012, 13, 56–74. [Google Scholar] [CrossRef] [PubMed]
- Kuhl, E.S.; Clifford, L.M.; Stark, L.J. Obesity in preschoolers: Behavioral correlates and directions for treatment. Obesity 2012, 20, 3–29. [Google Scholar] [CrossRef] [PubMed]
- Kakebeeke, T.; Lanzi, S.; Zysset, A.; Arhab, A.; Messerli-Bürgy, N.; Stuelb, K.; Leeger-Aschmann, C.S.; Schmutz, E.A.; Meyer, A.H.; Kriemler, S.; et al. Association between Body Composition and Motor Performance in Preschool Children. Obes. Facts. 2017, 10, 420–431. [Google Scholar] [CrossRef] [PubMed]
- Castetbon, K.; Andreyeva, T. Obesity and motor skills among 4 to 6-year-old children in the United States: Nationally-representative surveys. BMC Pediatr. 2012, 12, 28. [Google Scholar] [CrossRef] [PubMed]
- Okely, A.D.; Booth, M.L.; Chey, T. Relationships between body composition and fundamental movement skills among children and adolescents. Res. Q. Exerc. Sport 2004, 75, 238–247. [Google Scholar] [CrossRef] [PubMed]
- Prskalo, I.; Badric, M.; Kunjesic, M. The percentage of body fat in children and the level of their motor skills. Coll. Antropol. 2015, 1, 21–28. [Google Scholar]
- Barnett, L.M.; Lai, S.K.; Veldman, S.L.C.; Hardy, L.L.; Cliff, D.P.; Morgan, P.J.; Zask, A.; Lubans, D.R.; Shultz, S.P.; Ridgers, N.D.; et al. Correlates of gross motor competence in children and adolescents: A systematic review and meta-analysis. Sports Med. 2016, 46, 1663–1688. [Google Scholar] [CrossRef]
- Morano, M.; Colella, D.; Caroli, M. Gross motor skill performance in a sample of overweight and non-overweight preschool children. Int. J. Pediatr. Obes. 2011, 6, 42–46. [Google Scholar] [CrossRef]
- Spessato, B.; Gabbard, C.; Robinson, L.; Valentini, N. Body mass index, perceived and actual physical competence: The relationship among young children. Child Care Health Dev. 2013, 39, 845–850. [Google Scholar] [CrossRef]
- D’Hondt, E.; Gentier, I.; Deforche, B.; Tanghe, A.; De, B.I.; Lenoir, M. Weight loss and improved gross motor coordination in children as a result of multidisciplinary residential obesity treatment. Obesity 2011, 19, 1999–2005. [Google Scholar] [CrossRef]
- St Laurent, C.W.; Burkart, S.; Andre, C.; Spencer, R.M. Physical Activity, Fitness, School Readiness, and Cognition in Early Childhood: A Systematic Review. J. Phys. Act. Health 2021, 18, 1004–1013. [Google Scholar] [CrossRef] [PubMed]
- Moreau, D.; Morrison, A.B.; Conway, A.R. An ecological approach to cognitive enhancement: Complex motor training. Acta Psychol. 2015, 157, 44–55. [Google Scholar] [CrossRef] [PubMed]
- Tomporowski, P.D.; Davis, C.L.; Miller, P.H.; Naglieri, J.A. Exercise and children’s intelligence, cognition, and academic achievement. Educ. Psychol. Rev. 2008, 20, 111–131. [Google Scholar] [CrossRef] [PubMed]
- Koutsandréou, F.; Wegner, M.; Niemann, C.; Budde, H. Effects of motor vs. cardiovascular exercise training on children’s working memory. Med. Sci. Sports Exerc. 2016, 48, 1144–1152. [Google Scholar] [CrossRef] [PubMed]
- Pesce, C.; Crova, C.; Marchetti, M.; Struzzolino, I.; Masci, I.; Vannozzi, G.; Forte, R. Searching for cognitively optimal challenge point in physical activity for children with typical and atypical motor development. Ment. Health Phys. Act. 2013, 6, 172–180. [Google Scholar] [CrossRef]
- Schmidt, M.; Egger, F.; Benzing, V.; Jäger, K.; Conzelmann, A.; Roebers, C.M.; Pesce, C. Disentangling the relationship between children’s motor ability, executive function and academic achievement. PLoS ONE 2017, 12, e0182845. [Google Scholar] [CrossRef] [PubMed]
- Escolano-Pérez, E.; Herrero-Nivela, M.L.; Losada, J.L. Association Between Preschoolers’ Specific Fine (But Not Gross) Motor Skills and Later Academic Competencies: Educational Implications. Front. Psychol. 2020, 11, 1044. [Google Scholar] [CrossRef] [PubMed]
- Hudson, K.N.; Ballou, H.M.; Willoughby, M.T. Short report: Improving motor competence skills in early childhood has corollary benefits for executive function and numeracy skills. Dev. Sci. 2021, 24, e13071. [Google Scholar] [CrossRef]
- Kim, H.; Duran, C.A.K.; Cameron, C.E.; Grissmer, D. Developmental relations among motor and cognitive processes and mathematics skills. Child Dev. 2018, 89, 476–494. [Google Scholar] [CrossRef]
- Cameron, C.E.; Brock, L.; Hatfield, B.; Cottone, E.; Rubinstein, E.; LoCasale-Crouch, J.; Grissmer, D. Visuomotor integration and inhibitory control compensate for each other in school readiness. Dev. Psychol. 2015, 51, 1529–1543. [Google Scholar] [CrossRef]
- Luo, Z.; Jose, P.; Huntsinger, C.; Pigott, T. Fine motor skills and mathematics achievement in East Asian American and European American kindergartners and first graders. Br. J. Dev. Psychol. 2007, 25, 595–614. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).