Effectiveness on Quality of Life and Life Satisfaction for Older Adults: A Systematic Review and Meta-Analysis of Life Review and Reminiscence Therapy across Settings
Abstract
:1. Introduction
2. Methods
2.1. Search Strategy
2.2. Study Selection
2.3. Data Extraction
2.4. Quality Assessment
2.5. Data Synthesis and Analysis
3. Results
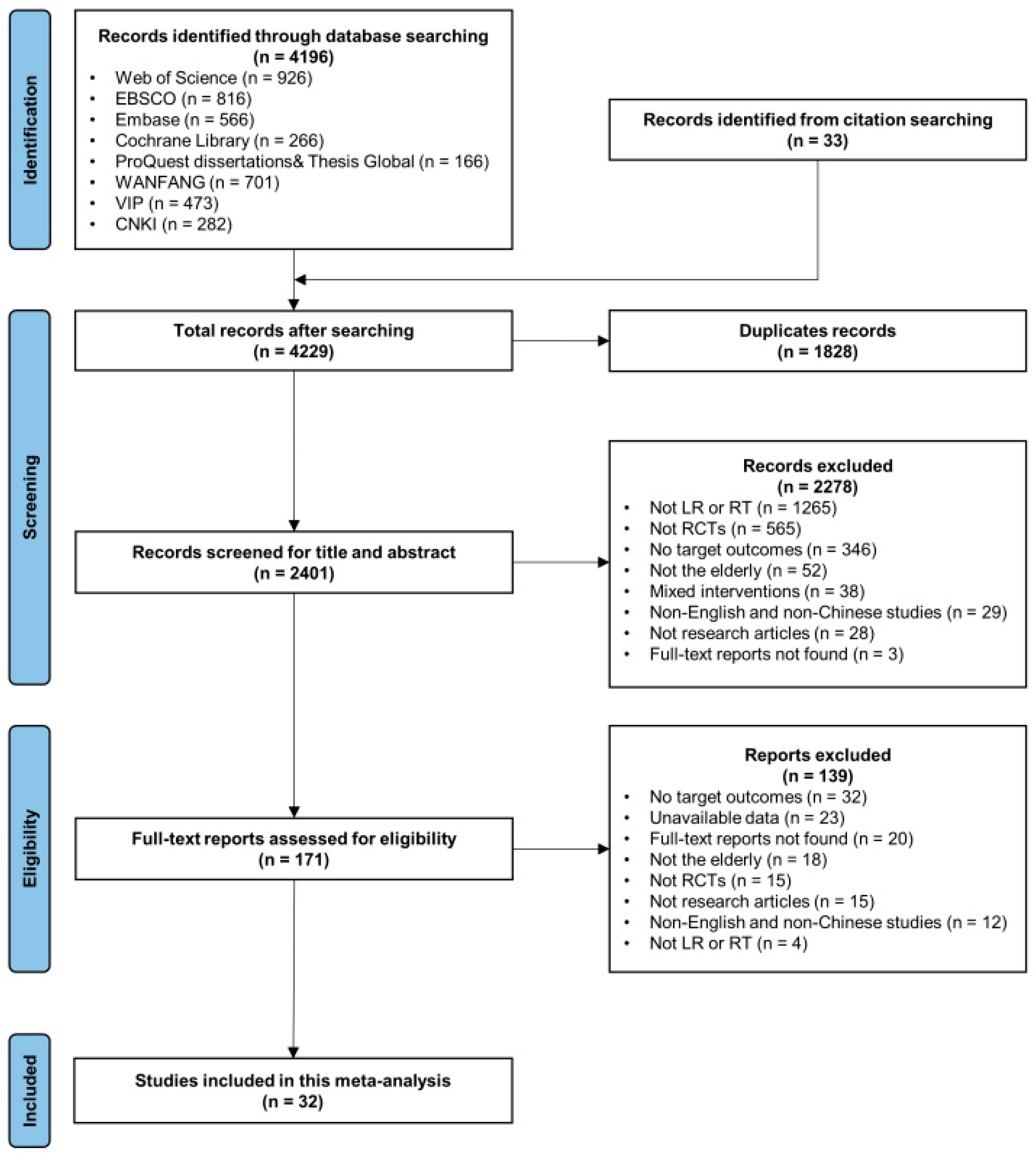
3.1. Study Selection
3.2. Study Characteristics
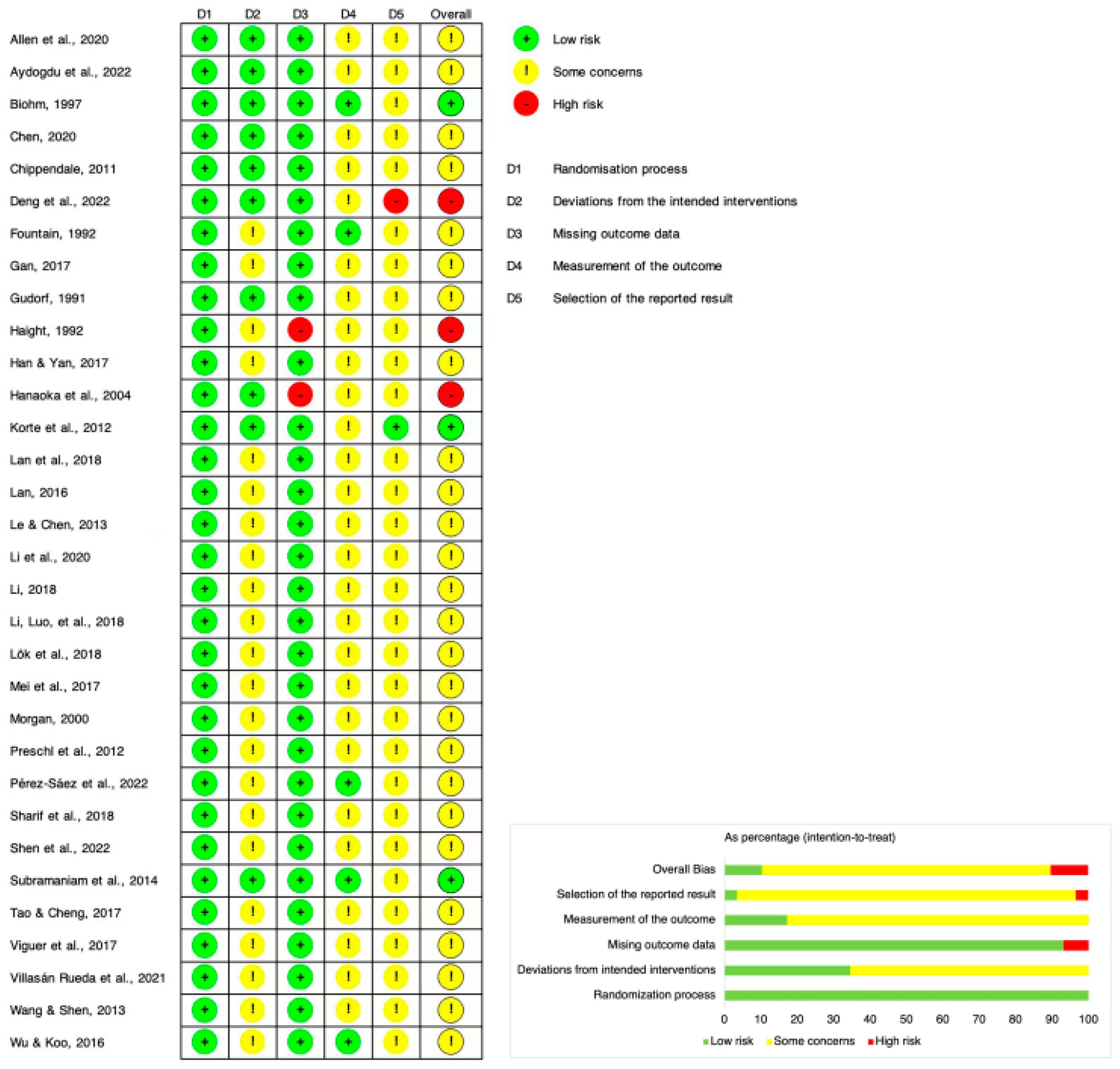
3.3. Risk of Bias
3.4. Main Outcomes
3.4.1. Quality of Life
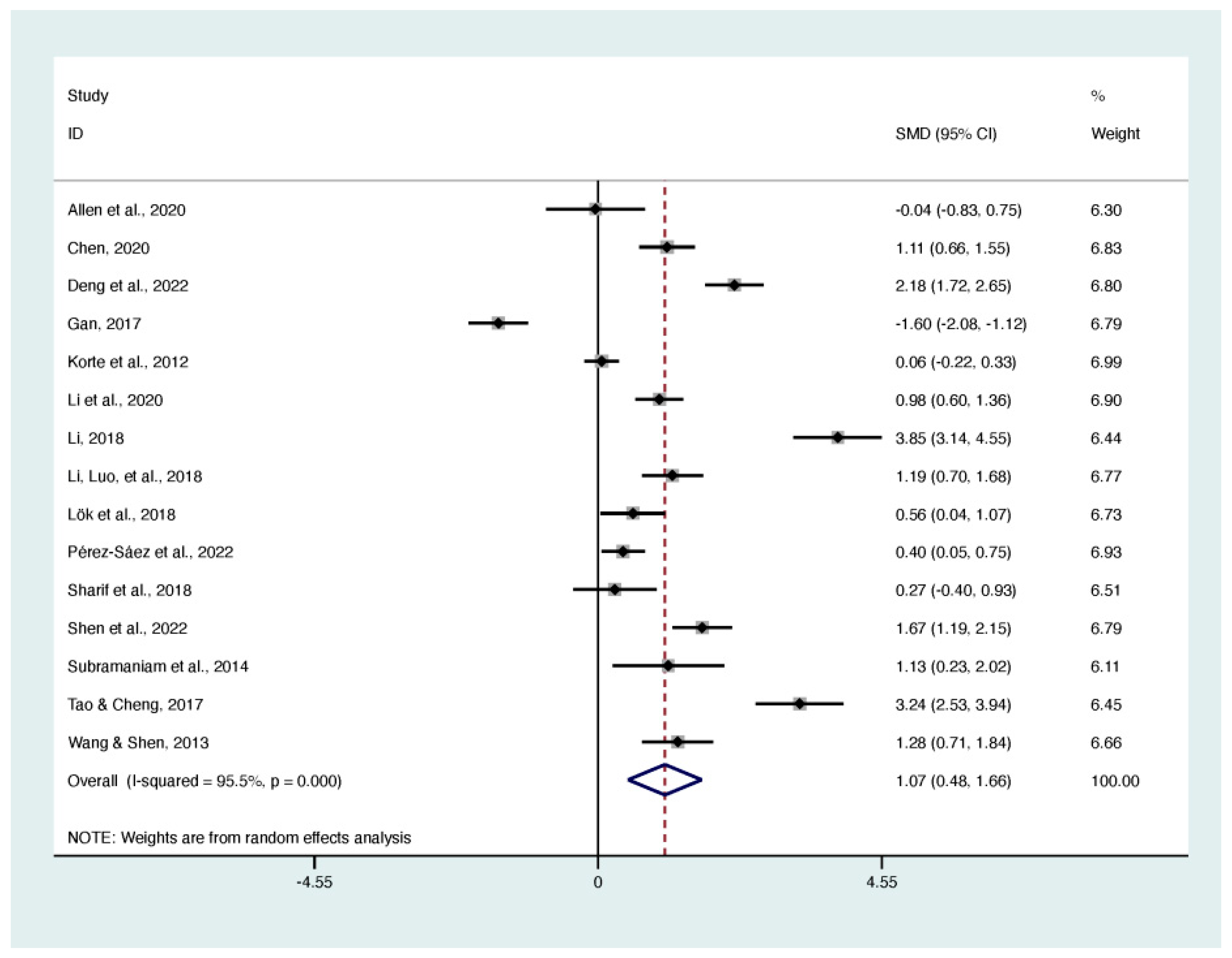
3.4.2. Life Satisfaction
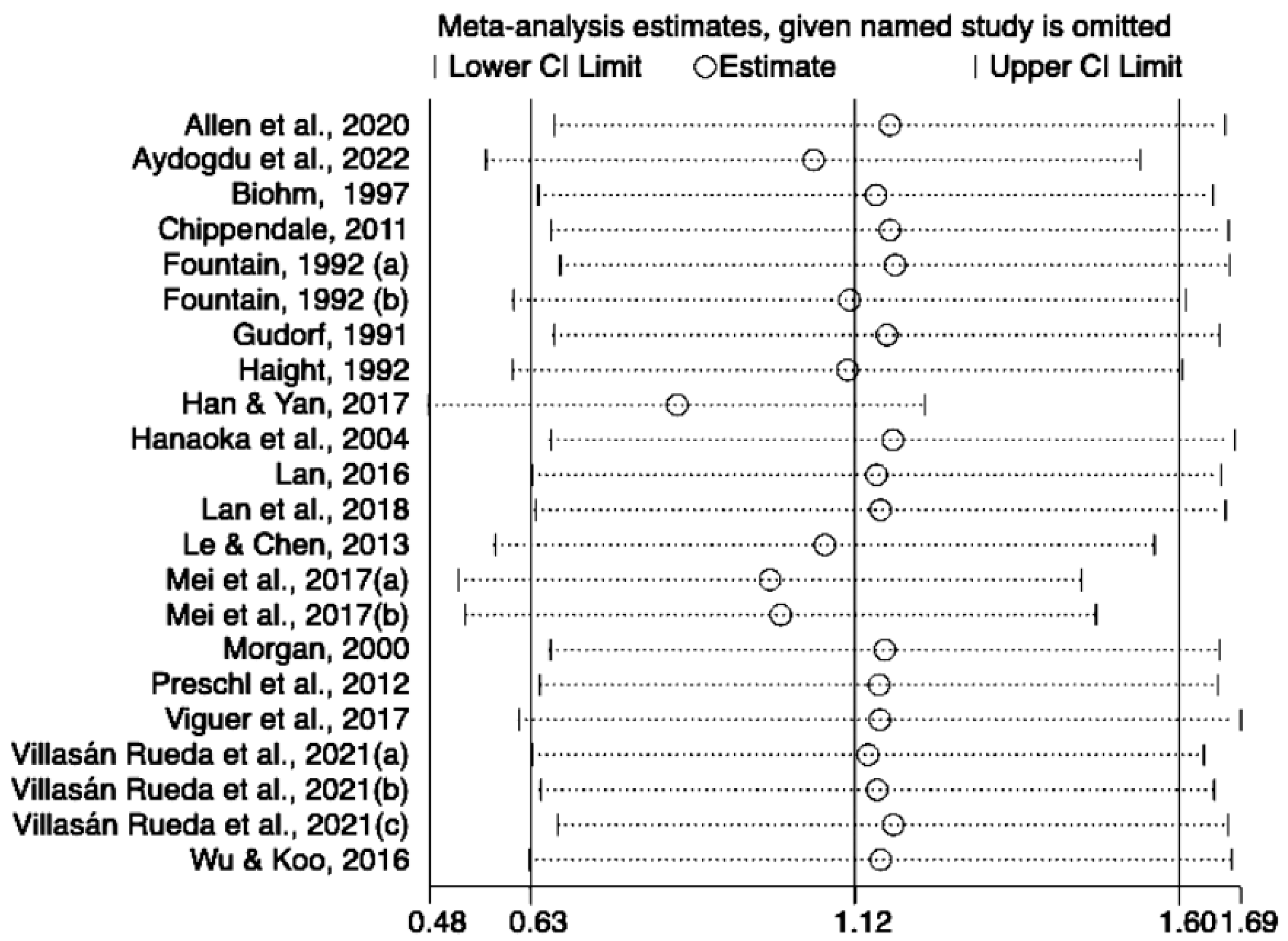
3.5. Sensitivity Analysis
3.6. Meta-Regression and Subgroup Analysis
3.6.1. Quality of Life
3.6.2. Life Satisfaction
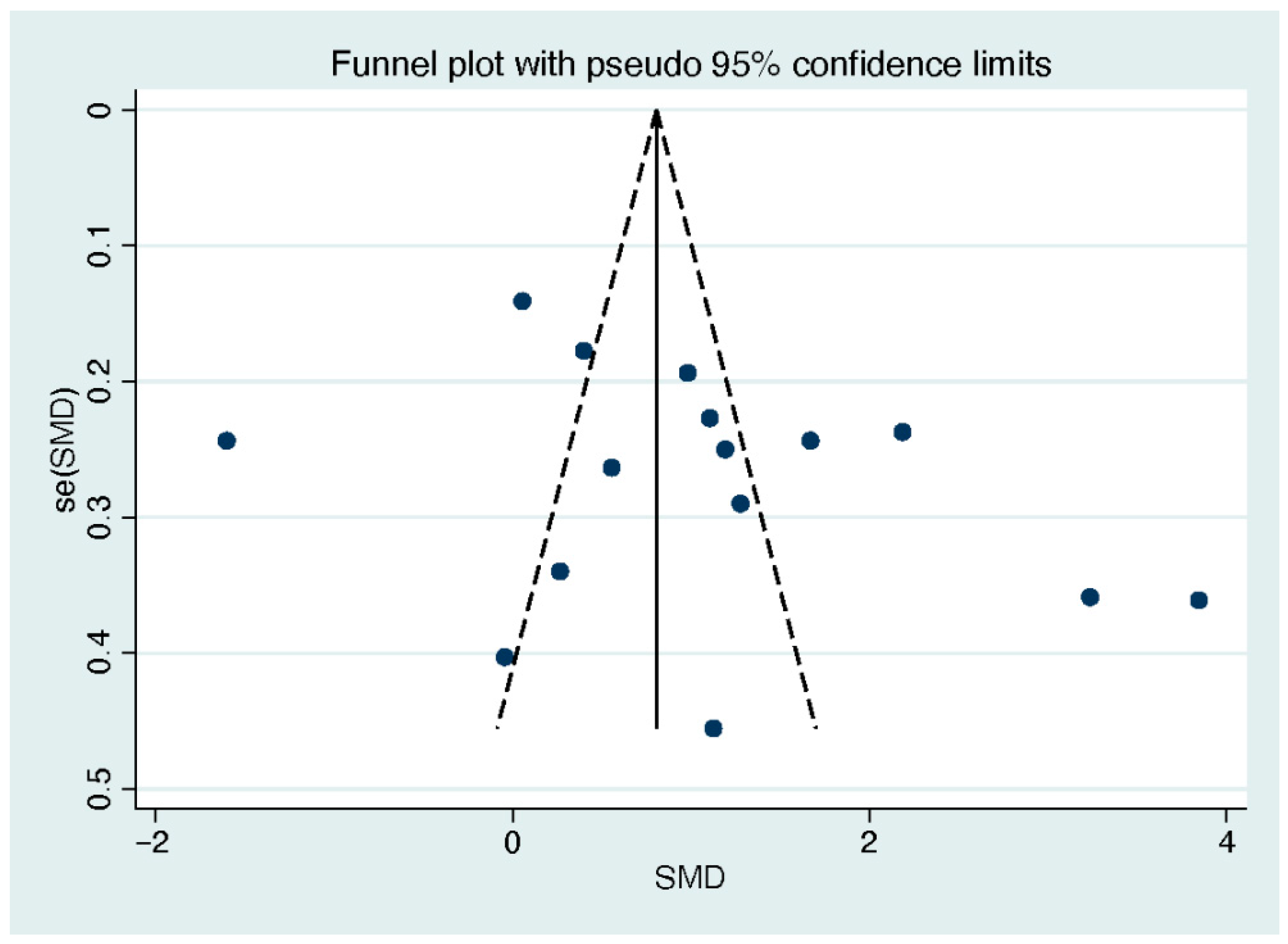
3.7. Publication Bias
4. Discussion
4.1. Main Findings
4.2. Implications for Future Studies
4.3. Strengths and Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Ageing and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 13 March 2023).
- World Health Organization. Active Ageing: A Policy Framework. World Health Organization. 2002. Available online: https://apps.who.int/iris/handle/10665/67215 (accessed on 7 June 2023).
- Bar-Tur, L. Fostering Well-Being in the Elderly: Translating Theories on Positive Aging to Practical Approaches. Front. Med. 2021, 8, 517226. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Mayoralas, G.; Rojo-Pérez, F.; Martínez-Martín, P.; Prieto-Flores, M.-E.; Rodríguez-Blázquez, C.; Martín-García, S.; Rojo-Abuín, J.-M.; Forjaz, M.-J. Active ageing and quality of life: Factors associated with participation in leisure activities among institutionalized older adults, with and without dementia. Aging Ment. Health 2015, 19, 1031–1041. [Google Scholar] [CrossRef] [PubMed]
- Steptoe, A.; Deaton, A.; Stone, A.A. Subjective wellbeing, health, and ageing. Lancet 2015, 385, 640–648. [Google Scholar] [CrossRef] [PubMed]
- Butler, R.N. The Life Review: An Interpretation of Reminiscence in the Aged. Psychiatry 1963, 26, 65–76. [Google Scholar] [CrossRef] [PubMed]
- Yan, Z.; Dong, M.; Lin, L.; Wu, D. Effectiveness of reminiscence therapy interventions for older people: Evidence mapping and qualitative evaluation. J. Psychiatr. Ment. Health Nurs. 2023, 30, 375–388. [Google Scholar] [CrossRef]
- Haber, D. Life review: Implementation, theory, research, and therapy. Int. J. Aging Hum. Dev. 2006, 63, 153–171. [Google Scholar] [CrossRef]
- Korte, J.; Majo, M.C.; Bohlmeijer, E.T.; Westerhof, G.J.; Smit, F. Cost-effectiveness of life-review for older adults with moderate depressive symptomatology: A pragmatic randomized controlled trial. J. Aging Stud. 2015, 34, 146–154. [Google Scholar] [CrossRef]
- Liu, Z.; Yang, F.; Lou, Y.; Zhou, W.; Tong, F. The Effectiveness of Reminiscence Therapy on Alleviating Depressive Symptoms in Older Adults: A Systematic Review. Front. Psychol. 2021, 12, 709853. [Google Scholar] [CrossRef]
- Schweighoffer, R.; Schumacher, A.M.; Blaese, R.; Walter, S.; Eckstein, S. A Systematic Review and Bayesian Network Meta-Analysis Investigating the Effectiveness of Psychological Short-Term Interventions in Inpatient Palliative Care Settings. Int. J. Environ. Res. Public Health 2022, 19, 7711. [Google Scholar] [CrossRef]
- Saragih, I.D.; Tonapa, S.I.; Yao, C.; Saragih, I.S.; Lee, B. Effects of reminiscence therapy in people with dementia: A systematic review and meta-analysis. J. Psychiatr. Ment. Health Nurs. 2022, 29, 883–903. [Google Scholar] [CrossRef]
- Woods, B.; O’Philbin, L.; Farrell, E.M.; Spector, A.E.; Orrell, M. Reminiscence therapy for dementia. Cochrane Database Syst. Rev. 2018, 3, CD001120. [Google Scholar] [CrossRef] [PubMed]
- Lan, X.; Xiao, H.; Chen, Y. Effects of life review interventions on psychosocial outcomes among older adults: A systematic review and meta-analysis. Geriatr. Gerontol. Int. 2017, 17, 1344–1357. [Google Scholar] [CrossRef] [PubMed]
- Shin, E.; Kim, M.; Kim, S.; Sok, S. Effects of Reminiscence Therapy on Quality of Life and Life Satisfaction of the Elderly in the Community: A Systematic Review. BMC Geriatr. 2023, 23, 420. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Xu, H.; Sui, X.; Zeng, T.; Leng, X.; Li, Y.; Li, F. Effects of Group Reminiscence Interventions on Depressive Symptoms and Life Satisfaction in Older Adults with Intact Cognition and Mild Cognitive Impairment: A Systematic Review. Arch. Gerontol. Geriatr. 2023, 114, 105103. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int. J. Surg. 2021, 372, n71. [Google Scholar] [CrossRef]
- Zhong, Q.; Chen, C.; Chen, S. Effectiveness of Life Review and Reminiscence for Active Ageing: A Systematic Review and Meta-Analysis. PROSPERO 2023 CRD42023424085. Available online: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42023424085 (accessed on 4 September 2023).
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions Version 6 (Updated July 2019). Available online: http://www.training.cochrane.org/handbook (accessed on 13 March 2023).
- Allen, A.P.; Doyle, C.; Roche, R.A.P. The impact of reminiscence on autobiographical memory, cognition and psychological well-being in healthy older adults. Eur. J. Psychol. 2020, 16, 317–330. [Google Scholar] [CrossRef]
- Aydogdu, O.; Tastan, S.; Kublay, G. The effects of the instrumental reminiscence therapy based on Roy’s adaptation model on adaptation, life satisfaction and happiness in older people: A randomized controlled trial. Int. J. Nurs. Pract. 2022, 9, e13101. [Google Scholar] [CrossRef]
- Biohm, K.A. The Use of A Group Reminiscence Intervention with Newly Admitted Nursing Home Residents. Ph.D. Thesis, The California School of Professional Psychology, San Diego, CA, USA, 1997. [Google Scholar]
- Chen, S.Y. Nostalgia therapy in the care of elderly stroke patients. Chin. Remedies Clin. 2020, 20, 1017–1019. [Google Scholar]
- Chippendale, T. The Effects of Life Review through Writing on Depressive Symptoms and Life Satisfaction in Older Adults. Ph.D. Thesis, The Steinhardt School of Culture, Education, and Human Development New York University, New York, NY, USA, 2011. [Google Scholar]
- Deng, R.Y.; Wei, J.; Qi, S.L. Effects of reminiscence therapy on mental health and cardiac rehabilitation in elderly patients with postoperative depression after PCI for myocardial infarction. Anhui Med. J. 2022, 43, 800–804. [Google Scholar] [CrossRef]
- Fountain, D.E. Life Review Groups: An Experimental Study of Religiosity, Life Satisfaction and Concomitant Behavioral Changes in Residents of Long Term Care Facilities. Ph.D. Thesis, The Ellen Whiteside McDonnell School of Social Work, Miami, FL, USA, 1992. [Google Scholar]
- Gan, L.B. Observation on the application effect of nostalgia therapy in the care of elderly dementia patients. Nurs. Res. 2017, 45, 1006–6845. [Google Scholar]
- Gudorf, G.E. The Effects of Life Review Therapy with Elderly Nursing Home Patients. Ph.D. Thesis, Institute for Clinical Social Work, Chicago, IL, USA, 1991. [Google Scholar]
- Haight, B.K. Long-Term Effects of a Structured Life Review Process. J. Gerontol. 1992, 47, P312–P315. [Google Scholar] [CrossRef]
- Han, Q.B.; Yan, W.J. Nostalgia therapy in palliative care for elderly stroke patients. J. Bengbu Med. Coll. 2017, 42, 1423–1424. [Google Scholar] [CrossRef]
- Hanaoka, H.; Okamura, H. Study on Effects of Life Review Activities on the Quality of Life of the Elderly: A Randomized Controlled Trial. Psychother. Psychosom. 2004, 73, 302–311. [Google Scholar] [CrossRef] [PubMed]
- Korte, J.; Bohlmeijer, E.T.; Cappeliez, P.; Smit, F.; Westerhof, G.J. Life review therapy for older adults with moderate depressive symptomatology: A pragmatic randomized controlled trial. Psychol. Med. 2012, 42, 1163–1173. [Google Scholar] [CrossRef] [PubMed]
- Lan, X.Y. Effects of Life Review on Mental Health among Frail Elders in Nursing Home: Randomised Controlled Trial. Ph.D. Thesis, Fujian Medical University, Fu Zhou, China, 2016. [Google Scholar]
- Lan, X.; Xiao, H.; Chen, Y.; Zhang, X. Effects of Life Review Intervention on Life Satisfaction and Personal Meaning among Older Adults with Frailty. J. Psychosoc. Nurs. Ment. Health Serv. 2018, 56, 30–36. [Google Scholar] [CrossRef]
- Le, Y.; Chen, Y.Y. Effect of structured group reminiscence on depressive symptoms and life satisfaction in elders. China Mod. Dr. 2013, 51, 110–112. [Google Scholar]
- Li, H. Effects of Nostalgia Therapy on Depressive Symptoms and Quality of Life in Elderly Stroke Patients. Jilin Yi Xue 2018, 39, 1368–1370. [Google Scholar] [CrossRef]
- Li, Y.Z.; Luo, L.X.; Huang, J.Y.; Yu, C.Y. A study on the effectiveness of nostalgia therapy intervention for patients with Alzheimer’s disease. Nurs. Pract. Res. 2018, 15, 154–155. [Google Scholar]
- Li, C.L.; Xiang, Q.L.; Zeng, L.; Lei, F.R.; Liu, D.M. Exploring the effect of individual nostalgia therapy on rural elderly inpatients in respiratory medicine. Prim. Care Forum 2020, 24, 4716–4718. [Google Scholar] [CrossRef]
- Lök, N.; Bademli, K.; Selçuk-Tosun, A. The effect of reminiscence therapy on cognitive functions, depression, and quality of life in Alzheimer patients: Randomized controlled trial. Int J Geriatr. Psychiatry 2019, 34, 47–53. [Google Scholar] [CrossRef]
- Mei, Y.; Lin, B.; Li, Y.; Ding, C.; Zhang, Z. Effects of modified 8-week reminiscence therapy on the older spouse caregivers of stroke survivors in Chinese communities: A randomized controlled trial. Int. J. Geriatr. Psychiatry 2018, 33, 633–641. [Google Scholar] [CrossRef]
- Morgan, S. The Impact of a Structured Life Review Process on People with Memory Problems Living in Care Homes. Ph.D. Thesis, University of Wales, Bangor, UK, 2000. [Google Scholar]
- Pérez-Sáez, E.; Justo-Henriques, S.I.; Alves Apóstolo, J.L. Multicenter randomized controlled trial of the effects of individual reminiscence therapy on cognition, depression and quality of life: Analysis of a sample of older adults with Alzheimer’s disease and vascular dementia. Clin. Neuropsychol. 2022, 36, 1975–1996. [Google Scholar] [CrossRef] [PubMed]
- Preschl, B.; Maercker, A.; Wagner, B.; Forstmeier, S.; Baños, R.M.; Alcañiz, M.; Castilla, D.; Botella, C. Life-review therapy with computer supplements for depression in the elderly: A randomized controlled trial. Aging Ment. Health 2012, 16, 964–974. [Google Scholar] [CrossRef]
- Sharif, F.; Jahanbin, I.; Amirsadat, A.; Moghadam, M.H. Effectiveness of Life Review Therapy on Quality of Life in the Late Life at Day Care Centers of Shiraz, Iran: A Randomized Controlled Trial. Int. J. Community Based Nurs. Midwifery 2018, 6, 136–145. [Google Scholar]
- Shen, H.; Song, X.H.; Wang, J.Q. Observation on the Effect of Nostalgia Therapy on Rehabilitation Effect of Elderly Patients with Alzheimer’ s Disease. Reflexol. Rehabil. Med. 2022, 3, 87–90+99. [Google Scholar]
- Subramaniam, P.; Woods, B.; Whitaker, C. Life review and life story books for people with mild to moderate dementia: A randomised controlled trial. Aging Ment. Health 2014, 18, 363–375. [Google Scholar] [CrossRef] [PubMed]
- Tao, R.; Cheng, Q. Effects of nostalgic care therapy on cognitive function and quality of life of dementia patients. China Contin. Med. Educ. 2017, 9, 263–264. [Google Scholar] [CrossRef]
- Viguer, P.; Satorres, E.; Fortuna, F.B.; Meléndez, J.C. A Follow-Up Study of a Reminiscence Intervention and Its Effects on Depressed Mood, Life Satisfaction, and Well-Being in the Elderly. J. Psychol. 2017, 151, 789–803. [Google Scholar] [CrossRef]
- Rueda, A.V.; Cabaco, A.S.; Mejía-Ramírez, M.; Justo-Henriques, S.I.; Carvalho, J.O. Improvement of the Quality of Life in Aging by Stimulating Autobiographical Memory. JCM 2021, 10, 3168. [Google Scholar] [CrossRef]
- Wang, L.Y.; Shen, C.Z. Intervention Practices for Dementia Based on Life Storybook. Chin. J. Gerontol. 2013, 33, 5239–5241. [Google Scholar] [CrossRef]
- Wu, L.-F.; Koo, M. Randomized controlled trial of a six-week spiritual reminiscence intervention on hope, life satisfaction, and spiritual well-being in elderly with mild and moderate dementia: Spiritual reminiscence and dementia. Int. J. Geriatr. Psychiatry 2016, 31, 120–127. [Google Scholar] [CrossRef] [PubMed]
- Ferrans, C.E. Quality of life: Conceptual issues. Semin. Oncol. Nurs. 1990, 6, 248–254. [Google Scholar] [CrossRef]
- Yang, T.B.; Zhang, J.H. Study on Measurement and Evaluation of Quality of Life of the Elderly. Chin. J. Gerontol. 2004, 24, 384–385. [Google Scholar] [CrossRef]
- Busija, L.; Pausenberger, E.; Haines, T.P.; Haymes, S.; Buchbinder, R.; Osborne, R.H. Adult measures of general health and health-related quality of life: Medical Outcomes Study Short Form 36-Item (SF-36) and Short Form 12-Item (SF-12) Health Surveys, Nottingham Health Profile (NHP), Sickness Impact Profile (SIP), Medical Outcomes Study Sh. Arthritis Care Res. 2011, 63, S383–S412. [Google Scholar] [CrossRef] [PubMed]
- The World Health Organization Quality of Life (WHOQOL). Available online: https://www.who.int/publications/i/item/WHO-HIS-HSI-Rev.2012.03 (accessed on 13 March 2023).
- Xu, L.; Li, S.; Yan, R.; Ni, Y.; Wang, Y.; Li, Y. Effects of reminiscence therapy on psychological outcome among older adults without obvious cognitive impairment: A systematic review and meta-analysis. Front. Psychiatry 2023, 14, 1139700. [Google Scholar] [CrossRef]
- Hilgeman, M.M.; Allen, R.S.; Snow, A.L.; Durkin, D.W.; DeCoster, J.; Burgio, L. Preserving Identity and Planning for Advance Care (PIPAC): Preliminary outcomes from a patient-centered intervention for individuals with mild dementia. Aging Ment. Health 2014, 18, 411–424. [Google Scholar] [CrossRef]
- Park, K.; Lee, S.; Yang, J.; Song, T.; Hong, G.-R.S. A systematic review and meta-analysis on the effect of reminiscence therapy for people with dementia. Int. Psychogeriatr. 2019, 31, 1581–1597. [Google Scholar] [CrossRef]
- Aghaei, A.; Khayyamnekouei, Z.; Yousefy, A. General Health Prediction Based on Life Orientation, Quality of Life, Life Satisfaction and Age. Procedia-Soc. Behav. Sci. 2013, 84, 569–573. [Google Scholar] [CrossRef]
- Zhu, Y. Active and Positive: The Connection between Active Aging and Positive Psychology. Open J. Soc. Sci. 2019, 7, 147–156. [Google Scholar] [CrossRef]



| Study | Country | Condition | Participant | Intervention | Outcome (Scale) | Follow-Up | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean Age (SD) | Female (%) | Health Condition | GRP/IDV | Setting | Conductor | Duration | Content | |||||
| Allen et al., 2020 [20] | Ireland | RT | 14 | 69.00 (4.84) | 71.43 | Healthy older adults | GRP | N/A | N/A | 60 min/session; 6 weekly sessions | A semi-structured reminiscence program | QoL (CASP-19); LS (SWLS) | N/A |
| Discussion | 11 | 68.80 (4.97) | 90.91 | Healthy older adults | GRP | N/A | N/A | 60 min/session; 6 weekly sessions | The present and future | QoL (CASP-19); LS (SWLS) | N/A | ||
| Aydogdu et al., 2022 [21] | Northern Cyprus | RT | 17 | 76.17 (9.21) | 64.71 | Without hearing problems or cognitive impairment | GRP | Nursing homes | The researcher | 45~60 min/session; 8 weekly sessions | Instrumental RT based on Roy’s adaptation model and group activities | LS (LSI-A) | N/A |
| No treatment | 17 | 73.94 (7.36) | 41.18 | Without hearing problems or cognitive impairment | N/A | N/A | N/A | N/A | N/A | LS (LSI-A) | N/A | ||
| Biohm, 1997 [22] | The United States | RT | 14 | N/A | 93.00 | Healthy older adults | GRP | Nursing homes | The investigator | 45 min/session; twice a week; 4 weeks | Depicting major events from past decades by large posters | LS (LSI-A) | 6 weeks |
| Discussion | 13 | N/A | 85.00 | Healthy older adults | GRP | Nursing homes | The investigator | 45 min/session; twice a week; 4 weeks | Depicting current events by large posters | LS (LSI-A) | 6 weeks | ||
| Chen, 2020 [23] | China | RT | 45 | 71.00 (5.30) | 42.22 | With stroke | IDV | Hospital | Nurse practitioner | 60 min/session; 6 weekly sessions | Discussion around the theme of reminiscence | QoL (WHOQOL) | N/A |
| Usual care | 45 | 70.90 (5.20) | 40.00 | With stroke | N/A | N/A | N/A | N/A | Health care and education | QoL (WHOQOL) | N/A | ||
| Chippendale, 2011 [24] | The United States | LR | 23 | 87.20 (6.30) | 69.60 | Without advanced disease | GRP | Senior residences | The researcher | 90 min/session, 8 weekly sessions | Writing and reading life stories | LS (LSI-A) | N/A |
| Waiting list | 22 | 80.80 (7.50) | 68.20 | Without advanced disease | N/A | N/A | N/A | N/A | N/A | LS (LSI-A) | N/A | ||
| Deng et al., 2022 [25] | China | RT | 58 | 70.31 (7.98) | 44.83 | With MI and depressive symptom after PCI | IDV | Hospital | The researcher | 30~45 min/session; 3 sessions/week, 6 weeks | Discussion around the theme of reminiscence | QoL (GQOLI-74) | N/A |
| Usual care | 57 | 69.61 (7.32) | 33.33 | With MI and depressive symptom after PCI | IDV | Hospital | N/A | N/A | Cognitive intervention, medication, psychological support, and cardiac rehabilitation exercises | QoL (GQOLI-74) | N/A | ||
| Fountain, 1992 [26] | The United States | LR | 27 | N/A | 89.00 | With multiple diagnoses including mild Alzheimer’s disease, chronic brain syndrome, assorted cardiovascular conditions | GRP | Health care center and nursing home | The researcher and the second-year group work students | 50~60 min/session; 12 bi-weekly sessions | Discussion around the theme of reminiscence | LS (RPGCMS) | N/A |
| LR coupled with religious themes | 25 | N/A | 84.00 | With multiple diagnoses including mild Alzheimer’s disease, chronic brain syndrome, assorted cardiovascular conditions | GRP | Health care center and nursing home | The researcher and a local retired Lutheran pastor | 12 bi-weekly sessions | Discussion around the theme of reminiscence by utilizing religion as principle | LS (RPGCMS) | N/A | ||
| No treatment | 20 | N/A | 85.00 | With multiple diagnoses including mild Alzheimer’s disease, chronic brain syndrome, assorted cardiovascular conditions | N/A | N/A | N/A | N/A | N/A | LS (RPGCMS) | N/A | ||
| Gan, 2017 [27] | China | RT | 45 | 71.50 (1.60) | 57.78 | With Alzheimer’s | IDV | Hospital | Professional nurses | N/A | Discussion around the theme of reminiscence | QoL (QOL-AD) | N/A |
| Usual care | 45 | 71.50 (1.30) | 31.11 | With Alzheimer’s | N/A | Hospital | Professional Nurses | N/A | Daily care | QoL (QOL-AD) | N/A | ||
| Gudorf, 1991 [28] | The United States | LR | 6 | 83.5 | 100.00 | With the ability to concentrate for 1 h | IDV | Home community | The researcher and the nursing home social worker | 60 min/session; 8 bi-weekly sessions | Discussion around the theme of life stories | LS (LSES) | 5 weeks |
| No treatment | 6 | 87.2 | 83.33 | With the ability to concentrate for 1 h | N/A | N/A | N/A | N/A | N/A | LS (LSES) | 5 weeks | ||
| Haight, 1992 [29] | The United States | LR | 10 | N/A | N/A | N/A | IDV | Home | The investigator and research assistants | 60 min/session; 6 weekly sessions | Guide the older person through his or her memories by attentive listening | LS (LSI-A) | 1 year |
| A friendly visit | 13 | N/A | N/A | N/A | N/A | Home | N/A | N/A | N/A | LS (LSI-A) | 1 year | ||
| Han & Yan, 2017 [30] | China | RT | 45 | N/A | N/A | With stroke | GRP | Hospital | Professional nurses | 6 weekly sessions | Reminiscence activities with songs, films, photos, and souvenirs | LS (LSI-A) | N/A |
| Usual care | 45 | N/A | N/A | With stroke | N/A | Hospital | N/A | N/A | Daily care and health education | LS (LSI-A) | N/A | ||
| Hanaoka et al., 2004 [31] | Japan | LR | 42 | 81.62 (5.09) | 85.71 | No history of mental disorders; without cognitive impairment | GRP | N/A | Therapists | 60 min/session; 8 weekly sessions | Discussion around the theme of reminiscence | LS (LSI-A) | 3 months |
| Discussion | 38 | 81.97 (6.33) | 86.84 | No history of mental disorders; without cognitive impairment | N/A | N/A | Therapists | 60 min/session; 8 weekly sessions | Discussion activities about health | LS (LSI-A) | 3 months | ||
| Korte et al., 2012 [32] | Netherlands | LR | 100 | 63.30 (6.20) | 80.00 | With slight to moderate depressive and anxiety symptoms | GRP | Mental health care institutions | Therapists | 120 min/session, 8 sessions | Discussion around the theme of “the stories we live by” | QoL (EQ-5D) | 3 months; 9 months |
| Usual care | 102 | 63.30 (6.80) | 73.50 | With slight to moderate depressive and anxiety symptoms | N/A | N/A | N/A | N/A | N/A | QoL (EQ-5D) | 3 months | ||
| Lan, 2016 [33] | China | LR | 31 | 83.06 (6.88) | 64.52 | With frailty | IDV | The nursing home | The researcher | 30~60 min/session; 6 weekly sessions | Discussion around the theme of life stories through photographs | LS (LSI-A) | N/A |
| Usual care | 31 | 82.90 (7.10) | 61.29 | With frailty | N/A | N/A | N/A | N/A | N/A | LS (LSI-A) | N/A | ||
| Lan et al., 2018 [34] | China | LR | 33 | 83.10 (6.50) | 67.60 | With frailty | IDV | The nursing home | The researcher | 30~60 min/session; 6 weekly sessions | Discussion around the theme of life stories through photographs | LS (LSI-A) | N/A |
| Usual care | 34 | 83.50 (6.60) | 62.20 | With frailty | N/A | N/A | N/A | N/A | N/A | LS (LSI-A) | N/A | ||
| Le & Chen, 2013 [35] | China | RT | 40 | 70.80 (16.20) | 50.00 | With mild or moderate depression | GRP | N/A | Professional nurses | 40~50 min/session; 6 weekly sessions | Reminiscence activities with songs, films, photos, and souvenirs | LS (LSI-A) | N/A |
| Usual care | 40 | 72.00 (17.30) | 55.00 | With mild or moderate depression | N/A | N/A | N/A | N/A | Daily care and health education | LS (LSI-A) | N/A | ||
| Li, 2018 [36] | China | RT | 45 | 63.70 (3.10) | 46.67 | With stroke | IDV | Hospital | A therapist | 4 weekly sessions | Reminiscence activities with songs letters, and meaningful items | QoL (KPS) | N/A |
| Usual care | 45 | 63.30 (3.10) | 44.44 | With stroke | N/A | Hospital | Doctors and nurses | N/A | Medication and health education | QoL (KPS) | N/A | ||
| Li, Luo et al., 2018 [37] | China | RT | 38 | 79.88 (5.56) | 42.11 | With Alzheimer’s | IDV | Hospital | The therapist | 45 min/session; 10 weekly sessions | Discussion around the theme of reminiscence | QoL (QOL-AD) | N/A |
| Usual care | 38 | 80.22 (5.25) | 52.63 | With Alzheimer’s | N/A | Hospital | N/A | 10 weeks | Daily treatment | QoL (QOL-AD) | N/A | ||
| Li et al., 2020 [38] | China | RT | 60 | 69.89 (2.38) | 40.00 | With chronic diseases | IDV | Hospital | Nurses | N/A | Reminiscence activities with music, photos, and books | QoL (SF-36) | N/A |
| Usual care | 60 | 70.48 (2.35) | 36.67 | With chronic diseases | N/A | Hospital | Nurses | N/A | Daily care and support | QoL (SF-36) | N/A | ||
| Lök et al., 2019 [39] | Turkey | RT | 30 | N/A | 60.00 | With Alzheimer’s | GRP | The nursing home | N/A | 60 min/session; 8 weekly sessions | Reminiscence activities with photographs, household goods, music, and foods | QoL (QOL-AD) | N/A |
| Control | 30 | N/A | 53.40 | With Alzheimer’s | N/A | N/A | N/A | N/A | N/A | QoL (QOL-AD) | N/A | ||
| Mei et al., 2018 [40] | China | RT | 44 | 69.67 (2.35) | 80.00 | With stroke | IDV | Caregivers’ homes | A psychologist | 45~60 min/session; 8 weekly sessions | Reminiscence activities with diaries, letters, old photos, songs, and newspapers | LS (SWLS) | 1 month; 3 months |
| Health education | 44 | 69.80 (5.58) | 75.00 | N/A | N/A | N/A | Community health workers | N/A | N/A | LS (SWLS) | 1 month; 3 months | ||
| Morgan, 2000 [41] | The United Kingdom | LR | 8 | 80.50 (5.75) | 75.00 | With mild to moderate dementia | IDV | Care homes | The therapist | 60 min/session; 12 weekly sessions | Life story book | LS (LSI-A) | 6 weeks |
| No treatment | 9 | 84.44 (7.81) | 77.80 | With mild to moderate dementia | N/A | N/A | N/A | N/A | N/A | LS (LSI-A) | 6 weeks | ||
| Pérez-Sáez et al., 2022 [42] | Portugal | RT | 62 | 82.39 (7.58) | 71.60 | With neurocognitive disorder | IDV | Social care institutions | Therapists | 50 min/session; 26 bi-weekly sessions | Reminiscence activities with images, music, riddles, and theme worksheets | QoL (QOL-AD) | N/A |
| Usual care | 68 | 82.68 (7.32) | 68.90 | With neurocognitive disorder | N/A | N/A | N/A | N/A | N/A | QoL (QOL-AD) | N/A | ||
| Preschl et al., 2012 [43] | Switzerland | LR | 20 | 72.50 (4.50) | 75.00 | With minimal or moderate depression | IDV | N/A | Therapists | 60~90 min/session; 6 weekly sessions | Structured life review by face to face and computer form | LS (LSI-A) | 3 months |
| Waiting list | 16 | 67.00 (3.10) | 56.30 | With minimal or moderate depression | N/A | N/A | N/A | six weeks in total | N/A | LS (LSI-A) | N/A | ||
| Sharif et al., 2018 [44] | Iran | LR | 17 | N/A | 52.90 | N/A | IDV | Day care centers | The researcher | 120 min/session; 8 bi-weekly sessions | N/A | QoL (WHOQOL-BREF) | 1 month |
| Usual care | 18 | N/A | 50.00 | N/A | N/A | Day care centers | N/A | N/A | N/A | QoL (WHOQOL-BREF) | 1 month | ||
| Shen et al., 2022 [45] | China | RT | 46 | 73.74 (4.77) | 43.48 | With Alzheimer’s | IDV | Hospital | Therapists | 40~60 min/session; 8 weekly sessions | Reminiscence activities with photos and meaningful items | QoL (QOL-AD) | N/A |
| Usual care | 46 | 73.70 (4.78) | 41.30 | With Alzheimer’s | N/A | Hospital | N/A | 8 weeks | Daily care and health education | QoL (QOL-AD) | N/A | ||
| Subramaniam et al., 2014 [46] | The United Kingdom | LR | 11 | 84.50 (6.70) | 72.70 | With dementia | IDV | Care homes | The therapist | 60 min/session; 12 weekly sessions | developing life story book for themselves | QoL (QOL-AD) | 6 weeks |
| Storybook as gift | 12 | 88.30 (6.00) | 66.70 | With dementia | N/A | Care homes | The therapist | 5 or 6 times over 12 weeks | Researcher worked with the participant’s relative to develop a life story book | QoL (QOL-AD) | 6 weeks | ||
| Tao & Cheng, 2017 [47] | China | RT | 37 | 71.20 (5.30) | 43.24 | With dementia | IDV | Hospital | N/A | 12 weekly sessions | Reminiscence activities with photos and meaningful items | QoL (QOL-AD) | N/A |
| Usual care | 37 | 70.80 (5.10) | 45.95 | With dementia | N/A | Hospital | N/A | N/A | Daily treatment | QoL (QOL-AD) | N/A | ||
| Viguer et al., 2017 [48] | The Dominican Republic | RT | 80 | 73.06 (6.90) | 56.30 | Without cognitive impairment or clinical depression | GRP | N/A | A trained psychologist | 120 min/session; 10 weekly sessions | Discussion around the theme of reminiscence | LS (LSI-A) | 3 months |
| Waiting list | 80 | 71.44 (6.30) | 51.20 | Without cognitive impairment or clinical depression | N/A | N/A | N/A | N/A | N/A | LS (LSI-A) | 3 months | ||
| Villasán Rueda et al., 2021 [49] | Spain | RT | 14 | N/A | N/A | Healthy aged | GRP | Day care centers | N/A | 60 min/session; 12 bi-weekly sessions | Positive reminiscence | LS (LSI-A) | N/A |
| Cognitive stimulation | 13 | N/A | N/A | Healthy aged | GRP | Social care institutions | N/A | 60 min/session; 12 bi-weekly sessions | Attention, perception, memory, language, inhibition, planning, reasoning, calculation, and drawing trainings | LS (LSI-A) | N/A | ||
| RT | 11 | N/A | N/A | With mild cognitive impairment | GRP | Social care institutions | N/A | 60 min/session; 12 bi-weekly sessions | Positive reminiscence | LS (LSI-A) | N/A | ||
| Cognitive stimulation | 13 | N/A | N/A | With mild cognitive impairment | GRP | Social care institutions | N/A | 60 min/session; 12 bi-weekly sessions | Attention, perception, memory, language, inhibition, planning, reasoning, calculation, and drawing trainings | LS (LSI-A) | N/A | ||
| RT | 20 | N/A | N/A | With Alzheimer’s | GRP | Social care institutions | N/A | 60 min/session; 12 bi-weekly sessions | Positive reminiscence | LS (LSI-A) | N/A | ||
| Cognitive stimulation | 6 | N/A | N/A | With Alzheimer’s | GRP | Social care institutions | N/A | 60 min/session; 12 bi-weekly sessions | Attention, perception, memory, language, inhibition, planning, reasoning, calculation, and drawing trainings | LS (LSI-A) | N/A | ||
| Wang & Shen, 2013 [50] | China | LR | 29 | 83.00 (6.91) | N/A | With Alzheimer’s, vascular dementia or mixed dementia | IDV | Hospital | Nurses | 30~45 min/session; 8 weekly sessions | Life story book | QoL (DQOL) | 4 weeks |
| Usual care | 29 | 82.40 (6.84) | N/A | With Alzheimer’s, vascular dementia or mixed dementia | N/A | Hospital | Nurses | N/A | Daily treatment | QoL (DQOL) | 4 weeks | ||
| Wu & Koo, 2016 [51] | China | RT | 53 | 73.50 (7.30) | 64.20 | With mild or moderate dementia | GRP | Hospital | The researcher | 60 min/session; 6 weekly sessions | Spiritual reminiscence activities | LS (LSI-A) | N/A |
| Interview | 50 | 73.60 (7.60) | 74.00 | With mild or moderate dementia | N/A | N/A | The researcher | N/A | N/A | LS (LSI-A) | N/A | ||
| Studies (n) | Participants (n) | I2 | SMD [95% CI] | p (Overall Effects) | p (Group Differences) | |
|---|---|---|---|---|---|---|
| Form of intervention | 0.006 | |||||
| Group | 3 | 287 | 34.40% | 0.18 [−0.15, 0.52] | 0.28 | |
| Individual | 12 | 993 | 95.80% | 1.29 [0.58, 2.01] | <0.001 | |
| Total sessions of intervention | 0.71 | |||||
| ≤8 sessions | 9 | 767 | 94.80% | 1.21 [0.48, 1.94] | <0.001 | |
| >8 sessions | 4 | 303 | 94.10% | 1.47 [0.33, 2.61] | <0.001 |
| Studies (n) | Participants (n) | I2 | SMD [95% CI] | p (Overall Effects) | p (Group Differences) | |
|---|---|---|---|---|---|---|
| Form of intervention | 0.69 | |||||
| Group | 14 | 793 | 92.90% | 1.04 [0.43, 1.65] | <0.001 | |
| Individual | 8 | 305 | 90.30% | 1.26 [0.40, 2.12] | <0.001 | |
| Total sessions of intervention | 0.006 | |||||
| ≤8 sessions | 15 | 772 | 94.20% | 1.46 [0.76, 2.15] | <0.001 | |
| >8 sessions | 7 | 326 | 37.50% | 0.44 [0.10, 0.77] | 0.14 | |
| Comparison | 0.06 | |||||
| Passive control | 8 | 376 | 74.20% | 0.59 [0.12, 1.07] | <0.001 | |
| Active control | 14 | 722 | 94.20% | 1.43 [0.70, 2.16] | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhong, Q.; Chen, C.; Chen, S. Effectiveness on Quality of Life and Life Satisfaction for Older Adults: A Systematic Review and Meta-Analysis of Life Review and Reminiscence Therapy across Settings. Behav. Sci. 2023, 13, 830. https://doi.org/10.3390/bs13100830
Zhong Q, Chen C, Chen S. Effectiveness on Quality of Life and Life Satisfaction for Older Adults: A Systematic Review and Meta-Analysis of Life Review and Reminiscence Therapy across Settings. Behavioral Sciences. 2023; 13(10):830. https://doi.org/10.3390/bs13100830
Chicago/Turabian StyleZhong, Qing, Cheng Chen, and Shulin Chen. 2023. "Effectiveness on Quality of Life and Life Satisfaction for Older Adults: A Systematic Review and Meta-Analysis of Life Review and Reminiscence Therapy across Settings" Behavioral Sciences 13, no. 10: 830. https://doi.org/10.3390/bs13100830
APA StyleZhong, Q., Chen, C., & Chen, S. (2023). Effectiveness on Quality of Life and Life Satisfaction for Older Adults: A Systematic Review and Meta-Analysis of Life Review and Reminiscence Therapy across Settings. Behavioral Sciences, 13(10), 830. https://doi.org/10.3390/bs13100830






