Dietary Fermentation Product of Aspergillus Oryzae Prevents Increases in Gastrointestinal Permeability (‘Leaky Gut’) in Horses Undergoing Combined Transport and Exercise
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Horses
2.2. Stress Challenge
2.3. Non-Challenged Controls
2.4. Sample Analysis
2.5. Data Analysis
3. Results
3.1. Gastrointestinal Barrier Function
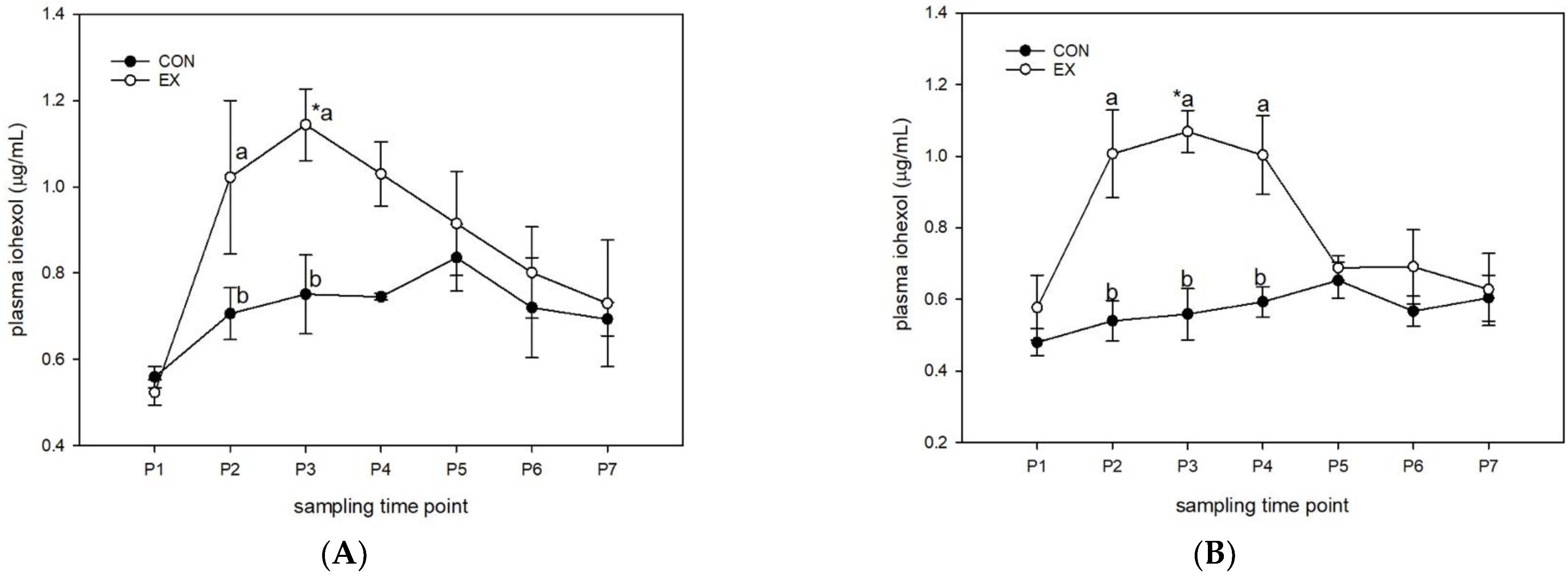
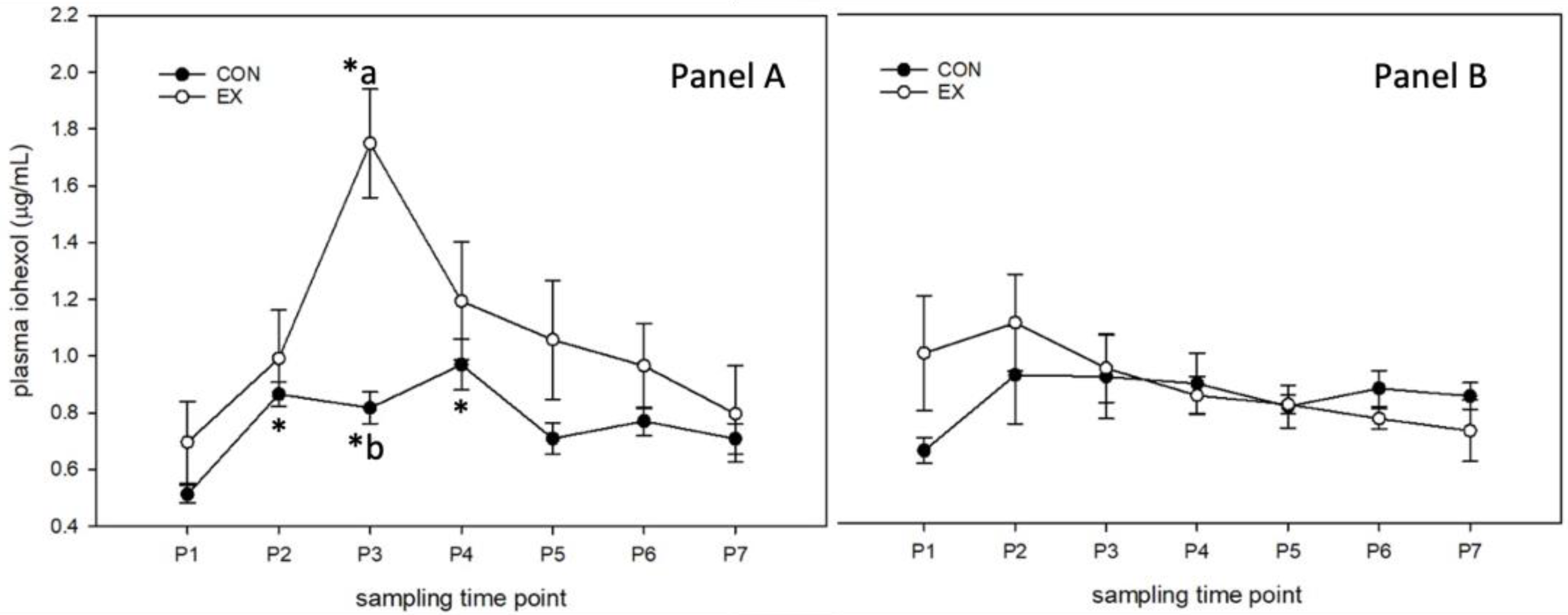
3.1.1. Control Diet (Figure 1)
3.1.2. Supplemented Diet (Figure 2)
3.1.3. Day 0 and Day 28 in Supplemented and Control Diets
3.2. Systemic Inflammation
3.2.1. Serum Amyloid A (SAA; Table 2)
Control Diet
Supplemented Diet
Day 0 and Day 28 in Supplemented and Control Diets
3.2.2. Lipopolysaccharide (LPS; Table 2)
Control Diet
Supplemented Diet
Day 0 and Day 28 in Supplemented and Control Diets
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Stewart, A.S.; Pratt-Phillips, S.; Gonzalez, L.M. Alterations in intestinal permeability: The role of the “Leaky Gut” in health and disease. J. Equine Vet. Sci. 2017, 52, 10–22. [Google Scholar] [CrossRef] [PubMed]
- Kompare, J. Leaky Gut Syndrome in Horses. Master’s Thesis, Michigan State University, East Lansing, MI, USA, 2013. [Google Scholar]
- Raspa, F.; Dinardo, F.R.; Vervuert, I.; Bergero, D.; Bottero, M.T.; Pattono, D.; Dalmasso, A.; Vinassa, M.; Valvassori, E.; Bruno, E.; et al. A Fibre- vs. cereal grain-based diet: Which is better for horse welfare? Effects on intestinal permeability, muscle characteristics and oxidative status in horses reared for meat production. J. Anim. Physiol. Anim. Nutr. 2022, 106, 313–326. [Google Scholar] [CrossRef] [PubMed]
- Karhu, E.; Forsgård, R.A.; Alanko, L.; Alfthan, H.; Pussinen, P.; Hämäläinen, E.; Korpela, R. Exercise and gastrointestinal symptoms: Running-induced changes in intestinal permeability and markers of gastrointestinal function in asymptomatic and symptomatic runners. Eur. J. Appl. Physiol. 2017, 117, 2519–2526. [Google Scholar] [CrossRef] [PubMed]
- Pugh, J.N.; Impey, S.G.; Doran, D.A.; Fleming, S.C.; Morton, J.P.; Close, G.L. Acute high-intensity interval running increases markers of gastrointestinal damage and permeability but not gastrointestinal symptoms. Appl. Physiol. Nutr. Metab. 2017, 42, 941–947. [Google Scholar] [CrossRef] [PubMed]
- Pasini, E.; Corsetti, G.; Assanelli, D.; Testa, C.; Romano, C.; Dioguardi, F.S.; Aquilani, R. Effects of chronic exercise on gut microbiota and intestinal barrier in human with type 2 diabetes. Minerva Med. 2019, 110, 3–11. [Google Scholar] [CrossRef]
- McGilloway, M.; Manley, S.; Aho, A.; Heeringa, K.N.; Lou, Y.; Squires, E.J.; Pearson, W. Gastrointestinal permeability and systemic inflammation increase following combined transport and exercise stress. Equine Vet. J. 2022. [Google Scholar] [CrossRef]
- Nishimura, S.; Aoi, W.; Kodani, H.; Kobayashi, Y.; Wada, S.; Kuwahata, M.; Higashi, A. Polysorbate 80-induced leaky gut impairs skeletal muscle metabolism in mice. Physiol. Rep. 2020, 8, e14629. [Google Scholar] [CrossRef]
- Fasano, A. Zonulin and its regulation of intestinal barrier function: The biological door to inflammation, autoimmunity, and cancer. Physiol. Rev. 2011, 91, 151–175. [Google Scholar] [CrossRef]
- Watts, T.; Berti, I.; Sapone, A.; Gerarduzzi, T.; Not, T.; Zielke, R.; Fasano, A. Role of the intestinal tight junction modulator zonulin in the pathogenesis of type I diabetes in BB diabetic-prone rats. Proc. Natl. Acad. Sci. USA 2005, 102, 2916–2921. [Google Scholar] [CrossRef]
- Akdis, C.A. Does the epithelial barrier hypothesis explain the increase in allergy, autoimmunity and other chronic conditions? Nat. Rev. Immunol. 2021, 21, 739–751. [Google Scholar] [CrossRef] [PubMed]
- Farshchi, M.K.; Azad, F.J.; Salari, R.; Mirsadraee, M.; Anushiravani, M. A Viewpoint on the leaky gut syndrome to treat allergic asthma: A novel opinion. J. Evid. Based Complement. Altern. Med. 2017, 22, 378–380. [Google Scholar] [CrossRef]
- Tajik, N.; Frech, M.; Schulz, O.; Schälter, F.; Lucas, S.; Azizov, V.; Dürholz, K.; Steffen, F.; Omata, Y.; Rings, A.; et al. Targeting zonulin and intestinal epithelial barrier function to prevent onset of arthritis. Nat. Commun. 2020, 11, 1995. [Google Scholar] [CrossRef]
- Kocot, A.M.; Jarocka-Cyrta, E.; Drabińska, N. Overview of the importance of biotics in gut barrier integrity. Int. J. Mol. Sci. 2022, 23, 2896. [Google Scholar] [CrossRef] [PubMed]
- Martel, J.; Chang, S.H.; Ko, Y.F.; Hwang, T.L.; Young, J.D.; Ojcius, D.M. Gut barrier disruption and chronic disease. Trends Endocrinol. Metab. 2022, 33, 247–265. [Google Scholar] [CrossRef]
- Collinet, A.; Grimm, P.; Jacotot, E.; Julliand, V. Biomarkers for monitoring the equine large intestinal inflammatory response to stress-induced dysbiosis and probiotic supplementation. J. Anim. Sci. 2022, 100, skac268. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.H.; Sim, Y.; Hwang, J.H.; Kwun, I.S.; Lim, J.H.; Kim, J.; Kim, J.I.; Baek, M.C.; Akbar, M.; Seo, W.; et al. Ellagic acid prevents binge alcohol-induced leaky gut and liver injury through inhibiting gut dysbiosis and oxidative stress. Antioxidants 2021, 10, 1386. [Google Scholar] [CrossRef] [PubMed]
- Nomura, R.; Tsuzuki, S.; Kojima, T.; Nagasawa, M.; Sato, Y.; Uefune, M.; Baba, Y.; Hayashi, T.; Nakano, H.; Kato, M.; et al. Administration of Aspergillus oryzae suppresses DSS-induced colitis. Food Chem. 2021, 4, 100063. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Jin, W.; Jiang, Y.; Xie, F.; Mao, S. Response of milk performance, rumen and hindgut microbiome to dietary Supplementation with Aspergillus oryzae fermentation extracts in dairy cows. Curr. Microbiol. 2022, 79, 113. [Google Scholar] [CrossRef]
- Chuang, W.Y.; Lin, W.C.; Hsieh, Y.C.; Huang, C.M.; Chang, S.C.; Lee, T.T. Evaluation of the combined use of Saccharomyces Cerevisiae and Aspergillus Oryzae with phytase fermentation products on growth, inflammatory, and intestinal morphology in broilers. Animals 2019, 9, 1051. [Google Scholar] [CrossRef] [PubMed]
- Ríus, A.; Kaufman, J.D.; Li, M.M.; Hanigan, M.D.; Ipharraguerre, I.R. Physiological responses of Holstein calves to heat stress and dietary supplementation with a postbiotic from Aspergillus oryzae. Sci. Rep. 2022, 12, 1587. [Google Scholar] [CrossRef] [PubMed]
- Koenig, J.; Cote, N. Equine gastrointestinal motility--ileus and pharmacological modification. Can. Vet. J. 2006, 47, 551–559. [Google Scholar] [PubMed]
- De Mare, L.; Boshuizen, B.; Plancke, L.; De Meeus, C.; De Bruijn, M.; Delesalle, C. Standardized exercise tests in horses: Current situation and future perspectives. Vlaams Diergeneeskd. Tijdschr. 2017, 86, 63–72. [Google Scholar] [CrossRef]
- Yang, Y.; Iwamoto, A.; Kumrungsee, T.; Okazaki, Y.; Kuroda, M.; Yamaguchi, S.; Kato, N. Consumption of an acid protease derived from Aspergillus oryzae causes bifidogenic effect in rats. Nutr. Res. 2017, 44, 60–66. [Google Scholar] [CrossRef] [PubMed]
- Krumbeck, J.A.; Rasmussen, H.E.; Hutkins, R.W.; Clarke, J.; Shawron, K.; Keshavarzian, A.; Walter, J. Probiotic Bifidobacterium strains and galactooligosaccharides improve intestinal barrier function in obese adults but show no synergism when used together as synbiotics. Microbiome 2018, 6, 121. [Google Scholar] [CrossRef] [PubMed]
- Long, A.; Nolen-Walston, R. Equine inflammatory markers in the twenty-first century: A focus on serum amyloid A. Vet Clin N. Am. Equine Pr. 2020, 36, 147–160. [Google Scholar] [CrossRef]
- Eckhardt, E.R.; Witta, J.; Zhong, J.; Arsenescu, R.; Arsenescu, V.; Wang, Y.; Ghoshal, S.; de Beer, M.C.; de Beer, F.C.; de Villiers, W.J. Intestinal epithelial serum amyloid A modulates bacterial growth in vitro and pro-inflammatory responses in mouse experimental colitis. BMC Gastroenterol. 2010, 10, 133. [Google Scholar] [CrossRef]
| Nutritional Analysis (as Fed) | |
|---|---|
| Crude Protein | 11.99% |
| Lysine | 0.49% |
| Crude Fat | 3.60% |
| Crude Fiber | 9.34% |
| Dry Matter | 89.09% |
| Calcium (total) | 0.74% |
| Phosphorus (total) | 0.52% |
| Sodium | 0.35% |
| Chloride | 0.53% |
| Potassium | 0.72% |
| Magnesium | 0.29% |
| Sulfur | 0.15% |
| Iron | 110.71 mg/kg |
| Manganese | 150.26 mg/kg |
| Zinc | 182.22 mg/kg |
| Copper | 36.46 mg/kg |
| Iodine | 0.98 mg/kg |
| Selenium | 0.40 mg/kg |
| Cobalt | 3.00 mg/kg |
| Vitamin A | 12.53 KIU/kg |
| Vitamin D3 | 2.51 KIU/kg |
| Vitamin E | 200.00 KIU/kg |
| Biotin | 1640.00 mcg/kg |
| D.E. Horse | 3.06 Mcal/kg |
| TDN Horse | 72.31% |
| Starch | 23.21% |
| SAA | LPS | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Day 0 | ||||||||||||
| CO | SUPP | CO | SUPP | |||||||||
| SED a | EX b | p ** | SED | EX | p ** | SED a | EX b | p ** | SED b | EX a | p ** | |
| P1 | 0.10 ± 0.10 | 0.22 ± 0.16 | 0.9 | 0.33 ± 0.33 | 0.08 ± 0.08 | 0.8 | 2.10 ± 0.09 | 2.18 ± 0.06 | 1.0 | 2.15 ± 0.04 | 2.06 ± 0.04 | 1.0 |
| P2 | 0.03 ± 0.03 | 0.12 ± 0.10 | 0.9 | 0.03 ± 0.03 | 0.00 ± 0.00 | 0.8 | 2.09 ± 0.06 | 2.23 ± 0.06 | 1.0 | 2.14 ± 0.02 | 2.09 ± 0.02 | 1.0 |
| P3 | 0.00 ± 0.00 | 0.52 ± 0.24 | 0.9 | 0.10 ± 0.10 | 0.23 ± 0.17 | 0.8 | 2.14 ± 0.06 | 2.22 ± 0.10 | 1.0 | 2.16 ± 0.05 | 2.13 ± 0.04 | 1.0 |
| P4 | 0.00 ± 0.00 | 0.46 ± 0.30 | 0.9 | 0.20 ± 0.20 | 0.03 ± 0.03 | 0.8 | 2.10 ± 0.06 | 2.24 ± 0.13 | 1.0 | 2.19 ± 0.03 | 2.11 ± 0.05 | 1.0 |
| P5 | 0.03 ± 0.03 | 0.74 ± 0.43 | 0.9 | 0.18 ± 0.18 | 0.10 ± 0.10 | 0.8 | 2.08 ± 0.04 | 2.19 ± 0.05 | 1.0 | 2.15 ± 0.04 | 2.10 ± 0.05 | 1.0 |
| P6 | 0.03 ± 0.03 | 0.78 ± 0.45 | 0.9 | 0.08 ± 0.08 | 0.00 ± 0.00 | 0.8 | 2.09 ± 0.04 | 2.24 ± 0.08 | 1.0 | 2.18 ± 0.01 | 2.14 ± 0.05 | 1.0 |
| P7 | 0.10 ± 0.10 | 0.86 ± 0.56 | 0.9 | 0.15 ± 0.15 | 0.30 ± 0.30 | 0.8 | 2.13 ± 0.12 | 2.21 ± 0.10 | 1.0 | 2.17 ± 0.04 | 2.13 ± 0.01 | 1.0 |
| p * | 0.78 | 0.70 | 0.92 | 0.96 | 0.71 | 0.99 | 0.91 | 0.98 | ||||
| Day 28 | ||||||||||||
| CO | SUPP | CO | SUPP | |||||||||
| SED a | EX b | p ** | SED | EX | p ** | SED a | EX b | p ** | SED b | EX a | p ** | |
| P1 | 0.00 ± 0.00 | 0.15 ± 0.15 | 1.0 | 0.17 ± 0.17 | 0.35 ± 0.25 | 0.8 | 2.10 ± 0.09 | 2.14 ± 0.03 | 0.68 | 2.20 ± 0.08 | 2.06 ± 0.04 | 0.11 |
| P2 | 0.00 ± 0.00 | 0.15 ± 0.12 | 1.0 | 0.07 ± 0.07 | 0.50 ± 0.50 | 0.8 | 2.04 ± 0.04 | 2.15 ± 0.05 | 0.20 | 2.15 ± 0.08 | 2.04 ± 0.04 | 0.22 |
| P3 | 0.00 ± 0.00 | 0.23 ± 0.17 | 1.0 | 0.23 ± 0.15 | 0.47 ± 0.37 | 0.8 | 2.07 ± 0.07 | 2.17 ± 0.05 | 0.26 | 2.13 ± 0.05 | 2.03 ± 0.03 | 0.26 |
| P4 | 0.00 ± 0.00 | 0.08 ± 0.05 | 1.0 | 0.07 ± 0.07 | 1.33 ± 1.00 | 0.8 | 2.00 ± 0.05 | 2.17 ± 0.04 | 0.05 | 2.16 ± 0.07 | 2.05 ± 0.05 | 0.20 |
| P5 | 0.03 ± 0.03 | 0.23 ± 0.23 | 1.0 | 0.03 ± 0.03 | 0.63 ± 0.41 | 0.8 | 2.04 ± 0.05 | 2.19 ± 0.07 | 0.10 | 2.24 ± 0.04 | 2.02 ± 0.03 | 0.01 |
| P6 | 0.03 ± 0.03 | 0.35 ± 0.22 | 1.0 | 0.13 ± 0.09 | 0.45 ± 0.45 | 0.8 | 2.08 ± 0.08 | 2.18 ± 0.08 | 0.25 | 2.24 ± 0.10 | 2.06 ± 0.04 | 0.05 |
| P7 | 0.10 ± 0.10 | 0.20 ± 0.20 | 1.0 | 0.35 ± 0.15 | 1.00 ± 0.53 | 0.8 | 2.07 ± 0.05 | 2.10 ± 0.08 | 0.68 | 2.18 ± 0.07 | 2.06 ± 0.05 | 0.17 |
| p * | 0.92 | 0.96 | 0.71 | 0.70 | 0.94 | 0.94 | 0.90 | 0.97 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
McGilloway, M.; Manley, S.; Aho, A.; Heeringa, K.N.; Whitacre, L.; Lou, Y.; Squires, E.J.; Pearson, W. Dietary Fermentation Product of Aspergillus Oryzae Prevents Increases in Gastrointestinal Permeability (‘Leaky Gut’) in Horses Undergoing Combined Transport and Exercise. Animals 2023, 13, 951. https://doi.org/10.3390/ani13050951
McGilloway M, Manley S, Aho A, Heeringa KN, Whitacre L, Lou Y, Squires EJ, Pearson W. Dietary Fermentation Product of Aspergillus Oryzae Prevents Increases in Gastrointestinal Permeability (‘Leaky Gut’) in Horses Undergoing Combined Transport and Exercise. Animals. 2023; 13(5):951. https://doi.org/10.3390/ani13050951
Chicago/Turabian StyleMcGilloway, Melissa, Shannon Manley, Alyssa Aho, Keisha N. Heeringa, Lynsey Whitacre, Yanping Lou, E. James Squires, and Wendy Pearson. 2023. "Dietary Fermentation Product of Aspergillus Oryzae Prevents Increases in Gastrointestinal Permeability (‘Leaky Gut’) in Horses Undergoing Combined Transport and Exercise" Animals 13, no. 5: 951. https://doi.org/10.3390/ani13050951
APA StyleMcGilloway, M., Manley, S., Aho, A., Heeringa, K. N., Whitacre, L., Lou, Y., Squires, E. J., & Pearson, W. (2023). Dietary Fermentation Product of Aspergillus Oryzae Prevents Increases in Gastrointestinal Permeability (‘Leaky Gut’) in Horses Undergoing Combined Transport and Exercise. Animals, 13(5), 951. https://doi.org/10.3390/ani13050951






