Abstract
Salmonella enterica is, globally, an important cause of human illness with beef being a significant attributable source. In the human patient, systemic Salmonella infection requires antibiotic therapy, and when strains are multidrug resistant (MDR), no effective treatment may be available. MDR in bacteria is often associated with the presence of mobile genetic elements (MGE) that mediate horizontal spread of antimicrobial resistance (AMR) genes. In this study, we sought to determine the potential relationship of MDR in bovine Salmonella isolates with MGE. The present study involved 111 bovine Salmonella isolates obtained collectively from specimens derived from healthy cattle or their environments at Midwestern U.S. feedyards (2000–2001, n = 19), or specimens from sick cattle submitted to the Nebraska Veterinary Diagnostic Center (2010–2020, n = 92). Phenotypically, 33/111 isolates (29.7%) were MDR (resistant to ≥3 drug classes). Based on whole-genome sequencing (WGS; n = 41) and PCR (n = 111), a MDR phenotype was strongly associated (OR = 186; p < 0.0001) with carriage of ISVsa3, an IS91-like Family transposase. In all 41 isolates analyzed by WGS ((31 MDR and 10 non-MDR (resistant to 0–2 antibiotic classes)), MDR genes were associated with carriage of ISVsa3, most often on an IncC type plasmid carrying blaCMY-2. The typical arrangement was floR, tet(A), aph(6)-Id, aph(3″)-Ib, and sul2 flanked by ISVsa3. These results suggest that AMR genes in MDR S. enterica isolates of cattle are frequently associated with ISVsa3 and carried on IncC plasmids. Further research is needed to better understand the role of ISVsa3 in dissemination of MDR Salmonella strains.
1. Introduction
Salmonella enterica subsp. enterica (S. enterica) is, globally, an important cause of human illness, and in the United States (U.S.), it is estimated to cause 1.35 million infections, 26,500 hospitalizations, and 420 deaths each year [1]. Although ranking behind seeded vegetables, eggs, and poultry, beef is a significant attributable source of S. enterica [2]. Specific to nontyphoidal Salmonella, beef ranks 14th, 8th, and 8th out of the top 37 pathogen–food pairs in burden of illness in the U.S. in terms of number of illnesses, basic cost, and economic cost, respectively [3]. In the human patient, systemic Salmonella infection requires antibiotic therapy [4,5], and when the strain is MDR (resistant to ≥3 antibiotic classes) [6], the case is particularly problematic. First-line antibiotic therapy for systemic Salmonella infections in humans includes third-generation cephalosporins (e.g., ceftriaxone), fluoroquinolones (e.g., ciprofloxacin), and macrolides (e.g., azithromycin) [4,5]. However, fluoroquinolones have adverse side effects in children and pregnant women [7,8], in which case ceftriaxone and azithromycin are the drugs of choice. Unfortunately, ceftriaxone and ciprofloxacin resistance in human Salmonella isolates has increased in recent years [9,10].
S. enterica is also a primary pathogen in cattle, mainly causing enteritis in calves between 2 and 6 weeks of age, but can also cause enteritis, pneumonia, and abortions in adult animals, with most clinical infections associated with S. Dublin and S. Typhimurium [11]. However, more than 143 serotypes have been found in cattle lacking clinical signs of illness, indicating a large reservoir of diversity in populations [12]. S. enterica is often associated with subclinical infections, but may have a morbidity of over 50% in calves, with a case–fatality rate approaching 100% without treatment [13]. The most common resistance pattern in S. Typhimurium is ampicillin, chloramphenicol, streptomycin, sulfamethoxazole, and tetracycline (ACSSuT) [13]. This MDR pattern has, historically, most often corresponded to a clone of S. Typhimurium known as bacteriophage definitive type (DT) 104 (DT104), which often causes severe disease in both animals and humans [14].
The prevalence of AMR and MDR in Salmonella isolated from cattle, their environments, and beef products has increased over the past few decades. The prevalence of MDR S. Newport isolates from cattle, their environments, and beef products in Canada increased from 2000 to 2002 compared to before 2000, with 50% of isolates resistant to at least 11 antimicrobials, including the extended-spectrum cephalosporins [15]. In a study of clinical Salmonella isolates from cattle in Alberta, Canada from 2006 to 2014, S. Typhimurium and S. Dublin constituted the majority of isolates, and the prevalence of MDR was 89.1% and 93.8%, respectively [13]. In S. Dublin isolates from cattle in California, compared to isolates from 1993 to 1999, there was an increase in resistance among quinolone and cephalosporin drugs from 2006 to 2010, and an increase in the number of isolates with an MDR profile [16].
In bacteria, the spread of AMR genes is mainly the result of mobile genetic elements (MGE), which enable intracellular and intercellular movement of DNA, e.g., insertion sequences (IS), transposons (Tn), integrons (In), plasmids, integrative conjugative elements (ICE), and integrative mobilizable elements (IME) [17,18]. DNA containing AMR genes is also spread intercellularly via transduction and transformation mechanisms [17]. Many MDR Salmonella such as S. Typhimurium DT104 contain an IME known as a Salmonella Genomic Island (SGI) [19]. SGI1 variants contain different combinations of genes responsible for the ACSSuT phenotype, and, in addition, those for resistance to florfenicol, gentamycin, spectinomycin, tobramycin, and trimethoprim [19]. To date, 12 variants of SGI1 are recognized among at least 16 different Salmonella serotypes [19].
Recent studies have shown that ICEMh1 and -like elements in respiratory pathogens of the Pasteurellaceae family readily spread among each other in cases of bovine respiratory disease (BRD), and have the potential to spread into Salmonella [20]. Spread of these ICEs is especially evident in outbreaks of BRD in high-risk stocker and feedlot calves following metaphylactic and therapeutic administration of antibiotics [21,22,23,24]. ICEMh1 in Mannheimia haemolytica and ICEMh1-like elements such as ICEPmu1 in Pasteurella multocida are fully transmissible and proven to integrate into P. multocida, M. haemolytica, and Escherichia coli recipients. They potentially integrate into Salmonella based on DNA analytical evidence of the target integration site in the chromosome. Each of these ICEs transmits a potent arsenal of antibiotic resistance. ICEPmu1 contains 12 resistance genes: strA and strB (conferring resistance to streptomycin), aphA1 (gentamicin), sul2 (sulfonamides), tet(H) (tetracyclines), floR (phenicols), erm(42) (macrolides and lincosamides), aadB (gentamicin), aadA15 (streptomycin and spectinomycin), blaOXA-2 (β-lactams), and msr(E) and mph(E) (macrolides). ICEMh1 contains five resistance genes: strA (aph(3″)-Ib), strB (aph(6)-Id), aphA1, sul2, and tet(H). Antibiotics for metaphylaxis (control) of BRD could potentially select for AMR Salmonella secondary to selection for respiratory pathogens carrying ICEMh1 and ICEMh1-like elements. In addition, they could directly select for AMR Salmonella strains that contain SGI1 variants.
We hypothesize that ICEMh1, ICEPmu1, or other ICEMh1-like elements occur in Salmonella isolates. To our knowledge, no studies have investigated this hypothesis. The objectives of this study were to determine, in a set of Salmonella enterica isolates from cattle or their environments, the frequency of: (1) AMR genes typically associated with ICEMh1 and ICEMh1-like integrative conjugative elements; (2) Salmonella Genomic Island 1 (SGI1) variants and their associated AMR genes; and (3) other mobile genetic elements and their potential association with MDR.
2. Materials and Methods
2.1. Bacterial Strains
2.1.1. S. enterica Isolates from Midwestern U.S. Feedyards from 2000 to 2001
All S. enterica strains used in this study (n = 111) were isolates from 2000 to 2001 (n = 19) or 2011 to 2020 (n = 92). The 19 isolates from 2000 to 2001 were a subset of 530 isolates from feedlot beef cattle feces or their pen environments in Midwestern U.S. feedyards [25] (Table 1). All 530 isolates had been serotyped and tested for antimicrobial susceptibility phenotype in 2006 using a standardized National Animal Resistance Monitoring System (NARMS) protocol, and also were tested by PCR for class 1 integron genes [26]. Of the 530 isolates from that study, 0 were positive for class 1 integron genes by PCR; however, based on the NARMS 2006 results, 13 were MDR (Table 1). These 13 MDR isolates were selected for inclusion in the present study; 6 other isolates that were resistant to only 1 antimicrobial that originated from the same sample or pen of cattle were also included for whole-genome sequence (WGS) and/or other test comparisons. Immediately prior to this study, all 19 strains were retested for antimicrobial susceptibility using the Sensititre BOPO7F veterinary plates (Thermo Fisher Scientific, Waltham, MA, USA) to provide additional data regarding their susceptibility to antimicrobials in current use for cattle, including those relevant for respiratory pathogens (Table 1). Based on the BOPO7F results, 2 of the 13 strains had become pan-susceptible in storage. Eleven of the 13 strains, including the 2 that had become pan-susceptible, and 6 non-MDR strains from the same study [26], were selected for WGS (Table 1).

Table 1.
Salmonella enterica isolates from 2000 to 2001 from feedlot beef cattle feces or pen environments used in this study.
2.1.2. Bacterial Strains Used as Controls for Multiplex qPCR (mqPCR) Assay for Detection of AMR Genes Associated with ICEPmu1 and ICEMh1
M. haemolytica strain 2308 was isolated from a bovine clinical sample by the NVDC from a diagnostic submission. This isolate had previously been determined by Sanger sequencing to contain eight AMR genes associated with ICEPmu1, namely aphA1, sul2, tetR(H), floR, erm(42), blaOXA2, msr(E), and mph(E), with four of these genes also associated with ICEMh1; all eight genes had been detected by a mqPCR assay (described below) that had been co-developed by one of the authors (J.D.L.) [27], hence M. haemolytica strain 2308 was validated for use as positive control for this mqPCR assay. E. coli strain 25922 (American Type Culture Collection) is a laboratory strain that does not possess these genes, and was used as a negative control for the mqPCR assay (described below).
2.1.3. Isolates from Nebraska Veterinary Diagnostic Center from 2011 to 2020
A second source of S. enterica strains was accessions from cattle systems to the Nebraska Veterinary Diagnostic Center (NVDC) during the period of 2011–2020. Of 98 Salmonella isolates identified from these accessions, 92 were viable from frozen stocks and included in the present study. Of these 92 isolates, 83 were from 42 of the 93 counties in Nebraska; 5 were from Missouri; and 1 each was from California, Colorado, Idaho, and Iowa. The 92 isolates had been serotyped previously as part of the diagnostic process, and included 27 different serotypes with S. Typhimurium (including 3 var. 5-) (n = 18), S. Newport (n = 13), S. Dublin (n = 10), S. Montevideo (n = 8), and S. Muenster (n = 7) constituting the 5 most prevalent and 60.9% (56/92) of the total (Table S1). A signalment (e.g., age, sex) and clinical history (e.g., diarrhea, abortion) and/or pathology data (e.g., enteritis, pneumonia) was provided in association with 84 (91.3%) and 78 (84.8%) of the cases, respectively. Salmonellae were most commonly isolated from accessions involving unweaned/neonatal calves (38.0%) and cows/heifers (29.3%) (Table S2). Overall, based on the clinical history and accompanying laboratory results, the Salmonella isolates were associated with disease (i.e., salmonellosis) in 81.5% of the accessions. Diarrheal disease (enteritis/colitis) and pneumonia were the most common manifestations, reported in 53.3% and 20.7% of the accessions, respectively.
The NVDC isolates were subjected to antimicrobial susceptibility testing either at the time of the accession or immediately prior to this study, if they had not been previously tested. Testing was conducted at the time of the accession either using the Sensititre BOPO6F or BOPO7F plate formats (Thermo Fisher Scientific Waltham, MA, USA), or immediately prior to this study using the Sensititre BOPO7F. Antimicrobial susceptibility testing was conducted using Clinical and Laboratory Standards Institute (CLSI, Annapolis, MD, USA) methods and recommended quality control strains for the broth microdilution assay [28]. Veterinary specific breakpoints were applied when available [29]. Of the 92 NVDC isolates, 22 (23.9%) were MDR, with serotypes S. Dublin (n = 10) and S. Newport (n = 5) combined representing 68.1% (15/22) of the MDR isolates (Table 2). Of the 22 MDR isolates, resistance was most frequent to florfenicol and sulfadimethoxine (95.4% each), followed sequentially by 1 or more of the tetracyclines (chlortetracycline, oxytetracycline, and/or tetracycline; 90.9%), ceftiofur (77.3%), and a fluoroquinolone (danofloxacin and/or enrofloxacin; 40.9%). Resistance to macrolides (clindamycin, gamithromycin, tiamulin, tilmicosin, tildipirosin tulathromycin, and tylosin tartrate) was considered intrinsic and not reported. Aminoglycoside test results (gentamicin, neomycin, and spectinomycin) were also largely excluded since breakpoints and assessments of susceptibility or resistance for Salmonella are difficult to determine. Twenty of the 22 MDR strains were selected for WGS.

Table 2.
MDR Salmonella enterica isolates from cattle systems accessions to the NVDC during the period of 2011–2020.
2.2. Culture of Bacterial Strains and DNA Preparation
Frozen stock cultures (−80 °C) of Salmonella strains were streaked for isolation onto Luria Broth (Miller, Appleton, WI, USA; LB) Agar (Becton, Dickinson and Company, Sparks, MD, USA) and incubated 18–24 h at 37 °C. A single well-isolated colony was used to inoculate 5 mL LB, and this culture was incubated 24 h, stationary at 37 °C. A 2-mL aliquot of broth culture was moved into the GeneJET DNA Genomic Purification Kit (Thermo Fisher Scientific, Waltham, MA, USA) to prepare the DNA template for mqPCR reactions. Extractions were performed according to the manufacturer’s protocol. Frozen stock cultures (−80 °C) of Mannhemia haemolytica control strains were streaked for isolation onto Trypticase Soy Agar (TSA) with 5% Sheep Blood (BD) and incubated 18–24 h at 37 °C. A single well-isolated colony was used to inoculate 50 mL Brain Heart Infusion (BHI) in a 250 mL Erlenmeyer flask, aerated at 150 rpm for 24 h, at 37 °C. A 2 mL aliquot of broth culture was transferred into the GeneJET DNA Genomic Purification Kit (Thermo Fisher Scientific, Waltham, MA, USA) to prepare the DNA template for mqPCR reactions. Extractions were performed according to the manufacturer’s protocol. Purified DNA concentration for each isolate was determined via NanoDrop One (Thermo Fisher Scientific, Waltham, MA, USA) with M. haemolytica strain 2308 and E. coli strain 29522 as the positive and negative organismal controls, respectively, for the mqPCR assay (described below) and Invitrogen UltraPure Water (Thermo Fisher Scientific, Waltham, MA, USA) in place of DNA as the negative reaction control.
2.3. mqPCR
The mqPCR assay and targets were in part based on previous work with applications to BRD pathogens [27]. Four-plex mqPCR (25-µL reaction) assays included targets, reagents, and primers as described in Table S4. The mqPCR reaction consisted of 12.5 µL of 2X Quantifast Multiplex PCR Master Mix (Qiagen), 1.0 μL of each primer probe mix (4 μL total) containing F (10 μM), R (10 μM), P (5 μM), 9.5 μL Invitrogen UltraPure Water (Thermo Fisher Scientific, Waltham, MA, USA), and 2.0 µL (5 ng/μL) of template DNA. mqPCR reactions were carried out in a CFX96 (Bio-Rad, Hercules, CA, USA) under the following conditions: 95 °C for 5 min, then 45 cycles of 95 °C for 15 s, 59 °C for 40 s.
2.4. Endpoint PCR
Frozen stock cultures (−80 °C) of bacterial strains were streaked for isolation onto Luria Broth (Miller; LB) Agar (Becton, Dickinson and Company, Sparks, MD) and incubated 18–24 h at 37 °C. A single well-isolated colony was picked, suspended in 50 μL of UltraPure Water, and heated at 95 °C in the thermocycler for 10 min. A 2.0 µL aliquot of this DNA template was used in the 25-µL PCR reaction. Individual 25-µL reaction PCR assays were conducted using primer pairs as shown in Table S5 [27,30,31]. The PCR reaction consisted of 2.5 µL 10X ThermoPol Reaction Buffer, 1.0 μL of each forward and reverse primer (10 μM each, 2 μL total), 0.5 µL dNTP mix (10 mM each dNTP), 0.25 µL NEB Taq DNA Polymerase (New England Biolabs, Ipswich, MA, USA), 17.75 µL UltraPure Water, and 2.0 µL (5 ng/μL) of template DNA. UltraPure Water volume was adjusted for multiplex PCR reactions. PCR reactions were carried out in a T100 Thermal Cycler (Bio-Rad, Hercules, CA, USA) under the following conditions: 95 °C for 5 min, then 30 cycles of 95 °C for 15 s, 59 °C for 40, 72 °C for 30 s, and a final elongation at 72 °C for 7 min. The positive organismal control was S. Typhimurium strain RM014 (this study), and the negative reaction control was UltraPure Water in place of DNA. PCR reactions were run on 1.2% agarose TAE gels stained with ethidium bromide and visualized on a ChemiDoc MP Imager (Bio-Rad, Hercules, CA, USA).
2.5. WGS
WGS was conducted at the Iowa State University Veterinary Diagnostic Laboratory by Dr. Ganwu Li. Pure cultures were used for DNA extraction with the MagMAX Pathogen RNA/DNA Kit (Thermo Fisher Scientific, Waltham, MA, USA) and a Kingfisher Flex instrument (Thermo Fisher Scientific, Waltham, MA, USA) following the manufacturer’s instructions. Nucleic acid was eluted into 45 μL of elution buffer and stored at −80 °C until used. Indexed genomic libraries were prepared using the Nextera XT DNA Library Prep Kit (Illumina, San Diego, CA, USA) and quantified by the Qubit fluorometer dsDNA HS kit (Thermo Fisher Scientific, Waltham, MA, USA). The library was sequenced on an Illumina MiSeq platform (Illumina, San Diego, CA, USA) with either MiSeq Reagent Kit v2 (500 cycle) or MiSeq® Reagent Kit v3 (600 cycle). For Nanopore sequencing, pure cultures were submitted to Iowa State University DNA Facility (Ames, IA, USA) for DNA extraction and Nanopore sequencing on the Oxford Nanopore GridION X5 (Oxford Nanopore Technologies, Oxfordshire, England).
2.6. Sequencing Quality Control and Genome Assembly
Following sequencing, Illumina short read quality was assessed using FastQC v0.11.7 (Babraham Bioinformatics, 2018, Babraham Institute, Cambridge, UK). BBDuk (v37.62) was used to trim adapters from the lllumina short reads, and any short reads with average quality score (Q score) below 30 were discarded. The porechop (v0.2.4) was used to trim adapters from the Nanopore long reads. The average sequencing depth of each isolate was estimated by dividing the total length of its cleaned reads by the genome size. Additionally, Illumina reads and Nanopore long reads from each isolate were hybrid de novo assembled using Unicycler (v0.4.9). Isolates with unclosed genomes were reassembled by Raven (v1.5.1) with Nanopore long reads and then polished by Pilon (v1.24) with Illumina short reads. All isolates sequenced in this study had >95× depth and N50 > 4.6 Mb with genome sizes between 4.6 and 5.0 Mb (Megabases; million bases). All the genomes were closed.
2.7. GenBank Accessions
All WGS data on the 41 isolates is available under NCBI BioProject PRJNA929056.
2.8. Bioinformatic and Statistical Analyses
Genomic DNA sequence similarity searches were conducted using BLAST+2.11.0 [32]. Genomes were annotated using NCBI Prokaryotic Genome Annotation Pipeline (PGAP) 2021-07-01.build5508 (https://www.ncbi.nlm.nih.gov/genome/annotation_prok/ accessed on 1 July 2021) [33]. Sequence visualization and analysis was conducted using Geneious Prime 2021.2.2 (https://www.geneious.com, accessed on 1 July 2021). AMR gene identification and verification was conducted using CARD 3.1.3 (https://card.mcmaster.ca/, accessed on 1 July 2021) [34] and ResFinder 4.1 2021-08-16 [35]. Maximum-likelihood phylogenies were estimated using PhyML 3.2 [36]. Sequence alignments were conducted using Muscle 3.8.425 [37]. Pan-genome analyses were conducted using Roary 3.13.0 [38]. Core phylogeny with metadata analysis was conducted using Phandango 1.3.0 [39]. The association between an MDR phenotype and ISVsa3 genotype (combined results of PCR and WGS) in the 111 S. enterica isolates was determined by calculation of the odds ratio (OR) with 95% confidence interval (CI) and p value (<0.05 interpreted as significant) using MedCalc® statistical software, Version 20.218 [40].
3. Results
3.1. Frequency of Antimicrobial Resistance (AMR) Genes Typically Associated with ICEMh1 and ICEMh1-like Integrative Conjugative Clements
Total genomic DNA extracted from all S. enterica isolates listed in Table 1 and Table S3 except RM001, RM002, RM003, RM004, RM005, and RM006 (n = 105) was tested by mqPCR for AMR genes located on ICEMh1 and ICEMh1-like elements, including tetR(H) (tetracycline), msr (macrolide), mph (macrolide), erm (macrolide), floR (phenicol), sul2 (sulfonamide), blaOXA2 (β-lactamase), and aphA1 (aminoglycoside). Additional genes tested for by endpoint PCR in these 105 isolates included blaCMY-2 (β-lactamase), ISVsa3 (IS91-like Family transposase), tet(A) (tetracycline), and sul2 (sulfonamide). By mqPCR, the frequency of isolates positive was floR, 30.5%; sul2, 30.5%; and aphA1, 4.8%, whereas 0% were positive for tetR(H), erm, msrE, mphE, or blaoxa2 (Table S6). Hence, the isolates were negative for most AMR genes carried by ICEMh1 and ICEMh1-like elements, suggesting that floR and sul2 were possibly associated with one or more other mobile genetic elements. Endpoint PCR assays revealed that 25.7%, 30.5%, and 28.6% were positive for blaCMY-2, ISVsa3, and tet(A), respectively (Table S6). Based on mqPCR and endpoint PCR results, the correlation coefficients (CORREL, Excel 2016) were 1.00 for floR versus ISVsa3 and 0.96 for sul2 versus ISVsa3, suggesting that floR and sul2 were associated with ISVsa3 instead of ICEMh1 and ICEMh1-like elements.
3.2. Frequency of Salmonella Genomic Island 1 (SGI1) and SGI1 Variants
In our previous study [26], 0 of 530 beef feedlot pen S. enterica isolates was positive by endpoint PCR for the class 1 integron gene (intI1), suggesting that SGI1 was not involved in MDR. We again analyzed the 19 MDR isolates from that study (Table 1) and the 22 NVDC MDR isolates (Table 2) for intI1 by WGS. By WGS, consistent with the previous study [25], 0 of 9 MDR feedlot pen isolates tested were positive for intI1; however, 3 of 22 WGS NVDC isolates (13.6%) and 3 of 41 WGS isolates (7.3%) overall were positive for intI1; all 3 intI1 positive isolates were MDR (Table S6). These three isolates (RM055, RM074, and RM101), in addition to intI1, had qacEΔ1 and sul1, and one (RM055) also had aadA2. Interestingly, none of these genes, which are markers of SGI1, were on the chromosome; all were on a plasmid that also carried ISVsa3 (Table S6).
3.3. Other Mobile Genetic Elements, Their Genomic Locations, and MDR Association
By WGS, all 41 isolates (100%) had the following AMR genes on the chromosome: aac(6′), aac(6′)-Iaa, and aadA (all involved in aminoglycoside resistance); ampH (a penicillin-binding protein; PBP); bacA (involved in bacitracin resistance); and mrdA (a PBP known to confer reduced susceptibility to carbapenems) (Table S6). However, the presence of these genes was not associated with AMR for the respective antibiotic classes. Instead, resistance was associated with the following: aminoglycoside with aph(3″)-Ib and aph(6)-Id; phenicol with floR; tetracycline with tet(A); sulfonamide with sul2; and β-lactam with blaCMY-2 (Table S6). A total of 25 out of 41 isolates were positive for all 5 genes: floR, tet(A), aph(6)-Id, aph(3″)-Ib, and sul2 (Table 3), typically arranged in that order and flanked by ISVsa3 (Figure 1 and Figure 2). Hence, an MDR phenotype was predominantly associated with carriage of ISVsa3 in which the genes were most often located on an IncC type plasmid that also carried blaCMY-2 (Table 4; Figure 1). Based on the combined results of endpoint PCR and WGS, 31/33 (93.9%) MDR isolates were positive for ISVsa3, whereas 6/78 non-MDR isolates (7.7%) were positive for ISVsa3 (OR = 186.00, p < 0.0001; Table 5). In addition, based on combined data from endpoint PCR and WGS, of the 111 isolates, the number (percentage) positive for the above-mentioned genes was: 38 (34.2%) for ISVsa3; 27 (24.3%) for blaCMY-2; 33 (29.7%) for floR; 30 (27.0%) for tet(A); 38 (34.2%) for sul2; and 31 (27.9%) for both aph(3″)-Ib and aph(6)-Id (Tables S6 and S7). The serotypes in which ISVsa3 was found included S. Derby, S. Uganda, S. Typhimurium, S. Newport, S. Dublin, S. Muenster, S. Heidelberg, and S. Saintpaul (Table S6).

Table 3.
Number of AMR genes associated with ISVsa3 and their locations in Salmonella enterica isolates as detected by WGS.
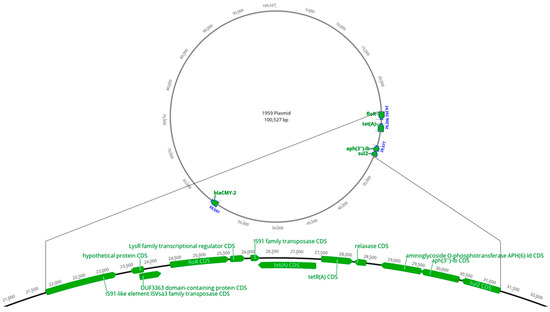
Figure 1.
Location of ISVsa3 and flanking antimicrobial resistance genes on a blaCMY-2 positive IncC plasmid of Salmonella Uganda isolate 1959.
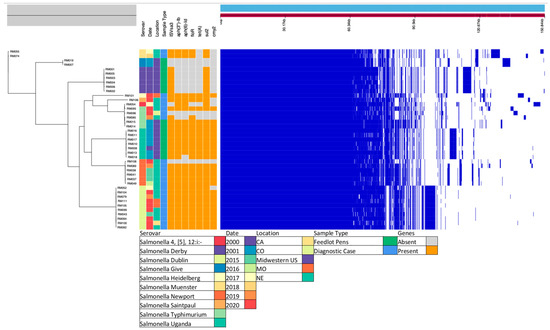
Figure 2.
Maximum-likelihood phylogenetic tree constructed from an alignment of core genes and selected metadata. The right panel shows a broad overview of the presence/absence of all genes sequenced for each strain. The phylogeny depicts the evolutionary relationship of the isolates sequenced. Ten serovars were represented in the metadata of the 41 S. enterica isolates subjected to WGS. These diagnostic cases and feedlot pen strains were isolated in eight different years spanning a ten-year period from different areas in the US. The presence and absence of ISVSa3 and pertinent genes can be visualized in orange and grey, respectively (presence of ISVsa3, 36/41; aph(3″)-Ib, 30/41; aph(6)-Id, 29/41; floR, 30/41; tetA, 27/41; sul2, 36/41; cmy2, 25/41). The core gene alignment to the right (in dark blue) reflects the conservation and diversion in these genomes.

Table 4.
Frequency of ISVsa3, associated AMR genes, and their genomic locations as detected by WGS.

Table 5.
A 2 × 2 contingency table showing association between MDR phenotype and ISVsa3 genotype with OR calculation.
3.4. Core Gene Alignment and Metadata
A phylogenetic tree was constructed from an alignment of core genes and selected metadata, depicting the evolutionary relationship of the isolates sequenced (Figure 2). The core gene alignment reflected the conservation and diversion in these genomes.
3.5. ISVsa3 and Associated AMR Genetic Segment Alignment
An alignment of the genetic segment of the 36 sequenced isolates carrying ISVsa3 and associated AMR genes is shown in Figure S1.
4. Discussion
In this study, the first objective was to address the hypothesis that ICEMh1, ICEPmu1 or other ICEMh1-like elements occur in Salmonella isolates. We found no evidence of these BRD pathogen-associated ICE elements in our collection of 111 isolates. It is possible that one or more of these ICE elements might have been detected if more isolates were tested, and if we had tested isolates representing a more widespread area of the country, different production settings, and cattle that had been subjected to metaphylactic treatment for BRD. A number of studies have assessed the effects of metaphylactic regimens for BRD on the prevalence and selection for AMR Salmonella in field trials. A randomized controlled longitudinal study that followed cattle through the entire feeding period to harvest found that one dose of tulathromycin administered to healthy cattle at feedlot arrival did not result in an increase in the prevalence or AMR of Salmonella [41]. We hypothesize that detection of ICEMh1, ICEPmu1, or other ICEMh1-like elements in Salmonella would be more likely if one were to culture large numbers of fecal or other samples from BRD high-risk calves having respiratory colonization with ICEMh1-positive M. haemolytica [21,22,23,24], and especially following metaphylactic treatment, but this was beyond the scope of our study. Information concerning antimicrobial treatment was not available, and that concerning the signalment and clinical history was also limited.
Our second objective was to address whether SGI1 or its variants were associated with MDR, and we found that only 3 MDR isolates (7.3%) had SGI1 genes, and in these isolates, the genes were carried on a plasmid that also carried ISVsa3. One of these three isolates (RM101) carried SGI1 genes on an IncC plasmid. SGI1 cannot transfer itself into a new host because it does not carry a full set of conjugation genes, but it is mobilizable, and can be transferred if an IncC plasmid is present in the donor [19]. SGI1 only excises from the chromosome in the presence of a helper plasmid [42], and although SGI1 is known to modify and use the conjugation apparatus encoded by IncC, the two (SGI1 and IncC) are incompatible [42]. SGI1 destabilizes IncA and IncC plasmids after a few generations and, conversely, the presence of an IncC plasmid enhances the recombination rate within SGI1, leading to the generation of SGI1 deletion variants [42]. Interestingly, in our study, 20 of 29 WGS isolates (69.0%) that, collectively, had 4 or 5 AMR genes carried them on an IncC plasmid.
Our third objective was to determine the frequency of other MGE and their association with MDR, which yielded the main finding of the study: MDR was strongly associated with the presence of ISVsa3 (IS91-like Family transposase). This appears to be a novel finding, although other investigators recently reported similar genetic and phenotypic AMR profiles in 15 MDR S. Dublin isolates from retail meat and human patients [43]. In that study, nothing was stated about ISVsa3, but when we searched the associated NCBI BioProject PRJNA357723 sequence data, we found ISVsa3 (also listed as IS91-like element) in 12 of the 15 isolates. Besides our finding that ISVsa3 was strongly associated with MDR in Salmonella, our results extend these findings in that ISVsa3 was found in MDR isolates in seven other serotypes besides S. Dublin.
Previous studies have shown that ISVsa3 was first identified in the fish pathogen Vibrio salmonicida [44], and made its way into other fish pathogens, e.g., Edwardsiella piscicida [45], and further into pathogens isolated from other animals and humans, e.g., Salmonella Choleraesuis and Acinetobacter baumannii [44], carrying with it high-level resistance to antibiotics such as the tetracyclines. ISVsa3 is frequently found on conjugative plasmids [44] and poses a significant threat to spread AMR.
ISVsa3 is an IS91-like MGE, referred to as an Insertion Sequence Common Region (ISCR) [46,47]. In our study, ISVsa3 was found to be in a conserved relationship with floR, tet(A), aph(6)-Id, aph(3″)-Ib, and sul2 in 72.2% (26 of 36 ISVsa3-positive) of the WGS S. enterica isolates. Due to this insertion sequence families’ unique method of transposition, they are capable of and frequently responsible for mobilizing many classes of AMR genes, and are considered an evolutionary feature of IncC plasmids [47,48]. In most positive strains in our study, this ISCR was located on plasmids, and particularly IncC, while only 3 of those carrying ISVsa3 and the associated AMR genes were found on the chromosome. The strong association of ISVsa3 with MDR in the Salmonella isolates in our study and the knowledge that ISCR frequently assemble multiple AMR genes and transpose them into conjugatable plasmids suggests this particular transposon poses a significant threat to increasing MDR. Further research is needed to better understand the role of ISVsa3 in dissemination of MDR in Salmonella.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/microorganisms11030631/s1, Table S1. Serotypes of Salmonella isolates from cattle in accessions submitted to the Nebraska Veterinary Diagnostic Center from 2011 to 2020; Table S2. Frequency of association of Salmonella isolation with bovine source and disease manifestation in Nebraska Veterinary Diagnostic Center accessions; Table S3. List of Salmonella isolates from Nebraska Veterinary Diagnostic Center arranged in chronological order of isolation with accompanying information concerning signalment, clinical history, sample type, serotype, and antimicrobial resistance phenotype; Table S4. Primers, probes, and products of multiplex qPCR assays; Table S5. Primer pairs and products used in endpoint PCR assays; Table S6. Antibiograms, mqPCR, endpoint PCR, and whole-genome sequencing results of Salmonella enterica isolates (n = 111); Table S7. Combined endpoint PCR and WGS results for ISVsa3, blaCMY-2, floR, tet(A), sul2, aph(3″)-Ib, and aph(6)-Id on Salmonella enterica isolates (n = 111); Figure S1. Alignment of the genetic segment of the 36 sequenced isolates carrying ISVsa3 and associated AMR genes.
Author Contributions
Conceptualization, R.A.M. and J.D.L.; methodology, J.D.L., G.L.L., and R.J.F.; software, R.J.F.; validation, R.A.M., J.D.L., G.L.L., and R.J.F.; formal analysis, R.A.M., G.L.L., and R.J.F.; investigation, G.L.L. and R.J.F.; resources, R.A.M., J.D.L., and G.L.L.; data curation, R.A.M., G.L.L., R.J.F., and E.N.M.; writing—original draft preparation, R.A.M., G.L.L., and R.J.F.; writing—review and editing, R.A.M., G.L.L., R.J.F., J.D.L., and E.N.M.; visualization, R.A.M., G.L.L., and R.J.F.; supervision, R.A.M., G.L.L., and J.D.L.; project administration, R.A.M.; funding acquisition, R.A.M. and J.D.L. All authors have read and agreed to the published version of the manuscript.
Funding
Funding for this project was provided by the Nebraska Beef Council and the Beef Checkoff.
Data Availability Statement
All WGS data on the 41 isolates is available under NCBI BioProject PRJNA929056. All other data are available within this article and the supplementary materials.
Acknowledgments
The authors thank Ganwu Li for conducting the whole-genome sequencing, and Macy Rasmussen and Brandon Stewart for excellent technical assistance in this project. Funding for this project was provided by the Nebraska Beef Council and the Beef Checkoff.
Conflicts of Interest
The authors declare no conflict of interest.
References
- CDC. Antibiotic Resistance Threats in the United States; U.S. Department of Health and Human Services, CDC: Atlanta, GA, USA, 2019. [Google Scholar]
- Richardson, L.C.; Bazaco, M.C.; Parker, C.C.; Dewey-Mattia, D.; Golden, N.; Jones, K.; Klontz, K.; Travis, C.; Kufel, J.Z.; Cole, D. An updated scheme for categorizing foods implicated in foodborne disease outbreaks: A tri-agency collaboration. Foodborne Pathog. Dis. 2017, 14, 701–710. [Google Scholar] [CrossRef] [PubMed]
- Scharff, R.L. Food attribution and economic cost estimates for meat- and poultry-related illnesses. J. Food Prot. 2020, 83, 959–967. [Google Scholar] [CrossRef] [PubMed]
- DuPont, H.L. Clinical practice. Bacterial diarrhea. N. Engl. J. Med. 2009, 361, 1560–1569. [Google Scholar] [CrossRef] [PubMed]
- Shane, A.L.; Mody, R.K.; Crump, J.A.; Tarr, P.I.; Steiner, T.S.; Kotloff, K.; Langley, J.M.; Wanke, C.; Warren, C.A.; Cheng, A.C.; et al. 2017 Infectious Diseases Society of America clinical practice guidelines for the diagnosis and management of infectious diarrhea. Clin. Infect. Dis. 2017, 65, e45–e80. [Google Scholar] [CrossRef]
- Magiorakos, A.P.; Srinivasan, A.; Carey, R.B.; Carmeli, Y.; Falagas, M.E.; Giske, C.G.; Harbarth, S.; Hindler, J.F.; Kahlmeter, G.; Olsson-Liljequist, B.; et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: An international expert proposal for interim standard definitions for acquired resistance. Clin. Microbiol. Infect. 2012, 18, 268–281. [Google Scholar] [CrossRef]
- Burkhardt, J.E.; Walterspiel, J.N.; Schaad, U.B. Quinolone arthropathy in animals versus children. Clin. Infect. Dis. 1997, 25, 1196–1204. [Google Scholar] [CrossRef]
- Choi, S.H.; Kim, E.Y.; Kim, Y.J. Systemic use of fluoroquinolone in children. Korean, J. Pediatr. 2013, 56, 196–201. [Google Scholar] [CrossRef]
- Medalla, F.; Hoekstra, R.M.; Whichard, J.M.; Barzilay, E.J.; Chiller, T.M.; Joyce, K.; Rickert, R.; Krueger, A.; Stuart, A.; Griffin, P.M. Increase in resistance to ceftriaxone and nonsusceptibility to ciprofloxacin and decrease in multidrug resistance among Salmonella strains, United States, 1996–2009. Foodborne Pathog. Dis. 2013, 10, 302–309. [Google Scholar] [CrossRef]
- Varma, J.K.; Molbak, K.; Barrett, T.J.; Beebe, J.L.; Jones, T.F.; Rabatsky-Her, T.; Smith, K.E.; Vugia, D.J.; Chang, H.G.; Angulo, F.J. Antimicrobial-resistant non-typhoidal Salmonella is associated with excess bloodstream infections and hospitalizations. J. Infect. Dis. 2005, 191, 554–561. [Google Scholar] [CrossRef]
- Barrow, P.A.; Jones, M.A.; Thomson, N. Salmonella. In Pathogenesis of Bacterial Infections in Animals; Wiley: Hoboken, NJ, USA, 2010; pp. 231–265. [Google Scholar] [CrossRef]
- Gutema, F.D.; Agga, G.E.; Abdi, R.D.; De Zutter, L.; Duchateau, L.; Gabriël, S. Prevalence and serotype diversity of Salmonella in apparently healthy cattle: Systematic review and meta-analysis of published studies, 2000–2017. Front. Vet. Sci. 2019, 6, 102. [Google Scholar] [CrossRef]
- Otto, S.J.G.; Ponich, K.L.; Cassis, R.; Goertz, C.; Peters, D.; Checkley, S.L. Antimicrobial resistance of bovine Salmonella enterica ssp. enterica isolates from the Alberta Agriculture and Forestry Disease Investigation Program (2006–2014). Can. Vet. J. 2018, 59, 1195–1201. [Google Scholar] [PubMed]
- Threlfall, E.J. Epidemic Salmonella typhimurium DT 104—A truly international multiresistant clone. J. Antimicrob. Chemother. 2000, 46, 7–10. [Google Scholar] [CrossRef] [PubMed]
- Poppe, C.; Martin, L.; Muckle, A.; Archambault, M.; McEwen, S.; Weir, E. Characterization of antimicrobial resistance of Salmonella Newport isolated from animals, the environment, and animal food products in Canada. Can. J. Vet. Res. 2006, 70, 105–114. [Google Scholar]
- Fritz, H.M.; Pereira, R.V.; Toohey-Kurth, K.; Marshall, E.; Tucker, J.; Clothier, K.A. Salmonella enterica serovar Dublin from cattle in California from 1993–2019: Antimicrobial resistance trends of clinical relevance. Antibiotics 2022, 11, 1110. [Google Scholar] [CrossRef] [PubMed]
- Partridge, S.R.; Kwong, S.M.; Firth, N.; Jensen, S. Mobile genetic elements associated with antimicrobial resistance. Clin. Microbiol. Rev. 2018, 31, e00088-17. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Li, X.; Xie, Y.; Bi, D.; Sun, J.; Li, J.; Tai, C.; Deng, Z.; Ou, H.Y. ICEberg 2.0: An updated database of bacterial integrative and conjugative elements. Nucleic Acids Res. 2019, 47, D660–D665. [Google Scholar] [CrossRef]
- Hall, R.M. Salmonella genomic islands and antibiotic resistance in Salmonella enterica. Future Microbiol. 2010, 5, 1525–1538. [Google Scholar] [CrossRef]
- Cameron, A.; Zaheer, R.; McAllister, T.A. Emerging variants of the integrative and conjugant element ICEMh1 in livestock pathogens: Structural insights, potential host range, and implications for bacterial fitness and antimicrobial therapy. Front. Microbiol. 2019, 10, 2608. [Google Scholar] [CrossRef]
- Snyder, E.; Credille, B.; Berghaus, R.; Giguère, S. Prevalence of multi drug antimicrobial resistance in Mannheimia haemolytica isolated from high-risk stocker cattle at arrival and two weeks after processing. J. Anim. Sci. 2017, 95, 1124–1131. [Google Scholar] [CrossRef]
- Snyder, E.R.; Alvarez-Narvaez, S.; Credille, B.C. Genetic characterization of susceptible and multi-drug resistant Mannheimia haemolytica isolated from high-risk stocker calves prior to and after antimicrobial metaphylaxis. Vet. Microbiol. 2019, 235, 110–117. [Google Scholar] [CrossRef]
- Snyder, E.; Credille, B. Mannheimia haemolytica and Pasteurella multocida in bovine respiratory disease: How are they changing in response to efforts to control them? Vet. Clin. N. Am. Food Anim. Pract. 2020, 36, 253–268. [Google Scholar] [CrossRef] [PubMed]
- Woolums, A.R.; Karisch, B.B.; Frye, J.G.; Epperson, W.; Smith, D.R.; Blanton, J., Jr.; Austin, F.; Kaplan, R.; Hiott, L.; Woodley, T.; et al. Multidrug resistant Mannheimia haemolytica isolated from high-risk beef stocker cattle after antimicrobial metaphylaxis and treatment for bovine respiratory disease. Vet. Microbiol. 2018, 221, 143–152. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.R.; Moxley, R.A.; Clowser, S.L.; Folmer, J.D.; Hinkley, S.; Erickson, G.E.; Klopfenstein, T.J. Use of rope devices to describe and explain the feedlot ecology of Salmonella by time and place. Foodborne Pathog. Dis. 2005, 2, 61–69. [Google Scholar] [CrossRef]
- Alam, M.J.; Renter, D.; Taylor, E.; Mina, D.; Moxley, R.; Smith, D. Antimicrobial susceptibility profiles of Salmonella enterica serotypes recovered from pens of commercial feedlot cattle using different types of composite samples. Curr. Microbiol. 2009, 58, 354–359. [Google Scholar] [CrossRef]
- Dutta, E.; Loy, J.D.; Deal, C.A.; Wynn, E.L.; Clawson, M.L.; Clarke, J.; Wang, B. Development of a multiplex real-time PCR assay for predicting macrolide and tetracycline resistance associated with bacterial pathogens of bovine respiratory disease. Pathogens 2021, 10, 64. [Google Scholar] [CrossRef] [PubMed]
- Clinical and Laboratory Standards Institute. VET01. In Performance Standards for Antimicrobial Disk and Dilution Susceptibility Tests for Bacteria Isolated From Animals, 5th ed.; Clinical and Laboratory Standards Institute: Annapolis, MD, USA, 2018; p. 156. [Google Scholar]
- Clinical and Laboratory Standards Institute. VET01S. In Performance Standards for Antimicrobial Disk and Dilution Susceptibility Tests for Bacteria Isolated From Animals, 5th ed.; Clinical and Laboratory Standards Institute: Annapolis, MD, USA, 2020; p. 250. [Google Scholar]
- Sidjabat, H.E.; Paterson, D.L.; Adams-Haduch, J.M.; Ewan, L.; Pasculle, A.W.; Muto, C.A.; Tian, G.B.; Doi, Y. Molecular epidemiology of CTX-M-producing Escherichia coli isolates at a tertiary medical center in Western Pennsylvania. Antimicrob. Agents Chemother. 2009, 53, 4733–4739. [Google Scholar] [CrossRef]
- Vikram, A.L.; Miller, E.; Arthur, T.M.; Bosilevac, J.M.; Wheeler, T.L.; Schmidt, J.W. Similar levels of antimicrobial resistance in US food service ground beef products with and without a “raised without antibiotics” claim. J. Food Prot. 2018, 81, 2007–2018. [Google Scholar] [CrossRef]
- Camacho, C.; Coulouris, G.; Avagyan, V.; Ma, N.; Papadopoulos, J.; Bealer, K.; Madden, T.L. BLAST+: Architecture and applications. BMC Bioinformatics 2009, 10, 421. [Google Scholar] [CrossRef] [PubMed]
- Tatusova, T.; DiCuccio, M.; Badretdin, A.; Chetvernin, V.; Nawrocki, E.P.; Zaslavsky, L.; Lomsadze, A.; Pruitt, K.D. NCBI prokaryotic genome annotation pipeline. Nucleic Acids Res. 2016, 44, 6614–6624. [Google Scholar] [CrossRef]
- Alcock, B.P.; Raphenya, A.R.; Lau, T.T.; Tsang, K.K.; Bouchard, M.; Edalatmand, A.; Huynh, W.; Nguyen, A.L.V.; Cheng, A.A.; Liu, S.; et al. CARD 2020: Antibiotic resistome surveillance with the Comprehensive Antibiotic Resistance Database. Nucleic Acids Res. 2020, 48, D517–D525. [Google Scholar]
- Bortolaia, V.; Kaas, R.F.; Ruppe, E.; Roberts, M.C.; Schwarz, S.; Cattoir, V.; Philippon, A.; Allesoe, R.L.; Rebelo, A.R.; Florensa, A.R.; et al. ResFinder 4.0 for predictions of phenotypes from genotypes. J. Antimicrob. Chemother. 2020, 75, 3491–3500. [Google Scholar] [CrossRef] [PubMed]
- Guindon, S.; Dufayard, J.F.; Lefort, V.; Anisimova, M.; Hordijk, W.; Gascuel, O. New algorithms and methods to estimate maximum-likelihood phylogenies: Assessing the performance of PhyML 3.0. Syst. Biol. 2010, 59, 307–321. [Google Scholar] [CrossRef] [PubMed]
- Edgar, R.C. MUSCLE: Multiple sequence alignment with high accuracy and high throughput. Nucleic Acids Res. 2004, 32, 1792–1797. [Google Scholar] [CrossRef] [PubMed]
- Page, A.J.; Cummins, C.A.; Hunt, M.; Wong, V.K.; Reuter, S.; Holden, M.T.G.; Fookes, M.; Falush, D.; Keane, J.A.; Parkhill, J. Roary: Rapid large-scale prokaryote pan genome analysis. Bioinformatics 2015, 31, 3691–3693. [Google Scholar] [CrossRef] [PubMed]
- Hadfield, J.; Croucher, N.J.; Goater, R.J.; Abudahab, K.; Aanensen, D.M.; Harris, S.R. Phandango: An interactive viewer for bacterial population genomics. Bioinformatics 2018, 34, 292–293. [Google Scholar] [CrossRef] [PubMed]
- MedCalc Software Ltd. Odds Ratio Calculator, Version 20.218. Available online: https://www.medcalc.org/calc/odds_ratio.php (accessed on 25 February 2023).
- Levent, G.; Schlochtermeier, A.; Ives, S.E.; Norman, K.N.; Lawhon, S.D.; Loneragan, G.H.; Anderson, R.C.; Vinasco, J.; Scott, H.M. Population dynamics of Salmonella enterica within beef cattle cohorts followed from single-dose metaphylactic antibiotic treatment until slaughter. Appl. Environ. Microbiol. 2019, 85, e01386-19. [Google Scholar] [CrossRef]
- Huguet, K.T.; Rivard, N.; Garneau, D.; Palanee, J.; Burrus, V. Replication of the Salmonella genomic island 1 (SGI1) triggered by helper IncC conjugative plasmids promotes incompatibility and plasmid loss. PLoS Genet. 2020, 16, e1008965. [Google Scholar] [CrossRef]
- Eyler, A.B.; M’ikanatha, M.M.; Xiaoli, L.; Dudley, E.G. Whole-genome sequencing reveals resistome of highly drug-resistant retail meat and human Salmonella Dublin. Zoonoses Public Health 2020, 67, 251–262. [Google Scholar] [CrossRef]
- He, T.; Wang, R.; Liu, D.; Walsh, T.R.; Zhang, R.; Yuan, L.; Yuebin, K.; Quanjiang, J.; Ruicheng, W.; Zhihai, L.; et al. Emergence of plasmid-mediated high-level tigecycline resistane in animals and humans. Nat. Microbiol. 2019, 4, 1450–1456. [Google Scholar] [CrossRef]
- Abdelhamed, H.; Ramachandran, R.; Ozdemir, O.; Waldbieser, G.; Lawrence, M.L. Characterization of a novel conjugative plasmid in Edwardsiella piscicida strain MS-18-199. Front. Cell. Infect. Microbiol. 2019, 9, 404. [Google Scholar] [CrossRef]
- Toleman, M.A.; Bennett, P.M.; Walsh, T.R. Common regions e.g., orf513 and antibiotic resistance: IS91-like elements evolving complex class 1 integrons. J. Antimicrob. Chemother. 2006, 58, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Toleman, M.A.; Bennett, P.M.; Walsh, T.R. ISCR elements: Novel gene-capturing systems of the 21st century? Microbiol. Mol. Biol. Rev. 2006, 70, 296–316. [Google Scholar] [CrossRef] [PubMed]
- Toleman, M.A.; Walsh, T.R. ISCR elements are key players in IncA/C plasmid evolution. Antimicrob. Agents Chemother. 2010, 54, 3534. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).