Abstract
The diagnosis of syphilis can be challenging for dermatologists and dermatopathologists. In particular, secondary syphilis can have different clinical and histopathological presentations. A granulomatous tissue response is an unusual finding in secondary syphilis. We report the case of a 77-year-old man who presented with a 4-week history of non-pruritic generalised macules, papules, nodules and plaques. Histopathologically, there was a dense perivascular and periadnexal lympho-histiocytic dermal infiltrate with non-palisading and non-caseifying epithelioid granulomas and abundant plasma cells. The diagnosis of syphilis was confirmed by serology and immunohistochemical detection of Treponema pallidum in the biopsy specimen. A brief overview of the diagnostic role of immunohistochemistry is also provided, with particular emphasis on reported cases of granulomatous secondary syphilis.
1. Introduction
Syphilis is a sexually transmitted disease caused by the Gram-negative microaerophilic spirochete Treponema pallidum, which has been called ‘the great imitator’ due to its protean clinical features. Indeed, it can be mistaken for many other dermatological conditions and remains a diagnostic challenge for dermatologists and dermatopathologists [1,2,3,4]. Correct recognition of the disease and its appropriate treatment in the early stages are essential to prevent serious complications. The painless chancre of primary syphilis is often overlooked by patients. Many of them seek medical attention in the secondary phase of the disease, characterised by a rash that may be associated with non-specific systemic symptoms. The skin lesions of secondary syphilis may have different clinical and histological presentations that are sometimes atypical.
Granulomatous inflammation is an unusual finding in secondary syphilis and may represent a diagnostic pitfall, whereas a granulomatous response is commonly seen in tertiary syphilis [2]. Several hypotheses have been proposed to explain the development of a granulomatous response in secondary syphilis, such as correlation with disease duration and/or involvement of a hypersensitivity reaction to Treponema pallidum [3]. Different granulomatous patterns have been described in secondary syphilis, including poorly defined granulomatous inflammation, sarcoid and palisade configurations, interstitial granulomatous inflammation or tuberculoid granuloma [2,5]. Potential histopathological differential diagnoses in similar pictures include a wide variety of conditions, such as granuloma annulare, interstitial granulomatous dermatitis associated with systemic or drug-induced diseases, sarcoidosis, Borrelia burgdorferi infection, leprosy, leishmaniasis, tuberculosis, atypical mycobacterial infections and deep-seated fungal infections [2,5,6].
We report a case of granulomatous secondary syphilis in an elderly man, diagnosed using serology and immunohistochemistry for the detection of Treponema pallidum in the skin biopsy specimen. The purpose of our manuscript is to emphasise the importance of immunohistochemistry for the diagnosis of syphilis, especially for patients with atypical presentations, even if the diagnostic role of immunohistochemistry in syphilis is probably overlooked in dermatological practice. Indeed, we provide a brief overview of the diagnostic role of immunohistochemical detection of Treponema pallidum in skin samples, focusing on the reported cases of granulomatous secondary syphilis.
2. Case Presentation
A 77-year-old man presented with a 4-week history of a non-pruritic eruption of disseminated skin lesions. He denied the presence of weight loss, fever, malaise or other symptoms. The patient suffered only from arterial hypertension treated with telmisartan for many years.
Prior to referral, routine laboratory test results revealed no relevant abnormalities, and an immunohistopathological analysis of a skin biopsy sample showed a polymorphous cellular infiltrate consisting of T- and B-lymphocytes, in the absence of atypical CD30+ cells, with numerous polyclonal plasma cells and histiocytes and some multinucleated giant cells arranged in scattered granulomas. Treatment with oral prednisone was initially prescribed, but it produced no benefit. Therefore, the patient’s general practitioner and private dermatologist recommended further evaluation at our outpatient clinic.
Physical examination at the time of the visit revealed numerous red-brownish papules with some macular and nodular lesions on his head, neck, trunk and limbs (Figure 1 and Figure 2), and lesions that coalesced to form plaques on the face (Figure 2A) and legs. A few discrete lesions were observed on the palms (Figure 1B) and plantar surfaces, while the genital areas were spared. A minority of lesions had a squamous surface. Painless opaline plaques in the oral cavity (Figure 3) and micropolyadenopathy were also present.
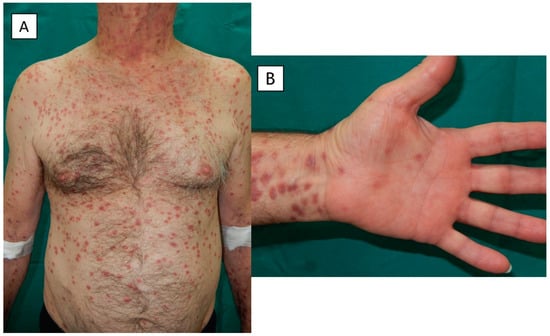
Figure 1.
(A) Numerous brownish red papules with some macular and nodular lesions on the trunk and upper limbs, and (B) a few discrete lesions on the palmar surfaces.
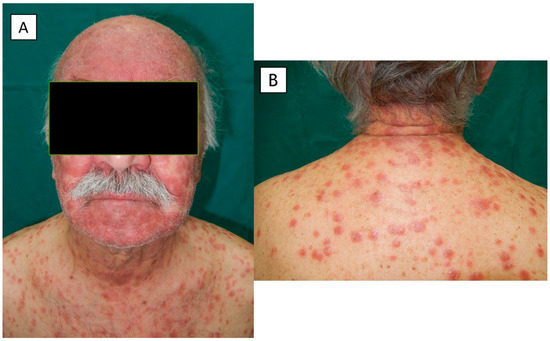
Figure 2.
(A,B) Macules, papules and nodules on the face, neck and trunk.

Figure 3.
Opaline plaques in the oral cavity.
Histopathological examination of a new skin biopsy specimen disclosed a dense perivascular and periadnexal lympho-histiocytic dermal infiltrate, with non-palisading epithelioid granulomas and abundant plasma cells (Figure 4, Figure 5 and Figure 6).
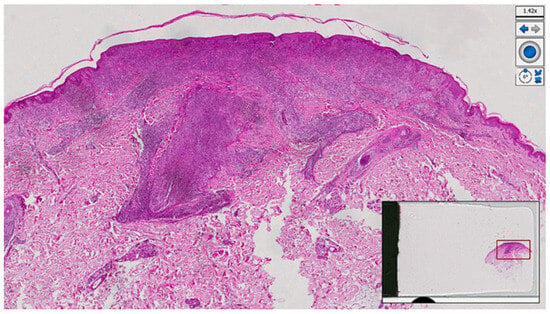
Figure 4.
Histological photomicrograph showing a dense, robust, band-like inflammation underneath the epidermis, and brisk superficial and deep perivascular inflammation (haematoxylin–eosin, original magnification 4×).
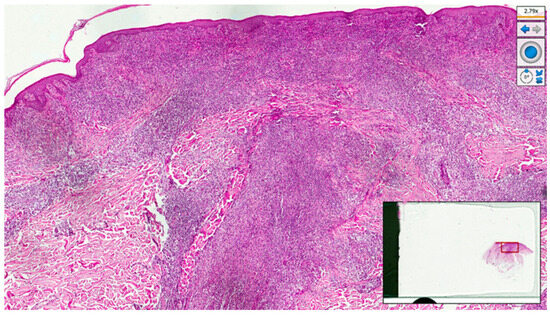
Figure 5.
Periadnexal and perivascular lympho-plasmocytic and histiocytic infiltrate (haematoxylin–eosin, original magnification 10×).
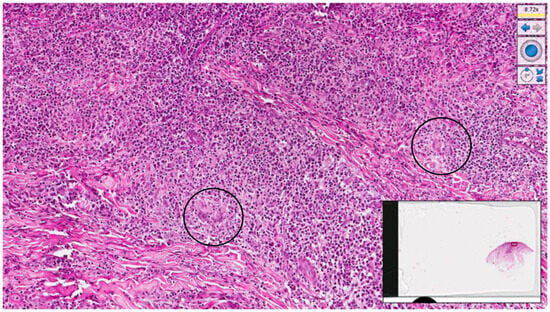
Figure 6.
Histological micrograph showing, at higher magnification, a lympho-plasmocytic and granulomatous infiltrate with some giant cells (black circle) (haematoxylin–eosin, original magnification 20×).
Ziehl–Neelsen and Grocott–Gomori’s methenamine silver stains were negative (not shown).
Additional laboratory investigations included serum angiotensin-converting enzyme, complement and autoantibodies. Antinuclear antibodies were positive at a titre of 1:320, and the other parameters were within the normal range. Moreover, the Venereal Disease Research Laboratory (VDRL) test and Treponema pallidum Haemagglutination Assay (TPHA) were positive, with titres of 1:32 and 1:640, respectively. Serology for hepatitis B and C viruses and human immunodeficiency virus (HIV) was non-reactive. The patient had no personal history of prior syphilis or other sexually transmitted diseases and denied any sexual activity over a long period of time, which remained unspecified despite repeated questions.
Taking into consideration the histopathological and serological findings, we decided to evaluate the presence of spirochetes in the biopsy specimen using immunohistochemistry for Treponema pallidum (primary polyclonal antibodies anti-Treponema pallidum, Biocare Medical, Concord, CA, USA, diluted at 1:400). Occasional spirochetes consistent with the Treponema pallidum species were detected (Figure 7).
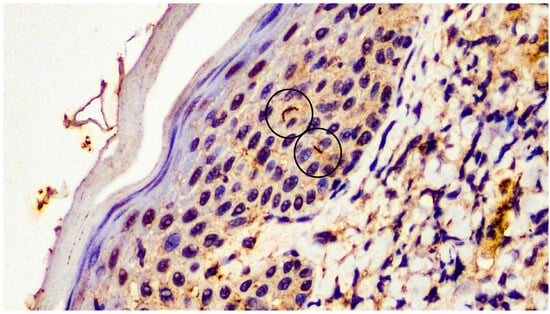
Figure 7.
Immunohistochemical analysis with anti-Treponema pallidum monoclonal antibody: presence of filamentous structures/spirochetes in the epidermis (black circle) (immunohistochemistry for anti-Treponema pallidum, original magnification 20×).
Treatment with 2.4 million units of intramuscular benzathine penicillin once weekly for three weeks caused a progressive improvement in skin lesions that resolved after 2 months with slight dyschromic changes. There was also a complete resolution of oral lesions and lymphadenopathy.
The VDRL titre showed a fourfold decline after 6 months.
3. Discussion
Syphilis has caused immense human suffering throughout history; however, the discovery of penicillin made it easy to treat, and its incidence has decreased dramatically over time. Nevertheless, there has recently been a resurgence in the incidence of syphilis, particularly in association with HIV co-infection [1]. Serologic testing with the combination of treponemal and nontreponemal tests is mandatory for the diagnosis of syphilis. However, the interpretation of such investigations can be difficult and no single test has been shown to have sufficient sensitivity and specificity to recognise all stages of the disease [7]. Furthermore, false-negative serology and delayed seroreactivity have been described in patients co-infected with HIV [8,9]. The direct detection of Treponema pallidum in tissue sections may be useful to confirm the diagnosis, at least in particular circumstances and especially in individuals with atypical presentations and/or equivocal serological test results. It should be noted that numerous spirochetes can be found in skin lesions during primary and early secondary syphilis, whereas spirochetes tend to disappear in later stages of the disease [10]. Several methods have been developed for the detection of Treponema pallidum [7,8].
Silver staining techniques, such as Warthin–Starry staining, are traditional methods used to identify Treponema pallidum in formalin-fixed, paraffin-embedded tissue biopsies, mostly from patients with primary or secondary syphilis, but these methods have low sensitivity and may produce false-positive or false-negative results [7]. Immunohistochemical analysis with primary antibodies against Treponema pallidum is more sensitive than silver staining and is significantly more sensitive and specific than dark-field microscopy on a lesion exudate [7,10,11]. Compared with a clinical diagnosis of secondary syphilis, immunohistochemistry using the avidin–biotin–peroxidase complex method has demonstrated excellent specificity in all studies, with a sensitivity ranging from 49% to 92% [7].
In a study evaluating 40 skin biopsy samples from patients with syphilis (72.5% with secondary syphilis) and 36 skin samples from control subjects with other diseases [12], the Warthin–Starry technique did not accurately identify spirochetes in any sample, giving negative or inconclusive results, whereas immunohistochemistry detected spirochetes only in skin samples from patients with syphilis and was associated with a sensitivity of 60%, a specificity of 100% and an accuracy of 78.9%.
However, some authors emphasised that the interpretation of immunohistochemical results must take clinical data into account and recommended a rigorous search for the typical Treponema pallidum histomorphology due to possible false-positive results with alcohol-resistant bacilli (such as Mycobacterium marinum) and other spirochetes, including Borrelia burgdorferi and Brachyspira [5,13,14].
Data from patients with secondary syphilis have suggested the absence of significant correlations between the detection of spirochetes via immunohistochemistry and serological titres or certain histological features, such as the pattern of inflammation, the degree of infiltrate, the number of plasma cells and the presence of granulomas [11].
In addition, the identification of Treponema pallidum in tissue sections via immunohistochemistry may be useful to clarify the aetiology of a granulomatous dermatitis [5], as in our case.
The literature contains a limited number of reports mentioning the use of immunohistochemical detection of Treponema pallidum in skin samples characterised by granulomatous inflammation to support the diagnosis of syphilis. We performed a literature review of cases of granulomatous secondary syphilis in which the diagnostic work-up included immunohistochemistry for the detection of spirochetes in skin biopsy specimens. Table 1 summarises the main findings observed in these cases [2,3,5,6,15,16,17,18,19,20,21,22,23].

Table 1.
Cases of granulomatous secondary syphilis present in the literature reporting results of immunohistochemistry for Treponema pallidum.
The literature search was performed in the PubMed database using the keywords ‘granuloma’ and ‘syphilis’ or ‘granulomatous syphilis’ and was limited to articles written in English and published until March 2023. In the reported cases of granulomatous secondary syphilis with available immunohistochemical results (Table 1), spirochetes in varying amounts were detected in most cases. In fact, immunohistochemistry did not demonstrate the presence of spirochetes in skin lesions in only one case [6].
As shown in Table 1 and previously described in a review article [2], granulomatous secondary syphilis can have a wide variety of clinical presentations. Papular and/or nodular eruptions have been most commonly observed, although a papular or nodular eruption does not necessarily correspond to a granulomatous histopathological picture. Skin lesions may vary in duration. It has been hypothesised that a granulomatous reaction occurs more frequently in secondary syphilis lesions with a long duration and has indeed been associated with manifestations lasting more than 4 weeks, although a granulomatous histopathological pattern has been documented in cases of shorter duration, even present for only 10 days before diagnosis [2]. As previously pointed out [2], involvement of the palmoplantar surfaces was absent in the majority of reported cases of granulomatous secondary syphilis and involvement of the oral mucosa was rarely described. Instead, our patient had some palmoplantar and oral lesions that contributed to the clinical suspicion of secondary syphilis. Another diagnostic clue for syphilis was the conspicuous infiltration of plasma cells on histopathology [4,24,25]. Despite positive serological test results for syphilis, our patient repeatedly reported a total absence of sexual intercourse for a long period time. We used immunohistochemistry with a polyclonal antibody against Treponema pallidum as an auxiliary diagnostic tool to assess the presence of spirochetes in lesional skin.
Our case confirms that the diagnosis of secondary syphilis must be considered in the context of granulomatous inflammation, especially in the presence of increased plasma cells [2], requiring further confirmatory tests. Serology remains of paramount importance, but immunohistochemistry may be regarded as a useful diagnostic tool, especially in patients with atypical or unclear features. Nevertheless, immunohistochemistry for Treponema pallidum is probably not very commonly used and known in dermatological practice.
In addition, syphilis should be included in the list of differential clinical diagnoses for diffuse eruptions of recent onset [23].
Author Contributions
Conceptualisation, F.A. and G.C.; methodology, F.A. and N.C.; software, G.B.M.; validation, F.A., N.C. and C.F.; formal analysis, M.G.; investigation, F.A. and G.C.; resources, T.L.; data curation, C.C. and V.I.; writing—original draft preparation, F.A.; writing—review and editing, N.C.; visualisation, C.F. and P.R.; supervision, G.A.V. and R.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Ghanem, K.G.; Ram, S.; Rice, P.A. The Modern Epidemic of Syphilis. N. Engl. J. Med. 2020, 382, 845–854. [Google Scholar] [CrossRef] [PubMed]
- Rysgaard, C.; Alexander, E.; Swick, B.L. Nodular secondary syphilis with associated granulomatous inflammation: Case report and literature review. J. Cutan. Pathol. 2014, 41, 370–379. [Google Scholar] [CrossRef]
- Magdaleno-Tapial, J.; Valenzuela-Oñate, C.; Ortiz-Salvador, J.M.; Hernández-Bel, P.; Alegre-De Miquel, V. Treponema Pallidum Epidermotropism in Nodular Secondary Syphilis. Indian J. Dermatol. 2018, 63, 509–511. [Google Scholar] [PubMed]
- Li, F.; Wang, T.; Wang, L. Secondary syphilis primarily presenting with multiple nodules on the scalp: Case report and published work review. J. Dermatol. 2017, 44, 1401–1403. [Google Scholar] [CrossRef]
- Sezer, E.; Luza, B.; Calonje, E. Secondary syphilis with an interstitial granuloma annulare-like histopathologic pattern. J. Cutan. Pathol. 2011, 38, 439–442. [Google Scholar] [CrossRef]
- Jin, A.; McLarney, B.D.; Hsu, S.; Lee, J.B. Granulomatous secondary syphilis: Another diagnostic pitfall for the dermatopathologist. J. Cutan. Pathol. 2023, 50, 209–212. [Google Scholar] [CrossRef] [PubMed]
- Theel, E.S.; Katz, S.S.; Pillay, A. Molecular and Direct Detection Tests for Treponema pallidum Subspecies pallidum: A Review of the Literature, 1964–2017. Clin. Infect. Dis. 2020, 71, S4–S12. [Google Scholar] [CrossRef]
- Buffet, M.; Grange, P.A.; Gerhardt, P.; Carlotti, A.; Calvez, V.; Bianchi, A.; Dupin, N. Diagnosing Treponema pallidum in secondary syphilis by PCR and immunohistochemistry. J. Investig. Dermatol. 2007, 127, 2345–2350. [Google Scholar] [CrossRef]
- Magri, F.; Donà, M.G.; Panetta, C.; Pontone, M.; Pimpinelli, F.; Cameli, N.; Cristaudo, A.; Zaccarelli, M.; Latini, A. Unusual clinical manifestation and challenging serological interpretation of syphilis: Insights from a case report. BMC Infect. Dis. 2021, 21, 521. [Google Scholar] [CrossRef] [PubMed]
- Martín-Ezquerra, G.; Fernandez-Casado, A.; Barco, D.; Jucglà, A.; Juanpere-Rodero, N.; Manresa, J.M.; de Almeida, L.M.; Rodríguez-Peralto, J.L.; Kutzner, H.; Cerroni, L.; et al. Treponema pallidum distribution patterns in mucocutaneous lesions of primary and secondary syphilis: An immunohistochemical and ultrastructural study. Hum. Pathol. 2009, 40, 624–630. [Google Scholar] [CrossRef]
- Hoang, M.P.; High, W.A.; Molberg, K.H. Secondary syphilis: A histologic and immunohistochemical evaluation. J. Cutan. Pathol. 2004, 31, 595–599. [Google Scholar] [CrossRef] [PubMed]
- Rosa, M.F.A.P.; Quintella, L.P.; Ferreira, L.C.; Cuzzi, T. Immunohistochemical detection of Treponema pallidum in skin samples with clinical and histopathological correlations and Warthin-Starry staining critical analysis. An. Bras. Dermatol. 2023, 98, 480–486. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Flores, A. Immunostaining for Treponema pallidum: Caution in its evaluation. Am. J. Dermatopathol. 2010, 32, 523–525. [Google Scholar] [CrossRef] [PubMed]
- Pettit, C.; McMurray, S.; Randall, M.B.; Jones, A.; Fisher, K. Highlighting a Potential Pitfall: Positive Treponema pallidum Immunohistochemical Stain in a Patient Without Syphilis. Am. J. Dermatopathol. 2019, 41, 924–926. [Google Scholar] [CrossRef]
- Glatz, M.; Achermann, Y.; Kerl, K.; Bosshard, P.P.; Cozzio, A. Nodular secondary syphilis in a woman. BMJ Case. Rep. 2013, 2013, bcr-2013-009130. [Google Scholar] [CrossRef]
- Hinojosa, J.A.; Maxim, E.; Garza-Chapa, J.I.; Tovar-Garza, A.; Susa, J. Diffuse Papular Rash in a Young Woman: Challenge. Am. J. Dermatopathol. 2019, 41, 82–83. [Google Scholar] [CrossRef]
- Hinojosa, J.A.; Maxim, E.; Garza-Chapa, J.I.; Tovar-Garza, A.; Susa, J. Diffuse Papular Rash in a Young Woman: Answer. Am. J. Dermatopathol. 2019, 41, 615–616. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.H.; Yang, T.H.; Chang, Y.S.; Chang, I.J. Granulomatous secondary syphilis with a facial annular sarcoidosis-like clinical and histopathological pattern. Australas. J. Dermatol. 2020, 61, e364–e365. [Google Scholar] [CrossRef]
- Phan, K.; Gorji, M.; Smith, S.D.; Harvey, R. Granulomatous secondary syphilis: Uncommon and atypical presentation. Int. J. Dermatol. 2020, 59, 270–272. [Google Scholar] [CrossRef]
- Henebeng, E.; Karasko, E.; Robinson-Bostom, L.; DiMarco, C. Secondary Syphilis With Elastophagocytosis: An Unusual Histologic Finding. Am. J. Dermatopathol. 2021, 43, 225–227. [Google Scholar] [CrossRef]
- Fernández-Camporro, A.; Calzada-González, J.M.; Arcos-González, P.; Rodríguez-Díaz, E. Granulomatous Secondary Syphilis Suggested by Histology: A Case Report. Actas. Dermosifiliogr. 2022, 113, S26–S28. [Google Scholar] [CrossRef] [PubMed]
- Yousefian, F.; Wang, H.; Yadlapati, S.; Cohen, J.A.; Browning, J.C. Granulomatous Secondary Syphilis: An Uncommon Presentation of the Great Imitator. Am. J. Med. 2023, 136, 25–26. [Google Scholar] [CrossRef]
- Saal, R.C.; Borda, L.J.; Pariser, R.J. Grouped follicular secondary syphilis: Case report and review of literature. Australas. J. Dermatol. 2023, 64, e168–e170. [Google Scholar] [CrossRef] [PubMed]
- Flamm, A.; Alcocer, V.M.; Kazlouskaya, V.; Kwon, E.J.; Elston, D. Histopathologic features distinguishing secondary syphilis from its mimickers. J. Am. Acad. Dermatol. 2020, 82, 156–160. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.K.; Li, J. Histologic Features of Secondary Syphilis. Dermatology 2020, 236, 145–150. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).