Human Responses to Different Built Hyperthermal Environments After Short-Term Heat Acclimation
Abstract
1. Introduction
2. Materials and Methods
2.1. Climate Chamber
2.2. Participants
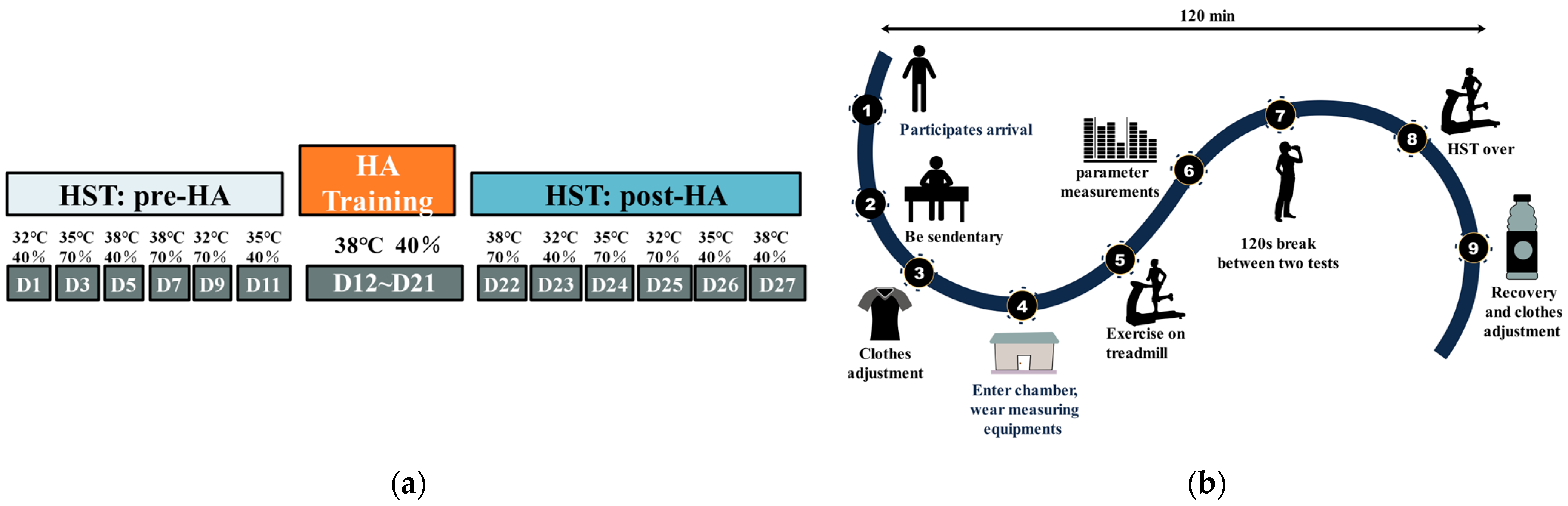
2.3. Experimental Design and Process
2.4. Measurements
2.4.1. Environmental Index
2.4.2. Physiological Index
2.4.3. Subjective Perception
2.5. Statistical Analyses
3. Results
3.1. Environmental Parameters
3.2. Physiological Parameters
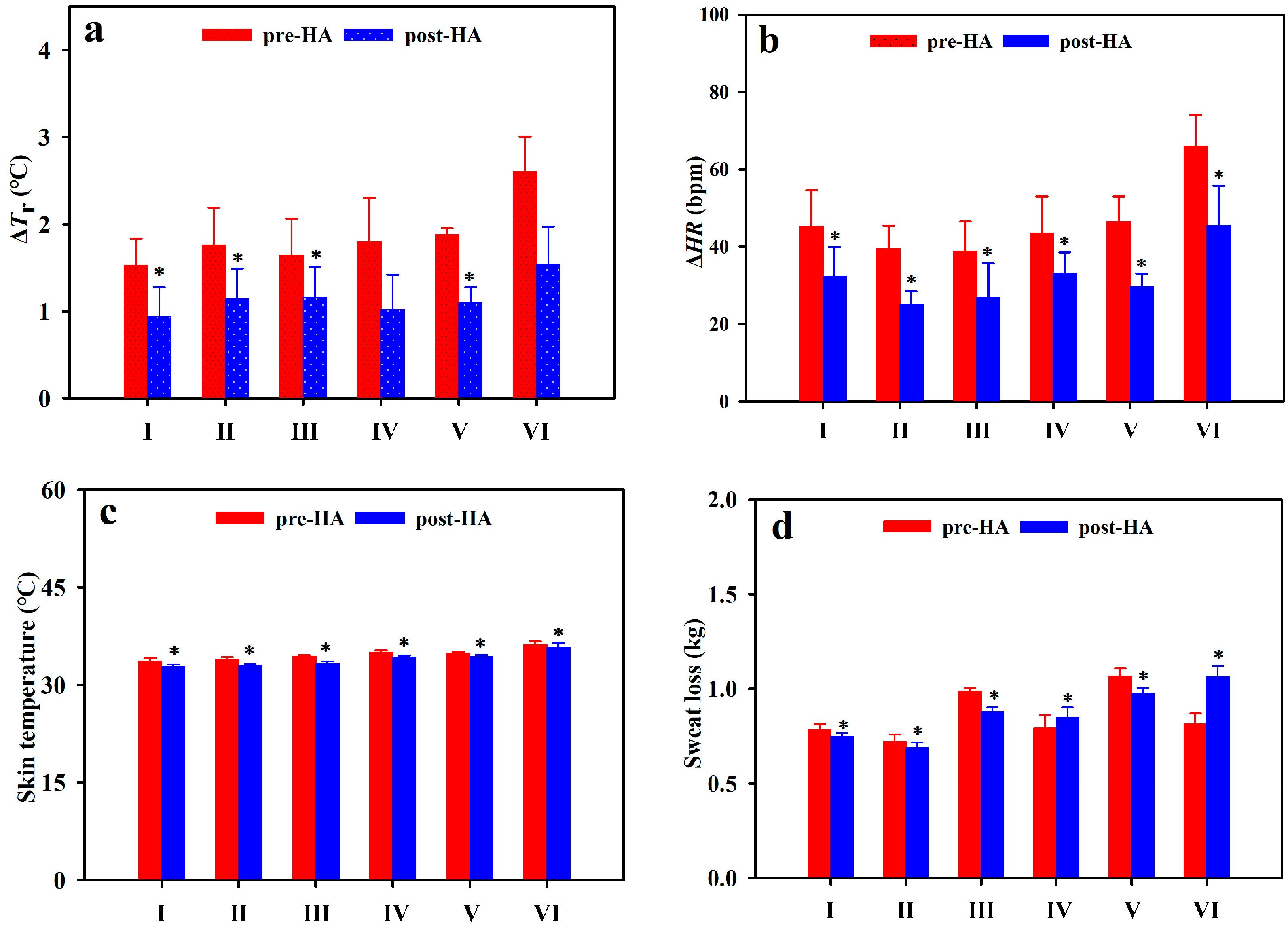
3.2.1. Rectal Temperature
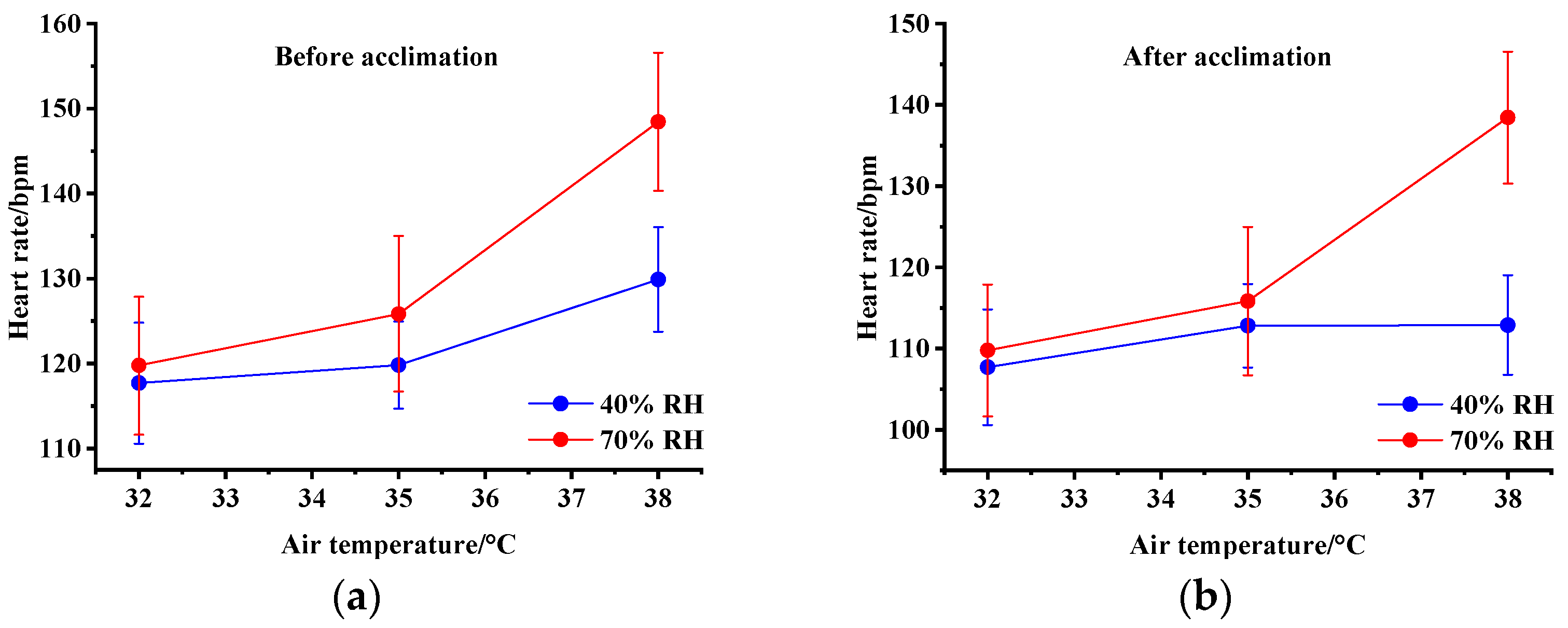
3.2.2. Heart Rate
3.2.3. Skin Temperature
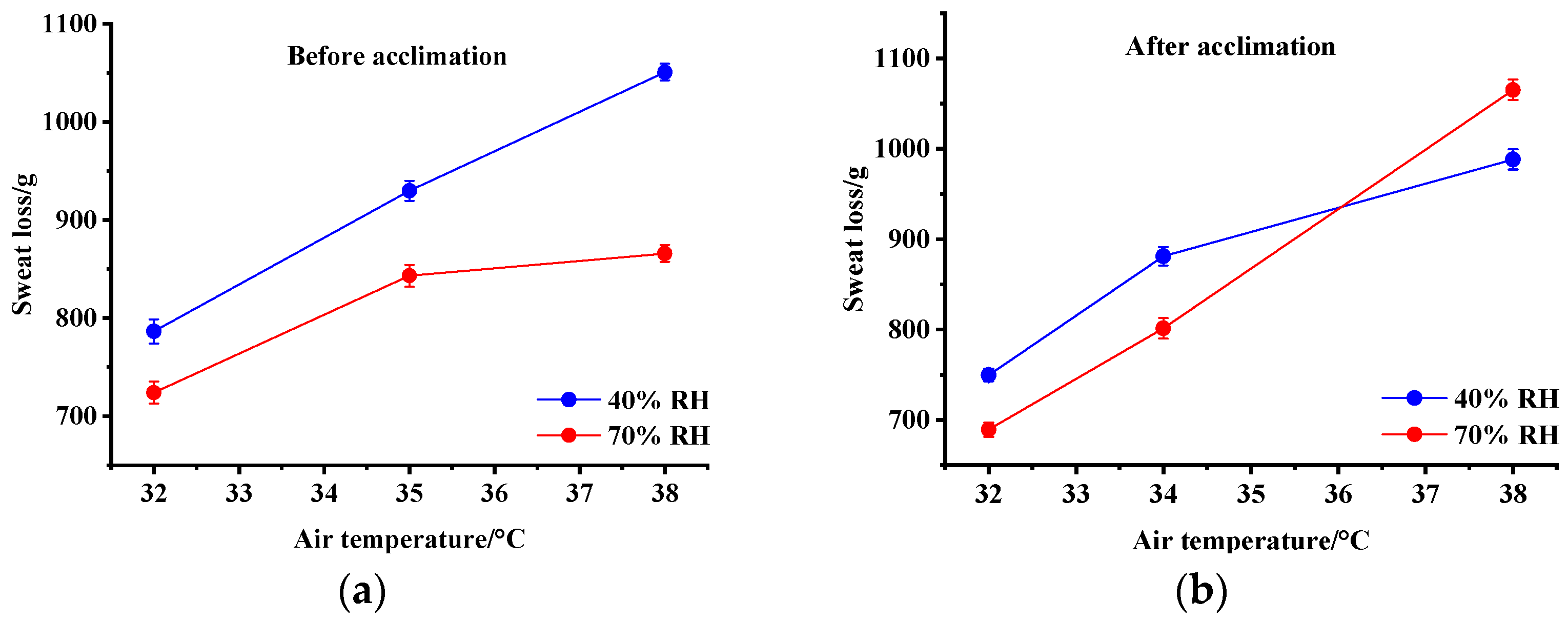
3.2.4. Sweat Loss
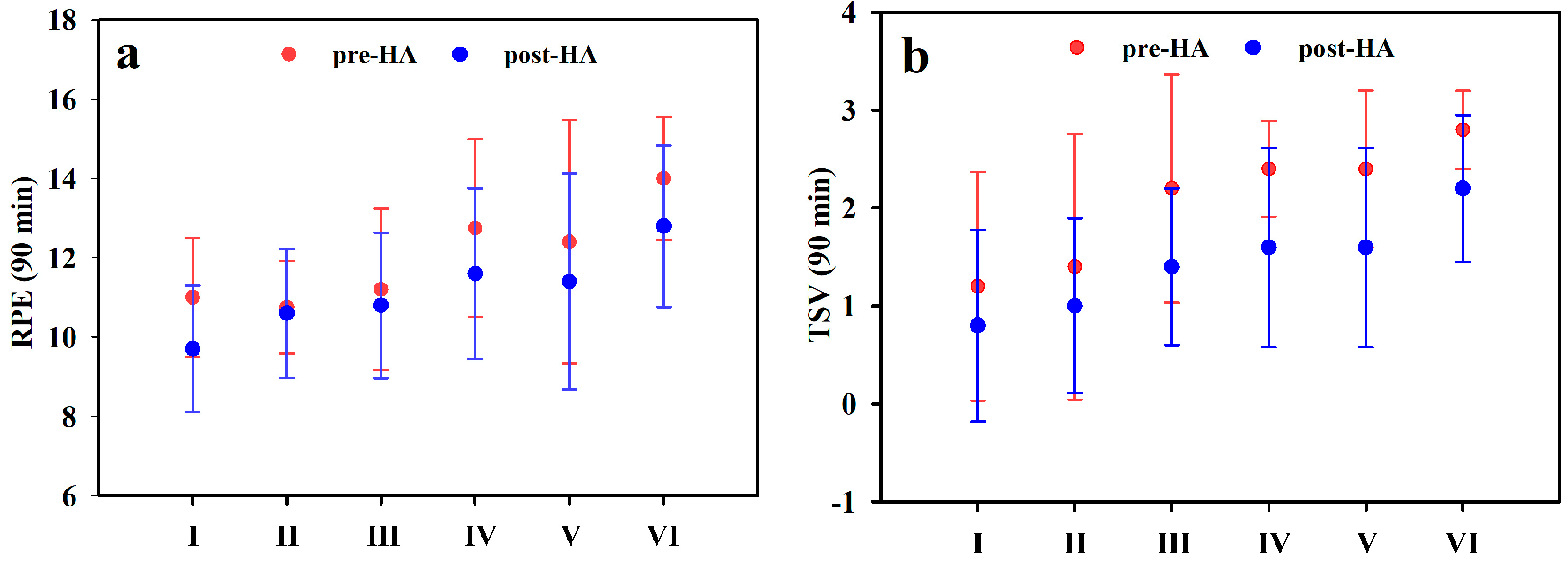
3.3. Psychological Parameters
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Shen, D.; Zhu, N. Influence of the temperature and relative humidity on human heat acclimatization during training in extremely hot environments. Build. Environ. 2015, 94, 1–11. [Google Scholar] [CrossRef]
- Azevedo, R.; Martins, C.; Teixeira, J.C.; Barroso, M. Obstacle clearance while performing manual material handling tasks in construction sites. Saf. Sci. 2014, 62, 205–213. [Google Scholar] [CrossRef]
- Shikdar, A.A.; Sawaqed, N.M. Worker productivity, and occupational health and safety issues in selected industries. Comput. Ind. Eng. 2003, 45, 563–572. [Google Scholar] [CrossRef]
- Zhang, S.; Zhu, N. Exercise heat acclimation causes human responses and safety performance improvements. J. Therm. Biol. 2021, 100, 103042. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.K.; Nio, A.Q.; Fun, D.C.; Teo, Y.S.; Von Chia, E.; Lim, C.L. Effects of heat acclimatisation on work tolerance and thermoregulation in trained tropical natives. J. Therm. Biol. 2012, 37, 366–373. [Google Scholar] [CrossRef]
- Nielsen, B.; Hales, J.R.; Strange, S.; Christensen, N.J.; Warberg, J.; Saltin, B. Human circulatory and thermoregulatory adaptations with heat acclimation and exercise in a hot, dry environment. J. Physiol. 1993, 460, 467–485. [Google Scholar] [CrossRef] [PubMed]
- Nadel, E.R.; Pandolf, K.B.; Roberts, M.F.; Stolwijk, J.A. Mechnisms of thermal acclimation to exercise and heat. J. Appl. Physiol. 1974, 37, 515–520. [Google Scholar] [CrossRef] [PubMed]
- Tyler, C.J.; Reeve, T.; Hodges, G.J.; Cheung, S.S. The Effects of Heat Adaptation on Physiology, Perception and Exercise Performance in the Heat: A Meta-Analysis. Sports Med. 2016, 46, 1699–1724. [Google Scholar] [CrossRef] [PubMed]
- Chong, D.; Zhu, N.; Luo, W.; Zhang, Z. Broadening human thermal comfort range based on short-term heat acclimation. Energy 2019, 176, 418–428. [Google Scholar] [CrossRef]
- Reeve, T.; Gordon, R.; Laursen, P.B.; Lee, J.K.; Tyler, C.J. Impairment of Cycling Capacity in the Heat in Well-Trained Endurance athletes After High-Intensity Short-Term Heat Acclimation. Int. J. Sports Physiol. Perform. 2019, 14, 1058–1065. [Google Scholar] [CrossRef] [PubMed]
- Gibson, O.R.; Mee, J.A.; Tuttle, J.A.; Taylor, L.; Watt, P.W.; Maxwell, N.S. Isothermic and fixed intensity heat acclimation methods induce similar heat adaptation following short and long-term timescales. J. Therm. Biol. 2015, 49, 55–65. [Google Scholar] [CrossRef] [PubMed]
- Liu, F. Intervention Study on Soldiers’ Acclimatization Training in Artificial Humid-Heat Environment. Chin. J. Soc. Med. 2019, 29, 128–130. [Google Scholar]
- Best, S.; Thompson, M.; Caillaud, C.; Holvik, L.; Fatseas, G.; Tammam, A. Exercise-heat acclimation in young and older trained cyclists. J. Sci. Med. Sport/Sports Med. Aust. 2014, 17, 677–682. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Ju, Y.; Min, Z.; Fang, Y.; Meng, J. Transcriptome analysis of grape leaves reveals insights into response to heat acclimation. Sci. Hortic. 2020, 272, 109554. [Google Scholar] [CrossRef]
- Fox, R.H.; Goldsmith, R.; Hampton, I.F.; Hunt, T.J. Heat acclimatization by controlled hyperthermia in hot dry and hot wet climates. J. Appl. Physiol. 1967, 22, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Tian, Z.; Zhu, N.; Zheng, G.; Wei, H. Experimental study on physiological and psychological effects of heat acclimatization in extreme hot environments. Build. Environ. 2011, 46, 2033–2041. [Google Scholar] [CrossRef]
- Swaen, G.M.H.; Van Amelsvoort, L.G.P.M.; Bültmann, U.; Kant, I.J. Fatigue as a risk factor for being injured in an occupational accident: Results from the Maastricht Cohort Study. Occup. Environ. Med. 2003, 60 (Suppl. 1), i88–i92. [Google Scholar] [CrossRef] [PubMed]
- Kondo, Y.; Hifumi, T.; Shimazaki, J.; Oda, Y.; Shiraishi, S.-I.; Hayashida, K. Comparison between the Bouchama and Japanese Association for Acute Medicine Heatstroke Criteria with Regard to the Diagnosis and Prediction of Mortality of Heatstroke Patients: A Multicenter Observational Study. Int. J. Environ. Res. Public Health 2019, 16, 3433. [Google Scholar] [CrossRef] [PubMed]
- Driscoll, T.R.; Cripps, R.; Brotherhood, J.R. Heat-related injuries resulting in hospitalisation in Australian sport. J. Sci. Med. Sport/Sports Med. Aust. 2008, 11, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Brager, G.S.; De Dear, R.J. Thermal adaptation in the built environment: A literature review. Energy Build. 1998, 27, 83–96. [Google Scholar] [CrossRef]
- Lorenzo, S.; Halliwill, J.R.; Sawka, M.N.; Minson, C.T. Heat acclimation improves aerobic performance. J. Appl. Physiol. 2010, 109, 1140–1147. [Google Scholar] [CrossRef] [PubMed]
- Poirier, M.P.; Gagnon, D.; Friesen, B.J.; Hardcastle, S.G.; Kenny, G.P. Whole-Body Heat Exchange during Heat Acclimation and Its Decay. Med. Sci. Sports Exerc. 2014, 47, 390–400. [Google Scholar] [CrossRef] [PubMed]
- Guy, J.H.; Pyne, D.B.; Deakin, G.B.; Miller, C.M.; Edwards, A.M. Acclimation Training Improves Endurance Cycling Performance in the Heat without Inducing Endotoxemia. Front. Physiol. 2016, 7, 318. [Google Scholar] [CrossRef] [PubMed]
- Scoon, G.S.; Hopkins, W.G.; Mayhew, S.; Cotter, J.D. Effect of post-exercise sauna bathing on the endurance performance of competitive male runners. J. Sci. Med. Sport/Sports Med. Aust. 2007, 10, 259–262. [Google Scholar] [CrossRef] [PubMed]
- Zurawlew, M.J.; Mee, J.A.; Walsh, N.P. Post-exercise Hot Water Immersion Elicits Heat Acclimation Adaptations That Are Retained for at Least Two Weeks. Front. Physiol. 2019, 10, 1080. [Google Scholar] [CrossRef] [PubMed]
- Chalmers, S.; Esterman, A.; Eston, R.; Bowering, K.J.; Norton, K. Short-Term Heat Acclimation Training Improves Physical Performance: A Systematic Review, and Exploration of Physiological Adaptations and Application for Team Sports. Sports Med. 2014, 44, 971–988. [Google Scholar] [CrossRef] [PubMed]
- Stone, B.L.; Ashley, J.D.; Skinner, R.M.; Polanco, J.P.; Walters, M.T.; Schilling, B.K.; Kellawan, J.M. Effects of a Short-Term Heat Acclimation Protocol in Elite Amateur Boxers. J. Strength Cond. Res. 2022; Ahead of Print. [Google Scholar] [CrossRef] [PubMed]
- Pryor, J.L.; Pryor, R.R.; Vandermark, L.W.; Adams, E.L.; VanScoy, R.M.; Casa, D.J.; Armstrong, L.E.; Lee, E.C.; DiStefano, L.J.; Anderson, J.M.; et al. Intermittent exercise-heat exposures and intense physical activity sustain heat acclimation adaptations. J. Sci. Med. Sport 2018, 22, 117–122. [Google Scholar] [CrossRef] [PubMed]
- Lan, L.; Lian, Z. Application of statistical power analysis—How to determine the right sample size in human health, comfort and productivity research. Build. Environ. 2010, 45, 1202–1213. [Google Scholar] [CrossRef]
- ISO: 28802; Ergonomics of the Physical Environment-Assessment of Environments by Means of an Environmental Survey Involving Physical Measurements of the Environment and Subjective Responses of People. International Organization for Standard: Geneva, Switzerland, 2012.
- ASHRAE. ANSI/ASHRAE Standard 55: Thermal Environmental Conditions for Human Occupancy; American Society of Heating, Refrigerating and Air-Conditioning Engineers: Atlanta, GA, USA, 2023. [Google Scholar]
- Miller, K.C.; Hughes, L.E.; Long, B.C.; Adams, W.M.; Casa, D.J. Validity of Core Temperature Measurements at 3 Rectal Depths During Rest, Exercise, Cold-Water Immersion, and Recovery. J. Athl. Train. 2017, 52, 332–338. [Google Scholar] [CrossRef] [PubMed]
- ISO: 9886; Evaluation of Thermal Strain by Physioligical Measurements. International Organization for Standardization: Geneva, Switzerland, 2004.
- Carlton, A.; Orr, R.M. The effects of fluid loss on physical performance: A critical review. J. Sport Health Sci. 2015, 4, 357–363. [Google Scholar] [CrossRef][Green Version]
- Milanez, V.F.; Lima, M.S.; Gobatto, C.A.; Perandini, L.A.; Nakamura, F.Y.; Ribeiro, L.F.P. Correlates of session-rate of perceived exertion (RPE) in a karate training session. Sci. Sports 2011, 26, 38–43. [Google Scholar] [CrossRef]
- Mclntyre, D.A. Indoor Climate; Applied Science Published LTD: London, UK, 1980. [Google Scholar]
- Taylor, N.A. Human Heat Adaptation. Compr. Physiol. 2014, 4, 325–365. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Quintero, M.; Siquier-Coll, J.; Bartolomé, I.; Robles-Gil, M.C.; Muñoz, D.; Maynar-Mariño, M. Three weeks of passive and intervallic heat at high temperatures (100 ± 2 °C) in a sauna improve acclimation to external heat (42 ± 2 °C) in untrained males. J. Therm. Biol. 2021, 96, 102837. [Google Scholar] [CrossRef] [PubMed]
- Garrett, A.T.; Creasy, R.; Rehrer, N.J.; Patterson, M.J.; Cotter, J.D. Effectiveness of short-term heat acclimation for highly trained athletes. Eur. J. Appl. Physiol. 2011, 112, 1827–1837. [Google Scholar] [CrossRef] [PubMed]
- Wagner, J.A.; Robinson, S.; Tzankoff, S.P.; Marino, R.P. Heat tolerance and acclimation to work in the heat in relation to age. J. Appl. Physiol. 1972, 33, 616–622. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, B. Heat Acclimation—Mechanisms of Adaption to Exercise in the Heat. Int. J. Sports Med. 1998, 19 (Suppl. 2), S154–S156. [Google Scholar] [CrossRef] [PubMed]
- Costello, J.T.; Stewart, K.L.; Stewart, I.B. The Effects of Metabolic Work Rate and Ambient Environment on Physiological Tolerance Times While Wearing Explosive and Chemical Personal Protective Equipment. J. Biomed. Biotechnol. 2015, 2015, 857536. [Google Scholar] [CrossRef] [PubMed]
- Alhadad, S.B.; Low, I.C.; Lee, J.K. Thermoregulatory responses to ice slurry ingestion during low and moderate intensity exercises with restrictive heat loss. J. Sci. Med. Sport 2020, 24, 105–109. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.K.; Shirreffs, S.M.; Maughan, R.J. Cold Drink Ingestion Improves Exercise Endurance Capacity in the Heat. Med. Sci. Sports Exerc. 2008, 40, 1637–1644. [Google Scholar] [CrossRef] [PubMed]



| Parameters | Instruments | Range | Accuracy |
|---|---|---|---|
| Air temperature and relative humidity | High-precision temperature and humidity recorder (MX1102A, HOBO, Onset, Beijing, China) | 0−50 °C, 1–90%, | ±0.2 °C, ±2% |
| Air velocity | Hot-wire anemometer (Testo, 425, Titisee-Neustadt, Germany) | 0–50 m/s | ±0.03 m/s |
| Black-bulb temperature | WBGT-2006 (Huiyi, Beijing, China) | −10–100 °C | ±0.5 °C |
| Conditions | Designed | Actual | ||||
|---|---|---|---|---|---|---|
| Temperature/°C | Relative Humidity/% | Temperature/°C | Relative Humidity/% | Air Velocity | ET* | |
| I | 32 | 40 | 31.9 ± 0.1 | 39.7 ± 1.8 | <0.1 m/s | 25.82 |
| II | 70 | 32.2 ± 0.1 | 70.3 ± 1.9 | 28.54 | ||
| III | 35 | 40 | 35.1 ± 0.1 | 40.2 ± 2.2 | 27.96 | |
| IV | 70 | 34.8 ± 0.2 | 70.4 ± 2.1 | 31.17 | ||
| V | 38 | 40 | 38.2 ± 0.1 | 40.3 ± 1.3 | 30.20 | |
| VI | 70 | 38.1 ± 0.2 | 69.8 ± 2.1 | 33.97 | ||
| HA training | 38 | 40 | 37.9 ± 0.1 | 39.8 ± 2.3 | 30.20 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, S.; Wang, Q.; Zhou, H.; Wang, T.; Jia, G. Human Responses to Different Built Hyperthermal Environments After Short-Term Heat Acclimation. Buildings 2025, 15, 2581. https://doi.org/10.3390/buildings15142581
Zhang S, Wang Q, Zhou H, Wang T, Jia G. Human Responses to Different Built Hyperthermal Environments After Short-Term Heat Acclimation. Buildings. 2025; 15(14):2581. https://doi.org/10.3390/buildings15142581
Chicago/Turabian StyleZhang, Shuai, Qingqin Wang, Haizhu Zhou, Tianyang Wang, and Guanguan Jia. 2025. "Human Responses to Different Built Hyperthermal Environments After Short-Term Heat Acclimation" Buildings 15, no. 14: 2581. https://doi.org/10.3390/buildings15142581
APA StyleZhang, S., Wang, Q., Zhou, H., Wang, T., & Jia, G. (2025). Human Responses to Different Built Hyperthermal Environments After Short-Term Heat Acclimation. Buildings, 15(14), 2581. https://doi.org/10.3390/buildings15142581






