Abstract
Background: Osteoarthritis of the hand and wrist is common and can have a significant impact on quality of life. Since the carpus consists of multiple bony structures, osteoarthritis can exist in many forms. Arthroplasty using implants has become the standard treatment for many larger joints. In carpal arthroplasty, many implants exist. To determine the most suitable implant in each individual patient, knowledge of the possibilities is important. This article aims to provide an overview of the more commonly used implants in carpal arthroplasty. Methods: This narrative review describes all types of carpal implants, namely, total wrist implants, first carpometacarpal implants, the Amandys® implant, the Pyrocardan® disc, pyrocarbon capitate resurfacing implants, the adaptive proximal scaphoid implant, and total carpal replacement. A literature search was conducted separately for each implant. All studies investigating implant performance were included. Results: Naturally, each implant showed different results. Implant arthroplasty is most often compared to either arthrodesis or resection arthroplasties. For joint replacing implants like total wrist implants or first carpometacarpal implants, the use of joint replacing implants seems to be beneficial in certain populations. Joint resurfacing implants show similar functional results to the comparable non-implant options. However, research on these implants is less prevalent. Regarding all implants, complication rates seemed either similar to or in favor of non-implant options. Almost no studies found a lower complication rate for implant usage. Conclusions: Carpal implants are a valid option in carpal osteoarthritis. Implants seem to perform comparably to non-implant options. Careful patient selection is required, especially since implants may carry a higher risk of complications.
1. Introduction
Joint osteoarthritis is a widespread healthcare problem. It is estimated that 13% of the global population is affected by osteoarthritis. In the population aged greater than 65 years, this number increases to 80–90% []. Much variance exists in the reported incidence of hand and wrist osteoarthritis. However, the most recent global burden of disease study shows an increase in hand and wrist osteoarthritis over the last decades [,]. Trapeziometacarpal arthritis, scaphotrapeziotrapezoid (STT) arthritis, proximal carpal row arthritis, and radioscapholunate (RSL) arthritis are some of the more common types of carpal osteoarthritis [,,]. Moreover, traumatic injuries of the carpal bones may lead to complex biomechanical changes in the carpal region like scapholunate advanced collapse (SLAC) or scaphoid nonunion advanced collapse (SNAC) [,].
Since the cause of symptoms in osteoarthritis is the degeneration of cartilage in the joint space causing bony contact, surgical treatment is often indicated. Most often, surgical treatment of carpal arthritis involves resecting a carpal bone either fully or partly. The aim is to relieve the pain caused by bony contact. However, after resection arthroplasty, the biomechanics of the joint are altered. Implant arthroplasty also aims to relieve complaints by eliminating the painful bony contact, in this case, by restoring anatomical function of the joint using implants. Treatment of osteoarthritis using implants is already established in the current medical landscape []. While carpal arthroplasty is used widely in orthopedic surgeries [], it is still emerging in the field of hand surgery [,].
Since the hand comprises multiple carpal bones, forming even more joint surfaces, the hand is susceptible to different forms of osteoarthritis. Therefore, a ‘one size fits all’ implant does not exist, and each patient should be carefully assessed to determine the best-fitting implant. Carpal arthroplasty involves a lot of different surgical modalities. Some are being utilized more often like arthroplasty of the trapeziometacarpal joint or total wrist arthroplasty []. However, some procedures are still only used selectively like total scaphoid arthroplasty or lunate arthroplasty [,]. Since data on very specific arthroplasty procedures may be available in limited quantities, the spectrum of the possibilities in carpal arthroplasty remains somewhat unclear. This narrative review aims to provide a comprehensive overview of the most common carpal arthroplasties based on the most recent literature.
2. Methods
This study is a narrative review including all types of carpal implants. To investigate the current state of research, a literature search was performed. After identification of the implants based on the literature and the authors’ experience, PubMed was searched to find all papers that describe the respective implants. The exact search prompts can be found in the Supplementary Materials. We included all studies concerning the applicable implant and primarily investigating the implant performance. Case series were included, and case reports were excluded for volume reasons. However, in the case of total scaphoid or lunate arthroplasty, we did include case reports due to a lack of other studies. For each separate search, the results were screened manually on title and abstract by the first author. The results of the search are described separately in each section. In addition, dedicated medical figures were created for each type of implant.
The implants were split into two groups, the first being joint replacing implants; these implants eliminate both the original joint surfaces after which the implant itself includes a component of articulation. The second group is joint resurfacing implants in which only one joint surface is either replaced or resurfaced.
3. Results
3.1. Joint Replacing Implants
3.1.1. Total Wrist Arthroplasty
Arthroplasty in which the entire wrist joint is replaced is one of the more routinely performed procedures in orthopedic surgery. For example, in the Netherlands, according to the Dutch arthroplasty registry, 235 total wrist arthroplasties were performed between 2017 and 2023 []. However, this is most likely under-reported, since registration completeness in the Dutch arthroplasty registry is not complete for hand and wrist implants []. Total wrist arthroplasty (TWA) was introduced in 1890 with the use of ivory implants. However, it was not until the 1960s and 1970s that wrist implants gained traction alongside the rise in hip arthroplasties []. First-generation implants were silicone implants. The second generation involved more metal-on-polyethylene articulation, while the third generation added anatomical orientations. The fourth generation added more modularity and relied less on cement [].
- Indication
The most common indication for TWA is rheumatoid arthritis. This group of patients represents 51–71% of all patients receiving TWAs [,,]. The second most common indication remains general osteoarthritis or post-traumatic osteoarthritis. This group most commonly consists of a younger, more active population []. Since TWA is a total arthroplasty, the state of the cartilage is not relevant to the indication.
- Evidence base
The search prompt described in appendix 1 produced 1896 results, of which 90 studies reported on the functional outcome of total wrist arthroplasty [,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,]. The earliest study was conducted in 1979 []. The 1980s and 1990s mainly comprised research on silicone arthroplasty. Recently, research has been focusing on fourth-generation implants. Multiple systematic reviews have been conducted [,,,].
- Technique
Multiple implants are currently on the market for TWA. However, they generally follow the same concepts. For the fourth generation of implants, two concepts are the most obvious. Proximal row carpectomy is always necessary to create space for the implant. One concept is the ellipsoid-shaped implant trying to mimic the original anatomical function of the joint more closely [,]. Some examples of this concept include the ReMotion® (Stryker Corporation, Kalamazoo, MI, USA) or the Freedom ® (Smith & Nephew, London, UK) implants in which the carpal plate is fixed to multiple carpal bones on the distal row (see Figure 1) [,]. Another possible concept is a ball-and-socket design found in the Motec® (Swemac Innovation AB, Linköping, Sweden) implant. This concept relies on a single screw through the capitate and into the third metacarpal fixing the carpal component, which is connected to the radial component through a ball-and-socket linkage (see Figure 2) []. Depending on the different implants, materials usually include titanium, alloys, and polyethylene.
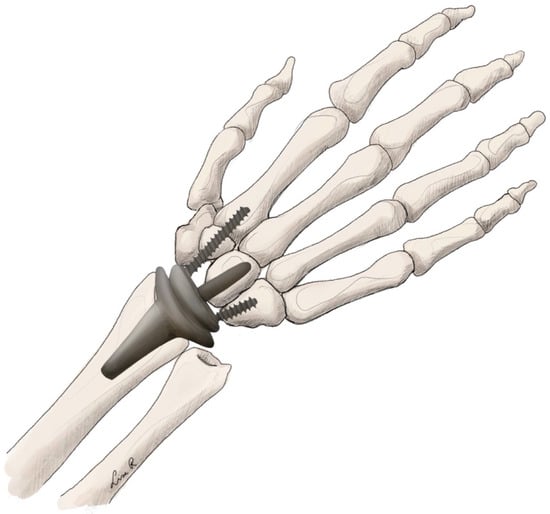
Figure 1.
Total wrist arthroplasty with ellipsoid implant.
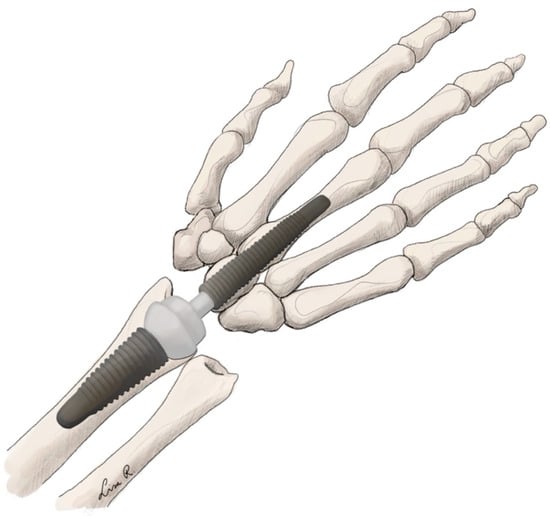
Figure 2.
Total wrist arthroplasty with ball-and-socket implant.
- Clinical findings
Currently, the fourth-generation implants are the most recent renditions used in TWA. Significant improvement over their predecessors has been shown in several studies [,,,]. The alternative treatment for wrist arthritis is arthrodesis of the wrist, eliminating motion in the wrist joint. Various studies have compared TWA to arthrodesis of the wrist joint. Most found no difference in general functional outcome between the two [,,,,,]. However, in a systematic review from 2018, wrist arthrodesis patients did seem to have a greater difficulty with specific tasks like personal hygiene []. Nevertheless, TWA was associated with high complication and reoperation rates [,,,,,,]. The most common complications of TWA are loosening of the carpal component, metacarpal cutout, and instability []. Still, the clinical impact of loosening on the patient satisfaction was not apparent []. TWA is usually performed on young and demanding populations, which may influence the stress on the implant and thereby its longevity.
3.1.2. Trapeziometacarpal Arthroplasty
The trapeziometacarpal joint is one of the most affected joints in carpal osteoarthritis [,]. For the treatment of trapeziometacarpal arthritis, resection arthroplasty, most often a trapeziectomy, is considered standard in most practices around the world. This could be combined with several types of ligamentous reconstructions to fill the remaining cavity and, in some cases, suspend the first metacarpal. Arthroplasty of the trapeziometacarpal joint was introduced in 1972 by Swanson [], originally using a silicone implant.
- Indication
The most common indication for trapeziometacarpal arthroplasty is osteoarthritis of the first carpometacarpal joint []. The typical patients are post-menopausal women who have been working with their hands their whole life. However, indications differ between countries. In the Netherlands, for example, arthroplasty of the trapeziometacarpal joint is only recommended in the experimental setting [], although a shift towards arthroplasty with an implant as a standard treatment has been seen in the last years.
- Evidence base
In our literature search, we identified 777 results of which 75 studies met the inclusion criteria [,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,]. Ball-and-socket implants for the trapeziometacarpal joint have been around since the 1970s. Since then, lots of case series have been published. Research into these implants has spiked since the last decade, with multiple randomized controlled trials (RCTs) and systematic reviews being published.
- Technique
Originally the anatomical saddle-like shape of the trapeziometacarpal joint was recreated in the early implants. However, due to complications, this was replaced by a ball-and-socket design [,]. These implants consist of a socket, which is placed in the trapezium, and an intramedullary component of the ball to attach it into the first metacarpal. Recently, the concept of dual mobility has been introduced []. This consists of a separate socket that can move to some degree inside the outer socket. In theory this may lead to lower complication rates, especially dislocation []. The most recent rendition is the TOUCH® (KeriMedical, Montpellier, France) implant [,,,] (see Figure 3). These implants are made from polyethylene and stainless steel, with full-titanium options available [].
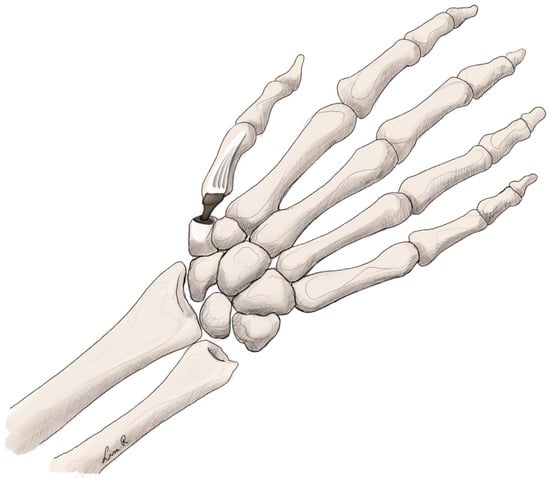
Figure 3.
Trapeziometacarpal arthroplasty using a ball-and-socket implant.
- Clinical Findings
Arthroplasty versus trapeziectomy still remains a debatable subject. Larger studies are starting to be published comparing these treatments. In some studies, arthroplasty seemed to be superior regarding strength and range of motion and other functional outcomes [,,,,,,,,,]. A recent systematic review has shown similar results with short-term benefits in recovery time associated with trapeziectomy []. When compared with arthrodesis, pinch precision seems to be better in joint replacement, while pinch strength is higher in arthrodesis []. Complication rates comparing trapeziectomy to arthroplasty are debatable. No significant differences were found in several studies [,,,,]. However, other studies did report higher complication rates in joint replacement [,,,,,,,,]. The most common complications seem to be tendinopathy, dislocation, implant loosening, and infection [,].
3.2. Joint Resurfacing Implants
3.2.1. Amandys® Interposition Spacer
In cases of severe wrist destruction due to degenerative conditions, treatment options are often limited. The most applied procedures are total wrist arthroplasty and total wrist arthrodesis [,]. These procedures are relatively intensive and rely on fixation to the bone. The Amandys® (Tornier SAS-Bioprofile Grenoble, Montbonnot-Saint-Martin, France) implant was introduced as a novel pyrocarbon interposition implant in 2012 [].
- Indication
The Amandys® implant is implanted in the radiocarpal and midcarpal space, making it suitable for the treatment of arthritis in the proximal area of the wrist joint like radiocarpal or midcarpal arthritis. To lower the risk of luxation, there should be no malalignment of the wrist, and the joint capsule and interosseus ligaments should ideally be completely intact []. However, despite the known injury of soft tissue in patients with rheumatoid arthritis, the implant has shown good results in the treatment of rheumatoid wrists. Although sometimes capsular reinforcement may be needed [], the indications do overlap with those of TWA.
- Evidence base
The search resulted in 11 studies. After screening, ten studies remained [,,,,,,,,,]. Since introduction in 2012, mainly case reports have been published, with one comparative study being published recently [].
- Technique
The implant is shaped elliptically in two planes and replaces the lunate and the proximal part of the scaphoid. Contrary to TWA, the implant does not require bony fixation but rather is a free-floating implant in the joint space. This eliminates component loosening as a possible complication []. Furthermore, it theoretically provides more-dynamic motion. The implant is manufactured entirely out of pyrocarbon, like most carpal implants currently (see Figure 4).
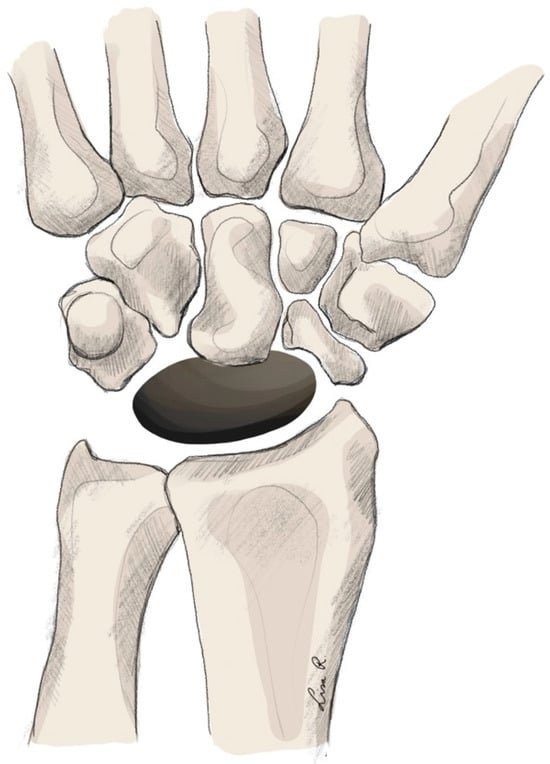
Figure 4.
Amandys® implant arthroplasty.
- Clinical findings
The first description of the implant described preliminary results with improved pain reduction and functionality. However, range of motion was not improved significantly []. More recent studies have also shown satisfactory results [,,,,]. However, a relatively high incidence of revision surgery has also been reported []. Some studies note the importance of capsular stability to prevent implant dislocation, which is the most common complication [,]. The only comparative study was retrospective and compared the Amandys implant with four-corner arthrodesis. The Amandys® implant was deemed to be non-inferior and associated with shorter immobilization periods [].
3.2.2. Adaptive Proximal Scaphoid Implant (APSI)
The scaphoid is commonly affected in the case of carpal osteoarthritis. Therefore, multiple implants target this bone. The adaptive proximal scaphoid implant was introduced in France in 2000 []. It is a relatively new implant. However, longer-term results are starting to be published currently [].
- Indication
Originally, the implant was specifically designed to treat styloscaphoid arthritis and prevent deterioration of existing nonunion or scapholunate dissociation into advanced collapsed states []. Usually, APSI treatment is used before advanced collapse, for example, in cases with nonunion of the scaphoid pole. However, it also provides alternative treatment for wrists already affected by SNAC or SLAC []. It is important to ensure that the cartilage of the scaphoid fossa and the capitolunate joint are intact [].
- Evidence base
The literature search yielded 27 results, of which seven studies were included in this overview [,,,,,,]. These studies all consisted of case series except for one systematic review. No prospective randomized controlled trials were described for this type of arthroplasty.
- Technique
The implant, like almost all interpositional carpal implants, is produced from pyrocarbon. This ensures good compatibility with the cartilage. The implant, as the name suggests, replaces the proximal pole of the scaphoid and articulates with the scaphoid fossa of the radius [] (see Figure 5).
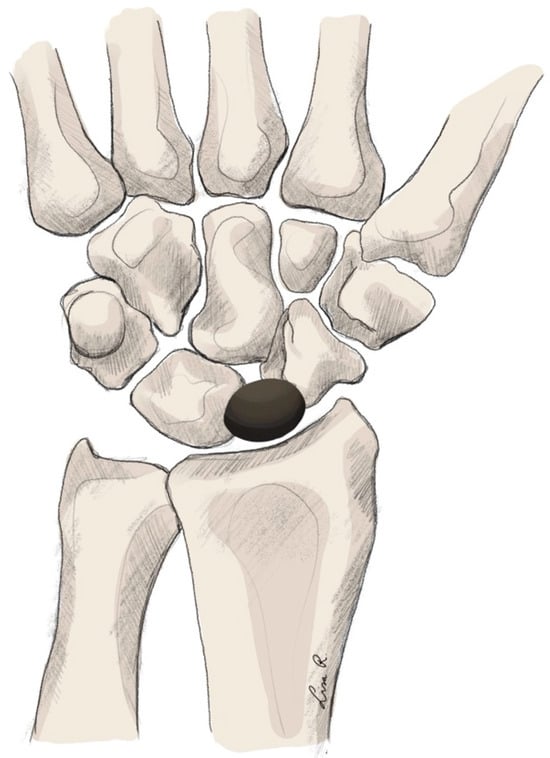
Figure 5.
Carpal arthroplasty using the APSI implant.
- Clinical findings
The only systematic review did show APSI to have comparable results to other surgical modalities like four-corner arthrodesis or total wrist arthrodesis []. A possible advantage being that it does not disable future salvage procedures. It is however more expensive than traditional arthrodesis []. Other studies show good functional results of the APSI arthroplasty [,,,,,]. Complication rates seem to be similar to those for other surgical modalities [,,,].
3.2.3. Total Carpal Replacement
In the early 1960s, silicone implants for the replacement of the scaphoid were introduced []. Biomechanically these implants performed very well. However, the silicone caused inflammation of the synovium, and the particles caused destruction in the wrist. Therefore, the titanium implant was introduced in the late 1980s []. Total lunate replacement had a similar development in the treatment of Kienbock’s disease.
- Indication
When scaphoid fractures occur, nonunion of the fracture is a notorious complication, since its management can be challenging. When severe arthritis or biomechanical complications like SNAC occur, more drastic surgical treatment is indicated. However, when scaphoid nonunion presents before instability or collapse, total scaphoid arthroplasty may be indicated [,].
Total replacement of the lunate can be considered in advanced Kienbock’s disease. However this indication does overlap with the indication for PRC, which is a more commonly performed technique [].
- Evidence base
The literature search provided 278 results, which were screened, after which nine studies provided information on total carpal replacement [,,,,,,,,]. Randomized controlled trials did not exist.
- Technique
In both scaphoid and lunate replacement arthroplasty, the entire carpal bone is resected and replaced by an implant. The physical properties of this implant may change. As described, early implants were made of silicone. However, due to complication rates, these are not used currently. The most used material seems to be titanium and pyrocarbon [,]. Ready-made implants are available for the lunate (see Figure 6). For the scaphoid, to provide patient-specific implants, 3D-printed titanium implants are used.
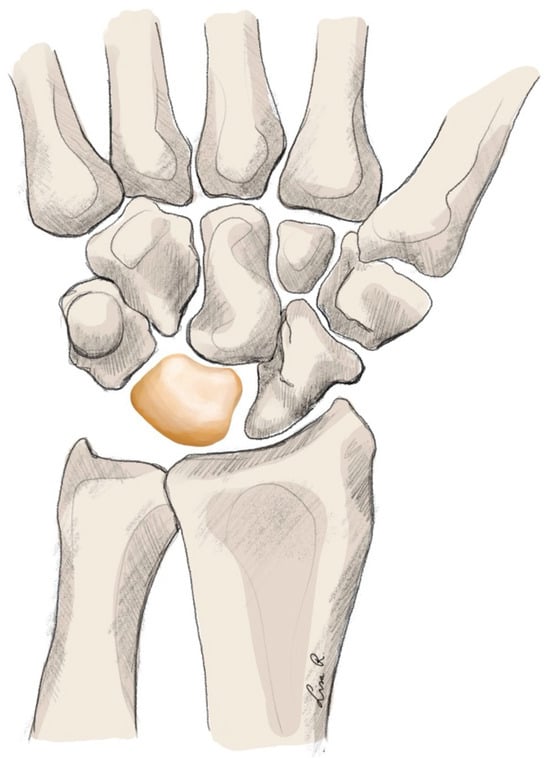
Figure 6.
Total carpal replacement arthroplasty.
- Clinical findings
Scaphoid replacement is not very well described in the current literature. Good functional outcomes are reported []. More recently, with 3D-printed scaphoids being available, implants have been showing promising functional outcomes [,]. No long-term results are available.
Lunate replacement arthroplasty with patient-specific implants is still in development. Ready-made implants do seem to have good results after follow-up [,]. The long-term results of these modern techniques remain uncertain. We do know that older techniques like silicone implants yielded unsatisfactory results with high complication rates upwards of 75% [,].
3.2.4. Pyrocarbon Capitate Resurfacing Implant (PCRI)
In cases of SLAC or SNAC in the wrist, management can be difficult. Traditionally treatment involved either four-corner arthrodesis or proximal row carpectomy (PRC). In PRC, the entire proximal row of the carpal bones is resected. This may be indicated in high-demand patients with arthritis sparing the lunate fossa, the distal radius, and the proximal pole of the capitate, since these surfaces will form the new wrist joint [].
- Indication
Treatment using PCRI may be indicated when the proximal pole of the capitate is affected. Since a PRC in patients with an affected proximal capitate will create a new joint in which osteoarthritis is already present, resurfacing the proximal capitate may provide better results after PRC []. Moreover, treatment with or without resurfacing implants is also based on the surgeon’s preference []. These procedures may also be indicated in severe Kienbock’s disease [,].
- Evidence base
The literature search provided 54 results, of which 10 studies were included [,,,,,,,,,]. The earliest study was published in 2014 []. Studies mainly consist of case series, sometimes including comparison to a retrospective cohort. However, large randomized controlled trials are non-existent.
- Technique
The PCRI is produced using pyrocarbon. The implant features a monobloc design with a slightly tilted head designed to articulate with the lunar fossa of the distal radius []. Firstly, a PRC procedure is performed, in which the scaphoid, lunate, and triquetrum are resected. After this procedure is finished, a minimal osteotomy of the proximal capitate is performed. Following this osteotomy, the stem of the implant is placed in the medullary cavity, and the joint capsule is closed [] (see Figure 7).
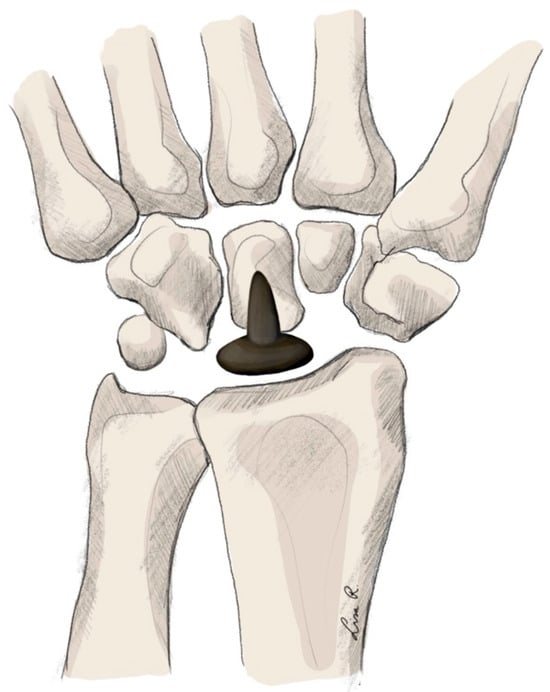
Figure 7.
Proximal capitate resurfacing implant arthroplasty.
- Clinical findings
Treatment with pyrocarbon resurfacing implants is only performed in a select group of patients. Recently, a systematic review was conducted. Proximal row carpectomy without capitate resurfacing implants showed a similar range of motion. However, the use of a PCRI is associated with better functional outcomes []. Other studies show similar favorable outcomes of PCRI [,,,]. Complication rates do seem higher compared with those for proximal row carpectomy [,,]. Luxation of the implant may be caused by difficulty in implant fixation. One review did report a lower percentage of conversion to total wrist arthrodesis compared with capsular interposition. However, follow-up was longer in the interposition groups [].
3.2.5. Pyrocardan® Disc Interposition Implant
Interposition arthroplasty is prevalent in carpal surgery. The Pyrocardan® disc is widely used to treat pisitriquetral, scaphotrapeziotrapeziodal, and trapeziometacarpal arthritis.
- Indication
As stated, indications for the Pyrocardan® disc vary from pisotriquetral arthritis [] to scaphotrapeziotrapeziodal arthritis [] and trapiezometacarpal arthritis [,]. These implants may also be used for salvage procedures after a failed trapeziectomy [].
- Evidence base
The literature search yielded 15 results. After screening, 13 of these studies provided information on implant performance [,,,,,,,,,,,,]. Two comparative studies were conducted [,].
- Technique
The surgical technique relies on the resurfacing of the carpal joint surface. The implant is made from pyrocarbon. The shaping is a biconcave disc. Based on the indication, carpal resection is performed, after which the implant is placed in this cavity. The implant allows for ligament-sparing insertion, which improves the likelihood of a biomechanically stable joint complex [] (see Figure 8).
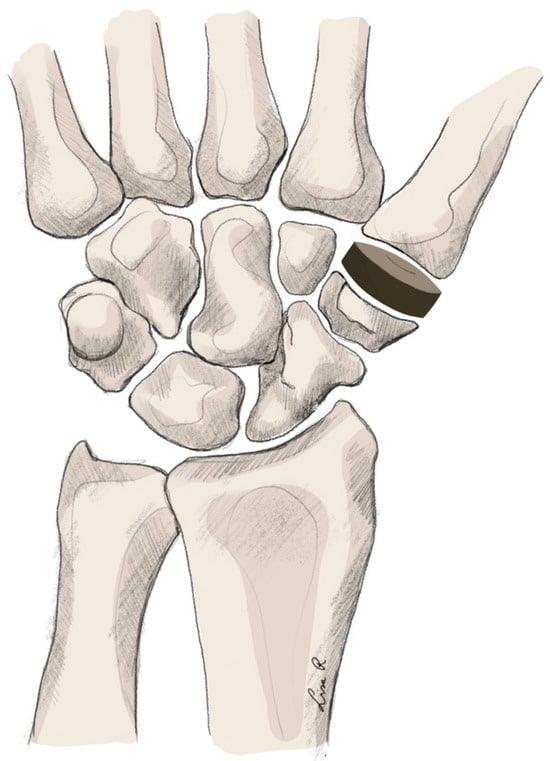
Figure 8.
Trapeziometacarpal arthroplasty using a Pyrocardan® implant.
- Clinical findings
Pyrocardan® implants in the trapeziometacarpal joint are proven to be effective. Studies suggest a survival rate of 94.3–97.5% [,,,]. The follow-up in these studies ranged from 2 to 10 years. Functionally, range of motion and grip strength were improved [,]. In salvage procedures after trapeziectomy was insufficient, the use of Pyrocardan® implants was shown to improve Quick-DASH scores []. When compared with resection arthroplasty, one study reported no significant difference in implant performance []. However, another study reported a better outcome in arthroplasty []. Complication rates were acceptable [,,]. The most notorious complication with this implant seems to be implant dislocation: one study reported a dislocation rate of 10.7% [], although some studies have not encountered dislocation of the implants [,]. Regarding the effect in pisotriquetral arthritis and scaphotrapeziotrapeziodal arthritis, a single case series for each indication showed good short-term results; however, long-term evidence is missing [,].
- Overview
To acquire an overview of the most relevant information discussed in this review, see Table 1.

Table 1.
Overview of carpal implants discussed in this review.
4. Discussion
Carpal arthroplasty concerns a heterogenic field providing the hand surgeon with a large repertoire of implants. This provides surgeons with the opportunity to offer tailored treatment modalities for each individual patient. Multiple factors play a role in deciding the best implant. The specific indication seems to be the most important, especially in joint resurfacing arthroplasties relying on the cartilage on the other joint surface to still be intact []. Moreover, supporting structures like the joint capsule or ligamentous structures need to be intact to prevent luxation of unconstrained implants [,,]. Hence, early intervention is necessary; otherwise, the ligaments or adjacent cartilage may already be destroyed [,]. In the case of total arthroplasties like TWA or arthroplasty of the first carpometacarpal joint, the state of the cartilage is less important, since they are not interposition implants and rely on bony fixation for stability.
It is important to note that the use of carpal implants is a safe technique that is already well established like the TWA or the PCRI [,], whilst also being relatively new, for example, the Amandys® and APSI arthroplasties. Since much heterogeneity exists in the configuration of osteoarthritis, and tailored treatment is becoming more relevant, it is beneficial for hand surgeons to have a broad knowledge of the available implants to enhance clinical decision-making.
This review covers a lot of different modalities in carpal arthroplasty. Since this is not a systematic review containing a meta-analysis, we cannot provide an objective and significant result concerning the performance of implants in the treatment of carpal osteoarthritis. However, when considering the results of the studies included in this review, a few key points do stand out.
Firstly, on average, implant arthroplasty does not seem to provide much better results than standard surgical treatment. Secondly, descriptions of complication rates vary from favoring non-implant arthroplasty to being similar for both modalities. Almost no studies describe a lower complication rate for implant arthroplasty. This suggests implant arthroplasty may be associated with a higher risk of complications. Considering these two points, surgeons should carefully consider the benefit of implant arthroplasty and take into account that it is often more expensive than non-implant arthroplasty.
The main drawback in the current literature for the lesser-described arthroplasties is the absence of large-scale, adequately powered, randomized controlled trials comparing arthroplasty to the current standard treatments for carpal arthritis.
This study has various limitations. Firstly, no statistical evaluation of the existing literature could be conducted due to the non-systematic nature of the review. Therefore, the aim of this paper is to provide broad information in all implants and on the state of the literature. Secondly, only one search engine was used. Therefore, some potential papers may have been excluded. Thirdly, for some implants, the evidence base was relatively thin. Therefore, it is difficult to adequately assess the performance of these implants based on the literature.
Overall, a recommendation in the use of carpal implants is the need for careful patient selection. The carpal region is biomechanically complex and is prone to implant complications like luxation. The success rate of arthroplasties, especially joint resurfacing arthroplasties like Amandys®, APSI, or PCRI, is largely dependent on the patency and stability of the surrounding tissues like the joint capsule and ligamentous structures. The surgeon needs to pay specific attention to these areas before indicating an arthroplasty.
In the current age of rapid technological development, expectations are that carpal implants will be further engineered and provide better outcomes. We have already seen the first 3D-printed implants [,]. The future will most likely be in personalized implants. Currently, techniques are being developed to provide possibilities in non-resecting, interpositional, patient-specific implants. These may be 3D-printed. However, other techniques are also available. This evolution in implant manufacturing may offer an opportunity to further personalize the implant selection. Naturally, since these modalities are currently under development, follow-up data will be necessary to provide data on the clinical outcome.
5. Conclusions
Selected patients can benefit from carpal arthroplasty. However, it is not yet the gold standard treatment for most arthritic conditions of the wrist. Complications are overall described as being either more common in implant arthroplasty or similar to those in standard treatment.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/jpm15120575/s1: File S1: PubMed search strategies for each implant type.
Author Contributions
Conceptualization, A.A.v.d.H., X.H.A.K. and R.M.S.; Methodology, A.A.v.d.H., X.H.A.K., R.M.S. and R.R.W.J.v.d.H.; Investigation, A.A.v.d.H.; Writing—original draft, A.A.v.d.H.; Writing—review and editing, A.A.v.d.H., L.E.R., X.H.A.K., R.M.S. and R.R.W.J.v.d.H.; Visualization, L.E.R.; Supervision, X.H.A.K., R.M.S. and R.R.W.J.v.d.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The original contributions presented in this study are included in the article. Further inquiries can be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Eakin, G.S.; Amodeo, K.L.; Kahlon, R.S. Arthritis and its Public Health Burden. Dela J. Public Health 2017, 3, 36–44. [Google Scholar] [CrossRef] [PubMed]
- Haugen, I.K.; Englund, M.; Aliabadi, P.; Niu, J.; Clancy, M.; Kvien, T.K.; Felson, D.T. Prevalence, incidence and progression of hand osteoarthritis in the general population: The Framingham Osteoarthritis Study. Ann. Rheum. Dis. 2011, 70, 1581–1586. [Google Scholar] [CrossRef]
- Wan, J.; Qian, X.; He, Z.; Zhu, Z.; Cheng, P.; Chen, A. Epidemiological trends of hand osteoarthritis from 1990 to 2019: Estimates from the 2019 Global Burden of Disease study. Front. Med. 2022, 9, 922321. [Google Scholar] [CrossRef] [PubMed]
- Viegas, S.F.; Patterson, R.M.; Hokanson, J.A.; Davis, J. Wrist anatomy: Incidence, distribution, and correlation of anatomic variations, tears, and arthrosis. J. Hand Surg. Am. 1993, 18, 463–475. [Google Scholar] [CrossRef] [PubMed]
- Wollstein, R.; Clavijo, J.; Gilula, L.A. Osteoarthritis of the Wrist STT Joint and Radiocarpal Joint. Arthritis 2012, 2012, 242159. [Google Scholar] [CrossRef]
- Wilder, F.V.; Barrett, J.P.; Farina, E.J. Joint-specific prevalence of osteoarthritis of the hand. Osteoarthr. Cartil. 2006, 14, 953–957. [Google Scholar] [CrossRef]
- Lane, R.; Tafti, D.; Varacallo, M.A. Scapholunate Advanced Collapse. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- Shah, C.M.; Stern, P.J. Scapholunate advanced collapse (SLAC) and scaphoid nonunion advanced collapse (SNAC) wrist arthritis. Curr. Rev. Musculoskelet. Med. 2013, 6, 9–17. [Google Scholar] [CrossRef]
- Hidajat, N.N.; Aditya, R.; Arsa, W.; Malik, R. Outcome Comparison between Carpometacarpal Arthroplasty and Trapeziectomy in Patients with Carpometacarpal Osteoarthritis: A Systematic review. Orthop. Rev. 2024, 16, 117651. [Google Scholar] [CrossRef]
- Marin, E.; Lanzutti, A. History of Metallic Orthopedic Materials. Metals 2025, 15, 378. [Google Scholar] [CrossRef]
- van den Hurk, A.A.; Lauwers, T.; Spekenbrink-Spooren, A.; Hommes, J.E.; van der Hulst, R.; Schols, R.M.; Keuter, X.H.A. Registration of carpometacarpal arthroplasty in the Dutch arthroplasty register: Impacting factors and participation. JPRAS Open 2025, 44, 49–57. [Google Scholar] [CrossRef]
- NVPC. Primaire Artrose van de Duimbasis. 2015. Available online: https://richtlijnendatabase.nl/richtlijn/primaire_artrose_van_de_duimbasis/primaire_artrose_duimbasis_-_korte_beschrijving.html (accessed on 1 January 2025).
- Teissier, J.; Teissier, P.; Toffoli, A. Trapeziometacarpal prostheses. Hand Surg. Rehabil. 2021, 40, S106–S116. [Google Scholar] [CrossRef] [PubMed]
- Alao, U.; Bodansky, D.; Hajipour, L.; Hayton, M.; Talwalkar, S. Pyrocarbon Lunate Replacements Perform Well at Two Years: A Retrospective Case Series and Technique from Two UK Tertiary Centres. J. Hand Surg. Asian Pac. Vol. 2022, 27, 1008–1012. [Google Scholar] [CrossRef]
- Rossello, M.I. A case of total scaphoid titanium custom-made 3D-printed prostheses with one-year follow-up. Case Rep. Plast. Surg. Hand Surg. 2020, 7, 7–12. [Google Scholar] [CrossRef] [PubMed]
- (LROI), Dutch Arthroplasty Register Jaarrapportage. 2024. Available online: https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwjw_4--vtaQAxXL1wIHHQ95ACkQFnoECBEQAQ&url=https%3A%2F%2Fwww.lroi.nl%2Fmedia%2Fprqogokg%2Fpdf-lroi-report-2024.pdf&usg=AOvVaw162bTFB6anNrzCRdSeQRNU&opi=89978449.2024 (accessed on 1 January 2025).
- van Santbrink, E.; van den Hurk, A.A.; Spekenbrink-Spooren, A.; Hommes, J.E.; Schols, R.M.; Keuter, X.H.A. Registration of finger implants in the Dutch arthroplasty registry (LROI). JPRAS Open 2024, 41, 215–224. [Google Scholar] [CrossRef] [PubMed]
- Reigstad, O. Total wrist arthroplasty: Recent advances and current recommendations. J. Hand Surg. Eur. Vol. 2025, 50, 34–41. [Google Scholar] [CrossRef]
- Townsend, C.B.; Paladino, J.; Ilyas, A.M. The Evolution & Outcomes of Total Wrist Arthroplasty: Current Concepts. SurgiColl 2024, 2. [Google Scholar] [CrossRef]
- Halim, A.; Weiss, A.C. Total Wrist Arthroplasty. J. Hand Surg. Am. 2017, 42, 198–209. [Google Scholar] [CrossRef]
- Melamed, E.; Marascalchi, B.; Hinds, R.M.; Rizzo, M.; Capo, J.T. Trends in the Utilization of Total Wrist Arthroplasty versus Wrist Fusion for Treatment of Advanced Wrist Arthritis. J. Wrist Surg. 2016, 5, 211–216. [Google Scholar] [CrossRef]
- Boeckstyns, M.E. Wrist arthroplasty—A systematic review. Dan. Med. J. 2014, 61, A4834. [Google Scholar]
- Monir, J.G.; McQuillan, T.J.; Suh, N. Total Wrist Arthroplasty Versus Wrist Fusion in Rheumatoid Arthritis. Hand Clin. 2025, 41, 85–91. [Google Scholar] [CrossRef]
- Truss, A.; Morris, G.; Sawalha, S.; Waseem, M. Intermediate and Long-Term Outcomes of the Universal 2 Total Wrist Replacement. J. Wrist Surg. 2024, 13, 457–462. [Google Scholar] [CrossRef]
- Matsui, Y.; Minami, A.; Kondo, M.; Ishikawa, J.; Motomiya, M.; Kawamura, D.; Iwasaki, N. Clinical Outcomes of Total Wrist Arthroplasty in Patients With Rheumatoid Arthritis: Minimum 10-Year Follow-Up Study. J. Hand Surg. Am. 2025, 50, 574–580. [Google Scholar] [CrossRef]
- Tham, A.; Ross, A.; Wright, J.; Martin, D.J.; Bransby-Zachary, M.; MacDonald, D.J.; Kennedy, I.W. Long-term outcomes of the Universal 2 total wrist arthroplasty. J. Orthop. 2025, 61, 103–108. [Google Scholar] [CrossRef]
- Reigstad, O.; Holm-Glad, T.; Korslund, J.; Myhre, C.; Thorkildsen, R.; Røkkum, M. Long-Term Outcomes of Wrist Arthroplasty Using the ReMotion™ Implant in Non-inflammatory Wrist Pathology. J. Hand Surg. Asian Pac. Vol. 2024, 29, 200–210. [Google Scholar] [CrossRef] [PubMed]
- Boeckstyns, M.E.H.; Herzberg, G. Complications after total wrist arthroplasty. J. Hand Surg. Eur. Vol. 2024, 49, 177–187. [Google Scholar] [CrossRef]
- Stringer, H.J.; Cash, T.; Kennedy, J.A.; Kandemir, G.; Newton, A.W.; Joyce, T.J.; Brown, D.J. Long-term results and explant analysis of the ReMotion total wrist arthroplasty. J. Hand Surg. Eur. Vol. 2024, 49, 995–1001. [Google Scholar] [CrossRef]
- Owen, D.H.; Booth, J.W.; Agius, P.A.; Perriman, D.M.; Smith, P.N.; Roberts, C.J. Union and Complication Rates After Total Wrist Arthrodesis: A Systematic Review and Meta-Analysis. J. Hand Surg. Am. 2025, 50, 508.e1–508.e12. [Google Scholar] [CrossRef]
- Chong, H.H.; Zabaglo, M.; Asif, A.; Boksh, K.; Kulkarni, K. A systematic review and network meta-analysis of outcomes after total wrist arthroplasty in inflammatory and non-inflammatory arthritis. J. Hand Surg. Eur. Vol. 2024, 49, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Brown, M.; Wharton, R.; Begum, R.; Trail, I.; Hayton, M.; Talwalkar, S. Total wrist arthroplasty with the Freedom® prosthesis: A short-term follow-up. J. Hand Surg. Eur. Vol. 2024, 49, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Redfern, J.A.I.; Mehta, N.; Farnebo, S.; McGuire, D.; Solomons, M.; Thomas Thorvaldson, K.; Estfan, R.; Brown, D.J. Complication rates and modes of short and medium-term failure in Motec total wrist arthroplasty: An international cohort study. J. Hand Surg. Eur. Vol. 2024, 49, 27–33. [Google Scholar] [CrossRef]
- Reigstad, O.; Holm-Glad, T.; Korslund, J.; Grimsgaard, C.; Thorkildsen, R.; Røkkum, M. 15-20 Year Follow-up After Wrist Arthroplasty Surgery—Revisiting the Development and Introduction of a New Prototype Concept for Total Wrist Arthroplasty. J. Hand Surg. Asian Pac. Vol. 2022, 27, 945–951. [Google Scholar] [CrossRef]
- Rodríguez-Nogué, L.; Martínez-Villén, G. Total wrist fusion versus total wrist prosthesis: A comparative study. J. Plast. Surg. Hand Surg. 2023, 57, 466–470. [Google Scholar] [CrossRef]
- Zijlker, H.J.A.; Ritt, M.; Beumer, A. Fourth-Generation Total Wrist Arthroplasty: A Systematic Review of Clinical Outcomes. J. Wrist Surg. 2022, 11, 456–464. [Google Scholar] [CrossRef]
- Holzbauer, M.; Mihalic, J.A.; Pollak, M.; Froschauer, S.M. Total Wrist Arthroplasty for Posttraumatic Wrist Osteoarthritis: A Cohort Study Comparing Three Indications. Life 2022, 12, 617. [Google Scholar] [CrossRef] [PubMed]
- Eschweiler, J.; Li, J.; Quack, V.; Rath, B.; Baroncini, A.; Hildebrand, F.; Migliorini, F. Total Wrist Arthroplasty—A Systematic Review of the Outcome, and an Introduction of FreeMove—An Approach to Improve TWA. Life 2022, 12, 411. [Google Scholar] [CrossRef]
- Biehl, C.; Stoll, M.; Heinrich, M.; Biehl, L.; Jung, J.; Heiss, C.; Szalay, G. Long-Term Results of the Modular Physiological Wrist Prosthesis (MPW®) in Patients with Inflammatory Diseases. Life 2021, 11, 355. [Google Scholar] [CrossRef]
- Martínez Villén, G.; Rodríguez Nogué, L. Universal 2™ total wrist arthroplasty: A single-surgeon 6.5-year follow-up study of 22 prostheses. Hand Surg. Rehabil. 2021, 40, 413–419. [Google Scholar] [CrossRef]
- Gendera, H.; Chandrasegaram-Shanmuganathan, S.; Walbeehm, R.; Samijo, S. Medium term outcomes of the Universal 2 total wrist arthroplasty in patients with degenerative or posttraumatic osteoarthritis of the wrist. Acta Orthop. Belg. 2020, 86, 549–554. [Google Scholar] [PubMed]
- Zhu, X.M.; Perera, E.; Gohal, C.; Dennis, B.; Khan, M.; Alolabi, B. A systematic review of outcomes of wrist arthrodesis and wrist arthroplasty in patients with rheumatoid arthritis. J. Hand Surg. Eur. Vol. 2021, 46, 297–303. [Google Scholar] [CrossRef] [PubMed]
- Fischer, P.; Sagerfors, M.; Jakobsson, H.; Pettersson, K. Total Wrist Arthroplasty: A 10-Year Follow-Up. J. Hand Surg. Am. 2020, 45, 780.e1–780.e10. [Google Scholar] [CrossRef]
- Matsui, Y.; Minami, A.; Kondo, M.; Ishikawa, J.; Motomiya, M.; Iwasaki, N. A Minimum 5-Year Longitudinal Study of a New Total Wrist Arthroplasty in Patients With Rheumatoid Arthritis. J. Hand Surg. Am. 2020, 45, 255.e1–255.e7. [Google Scholar] [CrossRef] [PubMed]
- Zijlker, H.J.A.; Ritt, M.; CB, I.J. Long-Term Results of Universal 2 Total Wrist Arthroplasty. J. Wrist Surg. 2019, 8, 317–320. [Google Scholar] [CrossRef]
- Froschauer, S.M.; Zaussinger, M.; Hager, D.; Behawy, M.; Kwasny, O.; Duscher, D. Re-motion total wrist arthroplasty: 39 non-rheumatoid cases with a mean follow-up of 7 years. J. Hand Surg. Eur. Vol. 2019, 44, 946–950. [Google Scholar] [CrossRef]
- Honecker, S.; Igeta, Y.; Al Hefzi, A.; Pizza, C.; Facca, S.; Liverneaux, P.A. Survival Rate on a 10-Year Follow-Up of Total Wrist Replacement Implants: A 23-Patient Case Series. J. Wrist Surg. 2019, 8, 24–29. [Google Scholar] [CrossRef]
- Berber, O.; Garagnani, L.; Gidwani, S. Systematic Review of Total Wrist Arthroplasty and Arthrodesis in Wrist Arthritis. J. Wrist Surg. 2018, 7, 424–440. [Google Scholar] [CrossRef]
- Giwa, L.; Siddiqui, A.; Packer, G. Motec Wrist Arthroplasty: 4 Years of Promising Results. J. Hand Surg. Asian Pac. Vol. 2018, 23, 364–368. [Google Scholar] [CrossRef] [PubMed]
- Brinkhorst, M.E.; Selles, R.W.; Dias, J.J.; Singh, H.P.; Feitz, R.; Moojen, T.M.; Hovius, S.E.R. Results of the Universal 2 Prosthesis in Noninflammatory Osteoarthritic Wrists. J. Wrist Surg. 2018, 7, 121–126. [Google Scholar] [CrossRef]
- Kennedy, I.W.; Ross, A.; Wright, J.; Martin, D.J.; Bransby-Zachary, M.; MacDonald, D.J. Universal 2 total wrist arthroplasty: High satisfaction but high complication rates. J. Hand Surg. Eur. Vol. 2018, 43, 375–379. [Google Scholar] [CrossRef]
- Reigstad, O.; Holm-Glad, T.; Bolstad, B.; Grimsgaard, C.; Thorkildsen, R.; Røkkum, M. Five- to 10-Year Prospective Follow-Up of Wrist Arthroplasty in 56 Nonrheumatoid Patients. J. Hand Surg. Am. 2017, 42, 788–796. [Google Scholar] [CrossRef]
- Pfanner, S.; Munz, G.; Guidi, G.; Ceruso, M. Universal 2 Wrist Arthroplasty in Rheumatoid Arthritis. J. Wrist Surg. 2017, 6, 206–215. [Google Scholar] [CrossRef] [PubMed]
- Hinds, R.M.; Capo, J.T.; Rizzo, M.; Roberson, J.R.; Gottschalk, M.B. Total Wrist Arthroplasty Versus Wrist Fusion: Utilization and Complication Rates as Reported by ABOS Part II Candidates. Hand 2017, 12, 376–381. [Google Scholar] [CrossRef]
- Badge, R.; Kailash, K.; Dickson, D.R.; Mahalingam, S.; Raza, A.; Birch, A.; Nuttall, D.; Murali, S.R.; Hayton, M.J.; Talwalkar, S.; et al. Medium-term outcomes of the Universal-2 total wrist arthroplasty in patients with rheumatoid arthritis. Bone Jt. J. 2016, 98-B, 1642–1647. [Google Scholar] [CrossRef]
- Sagerfors, M.; Gupta, A.; Brus, O.; Pettersson, K. Total Wrist Arthroplasty: A Single-Center Study of 219 Cases With 5-Year Follow-up. J. Hand Surg. Am. 2015, 40, 2380–2387. [Google Scholar] [CrossRef]
- Sagerfors, M.; Gupta, A.; Brus, O.; Rizzo, M.; Pettersson, K. Patient related functional outcome after total wrist arthroplasty: A single center study of 206 cases. Hand Surg. 2015, 20, 81–87. [Google Scholar] [CrossRef]
- Boeckstyns, M.E.; Herzberg, G. Periprosthetic osteolysis after total wrist arthroplasty. J. Wrist Surg. 2014, 3, 101–106. [Google Scholar] [CrossRef]
- Yeoh, D.; Tourret, L. Total wrist arthroplasty: A systematic review of the evidence from the last 5 years. J. Hand Surg. Eur. Vol. 2015, 40, 458–468. [Google Scholar] [CrossRef]
- Cooney, W.; Manuel, J.; Froelich, J.; Rizzo, M. Total wrist replacement: A retrospective comparative study. J. Wrist Surg. 2012, 1, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Bidwai, A.S.; Cashin, F.; Richards, A.; Brown, D.J. Short to medium results using the remotion total wrist replacement for rheumatoid arthritis. Hand Surg. 2013, 18, 175–178. [Google Scholar] [CrossRef]
- Zhu, Z.; Zhang, C.; Zhao, S.; Dong, Y.; Zeng, B. Partial wrist arthrodesis versus arthroplasty for distal radius giant cell tumours. Int. Orthop. 2013, 37, 2217–2223. [Google Scholar] [CrossRef] [PubMed]
- Herzberg, G.; Boeckstyns, M.; Sorensen, A.I.; Axelsson, P.; Kroener, K.; Liverneaux, P.; Obert, L.; Merser, S. “Remotion” total wrist arthroplasty: Preliminary results of a prospective international multicenter study of 215 cases. J. Wrist Surg. 2012, 1, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Boeckstyns, M.E.; Herzberg, G.; Merser, S. Favorable results after total wrist arthroplasty: 65 wrists in 60 patients followed for 5–9 years. Acta Orthop. 2013, 84, 415–419. [Google Scholar] [CrossRef]
- Ogunro, S.; Ahmed, I.; Tan, V. Current indications and outcomes of total wrist arthroplasty. Orthop. Clin. North. Am. 2013, 44, 371–379. [Google Scholar] [CrossRef]
- Morapudi, S.P.; Marlow, W.J.; Withers, D.; Ralte, P.; Gabr, A.; Waseem, M. Total wrist arthroplasty using the Universal 2 prosthesis. J. Orthop. Surg. 2012, 20, 365–368. [Google Scholar] [CrossRef]
- Reigstad, O.; Lütken, T.; Grimsgaard, C.; Bolstad, B.; Thorkildsen, R.; Røkkum, M. Promising one- to six-year results with the Motec wrist arthroplasty in patients with post-traumatic osteoarthritis. J. Bone Jt. Surg. Br. 2012, 94, 1540–1545. [Google Scholar] [CrossRef] [PubMed]
- Nydick, J.A.; Greenberg, S.M.; Stone, J.D.; Williams, B.; Polikandriotis, J.A.; Hess, A.V. Clinical outcomes of total wrist arthroplasty. J. Hand Surg. Am. 2012, 37, 1580–1584. [Google Scholar] [CrossRef] [PubMed]
- McCullough, M.B.; Adams, B.D.; Grosland, N.M. Postoperative analysis of patients who received the Universal 2 total wrist implant system. J. Appl. Biomech. 2012, 28, 466–472. [Google Scholar] [CrossRef] [PubMed]
- Harlingen, D.; Heesterbeek, P.J.; Vos, M. High rate of complications and radiographic loosening of the biaxial total wrist arthroplasty in rheumatoid arthritis: 32 wrists followed for 6 (5–8) years. Acta Orthop. 2011, 82, 721–726. [Google Scholar] [CrossRef]
- Krukhaug, Y.; Lie, S.A.; Havelin, L.I.; Furnes, O.; Hove, L.M. Results of 189 wrist replacements. A report from the Norwegian Arthroplasty Register. Acta Orthop. 2011, 82, 405–409. [Google Scholar] [CrossRef]
- Ferreres, A.; Lluch, A.; Del Valle, M. Universal total wrist arthroplasty: Midterm follow-up study. J. Hand Surg. Am. 2011, 36, 967–973. [Google Scholar] [CrossRef]
- Ward, C.M.; Kuhl, T.; Adams, B.D. Five to ten-year outcomes of the Universal total wrist arthroplasty in patients with rheumatoid arthritis. J. Bone Jt. Surg. Am. 2011, 93, 914–919. [Google Scholar] [CrossRef]
- Kamal, R.; Weiss, A.P. Total wrist arthroplasty for the patient with non-rheumatoid arthritis. J. Hand Surg. Am. 2011, 36, 1071–1072. [Google Scholar] [CrossRef] [PubMed]
- Herzberg, G. Prospective study of a new total wrist arthroplasty: Short term results. Chir. Main 2011, 30, 20–25. [Google Scholar] [CrossRef]
- van Winterswijk, P.J.; Bakx, P.A. Promising clinical results of the universal total wrist prosthesis in rheumatoid arthritis. Open Orthop. J. 2010, 4, 67–70. [Google Scholar] [CrossRef]
- Cavaliere, C.M.; Chung, K.C. A systematic review of total wrist arthroplasty compared with total wrist arthrodesis for rheumatoid arthritis. Plast. Reconstr. Surg. 2008, 122, 813–825. [Google Scholar] [CrossRef]
- Kistler, U.; Weiss, A.P.; Simmen, B.R.; Herren, D.B. Long-term results of silicone wrist arthroplasty in patients with rheumatoid arthritis. J. Hand Surg. Am. 2005, 30, 1282–1287. [Google Scholar] [CrossRef]
- Lundborg, G.; Besjakov, J.; Brånemark, P.I. Osseointegrated wrist-joint prostheses: A 15-year follow-up with focus on bony fixation. Scand. J. Plast. Reconstr. Surg. Hand Surg. 2007, 41, 130–137. [Google Scholar] [CrossRef]
- Radmer, S.; Andresen, R.; Sparmann, M. Total wrist arthroplasty in patients with rheumatoid arthritis. J. Hand Surg. Am. 2003, 28, 789–794. [Google Scholar] [CrossRef] [PubMed]
- Murphy, D.M.; Khoury, J.G.; Imbriglia, J.E.; Adams, B.D. Comparison of arthroplasty and arthrodesis for the rheumatoid wrist. J. Hand Surg. Am. 2003, 28, 570–576. [Google Scholar] [CrossRef] [PubMed]
- Takwale, V.J.; Nuttall, D.; Trail, I.A.; Stanley, J.K. Biaxial total wrist replacement in patients with rheumatoid arthritis. Clinical review, survivorship and radiological analysis. J. Bone Jt. Surg. Br. 2002, 84, 692–699. [Google Scholar] [CrossRef]
- Divelbiss, B.J.; Sollerman, C.; Adams, B.D. Early results of the Universal total wrist arthroplasty in rheumatoid arthritis. J. Hand Surg. Am. 2002, 27, 195–204. [Google Scholar] [CrossRef]
- Radmer, S.; Andresen, R.; Sparmann, M. Wrist arthroplasty with a new generation of prostheses in patients with rheumatoid arthritis. J. Hand Surg. Am. 1999, 24, 935–943. [Google Scholar] [CrossRef]
- Courtman, N.H.; Sochart, D.H.; Trail, I.A.; Stanley, J.K. Biaxial wrist replacement. Initial results in the rheumatoid patient. J. Hand Surg. Br. 1999, 24, 32–34. [Google Scholar] [CrossRef]
- Menon, J. Universal Total Wrist Implant: Experience with a carpal component fixed with three screws. J. Arthroplast. 1998, 13, 515–523. [Google Scholar] [CrossRef]
- Meuli, H.C. Total wrist arthroplasty. Experience with a noncemented wrist prosthesis. Clin. Orthop. Relat. Res. 1997, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Cobb, T.K.; Beckenbaugh, R.D. Biaxial total-wrist arthroplasty. J. Hand Surg. Am. 1996, 21, 1011–1021. [Google Scholar] [CrossRef] [PubMed]
- Lirette, R.; Kinnard, P. Biaxial total wrist arthroplasty in rheumatoid arthritis. Can. J. Surg. 1995, 38, 51–53. [Google Scholar]
- Meuli, H.C.; Fernandez, D.L. Uncemented total wrist arthroplasty. J. Hand Surg. Am. 1995, 20, 115–122. [Google Scholar] [CrossRef]
- Kraay, M.J.; Figgie, M.P. Wrist arthroplasty with the trispherical total wrist prosthesis. Semin. Arthroplast. 1995, 6, 37–43. [Google Scholar]
- Stanley, J.K.; Tolat, A.R. Long-term results of Swanson silastic arthroplasty in the rheumatoid wrist. J. Hand Surg. Br. 1993, 18, 381–388. [Google Scholar] [CrossRef] [PubMed]
- Lundkvist, L.; Barfred, T. Total wrist arthroplasty. Experience with Swanson flexible silicone implants, 1982–1988. Scand. J. Plast. Reconstr. Surg. Hand Surg. 1992, 26, 97–100. [Google Scholar] [CrossRef] [PubMed]
- Jolly, S.L.; Ferlic, D.C.; Clayton, M.L.; Dennis, D.A.; Stringer, E.A. Swanson silicone arthroplasty of the wrist in rheumatoid arthritis: A long-term follow-up. J. Hand Surg. Am. 1992, 17, 142–149. [Google Scholar] [CrossRef]
- Figgie, M.P.; Ranawat, C.S.; Inglis, A.E.; Sobel, M.; Figgie, H.E., 3rd. Trispherical total wrist arthroplasty in rheumatoid arthritis. J. Hand Surg. Am. 1990, 15, 217–223. [Google Scholar] [CrossRef]
- Haloua, J.P.; Collin, J.P.; Schernberg, F.; Sandre, J. Arthroplasty of the rheumatoid wrist with Swanson implant. Long-term results and complications. Ann. Chir. Main 1989, 8, 124–134. [Google Scholar] [CrossRef]
- Comstock, C.P.; Louis, D.S.; Eckenrode, J.F. Silicone wrist implant: Long-term follow-up study. J. Hand Surg. Am. 1988, 13, 201–205. [Google Scholar] [CrossRef]
- Figgie, H.E., 3rd; Ranawat, C.S.; Inglis, A.E.; Straub, L.R.; Mow, C. Preliminary results of total wrist arthroplasty in rheumatoid arthritis using the Trispherical total wrist arthroplasty. J. Arthroplast. 1988, 3, 9–15. [Google Scholar] [CrossRef]
- Cimino, P.M.; Riordan, D.; Edmunds, J.O.; Brunet, M.E.; Haddad, R.J., Jr.; Davis, M.J. Wrist arthroplasty: A retrospective study. Orthopedics 1987, 10, 337–341. [Google Scholar] [CrossRef] [PubMed]
- Vicar, A.J.; Burton, R.I. Surgical management of the rheumatoid wrist–fusion or arthroplasty. J. Hand Surg. Am. 1986, 11, 790–797. [Google Scholar] [CrossRef] [PubMed]
- Dennis, D.A.; Ferlic, D.C.; Clayton, M.L. Volz total wrist arthroplasty in rheumatoid arthritis: A long-term review. J. Hand Surg. Am. 1986, 11, 483–490. [Google Scholar] [CrossRef]
- Fatti, J.F.; Palmer, A.K.; Mosher, J.F. The long-term results of Swanson silicone rubber interpositional wrist arthroplasty. J. Hand Surg. Am. 1986, 11, 166–175. [Google Scholar] [CrossRef] [PubMed]
- McCombe, P.F.; Millroy, P.J. Swanson silastic wrist arthroplasty. A retrospective study of fifteen cases. J. Hand Surg. Br. 1985, 10, 199–201. [Google Scholar] [CrossRef]
- Nylén, S.; Sollerman, C.; Haffajee, D.; Ekelund, L. Swanson implant arthroplasty of the wrist in rheumatoid arthritis. J. Hand Surg. Br. 1984, 9, 295–299. [Google Scholar] [CrossRef] [PubMed]
- Schernberg, F.; Gerard, Y.; Collin, J.P.; Teinturier, P. Arthroplasty of the rheumatoid wrist by silicone implants. Experience with forty cases. Ann. Chir. Main 1983, 2, 18–26. [Google Scholar] [CrossRef]
- Davis, R.F.; Weiland, A.J.; Dowling, S.V. Swanson implant arthroplasty of the wrist in rheumatoid arthritis. Clin. Orthop. Relat. Res. 1982, 132–137. [Google Scholar] [CrossRef] [PubMed]
- Allieu, Y.; Asencio, G.; Brahin, B.; Gomis, R.; Bahri, H. First results of arthroplasty of the wrist by Swanson’s implant. Twenty-five cases. Ann. Chir. Main 1982, 1, 307–318. [Google Scholar] [CrossRef]
- Lamberta, F.J.; Ferlic, D.C.; Clayton, M.L. Volz total wrist arthroplasty in rheumatoid arthritis: A preliminary report. J. Hand Surg. Am. 1980, 5, 245–252. [Google Scholar] [CrossRef]
- Goodman, M.J.; Millender, L.H.; Nalebuff, E.D.; Phillips, C.A. Arthroplasty of the rheumatoid wrist with silicone rubber: An early evaluation. J. Hand Surg. Am. 1980, 5, 114–121. [Google Scholar] [CrossRef]
- Beckenbaugh, R.D. Total joint arthroplasty. The wrist. Mayo Clin. Proc. 1979, 54, 513–515. [Google Scholar]
- Rossello, M.I.; Zotta, I.; Rossello, C.; Formica, M.; Zoccolan, A. Total Wrist Arthroplasty with Integra Freedom(®) Implants: A Pilot Study with a New Evaluation System. Indian J. Orthop. 2022, 56, 1040–1047. [Google Scholar] [CrossRef] [PubMed]
- Swanson, A.B. Disabling arthritis at the base of the thumb: Treatment by resection of the trapezium and flexible (silicone) implant arthroplasty. J. Bone Jt. Surg. Am. 1972, 54, 456–471. [Google Scholar] [CrossRef]
- Frey, P.E.; Daeschler, S.C.; Naseri, Y.; Franzen, M.; Sommer, J.; Harhaus, L.; Panzram, B. TOUCH® duo-mobile prosthesis in TMC osteoarthritis: Two-year results and practical insights regarding key surgical steps and complication management. Arch. Orthop. Trauma. Surg. 2025, 145, 308. [Google Scholar] [CrossRef] [PubMed]
- Falaise, C.; Boulat, S. Five-to-8-year prospective follow-up of 61 Touch® trapeziometacarpal prostheses. Hand Surg. Rehabil. 2025, 44, 102167. [Google Scholar] [CrossRef]
- Simón-Pérez, C.; Frutos-Reoyo, E.J.; Martín-Ferrero, M.; Aguado-Maestro, I.; Guirao-Cano, L.; Martínez-Martínez, F. Total Arthroplasty Versus Trapeziectomy With Ligamentoplasty for Trapeziometacarpal Osteoarthritis: 5-year Outcomes. Clin. Orthop. Relat. Res. 2025, 483, 1312–1322. [Google Scholar] [CrossRef] [PubMed]
- Villari, E.; Langone, L.; Pilla, F.; Chiaramonte, I.; Ramponi, L.; Faldini, C. Dual mobility trapeziometacarpal prosthesis: A review of the current literature. Hand Surg. Rehabil. 2025, 44, 102107. [Google Scholar] [CrossRef]
- Jurča, J.; Vlach, M.; Havlas, V. Total joint arthroplasty of the thumb CMC joint. Arch. Orthop. Trauma. Surg. 2025, 145, 127. [Google Scholar] [CrossRef] [PubMed]
- Correia, G.; Ribeiro, E.; Correia, R.; Ribau, M.; Varanda, P.; Ribeiro, J.; Rodrigues, L.F. Trapeziometacarpal Joint Arthroplasty: Medium-Term Clinical Outcomes and Survival. Cureus 2024, 16, e72888. [Google Scholar] [CrossRef]
- Caignol, H.; Delgove, A.; Abi-Chahla, M.L.; Strugarek, C.; Delesque, A.; Pelet, H. Functional outcome of trapeziometacarpal prostheses in pan-trapezial osteoarthritis. Hand Surg. Rehabil. 2025, 44, 102025. [Google Scholar] [CrossRef] [PubMed]
- Maling, L.; Rooney, A. Outcomes of dual-mobility trapeziometacarpal arthroplasties: A systematic review. J. Hand Surg. Eur. Vol. 2025, 50, 587–595. [Google Scholar] [CrossRef]
- Piccirilli, E.; di Sette, P.; Rampoldi, M.; Primavera, M.; Salvati, C.; Tarantino, U. Comparative Analysis of Prosthetic (Touch) and Arthroplastic Surgeries for Trapeziometacarpal Arthrosis: Functional Outcomes and Patient Satisfaction With a 2-Year Follow-Up. J. Hand Surg. Glob. Online 2024, 6, 500–503. [Google Scholar] [CrossRef]
- Falkner, F.; Tümkaya, A.M.; Thomas, B.; Böcker, A.; Aman, M.; Bickert, B.; Harhaus, L.; Panzram, B. Resection arthroplasty versus dual mobility prosthesis in the treatment of trapeziometacarpal joint osteoarthritis: A 3 year non-randomized prospective study. J. Orthop. 2024, 57, 72–78. [Google Scholar] [CrossRef]
- Toffoli, A.; Degeorge, B.; Cloquell, Y.; Teissier, P.; Teissier, J. MAÏA Trapeziometacarpal Joint Arthroplasty: Clinical and Radiological Outcomes of 76 Patients With More Than 10 Years of Follow-Up. J. Hand Surg. Am. 2024, 49, 846–856. [Google Scholar] [CrossRef]
- Frey, P.E.; Bühner, C.; Falkner, F.; Harhaus, L.; Panzram, B. Mid- and long-term clinical results of the Elektra and Moovis prosthesis for trapeziometacarpal joint replacement. BMC Musculoskelet. Disord. 2024, 25, 332. [Google Scholar] [CrossRef]
- Windhofer, C.M.; Neureiter, J.; Schauer, J.; Zimmermann, G.; Hirnsperger, C. Trapeziectomy versus Maïa Prosthesis in Trapeziometacarpal Osteoarthritis. J. Wrist Surg. 2024, 13, 142–150. [Google Scholar] [CrossRef]
- Van Geel, P.; Decramer, A.; Top, A.; Muermans, S.; Ryckaert, T.; Vanmierlo, B. Thumb Arthroplasty as Reliable Long-term Solution for Trapeziometacarpal Osteoarthritis: A Minimum of 15 Years of Follow-up. Hand 2024, 20, 588–593. [Google Scholar] [CrossRef]
- Guzzini, M.; Arioli, L.; Annibaldi, A.; Pecchia, S.; Latini, F.; Ferretti, A. Interposition Arthroplasty versus Dual Cup Mobility Prosthesis in Treatment of Trapeziometacarpal Joint Osteoarthritis: A Prospective Randomized Study. Hand 2024, 19, 1260–1268. [Google Scholar] [CrossRef]
- Herren, D.B.; Marks, M.; Neumeister, S.; Schindele, S. Short-term recovery after implant versus resection arthroplasty in trapeziometacarpal joint osteoarthritis. J. Hand Surg. Eur. Vol. 2023, 48, 1048–1055. [Google Scholar] [CrossRef] [PubMed]
- de Jong, T.R.; Bonhof-Jansen, E.; Brink, S.M.; de Wildt, R.P.; van Uchelen, J.H.; Werker, P.M.N. Total joint arthroplasty versus trapeziectomy in the treatment of trapeziometacarpal joint arthritis: A randomized controlled trial. J. Hand Surg. Eur. Vol. 2023, 48, 884–894. [Google Scholar] [CrossRef]
- Seth, I.; Bulloch, G.; Seth, N.; Fogg, Q.; Hunter-Smith, D.J.; Rozen, W.M. Efficacy and Safety of Different Trapezium Implants for Trapeziometacarpal Joint Osteoarthritis: A Systematic Review and Meta-Analysis. Hand 2024, 19, 1242–1251. [Google Scholar] [CrossRef] [PubMed]
- Herren, D.B.; Marks, M.; Neumeister, S.; Schindele, S. Low complication rate and high implant survival at 2 years after Touch® trapeziometacarpal joint arthroplasty. J. Hand Surg. Eur. Vol. 2023, 48, 877–883. [Google Scholar] [CrossRef]
- Falkner, F.; Tümkaya, A.M.; Thomas, B.; Panzram, B.; Bickert, B.; Harhaus, L. Dual mobility prosthesis for trapeziometacarpal osteoarthritis: Results from a prospective study of 55 prostheses. J. Hand Surg. Eur. Vol. 2023, 48, 566–574. [Google Scholar] [CrossRef]
- Chiche, L.; Chammas, P.E.; Vial D’Allais, P.; Lazerges, C.; Coulet, B.; Chammas, M. Long-term survival analysis of 191 MAÏA® prostheses for trapeziometacarpal arthritis. J. Hand Surg. Eur. Vol. 2023, 48, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Fauquette, P.J.; Deken-Delannoy, V.; Chantelot, C.; Saab, M. The ISIS® prosthesis in 77 cases of trapeziometacarpal arthritis: Outcomes and survival at a minimum follow-up of 5 years. J. Hand Surg. Eur. Vol. 2023, 48, 108–114. [Google Scholar] [CrossRef] [PubMed]
- Buffet, A.; Lucot-Royer, L.; Pichonnat, M.; Menu, G.; De Bie, A.; Obert, L.; Loisel, F. ISIS trapeziometacarpal arthroplasty: What are the outcomes in male patients? Hand Surg. Rehabil. 2022, 41, 463–469. [Google Scholar] [CrossRef]
- Gonzalez-Espino, P.; Pottier, M.; Detrembleur, C.; Goffin, D. Touch® double mobility arthroplasty for trapeziometacarpal osteoarthritis: Outcomes for 92 prostheses. Hand Surg. Rehabil. 2021, 40, 760–764. [Google Scholar] [CrossRef]
- Raj, S.; Clay, R.; Ramji, S.; Shaunak, R.; Dadrewalla, A.; Sinha, V.; Shaunak, S. Trapeziectomy versus joint replacement for first carpometacarpal (CMC 1) joint osteoarthritis: A systematic review and meta-analysis. Eur. J. Orthop. Surg. Traumatol. 2022, 32, 1001–1021. [Google Scholar] [CrossRef]
- Martin-Ferrero, M.A.; Trigueros-Larrea, J.M.; Martin-de la Cal, E.; Coco-Martin, B.; Simon-Perez, C. Long-Term Results of Joint Arthroplasty with Total Prosthesis for Trapeziometacarpal Osteoarthritis in Patients over 65 Years of Age. Geriatrics 2021, 6, 65. [Google Scholar] [CrossRef]
- Lussiez, B.; Falaise, C.; Ledoux, P. Dual mobility trapeziometacarpal prosthesis: A prospective study of 107 cases with a follow-up of more than 3 years. J. Hand Surg. Eur. Vol. 2021, 46, 961–967. [Google Scholar] [CrossRef]
- Piacenza, A.; Vittonetto, D.; Rossello, M.I.; Testa, M. Arthrodesis Versus Arthroplasty in Thumb Carpometacarpal Osteoarthritis: Impact on Maximal Voluntary Force, Endurance, and Accuracy of Pinch. J. Hand Surg. Am. 2022, 47, 90.e1–90.e7. [Google Scholar] [CrossRef] [PubMed]
- Borgers, A.; Verstreken, A.; Vanhees, M.; Verstreken, F. Primary endoprosthetic replacement of the arthritic CMC-1 joint. Oper. Orthop. Traumatol. 2021, 33, 228–244. [Google Scholar] [CrossRef]
- Seaourt, A.C.; Dap, F.; Dautel, G.; Athlani, L. Comparison between the MAIA® Implant and Trapeziectomy for Trapeziometacarpal Osteoarthritis: Outcomes at 9 Years’ Follow-Up. J. Hand Surg. Asian Pac. Vol. 2021, 26, 158–165. [Google Scholar] [CrossRef] [PubMed]
- Kirkeby, L.; Frost, P.; Hansen, T.B.; Svendsen, S.W. Influence of Occupational Hand Force Requirements on Return to Work, Pain, and Disability After Trapeziometacarpal Total Joint Arthroplasty: A 12-Month Follow-Up Study. J. Hand Surg. Am. 2021, 46, 714.e1–714.e10. [Google Scholar] [CrossRef]
- Lee, J.K.; Yoon, B.H.; Lee, H.I.; Kim, C.; Choi, S.; Han, S.H. Prosthetic Replacement Has a Clinical Outcome Superior to That of Trapeziectomy With Ligament Reconstruction and Tendon Interposition: A Meta-Analysis. Orthopedics 2021, 44, e151–e157. [Google Scholar] [CrossRef]
- Vanmierlo, B.; Buitenweg, J.; Vanmierlo, T.; Van Royen, K.; Bonte, F.; Goubau, J. Ivory Arthroplasty for Trapeziometacarpal Joint Arthritis in Men: Analysis of Clinical Outcome and Implant Survival. Hand 2022, 17, 440–446. [Google Scholar] [CrossRef]
- De Smet, A.; Vanhove, W.; Benis, S.; Verstraete, M.; Hollevoet, N. Ten-year outcomes of the Arpe prosthesis for the treatment of osteoarthritis of the trapeziometacarpal joint. Acta Orthop. Belg. 2020, 86, 131–136. [Google Scholar]
- Verhulst, K.; Dauwe, J.; Van Nuffel, M.; De Smet, L. Short-term outcome trapeziectomy with ligament reconstruction and tendon interposition versus trapeziometacarpal prosthesis: A literature review. Acta Orthop. Belg. 2020, 86, 122–130. [Google Scholar]
- Dumartinet-Gibaud, R.; Bigorre, N.; Raimbeau, G.; Jeudy, J.; Saint Cast, Y. Arpe total joint arthroplasty for trapeziometacarpal osteoarthritis: 80 thumbs in 63 patients with a minimum of 10 years follow-up. J. Hand Surg. Eur. Vol. 2020, 45, 465–469. [Google Scholar] [CrossRef] [PubMed]
- Tchurukdichian, A.; Guillier, D.; Moris, V.; See, L.A.; Macheboeuf, Y. Results of 110 IVORY® prostheses for trapeziometacarpal osteoarthritis with a minimum follow-up of 10 years. J. Hand Surg. Eur. Vol. 2020, 45, 458–464. [Google Scholar] [CrossRef]
- Martins, A.; Charbonnel, S.; Lecomte, F.; Athlani, L. The Moovis® implant for trapeziometacarpal osteoarthritis: Results after 2 to 6 years. J. Hand Surg. Eur. Vol. 2020, 45, 477–482. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Garrido, D.; Triviño-Mayoral, V.; Delgado-Alcala, V.; Cervera-Irimia, J.; Medina-Lorca, M.; Sánchez-Sánchez, F.; Ibáñez-Vicente, C.; Pérez-Gurbindo, I.; Meccariello, L.; Rollo, G.; et al. Five year long term results of total joint arthroplasties in the treatment of trapeziometacarpal osteoarthritis. Acta Biomed. 2019, 90, 451–456. [Google Scholar] [CrossRef] [PubMed]
- Tchurukdichian, A.; Gerenton, B.; Moris, V.; See, L.A.; Stivala, A.; Guillier, D. Outcomes of Double-Mobility Prosthesis in Trapeziometacarpal Joint Arthritis With a Minimal 3 Years of Follow-Up: An Advantage for Implant Stability. Hand 2021, 16, 368–374. [Google Scholar] [CrossRef]
- Thorkildsen, R.D.; Røkkum, M. Trapeziectomy with LRTI or joint replacement for CMC1 arthritis, a randomised controlled trial. J. Plast. Surg. Hand Surg. 2019, 53, 361–369. [Google Scholar] [CrossRef]
- Andrzejewski, A.; Ledoux, P. Maïa® trapeziometacarpal joint arthroplasty: Survival and clinical outcomes at 5 years’ follow-up. Hand Surg. Rehabil. 2019, 38, 169–173. [Google Scholar] [CrossRef]
- Dreant, N.; Poumellec, M.A. Total Thumb Carpometacarpal Joint Arthroplasty: A Retrospective Functional Study of 28 MOOVIS Prostheses. Hand 2019, 14, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Vissers, G.; Goorens, C.K.; Vanmierlo, B.; Bonte, F.; Mermuys, K.; Fils, J.F.; Goubau, J.F. Ivory arthroplasty for trapeziometacarpal osteoarthritis: 10-year follow-up. J. Hand Surg. Eur. Vol. 2019, 44, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Erne, H.; Scheiber, C.; Schmauss, D.; Loew, S.; Cerny, M.; Ehrl, D.; Schmauss, V.; Machens, H.G.; Muhl, P. Total Endoprosthesis Versus Lundborg’s Resection Arthroplasty for the Treatment of Trapeziometacarpal Joint Osteoarthritis. Plast. Reconstr. Surg. Glob. Open 2018, 6, e1737. [Google Scholar] [CrossRef]
- Toffoli, A.; Teissier, J. MAÏA Trapeziometacarpal Joint Arthroplasty: Clinical and Radiological Outcomes of 80 Patients With More than 6 Years of Follow-Up. J. Hand Surg. Am. 2017, 42, 838.e1–838.e8. [Google Scholar] [CrossRef] [PubMed]
- Cootjans, K.; Vanhaecke, J.; Dezillie, M.; Barth, J.; Pottel, H.; Stockmans, F. Joint Survival Analysis and Clinical Outcome of Total Joint Arthroplasties With the ARPE Implant in the Treatment of Trapeziometacarpal Osteoarthritis With a Minimal Follow-Up of 5 Years. J. Hand Surg. Am. 2017, 42, 630–638. [Google Scholar] [CrossRef]
- Spaans, A.J.; van Minnen, L.P.; Weijns, M.E.; Braakenburg, A.; van der Molen, A.B. Retrospective Study of a Series of 20 Ivory Prostheses in the Treatment of Trapeziometacarpal Osteoarthritis. J. Wrist Surg. 2016, 5, 131–136. [Google Scholar] [CrossRef]
- Thillemann, J.K.; Thillemann, T.M.; Munk, B.; Krøner, K. High revision rates with the metal-on-metal Motec carpometacarpal joint prosthesis. J. Hand Surg. Eur. Vol. 2016, 41, 322–327. [Google Scholar] [CrossRef] [PubMed]
- Huang, K.; Hollevoet, N.; Giddins, G. Thumb carpometacarpal joint total arthroplasty: A systematic review. J. Hand Surg. Eur. Vol. 2015, 40, 338–350. [Google Scholar] [CrossRef]
- Chug, M.; Williams, N.; Benn, D.; Brindley, S. Outcome of uncemented trapeziometacarpal prosthesis for treatment of thumb carpometacarpal joint arthritis. Indian. J. Orthop. 2014, 48, 394–398. [Google Scholar] [CrossRef]
- Martin-Ferrero, M. Ten-year long-term results of total joint arthroplasties with ARPE® implant in the treatment of trapeziometacarpal osteoarthritis. J. Hand Surg. Eur. Vol. 2014, 39, 826–832. [Google Scholar] [CrossRef]
- Goubau, J.F.; Goorens, C.K.; Van Hoonacker, P.; Berghs, B.; Kerckhove, D.; Scheerlinck, T. Clinical and radiological outcomes of the Ivory arthroplasty for trapeziometacarpal joint osteoarthritis with a minimum of 5 years of follow-up: A prospective single-centre cohort study. J. Hand Surg. Eur. Vol. 2013, 38, 866–874. [Google Scholar] [CrossRef]
- Eecken, S.V.; Vanhove, W.; Hollevoet, N. Trapeziometacarpal joint replacement with the Arpe prosthesis. Acta Orthop. Belg. 2012, 78, 724–729. [Google Scholar]
- Klahn, A.; Nygaard, M.; Gvozdenovic, R.; Boeckstyns, M.E. Elektra prosthesis for trapeziometacarpal osteoarthritis: A follow-up of 39 consecutive cases. J. Hand Surg. Eur. Vol. 2012, 37, 605–609. [Google Scholar] [CrossRef]
- Johnston, P.; Getgood, A.; Larson, D.; Chojnowski, A.J.; Chakrabarti, A.J.; Chapman, P.G. De la Caffinière thumb trapeziometacarpal joint arthroplasty: 16-26 year follow-up. J. Hand Surg. Eur. Vol. 2012, 37, 621–624. [Google Scholar] [CrossRef]
- Lemoine, S.; Wavreille, G.; Alnot, J.Y.; Fontaine, C.; Chantelot, C. Second generation GUEPAR total arthroplasty of the thumb basal joint: 50 months follow-up in 84 cases. Orthop. Traumatol. Surg. Res. 2009, 95, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Hansen, T.B.; Snerum, L. Elektra trapeziometacarpal prosthesis for treatment of osteoarthrosis of the basal joint of the thumb. Scand. J. Plast. Reconstr. Surg. Hand Surg. 2008, 42, 316–319. [Google Scholar] [CrossRef] [PubMed]
- Ulrich-Vinther, M.; Puggaard, H.; Lange, B. Prospective 1-year follow-up study comparing joint prosthesis with tendon interposition arthroplasty in treatment of trapeziometacarpal osteoarthritis. J. Hand Surg. Am. 2008, 33, 1369–1377. [Google Scholar] [CrossRef] [PubMed]
- Badia, A.; Sambandam, S.N. Total joint arthroplasty in the treatment of advanced stages of thumb carpometacarpal joint osteoarthritis. J. Hand Surg. Am. 2006, 31, 1605–1614. [Google Scholar] [CrossRef]
- Regnard, P.J. Electra trapezio metacarpal prosthesis: Results of the first 100 cases. J. Hand Surg. Br. 2006, 31, 621–628. [Google Scholar] [CrossRef]
- De Smet, L.; Sioen, W.; Spaepen, D.; Van Ransbeeck, H. Total joint arthroplasty for osteoarthritis of the thumb basal joint. Acta Orthop. Belg. 2004, 70, 19–24. [Google Scholar]
- van Cappelle, H.G.; Elzenga, P.; van Horn, J.R. Long-term results and loosening analysis of de la Caffinière replacements of the trapeziometacarpal joint. J. Hand Surg. Am. 1999, 24, 476–482. [Google Scholar] [CrossRef] [PubMed]
- Hannula, T.T.; Nahigian, S.H. A preliminary report: Cementless trapeziometacarpal arthroplasty. J. Hand Surg. Am. 1999, 24, 92–101. [Google Scholar] [CrossRef]
- Wachtl, S.W.; Guggenheim, P.R.; Sennwald, G.R. Cemented and non-cemented replacements of the trapeziometacarpal joint. J. Bone Jt. Surg. Br. 1998, 80, 121–125. [Google Scholar] [CrossRef]
- Wachtl, S.W.; Sennwald, G.R. Non-cemented replacement of the trapeziometacarpal joint. J. Bone Jt. Surg. Br. 1996, 78, 787–792. [Google Scholar] [CrossRef]
- Nicholas, R.M.; Calderwood, J.W. De la Caffinière arthroplasty for basal thumb joint osteoarthritis. J. Bone Jt. Surg. Br. 1992, 74, 309–312. [Google Scholar] [CrossRef]
- Søndergaard, L.; Konradsen, L.; Rechnagel, K. Long-term follow-up of the cemented Caffinière prosthesis for trapezio-metacarpal arthroplasty. J. Hand Surg. Br. 1991, 16, 428–430. [Google Scholar] [CrossRef] [PubMed]
- Boeckstyns, M.E.; Sinding, A.; Elholm, K.T.; Rechnagel, K. Replacement of the trapeziometacarpal joint with a cemented (Caffinière) prosthesis. J. Hand Surg. Am. 1989, 14, 83–89. [Google Scholar] [CrossRef]
- Ferrari, B.; Steffee, A.D. Trapeziometacarpal total joint replacement using the Steffee prosthesis. J. Bone Jt. Surg. Am. 1986, 68, 1177–1184. [Google Scholar] [CrossRef]
- Alnot, J.Y.; Saint Laurent, Y. Total trapeziometacarpal arthroplasty. Report on seventeen cases of de generative arthritis of the trapeziometacarpal joint. Ann. Chir. Main 1985, 4, 11–21. [Google Scholar] [CrossRef]
- August, A.C.; Coupland, R.M.; Sandifer, J.P. Short term review of the De La Caffiniere trapeziometacarpal arthroplasty. J. Hand Surg. Br. 1984, 9, 185–188. [Google Scholar] [CrossRef]
- Braun, R.M. Total joint replacement at the base of the thumb—Preliminary report. J. Hand Surg. Am. 1982, 7, 245–251. [Google Scholar] [CrossRef] [PubMed]
- de la Caffiniere, J.Y.; Aucouturier, P. Trapezio-metacarpal arthroplasty by total prosthesis. Hand 1979, 11, 41–46. [Google Scholar] [CrossRef]
- Bellemère, P.; Lussiez, B. Thumb Carpometacarpal Implant Arthroplasty. Hand Clin. 2022, 38, 217–230. [Google Scholar] [CrossRef] [PubMed]
- Newton, A.; Talwalkar, S. Arthroplasty in thumb trapeziometacarpal (CMC joint) osteoarthritis: An alternative to excision arthroplasty. J. Orthop. 2023, 35, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Froschauer, S.M.; Holzbauer, M.; Mihalic, J.A.; Kwasny, O. TOUCH® Prosthesis for Thumb Carpometacarpal Joint Osteoarthritis: A Prospective Case Series. J. Clin. Med. 2021, 10, 4090. [Google Scholar] [CrossRef]
- KeriMedical. TOUCH Prosthesis Implant Information. Available online: https://www.kerimedical.com/en/portail-kerimedical-en/home-professional/touch-2/ (accessed on 1 January 2025).
- Liukkonen, R.; Karjalainen, V.L.; Kvist, R.; Vaajala, M.; Ponkilainen, V.; Karjalainen, T. Total joint arthroplasty for thumb carpometacarpal joint osteoarthritis: A systematic review and meta-analysis of randomized controlled trials. Acta Orthop. 2024, 95, 325–332. [Google Scholar] [CrossRef]
- Jager, T.; Barbary, S.; Dap, F.; Dautel, G. Evaluation of postoperative pain and early functional results in the treatment of carpometacarpal joint arthritis. Comparative prospective study of trapeziectomy vs. MAIA® prosthesis in 74 female patients. Chir. Main 2013, 32, 55–62. [Google Scholar] [CrossRef]
- Bricout, M.; Rezzouk, J. Complications and failures of the trapeziometacarpal Maia® prosthesis: A series of 156 cases. Hand Surg. Rehabil. 2016, 35, 190–198. [Google Scholar] [CrossRef]
- Bellemère, P.; Maes-Clavier, C.; Loubersac, T.; Gaisne, E.; Kerjean, Y. Amandys® implant: Novel pyrocarbon arthroplasty for the wrist. Chir. Main 2012, 31, 176–187. [Google Scholar] [CrossRef]
- Tanwin, Y.; Maes-Clavier, C.; Lestienne, V.; Gaisne, E.; Loubersac, T.; Kerjean, Y.; Bellemère, P. Medium-Term Outcomes for Amandys Implant: A 5-Year Minimum Follow-Up of 63 Cases. J. Wrist Surg. 2022, 11, 6–15. [Google Scholar] [CrossRef]
- Lestienne, V.; Chaves, C.; Tanwin, Y.; Loubersac, T.; Gaisne, E.; Kerjean, Y.; Bellemère, P. Results of interposition arthroplasty with the Amandys® pyrocarbon implant in rheumatoid wrist at a mean 5 years’ follow-up. Hand Surg. Rehabil. 2021, 40, 579–587. [Google Scholar] [CrossRef]
- Lozano, A.; Cointat, C.; Bouju, Y.; Kerjean, Y.; Lecoq, F.A.; Bellemère, P. Amandys® versus four-corner fusion in patients aged over 50 years: Long-term retrospective study in stage 3 wrist osteoarthritis. J. Hand Surg. Eur. Vol. 2024, 50, 403–410. [Google Scholar] [CrossRef]
- Wharton, R.M.H.; Sigamoney, K.V.; Hayton, M.J. Amandys pyrocarbon wrist replacement: Early outcomes following 20 consecutive cases. J. Hand Surg. Eur. Vol. 2023, 48, 809–811. [Google Scholar] [CrossRef] [PubMed]
- Gvozdenovic, R.; Vadstrup, L.S. A high incidence of early failure after Amandys® wrist interposition arthroplasty among 13 cases. J. Hand Surg. Eur. Vol. 2022, 47, 215–216. [Google Scholar] [CrossRef]
- Marie, C.; Aribert, M.; Bouyer, M.; Forli, A.; Corcella, D. Clinical, functional, and radiological results of the Amandys® interposition arthroplasty in 13 cases of wrist osteoarthritis. Hand Surg. Rehabil. 2021, 40, 420–426. [Google Scholar] [CrossRef] [PubMed]
- Bellemère, P.; Maes-Clavier, C.; Loubersac, T.; Gaisne, E.; Kerjean, Y.; Collon, S. Pyrocarbon interposition wrist arthroplasty in the treatment of failed wrist procedures. J. Wrist Surg. 2012, 1, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Daruwalla, Z.J.; Davies, K.L.; Shafighian, A.; Gillham, N.R. Early results of a prospective study on the pyrolytic carbon (pyrocarbon) Amandys® for osteoarthritis of the wrist. Ann. R. Coll. Surg. Engl. 2012, 94, 496–501. [Google Scholar] [CrossRef]
- Pierrart, J.; Bourgade, P.; Mamane, W.; Rousselon, T.; Masmejean, E.H. Novel approach for posttraumatic panarthritis of the wrist using a pyrocarbon interposition arthroplasty (Amandys®): Preliminary series of 11 patients. Chir. Main 2012, 31, 188–194. [Google Scholar] [CrossRef]
- Pequignot, J.P.; Lussiez, B.; Allieu, Y. A adaptive proximal scaphoid implant. Chir. Main 2000, 19, 276–285. [Google Scholar] [CrossRef]
- Mosillo, G.; Basso, M.A.; Balato, G.; Bernasconi, A.; Coviello, A.; Tamborini, F.; Poggetti, A.; Smeraglia, F. Adaptive proximal scaphoid implant (APSI): A systematic review of the literature. Orthop. Rev. 2022, 14, 30721. [Google Scholar] [CrossRef] [PubMed]
- Aribert, M.; Bouju, Y.; Chaise, F.; Loubersac, T.; Gaisne, E.; Bellemère, P. Adaptive Proximal Scaphoid Implant (APSI): 10-year outcomes in patients with SNAC wrists. Hand Surg. Rehabil. 2019, 38, 34–43. [Google Scholar] [CrossRef] [PubMed]
- Ferrero, M.; Carità, E.; Giacalone, F.; Teodori, J.; Donadelli, A.; Laterza, M.; Corain, M.; Battiston, B. Prosthetic Replacement of the Scaphoid Proximal Pole: Should It Be the Future? Hand 2022, 17, 899–904. [Google Scholar] [CrossRef]
- Poumellec, M.A.; Camuzard, O.; Pequignot, J.P.; Dreant, N. Adaptive Proximal Scaphoid Implant: Indications and Long-Term Results. J. Wrist Surg. 2019, 8, 344–350. [Google Scholar] [CrossRef]
- Santos, F.L.; Ferreira, A.; Grazina, R.; Sá, D.; Canela, P.; Lemos, R. APSI scaphoid hemiarthroplasty—Long-term results. Rev. Bras. Ortop. 2018, 53, 582–588. [Google Scholar] [CrossRef]
- Gras, M.; Wahegaonkar, A.L.; Mathoulin, C. Treatment of Avascular Necrosis of the Proximal Pole of the Scaphoid by Arthroscopic Resection and Prosthetic Semireplacement Arthroplasty Using the Pyrocarbon Adaptive Proximal Scaphoid Implant (APSI): Long-Term Functional Outcomes. J. Wrist Surg. 2012, 1, 159–164. [Google Scholar] [CrossRef]
- Daruwalla, Z.J.; Davies, K.; Shafighian, A.; Gillham, N.R. An alternative treatment option for scaphoid nonunion advanced collapse (SNAC) and radioscaphoid osteoarthritis: Early results of a prospective study on the pyrocarbon adaptive proximal scaphoid implant (APSI). Ann. Acad. Med. Singap. 2013, 42, 278–284. [Google Scholar] [CrossRef] [PubMed]
- Spingardi, O.; Rossello, M.I. The total scaphoid titanium arthroplasty: A 15-year experience. Hand 2011, 6, 179–184. [Google Scholar] [CrossRef]
- Henry, M. Outcomes assessment of lunate replacement arthroplasty with intrinsic carpal ligament reconstruction in Kienböck’s disease. Hand 2014, 9, 364–369. [Google Scholar] [CrossRef]
- Geuskens, W.; Verstreken, A.; Stroobants, E.; Verstreken, F. Titanium patient-specific scaphoid replacement for unreconstructable nonunions: A case series study. J. Hand Surg. Eur. Vol. 2025, 50, 486–491. [Google Scholar] [CrossRef]
- Parwaiz, H.; Elnikety, S. More than 40 years’ follow-up of an unconstrained metal lunate replacement for the treatment of Kienböck’s disease. BMJ Case Rep. 2018, 2018, 1–4. [Google Scholar] [CrossRef]
- O’Flanagan, S.J.; Curtin, J. Lunate Silastic arthroplasty in Kienbock’s disease. J. R. Coll. Surg. Edinb. 1992, 37, 52–56. [Google Scholar]
- Vaghela, K.R.; Selby, A.; Heras-Palou, C.; Johnson, N. Lunate prosthetic arthroplasty for the treatment of Kienbock’s disease: A systematic review. J. Hand Microsurg. 2025, 17, 100199. [Google Scholar] [CrossRef] [PubMed]
- Alexander, A.H.; Turner, M.A.; Alexander, C.E.; Lichtman, D.M. Lunate silicone replacement arthroplasty in Kienböck’s disease: A long-term follow-up. J. Hand Surg. Am. 1990, 15, 401–407. [Google Scholar] [CrossRef] [PubMed]
- Wagner, E.R.; Barras, L.A.; Harstad, C.; Elhassan, B.T.; Moran, S.L. Proximal Row Carpectomy in Young Patients. JBJS Essent. Surg. Tech. 2021, 11, e19.00054. [Google Scholar] [CrossRef]
- Fulchignoni, C.; Caviglia, D.; Rocchi, L. Resurfacing capitate pyrocarbon implant after proximal row carpectomy: A litterature review. Orthop. Rev. 2020, 12, 8679. [Google Scholar] [CrossRef]
- Giacalone, F.; di Summa, P.G.; Fenoglio, A.; Sard, A.; Dutto, E.; Ferrero, M.; Bertolini, M.; Garcia-Elias, M. Resurfacing Capitate Pyrocarbon Implant versus Proximal Row Carpectomy Alone: A Comparative Study to Evaluate the Role of Capitate Prosthetic Resurfacing in Advanced Carpal Collapse. Plast. Reconstr. Surg. 2017, 140, 962–970. [Google Scholar] [CrossRef]
- Hones, K.M.; Rakauskas, T.R.; Hao, K.A.; Densley, S.; Kim, J.; Wright, T.W.; Chim, H. Proximal Row Carpectomy with and without Capitate Resurfacing: A Preliminary Systematic Review and Meta-Analysis. JBJS Rev. 2024, 12, e24. [Google Scholar] [CrossRef] [PubMed]
- Rieussec, C.; Caillard, G.; Helfter, L.; Girard, P.; Forli, A.; Corcella, D. Comparison of proximal row carpectomy with RCPI® versus proximal row carpectomy with Eaton’s capsular interposition in the management of advanced wrist osteoarthritis. Orthop. Traumatol. Surg. Res. 2024, 110, 103783. [Google Scholar] [CrossRef] [PubMed]
- Marcuzzi, A.; Pederiva, D.; Pilla, F.; Canovi, A.; Corradini, A.; Adani, R.; Ruffilli, A.; Faldini, C.; Vita, F. The use of resurfacing capitate pyrocarbon implants (RCPI) in chronic diseases of the wrist: Outcomes of more than 100 cases. Musculoskelet. Surg. 2024, 108, 367–371. [Google Scholar] [CrossRef]
- Pelet, H.; Delgove, A.; Morchikh, A.; Dunet, B.; Harper, L.; Laumonerie, P.; Abi-Chahla, M.L. Long-term results of first row carpectomy with proximal capitate resurfacing using a pyrocarbon implant. J. Hand Surg. Eur. Vol. 2023, 48, 561–565. [Google Scholar] [CrossRef]
- Perry, A.C.; Wilkes, C.; Curran, M.W.T.; Ball, B.J.; Morhart, M.J. Proximal Row Carpectomy Modifications for Capitate Arthritis: A Systematic Review. J. Wrist Surg. 2023, 12, 86–94. [Google Scholar] [CrossRef] [PubMed]
- De Vitis, R.; Passiatore, M.; Cilli, V.; Pamelin, E.; Velluto, C.; Ceravolo, I.; D’Orio, M.; Ferrari, F.; Taccardo, G. Secondary Wrist Arthritis in Active Workers: Does Capitate Pyrocarbon Resurfacing (RCPI) Improve Proximal Row Carpectomy? A Retrospective Cohort Study. J. Hand Surg. Asian Pac. Vol. 2021, 26, 625–634. [Google Scholar] [CrossRef]
- Ferrero, M.; di Summa, P.G.; Giacalone, F.; Senesi, L.; Sapino, G.; Battiston, B. Salvage of advanced carpal collapse: Proximal row carpectomy with pyrocarbon resurfacing of the capitate versus four-corner arthrodesis. J. Hand Surg. Eur. Vol. 2020, 45, 687–692. [Google Scholar] [CrossRef] [PubMed]
- Marcuzzi, A.; Ozben, H.; Russomando, A. The use of a pyrocarbon capitate resurfacing implant in chronic wrist disorders. J. Hand Surg. Eur. Vol. 2014, 39, 611–618. [Google Scholar] [CrossRef] [PubMed]
- Rocchi, L.; De Vitis, R.; Pietramala, S.; Fulchignoni, C.; D’Orio, M.; Mazzone, V.; Marcuzzi, A. Resurfacing Capitate Pyrocarbon Implant for the treatment of advanced wrist arthritis in the elderly: A retrospective study. Eur. Rev. Med. Pharmacol. Sci. 2022, 26, 92–99. [Google Scholar] [CrossRef]
- Bellemère, P.; Aribert, M.; Choughri, H.; Leroy, M.; Gaisne, E. Treatment of Pisotriquetral Arthritis by Pyrocarbon Interposition Arthroplasty. J. Wrist Surg. 2018, 7, 2–10. [Google Scholar] [CrossRef]
- Gauthier, E.; Truffandier, M.V.; Gaisne, E.; Bellemère, P. Treatment of scaphotrapeziotrapezoid osteoarthritis with the Pyrocardan® implant: Results with a minimum follow-up of 2 years. Hand Surg. Rehabil. 2017, 36, 113–121. [Google Scholar] [CrossRef]
- Chiarella, G.; Ardouin, L.; Lecoq, F.A.; Sos, C.; Bellemère, P. Pyrocardan® implant interposition in the trapeziometacarpal joint: Outcomes at a minimum 10 years’ follow-up. Hand Surg. Rehabil. 2025, 44, 102074. [Google Scholar] [CrossRef]
- Lauwers, T.M.; Brouwers, K.; Staal, H.; Hoekstra, L.T.; van der Hulst, R.R. Early outcomes of Pyrocardan® implants for trapeziometacarpal osteoarthritis. Hand Surg. Rehabil. 2016, 35, 407–412. [Google Scholar] [CrossRef]
- Pouedras, M.; Chaves, C.; Gaisne, E.; Ardouin, L.; Bellemère, P. Pyrocardan® implant after failed trapeziectomy. Hand Surg. Rehabil. 2021, 40, 51–56. [Google Scholar] [CrossRef]
- O’Halloran, A.; Tiedt, L.; Flannery, O. Functional and patient reported outcomes of Pyrocardan implants for carpometacarpal osteoarthritis. Ir. J. Med. Sci. 2024, 193, 2819–2824. [Google Scholar] [CrossRef]
- Cholley-Roulleau, M.; Dautel, G.; Dap, F.; Hossu, G.; Bellemère, P.; Athlani, L. Comparison between scaphotrapeziotrapezoid arthrodesis and Pyrocardan® implant for isolated scaphotrapeziotrapezoid osteoarthritis. Orthop. Traumatol. Surg. Res. 2024, 111, 103867. [Google Scholar] [CrossRef]
- Jørgensen, R.W.; Anderson, K.A.; Odgaard, A.; Jensen, C.H. Pyrocardan Implant Arthroplasty for Carpometacarpal Osteoarthritis of the Thumb: A Comparative Study with a Historical Control Group. J. Wrist Surg. 2023, 12, 324–330. [Google Scholar] [CrossRef]
- Cholley-Roulleau, M.; Bouju, Y.; Lecoq, F.A.; Fournier, A.; Bellemère, P. Pyrocardan Scaphotrapeziotrapezoid Joint Arthroplasty for Isolated Osteoarthritis: Results after a Mean Follow-Up of 5 Years. J. Wrist Surg. 2022, 11, 262–268. [Google Scholar] [CrossRef]
- Smeraglia, F.; Basso, M.A.; Famiglietti, G.; Cozzolino, A.; Balato, G.; Bernasconi, A. Pyrocardan® interpositional arthroplasty for trapeziometacarpal osteoarthritis: A minimum four year follow-up. Int. Orthop. 2022, 46, 1803–1810. [Google Scholar] [CrossRef]
- Logan, J.; Peters, S.E.; Strauss, R.; Manzanero, S.; Couzens, G.B.; Ross, M. Pyrocardan Trapeziometacarpal Joint Arthroplasty-Medium-Term Outcomes. J. Wrist Surg. 2020, 9, 509–517. [Google Scholar] [CrossRef]
- Gerace, E.; Royaux, D.; Gaisne, E.; Ardouin, L.; Bellemère, P. Pyrocardan® implant arthroplasty for trapeziometacarpal osteoarthritis with a minimum follow-up of 5 years. Hand Surg. Rehabil. 2020, 39, 528–538. [Google Scholar] [CrossRef] [PubMed]
- Russo, S.; Bernasconi, A.; Busco, G.; Sadile, F. Treatment of the trapeziometacarpal osteoarthritis by arthroplasty with a pyrocarbon implant. Int. Orthop. 2016, 40, 1465–1471. [Google Scholar] [CrossRef] [PubMed]
- Odella, S.; Querenghi, A.M.; Sartore, R.; De Felice, A.; Dacatra, U. Trapeziometacarpal osteoarthritis: Pyrocarbon interposition implants. Joints 2014, 2, 154–158. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).