Advances in DNA sequencing technologies are revealing a vast genetic heterogeneity in human population, which may predispose to metabolic alterations if the activity of metabolic enzymes is affected [1,2,3,4]. Mutations and polymorphism may affect several protein functions simultaneously, such as catalysis, regulation, ligand binding, intracellular folding, degradation, aggregation and transport [5,6,7,8,9,10,11,12]. This is a consequence of the propagation of local stability effects across the protein structure [11,13,14,15,16,17,18] (Figure 1). In this Special Issue, we focus on three critical aspects currently under development regarding metabolic diseases with a genetic origin, namely the high-throughput computation of genotype–phenotype correlations [19], their treatment using natural or pharmacological chaperones [20,21] and the inhibition of altered metabolic routes to prevent the accumulation of toxic intermediates [22].
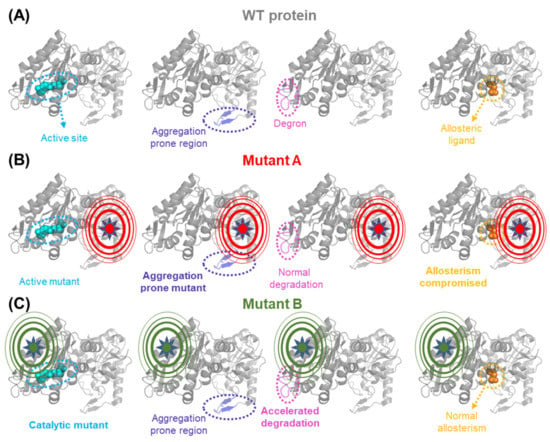
Figure 1.
Long-range propagation of mutational effects causes pleiotropic effects on protein functional features. (A) The WT form of a protein contains different functional sites: an active site, a region whose conformation determines protein aggregation, a flexible degron that controls protein degradation and a regulatory binding site for an allosteric ligand. (B,C) Pleiotropic effects of two model mutations destabilizing different regions of the protein. Note that the propagation of mutational effects in mutant A enhances protein aggregation and affects the regulatory binding site, while mutant B affects active site performance and accelerates protein degradation.
Most human proteins are oligomeric. Human alanine:glyoxylate aminotransferase (AGT) is responsible for glyoxylate detoxification in human liver peroxisomes, and inherited mutations lead to a life-threatening metabolic disease called primary hyperoxaluria type I (PH1), characterized by oxalate accumulation and liver and kidney failure [11,23]. Dindo and coworkers describe in this Special Issue the importance of the dimerization of human alanine:glyoxylate amino transferase (AGT) for the proper folding of the enzyme in cells and its import to peroxisomes, where the enzyme is metabolically useful, as well as the chaperone role of the protein cofactor pyridoxal 5′-phosphate (PLP) for dimerization and function [24]. More recently, the same group have described the successful development of pharmacological chaperones that partially restore the normal AGT activity of PH1-causing mutations [25]. Moya-Garzón and coworkers present in this Special Issue an alternative for the treatment of PH1 based on inhibitors of oxalate formation that is currently under further development by using tools from medicinal chemistry [22,26]. Human galactose 1-phosphate uridylyltransferase (GALT) is also a dimeric protein involved in the metabolism of galactose, and whose deficiency due to inherited mutations leads to galactosemia type I (GT1) [27]. The recently reported structure for GALT has allowed us to rationalize the effect of many disease-causing mutations, although many aspects of GT1 pathophysiology remain unclear [27]. The pathological mechanisms as well as novel therapies (mechanism- or phenomenological-based) and disease models are extensively discussed for GT1 in this Special Issue by Banford and coworkers [28] and Delnoy and coworkers [29].
Another example of oligomeric protein with a very complex regulation (through product inhibition and several phosphorylation events at the N-terminal domain), for which structural information has been recently provided is Tyrosine hydroxylase (TH) [30], the rate-limiting enzyme in catecholamine biosynthesis. The recently available high-resolution structural information for TH will likely improve our capacity to predict functional or folding effects of inherited mutations in the TH associated with Dopa-responsive dystonia (DRD), DA deficiency and Parkinsonisms [30]. In this Special Issue, Nygaard and coworkers deeply discussed multiple aspects of DRD, including genotype–phenotype correlations based on structural and experimental evidence as well as different therapeutic approaches such as pharmacological chaperones, gene- and enzyme-replacement therapies [31].
Pharmacophores found in high-throughput screening campaigns are promising as pharmacological chaperones for the treatment of inherited metabolic disease, although they often show drawbacks regarding solubility, bioavailability and side-effects [21,32,33]. In this Special Issue, Bernardo-Seisdedos and coworkers described the improvement of Ciclopirox as a repurposed drug for the treatment Congenital Erythropoietic Porphyria (CEP), a disease caused by a deficiency in the UROIIIS protein [7,33,34]. This type of optimization is fundamental to bringing basic studies to the clinical realm.
Overall, this Special Issue addresses several fundamental questions on the prediction of phenotypes and novel therapies for Personalized Medicine in Inborn Errors of Metabolism. It is important to highlight that all the groups that have contributed to this Special Issue are currently working on the improvement of the different mechanistic and therapeutic approaches presented. The exception is Prof. David J. Timson, who sadly passed away last summer. We hope that we will update all these studies in 2023.
Funding
The research of A.L.P. was supported by the ERDF/Spanish Ministry of Science, Innovation, and Universities—State Research Agency (grant RTI2018-096246-B-I00), Consejería de Economía, Conocimiento, Empresas, y Universidad, Junta de Andalucía (grant P18-RT-2413), and ERDF/Counseling of Economic transformation, Industry, Knowledge, and Universities (grant B-BIO-84-UGR20).
Conflicts of Interest
The author declares no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- McInnes, G.; Sharo, A.G.; Koleske, M.L.; Brown, J.E.H.; Norstad, M.; Adhikari, A.N.; Wang, S.; Brenner, S.E.; Halpern, J.; Koenig, B.A.; et al. Opportunities and Challenges for the Computational Interpretation of Rare Variation in Clinically Important Genes. Am. J. Hum. Genet. 2021, 108, 535–548. [Google Scholar] [CrossRef] [PubMed]
- Lek, M.; Karczewski, K.J.; Minikel, E.V.; Samocha, K.E.; Banks, E.; Fennell, T.; O’Donnell-Luria, A.H.; Ware, J.S.; Hill, A.J.; Cummings, B.B.; et al. Analysis of Protein-Coding Genetic Variation in 60,706 Humans. Nature 2016, 536, 285–291. [Google Scholar] [CrossRef] [PubMed]
- Manolio, T.A.; Fowler, D.M.; Starita, L.M.; Haendel, M.A.; MacArthur, D.G.; Biesecker, L.G.; Worthey, E.; Chisholm, R.L.; Green, E.D.; Jacob, H.J.; et al. Bedside Back to Bench: Building Bridges between Basic and Clinical Genomic Research. Cell 2017, 169, 6–12. [Google Scholar] [CrossRef] [PubMed]
- Pacheco-Garcia, J.L.; Cagiada, M.; Tienne-Matos, K.; Salido, E.; Lindorff-Larsen, K.; Pey, L.A. Effect of Naturally-Occurring Mutations on the Stability and Function of Cancer-Associated NQO1: Comparison of Experiments and Computation. Front. Mol. Biosci. 2022, 9, 1063620. [Google Scholar] [CrossRef]
- Flydal, M.I.; Martinez, A. Phenylalanine Hydroxylase: Function, Structure, and Regulation. IUBMB Life 2013, 65, 341–349. [Google Scholar] [CrossRef] [PubMed]
- Hnízda, A.; Majtan, T.; Liu, L.; Pey, A.L.; Carpenter, J.F.; Kodíček, M.; Kožich, V.; Kraus, J.P. Conformational Properties of Nine Purified Cystathionine β-Synthase Mutants. Biochemistry 2012, 51, 4755–4763. [Google Scholar] [CrossRef]
- Blouin, J.-M.; Bernardo-Seisdedos, G.; Sasso, E.; Esteve, J.; Ged, C.; Lalanne, M.; Sanz-Parra, A.; Urquiza, P.; de Verneuil, H.; Millet, O.; et al. Missense UROS Mutations Causing Congenital Erythropoietic Porphyria Reduce UROS Homeostasis That Can Be Rescued by Proteasome Inhibition. Hum. Mol. Genet. 2017, 26, 1565–1576. [Google Scholar] [CrossRef]
- Rivera-Barahona, A.; Navarrete, R.; García-Rodríguez, R.; Richard, E.; Ugarte, M.; Pérez-Cerda, C.; Pérez, B.; Gámez, A.; Desviat, L.R. Identification of 34 Novel Mutations in Propionic Acidemia: Functional Characterization of Missense Variants and Phenotype Associations. Mol. Genet. Metab. 2018, 125, 266–275. [Google Scholar] [CrossRef]
- Salido, E.; Pey, A.L.; Rodriguez, R.; Lorenzo, V. Primary Hyperoxalurias: Disorders of Glyoxylate Detoxification. Biochim. Biophys. Acta Mol. Basis Dis. 2012, 1822, 1453–1464. [Google Scholar] [CrossRef]
- Pey, A.L.; Padín-Gonzalez, E.; Mesa-Torres, N.; Timson, D.J. The Metastability of Human UDP-Galactose 4′-Epimerase (GALE) Is Increased by Variants Associated with Type III Galactosemia but Decreased by Substrate and Cofactor Binding. Arch. Biochem. Biophys. 2014, 562, 103–114. [Google Scholar] [CrossRef]
- Medina-Carmona, E.; Betancor-Fernández, I.; Santos, J.; Mesa-Torres, N.; Grottelli, S.; Batlle, C.; Naganathan, A.N.; Oppici, E.; Cellini, B.; Ventura, S.; et al. Insight into the Specificity and Severity of Pathogenic Mechanisms Associated with Missense Mutations through Experimental and Structural Perturbation Analyses. Hum. Mol. Genet. 2019, 28, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Pacheco-Garcia, J.L.; Anoz-Carbonell, E.; Vankova, P.; Kannan, A.; Palomino-Morales, R.; Mesa-Torres, N.; Salido, E.; Man, P.; Medina, M.; Naganathan, A.N.; et al. Structural Basis of the Pleiotropic and Specific Phenotypic Consequences of Missense Mutations in the Multifunctional NAD(P)H:Quinone Oxidoreductase 1 and Their Pharmacological Rescue. Redox Biol. 2021, 46, 102112. [Google Scholar] [CrossRef]
- Naganathan, A.N. Modulation of Allosteric Coupling by Mutations: From Protein Dynamics and Packing to Altered Native Ensembles and Function. Curr. Opin. Struct. Biol. 2019, 54, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Rajasekaran, N.; Naganathan, A.N. A Self-Consistent Structural Perturbation Approach for Determining the Magnitude and Extent of Allosteric Coupling in Proteins. Biochem. J. 2017, 474, 2379–2388. [Google Scholar] [CrossRef]
- Rajasekaran, N.; Sekhar, A.; Naganathan, A.N. A Universal Pattern in the Percolation and Dissipation of Protein Structural Perturbations. J. Phys. Chem. Lett. 2017, 8, 4779–4784. [Google Scholar] [CrossRef]
- Rajasekaran, N.; Suresh, S.; Gopi, S.; Raman, K.; Naganathan, A.N. A General Mechanism for the Propagation of Mutational Effects in Proteins. Biochemistry 2017, 56, 294–305. [Google Scholar] [CrossRef] [PubMed]
- Pacheco-García, J.L.; Loginov, D.S.; Naganathan, A.N.; Vankova, P.; Cano-Muñoz, M.; Man, P.; Pey, A.L. Loss of Stability and Unfolding Cooperativity in HPGK1 upon Gradual Structural Perturbation of Its N-Terminal Domain Hydrophobic Core. Sci. Rep. 2022, 12, 17200. [Google Scholar] [CrossRef] [PubMed]
- Pacheco-Garcia, J.L.; Loginov, D.S.; Anoz-Carbonell, E.; Vankova, P.; Palomino-Morales, R.; Salido, E.; Man, P.; Medina, M.; Naganathan, A.N.; Pey, A.L. Allosteric Communication in the Multifunctional and Redox NQO1 Protein Studied by Cavity-Making Mutations. Antioxidants 2022, 11, 1110. [Google Scholar] [CrossRef]
- Stein, A.; Fowler, D.M.; Hartmann-Petersen, R.; Lindorff-Larsen, K. Biophysical and Mechanistic Models for Disease-Causing Protein Variants. Trends Biochem. Sci. 2019, 44, 575–588. [Google Scholar] [CrossRef]
- Martinez, A.; Calvo, A.C.; Teigen, K.; Pey, A.L. Chapter 3 Rescuing Proteins of Low Kinetic Stability by Chaperones and Natural Ligands. Phenylketonuria, a Case Study, 1st ed.; Elsevier Inc.: Amsterdam, The Netherlands, 2008; Volume 83, ISBN 9780123745941. [Google Scholar]
- Pey, A.L.; Ying, M.; Cremades, N.; Velazquez-Campoy, A.; Scherer, T.; Th??ny, B.; Sancho, J.; Martinez, A. Identification of Pharmacological Chaperones as Potential Therapeutic Agents to Treat Phenylketonuria. J. Clin. Investig. 2008, 118, 2858–2867. [Google Scholar] [CrossRef]
- Moya-Garzon, M.D.; Rodriguez-Rodriguez, B.; Martin-Higueras, C.; Franco-Montalban, F.; Fernandes, M.X.; Gomez-Vidal, J.A.; Pey, A.L.; Salido, E.; Diaz-Gavilan, M. New Salicylic Acid Derivatives, Double Inhibitors of Glycolate Oxidase and Lactate Dehydrogenase, as Effective Agents Decreasing Oxalate Production. Eur. J. Med. Chem. 2022, 237, 114396. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Higuero, J.Á.; Betancor-Fernández, I.; Mesa-Torres, N.; Muga, A.; Salido, E.; Pey, A.L. Structural and Functional Insights on the Roles of Molecular Chaperones in the Mistargeting and Aggregation Phenotypes Associated with Primary Hyperoxaluria Type I. In Advances in Protein Chemistry and Structural Biology; 2019; Volume 114, pp. 119–152. ISBN 9780128155578. [Google Scholar] [PubMed]
- Dindo, M.; Ambrosini, G.; Oppici, E.; Pey, A.L.; O’Toole, P.J.; Marrison, J.L.; Morrison, I.E.G.; Butturini, E.; Grottelli, S.; Costantini, C.; et al. Dimerization Drives Proper Folding of Human Alanine:Glyoxylate Aminotransferase But Is Dispensable for Peroxisomal Targeting. J. Pers. Med. 2021, 11, 273. [Google Scholar] [CrossRef] [PubMed]
- Grottelli, S.; Annunziato, G.; Pampalone, G.; Pieroni, M.; Dindo, M.; Ferlenghi, F.; Costantino, G.; Cellini, B. Identification of Human Alanine-Glyoxylate Aminotransferase Ligands as Pharmacological Chaperones for Variants Associated with Primary Hyperoxaluria Type 1. J. Med. Chem. 2022, 65, 9718–9734. [Google Scholar] [CrossRef]
- Moya-Garzon, M.D.; Gomez-Vidal, J.A.; Alejo-Armijo, A.; Altarejos, J.; Rodriguez-Madoz, J.R.; Fernandes, M.X.; Salido, E.; Salido, S.; Diaz-Gavilan, M. Small Molecule-Based Enzyme Inhibitors in the Treatment of Primary Hyperoxalurias. J. Pers. Med. 2021, 11, 74. [Google Scholar] [CrossRef] [PubMed]
- McCorvie, T.J.; Kopec, J.; Pey, A.L.; Fitzpatrick, F.; Patel, D.; Chalk, R.; Shrestha, L.; Yue, W.W. Molecular Basis of Classic Galactosemia from the Structure of Human Galactose 1-Phosphate Uridylyltransferase. Hum. Mol. Genet. 2016, 25, 2234–2244. [Google Scholar] [CrossRef]
- Banford, S.; McCorvie, T.J.; Pey, A.L.; Timson, D.J. Galactosemia: Towards Pharmacological Chaperones. J. Pers. Med. 2021, 11, 106. [Google Scholar] [CrossRef]
- Delnoy, B.; Coelho, A.I.; Rubio-Gozalbo, M.E. Current and Future Treatments for Classic Galactosemia. J. Pers. Med. 2021, 11, 75. [Google Scholar] [CrossRef]
- Bueno-Carrasco, M.T.; Cuéllar, J.; Flydal, M.I.; Santiago, C.; Kråkenes, T.-A.; Kleppe, R.; López-Blanco, J.R.; Marcilla, M.; Teigen, K.; Alvira, S.; et al. Structural Mechanism for Tyrosine Hydroxylase Inhibition by Dopamine and Reactivation by Ser40 Phosphorylation. Nat. Commun. 2022, 13, 74. [Google Scholar] [CrossRef]
- Nygaard, G.; Szigetvari, P.D.; Grindheim, A.K.; Ruoff, P.; Martinez, A.; Haavik, J.; Kleppe, R.; Flydal, M.I. Personalized Medicine to Improve Treatment of Dopa-Responsive Dystonia-A Focus on Tyrosine Hydroxylase Deficiency. J. Pers. Med. 2021, 11, 1186. [Google Scholar] [CrossRef]
- Segovia-Falquina, C.; Vilas, A.; Leal, F.; del Caño-Ochoa, F.; Kirk, E.P.; Ugarte, M.; Ramón-Maiques, S.; Gámez, A.; Pérez, B. A Functional Platform for the Selection of Pathogenic Variants of PMM2 Amenable to Rescue via the Use of Pharmacological Chaperones. Hum. Mutat. 2022, 43, 1430–1442. [Google Scholar] [CrossRef] [PubMed]
- Urquiza, P.; Laín, A.; Sanz-Parra, A.; Moreno, J.; Bernardo-Seisdedos, G.; Dubus, P.; González, E.; Gutiérrez-de-Juan, V.; García, S.; Eraña, H.; et al. Repurposing Ciclopirox as a Pharmacological Chaperone in a Model of Congenital Erythropoietic Porphyria. Sci. Transl. Med. 2018, 10, eaat7467. [Google Scholar] [CrossRef] [PubMed]
- Bernardo-Seisdedos, G.; Charco, J.M.; SanJuan, I.; García-Martínez, S.; Urquiza, P.; Eraña, H.; Castilla, J.; Millet, O. Improving the Pharmacological Properties of Ciclopirox for Its Use in Congenital Erythropoietic Porphyria. J. Pers. Med. 2021, 11, 485. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).