Abstract
Delirium in ICU patients is a complication associated with many adverse consequences. Given the high prevalence of this complication in critically ill patients, it is essential to develop and implement an effective management protocol to prevent delirium. Given that the cause of delirium is multifactorial, non-pharmacological multicomponent interventions are promising strategies for delirium prevention. (1) Background: To identify and evaluate published systematic review on non-pharmacological nursing interventions to prevent delirium in intensive care unit patients. (2) Methods: An umbrella review guided by the Joanna Briggs Institute was utilized. Data were obtained from PubMed, Scopus, EBSCO, Web of Science, Cochrane Library, and Google Scholar. The last search was conducted on 1 May 2022. (3) Results: Fourteen reviews met the inclusion criteria. Multicomponent interventions are the most promising methods in the fight against delirium. The patient’s family is an important part of the process and should be included in the delirium prevention scheme. Light therapy can improve the patient’s circadian rhythm and thus contribute to reducing the incidence of delirium. (4) Conclusions: Non-pharmacological nursing interventions may be effective in preventing and reducing the duration of delirium in ICU patients.
1. Background
Delirium is defined as an acute cognitive impairment accompanied by fluctuations in mental status and altered attention and awareness [1,2]. This disorder is frequently caused by acute illness, trauma, surgery, adverse drug reactions, or drug withdrawal. The exact cause of delirium is still unclear, but the etiology is thought to be multifactorial [3]. Delirium has an adverse effect on patient outcomes, is an independent predictor of mortality, increases ICU length of stay, and causes cognitive impairment [4,5]. It is estimated that delirium affects up to 80% of patients in intensive care units [6]. One of the major determinants of delirium is old age [7]. In addition, risk factors include severity of illness, previous dementia, malnutrition, emergency surgery or trauma prior to ICU admission, mechanical ventilation, and anxiety [8,9,10]. There are also risk factors that are modifiable. These are mostly environmental variables such as lack of visible daylight, immobilization, isolation, noise, lack of information about the tasks performed, inadequate patient care by the medical staff, untreated pain, and use of some medications [9,11,12].
Evidence-based medicine (EBM) analyses have not identified an effective pharmacological intervention for the prevention and treatment of delirium [13]. Therefore, there is a need to develop a safe and effective strategy. The preferable methods are non-pharmacological interventions [14,15]. The possible benefit of melatonin and its antagonists has been reported, but clinical data are inconclusive, and this intervention needs further study [16,17,18]. Studies have identified a correlation between thiamine deficiency and delirium [19]. There is a potential benefit of thiamine supplementation on the prevalence of delirium. However, due to the small number of studies, no clear conclusions can be drawn on how and with what effect to implement the prevention and treatment of delirium with thiamine [20,21,22].
Studies on use of non-pharmacological interventions in patients in non-ICU wards have shown a reduction in the incidence of delirium [23,24,25].
1.1. Aim
To identify effective non-pharmacological interventions for the prevention of delirium in ICU patients and identify other potential benefits of these methods.
1.2. What Is Already Known about the Topic?
- Delirium is a common complication of hospitalization among ICU patients.
- It has an impact on treatment outcomes, increases mortality, and prolongs hospitalization and cognitive impairment.
- Delirium still remains undiagnosed among ICU patients.
- Patient assessment for delirium is still not common practice in all countries.
1.3. What This Paper Adds?
- Non-pharmacological nursing interventions can be effective in preventing and reducing the duration of delirium in ICU patients.
- Multi-component interventions have the highest efficacy.
- The family is an important part of the prevention of delirium.
- Light therapy can improve the patient’s circadian rhythm.
- Improving sleep quality may reduce the incidence of delirium.
- Medical staff should be aware of and implement the practice of delirium assessment in patients in intensive care units.
2. Methods
An umbrella review methodology was used to identify and evaluate published systematic reviews on non-pharmacological nursing interventions to prevent delirium in intensive care unit patients. In medical research, an umbrella review is a review of systematic reviews or meta-analyses. They can also be called review reviews, systematic review summaries, or review syntheses. Umbrella reviews are among the highest bodies of medical evidence available today [26,27]. Therefore, to answer the research question, we decided to conduct this type of review.
2.1. Review Questions
What are effective non-pharmacological nursing interventions to prevent delirium in intensive care unit patients?
2.2. Search Strategy
Two authors systematically searched the following databases: PubMed, Scopus, EBSCO, Web of Science, and Cochrane Library databases. The following keywords were used: “ICU”, “critical care”, ”critical illnesses”, “non-pharmacological interventions”, “multicomponent interventions”, “earplugs”, “noise reduction”, “eye masks”, “lighting control”, “education”, “orientation”, “cognitive therapy”, “bright light therapy”, “music therapy”, “physical therapy”, “early mobilization”, “exercise”, “delirium”, “delirium prevention”, “systematic review”. Keywords with their combinations using AND or OR were entered. All publications were examined by title and abstract to exclude irrelevant records. Second, a manual search of the Internet using Google Scholar was conducted to find additional systematic reviews. Any discrepancies were resolved through discussion with the four researchers, and at the end of the selection process, full agreement was reached on the articles to be included. Data including author (first), aim, participants, interventions, results, and findings were extracted from all eligible studies. The initial search was from inception to 20 March 2022, with a final search on 1 May 2022. The reviews were included if all the following criteria were satisfied.
2.3. Inclusion and Exclusion Criteria
Studies published in the English language were included. The inclusion and exclusion criteria were developed according to the PICOS criteria for including or excluding articles in the umbrella review (Table 1).

Table 1.
PICO criteria used to develop the research question and include or exclude studies.
2.4. Data Collection
The data extraction form, based on the JBI umbrella review guidelines [28], was used, and the most important information in the studies was included. This extraction was undertaken by two reviewers independently. The information collected from the reviewers comprised the following: author (first), type of review, methodology/search strategy, and number of studies included. The results of data collection are presented in Table 2. The following data were collected from the studies included in the reviews: author (first), aim, participants, interventions, results, and findings. The results are presented in Table 4.

Table 2.
Results of data collection.
2.5. Quality Assessment
The methodology for JBI umbrella reviews was followed [28]. Two authors assessed the methodological quality of the reviews for inclusion using the JBI Critical Appraisal Checklist for Systematic Reviews and Research Syntheses, which provides a checklist with 11 criteria (Q1–Q11). Each question must be answered yes, no, uncertain, or not applicable. The results of this evaluation are presented in Table 3 [52].

Table 3.
Critical appraisal results for included studies using the URARI.
3. Results
A total of 1305 records was initially obtained from the databases: PubMed—383, Scopus—10, EBSCO—179, Web of Science—276, Cochrane Library—139, and Google Scholar—318. After discarding duplicates and selecting titles and abstracts, 1279 were excluded, leaving 26 articles that were analyzed full text. Of these, 12 were excluded for failing to meet the inclusion criteria or the objective of the umbrella review. Fourteen reviews met the inclusion criteria [31,32,34,35,41,42,43,44,45,46,53,54]. The results are presented in Figure 1.
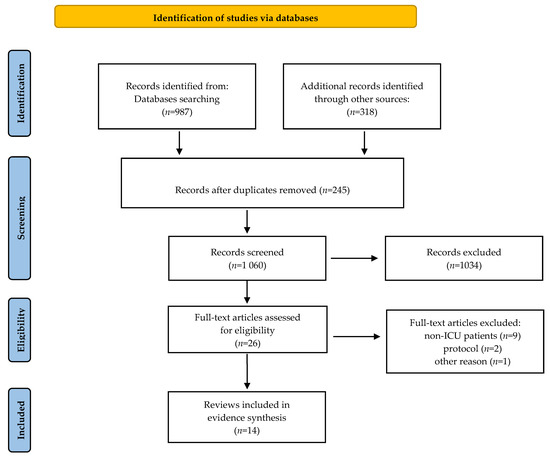
Figure 1.
PRISMA flow diagram [38].
The review focused on non-pharmacological interventions used in ICUs for delirium. We excluded a number of reviews that analyzed pharmacological interventions or in which non-ICU patients were the study participants. However, we acknowledge that two publications reviewed studies of both pharmacological and non-pharmacological methods [35,45]. Given the clear classification of methods in these reviews, we decided to include them in our review. We only considered analyzing non-pharmacological methods. In the reviews by Luther et al. and Saritas et al. on non-pharmacological interventions, the authors included one study each using melatonin/ramelteon [32,46]. We also decided to include these reviews, excluding the melatonin/ramelteon studies.
3.1. Main Findings and Conclusions of the Reviews
Table 4 summarizes the main findings of the umbrella review.

Table 4.
Tabular presentation of qualitative findings of the umbrella review.
3.2. Effects of Non-Pharmacological Nursing Interventions
Due to the presence of heterogeneous interventions in the literature, the authors decided to classify the effects of non-pharmacological nursing interventions into four main groups, which were named as follows: multicomponent non-pharmacological interventions (MLT), early mobilization (EM), family participation (FP), and environment interventions (EI). The rationale for the selection of each subtheme is presented below.
3.3. Multi-Component Non-Pharmacological Interventions
Luther et al., in their review, identified two non-pharmacological multicomponent interventions such as light and noise reduction and frequent patient orientation, listening to music, use of glasses, earplugs/eye covers, noise reduction, and use of natural light/darkened lighting in the evening, which were found to be effective in reducing the incidence and duration of delirium [28]. Furthermore, in the review by Kang et al., multicomponent interventions were found to be the most effective in reducing the incidence of delirium but not significant in reducing its duration. In this review, multicomponent interventions included combining some of the nine interventions or using a bundle of ABCDE [35]. The analysis in the review by Deng et al. showed that MLT was most effective in reducing the number of days of delirium and reducing ICU stay, although these results were not statistically significant. MLT was the third most effective in reducing the incidence of delirium and the second most effective in reducing in-hospital mortality [38]. The effect of multicomponent interventions in the review by Liang et al. was statistically significant in the combined analysis for the outcomes—reduction in incidence and duration of delirium, length of ward stays, and mortality [41]. According to a review by Chen et al., a multicomponent intervention consisting of seven complexes such as physical activity, family participation, cognitive stimulation, reorientation, sensory stimulation, environmental control, clinical adjustment, reorientation, sensory stimulation, environmental control, and clinical adjustment as a whole was the most effective intervention in preventing delirium in intensive care units. Interestingly, multicomponent interventions that did not include early mobilization and family participation did not show a statistically significant effect on reducing the incidence of delirium (multitreatment B: i.e., health education, reorientation, effective communication, environment control, and clinical adjustment; C: i.e., reorientation, effective communication, environment control, and clinical adjustment; D: i.e., reorientation, environment control, relaxation, and early mobilization; E: i.e., cognitive stimulation, reorientation, and family participation) [48].
3.4. Early Mobilization
In a review by Liang et al., seven studies analyzed the impact of early mobilization. The analysis showed positive effects in reducing the incidence (five studies) and reducing the duration of delirium (four studies). This evidence was assessed as of moderate reliability [41]. In contrast, Chen et al. found that physical activity alone did not significantly prevent delirium in the intensive care unit. However, physical activity combined with family participation had a greater effect on reducing delirium [48]. We identified one review that examined the effect of cognitive exercise on the duration of delirium in ICU patients. The meta-analysis results showed that cognitive exercise significantly reduced the incidence of delirium and the length of hospital stay in ICU patients with delirium [51].
3.5. Family Participation
An analysis by Qin et al. showed that family intervention was associated with a 24% lower risk of delirium and fewer days of delirium. However, it had no effect on the length of intensive care unit stay, duration of ventilation, or patient mortality [47]. One study included in a review by Bannon et al. showed a statistically significant difference in the duration of delirium between the patient’s reorientation with the voice of the family, and the voice of the unknown and the control group [31]. The analysis by Deng et al., on the other hand, found that family participation was the most effective intervention in reducing the incidence of delirium, followed by EP, MLT, CHI, PEI, and SR [38]. Of the studies in the Liang et al. review, five included family involvement. Four of these measured the incidence of delirium, and the outcome showed a significantly statistical effect on reducing the incidence of delirium (moderate confidence evidence). In addition, an analysis of three of the studies also showed a positive effect on the length of stay in the ICU, although the reliability of the evidence was assessed as very low [41]. A review by Nassar Junior et al. compared flexible and restrictive visiting policies in intensive care units. Two studies assessed the incidence of delirium in a total of 354 patients. Flexible visiting policies were associated with a lower incidence of delirium [34].
3.6. Environmental Interventions
In a review by Luther et al., studies relating to bright light therapy (BLT) and the use of dynamic light therapy (DLT) as single interventions showed no statistically significant differences in the incidence of delirium, although BLT therapy showed a positive effect on improving the circadian rhythm of patients [32]. In the Herling et al. review, two studies with environmental interventions (earplugs and lighting) were analyzed. In both studies, no significant differences were found with relation to the incidence of delirium [36]. A review of studies by Litton et al. found that implementation of sleep hygiene interventions, including the use of earplugs in patients admitted to the ICU, was associated with a significant reduction in the risk of delirium [30]. These outcomes agree with the review of Locihová et al. that confirm that the interventions of earplugs, eye masks, and relaxing music reduce the incidence of delirium significantly [33]. In a review by Liang et al., two studies analyzed the effect of music on the incidence of delirium. The results showed a significant effect on reducing the incidence of delirium [41].
4. Discussion
The incidence of delirium in ICU patients is a complication that is associated with many adverse consequences. It negatively affects not only cognitive function but also the outcomes of treatments of ICU patients and generates extremely high costs [25,51]. Due to the high incidence of this complication in critically ill patients, it is necessary to develop and implement an effective management scheme to prevent delirium [54]. Given that the cause of delirium is multifactorial, non-pharmacological multicomponent interventions are promising strategies for the prevention of delirium [55].
In the total effect analysis, non-pharmacological interventions in the review by Kanga et al. were found to be statistically significant for the onset and duration of delirium [35]. Sahawneh et al., in their integrative review, found a positive effect of non-pharmacological interventions in all eight quantitative studies, although four studies used only a single component intervention. Therefore, it can be speculated that a combination of some single interventions may have an even better effect [56]. Similarly, in the Liang et al. study, comparison of all non-pharmacological interventions, in a pooled analysis, with the control group showed a significant effect on reducing the incidence and duration of delirium and length of stay in the ICU. The reliability of this evidence was rated as low. In addition, multicomponent interventions had a higher odds ratio (OR) than single component interventions [41]. This supports the hypothesis that combining single interventions is a more effective strategy. Saritas et al. noted that all interventions from their study were effective, although not sufficient. Therefore, they also recommend the use of multicomponent methods [46]. Bannon et al. reported that although there is insufficient evidence that single or multifactorial interventions are effective, multicomponent interventions may be more reliable [31].
Herling et al. noted that physical, cognitive, and occupational therapy interventions have the potential to prevent or shorten the duration of delirium [36]. Schweitckert et al. studied the impact of early physical and occupational therapy on critically ill patients. The study showed that whole-body rehabilitation, consisting of discontinuation of sedation and physical and occupational therapy in the earliest days of critical illness, resulted in better functional outcomes at hospital discharge, shorter duration of delirium, and more ventilator-free days compared with standard care [54]. Xu et al. found a positive effect of cognitive exercise to reduce the duration of delirium and the length of hospital stay in ICU patients with delirium [51]. At the time of writing the Herling et al. review, several studies that may have influenced perceptions of early mobilization of ICU patients for delirium prevention were in progress [36,57,58]. We reached out to the authors of these studies. Unfortunately, in the final study by Wright et al., the effect of more intensive physical rehabilitation on delirium was not assessed in either primary or secondary outcomes [57]. In the review by Doiron et al., only two studies were included that reported the number of days spent in the ICU and the number of days in hospital with delirium [58]. The results of one study have already been cited [59]. In contrast, in the results of the second study, no difference was found between the groups [60]. However, the results of a study by Chen et al. showed that a multicomponent intervention that included early mobilization combined with family participation and other non-pharmacological interventions significantly reduced the incidence of delirium in the intensive care unit [48].
Single light therapy interventions have shown inconclusive results. However, a study by Engwall et al. showed the benefit of using a lighting system specifically tailored to supporting patients’ circadian rhythms on patients’ psychological well-being. Patients described bright light as healthy, pleasant, and having a positive effect on their mood and sense of security [61]. Additionally, in the review by Luther et al., the effects of MLT and light therapy (BLT and DLA) on circadian rhythm were assessed [32]. The study by Guo et al. showed a statistically-significant increase in melatonin and a decrease in cortisol in postoperative nocturnal urine levels in the MLT intervention group. These results suggest an improvement in the circadian rhythm with multicomponent interventions [62]. On the other hand, a study by Ono et al. showed better circadian cycle outcomes in the BLT treatment group [63]. The results from this review may therefore suggest that the use of these two methods in combination may increase their effectiveness in improving patients’ circadian rhythms and thus contribute to the prevention of delirium [32]. Although the Kang et al. analysis also found no significant effect of environmental interventions on the incidence and duration of delirium, it should be noted that single environmental interventions were components of multicomponent interventions [35]. Similarly, in the Herling et al. review, the study found no significant effect of earplug use or lighting on the incidence of delirium. However, it was observed that in patients sleeping with earplugs, delirium occurred later [36]. In contrast, this contradicts the results of the Litton et al., review, in which the placement of earplugs in patients admitted to the intensive care unit, either alone or as part of a sleep hygiene improvement package, was associated with a significant reduction in the risk of delirium [30]. The potential positive effect of using earplugs and eye masks on improving sleep quality and reducing the incidence of delirium was also demonstrated in a review by Locihová et al. [33].
Family involvement in the patient care process (F) in the ICU was a recent addition to the ABCDEF packet [64]. Deng et al., in their review, conducted a network meta-analysis that showed FP to be the most effective intervention in reducing the incidence of delirium, followed by EP, MLT, CHI, PEI and SR. [31]. In the Bannon et al. review, only family voice reorientation had a beneficial effect on delirium duration [36]. This suggests that the family may be an important part of the strategy to fight delirium in ICUs. Reviews of the literature by Qin et al. and Pabón-Martínez et al. confirmed that family interventions reduced the incidence of delirium [46,65]. Interventions for family participation in delirium prevention, in the Pabón-Martínez et al. scoping review, included flexible visiting hours, and direct and indirect (via audio-media) reorientation of the patient in the ICU. The study reported an association between flexible visiting and a reduction in the incidence of delirium. Other benefits of flexible visiting and patient reorientation were increased delirium-free days, reduced delirium duration, reduced incidence of infections, and reduced length of hospital stay [66]. Similarly, the review by Nassar Junior et al. found that flexible visiting policies were associated with a lower incidence of delirium. In addition, flexible visits were associated with a lower severity of anxiety symptoms among ICU patients. Involving the family in the therapeutic process had positive effects, not only for the ICU patients but also for the family itself [34]. This is consistent with a study by Kleinpell et al., which found that after implementing a project to promote and involve families in the intensive care unit, family members reported statistically significant increases in overall satisfaction, satisfaction with decision-making, and satisfaction with quality of care [67]. At the same time, we would also like to point out and agree with the researchers Chen et al. that the implementation of multifactorial interventions may put additional workloads on ICU nurses. Therefore, a multidisciplinary team should be involved in the care [48].
5. Conclusions
Non-pharmacological nursing interventions may be effective in preventing and shortening the duration of delirium in ICU patients. Due to the multifactorial etiology of delirium, multicomponent non-pharmacological interventions are the most promising methods. Moreover, they have shown the highest efficacy in many studies. The patient’s family is an important part of delirium prevention and should be involved in the therapeutic process. An additional benefit of including the family is to improve the families’ perceptions of the work of the medical staff. Light therapy may improve the patient’s circadian rhythm and thus reduce the incidence of delirium.
The most desirable aspect of patient-centered care for delirium is risk minimization and prevention. Medical staff should be aware of and implement delirium assessment practices and methods to minimize the risk of delirium in intensive care unit patients.
6. Implications for Practice
Non-pharmacological multifactorial interventions should be implemented in clinical practice in a scheme to prevent delirium in the ICU. Early mobilization, cognitive exercise, and rehabilitation of the whole body—physical therapy, occupational therapy, early movement, and transfer from bed to chair—can have positive effects. Regarding family involvement, we recommend introducing delirium education projects for the family, an extended visitation model, and acoustic reorientation developed by a family member. Through small activities such as orienting the patient to the date, place, and space; discussing current family events; and providing assistive devices that the patient uses every day (hearing aid, glasses), the family can stimulate cognitive, orientation, and memory processes. Single light therapy interventions, although not showing clear results, in combination with other interventions, e.g., noise reduction, use of music, eye masks, and ear plugs, can show beneficial results and support the circadian rhythm of patients. Care focused on delirium prevention should include the involvement of a multidisciplinary team including nurses, doctors, physiotherapists, psychologists, and occupational therapists.
7. Implications for Future Research
The studies that were included in the reviews mainly focused on the effect of non-pharmacological interventions on outcomes such as incidence, duration of delirium, length of hospital stay, and mortality. We suggest that future studies should also consider the impact of non-pharmacological interventions on patients’ short- and long-term cognitive function outcomes. Multifactorial interventions have been shown to be effective in reducing the incidence of delirium, but it is not always clear which combination of interventions led to the effect. Future studies should clearly specify which single interventions were combined. In addition, we suggest that future research should focus on combining single interventions, which have shown potential benefits against delirium, e.g., bright light therapy, into multicomponent interventions.
Author Contributions
Conceptualization, S.L. and W.M.-D.; methodology, S.L. and W.M.-D.; formal analysis, S.L. and W.M.-D.; writing—original draft preparation, S.L. and W.M.-D.; writing—review and editing, S.L., W.M.-D., A.F. and S.K.; visualization, W.M.-D., A.F. and B.O.; supervision, A.F. and B.O. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The authors declare that the data of this research are available from the correspondence author upon request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Hshieh, T.T.; Inouye, S.K.; Oh, E.S. Delirium in the Elderly. Psychiatr. Clin. N. Am. 2018, 41, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Volland, J.; Fisher, A.; Drexler, D. Preventing and identifying hospital-acquired delirium. Nursing 2020, 50, 32–37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilson, J.E.; Mart, M.F.; Cunningham, C.; Shehabi, Y.; Girard, T.D.; MacLullich, A.M.J.; Slooter, A.J.C.; Ely, E.W. Delirium. Nat. Rev. Dis. Prim. 2020, 6, 90. [Google Scholar] [CrossRef] [PubMed]
- Kotfis, K.; Marra, A.; Ely, E.W. ICU delirium—A diagnostic and therapeutic challenge in the intensive care unit. Anaesthesiol. Intensiv. Ther. 2018, 50, 128–140. [Google Scholar] [CrossRef] [Green Version]
- Ely, E.W.; Shintani, A.; Truman, B.; Speroff, T.; Gordon, S.M.; Harrell, F.E.; Inouye, S.K.; Bernard, G.R.; Dittus, R.S. Delirium as a Predictor of Mortality in Mechanically Ventilated Patients in the Intensive Care Unit. J. Am. Med. Assoc. 2004, 291, 1753–1762. [Google Scholar] [CrossRef] [Green Version]
- Hayhurst, C.J.; Pandharipande, P.P.; Hughes, C.G. Intensive Care Unit Delirium: A Review of Diagnosis, Prevention, and Treatment. Anesthesiology 2016, 125, 1229–1241. [Google Scholar] [CrossRef] [Green Version]
- Inouye, S.K.; Bogardus, S.T.; Baker, D.I.; Leo-Summers, L.; Cooney, L.M. The hospital elder life program: A model of care to prevent cognitive and functional decline in older hospitalized patients. J. Am. Geriatr. Soc. 2000, 48, 1697–1706. [Google Scholar] [CrossRef]
- Tran, N.N.; Hoang, T.P.N.; Ho, T.K.T. Diagnosis and risk factors for delirium in elderly patients in the emergency rooms and intensive care unit of the national geriatric hospital emergency department: A cross-sectional observational study. Int. J. Gen. Med. 2021, 14, 6505–6515. [Google Scholar] [CrossRef]
- Ozga, D.; Krupa, S.; Witt, P.; Mędrzycka-Dabrowska, W. Nursing interventions to prevent delirium in critically ill patients in the intensive care unit during the covid19 pandemic—narrative overview. Healthcare 2020, 8, 578. [Google Scholar] [CrossRef]
- McKenzie, J.; Joy, A. Family intervention improves outcomes for patients with delirium: Systematic review and meta-analysis. Australas. J. Ageing 2020, 39, 21–30. [Google Scholar] [CrossRef]
- Hipp, D.M.; Ely, E.W. Pharmacological and Nonpharmacological Management of Delirium in Critically Ill Patients. Neurotherapeutics 2012, 9, 158–175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pun, B.T.; Ely, E.W. The importance of diagnosing and managing ICU delirium. Chest 2007, 132, 624–636. [Google Scholar] [CrossRef] [PubMed]
- Krupa, S.; Ozga, D. Review of the Literature on the Occurrence of Delirium after Veno-Venous and Veno-Arterial Extracorporeal Membrane Oxygenation: A Systematic Review. Dement. Geriatr. Cogn. Dis. Extra 2019, 9, 374–380. [Google Scholar] [CrossRef] [PubMed]
- Cascella, M.; Fiore, M.; Leone, S.; Carbone, D.; Di Napoli, R. Current controversies and future perspectives on treatment of intensive care unit delirium in adults. World J. Crit. Care Med. 2019, 8, 18–27. [Google Scholar] [CrossRef]
- Devlin, J.W.; Skrobik, Y.; Gélinas, C.; Needham, D.M.; Slooter, A.J.C.; Pandharipande, P.P.; Watson, P.L.; Weinhouse, G.L.; Nunnally, M.E.; Rochwerg, B.; et al. Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU. Crit. Care Med. 2018, 46, e825–e873. [Google Scholar] [CrossRef] [Green Version]
- Blodgett, T.J.; Blodgett, N.P. Melatonin and melatonin-receptor agonists to prevent delirium in hospitalized older adults: An umbrella review. Geriatr. Nurs. 2021, 42, 1562–1568. [Google Scholar] [CrossRef]
- Khaing, K.; Nair, B.R. Melatonin for delirium prevention in hospitalized patients: A systematic review and meta-analysis. J. Psychiatr. Res. 2021, 133, 181–190. [Google Scholar] [CrossRef]
- Ng, K.T.; Teoh, W.Y.; Khor, A.J. The effect of melatonin on delirium in hospitalised patients: A systematic review and meta-analyses with trial sequential analysis. J. Clin. Anesth. 2020, 59, 74–81. [Google Scholar] [CrossRef]
- Osiezagha, K.; Ali, S.; Freeman, C.; Barker, N.C.; Jabeen, S.; Maitra, S.; Olagbemiro, Y.; Richie, W.; Bailey, T.K. Thiamine deficiency and delirium. Innov. Clin. Neurosci. 2013, 10, 26–32. [Google Scholar]
- McKenzie, C.A.; Page, V.J.; Strain, W.D.; Blackwood, B.; Ostermann, M.; Taylor, D.; Peter, E.; Spronk, P.E.; McAuley, D.F. Parenteral thiamine for prevention and treatment of delirium in critically ill adults: A systematic review protocol. Syst. Rev. 2020, 9, 131. [Google Scholar] [CrossRef]
- Sedhai, Y.R.; Shrestha, D.B.; Budhathoki, P.; Jha, V.; Mandal, S.K.; Karki, S.; Baniya, R.; Cable, C.A.; Kashiouris, M.G. Effect of thiamine supplementation in critically ill patients: A systematic review and meta-analysis. J. Crit. Care 2021, 65, 104–115. [Google Scholar] [CrossRef] [PubMed]
- Lange, S.; Mędrzycka-Dąbrowska, W.; Friganovic, A.; Oomen, B.; Krupa, S. Delirium in critical illness patients and the potential role of thiamine therapy in prevention and treatment: Findings from a scoping review with implications for evidence-based practice. Int. J. Environ. Res. Public Health 2021, 18, 8809. [Google Scholar] [CrossRef] [PubMed]
- Martinez, F.; Tobar, C.; Hill, N. Preventing delirium: Should non-pharmacological, multicomponent interventions be used? A systematic review and meta-analysis of the literature. Age Ageing 2015, 44, 196–204. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burton, J.K.; E Craig, L.; Yong, S.Q.; Siddiqi, N.; A Teale, E.; Woodhouse, R.; Barugh, A.J.; Shepherd, A.M.; Brunton, A.; Freeman, S.C.; et al. Non-pharmacological interventions for preventing delirium in hospitalised non-ICU patients. Cochrane Database Syst. Rev. 2021, 2021, CD013307. [Google Scholar] [CrossRef] [Green Version]
- Rivosecchi, R.M.; Smithburger, P.L.; Svec, S.; Campbell, S.; Kane-Gill, S.L. Nonpharmacological interventions to prevent delirium: An evidence-based systematic review. Crit. Care Nurse 2015, 35, 39–49. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Papatheodorou, S.I.; Evangelou, E. Umbrella Reviews: What They Are and Why We Need Them. Methods Mol. Biol. 2022, 2345, 135–146. [Google Scholar] [CrossRef]
- Papatheodorou, S.I. Umbrella reviews: What they are and why we need them. Eur. J. Epidemiol. 2019, 34, 543–546. [Google Scholar] [CrossRef]
- Aromataris, E.; Fernandez, R.; Godfrey, C.; Holly, C.; Khalil, H.; Tungpunkom, P. The Joanna Briggs Institute Reviewers’ Manual 2014 Methodology for JBI Umbrella Reviews; The Joanna Briggs Institute: Adelaide, Australia, 2014. [Google Scholar]
- Zhang, H.; Lu, Y.; Liu, M.; Zou, Z.; Wang, L.; Xu, F.-Y.; Shi, X.-Y. Strategies for prevention of postoperative delirium: A systematic review and meta-analysis of randomized trials. Crit. Care 2013, 17, R47. [Google Scholar] [CrossRef] [Green Version]
- Litton, E.; Carnegie, V.; Elliott, R.; Webb, S.A.R. The Efficacy of Earplugs as a Sleep Hygiene Strategy for Reducing Delirium in the ICU: A Systematic Review and Meta-Analysis. Crit. Care Med. 2016, 44, 992–999. [Google Scholar] [CrossRef]
- Bannon, L.; McGaughey, J.; Verghis, R.; Clarke, M.; McAuley, D.F.; Blackwood, B. The effectiveness of non-pharmacological interventions in reducing the incidence and duration of delirium in critically ill patients: A systematic review and meta-analysis. Intensiv. Care Med. 2019, 45, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luther, R.; McLeod, A. The effect of chronotherapy on delirium in critical care—A systematic review. Nurs. Crit. Care 2018, 23, 283–290. [Google Scholar] [CrossRef] [PubMed]
- Locihová, H.; Axmann, K.; Padyšáková, H.; Fejfar, J. Effect of the use of earplugs and eye mask on the quality of sleep in intensive care patients: A systematic review. J. Sleep Res. 2018, 27, e12607. [Google Scholar] [CrossRef] [PubMed]
- Nassar, A.P.; Besen, B.A.M.P.; Robinson, C.C.; Falavigna, M.; Teixeira, C.; Rosa, R.G. Flexible versus restrictive visiting policies in ICUs: A systematic review and meta-analysis. Crit. Care Med. 2018, 46, 1175–1180. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.; Lee, M.; Ko, H.; Kim, S.; Yun, S.; Jeong, Y.; Ch, Y. Effect of nonpharmacological interventions for the prevention of delirium in the intensive care unit: A systematic review and meta-analysis. J. Crit. Care 2018, 48, 372–384. [Google Scholar] [CrossRef] [PubMed]
- Herling, S.F.; Greve, I.E.; Vasilevskis, E.E.; Egerod, I.; Mortensen, C.B.; Møller, A.M.; Svenningsen, H.; Thomsen, T. Interventions for preventing intensive care unit delirium in adults. Cochrane Database Syst. Rev. 2018, 11, CD009783. [Google Scholar] [CrossRef]
- Janssen, T.L.; Alberts, A.R.; Hooft, L.; Mattace-Raso, F.U.S.; Mosk, C.A.; Van Der Laan, L. Prevention of postoperative delirium in elderly patients planned for elective surgery: Systematic review and meta-analysis. Clin. Interv. Aging 2019, 14, 1095–1117. [Google Scholar] [CrossRef] [Green Version]
- Deng, L.-X.; Cao, L.; Zhang, L.-N.; Peng, X.-B.; Zhang, L. Non-pharmacological interventions to reduce the incidence and duration of delirium in critically ill patients: A systematic review and network meta-analysis. J. Crit. Care 2020, 60, 241–248. [Google Scholar] [CrossRef]
- León-Salas, B.; Trujillo-Martín, M.M.; Del Castillo, L.P.M.; García-García, J.; Pérez-Ros, P.; Rivas-Ruiz, F.; Serrano-Aguilar, P. Multicomponent Interventions for the Prevention of Delirium in Hospitalized Older People: A Meta-Analysis. J. Am. Geriatr. Soc. 2020, 68, 2947–2954. [Google Scholar] [CrossRef]
- Ludolph, P.; Msc, J.S.; Kunzler, A.M.; Rösch, R.; Geschke, K.; Vahl, C.F.; Lieb, K. Non-Pharmacologic Multicomponent Interventions Preventing Delirium in Hospitalized People. J. Am. Geriatr. Soc. 2020, 68, 1864–1871. [Google Scholar] [CrossRef]
- Liang, S.; Chau, J.P.C.; Lo, S.H.S.; Zhao, J.; Choi, K.C. Effects of nonpharmacological delirium-prevention interventions on critically ill patients’ clinical, psychological, and family outcomes: A systematic review and meta-analysis. Aust. Crit. Care 2021, 34, 378–387. [Google Scholar] [CrossRef]
- Ekeozor, C.U.; Jeyaruban, D.; Lasserson, D. Where should patients with or at risk of delirium be treated in an acute care system? Comparing the rates of delirium in patients receiving usual care vs alternative care: A systematic review and meta-analysis. Int. J. Clin. Pract. 2021, 75, e13859. [Google Scholar] [CrossRef]
- de Foubert, M.; Cummins, H.; McCullagh, R.; Brueton, V.; Naughton, C. Systematic review of interventions targeting fundamental care to reduce hospital-associated decline in older patients. J. Adv. Nurs. 2021, 77, 4661–4678. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Lee, J.; Kim, J.; Jung, Y. Non-pharmacological nursing interventions for prevention and treatment of delirium in hospitalized adult patients: Systematic review of randomized controlled trials. Int. J. Environ. Res. Public Health 2021, 18, 8853. [Google Scholar] [CrossRef] [PubMed]
- Burry, L.D.; Cheng, W.; Williamson, D.R.; Adhikari, N.K.; Egerod, I.; Kanji, S.; Martin, C.M.; Hutton, B.; Rose, L. Pharmacological and non-pharmacological interventions to prevent delirium in critically ill patients: A systematic review and network meta-analysis. Intensiv. Care Med. 2021, 47, 943–9460. [Google Scholar] [CrossRef]
- Saritas, S.; Tarlaci, S. A Systematic Review of Non-Pharmacological Interventions to Prevent Delirium at Intensive Care Units. Psychiatry Behav. Sci. 2021, 11, 141–147. [Google Scholar] [CrossRef]
- Qin, M.; Gao, Y.; Guo, S.; Lu, X.; Zhu, H.; Li, Y. Family intervention for delirium for patients in the intensive care unit: A systematic meta-analysis. J. Clin. Neurosci. 2022, 96, 114–119. [Google Scholar] [CrossRef]
- Chen, T.J.; Traynor, V.; Wang, A.Y.; Shih, C.Y.; Tu, M.C.; Chuang, C.H.; Chiu, H.-Y.; Chang, H.-C. Comparative Effectiveness of Non-Pharmacological Interventions for Preventing Delirium in Critically Ill Adults: A Systematic Review and Network Meta-Analysis. Int. J. Nurs. Stud. 2022, 131, 104239. [Google Scholar] [CrossRef]
- Liu, J.; Wang, J. Efficacy of EWINDOW for prevention of delirium at intensive care units: A protocol for systematic review and meta-analysis. Medicine 2022, 101, e28598. [Google Scholar] [CrossRef]
- Bohart, S.; Møller, A.M.; Andreasen, A.S.; Waldau, T.; Lamprecht, C.; Thomsen., T. Effect of Patient and Family Centred Care interventions for adult intensive care unit patients and their families: A systematic review and meta-analysis. Intensiv. Crit. Care Nurs. 2022, 69, 103156. [Google Scholar] [CrossRef]
- Xu, C.; Chen, Z.; Zhang, L.; Guo, H. Systematic review and meta-analysis on the incidence of delirium in intensive care unit inpatients after cognitive exercise intervention. Ann. Palliat. Med. 2022, 11, 663–672. [Google Scholar] [CrossRef]
- Aromataris, E.; Munn, Z. JBI Manual for Evidence Synthesis; The Joanna Briggs Institute: Adelaide, Australia, 2020. [Google Scholar] [CrossRef]
- Pezzullo, L.; Streatfeild, J.; Hickson, J.; Teodorczuk, A.; Agar, M.R.; Caplan, G.A. Economic impact of delirium in Australia: A cost of illness study. BMJ Open 2019, 9, e027514. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cavallazzi, R.; Saad, M.; Marik, P.E. Delirium in the ICU: An overview. Ann. Intensiv. Care 2012, 2, 49. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eckstein, C.; Burkhardt, H. Multicomponent, nonpharmacological delirium interventions for older inpatients: A scoping review. Z. Gerontol. Geriatr. 2019, 52, 229–242. [Google Scholar] [CrossRef] [Green Version]
- Sahawneh, F.; Boss, L. Non-pharmacologic interventions for the prevention of delirium in the intensive care unit: An integrative review. Nurs. Crit. Care 2021, 26, 166–175. [Google Scholar] [CrossRef] [PubMed]
- Wright, S.E.; Thomas, K.; Watson, G.; Baker, C.; Bryant, A.; Chadwick, T.J.; Jing Shen, J.; Wood, R.; Wilkinson, J.; Mansfield, L.; et al. Intensive versus standard physical rehabilitation therapy in the critically ill (EPICC): A multicentre, parallel-group, randomised controlled trial. Thorax 2018, 73, 213–221. [Google Scholar] [CrossRef] [Green Version]
- Doiron, K.; Hoffmann, T.; Beller, E. Early intervention (mobilization or active exercise) for critically ill adults in the intensive care unit (Review). Cochrane Database Syst. Rev. 2018. [Google Scholar] [CrossRef] [Green Version]
- Schweickert, W.D.; Pohlman, M.C.; Pohlman, A.S.; Nigos, C.; Pawlik, A.J.; Esbrook, C.L.; Spears, L.; Miller, M.; Franczyk, M.; Deprizio, D.; et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: A randomised controlled trial. Lancet 2009, 373, 1874–1882. [Google Scholar] [CrossRef]
- Morris, P.E.; Berry, M.J.; Files, D.C.; Thompson, J.C.; Hauser, J.; Flores, L.; Dhar, S.; Chmelo, E.; Lovato, J.; Case, L.D. Standardized rehabilitation and hospital length of stay among patients with acute respiratory failure a randomized clinical trial. JAMA—J. Am. Med. Assoc. 2016, 315, 2694–2702. [Google Scholar] [CrossRef]
- Engwall, M.; Fridh, I.; Johansson, L.; Bergbom, I.; Lindahl, B. Lighting, sleep and circadian rhythm: An intervention study in the intensive care unit. Intensiv. Crit. Care Nurs. 2015, 31, 325–335. [Google Scholar] [CrossRef] [Green Version]
- Guo, Y.; Sun, L.; Li, L.; Jia, P.; Zhang, J.; Jiang, H.; Jiang, W. Impact of multicomponent, nonpharmacologic interventions on perioperative cortisol and melatonin levels and postoperative delirium in elderly oral cancer patients. Arch. Gerontol. Geriatr. 2016, 62, 112–117. [Google Scholar] [CrossRef]
- Ono, H.; Taguchi, T.; Kido, Y.; Fujino, Y.; Doki, Y. The usefulness of bright light therapy for patients after oesophagectomy. Intensiv. Crit. Care Nurs. 2011, 27, 158–166. [Google Scholar] [CrossRef] [PubMed]
- Kleinpell, R.; Zimmerman, J.; Vermoch, K.L.; Harmon, L.A.; Vondracek, H.; Hamilton, R.; Hanson, B.; Hwang, D.Y. Promoting Family Engagement in the ICU: Experience from a National Collaborative of 63 ICUs. Crit. Care Med. 2019, 47, 1692–1698. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Pabón-Martínez, B.A.; Rodríguez-Pulido, L.I.; Henao-Castaño, A.M. The family in preventing delirium in the intensive care unit: Scoping review. Enferm. Intensiva 2022, 33, 33–43. [Google Scholar] [CrossRef]
- Ely, E.W. The ABCDEF bundle: Science and philosophy of how ICU liberation serves patients and families. Crit. Care Med. 2017, 45, 321–330. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).