Abstract
Brachial–ankle pulse wave velocity (baPWV) and cardiovascular (CV) biomarkers are correlated with clinical cardiovascular diseases (CVDs) in patients with kidney disease. However, limited studies evaluated the relationship between baPWV and CV biomarkers in hemodialysis patients. This study investigated the relationship between circulating CV biomarkers and baPWV in patients on hemodialysis. Hemodialysis patients were enrolled between August 2016 and January 2017 for the measurement of baPWV, traditional CV biomarkers, including high-sensitivity troponin-T (hsTnT) and N-terminal pro-B-type natriuretic peptide (NT-proBNP), and novel CV biomarkers, including Galectin-3, Cathepsin D, placental growth factor, Endocan-1, and Fetuin-A. The independent association was assessed by multivariate-adjusted linear regression analysis to control for potential confounders. The final analysis included 176 patients (95 men and 81 women) with a mean age of 60 ± 11 y old. After adjusting for age and sex, hsTnT (p < 0.01), NT-proBNP (p = 0.01), Galectin-3 (p = 0.03), and Cathepsin D (p < 0.01) were significantly directly correlated with baPWV. The direct correlation with baPWV existed in multivariable linear regression models with a β of 0.1 for hsTnT and 0.1 for Cathepsin D. The direct relationship between baPWV and CV biomarkers, particularly with hsTnT and Cathepsin D, may be helpful for risk stratification of hemodialysis patients.
1. Introduction
Chronic kidney disease (CKD) is a prevalent global health issue, with a prevalence rate of 15%, and accounts for about 1.1 million deaths annually [1,2]. Patients with end-stage renal disease (ESRD) have higher morbidity and mortality than those with cardiovascular diseases (CVDs) [3]. Despite ongoing breakthroughs in treatment, CVDs are now recognized as the primary cause of death in 54–58% of hemodialysis patients due to major adverse cardiovascular events (MACEs), including cerebrovascular disease or coronary artery disease (CAD) [4]. Better tools to stratify chronic hemodialysis patients at higher cardiovascular risk can help clinicians improve such patients’ clinical outcomes.
Several CV biomarkers are considered to provide more information regarding progressed kidney injury and cardiovascular risk to predict MACEs in managing patients with ESRD [5]. High-sensitivity troponin-T (hsTnT) and N-terminal pro-B-type natriuretic peptide (NT-proBNP) are traditional CV biomarkers highly associated with CVD in ESRD patients. In recent years, novel CV biomarkers, such as Annexin A5, Cystatin C, Plasminogen activator inhibitor-1 (PAI-1), P-Selectin, Tissue inhibitor of metalloproteinase (TIMP-1), Endocan, placental growth factor (PLGF), Galectin-3, Fetuin-A, and Cathepsin D have been studied on the clinical prognostic prediction of CV risk in different clinical settings [6,7,8,9,10,11,12,13,14,15,16,17]. Among them, Endocan [8,9], placental growth factor (PLGF) [10,11], Galectin-3 [12,13], Fetuin-A [14,15], and Cathepsin D [16,17] have been demonstrated to act as important CV risk predictors in the CKD patients; therefore, they were selected to be analyzed in our study. The concept of adaptive enrichment design leads to the future use of a biomarker in decisions regarding appropriate treatment [18].
Brachial–ankle pulse wave velocity (baPWV) is an easily applied and noninvasive measurement using an independent cuff on four limbs based on an oscillometric approach. Increased baPWV correlates with a high tendency of arterial stiffness [19], one of the underlying mechanisms of MACEs in ESRD [20,21,22]. A high baPWV is related to CV risk in pre-dialysis CKD patients [23], but its role as an indicator of CVD progression in ESRD has not been established [24].
CV biomarkers and baPWV are well-validated methods that can be easily measured in the hemodialysis unit. However, the significance of the relationship between CV biomarkers and baPWV in ESRD patients has not been well-clarified, and limited studies are focusing on the clinical efficacy of the combined use of baPWV with other biomarkers in the ESRD setting. Thus, the present study aimed to analyze the association between circulating CV biomarkers and baPWV in hemodialysis patients to investigate the underlying importance of CV risk prediction in ESRD patients.
2. Materials and Methods
2.1. Subjects
The study was conducted in the dialysis clinic of a provincial hospital in southern Taiwan between August 2016 and January 2017. In total, 193 patients who underwent hemodialysis 3 times a week using high-flux dialyzers were enrolled. Each hemodialysis session lasted 3.5–4 h, with a 500 mL/min dialysate flow rate and 250–300 mL/min blood flow rate. The Institutional Review Board of Kaohsiung Medical University Hospital approved the research protocol (KMUHIRB-E(I)-20160095), and all patients provided written informed consent. All clinical investigations were according to the Declaration of Helsinki’s standards and principles.
2.2. Comorbidity, Clinical Data, and Traditional CV Biomarkers
All patients’ sociodemographic data (age, gender, and smoking), dialysis vintage, dialysis access (fistula vs. graft), medical history, and biochemical data were obtained from the electronic health care system records. BMI was calculated by dividing patient weight by height squared. A blood pressure of 140/90 mmHg or greater, or the usage of antihypertensive drugs, was considered hypertension, with diabetes defined as an HbA1C of 6.5% or greater or the use of antidiabetics. Physicians’ diagnoses were used to determine a patient’s history of hyperlipidemia, CAD, and cerebrovascular illness. Hemoglobin, albumin, low-density lipoprotein cholesterol (LDL-C), ion calcium, phosphate, C-reactive protein, and single pool Kt/V (dialysis clearance) were recorded. The chemiluminescence technique (Roche Diagnostics Instrument) was used to evaluate two classic CV biomarkers, hsTnT and NT-proBNP (Supplementary Table S1).
2.3. Measurement of BaPWV
BaPWV was measured using an automated waveform analyzer (VP-1000, Colin, Komaki, Japan) 10–30 min before the hemodialysis session [25]. Transmission distance/transmission time was used to compute the baPWV, with the highest bilateral baPWV values used to determine the representative value for this analysis.
2.4. Multiplex Analysis of Novel CV Biomarkers
Serum levels of Endocan-1, PLGF, Fetuin-A, Cathepsin D, and Galectin-3 were evaluated using the MILLIPLEX MAP technology (Luminex) (Supplementary Table S1). Blood samples were taken using the arteriovenous shunt before the planned hemodialysis session in the middle of the week after an overnight fast. The serum was collected by centrifugation at 1500 rpm for 10 min at 4 °C and stored at −80 °C until use. The Luminex (Millipore, St. Charles, MO, USA), which combines the concept of a sandwich immunoassay with fluorescent-bead-based technology, allows for individual and multiplex analysis of several analytes in a single microtiter well. The multiplex immunobead tests were performed in a 96-well microplate format according to the manufacturer’s instructions. Briefly, PBS/bovine serum albumin was used to block the filter-bottom, 96-well microplate (Millipore, Billerica, MA, USA) for 10 min; then, 5-fold serial dilutions were prepared from the premixed standards to generate a 7-point standard curve. In duplicate wells, 50 µL of standards or patient sera were mixed with 50 µL of the bead mixture and incubated for one hour at room temperature. The wells were washed three times with wash buffer using a vacuum manifold and then incubated in the dark for 45 min with steady shaking with phycoerythrin (PE)-conjugated secondary antibody. The wells were washed twice, and assay buffer was added to each well (Millipore, St. Charles, MO, USA). The median fluorescence intensity was measured, and the sample concentrations were determined by the five-parameter logistic curve fitting approach through the Milliplex Analyst Software (Viagene Tech, Carlisle, MA, USA).
2.5. Statistical Analysis
Descriptive data are presented as mean and standard deviation (SD) or percentages as appropriate. The Kolmogorov–Smirnov test was used to determine if the data were normally distributed. The chi-square test for categorical variables, the independent t-test for continuous variables with nearly normal distribution, or the Mann–Whitney U test for continuous variables with skewed distribution was used to assess differences between groups. Multiple CV biomarkers linked to baPWV were screened and assessed using linear regression adjusted for age and gender. The distribution of CV biomarker values and baPWV were plotted, and Spearman rank correlation coefficients were calculated. A multivariate-adjusted linear regression analysis was used to investigate the connection between serum CV biomarkers and baPWV by controlling for relevant confounders to find independent variables. Stepwise procedures were used to identify relevant demographic factors, comorbidities, and clinical laboratory data to control variables, with a p < 0.05 for model entrance and a p > 0.1 for model removal. SAS statistical software was used for all statistical analyses (version 9.4; SAS Institute Inc., Cary, NC, USA), and the data are presented as a β with 95% CI. Statistical significance was defined as a two-tailed p < 0.05.
3. Results
3.1. Study Flowchart and Baseline Characteristics of Patients
The study involved 193 patients over the age of 30 y old who had been on dialysis for at least 90 d. After excluding patients who refused to complete the ankle–brachial index (ABI)-form system (n = 5), patients with atrial fibrillation (n = 4), patients with bilateral below-the-knee amputations (n = 3), and patients who had been hospitalized for four weeks before research enrolment (n = 5), the final analysis included 176 patients (95 men and 81 women) (Figure 1).
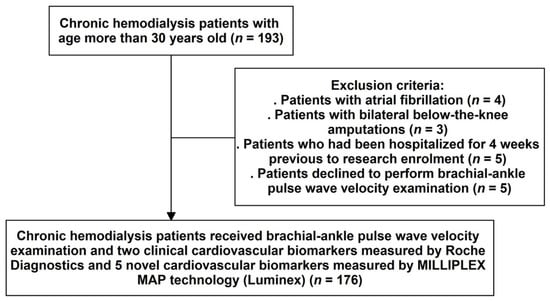
Figure 1.
Sample derivation flowchart.
The patients’ baseline characteristics are presented in Table 1, showing that they had a mean age of 60 ± 11 y old and an average of 91.8 ± 64.3 mo hemodialysis vintage. The mean systolic and diastolic blood pressure was 156 ± 25.5 mmHg and 81.5 ± 14.6 mmHg, respectively. The median blood levels of clinical laboratory data were 10.4 mg/dL hemoglobin, 3.9 mg/dL albumin, 87.5 mg/dL LDL-C, 4.7 mg/dL ion calcium, 4.7 mg/dL phosphate, 0.2 mg/L in C-reactive protein, and 1.6 single pool Kt/V (dialysis dose). The median blood levels of clinical and novel CV biomarkers were 0.1 ng/mL hsTnT, 2.8 ng/mL NT-proBNP, 1.4 ng/mL Endocan-1, 0.01 pg/mL PLGF, 82.5 ng/mL Fetuin-A, 1 ng/mL Galectin-3, and 6.4 ng/mL Cathepsin D.

Table 1.
The baseline characteristics in hemodialysis participants.
3.2. The Linear Association between CV Biomarkers and BaPWV
After adjusting for age and sex, hsTnT (p < 0.01), NT-proBNP (p = 0.01), Galectin-3 (p = 0.03), and Cathepsin D (p < 0.01) were significantly directly associated with baPWV in hemodialysis patients (Table 2). The direct correlation of four CV biomarkers (hsTnT, NT-proBNP, Galectin-3, and Cathepsin D in log-transformed value) and baPWV (log-transformed value) is shown in a scatter plot with a spline line (Figure 2). Furthermore, the mean values of CV biomarkers and multiple comparisons corresponding to the quartiles groups of the baPWV were found to demonstrate the dose–response effect (Figure 3).

Table 2.
Relationship between cardiovascular disease biomarkers and brachial–ankle pulse wave velocity in hemodialysis patients.
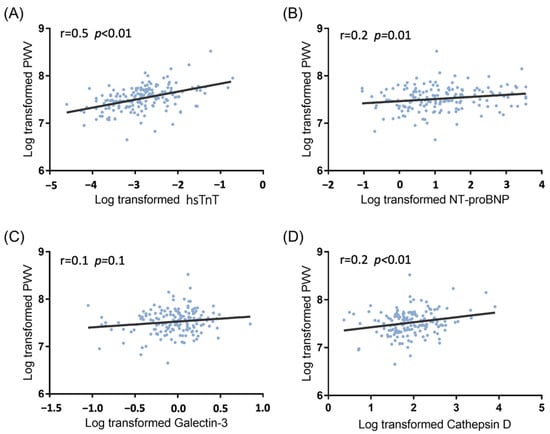
Figure 2.
Scatter plots with spline lines demonstrated selected CV biomarkers’ direct association with brachial–ankle pulse wave velocity in hemodialysis patients: (A) high-sensitivity troponin T (r = 0.5, p < 0.01); (B) N-terminal pro-brain natriuretic peptide (r = 0.2, p = 0.01); (C) Galectin 3 (r = 0.1, p = 0.1); (D) Cathepsin D (r = 0.2, p < 0.01).
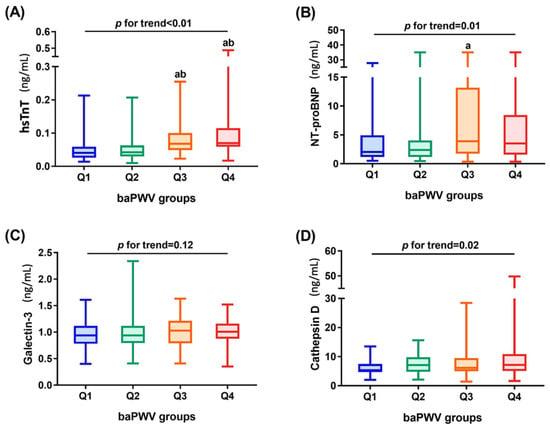
Figure 3.
The mean values of CV biomarkers in quartile groups of brachial–ankle pulse wave velocity among hemodialysis patients: (A) high-sensitivity troponin T (p for trend < 0.01); (B) N-terminal pro-brain natriuretic peptide (p for trend 0.01); (C) Galectin 3 (p for trend = 0.12); (D) Cathepsin D (p for trend = 0.02). Multiple comparisons were performed by Dunn’s multiple comparison test (a. significant difference from Q1; b. significant difference from Q2). Statistical significance was defined as p < 0.05.
3.3. Multivariable Linear Regression Model Analysis
Supplementary Table S2 demonstrates the correlation between baPWV and clinical parameters and biochemical blood profiles in a simple linear regression model to determine the potential confounders for multivariable adjustment. The univariate and age-, sex-adjusted linear regression models showed a direct association between four CV biomarkers (hsTnT, NT-proBNP, Galectin-3, and Cathepsin D in log-transformed value) and baPWV (log-transformed value) levels (Model 1 and Model 2 in Table 3). Considering age, sex, smoking history, body mass index, systolic blood pressure, diastolic blood pressure, hemodialysis vintage, cause of end-stage kidney disease, diabetes mellitus, hypertension, albumin, low-density lipoprotein, iron calcium, and C-reactive protein are important contributing factors to arterial stiffness and several of them identified in single linear regression analysis (Supplementary Table S2), so these covariates were controlled in multivariable linear regression models. A significantly direct correlation remained between baPWV and hsTnT (β 0.1, 95% CI 0.04–0.2, p < 0.01) as well as Cathepsin D (β 0.1, 95% CI 0.02–0.1, p = 0.01) (Model 3 in Table 3). Furthermore, the direct association remained significantly between CV biomarkers (hsTnT and Cathepsin D) and baPWV values in the multivariable-adjusted linear regression model with stepwise covariate selection (Supplementary Table S3).

Table 3.
Association between circulating CV biomarker levels (log-transformed) and brachial–ankle pulse wave velocity (log-transformed) in hemodialysis participants using the multivariable-adjusted linear regression model.
4. Discussion
The present study retrospectively investigated the association between baPWV and serum levels of classical and novel CV biomarkers in 176 patients undergoing long-term hemodialysis. There were direct linear correlations between CV biomarkers (hsTnT, NT-proBNP, Galectin-3, and Cathepsin D) and baPWV after adjusting for age and sex. Furthermore, an independent relationship was confirmed by the multivariable-adjusted linear regression model between baPWV and two biomarkers—hsTnT and Cathepsin D—indicating the link between peripheral vascular disease evaluation and proteins from cardiac origin. Thus, PWV not only represents a marker of peripheral vascular disease but is also a marker of cardiac disease in hemodialysis patients.
ESRD patients on maintenance hemodialysis have a 20-fold higher CV mortality rate than the general population, with an almost 10-fold higher incidence of MACE, such as cerebrovascular events or myocardial infarction [21]. Arterial stiffness is a major cause of atherosclerosis and vascular calcification, which are highly associated with CV morbidity risk in these patients [21,26]. Reduced vessel compliance and distensibility defining arterial stiffness cause greater pressure pulse transmission velocity along the arteries and are inversely correlated with PWV [27]. Compared with the direct measurement of carotid-femoral (cf) PWV and aortic PWV, baPWV can be more easily used by clinicians due to its simplicity and convenience [28]. A meta-analysis by Vlachopoulos et al. [29] demonstrated that every 1 m/s increase in baPWV was linked with a 12% increase in MACE occurrence and baPWV serves as a stronger predictor of prognosis in CVD and ESRD patients aged 59.04 to 63.36 y, a similar age to our study population (60 ± 11 y). However, Tripepi et al. [24] more recently showed minimal prognostic superiority of PWV over simple risk prediction scores in the hemodialysis population and questioned the accuracy of PWV alone for CV risk stratification. Similar to previous studies [30,31,32], factors such as age (p < 0.01), systolic blood pressure (p < 0.01), diastolic blood pressure (p < 0.01), hemodialysis vintage (p = 0.03), diabetes mellitus (p < 0.01), hypertension (p < 0.01), albumin (p < 0.01), ion calcium (p = 0.02), and C-reactive protein (p < 0.01) were significantly associated with baPWV (Supplementary Table S2), suggesting that these factors could be taken into accounts in multivariable-adjusted linear regression models (Table 3) for investigating the association between circulating CV biomarkers and baPWV.
Both hsTnT and NT-proBNP are classical CV biomarkers that play an important role in reflecting the subclinical damage and stress of the myocardium. The clinical utility of hsTnT and NT-proBNP in heart failure and CAD assessment has been well-validated, with hsTNT and NT-proBNP more frequently linked to the development of heart failure in CKD patients than CAD [5,33]. Arterial stiffness can intensify left ventricle afterload and exacerbate cardiac dysfunction over time [34], so the association between PWV and hsTnT and/or NT-proBNP has been discussed in several studies [35,36,37,38,39]. In the Atherosclerosis Risk in Communities Study, Liu et al. [37] reported a direct association between cfPWV measures and CV biomarkers in 3348 patients that were stronger for NT-proBNP than for hsTnT in the older population without previous CVD. However, for hemodialysis patients, Otsuka et al. [36] demonstrated that hsTnT, left ventricle ejection fraction < 50%, and baPWV were more powerful predictors of MACE than baPWV alone in univariate analysis. In the present study, the significantly direct association between baPWV and hsTnT remained after adjusting for confounders in the multivariable-adjusted model.
Galectin-3 is a β-galactoside-binding lectin (29–35 kDa) primarily released by activated macrophages, as well as other inflammatory cells in CV and renal systems [40,41,42]. A direct relationship between Galectin-3 and arterial stiffness, assessed by cfPWV, among hemodialysis patients was validated by Zhang et al. [12] after accounting for single pool Kt/V (an indicator of hemodialysis influence) in a multivariable regression model. Several theories have been proposed about the possible mechanisms. Galectin-3 is involved in lipid accumulation and chronic inflammation, which can be worsened in regular hemodialysis patients leading to arterial stiffness and atherosclerosis [43,44]. In our study, the direct association between baPWV and Galectin-3 was also examined in the multivariable-adjusted model, but the independent characteristics of Galectin-3 (p = 0.1) in predicting CV risk among hemodialysis patients were not significant.
Another novel CV biomarker is Cathepsin D, a cysteine protease enzyme released by macrophages, vascular smooth muscle cells, and endothelial cells in atherosclerotic plaques [45,46]. The secretion of Cathepsin D can be enhanced by inflammatory triggers into the extracellular matrix and can modify LDL by its hydrolytic ability to facilitate foam cell accumulation in the intima of the artery [47,48]. Cathepsin D is also involved in macrophage/foam cell apoptosis, causing plaque instability, an important determinant of MACE [49]. The pathological role of Cathepsin D in contributing to carotid intima–media thickness (CIMT) has been proposed by previous studies, and a direct correlation was reported in nondiabetic hypertensive patients [50] and hemodialysis patients [16]. Li et al. [51] indicated that both CIMT and PWV are predictors of developing atherosclerosis in hemodialysis patients, explaining the significant direct association between baPWV and Cathepsin D after multivariable-adjusted model analysis in the present study.
The pioneered findings of the present study suggest that using baPWV combined with classical CV biomarkers such as hsTnT and/or novel biomarkers such as Cathepsin D may provide more predictive information on CV morbidity and mortality in the ESRD population requiring regular hemodialysis. Moreover, baPWV, hsTnT, and Cathepsin D can also be beneficial in managing chronic hemodialysis patients as therapeutic indicators of ameliorating arterial stiffness. Large population trials are required in the future to determine if combining baPWV, hsTnT, and Cathepsin D improve CV risk prediction and reduce MACEs in ESRD patients on hemodialysis.
This study has several limitations. First, a causal association could not be determined due to the cross-sectional study design, so longitudinal investigations should be performed. Second, this study was limited to a single regional hospital, restricting the number of patients and their selection. Furthermore, because peritoneal dialysis patients were not included in this study, the findings may not be relevant to peritoneal dialysis patients. Third, the baPWV and bone turnover biomarkers were only measured once, which might have resulted in misclassification. Fourth, not all potential variables, such as food habits, genetic factors, medicines, and whole blood viscosity, were included in this study. For whole blood viscosity, in particular, Kobayashi et al. [52] applied the transit time of heparinized whole blood through slit pores as a whole blood viscosity indicator with baPWV to suggest the role of blood rheology in the progression of atherosclerosis in hemodialysis patients. Years later, Jung et al. [53] validated the impact of changes in systolic and diastolic whole blood viscosity on the overall survival of ESRD patients during hemodialysis. We will refer to published measurements to investigate the association between blood viscosity and CV biomarkers in hemodialysis patients in our future studies.
5. Conclusions
This study demonstrated a significant direct association between baPWV and CV biomarkers, especially hsTnT and Cathepsin D, in hemodialysis patients. The clinical use of baPWV combined with these CV biomarkers may serve as effective CV risk predictors or therapeutic indicators for the ESRD population undergoing regular hemodialysis.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jpm12040636/s1, Supplementary Table S1. List of cardiovascular biomarkers measured in this study. Supplementary Table S2. The relationship between log-transformed brachial-ankle pulse wave velocity and clinical parameters and biochemical blood profiles in the simple linear regression model. Supplementary Table S3. Association between circulating CV biomarker levels (log-transformed) and brachial-ankle pulse wave velocity (log-transformed) in hemodialysis participants using the multivariable-adjusted linear regression model with stepwise procedure selected covariates.
Author Contributions
Supervision, P.-H.W. and S.-J.H.; writing—original draft preparation, P.-R.C. and P.-H.W.; writing—review and editing, P.-R.C. and P.-H.W.; data curation—P.-H.W., P.-Y.W., T.-H.H., J.-C.H., S.-C.C., S.-C.L., M.-C.K., Y.-W.C., Y.-L.H., J.-M.C. and S.-J.H. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by grants from the Ministry of Science and Technology, Taiwan (MOST 107-2314-B-037-021-MY2, MOST 109-2314-B-037-088), Kaohsiung Medical University Hospital, Taiwan (KMUH102-2R09, KMUH104-4R09, KMUH105-5R16, KMUH109-9R16, KMUH110-0M12, KMUH110-0M13, KMUH-DK(B)110003-1, KMUH-DK(B)110003-3), and Kaohsiung Medical University (KMU-DK(B)110003, KMU-Q108024, NPUST-KMU-111-P001, and NHRIKMU-111-I001-3).
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by Kaohsiung Medical University Hospital (KMUHIRB-E(I)-20160095).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding authors. The data are not publicly available due to privacy issues.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Lv, J.-C.; Zhang, L.-X. Prevalence and Disease Burden of Chronic Kidney Disease. Adv. Exp. Med. Biol. 2019, 1165, 3–15. [Google Scholar] [CrossRef] [PubMed]
- Glassock, R.J.; Warnock, D.G.; Delanaye, P. The global burden of chronic kidney disease: Estimates, variability and pitfalls. Nat. Rev. Nephrol. 2016, 13, 104–114. [Google Scholar] [CrossRef] [PubMed]
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Williams, B. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef] [PubMed]
- Vallianou, N.G.; Mitesh, S.; Gkogkou, A.; Geladari, E. Chronic Kidney Disease and Cardiovascular Disease: Is there Any Relationship? Curr. Cardiol. Rev. 2019, 15, 55–63. [Google Scholar] [CrossRef]
- Provenzano, M.; Andreucci, M.; De Nicola, L.; Garofalo, C.; Battaglia, Y.; Borrelli, S.; Gagliardi, I.; Faga, T.; Michael, A.; Mastroroberto, P.; et al. The Role of Prognostic and Predictive Biomarkers for Assessing Cardiovascular Risk in Chronic Kidney Disease Patients. BioMed Res. Int. 2020, 2020, 2314128. [Google Scholar] [CrossRef] [PubMed]
- Maloberti, A.; Meani, P.; Vallerio, P.; Varrenti, M.; Casadei, F.; Musca, F.; Facchetti, R.; Di Blasio, A.M.; Ravassa, S.; Mancia, G.; et al. Annexin A5 in treated hypertensive patients and its association with target organ damage. J. Hypertens. 2017, 35, 154–161. [Google Scholar] [CrossRef]
- Maloberti, A.; Farina, F.; Carbonaro, M.; Piccinelli, E.; Bassi, I.; Pansera, F.; Grassi, G.; Mancia, G.; Palestini, P.; Giannattasio, C. In healthy normotensive subjects age and blood pressure better predict subclinical vascular and cardiac organ damage than atherosclerosis biomarkers. Blood Press. 2018, 27, 262–270. [Google Scholar] [CrossRef]
- Yilmaz, M.I.; Siriopol, D.; Saglam, M.; Kurt, Y.G.; Unal, H.U.; Eyileten, T.; Gok, M.; Cetinkaya, H.; Oguz, Y.; Sari, S.; et al. Plasma endocan levels associate with inflammation, vascular abnormalities, cardiovascular events, and survival in chronic kidney disease. Kidney Int. 2014, 86, 1213–1220. [Google Scholar] [CrossRef] [Green Version]
- Pawlak, K.; Mysliwiec, M.; Pawlak, D. Endocan—The new endothelial activation marker independently associated with soluble endothelial adhesion molecules in uraemic patients with cardiovascular disease. Clin. Biochem. 2015, 48, 425–430. [Google Scholar] [CrossRef]
- Matsui, M.; Samejima, K.-I.; Takeda, Y.; Tanabe, K.; Morimoto, K.; Okamoto, K.; Tagawa, M.; Onoue, K.; Okayama, S.; Kawata, H.; et al. Prognostic Impact of Placental Growth Factor on Mortality and Cardiovascular Events in Dialysis Patients. Am. J. Nephrol. 2015, 42, 117–125. [Google Scholar] [CrossRef]
- Matsui, M.; Uemura, S.; Takeda, Y.; Samejima, K.-I.; Matsumoto, T.; Hasegawa, A.; Tsushima, H.; Hoshino, E.; Ueda, T.; Morimoto, K.; et al. Placental Growth Factor as a Predictor of Cardiovascular Events in Patients with CKD from the NARA-CKD Study. J. Am. Soc. Nephrol. 2015, 26, 2871–2881. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, Q.; Yin, K.; Zhu, M.; Lin, X.; Fang, Y.; Lu, J.; Li, Z.; Ni, Z. Galectin-3 is associated with arterial stiffness among hemodialysis patients. Biomarkers Med. 2019, 13, 437–443. [Google Scholar] [CrossRef] [PubMed]
- Hsu, B.-G.; Wang, C.-H.; Lai, Y.-H.; Tsai, J.-P. Serum Galectin-3 Level Is Positively Associated with Endothelial Dysfunction in Patients with Chronic Kidney Disease Stage 3 to 5. Toxins 2021, 13, 532. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.; Ji, Y.; Ju, H.; Chen, H.; Sun, M. Circulating Fetuin-A and Risk of All-Cause Mortality in Patients with Chronic Kidney Disease: A Systematic Review and Meta-Analysis. Front. Physiol. 2019, 10, 966. [Google Scholar] [CrossRef] [PubMed]
- Sevinc, C.; Yilmaz, G.; Ustundag, S. The relationship between calcification inhibitor levels in chronic kidney disease and the development of atherosclerosis. Ren. Fail. 2021, 43, 1349–1358. [Google Scholar] [CrossRef]
- Moallem, S.A.; Nazemian, F.; Eliasi, S.; Alamdaran, S.A.; Shamsara, J.; Mohammadpour, A.H. Correlation between cathepsin D serum concentration and carotid intima-media thickness in hemodialysis patients. Int. Urol. Nephrol. 2010, 43, 841–848. [Google Scholar] [CrossRef]
- Yamamoto-Nonaka, K.; Koike, M.; Asanuma, K.; Takagi, M.; Trejo, J.A.O.; Seki, T.; Hidaka, T.; Ichimura, K.; Sakai, T.; Tada, N.; et al. Cathepsin D in Podocytes Is Important in the Pathogenesis of Proteinuria and CKD. J. Am. Soc. Nephrol. 2016, 27, 2685–2700. [Google Scholar] [CrossRef] [Green Version]
- Heerspink, H.J.L.; Parving, H.-H.; Andress, D.L.; Bakris, G.; Correa-Rotter, R.; Hou, F.-F.; Kitzman, D.W.; Kohan, D.; Makino, H.; McMurray, J.J.V.; et al. Atrasentan and renal events in patients with type 2 diabetes and chronic kidney disease (SONAR): A double-blind, randomised, placebo-controlled trial. Lancet 2019, 393, 1937–1947. [Google Scholar] [CrossRef]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.; Coca, A.; De Simone, G.; Dominiczak, A.; et al. 2018 Practice Guidelines for the management of arterial hypertension of the European Society of Hypertension and the European Society of Cardiology: ESH/ESC Task Force for the Management of Arterial Hypertension. J. Hypertens. 2018, 36, 2284–2309. [Google Scholar] [CrossRef] [Green Version]
- Ohkuma, T.; Ninomiya, T.; Tomiyama, H.; Kario, K.; Hoshide, S.; Kita, Y.; Yamashita, T. Brachial-Ankle Pulse Wave Velocity and the Risk Prediction of Cardiovascular Disease: An Individual Participant Data Meta-Analysis. Hypertension 2017, 69, 1045–1052. [Google Scholar] [CrossRef]
- Avramovski, P.; Janakievska, P.; Sotiroski, K.; Zafirova-Ivanovska, B.; Sikole, A. Aortic pulse wave velocity is a strong predictor of all-cause and cardiovascular mortality in chronic dialysis patients. Ren Fail. 2014, 36, 176–186. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Townsend, R.R. Arterial Stiffness in CKD: A Review. Am. J. Kidney Dis. 2019, 73, 240–247. [Google Scholar] [CrossRef] [PubMed]
- Hyun, Y.Y.; Kim, H.; Oh, K.-H.; Ahn, C.; Park, S.K.; Chae, N.W.; Han, S.H.; Kim, Y.-S.; Lee, S.W.; Kim, C.S.; et al. Arterial Stiffness as a Risk Factor for Subclinical Coronary Artery Calcification in Predialysis Chronic Kidney Disease: From the KNOW-CKD Study. Kidney Blood Press. Res. 2019, 44, 426–434. [Google Scholar] [CrossRef] [PubMed]
- Tripepi, G.; Agharazii, M.; Pannier, B.; D’Arrigo, G.; Mallamaci, F.; Zoccali, C.; London, G. Pulse Wave Velocity and Prognosis in End-Stage Kidney Disease. Hypertension 2018, 71, 1126–1132. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.H.; Lin, Y.T.; Wu, P.Y.; Huang, J.C.; Chen, S.C.; Chang, J.M.; Chen, H.C. A Low Ankle-Brachial Index and High Brachial-Ankle Pulse Wave Velocity Are Associated with Poor Cognitive Function in Patients Undergoing Hemodialysis. Dis. Markers 2019, 2019, 9421352. [Google Scholar] [CrossRef] [PubMed]
- Zoccali, C.; Mallamaci, F.; Tripepi, G. Traditional and emerging cardiovascular risk factors in end-stage renal disease. Kidney Int. 2003, 63, S105–S110. [Google Scholar] [CrossRef] [Green Version]
- Cecelja, M.; Chowienczyk, P. Role of arterial stiffness in cardiovascular disease. JRSM Cardiovasc. Dis. 2012, 1, 1–10. [Google Scholar] [CrossRef]
- Sugawara, J.; Hayashi, K.; Yokoi, T.; Cortez-Cooper, M.Y.; DeVan, A.E.; Anton, M.A.; Tanaka, H. Brachial-ankle pulse wave velocity: An index of central arterial stiffness? J. Hum. Hypertens. 2005, 19, 401–406. [Google Scholar] [CrossRef]
- Vlachopoulos, C.; Aznaouridis, K.; Terentes-Printzios, D.; Ioakeimidis, N.; Stefanadis, C. Prediction of cardiovascular events and all-cause mortality with brachial-ankle elasticity index: A systematic review and meta-analysis. Hypertension 2012, 60, 556–562. [Google Scholar] [CrossRef] [Green Version]
- Fujiwara, Y.; Chaves, P.; Takahashi, R.; Amano, H.; Kumagai, S.; Fujita, K.; Yoshida, H.; Wang, D.G.; Varadhan, R.; Uchida, H.; et al. Relationships between brachial-ankle pulse wave velocity and conventional atherosclerotic risk factors in community-dwelling people. Prev. Med. 2004, 39, 1135–1142. [Google Scholar] [CrossRef]
- Kuang, D.-W.; Li, C.-L.; Kuok, U.-I.; Cheung, K.; Lio, W.-I.; Xin, J. Risk factors associated with brachial–ankle pulse wave velocity among peritoneal dialysis patients in Macao. BMC Nephrol. 2012, 13, 143. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, C.S.; Bae, E.H.; Ma, S.K.; Han, S.H.; Lee, K.-B.; Lee, J.; Oh, K.-H.; Chae, D.W.; Kim, S.W. Representatives of the KNOW-CKD Study Group Chronic Kidney Disease-Mineral Bone Disorder in Korean Patients: A Report from the KoreaN Cohort Study for Outcomes in Patients With Chronic Kidney Disease (KNOW-CKD). J. Korean Med. Sci. 2017, 32, 240–248. [Google Scholar] [CrossRef] [PubMed]
- Matsushita, K.; Sang, Y.; Ballew, S.H.; Astor, B.C.; Hoogeveen, R.C.; Solomon, S.D.; Coresh, J. Cardiac and kidney markers for cardiovascular prediction in individuals with chronic kidney disease: The Atherosclerosis Risk in Communities study. Arter. Thromb. Vasc. Biol. 2014, 34, 1770–1777. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roman, M.J.; Ganau, A.; Saba, P.S.; Pini, R.; Pickering, T.G.; Devereux, R.B. Impact of Arterial Stiffening on Left Ventricular Structure. Hypertension 2000, 36, 489–494. [Google Scholar] [CrossRef] [Green Version]
- Feistritzer, H.-J.; Reinstadler, S.J.; Klug, G.; Kremser, C.; Rederlechner, A.; Mair, J.; Müller, S.; Franz, W.-M.; Metzler, B. N-terminal pro-B-type natriuretic peptide is associated with aortic stiffness in patients presenting with acute myocardial infarction. Eur. Heart J. Acute Cardiovasc. Care 2016, 5, 560–567. [Google Scholar] [CrossRef]
- Otsuka, K.; Nakanishi, K.; Shimada, K.; Nakamura, H.; Inanami, H.; Nishioka, H.; Yoshiyama, M. Ankle-brachial index, arterial stiffness, and biomarkers in the prediction of mortality and outcomes in patients with end-stage kidney disease. Clin. Cardiol. 2019, 42, 656–662. [Google Scholar] [CrossRef] [Green Version]
- Liu, S.; Kim, E.D.; Wu, A.; Meyer, M.L.; Cheng, S.; Hoogeveen, R.C.; Ballantyne, C.M.; Tanaka, H.; Heiss, G.; Selvin, E.; et al. Central and peripheral pulse wave velocity and subclinical myocardial stress and damage in older adults. PLoS ONE 2019, 14, e0212892. [Google Scholar] [CrossRef]
- Hitsumoto, T. Relationships between the arterial velocity pulse index as a novel marker of atherosclerosis and biomarkers of cardiac or renal condition in patients with type 2 diabetes mellitus. Diabetol. Int. 2017, 9, 48–55. [Google Scholar] [CrossRef]
- Odaira, M.; Tomiyama, H.; Matsumoto, C.; Yoshida, M.; Shiina, K.; Nagata, M.; Yamashina, A. Strength of relationships of the pulse wave velocity and central hemodynamic indices with the serum N-terminal fragment B-type natriuretic peptide levels in men: A worksite cohort study. Circ. J. 2012, 76, 1928–1933. [Google Scholar] [CrossRef] [Green Version]
- Yang, R.Y.; Rabinovich, G.A.; Liu, F.T. Galectins: Structure, function and therapeutic potential. Expert Rev. Mol. Med. 2008, 10, e17. [Google Scholar] [CrossRef]
- Sharma, U.C.; Pokharel, S.; Van Brakel, T.J.; van Berlo, J.; Cleutjens, J.P.M.; Schroen, B.; André, S.; Crijns, H.J.G.M.; Gabius, H.-J.; Maessen, J.; et al. Galectin-3 Marks Activated Macrophages in Failure-Prone Hypertrophied Hearts and Contributes to Cardiac Dysfunction. Circulation 2004, 110, 3121–3128. [Google Scholar] [CrossRef] [PubMed]
- Dong, R.; Zhang, M.; Hu, Q.; Zheng, S.; Soh, A.; Zheng, Y.; Yuan, H. Galectin-3 as a novel biomarker for disease diagnosis and a target for therapy (Review). Int. J. Mol. Med. 2018, 41, 599–614. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Madrigal-Matute, J.; Lindholt, J.S.; Fernandez-Garcia, C.E.; Martin, A.B.; Burillo, E.; Zalba, G.; Beloqui, O.; Llamas-Granda, P.; Ortiz, A.; Egido, J.; et al. Galectin-3, a Biomarker Linking Oxidative Stress and Inflammation with the Clinical Outcomes of Patients with Atherothrombosis. J. Am. Heart Assoc. 2014, 3, e000785. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Locatelli, F.; Canaud, B.; Eckardt, K.-U.; Stenvinkel, P.; Wanner, C.; Zoccali, C. Oxidative stress in end-stage renal disease: An emerging threat to patient outcome. Nephrol. Dial. Transplant. 2003, 18, 1272–1280. [Google Scholar] [CrossRef]
- Barderas, M.G.; Dardé, V.M.; de la Cuesta, F.; Martin-Ventura, J.L.; Blanco-Colio, L.M.; Jiménez-Narcher, J.; Vivanco, F. Proteomic analysis of circulating monocytes identifies cathepsin D as a potential novel plasma marker of acute coronary syndromes. Clin. Med. Cardiol. 2008, 2, 191–200. [Google Scholar] [CrossRef]
- Liu, J.; Sukhova, G.K.; Sun, J.-S.; Xu, W.-H.; Libby, P.; Shi, G.-P. Lysosomal Cysteine Proteases in Atherosclerosis. Arter. Thromb. Vasc. Biol. 2004, 24, 1359–1366. [Google Scholar] [CrossRef] [Green Version]
- Benes, P.; Vetvicka, V.; Fusek, M. Cathepsin D—Many functions of one aspartic protease. Crit. Rev. Oncol. Hematol. 2008, 68, 12–28. [Google Scholar] [CrossRef] [Green Version]
- Hakala, J.K.; Oksjoki, R.; Laine, P.; Du, H.; Grabowski, G.A.; Kovanen, P.T.; Pentikaïnen, M.O. Lysosomal Enzymes Are Released From Cultured Human Macrophages, Hydrolyze LDL In Vitro, and Are Present Extracellularly in Human Atherosclerotic Lesions. Arter. Thromb. Vasc. Biol. 2003, 23, 1430–1436. [Google Scholar] [CrossRef] [Green Version]
- Li, W.; Yuan, X.-M. Increased Expression and Translocation of Lysosomal Cathepsins Contribute to Macrophage Apoptosis in Atherogenesis. Ann. N. Y. Acad. Sci. 2004, 1030, 427–433. [Google Scholar] [CrossRef]
- Özkayar, N.; Akyel, F.; Barça, A.N.; Pişkinpaşa, S.V.; Turhan, T.; Ateş, I.; DeDe, F. The relation between serum cathepsin D level and carotid intima-media thickness in nondiabetic hypertensive patients. Turk. J. Med Sci. 2016, 46, 13–17. [Google Scholar] [CrossRef]
- Li, Z.; Qin, Y.; Du, L.; Luo, X. An improvement of carotid intima-media thickness and pulse wave velocity in renal transplant recipients. BMC Med. Imaging 2018, 18, 23. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, S.; Okamoto, K.; Maesato, K.; Moriya, H.; Ohtake, T. Important role of blood rheology in atherosclerosis of patients with hemodialysis. Hemodial. Int. 2005, 9, 268–274. [Google Scholar] [CrossRef] [PubMed]
- Jung, J.H.; Chae, Y.J.; Lee, D.H.; Cho, Y.I.; Ko, M.M.; Park, S.K.; Kim, W. Changes in whole blood viscosity during hemodialysis and mortality in patients with end-stage renal disease. Clin. Hemorheol. Microcirc. 2017, 65, 285–297. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).