Abstract
Background/Objectives: Sepsis is a leading cause of mortality. The AST/ALT ratio may serve as a valuable marker for prediction in patients with various diseases. This study analyzed the prognostic value of this ratio in patients with sepsis. Methods: A retrospective analysis was performed on data from a prospective registry of septic shock patients, collected across multiple centers from October 2015 to December 2022. The main outcome of interest was mortality within 28 days. We evaluated the predictive accuracy of 28-day mortality for variables with the Sequential Organ Failure Assessment (SOFA) score, aspartate transaminase (AST) levels, alanine transaminase (ALT) levels, the AST/ALT ratio, and the combination of the SOFA + AST/ALT ratio using the area under the receiver operating characteristics curve (AUROC). A Kaplan–Meier curve was used to compare the 28-day mortality between the AST/ALT subgroups (≥1.84 and <1.84). Stepwise multivariable Cox proportional hazards analyses were performed to determine the association between 28-day mortality and an AST/ALT ratio ≥ 1.84. Results: The AST/ALT ratio had a significantly higher discriminatory ability for predicting 28-day mortality compared to either AST or ALT. In addition, combining the AST/ALT ratio with the SOFA score improved the predictive accuracy compared to the SOFA alone. A multivariable Cox regression analysis demonstrated that an AST/ALT ratio ≥ 1.84 was associated with a higher risk of death within 28 days. Conclusions: The AST/ALT ratio at emergency department admission in sepsis patients is associated with 28-day mortality and, when combined with the SOFA score, provides additional prognostic information with moderate accuracy.
1. Introduction
Sepsis is a life-threatening state caused by a dysregulated response of the host to infection. When it is accompanied by circulatory and cellular/metabolic abnormalities, it is classified as septic shock, which often results in increased mortality [1]. Sepsis remains one of the significant contributors to mortality in emergency departments (EDs) and intensive care units (ICUs) [2,3]. In 2017, there were an estimated 48.9 million new cases of sepsis globally, resulting in approximately 11 million deaths. This represented 19.7% of all deaths worldwide [4].
Sepsis-associated organ dysfunction is commonly assessed using the Sequential Organ Failure Assessment (SOFA) score. This scoring system evaluates clinical indicators such as the mean arterial pressure (MAP), urine output, Glasgow Coma Scale (GCS), and laboratory test results, including the PaO2, platelet count, and levels of creatinine and bilirubin [1,5]. A SOFA score of 2 or more points is linked to a hospital mortality rate greater than 10% [1]. Among the organs assessed by this scoring system, the liver (the largest gland in the body) plays a critical role in maintaining metabolic and immune system homeostasis [6]. In particular, when complications such as liver dysfunction or failure occur as a result of sepsis, they can significantly influence the prognosis and mortality of the disease [6,7].
One factor linked to liver damage is the aspartate aminotransferase (AST)/alanine aminotransferase (ALT) ratio, first introduced by Fernando De Ritis in 1957. The ratio is correlated with various liver diseases [8,9] and is significantly associated with several conditions, including malignant tumors, stroke, myocardial infarction, limb ischemia, renal failure, and respiratory failure, serving as both a prognostic and predictive marker of poor outcomes [10,11,12,13,14]. Furthermore, it may be a valuable prognostic factor in patients with sepsis [15,16]. However, most studies have been single-center investigations with relatively small sample sizes [15,16].
Therefore, in this study, we included a large cohort of patients from multiple centers to analyze whether the AST/ALT ratio offers meaningful prognostic value in sepsis patients and whether these findings can be generalized.
2. Materials and Methods
2.1. Study Design
Using a dataset derived from the multicenter Korean Shock Society (KoSS) registry, which prospectively collected data between October 2015 and December 2022, we conducted a retrospective observational study. The KoSS operates as a nationwide collaborative network aimed at enhancing sepsis diagnosis and treatment strategies. A prospective registry was initiated in October 2015 to collect standardized data on the septic shock patients seen at the EDs of 12 university-affiliated hospitals in South Korea [17,18,19]. The eligible participants were adults aged over 18 years who had either suspected or confirmed infection, along with signs of hypoperfusion or refractory hypotension [20]. As the implementation of the KoSS registry began before the publication of the Sepsis-3 criteria, this inclusion approach was based on the refractory sepsis-induced hypotension or tissue hypoperfusion definition in the 2012 Surviving Sepsis Campaign (SSC) guidelines and was consistently maintained throughout the study period to ensure uniform enrollment [17,21,22]. Hypoperfusion was determined by a lactate level of 4 mmol/L or higher, while refractory hypotension referred to ongoing low blood pressure (MAP < 70 mmHg, SBP < 90 mmHg, or a reduction in SBP > 40 mmHg) following intravenous (IV) fluid replacement (20–30 mL/kg or ≥1 L crystalloid solution) or the need for vasopressor support despite fluid administration [22]. In addition, we separately identified patients who fulfilled the Sepsis-3 criteria of septic shock for the analysis. Septic shock based on the Sepsis-3 criteria was defined as sepsis with sustained hypotension requiring vasopressors to maintain an MAP ≥ 65 mmHg and a serum level of lactate > 2 mmol/L [1]. In addition, all patients were enrolled at the ED upon their initial presentation, prior to any ICU admission.
The exclusion criteria included patients with missing data, those transferred to another hospital, those with do-not-resuscitate orders, those lost to follow-up, and those with liver disease. The ethical approval for this study was granted by the institutional review boards (IRBs) of each participating institution, and informed consent was waived by the IRBs of each participating institution in accordance with ethical regulations. Although the KoSS registry is an ongoing prospective database, this study included only patients enrolled up to December 2022, in accordance with the IRB-approved protocol.
2.2. Data Collection
The KoSS registry includes standardized definitions for 200 variables [23]. The coordinator of each hospital anonymized and gathered data employing standardized web-based reporting forms. The patient enrollment and data collection were carried out jointly by the attending emergency physicians and trained research coordinators at each site. To maintain data integrity, the system automatically screened for extreme or erroneous values. A quality control committee, consisting of emergency medicine specialists, investigators, and regional research coordinators from each participating hospital, was established to consistently monitor and assess the quality of the data.
The following data were extracted from the registry: baseline clinical characteristics, comorbidities, vital signs, severity scores (SOFA score and Acute Physiology and Chronic Health Evaluation [APACHE] II upon enrollment), suspected infection, laboratory findings (white blood cells, hemoglobin, platelet count, sodium, chloride, potassium, creatinine, C-reactive protein [CRP], blood urea nitrogen, procalcitonin, lactate, international normalized ratio [INR], pH, albumin, alanine transaminase [ALT], aspartate transaminase [AST], and AST/ALT ratio), interventions (including renal replacement therapy [RRT], steroid use, and mechanical ventilation [MV]), and outcomes. The laboratory results were based on the initial findings upon the patients’ ED arrival.
The APACHE II score used in this study was the lowest score within 24 h of the ED arrival, and the SOFA score was recorded upon the registry enrollment. Mortality within 28 days served as the primary outcome, whereas secondary outcomes included mortality within 90 days, ICU admission, MV, and RRT within 24 h.
2.3. Statistical Analysis
The continuous variables were summarized as the median and interquartile range (IQR) or the mean and standard deviation, based on the Shapiro–Wilk test results. The categorical variables were presented as counts (percentages) and analyzed using the Fisher’s exact test or the χ2 test. The continuous variables were compared using either the Mann–Whitney U test or the t-test.
We evaluated the AST/ALT ratio, which has been suggested to be a predictor of mortality in sepsis in recent studies, by comparing it with the SOFA score [15,16]. The discriminatory capacity for 28- and 90-day mortality was assessed by comparing the area under the receiver operating characteristic curve (AUROC) for each variable (SOFA, AST, ALT, and AST/ALT ratio) and in combination with the SOFA and the AST/ALT ratio. Specific AUROC values with 95% confidence intervals (CIs) were determined. By using Youden’s index, we identified the optimal cut-off value for the AST/ALT ratio. Based on this cut-off (≥1.84 and <1.84), the patients were grouped into two subgroups.
Kaplan–Meier curves were generated to compare the 28- and 90-day mortality between the AST/ALT subgroups. A stepwise multivariable Cox proportional hazards regression was conducted to assess the association between the AST/ALT ratio (≥1.84) and the primary and secondary outcomes. The proportional hazards assumption for the Cox analysis was evaluated through Schoenfeld residuals. These analyses were also performed in the subgroup of patients with septic shock, as defined by the Sepsis-3 criteria. A two-tailed p-value of less than 0.05 was interpreted as indicating statistical significance.
We used R software (version 4.2.2, The R Foundation, Vienna, Austria) and Python (version 3.12), with libraries such as NumPy (version 2.0.2), Pandas (version 2.2.2), Matplotlib (version 3.10.0), and Seaborn (version 0.13.2) for the data visualization, manipulation, and statistical testing.
3. Results
In total, 8787 subjects were enrolled in the KoSS registry between October 2015 and December 2022. Of these, 4306 patients were excluded due to missing data, 128 were transferred to other hospitals, 176 had do-not-resuscitate orders, 92 were lost to follow-up, and 571 had chronic liver disease. Finally, 4481 patients were included in this study (Figure 1).
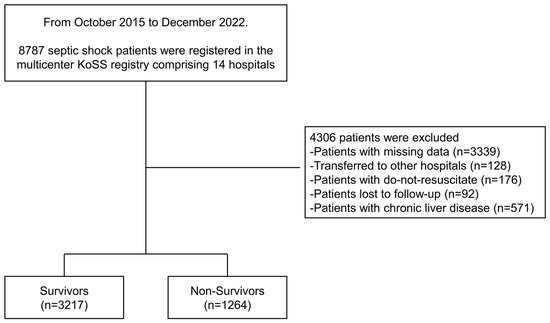
Figure 1.
Study flow of patient inclusion and exclusion criteria.
The baseline characteristics of the 28-day survivor and non-survivor groups are summarized in Table 1. The 28-day mortality rate was 28.2% (n = 1264). The non-survivor group was older than the survivor group (72 years vs. 69 years, p < 0.01), and the proportion of females was lower in the non-survivor group compared to the survivor group (40.7% vs. 44.2%, p = 0.01). Across all patients, hypertension was the most frequent comorbidity.

Table 1.
Comparison of clinical characteristics based on 28-day mortality outcomes.
As shown in Table 2, the proportion of patients with septic shock based on the Sepsis-3 criteria was more frequent in the 28-day non-survivor group (79.1% vs. 59.5%, p < 0.01). Regarding the sepsis-related scores, the SOFA score (median 8 vs. 5, p < 0.01) and the APACHE II score (median 26 vs. 19, p < 0.01) were significantly higher in the non-survivor group. The most prevalent infection source in that group was respiratory infection (36.1%), while intra-abdominal infection was most frequent in the survivor group (33.9%). In the non-survivor group, increased serum levels of lactate (5.2 vs. 2.9 mmol/L, p < 0.01), CRP (17.3 vs. 13.8 mg/dL, p < 0.01), and the AST/ALT ratio (1.91 vs. 1.47, p < 0.01) were observed. In addition, the use of MV and RRT within 24 h was significantly higher in the non-survivor group vs. the survivor group (53.6% vs. 15% and 24.9% vs. 5.8%, respectively; p < 0.01).

Table 2.
Septic shock-related data and laboratory findings according to 28-day mortality.
The discrimination of 28-day mortality was significantly higher using the AST/ALT ratio (AUROC, 0.62; 95% CI, 0.61–0.64) compared to either AST (AUROC, 0.56; 95% CI, 0.54–0.58) or ALT (AUROC, 0.50; 95% CI, 0.48–0.52) (Figure 2A). Furthermore, when combining the AST/ALT ratio with the SOFA score, the AUROC for the SOFA + AST/ALT ratio (AUROC, 0.71; 95% CI, 0.70–0.73) was greater than for the SOFA score alone (AUROC, 0.69; 95% CI, 0.68–0.71). A similar trend was observed for 90-day mortality (Figure 2B).
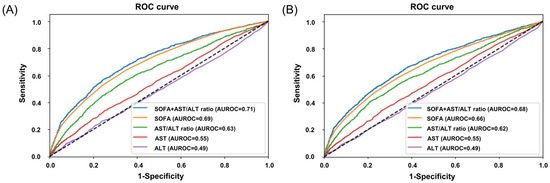
Figure 2.
The ROC curves for 28- and 90-day mortality. (A) The ROC curves for 28-day mortality. The AUROC for the SOFA + AST/ALT ratio is 0.71 (95% CI, 0.69–0.73, p < 0.01), SOFA is 0.69 (95% CI, 0.68–0.71, p < 0.01), AST/ALT ratio is 0.63 (95% CI, 0.61–0.65, p < 0.01), AST is 0.55 (95% CI, 0.53–0.57, p < 0.01), and ALT is 0.49 (95% CI, 0.47–0.51, p = 0.86). (B) The ROC curves for 90-day mortality. The AUROC for the SOFA + AST/ALT ratio is 0.68 (95% CI, 0.67–0.70, p < 0.01), SOFA is 0.66 (95% CI, 0.65–0.68, p < 0.01), AST/ALT ratio is 0.62 (95% CI, 0.60–0.64, p < 0.01), AST is 0.55 (95% CI, 0.53–0.56, p < 0.01), and ALT is 0.49 (95% CI, 0.47–0.50, p = 0.63).
Table 3 presents the hazard ratios for both the primary and secondary outcomes, derived from univariable and multivariable Cox proportional hazards models. In the multivariable analysis, the AST/ALT ratio ≥ 1.84 was significantly associated with 28-day mortality (adjusted HR, 1.46; 95% CI, 1.30–1.64; p < 0.01), 90-day mortality (adjusted HR, 1.33; 95% CI, 1.20–1.46; p < 0.01), MV within 24 h (adjusted HR, 1.28; 95% CI, 1.13–1.43; p < 0.01), and RRT within 24 h (adjusted HR, 1.50; 95% CI, 1.25–1.80; p < 0.01). However, no significant association was found with ICU admission (adjusted HR, 1.01; 95% CI, 0.91–1.11; p = 0.85).

Table 3.
The univariable and multivariable Cox regression analyses of the AST/ALT ratio for predicting primary and secondary outcomes.
Figure 3 shows the survival probability for 28-day and 90-day mortality below and above the cut-off point of the AST/ALT ratio. An AST/ALT ratio ≥ 1.84 was significantly associated with increased 28-day and 90-day mortality (log-rank test, p < 0.01). In the subgroup of patients with septic shock (Sepsis-3 definition), the results of the Cox regression (Table S1), ROC curves (Figure S1), and Kaplan–Meier curves (Figure S2) for 28- and 90-day mortality were comparable to those of the overall cohort (refer to the Supplementary Materials).
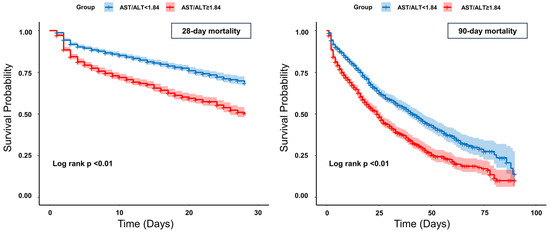
Figure 3.
Kaplan–Meier curves for 28-day and 90-day mortality.
4. Discussion
We analyzed the AST/ALT ratio in sepsis patients and found that an AST/ALT ratio ≥ 1.84 is associated with both 28- and 90-day mortality. Furthermore, combining the AST/ALT ratio with the SOFA score improved the prognostic value, although the predictive accuracy of both the AST/ALT ratio alone and in combination with the SOFA score remained moderate. Previous studies have evaluated various tools for predicting mortality, including the Modified Early Warning Score, quick Sequential Organ Failure Assessment, National Early Warning Score, and Universal Vital Assessment. Depending on the study cohort, these tools have demonstrated poor to moderate predictive performance for mortality [24,25,26]. In this context, the moderate performance of the combined AST/ALT ratio and SOFA score could still be valuable for diagnosis and prognosis prediction in sepsis patients. Our findings align with earlier single-center studies that proposed AST/ALT ratio cut-off values of 1.84 and 1.22 for predicting sepsis outcomes [15,16]. To the best of our knowledge, this is the first multi-center study with a large patient cohort to analyze this association.
The liver is essential for a wide range of physiological functions, including detoxification, storage, energy and nutrient regulation, and coagulation, which makes it a key organ in metabolic and immune processes. In sepsis patients, the liver may be damaged by pathogens, toxins, and inflammatory substances, leading to hepatocellular dysfunction, characterized by impaired synthetic and clearance functions. Sepsis-induced liver injury is driven by multiple interconnected mechanisms, including systemic inflammation, oxidative stress, mitochondrial dysfunction, and microvascular hypoperfusion [27]. The activation of Toll-like receptors and NOD-like receptors on Kupffer cells by pathogen-associated molecular patterns leads to the massive production of pro-inflammatory cytokines, resulting in hepatocyte apoptosis and necrosis [27,28]. In addition, oxidative stress, mitochondrial damage, hypoxic hepatitis due to circulatory failure, and bacterial translocation via the gut–liver axis also play critical roles in hepatic injury during sepsis [27,29]. These intertwined processes not only contribute to liver dysfunction but also correlate with increased disease severity and mortality. These damages can result in irreversible hepatocyte injury, contributing to overall liver dysfunction [6]. Such hepatocellular damage leads to the release of AST and ALT into the bloodstream, causing elevated levels of these enzymes. In septic patients, the high metabolic demands for nutrients and oxygen can induce tissue and cellular hypoxia, potentially leading to microcirculatory collapse and tissue ischemia in the liver [16,30].
In a healthy state, the liver cell turnover and enzyme removal from the plasma are balanced. The hepatic AST to ALT ratio is typically approximately 2:1. Given that the half-lives of AST and ALT are 18 and 36 h, respectively, this ratio remains relatively stable. AST is more involved in aerobic glycolysis, while ALT participates in the glucose–alanine cycle and anaerobic metabolism. However, this balance can be disrupted by various factors, including viral hepatitis, alcoholic liver disease, and muscle disorders [8]. Recent studies have suggested that an increased AST/ALT ratio can help predict risk and mortality in cancer patients [31,32,33,34,35]. This increase in cancer is reportedly linked to the Warburg effect, where cancer cells preferentially undergo aerobic glycolysis, increasing the glucose uptake and lactate production even in the presence of oxygen [36]. Similarly, in patients with sepsis, immune system activation causes immune cells like macrophages, dendritic cells, and T cells to shift from oxidative phosphorylation to aerobic glycolysis [37]. Previous studies have also indicated that an elevated AST/ALT ratio is helpful in predicting the prognosis of sepsis patients [15,16]. Our findings suggest that using the AST/ALT ratio offers better discrimination of mortality risk in sepsis patients.
In addition, while ALT is relatively specific to the liver, AST is also found in other tissues, including the heart, skeletal muscle, brain, and kidneys [10,38]. Therefore, an elevated AST/ALT ratio may reflect not only hepatic oxidative stress and mitochondrial injury but also multi-organ damage [39,40,41]. Previous studies have reported that a higher AST/ALT ratio correlates with increased levels of inflammatory markers [42,43]. Systemic inflammatory responses, oxidative stress, mitochondrial dysfunction, and multiple organ failure are all common features observed in patients with severe sepsis [44]. Thus, an elevated AST/ALT ratio may serve as a potential predictor of poor prognosis in sepsis patients.
In this study, it was confirmed that using both the SOFA score and the AST/ALT ratio together provides better discrimination of mortality than using the SOFA score alone. The SOFA score incorporates various clinical indicators, such as the MAP, GCS, and urine output, along with laboratory test results such as the PaO2, platelet count, creatinine, and bilirubin, to provide a comprehensive assessment of organ function [1]. Among these, bilirubin serves as an indicator of liver damage [1]. Liver damage due to hypoxemia or hypoperfusion caused by sepsis affects bile synthesis, leading to elevated total bilirubin levels [45]. However, liver failure resulting from sepsis does not always lead to simultaneous increases in the serum levels of bilirubin and the AST/ALT ratio [6,46,47]. Therefore, although the SOFA score does not account for the AST/ALT ratio, incorporating this ratio, which can reflect liver dysfunction, may improve the ability to discriminate mortality in sepsis patients, as suggested by our results.
In this study, a cut-off value of 1.84 for the AST/ALT ratio was associated with an increased risk of mortality. Similar findings have been reported in previous studies. For example, one study that analyzed 30-day mortality in sepsis patients suggested a cut-off value of 1.8 [15], while another study, which analyzed 180-day mortality in sepsis patients, proposed a cut-off of 1.22 [16]. This variation in cut-off values is likely due to differences in the time frame of mortality and the study populations, with one study focusing on internal ICU patients and the other on surgical ICU patients. However, the cut-off value of 1.84 identified in this study, which analyzed all sepsis patients admitted to the ED and considered both 28-day and 90-day mortality, appears to be meaningful. In addition, the AST/ALT ratio can increase to ≥2.0 in liver-related conditions such as acute viral hepatitis, alcoholic hepatitis, or fulminant hepatitis [8]. Considering the cut-off values reported in previous sepsis-related studies and the extent of the ratio increases seen in other liver diseases, the 1.84 cut-off value suggested by this study is likely to be clinically significant for the management of sepsis.
This work is significant for the analysis of sepsis and the AST/ALT ratio, enrolling a large cohort of patients across multiple centers. However, several limitations should be considered. First, we did not assess dynamic changes in the AST/ALT ratio during the hospital stay. Nevertheless, the analysis of initial test results at the time of the ED visit provided meaningful insights, suggesting that early ED values can be helpful for prognosis prediction. Future research is needed to examine the dynamic changes in the ratio over time. Second, the exclusion of 3735 patients (42.5%) due to missing data raises the possibility of selection bias. These excluded patients may have differed in their clinical severity or treatment patterns, potentially limiting the generalizability of our findings. Future studies should consider minimizing missing data and evaluating the impact of such exclusions. Third, while our study included data from multiple centers and a large cohort, it was conducted in a single country, which limits the applicability of our findings to populations in other countries or with different ethnic groups. As a result, the generalizability of the findings to other populations may be restricted. To address this, additional large-scale studies involving diverse ethnicities and countries are required, taking these factors into account.
5. Conclusions
A higher AST/ALT ratio at the time of the ED visit in sepsis patients is associated with 28-day and 90-day mortality. Combining the AST/ALT ratio with the SOFA score improves the prognostic value, although the predictive accuracy of both the AST/ALT ratio alone and in combination with the SOFA score remains moderate. Given the multicenter design and large sample size, our findings may have potential generalizability to broader emergency department populations; however, this should be interpreted with caution due to the high rate of patient exclusions and the study’s limitation to a single country and ethnic group.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/diagnostics15141773/s1, Table S1: Univariable and multivariable Cox regression analyses of the AST/ALT ratio for predicting primary and secondary outcomes in Sepsis-3-defined septic shock; Figure S1: ROC curves for 28- and 90-day mortality in septic shock based on the Sepsis-3 criteria; Figure S2: Kaplan-Meier curves for 28-day and 90-day mortality in septic shock based on the Sepsis-3 criteria.
Author Contributions
Conceptualization, G.J.S. and S.H.; methodology, S.C. (Sungwoo Choi); software, S.C. (Sungwoo Choi); validation, S.C. (Sungwoo Choi) and S.H.; formal analysis, S.-H.C. and W.Y.K.; investigation, S.N., S.P.C., T.H.L. and S.C. (Sangchun Choi); resources, S.N., S.P.C., T.H.L. and S.C. (Sangchun Choi); data curation, S.N. and T.H.L.; writing—original draft preparation, S.C. (Sungwoo Choi), S.N. and T.G.S.; writing—review and editing, S.C. (Sungwoo Choi), T.G.S. and S.H.; visualization, S.-H.C. and W.Y.K.; supervision, S.H.; project administration, G.J.S. and T.G.S.; funding acquisition, T.G.S. and S.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by a grant from the Patient-Centered Clinical Research Coordinating Center (PACEN) funded by the Ministry of Health & Welfare, Republic of Korea (grant number: RS-2024-00398566) to T.G.S. This work was supported by the Soonchunhyang University research fund (grant no. 2025-0027).
Institutional Review Board Statement
The study received IRB approval from all participating centers. (1) Asan Medical Center (S2015-1918-0002, 17 November 2015) (2) Gangnam Sacred Heart Hospital (2015-11-142, 26 November 2015) (3) Gangnam Severance Hospital (3-2015-0227, 27 October 2015) (4) Hanyang University Hospital (HYUH 2015-11-013-022, 29 December 2015) (5) Korea University Anam Hospital (HRPC2016-184, 26 November 2015) (6) Korea University Kuro Hospital (KUGH15358-001, 25 February 2016) (7) Samsung Medical Center (SMC2015-09-057-057, 23 October 2015) (8) Seoul National University Hospital (J-1408-003-599, 11 August 2014) (9) Seoul National University Bundang Hospital (B-1409/266-401, 2 September 2014) (10) Severance Hospital (4-2015-0929, 30 November 2015) (11) Seoul National University Boramae Hospital (IRB-16-2014-36, 29 July 2014) (12) Soonchunhyang University Bucheon Hospital (IRB No. 2023-04-019, 16 May 2023).
Informed Consent Statement
Informed consent was waived by each participating center’s institutional review board.
Data Availability Statement
The dataset supporting the findings of this study is available upon reasonable request from the corresponding authors (Tae Gun Shin, drshin88@gmail.com; Tel.: +82-2-3410-2053 and Sangsoo Han, brayden0819@daum.net; Tel.: +82-32-621-5116) or the Korean Shock Society (Koss) (59club@daum.net) upon reasonable request.
Acknowledgments
We sincerely thank the investigators of the Korean Shock Society (KoSS) for their contributions to patient enrollment, data collection, and maintenance of the registry. (1) Korea University Anam Hospital: Juhyun Song, Kap Su Han. (2) Samsung Medical Center: Sung Yeon Hwang, Gun Tak Lee. (3) Gangnam Severance Hospital: Taeyoung Kong, Eunah Han. (4) Asan Medical Center: Seung Mok Ryoo, Sang-Min Kim. (5) Korea University Guro Hospital: Sung-Joon Park. (6) Severance Hospital: Jin Ho Beom, Yoo Seok Park. (7) Hanyang University Seoul Hospital: Byuk Sung Ko. (8) Kyung Hee University Hospital: Han Sung Choi, Woon Yong Kwon, Seok Hun Ko, Ki Young Jeong. (9) Seoul National University Hospital: Yoon Sun Jung, Taegyun Kim. (10) Seoul National University Bundang Hospital: You Hwan Jo, Ji Eun Hwang. (11) Hallym University Kangnam Sacred Heart Hospital: Gu Hyun Kang. (12) Chungnam National University Hospital: Hong Joon Ahn. (13) CHA Gumi Medical Center: Kihwan Choi. (14) Seoul St. Mary’s Hospital, College of Medicine: Hyo Jin Bang. (15) Dong-A University Hospital: Jinwoo Jeoung, Min Joon Seo. (16) Ajou University Hospital: Heewon Yang. (17) Chung-Ang University Hospital: Chiwon Ahn. (18) Hanyang University Guri Hospital: Changsun Kim, Hyungoo Shin. (19) Seoul Metropolitan Government–Seoul National University Boramae Medical Center: Jonghwan Shin, Hui Jai Lee. (20) Korea University Ansan Hospital: Hanjin Cho, Sejoong Ahn. (21) CHA Bundang Medical Center: Kyuseok Kim. We also thank Ji Eun Moon (Department of Biostatistics, Clinical Trial Center, Soonchunhyang University Bucheon Hospital) for statistical consultation.
Conflicts of Interest
The authors report no potential conflicts of interest.
Abbreviations
The abbreviations listed below are used in this paper:
| AST | Aspartate Transaminase |
| ALT | Alanine Transaminase |
| SOFA | Sequential Organ Failure Assessment |
| APACHE II | Acute Physiology and Chronic Health Evaluation II |
| CRP | C-reactive Protein |
| INR | International Normalized Ratio |
| MV | Mechanical Ventilation |
| RRT | Renal Replacement Therapy |
| ED | Emergency Department |
| ICU | Intensive Care Unit |
| KoSS | Korean Shock Society |
| MAP | Mean Arterial Pressure |
| GCS | Glasgow Coma Scale |
| IV | Intravenous |
| HR | Hazard Ratio |
| AUROC | Area Under the Receiver Operating Characteristics Curve |
| IQR | Interquartile Range |
| IRB | Institutional Review Board |
| SBP | Systolic Blood Pressure |
| CI | Confidence Interval |
References
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.-D.; Coopersmith, C.M.; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef] [PubMed]
- Namgung, M.; Ahn, C.; Park, Y.; Kwak, I.-Y.; Lee, J.; Won, M. Mortality among adult patients with sepsis and septic shock in Korea: A systematic review and meta-analysis. Clin. Exp. Emerg. Med. 2023, 10, 157–171. [Google Scholar] [CrossRef] [PubMed]
- Suh, G.J.; Shin, T.G.; Kwon, W.Y.; Kim, K.; Jo, Y.H.; Choi, S.-H.; Chung, S.P.; Kim, W.Y. Hemodynamic management of septic shock: Beyond the Surviving Sepsis Campaign guidelines. Clin. Exp. Emerg. Med. 2023, 10, 255–264. [Google Scholar] [CrossRef] [PubMed]
- Rudd, K.E.; Johnson, S.C.; Agesa, K.M.; Shackelford, K.A.; Tsoi, D.; Kievlan, D.R.; Colombara, D.V.; Ikuta, K.S.; Kissoon, N.; Finfer, S.; et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: Analysis for the Global Burden of Disease Study. Lancet 2020, 395, 200–211. [Google Scholar] [CrossRef]
- Vincent, J.L.; Moreno, R.; Takala, J.; Willatts, S.; De Mendonça, A.; Bruining, H.; Reinhart, C.K.; Suter, P.M.; Thijs, L.G. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. Intensive Care Med. 1996, 22, 707–710. [Google Scholar] [CrossRef]
- Yan, J.; Li, S.; Li, S. The role of the liver in sepsis. Int. Rev. Immunol. 2014, 33, 498–510. [Google Scholar] [CrossRef]
- Canabal, J.M.; Kramer, D.J. Management of sepsis in patients with liver failure. Curr. Opin. Crit. Care 2008, 14, 189–197. [Google Scholar] [CrossRef]
- Botros, M.; Sikaris, K.A. The De Ritis ratio: The test of time. Clin. Biochem. Rev. 2013, 34, 117–130. [Google Scholar]
- De Ritis, F.; Coltorti, M.; Giusti, G. An enzymic test for the diagnosis of viral hepatitis: The transaminase serum activities. Clin. Chim. Acta 1957, 2, 70–74. [Google Scholar] [CrossRef]
- Gao, F.; Chen, C.; Lu, J.; Zheng, J.; Ma, X.-C.; Yuan, X.-Y.; Huo, K.; Han, J.-F. De Ritis ratio (AST/ALT) as an independent predictor of poor outcome in patients with acute ischemic stroke. Neuropsychiatr. Dis. Treat. 2017, 13, 1551–1557. [Google Scholar] [CrossRef]
- Pilarczyk, K.; Carstens, H.; Heckmann, J.; Canbay, A.; Koch, A.; Pizanis, N.; Jakob, H.; Kamler, M. The aspartate transaminase/alanine transaminase (DeRitis) ratio predicts mid-term mortality and renal and respiratory dysfunction after left ventricular assist device implantation. Eur. J. Cardio-Thorac. Surg. 2017, 52, 781–788. [Google Scholar] [CrossRef] [PubMed]
- Rief, P.; Pichler, M.; Raggam, R.; Hafner, F.; Gerger, A.; Eller, P.; Fuchs, D.; Strasser, T. The AST/ALT (De-Ritis) ratio: A novel marker for critical limb ischemia in peripheral arterial occlusive disease patients. Medicine 2016, 95, e3843. [Google Scholar] [CrossRef] [PubMed]
- Steininger, M.; Winter, M.-P.; Reiberger, T.; Koller, L.; El-Hamid, F.; Forster, S.; Schnaubelt, S.; Hengstenberg, C.; Distelmaier, K.; Goliasch, G.; et al. De-Ritis Ratio Improves Long-Term Risk Prediction after Acute Myocardial Infarction. J. Clin. Med. 2018, 7, 474. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Chen, L.; Wang, Y.; Tan, W.; Huang, Z. Prognostic value of aspartate transaminase to alanine transaminase (De Ritis) ratio in solid tumors: A pooled analysis of 9400 patients. OncoTargets Ther. 2019, 12, 5201–5213. [Google Scholar] [CrossRef]
- Schupp, T.; Weidner, K.; Rusnak, J.; Jawhar, S.; Forner, J.; Dulatahu, F.; Brück, L.M.; Hoffmann, U.; Bertsch, T.; Weiß, C.; et al. Diagnostic and prognostic value of the AST/ALT ratio in patients with sepsis and septic shock. Scand. J. Gastroenterol. 2023, 58, 392–402. [Google Scholar] [CrossRef]
- Zhao, P.-Y.; Yao, R.-Q.; Ren, C.; Li, S.-Y.; Li, Y.-X.; Zhu, S.-Y.; Yao, Y.-M.; Du, X.-H. De Ritis ratio as a significant prognostic factor in patients with sepsis: A retrospective analysis. J. Surg. Res. 2021, 264, 375–385. [Google Scholar] [CrossRef]
- Park, H.; Shin, T.G.; Kim, W.Y.; Jo, Y.H.; Hwang, Y.J.; Choi, S.-H.; Lim, T.H.; Han, K.S.; Shin, J.; Suh, G.J.; et al. A quick Sequential Organ Failure Assessment–negative result at triage is associated with low compliance with sepsis bundles: A retrospective analysis of a multicenter prospective registry. Clin. Exp. Emerg. Med. 2022, 9, 84–92. [Google Scholar] [CrossRef]
- Lee, H.J.; Ko, B.S.; Ryoo, S.M.; Han, E.; Suh, G.J.; Choi, S.-H.; Chung, S.P.; Lim, T.H.; Kim, W.Y.; Kwon, W.Y.; et al. Modified cardiovascular SOFA score in sepsis: Development and internal and external validation. BMC Med. 2022, 20, 263. [Google Scholar] [CrossRef]
- You, J.S.; Park, Y.S.; Chung, S.P.; Lee, H.S.; Jeon, S.; Kim, W.Y.; Shin, T.G.; Jo, Y.H.; Kang, G.H.; Choi, S.H.; et al. Relationship between time of emergency department admission and adherence to the Surviving Sepsis Campaign bundle in patients with septic shock. Crit. Care 2022, 26, 43. [Google Scholar] [CrossRef]
- Peake, S.L.; Delaney, A.; Bailey, M.; Bellomo, R.; Cameron, P.A.; Cooper, D.J.; Higgins, A.M.; Holdgate, A.; Howe, B.D.; Webb, S.A.; et al. Goal-directed resuscitation for patients with early septic shock. N. Engl. J. Med. 2014, 371, 1496–1506. [Google Scholar]
- Ryoo, S.M.; Kang, G.H.; Shin, T.G.; Hwang, S.Y.; Kim, K.; Jo, Y.H.; Park, Y.S.; Choi, S.-H.; Yoon, Y.H.; Kwon, W.Y.; et al. Clinical outcome comparison of patients with septic shock defined by the new sepsis-3 criteria and by previous criteria. J. Thorac. Dis. 2018, 10, 845–853. [Google Scholar] [CrossRef] [PubMed]
- Dellinger, R.P.; Levy, M.M.; Rhodes, A.; Annane, D.; Gerlach, H.; Opal, S.M.; Sevransky, J.E.; Sprung, C.L.; Douglas, I.S.; Jaeschke, R.; et al. Surviving sepsis campaign: International guidelines for management of severe sepsis and septic shock: 2012. Crit. Care Med. 2013, 41, 580–637. [Google Scholar] [CrossRef] [PubMed]
- Shin, T.G.; Hwang, S.Y.; Kang, G.H.; Kim, W.Y.; Ryoo, S.M.; Kim, K.; Jo, Y.H.; Chung, S.P.; Joo, Y.S.; Beom, J.H.; et al. Korean Shock Society septic shock registry: A preliminary report. Clin. Exp. Emerg. Med. 2017, 4, 146–153. [Google Scholar] [CrossRef] [PubMed]
- Klinger, A.; Mueller, A.; Sutherland, T.; Mpirimbanyi, C.; Nziyomaze, E.; Niyomugabo, J.-P.; Niyonsenga, Z.; Rickard, J.; Talmor, D.S.; Riviello, E. Predicting mortality in adults with suspected infection in a Rwandan hospital: An evaluation of the adapted MEWS, qSOFA and UVA scores. BMJ Open 2021, 11, e040361. [Google Scholar] [CrossRef]
- Bonnewell, J.P.; Rubach, M.P.; Madut, D.B.; Carugati, M.; Maze, M.J.; Kilonzo, K.G.; Lyamuya, F.; Marandu, A.; Kalengo, N.H.; Lwezaula, B.F.; et al. Performance Assessment of the Universal Vital Assessment Score vs Other Illness Severity Scores for Predicting Risk of In-Hospital Death Among Adult Febrile Inpatients in Northern Tanzania, 2016-2019. JAMA Netw. Open 2021, 4, e2136398. [Google Scholar] [CrossRef]
- Adegbite, B.R.; Edoa, J.R.; Ndoumba, W.F.N.; Mbadinga, L.B.D.; Mombo-Ngoma, G.; Jacob, S.T.; Rylance, J.; Hänscheid, T.; Adegnika, A.A.; Grobusch, M.P. A comparison of different scores for diagnosis and mortality prediction of adults with sepsis in Low-and-Middle-Income Countries: A systematic review and meta-analysis. eClinicalMedicine 2021, 42, 101184. [Google Scholar] [CrossRef]
- Xu, X.; Yang, T.; An, J.; Li, B.; Dou, Z. Liver injury in sepsis: Manifestations, mechanisms and emerging therapeutic strategies. Front. Immunol. 2025, 16, 1575554. [Google Scholar] [CrossRef]
- Alves, G.F.; Aimaretti, E.; Einaudi, G.; Mastrocola, R.; de Oliveira, J.G.; Collotta, D.; Porchietto, E.; Aragno, M.; Cifani, C.; Sordi, R.; et al. Collino Pharmacological Inhibition of FAK-Pyk2 Pathway Protects Against Organ Damage and Prolongs the Survival of Septic Mice. Front. Immunol. 2022, 13, 837180. [Google Scholar] [CrossRef]
- Guo, Y.; Guo, W.; Chen, H.; Sun, J.; Yin, Y. Mechanisms of sepsis-induced acute liver injury: A comprehensive review. Front. Cell. Infect. Microbiol. 2025, 15, 1504223. [Google Scholar] [CrossRef]
- Sookoian, S.; Castaño, G.O.; Scian, R.; Fernández Gianotti, T.; Dopazo, H.; Rohr, C.; Gaj, G.; San Martino, J.; Sevic, I.; Flichman, D.; et al. Serum aminotransferases in nonalcoholic fatty liver disease are a signature of liver metabolic perturbations at the amino acid and Krebs cycle level. Am. J. Clin. Nutr. 2016, 103, 422–434. [Google Scholar] [CrossRef]
- Bezan, A.; Mrsic, E.; Krieger, D.; Stojakovic, T.; Pummer, K.; Zigeuner, R.; Hutterer, G.C.; Pichler, M. The Preoperative AST/ALT (De Ritis) Ratio Represents a Poor Prognostic Factor in a Cohort of Patients with Nonmetastatic Renal Cell Carcinoma. J. Urol. 2015, 194, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.L.; Li, J.P.; Li, L.F.; Zeng, T.; He, X. Elevated Preoperative Serum Alanine Aminotransferase/Aspartate Aminotransferase (ALT/AST) Ratio Is Associated with Better Prognosis in Patients Undergoing Curative Treatment for Gastric Adenocarcinoma. Int. J. Mol. Sci. 2016, 17, 911. [Google Scholar] [CrossRef] [PubMed]
- Ghahari, M.; Salari, A.; Ghafoori Yazdi, M.; Nowroozi, A.; Fotovat, A.; Momeni, S.A.; Razzaghi, M.; Lotfi, M.; Shakiba, B. Association Between Preoperative De Ritis (AST/ALT) Ratio and Oncological Outcomes Following Radical Cystectomy in Patients With Urothelial Bladder Cancer. Clin. Genitourin. Cancer 2022, 20, e89–e93. [Google Scholar] [CrossRef] [PubMed]
- Riedl, J.M.; Posch, F.; Prager, G.; Eisterer, W.; Oehler, L.; Sliwa, T.; Wilthoner, K.; Petzer, A.; Pichler, P.; Hubmann, E.; et al. The AST/ALT (De Ritis) ratio predicts clinical outcome in patients with pancreatic cancer treated with first-line nab-paclitaxel and gemcitabine: Post hoc analysis of an Austrian multicenter, noninterventional study. Ther. Adv. Med. Oncol. 2020, 12, 1758835919900872. [Google Scholar] [CrossRef]
- Zhou, J.; He, Z.; Ma, S.; Liu, R. AST/ALT ratio as a significant predictor of the incidence risk of prostate cancer. Cancer Med. 2020, 9, 5672–5677. [Google Scholar] [CrossRef]
- Liberti, M.V.; Locasale, J.W. The Warburg Effect: How Does it Benefit Cancer Cells? Trends Biochem. Sci. 2016, 41, 211–218. [Google Scholar] [CrossRef]
- Yang, L.; Xie, M.; Yang, M.; Yu, Y.; Zhu, S.; Hou, W.; Kang, R.; Lotze, M.T.; Billiar, T.R.; Wang, H.; et al. PKM2 regulates the Warburg effect and promotes HMGB1 release in sepsis. Nat. Commun. 2014, 5, 4436. [Google Scholar] [CrossRef]
- Xu, Z.; Xu, B. Nonlinear association between AST/ALT ratio and 28-day all-cause mortality following ICU admission in critically ill cirrhotic patients: A retrospective cohort study. BMC Gastroenterol. 2025, 25, 367. [Google Scholar] [CrossRef]
- Botezelli, J.D.; Cambri, L.T.; Ghezzi, A.C.; Dalia, R.A.; Voltarelli, F.A.; de Mello, M.A.R. Fructose-rich diet leads to reduced aerobic capacity and to liver injury in rats. Lipids Health Dis. 2012, 11, 78. [Google Scholar] [CrossRef]
- Li, Y.; Tao, Y.; Xu, J.; He, Y.; Zhang, W.; Jiang, Z.; He, Y.; Liu, H.; Chen, M.; Zhang, W.; et al. Hyperoxia Provokes Time- and Dose-Dependent Gut Injury and Endotoxemia and Alters Gut Microbiome and Transcriptome in Mice. Front. Med. 2021, 8, 732039. [Google Scholar] [CrossRef]
- Dresen, E.; Pimiento, J.M.; Patel, J.J.; Heyland, D.K.; Rice, T.W.; Stoppe, C. Overview of oxidative stress and the role of micronutrients in critical illness. J. Parenter. Enter. Nutr. 2023, 47 (Suppl. S1), S38–S49. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Li, J.; Ren, Y.; Shi, H.; Rong, X.; Zhang, X.; Shao, Y.; Wu, R.; Chu, M.; Qiu, H. Association between alanine aminotransferase/aspartate aminotransferase ratio (AST/ALT Ratio) and coronary artery injury in children with Kawasaki disease. Cardiol. Res. Pract. 2020, 2020, 8743548. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Shi, X.; Pan, Y. The Association of Aspartate Aminotransferase/Alanine Aminotransferase Ratio with Diabetic Nephropathy in Patients with Type 2 Diabetes. Diabetes Metab. Syndr. Obes. 2021, 14, 3831–3837. [Google Scholar] [CrossRef] [PubMed]
- Galley, H.F. Oxidative stress and mitochondrial dysfunction in sepsis. Br. J. Anaesth. 2011, 107, 57–64. [Google Scholar] [CrossRef]
- Giannakopoulos, K.; Hoffmann, U.; Ansari, U.; Bertsch, T.; Borggrefe, M.; Akin, I.; Behnes, M. The Use of Biomarkers in Sepsis: A Systematic Review. Curr. Pharm. Biotechnol. 2017, 18, 499–507. [Google Scholar] [CrossRef]
- Woźnica, E.A.; Inglot, M.; Woźnica, R.K.; Łysenko, L. Liver dysfunction in sepsis. Adv. Clin. Exp. Med. 2018, 27, 547–552. [Google Scholar] [CrossRef]
- Nesseler, N.; Launey, Y.; Aninat, C.; Morel, F.; Mallédant, Y.; Seguin, P. Clinical review: The liver in sepsis. Crit. Care 2012, 16, 235–238. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).