Abstract
Clinical decision-making for diagnosing and treating oral and dental diseases consolidates multiple sources of complex information, yet individual clinical judgements are often made intuitively on limited heuristics to simplify decision making, which may lead to errors harmful to patients. This study aimed at systematically evaluating dental practitioners’ clinical decision-making processes during diagnosis and treatment planning under uncertainty. A scoping review was chosen as the optimal study design due to the heterogeneity and complexity of the topic. Key terms and a search strategy were defined, and the articles published in the repository of the National Library of Medicine (MEDLINE/PubMed) were searched, selected, and analysed in accordance with PRISMA-ScR guidelines. Of the 478 studies returned, 64 relevant articles were included in the qualitative synthesis. Studies that were included were based in 27 countries, with the majority from the UK and USA. Articles were dated from 1991 to 2022, with all being observational studies except four, which were experimental studies. Six major recurring themes were identified: clinical factors, clinical experience, patient preferences and perceptions, heuristics and biases, artificial intelligence and informatics, and existing guidelines. These results suggest that inconsistency in treatment recommendations is a real possibility and despite great advancements in dental science, evidence-based practice is but one of a multitude of complex determinants driving clinical decision making in dentistry. In conclusion, clinical decisions, particularly those made individually by a dental practitioner, are potentially prone to sub-optimal treatment and poorer patient outcomes.
1. Introduction
Central to medical ethics is the premise “primum non nocere”—first do no harm. The dental profession has taken significant strides in the past century to reduce patient harm. However, the quality of provision of dentistry globally remains highly variable, and this is often partially attributable to clinician and patient factors. For example, a recent study found that 21.1% of dentists reported wrong tooth extraction [1]. Clearly, diagnostic and treatment planning errors contribute to patient harm. In a primary setting, dentists routinely diagnose and plan treatment in isolation, relying largely on their own decision-making capabilities. Clinical decision-making utilises both cognitive (analytical) and intuitive (non-analytical) processes to consolidate the complex information available into a treatment plan [2,3,4]. Decisions are made under many unpredictable conditions, including patient specific factors or preferences, financial constraints, technical factors regarding treatment, and the clinician’s knowledge, experience, emotional state, and fatigue [5,6].
Individual judgements are often made intuitively on a limited number of heuristics and biases. This process streamlines decision making into a simpler task, which enables the decision to be made in an efficient and timely manner. Fast thinking, though, can lead to severe and systematic errors [7]. Clinicians relying on the intuition-based heuristics such as ‘representativeness’ and ‘availability’ may disregard probabilistic, systematic, and check-listed thinking [8].
In an age of evidence-based dentistry, algorithms, informatics, and big data, there is real hope for further reductions to patient harm by enhancing clinician decisions. Contemporary software has already demonstrated its utility in assisting the diagnosis and management of dental diseases across a variety of specialties. Foreseeably, rapid improvements in AI technologies will likely make such clinical support ever more valuable and common place [9,10].
Clinical decision-making guidelines and augmentations to patient informed consent both have parts to play in limiting the role of clinician cognitive biases and heuristics in patient harm [11,12,13,14].
Decision making under uncertainty has now been researched for over 60 years and has been widely applied in economic and geo-political situations. There is, however, a paucity in its application to health care—particularly dentistry. Given that dental treatment plans can also be viewed as clinical decision making under uncertainty, the purpose of this scoping review is to investigate the underlying process of decision making in clinical dentistry and the factors that influence an individual clinician when diagnosing and treatment planning a case.
2. Methods
2.1. Search Strategy
A preliminary search strategy was devised initially in MEDLINE Ovid. During the preliminary search, keywords relevant to the topic ‘decision making under uncertainty within dentistry’ were included to gauge the range of literature available. These included search terms: ‘group OR collective’, ‘diagnos*’ OR ‘deci*’, ‘dent*’. The search string was then further developed, and sensitivity analysis of several searches was undertaken using some landmark papers as guiding references.
The search strategy was created based on the three keywords associated with the review topic.
- ‘dentist* OR dental’ restricted the records to the oral healthcare field.
- ‘decision OR diagnosis OR treatment OR management OR guideline’ limited result articles to diagnosis and treatment planning, which are both vital clinical decisions in dentistry.
- ‘decision making process OR heuristi* OR intuition OR clinical reasoning OR clinical judgment OR collective intelligence OR informatives’ narrowed down papers to involve the thought processes of clinicians involved in the studies.
These three domains were combined with Boolean operators as appropriate. The final search string was conducted through PubMed as follows: (dentist*[Title/Abstract] or dental[Title/Abstract]) AND (decision making process[Title/Abstract] or heuristi*[Title/Abstract] or intuition[Title/Abstract] or clinical reasoning[Title/Abstract] or clinical judgement[Title/Abstract] or collective intelligence[Title/Abstract] or informatics[Title/Abstract]) AND (decision[Title/Abstract] OR diagnosis[Title/Abstract] or treatment [Title/Abstract] or management[Title/Abstract] or guideline[Title/Abstract]).
2.2. Eligibility Criteria
Articles were evaluated initially based on their titles and abstracts by 2 researchers independently. If a disagreement occurred, a third researcher served as a judge to make the final decision. Adhering to the Cochrane guidelines, a lenient policy was adopted during the selection process where there were any uncertainties. In cases of further disagreement or ambiguity, a meeting was held to discuss the decision of inclusion, with the senior authors (MG and NC) to determine the final outcome.
Articles were included in the scoping review if they satisfied the following criteria:
- Primary healthcare setting, focusing on the dental field.
- Studies conducted or available in English.
- Making clinical decisions in diagnosis, treatment, or patient management.
- Clinical decisions can be made on real or hypothetical cases.
Articles were excluded from the scoping review due to any of the following criteria:
- The contents of the article were irrelevant to the scoping review and did not discuss clinical decision making within the dental field.
- Review articles that lacked original research results.
- Article was not available in English.
- Article full text was not available.
2.3. Data Extraction and Analysis
The full texts of the articles included were accessed and data extraction was undertaken using a master table. Additional articles that did not meet the inclusion criteria were excluded if missed by the initial screening. The information extracted to the master table included study design, number of participants, data collection method, and main conclusion drawn.
3. Results
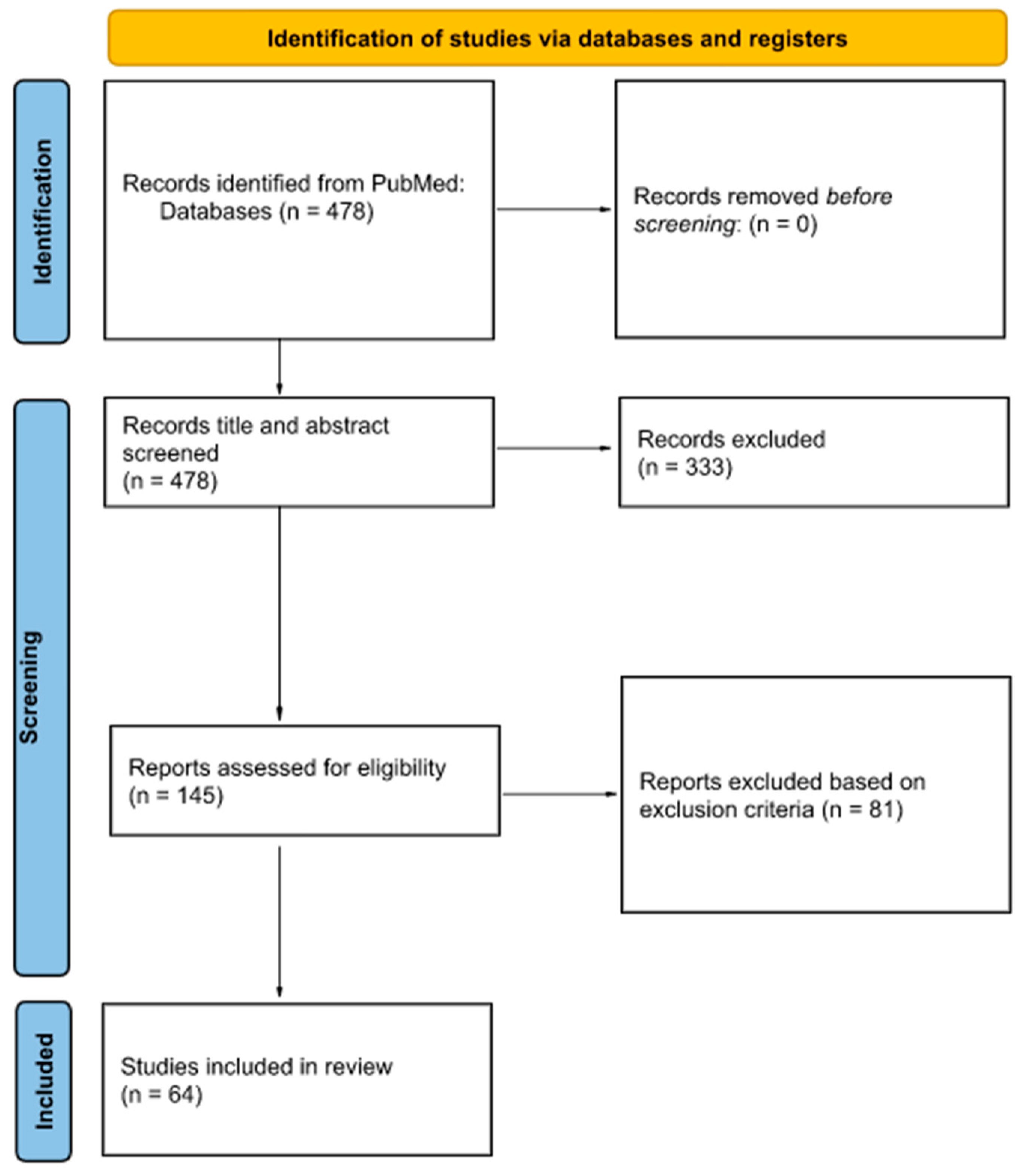
As of 4 June 2022, our search strategy on PubMed yielded 478 results. Each article was assessed for eligibility and 64 were included in the qualitative synthesis (Table S1). Of the 81 excluded (based on exclusion criteria), 45 lacked original research, 29 were not relevant, 6 were inaccessible, and 1 was excluded as the participants were not from a dental background. Details of the article selection process are illustrated by a PRISMA flowchart (Figure 1).
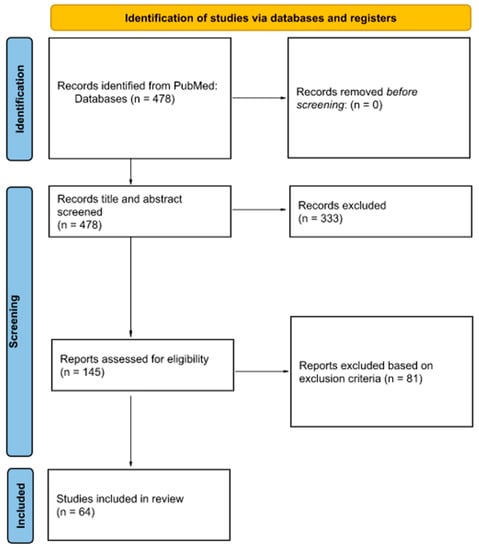
Figure 1.
Flowchart for study selection in accordance with Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) guidelines.
3.1. Study Characteristics
By year of their publication, studies included ranged from 1991 to 2022. Of the 64 articles, 46 were published in the last 10 years (2012 to 2022), greatly exceeding the number of articles that were written before from 1991 to 2011.
Studies were based in 27 countries, but were predominantly from the United States (n = 13) and the United Kingdom (n = 13). Out of all the studies except 1, which represents ‘qualified academicians’, 12 involved participants in a dental setting either as patients, dental students, general dentists, dental specialists, dental hygienists, or assistants. Dental specialties were diversely represented, with orthodontists, paediatric dentists, endodontists, prosthodontists, oral maxillofacial surgeons, oral medicine specialists, and dento-maxillofacial radiologists.
All studies were observational studies except four [15,16,17,18], which were experimental studies. The types of observational studies included were a mixture of descriptive studies (case report, case series, cross-sectional, qualitative studies) and analytic studies (cohort, case-control). The most common methods of data collection were questionnaires/surveys and semi-structured interviews. Only one randomised controlled trial was reviewed [17], and the Delphi method was used in four studies [14,19,20,21].
Under the umbrella of decision making under uncertainty in dentistry, the roles of six major recurring themes were identified: heuristics and biases, clinical factors, clinical experience, patient preferences and perceptions, artificial intelligence and informatics, and existing guidelines.
Of note, the first article about artificial intelligence & informatics was published in 2008. However, most studies on this topic are concentrated between 2017 and 2022 (7 of 10 studies), suggesting that it is a rising field of research. Furthermore, 10 of the 11 studies investigating dental patient perception, preference, and patient-centred care were published before 2016.
The main findings of the six themes are reported in the following paragraphs.
3.2. Heuristics and Biases Related to the Decision-Making Process
Of the 64 studies included in the review, 13 examined the effect of various common heuristics and biases on the decision-making process in dental settings (Table 1).

Table 1.
Extracted articles that investigated heuristics and biases related to the decision-making process.
Decision making was demonstrated to be impacted due to clinician education and preferences as well as patient characteristics. Practitioners were more likely to pursue procedures that they enjoyed and were influenced by their “frame of mind” [26]. In high-cost healthcare interventions, e.g., implants, clinical decisions made by practitioners are influenced by assumptions about patient characteristics and financial status [29,32]. Decision making was influenced by dentists’ self-confidence [32], intuitive shortcuts based on prior experiences [33], and differential understanding of the progression of disease [25].
Biases that affect clinical decision-making include those that affect the dentists’ perceptions of the patient. Many patients with a history of addiction and mental illness revealed they felt excluded from the decision-making process [28]. Social and behavioural determinants were also demonstrated to impact decision making [22], suggesting that both implicit and confirmation bias alter this process. Age was a major theme in two studies [27,30] discussing endodontic treatment. Older patients were more likely to receive more invasive treatment in asymptomatic and symptomatic cases, despite no firm evidence supporting age significantly altering the effectiveness of vital pulp therapy [27].
3.3. Clinical Factors Affecting Clinical Decision-Making
Study results from 15 included papers revealed that clinicians rely on subjective clinical interpretation of investigations such as patient history, visual oral examinations, and radiographic interpretations to form a diagnosis and treatment plan (Table 2).

Table 2.
Extracted articles that investigated clinical factors affecting clinical decision making under uncertainty.
Seven studies assessed the influence of patient factors on confidence in clinical decision making [23,37,38,40,43,44,45,46]. The following inherent factors were considered important in clinical decision making: patient age, dental history, clarity of communication, social circumstances, functional aesthetic demands, smoking and alcohol consumption, and medical history [23]. Studies also show that the complexity and severity of the patient’s condition affected diagnostic accuracy, confidence in treatment planning, and the decision to refer [37,38,40,43,44,45,46]. For example, clinicians more confidently selected patients with fewer missing teeth and no bone loss for treatment by implant replacement [40]. Similarly, crowding severity and soft tissue profile influence orthodontic decision making [38]. Referral of potentially malignant diseases to oral medicine specialists depended on lesion colour, cause, location, duration, pattern, and size [43]. The decision to extract periodontally affected teeth or refer to a specialist is influenced by case complexity, dictated by factors such as mobility, severe attachment loss, and radiographic bone loss [45]. In paediatric patients, crying was an accurate indicator of dental anxiety, which influenced the clinical decision to use sedation [46].
Four studies found that the type of treatment had effects on confidence in clinical decision making [23,24,36,41]. Procedural predictability, technical difficulty and risk of iatrogenic damage influenced the clinician’s confidence in decision making [36]. McGeown et al. adds that equipment limits and time and facilities also played a role, while Fu et al. considered timing of clinical findings as important for confidence in treatment planning, where late detection of tooth eruption disturbances can lead to greater complexity [23]. Ilgunas et al. emphasizes the negative effect that time pressure has on accurate clinical decision making in relation to TMD management [24].
Four studies assessed the influence of radiographs on confidence in clinical decision making [35,39,42,47]. Information obtained from radiographs on the depth of a lesion influences the decision to treat. Clinicians were more confident with their decision when lesions involved the inner half of dentine [39]. Despite the importance of bitewing radiographs in the decision-making process, visual examination of caries via ICDAS lead to more accurate diagnosis [42]. Furthermore, clinicians were more confident with their clinical decisions when based off a cone beam CT compared with a periapical radiograph or OPG [35,47].
3.4. Clinical Experience Affecting Confidence in Decision Making
There were 13 extracted studies which focused on clinician factors associated with clinical decision making (Table 3). It was revealed that practitioners with more years of experience were associated with greater diagnostic accuracy in comparison to students [48]. Similar conclusions were drawn regarding extraction in periodontally affected teeth [49,50] and prosthodontic cases [51], linking greater experience with well-founded and conservative treatment decisions. However, more experience also led to greater variability in treatment recommendations [52] and did not alter the perceived difficulty [36]. Greater clinical experience was also shown to increase the practitioners’ confidence in producing an accurate diagnosis in dental hygienists [53,54].

Table 3.
Extracted articles that investigated clinical experience affecting confidence in decision making under uncertainty.
Clinician knowledge and education were also influences in decision making [57]. Dentists have an interest in evidence-based practice principles to improve their personal knowledge, skills, and treatment quality [59]. Most dental practitioners are open to integrating new standards into their practice, although outdated procedures were still prevalent under certain circumstances [58] due to non-clinical factors such as NHS regulations. Likewise, in TMJ disc displacement cases, frontline clinicians expressed high degrees of uncertainty due to lack of knowledge, skills, and experience within the area [56]. Finally, the time of graduation for Australian practitioners was correlated to delays in invasive caries intervention of permanent teeth [55].
3.5. Patient Preferences and Perceptions in Clinical Decision-Making
Of the extracted articles, 12 included study designs that investigated the impact of patient preferences on the clinical decision-making process in dentistry. A summary of these studies is shown (Table 4).

Table 4.
Extracted articles that investigated patient preferences and perceptions in clinical decision making under uncertainty.
Common findings indicate the preference of patients to be active in the clinical decision-making process [34,61,66]. On the contrary, one study reported that significantly more patients had preferences for information rather than a preference for actual involvement [65]. This result parallels the findings of Johnson et al., which reported a specific decision aid can yield a significant improvement in patient knowledge [17].
Patient-centred care is an approach to healthcare whereby care decisions are driven by the individual’s needs, preferences and desired outcomes [67]. Dental literature shows that by using a patient-centred method to generate information, patients will feel more involved in the decision-making process, and a better patient-practitioner relationship can be established [62,63]. No conclusive evidence supports a definitive association between patient preferences and their gender, as some studies reported a significant difference while others did not [64,65]. However, patient anxiety was shown to influence the decision-making process, and its identification was important in assisting dentists to achieve an ultimately successful outcome for their patients [46].
Studies reported that shared decision making was based on both clinical and contextual factors such as patients’ views [26,60]. One study, however, reported that shared decision making is more limited in high-cost intervention settings [29]. While a preference for shared decision making proves to be the cornerstone finding of these studies, evidence suggests that both patients and practitioners carry preferences that affect the decision-making process [34].
3.6. Artificial Intelligence and Informatics in Decision-Making
Out of the included studies, 11 of the papers included in this review were considered as relating to AI (artificial intelligence) and informatics (Table 5). Six of these papers developed and tested an intelligent AI model, of which two investigated the clinical viability of an AI model in making classifications from panoramic radiographs [18,68]. The other four papers [16,19,21,69] evaluated the effectiveness of incorporating AI models in making clinical diagnoses.

Table 5.
Extracted articles that investigated artificial intelligence and informatics in clinical decision making under uncertainty.
This review also includes two survey studies with the intention of ascertaining the receptibility of computer programs in the teaching of dentistry [72,74]. The remaining papers include a case presentation demonstrating the digital orthodontic workflow and its advantages/disadvantages [71], a cohort study assessing the possibility of standardising dentally relevant diagnostic terminology in electronic records [73], and an analysis of information.
3.7. Use of Existing Guidelines in Clinical Decision Making
Of the extracted studies, 11 studies outlined guidelines for clinical decision making in dentistry, as seen in Table 6. One study proposed use of a framework for managing data elements in oral disease diagnoses, which achieved nearly 95% agreement amongst experts, enabling consistency and transparency [19].
While it has been suggested that clinical guidelines often oversimplify treatment decision-making regarding implants, numerous studies highlighted the importance of considering multiple factors before selecting, preparing, or saving implants, particularly the patient’s medical history, bone quality, and implant location [30,75,76,77]. This was echoed by studies investigating surgical, extractive, and sedative decision making, which suggest consideration of patient factors such as medical history, including oncological prognosis and the level of dental anxiety [78,79,80,81].
Additionally, the use of assessment models for more systematic, transparent, and reproducible decision-making, such as for instrument selection and caries assessment, has been explored. While some assessment models had potential to be clinically applicable, others only found agreement with clinical judgement sometimes [14,82].

Table 6.
Extracted articles that investigated the use of existing guidelines in clinical decision making under uncertainty.
Table 6.
Extracted articles that investigated the use of existing guidelines in clinical decision making under uncertainty.
| Author | Year | Main Findings | Study Design |
|---|---|---|---|
| Abbas et al. [81] | 2022 | An indication of a sedation requirement tool can be used in patients with dental anxiety and those needing complex planned dental treatment. | Cross-sectional |
| Deniz et al. [14] | 2022 | Proposed a framework of multi-criteria decision making for Nickel Titanium instruments selection. | Case study |
| Amadi et al. [80] | 2021 | Treatment for geriatric populations must consider patient factors, such as bone atrophy, reduced tissue healing capacity, and medical history. | Case report |
| Korsch et al. [75] | 2021 | Comorbidities may lead to general refusal of pre-implantological methods to treat atrophic tooth gaps. | Clinical trial |
| Tarnow et al. [77] | 2021 | Key factors influencing decision making regarding implants in malposition include their restorative position, disease status, and depth. | Case report |
| Ehtesham et al. [19] | 2020 | A consensus-based framework for essential data elements in differential diagnoses of oral diseases was successfully made. | Cross-sectional |
| Eliyas et al. [78] | 2020 | Head and neck cancer patients on long-term antiangiogenic medication are at higher risk of complications from dental extractions. | Case report |
| Brescia et al. [79] | 2019 | One must consider many factors to select the appropriate surgical approach for removal of foreign modies in the maxillary sinus. | Case series |
| Chatzopoulos et al. [76] | 2018 | Root canal treatment exhibited a higher failure rate than implant treatment. Selection of either should be based on multiple factors, such as age and anxiety. | Cross-sectional |
| Hänsel Petersson et al. [82] | 2016 | Caries risk assessment based on clinical judgement and the Cariogram model gave similar results for patients predicted at a low level of future disease. | Cross-sectional |
| Su et al. [30] | 2014 | There is no irrefutable clinical guideline that can be followed for whether a tooth should be replaced with an implant, or be treated and maintained. | Cross-sectional |
4. Discussion
Decision making in dentistry is complex and dependent on a number of factors. In this scoping review, we identified the following: heuristics and biases, clinical factors, clinical experience, patient preference, intelligence and informatics, and existing guidelines. These factors can substantially influence the clinical decisions made in regards to diagnosis and treatment planning when conducted by a single dental practitioner, potentially leading to suboptimal treatment and poorer patient outcomes.
4.1. Heuristics and Biases
Rather than an objective analysis of a case, post hoc justifications of courses of care are made primarily due to intuitive reasoning [23]. Analysis of these “diagnostic thinking processes” revealed that inter-clinician variability was not due to inadequate diagnostic process. Rather, this variability was attributable to the concepts signaling the need to intervene, which are influenced by prior experience. Since dental students are exposed to environments with high levels of decay, they are primed to expect decay and hence place restorations regularly. [33]. Diagnostic processes could incorporate two processes to assist clinical decision making. The first process involves pattern recognition and the second process is explicitly analytical. This allows clinicians to appropriately treat typical presentations and adopt a more analytical perspective in atypical cases [31].
Lack of education about certain disorders, lack of insight in ability, and differential interpretations altered treatment outcomes. Analysis of TMD management by GDPs determined that some patterns for treating TMD were inadequate and reflected a “culture of generalisations”, highlighting that lack of education leads to substandard care [24]. Clinicians’ current state of mind and enjoyment of certain procedures predisposed them to pursue certain treatments [26]. “Weaker students” often lacked insight of their true competence and overestimated their abilities, which may result in poorer outcomes. Men more often overestimate their abilities than women [32]. Another cause of the high individual variation for retreatment is due to the clinicians’ interpretation of where on the continuum of periapical health a patient is. This results in disagreement as to what constitutes optimal treatment [25]. Treatment provided is directly affected by clinician factors, such as clinician education, frame of mind, and assumption of a patient’s financial status [26,29,32]. Therefore, it may be postulated that collective diagnosis may reduce sources of bias and error when treatment planning. Whilst the effects of collective intelligence on decision-making accuracy in medicine is relatively well studied, our results reveal a scarcity of literature on its potential application in dentistry [83].
4.2. Clinical Factors
A number of clinical factors play a role in the practitioner’s confidence when making diagnostic and treatment decisions. These can be broken down into three groups: patient factors, treatment complexity, and clinical information obtained from examination and further investigations. The magnitude of the effects that these factors have on decision making is dependent on the particular case. For example, smoking status plays an important role in diagnosis of potentially malignant lesions in the mouth [43], but not so much when treatment planning for composite restorations. Results also identified some non-clinical factors that included time, facilities, and dental anxiety, which further affected the clinician’s decision-making ability.
4.3. Clinical Experience
The experience of the clinician is correlated with confidence in providing accurate diagnoses and appropriate treatment plans. This is also seen in psychology [84], where experience was a strong predictor for diagnostic accuracy, primarily due to exposure to more clinical cases. The education of the clinician influences core principles and philosophies behind treatment decisions, with more recent education and professional development producing clinicians that tend to practice with updated and conservative philosophies, preserving tooth structure where possible.
The intermediate phenomena observed in a specific study [48] suggests that clinical experience allows for an ‘encapsulated’ mode of clinician information processing and diagnosis compared to a more ‘elaborated’ response from dental students, possibly due to factors such as appointment time constraints and profit-driven pressures that are applied to practicing dentists. Practitioners may also become more pragmatic in their clinical practice and decision making [55], although more research is still needed within the area to investigate the reasoning behind these changes.
4.4. Patient Preference
Ultimately, the choice of action to be taken lies in the hands of the patient, although the different values and preferences of patients determine which decision will be taken. The majority of the papers examined indicated a preference for patients to be involved in the decision-making process. Results indicated that while clinical factors are important in this process, they are ultimately overruled by patient preferences [26]. This is likely to have implications in the clinical setting, as the nature of preferences are subject to bias and predispositions. In particular, both anxiety and patients’ impressions of dentists’ personality are shown to mediate both the treatment and decision-making process [34,46]. Overall, a desire for shared decision making proves common to the majority of studies that examined the effects of patient preference, although gaps in the literature do exist. Most of the information published that addresses this factor are a part of specific dental-related cases reports. As such, prospective studies may wish to design a study that focuses on the variety of patient preferences and perceptions that impact the treatment and decision-making process in dentistry. This will likely assist in accurately dissecting the decision-making process, thus allowing for the possibility of improved treatment outcomes and concord in the shared decision-making process.
4.5. Intelligence and Informatics
Choi et al. and Tuzoff et al. highlight the possibility of AI usage to aid in interpretation of dental radiographs [18,68]. Several papers—in addition to those included in this review—have advocated for the use of computer-aided diagnosis (CAD) as a means of providing an interface for managing and simplifying complex variables involved in the traditional clinical diagnosis process [19,21,69,74,85]. The use of computer programs in dentistry has been rapidly evolving for quite some time now with the advent and popularisation of digital workflow systems providing a way to improve communication—both between practitioners and with patients—as well as a means of improving overall efficiency and decreasing laboratory workload [70,71,86,87].
The papers in this review all explored the efficacy of AI with a positive outlook. The shortcomings of these programs, however, cannot be ignored. The studies included were primarily cohort or cross-sectional studies with few participants, rather than clinical trials, and studies that tested the clinical efficacy of an AI program did so using simulation cases as opposed to real-life clinical cases. It is evident that further clinical testing of these programs are required; however, a fundamental constraint persists in measuring the accuracy of clinical decision making due to its subjective nature and its inherent biases, which leads to inter-practitioner discrepancies. Thus, obtaining an objective measure of clinical decision-making accuracy may be considered almost impracticable. Nevertheless, it is our optimistic perspective that AI-based technology will persist in expanding its horizons and potentially assimilate into clinical dentistry in the future.
4.6. Use of Existing Guidelines
Clinical practice guidelines include practice recommendations informed by unbiased systematic reviews of evidence, and an assessment of the benefit and the harms of alternative treatment options. As such, clinical guidelines guide the clinical decision making of dental practitioners by standardising appropriate healthcare for specific clinical circumstances. For example, the framework suggested by Ehtesham et al. of essential data elements to form a differential diagnosis for oral diseases achieved a high level of agreement, and has the potential to become a uniform professional criterion [19]. However, the study may have been limited by geographic bias, and future studies would therefore benefit from wider participant sampling.
Dentists should consider the specifics of the individual patient, and assess the applicability of existing guidelines. The guidelines suggested by numerous studies emphasised patient-centred care and the importance of considering patient factors during treatment [75,76,78,81]. For example, a history of endocarditis and bisphosphonates may lead to a general refusal of implants [75,76]. However, these studies had low response rates, a limited number of patients, and were retrospective, which may limit their ability to generalise results. Future studies should thereby aim to investigate a greater number of patients and be prospective studies.
5. Conclusions
Decision making in dentistry, despite its importance to patient care, remains an under-researched domain. Clinical judgement is highly complex and dependent on experience; discrepancies between practitioners is ultimately inevitable, with cognitive heuristics and biases being formed from personal education, clinical experience, and self-confidence. Unsurprisingly, a clinician’s inclination towards procedures, estimation of their abilities, and psychological state can impact the quality of care a patient receives. Ultimately, shared decisions are made between the practitioner and patient with preferences and contextual factors influencing the agreed treatment plan.
Although novel, AI models and informatics have the potential to assist traditional clinical decision-making, but larger and more rigorous studies are warranted to determine if there is significant clinical benefit to be obtained. Reference to guidelines may update and supplement personal experience. Realistically, individual diagnostic or treatment planning errors are unlikely to be fully eliminated due to the various human elements that define clinical dentistry.
There are inherent limitations to scoping reviews, including the potential to miss articles due to the database selection. “Gray” literature, or literature of borderline relevance, may have been excluded, and studies not published in English were not reported here. The results of our study reveal a network of determinants influencing a dentist acting as a sole decision-maker under uncertainty. Inconsistency in treatment recommendations between clinicians is a real possibility, increasing the risk of sub-optimal treatment being provided and poorer patient outcomes. Evidently, there exists a need for additional research into methods of improving clinical decision-making accuracy in the dental setting, which aim to minimise error and place patient safety at the forefront.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/diagnostics13061076/s1, Table S1: Extraction table consisting of the 64 articles that satisfied the inclusion criteria as identified by the PRISMA flowchart.
Author Contributions
Conceptualization and methodology, M.G. and N.C.; formal analysis, investigation, data curation, writing—original draft preparation, A.I.K.M., J.B., J.C., D.B.-K., A.D., K.B., M.B., N.A. and S.S.H.C.; writing—review and editing, supervision, M.G. and N.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Full datasets are available upon reasonable request to the corresponding author.
Acknowledgments
The authors would like to acknowledge the support of the University of Melbourne and STEMM Research for making the necessary bibliographic resources available.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Jan, A.; Albenayan, R.; Alsharkawi, D.; Jadu, F. The prevalence and causes of wrong tooth extraction. Niger. J. Clin. Pract. 2019, 22, 1706. [Google Scholar]
- Braude, H.D. Clinical intuition versus statistics: Different modes of tacit knowledge in clinical epidemiology and evidence-based medicine. Theor. Med. Bioeth. 2009, 30, 181–198. [Google Scholar] [CrossRef]
- Lucchiari, C.; Pravettoni, G. Cognitive balanced model: A conceptual scheme of diagnostic decision making. J. Eval. Clin. Pract. 2012, 18, 82–88. [Google Scholar] [CrossRef]
- Marcum, J.A. An integrated model of clinical reasoning: Dual-process theory of cognition and metacognition. J. Eval. Clin. Pract. 2012, 18, 954–961. [Google Scholar] [CrossRef] [PubMed]
- Dunphy, B.C.; Cantwell, R.; Bourke, S.; Fleming, M.; Smith, B.; Joseph, K.S.; Dunphy, S.L. Cognitive elements in clinical decision-making. Adv. Health Sci. Educ. 2010, 15, 229–250. [Google Scholar] [CrossRef] [PubMed]
- Feller, L.; Lemmer, J.; Nemutandani, M.S.; Ballyram, R.; Khammissa, R.A.G. Judgment and decision-making in clinical dentistry. Int. J. Med. Res. 2020, 48, 0300060520972877. [Google Scholar] [CrossRef]
- Tversky, A.; Kahneman, D. Judgment under Uncertainty: Heuristics and Biases: Biases in judgments reveal some heuristics of thinking under uncertainty. Science 1974, 185, 1124–1131. [Google Scholar] [CrossRef]
- Kahneman, D.; Tversky, A. On the psychology of prediction. Psychol. Rev. 1973, 80, 237. [Google Scholar] [CrossRef]
- Butera, A.; Maiorani, C.; Gallo, S.; Pascadopoli, M.; Buono, S.; Scribante, A. Dental Erosion Evaluation with Intact-Tooth Smartphone Application: Preliminary Clinical Results from September 2019 to March 2022. Sensors 2022, 22, 5133. [Google Scholar] [CrossRef]
- Khanagar, S.B.; Al-Ehaideb, A.; Maganur, P.C.; Vishwanathaiah, S.; Patil, S.; Baeshen, H.A.; Sarode, S.C.; Bhandi, S. Developments, application, and performance of artificial intelligence in dentistry–A systematic review. J. Dent. Sci. 2021, 16, 508–522. [Google Scholar] [CrossRef]
- Chin-Yee, B.; Upshur, R. Clinical judgement in the era of big data and predictive analytics. J. Eval. Clin. Pract. 2018, 24, 638–645. [Google Scholar] [CrossRef] [PubMed]
- Woolf, S.H.; Grol, R.; Hutchinson, A.; Eccles, M.; Grimshaw, J. Potential benefits, limitations, and harms of clinical guidelines. BMJ 1999, 318, 527–530. [Google Scholar] [CrossRef]
- Faggion, C.M., Jr. The development of evidence-based guidelines in dentistry. J. Dent. Educ. 2013, 77, 124–136. [Google Scholar] [CrossRef]
- Deniz, N.; Orhan, E.O. Development of a multi-criteria decision-making–based assessment model for dental material selection: Engine-driven nickel-titanium instruments case study. Clin. Oral Investig. 2022, 26, 2645–2659. [Google Scholar] [CrossRef]
- Alkahtani, A.; Anderson, P.; Baysan, A. The performance of SoproLIFE for early detection of coronal caries using the International Caries Classification and Management System-A preliminary laboratory-based study. Photodiagnosis Photodyn. Ther. 2021, 35, 102422. [Google Scholar] [CrossRef] [PubMed]
- Thanathornwong, B. Bayesian-based decision support system for assessing the needs for orthodontic treatment. Healthc. Inform. Res. 2018, 24, 22–28. [Google Scholar] [CrossRef] [PubMed]
- Johnson, B.R.; Schwartz, A.; Goldberg, J.; Koerber, A. A chairside aid for shared decision making in dentistry: A randomized controlled trial. J. Dent. Educ. 2006, 70, 133–141. [Google Scholar] [CrossRef]
- Choi, E.; Lee, S.; Jeong, E.; Shin, S.; Park, H.; Youm, S.; Son, Y.; Pang, K. Artificial intelligence in positioning between mandibular third molar and inferior alveolar nerve on panoramic radiography. Sci. Rep. 2022, 12, 2456. [Google Scholar] [CrossRef]
- Ehtesham, H.; Safdari, R.; Mansourian, A.; Tahmasebian, S.; Mohammadzadeh, N.; Pourshahidi, S. Management of the essential data element in the differential diagnosis of oral medicine: An effective step in promoting oral health. J. Educ. Health Promot. 2020, 9, 255. [Google Scholar]
- Moore, C.; McLister, C.; O’Neill, C.; Donnelly, M.; McKenna, G. Pre-radiotherapy dental extractions in patients with head and neck cancer: A Delphi study. J. Dent. 2020, 97, 103350. [Google Scholar] [CrossRef]
- Ehtesham, H.; Safdari, R.; Mansourian, A.; Tahmasebian, S.; Mohammadzadeh, N.; Pourshahidi, S. Developing a new intelligent system for the diagnosis of oral medicine with case-based reasoning approach. Oral Dis. 2019, 25, 1555–1563. [Google Scholar] [CrossRef]
- Meyer, B.D.; Hansen, M.; Sweeney, K.; McDaniel, J.; Townsend, J. Calibrating Pediatric Dental Faculty: Caries Management in Primary Teeth. Pediatr. Dent. 2022, 44, 95–98. [Google Scholar] [PubMed]
- McGeown, D.; Mac Giolla Phadraig, C.; Whelehan, D.; Nunn, J.H. Dental decision-making under general anesthesia for patients with disabilities: A qualitative study. Spec. Care Dentist. 2022, 42, 20–27. [Google Scholar] [CrossRef] [PubMed]
- Ilgunas, A.; Lövgren, A.; Fjellman-Wiklund, A.; Häggman-Henrikson, B.; Karlsson Wirebring, L.; Lobbezoo, F.; Visscher, C.M.; Durham, J. Conceptualizing the clinical decision-making process in managing temporomandibular disorders: A qualitative study. Eur. J. Oral Sci. 2021, 129, e12811. [Google Scholar] [CrossRef]
- Helayl Al Waqdani, N.; Alomari, M.; Al-Dhalaan, R.M.; Alwaqdani, R. Decision making process by senior residents of Saudi Board in restorative dentistry for nonsurgical endodontic retreatment: A retrospective study. Saudi. Dent. J. 2021, 33, 78–84. [Google Scholar] [CrossRef]
- Dawson, V.S.; Fransson, H.; Wolf, E. Coronal restoration of the root filled tooth—A qualitative analysis of the dentists’ decision-making process. Int. Endod. J. 2021, 54, 490–500. [Google Scholar] [CrossRef] [PubMed]
- Careddu, R.; Plotino, G.; Cotti, E.; Duncan, H.F. The management of deep carious lesions and the exposed pulp amongst members of two European endodontic societies: A questionnaire-based study. Int. Endod. J. 2021, 54, 366–376. [Google Scholar] [CrossRef]
- Brondani, M.A.; Alan, R.; Donnelly, L. Stigma of addiction and mental illness in healthcare: The case of patients’ experiences in dental settings. PLoS ONE 2017, 12, e0177388. [Google Scholar] [CrossRef]
- Vernazza, C.R.; Rousseau, N.; Steele, J.G.; Ellis, J.S.; Thomason, J.M.; Eastham, J.; Exley, C. Introducing high-cost health care to patients: Dentists’ accounts of offering dental implant treatment. Community Dent. Oral Epidemiol. 2015, 43, 75–85. [Google Scholar] [CrossRef]
- Su, H.; Liao, H.F.; Fiorellini, J.P.; Kim, S.; Korostoff, J. Factors affecting treatment planning decisions for compromised anterior teeth. Int. J. Periodontics Restor. Dent. 2014, 34, 389–398. [Google Scholar]
- Khatami, S.; MacEntee, M.I.; Pratt, D.D.; Collins, J.B. Clinical reasoning in dentistry: A conceptual framework for dental education. J. Dent. Educ. 2012, 76, 1116–1128. [Google Scholar] [CrossRef]
- Devlin, H. Students’ perception of the prognosis for a single-surface amalgam restoration. Eur. J. Dent. Educ. 2012, 16, 86–90. [Google Scholar] [CrossRef] [PubMed]
- Maupomé, G.; Sheiham, A. Clinical decision-making in restorative dentistry. Content-analysis of diagnostic thinking processes and concurrent concepts used in an educational environment. Eur. J. Dent. Educ. 2000, 4, 143–152. [Google Scholar] [CrossRef] [PubMed]
- Redford, M.; Gift, H.C. Dentist-patient interactions in treatment decision-making: A qualitative study. J. Dent. Educ. 1997, 61, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Luz, L.B.; Vizzotto, M.B.; Xavier, P.N.I.; Vianna-Wan. nzeler, A.M.; Dias da Silveira, H.L.; Montagner, F. The Impact of Cone-beam Computed Tomography on Diagnostic Thinking, Treatment Option, and Confidence in Dental Trauma Cases: A Before and After Study. J. Endod. 2022, 48, 320–328. [Google Scholar] [CrossRef]
- Liew, J.; Zainal Abidin, I.; Cook, N.; Kanagasingam, S. Clinical decision-making in complex endodontic cases between postgraduate students across dental specialties at a UK dental school: A pilot study. Eur. J. Dent. Educ. 2022, 26, 707–716. [Google Scholar] [CrossRef]
- Kafantaris, S.N.; Tortopidis, D.; Pissiotis, A.L.; Kafantaris, N.M. Factors Affecting Decision-Making For Congenitally Missing Permanent Maxillary Lateral Incisors: A Retrospective Study. Eur. J. Prosthodont. Restor. Dent. 2020, 28, 43–52. [Google Scholar]
- Evrard, A.; Tepedino, M.; Cattaneo, P.M.; Cornelis, M.A. Which factors influence orthodontists in their decision to extract? A questionnaire survey. J. Clin. Exp. Dent. 2019, 11, e432–e438. [Google Scholar] [CrossRef]
- Leal, S.C.; Barros, B.V.; Cabral, R.N.; Ferrari, J.C.L.; de Menezes Abreu, D.M.; Ribeiro, A.P.D. Dental caries lesions in primary teeth without obvious cavitation: Treatment decision-making process. Int. J. Paediatr. Dent. 2019, 29, 422–428. [Google Scholar] [CrossRef]
- Cosyn, J.; Raes, S.; De Meyer, S.; Raes, F.; Buyl, R.; Coomans, D.; De Bruyn, H. An analysis of the decision-making process for single implant treatment in general practice. J. Clin. Periodontol. 2012, 39, 166–172. [Google Scholar] [CrossRef]
- Fu, P.S.; Wang, J.C.; Chen, C.H.; Huang, T.K.; Tseng, C.H.; Hung, C.C. Management of unilaterally deep impacted first, second, and third mandibular molars. Angle Orthod. 2012, 82, 565–571. [Google Scholar] [CrossRef] [PubMed]
- Diniz, M.B.; Lima, L.M.; Eckert, G.; Zandona, A.G.; Cordeiro, R.C.; Pinto, L.S. In vitro evaluation of ICDAS and radiographic examination of occlusal surfaces and their association with treatment decisions. Oper. Dent. 2011, 36, 133–142. [Google Scholar] [CrossRef]
- Brocklehurst, P.R.; Baker, S.R.; Speight, P.M. Factors which determine the referral of potentially malignant disorders by primary care dentists. J. Dent. 2010, 38, 569–578. [Google Scholar] [CrossRef] [PubMed]
- Korduner, E.K.; Söderfeldt, B.; Kronström, M.; Nilner, K. Decision making among Swedish general dental practitioners concerning prosthodontic treatment planning in a shortened dental arch. Eur. J. Prosthodont. Restor. Dent. 2010, 18, 43–47. [Google Scholar]
- Moreira, C.H.; Zanatta, F.B.; Antoniazzi, R.; Meneguetti, P.C.; Rösing, C.K. Criteria adopted by dentists to indicate the extraction of periodontally involved teeth. J. Appl. Oral Sci. 2007, 15, 437–441. [Google Scholar] [CrossRef] [PubMed]
- Holmes, R.D.; Girdler, N.M. A study to assess the validity of clinical judgement in determining paediatric dental anxiety and related outcomes of management. Int. J. Paediatr. Dent. 2005, 15, 169–176. [Google Scholar] [CrossRef]
- Danforth, R.A.; Peck, J.; Hall, P. Cone beam volume tomography: An imaging option for diagnosis of complex mandibular third molar anatomical relationships. J. Calif Dent. Assoc. 2003, 31, 847–852. [Google Scholar]
- Klomp, H.J.; Eberhard, J.; Hren, S.; Hedderich, J.; Schmidt, H.G. The role of pathophysiological explanations in clinical case representations of dental students and experts. Eur. J. Dent. Educ. 2009, 13, 58–65. [Google Scholar] [CrossRef]
- Mecler, N.; Rodrigues, R.M.; Silva, A.M.P.; Fernandes, A.C.; Almeida, B.M.; Gonçalves, L.S.; Canabarro, A.; Ferreira, D.C. Role of professional expertise in the decision-making process for periodontally compromised teeth. Gen. Dent. 2022, 70, 62–68. [Google Scholar]
- Moreira Paulo Tolentino, P.; Graziele Rodrigues, L.; Miranda de Torres, É.; Franco, A.; Ferreira Silva, R. Tooth Extractions in Patients with Periodontal Diseases and Clinical Decision-Making Process. Acta Stomatol. Croat. 2019, 53, 141–149. [Google Scholar] [CrossRef]
- Bishti, S.; Lautensack, J.; Türp, J.C.; Wolfart, S. Does professional experience save teeth? A survey among prosthodontists. Clin. Oral Investig. 2018, 22, 1001–1008. [Google Scholar] [CrossRef] [PubMed]
- Cosyn, J.; De Bruyn, H. Interclinician disparity in periodontal decision making: Need for consensus statements on surgical treatment. J. Periodontal. Res. 2007, 42, 311–317. [Google Scholar] [CrossRef]
- Williams, K.B.; Burgardt, G.J.; Rapley, J.W.; Bray, K.K.; Cobb, C.M. Referring periodontal patients: Clinical decision making by dental and dental hygiene students. J. Dent. Educ. 2014, 78, 445–453. [Google Scholar] [CrossRef] [PubMed]
- Swigart, D.J.; Gurenlian, J.R.; Rogo, E.J. Dental hygiene diagnosis: A qualitative descriptive study of dental hygienists. Can. J. Dent. Hyg. 2020, 54, 113. [Google Scholar]
- Keys, T.; Burrow, M.F.; Rajan, S.; Rompre, P.; Doméjean, S.; Muller-Bolla, M.; Manton, D.J. Carious lesion management in children and adolescents by Australian dentists. Aus. Dent. J. 2019, 64, 282–292. [Google Scholar] [CrossRef]
- Al-Baghdadi, M.; Green, R.; Durham, J.; Steele, J.; Araujo-Soares, V. Decision-making in the management of TMJ disc displacement without reduction: A qualitative study. J. Dent. 2019, 91, 103223. [Google Scholar] [CrossRef]
- Korduner, E.K.; Collin Bagewitz, I.; Vult von Steyern, P.; Wolf, E. Prosthodontic decision-making relating to dentitions with compromised molars: The perspective of Swedish General Dental Practitioners. J. Oral Rehabil. 2016, 43, 967–976. [Google Scholar] [CrossRef]
- Maidment, Y.; Durey, K.; Ibbetson, R. Decisions about restorative dental treatment among dentists attending a postgraduate continuing professional development course. Br. Dent. J. 2010, 209, 455–459. [Google Scholar] [CrossRef] [PubMed]
- Yusof, Z.Y.; Han, L.J.; San, P.P.; Ramli, A.S. Evidence-based practice among a group of Malaysian dental practitioners. J. Dent. Educ. 2008, 72, 1333–1342. [Google Scholar] [CrossRef]
- Barber, A.; Puryer, J.; Leary, S.; McNally, L.; O’Sullivan, D. Attitudes towards prosthodontic clinical decision-making for edentulous patients among south west deanery dental foundation year one dentists. Dent. J. 2016, 4, 12. [Google Scholar] [CrossRef]
- Azarpazhooh, A.; Dao, T.; Ungar, W.J.; Chaudry, F.; Figueiredo, R.; Krahn, M.; Friedman, S. Clinical decision making for a tooth with apical periodontitis: The patients’ preferred level of participation. J. Endod. 2014, 40, 784–789. [Google Scholar] [CrossRef] [PubMed]
- Özhayat, E.B.; Gotfredsen, K.; Elverdam, B.; Scient, M.; Öwall, B. Patient-Generated Aspects in Oral Rehabilitation Decision Making. II. Comparison of an Individual Systematic Interview Method and the Oral Health Impact Profile. Int. J. Prosthodont. 2010, 23, 421–428. [Google Scholar] [PubMed]
- Özhayat, E.B.; Gotfredsen, K.; Elverdam, B.; Öwall, B. Patient-generated aspects in oral rehabilitation decision making I. Comparison of traditional history taking and an individual systematic interview method. J. Oral Rehabil. 2009, 36, 726–736. [Google Scholar] [CrossRef] [PubMed]
- Gilmore, D.; Sturmey, P.; Newton, J.T. A comparison of the impact of information from a clinician and research-based information on patient treatment choice in dentistry. J. Public Health Dent. 2006, 66, 242–247. [Google Scholar] [CrossRef]
- Schouten, B.C.; Eijkman, M.A.; Hoogstraten, J. Information and participation preferences of dental patients. J. Dent. Res. 2004, 83, 961–965. [Google Scholar] [CrossRef]
- Watted, N.; Witt, E.; Bill, J.S. A therapeutic concept for the combined orthodontic surgical correction of angle Class II deformities with short-face syndrome: Surgical lengthening of the lower face. Clin. Orthod. Res. 2000, 3, 78–93. [Google Scholar] [CrossRef] [PubMed]
- Carbone, S.; Kokorelias, K.M.; Berta, W.; Law, S.; Kuluski, K. Stakeholder involvement in care transition planning for older adults and the factors guiding their decision-making: A scoping review. BMJ Open 2022, 12, e059446. [Google Scholar] [CrossRef]
- Tuzoff, D.V.; Tuzova, L.N.; Bornstein, M.M.; Krasnov, A.S.; Kharchenko, M.A.; Nikolenko, S.I.; Sveshnikov, M.M.; Bednenko, G.B. Tooth detection and numbering in panoramic radiographs using convolutional neural networks. Dent. Radiol. 2019, 48, 20180051. [Google Scholar] [CrossRef]
- Nam, Y.; Kim, H.G.; Kho, H.S. Differential diagnosis of jaw pain using informatics technology. J. Oral Rehabil. 2018, 45, 581–588. [Google Scholar] [CrossRef]
- Li, S.; Williams, K.S.; Medam, J.K.; Patel, J.S.; Gonzalez, T.; Thyvalikakath, T.P. Retrospective Study of the Reasons and Time Involved for Dental Providers’ Medical Consults. Front. Digit. Health 2022, 4, 838538. [Google Scholar] [CrossRef] [PubMed]
- Perakis, N.; Cocconi, R. The decision-making process in interdisciplinary treatment: Digital versus conventional approach. A case presentation. Int. J. Esthet. Dent. 2019, 14, 212–224. [Google Scholar] [PubMed]
- Deshpande, S.; Chahande, J.; Rathi, A. Mobile learning app: A novel method to teach clinical decision making in prosthodontics. Educ. Health 2017, 30, 31. [Google Scholar] [CrossRef] [PubMed]
- White, J.M.; Kalenderian, E.; Stark, P.C.; Ramoni, R.L.; Vaderhobli, R.; Walji, M.F. Evaluating a dental diagnostic terminology in an electronic health record. J. Dent. Educ. 2011, 75, 605–615. [Google Scholar] [CrossRef]
- Rios Santos, J.V.; Castello Castaneda, C.; Bullón, P. Development of a computer application to help in the decision-making process in teaching dentistry. Med. Oral Patol. Oral Cir. Bucal 2008, 13, E65–E70. [Google Scholar] [PubMed]
- Korsch, M.; Walther, W.; Robra, B.; Sahin, A.; Hannig, M.; Bartols, A. How do specialist surgeons treat the atrophic tooth gap? A vignette-based study among maxillofacial and oral surgeons. BMC Oral Health. 2021, 21, 331. [Google Scholar] [CrossRef] [PubMed]
- Chatzopoulos, G.; Koidou, V.; Lunos, S.; Wolff, L. Implant and root canal treatment: Survival rates and factors associated with treatment outcome. J. Dent. 2018, 71, 61–66. [Google Scholar] [CrossRef]
- Tarnow, D.; Chu, S. When to save or remove implants in the smile zone: A clinical report of maxillary lateral incisor implants in malposition. Jf Esthet. Restor. Dent. 2021, 33, 194–201. [Google Scholar] [CrossRef]
- Eliyas, S.; Porter, R. An impossible choice: MRONJ vs ORN? The difficulties of the decision-making process for head and neck cancer patients on long-term anti-angiogenic medication. Br. Dent. J. 2020, 229, 587–590. [Google Scholar] [CrossRef]
- Brescia, G.; Fusetti, S.; Apolloni, F.; Marioni, G.; Saia, G. Displaced Dental Materials in the Maxillary Sinus: An Original Series. Analysis and Definition of a Surgical Decision-Making Process. Ann. Otol. Rhinol. 2019, 128, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Amadi, J.; Delitala, F.; Liberatore, G.; Scozzafava, E.; Brevi, B. Treatment decision-making for a post-traumatic malocclusion in an elderly patient: A case report. Dent. Traumatol. 2021, 37, 725–731. [Google Scholar] [CrossRef] [PubMed]
- Abbas, B.; Maqsood, A.; Rahat Geelani, S.; Sattar, M.; Rahim, M.; Khurshid, Z. Estimating the Need for Sedation in Patients with Dental Anxiety and Medical Complexities Reporting to Tertiary Care Dental Hospital Using the IOSN Tool. Int. J. Dent. 2022, 2022, 5824429. [Google Scholar] [CrossRef] [PubMed]
- Hänsel Petersson, G.; Åkerman, S.; Isberg, P.; Ericson, D. Comparison of risk assessment based on clinical judgement and Cariogram in addition to patient perceived treatment need. BMC Oral Health 2016, 17, 13. [Google Scholar] [CrossRef] [PubMed]
- Radcliffe, K.; Lyson, H.C.; Barr-Walker, J.; Sarkar, U. Collective intelligence in medical decision-making: A systematic scoping review. BMC Med. Inform. Decis. Mak. 2019, 19, 158. [Google Scholar] [CrossRef] [PubMed]
- Brammer, R. Effects of experience and training on diagnostic accuracy. Psychol. Assess. 2002, 14, 110. [Google Scholar] [CrossRef]
- Abbey, L.M. Computer Based Decision Support: The Substrate for Dental Practice in the 21st Century. J. Dent. Educ. 1991, 55, 262–263. [Google Scholar] [CrossRef] [PubMed]
- Chan, H.P.; Hadjiiski, L.M.; Samala, R.K. Computer-aided diagnosis in the era of deep learning. Med. Phys. 2020, 47, e218–e227. [Google Scholar] [CrossRef]
- Alghazzawi, T.F. Advancements in CAD/CAM technology: Options for practical implementation. J. Prosthodont. Res. 2016, 60, 72–84. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).