Abstract
Background: To qualitatively and quantitatively review the reliability of palatal rugae as a tool for personal identification following orthodontic treatment. Methods: Cross-sectional retrospective studies assessing the accuracy of matching palatal rugae pattern pre- and post-orthodontic treatment were identified from PubMed and SCOPUS databases. The title and abstract of the articles identified in the search were screened for potential duplicates and relevancy to the topic of interest. The full text of the articles selected in the screening was analyzed using the inclusion and exclusion criteria. Quantitative analysis of the studies representing coherent data in terms of age and treatment choice was performed using RevMan software. Results: Out of 64 screened articles, only 18 articles fulfilled the eligibility criteria and were included in the systematic review. Out of these 18 articles, only 3 studies had data compatible with the quantitative analysis. Significant changes were noted in lateral first rugae in transverse bilateral direction (p = 0.02) and between second and third lateral rugae of the left side in the anteroposterior direction (p = 0.04). Despite the dimensional changes, observers in most studies were able to accurately (>90%) match the palatal rugae pre- and post-orthodontic treatment through visual observation. Conclusion: The accuracy of the visual matching, despite the significant dimensional changes, indicates that morphology could have potentially been the major matching factor. Thus, a combination of dimensional and morphological evaluation of the palatal rugae could potentially increase the accuracy of personal identification.
1. Introduction
Palatal rugae are the irregular connective tissue also known as “plicae palatinae”. These are anatomical folds located posterior to the incisive papilla in the palatal anterior third. These folds, which form as early as 3 months in utero, are largely attributed to the hardened connective tissue that covers the bone. Their orientation and pattern are formed in the fourth month of intrauterine life. Their uniqueness lies in the fact that they are stable and show post-mortem resistance [1] until oral mucosal degeneration after death [2,3]. Their anatomical location on the internal aspect of the oral cavity protects them from different environmental factors including rising temperature, palatal infections, trauma, and tooth exfoliation and eruption [4,5,6]. They are considered suitable landmarks for forensic identification [7,8,9].
Palatine rugae analysis has been proved to be a good alternative or adjunct method for identification where teeth are lost. Allen proposed its potential role as a means for personal identification in 1889 and the term “Palatal rugoscopy” was first proposed by the Spanish investigator Trobo Hermosa in 1932 [10]. Palatal rugae can be recorded through casts or plaster models, which act as an essential aid in orthodontic diagnosis and treatment planning [9]. However, with evolving technology, diagnostic tools have evolved into digitized mapping and 3D scanning [11,12].
Though palatal rugae are still considered a reliable tool for identification, it is imperative to acknowledge rugae patterns can undergo changes due to several factors including orthodontic treatments, surgical palatal repairs, and extractions of adjacent teeth [13,14,15]. Questions have also been raised as to the growth-related stability of the rugae. Given the increasing literature suggesting the instability of palatal rugae, there appears to be a lack of consensus in identifications made solely based on the palatal rugae. Among the various factors suggested that cause changes in the palatal rugae, the effect of orthodontic treatment is the most well-explored. Thus, the present systematic review and meta-analysis were formulated to qualitatively and quantitatively analyze the effect of orthodontic treatment on the stability of palatine rugae.
2. Materials and Methods
Protocol and registration: PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) and MOOSE (Meta-Analysis of Observational Studies in Epidemiology) guidelines were strictly adhered to in the present systematic review and meta-analysis. The PROSPERO registration number for the review is CRD42020214804.
Inclusion criteria: Original studies in the English language discussing any changes in the palatal rugae pattern before and after orthodontic treatment were included.
Exclusion criteria: Reviews, short articles (commentary, letters, correspondent pieces), and articles not in the English language were excluded.
Focused question: “Are palatal rugae a reliable marker for personal identification following orthodontic treatment?”
Search strategy: Databases including the SCOPUS and PubMed were used for mining the data. Any relevant articles obtained from cross-referencing the screened articles were also included if they satisfied the inclusion criteria. Medical subject heading combinations, including Palatal rugae and forensic odontology, Palatal rugae and orthodontic treatment, Palatal rugae and orthodontic treatment, and forensic odontology were used for mining the data.
Study selection and data extraction: The review was conducted in two steps by two reviewers (S.S.K. and A.A.G.) as follows:
1st step: All the identified articles were screened using their title and abstract. Duplicates and articles irrelevant to the topic of interest were excluded.
2nd step: The articles included from the 1st step were analyzed using their full texts. Articles not satisfying the inclusion criteria were excluded.
Vital data including the sample details, orthodontic treatment modality employed, and the mean changes noted in the palatal rugae were retrieved from the included studies.
Statistical analysis: Kappa statistics were used to assess the inter-observer reliability (Cohen’s kappa coefficient [κ]) between SK and AG. Quantitative analysis of the studies representing coherent data in terms of age and treatment choice has been performed using RevMan software, Version 5.4. Risk of bias analysis: Joanna Briggs’s critical appraisal tool for cross-sectional studies was employed to assess the risk of bias in the included studies. The reason for considering all the included studies as cross-sectional was that although the data of pre- and post-orthodontic treatment were extracted, they were extracted at a single time point as retrospective data.
3. Results
Study selection: The workflow of systematic review has been summarized in Figure 1. A total of 64 articles, including 31 from PubMed and 33 from Scopus, have been retrieved using the keywords. Screening the titles and abstracts of the identified articles revealed that 40 articles were either duplicate or were not related to the topic of interest and thus were excluded. The full text of the remaining 24 articles was assessed using the selection criteria. Only 18 fulfilled the eligibility criteria and were included in the systematic review. κ value of 0.96 and 0.98 was obtained for the 1st and 2nd step of the review process, indicating a good overall inter-observer reliability. Table 1 summarizes the data extracted from the included studies.
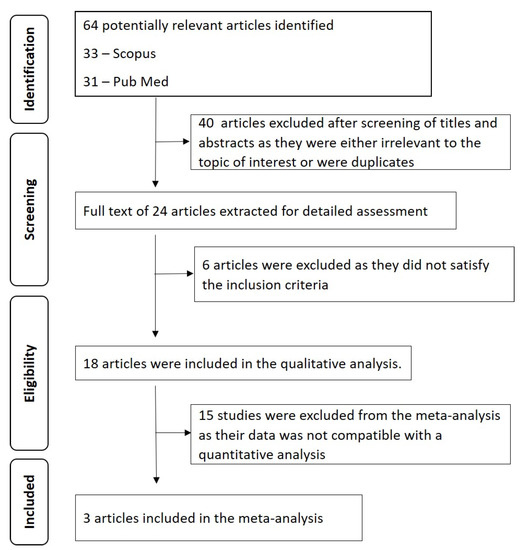
Figure 1.
Prisma flowchart summarizing the workflow of the systematic review.

Table 1.
Summary of the data extracted from the included studies.
Joanna Brigg’s risk of bias assessment: Out of 18 studies, 11 showed a moderate risk of bias [8,19,20,22,24,26,27,29,30,31,32] and 7 showed a low risk of bias [16,17,18,21,23,25,28] (Table 2). Inclusion criteria have been properly defined by seven studies [17,18,21,23,25,28,32]. Details of the subjects included in the studies, objectives, and standard criteria used for the measurement and the reliability and validity of the exposure measurement tool have been described by thirteen studies [8,16,17,18,19,20,21,22,23,24,25,26,28]. Five studies did not provide details of the selected subjects [27,29,30,31,32]. Confounding factors were considered in three studies [16,23,25]. Reliability in outcome measurement and appropriate statistical analysis were assessed in all eighteen studies.

Table 2.
Joanna Brigg’s risk of bias assessment of the included studies.
Study characteristics: Of the studies included in the review, six were from India [16,18,19,27,32], four from the United States of America [17,19,22,24], two from China [23,25], and one each from Japan [20], Egypt [21], Greece [26], Portugal [28], Jordan [30], and Pakistan [31]. All the included studies compared the palatal rugae pre- and post-orthodontic treatment. The orthodontic treatments used in the included studies were rapid maxillary expansion [18,32], retraction of maxillary anterior teeth with straight wire with or without extraction [8,19,20,21,22,23], use of headgears, and functional appliances including fixed orthodontic appliances [24,31] and pre-adjusted edgewise therapy [29].
Diagnostic Modalities used for comparing palatal rugae pre and post orthodontic treatment: Methods for evaluating the rugae included the use of plaster models or casts. Some authors also used 3D images of casts, scanning of the cast using a Simplex DP 30 computer scanner, and lateral cephalometric radiographs, while some studies included digital images of palatal rugae with DSLR [17,20,21,22,23]. Subjective assessment of casts was carried out by evaluating by visual matching by observers [19,23,25,26,28,29,30,32]. For objective evaluation, most of the studies used medial and lateral points of all the three rugae as landmarks and evaluated transverse and anteroposterior distances between them [8,17,18,19,20,21,24,30,32]. Other dimensional measurements in the included studies were: measurement of the perpendicular distances from the medial and lateral points until the mid-palatal raphae [21,24]; measurement of the inter-canine distance and evaluation of the ratio between inter-canine width and lateral dimension of the 3rd rugae [27]; evaluation of the molar and incisor movements relative to each ruga before and after treatment [22].
Qualitative analysis of the effect of orthodontic treatment on the palatal rugae: The studies gave conflicting results on the stability of the rugae pattern after orthodontic treatments. Shetty, D. et al., Xiu-Ping Wu et al., Jang, I. et al., Shukla, D. et al., Li, B. et al., Stavrianos, C. et al., Samyukta S, Abilasha R and Abdul Aziz, and H.M. et al. reported that the changes occurring with orthodontic treatment do not significantly alter the rugae patterns and hence rugae patterns can be used as reliable forensic markers [16,19,20,21,23,25,26,27]. Braga S and Caldas IM and Ali, B. et al. reported that only shapes (morphology) of palatal rugae can be considered a reliable marker for forensic identification but not the lengths (dimensions) [28,31]. Abdul Aziz, H.M. et al. and Shukla, D. et al. stated that the third palatal rugae are the most stable landmark to be used in forensic odontology [19,21]. Jang, I. et al. went one step further and reported the medial points of the third palatal rugae to be the most stable [20]. Bailey, L.J. et al. reported the usage of both medial and lateral points of the third palatal rugae as stable anatomic reference points [8]. Almeida, M.A. et al. questioned the stability of lateral points of all the three rugae and stressed the usage of medial points as stable reference points [24]. Kapoor P and Miglani R recorded the transverse changes in the rugae pattern in the order of 3rd rugae > 2nd rugae > 1st rugae [18]. Deepak, V. et al. and Mustafa, A. G. et al., however, questioned the reliability of these palatine rugae as forensic markers [29,30].
Quantitative analysis of the effect of orthodontic treatment on the palatal rugae: Out of the 18 studies in the systematic review, only 6 studies provided objective measurement in palatal rugae pattern (transverse or anteroposterior) concerning their medial and lateral points before and after orthodontic treatment [8,17,19,20,21,24]. The remaining 12 studies either presented only subjective data related to the morphological pattern of rugae or objective data (inter-canine width, distance from the molars and incisors) not related to transverse or anteroposterior measurements of the medial and lateral points of the rugae. In some studies, only visual matching by observers was used as the assessing tool. Also, 18 studies included in the systematic review differed in several parameters in their methodologies including the age of subjects selected, choice of treatment, duration of treatment, etc. Due to these methodological variations, only three studies with objective data could be included in the meta-analysis where the choice of treatment and age of the study participants were similar [8,19,21].
Data from the three studies included in the meta-analysis was converted to mm (eg: 1 pixel = 0.264558 mm for an image of 96 dpi and 1 pixel = 0.08466 mm for an image of 300 dpi). The relevant data, including mean deviations before and after orthodontic treatment and respective standard deviations, were used to create a forest plot with the help of Revman software (Figure 2 and Figure 3). As depicted by the meta-analysis and the forest plots, significant changes have been observed in the lateral first rugae in transverse bilateral direction (p = 0.02) and two to three lateral rugae of the left side in the anteroposterior direction (p = 0.04). There were no significant changes noted in the rest of the assessed rugae dimensions.
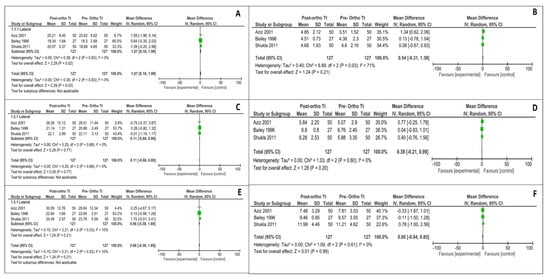
Figure 2.
Meta-analysis summarizing the effect of the orthodontic treatment on the transverse dimensions. (A) Transverse bilateral changes in first palatal rugae (lateral); (B) Transverse bilateral changes in first palatal rugae (medial); (C) Transverse bilateral changes in second palatal rugae (lateral); (D) Transverse bilateral changes in second palatal rugae (medial); (E) Transverse bilateral changes in third palatal rugae (lateral); (F) Transverse bilateral changes in third palatal rugae (medial).
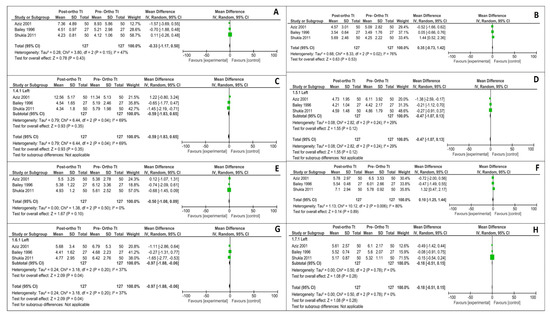
Figure 3.
Meta-analysis summarizing the effect of the orthodontic treatment on the anteroposterior dimensions. (A) Antero-posterior changes between 1–2 rugae of right side (lateral); (B) Antero-posterior changes between 1–2 rugae of right side (medial); (C) Antero-posterior changes between 1–2 rugae of left side (lateral); (D) Antero-posterior changes between 1–2 rugae of left side (medial); (E) Antero-posterior changes between 2–3 rugae of right side (lateral); (F) Antero-posterior changes between 2–3 rugae of right side (medial); (G) Antero-posterior changes between 2–3 rugae of left side (lateral); (H) Antero-posterior changes between 2–3 rugae of the left side (medial).
4. Discussion
Palatal rugae are often used as an identification tool in forensic dentistry as the tissue is resistant to decomposition due to the protection rendered by the buccal pad of fat and teeth. Also, similar to the fingerprint, the palatal rugae pattern is unique for every individual and allows identification. The age changes in the palatal rugae pattern are minimal and hence could aid as an adjunct tool in forensic dentistry, especially in edentulous patients. However, significant changes in the rugae pattern could occur as a result of surgery, orthodontic treatment (which could range from minor corrections in the alignment of teeth to complicated procedures such as arch expansion, use of headgears, functional appliances, and orthognathic surgery), or extraction of teeth. Considerable published literature is available that has assessed and reported the palatal rugae pattern before and after orthodontic treatment. With the available information, the present systematic review with meta-analysis was formulated to assess the reliability of palatal rugae for personal identification following orthodontic treatment.
In the present systematic review, the nature of orthodontic treatment in the included articles ranged from rapid maxillary [18,32], retraction of maxillary anterior teeth with straight wire with or without extraction [8,19,20,21,22,23], use of headgears and functional appliances including fixed orthodontic appliances [24,31], and pre-adjusted edgewise therapy [29]. The diagnostic modalities used for the assessment of palatal rugae patterns varied among the included studies, leading to heterogeneity. However, Taneva, E.D. et al. had compared two different techniques for the assessment of the rugae pattern and reported no significant differences in the two techniques [17]. Hence it may be potentially inferred that the variations in the palatal rugae pattern reported by the included study due to the differences in the diagnostic modalities could be minimal.
Most of the included studies demonstrated no significant changes in morphologic alterations in the rugae pattern following orthodontic treatment and thus concluded that palatal rugae could be considered a reliable tool in forensic dentistry. Also, few studies had reported that the third palatal rugae were the most reliable landmark for forensic identification [7,8,18,20,21,24]. Considering the stability of medial and lateral points of the palatal rugae in rendering accurate forensic information, contradictory results were reported in the published data included in the present review. While Jang, I. et al. and Almeida, M.A. et al. reported the medial points of the third palatal rugae to be most stable, Bailey, L.J. et al. reported that both medial and lateral points of the third palatal rugae were stable anatomic reference points [8,20,24]. These differences could be attributed to the type of orthodontic treatment rendered to the study participants and the sample size employed in the studies.
On the contrary, few studies have reported changes in the palatal rugae pattern following orthodontic treatment. Kapoor, P. and Miglani, R. reported that the 3rd rugae underwent maximum changes in the transverse pattern [18]. Deepak, V. et al. and Mustafa, A.G. et al. questioned the reliability of these palatine rugae as forensic markers [29,30]. This highlights the importance of maintaining dental records and cast models before and after orthodontic treatment, which could later render forensic information despite minor changes in the pattern. However, both the studies had a moderate risk of bias and did not report details of the selected study participants. The quantitative changes in the palatal rugae pattern before and after orthodontic treatment were assessed in only six out of the eighteen studies included. The remaining twelve studies had assessed only morphological alterations. However, only in three [8,19,21] out of six studies with quantitative data, the type of orthodontic treatment was similar and the age of the study participants was above 18 years. Age was a major factor as in participants below 18 years, the influence of the growth spurt on the rugae pattern could have been a potential confounder. A meta-analysis of the three studies revealed a significant transverse bilateral change in the lateral first rugae (p = 0.02) and anteroposterior change in the 2–3 lateral rugae of the left side (p = 0.04), respectively. There were no significant changes in the other rugae points assessed. The significant quantitative change in the transverse dimension of the lateral first rugae and the anteroposterior dimension of the second to third lateral rugae could be attributed to the fact that in all three studies, retraction of maxillary anterior teeth was carried out along with the extraction of premolars. Considering the role of tooth extraction on the palatal rugae pattern, very few studies had compared the changes in rugae pattern and reported no significant difference in the morphological pattern, while a few studies had only assessed the rugae pattern with orthodontic treatment and extraction [8,19,20,21,22,23]. However, in the present meta-analysis, we observed quantitative change in a transverse direction. Hence, the results must be viewed with caution owing to the heterogeneity of data and sample size. Further studies have to be carried out to assess the exact role of extraction on palatal rugae patterns [8,19,21].
Shukla, D. et al., Aziz, H.M.A., and Sabet, N.E. assessed the quantitative changes in right and left palatal rugae in the anteroposterior direction [19,21]. Comparison of quantitative changes in the anteroposterior direction of palatal rugae in various types of orthodontic treatment including extraction, non-extraction, head-gear, and functional appliance was reported by Bailey, L.J. et al. and Almeida, M.A. et al. [8,24]. However, the third rugae were found to be more stable in comparison with the first and second, which is concurrent with the previously reported literature on the stability in the morphologic pattern of the third rugae. Despite significant overall dimensional changes, observers were able to make a highly accurate (>90%) matching between the pre- and post-treatment casts using the morphological pattern of the rugae. This can be explained by the observations of the individual studies wherein the morphological pattern of the rugae was reported to be unchanged [16,19,25,28,31,32] despite the orthodontic treatment. Palatal rugae can thus be a reliable tool for personal identification by a combination of objective assessment of the morphologic pattern of palatal rugae and quantitative dimensional assessment, thereby reducing intraobserver and interobserver bias. Also, the findings of the present review must be viewed with caution, considering the moderate risk of bias in 11 of the included studies. Future studies assessing the changes in palatal rugae patterns following orthodontic treatment must focus on minimizing the confounding factors. Studies on the duration of stability of palatal rugae with changes in body weight also have to be conducted to determine the reliability of palatal rugae patterns as forensic tools.
5. Conclusions
Based on the results of the quantitative analysis, significant changes were noted in the lateral first rugae in the transverse bilateral direction (p = 0.02) and between the second and third lateral rugae of the left side in the anteroposterior direction (p = 0.04). Hence, identification made solely based on the dimensional parameters of landmarks of the palatine rugae may not be a reliable tool for personal identification. However, the qualitative review revealed that the observers, through visual comparison of the casts, were able to match pre- and post-orthodontic casts accurately (>90%). During the visual comparison, no objective measurements are taken into account. Thus, the matching is purely subjective and could potentially carry significant inter-observer bias. The accuracy (>90%) of matching noted in the review despite the non-significant dimensional changes could indicate the relative stability of the rugae morphology. It is also likely that there are changes in the morphology that are not perceived by the human eye, which, in the present scenario, led to increased accuracy in matching. Despite the high matching obtained from the visual comparison, it is vital to acknowledge its inherent subjectivity. Combining the dimensional quantitative measurements with morphology could potentially overcome the inter-observer bias and increase the accuracy of palatine rugae-based personal identification. Also, future studies must integrate 3D digital images of the palatal rugae (pre- and post-orthodontic treatment) with artificial intelligence (AI), as, unlike a human eye, the AI would be able to perceive even the mildest of changes and provide an objective assessment of the effect of the orthodontic treatment on the palatal rugae.
Author Contributions
Conceptualization, A.A.G., S.K., and A.A.; methodology, W.A. and Z.H.A.; software, S.M.A.F. and S.K.; validation, S.V., A.A.G., S.M., and Z.K; formal analysis, V.P.V. and G.S.; investigation, A.A. and W.A.; resources, H.D.; data curation, Z.K. and S.P.; writing—original draft preparation, A.A.G., S.S.K., A.A., W.A., Z.H.A., S.M.A.F., and S.S.K.; writing—review and editing, S.M., H.D., Z.K., V.P.V., S.V., G.S., and S.P.; visualization, G.S. and S.M.A.F.; supervision, Z.H.A. and H.D.; project administration, S.P. and A.A.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Tonge, C.H.; Luke, D.A. Dental anatomy: The palate. Dent. Updat. 1985, 12, 461–467. [Google Scholar]
- Hauser, G.; Daponte, A.; Roberts, M.J. Palatal rugae. J. Anat. 1989, 165, 237–249. [Google Scholar] [PubMed]
- Buchtová, M.; Tichý, F.; Putnová, I.; Míšek, I. The development of palatal rugae in the European pine vole, Microtus subterraneus (Arvicolidae, Rodentia). Folia Zool. 2003, 52, 127–136. [Google Scholar]
- Figini, A.R.d.L.; Leitão e Silva, J.R.; Jobim, L.F.; Silva, M.d. Identificaҫão Humana, 2nd ed.; Millennium: Campinas, Brazil, 2003; ISBN 9788576250029. [Google Scholar]
- Muthusubramanian, M.; Limson, K.S.; Julian, R. Analysis of rugae in burn victims and cadavers to simulate rugae identification in cases of incineration and decomposition. J. Forensic Odontostomatol. 2005, 23, 26–29. [Google Scholar] [PubMed]
- Sivaraj, A. Significance of Palatal Rugae in Orthodontics. J. Orofac Res. 2013, 3, 202–209. [Google Scholar] [CrossRef]
- Yamazaki, Y. Cross-sectional study of plicae palatinae transversae in the Japanese. Antrhopol. Rep. Niigata 1962, 34, 59–76. [Google Scholar]
- Bailey, L.B.J.; Abbas, E.; Almeida, M.A. Stability of the Palatal Rugae as Landmarks for Analysis of Dental Casts in Extraction and Nonextraction Cases. Angle Orthod. 1996, 66, 73–78. [Google Scholar] [CrossRef]
- English, W.R.; Robison, S.F.; Summitt, J.B.; Oesterle, L.J.; Brannon, R.B.; Morlang, W.M. Individuality of Human Palatal Rugae. J. Forensic Sci. 1988, 33, 12479J. [Google Scholar] [CrossRef]
- Moya Pueyo, V.; Roldán Garrido, B.; Sánchez Sánchez, J.A.; Bascones Martínez, A. Odontología Legal y Forense; Masson: Issy-les-Moulineaux, France, 1994; ISBN 8431106646. [Google Scholar]
- Patzelt, S.B.M.; Emmanouilidi, A.; Stampf, S.; Strub, J.R.; Att, W. Accuracy of full-arch scans using intraoral scanners. Clin. Oral Investig. 2014, 18, 1687–1694. [Google Scholar] [CrossRef]
- Kravitz, N.D.; Groth, C.; Jones, P.E.; Graham, J.W.; Redmond, W.R. Intraoral digital scanners. J. Clin. Orthod. 2014, 48, 337–347. [Google Scholar]
- Kim, H.K.; Moon, S.C.; Lee, S.J.; Park, Y.S. Three-dimensional biometric study of palatine rugae in children with a mixed-model analysis: A 9-year longitudinal study. Am. J. Orthod. Dentofac. Orthop. 2012, 141, 590–597. [Google Scholar] [CrossRef] [PubMed]
- Simmons, J.D.; Moore, R.N.; Erickson, L.C. A Longitudinal Study of Anteroposterior Growth Changes in the Palatine Rugae. J. Dent. Res. 1987, 66, 1512–1515. [Google Scholar] [CrossRef] [PubMed]
- Barbieri, A.A.; Scoralick, R.A.; Naressi, S.C.M.; Moraes, M.E.L.; Daruge, E. The Evidence of the Rugoscopy Effectiveness as a Human Identification Method in Patients Submitted to Rapid Palatal Expansion. J. Forensic Sci. 2013, 58. [Google Scholar] [CrossRef] [PubMed]
- Shetty, D.; Chowdhary, M.; Gupta, A.; Juneja, A.; Jain, A.; Khanna, K.; Pruthi, N. Assessment of palatal rugae pattern and their reproducibility for application in forensic analysis. J. Forensic Dent. Sci. 2013, 5, 106. [Google Scholar] [CrossRef] [PubMed]
- Taneva, E.; Johnson, A.; Viana, G.; Evans, C. 3D evaluation of palatal rugae for human identification using digital study models. J. Forensic Dent. Sci. 2015, 7, 244. [Google Scholar] [CrossRef] [PubMed]
- Kapoor, P.; Miglani, R. Transverse changes in lateral and medial aspects of palatal rugae after mid palatal expansion: A pilot study. J. Forensic Dent. Sci. 2015, 7, 8. [Google Scholar] [CrossRef] [PubMed]
- Shukla, D.; Chowdhry, A.; Bablani, D.; Jain, P.; Thapar, R. Establishing the reliability of palatal rugae pattern in individual identification (following orthodontic treatment). J. Forensic Odontostomatol. 2011, 29, 20–29. [Google Scholar]
- Jang, I.; Tanaka, M.; Koga, Y.; Iijima, S.; Yozgatian, J.H.; Cha, B.K.; Yoshida, N. A novel method for the assessment of three-dimensional tooth movement during orthodontic treatment. Angle Orthod. 2009, 79, 447–453. [Google Scholar] [CrossRef]
- Abdel-Aziz, H.M.; Sabet, N.E. Palatal rugae area: A landmark for analysis of pre- and post-orthodontically treated adult Egyptian patients. East. Mediterr. Health J. 2001, 7, 60–66. [Google Scholar] [CrossRef]
- Hoggan, B.R.; Sadowsky, C. The use of palatal rugae for the assessment of anteroposterior tooth movements. Am. J. Orthod. Dentofac. Orthop. 2001, 119, 482–488. [Google Scholar] [CrossRef]
- Xiu-Ping, W.; Jian-Ning, H.; Pan, F.; Yu-Jin, W.; Li, B. Analysis of Palatal Rugae Morphology Before and After Orthodontic Treatment by a Digital Image Recognition System. Int. J. Morphol. 2017, 35, 420–424. [Google Scholar] [CrossRef]
- Almeida, M.A.; Phillips, C.; Kula, K.; Tulloch, C. Stability of the palatal rugae as landmarks for analysis of dental casts. Angle Orthod. 1995, 65, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Bing, L.; Kwon, T.-G.; Xiao, W.; Kyung, H.-M.; Yun, K.-M.; Wu, X.-P. Model Analysis of Anatomical Morphology Changes of Palatal Rugae Before and After Orthodontic Treatment. Int. J. Morphol. 2017, 35, 1224–1229. [Google Scholar] [CrossRef][Green Version]
- Stavrianos, C.; Ioannidou-Marathiotou, I.; Pantelidou, O.; Petalotis, N.; Samara, E.; Tatsis, D. In vitro examination of credibility of general and specific morphological characteristics of human palatal rugae in the process of recognition/identification or disassociation. Res. J. Med. Sci. 2012, 6, 261–265. [Google Scholar]
- Samyukta, S.; Abilasha, R. Relationship of the lateral dimension of the palatal rugae to the width of the palate. Int. J. Pharm. Technol. 2016, 8, 18284–18289. [Google Scholar]
- Braga, S.; Caldas, I.M. Study of palatal rugae pattern following orthodontic treatment. Aust. J. Forensic Sci. 2016, 48, 305–311. [Google Scholar] [CrossRef]
- Deepak, V.; Malgaonkar, N.I.; Shah, N.K.; Nasser, A.S.; Dagrus, K.; Bassle, T. Palatal rugae patterns in orthodontically treated cases, are they a reliable forensic marker? J. Int. Oral Health JIOH 2014, 6, 89–95. [Google Scholar]
- Mustafa, A.G.; Allouh, M.Z.; Alshehab, R.M. Morphological changes in palatal rugae patterns following orthodontic treatment. J. Forensic Leg. Med. 2015, 31, 19–22. [Google Scholar] [CrossRef]
- Ali, B.; Shaikh, A.; Fida, M. Stability of Palatal Rugae as a Forensic Marker in Orthodontically Treated Cases. J. Forensic Sci. 2016, 61, 1351–1355. [Google Scholar] [CrossRef]
- Shailaja, A.; Umme Romana, I.; Narayanappa, G.; Smitha, T.; Gowda, N.; Vedavathi, H. Assessment of palatal rugae pattern and its significance in orthodontics and forensic odontology. J. Oral Maxillofac. Pathol. 2018, 22, 430. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).