Abstract
Poor sleep adversely affects health and may cause obesity. Poor sleep includes short sleep duration, low quality of sleep, and sleep discrepancy. Although most studies have focused on the association between sleep duration and obesity, poor sleep is a significant risk factor for obesity. Adolescents have characteristic sleep patterns which correspond to poor sleep. Adolescents sleep late due to various biological and psychosocial factors; also, they wake up early to be on time for school. This causes them to sleep less. To make up for this sleep debt, adolescents sleep more on non-school days, which causes sleep discrepancies. Therefore, since adolescents have characteristic sleep patterns, an in-depth investigation is needed to identify whether poor sleep is a risk for obesity. This article presents an overview of the characteristic sleep patterns of adolescents, and reviews studies on the association of each sleep pattern with obesity.
1. Introduction
Sleep plays an important role in health because poor sleep leads to adverse effects on health. Poor sleep, which includes deprivation, low quality, disruption, and discrepancy of sleep, not only causes sleepiness and decline in performance but is also linked to various health problems [1,2,3,4,5,6,7]. In particular, poor sleep is thought to be associated with obesity and metabolic disease [1], because obesity and sleep insufficiency increase in parallel [2]. Moreover, sleep duration and quality [4,8,9], as well as circadian systems [10] play important roles in metabolic regulation.
Over the last century, most countries have witnessed the prevalence of poor sleep among adolescents [11,12,13,14], which has adversely affected their health [5,6,15,16]. However, adolescents, unlike adults, have characteristic sleep patterns for physiological and psychosocial reasons. The sleep patterns in adolescents are characterized by delayed sleep phases, shorter sleep durations, and larger differences in sleep timing and duration between school and non-school days [17,18], all of which may result in poor sleep. Therefore, in the case of adolescents, the question of whether poor sleep affects obesity should be further discussed in consideration of these characteristic sleep patterns.
This review focuses on the links between poor sleep and obesity in adolescents. The poor sleep patterns in adolescents have been classified into three categories: short sleep duration, delayed sleep phase, and sleep discrepancy between school and non-school days. The effects of these sleep patterns on obesity in adolescents are reviewed in this paper. In addition, the recent findings on adolescent sleep status and sleep recommendations for adolescents are summarized.
2. Characteristic Sleep Patterns in Adolescents
Characteristic sleep patterns in adolescents comprise a delayed sleep phase (significant tendency towards later bedtimes and wake-up times), shorter sleep duration, and irregular sleep patterns across the week (discrepancy between weekdays and weekends). These sleep patterns are mainly regulated by biological and psychosocial factors.
2.1. Biological Factors
Biological factors affecting sleep patterns include circadian rhythms and homeostatic sleep systems. Circadian timing systems, which regulate the circadian rhythm, have been localized to the suprachiasmatic nuclei of the hypothalamus [19]. Circadian rhythm oscillates over a period of approximately 24 h and controls almost every function of metabolism from the sleep/wake cycle to fasting/feeding behavior [20]. It is a self-regulating and self-sustained clockwork mechanism that synchronizes with the solar cycle. The circadian rhythm is sensitive to light, especially during nighttime [21], and the daily variation of daylight and darkness is the primary synchronizing stimulus for the circadian rhythm [22]. Extended light at the end of daytime or beginning of nighttime moves the circadian rhythm later, and bright light at the end of nighttime or beginning of daytime moves the circadian rhythm earlier [23].
The melatonin hormone, secreted by the pineal gland, is associated with circadian rhythm, and is regulated with changes in the rhythm. Melatonin is rarely secreted during the daytime, but its secretion increases in the evening. Its level is maintained throughout the nighttime and falls when it is time to wake up. Similar to circadian rhythms, the secretion of melatonin is also suppressed by light [24], especially by the short-wavelength of ~460 nm [25], but also by ambient room light [26].
The homeostatic sleep system is dependent on prior sleep/wake conditions, i.e., extended wake attempts to sleep, and prolonged sleep tries to favor waking, regardless of the time of day. The homeostatic sleep system is primarily derived from the slow waves in the sleep electroencephalogram. The slow wave activity is sensitive to prior sleep/wake history, and increases with prolonged waking in a dose-dependent manner [27]. The slow-wave sleep is high at the beginning of the nocturnal sleep episode when sleep pressure is the greatest and declines over the night’s successive non-rapid eye movement episodes [28].
Adolescents show delayed sleep phases, marked by late sleeping and waking up habits [21]. Actigraphic sleep measurements reflect significant delays in sleep onset time with increasing age in adolescents [29]. This is because the circadian timing system changes during puberty due to a positive association of the pubertal stage with later circadian timing [30]. In addition, the release of nocturnal melatonin is delayed in adolescents, leading to a sleep phase delayed by approximately 2 h [31]. These changes reflect a normative developmental course of the circadian clock that shifts toward eveningness around puberty, peaks at around 16 years of age, and shifts back during early adulthood [21,32]. The later circadian timing was found to be related to a longer intrinsic period [33], and a slower accumulation of the “sleep drive” in adolescence [34], making it difficult for most adolescents to fall asleep early. Therefore, the sleep pattern in adolescents is delayed by 2–3 h relative to that in adults [35].
2.2. Psychosocial Factors
The circadian timing system undergoes developmental changes during adolescence due to behavioral factors, such as social and scholastic obligations [21]. In adolescence, the increasing demands for academic performance cause adolescents to stay awake longer, resulting in delayed sleep/wake cycles [21]. School-day bedtimes are clearly related to age, as adolescents go to bed later as they grow older [21,35]. Older adolescents have to spend more time on homework or academic activities after school, and as their academic needs increase, they have no choice but to go to bed later. Additionally, the recent development of social media and electronic devices, such as smartphones, encourages nighttime activity and further delays bedtime [36,37]. As the circadian rhythm is sensitive to nighttime light [21], an increased usage of electronic devices delays the circadian rhythm.
2.3. Sleep Phases and Duration
These biological and psychosocial factors affect not only the sleep phases but also sleep duration. Most teenagers have to wake up early to reach school on time; hence, they do not get enough sleep. Academic demands/stress and early school start times are the most important contributing factors for sleep deprivation among adolescents [13]. For example, older adolescents are more burdened with social and academic obligations than younger adolescents. Therefore, the older they are, the later the sleep phase is and the lesser is their duration of sleep [29,35,38,39]. However, later school start times are associated with longer sleep duration, primarily due to delayed wake-up times [40,41,42].
Sleep phases of adolescents have been described separately for school days and non-school days as adolescent sleep is typically more variable across a week. The sleep phase is similar among adolescents and adults on school days, but it is drastically delayed by 3 h on non-school days for adolescents, but by only 1 h in adults [43]. This means, physiologically and/or psychosocially, that the sleep phase in adolescents is delayed by 2 h relative to that in adults, and early school start times conflict with this sleep phase delay [21]. This causes a shorter duration of sleep, i.e., sleep debt during school days, and an attempt to catch up over the weekend, leading to greater differences in sleep patterns between school and non-school days [40]. In other words, adolescents tend to sleep longer and later on weekends and holidays to compensate for their physiological sleep pattern changes and sleep debts during the school days. In a meta-analysis, the mean non-school day bedtime was consistently later than the mean school day bedtime, but the significantly later non-school day wake-up time indicated that the mean sleep duration on non-school days was 91.6 min longer than that on school days [35]. The difference between the wake-up times on school days and non-school days was approximately 1.5–3 h for 10–13-year-old adolescents and 3–4 h for high school students [21]. These results indicate that sleep insufficiency on school days results in the creation of sleep debt, and is compensated by more later wake-up times on non-school days. This discrepancy in sleep times between school and non-school days is called “social jetlag”. Social jetlag was observed in all countries, as bedtimes were consistently later and sleep durations were always longer on non-school days than school days [39].
In summary, adolescents prefer late sleep phases, have a shorter sleep duration, and show a large discrepancy in sleep patterns between weekdays and weekends due to biological and psychosocial factors.
3. Association between Sleep Duration and Adolescent Obesity
As described above, adolescents sleep for a shorter duration because of the late sleep phase due to the physiological and psychosocial factors as well as the need to wake up early to be on time for school. Several studies investigating the link between sleep duration and obesity in adolescents have found that a short sleep duration increases the risk of obesity [44,45,46,47,48,49,50]. Sleep duration is strongly associated with body weight status [44], as objectively measured sleep duration is inversely associated with body mass index (BMI) [45,46,47,48,49,50]. In a cross-sectional and longitudinal study, the z-score for BMI decreased by −0.22 in the cross-sectional analyses and −0.05 in the longitudinal analysis for each additional hour of sleep [48]. Moreover, sleep duration in childhood affects body weight in adolescence, and age-appropriate sleep patterns in childhood have been found to be associated with adolescent body weight in a longitudinal study [16]. However, not all studies have shown that short sleep duration increases the risk of obesity in adolescents. Some studies have shown a non-significant association between sleep duration and BMI z-score [51,52,53,54,55,56].
Several meta-analyses [1,57,58,59,60,61,62,63,64,65] investigating the association between sleep duration and obesity/overweight status or BMI have shown that sleep duration affects obesity in adolescents (Table 1). Although one study did not specify the method of measuring sleep, three studies analyzed sleep status based on self-reporting and/or by parents, whereas the remaining studies objectively measured sleep duration in addition to self and/or parents’ reporting. Except for one meta-analysis [61], the remaining studies reported that short sleep duration had significantly higher risk of obesity/overweight status and/or increased BMI in pediatric populations [1,57,58,59,60,62,63,64,65]. Short sleep increased the risk of obesity/overweight status by as little as 1.40 times [64] and as much as 2.15 times [59] and decreased the BMI by −0.03 point for every additional hour of sleep [63]. Although one study failed to show a significant effect of sleep duration on changes in BMI, the authors stated that the improvement of sleep duration in children could affect their BMI, nutrition, and physical activity [61]. This is because in some of the studies reviewed by Yoong et al. [61], improvements in sleep duration resulted in weight/BMI loss, and restricted sleep duration increased total calorie intake and sweet/desert intake. Therefore, it is understood that sleep duration can increase the risk of obesity/overweight status in adolescents, despite inconsistency among the results.

Table 1.
Meta-analysis studies on the association between sleep duration and obesity in adolescents.
Several reasons have been proposed for the increased risk of obesity due to short sleep duration in adolescents. First, short sleep duration causes bad eating habits. Short sleep duration also increases the chance for intake of late-night snacks and food due to long waking times [66,67]. Additionally, short sleep duration is associated with greater responses to external stimuli, such as the sight or smell of food [67]. Children who reduced their sleep by 1.5 h per night for 1 week consumed 134 kcal more per day than those whose daily sleep was increased by the same amount [68]. In adolescents, the total calorie intake was 11% higher due to restricted sleep periods [69]. In addition, several studies have shown that short sleep increases the desire for unhealthy foods. Short sleep duration was associated with an increased intake of fast food and sweets but a decreased intake of fruit and vegetables [70]. The sleep restriction period in adolescents showed a trend of higher consumption of foods with a high glycemic index, such as sweets or desserts, and carbohydrates [69,71]. A systematic review, using data from 33 studies, also showed an association between short sleep duration and less favorable diet quality in children [72]. These psychological eating behaviors due to short sleep duration might be caused by hormonal disturbances related to metabolism and appetite. Second, a short sleep duration leads to endocrine changes causing excess weight gain. In healthy adolescents, the evaluation of the homeostasis model assessment of insulin resistance index increased with an experimental decrease of sleep duration to 4 h per night for 3 consecutive days compared to that with a long-term sleep of 9 h per night [73]. In addition, a short sleep duration is linked to decreased energy expenditure and increased leptin levels [68], leading to further weight gain. Lastly, a short sleep duration leads to physical inactivity due to fatigue and increased screen time [66].
Although it cannot be conclusively established that short sleep duration increases the risk of obesity in adolescents, it is thought to positively influence increased calorie intake, preference for unhealthy foods, altered hormonal levels affecting body weight, and a reduction in physical activity. Therefore, a sufficient sleep duration is recommended to prevent adolescent obesity.
4. Association between Bedtime and Adolescent Obesity
Although existing research has traditionally focused on sleep duration as a key contributor to obesity, there is growing interest in evaluating the role of sleep timing, especially late bedtimes [5,74,75,76]. As discussed earlier, the most notable feature of adolescent sleep patterns is the delayed sleep phase. Therefore, it is important to understand whether late bedtimes increase the risk of adolescent obesity.
Bedtime is thought to be a risk factor for obesity [35,74,77,78,79]. The later bedtime/later wake-up time adolescent group was associated with higher BMI than the early bedtime/early wake-up time adolescent group, despite a similar sleep duration [77]. In addition, the later bedtime group positively correlated with the BMI z-score [49,74] with a BMI increase of 2.1 kg/m2 for every additional hour of bedtime delay, regardless of sleep duration [78]. Furthermore, the later bedtime/later wake-up time adolescents were 2.16 times more at risk of obesity than the early bedtime/early wake-up time adolescents [15]. Studies have suggested that bedtime could provide a more precise understanding of the association between sleep and obesity [74,80] rather than sleep duration. However, the precise association between bedtime and weight status was unclear in some studies [48,51,54]. The discrepancies in results may be due to differing research methodologies. Although less research has focused on the importance of bedtime compared to sleep duration, bedtime may be an important factor for obesity in adolescents.
Late bedtimes potentially affect dietary behaviors and diet-related health outcomes, which could be the main reason for the increasing risk of adolescent obesity due to late bedtimes. Late bedtimes may also cause increased eating late at night due to staying up late. In addition, although later bedtimes may lead to shorter sleep duration [81], later bedtimes were also associated with less healthy eating behavior, such as less fruit and vegetable intake and more sweetened beverages/fast food intake despite adjusting for sleep duration [5,49,81,82]. The odds of missing breakfast were also significantly higher in cases of late bedtimes [83].
Similar to short sleep duration, late bedtime also affects the amount of physical activity. The late sleep/late wake-up category adolescents had fewer minutes of moderate-to-vigorous physical activity [15,82], while experiencing 48 min more of screen time per day [15] compared to that of adolescents in the early sleep/early wake-up category.
Therefore, further studies are required for a better understanding of the effect of bedtime on adolescent obesity, as this area is a potentially promising target for interventions aimed at reducing adolescent obesity. Large-scale studies are also required to explore the effect of wake-up time on adolescent obesity, as early school start times may be a major cause of insufficient sleep among adolescents.
5. Association between Sleep Discrepancy (Social Jetlag) and Adolescent Obesity
As mentioned earlier, most adolescents suffer from “social jetlag.” Adolescents who sleep late biologically and psychosocially are forced to wake up early because of school start times, resulting in sleep deprivation. The sleep debt during school days is compensated by trying to get enough sleep during non-school days. Due to physiologically delayed sleep phases, adolescents sleep later, sleep longer, and wake up later on non-school days. A recent study reported that adolescents obtained an average of 1.4 h more sleep on non-school days than on school days, in addition to shifting bedtimes by nearly 70 min later and wake-up times by nearly 160 min later [84]. Although oversleeping on non-school days may make up for the sleep deprivation during school days, the resulting circadian disruption across the week may lead to obesity in adolescents [85].
It is necessary to examine the effect of sleep discrepancy on obesity in adolescents from two distinct angles. First, whether the sleep duration discrepancy between school and non-school days affect the body weight status of adolescents. Oversleeping or catching up sleep on non-school days can either protect or increase the risk of obesity/overweight status. Research on this is insufficient, and most reports have shown null findings on the harmfulness of oversleeping during non-school days on adolescent obesity [84,86,87]. However, one large-scale cross-sectional study found a significant association between the difference in sleep duration on school days versus non-school days and obesity/overweight status in adolescent females, but not in adolescent males [88]. Second, whether the difference in sleep timing, including bedtime and wake-up time, between school and non-school days increases the risk of adolescent obesity. This difference, called social jetlag, can increase the risk of obesity due to frequent disruption of the circadian rhythm. One study found that overweight/obese adolescents had significantly later bedtimes (average 25 min) during non-school days compared to that of subjects with normal weight, and delayed bedtimes were an independent predictor of higher BMI z-scores [86]. In a large-scale cross-sectional study, social jetlag was associated with increased waist circumference and fat mass index in early adolescent girls, while no such associations were observed in adolescent boys [89]. Another cross-sectional study also showed that social jetlag was positively associated with the BMI z-score and waist-to-height ratios in older adolescents [90]. These findings may be a result of disrupted circadian rhythms caused by differences in sleep timing between school and non-school days. However, it is still controversial, as some studies have also shown that the sleep timing differences between school and non-school days were not associated with body weight status [84,88]. In addition, the results of the link between social jetlag and obesity varied by gender [88,90]. The reason for the difference in results according to gender is unclear, but sociocultural factors and biological factors are thought to have an effect [88,90].
Therefore, it is too early to conclude whether “social jetlag” adversely affects obesity/overweight status in adolescents. However, it is necessary to pay attention to social jetlag in adolescents, and further in-depth research is necessary to understand the effect of social jetlag on adolescent obesity. Social efforts such as adjustment of school schedules including the school start time might be necessary.
6. Current Sleep Pattern Status in Adolescents
Although sleep patterns, such as sleep duration, chronotype, and discrepancy between school and non-school days, are considered to have an important effect on the risk of obesity/overweight status in adolescents, the sleep patterns of adolescents are getting worse. Over the past century, children’s sleep duration has decreased by 0.75 min each year [91], and the rate of change is highest in older children on school days [91,92]. Even though the National Sleep Foundation recommends that adolescents must receive 8–10 h of night sleep [93], the average estimated sleep duration of adolescents aged 10–19 years was approximately 5.5–9.5 h, which varied largely depending on the region (Figure 1). Usually, Asian adolescents sleep less than those in other regions. Asian children sleep 1–2 h less each day than European children and 40–60 min less each day than American children [38]. The difference in sleep duration seems to be influenced by cultural rather than environmental factors (e.g., daylight duration) [35]. Both genetic and socio-cultural differences can also affect sleep duration in adolescents [94].
It is thought that Asian adolescents sleep less because they go to bed later than those in other regions. In a meta-analysis study, the mean Asian bedtime was 11:23 pm, while the North American bedtime was 10:06 pm [35]. The difference in bedtime may suggest the influence of cultural factors, as there is little difference in the geographical latitude [35]. For example, adolescents in China finish school at 8:30 pm [14], which is likely to be later than the end time for schools in North America. Conversely, the wake-up time is relatively consistent across regions and age groups on both school days and non-school days [35]. These results partially explain why Asian adolescents sleep less than those in other regions.
However, only 27% of adolescents in 20 cities in the United States [16] meet the sleep requirements recommendation by the American Academy of Sleep Medicine [95]. According to the reports of the Centers for Disease Control, two-thirds of all adolescents do not meet the recommended sleep requirements, as they sleep for ≤7 h on school days [96].
Several sleep recommendations for children and adolescents have been established (Table 2). Each sleep duration recommendation differs slightly, and it is unclear which sleep recommendations are the most appropriate. In addition, the appropriateness of these sleep recommendations is still uncertain, as ideally the sleep recommendations should be based on ideal sleep duration. The ideal sleep duration to maintain normal mental and physical function is still unknown, because the optimal sleep duration may differ both inter-individually and intra-individually [94]. Different optimal sleep durations, depending on individual cognitive tasks [97] and genetic variations [98], may be required. Therefore, establishing a global standard of optimal sleep is difficult. Furthermore, to the best of our knowledge there are no recommendations regarding the optimal sleep timing or sleep discrepancy across the week. Therefore, from the perspective of preventing obesity in adolescents, appropriate recommendations are needed for proper sleep duration, sleep time and wake-up time, and management of school days and non-school days. This requires better-planned research focusing on sleep patterns in adolescents.

Table 2.
Recommendations for sleep in children.
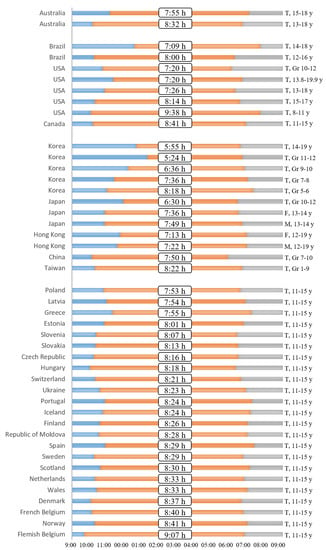
Figure 1.
Current global sleep status in adolescents. The European and Canadian data was acquired from Gariepy et al. [39], with permission from Elsevier. Rest of the data was collected from the cited references [13,14,99,100,101,102,103,104,105,106,107,108,109,110,111,112].
7. Conclusions
Adolescents have a characteristic sleep pattern. Appropriate sleep for adolescents is essential, as it plays a crucial role in preventing obesity/overweight status. However, not only is there a lack of appropriate sleep recommendation standards, but also the majority of adolescents do not sleep as currently recommended. Therefore, to prevent obesity among adolescents, it is necessary to encourage them to follow the sleep recommendation protocols as well as to develop a social atmosphere conducive to appropriate sleep and better health. Finally, appropriate sleep recommendation standards for adolescents should be established through further research.
Author Contributions
Conceptualization, A.K. and Y.C.; methodology, A.K.; investigation, A.K.; data curation, Y.C. and S.K.; writing—original draft preparation, A.K., Y.C., S.K. and K.S.; writing—review and editing, A.K., J.S., and H.W.C.; visualization, Y.C.; supervision, H.-S.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Cappuccio, F.P.; Taggart, F.M.; Kandala, N.-B.; Currie, A.; Peile, E.; Stranges, S.; Miller, M.A. Meta-analysis of short sleep duration and obesity in children and adults. Sleep 2008, 31, 619–626. [Google Scholar] [CrossRef] [PubMed]
- Patel, S.R. Reduced sleep as an obesity risk factor. Obes. Rev. 2009, 10 (Suppl. 2), 61–68. [Google Scholar] [CrossRef] [PubMed]
- Hayes, J.F.; Balantekin, K.N.; Altman, M.; Wilfley, D.E.; Taylor, C.B.; Williams, J. Sleep Patterns and Quality Are Associated with Severity of Obesity and Weight-Related Behaviors in Adolescents with Overweight and Obesity. Child. Obes. 2018, 14, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Spiegel, K.; Tasali, E.; Leproult, R.; Van Cauter, E. Effects of poor and short sleep on glucose metabolism and obesity risk. Nat. Rev. Endocrinol. 2009, 5, 253–261. [Google Scholar] [CrossRef] [PubMed]
- Golley, R.K.; Maher, C.A.; Matricciani, L.; Olds, T.S. Sleep duration or bedtime? Exploring the association between sleep timing behaviour, diet and BMI in children and adolescents. Int. J. Obes. 2013, 37, 546–551. [Google Scholar] [CrossRef]
- Touitou, Y. Adolescent sleep misalignment: A chronic jet lag and a matter of public health. J. Physiol. Paris. 2013, 107, 323–326. [Google Scholar] [CrossRef]
- Nedeltcheva, A.V.; Kilkus, J.M.; Imperial, J.; Kasza, K.; Schoeller, D.A.; Penev, P.D. Sleep curtailment is accompanied by increased intake of calories from snacks. Am. J. Clin. Nutr. 2009, 89, 126–133. [Google Scholar] [CrossRef]
- Taheri, S.; Lin, L.; Austin, D.; Young, T.; Mignot, E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004, 1, e62. [Google Scholar] [CrossRef]
- Hung, H.-C.; Yang, Y.-C.; Ou, H.-Y.; Wu, J.-S.; Lu, F.-H.; Chang, C.-J. The association between self-reported sleep quality and overweight in a Chinese population. Obesity 2013, 21, 486–492. [Google Scholar] [CrossRef]
- Gonnissen, H.K.J.; Rutters, F.; Mazuy, C.; Martens, E.A.P.; Adam, T.C.; Westerterp-Plantenga, M.S. Effect of a phase advance and phase delay of the 24-h cycle on energy metabolism, appetite, and related hormones. Am. J. Clin. Nutr. 2012, 96, 689–697. [Google Scholar] [CrossRef]
- Owens, J.; Adolescent Sleep Working Group; Committee on Adolescence. Insufficient sleep in adolescents and young adults: An update on causes and consequences. Pediatrics 2014, 134, e921–e932. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.-S.; Wang, C.-H.; Guilleminault, C. An epidemiologic study of sleep problems among adolescents in North Taiwan. Sleep Med. 2010, 11, 1035–1042. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.-K.; Kim, J.K.; Patel, S.R.; Lee, J.-H. Age-related changes in sleep/wake patterns among Korean teenagers. Pediatrics 2005, 115, 250–256. [Google Scholar] [CrossRef]
- Liu, X.; Zhao, Z.; Jia, C.; Buysse, D.J. Sleep patterns and problems among chinese adolescents. Pediatrics 2008, 121, 1165–1173. [Google Scholar] [CrossRef] [PubMed]
- Olds, T.S.; Maher, C.A.; Matricciani, L. Sleep duration or bedtime? Exploring the relationship between sleep habits and weight status and activity patterns. Sleep 2011, 34, 1299–1307. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Hale, L.; Chang, A.-M.; Nahmod, N.G.; Master, L.; Berger, L.M.; Buxton, O.M. Longitudinal associations of childhood bedtime and sleep routines with adolescent body mass index. Sleep 2019, 42, zsy202. [Google Scholar] [CrossRef]
- Crowley, S.J.; Wolfson, A.R.; Tarokh, L.; Carskadon, M.A. An update on adolescent sleep: New evidence informing the perfect storm model. J. Adolesc. 2018, 67, 55–65. [Google Scholar] [CrossRef]
- Olds, T.; Maher, C.; Blunden, S.; Matricciani, L. Normative data on the sleep habits of Australian children and adolescents. Sleep 2010, 33, 1381–1388. [Google Scholar] [CrossRef][Green Version]
- Moore, R.Y. Circadian rhythms: Basic neurobiology and clinical applications. Annu. Rev. Med. 1997, 48, 253–266. [Google Scholar] [CrossRef]
- Çakmur, H. Circadian Rhythm and Chronobiology. In Circadian Rhythm—Cellular and Molecular Mechanisms; IntechOpen: London, UK, 2018. [Google Scholar] [CrossRef]
- Crowley, S.J.; Acebo, C.; Carskadon, M.A. Sleep, circadian rhythms, and delayed phase in adolescence. Sleep Med. 2007, 8, 602–612. [Google Scholar] [CrossRef]
- Peek, C.B.; Affinati, A.H.; Ramsey, K.M.; Kuo, H.-Y.; Yu, W.; Sena, L.A.; Ilkayeva, O.; Marcheva, B.; Kobayashi, Y.; Omura, C.; et al. Circadian clock NAD+ cycle drives mitochondrial oxidative metabolism in mice. Science 2013, 342, 1243417. [Google Scholar] [CrossRef] [PubMed]
- Khalsa, S.B.S.; Jewett, M.E.; Cajochen, C.; Czeisler, C.A. A phase response curve to single bright light pulses in human subjects. J. Physiol. 2003, 549, 945–952. [Google Scholar] [CrossRef] [PubMed]
- Lewy, A.J.; Wehr, T.A.; Goodwin, F.K.; Newsome, D.A.; Markey, S.P. Light suppresses melatonin secretion in humans. Science 1980, 210, 1267–1269. [Google Scholar] [CrossRef] [PubMed]
- Brainard, G.C.; Hanifin, J.P.; Greeson, J.M.; Byrne, B.; Glickman, G.; Gerner, E.; Rollag, M.D. Action spectrum for melatonin regulation in humans: Evidence for a novel circadian photoreceptor. J. Neurosci. 2001, 21, 6405–6412. [Google Scholar] [CrossRef]
- Smith, K.A.; Schoen, M.W.; Czeisler, C.A. Adaptation of human pineal melatonin suppression by recent photic history. J. Clin. Endocrinol. Metab. 2004, 89, 3610–3614. [Google Scholar] [CrossRef]
- Skorucak, J.; Weber, N.; Carskadon, M.A.; Reynolds, C.; Coussens, S.; Achermann, P.; Short, M.A. Homeostatic response to sleep restriction in adolescents. Sleep 2021, 44, zsab106. [Google Scholar] [CrossRef]
- Daan, S.; Beersma, D.G.; Borbély, A.A. Timing of human sleep: Recovery process gated by a circadian pacemaker. Am. J. Physiol. 1984, 246, R161–R183. [Google Scholar] [CrossRef]
- Sadeh, A.; Dahl, R.E.; Shahar, G.; Rosenblat-Stein, S. Sleep and the transition to adolescence: A longitudinal study. Sleep 2009, 32, 1602–1609. [Google Scholar] [CrossRef]
- Carskadon, M.A.; Acebo, C.; Jenni, O.G. Regulation of adolescent sleep: Implications for behavior. Ann. N. Y. Acad. Sci. 2004, 1021, 276–291. [Google Scholar] [CrossRef]
- Frey, S.; Balu, S.; Greusing, S.; Rothen, N.; Cajochen, C. Consequences of the timing of menarche on female adolescent sleep phase preference. PLoS ONE 2009, 4, e5217. [Google Scholar] [CrossRef]
- Randler, C.; Faßl, C.; Kalb, N. From Lark to Owl: Developmental changes in morningness-eveningness from new-borns to early adulthood. Sci. Rep. 2017, 7, 45874. [Google Scholar] [CrossRef]
- Duffy, J.F.; Czeisler, C.A. Age-related change in the relationship between circadian period, circadian phase, and diurnal preference in humans. Neurosci. Lett. 2002, 318, 117–120. [Google Scholar] [CrossRef]
- Taylor, D.J.; Jenni, O.G.; Acebo, C.; Carskadon, M.A. Sleep tendency during extended wakefulness: Insights into adolescent sleep regulation and behavior. J. Sleep Res. 2005, 14, 239–244. [Google Scholar] [CrossRef] [PubMed]
- Gradisar, M.; Gardner, G.; Dohnt, H. Recent worldwide sleep patterns and problems during adolescence: A review and meta-analysis of age, region, and sleep. Sleep Med. 2011, 12, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Oka, Y.; Suzuki, S.; Inoue, Y. Bedtime activities, sleep environment, and sleep/wake patterns of Japanese elementary school children. Behav. Sleep Med. 2008, 6, 220–233. [Google Scholar] [CrossRef]
- Bartel, K.A.; Gradisar, M.; Williamson, P. Protective and risk factors for adolescent sleep: A meta-analytic review. Sleep Med. Rev. 2015, 21, 72–85. [Google Scholar] [CrossRef]
- Olds, T.; Blunden, S.; Petkov, J.; Forchino, F. The relationships between sex, age, geography and time in bed in adolescents: A meta-analysis of data from 23 countries. Sleep Med. Rev. 2010, 14, 371–378. [Google Scholar] [CrossRef]
- Gariepy, G.; Danna, S.; Gobiņa, I.; Rasmussen, M.; Gaspar de Matos, M.; Tynjälä, J.; Janssen, I.; Kalman, M.; Villeruša, A.; Husarova, D.; et al. How Are Adolescents Sleeping? Adolescent Sleep Patterns and Sociodemographic Differences in 24 European and North American Countries. J. Adolesc. Health 2020, 66, S81–S88. [Google Scholar] [CrossRef]
- Wheaton, A.G.; Chapman, D.P.; Croft, J.B. School Start Times, Sleep, Behavioral, Health, and Academic Outcomes: A Review of the Literature. J. Sch. Health 2016, 86, 363–381. [Google Scholar] [CrossRef]
- Marx, R.; Tanner-Smith, E.E.; Davison, C.M.; Ufholz, L.-A.; Freeman, J.; Shankar, R.; Newton, L.; Brown, R.S.; Parpia, A.S.; Cozma, I.; et al. Later school start times for supporting the education, health, and well-being of high school students. Cochrane Database Syst. Rev. 2017, 7, CD009467. [Google Scholar]
- Minges, K.E.; Redeker, N.S. Delayed school start times and adolescent sleep: A systematic review of the experimental evidence. Sleep Med. Rev. 2016, 28, 86–95. [Google Scholar] [CrossRef] [PubMed]
- Roenneberg, T.; Wirz-Justice, A.; Merrow, M. Life between clocks: Daily temporal patterns of human chronotypes. J. Biol. Rhythms. 2003, 18, 80–90. [Google Scholar] [CrossRef] [PubMed]
- Collings, P.J.; Ball, H.L.; Santorelli, G.; West, J.; Barber, S.E.; McEachan, R.R.; Wright, J. Sleep Duration and Adiposity in Early Childhood: Evidence for Bidirectional Associations from the Born in Bradford Study. Sleep 2017, 40, zsw054. [Google Scholar] [CrossRef] [PubMed]
- Katzmarzyk, P.T.; Barreira, T.V.; Broyles, S.T.; Champagne, C.M.; Chaput, J.-P.; Fogelholm, M.; Hu, G.; Johnson, W.D.; Kuriyan, R.; Kurpad, A.; et al. Relationship between lifestyle behaviors and obesity in children ages 9-11, Results from a 12-country study. Obesity 2015, 23, 1696–1702. [Google Scholar] [CrossRef] [PubMed]
- Chaput, J.-P.; Lambert, M.; Gray-Donald, K.; McGrath, J.J.; Tremblay, M.S.; O’Loughlin, J.; Tremblay, A. Short sleep duration is independently associated with overweight and obesity in Quebec children. Can. J. Public Health 2011, 102, 369–374. [Google Scholar] [CrossRef]
- Cespedes Feliciano, E.M.; Quante, M.; Rifas-Shiman, S.L.; Redline, S.; Oken, E.; Taveras, E.M. Objective Sleep Characteristics and Cardiometabolic Health in Young Adolescents. Pediatrics 2018, 142, e20174085. [Google Scholar] [CrossRef]
- Taylor, R.W.; Williams, S.M.; Galland, B.C.; Farmer, V.L.; Meredith-Jones, K.A.; Schofield, G.; Mann, J.I. Quantity versus quality of objectively measured sleep in relation to body mass index in children: Cross-sectional and longitudinal analyses. Int. J. Obes. 2020, 44, 803–811. [Google Scholar] [CrossRef]
- Arora, T.; Taheri, S. Associations among late chronotype, body mass index and dietary behaviors in young adolescents. Int. J. Obes. 2015, 39, 39–44. [Google Scholar] [CrossRef]
- Wilkie, H.J.; Standage, M.; Gillison, F.B.; Cumming, S.P.; Katzmarzyk, P.T. Multiple lifestyle behaviours and overweight and obesity among children aged 9–11 years: Results from the UK site of the International Study of Childhood Obesity, Lifestyle and the Environment. BMJ Open. 2016, 6, e010677. [Google Scholar] [CrossRef]
- Thumann, B.F.; Buck, C.; De Henauw, S.; Hadjigeorgiou, C.; Hebestreit, A.; Lauria, F.; Lissner, L.; Molnár, D.; Moreno, L.A.; Veidebaum, T.; et al. Cross-sectional associations between objectively measured sleep characteristics and body mass index in European children and adolescents. Sleep Med. 2021, 84, 32–39. [Google Scholar] [CrossRef]
- Mcneil, J.; Tremblay, M.S.; Leduc, G.; Boyer, C.; Bélanger, P.; Leblanc, A.G.; Borghese, M.M.; Chaput, J.-P. Objectively-measured sleep and its association with adiposity and physical activity in a sample of Canadian children. J. Sleep Res. 2015, 24, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Gomes, T.N.; Katzmarzyk, P.T.; dos Santos, F.K.; Souza, M.; Pereira, S.; Maia, J.A.R. Overweight and obesity in Portuguese children: Prevalence and correlates. Int. J. Environ. Res. Public Health 2014, 11, 11398–11417. [Google Scholar] [CrossRef] [PubMed]
- Mi, S.J.; Kelly, N.R.; Brychta, R.J.; Grammer, A.C.; Jaramillo, M.; Chen, K.Y.; Fletcher, L.A.; Bernstein, S.B.; Courville, A.B.; Shank, L.; et al. Associations of sleep patterns with metabolic syndrome indices, body composition, and energy intake in children and adolescents. Pediatr. Obes. 2019, 14, e12507. [Google Scholar] [CrossRef] [PubMed]
- Michels, N.; Verbeiren, A.; Ahrens, W.; De Henauw, S.; Sioen, I. Children’s sleep quality: Relation with sleep duration and adiposity. Public Health 2014, 128, 488–490. [Google Scholar] [CrossRef]
- Rognvaldsdottir, V.; Gudmundsdottir, S.L.; Brychta, R.J.; Hrafnkelsdottir, S.M.; Gestsdottir, S.; Arngrimsson, S.A.; Chen, K.Y.; Johannsson, E. Sleep deficiency on school days in Icelandic youth, as assessed by wrist accelerometry. Sleep Med. 2017, 33, 103–108. [Google Scholar] [CrossRef]
- Chen, X.; Beydoun, M.A.; Wang, Y. Is sleep duration associated with childhood obesity? A systematic review and meta-analysis. Obesity 2008, 16, 265–274. [Google Scholar] [CrossRef]
- Ruan, H.; Xun, P.; Cai, W.; He, K.; Tang, Q. Habitual Sleep Duration and Risk of Childhood Obesity: Systematic Review and Dose-response Meta-analysis of Prospective Cohort Studies. Sci. Rep. 2015, 5, 16160. [Google Scholar] [CrossRef]
- Fatima, Y.; Doi, S.A.R.; Mamun, A.A. Longitudinal impact of sleep on overweight and obesity in children and adolescents: A systematic review and bias-adjusted meta-analysis. Obes. Rev. 2015, 16, 137–149. [Google Scholar] [CrossRef]
- Wu, Y.; Gong, Q.; Zou, Z.; Li, H.; Zhang, X. Short sleep duration and obesity among children: A systematic review and meta-analysis of prospective studies. Obes. Res. Clin. Pract. 2017, 11, 140–150. [Google Scholar] [CrossRef]
- Yoong, S.L.; Chai, L.K.; Williams, C.M.; Wiggers, J.; Finch, M.; Wolfenden, L. Systematic review and meta-analysis of interventions targeting sleep and their impact on child body mass index, diet, and physical activity. Obesity 2016, 24, 1140–1147. [Google Scholar] [CrossRef]
- Li, L.; Zhang, S.; Huang, Y.; Chen, K. Sleep duration and obesity in children: A systematic review and meta-analysis of prospective cohort studies. J. Paediatr. Child Health 2017, 53, 378–385. [Google Scholar] [CrossRef] [PubMed]
- Miller, M.A.; Kruisbrink, M.; Wallace, J.; Ji, C.; Cappuccio, F.P. Sleep duration and incidence of obesity in infants, children, and adolescents: A systematic review and meta-analysis of prospective studies. Sleep 2018, 41, zsy018. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Miller, M.A.; Cappuccio, F.P. Short duration of sleep and incidence of overweight or obesity in Chinese children and adolescents: A systematic review and meta-analysis of prospective studies. Nutr. Metab. Cardiovasc. Dis. 2021, 31, 363–371. [Google Scholar] [CrossRef] [PubMed]
- Deng, X.; He, M.; He, D.; Zhu, Y.; Zhang, Z.; Niu, W. Sleep duration and obesity in children and adolescents: Evidence from an updated and dose–response meta-analysis. Sleep Med. 2021, 78, 169–181. [Google Scholar] [CrossRef]
- Shochat, T.; Cohen-Zion, M.; Tzischinsky, O. Functional consequences of inadequate sleep in adolescents: A systematic review. Sleep Med. Rev. 2014, 18, 75–87. [Google Scholar] [CrossRef]
- Burt, J.; Dube, L.; Thibault, L.; Gruber, R. Sleep and eating in childhood: A potential behavioral mechanism underlying the relationship between poor sleep and obesity. Sleep Med. 2014, 15, 71–75. [Google Scholar] [CrossRef]
- Hart, C.N.; Carskadon, M.A.; Considine, R.V.; Fava, J.L.; Lawton, J.; Raynor, H.A.; Jelalian, E.; Owens, J.; Wing, R. Changes in children’s sleep duration on food intake, weight, and leptin. Pediatrics 2013, 132, e1473–e1480. [Google Scholar] [CrossRef]
- Simon, S.L.; Field, J.; Miller, L.E.; DiFrancesco, M.; Beebe, D.W. Sweet/dessert foods are more appealing to adolescents after sleep restriction. PLoS ONE 2015, 10, e0115434. [Google Scholar]
- Westerlund, L.; Ray, C.; Roos, E. Associations between sleeping habits and food consumption patterns among 10-11-year-old children in Finland. Br. J. Nutr. 2009, 102, 1531–1537. [Google Scholar] [CrossRef]
- Beebe, D.W.; Simon, S.; Summer, S.; Hemmer, S.; Strotman, D.; Dolan, L.M. Dietary intake following experimentally restricted sleep in adolescents. Sleep 2013, 36, 827–834. [Google Scholar] [CrossRef]
- Felső, R.; Lohner, S.; Hollódy, K.; Erhardt, É.; Molnár, D. Relationship between sleep duration and childhood obesity: Systematic review including the potential underlying mechanisms. Nutr. Metab. Cardiovasc. Dis. 2017, 27, 751–761. [Google Scholar] [CrossRef] [PubMed]
- Klingenberg, L.; Chaput, J.-P.; Holmbäck, U.; Visby, T.; Jennum, P.; Nikolic, M.; Astrup, A.; Sjödin, A. Acute Sleep Restriction Reduces Insulin Sensitivity in Adolescent Boys. Sleep 2013, 36, 1085–1090. [Google Scholar] [CrossRef] [PubMed]
- Jarrin, D.C.; McGrath, J.J.; Drake, C.L. Beyond sleep duration: Distinct sleep dimensions are associated with obesity in children and adolescents. Int. J. Obes. 2013, 37, 552–558. [Google Scholar] [CrossRef] [PubMed]
- Thind, H.; Davies, S.L.; Lewis, T.; Pekmezi, D.; Evans, R.; Baskin, M.L. Does Short Sleep Lead to Obesity Among Children and Adolescents? Current Understanding and Implications. Am. J. Lifestyle Med. 2015, 9, 428–437. [Google Scholar] [CrossRef]
- Chaput, J.-P. Sleep patterns, diet quality and energy balance. Physiol. Behav. 2014, 134, 86–91. [Google Scholar] [CrossRef]
- Randler, C.; Haun, J.; Schaal, S. Assessing the influence of sleep-wake variables on body mass index (BMI) in adolescents. Eur. J. Psychol. 2013, 9, 339–347. Available online: https://ejop.psychopen.eu/article/view/558 (accessed on 1 March 2022). [CrossRef]
- Asarnow, L.D.; McGlinchey, E.; Harvey, A.G. Evidence for a Possible Link between Bedtime and Change in Body Mass Index. Sleep 2015, 38, 1523–1527. [Google Scholar] [CrossRef]
- Spaeth, A.M.; Hawley, N.L.; Raynor, H.A.; Jelalian, E.; Greer, A.; Crouter, S.E.; Coffman, D.L.; Carskadon, M.A.; Owens, J.A.; Wing, R.R.; et al. Sleep, energy balance, and meal timing in school-aged children. Sleep Med. 2019, 60, 139–144. [Google Scholar] [CrossRef]
- Fleig, D.; Randler, C. Association between chronotype and diet in adolescents based on food logs. Eat. Behav. 2009, 10, 115–118. [Google Scholar] [CrossRef]
- Grummon, A.H.; Sokol, R.L.; Lytle, L.A. Is late bedtime an overlooked sleep behaviour? Investigating associations between sleep timing, sleep duration and eating behaviours in adolescence and adulthood. Public Health Nutr. 2021, 24, 1671–1677. [Google Scholar] [CrossRef]
- Harrex, H.A.L.; Skeaff, S.A.; Black, K.E.; Davison, B.K.; Haszard, J.J.; Meredith-Jones, K.; Quigg, R.; Saeedi, P.; Stoner, L.; Wong, J.E.; et al. Sleep timing is associated with diet and physical activity levels in 9-11-year-old children from Dunedin, New Zealand: The PEDALS study. J. Sleep Res. 2018, 27, e12634. [Google Scholar] [CrossRef] [PubMed]
- Agostini, A.; Lushington, K.; Kohler, M.; Dorrian, J. Associations between self-reported sleep measures and dietary behaviours in a large sample of Australian school students (n = 28,010). J. Sleep Res. 2018, 27, e12682. [Google Scholar] [CrossRef] [PubMed]
- Berry, K.M.; Berger, A.T.; Laska, M.N.; Erickson, D.J.; Lenk, K.M.; Iber, C.; Full, K.M.; Wahlstrom, K.; Redline, S.; Widome, R. Weekend night vs. school night sleep patterns, weight status, and weight-related behaviors among adolescents. Sleep Health 2021, 7, 572–580. [Google Scholar] [CrossRef] [PubMed]
- Roenneberg, T.; Allebrandt, K.V.; Merrow, M.; Vetter, C. Social jetlag and obesity. Curr. Biol. 2012, 22, 939–943. [Google Scholar] [CrossRef]
- Chung, K.-F.; Kan, K.K.-K.; Yeung, W.-F. Sleep duration, sleep–wake schedule regularity, and body weight in Hong Kong Chinese adolescents. Biol. Rhythm. Res. 2013, 44, 169–179. [Google Scholar] [CrossRef]
- Quan, S.F.; Combs, D.; Parthasarathy, S. Impact of Sleep Duration and Weekend Oversleep on Body Weight and Blood Pressure in Adolescents. Southwest J. Pulm. Crit. Care 2018, 16, 31–41. [Google Scholar] [CrossRef]
- Schneider, A.C.; Zhang, D.; Xiao, Q. Adolescent sleep characteristics and body-mass index in the Family Life, Activity, Sun, Health, and Eating (FLASHE) Study. Sci. Rep. 2020, 10, 13277. [Google Scholar] [CrossRef]
- Cespedes Feliciano, E.M.; Rifas-Shiman, S.L.; Quante, M.; Redline, S.; Oken, E.; Taveras, E.M. Chronotype, Social Jet Lag, and Cardiometabolic Risk Factors in Early Adolescence. JAMA Pediatr. 2019, 173, 1049–1057. [Google Scholar] [CrossRef]
- Malone, S.K.; Zemel, B.; Compher, C.; Souders, M.; Chittams, J.; Thompson, A.L.; Pack, A.; Lipman, T.H. Social jet lag, chronotype and body mass index in 14–17-year-old adolescents. Chronobiol. Int. 2016, 33, 1255–1266. [Google Scholar] [CrossRef]
- Matricciani, L.; Olds, T.; Petkov, J. In search of lost sleep: Secular trends in the sleep time of school-aged children and adolescents. Sleep Med. Rev. 2012, 16, 203–211. [Google Scholar] [CrossRef]
- Galland, B.C.; Short, M.A.; Terrill, P.; Rigney, G.; Haszard, J.J.; Coussens, S.; Foster-Owens, M.; Biggs, S.N. Establishing normal values for pediatric nighttime sleep measured by actigraphy: A systematic review and meta-analysis. Sleep 2018, 41, zsy017. [Google Scholar] [CrossRef] [PubMed]
- Hirshkowitz, M.; Whiton, K.; Albert, S.M.; Alessi, C.; Bruni, O.; DonCarlos, L.; Hazen, N.; Herman, J.; Adams Hillard, P.J.; Katz, E.S.; et al. National Sleep Foundation’s updated sleep duration recommendations: Final report. Sleep Health 2015, 1, 233–243. [Google Scholar] [CrossRef]
- Matricciani, L.; Blunden, S.; Rigney, G.; Williams, M.T.; Olds, T.S. Children’s sleep needs: Is there sufficient evidence to recommend optimal sleep for children? Sleep 2013, 36, 527–534. [Google Scholar] [CrossRef]
- Paruthi, S.; Brooks, L.J.; D’Ambrosio, C.; Hall, W.A.; Kotagal, S.; Lloyd, R.M.; Malow, B.A.; Maski, K.; Nichols, C.; Quan, S.F.; et al. Recommended Amount of Sleep for Pediatric Populations: A Consensus Statement of the American Academy of Sleep Medicine. J. Clin. Sleep Med. 2016, 12, 785–786. [Google Scholar] [CrossRef]
- Wheaton, A.G.; Olsen, E.O.; Miller, G.F.; Croft, J.B. Sleep Duration and Injury-Related Risk Behaviors Among High School Students—United States, 2007–2013. Morb. Mortal. Wkly. Rep. 2016, 65, 337–341. [Google Scholar] [CrossRef]
- Eide, E.R.; Showalter, M.H. Sleep and Student Achievement. East Econ. J. 2012, 38, 512–524. [Google Scholar] [CrossRef]
- He, Y.; Jones, C.R.; Fujiki, N.; Xu, Y.; Guo, B.; Holder, J.L., Jr.; Rossner, M.J.; Nishino, S.; Fu, Y.-H. The transcriptional repressor DEC2 regulates sleep length in mammals. Science 2009, 325, 866–870. [Google Scholar] [CrossRef]
- Warner, S.; Murray, G.; Meyer, D. Holiday and school-term sleep patterns of Australian adolescents. J. Adolesc. 2008, 31, 595–608. [Google Scholar] [CrossRef]
- Short, M.A.; Gradisar, M.; Wright, H.; Lack, L.C.; Dohnt, H.; Carskadon, M.A. Time for bed: Parent-set bedtimes associated with improved sleep and daytime functioning in adolescents. Sleep 2011, 34, 797–800. [Google Scholar] [CrossRef]
- Teixeira, L.R.; Fischer, F.M.; de Andrade, M.M.M.; Louzada, F.M.; Nagai, R. Sleep patterns of day-working, evening high-schooled adolescents of São Paulo, Brazil. Chronobiol. Int. 2004, 21, 239–252. [Google Scholar] [CrossRef]
- Andrade, M.M.; Benedito-Silva, A.A.; Domenice, S.; Arnhold, I.J.; Menna-Barreto, L. Sleep characteristics of adolescents: A longitudinal study. J. Adolesc. Health 1993, 14, 401–406. [Google Scholar] [CrossRef]
- Bryant Ludden, A.; Wolfson, A.R. Understanding adolescent caffeine use: Connecting use patterns with expectancies, reasons, and sleep. Health Educ. Behav. 2010, 37, 330–342. [Google Scholar] [CrossRef]
- Wolfson, A.R.; Carskadon, M.A.; Acebo, C.; Seifer, R.; Fallone, G.; Labyak, S.E.; Martin, J.L. Evidence for the validity of a sleep habits survey for adolescents. Sleep 2003, 26, 213–216. [Google Scholar] [CrossRef]
- Gradisar, M.; Wolfson, A.R.; Harvey, A.G.; Hale, L.; Rosenberg, R.; Czeisler, C.A. The sleep and technology use of Americans: Findings from the National Sleep Foundation’s 2011 Sleep in America poll. J. Clin. Sleep Med. 2013, 9, 1291–1299. [Google Scholar] [CrossRef]
- Knutson, K.L.; Lauderdale, D.S. Sociodemographic and behavioral predictors of bed time and wake time among US adolescents aged 15 to 17 years. J. Pediatr. 2009, 154, 426–430.e1. [Google Scholar] [CrossRef]
- Spilsbury, J.C.; Storfer-Isser, A.; Drotar, D.; Rosen, C.L.; Kirchner, L.H.; Benham, H.; Redline, S. Sleep behavior in an urban US sample of school-aged children. Arch. Pediatr. Adolesc. Med. 2004, 158, 988–994. [Google Scholar] [CrossRef]
- Kim, S.J.; Lee, Y.J.; Cho, S.-J.; Cho, I.-H.; Lim, W.; Lim, W. Relationship between weekend catch-up sleep and poor performance on attention tasks in Korean adolescents. Arch. Pediatr. Adolesc. Med. 2011, 165, 806–812. [Google Scholar] [CrossRef]
- Honda, M.; Genba, M.; Kawakami, J.; Nishizono-Maher, A. A sleep and life-style survey of Japanese high school boys: Factors associated with frequent exposure to bright nocturnal light. Sleep Biol. Rhythm. 2008, 6, 110–119. [Google Scholar] [CrossRef]
- Gaina, A.; Sekine, M.; Hamanishi, S.; Chen, X.; Kagamimori, S. Gender and temporal differences in sleep-wake patterns in Japanese schoolchildren. Sleep 2005, 28, 337–342. [Google Scholar]
- Chung, K.-F.; Cheung, M.-M. Sleep-wake patterns and sleep disturbance among Hong Kong Chinese adolescents. Sleep 2008, 31, 185–194. [Google Scholar] [CrossRef]
- Shur-Fen Gau, S. Prevalence of sleep problems and their association with inattention/hyperactivity among children aged 6–15 in Taiwan. J. Sleep Res. 2006, 15, 403–414. [Google Scholar] [CrossRef]
- Children’s Sleep Requirements. Available online: https://www.stlukes-stl.com/services/sleep-medicine/documents/pediatricsleep/children_sleep_reqmt.pdf (accessed on 1 December 2021).
- Carter, K.A.; Hathaway, N.E.; Lettieri, C.F. Common sleep disorders in children. Am. Fam. Physician 2014, 89, 368–377. [Google Scholar]
- Iglowstein, I.; Jenni, O.G.; Molinari, L.; Largo, R.H. Sleep duration from infancy to adolescence: Reference values and generational trends. Pediatrics 2003, 111, 302–307. [Google Scholar] [CrossRef]
- Crosby, B.; LeBourgeois, M.K.; Harsh, J. Racial differences in reported napping and nocturnal sleep in 2- to 8-year-old children. Pediatrics 2005, 115, 225–232. [Google Scholar] [CrossRef]
- Heussler, H.S. 9. Common causes of sleep disruption and daytime sleepiness: Childhood sleep disorders II. Med. J. Aust. 2005, 182, 484–489. [Google Scholar] [CrossRef]
- Your Guide to Healthy Sleep. US Department of Health and Human Services. Available online: www.nhlbi.nih.gov/health/public/sleep/healthy_sleep.pdf (accessed on 1 December 2021).
- How Much Sleep Do We Really Need? Available online: www.sleepfoundation.org/article/how-sleep-works/how-much-sleep-do-we-really-need (accessed on 1 December 2021).
- Carskadon, M.A.; Harvey, K.; Duke, P.; Anders, T.F.; Litt, I.F.; Dement, W.C. Pubertal changes in daytime sleepiness. Sleep 1980, 2, 453–460. [Google Scholar]
- Changes in Sleep with Age. Available online: http://healthysleep.med.harvard.edu/healthy/science/variations/changes-in-sleep-with-age (accessed on 1 December 2021).
- Ferber, R. Sleep, sleeplessness, and sleep disruptions in infants and young children. Ann. Clin. Res. 1985, 17, 227–234. [Google Scholar]
- Dijk, D.J.; Duffy, J.F.; Czeisler, C.A. Contribution of circadian physiology and sleep homeostasis to age-related changes in human sleep. Chronobiol. Int. 2000, 17, 285–311. [Google Scholar] [CrossRef]
- Ohayon, M.M.; Carskadon, M.A.; Guilleminault, C.; Vitiello, M.V. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: Developing normative sleep values across the human lifespan. Sleep 2004, 27, 1255–1273. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).