Abstract
Emissions from residential solid fuel burning in densely populated low-income settlements is a significant source of air pollution over the South African Highveld. The area is densely populated and highly industrialized, resulting in high concentrations of pollutants over the area. Although emissions from industrial sources are much larger, exposure to household emissions poses the most significant risk to human health. Interventions aimed at reducing solid fuel burning in low-income settlements on the Highveld have the potential to reduce exposure, but quantifying their true impact remains a challenge. We aimed to estimate the health and associated economic benefits of the regional implementation of thermal insulation as intervention measure in low-income settlements to predict the potential impact on the regional scale. We used a land use type regression model to estimate pre-intervention PM2.5 concentrations over the Highveld and then used sampled post-intervention air quality data from a pilot offset programme to relate changes in air quality to changes in avoided premature mortalities. We estimate that the large-scale implementation of this intervention could result in 143 avoided premature mortalities with an estimated economic benefit of just under ZAR (2011) 341.6 million, equivalent to USD (2011) 49.4 million.
1. Introduction
The Highveld region of South Africa is an extensive interior plateau that occupies the largest portion of land area in the country. It is a region well known for its poor air quality. Due to rich coal reserves in the area, many coal-fired power plants and heavy industries are located there. Meteorological conditions over the region lead to an accumulation and re-circulation of pollutants. This is mainly due to the prevalence of a subtropical high that leads to weak pressure gradients and the formation of inversion layers that limit the vertical dilution of pollutants [1]. The region is the most densely populated in South Africa, resulting in large-scale population exposure to pollutants that are harmful to human health. The current poor air quality and potential for further deterioration has led to the declaration of two priority air quality management areas, the Vaal Triangle Air Shed Priority Area (VTAPA) and Highveld Priority Area (HPA), in terms of Chapter 4 of the National Environmental Management: Air Quality Act no.39 of 2004 [2].
Although overall emissions from industrial, mining, and other commercial sources are mostly higher than emissions attributable to household combustion in both priority areas, the impact of the latter on human health is of far greater significance [3,4]. Global exposure to household air pollution decreased between 1990 and 2019, but it remains one of the largest environmental health risks to human health, particularly in Asia, Central and South America, and Africa [5,6]. Smoke from solid fuel and coal burning contain a large number of pollutants known to be hazardous to human health and is emitted at much lower levels, where human exposure is at its highest and pollutant dispersal is limited. Epidemiological evidence links exposure to HAP to diseases such as acute lower respiratory infections (ALRI), chronic obstructive pulmonary disease (COPD), lung cancer, cancer of the nasopharynx and larynx, tuberculosis, perinatal diseases and low birthweight, eye diseases and cataracts, cardiovascular disease, and stroke [7,8,9,10]. Strong evidence shows PM2.5 to be the pollutant of greatest concern to human health. Worldwide, PM2.5 is considered to serve as a general indicator of the anthropogenic pollution mix of concern and is most frequently used in health risk assessments as a marker for pollution [6,8,11]. PM2.5 is also the pollutant of focus for this study.
The HAP burden of disease is not distributed equally amongst or within countries and communities; globally, the brunt of this burden rests on the poor and vulnerable populations; women, children, the elderly, and the sickly are by far the worst affected. Southern Africa is no different, the frequent use of solid fuels for household energy needs is still significantly concentrated among the poor and a major driver of health inequalities between communities [12]. Over the Highveld, household combustion is the major source of PM pollution in solid fuel burning communities, especially during winter months when coal is used for space heating and cooking. Peak emission times often coincide with periods of poor atmospheric dispersion potential, causing high pollution concentrations over low-income residential areas in the region [13,14,15]. High intra-community variability is also frequently measured within these communities, leading to further health inequalities and adding to the complexity of quantifying risks and impacts [16].
The negative health impacts of air pollution also place a significant economic burden on affected individuals, their families, the public healthcare system, and the economy of a country. These costs include the costs associated with illness or premature death and loss of productivity and income due to illness. Global air pollution-related health costs were estimated to be USD 21 billion in 2015 and are expected to increase to USD 176 billion in 2060 [10]. The true economic impact of air pollution-related morbidity and mortality remains underestimated, and consequently, the true benefits of reducing exposure and improving air quality may be substantially larger than previously estimated [11].
The South African Department of Environmental affairs (DEA) published Air Quality Offset guidelines in March 2016 [17]. The guidelines propose offset programmes as a complimentary measure to help “address complex pollution sources by allowing concerted efforts by both government and polluting industries to clean up the air” [17] (p. 7) Residential solid fuel burning is a specifically mentioned target source for offset programs. The guidelines clearly state that an offset should counterbalance the environmental impacts of a pollutant from one source by decreasing emissions from another source that has an equivalent impact [17]. The implementation of air quality offsets programmes has been a requirement of some Atmospheric Emission Licenses (AEL) since April 2015 and several pilot offset programmes aimed at reducing emissions from solid fuel burning were implemented in low-income settlements. A few challenges and shortcomings were identified during the course of these projects, some regarding the implementation of offsets and others regarding quantifying the impacts of interventions [13,18]. There seems to be a consensus however, that the health impacts of interventions should be quantified and used as a measure of their effectiveness and suitability for large-scale rollout. Interventions (and pilot offset programmes) are typically tested and implemented at the community scale to determine suitability for larger scale rollout. Previous studies of various intervention methods revealed no significant improvements in overall ambient air quality, but did show improvements on the household scale [13,19]. Small changes in air quality at the community level only provide marginal changes in health risk for the exposed population, but the sum of the same reductions in a larger population and at a larger scale could result in significant health and economic benefits [10,20,21].
A need thus exists to model the impact of individual pilot offset projects on a larger scale. This could provide a much clearer picture of their true impact and will better inform decision-making and the allocation of resources. A Health Impact Assessment (HIA) could be a useful tool to quantify the health and economic benefits of air pollution interventions. Assessing the success of interventions based on findings made in only one area, community, or population could lead to the wrong conclusions due to many confounding and interactive factors that vary over time, space, and populations. Using site-specific air quality, population, and health data to model the impact of an intervention over the regional scale could provide a better estimate of its true impact. This study will aim to fill this gap by estimating the impact that the large-scale implementation of thermal insulation as an intervention measure could have on the air quality and population health in densely populated low-income settlements on the Highveld. The health benefits (in terms of reduced premature mortality) and the economic value of these benefits are calculated in order to quantify the health and economic impacts that an offset program could have on the regional scale. Attaching a monetary value to improved health outcomes could further inform decision making regarding the suitability of this offset for the private sector and government alike.
2. Study Area
The study area includes two priority air quality management areas declared in terms of Section 18. (1) of the National Environmental Management: Air Quality Act (NEMAQA) of 2004. The Vaal Triangle Air shed Priority Area (VTAPA) was the first priority area to be declared in South Africa in 2006 due to elevated pollutant concentrations within the area. The Highveld Priority Area (HPA) was declared by the minister in 2007, for the same reasons [22]. As both these priority areas overlap provincial boundaries (Free State, Gauteng, and Mpumalanga), NEMAQA mandates the DEA as the “lead agent” in the management of these areas.
The study area is delineated along the administrative boundaries of the local municipalities within each priority area. Within the VTAPA, there are four municipalities in two provinces (Free State and Gauteng) and within the HPA, ten municipalities in two provinces (Gauteng and Mpumalanga). The total population count of all areas included in the study area at the last complete census in 2011 was 10,134,241 [23]. Figure 1 indicates the location of the study area in South Africa and the municipalities included in the analysis.
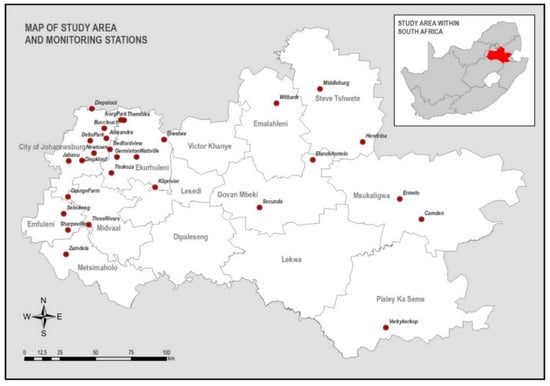
Figure 1.
Study area and monitoring stations.
3. Data and Methods
Health impact assessments use data from available epidemiological studies and routine environmental and health data to estimate the impacts of air quality on the health of a given population. This study took a predictive approach, as it aimed to assess the future health impact of a specific intervention measure. This approach does require making assumptions about future trends involving the study population, health outcomes, the time required to achieve decrease pollutant levels, or when health outcomes will occur [24].
A variety of tools exist to aid analysts, but the majority use the same inputs and process to relate changes in air quality to health outcomes in a particular population. To better fit the context of this study and the high spatial resolution required to most accurately estimate exposure to PM2.5 from residential solid fuel burning, we used the small area level census dataset to deploy a land use type ordinary least squares model. This model provided estimates of mean PM2.5 concentrations that were used together with the census data to identify areas where health benefits associated with reduced residential solid fuel burning could be expected. The HIA was then conducted in these identified areas, using the well-established health impact function approach [25,26] represented by Equation (1) below:
ΔY = Y0 (1-eβΔPM) × Pop
In the context of this study, ΔY represents the change in the number of premature all-cause mortalities; Y0 the baseline all-cause mortality incidence; β the risk coefficient (concentration-response function) derived from epidemiological studies; ΔPM the change in PM exposure after implementation of the intervention (µg m−3), and Pop the size of the exposed population. The following sections will discuss the data and methods used to derive each of these required inputs.
3.1. Air Quality Data
Air quality data is a key input for HIA. In order to calculate the health effects of improvements in air quality, two datasets are needed. Firstly, baseline air quality conditions (where emissions have not yet been controlled) need to be established. These baseline conditions are then used as a reference scenario against which to compare the intervention or control scenario [25]. The control scenario generally represents air quality levels after the implementation of a new policy. In this case, the control scenario represents changes after the implementation of thermal insulation as an intervention measure.
Monitoring data for PM10 and PM2.5 were obtained from the South African Air Quality Information System (SAAQIS). Data were requested for all monitoring stations in the study area from 1998 to 2012. Figure 1 indicates the locations and names of monitoring sites used in this study. Seventeen of the thirty monitoring stations used are situated in densely populated low-income settlements, seven in low-density residential areas, two in areas with heavy urban traffic, one at a power station, one in a rural area, and one in the CBD of Johannesburg. The raw datasets were merged and processed into a final dataset. An automated quality control (QC) was performed, and problematic values were flagged. Flagged data were inspected manually to determine the validity of the potential problems. The data for any problem periods were set to missing.
3.1.1. Baseline Scenario
Various methods were considered to create a representative baseline scenario including the use of a refined dispersion model such as CALPUFF or a comprehensive air quality model such as CAMx. Both models offer considerable benefits including the consistent spatial distribution of the variable of interest and the ability to model basic (CALPUFF) and advanced (CAMx) chemical processes such as secondary particle generation. These models require detailed emissions inventories and meteorological data to run, however. This, along with the fact that neither model was designed for near ground, high resolution modelling made them unsuitable for this study. For HIA in low-income areas, the high spatial and low temporal variability of annual PM concentrations need to be presented as accurately as possible, as these areas house a significant portion of South African society. Areas located just outside low-income areas typically show less annual spatial variability [14]. Monitoring data is the only reliable way to do this, even when considering the limited amount of monitoring sites and high spatial variability in the study area. For these reasons, we used a land use type ordinary least squares regression, using available monitoring data to create the baseline PM2.5 concentrations for this study.
We used data from the 2011 Census for this part of the analysis with enumeration areas (EAs) as the scale of analysis. EAs are the smallest geographical areas into which the country is divided for the census (also called the ‘small area level dataset’). The census dataset includes a large number of housing and household goods and services-related statistics, including energy/fuel use, access to basic services, and type of dwelling. The underlying philosophy of this approach is very similar to that of Wright and Diab (2011) [27], who also used census data to better represent the socio-economic factors that play such an important role in exposure and vulnerability to adverse health impacts in this context. We used PM10 concentrations as the dependent variable. To avoid overfitting data and covariance between variables, only a few independent variables that represent the important drivers of ambient air quality in low-income settlements were included:
- Percentage of households using “dirty” fuels for cooking, heating, or lighting in each EA.
- Percentage of informal households in each EA.
- Population density in each EA.
We trained the model using the variables obtained from different sources within a 250 m radius of each of the available monitoring stations, and the EA layer of the 2011 census data used to deploy the model. Figure 2 illustrates how this method filled the “gaps” in air quality data relative to the population in the study area.
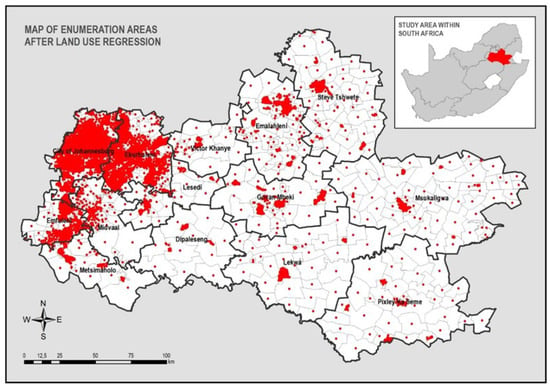
Figure 2.
Map of numeration areas after land use regression.
We converted PM10 concentrations to PM2.5 using a conversion factor of 0.5. This conversion factor is recommended for use in urban areas of developing countries by the World Health Organisation (WHO) [28]. Mean annual PM10 and PM2.5 concentrations for each monitoring station are shown in Figure 3.
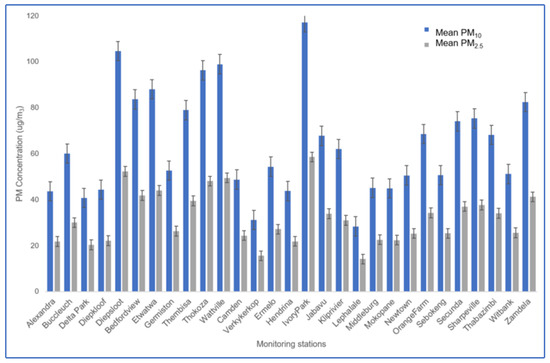
Figure 3.
Mean annual PM concentrations by monitoring station.
3.1.2. Control Scenario
For an accurate representation in the context of the study, we used findings from a pilot air quality offset project in the community of KwaDela to estimate post intervention air quality improvements. The township of KwaDela lies within the administrative borders of the Msukaligwa local municipality. The community of KwaDela is very representative of low-income settlements on the Highveld in terms of household size, age and sex ratios, annual household income, and employment status.
KwaDela was chosen for the project site because of these population characteristics, along with its geographic location far from industrial and other urban sources, small population size (total population of 3786 and 1000 total households), and high levels of dependence on solid fuel burning for cooking and space heating. A total of 790 out of 1000 households in the settlement reported using solid fuels at the time of the intervention. The project involved a pre-intervention air quality sampling campaign in the cold and warm seasons of 2013–2014, followed by the retrofitting of 505 houses with thermal insulation from February to June 2014, and a post-intervention sampling campaign in the cold and warm months of 2014 and early 2015. Only formal housing structures were retrofitted with thermal insulation. The total cost of implementation for this intervention was ZAR (2013) 6.5 million or ZAR (2013) 12,000 per house. This converts to a total of USD (2013) 676,000 or USD (2013) 1227 per house.
The standard deviation of sampled PM2.5 concentrations in KwaDela was on the same order of magnitude as the mean. This large variability would make it difficult to detect relatively small decreases due to better thermal insulation. In this case, we used the difference between the two observed pre- and post- intervention means (4 ug/m3) to estimate the effect the intervention had on ambient air quality in KwaDela (using Cohen’s d). For this campaign, the difference did not obtain statistical significance (d = 0.6). Thermal comfort improved in all retrofitted houses and households reported using fewer solid fuels, indicating a positive impact on the household scale.
As the aim of this study was to estimate the health and economic benefits of the regional implementation of thermal insulation, we used the difference between the means of the two sampling campaigns as the control value. The control value of 4 ug/m3 was applied to all EAs where more than 10% of households reported using dirty fuels as an energy source for either lighting, cooking, or heating. PM2.5 concentrations in areas where less than 10% of households reported using dirty fuels were left unchanged. △ values in the control dataset were thus either 0 ug/m3 or 4 ug/m3, in order to estimate health benefits of air quality improvements in only those areas where dirty fuels are used.
3.2. Choice of Concentration-Response Function
Concentration-response functions (CRF) are derived from epidemiological studies. They represent the statistical relationship between a certain adverse health effect and ambient air pollution concentrations. The choice of health outcomes to include in an assessment is largely based on available evidence from epidemiological and scientific literature and the availability of data regarding baseline incidence rates. To be truly representative, incidence rates should ideally be collected at the place and scale of assessment (e.g., city, province, local municipality) and should match the age cohort being studied [29].
This study aimed to establish the long-term health and economic benefits of thermal insulation as an air pollution intervention measure in low-income settlements. Therefore, only long-term benefits associated with improved air quality were included in this analysis. In order to minimise double counting the health effects of reduced PM2.5 concentrations, our analysis was limited to the impacts of reduced PM2.5 emissions on premature all-cause mortality, as reliable morbidity and hospital admission records are difficult to collect in South Africa. No long-term epidemiological studies to establish local CRFs have been conducted in South Africa [30] and therefore, the most suitable CRF had to be identified from literature.
To estimate the impacts of reduced PM2.5 on premature all-cause mortality, we chose the CRF from the extended analysis of the ACS cohort study by Krewski et al. (2009) [31] due to the statistical power of a cohort study spanning 35 years. Their risk estimate for all-cause mortality (Table 1) was calculated using a random effects Cox model that controlled for 7 ecological and 44 individual covariates, based on average exposure levels for over 116 US cities.

Table 1.
Risk estimate from Krewski et al., 2009.
3.3. Population Data and Baseline All-Cause Mortality Incidence
We used population data from the 2011 census at the EA level to establish the number of people exposed in each area. Using data at such a high spatial resolution is needed in order to take the high spatial variably in population densities and living conditions that influence household emissions and population exposure to HAP into account. The census dataset provides an age breakdown of the population in each EA and thus it was possible to calculate the population aged ≥ 30 for each EA, to better match the CRF [31] chosen for this study.
Mortality by cause of death statistics for 2011 were obtained at the local municipality level from Statistics South Africa. Data were extracted according to the ICD 10 code for main cause of death (ICD 10 A00-Y98) for all deaths that occurred at age ≥ 30. The remaining data were then sorted according to local municipality of death and the total number of deaths ≥ 30 for each municipality calculated. The baseline mortality rate for each municipality was then calculated (total population ≥ 30/total mortality ≥ 30) to be applied to each EA within the administrative border of each respective municipality. For this study, we assume that the annual birth and mortality rates remain constant at the 2011 count, and that there is no migration. This will result in underestimations of future health benefits but should still provide a good estimate of the impacts of improved air quality on the study population.
3.4. Health Impact Assessment
All inputs discussed above were applied to each EA on the census 2011 dataset for the study area (n = 14,330). The health impact for each small area was calculated using Equation (1) discussed above. Health impacts were thus calculated for each EA using site-specific air quality data, population numbers, and mortality incidence rates. Results for each EA were then sorted by local municipality and summed. In our main analysis, we made the same assumptions as Broome et al. (2015) and Fann et al. (2012) [25,26]:
- We assumed the intervention to cause immediate reductions in PM2.5 and that this would have an immediate impact on health, continuing for 20 years;
- That all PM2.5 related deaths are attributable to exposure to our modelled air quality, occurring over a 20-year period, with the largest number of avoided deaths occurring in the earlier years.
3.5. Economic Valuation of Health Benefits
When calculating the economic value of health benefits, we do not calculate the value of an individual life, but rather the sum of all small individual changes in risk [32]. For this study, we used the Value of a Statistical Life (VSL) for economic valuation, a widely used method to estimate the economic value of avoided premature mortality [32,33]. There is currently no standard VSL available for South Africa, thus we adapted the United States Environmental Protection Agency’s (US EPA) standard VSL by using the benefits transfer technique. This method was used by Leiman et al. (2007) [34] when they evaluated the economic value of reduced healthcare costs of urban air pollution in South Africa. The benefits transfer technique involves adjusting the VSL from the original study to reflect the differences in income, income growth, inflation, and Purchasing Power Parity (PPP) between study areas. Thus, these adjustments reflect changes in real income over time [35]. We converted the US EPA standard VSL (in USD 2008) to a 2011 South African Rand (ZAR) value using the following formula:
where VSL (ZAR 2011) is the converted VSL value for South Africa in 2013 ZAR; VSLUS,2008 is the VSL value for the United States in 2008 USD; Y is the per capita GDP of South Africa and the United States in 2008, expressed in international (Purchasing Power Parity (PPP)-adjusted) dollars, and elasticity represents the income elasticity of the VSL. In this case, we used the US EPA recommended value of 0.40, as well as the more conservative elasticity used by Leiman et al. (2007) [34], for comparison purposes. PPPSA,2008 is the PPP index in 2008 (in units of ZAR per International dollar) and CPI represents the consumer price index for South Africa in 2011 and 2008, respectively. All economic data for the US and South Africa were obtained from the World Bank Open Data database in 2017. The VSL values used in this study are presented in Table 2 below.

Table 2.
VSL for South Africa in ZAR 2011.
The VSL was multiplied with the avoided premature mortalities calculated in each EA and aggregated at the local municipality level.
4. Results
4.1. Air Quality Estimates
A land use type ordinary least squares regression was performed to predict the relationship between variance in PM10 concentrations and the population density (POPDENS), percentage of households using dirty fuels (DIRTY), and percentage of informal households (INFORMAL) in each EA. The mean R2 (0.815) shows that 85% of PM10 variability is related to the population density, % of household using dirty fuels, and % of informal households in the study area. The adjusted R2 (0.790), used to assess the number of predictors included in the analysis, indicates that the number of predictors used in the regression are a good fit. The percentage of informal households showed the strongest positive correlation with PM10 concentrations (r = 0.45) followed by much weaker positive correlations for the percentage of dirty fuels (r = 0.0023) and population density (r = 0.0021). Model output is summarised in Table 3.

Table 3.
Land use type regression output.
A total of 3056 (n = 14,330) EAs were identified as areas where more than 10% of households reported using dirty fuels (total number of households: 586,308). This represents 21% of the total EAs within the study area (Table 4). Municipalities where more than 50% of EAs were identified as suitable control areas include Pixley Ka Seme (92%), Msukaligwa (83%), Victor Khanye (80%), Lekwa (65%), Lesedi (54%), Govan Mbeki (53%), and Steve Tshwete (52%). Much lower percentages of EAs were identified in major urban areas. The lowest percentage recorded was for the City of Johannesburg (6%), followed by Emfuleni (10%) and Ekurhuleni (23%). Overall, populations of municipalities located in the HPA show a much higher reliance on solid fuel burning than those in the VTAPA. Total control areas identified for each municipality are summarised in Table 4.

Table 4.
Total number of Enumeration Areas (EAs) per municipality and number of EAs included in the Health Impact Assessment (HIA) per municipality.
Our land use regression model showed high spatial variability of PM2.5 concentrations over the Highveld (Figure 4). This conforms to our current understanding of the high impact of residential solid fuel burning emissions with limited spatial extent during stable conditions. The model did not however show dispersion between source areas and does not accurately represent areas of low concentrations. Most of the area shows typical background PM2.5 concentrations of between 20 to 30 ug/m3. The spatial variability of modelled baseline concentrations closely matches the population distribution in the area, with highest concentrations in densely populated areas. The spatial distribution of baseline PM2.5 concentrations is mapped in Figure 4.
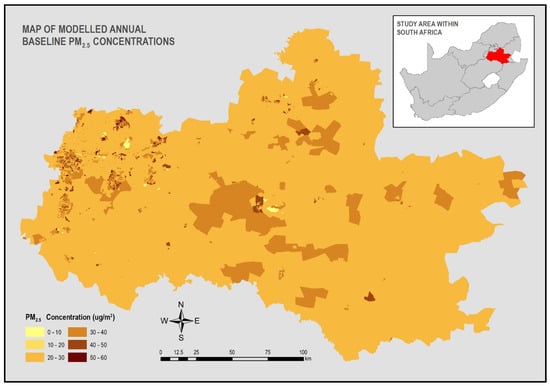
Figure 4.
Map of modelled annual baseline PM2.5 concentrations.
4.2. Estimates of Avoided PM2.5 Mortalities and Related Economic Benefits
We estimate that reducing PM2.5 exposure by 4 ug/m3 in the identified 21% of EAs on the Highveld will result in 143 (95% CI: −52–276) avoided premature deaths over 20 years. It is important to note that these deaths are not avoided altogether, but only deferred to the future. The economic benefits associated with these avoided premature mortalities are estimated to be just under ZAR (2011) 1.8 billion (0.4 elasticity) and ZAR (2011) 380 million (1.5 elasticity). This large difference in estimates reiterates the need for careful consideration of the study context when using the benefits transfer technique. We believe the conservative estimate by Leiman et al. (2007) to be more representative in the context of this study, as life expectancy was 19 years higher in the United States (78 years) than in South Africa (59 years) in 2011 according to the World Bank data bank of World Development Indicators. All further discussions of economic benefits will thus refer to estimates calculated using their chosen elasticity of 1.5. Table 5 summarises the economic valuations for both elasticities.

Table 5.
Summary of health and economic benefits per municipality.
5. Discussion
The metropolitan municipality of Ekurhuleni would benefit the most from air quality improvements in low-income settlements, with an estimated 49 avoided premature mortalities. The economic benefit of these avoided deaths is estimated to be just under ZAR (2011) 120 million (USD 17.4 million). Ekurhuleni is densely populated (1609 persons/km2) and 22.6% of the population lived in informal housing in 2011. Of the residents, 82% had access to electricity in 2011, but 23% of the EAs within the city were identified as areas where solid fuel burning could cause air quality problems.
Estimates for the only other metropolitan municipality in the study area, City of Johannesburg, is significantly lower (11 avoided premature mortalities valued at ZAR 2011 28.7 million or 2011 USD 4.1 million), despite the fact that the city is the most densely populated area in South Africa at 2696 persons/km2. In this municipality, 90.8% of the population had access to electricity and 81.4% lived in formal housing in 2011. Only 6% of EAs within the administrative boundaries of Johannesburg were identified as areas where more than 10% of households reported using dirty fuels. This large contrast between the two major metropolitan areas highlights the important role that living conditions and access to infrastructure have in determining public health and population exposure in this context. The spatial distribution of health and economic benefits are illustrated in Figure 5. The municipalities with the second highest estimated health benefits are Lesedi and Msukaligwa, both situated in the HPA. Thirteen avoided premature mortalities were predicted for each municipality. The combined economic benefits of these 26 avoided deaths were estimated to be just over ZAR (2011) 68 million (2011 USD 9.8 million).
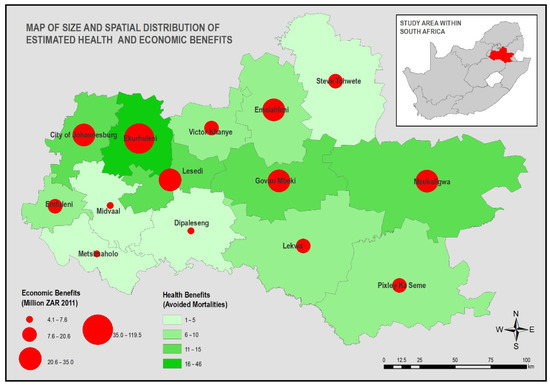
Figure 5.
Size and spatial distribution of estimated health and economic benefits.
Overall, both municipalities are sparsely populated, Msukaligwa at 25 persons/km2 and Lesedi at 67 persons km2, but in certain EAs, population densities were much higher. Wesselton, a township outside Ermelo in Msukaligwa, is very densely populated with 14,689 persons/km2, for example. This high spatial variability again highlights the need to use population data at the highest spatial resolution available for HIA in this context.
Large parts of the population in both these municipalities are reliant on solid fuel burning to supplement their energy needs: 54% of EAs in Lesedi and 83% of EAs in Msukaligwa were identified for inclusion in the HIA. The reliance on solid fuels in Msukaligwa could be due to the fact that only 75% of the population in Msukaligwa had access to electricity, and 25% of the population lived in informal dwellings in 2011 (StatsSA, 2012). The municipality is also located close to the Mpumalanga coalfields, where coal is widely available as a cheaper alternative fuel source. The population of Lesedi is smaller than that of Msukaligwa by almost 50,000 people and 90% of the population had access to electricity in 2011, yet the health benefits for both municipalities are estimated to be the same. This could be ascribed to higher overall population density in Lesedi. All other results of the HIA and economic valuation are summarised by municipality in Table 4.
The cost of retrofitting one house with thermal insulation in KwaDela was ZAR 12,000 (USD 1227), with a total cost of ZAR 6.5 million for 505 houses in 2013. Since this analysis was conducted at the EA scale, it is not possible to accurately compare the estimated economic benefits of reduced premature mortality with the cost of installation per eligible household. Avoided premature mortality is only one avoided health outcome; the benefits of avoided morbidity, hospital admissions and lost productivity, for example, are not accounted for in this analysis. Moreover, not all households in identified EAs use solid fuels for their energy needs, calculating the cost of implementation per EA will therefore lead to an overestimation of implementation costs. For example, implementation of this intervention in all 321,922 formal housing structures located in the identified EAs will amount to ZAR (2013) 3,863,064,000 or USD (2013) 401,758,656.
Calculating an accurate cost of implementation will require analysis at the household scale and was not in the scope of this study. Our analysis did reveal specific areas that could be considered for this type of intervention. Thermal insulation will most probably not be a cost-effective intervention in the VTAPA, where our analysis showed low household reliance on solid fuels. The intervention could however be successful in the HPA, especially in municipalities where more than 50% of EAs were identified as suitable control areas. These include Pixley Ka Seme (92%), Msukaligwa (83%), Victor Khanye (80%), Lekwa (65%), Lesedi (54%), Govan Mbeki (53%), and Steve Tshwete (52%). Our method is a useful tool to identify areas that warrant further investigation to establish suitability and cost effectiveness for implementation of this specific intervention measure.
6. Conclusions
The impact of household emissions on ambient air quality is problematic to assess, due to the high spatial variability between areas of high concentration and socio-economic conditions that drive household solid fuel use within communities. A land use regression model was deployed using the small area level census dataset in order to more accurately estimate the spatial variation in mean annual PM2.5 concentrations over the region and identify areas where socio-economic factors could contribute to HAP. Estimates of mean PM2.5 concentrations were used together with the census data to identify areas where reduced residential solid fuel burning could decrease population exposure. This approach used freely available data and can provide insights to specific locations where certain intervention measures could be most effective, based on the socio-economic characteristics of communities. Considering the limited resources available in developing countries like South Africa, this community centred approach could provide cost effective, evidence-based guidance to air quality management policies and regulations.
The use of spatially representative baseline ambient PM concentrations, population densities, incidence data, and delta (control) values provided a more representative analysis scenario, and can be helpful in targeting and reducing air quality-related health inequities in South Africa. Overall, populations of municipalities located in the HPA show a much higher reliance on solid fuel burning than those in the VTAPA. The HPA could thus be a better area for large-scale roll out of thermal insulation as part of air quality offset programs. Results indicate that reducing PM2.5 concentrations in areas where residents burn solid fuels by 4 ug/m3 would result in an estimated 143 avoided premature mortalities. The economic value of these benefits was estimated to be ZAR (2011) 370.1 million. A more spatially refined analysis is needed to compare the intervention implementation cost in all identified households to the estimated economic benefits of reduced premature mortalities. Socio-economic variables will also need to be adjusted depending on geographic location and intervention type. Further analysis on the costs of other air pollution-related health outcomes should be conducted, as mortality-related costs represent only the most severe outcome. We need better estimations of the true health and cost benefits of improved air quality in order to design and implement targeted mitigation and management approaches.
Limitations of this Study
Transferring the health impacts and economic valuations calculated for populations in developed countries onto our study population introduced considerable uncertainty to our results. The demographic profile, socio-economic conditions, and pollutant mix in our study population and area differ considerably from the population used by Krewski et al. (2009) to derive the CRF used in this study. The Integrated Exposure Response (IER) functions developed for the Global Burden of Disease (GBD) assessment could provide better estimates. The IERs were developed for cause-specific morbidity and mortality (Smith et al., 2014). Since the scope of this study included all-cause mortality to avoid double counting attributable mortalities, these IERs were not used. Assumptions made that population growth-, death-, and migration rates remained steady at the 2011 rates will result in an underestimation of the health benefits assumed to occur over 20 years. Our results should thus be interpreted as a conservative estimate. Limited monitored air quality data available for the study area could lead to the over- or under-estimation of population exposure. Since 17 out of the 30 monitoring stations used to estimate baseline air quality were situated in densely populated low-income settlements, we believe the data to be representative of exposure levels in our study population.
Despite the limitations and assumptions that were made during this HIA process, we believe that it could be a valuable tool to help identify areas where interventions would be most effective by taking a more community-centred approach to air quality management measures.
Author Contributions
Conceptualisation, L.F.L., R.P.B. and S.J.P.; methodology, L.F.L., R.P.B. and S.J.P.; formal analysis, L.F.L. and R.P.B.; data curation, L.F.L. and R.P.B.; writing—original draft preparation, L.F.L.; writing—review and editing, L.F.L., R.P.B. and S.J.P.; supervision, R.P.B. and S.J.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded in part by a National Research Foundation (NRF) institutional block grant awarded to L.F.L. by North-West University.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The authors would like to thank the following institutions for the provision of data: the South African Weather Service (SAWS) for the provision of monitored air quality data and Statistics South Africa (StatsSA) for the provision of mortality data for local municipalities.
Acknowledgments
L.F.L. would like to thank Eunice Erasmus for her assistance with technical editing and map creation for this study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Wenig, M.; Spichtinger, N.; Stohl, A.; Held, G.; Beirle, S.; Wagner, T.; Jähne, B.; Platt, U. Intercontinental transport of nitrogen oxide pollution plumes. Atmos. Chem. Phys. Discuss. 2003, 3, 387–393. [Google Scholar] [CrossRef] [Green Version]
- Food and Agriculture Organization of the United Nations. National Environmental Management: Air Quality Act No. 39 of 2004; Department of Environmental Affairs: Pretoria, South Africa, 2004.
- Kerimray, A.; Rojas-Solórzano, L.R.; Torkmahalleh, M.A.; Hopke, P.K.; Gallachoir, B.O. Coal use for residential heating: Patterns, health implications and lessons learned. Energy Sustain. Dev. 2017, 40, 19–30. [Google Scholar] [CrossRef]
- Ezzati, M.; Kammen, D.M. The health impacts of exposure to indoor air pollution from solid fuels in developing countries: Knowledge, gaps, and data needs. Environ. Health Perspect. 2002, 110, 1057–1068. [Google Scholar] [CrossRef] [Green Version]
- Abbafati, C.; Abbas, K.M.; Abbasi-Kangevari, M.; Abd-Allah, F.; Abdelalim, A.; Abdollahi, M.; Abdollahpour, I.; Abegaz, K.H.; Abolhassani, H.; Aboyans, V.; et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1223–1249. [Google Scholar] [CrossRef]
- Shupler, M.; Godwin, W.; Frostad, J.; Gustafson, P.; Arku, R.E.; Brauer, M. Global estimation of exposure to fine particulate matter (PM2.5) from household air pollution. Environ. Int. 2018, 120, 354–363. [Google Scholar] [CrossRef]
- Smith, K.R.; Bruce, N.; Balakrishnan, K.; Adair-Rohani, H.; Balmes, J.; Chafe, Z.; Dherani, M.; Hosgood, H.D.; Mehta, S.; Pope, D.; et al. Millions Dead: How Do We Know and What Does It Mean? Methods Used in the Comparative Risk Assessment of Household Air Pollution. Annu. Rev. Public Health 2014, 35, 185–206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adamkiewicz, Ł.; Kryza, M.; Mucha, D.; Werner, M.; Gayer, A.; Drzeniecka-Osiadacz, A.; Sawiński, T. Estimating Health Impacts Due to the Reduction of Particulate Air Pollution from the Household Sector Expected under Various Scenarios. Appl. Sci. 2020, 11, 272. [Google Scholar] [CrossRef]
- Clifford, A.; Lang, L.; Chen, R.; Anstey, K.J.; Seaton, A. Exposure to air pollution and cognitive functioning across the life course—A systematic literature review. Environ. Res. 2016, 147, 383–398. [Google Scholar] [CrossRef] [PubMed]
- Pope, C.A.; Cohen, A.J.; Burnett, R.T. Cardiovascular Disease and Fine Particulate Matter. Circ. Res. 2018, 122, 1645–1647. [Google Scholar] [CrossRef]
- Birnbaum, H.G.; Carley, C.D.; Desai, U.; Ou, S.; Zuckerman, P.R. Measuring The Impact Of Air Pollution On Health Care Costs. Health Aff. 2020, 39, 2113–2119. [Google Scholar] [CrossRef] [PubMed]
- Umuhoza, S.M.; Ataguba, J.E. Inequalities in health and health risk factors in the Southern African Development Community: Evidence from World Health Surveys. Int. J. Equity Health 2018, 17, 52. [Google Scholar] [CrossRef] [Green Version]
- Adesina, J.; Piketh, S.; Qhekwana, M.; Burger, R.; Language, B.; Mkhatshwa, G. Quantifying the effect of air quality offsets on household air pollution and thermal comfort on the South Africa Highveld. Clean Air J. 2020, 30, 1. [Google Scholar] [CrossRef]
- Hersey, S.P.; Garland, R.M.; Crosbie, E.; Shingler, T.; Sorooshian, A.; Piketh, S.; Burger, R. An overview of regional and local characteristics of aerosols in South Africa using satellite, ground, and modeling data. Atmos. Chem. Phys. 2015, 15, 4259–4278. [Google Scholar] [CrossRef] [Green Version]
- Friedl, A.; Holm, D.; John, J.; Kornelius, G.; Pauw, C.J.; Oosthuizen, R.; Van Niekerk, A.S. Air pollution in dense, low-income settlement in South Africa. In Proceedings of the Annual National Association for Clean Air (NACA) Conference, Nelspruit, South Africa, 1–3 October 2008. [Google Scholar]
- Moletsane, S.D.; Lindeque, F.; Language, B.; Nkosi, N.C.; Adesina, J.A.; Burger, R.P.; Mkhatshwa, G.; Piketh, S.J. Intra-urban variability of PM2.5 in a dense, low-income settlement on the South African Highveld. Clean Air J. 2021, 31, 1–9. [Google Scholar] [CrossRef]
- DEA. Air Quality Offsets Guideine; Department of Environmental Affairs: Pretoria, South Africa, 2016.
- Van Niekerk, W. From technology transfer to participative design: A case study of pollution prevention in South African town-ships. J. Energy S. Afr. 2006, 17, 58–63. [Google Scholar] [CrossRef]
- Adesina, J.; Piketh, S.; Qhekwana, M.; Burger, R.; Language, B.; Mkhatshwa, G. Contrasting indoor and ambient particulate matter concentrations and thermal comfort in coal and non-coal burning households at South Africa Highveld. Sci. Total Environ. 2020, 699, 134403. [Google Scholar] [CrossRef]
- West, J.J.; Cohen, A.; Dentener, F.; Brunekreef, B.; Zhu, T.; Armstrong, B.; Bell, M.; Brauer, M.; Carmichael, G.; Costa, D.L.; et al. What We Breathe Impacts Our Health: Improving Understanding of the Link between Air Pollution and Health. Environ. Sci. Technol. 2016, 50, 4895–4904. [Google Scholar] [CrossRef]
- Pope, C.A.; Dockery, D.W. 2006 CRITICAL REVIEW Health Effects of Fine Particulate Air Pollution: Lines that Connect. J. Air Waste Manag. Assoc. 2006, 56, 709–742. [Google Scholar] [CrossRef]
- Department of Environmental Affairs (DEA). Highveld Priority Area Air Quality Management Plan Executive Summary; Department of Environmental Affairs: Pretoria, South Africa, 2012.
- Statistics South Africa Statistics by Place. Available online: http://www.statssa.gov.za/?page_id=964 (accessed on 5 November 2017).
- Pascal, M.; Corso, M.; Chanel, O.; Declercq, C.; Badaloni, C.; Cesaroni, G.; Henschel, S.; Meister, K.; Haluza, D.; Martin-Olmedo, P.; et al. Assessing the public health impacts of urban air pollution in 25 European cities: Results of the Aphekom project. Sci. Total Environ. 2013, 449, 390–400. [Google Scholar] [CrossRef] [PubMed]
- Fann, N.; Lamson, A.D.; Anenberg, S.C.; Wesson, K.; Risley, D.; Hubbell, B.J. Estimating the National Public Health Burden Associated with Exposure to Ambient PM2.5 and Ozone. Risk Anal. 2012, 32, 81–95. [Google Scholar] [CrossRef] [PubMed]
- Broome, R.A.; Fann, N.; Cristina, T.J.N.; Fulcher, C.; Duc, H.; Morgan, G. The health benefits of reducing air pollution in Sydney, Australia. Environ. Res. 2015, 143, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Wright, C.Y.; Diab, R. Air pollution and vulnerability: Solving the puzzle of prioritization. J. Environ. Health 2011, 73, 56–64. [Google Scholar] [PubMed]
- WHO. Air Quality Guidelines. Global Update 2005; World Health Orginization Regional Office for Europe: Copenhagen, Denmark, 2006. [Google Scholar]
- Fann, N.; Fulcher, C.M.; Hubbell, B.J. The influence of location, source, and emission type in estimates of the human health benefits of reducing a ton of air pollution. Air Qual. Atmos. Health 2009, 2, 169–176. [Google Scholar] [CrossRef] [Green Version]
- Shezi, B.; Wright, C.Y. Household air pollution exposure and respiratory health outcomes: A narrative review update of the South African epidemiological evidence. Clean Air J. 2018, 28, 43–56. [Google Scholar] [CrossRef]
- Krewski, D.; Jerrett, M.; Burnett, R.T.; Ma, R.; Hughes, E.; Shi, Y.; Turner, M.C.; Pope, C.A., III; Thurston, G.; Calle, E.E.; et al. Extended Follow-Up and Spatial Analysis of the American Cancer Society Study Linking Particulate Air Pollution and Mortality; Health Effects Institute: Boston, MA, USA, 2009. [Google Scholar]
- OECD. Valuing Mortality Risk Reductions in Regulatory Analysis of Environmental, Health and Transport Policies: Policy Implications; Organization for Economic Co-operation and Development: Paris, France, 2011. [Google Scholar]
- Chanel, O. Guidelines on Monetary Cost Calculations Related to Air-Pollution Health Impacts: Aphekom Project; Institut de Veille Sanitaire: Saint-Maurice, France, 2011. [Google Scholar]
- Leiman, A.; Standish, B.; Boting, A.; Van Zyl, H. Reducing the healthcare costs of urban air pollution: The South African experience. J. Environ. Manag. 2007, 84, 27–37. [Google Scholar] [CrossRef]
- Hammitt, J.K.; Robinson, L.A. The Income Elasticity of the Value per Statistical Life: Transferring Estimates between High and Low Income Populations. J. Benefit-Cost Anal. 2011, 2, 1–29. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).