Abstract
Nephrolithiasis ranks third among urological diseases in terms of prevalence, making up about 15% of cases. The continued increase in the incidence of nephrolithiasis is most probably due to changes in eating habits (high protein, sodium, and sugar diets) and lifestyle (reduced physical activity) in all developed countries. Some 80% of all kidney stones cases are oxalate urolithiasis, which is also characterized by the highest risk of recurrence. Frequent relapses of nephrolithiasis contribute to severe complications and high treatment costs. Unfortunately, there is no known effective way to prevent urolithiasis at present. In cases of diet-related urolithiasis, dietary changes may prevent recurrence. However, in some patients, the condition is unrelated to diet; in such cases, there is evidence to support the use of stone-related medications. Interestingly, a growing body of evidence indicates the potential of the microbiome to reduce the risk of developing renal colic. Previous studies have primarily focused on the use of Oxalobacter formigenes in patients with urolithiasis. Unfortunately, this bacterium is not an ideal probiotic due to its antibiotic sensitivity and low pH. Therefore, subsequent studies sought to find bacteria which are capable of oxalate degradation, focusing on well-known probiotics including Lactobacillus and Bifidobacterium strains, Eubacterium lentum, Enterococcus faecalis, and Escherichia coli.
1. Introduction
Nephrolithiasis is characterized by the presence of insoluble deposits in the urinary tract, so-called stones, that obstruct the proper urine flow. These deposits are a result of increased calcium, oxalic acid, phosphate, urate, and cystine levels in the urine. Unfortunately, the incidence of urolithiasis has dramatically increased over the past 30 years, likely due to environmental changes, including inadequate diet and physical activity [1]. Nowadays, nephrolithiasis ranks third in the list of the most common urological diseases [2]. The incidence of urolithiasis ranges from 7 to 13% in North America, 5 to 9% in Europe, and 1 to 5% in Asia. Nephrolithiasis most often occurs in men aged 40–50 years, and in women aged 50–70 [3,4,5]. Epidemiological data have confirmed that the propensity to form deposits in the urinary tract depends on sex, ethnicity, and geography. Until recently, men were characterized as being 2–3-times more likely to develop kidney stones than women. However, a recent analysis suggested that this disparity is disappearing. Between 1970 and 2000, in Minnesota (the United States), the male to female ratio of kidney stone incidents reduced from 3.1 to 1.3 [6]. This increase in the frequency of nephrolithiasis in women might be due to changes in lifestyle and diet causing obesity, a known risk factor for deposit formation in the urinary tract [7]. In addition to its widespread occurrence, nephrolithiasis is also characterized by a high risk of recurrence. The spontaneous five-year recurrence rate is 35 to 50% following the first renal colic [8]. Moreover, in cases of patients who do not use meta-phylaxis, the relapse rate of secondary deposits is estimated to be 10–23% per year, 50% in 5–10 years, and 75% in 20 years after the first occurrence [9]. Unfortunately, urolithiasis recurrence contributes to the development of several complications, such as pyelonephritis, urinary tract infection, renal insufficiency, and even urinary tract cancer [10,11]. The high prevalence and recurrence of urolithiasis in the general population also contribute to high medical care costs. In the United States, the total cost of healthcare for urolithiasis patients was about $2.1 billion in 2000 [12]. Interestingly, it has been estimated that by 2030, this figure will increase by $1.24 billion per year because of the rising prevalence of obesity and diabetes [13].
As noted above, deposits in the urinary tract can vary in their chemical composition; however, 80% of stones are calcium-based, 9% uric acid-based, 10% struvite-based, and 1% are cystine stones [14]. Among all types of urinary calcium stones, 50% are calcium oxalate deposits, 5% are calcium phosphate, and 45% are a mixture of both kinds [15]. Kidney stone formation is a complex and multifactorial process that depends on intrinsic (age, sex, and heredity) and extrinsic (geography, climate, dietary, mineral composition, and water intake) factors [16]. Common risk factors for the development of nephrolithiasis are presented in Table 1.

Table 1.
Risk factors of nephrolithiasis development.
Importantly, disturbing epidemiological data suggest the existence of additional risk factors for the development of urolithiasis. In the last 15 years, the incidence of kidney stones in the United States has doubled, making its prevalence equivalent to that of diabetes. This increase was mainly recorded among children and women. These alarming changes in the incidence of urolithiasis have contributed to the search for new determinants of nephrolithiasis. Additionally, antibiotics and their impact on the composition of the intestinal and urinary microbiome have been examined. Epidemiological analyses have shown that 30% of patients are prescribed at least one antibiotic per year, and previous studies have linked oral antibiotic use with increased prevalence of kidney stones among children and adults [22,23]. Interestingly, Ferraro et al. [24] confirmed the relationship between exposure to antibiotics and changes in the chemical composition of urine. Exposure to antibiotics for at least two months resulted in a decrease in urine pH and urinary citrate levels, suggesting that there is a complex correlation between the gut and urinary tract in kidney stones [24]. These results were confirmed by Stern and colleagues [25]. Genetic hypercalciuric stone-forming rats were characterized by decreased urine pH and urinary citrate levels [25]. Miller et al. [26] confirmed previous reports which found that the multispecies bacterial network, containing, e.g., Ruminococcus, Oscillospira, Desulvovibrio and Methanobrevibacter, maintains oxalate homeostasis [26]. Thus, the present study aimed to identify unique changes in the gut microbiome of patients with kidney stones compared to controls. The obtained results showed that Bacteroides was 3.4 times more abundant in the kidney stone group compared to the control, while Prevotella was 2.8 times more abundant in the control group compared to the kidney stones group [27]. Thus, the presented results suggest the existence of an entero-renal axis as the pathway between the gut microbiome, gut metabolites, and urine chemistry, which determines human health and disease [24].
Kidney stones form when urine contains more dissolved material (such as calcium, oxalate, and uric acid) than can be dissolved under normal circumstances [28]. The mechanism of deposit in the urinary tract is presented in Figure 1. The level of calcium in the urine depends on the calcium content in the diet, as well as on the correct function of the metabolic pathways; e.g., with low calcium intake, increased calcium level in the urine may be a consequence of increased bone resorption. In turn, urinary oxalate comes mostly from endogenous metabolic processes, although an additional source may be the increased absorption of oxalate in the intestine with concomitant higher calcium intake [29,30]. Interestingly, dietary oxalate may account for almost 50% of the daily oxalate excreted in urine. Moreover, calcium oxalate stones have an increased propensity to form in the presence of elevated oxalate, even without elevated calcium [31]. Thus, most research efforts to reduce the recurrence of kidney stones have focused on reducing the amount of oxalate consumed. Currently, beyond changes to diet, there is no effective way to lower urinary oxalate level in stone formers. An analysis of fecal samples showed that patients with recurrent idiopathic calcium stones exhibited lower fecal microbial diversity than controls. In particular, these samples were characterized by low levels of bacteria capable of oxalate degradation [32]. Therefore, previous studies have suggested that probiotic bacteria, especially O. formigenes, Lactobacillus spp. and Bifidobacterium spp., which can degrade dietary oxalate in the gastrointestinal tract allowing it to be absorbed, may help reduce urinary oxalate levels [33].
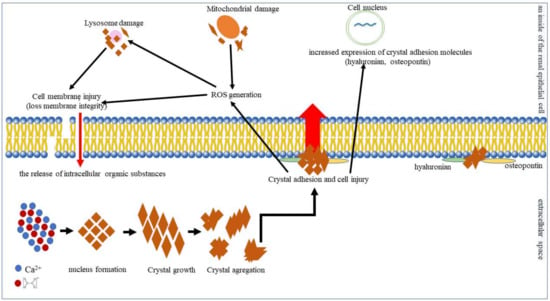
Figure 1.
In supersaturated urine, calcium and oxalate combine to form initially microscopic insoluble crystals. This is the first stage of deposit formation (nucleus formation). Then, individual microcrystals combine into larger forms (crystal growth), which, in turn, can aggregate together to form large, stable deposits (crystal aggregation) [34,35]. In the next stage, the crystals interact with the cells of the renal tubular epithelium. Crystal–cell interaction causes the movement of crystals from the basolateral side of cells to the basal membrane [36]. Injured cells release substances such as the kidney fragment of prothrombin−1 or other anionic proteins that induce crystal agglomeration [37]. Moreover, injured cells can invert their cell membrane, which is anionic to the urinary environment and acts as a place of crystal adhesion. The inverted cell membrane makes it easy for other crystals to attach [38]. Exposure to calcium oxalate crystals induces oxidative stress in renal epithelial cells. In addition, calcium oxalate influences the composition and function of the renal epithelial cell membrane. Calcium oxalate crystals destroy tight junctions and the polarity of the cell membrane that carries the components of the basolateral or tight junction region to the apical surface of the cell, which, in turn, leads to rupture of the cell membrane and the release of intracellular organic substances. Damaged tubular epithelial cells also show increased expression of crystal adhesion molecules such as hyaluronan, osteopontin, and CD44, which promote crystal adhesion and retention. Endocytosed crystals adversely affect mitochondrial function, causing abnormality in the respiratory chain and increasing the mitochondrial production of reactive oxygen species (ROS), which may damage, and induce apoptosis of, renal epithelial cells [39].
2. Oxalobacter formigenes
2.1. Characteristics of Oxalobacter formigenes
Oxalobacter formigenes comprises immobile, nonspore-forming, obligate, anaerobic, Gram-negative rods which inhabit the human colon and ruminant rumen. It was discovered by Allison and coworkers in 1985 [40]. The characteristics of O. formigenes are presented in Table 2. Due to oxalate use as the sole source of carbon and energy, O. formigenes is called a specialist oxalotroph. Thus, this bacteria can degrade ingested oxalate and reduce intestinal absorption, as well as stimulating the excretion of oxalate from the colon, thereby providing protection from hyperoxaluria, when it presents in the gut microflora [41,42]. It has been assumed that the number of O. formigenes cells per gram of stool is 107, and the efficiency of the oxalate degradation process in this environment has been estimated to be 0.1–4.4 nmol per hour per g of stool [43]. However, previous studies have shown that the prevalence of O. formigenes varies among the general population. One epidemiological study suggested that O. formigenes colonization is associated with the age of the individual, reaching 100% detection in children, and only 40–60% in adults [44]. Interestingly, Sidhu et al. [45] found that feces collected from newborns and infants less than nine months old showed an absence of O. formigenes, but that this bacterium was detectable in the feces of children of crawling age. Almost all children between six and eight years old were colonized, but the colonization rate reduced in older children to around that found in the adult population (around 70%) [45]. This variation in O. formigenes colonization may be due to high bacterial sensitivity to antibiotics, the use of which is more common among the older population. Previous studies showed that a significantly reduced level of O. formigenes gut colonization was associated with increased use of antibiotics and other drugs, particularly in the treatment of cystic fibrosis, inflammatory bowel disease, Crohn′s disease, and jejunoileal bypass surgery [44,45].

Table 2.
Characteristics of Oxalobacter formigenes.
The ability of O. formigenes to metabolize oxalate may be attributed to the presence of two enzymes, i.e., formyl-CoA-transferase and oxalyl-CoA-decarboxylase. O. formigenes takes up oxalate via the OxIT transporter encoded by the OxIT. This transport relies on the extracellular uptake of oxaloacetate in return for the formate released from the cell. In bacterial cells, formyl-CoA transferase (encoded by fcr) activates the oxalate by adding coenzyme A molecules with the formation of oxalyl-CoA. Then, oxalyl-CoA is decarboxylated by oxalyl-CoA decarboxylase (encoded by oxc). The oxalyl-CoA decarboxylase produces CO2 and formate, which are used by OxIT to transport oxalate. Oxalate decarboxylation generates a proton pump gradient that induces ATP production, coupling with oxalate–formate transport [46]. Oxalate metabolism is presented in Figure 2.
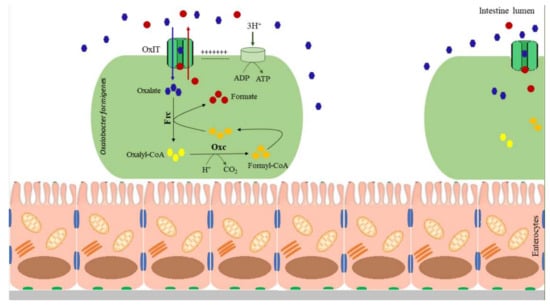
Figure 2.
Oxalate metabolism by Oxalobacter formigenes. OxIT—oxalate transporter, Oxc—oxalyl-CoA decarboxylase, Frc—formyl-CoA transferase.
2.2. Oxalobacter formigenes and Kidney Stone Course
Previous analyses have shown that up to 40% of the oxalate present in the urine may come from the intestines. These results suggest that limiting the absorption of oxalate in the gut may be important for minimizing the risk of developing or recurring urolithiasis [47]. O. formigenes regulates intraluminal oxalate availability by degrading dietary oxalate, using oxalate as an obligatory energy source, thereby reducing intestinal oxalate absorption and urinary excretion [48]. Consequently, oxalate degradable O. formigenes limits the availability of oxalate for intestinal absorption. However, the intestinal colonization by O. formigenes does not affect other factors related to the development of urolithiasis, such as concentration of calcium, uric acid, sodium, citrate and magnesium in the urine [47]. Hatch et al. [48] suggested that O. formigenes may also interact physiologically with the colonic mucous membrane by inducing enteric oxalate secretion, leading to additional reduction of urinary oxalate excretion [48]. This ability to break down oxalate and reduce urinary oxalate excretion suggests the possible clinical application of O. formigenes in the treatment and prevention of oxalate nephrolithiasis. Unfortunately, a composition analysis did not confirm the presence of O. formigenes in probiotics available on the market which state this bacteria among their ingredients. This suggests that the production of products containing O. formigenes is challenging [49]. The difficulty in making probiotics containing O. formigenes may be due to its sensitivity to oxygen and low pH, strict oxalate demand for growth, and intolerance to the processes which are commonly involved in the manufacture, storage, and distribution of probiotic products. However, recent results suggested that individual strains of O. formigenes may differ in their resistance to the above-mentioned stress stimuli [50]. A molecular analysis showed that some O. formigenes strains can tolerate a lack of calcium oxalate. Prolonged starvation for some bacteria results in growth advantage in the stationary phase (GASP). The GASP phenotype results from stable mutations that provide an improved ability to survive during starvation and temporarily obtain energy from the transformation of other compounds. Similarly, some O. formigenes strains have shown the ability to temporarily acclimatize to aerobic conditions due to the presence of superoxide dismutase [50]. Therefore, O. formigenes is an extensively studied bacterium for the prevention of urolithiasis, and extensive research has been carried out in search of strains which are resistant to the production conditions of probiotics. On the other hand, a previous study suggested that the way O. formigenes is administered determines its effectiveness in terms of colonizing the gut. Successful and long-lasting colonization has been observed in healthy adults where O. formigenes was formulated as a spread on a turkey sandwich with a sodium oxalate load [51], while colonization of the intestines of O. formigenes provided either in lyophilized form or as a frozen cell paste to patients with primary hyperoxaluria was unsuccessful [52]. Thus, further detailed studies on the sensitivity of individual O. formigenes strains to production conditions are necessary.
Previous studies showed that rats fed a diet containing 0.5–1.5% oxalate which became colonized with O. formigenes were characterized by decreased urinary oxalate levels, compared with noncolonized rats on the same diet [48,53,54]. It should be remembered that the dose of O. formigenes administered orally limits the speed and effectiveness of the final gut colonization, due to the low pH of the stomach, which is considered to be the main barrier to the survival of ingested bacteria in the gut. Therefore, a comparative analysis of different doses of O. formingens (1 × 103, 1 × 105, 1 × 107, 1 × 109 CFU), given to subjects on an oxalate-rich diet, showed that the level of the urinary oxalate extraction decrease was directly proportional to the dose of bacteria [54]. Similarly, human studies confirmed that daily intake of O. formigenes can lead to reduced urinary oxalate levels in patients on a diet which is high in calcium oxalate [51,52]. The reduced urinary oxalate levels in subjects on an oxalate-rich diet confirmed in vivo that O. formigenes may be an effective probiotic in preventing the formation of deposits in the urinary tract. Unfortunately, despite achieving statistically significant differences in both of the presented studies, the results were characterized by a low degree of certainty, since the study groups consisted of a small number of patients—four in the case of Duncan’s study and nine in Hoppe’s study [51,52]. On the other hand, a study involving 35 first-time calcium oxalate stone formers and ten control subjects confirmed that urolithiasis patients were characterized by lower levels of O. formigenes gut colonization than healthy volunteers. Intestinal O. formingens was detected in only 26% of stone formers compared with 60% of the control group. Although the obtained results showed that the average urinary oxalate excretion by both groups was similar (38.6 mg/day vs. 40.8 mg/day), among patients with stones, O. formigenes-negative patients were characterized by higher urinary oxalate concentrations than those testing positive, which clearly confirms the role of O. formigenes in oxalate degradation in vivo [49]. Similarly, Siener et al. [55] also confirmed that patients with urolithiasis are characterized by a low level of O. formigenes colonization. Among 37 patients, only 11 were O. formigenes-positive. Additionally, the mean plasma oxalate concentration was more than threefold higher in patients without O. formigenes than patients with this bacteria [55]. Kaufman et al. [56] also showed that adults with kidney stone disease were characterized by less intestinal tract O. formigenes colonization than healthy subjects, and that urinary oxalate exertion might depend upon bacterial colonization [56]. This was the first large study (247 patients with recurrent calcium oxalate stones and 259 controls) conducted under controlled conditions to reliably confirm the potential of O. formigenes in the prevention of urolithiasis. Interestingly, additional analyses by Kaufman and colleagues showed that the prevalence of O. formigenes colonization in the studied population depended on the rate of recurrent stone incidence [56]. Siener and colleagues [55] found that O. formigenes colonization was 67, 33, and 16% in patients with one, two to four, and more than four stone episodes, respectively [55]. Thus, gut colonization of O. formigenes might lead to a 70% reduction in the risk of recurrent stone disease [55,56], and intestinal recolonization may be effective in reducing the development and recurrence of urolithiasis.
Unfortunately, an animal study reported that O. formigenes colonization is transient. Five to 10 days after the oxalate withdrew, the fecal population of O. formigenes was undetectable by polymerase chain reaction (PCR). However, as mentioned above, the colonization efficiency may also be influenced by the selection of an appropriate strain of O. formigenes, i.e., one which is resistant to the presence of oxygen and low pH, as well as the selection of an appropriate method of administration. On the other hand, animals with chronic hyperoxaluria on an oxalate-rich diet showed decreased urinary oxalate within two days of initiating O. formigenes supplementation [54]. These results demonstrate the high effectiveness of O. formigenes in reducing urinary oxalate levels. However, the temporary colonization of the intestines with this bacteria means that in order to achieve a lasting reduction in the risk of developing urolithiasis, continuous or repeated treatment may be necessary. Moreover, epidemiological studies showed that O. formigenes prevalence in developed countries is lower than in developing countries. O. formigenes occurrence in the United States population was estimated at 31–38%, while in India, this figure was 60–77% level [57,58,59]. These differences in the levels of O. formigenes gut colonization among individuals may be due to different medical practices. Studies conducted so far have shown a high sensitivity of O. formigenes to antibiotics use [53,60]. A comparative analysis showed that O. formigenes prevalence in the Amerindians of the Yanomami-Sanema and Yekwana ethnic groups in Venezuela and the Hadza in Tanzania was higher than in adults from the USA. The analyzed tribes were characterized by a general lack of contact with modern medical practices, including antibiotic therapy [61]. A human study confirmed that Helicobacter pylori eradication using antibiotics caused loss of O. formigenes colonization for at least six months post-treatment [60,62]. Therefore, antibiotics may affect the number of bacteria in the gut, which, in turn, translates into an increased risk of developing kidney stones in people frequently receiving antibiotics. In addition to antibiotics, the level of O. formigenes colonization also depends on diet. Jiang et al. [63] found that the amount of calcium and oxalate in the diet affects the number of bacteria. Eleven O. formigenes-positive and 11 O. formigenes-negative patients were administered diets with controlled calcium and oxalate contents. In the first phase, dietary oxalate intake was varied (50 mg daily for the first week, 250 mg for the second week and 750 mg for the third week), while calcium consumption was fixed at 1000 mg daily. For the second phase, dietary calcium intake was varied (400 mg daily for the first week, 1000 mg for the second week and 2000 mg for the third week), while oxalate was fixed at 250 mg daily. Tests showed that the mean O. formigenes level increased 10-fold when dietary oxalate increased 15-fold, while there was a decrease in O. formigenes content with increasing calcium intake [63]. The sensitivity of O. formigenes to selected antibiotics and diet is a significant factor limiting the use of this bacterium in the prevention of urolithiasis. Nevertheless, the development of an effective dosing regimen of O. formigenes after antibiotic therapy and the modification of dietary habits may positively affect the effectiveness of O. formigenes in preventing the formation of deposits in the urinary tract [60,61,63].
However, studies on the differentiation of the composition of the intestinal microflora in patients with urinary stones have shown that antibiotic therapy promotes the development of urolithiasis not only due to the reduction of O. formigenes colonization, but also by modifying the composition of the entire intestinal microflora. The gut microbiome is a complex ecosystem, harboring a large number of species, including bacteria metabolizing oxalate that build complex functional networks among each other. Typically, the gut plays an important role in the metabolism of oxalate, which lowers the risk of kidney stone formation. The relationship between the gut and kidneys is called the gut–kidney axis [64]. The importance of the gut–kidney axis in the development of urolithiasis is emphasized by the fact that hyperoxaluria, observed in the course of urolithiasis, may increase intestinal permeability. Disturbances in the intestinal microflora that accompany urolithiasis can induce damage to the intestinal barrier. Increased intestinal permeability promotes the translocation of bacterial waste products that induce a response to the developing inflammation in the intestinal and urinary tract [65]. A previous analysis showed that people who form kidney stones were characterized by microbial dysbiosis, including an abnormal abundance of eubacteria, archaea, eukaryotes and even fungi. In addition to O. formigenes, research to date has also indicated the insufficiency of Ruminococcus and Oscillospira as causes of abnormal oxalate homeostasis in the gut [66]. A metagenomics analysis showed that the fecal microbiomes of stone formers exhibited reduced biodiversity and numbers. Patients with kidney stones were characterized by selective depletion of Faecalibacterium prausnitzii, Prevotella, Dialister, Dorea, and Enterobacter. Moreover, high Sutterella, Veillonella, and Peptococcus abundance were significantly correlated with urinary oxalate excretion [64]. Another study showed that changes in the microbiome which may contribute to the onset of kidney stones were associated with a depletion of Lacttobacillus and an increased amount of pathogenic Enterobacteriaceae [66].
Therefore, even effective colonization of the intestines by O. formigenes in patients with impaired intestinal microbiomes may be ineffective in the prevention of urolithiasis, and the proper functioning of the gut–kidney axis may not depend only on the presence of O. formigenes. Importantly, the discrepancies presented above regarding the effectiveness of the use of preparations containing O. formigenes in the prophylaxis of urolithiasis may result from disturbances of the entire intestinal microflora, and not just intestinal colonization by O. formigenes, although this requires further analysis [64].
Interestingly, due to the excellent ability of O. formigenes to break down oxalate, this bacterium in the form of an oral probiotic has been the subject of clinical trials. Phase I/II clinical trials demonstrated that the twice-daily treatment for eight weeks with the Oxabact® OC5 formulation containing O. formigenes did not reduce urinary oxalate excretion in patients diagnosed with primary hyperoxaluria. However, additional analysis of the ratio of urinary oxalate excretion to urinary creatinine excretion showed a significant increase after eight weeks of treatment in the treated group compared with the placebo group. Unfortunately, even though phase II/III clinical trials showed that the 24-week treatment with Oxabact™ OC3 was safe and well-tolerated in patients with primary hyperoxaluria, no effects were noted of the treatment on urinary oxalate levels or on the ratio of urinary oxalate excretion to urinary creatinine excretion [67,68,69].
A summary of previous studies using O. formigenes for the prevention of urolithiasis is presented in Table 3.

Table 3.
A summary of previous studies on the use of O. formigenes for the prevention of urolithiasis.
3. Lactobacillus spp.
3.1. Characteristics of Lactobacillus spp.
Lactobacillus species are Gram-positive, nonspore-forming rods occurring in high numbers in the human gut. The characteristics of Lactobacillus spp. are presented in Table 4. Lactobacillus spp. is generally considered to be an oxygen-tolerant anaerobic with fermentative metabolism. Lactobacillus are homofermentative or heterofermentative bacteria. Lactobacillus, as a homofermentative bacterium, metabolizes hexoses through the glycolysis pathway to lactate, while as a heterofermentative bacterium, it metabolizes hexoses through the phosphoketolase pathway to lactate, CO2, and acetate or ethanol [70]. Moreover, Lactobacillus species are called “generalist oxalotrophs” since, in contrast to O. formigenes, they can grow using a range of energy sources in addition to oxalate [71]. These bacteria are approved as generally regarded as safe (GRAS) for human consumption by the United States Food and Drug Administration (FDA). Thus, they have been used widely as probiotics to promote human health [72]. Lactobacillus spp. is a crucial component of the gut microbiome which is involved in the prevention and treatment of irritable bowel syndrome, inflammatory bowel disease (L. plantarum), acute diarrhea (L. casei), urogenital disease, dental caries, and food hypersensitivity (L. reuteri), as well as in the prevention of infections such as H. pylori and Clostridium difficile (L. casei, L. reuteri) [73,74,75,76,77].

Table 4.
Characteristics of Lactobacillus spp.
L. casei improves the body’s response to glucose and weight gain, and thus, may be used in type II diabetes therapy [78]. Interestingly, a growing body of evidence suggests that certain probiotic species, including L. casei, L. helveticus, and L. rhamnosus, can modulate mood, increase stress resilience, and alleviate anxiety [79]. Recent studies also indicate the participation of Lactobacillus spp. in the prevention of kidney stones [80].
3.2. Lactobacillus and Kidney Stone Prevention
Previous in vitro studies showed that only some of Lactobacillus and Bifidobacterium strains have oxc-like genes which provide oxalate degradability. Therefore, the various strains of these species showed highly variable oxalate degrading capacity [81,82,83]. A molecular analysis showed that frc and oxc genes encoding functional oxalate-degrading enzymes were identified in L. acidophilus NCFM and L. gasseri AM63T. Oxc and frc expressions were induced as an operon in the presence of oxalate under acid conditions [71,84]. Additionally, Murphy et al. [85] showed that among the various analyzed strains, only L. animalis 223C, L. animalis 5323, L. murinus 1222, and L. murinus 3133 showed the ability to decompose oxalate in vitro. However, an animal study confirmed that among the studied strains, only L. animalis 223C and L. animalis 5323 reduced oxalate excretion in vivo [85]. These results prove that Lactobacillus strains show the ability to degrade oxalate, and thus, their potential for clinical application. Moreover, the mismatch between in vitro and in vivo test results emphasizes that in vitro oxalate degradation does not reflect the ability of bacteria to metabolize oxalate in vivo after intestine colonization, and that proving the efficacy of a given bacterium in a clinical setting requires long-term research. A subsequent in vitro study confirmed that L. acidophilus, L. gasseri, L. salivarius AB11, L. fermentum TY12 and five strains of L. fermentum sp., Weissella confuse, and W. cibaria showed oxalate degrading ability. However, only L. acidophilus, L. gasseri, and L. salivarius AB11 were characterized by good adhesion to epithelial cells and strong antimicrobial activity. Moreover, these Lactobacillus strains also exhibited resistance to kanamycin, rifampicin, and ampicillin, but were sensitive to chloramphenicol and erythromycin. Thus, these strains may be good probiotic candidates for preventing hyperoxaluria, also in patients who have recently been treated with antibiotics [86]. Additionally, Giardina et al. [87] found that L. plantarum PBS067 and L. acidophilus LA-14 exhibited not only the ability to break down oxalate, but also may modulate the release of inflammation mediators associated with oxalate accumulation in the human gastrointestinal tract.
L. plantarum PBS067, B. breve PBS077 and B. longum PBS108 increased the production of IL-4, IL-10, IFN-γ and IL-12p70. Therapy with these probiotic bacteria not only contributed to the active degradation of oxalate, but also reduced the number of inflammatory events associated to with oxalate accumulation by stimulating cytokine production. Therefore, this therapy may be recognized as an innovative biological tool for the prevention and therapeutic treatment of kidney stones [87].
Screening different probiotic strains for their in vitro ability showed that L. paracasei LPC09 (DSM 24243) was characterized by the highest level of oxalate degrading activity (breakdown 68.5% of 10 mM ammonium oxalate). L. gasserii LGS01 (68.4%), L. gasseri LGS02 (66.2%), L. acidophilus LA07 (54.3%), and L. acidophilus LA02 (51.4%) showed a slightly lower ability to decompose ammonium oxalate in vitro. Among other studied bacterial strains, L. reuteri LRE03, L. reuteri LRE02, and L. rhamnosus LR06 degraded over 20% of the oxalate present in the medium. An indispensable advantage of these probiotic bacteria is that they have been classified as GRAS for human consumption by FDA. Therefore, it is only necessary to confirm their ability to degrade oxalate in vivo by clinical tests. This could allow the use of the tested probiotics to be extended to the prophylaxis of urolithiasis [83]. A subsequent evaluation of oxalate degradation in vitro confirmed that L. acidophilus, L. plantarum, L. brevis, Streptococcus thermophilus, and Bifidobacterum infantis may be used as potential probiotic strains. L. acidophilus was characterized by the highest percentage breakdown of 10 mM ammonium oxalate (11.8%) and L. brevis the lowest (0.9%). S. thermophilus and B. infantis degraded 2.3% and 5.3% ammonium oxalate, respectively [80]. Other bacteria which are capable of reducing intestinal oxalate absorption are L. casei HY2743 and L. casei HY7201 [88]. An animal study confirmed that rats treated with L. casei HY2743 and L. casei HY7201 showed decreased urine oxalate excretion compared to the group without Lactobacillus supplementation. Moreover, a microscope examination of rat kidneys confirmed a lower abundance of crystals in the group with L. casei HY7201 therapy than controls, confirming the effectiveness of the tested probiotics in preventing the formation of stones in the urinary tract [89].
Other in vivo studies showed that the administration of probiotic Lactiplantibacillus plantarum N-1 (LPN1) for four weeks prior to the initiation of hyperoxaluria, induced by ethylene glycol, inhibited the development of oxalate deposits in the kidney. Additionally, rats subjected to preventive intervention with LPN1 showed reduced expression of oxalic acid and renal osteopontin and CD44 in the urine, as well as improved ethylene glycol-induced enteritis and barrier function due to reduced LPS (lipopolysaccharide) and TLR4 (Toll-like receptor 4)/NF-κB (nuclear factor kappa-light-chain-enhancer of activated B cells) signaling in serum and upregulation of claudin -2 of the colon. Additionally, they showed increased production of short-chain fatty acids (SCFA) and an abundance of beneficial SCFA-producing bacteria, mainly from the Lachnospiraceae and Ruminococcaceae families. As such, it was observed that the LPN1 probiotic can prevent ethylene glycol-induced hyperoxaluria by regulating the gut microflora and improving gut barrier function [90].
Similar to O. formigenes, Lactobacillus strains have been tested extensively in clinical trials. Due to the fact that studies conducted so far have shown that multistrain probiotics seem to be more effective than single strains, clinical studies on probiotics with a prophylactic potential against urolithiasis have mainly included mixtures of various probiotic bacteria. However, it should be remembered that it is currently unclear whether the improved efficacy of the bacterial blend is due to synergistic interactions between strains or a consequence of the higher probiotic dose used in some studies [91]. Campieri et al. [80] found that a mixture of freeze-dried Lactobacillus strains (L. acidophilus, L. plantarum, and L. brevis), B. infantis, and S. thermophilus, administered as a daily dose at 8 × 1011 CFU, caused a significant reduction in the urinary excretion of oxalate, i.e., by about 40% (55.5 ± 19.6 mg/24 h reduced to 35.5 ± 15.9 mg/24 h), in six patients with idiopathic calcium oxalate urolithiasis and mild hyperoxaluria after four weeks probiotic therapy [80]. Similarly, in the case of patients with chronic fat malabsorption, calcium oxalate stones, and hyperoxaluria, therapy using an Oxadrop® probiotic preparation (VSL Pharmaceuticals, Rome, Italy) containing L. acidophilus, B. infantis, S. thermophilus, and L. brevis (mixed in a 1:1:4:4 weight and prepared as a granulate contained 2 × 1011 bacteria/1 g preparation) was associated with decreased urinary oxalate excretion. Additionally, urinary oxalate excretion was dependent on the dose of the probiotic taken; ten patients received increasing doses of Oxadrop®—4, 8, and 12 g—for one month each (the total duration of therapy was three months). Taking 4 g of Oxadrop® per day reduced urinary oxalate excretion by 19%; this increased to 24% when 8 g per day were administered [92]. Thus, it would seem that Oxadrop® can effectively reduce the risk of further attacks of renal colic. On the other hand, in a randomized, placebo-controlled trial, no effect of Oxadrop® on urinary oxalate excretion was observed in mildly hyperoxaluric stone formers after 28 or 56 days of probiotic therapy [93,94]. Additionally, Lieske et al. [93] found that Oxadrop® and Agri-King Synbiotic (Fulton, IL, USA) containing Enterococcus faecium, Saccharomyces cerevisiae subsp. Boulardi, and S. cerevisiae did not influence urinary oxalate levels in patients on a restricted oxalate diet. The obtained results suggested that diet was more effective at preventing the formation of urinary stones than the tested probiotics [93]. Similarly, in the case of a five-week therapy with the Oxadrop® preparation, a daily dose of 8 × 1011 CFU (4g/day) showed no effect on urinary and plasma oxalate levels in 20 healthy volunteers who were on an oxalate-rich diet for six weeks [95]. These discrepancies may result from the strictness of the test qualification procedure and the method of controlling the course of the tests. Ferraz et al. [96] showed that another lactic acid bacteria mixture containing L. casei and B. breve might reduce urinary oxalate excretion in seven stone-forming patients; however, the extraction level may be dependent on dietary oxalate intake, i.e., with low oxalate intake, the reduction in urinary oxalate levels may not be as significant as in patients on an oxalate-rich diet [96]. The beneficial effect of Bifidobacterium spp. and Lactobacterium spp. was also confirmed in studies on VSL#3® (Sigma-Tau pharmaceuticals, Inc., Gaithersburg, MD, USA). This probiotic supplement consists of freeze-dried live lactic acid bacterial culture, including Streptococcus thermophilus, three strains of Bifidobacterium species (B. breve, B. longum, and B. infantis), and four strains of Lactobacillus species (L. acidophilus, L. plantarum, L. paracasei, and L. delbrueckii subsp. Bulgaricus). Each sachet of VSL#3® contains 450 billion live bacteria. The daily ingestion for four weeks of one packet of VSL#3® by patients with high oxalate absorption levels led to the reduction of gastrointestinal oxalate absorption, and thus, could decrease the risk of kidney stones [97]. Furthermore, Al-Wahsh et al. [97] confirmed that eleven healthy nonstone formers on a high oxalate diet (176 mg oxalate per day) after VSL#3® therapy were characterized by reduced urinary oxalate and increased oxalate absorption. However, a comparative analysis of the effectiveness of two different doses of the preparation (one and two sachets) showed no significant difference [97]. It should be noted that studies on the beneficial effects of VSL#3® were limited to a small research group. Therefore, it is necessary to conduct a large randomized and controlled trial to confirm the results obtained so far.
A summary of previous studies on the use of Lactobacillus spp. in urolithiasis prevention is presented in Table 5.

Table 5.
A summary of previous studies on the use of Lactobacillus spp. for the prevention of urolithiasis.
4. Bifidobacterium spp.
4.1. Characteristic of Bifidobacterium
Bifidobacterium was first isolated in 1899 from the feces of breast-fed infants [98]. Bifidobacterium species are Gram-positive, nonspore-forming coryneform rods occurring in high numbers in the human gut. The characteristics of Bifidobacterium spp. are presented in Table 6. These bacteria are approved as GRAS for human consumption by the FDA. Thus, they are used widely as probiotics to promote human health [99]. Numerous studies have found that the presence of Bifidobacterium in the human large intestine provides many human health benefits. Bifidobacterium may be useful for constipation treatment in elderly individuals who suffer from long colonic transit times [100]. The addition of large numbers of lactose-digesting cultures, including Bifidobacterium spp., to dairy products, may also contribute to alleviating the symptoms of lactose intolerance [101]. Interestingly, some Bifidobacterium spp. shows the ability to magazine cholesterol in their cell membranes. Therefore, these bacteria, including B. animalis subsp. Lactis, and L. acidophilus, may contribute to the reduction of plasma cholesterol [102]. Additionally, previous studies showed that Bifidobacterium may be involved in oxalate degradation in the gastrointestinal tract. Oxalate degradation by some strains of Bifidobacterium is possible due to oxalyl-coenzyme A (CoA) decarboxylase activity encoded by oxc, which is key to the oxalate degradation process, and catalyzes the decarboxylation of oxalyl-CoA to formyl-CoA [103].

Table 6.
Characteristics of Bifidobacterium spp.
4.2. Bifidobacterium and Kidney Stone Prevention
In addition to well-known Lactobacillus probiotics, other probiotic strains of Bifidobacterium have shown the ability to degrade oxalate. A molecular analysis identified oxc and frc homologues in a few Bifidobacterium species, including B. animalis subsp. Lactis, B. dentium, B. gallicum, B. pseudocatenulatum, and B. pseudolongum, suggesting that these bacteria may have the ability to break down calcium oxalate. In vitro studies showed that among 12 studied bacterial strains, B. lactis DSM 10140, isolated from yoghurt, showed the highest oxalate-degrading activity (degrading 60.6% of available oxalate). Other bacterial strains with high oxalate degradation activity were B. adolescentis MB 238 (57% of available oxalate), B. animalis ATCC 27536 (49%), B. breve MB 283 (37.8%), B. longum MB 282 (35.2%), and B. longum ATCC 15707 (35%). The strain analysis also showed that the oxalate-degrading ability of several Bifidobacterium species was strain-specific. B. breve MB 283 degraded 37.8% of available oxalate, whereas B. breve MB 151 degraded only 1% [103]. Interestingly, in the case of B. breve PBS077 and B. longum PBS078, Giardina et al. [87] reported that these bacteria could degrade oxalate as well as modulate the immune response associated with oxalate accumulation in the gastrointestinal tract by modulating the production of pro- and anti-inflammatory cytokines. This immunomodulation was found to contribute to a reduction of inflammatory events associated with oxalate accumulation [87]. In another study, screening different Bifidobacterium strains for their in vitro ability to metabolize oxalates showed that B. breve BR03 degraded 28.2% of oxalate, B. animalis—27.7%, B. longum BL03—25.3%, and B. lactis BA05—15.5% [83]. Another Bifidobacterium species capable of degrading oxalate in vitro is B. infantis, which showed about 5% degradation of available oxalate. Moreover, unlike other probiotic bacteria tested (L. acidophilus, L. plantarum, L. brevis, and S. thermophilus), only B. infantis showed good degrading activity as well as rapid growth in an oxalate-containing medium [80]. Thus, B. infantis can more easily colonize the intestines of patients who are prone to the formation of urinary stones. Moreover, the use of a probiotic mix which has a high oxalate degradation activity but slow growth under conditions of high oxalate concentration may contribute to the rapid enhancement of oxalate degradation [80]. Therefore, when looking for bacteria among known probiotics which are capable of decomposing oxalate, it should be remembered that the selected strains must be characterized by the ability to both decompose and grow in an environment with a high concentration of oxalate, as well as by resistance to antibiotic therapy.
As with Lactobacillus, the ability of Bifidobacterium to decompose oxalate in vitro does not guarantee its degradation in vivo. Therefore, both animal and clinical trials should be conducted to verify the potential effectiveness of selected Bifidobacterium strains in reducing the risk of the development of urolithiasis. An animal study confirmed that B. animalis subsp. Lactis DSM 10140 is able to degrade oxalate. Mice with a deficiency in the hepatic alanine-glyoxylate aminotransferase (Agxt−/−, mouse model for primary hyperoxaluria) and wild-type mice after probiotic treatment, who were fed an oxalate-supplemented diet, showed increased ability to degrade dietary oxalate, thus limiting its absorption across the intestine and reducing urinary oxalate excretion. B. animalis subsp. Lactis DSM 10140 colonization was at a higher level in wild-type mice than in knockout mice. However, there were no significant changes to net oxalate secretion from the intestine in colonized animals. Therefore, these results suggest that colonization with B. animalis subsp. Lactis decreases urinary oxalate excretion by degrading dietary oxalate, thus limiting its absorption across the intestine, but that it does not promote enteric oxalate excretion, as in the case of O. formigenes. [104]. Hatch et al. [105] showed that the combined administration of the human Oxalobacter strain, HC-1, and B. animalis reduced urinary oxalate excretion in Agxt knockout mice compared with the same mice before therapy. However, mice that received the combined inoculum were characterized by 16% less urinary oxalate excretion than those that received HC-1 alone, which confirms the results indicating that the Oxalobacter strain is the best for decomposing oxalate. Additionally, the obtained results indicated that the inclusion of these strains in probiotic mixture may adversely affect their ability to break down oxalate. Therefore, paradoxically, a composition consisting of different strains, each of which individually exhibits oxalate metabolizing activity, may prove ineffective [105].
Unfortunately, only one clinical trial has been conducted to date. The obtained results showed that treatment with a mix of probiotics (L. acidophilus, L. plantarum, L. brevis, S. thermophilus, and B. infantis) caused a significant reduction in the excretion of oxalate in all six patients with idiopathic calcium oxalate urolithiasis and mild hyperoxaluria. Therefore, the proposed mixture of probiotics may prove effective for the prevention of urolithiasis. However, in order to unequivocally evaluate the effectiveness of the tested mixture, it is necessary to conduct these studies on a much larger population. [80].
A summary of previous studies using Bifdobacterum spp. for the prevention of urolithiasis is presented in Table 7.

Table 7.
A summary of previous studies on the use of Bifdobacterum spp. for the prevention of urolithiasis.
5. Other Bacteria Associated with Oxalate Metabolism
Eubacterium is the second most common bacterial genus found in the gastrointestinal tract in humans, after Bacteroides. E. genus is anaerobic and produces nonspore-forming, Gram-positive rods. Ito and colleagues [106] isolated E. lentum WHY-1 from the feces of a Japanese male and found that it could be used to reduce the oxalate content of tea in vitro [106]. Moreover, further in vitro studies showed that E. lentum WYH-1 decomposed 100% of 1 mg/mL oxalate in an artificial intestinal juice [107]. Intestinal juice contains bile salts which have an antibacterial effect. Bile salt compounds destroy bacterial membranes, denature proteins, chelate iron and calcium, cause oxidative DNA damage, and control the expression of eukaryotic genes involved in host defense and immunity. Consequently, the ability of E. lentum to multiply and degrade oxalate in the presence of bile salts indicates the clinical applicability of these bacteria [106,107]. Unfortunately, no studies to date have confirmed the ability of E. lentum to degrade oxalate in vivo.
Enterococcus faecalis is a Gram-positive facultative anaerobe, occurring as single cocci or in chains of various lengths. E. faecalis is an intestinal commensal; however, it is also a significant opportunistic pathogen, causing urinary tract and wound infections [108]. Moreover, E. faecalis is called “generalist oxalotroph”, since it only utilizes oxalate as a carbon source in the absence of alternative energy supplies [109]. Hokama et al. [109] found that E. faecalis, isolated from human stool under anaerobic conditions, showed oxalate-degrading ability in vitro. Moreover, a protein analysis confirmed that oxalate-degrading E. faecalis produced three proteins with molecular weights of 65, 48, and 40 kDa that were not produced by nonoxalate-degrading E. faecalis. Two of these proteins were homologues of oxalyl-coenzyme A-decarboxylase (65 kDa) and formyl-coenzyme A-transferase (48 kDa), which are found in O. formigenes [109]. Interestingly, these proteins were not expressed under conditions where the oxalate-degrading strains of E. faecalis had access to other energy sources. Therefore, the active expression of the detected proteins is a mechanism induced by unfavorable environmental conditions which enable the survival of bacteria that only have access to oxalate as an energy source [109]. Due to the fact that E. faecalis is an opportunistic pathogen that can use oxalate as an alternative energy source, the clinical application of this bacterium as a probiotic for reducing the risk of developing stones in the urinary tract is severely limited.
Similar to E. faecalis, homologues of the genes characteristic of O. fomingenes have been identified in Escherichia coli. YfdW from E. coli is a formyl-CoA transferase [110] and YfdU is an oxalyl-CoA decarboxylase [111,112]. The presence of these genes suggests the ability of E. coli to degrade oxalate. Unfortunately, studies conducted to date have not confirmed that E. coli bacteria are capable of decomposing oxalate. On the other hand, certain freshly isolated fecal E. coli strains initially showed improved growth on an oxalate-supplemented medium, but this phenotype was soon lost upon further subculturing, which significantly limits the clinical application of these bacteria in patients with kidney stones [113].
6. B. subtilis and L. plantarum as Novel Recombinant Approaches
The ability to prevent the formation of urinary stones is also demonstrated by B. subtills. Al and colleagues [114], using the Drosophila melanogaster model of urolithiasis as a high-throughput screening platform to evaluate the therapeutic potential of oxalate-degrading bacteria in calcium oxalate nephrolithiasis, found that Bacillus subtilis 168 (BS168) is promising candidate for the prevention of oxalate-induced microbiota dysbiosis. The studied BS168 was characterized by preferential growth in high oxalate concentrations and an ability to rapidly and stably colonize the D. melanogaster intestinal tract for as long as five days. These results were confirmed by in vitro study, which demonstrated that established MDCK renal cells treated with BS168 showed reduced adhesion and aggregation of calcium oxalate crystals. Thus, BS168 could represent a novel therapeutic adjunct to reduce the incidence of recurrent calcium oxalate nephrolithiasis in high-risk patients [114].
Another possible solution to excessive oxalate deposition is the use of pure enzyme products derived from bacteria. Such solutions allow the use of human pathogenic bacteria for the production of desired enzymes. The first reports on the application of enzymes only, rather than whole bacteria, supported the use of B. subtilis oxalate decarboxylase (OxDC) enzyme. This enzyme was expressed in E. coli and then purified [115,116]. Next, the enzyme crystals were crosslinked with glutaraldehyde and administered at a daily dose of 200 mg for 16 days to mice suffering from hyperoxaluria (mouse model with Agxt gene mutation). The used preparation reduced the fecal and urinary oxalate concentrations of the mice by 72% and 44% respectively, compared with a placebo group [116]. Interestingly, the administration of ethylene glycol, which induced nephrocalcinosis and kidney failure, and 80 mg/day OxDC- CLEC (cross-linked formulation of oxalate-decarboxylase) caused a 40% reduction of urinary oxalate and prevented the development of ethylene glycol-induced kidney pathology [116]. Cowley et al. [117] proposed to modify the B. subtilis enzyme by replacing the cysteine residue at position 383 with serine. This modification was intended to prevent protein aggregation while maintaining the proper functionality of the enzyme [117]. Importantly, OxDC exhibits optimal activity at acidic pH (3.5–5.0), and requires the presence of catalytic amounts of molecular oxygen. Due to its low pH activity, OxDC can degrade oxalate in the stomach, thus reducing the level excreted in the urine; as such, it can effectively reduce the risk of developing urolithiasis [117]. Moreover, toxicity analyses confirmed the safety of the modified formulation, and preliminary clinical studies confirmed the potential of the modified enzyme to reduce urinary oxalate [118]. Another solution to the problem of oxalate degradation is the use of recombinant probiotic bacteria. For this purpose, the probiotic bacteria that have the best ability to colonize the intestines should be selected, and the gene encoding the oxalate-degrading enzyme should be introduced into their genetic material [119]. A previous study suggested that L. plantarum NC8 could be used as a bacterium into which the vector with the OxDC gene will be introduced. L. plantarum NC8 is a probiotic bacterium recognized by the FDA as GRAS that does not normally express oxalate decarboxylase [120]. However, the creation of good recombinants is difficult. Previous studies confirmed that in the case of recombinants, it is important to select the appropriate promoter that determines the expression of the desired gene. Studies on the appropriate OxDC introducing vector have shown that the recombinants obtained may or may not secrete the enzyme on the cell outside. The first data indicated OxDC gene cloning into a shuttle vector in which expression was regulated by a sakacin-P-inducible promoter (pSIP high-level expression system), and that the production of an active recombinant OxDC protein is intracellular [121]. On the other hand, Sasikumar and colleagues [122] proposed the introduction into the p-SIP vector of both OxDC and homologous peptide sequences (Lp_0373 or Lp_3050), which allowed extracellular secretion of the functional enzyme by the obtained recombinant. The recombinants gained in this approach were able to degrade 50% of the oxalate present in the medium [122,123,124]. In the next study, the pSIP409 vector was used, in which the inducible promoter (P orfX) was replaced with a constitutive promoter (P ldhL), and the gene gusA was replaced with oxdC. As a consequence, recombinant L. plantarum which was capable of secreting dehydrogenase and degrading 90% of the oxalate contained in the medium, compared to 15% by the wild type, was obtained [125]. Moreover, animal studies confirmed that rats treated with recombinant strains of L. plantarum, i.e., WCFS1OxdC (strain secretes the functional OxdC outside cells) and NC8OxdC (strain nonsecretes the functional OxdC outside cells), were characterized by reduced urinary oxalate excretion and crystal deposition of calcium oxalate due to increased intestinal oxalate degradation [122,126].
7. Conclusions
The increase in the incidence of nephrolithiasis and the high rate of relapse have emphasized the need to develop effective methods to prevent the onset of this condition. Currently, patients with oxalate stone formation are only advised to follow an appropriate diet. Therefore, in recent years, there has been increasing interest in probiotic bacteria which are capable of degrading oxalate. A comparison of the most studied probiotics in terms of the prevention of urolithiasis is presented in the Table 8. Most research to date has focused primarily on O. fomingenes, which is an absolute oxalotroph with high sensitivity to antibiotics and the conditions of probiotic formulation processes, such as low pH and oxygen conditions. Therefore, the potential to use O. formingens for the prevention of urolithiasis is limited. Nonetheless, the undoubted advantage is that of all studied bacteria, O. formigenes has the highest oxalate-degrading capacity. Interestingly, later studies indicated the existence of O. formigenes strains characterized by resistance to low pH and the presence of oxygen, which confirmed the potential for the clinical use of O. formigenes. Therefore, it is necessary to conduct extensive research to select strains which are characterized by low levels of sensitivity to the aforementioned conditions. Unfortunately, as stated above, the use of O. formigenes is not effective in patients undergoing recent or current antibiotic therapy. A possible solution to the problem of antibiotic sensitivity could be the use of a mixture of probiotics, which would partially eliminate the problem of intestinal colonization. Reports have suggested that the use of a mixture of various probiotics may also be a good solution owing to the participation of the complete intestinal microflora in the degradation of oxalate and the reduction of its excretion in urine. Moreover, the use of a mixture of probiotic bacteria containing Lactobacillus or Bifidobacterium strains increases the degree of similarity of effective intestinal colonization. In patients with urolithiasis, the high concentration of oxalate in the intestine significantly restricts the growth and multiplication of most known probiotic bacteria, as only a few strains can obtain energy from oxalate. Therefore, the use of a mixture of bacteria with different growth potentials under conditions of high oxalate concentrations will result in the growth of bacteria which are capable of metabolizing oxalate in the initial stage, and when its concentration decreases due to the activity of those bacteria, the remaining probiotic bacteria will start to develop. Therefore, supplementation with a mixture of microorganisms can effectively restore the microbiological balance and provide effective prevention against urolithiasis. Unfortunately, to our knowledge, no research has interpreted disturbances of the intestinal microflora as a whole. Moreover, it should be emphasized that most human studies have numerous limitations. The vast majority of such studies are based on small research groups, i.e., a dozen or so people, who are often on an uncontrolled diet. Studies on Lactobacillus spp. and Bifidobacterium spp. are largely limited to in vitro and animal studies, which already indicate differences in the ability of these bacteria to metabolize oxalate in vitro and in vivo. Therefore, there is a need to conduct further studies under strictly controlled conditions involving a larger population.

Table 8.
Characteristics of O. formigenes, Lactobacillus and Bifidobacterium in the prevention of urolithiasis.
Author Contributions
Conceptualization, P.W.; investigation, P.W.; writing-original draft preparation, P.W.; visualization, P.W.; writing-review and editing, M.B. and J.S.-B.; supervision, P.W. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no competing financial and/or nonfinancial interests.
References
- Mayans, L. Nephrolithiasis. Prim. Care 2019, 46, 203–212. [Google Scholar] [CrossRef]
- Romero, V.; Akpinar, H.; Assimos, D.G. Kidney stones: A global picture of prevalence, incidence, and associated risk factors. Rev. Urol. 2010, 12, e86–e96. [Google Scholar]
- Ramello, A.; Vitale, C.; Marangella, M. Epidemiology of nephrolithiasis. J. Nephrol. 2000, 13, 45–50. [Google Scholar]
- Pinduli, I.; Spivacow, R.; del Valle, E.; Vidal, S.; Negri, A.L.; Previgliano, H.; Farias Edos, R.; Andrade, J.H.; Negri, G.M.; Boffi-Boggero, H.J. Prevalence of urolithiasis in the autonomous city of Buenos Aires, Argentina. Urol. Res. 2006, 34, 8–11. [Google Scholar] [CrossRef] [PubMed]
- Medina-Escobedo, M.; Zaidi, M.; Real-de Leon, E.; Orozco-Rivadeneyra, S. Urolithiasis prevalence and risk factors in Yucatan, Mexico. Salud Publica Mex. 2002, 44, 541–545. [Google Scholar] [CrossRef] [Green Version]
- Lieske, J.C.; Peña de la Vega, L.S.; Slezak, J.M.; Bergstralh, E.J.; Leibson, C.L.; Ho, K.L.; Gettman, M.T. Renal stone epidemiology in Rochester, Minnesota: An update. Kidney Int. 2006, 69, 760–764. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scales, C.D., Jr.; Curtis, L.H.; Norris, R.D.; Springhart, W.P.; Sur, R.L.; Schulman, K.A.; Preminger, G.M. Changing gender prevalence of stone disease. J. Urol. 2007, 177, 979–982. [Google Scholar] [CrossRef]
- Uribarri, J.; Oh, M.S.; Carroll, H.J. The first kidney stone. Ann. Intern. Med. 1989, 111, 1006–1009. [Google Scholar] [CrossRef] [PubMed]
- Moe, O.W. Kidney stones: Pathophysiology and medical management. Lancet 2006, 367, 333–344. [Google Scholar] [CrossRef]
- Miano, R.; Germani, S.; Vespasiani, G. Stones and urinary tract infections. Urol. Int. 2007, 79, 32–36. [Google Scholar] [CrossRef]
- Chow, W.H.; Lindblad, P.; Gridley, G.; Nyren, O.; McLaughlin, J.K.; Linet, M.S.; Pennello, G.A.; Adami, H.O.; Fraumeni, J.J. Risk of urinary tract cancers following kidney or ureter stones. J. Natl. Cancer Inst. 1997, 89, 1453–1457. [Google Scholar] [CrossRef] [PubMed]
- Pearle, M.S.; Calhoun, E.A.; Curhan, G.C. Urologic Diseases of America Project. Urologic diseases in America project: Urolithiasis. J. Urol. 2005, 173, 848–857. [Google Scholar] [CrossRef]
- Antonelli, J.A.; Maalouf, N.M.; Pearle, M.S.; Lotan, Y. Use of the National Health and Nutrition Examination Survey to calculate the impact of obesity and diabetes on cost and prevalence of urolithiasis in 2030. Eur. Urol. 2014, 66, 724–729. [Google Scholar] [CrossRef] [Green Version]
- Chung, M.J. Urolithiasis and nephrolithiasis. JAAPA 2017, 30, 49–50. [Google Scholar] [CrossRef]
- Chaudhary, A.; Singla, S.K.; Tandon, C. In vitro Evaluation of Terminalia arjuna on Calcium Phosphate and Calcium Oxalate Crystallization. Indian J. Pharm. Sci. 2010, 72, 340–345. [Google Scholar]
- Alelign, T.; Petros, B. Kidney Stone Disease: An Update on Current Concepts. Adv. Urol. 2018, 2018, 3068365. [Google Scholar] [CrossRef]
- Scales, C.D., Jr.; Smith, A.C.; Hanley, J.M.; Saigal, C.S. Urologic Diseases in America Project. Prevalence of kidney stones in the United States. Eur. Urol. 2012, 62, 160–165. [Google Scholar] [CrossRef] [Green Version]
- Curhan, G.C.; Willett, W.C.; Rimm, E.B.; Stampfer, M.J. Family history and risk of kidney stones. J. Am. Soc. Nephrol. 1997, 8, 1568–1573. [Google Scholar] [CrossRef]
- Stamatelou, K.K.; Francis, M.E.; Jones, C.A.; Nyberg, L.M.; Curhan, G.C. Time trends in reported prevalence of kidney stones in the United States: 1976–1994. Kidney Int. 2003, 63, 1817–1823. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Soucie, J.M.; Thun, M.J.; Coates, R.J.; McClellan, W.; Austin, H. Demographic and geographic variability of kidney stones in the United States. Kidney Int. 1994, 46, 893–899. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferraro, P.M.; Bargagli, M.; Trinchieri, A.; Gambaro, G. Risk of Kidney Stones: Influence of Dietary Factors, Dietary Patterns, and Vegetarian-Vegan Diets. Nutrients 2020, 12, 779. [Google Scholar] [CrossRef] [Green Version]
- Tasian, G.E.; Jemielita, T.; Goldfarb, D.S.; Copelovitch, L.; Gerber, J.S.; Wu, Q.; Denburg, M.R. Oral antibiotic exposure and kidney stone disease. J. Am. Soc. Nephrol. 2018, 29, 1731–1740. [Google Scholar] [CrossRef]
- Tasian, G.; Miller, A.; Lange, D. Antibiotics and Kidney Stones: Perturbation of the Gut-Kidney Axis. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 2019, 74, 724–726. [Google Scholar] [CrossRef] [Green Version]
- Ferraro, P.M.; Curhan, G.C.; Gambaro, G.; Taylort, E.N. Antibiotic Use and Risk of Incident Kidney Stones in Female Nurses. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 2019, 74, 736–741. [Google Scholar] [CrossRef] [PubMed]
- Stern, J.M.; Burk, R.D.; Asplin, J.; Krieger, N.S.; Suadicani, S.O.; Wang, Y.; Usyk, M.; Lee, J.A.; Chen, L.; Becker, J.; et al. Kidney stone formation and the gut microbiome are altered by antibiotics in genetic hypercalciuric stone-forming rats. Urolithiasis 2021, 49, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Miller, A.W.; Orr, T.; Dearing, D.; Monga, M. Loss of function dysbiosis associated with antibiotics and high fat, high sugar diet. ISME J. 2019, 13, 1379–1390. [Google Scholar] [CrossRef] [PubMed]
- Stern, J.M.; Moazami, S.; Qiu, Y.; Kurland, I.; Chen, Z.; Agalliu, I.; Burk, R.; Davies, K.P. Evidence for a distinct gut microbiome in kidney stone formers compared to non-stone formers. Urolithiasis 2016, 44, 399–407. [Google Scholar] [CrossRef]
- Basavaraj, D.R.; Biyani, C.S.; Browning, A.J.; Cartledge, J.J. The role of urinary kidney stone inhibitors and promoters in the pathogenesis of calcium containing renal stones. EAU-EBU Update Ser. 2007, 5, 126–136. [Google Scholar] [CrossRef]
- Taylor, E.N.; Curhan, G.C. Oxalate intake and the risk for nephrolithiasis. J. Am. Soc. Nephrol. 2007, 18, 2198–2204. [Google Scholar] [CrossRef] [Green Version]
- Zabłocka, A.; Janusz, M. The two faces of reactive oxygen species. Postepy Hig. Med. Dosw. 2008, 62, 118–124. [Google Scholar]
- Holmes, R.P.; Goodman, H.O.; Assimos, D.G. Contribution of dietary oxalate to urinary oxalate excretion. Kidney Int. 2001, 59, 270. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ticinesi, A.; Milani, C.; Guerra, A.; Allegri, F.; Lauretani, F.; Nouvenne, A.; Mancabelli, L.; Lugli, G.A.; Turroni, F.; Duranti, S.; et al. Understanding the gut-kidney axis in nephrolithiasis: An analysis of the gut microbiota composition and functionality of stone formers. Gut 2018, 67, 2097–2106. [Google Scholar] [CrossRef]
- Lieske, J.C. Probiotics for prevention of urinary stones. Ann. Transl. Med. 2017, 5, 29. [Google Scholar] [CrossRef]
- Aggarwal, K.P.; Narula, S.; Kakkar, M.; Tandon, C. Nephrolithiasis: Molecular mechanism of renal stone formation and the critical role played by modulators. BioMed Res. Int. 2013, 2013, 21. [Google Scholar] [CrossRef] [Green Version]
- Ratkalkar, V.N.; Kleinman, J.G. Mechanisms of stone formation. Clin. Rev. Bone Mineral. Metab. 2011, 9, 187–197. [Google Scholar] [CrossRef] [Green Version]
- Courbebaisse, M.; Prot-Bertoye, C.; Bertocchio, J.; Baron, S.; Maruani, G.; Briand, S.; Daudon, M.; Houillier, P. Nephrolithiasis of adult: From mechanisms to preventive medical treatment. Rev. Med Int. 2017, 38, 4452. [Google Scholar]
- Moryama, M.T.; Domiki, C.; Miyazawa, K.; Tanaka, T.; Suzuki, K. Effects of oxalate exposure on Madin-Darby canine kidney cells in culture: Renal prothrombin fragment-1 mRNA expression. Urol. Res. 2005, 33, 470–475. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.R.; Glenton, P.A.; Backov, R.; Talham, D.R. Presence of lipids in urine, crystals and stones: Implications for the formation of kidney stones. Kidney Int. 2002, 62, 2062–2072. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bhadja, P.; Lunagariya, J.; Ouyang, J.M. Seaweed sulphated polysaccharide as an inhibitor of calcium oxalate renal stone formation. J. Funct. Foods 2016, 27, 685–694. [Google Scholar] [CrossRef]
- Allison, M.J.; Dawson, K.A.; Mayberry, W.R.; Foss, J.G. Oxalobacter formigenes gen. nov., sp. Nov.: Oxalate-degrading anaerobes that inhabit the gastrointestinal tract. Arch. Microbiol. 1985, 141, 1–7. [Google Scholar] [CrossRef]
- Mehta, M.; Goldfarb, D.S.; Nazzal, L. The role of the microbiome in kidney stone formation. Int. J. Surg. 2016, 36, 607–612. [Google Scholar] [CrossRef]
- Dawson, K.A.; Allison, M.J.; Hartman, P.A. Isolation and some characteristics of anaerobic oxalate-degrading bacteria from the rumen. Appl. Environ. Microbiol. 1980, 40, 833–839. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Allison, M.J.; Cook, H.M.; Milne, D.B.; Gallagher, S.; Clayman, R.V. Oxalate degradation by gastrointestinal bacteria from humans. J. Nutr. 1986, 116, 455–460. [Google Scholar] [CrossRef] [PubMed]
- Sidhu, H.; Hoppe, B.; Hesse, A.; Tenbrock, K.; Brömme, S.; Rietschel, E.; Peck, A.B. Absence of Oxalobacter formigenes in cystic fibrosis patients: A risk factor for hyperoxaluria. Lancet 1998, 352, 1026–1029. [Google Scholar] [CrossRef]
- Sidhu, H.; Enatska, L.; Ogden, S.; Williams, W.N.; Allison, M.J.; Peck, A.B. Evaluating Children in the Ukraine for Colonization with the Intestinal Bacterium Oxalobacter formigenes, Using a Polymerase Chain Reaction-based Detection System. Mol. Diagn. 1997, 2, 89–97. [Google Scholar] [CrossRef]
- Anantharam, V.; Allison, M.J.; Maloney, P.C. Oxalate: Formate exchange. The basis for energy coupling in Oxalobacter. J. Biol. Chem. 1989, 264, 7244. [Google Scholar] [CrossRef]
- Troxel, S.A.; Sidhu, H.; Kaul, P.; Low, R.K. Intestinal Oxalobacter formigenes colonization in calcium oxalate stone formers and its relation to urinary oxalate. J. Endourol. 2003, 17, 173–176. [Google Scholar] [CrossRef]
- Hatch, M.; Cornelius, J.; Allison, M.; Sidhu, H.; Peck, A.; Freel, R.W. Oxalobacter sp. Reduces urinary oxalate excretion by promoting enteric oxalate secretion. Kidney Int. 2006, 69, 691–698. [Google Scholar] [CrossRef] [Green Version]
- Ellis, M.E.; Mobley, J.A.; Holmes, R.P.; Knight, J. Proteome Dynamics of the Specialist Oxalate Degrader Oxalobacter formigenes. J. Proteom. Bioinform. 2016, 9, 19–24. [Google Scholar]
- Ellis, M.L.; Dowell, A.E.; Li, X.; Knight, J. Probiotic properties of Oxalobacter formigenes: An in vitro examination. Arch. Microbiol. 2016, 198, 1019–1026. [Google Scholar] [CrossRef] [Green Version]
- Duncan, S.H.; Richardson, A.J.; Kaul, P.; Holmes, R.P.; Allison, M.J.; Stewart, C.S. Oxalobacter formigenes and its potential role in human health. Appl. Environ. Microbiol. 2002, 68, 3841–3847. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoppe, B.; Beck, B.; Gatter, N.; von Unruh, G.; Tischer, A.; Hesse, A.; Laube, N.; Kaul, P.; Sidhu, H. Oxalobacter formigenes: A potential tool for the treatment of primary hyperoxaluria type 1. Kidney Int. 2006, 70, 1305–1311. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sidhu, H.; Schmidt, M.E.; Cornelius, J.G.; Thamilselvan, S.; Khan, S.R.; Hesse, A.; Peck, A.B. Direct correlation between hyperoxaluria/oxalate stone disease and the absence of the gastrointestinal tract-dwelling bacterium Oxalobacter formigenes: Possible prevention by gut recolonization or enzyme replacement therapy. J. Am. Soc. Nephrol. 1999, 10, 334–340. [Google Scholar]
- Sidhu, H.; Allison, M.J.; Chow, J.M.; Clark, A.; Peck, A.B. Rapid reversal of hyperoxaluria in a rat model after probiotic administration of Oxalobacter formigenes. J. Urol. 2001, 166, 1487–1491. [Google Scholar] [CrossRef]
- Siener, R.; Bangen, U.; Sidhu, H.; Hönow, R.; von Unruh, G.; Hesse, A. The role of Oxalobacter formigenes colonization in calcium oxalate stone disease. Kidney Int. 2013, 83, 1144–1149. [Google Scholar] [CrossRef] [Green Version]
- Kaufman, D.W. Oxalobacter formigenes may reduce the risk of calcium oxalate kidney stones. J. Am. Soc. Nephrol. 2008, 19, 1197–1203. [Google Scholar] [CrossRef] [Green Version]
- Kwak, C.; Jeong, B.C.; Lee, J.H.; Kim, H.K.; Kim, E.C.; Kim, H.H. Molecular identification of Oxalobacter formigenes with the polymerase chain reaction in fresh or frozen fecal samples. BJU Int. 2001, 88, 627–632. [Google Scholar] [CrossRef] [PubMed]
- Kodama, T.; Mikami, K.; Akakura, K.; Takei, K.; Naya, Y.; Ueda, T.; Ito, H. Detection of Oxalobacter formigenes in human feces and study of related genes in a new oxalate-degrading bacterium. Hinyokika Kiyo 2003, 49, 371–376. [Google Scholar]
- Kumar, R.; Mukherjee, M.; Bhandari, M.; Kumar, A.; Sidhu, H.; Mittal, R.D. Role of Oxalobacter formigenes in calcium oxalate stone disease: A study from North India. Eur. Urol. 2002, 41, 318–322. [Google Scholar] [CrossRef]
- Kharlamb, V.; Schelker, J.; Francois, F.; Jiang, J.; Holmes, R.P.; Goldfarb, D.S. Oral antibiotic treatment of Helicobacter pylori leads to persistently reduced intestinal colonization rates with Oxalobacter formigenes. J. Endourol. 2011, 25, 1781–1785. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- PeBenito, A.; Nazzal, L.; Wang, C.; Li, H.; Jay, M.; Noya-Alarcon, O.; Contreras, M.; Lander, O.; Leach, J.; Dominguez-Bello, M.G.; et al. Comparative prevalence of Oxalobacter formigenes in three human populations. Sci. Rep. 2019, 9, 574. [Google Scholar] [CrossRef] [Green Version]
- Nazzal, L.; Francois, F.; Henderson, N.; Liu, M.; Li, H.; Koh, H.; Wang, C.; Gao, Z.; Perez, G.P.; Asplin, J.R.; et al. Effect of antibiotic treatment on Oxalobacter formigenes colonization of the gut microbiome and urinary oxalate excretion. Sci. Rep. 2021, 11, 16428. [Google Scholar] [CrossRef] [PubMed]
- Jiang, J.; Knight, J.; Easter, L.H.; Neiberg, R.; Holmes, R.P.; Assimos, D.G. Impact of dietary calcium and oxalate, and Oxalobacter formigenes colonization on urinary oxalate excretion. J. Urol. 2011, 186, 135–139. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ticinesi, A.; Nouvenne, A.; Meschi, T. Gut microbiome and kidney stone disease: Not just an Oxalobacter story. Kidney Int. 2019, 96, 25–27. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.Y.; Chen, D.Q.; Chen, L.; Liu, J.R.; Vaziri, N.D.; Guo, Y.; Zhao, Y.Y. Microbiome-metabolome reveals the contribution of gut-kidney axis on kidney disease. J. Transl. Med. 2019, 17, 5. [Google Scholar] [CrossRef] [Green Version]
- Pedro, R.N.; Aslam, A.U.; Bello, J.O.; Bhatti, K.H.; Philipraj, J.; Sissoko, I.; Vasconcellos, G.S.; Trinchieri, A.; Buchholz, N. Nutrients, vitamins, probiotics and herbal products: An update of their role in urolithogenesis. Urolithiasis 2020, 48, 285–301. [Google Scholar] [CrossRef]
- Daniel, S.L.; Moradi, L.; Paiste, H.; Wood, K.D.; Assimos, D.G.; Holmes, R.P.; Nazzal, L.; Hatch, M.; Knight, J. Forty Years of Oxalobacter formigenes, a Gutsy Oxalate-Degrading Specialist. Appl. Environ. Microbiol. 2021, 87, 0054421. [Google Scholar] [CrossRef] [PubMed]
- Milliner, D.; Hoppe, B.; Groothoff, J. A randomised Phase II/III study to evaluate the efficacy and safety of orally administered Oxalobacter formigenes to treat primary hyperoxaluria. Urolithiasis 2018, 46, 313–323. [Google Scholar] [CrossRef]
- Hoppe, B.; Niaudet, P.; Salomon, R.; Harambat, J.; Hulton, S.A.; Van’t Hoff, W.; Moochhala, S.H.; Deschênes, G.; Lindner, E.; Sjögren, A.; et al. A randomised Phase I/II trial to evaluate the efficacy and safety of orally administered Oxalobacter formigenes to treat primary hyperoxaluria. Pediatr. Nephrol. 2017, 32, 781–790. [Google Scholar] [CrossRef]
- Gänzle, M.G. Lactic metabolism revisited: Metabolism of lactic acid bacteria in food fermentations and food spoilage. Curr. Opin. Food Sci. Food Microbiol. Funct. Foods Nutr. 2015, 2, 106–117. [Google Scholar] [CrossRef]
- Lewanika, T.R.; Reid, S.J.; Abratt, V.R.; Macfarlane, G.T.; Macfarlane, S. Lactobacillus gasseri Gasser AM63T degrades oxalate in a multistage continuous culture simulator of the human colonic microbiota. FEMS Microbiol. Ecol. 2007, 61, 110–120. [Google Scholar] [CrossRef] [Green Version]
- Martín, R.; Langella, P. Emerging Health Concepts in the Probiotics Field: Streamlining the Definitions. Front. Microbiol. 2019, 10, 1047. [Google Scholar] [CrossRef] [Green Version]
- Le, B.; Yang, S.H. Efficacy of Lactobacillus plantarum in Prevention of Inflammatory Bowel disease. Toxicol. Rep. 2018, 5, 314–317. [Google Scholar] [CrossRef]
- Mu, Q.; Tavella, V.J.; Luo, X.M. Role of Lactobacillus reuteri in Human Health and Diseases. Front. Microbiol. 2018, 9, 757. [Google Scholar] [CrossRef] [PubMed]
- Bai, A.P.; Ouyang, Q. Probiotics and Inflammatory Bowel Disease. Postgrad. Med. J. 2006, 82, 376–382. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heeney, D.D.; Gareau, M.G.; Marco, M.L. Intestinal Lactobacillus in health and disease, a driver or just along for the ride? Curr. Opin. Biotechnol. 2018, 49, 140–147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kinross, J.M.; von Roon, A.C.; Holmes, E.; Darzi, A.; Nicholson, J.K. The human gut microbiome: Implications for future health care. Curr. Gastroenterol. Rep. 2008, 10, 396–403. [Google Scholar] [CrossRef]
- Dang, F.; Jiang, Y.; Pan, R.; Zhou, Y.; Wu, S.; Wang, R.; Zhuang, K.; Zhang, W.; Li, T.; Man, C. Administration of Lactobacillus paracasei ameliorates type 2 diabetes in mice. Food Funct. 2018, 9, 3630–3639. [Google Scholar] [CrossRef] [PubMed]
- Oriach, C.S.; Robertson, R.C.; Stanton, C.; Cryan, J.F.; Dinanad, T.G. Food for Thought: The Role of Nutrition in the Microbiota-Gut-Brain Axis. Clin. Nutr. Exp. 2016, 6, 25–38. [Google Scholar] [CrossRef] [Green Version]
- Campieri, C.; Campieri, M.; Bertuzzi, V.; Swennen, E.; Matteuzzi, D.; Stefoni, S.; Pirovano, F.; Centi, C.; Ulisse, S.; Famularo, G.; et al. Reduction of oxaluria after an oral course of lactic acid bacteria at high concentration. Kidney Int. 2001, 60, 1097–1105. [Google Scholar] [CrossRef] [Green Version]
- Turroni, S.; Vitali, B.; Bendazzoli, C.; Candela, M.; Gotti, R.; Federici, F.; Pirovano, F.; Brigidi, P. Oxalate consumption by lactobacilli: Evaluation of oxalyl-CoA decarboxylase and formyl-CoA transferase activity in Lactobacillus acidophilus. J. Appl. Microbiol. 2007, 103, 1600–1609. [Google Scholar] [CrossRef]
- Turroni, S.; Bendazzoli, C.; Dipalo, S.C.; Candela, M.; Vitali, B.; Gotti, R.; Brigidi, P. Oxalate-degrading activity in Bifidobacterium animalis subsp. lactis: Impact of acidic conditions on the transcriptional levels of the oxalyl coenzyme A (CoA) decarboxylase and formyl-CoA transferase genes. Appl. Environ. Microbiol. 2010, 76, 5609–5620. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mogna, L.; Pane, M.; Nicola, S.; Raiteri, E. Screening of different probiotic strains for their in vitro ability to metabolise oxalates: Any prospective use in humans? J. Clin. Gastroenterol. 2014, 48, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Azcarate-Peril, M.A.; Bruno-Barcena, J.M.; Hassan, H.M.; Klaenhammer, T.R. Transcriptional and functional analysis of oxalyl-coenzyme A (CoA) decarboxylase and formyl-CoA transferase genes from Lactobacillus acidophilus. Appl. Environ. Microbiol. 2006, 72, 1891–1899. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murphy, C.; Murphy, S.; O’Brien, F.; O’Donoghue, M.; Boileau, T.; Sunvold, G.; Reinhart, G.; Kiely, B.; Shanahan, F.; O’Mahony, L. Metabolic activity of probiotics-oxalate degradation. Vet. Microbiol. 2009, 136, 100–107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gomathi, S.; Sasikumar, P.; Anbazhagan, K.; Sasikumar, S.; Kavitha, M.; Selvi, M.S.; Selvam, G.S. Screening of indigenous oxalate degrading lactic acid bacteria from human faeces and South Indian fermented foods: Assessment of probiotic potential. Sci. World J. 2014, 2014, 648059. [Google Scholar] [CrossRef] [Green Version]
- Giardina, S.; Scilironi, C.; Michelotti, A.; Samuele, A.; Borella, F.; Daglia, M.; Marzatico, F. In vitro anti-inflammatory activity of selected oxalate-degrading probiotic bacteria: Potential applications in the prevention and treatment of hyperoxaluria. J. Food Sci. 2014, 79, M384–M390. [Google Scholar] [CrossRef]
- Okombo, J.; Liebman, M. Probiotic-induced reduction of gastrointestinal oxalate absorption in healthy subjects. Urol. Res. 2010, 38, 169–178. [Google Scholar] [CrossRef]
- Kwak, C.; Jeong, B.C.; Ku, J.H.; Kim, H.H.; Lee, J.J.; Huh, C.S.; Baek, Y.J.; Lee, S.E. Prevention of nephrolithiasis by Lactobacillus in stone-forming rats: A preliminary study. Urol. Res. 2006, 34, 265–270. [Google Scholar] [CrossRef]
- Wei, Z.; Cui, Y.; Tian, L.; Liu, Y.; Yu, Y.; Jin, X.; Li, H.; Wang, K.; Sun, Q. Probiotic Lactiplantibacillus plantarum N-1 could prevent ethylene glycol-induced kidney stones by regulating gut microbiota and enhancing intestinal barrier function. FASEB J. 2021, 35, e21937. [Google Scholar] [CrossRef]
- Chapman, C.M.; Gibson, G.R.; Rowland, I. Health benefits of probiotics: Are mixtures more effective than single strains? Eur. J. Nutr. 2011, 50, 1–17. [Google Scholar] [CrossRef]
- Lieske, J.C.; Goldfarb, D.S.; De Simone, C.; Regnier, C. Use of a probiotic to decrease enteric hyperoxaluria. Kidney Int. 2005, 68, 1244–1249. [Google Scholar] [CrossRef] [Green Version]
- Lieske, J.C.; Tremaine, W.J.; De Simone, C.; O’Connor, H.M.; Li, X.; Bergstralh, E.J.; Goldfarb, D.S. Diet, but not oral probiotics, effectively reduces urinary oxalate excretion and calcium oxalate supersaturation. Kidney Int. 2010, 78, 1178–1185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goldfarb, D.S.; Modersitzki, F.; Asplin, J.R. A randomized, controlled trial of lactic acid bacteria for idiopathic hyperoxaluria. Clin. J. Am. Soc. Nephrol. 2007, 2, 745–749. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Siener, R.; Bade, D.J.; Hesse, A.; Hoppe, B. Dietary hyperoxaluria is not reduced by treatment with lactic acid bacteria. J. Transl. Med. 2013, 11, 306. [Google Scholar] [CrossRef] [Green Version]
- Ferraz, R.R.; Marques, N.C.; Froeder, L.; Menon, V.B.; Siliano, P.R.; Baxmann, A.C.; Heilberg, I.P. Effects of Lactobacillus casei and Bifidobacterium breve on urinary oxalate excretion in nephrolithiasis patients. Urol. Res. 2009, 37, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Al-Wahsh, I.; Wu, Y.; Liebman, M. Acute probiotic ingestion reduces gastrointestinal oxalate absorption in healthy subjects. Urol. Res. 2012, 40, 191–196. [Google Scholar] [CrossRef]
- Tisser, M.H. La reaction chromophile d’Escherichia et le Bacterium coli. C. R. Soc. Biol. 1899, 51, 943. [Google Scholar]
- Picard, C.; Fioramonti, J.; Francois, A.; Robinson, T.; Neant, F.; Matuchansky, C. Review article: Bifidobacteria as probiotic agents—physiological effects and clinical benefits. Aliment. Pharmacol. Ther. 2005, 22, 495–512. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, D.J. Screening of intestinal microflora for effective probiotic bacteria. J. Agric. Food Chem. 2001, 49, 1751–1760. [Google Scholar] [CrossRef]
- Jiang, T.A.; Mustapha, A.; Savaiano, D.A. Improvement of lactose digestion in humans by ingestion of unfermented milk containing Bifidobacterium longum. J. Dairy Sci. 1996, 79, 750–757. [Google Scholar] [CrossRef]
- Ataie-Jafari, A.; Larijani, B.; Alavi Majd, H.; Tahbaz, F. Cholesterol-lowering effect of probiotic yogurt in comparison with ordinary yogurt in mildly to moderately hypercholesterolemic subjects. Ann. Nutr. Metab. 2009, 54, 22–27. [Google Scholar] [CrossRef]
- Federici, F.; Vitali, B.; Gotti, R.; Pasca, M.R.; Gobbi, S.; Peck, A.B.; Brigidi, P. Characterization and heterologous expression of the oxalyl coenzyme A decarboxylase gene from Bifidobacterium lactis. Appl. Environ. Microbiol. 2004, 70, 5066–5073. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klimesova, K.; Whittamore, J.M.; Hatch, M. Bifidobacterium animalis subsp. lactis decreases urinary oxalate excretion in a mouse model of primary hyperoxaluria. Urolithiasis 2015, 43, 107–117. [Google Scholar] [CrossRef] [Green Version]
- Hatch, M.; Freel, R.W. A human strain of Oxalobacter (HC-1) promotes enteric oxalate secretion in the small intestine of mice and reduces urinary oxalate excretion. Urolithiasis 2013, 41, 379–384. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ito, H.; Miura, N.; Masai, M.; Yamamoto, K.; Hara, T. Reduction of oxalate content of foods by the oxalate degrading bacterium, Eubacterium lentum WYH-1. Int. J. Urol. 1996, 3, 31–34. [Google Scholar] [CrossRef] [PubMed]
- Ito, H.; Kotake, T.; Masai, M. In vitro degradation of oxalic acid by human faeces. Int. J. Urol. 1996, 3, 207–211. [Google Scholar] [CrossRef]
- Fiore, E.; Van Tyne, D.; Gilmore, M.S. Pathogenicity of Enterococci. Microbiol. Spectr. 2019, 7, 10. [Google Scholar] [CrossRef]
- Hokama, S.; Honma, Y.; Toma, C.; Ogawa, Y. Oxalate-degrading Enterococcus faecalis. Microbiol. Immunol. 2000, 44, 235–240. [Google Scholar] [CrossRef]
- Toyota, C.G.; Berthold, C.L.; Gruez, A.; Jonsson, S.; Lindqvist, Y.; Cambillau, C.; Richards, N.G. Differential substrate specificity and kinetic behavior of Escherichia coli YfdW and Oxalobacter formigenes formyl coenzyme A transferase. J. Bacteriol. 2008, 190, 2556–2564. [Google Scholar] [CrossRef] [Green Version]
- Toyota, C.G. Oxalate Metabolizing Enzymes of Oxalobacter Formigenes and Escherichia coli. Ph.D. Thesis, University of Florida, Gainesville, FL, USA, 2008. [Google Scholar]
- Werther, T.; Zimmer, A.; Wille, G.; Golbik, R.; Weiss, M.S.; Konig, S. New insights into structure-function relationships of oxalyl CoA decarboxylase from Escherichia coli. FEBS J. 2010, 277, 2628–2640. [Google Scholar] [CrossRef] [PubMed]
- Abratt, V.R.; Reid, S.J. Oxalate-degrading bacteria of the human gut as probiotics in the management of kidney stone disease. Adv. Appl. Microbiol. 2010, 72, 63–87. [Google Scholar] [PubMed]
- Al, K.F.; Daisley, B.A.; Chanyi, R.M.; Bjazevic, J.; Razvi, H.; Reid, G.; Burton, J.P. Oxalate-Degrading Bacillus subtilis Mitigates Urolithiasis in a Drosophila melanogaster Model. mSphere 2020, 5, e00498-20. [Google Scholar] [CrossRef] [PubMed]
- Just, V.J.; Stevenson, C.E.M.; Bowater, L.; Tanner, A.; Lawson, D.M.; Bornemann, S. A closed conformation of Bacillus subtilis oxalate decarboxylase OxdC provides evidence for the true identity of the active site. J. Biol. Chem. 2004, 279, 19867–19874. [Google Scholar] [CrossRef] [Green Version]
- Grujic, D.; Salido, E.C.; Shenoy, B.C.; Langman, C.B.; McGrath, M.E.; Patel, R.J.; Rashid, A.; Mandapati, S.; Jung, C.W.; Margolin, A.L. Hyperoxaluria is reduced and nephrocalcinosis prevented with an oxalate-degrading enzyme in mice with hyperoxaluria. Am. J. Nephrol. 2009, 29, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Cowley, A.B.; Poage, D.W.; Dean, R.R.; Meschter, C.L.; Ghoddusi, M.; Li, Q.-S.; Sidhu, H. 14-day repeat-dose oral toxicity evaluation of oxazyme in rats and dogs. Int. J. Toxicol. 2010, 29, 20–31. [Google Scholar] [CrossRef] [PubMed]
- Mufarrij, P.W.; Lange, J.N.; Knight, J.; Assimos, D.G.; Holmes, R.P. The effects of Oxazyme on oxalate degradation: Results and implications of in vitro experiments. J. Endourol. 2013, 27, 284–287. [Google Scholar] [CrossRef]
- Yadav, A.K.; Tyagi, A.; Kumar, A.; Saklani, A.C.; Grover, S.; Batish, V.K. Adhesion of indigenous Lactobacillus plantarum to gut extracellular matrix and its physicochemical characterization. Arch. Microbiol. 2014, 197, 155–164. [Google Scholar] [CrossRef]
- Kolandaswamy, A.; George, L.; Sadasivam, S. Heterologous expression of oxalate decarboxylase in Lactobacillus plantarum NC8. Curr. Microbiol. 2009, 58, 117–121. [Google Scholar] [CrossRef]
- Sørvig, E.; Grönqvist, S.; Naterstad, K.; Mathiesen, G.; Eijsink, V.G.H.; Axelsson, L. Construction of vectors for inducible gene expression in Lactobacillus sakei and L. plantarum. FEMS Microbiol. Lett. 2003, 229, 119–126. [Google Scholar] [CrossRef] [Green Version]
- Sasikumar, P.; Gomathi, S.; Anbazhagan, K.; Abhishek, A.; Paul, E.; Vasudevan, V.; Sasikumar, S.; Selvam, G.S. Recombinant Lactobacillus plantarum expressing and secreting heterologous oxalate decarboxylase prevents renal calcium oxalate stone deposition in experimental rats. J. Biomed. Sci. 2014, 21, 86. [Google Scholar] [CrossRef] [Green Version]
- Mathiesen, G.; Sveen, A.; Brurberg, M.B.; Fredriksen, L.; Axelsson, L.; Eijsink, V.G. Genome-wide analysis of signal peptide functionality in Lactobacillus plantarum WCFS1. BMC Genom. 2009, 10, 425. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mathiesen, G.; Sveen, A.; Piard, J.-C.; Axelsson, L.; Eijsink, V.G.H. Heterologous protein secretion by Lactobacillus plantarum using homologous signal peptides. J. Appl. Microbiol. 2008, 105, 215–226. [Google Scholar] [CrossRef] [PubMed]
- Anbazhagan, K.; Sasikumar, P.; Gomathi, S.; Priya, H.P.; Selvam, G.S. In vitro degradation of oxalate by recombinant Lactobacillus plantarum expressing heterologous oxalate decarboxylase. J. Appl. Microbiol. 2013, 115, 880–887. [Google Scholar] [CrossRef]
- Sasikumar, P.; Gomathi, S.; Anbazhagan, K.; Baby, A.E.; Sangeetha, J.; Selvam, G.S. Genetically engineered Lactobacillus plantarum WCFS1 constitutively secreting heterologous oxalate decarboxylase and degrading oxalate under in vitro. Curr. Microbiol. 2014, 69, 708–715. [Google Scholar] [CrossRef]
- Charteris, W.P.; Kelly, P.M.; Morelli, L.; Collins, J.K. Antibiotic susceptibility of potentially probiotic Lactobacillus species. J. Food Prot. 1998, 61, 1636–1643. [Google Scholar] [CrossRef]
- Moubareck, C.; Gavini, F.; Vaugien, L.; Butel, M.J.; Doucet-Populaire, F. Antimicrobial susceptibility of bifidobacteria. J. Antimicrob. Chemother. 2005, 55, 38–44. [Google Scholar] [CrossRef] [Green Version]
- Maresca, D.; Zotta, T.; Mauriello, G. Adaptation to Aerobic Environment of Lactobacillus johnsonii/gasseri Strains. Front. Microbiol. 2018, 9, 157. [Google Scholar] [CrossRef]
- Fuochi, V.; Petronio, G.P.; Lissandrello, E.; Furneri, P.M. Evaluation of resistance to low pH and bile salts of human Lactobacillus spp. isolates. Int. J. Immunopathol. Pharmacol. 2015, 28, 426–433. [Google Scholar] [CrossRef] [Green Version]
- Sánchez, B.; Champomier-Vergès, M.C.; Collado, M.; Anglade, P.; Baraige, F.; Sanz, Y.; de los Reyes-Gavilán, C.G.; Margolles, A.; Zagorec, M. Low-pH adaptation and the acid tolerance response of Bifidobacterium longum biotype longum. Appl. Environ. Microbiol. 2007, 73, 6450–6459. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shimamura, S.; Abe, F.; Ishibashi, N.; Miyakawa, H.; Yaeshima, T.; Araya, T.; Tomita, M. Relationship between oxygen sensitivity and oxygen metabolism of Bifidobacterium species. J. Dairy Sci. 1992, 75, 3296–3306. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).