Simple Summary
In 2022, roughly 54 million people worldwide were alive within 5 years of receiving a cancer diagnosis and, with improved technology and treatments, this group is growing fast. However, cancer survivors often experience higher health burden and poorer quality of life (QoL) compared to the general population. Little is known about what contributes to these poor health outcomes, especially what role the social factors might play. This study aims to assess the impact of social factors—including role functioning, social functioning and social support—on the QoL of cancer survivors. This secondary analysis of a cross-sectional study called “The Compass” by the Icelandic Cancer Society included 1200 cancer survivors. The analyses were stratified by gender and cancer type (breast, prostate and colorectal). Taking gender and cancer type-based predictors into consideration in survivorship care could improve patients’ health-related quality of life.
Abstract
Background/Objectives: With improved technology and cancer treatments, the number of cancer survivors is growing. However, many cancer survivors experience long-term effects of cancer and its treatment, leading to a high health burden and poorer quality of life (QoL). A growing body of literature has explored the relationship between sociodemographic variables and QoL among cancer patients, although findings remain mixed. This study aims to assess the impact of social factors—role functioning, social functioning and social support—on the QoL of Icelandic cancer survivors diagnosed between 2015 and 2019, stratified by gender and cancer type (breast, prostate and colorectal cancer). Method: This study is a secondary analysis study, using data from a cross-sectional study conducted by the Icelandic Cancer Society in 2020–2021. In total, 1200 cancer survivors participated. Results: Multiple regression showed that less depressive symptoms, higher role and social functioning, better instrumental social support, higher educational attainment and income, less financial difficulties and lower age were significantly associated with higher QoL among participants. Conclusions: cancer survivors’ global health status/QoL is highly influenced by role functioning and depression symptoms, while other predictive factors, including social functioning, social support, education and income, vary by gender and cancer type.
1. Introduction
As of 2022, roughly 54 million people worldwide were alive within 5 years of receiving a cancer diagnosis [1]. Additionally, 20 million people received a new diagnosis and 9.7 million people died [2]. The most commonly diagnosed cancer types are breast, lung, colorectal and prostate [3]. In Iceland, between 2020 and 2024, an average of 2055 people were diagnosed with cancer annually, with incidence rates of 615 per 100,000 for men and 552 per 100,000 for women. The mortality rates were 218.7 per 100,000 for men and 182.6 per 100,000 for women, while the five-year overall survival rate reached 70% [4].
With the aging population and advances in cancer detection, technology and treatments, the number of cancer survivors is growing [5,6]. However, cancer survivors often experience an array of challenges that affect their overall health and well-being, including physical [7,8], emotional [8,9,10,11,12] and social dimensions [12,13,14,15,16,17]. As the number of survivors continues to increase, attention is shifting to long-term quality of life (QoL).
Quality of life is a multidimensional concept that encompasses all aspects of a person’s well-being. A closely related concept, health-related quality of life (HRQoL), is a more specific subset that specifically refers to individuals’ perceptions of their physical, emotional, mental and functional well-being, and how these affect their daily life, including work, relationships, and leisure [18]. Two core components of HRQoL are role and social functioning. Social functioning refers to an individual’s ability to interact with their social environment and fulfill their social roles [19]. Role functioning refers to how well an individual performs in the various roles they occupy in their life, such as those related to family, workplace, and community. Limited research has specifically addressed the role of these two factors in cancer survivorship, but studies show that impairments in these areas can significantly affect overall well-being and life satisfaction [20]. While increasing survival rates is the primary goal of treatment, an equally important objective is maintaining quality of life during and after cancer treatment and preventing its deterioration.
A growing body of literature has explored the relationship between sociodemographic variables and QoL among cancer patients, although the findings remain mixed. Some studies have found a significant relationship between QoL and age [21,22,23,24,25,26], gender [22,25,26,27,28,29,30,31,32,33], education [21,25,34,35,36], economic condition [21,25], marital status [21], employment [26,28] and family size [37], while others have found no such association [25,38,39,40,41]. Despite this, gender differences seem to play a critical role in shaping the QoL and social experiences of cancer survivors. Studies examining QoL predictors reveal both gender-specific predictors and common predictors. The QoL of female cancer survivors is predicted by pain intensity [42,43], body image concerns [43], financial strain, employment status and optimism [44], while male survivors’ QoL is more strongly predicted by limited health literacy [45] and sexual health issues [43]. Common predictors of QoL include cognitive impairment [45], energy level, social support and depression [42,44,45]. Depression has consistently been shown to negatively affect QoL in cancer patients. High rates of depression have been reported in this population [8,9], and depression has been associated with poorer treatment outcomes and increased cancer-specific and all-cause mortality [10,11,46,47].
Men and women tend to adopt different coping mechanisms, often reflecting existing gender norms [48]. While men tend to favor problem-solving or avoidance [49,50,51], women favor emotional coping strategies, such as sharing experiences and seeking social support [48,50,51,52,53,54]. These gendered patterns may affect how individuals respond to illness, express their experiences and seek help [55]. From a public health perspective, understanding these gendered patterns is essential for developing tailored interventions.
Social factors play a crucial role and have been termed one of the most important factors in determining the QoL in chronic illness [12,44]. A cancer diagnosis can disrupt social functioning, reduce social participation, and alter relationships. Survivors often experience decreased energy and motivation for social activities, a diminished social network, and changes in social roles [56]. However, strong social ties and support networks have been shown to enhance QoL, improve health outcomes, reduce mortality risk [14,15,16,17], increase life satisfaction and lower levels of depression [15,57]. Survivors with higher QoL tend to experience greater social and role functioning [29,37,58,59,60,61,62,63,64,65] and lower levels of social isolation [15,66] compared to those with lower QoL.
Social support is a key factor when adapting to a cancer diagnosis [35]. Research on social support and health show that experiencing high levels of social support is associated with a 25% decrease in relative risk for cancer mortality [17] and higher QoL [15,27,29,35]. Social support has four subtypes, all of which are predictive of overall QoL, including emotional and instrumental social support [67]. Emotional social support addresses a person’s emotional and psychological needs, expressing care, concern, empathy and understanding, while instrumental social support involves providing practical assistance to someone to manage their immediate needs. This includes offering a ride to a doctor’s appointment and helping with chores [68]. These two types of social support are associated with higher social and emotional well-being [15].
Study Aim
Given the increasing numbers of cancer survivors, it is essential to identify the social factors that contribute to better quality of life. This study aims to explore the association between social factors and QoL among cancer survivors in Iceland, with a specific focus on gender and the three most common cancer types in the sample (breast cancer, prostate cancer and colorectal cancer). The analyses will be stratified by gender and cancer type to explore the association between social factors and QoL in more detail and to identify potential areas for intervention to improve QoL in this growing population.
2. Materials and Methods
2.1. Participants
This is a secondary analysis of existing data, utilizing data from the “Compass” (“Áttavitinn”), a cross-sectional study conducted by the Icelandic Cancer Society. In June, all individuals (18–80+ years old) who had been diagnosed with cancer between 2015 and 2019 were invited to participate in this study via a mailed invitation letter. Information on cancer participants was gathered from the Cancer Registry of Iceland, and participation consisted of answering a questionnaire, either electronically or in print, with informed consent obtained. The data was collected between 8 June 2020 and 1 May 2021. A total of 4575 individuals received an invitation to participate in this study, and a total of 1840 individuals answered the questionnaire, yielding a 40% response rate [69].
For the present study, only individuals who had completed their cancer treatment were included, n = 1200 (Figure 1). To conduct an analysis based on cancer type, the three most common cancer types were selected, including breast cancer (BC, n = 391), prostate cancer (PC, n = 167) and colorectal cancer (CC, n = 147).
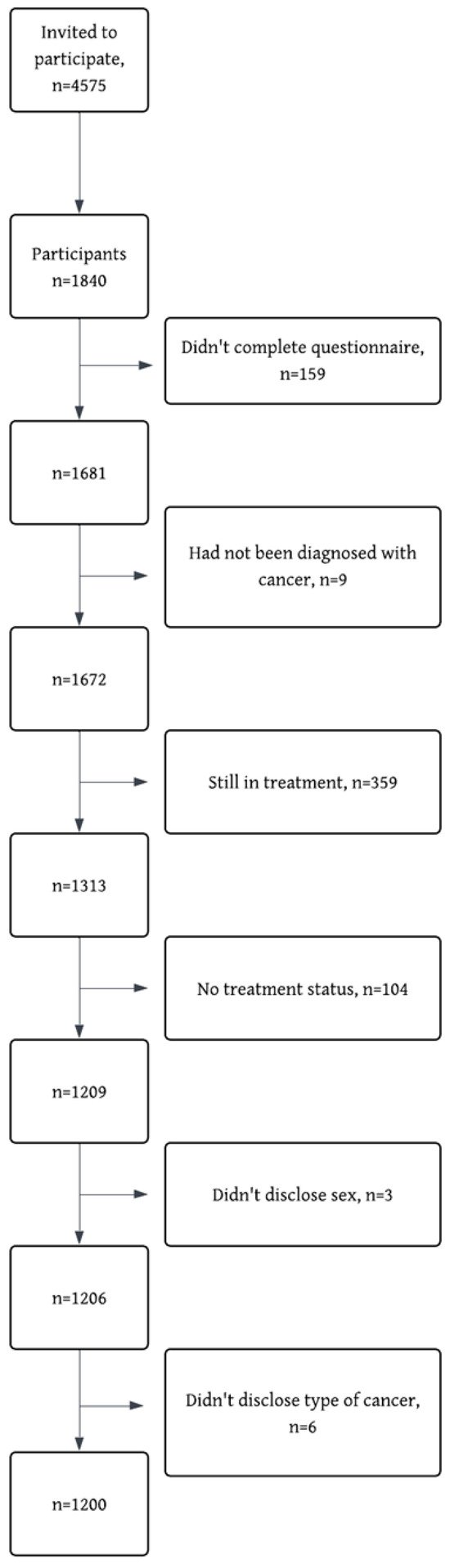
Figure 1.
STROBE flow diagram of reasons for exclusion and missing data.
2.2. Instruments
2.2.1. Demographic Characteristics
Information about participants‘ age and gender was gathered from Registry Iceland, while level of education, marital status, number of children, occupational status, income and number of treatments were obtained via the questionnaire.
2.2.2. EORTC-QLQ-C30
The EORTC-QLQ-C30 is a widely used 30-item questionnaire that assesses the health-related QoL of cancer patients [70] and includes items measuring QoL (termed “global health status/QoL” in the questionnaire), role functioning, social functioning and financial difficulties. The questionnaire has adequate reliability, with a Cronbach’s alpha of 0.56 to 0.90 in previous studies [71,72,73] and 0.91 in the current study. The alpha for individual scales was adequate, with 0.90 for the global health status/QoL scale, 0.91 for role functioning and 0.89 for social functioning.
The 30 items are divided into five functional scales, nine symptom scales and one global health status/QoL scale. In addition, a QLQ summary score can be calculated based on all items. However, it is not advised to use this score for further analysis, but rather use the global health status/QoL scale as the outcome variable [74], as is applied in this study. Each scale is measured by between one and five items, with the responses rated on a 4-point Likert scale, ranging from 1 = Not at All to 4 = Very Much. The only exception to this is the global health status/QoL scale, which is rated on a 7-point Likert scale ranging from 1 = Very poor to 7 = Excellent. Scores were converted to a 0–100 scale according to the EORTC scoring manual, where higher scores indicate better quality of life or functioning. Missing values were imputed using the mean of the completed items within a scale, provided that at least half of the items in that scale had been answered, in line with EORTC recommendations [74]. Previous research has established thresholds for clinical importance (TCIs) that vary across the questionnaire’s subscales. For example, scores below 58 on role or social functioning indicate clinically important impairment, while scores above 17 on financial difficulties reflect a clinically important problem [75]. When evaluating change over time, a 10-point difference has often been used as a threshold for meaningful change. However, this cut-off has been debated, and consensus on the interpretation of QLQ-C30 scores is still lacking [76,77].
2.2.3. PHQ-9
Patient Health Questionnaire (PHQ-9) measures symptoms of depression and contains 9 items intended to screen for and measure depression severity [78]. The response scale is coded as 0 = Not at all, 1 = Several days, 2 = More than half the days, 3 = Nearly every day. A total score is calculated by summing responses. A score of 1–4 indicates minimal depression; 5–9 mild depression; 10–14 moderate depression; 15–19 moderately severe depression; and 20–27 severe depression [78]. In this study, the total score was used in the analysis to represent symptoms of depression. The questionnaire has adequate reliability, with a Cronbach’s alpha of 0.86 to 0.89 in previous studies [78,79] and 0.90 in the current study.
2.2.4. The Compass
The Compass is a 110-item survey tool based on a Danish survey called “the Barometer survey” [80] and has been adapted to Icelandic society. The survey comprises questions assessing demographic factors and experiences with the diagnostic process and cancer treatment. In this study, information on the level of education, marital status, number of children, occupational status, personal income and number of treatments obtained via the questionnaire was used. Additionally, variables measuring emotional and instrumental social support were used (Table 1).

Table 1.
Variable description.
2.3. Statistical Analysis
Statistical analyses were performed in R studio, version 2025.05.0. Descriptive statistics for the sample characteristics, outcome variable and covariates were calculated (Table 2), followed by a correlation analysis (Table 3). To score the variables from the EORTC-QLQ-C30 scale, global health status/QoL and role and social functioning, a package called PROscorer was used. The package is specifically designed to score patient-reported outcomes such as the QLQ-C30 questionnaire. In the case of missing data, mean imputation was used and performed by the PROscorer package, as directed by the EORTC manual.

Table 2.
Descriptive statistics for participants who finished cancer therapy.

Table 3.
Correlation matrix for the variables in the regression model.
To explore the association between social variables and the global health status/QoL of cancer survivors following cancer therapy, a multiple linear regression was conducted using the enter method. Social factors (role and social functioning, instrumental and emotional social support) and depression were entered into the model simultaneously to assess their individual contributions to the outcome, while controlling for the effects of the other variables (demographic) in the model. Standardized beta coefficients were reported to indicate the strength and direction of the associations between the predictors and the outcome. The analysis was stratified by gender for the whole sample to explore gender differences and by cancer type to explore cancer-specific relationships.
This study had adequate power to conduct the proposed analyses across the three major cancer groups. However, after more in-depth analyses, the PC and CC groups had decreased due to missing data in the social support variable (PC, n = 28 and CC, n = 28). Therefore, ad hoc power analysis was performed in Gpower,(version 3.1.9.6) which confirmed that this study still had adequate power. To improve power and to increase the sample size for those two groups, we removed the variable with the highest number of missing data (instrumental social support) from the analysis for these two groups but included it in the analysis for the breast cancer group.
3. Results
3.1. Socio-Demographic Characteristics
Roughly 60% of the sample were female, the average age was 62.0 years (SD = 11.8, range 23–85), and the mean age at diagnosis was 58.9 years old (SD = 11.9, range 18–80). Most of the sample lived in the greater Reykjavík area (64.1%) and were married or cohabiting (79.2%). More than a third of the sample had a university degree (38.9%) and this trend was consistent across all three cancer types. Compared to the other cancer types, the individuals in the breast cancer group were, on average younger, diagnosed earlier, more likely to have children under the age of 18 at home, had undergone more treatment types and experienced greater financial difficulties (Table 2).
The average score on the global health status/QoL scale was 72.3 among all cancer types, 70.4 among women and 75.1 for men, all of which are higher than published reference values (61.3) [81]. There was a significant difference between global health status/QoL scores among the three cancer types, with 70.6 points among breast cancer survivors, 77.0 among prostate cancer survivors and 73.4 among colorectal cancer survivors. On average, the prostate cancer survivors had the highest average score on global health status/QoL, role functioning, social functioning and emotional social support, compared to the other two cancer types (Table 2).
Regarding depression symptoms, a total of 14.7% of breast cancer survivors experienced moderate-to-severe depression symptoms, compared to 6.9% among the colorectal cancer survivors and 3.7% of the prostate cancer survivors. The majority of the participants had minimal symptoms of depression (65%).
3.2. Inferential Statistics
To analyze the association of social variables with global health status/QoL, a correlation matrix using Pearson correlation was generated for all variables of interest (Table 3). Most correlations were small (|r| < 0.30), although a higher correlation was observed between some variables: SF and RF (r = 0.65, p < 0.001), QL and SF (r = 0.59, p < 0.001), QL and RF (r = 0.63, p < 0.001) and ISS and ESS (r = 0.70, p < 0.001) (Figure 2). Despite several correlations reaching statistical significance, the effect sizes indicated weak associations overall. The correlations among the predictors were well below levels of concern for multicollinearity (r < 0.80), and therefore all variables were retained for subsequent analyses.
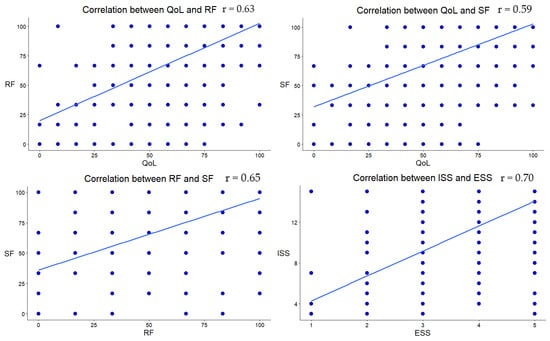
Figure 2.
Scatterplot of the highest significant correlation coefficients. The blue dots represent individual scores on each variable.
3.2.1. All Survivors
The results of multiple regression models for global health status/QoL showed that age, education, financial difficulties, role and social functioning, instrumental social support and depression were all significant predictors of global health status/QoL among all cancer survivors (Table 4 and Figure 3). The analysis shows that older age (β = −0.11, p = 0.01), experiencing more financial difficulties (β = −0.08, p = 0.02) and more depression symptoms (β = −0.42, p ≤ 0.001) were negatively associated with global health status/QoL, while better role functioning (β = 0.26, p ≤ 0.001), higher education levels (secondary school = β = 0.23, p = 0.02; trade school education = β = 0.26, p = 0.01; university degree = β = 0.24, p = 0.01), better social functioning (β = 0.14, p ≤ 0.001) and better instrumental social support (β = 0.12, p = 0.01) were all positively associated with global health status/QoL.

Table 4.
Regression coefficients for predicting global health status/QoL among cancer survivors.
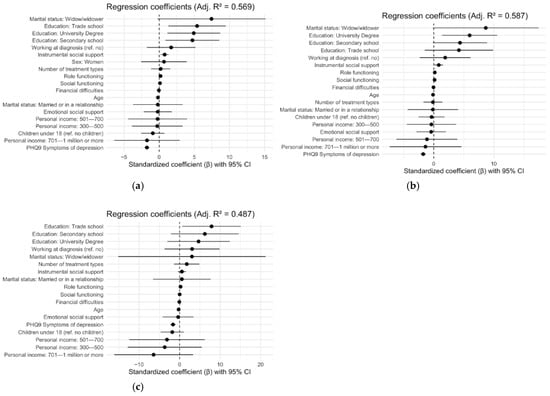
Figure 3.
Forest plots illustrate the results from the regression analysis from Table 4. The following panels show (a) regression analysis, group: all survivors; (b) regression analysis, group: women; (c) regression analysis, group: men.
3.2.2. Gender Differences
Among women, global health status/QoL was most negatively affected by experiencing depressive symptoms (β = −0.41, p ≤ 0.001), while having university education (β = 0.28, p = 0.01), better role functioning (β = 0.23, p ≤ 0.001), better social functioning (β = 0.18, p ≤ 0.001) and receiving more instrumental social support (β = 0.12, p = 0.03) were positively associated with global health status/QoL.
Among men, having trade school education (β = 0.41, p = 0.02) and better role functioning (β = 0.35, p ≤ 0.001) were positively associated with global health status/QoL, while experiencing depressive symptoms was negatively associated, β = −0.39, p ≤ 0.001.
3.2.3. Cancer Type
Role functioning and depression were significant predictors of global health status/QoL across all cancer types of interest. However, the demographic predictors associated with global health status/QoL varied by cancer type (Table 5 and Figure 4). The multiple regression analysis indicated that a better global health status/QoL among breast cancer survivors was positively associated with higher educational levels (secondary school, β = 0.50, p = 0.001; trade school education, β = 0.46, p = 0.012; university degree, β = 0.41, p = 0.008) and better role functioning, (β = 0.27, p ≤ 0.001), while experiencing more depressive symptoms was negatively associated with global health status/QoL, β = −0.41, p ≤ 0.00. For prostate cancer survivors, better role functioning was positively associated with global health status/QoL (β = 0.47, p ≤ 0.001), while experiencing more symptoms of depression was negatively associated with global health status/QoL scores (β = −0.37, p ≤ 0.001). Among colorectal cancer survivors, having a medium income was positively associated with global health status/QoL (β = 0.63, p = 0.045), along with better role functioning (β = 0.47, p ≤ 0.001), while experiencing more symptoms of depression was negatively associated with scores (β = −0.23, p = 0.046) (Table 5 and Figure 4).

Table 5.
Regression coefficients for predicting global health status/QoL among cancer survivors—by cancer type.
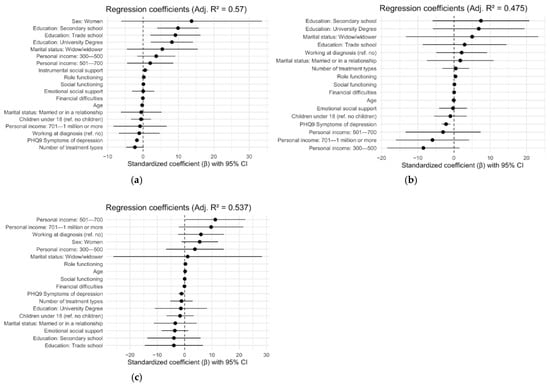
Figure 4.
The forest plots illustrate the results from the regression analysis from Table 5. The following panels show (a) regression analysis, group: breast cancer survivors; (b) regression analysis, group: prostate cancer survivors; (c) regression analysis, group: colorectal cancer survivors.
4. Discussion
The average global health burden/QoL score of the sample was 72.3 points on a scale from 0 to 100, which is above existing reference values. The scores differed significantly between cancer types and gender and were predicted by different demographic and social factors. Across the entire sample, the strongest predictor of global health status/QoL was the presence of depressive symptoms, followed by educational attainment, role functioning, social functioning, instrumental social support, age and financial difficulties. These results are consistent with previous research, highlighting the detrimental impact and high prevalence of depression on QoL [10,11,46,47], the positive associations between enhanced role and social functioning and higher QoL [29,37,58,59,60,61,62,63,64,65] and between greater social support and improved QoL [15,27,29,35].
Regarding socioeconomic variables—specifically education, income and financial difficulties—our findings indicate that individuals with better socioeconomic conditions generally report higher levels of QoL. In particular, higher educational attainment and fewer financial difficulties were associated with better QoL outcomes across the sample. These results are consistent with previous studies [82,83].
4.1. Gender Differences
An important contribution of the present study is the identification of gender differences in social predictors of global health status/QoL. The global health status/QoL of both men and women is highly associated with both depression, role functioning and education. Among men, role functioning was the only significant social predictor, whereas for women, role functioning, social functioning and instrumental social support were all significant predictors. These findings suggest that women’s global health status/QoL may depend more on the quality and availability of social networks and support systems compared to men. This is consistent with previous research on gender differences in coping styles, which emphasizes women’s greater reliance on social support and interpersonal sharing [5,48,50,51,52,53,54]. Such differences may help explain the broader influence of social variables observed among female survivors.
4.2. Cancer Specific Predictors
Global health status/QoL among all cancer types was highly associated with depression and role functioning. However, this study identified cancer-specific differences in demographic predictors. Global health status/QoL was linked to educational level in breast cancer survivors but not in prostate or colorectal cancer survivors. Among the colorectal survivors, having a medium personal income was associated with higher global health status/QoL compared with the lowest personal income group. This association was not observed in other cancer groups. This indicates that the influence of demographic factors on global health status/QoL is not universal but may instead reflect challenges specific to certain cancer diagnoses, populations and treatments. Considering these diagnosis-specific factors in survivorship could help improve outcomes.
4.3. Importance of Social Variables
The consistent predictive value of role functioning across cancer types underscores the critical role that returning to everyday activities plays in enhancing QoL after surviving cancer. Role functioning represents an essential dimension of quality of life, as it connects individuals to purpose, identity and social contribution. In addition to fulfilling basic tasks, role functioning reflects a sense of purpose in life, such as being a parent to one’s children, being a useful worker or member of society, and the broader experience of having a valued role in society. These components are not only integral to individual identity and self-worth but also to social relationships, highlighting the importance of role functioning as a key factor in both clinical and public health contexts. Disruptions in role functioning can therefore have wide-ranging implications for both individual adjustment and collective life [84]. Interventions to restore role functioning include targeted peer groups, patient organizations that facilitate reintegration into daily life, and structured exercise programs [85]. However, the success of these efforts often depends on addressing underlying psychological challenges.
This emphasizes the need for comprehensive strategies that combine targeted rehabilitation, support groups and mental health interventions to help survivors re-engage with daily roles despite potential limitations. In particular, the strong influence of depressive symptoms on global health status/QoL across cancer groups underscores the importance of systematic mental health screening and support. Early identification and treatment of depressive symptoms may improve overall outcomes for cancer survivors.
4.4. Strengths and Limitations
This study’s strengths include a relatively large sample, which enabled testing of a comprehensive model incorporating both psychosocial and demographic variables, as well as a diverse sample including multiple cancer types.
However, some limitations should be acknowledged. A key limitation is the uncertainty regarding how representative the study sample is of the entire population of cancer patients in Iceland, given that over a third of the participants had a university degree, potentially introducing response bias. Participation required computer literacy and access to electronic IDs, which may have introduced selection bias [86]. Despite the rather large sample, specific cancer groups had relatively small sample sizes, which may have limited the ability to examine certain variables. The cross-sectional design prevents conclusions about causality, and the reliance on self-reported data may have introduced reporting bias. Furthermore, in relation to gender-specific analysis, it would have been more relevant to evaluate a cohort of cancer survivors of both sexes treated for the same anatomical location (e.g., lung cancer), rather than for gender-specific cancers such as breast and prostate. However, this was not feasible due to small sample sizes. Such an approach would have allowed a more direct comparison of factors influencing quality of life by reducing bias related to cancer type, treatment regimen and long-term side effects. Finally, although multiple cancer types were included in the analysis, this study did not account for type of treatment or time since diagnosis, both of which could influence global health status/QoL.
Future research should continue to investigate the impact of social factors on the QoL of cancer survivors by gender, time since diagnosis and various cancer and treatment types in longitudinal studies to better understand the association between social predictors and QoL.
5. Conclusions
In conclusion, cancer survivors’ global health status/QoL is influenced by a range of social, demographic and psychological factors, underscoring the importance of a comprehensive approach to survivorship care that is tailored to cancer type and gender. Role functioning is a central dimension of quality of life, as it anchors purpose, identity and social contribution. It reflects the capacity to parent, to contribute productively and to occupy valued roles within society—all of which are vital elements of self-worth and social connectedness. Disruptions in role functioning can therefore undermine both individual well-being and collective adjustment. Considering the predictive factors identified in this study, women may particularly benefit from programs that enhance role and social functioning and improve access to instrumental support, while men may benefit more from interventions focused primarily on role functioning. Interventions aimed at restoring role functioning and addressing depression are likely to benefit all survivors, regardless of gender or cancer type.
Author Contributions
Conceptualization, S.Á.A., H.L.H.J., G.H.Þ., S.E.E., J.E.T. and S.G.; methodology, S.Á.A., H.L.H.J., G.H.Þ., S.E.E., J.E.T. and S.G.; formal analysis, S.Á.A.; data curation, S.Á.A.; writing—original draft preparation, S.Á.A.; writing—review and editing, H.L.H.J., G.H.Þ., S.E.E., J.E.T. and S.G.; visualization, S.Á.A.; supervision, H.L.H.J. and S.G.; project administration, H.L.H.J., G.H.Þ., J.E.T. and S.G.; funding acquisition, G.H.Þ. and J.E.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the National Bioethics Committee (number 20-006, approved on 1 April 2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The datasets presented in this article are not readily available because of personal protection laws. Requests to access the datasets should be directed to the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Jemal, A.; Sung, H.; Kelly, K.; Soerjomataram, I.; Bray, F. The Cancer Atlas [Internet]. American Cancer Society & the International Agency for Research on Cancer. 2025, p. 76. Available online: https://canceratlas.cancer.org/ (accessed on 6 August 2025).
- Sung, H.; Jiang, C.; Siegel, R.; Jemal, A. Global Cancer Facts & Figures, 5th ed.; American Cancer Society: Atlanta, GA, USA, 2024; p. 1. [Google Scholar]
- World Health Organization. Cancer [Internet]. 2025. Available online: https://www.who.int/news-room/fact-sheets/detail/cancer (accessed on 13 April 2025).
- Krabbameinsfélagið. Yfirlitstölfræði [Internet]. 2025. Available online: https://www.krabb.is/krabbamein/tolfraedi/krabbamein-og-gaedaskraning/heildartolfraedi-meina (accessed on 13 April 2025).
- Parry, C.; Kent, E.E.; Mariotto, A.B.; Alfano, C.M.; Rowland, J.H. Cancer survivors: A booming population. Cancer Epidemiol. Biomark. Prev. 2011, 20, 1996–2005. [Google Scholar] [CrossRef]
- Tonorezos, E.; Devasia, T.; Mariotto, A.B.; Mollica, M.A.; Gallicchio, L.; Green, P.; Doose, M.; Brick, R.; Streck, B.; Reed, C.; et al. Prevalence of cancer survivors in the United States. JNCI J. Natl. Cancer Inst. 2024, 116, 1784–1790. [Google Scholar] [PubMed]
- Tu, H.; Wen, C.P.; Tsai, S.P.; Chow, W.-H.; Wen, C.; Ye, Y.; Zhao, H.; Tsai, M.K.; Huang, M.; Dinney, C.P.; et al. Cancer risk associated with chronic diseases and disease markers: Prospective cohort study. BMJ 2018, 360, k134. Available online: https://www.bmj.com/content/360/bmj.k134 (accessed on 24 June 2025). [CrossRef] [PubMed]
- Krebber, A.M.H.; Buffart, L.M.; Kleijn, G.; Riepma, I.C.; de Bree, R.; Leemans, C.R.; Becker, A.; Brug, J.; van Straten, A.; Cuijpers, P.; et al. Prevalence of depression in cancer patients: A meta-analysis of diagnostic interviews and self-report instruments. Psycho-Oncology 2014, 23, 121–130. [Google Scholar] [CrossRef]
- Linden, W.; Vodermaier, A.; MacKenzie, R.; Greig, D. Anxiety and depression after cancer diagnosis: Prevalence rates by cancer type, gender, and age. J. Affect. Disord. 2012, 141, 343–351. [Google Scholar] [CrossRef]
- Smith, H.R. Depression in cancer patients: Pathogenesis, implications and treatment (Review). Oncol. Lett. 2015, 9, 1509–1514. [Google Scholar] [CrossRef]
- Wang, Y.-H.; Li, J.-Q.; Shi, J.-F.; Que, J.-Y.; Liu, J.-J.; Lappin, J.M.; Leung, J.; Ravindran, A.V.; Chen, W.-Q.; Qiao, Y.-L.; et al. Depression and anxiety in relation to cancer incidence and mortality: A systematic review and meta-analysis of cohort studies. Mol. Psychiatry 2020, 25, 1487–1499. [Google Scholar] [PubMed]
- Gudina, A.T.; Cheruvu, V.K.; Gilmore, N.J.; Kleckner, A.S.; Arana-Chicas, E.; Kehoe, L.A.; Belcher, E.K.; Cupertino, A.P. Health related quality of life in adult cancer survivors: Importance of social and emotional support. Cancer Epidemiol. 2021, 74, 101996. [Google Scholar]
- American Cancer Society. Late and Long-Term Effects of Cancer [Internet]. 2024. Available online: https://www.cancer.org/cancer/survivorship/long-term-health-concerns/long-term-side-effects-of-cancer.html (accessed on 18 March 2025).
- Lim, J.W.; Zebrack, B. Social networks and quality of life for long-term survivors of leukemia and lymphoma. Support. Care Cancer 2006, 14, 185–192. [Google Scholar] [CrossRef]
- Kroenke, C.H.; Kwan, M.L.; Neugut, A.I.; Ergas, I.J.; Wright, J.D.; Caan, B.J.; Hershman, D.; Kushi, L.H. Social networks, social support mechanisms, and quality of life after breast cancer diagnosis. Breast Cancer Res. Treat. 2013, 139, 515–527. [Google Scholar] [CrossRef]
- Payne, N.; Kelly, E.P.; Pawlik, T.M. Assessing structure and characteristics of social networks among cancer survivors: Impact on general health. Support. Care Cancer 2019, 27, 3045–3051. [Google Scholar] [CrossRef]
- Pinquart, M.; Duberstein, P.R. Associations of social networks with cancer mortality: A meta-analysis. Crit. Rev. Oncol./Hematol. 2010, 75, 122–137. [Google Scholar] [CrossRef]
- Gill, T.M.; Feinstein, A.R. A Critical Appraisal of the Quality of Quality-of-Life Measurements. JAMA 1994, 272, 619–626. [Google Scholar] [CrossRef] [PubMed]
- Bosc, M. Assessment of social functioning in depression. Compr. Psychiatry 2000, 41, 63–69. [Google Scholar] [CrossRef]
- Gamper, E.M.; Petersen, M.A.; Aaronson, N.; Costantini, A.; Giesinger, J.M.; Holzner, B.; Kemmler, G.; Oberguggenberger, A.; Singer, S.; Young, T.; et al. Development of an item bank for the EORTC Role Functioning Computer Adaptive Test (EORTC RF-CAT). Health Qual. Life Outcomes 2016, 14, 72. [Google Scholar] [CrossRef]
- Dixit, J.; Gupta, N.; Kataki, A.; Roy, P.; Mehra, N.; Kumar, L.; Singh, A.; Malhotra, P.; Gupta, D.; Goyal, A.; et al. Health-related quality of life and its determinants among cancer patients: Evidence from 12,148 patients of Indian database. Health Qual. Life Outcomes 2024, 22, 26. [Google Scholar] [CrossRef]
- Geue, K.; Sender, A.; Schmidt, R.; Richter, D.; Hinz, A.; Schulte, T.; Brähler, E.; Stöbel-Richter, Y. Gender-specific quality of life after cancer in young adulthood: A comparison with the general population. Qual. Life Res. 2014, 23, 1377–1386. [Google Scholar] [CrossRef]
- Hung, H.; Wu, L.; Chen, K. Determinants of Quality of Life in Lung Cancer Patients. J. Nurs. Sch. 2018, 50, 257–264. [Google Scholar] [CrossRef] [PubMed]
- Biparva, A.J.; Raoofi, S.; Rafiei, S.; Kan, F.P.; Kazerooni, M.; Bagheribayati, F.; Masoumi, M.; Doustmehraban, M.; Sanaei, M.; Zarabi, F.; et al. Global quality of life in breast cancer: Systematic review and meta-analysis. BMJ Support. Palliat. Care 2024, 13, e528–e536. [Google Scholar] [CrossRef]
- Meneguin, S.; Alves, I.G.; Camargo, H.T.F.; Pollo, C.F.; Segalla, A.V.Z.; de Oliveira, C. Comparative Study of the Quality of Life and Coping Strategies in Oncology Patients. Eur. J. Investig. Health Psychol. Educ. 2024, 14, 339–350. [Google Scholar] [CrossRef] [PubMed]
- Polanski, J.; Jankowska-Polanska, B.; Rosinczuk, J.; Chabowski, M.; Szymanska-Chabowska, A. Quality of life of patients with lung cancer. OncoTargets Ther. 2016, 9, 1023–1028. [Google Scholar] [CrossRef] [PubMed]
- Ayalon, R.; Bachner, Y.G. Medical, social, and personal factors as correlates of quality of life among older cancer patients with permanent stoma. Eur. J. Oncol. Nurs. 2019, 38, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Chagani, P.; Parpio, Y.; Gul, R.; Jabbar, A.A. Quality of life and its determinants in adult cancer patients undergoing chemotherapy treatment in Pakistan. Asia-Pac. J. Oncol. Nurs. 2017, 4, 140–146. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Rodríguez, I.; Hombrados-Mendieta, I.; Melguizo-Garín, A.; Martos-Méndez, M.J. The Importance of Social Support, Optimism and Resilience on the Quality of Life of Cancer Patients. Front. Psychol. 2022, 13, 833176. Available online: https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2022.833176/full (accessed on 17 February 2025). [CrossRef]
- Laghousi, D.; Jafari, E.; Nikbakht, H.; Nasiri, B.; Shamshirgaran, M.; Aminisani, N. Gender differences in health-related quality of life among patients with colorectal cancer. J. Gastrointest. Oncol. 2019, 10, 453–461. Available online: https://jgo.amegroups.org/article/view/27616 (accessed on 4 August 2025). [CrossRef]
- Zhou, J.; Wang, Z.; Chen, X.; Li, Q. Gender Differences in Psychosocial Outcomes and Coping Strategies of Patients with Colorectal Cancer: A Systematic Review. Healthcare 2023, 11, 2591. [Google Scholar] [CrossRef]
- Cherepanov, D.; Palta, M.; Fryback, D.G.; Robert, S.A. Gender differences in health-related quality-of-life are partly explained by sociodemographic and socioeconomic variation between adult men and women in the US: Evidence from four US nationally representative data sets. Qual. Life Res. 2010, 19, 1115–1124. [Google Scholar] [CrossRef]
- Bonhof, C.S.; de Rooij, B.H.; Schoormans, D.; Wasowicz, D.K.; Vreugdenhil, G.; Mols, F. Sex differences in health-related quality of life and psychological distress among colorectal cancer patients: A 2-year longitudinal study. J. Cancer Surviv. 2024. [Google Scholar] [CrossRef]
- Levinsen, A.K.G.; Kjaer, T.K.; Thygesen, L.C.; Maltesen, T.; Jakobsen, E.; Gögenur, I.; Borre, M.; Christiansen, P.; Zachariae, R.; Christensen, P.; et al. Social inequality in cancer survivorship: Educational differences in health-related quality of life among 27,857 cancer survivors in Denmark. Cancer Med. 2023, 12, 20150–20162. [Google Scholar] [CrossRef]
- Osann, K.; Hsieh, S.; Nelson, E.L.; Monk, B.J.; Chase, D.; Cella, D.; Wenzel, L. Factors associated with poor quality of life among cervical cancer survivors: Implications for clinical care and clinical trials. Gynecol. Oncol. 2014, 135, 266–272. [Google Scholar] [CrossRef]
- Schwartz, R.M.; Bevilacqua, K.G.; Alpert, N.; Liu, B.; Dharmarajan, K.V.; Ornstein, K.A.; Taioli, E. Educational Attainment and Quality of Life among Older Adults before a Lung Cancer Diagnosis. J. Palliat. Med. 2020, 23, 498–505. [Google Scholar] [CrossRef]
- Karunanithi, G.; Sagar, R.P.; Joy, A.; Vedasoundaram, P. Assessment of Psychological Distress and its Effect on Quality of Life and Social Functioning in Cancer Patients. Indian J. Palliat. Care 2018, 24, 72–77. [Google Scholar] [PubMed]
- Dehkordi, A.; Heydarnejad, M.S.; Fatehi, D. Quality of Life in Cancer Patients undergoing Chemotherapy. Oman Med. J. 2009, 24, 204–207. [Google Scholar] [CrossRef] [PubMed]
- Firkins, J.; Hansen, L.; Driessnack, M.; Dieckmann, N. Quality of life in “chronic” cancer survivors: A meta-analysis. J. Cancer Surviv. 2020, 14, 504–517. [Google Scholar] [CrossRef]
- Heydarnejad, M.S.; Hassanpour, D.A.; Solati, D.K. Factors affecting quality of life in cancer patients undergoing chemotherapy. Afr. Health Sci. 2011, 11, 266–270. [Google Scholar]
- Koch, M.; Hjermstad, M.J.; Tomaszewski, K.; Tomaszewska, I.; Hornslien, K.; Harle, A.; Arraras, J.; Morag, O.; Pompili, C.; Ioannidis, G.; et al. Gender effects on quality of life and symptom burden in patients with lung cancer: Results from a prospective, cross-cultural, multi-center study. J. Thorac. Dis. 2020, 12, 4253–4261. Available online: https://jtd.amegroups.org/article/view/43093 (accessed on 5 August 2025). [CrossRef] [PubMed]
- Pud, D. Gender differences in predicting quality of life in cancer patients with pain. Eur. J. Oncol. Nurs. 2011, 15, 486–491. [Google Scholar] [CrossRef]
- Trinquinato, I.; Marques da Silva, R.; Ticona Benavente, S.B.; Cristine Antonietti, C.; Siqueira Costa Calache, A.L. Gender differences in the perception of quality of life of patients with colorectal cancer. Investig. Educ. Enferm. 2017, 35, 320–329. [Google Scholar] [CrossRef]
- Csuka, S.I.; Rohánszky, M.; Thege, B.K. Gender differences in the predictors of quality of life in patients with cancer: A cross sectional study. Eur. J. Oncol. Nurs. 2024, 68, 102492. [Google Scholar] [CrossRef]
- Nasrabadi, F.K.; Rahimzadeh, S. The Role of Gender in the Quality of Life of Cancer Survivors: Health Literacy and Cognitive Functioning. Int. J. Cancer Manag. 2024, 17, e149321. Available online: https://brieflands.com/articles/ijcm-149321#abstract (accessed on 5 August 2025). [CrossRef]
- Pinquart, M.; Duberstein, P.R. Depression and cancer mortality: A meta-analysis. Psychol. Med. 2010, 40, 1797–1810. [Google Scholar] [CrossRef]
- Satin, J.R.; Linden, W.; Phillips, M.J. Depression as a predictor of disease progression and mortality in cancer patients: A meta-analysis. Cancer 2009, 115, 5349–5361. [Google Scholar] [CrossRef] [PubMed]
- Meléndez, J.C.; Mayordomo, T.; Sancho, P.; Tomás, J.M. Coping strategies: Gender differences and development throughout life span. Span. J. Psychol. 2012, 15, 1089–1098. [Google Scholar] [CrossRef]
- Kirchner, T.; Forns, M.; Muñoz, D.; Pereda, N. Psychometric properties and dimensional structure of the Spanish version of the Coping Responses Inventory-Adult Form. Psicothema 2008, 20, 902–909. [Google Scholar]
- Ptacek, J.T.; Smith Ronald, E.; Zanas, J. Gender, Appraisal, and Coping: A Longitudinal Analysis. J. Pers. 1992, 60, 747–770. [Google Scholar] [CrossRef]
- Vingerhoets, A.J.J.M.; Heck, G.L.V. Gender, coping and psychosomatic symptoms. Psychol. Med. 1990, 20, 125–135. [Google Scholar] [CrossRef] [PubMed]
- Yeh, S.-C.J.; Huang, C.-H.; Chou, H.-C.; Wan, T.T.H. Gender Differences in Stress and Coping among Elderly Patients on Hemodialysis. Sex Roles 2009, 60, 44–56. [Google Scholar] [CrossRef]
- Tamres, L.K.; Janicki, D.; Helgeson, V.S. Sex Differences in Coping Behavior: A Meta-Analytic Review and an Examination of Relative Coping. Pers. Soc. Psychol. Rev. 2002, 6, 2–30. [Google Scholar] [CrossRef]
- Rose, A.J.; Rudolph, K.D. A review of sex differences in peer relationship processes: Potential trade-offs for the emotional and behavioral development of girls and boys. Psychol. Bull. 2006, 132, 98–131. [Google Scholar] [CrossRef]
- Powroznik, K.; Stepanikova, I.; Cook, K.S. Growth from Trauma: Gender Differences in the Experience of Cancer and Long-term Survivorship. In Gender, Women’s Health Care Concerns and Other Social Factors in Health and Health Care [Internet]; Emerald Publishing Limited: Leeds, UK, 2018; pp. 17–36. Available online: https://www.emerald.com/insight/content/doi/10.1108/s0275-495920180000036001/full/html (accessed on 4 July 2025).
- van Roij, J.; Brom, L.; Youssef-El Soud, M.; van de Poll-Franse, L.; Raijmakers, N.J.H. Social consequences of advanced cancer in patients and their informal caregivers: A qualitative study. Support Care Cancer Off. J. Multinatl. Assoc. Support Care Cancer 2019, 27, 1187–1195. [Google Scholar] [CrossRef]
- LeMasters, T.; Madhavan, S.; Sambamoorthi, U.; Kurian, S. A population-based study comparing HRQoL among breast, prostate, and colorectal cancer survivors to propensity score matched controls, by cancer type, and gender. Psycho-Oncology 2013, 22, 2270–2282. [Google Scholar] [CrossRef]
- Arndt, V.; Merx, H.; Stegmaier, C.; Ziegler, H.; Brenner, H. Quality of Life in Patients With Colorectal Cancer 1 Year After Diagnosis Compared With the General Population: A Population-Based Study. J. Clin. Oncol. 2004, 22, 4829–4836. [Google Scholar] [CrossRef]
- Graells-Sans, A.; Serral, G.; Puigpinós-Riera, R.; Grupo Cohort DAMA. Social inequalities in quality of life in a cohort of women diagnosed with breast cancer in Barcelona (DAMA Cohort). Cancer Epidemiol. 2018, 54, 38–47. [Google Scholar] [CrossRef] [PubMed]
- Husson, O.; Zebrack, B.J.; Block, R.; Embry, L.; Aguilar, C.; Hayes-Lattin, B.; Cole, S. Health-Related Quality of Life in Adolescent and Young Adult Patients With Cancer: A Longitudinal Study. J. Clin. Oncol. 2017, 35, 652–659. [Google Scholar] [CrossRef]
- Islam, N.; Atreya, A.; Nepal, S.; Uddin, K.J.; Kaiser, R.; Menezes, R.G.; Lasrado, S.; Abdullah-Al-Noman, M. Assessment of quality of life (QOL) in cancer patients attending oncology unit of aTeaching Hospital in Bangladesh. Cancer Rep. 2023, 6, e1829. [Google Scholar] [CrossRef] [PubMed]
- Loge, J.H.; Abrahamsen, A.F.; Ekeberg, Ø.; Kaasa, S. Reduced health-related quality of life among Hodgkin’s disease survivors: A comparative study with general population norms. Ann. Oncol. 1999, 10, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Sun, F.-K.; Lu, C.-Y.; Yao, Y.; Chiang, C.-Y. Social functioning, depression, and quality of life among breast cancer patients: A path analysis. Eur. J. Oncol. Nurs. 2023, 62, 102237. [Google Scholar] [CrossRef]
- Zang, Y.; Qiu, Y.; Sun, Y.; Fan, Y. Baseline functioning scales of EORTC QLQ-C30 predict overall survival in patients with gastrointestinal cancer: A meta-analysis. Qual. Life Res. 2024, 33, 1455–1468. [Google Scholar] [CrossRef]
- Lara-Morales, A.; Soto-Ruiz, N.; Agudelo-Suárez, A.A.; García-Vivar, C. Social determinants of health in post-treatment cancer survivors: Scoping review. Eur. J. Oncol. Nurs. 2024, 70, 102614. [Google Scholar] [CrossRef]
- Liang, Y.; Hao, G.; Wu, M.; Hou, L. Social isolation in adults with cancer: An evolutionary concept analysis. Front. Psychol. 2022, 13, 973640. [Google Scholar] [CrossRef]
- Weiss, R. The provision of social relationships. In Doing unto Others: Joining, Molding, Conforming, Helping, Loving; Rubin, Z., Ed.; Prentice Hall: Englewood Cliffs, NJ, USA, 1974; pp. 17–26. [Google Scholar]
- Semmer, N.K.; Elfering, A.; Jacobshagen, N.; Perrot, T.; Beehr, T.A.; Boos, N. The emotional meaning of instrumental social support. Int. J. Stress Manag. 2008, 15, 235–251. [Google Scholar] [CrossRef]
- Torfadóttir, J.E.; Guðmundsdóttir, R.B.; Unnarsdóttir, A.B.; Þorvaldsdóttir, H.; Einarsdóttir, S.E.; Haraldsdóttir, Á.; Pálsson, G. Krabbameinsfélagið. Áttavitinn—Vísaðu Okkur Veginn: Rannsókn á Reynslu Fólks sem Greindist með Krabbamein á Árunum 2015–2019. 2024. Available online: https://www.krabb.is/media/attavitinn-fyrsti-hluti.pdf (accessed on 13 April 2025).
- Aaronson, N.K.; Ahmedzai, S.; Bergman, B.; Bullinger, M.; Cull, A.; Duez, N.J.; Filiberti, A.; Flechtner, H.; Fleishman, S.B.; De Haes, J.C.; et al. The European Organization for Research and Treatment of Cancer QLQ-C30: A Quality-of-Life Instrument for Use in International Clinical Trials in Oncology. JNCI J. Natl. Cancer Inst. 1993, 85, 365–376. [Google Scholar] [CrossRef]
- Ou, Z.; Tang, Y.; Fu, J.; Doucette, J.; Murimi, I.B. Patient-Reported Outcome Measures in Breast Cancer: A Systematic review of EORTC QLQ-C30, FACT-B, and EORTC QLQ-BR23 Development and validation. Value Health 2019, 22, S530. [Google Scholar] [CrossRef]
- Cankurtaran, E.S.; Ozalp, E.; Soygur, H.; Ozer, S.; Akbiyik, D.I.; Bottomley, A. Understanding the reliability and validity of the EORTC QLQ-C30 in Turkish cancer patients. Eur. J. Cancer Care (Engl.) 2008, 17, 98–104. [Google Scholar] [CrossRef]
- Osoba, D.; Aaronson, N.; Zee, B.; Sprangers, M.; te Velde, A. Modification of the EORTC QLQ-C30 (version 2.0) based on content validity and reliability testing in large samples of patients with cancer. The Study Group on Quality of Life of the EORTC and the Symptom Control and Quality of Life Committees of the NCI of Canada Clinical Trials Group. Qual. Life Res. Int. J. Qual. Life Asp. Treat Care Rehabil. 1997, 6, 103–108. [Google Scholar]
- Fayers, P.M.; Aaronson, N.K.; Bjordal, K.; Groenvold, M.; Curran, D.; Bottomley, A. The EORTC QLQ-C30 Scoring Manual, 3rd ed.; European Organisation for Research and Treatment of Cancer: Brussels, Belgium, 2001; Available online: https://qol.eortc.org/manual/scoring-manual/ (accessed on 9 July 2025).
- Giesinger, J.M.; Loth, F.L.; Aaronson, N.K.; Arraras, J.I.; Caocci, G.; Efficace, F.; Groenvold, M.; van Leeuwen, M.; Petersen, M.A.; Ramage, J.; et al. Thresholds for clinical importance were established to improve interpretation of the EORTC QLQ-C30 in clinical practice and research. J. Clin. Epidemiol. 2020, 118, 1–8. [Google Scholar] [CrossRef]
- Coon, C.D.; Schlichting, M.; Zhang, X. Interpreting Within-Patient Changes on the EORTC QLQ-C30 and EORTC QLQ-LC13. Patient 2022, 15, 691–702. [Google Scholar] [CrossRef] [PubMed]
- Cocks, K.; King, M.T.; Velikova, G.; Fayers, P.M.; Brown, J.M. Quality, interpretation and presentation of European Organisation for Research and Treatment of Cancer quality of life questionnaire core 30 data in randomised controlled trials. Eur. J. Cancer Oxf. Engl. 2008, 44, 1793–1798. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Ajele, K.W.; Idemudia, E.S. Charting the course of depression care: A meta-analysis of reliability generalization of the patient health questionnaire (PHQ- 9) as the measure. Discov. Ment. Health 2025, 5, 50. [Google Scholar] [CrossRef]
- Kræftens Bekæmpelse. Barometerundersøgelsen [Internet]. 2024. Available online: https://www.cancer.dk/om-os/det-arbejder-vi-for/barometerundersoegelsen/ (accessed on 15 April 2025).
- Scott, N.W.; Fayers, P.M.; Aaronson, N.K.; Bottomley, A.; de Graeff, A.; Groenvold, M.; Gundy, C.; Koller, M.; Petersen, M.A.; Sprangers, M. EORTC QLQ-C30 Reference Values [Internet]. EORTC Quality of Life Group. 2008. Available online: https://qol.eortc.org/manual/reference-values/ (accessed on 26 August 2025).
- Ashing-Giwa, K.T.; Lim, J.W. Examining the Impact of Socioeconomic Status and Socioecologic Stress on Physical and Mental Health Quality of Life Among Breast Cancer Survivors. Oncol. Nurs. Forum 2009, 36, 79–88. [Google Scholar] [CrossRef] [PubMed]
- Wingen, T.; Englich, B.; Estal-Muñoz, V.; Mareva, S.; Kassianos, A.P. Exploring the Relationship between Social Class and Quality of Life: The Mediating Role of Power and Status. Appl. Res. Qual. Life 2021, 16, 1983–1998. [Google Scholar] [CrossRef]
- Thoits, P.A. Role-Identity Salience, Purpose and Meaning in Life, and Well-Being among Volunteers. Soc. Psychol. Q. 2012, 75, 360–384. [Google Scholar] [CrossRef]
- Murnaghan, S.; Scruton, S.; Urquhart, R. Psychosocial interventions that target adult cancer survivors’ reintegration into daily life after active cancer treatment: A scoping review. JBI Evid. Synth. 2023, 22, 607–656. [Google Scholar] [CrossRef]
- Torfadóttir, J.E.; Einarsdóttir, S.E.; Helgason, Á.R.; Þórisdóttir, B.; Guðmundsdóttir, R.B.; Unnarsdóttir, A.B.; Tryggvadóttir, L.; Birgisson, H.; Þorvaldsdóttir, G.H. Áttavitinn—Rannsókn á reynslu einstaklinga af greiningu og með ferð krabbameina á Íslandi árin 2015–2019. Læknablaðið 2022, 108, 447–454. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).