Melanoma of the Scalp and Neck: A Population-Based Analysis of Survival and Treatment Patterns
Abstract
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
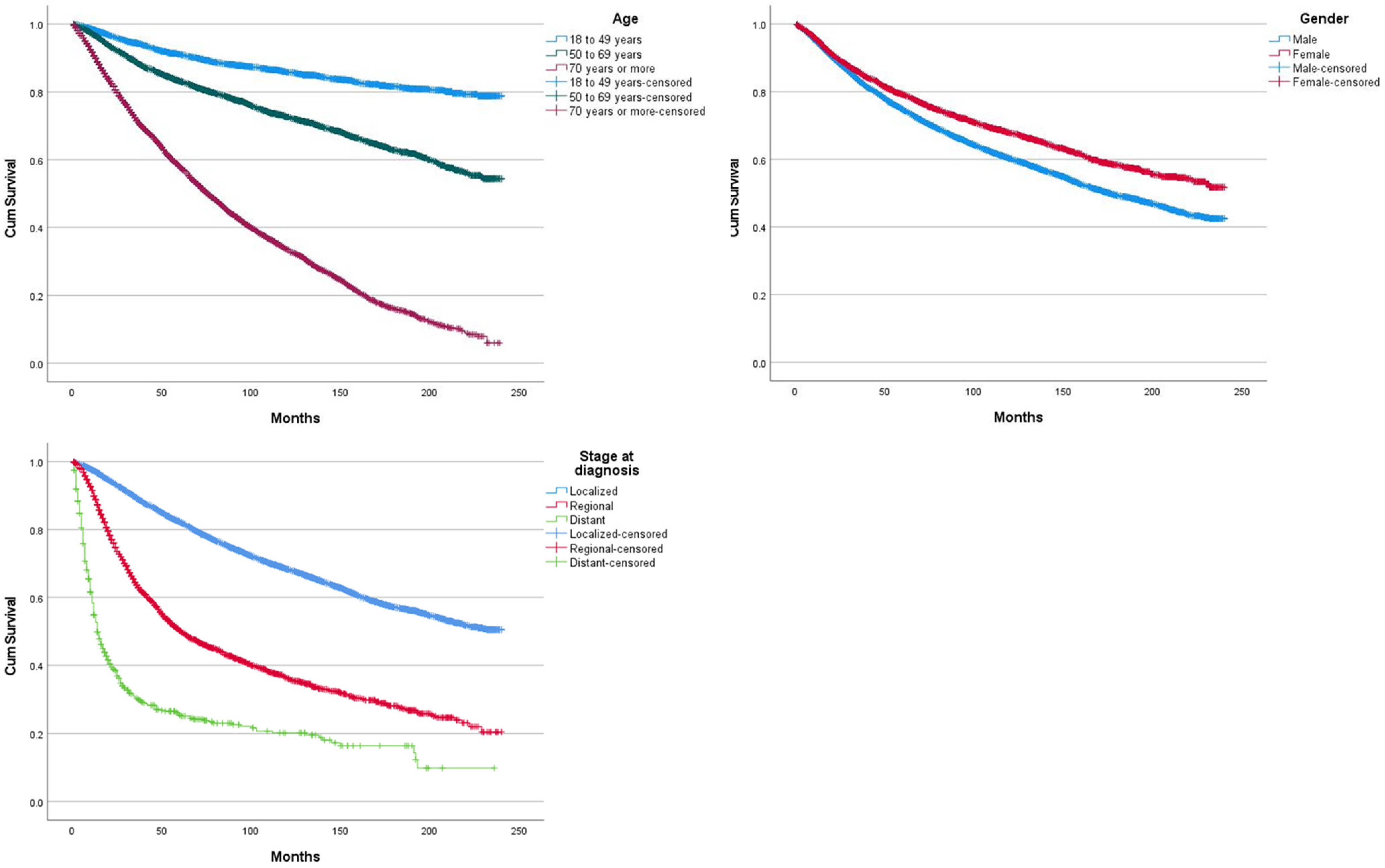
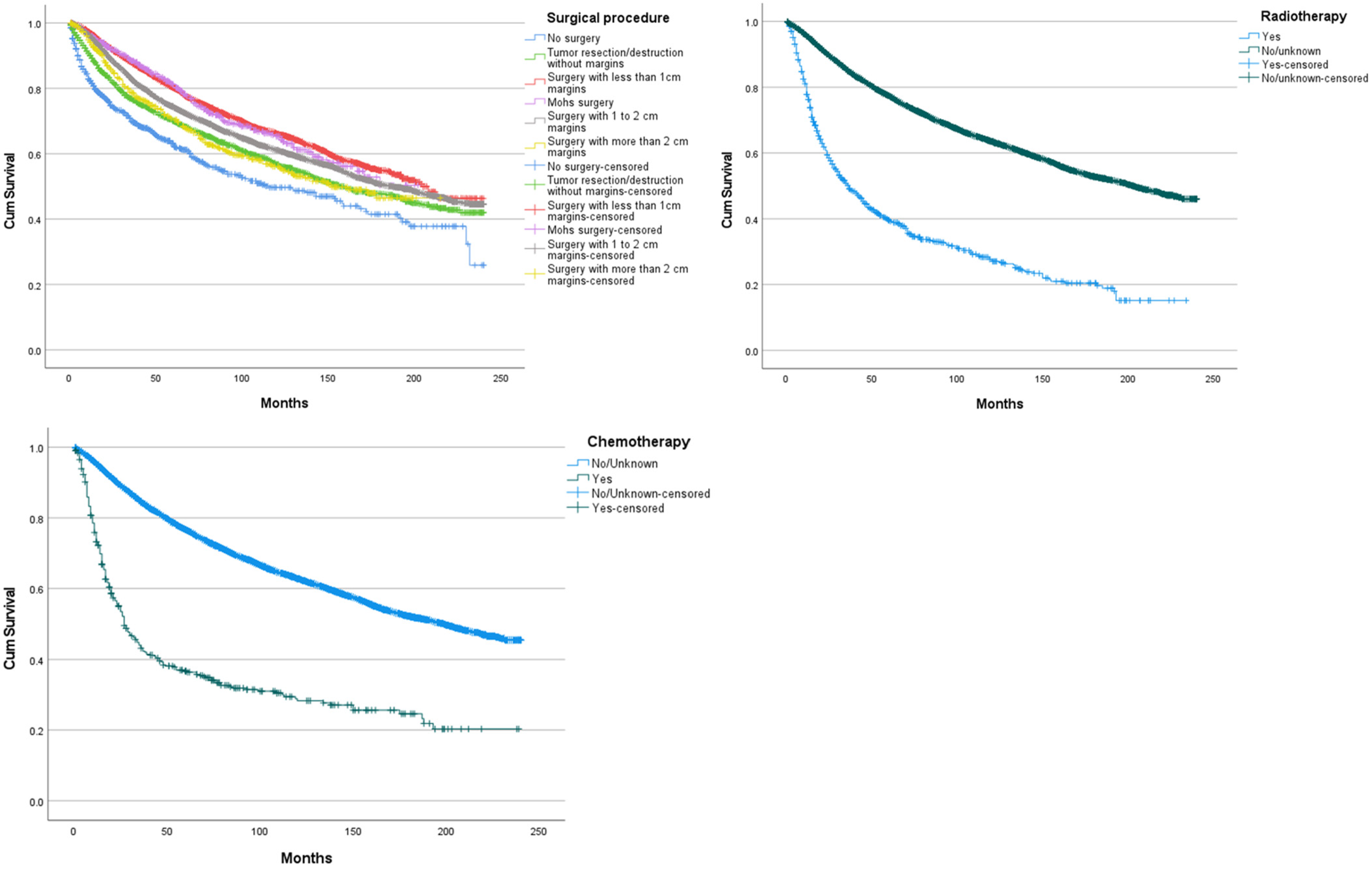
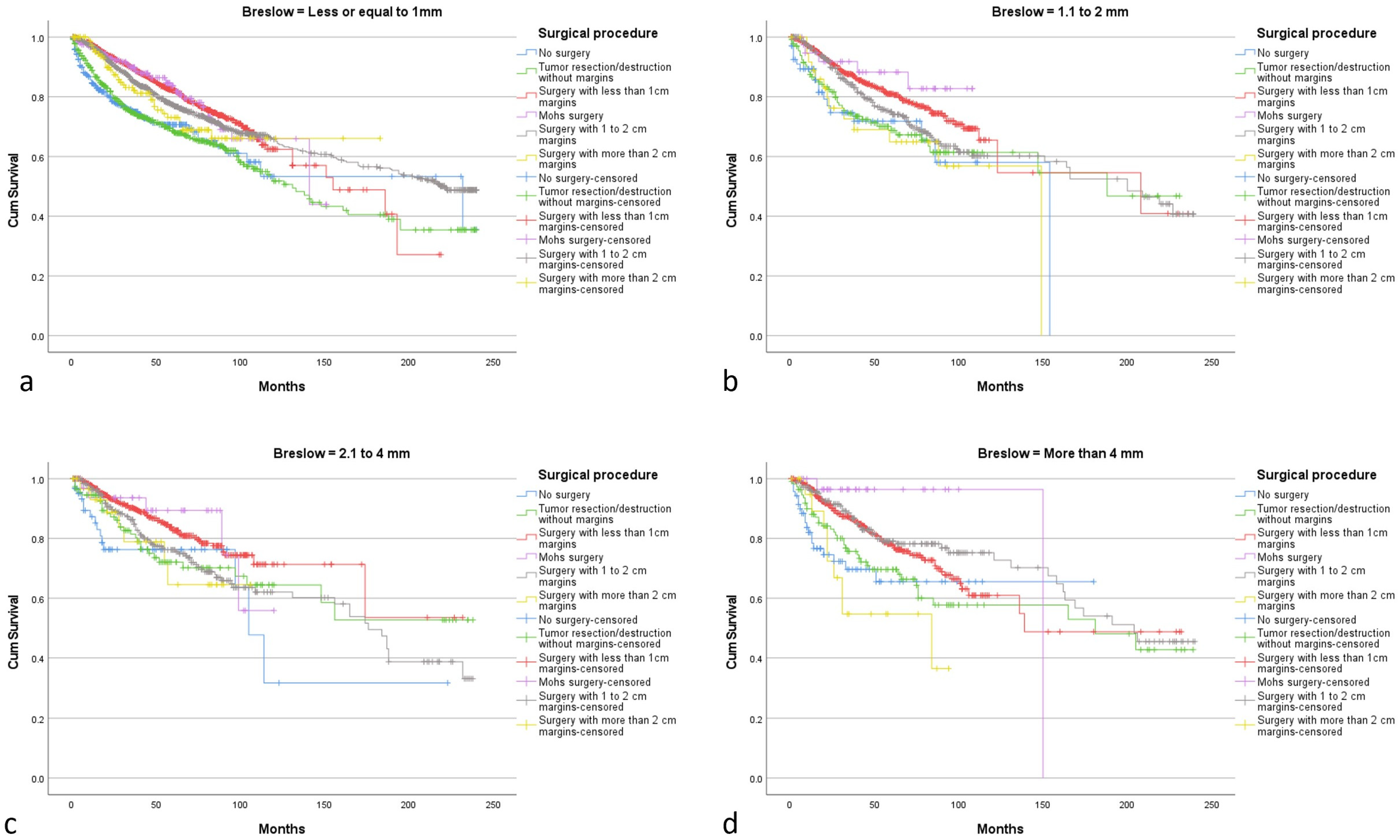
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Li, Z.; Fang, Y.; Chen, H.; Zhang, T.; Yin, X.; Man, J.; Yang, X.; Lu, M. Spatiotemporal Trends of the Global Burden of Melanoma in 204 Countries and Territories from 1990 to 2019: Results from the 2019 Global Burden of Disease Study. Neoplasia 2022, 24, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Linos, E.; Swetter, S.M.; Cockburn, M.G.; Colditz, G.A.; Clarke, C.A. Increasing Burden of Melanoma in the United States. J. Investig. Dermatol. 2009, 129, 1666–1674. [Google Scholar] [CrossRef]
- Krensel, M.; Schäfer, I.; Augustin, M. Cost-of-Illness of Melanoma in Europe—A Systematic Review of the Published Literature. J. Eur. Acad. Dermatol. Venereol. 2019, 33, 504–510. [Google Scholar] [CrossRef]
- Rigel, D.S.; Carucci, J.A. Malignant Melanoma: Prevention, Early Detection, and Treatment in the 21st Century. CA. Cancer J. Clin. 2000, 50, 215–236. [Google Scholar] [CrossRef]
- Porto, A.C.; Pinto Blumetti, T.; Oliveira Santos Filho, I.D.D.A.; Calsavara, V.F.; Duprat Neto, J.P.; Tavoloni Braga, J.C. Primary Cutaneous Melanoma of the Scalp: Patterns of Clinical, Histological and Epidemiological Characteristics in Brazil. PLoS ONE 2020, 15, e0240864. [Google Scholar] [CrossRef]
- Huismans, A.M.; Haydu, L.E.; Shannon, K.F.; Quinn, M.J.; Saw, R.P.M.; Spillane, A.J.; Stretch, J.R.; Thompson, J.F. Primary Melanoma Location on the Scalp Is an Important Risk Factor for Brain Metastasis: A Study of 1687 Patients with Cutaneous Head and Neck Melanomas. Ann. Surg. Oncol. 2014, 21, 3985–3991. [Google Scholar] [CrossRef] [PubMed]
- de Giorgi, V.; Rossari, S.; Gori, A.; Grazzini, M.; Savarese, I.; Crocetti, E.; Cervadoro, E.; Massi, D. The Prognostic Impact of the Anatomical Sites in the “Head and Neck Melanoma”: Scalp versus Face and Neck. Melanoma Res. 2012, 22, 402–405. [Google Scholar] [CrossRef]
- Wood, R.P.; Heyworth, J.S.; McCarthy, N.S.; Mauguen, A.; Berwick, M.; Thomas, N.E.; Millward, M.J.; Anton-Culver, H.; Cust, A.E.; Dwyer, T.; et al. Association of Known Melanoma Risk Factors with Primary Melanoma of the Scalp and Neck. Cancer Epidemiol. Biomark. Prev. 2020, 29, 2203–2210. [Google Scholar] [CrossRef]
- Howard, M.D.; Wee, E.; Wolfe, R.; McLean, C.A.; Kelly, J.W.; Pan, Y. Anatomic Location of Primary Melanoma: Survival Differences and Sun Exposure. J. Am. Acad. Dermatol. 2019, 81, 500–509. [Google Scholar] [CrossRef]
- Amin, M.B.; Greene, F.L.; Edge, S.B.; Compton, C.C.; Gershenwald, J.E.; Brookland, R.K.; Meyer, L.; Gress, D.M.; Byrd, D.R.; Winchester, D.P. The Eighth Edition AJCC Cancer Staging Manual: Continuing to Build a Bridge from a Population-Based to a More “Personalized” Approach to Cancer Staging. CA Cancer J. Clin. 2017, 67, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Swetter, S.M.; Thompson, J.A.; Albertini, M.R.; Barker, C.A.; Baumgartner, J.; Boland, G.; Chmielowski, B.; DiMaio, D.; Durham, A.; Fields, R.C.; et al. NCCN Guidelines® Insights: Melanoma: Cutaneous, Version 2.2021. J. Natl. Compr. Cancer Netw. JNCCN 2021, 19, 364–376. [Google Scholar] [CrossRef] [PubMed]
- Ethun, C.G.; Delman, K.A. The Importance of Surgical Margins in Melanoma. J. Surg. Oncol. 2016, 113, 339–345. [Google Scholar] [CrossRef] [PubMed]
- Lachiewicz, A.M.; Berwick, M.; Wiggins, C.L.; Thomas, N.E. Survival Differences Between Patients With Scalp or Neck Melanoma and Those With Melanoma of Other Sites in the Surveillance, Epidemiology, and End Results (SEER) Program. Arch. Dermatol. 2008, 144, 515–521. [Google Scholar] [CrossRef] [PubMed]
- Saaiq, M.; Zalaudek, I.; Rao, B.; Lee, Y.; Rudnicka, L.; Czuwara, J.; Giuffrida, R.; Wollina, U.; Jafferany, M.; Lotti, T.; et al. A Brief Synopsis on Scalp Melanoma. Dermatol. Ther. 2020, 33, e13795. [Google Scholar] [CrossRef]
- Dabouz, F.; Barbe, C.; Lesage, C.; Le Clainche, A.; Arnoult, G.; Hibon, E.; Bernard, P.; Grange, F. Clinical and Histological Features of Head and Neck Melanoma: A Population-Based Study in France. Br. J. Dermatol. 2015, 172, 707–715. [Google Scholar] [CrossRef]
- Fadaki, N.; Li, R.; Parrett, B.; Sanders, G.; Thummala, S.; Martineau, L.; Cardona-Huerta, S.; Miranda, S.; Cheng, S.-T.; Miller, J.R.; et al. Is Head and Neck Melanoma Different from Trunk and Extremity Melanomas with Respect to Sentinel Lymph Node Status and Clinical Outcome? Ann. Surg. Oncol. 2013, 20, 3089–3097. [Google Scholar] [CrossRef]
- Sparks, D.S.; Read, T.; Lonne, M.; Barbour, A.P.; Wagels, M.; Bayley, G.J.; Smithers, B.M. Primary Cutaneous Melanoma of the Scalp: Patterns of Recurrence. J. Surg. Oncol. 2017, 115, 449–454. [Google Scholar] [CrossRef]
- Licata, G.; Scharf, C.; Ronchi, A.; Pellerone, S.; Argenziano, G.; Verolino, P.; Moscarella, E. Diagnosis and Management of Melanoma of the Scalp: A Review of the Literature. Clin. Cosmet. Investig. Dermatol. 2021, 14, 1435–1447. [Google Scholar] [CrossRef]
- Benati, E.; Longo, C.; Bombonato, C.; Moscarella, E.; Alfano, R.; Argenziano, G. Baldness and Scalp Melanoma. J. Eur. Acad. Dermatol. Venereol. 2017, 31, e528–e530. [Google Scholar] [CrossRef]
- de Vries, E.; Nijsten, T.E.C.; Visser, O.; Bastiaannet, E.; van Hattem, S.; Janssen-Heijnen, M.L.; Coebergh, J.-W.W. Superior Survival of Females among 10,538 Dutch Melanoma Patients Is Independent of Breslow Thickness, Histologic Type and Tumor Site. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2008, 19, 583–589. [Google Scholar] [CrossRef]
- Pollack, L.A.; Li, J.; Berkowitz, Z.; Weir, H.K.; Wu, X.-C.; Ajani, U.A.; Ekwueme, D.U.; Li, C.; Pollack, B.P. Melanoma Survival in the United States, 1992 to 2005. J. Am. Acad. Dermatol. 2011, 65, S78.e1–S78.e10. [Google Scholar] [CrossRef] [PubMed]
- Forman, S.B.; Ferringer, T.C.; Peckham, S.J.; Dalton, S.R.; Sasaki, G.T.; Libow, L.F.; Elston, D.M. Is Superficial Spreading Melanoma Still the Most Common Form of Malignant Melanoma? J. Am. Acad. Dermatol. 2008, 58, 1013–1020. [Google Scholar] [CrossRef]
- Susok, L.; Stücker, M.; Bechara, F.G.; Stockfleth, E.; Gambichler, T. Multivariate Analysis of Prognostic Factors in Patients with Nodular Melanoma. J. Cancer Res. Clin. Oncol. 2021, 147, 2759–2764. [Google Scholar] [CrossRef] [PubMed]
- Cappello, Z.J.; Augenstein, A.C.; Potts, K.L.; McMasters, K.M.; Bumpous, J.M. Sentinel Lymph Node Status Is the Most Important Prognostic Factor in Patients with Melanoma of the Scalp. Laryngoscope 2013, 123, 1411–1415. [Google Scholar] [CrossRef] [PubMed]
- Wong, S.L.; Balch, C.M.; Hurley, P.; Agarwala, S.S.; Akhurst, T.J.; Cochran, A.; Cormier, J.N.; Gorman, M.; Kim, T.Y.; McMasters, K.M.; et al. Sentinel Lymph Node Biopsy for Melanoma: American Society of Clinical Oncology and Society of Surgical Oncology Joint Clinical Practice Guideline. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2012, 30, 2912–2918. [Google Scholar] [CrossRef]
- Garbe, C.; Amaral, T.; Peris, K.; Hauschild, A.; Arenberger, P.; Bastholt, L.; Bataille, V.; Del Marmol, V.; Dréno, B.; Fargnoli, M.C.; et al. European Consensus-Based Interdisciplinary Guideline for Melanoma. Part 1: Diagnostics—Update 2019. Eur. J. Cancer Oxf. Engl. 1990 2020, 126, 141–158. [Google Scholar] [CrossRef]
- Gimotty, P.A.; Shore, R.; Lozon, N.L.; Whitlock, J.; He, S.; Vigneau, F.D.; Dickie, L.; Elder, D.E.; Xu, X.; Schwartz, A.G.; et al. Miscoding of Melanoma Thickness in SEER: Research and Clinical Implications. J. Investig. Dermatol. 2016, 136, 2168–2172. [Google Scholar] [CrossRef]
- Stiegel, E.; Xiong, D.; Ya, J.; Funchain, P.; Isakov, R.; Gastman, B.; Vij, A. Prognostic Value of Sentinel Lymph Node Biopsy According to Breslow Thickness for Cutaneous Melanoma. J. Am. Acad. Dermatol. 2018, 78, 942–948. [Google Scholar] [CrossRef]
- Munsch, C.; Lauwers-Cances, V.; Lamant, L.; Gentil, C.; Rochaix, P.; Garrido, I.; Lopez, R.; Chevreau, C.; Paul, C.; Meyer, N. Breslow Thickness, Clark Index and Ulceration Are Associated with Sentinel Lymph Node Metastasis in Melanoma Patients: A Cohort Analysis of 612 Patients. Dermatol. Basel Switz. 2014, 229, 183–189. [Google Scholar] [CrossRef]
- Shaikh, W.R.; Dusza, S.W.; Weinstock, M.A.; Oliveria, S.A.; Geller, A.C.; Halpern, A.C. Melanoma Thickness and Survival Trends in the United States, 1989 to 2009. J. Natl. Cancer Inst. 2016, 108, djv294. [Google Scholar] [CrossRef]
- Tas, F.; Erturk, K. Scalp Melanoma Is Associated with High Mitotic Rate and Is a Poor Prognostic Factor for Recurrence and Outcome. Melanoma Res. 2017, 27, 387–390. [Google Scholar] [CrossRef] [PubMed]
- Gershenwald, J.E.; Scolyer, R.A.; Hess, K.R.; Sondak, V.K.; Long, G.V.; Ross, M.I.; Lazar, A.J.; Faries, M.B.; Kirkwood, J.M.; McArthur, G.A.; et al. Melanoma Staging: Evidence-Based Changes in the American Joint Committee on Cancer Eighth Edition Cancer Staging Manual. CA Cancer J. Clin. 2017, 67, 472–492. [Google Scholar] [CrossRef] [PubMed]
- Kashani-Sabet, M.; Miller III, J.R.; Lo, S.; Nosrati, M.; Stretch, J.R.; Shannon, K.F.; Spillane, A.J.; Saw, R.P.M.; Cleaver, J.E.; Kim, K.B.; et al. Reappraisal of the Prognostic Significance of Mitotic Rate Supports Its Reincorporation into the Melanoma Staging System. Cancer 2020, 126, 4717–4725. [Google Scholar] [CrossRef] [PubMed]
- Koskivuo, I.; Giordano, S.; Veräjänkorva, E.; Vihinen, P. One-Cm Versus 2-Cm Excision Margins for Patients With Intermediate Thickness Melanoma: A Matched-Pair Analysis. Dermatol. Surg. Off. Publ. Am. Soc. Dermatol. Surg. Al 2015, 41, 1130–1136. [Google Scholar] [CrossRef] [PubMed]
- Hanna, S.; Lo, S.N.; Saw, R.P. Surgical Excision Margins in Primary Cutaneous Melanoma: A Systematic Review and Meta-Analysis. Eur. J. Surg. Oncol. 2021, 47, 1558–1574. [Google Scholar] [CrossRef] [PubMed]
- Hu, A.C.; Lee, S.A.; Clark, E.G.; Yamamoto, M.; Jakowatz, J.G.; Evans, G.R.D. Impact of Immediate Surgical Reconstruction Following Wide Local Excision of Malignant Head and Neck Melanoma. Plast. Reconstr. Surg. Glob. Open 2020, 8, e2661. [Google Scholar] [CrossRef]
- Han, A.Y.; Dhanjani, S.; Pettijohn, K.; Patel, P.B.; John, M.A.S. Optimal Resection Margin for Head and Neck Cutaneous Melanoma. Laryngoscope 2019, 129, 1386–1394. [Google Scholar] [CrossRef]
- Tagliaferri, L.; Lancellotta, V.; Fionda, B.; Mangoni, M.; Casà, C.; Di Stefani, A.; Pagliara, M.M.; D’Aviero, A.; Schinzari, G.; Chiesa, S.; et al. Immunotherapy and Radiotherapy in Melanoma: A Multidisciplinary Comprehensive Review. Hum. Vaccines Immunother. 2022, 18, 1903827. [Google Scholar] [CrossRef]
- Finn, L.; Markovic, S.N.; Joseph, R.W. Therapy for Metastatic Melanoma: The Past, Present, and Future. BMC Med. 2012, 10, 23. [Google Scholar] [CrossRef]
- Kwak, M.; Farrow, N.; Salama, A.K.; Mosca, P.J.; Hanks, B.A.; Slingluff, C.L.; Beasley, G.M. Updates in Adjuvant Systemic Therapy for Melanoma. J. Surg. Oncol. 2019, 119, 222–231. [Google Scholar] [CrossRef]

| Variable | N (%) |
|---|---|
| Total | 20,728 (100) |
| Age | |
| Mean (SD) | 62.5 (16.5) |
| 18 to 49 years | 4449 (21.5) |
| 50 to 69 years | 8546 (41.2) |
| 70 years or more | 7733 (37.3) |
| Gender | |
| Male | 15,814 (76.3) |
| Female | 4914 (23.7) |
| Histologic subtype | |
| 8720/3 Malignant melanoma, NOS | 9259 (44.4) |
| 8721/3 Nodular melanoma | 2000 (9.6) |
| 8742/3 Lentigo maligna melanoma | 2570 (12.4) |
| 8743/3 Superficial spreading melanoma | 5351 (25.8) |
| 8745/3 Desmoplastic melanoma, malignant | 636 (3.1) |
| 8772/3 Spindle cell melanoma, NOS | 483 (2.3) |
| Other subtypes | 429 (2.1) |
| Race | |
| White | 19,823 (95.6) |
| Black | 55 (0.3) |
| Asian/pacific islander | 87 (0.4) |
| American Indian/Alaska Native | 47 (0.2) |
| Unknown | 716 (3.5) |
| Stage | |
| In situ | 7 (<1) |
| Localized | 16,365 (79) |
| Regional | 2885 (13.9) |
| Distant | 599 (2.9) |
| Unknown | 872 (4.2) |
| Surgical procedure | |
| No surgery | 1053 (5.1) |
| Tumor resection/destruction without margin | 2351 (11.3) |
| Mohs surgery | 686 (3.3) |
| Surgery with <1 cm margins | 9326 (45) |
| Surgery with 1 to 2 cm margins | 6563 (31.7) |
| Surgery with >2 cm margins | 600 (2.9) |
| Unknown | 149 (0.7) |
| Radiotherapy | |
| Yes | 806 (3.9) |
| No/unknown | 19,922 (96.1) |
| Chemotherapy | |
| Yes | 434 (2.1) |
| No/unknown | 20,294 (97.9) |
| Breslow | |
| N = 10,124 | |
| Mean (SD) | 1.49 mm (2.09) |
| Ulceration | |
| Yes | 2377 (11.5) |
| No | 11,937 (57.6) |
| Unknown | 6414 (30.9) |
| Mitotic rate (mitosis per mm2) | |
| 2 or less | 4820 (23.3) |
| 3 to 10 | 1645 (7.9) |
| 11 or more | 503 (2.4) |
| Unknown | 6968 (33.6) |
| Variable | N (%) |
| Breslow Thickness | ||||
|---|---|---|---|---|
| Surgical Procedure | ≤1 mm N = 6451 | 1.1–2 mm N = 1370 | 2.1–4 mm N = 1121 | >4 mm N = 978 |
| No surgery | 416 | 68 | 66 | 70 |
| Tumor resection/destruction without margins | 659 | 134 | 115 | 112 |
| Mohs surgery | 254 | 45 | 35 | 32 |
| Surgery with <1 cm margins | 3434 | 718 | 599 | 528 |
| Surgery with 1–2 cm margins | 1529 | 367 | 274 | 214 |
| Surgery with >2 cm margins | 159 | 38 | 32 | 22 |
| Variables | Exp(B) | 95% CI | p-Value |
|---|---|---|---|
| Age a | |||
| 18 to 49 years | ref | ||
| 50 to 69 years | 2.142 | 1.947–2.358 | <0.005 |
| 70 years or more | 6.982 | 6.368–7.654 | <0.005 |
| Gender b | |||
| Male | ref | ||
| Female | 0.897 | 0.844–0.954 | <0.005 |
| Histologic subtype c | |||
| 8720/3 Malignant melanoma, NOS | ref | ||
| 8721/3 Nodular melanoma | 1.879 | 1.746–2.022 | <0.005 |
| 8742/3 Lentigo maligna melanoma | 0.709 | 0.653–0.770 | <0.005 |
| 8743/3 Superficial spreading melanoma | 0.815 | 0.761–0.872 | <0.005 |
| 8745/3 Desmoplastic melanoma, malignant 8772/3 Spindle cell melanoma, NOS | 1.177 1.480 | 1.039–1.333 1.299–1.685 | 0.010 <0.005 |
| Stage d | |||
| Localized | ref | ||
| Regional | 1.856 | 1. 595–2.160 | <0.005 |
| Distant | 4.228 | 3.310–5.401 | <0.005 |
| Surgical procedure e | |||
| No surgery | ref | ||
| Tumor resection/destruction without margin | 0.756 | 0.662–0.864 | <0.005 |
| Surgery with <1 cm margins | 0.568 | 0.501–0.642 | <0.005 |
| Mohs surgery | 0.606 | 0.483–0.711 | <0.005 |
| Surgery with 1 to 2 cm margins | 0.654 | 0.578–0.740 | <0.005 |
| Surgery with >2 cm margins | 0.621 | 0.519–0.741 | <0.005 |
| Radiotherapy f | |||
| No/unknown | ref | ||
| Yes | 1.351 | 1.217–1.500 | <0.005 |
| Chemotherapy g | |||
| No/unknown | ref | ||
| Yes | 1.514 | 1.323–1.732 | <0.005 |
| Breslow thickness h | |||
| ≤1 mm | ref | ||
| 1.1–2 mm | 1.043 | 0.919–1.183 | 0.515 |
| 2.1–4 mm | 0.985 | 0.854–1.135 | 0.834 |
| >4 mm | 1.031 | 0.891–1.192 | 0.684 |
| Ulceration h | |||
| No | ref | ||
| Yes | 2.085 | 1.940–2.241 | <0.005 |
| Mitotic rate (mitosis per mm2) h | |||
| 2 or less | ref | ||
| 3 to 10 | 2.104 | 1.875–2.360 | <0.005 |
| 11 or more | 2.346 | 1.988–2.768 | <0.005 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scampa, M.; Mégevand, V.; Viscardi, J.A.; Giordano, S.; Kalbermatten, D.F.; Oranges, C.M. Melanoma of the Scalp and Neck: A Population-Based Analysis of Survival and Treatment Patterns. Cancers 2022, 14, 6052. https://doi.org/10.3390/cancers14246052
Scampa M, Mégevand V, Viscardi JA, Giordano S, Kalbermatten DF, Oranges CM. Melanoma of the Scalp and Neck: A Population-Based Analysis of Survival and Treatment Patterns. Cancers. 2022; 14(24):6052. https://doi.org/10.3390/cancers14246052
Chicago/Turabian StyleScampa, Matteo, Vladimir Mégevand, Juan A. Viscardi, Salvatore Giordano, Daniel F. Kalbermatten, and Carlo M. Oranges. 2022. "Melanoma of the Scalp and Neck: A Population-Based Analysis of Survival and Treatment Patterns" Cancers 14, no. 24: 6052. https://doi.org/10.3390/cancers14246052
APA StyleScampa, M., Mégevand, V., Viscardi, J. A., Giordano, S., Kalbermatten, D. F., & Oranges, C. M. (2022). Melanoma of the Scalp and Neck: A Population-Based Analysis of Survival and Treatment Patterns. Cancers, 14(24), 6052. https://doi.org/10.3390/cancers14246052







