Cancer Histology and Natural History of Patients with Lung Cancer and Venous Thromboembolism
Abstract
:Simple Summary
Abstract
1. Introduction
2. Methods
2.1. Patients
2.2. Inclusion Criteria
2.3. Follow-Up
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
References
- Mulder, F.I.; Horváth-Puhó, E.; van Es, N.; van Laarhoven, H.W.M.; Pedersen, L.; Moik, F.; Ay, C.; Büller, H.R.; Sørensen, H.T. Venous thromboembolism in cancer patients: A population-based cohort study. Blood 2021, 137, 1959–1969. [Google Scholar] [CrossRef] [PubMed]
- Prandoni, P.; Lensing, A.W.; Piccioli, A.; Bernardi, E.; Simioni, P.; Girolami, B.; Marchiori, A.; Sabbion, P.; Prins, M.H.; Noventa, F.; et al. Recurrent venous thromboembolism and bleeding complications during anticoagulant treatment in patients with cancer and venous thrombosis. Blood 2002, 100, 3484–3488. [Google Scholar] [CrossRef] [PubMed]
- Chew, H.K.; Davies, A.M.; Wun, T.; Harvey, D.; Zhou, H.; White, R.H. The incidence of venous thromboembolism among patients with primary lung cancer. J. Thromb. Haemost. 2008, 6, 601–608. [Google Scholar] [CrossRef] [PubMed]
- Connolly, G.C.; Menapace, L.; Safadjou, S.; Francis, C.W.; Khorana, A.A. Prevalence and clinical significance of incidental and clinically suspected venous thromboembolismin lung cancer patients. Clin. Lung Cancer 2013, 14, 713–718. [Google Scholar] [CrossRef] [PubMed]
- Farge, D.; Frere, C.; Connors, J.M.; Khorana, A.A.; Kakkar, A.; Ay, C.; Muñoz, A.; Brenner, B.; Prata, P.H.; Brilhante, D.; et al. 2022 international clinical practice guidelines for the treatment and prophylaxis of venous thromboembolism in patients with cancer, including patients with COVID-19. Lancet Oncol. 2022, 23, e334–e347. [Google Scholar] [CrossRef]
- Key, N.S.; Khorana, A.A.; Kuderer, N.M.; Bohlke, K.; Lee, A.Y.Y.; Arcelus, J.I.; Wong, S.L.; Balaban, E.P.; Flowers, C.R.; Francis, C.W.; et al. Venous thromboembolism prophylaxis and treatment in patients with cancer: ASCO clinical practice guideline update. J. Clin. Oncol. 2020, 38, 496–520. [Google Scholar] [CrossRef] [PubMed]
- Muñoz Martín, A.J.; Gallardo Díaz, E.; García Escobar, I.; Macías Montero, R.; Martínez-Marín, V.; Pachón Olmos, V.; Pérez Segura, P.; Quintanar Verdúguez, T.; Salgado Fernández, M. SEOM clinical guideline of venous thromboembolism (VTE) and cancer (2019). Clin. Transl. Oncol. 2020, 22, 171–186. [Google Scholar] [CrossRef]
- Mahe, I.; Chidiac, J.; Bertoletti, L.; Font, C.; Trujillo-Santos, J.; Peris, M.; Ductor, C.P.; Nieto, S.; Grandone, E.; Monreal, M.; et al. The clinical course of venous thromboembolism may differ according to cancer site. Am. J. Med. 2017, 130, 337–347. [Google Scholar] [CrossRef]
- Lecumberri, R.; Ruiz-Artacho, P.; Tzoran, I.; Brenner, B.; Farge-Bancel, D.; Ay, C.; Rosa, V.; Iria, F.; Hernández-Blasco, L.; Santos, J.T.; et al. Outcome of cancer-associated venous thromboembolism is more favorable among patients with hematologic malignancies than in those with solid tumors. Thromb. Haemost. 2022. [Google Scholar] [CrossRef]
- Agnelli, G.; Muñoz, A.; Franco, L.; Mahé, I.; Brenner, B.; Connors, J.M.; Gussoni, G.; Hamulyak, E.N.; Lambert, C.; Suero, M.R.; et al. Apixaban and dalteparin for the treatment of venous thromboembolism in patients with different sites of cancer. Thromb. Haemost. 2021, 122, 796–807. [Google Scholar] [CrossRef]
- Ferlay, J.; Colombet, M.; Soerjomataram, I.; Mathers, C.; Parkin, D.M.; Piñeros, M.; Znaor, A.; Bray, F. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int. J. Cancer 2019, 144, 1941–1953. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Artacho, P.; Trujillo-Santos, J.; Lopez-Jimenez, L.; Font, C.; Díaz-Pedroche, M.D.C.; Sánchez Muñoz-Torrero, J.F.; Peris, M.L.; Skride, A.; Maestre, A.; Monreal, M.; et al. Clinical characteristics and outcomes of patients with lung cancer and venous thromboembolism. TH Open 2018, 2, e210–e217. [Google Scholar] [CrossRef] [PubMed]
- Walker, A.J.; Baldwin, D.R.; Card, T.R.; Powell, H.A.; Hubbard, R.B.; Grainge, M.J. Risk of venous thromboembolism in people with lung cancer: A cohort study using linked UK healthcare data. Br. J. Cancer 2016, 115, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Tsubata, Y.; Hotta, T.; Hamai, K.; Furuya, N.; Yokoyama, T.; Saito, R.; Nakamura, A.; Masuda, T.; Hamaguchi, M.; Kuyama, S.; et al. new risk-assessment tool for venous thromboembolism in advanced lung cancer: A prospective, observational study. J. Hematol. Oncol. 2022, 15, 40. [Google Scholar] [CrossRef]
- Alexander, M.; Kirsa, S.; Wolfe, R.; MacManus, M.; Ball, D.; Solomon, B.; Burbury, K. Thromboembolism in lung cancer-an area of urgent unmet need. Lung Cancer 2014, 84, 275–280. [Google Scholar] [CrossRef]
- Zhang, Y.; Yang, Y.; Chen, W.; Guo, L.; Liang, L.; Zhai, Z.; Wang, C.; Group, C.V. China venous thromboembolism (VTE) study group. Prevalence and associations of VTE in patients with newly diagnosed lung cancer. Chest 2014, 146, 650–658. [Google Scholar] [CrossRef]
- Jaureguízar, A.; Jiménez, D.; Bikdeli, B.; Ruiz-Artacho, P.; Muriel, A.; Tapson, V.; López-Reyes, R.; Valero, B.; Kenet, G.; Monreal, M.; et al. RIETE investigators. Heart rate and mortality in patients with acute symptomatic pulmonary embolism. Chest 2022, 161, 524–534. [Google Scholar] [CrossRef]
- Lecumberri, R.; Ruiz-Artacho, P.; Trujillo-Santos, J.; Brenner, B.; Barillari, G.; Ruiz-Ruiz, J.; Lorente, M.A.; Verhamme, P.; Vázquez, F.J.; Weinberg, I.; et al. RIETE investigators. management and outcomes of cancer patients with venous thromboembolism presenting with thrombocytopenia. Thromb. Res. 2020, 195, 139–145. [Google Scholar] [CrossRef]
- Bikdeli, B.; Jimenez, D.; Hawkins, M.; Ortíz, S.; Prandoni, P.; Brenner, B.; Decousus, H.; Masoudi, F.A.; Trujillo-Santos, J.; Krumholz, H.M.; et al. Rationale, design and methodology of the computerized registry of patients with venous thromboembolism (RIETE). Thromb. Haemost. 2018, 118, 214–224. [Google Scholar] [CrossRef]
- de Winter, M.A.; Dorresteijn, J.A.N.; Ageno, W.; Ay, C.; Beyer-Westendorf, J.; Coppens, M.; Klok, F.A.; Moustafa, F.; Riva, N.; Artacho, P.C.; et al. Estimating bleeding risk in patients with cancer-associated thrombosis: Evaluation of existing risk scores and development of a new risk score. Thromb. Haemost. 2022, 122, 818–829. [Google Scholar] [CrossRef]
- Lyman, G.H. Venous thromboembolism in the patient with cancer: Focus on burden of disease and benefits of thromboprophylaxis. Cancer 2011, 117, 1334–1349. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.; Korn, J.R.; Mallick, R.; Friedman, M.; Nichols, C.; Menzin, J. Incidence of venous thromboembolism among chemotherapy-treated patients with lung cancer and its association with mortality: A retrospective database study. J. Thromb. Thrombolysis 2012, 34, 446–456. [Google Scholar] [CrossRef] [PubMed]
- Kourelis, T.V.; Wysokinska, E.M.; Wang, Y.; Yang, P.; Mansfield, A.S.; Tafur, A.J. Early venous thromboembolic events are associated with worse prognosis in patients with lung cancer. Lung Cancer 2014, 86, 358–362. [Google Scholar] [CrossRef]
- Leiva, O.; Connors, J.M.; Al-Samkari, H. Impact of tumor genomic mutations on thrombotic risk in cancer patients. Cancers 2020, 12, 1958. [Google Scholar] [CrossRef]
- Zhua, V.W.; Zhaoc, J.J.; Gao, Y.; Syn, N.L.; Zhang, S.S.; Ou, S.H.; Bauer, K.A.; Nagasaka, M. Thromboembolism in ALK+ and ROS1+NSCLC patients: A systematic review and meta-analysis. Lung Cancer 2021, 157, 147–155. [Google Scholar] [CrossRef] [PubMed]
| Adenocarcinoma | Squamous | Small-Cell | Other | |
|---|---|---|---|---|
| Patients, N | 293 | 98 | 44 | 47 |
| Clinical characteristics | ||||
| Male gender | 200 (68%) | 85 (87%) ‡ | 32 (73%) | 37 (79%) |
| Age (mean years ± SD) | 63 ± 11 | 67 ± 9.1 ‡ | 66 ± 8.2 | 65 ± 8.6 |
| Body weight (mean kg ± SD) | 71 ± 13 | 71 ± 11 | 75 ± 13 | 72 ± 13 |
| Smoking habit | 52 (19%) | 25 (27%) | 11 (26%) | 12 (27%) |
| Chronic lung disease | 67 (23%) | 42 (43%) ‡ | 9 (21%) | 12 (26%) |
| Chronic heart failure | 13 (4.4%) | 5 (5.1%) | 1 (2.3%) | 2 (4.3%) |
| Additional risk factors for VTE | ||||
| Recent surgery | 15 (5.1%) | 6 (6.1%) | 2 (4.5%) | 4 (8.5%) |
| Immobility ≥ 4 days | 64 (22%) | 13 (13%) | 7 (16%) | 8 (17%) |
| Use of estrogens | 5 (1.7%) | 3 (3.1%) | 1 (2.3%) | 0 |
| None of the above | 215 (73%) | 77 (79%) | 35 (80%) | 36 (77%) |
| Prior VTE | 17 (5.8%) | 8 (8.2%) | 5 (11%) | 2 (4.3%) |
| Initial VTE presentation | ||||
| Pulmonary embolism | 211 (72%) | 66 (67%) | 32 (73%) | 25 (53%) † |
| In patients with PE | ||||
| SBP levels < 90 mm Hg | 10 (5.1%) | 1 (1.6%) | 0 | 2 (8.3%) |
| Heart rate > 100 bpm (N = 311) | 74 (38%) | 20 (32%) | 8 (27%) | 8 (35%) |
| Sat O2 levels (mean % ± SD) | 90 ± 8.1 | 92 ± 4.6 | 93 ± 3.8 | 94 ± 3.7 |
| PESI ≥ 105 points | 128 (61%) | 54 (82%) † | 22 (69%) * | 17 (68%) |
| Lower-limb DVT | 53 (18%) | 20 (20%) | 8 (18%) | 12 (26%) |
| Upper-limb DVT | 29 (9.9%) | 14 (14%) | 4 (9.1%) | 10 (21%) * |
| Cancer characteristics | ||||
| Metastases | 240 (82%) | 53 (54%) ‡ | 30 (68%) * | 31 (67%) * |
| Time since cancer diagnosis | ||||
| Median months (IQR) | 2 (0–11) | 5 (2–15) ‡ | 4 (1–11) * | 3 (0–10) |
| <90 days | 139 (50%) | 24 (26%) ‡ | 13 (31%) * | 21 (48%) |
| Stage III–IV | 266 (91%) | 76 (78%) | 42 (96%) | 43 (92%) |
| ECOG 3–4 | 61 (21%) | 16 (17%) | 6 (14%) | 9 (19%) |
| Concomitant therapies | ||||
| Antiplatelets | 43 (15%) | 25 (26%) * | 7 (16%) | 9 (19%) |
| Corticosteroids | 89 (30%) | 24 (25%) | 12 (27%) | 11 (23%) |
| Blood tests | ||||
| Anemia | 159 (54%) | 72 (74%) ‡ | 26 (59%) | 33 (70%) * |
| Leukocyte count > 11,000/µL | 106 (37%) | 29 (31%) | 9 (19%) | 10 (22%) |
| Platelet count < 100,000/µL | 9 (3.1%) | 10 (10%) † | 1 (2.3%) | 3 (6.4%) |
| Platelet count > 450,000/µL | 14 (4.8%) | 8 (8.2%) | 5 (11%) | 9 (19%) ‡ |
| CrCl levels < 60 mL/min | 50 (17%) | 22 (22%) | 11 (25%) | 8 (17%) |
| Adenocarcinoma | Squamous | Small-Cell | Others | |
|---|---|---|---|---|
| Patients, N | 293 | 98 | 44 | 47 |
| Duration of therapy | ||||
| Mean days (±SD) | 184 ± 212 | 195 ± 261 | 214 ± 203 | 175 ± 236 |
| Median days (IQR) | 114 (47–210) | 105 (38–218) | 160 (91–232) | 87 (44–203) * |
| Duration > 6 months | 100 (35%) | 30 (32%) | 18 (41%) | 12 (26%) |
| Initial therapy | ||||
| Low-molecular-weight heparin | 260 (89%) | 89 (91%) | 40 (91%) | 39 (83%) |
| Mean LMWH dose (IU/kg/day) | 169 ± 41 | 170 ± 44 | 164 ± 42 | 164 ± 43 |
| Unfractionated heparin | 3 (1.0%) | 0 | 0 | 2 (4.3%) |
| Thrombolytics | 6 (2.0%) | 0 | 1 (2.3%) | 0 |
| Direct oral anticoagulants | 1 (0.3%) | 0 | 0 | 0 |
| Inferior vena cava filter | 2 (0.7%) | 1 (1.0%) | 0 | 0 |
| Long-term therapy | ||||
| Low-molecular-weight heparin | 240 (82%) | 74 (76%) | 39 (89%) | 40 (85%) |
| Mean LMWH dose (IU/kg/day) | 159 ± 38 | 153 ± 37 | 155 ± 35 | 149 ± 47 |
| Vitamin K antagonists | 14 (4.8%) | 6 (6.1%) | 1 (2.3%) | 1 (2.1%) |
| Direct oral anticoagulants | 2 (0.7%) | 1 (1.0%) | 0 | 1 (2.1%) |
| Oncological therapy | ||||
| Chemotherapy | 150 (52%) | 55 (59%) | 29 (66%) | 23 (55%) |
| Radiotherapy | 60 (21%) | 22 (24%) | 11 (25%) | 10 (24%) |
| Other | 12 (4.1%) | 7 (7.1%) | 5 (11%) * | 1 (2.1%) |
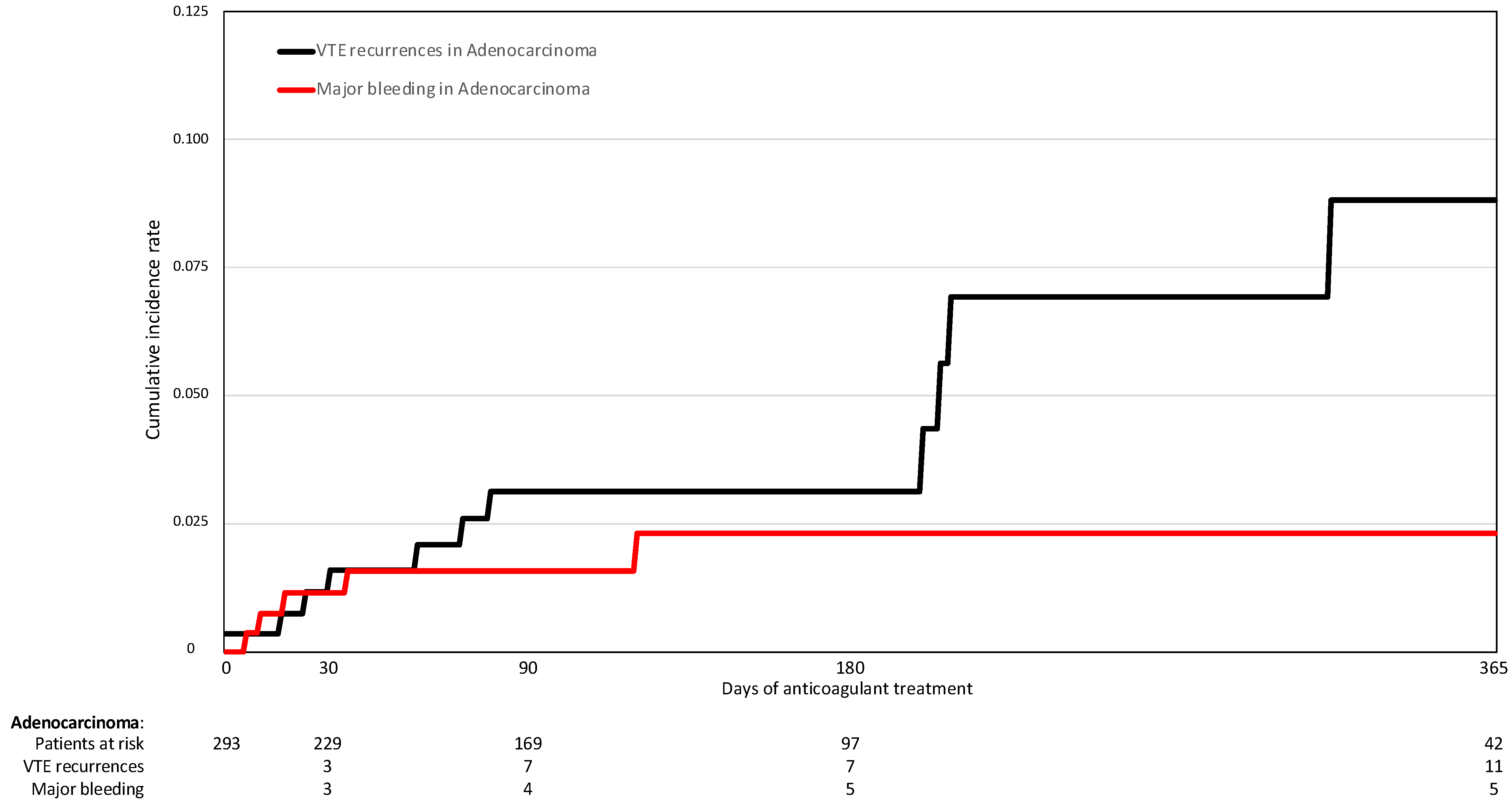
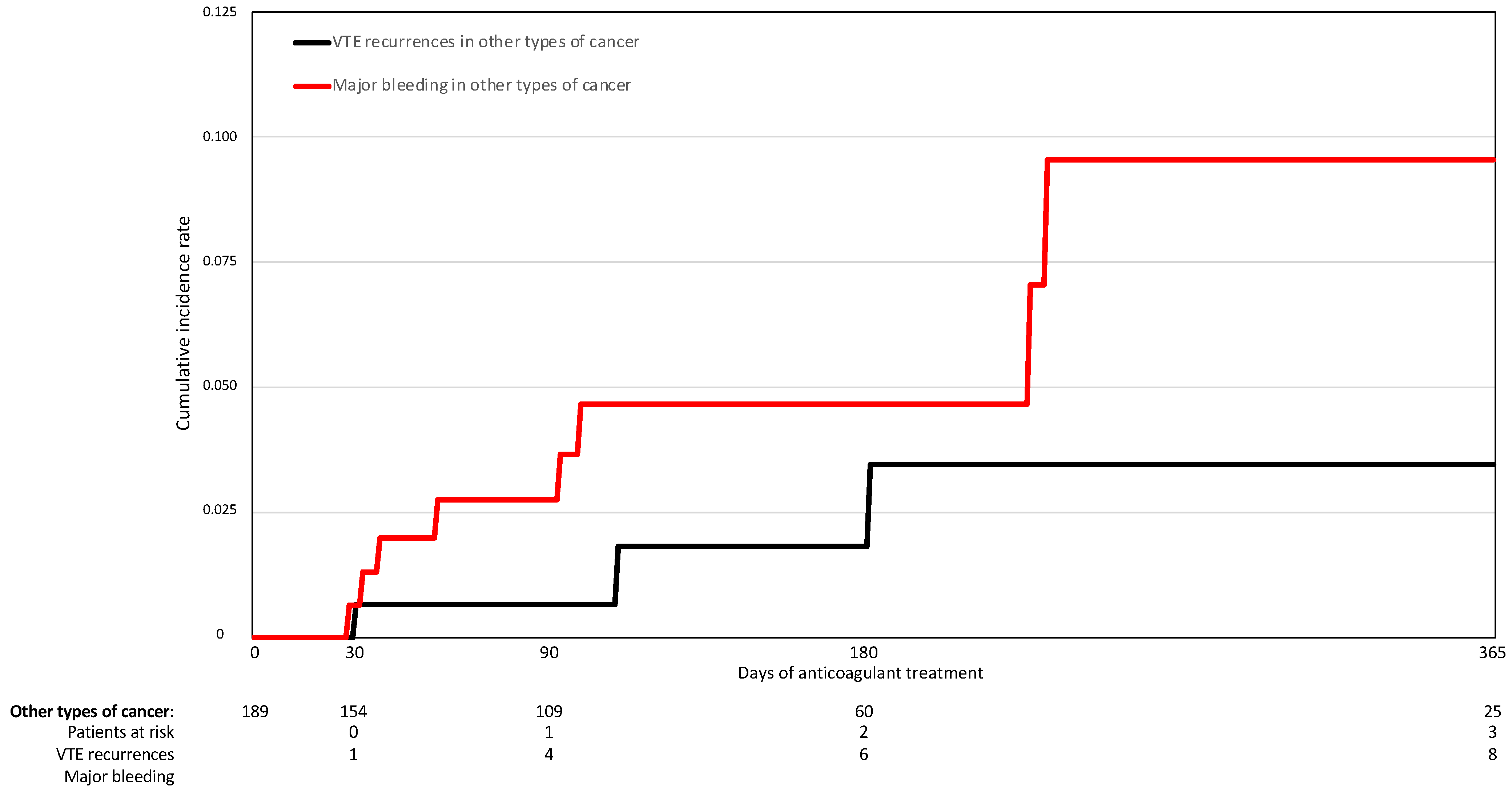
| Adenocarcinoma | Squamous | Small-Cell | Other | |||||
|---|---|---|---|---|---|---|---|---|
| N | Events per 100 Patient-Years | N | Events per 100 Patient-Years | N | Events per 100 Patient-Years | N | Events per 100 Patient-Years | |
| Patients, N | 293 | 98 | 44 | 47 | ||||
| Patient-years of therapy | 106 | 101 | 153 | 85 | ||||
| PE recurrences | 7 | 4.93 (1.98–10.1) | 0 | - | 1 | 4.01 (0.05–22.3) | 1 | 47.7 (0.06–26.5) |
| DVT recurrences | 4 | 2.82 (0.76–7.21) | 1 | 2.08 (0.03–11.5) | 0 | - | 0 | - |
| VTE recurrences | 11 | 7.74 (3.86–13.9) | 1 | 2.08 (0.03–11.5) | 1 | 4.01 (0.05–22.3) | 1 | 4.76 (0.06–26.5) |
| Major bleeding | 6 | 4.22 (1.54–9.19) | 4 | 8.30 (2.23–21.3) | 3 | 12.0 (2.42–35.2) | 2 | 9.53 (1.07–34.4) |
| Gastrointestinal | 2 | 1.41 (0.16–5.08) | 2 | 4.15 (0.47–15.0) | 0 | - | 0 | - |
| Intracranial | 2 | 1.41 (0.16–5.08) | 0 | - | 2 | 8.03 (0.90–29.0) * | 0 | - |
| Menorrhagia | 1 | 0.70 (0.01–3.92) | 0 | - | 0 | - | 0 | - |
| Retroperitoneal | 1 | 0.70 (0.01–3.92) | 0 | - | 1 | 4.01 (0.05–22.3) | 0 | - |
| Hemopericardium | 0 | - | 1 | 2.08 (0.03–11.5) | 0 | - | 1 | 4.76 (0.06–26.5) |
| Hemoptysis | 0 | - | 1 | 2.08 (0.03–11.5) | 0 | - | 1 | 4.76 (0.06–26.5) |
| All-cause death | 141 | 99.3 (83.6–117) | 39 | 81.0 (57.6–110) | 16 | 64.2 (36.7–104) | 22 | 105 (65.7–159) |
| Fatal PE | 10 | 7.04 (3.37–12.9) | 0 | - | 0 | - | 0 | - |
| Fatal bleeding | 1 | 0.70 (0.01–3.92) | 0 | - | 1 | 4.01 (0.05–22.3) | 0 | - |
| Hazard Ratio (95%CI) | p Value | |
|---|---|---|
| Univariable analysis | ||
| VTE recurrences | 2.35 (0.66–8.42) | 0.190 |
| Major bleeding | 0.46 (0.16–1.30) | 0.145 |
| Overall death | 1.15 (0.87–1.52) | 0.322 |
| Fatal PE | 6.5 (0.83–50.6) | 0.075 |
| Fatal bleeding | 0.64 (0.04–10.2) | 0.752 |
| Multivariable analysis | ||
| VTE recurrences | 3.79 (0.76–18.8) | 0.103 |
| Major bleeding | 0.29 (0.09–0.95) | 0.042 |
| Overall death | 1.02 (0.76–1.36) | 0.902 |
| Fatal PE | 5.74 (0.73–45.0) | 0.096 |
| Fatal bleeding | 0.62 (0.04–9.94) | 0.736 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ruiz-Artacho, P.; Lecumberri, R.; Trujillo-Santos, J.; Font, C.; López-Núñez, J.J.; Peris, M.L.; Díaz Pedroche, C.; Lobo, J.L.; López Jiménez, L.; López Reyes, R.; et al. Cancer Histology and Natural History of Patients with Lung Cancer and Venous Thromboembolism. Cancers 2022, 14, 4127. https://doi.org/10.3390/cancers14174127
Ruiz-Artacho P, Lecumberri R, Trujillo-Santos J, Font C, López-Núñez JJ, Peris ML, Díaz Pedroche C, Lobo JL, López Jiménez L, López Reyes R, et al. Cancer Histology and Natural History of Patients with Lung Cancer and Venous Thromboembolism. Cancers. 2022; 14(17):4127. https://doi.org/10.3390/cancers14174127
Chicago/Turabian StyleRuiz-Artacho, Pedro, Ramón Lecumberri, Javier Trujillo-Santos, Carme Font, Juan J. López-Núñez, María Luisa Peris, Carmen Díaz Pedroche, José Luis Lobo, Luciano López Jiménez, Raquel López Reyes, and et al. 2022. "Cancer Histology and Natural History of Patients with Lung Cancer and Venous Thromboembolism" Cancers 14, no. 17: 4127. https://doi.org/10.3390/cancers14174127
APA StyleRuiz-Artacho, P., Lecumberri, R., Trujillo-Santos, J., Font, C., López-Núñez, J. J., Peris, M. L., Díaz Pedroche, C., Lobo, J. L., López Jiménez, L., López Reyes, R., Jara Palomares, L., Pedrajas, J. M., Mahé, I., Monreal, M., & The RIETE Investigators. (2022). Cancer Histology and Natural History of Patients with Lung Cancer and Venous Thromboembolism. Cancers, 14(17), 4127. https://doi.org/10.3390/cancers14174127







