Simple Summary
Pancreatic cancer is a lethal malignant neoplasm with less than 10% 5-year relative survival after the initial diagnosis. Several factors may be related to the poor prognosis of pancreatic cancer, including the rapid tumor progression, increased metastatic propensity, insignificant symptoms, shortage of early diagnostic biomarkers, and its tendency toward resistance to both chemotherapy and radiotherapy. Pancreatic neoplastic cells interact intimately with a complicated microenvironment that can foster drug resistance, metastasis, or relapse in pancreatic cancer. In addition, evidence shows that perioperative factors, including surgical manipulation, anesthetics, or analgesics, might alter the tumor microenvironment and cancer progression. This review outlines the up-to-date knowledge of anesthesia implications in the pancreatic microenvironment and provides future anesthetic strategies for improving pancreatic cancer survival.
Abstract
Pancreatic malignancy is a lethal neoplasm, as well as one of the leading causes of cancer-associated mortality, having a 5-year overall survival rate of less than 10%. The average life expectancy of patients with advanced pancreatic cancer does not exceed six months. Although surgical excision is a favorable modality for long-term survival of pancreatic neoplasm, metastasis is initially identified in nearly 80% of the patients by the time of diagnosis, making the development of therapeutic policy for pancreatic cancer extremely daunting. Emerging evidence shows that pancreatic neoplastic cells interact intimately with a complicated microenvironment that can foster drug resistance, metastasis, or relapse in pancreatic cancer. As a result, the necessity of gaining further insight should be focused on the pancreatic microenvironment contributing to cancer progression. Numerous evidence reveals that perioperative factors, including surgical manipulation and anesthetics (e.g., propofol, volatile anesthetics, local anesthetics, epidural anesthesia/analgesia, midazolam), analgesics (e.g., opioids, non-steroidal anti-inflammatory drugs, tramadol), and anesthetic adjuvants (such as ketamine and dexmedetomidine), might alter the tumor microenvironment and cancer progression by affecting perioperative inflammatory or immune responses during cancer surgery. Therefore, the anesthesiologist plays an important role in perioperative management and may affect surgical outcomes. However, the literature on the impact of anesthesia on the pancreatic cancer microenvironment and progression is limited. This review summarizes the current knowledge of the implications of anesthesia in the pancreatic microenvironment and provides future anesthetic strategies for improving pancreatic cancer survival rates.
1. Introduction
Pancreatic cancer (PC) is a lethal malignant neoplasm. It is considered one of the leading causes of cancer-associated mortality, having a 5-year overall survival rate of less than 10% [1]. The average life expectancy of patients with advanced PC does not exceed six months [2]. Several factors related to the poor prognosis of PC include insignificant symptoms, shortage of early diagnostic biomarkers, rapid progression of the disease, increased metastatic propensity, and the disease’s tendency toward resistance to both chemotherapy and radiotherapy [3,4]. Early resection of the neoplasm is potentially the most successful treatment regime for such aggressive malignancy. However, by the time of diagnosis, metastasis is initially identified in approximately 80% of the patients, making PC treatment extremely challenging [5,6]. Despite several studies outlining various signal pathways involved in PC progression, the mechanisms of tumor progression are poorly understood.
The pancreatic microenvironment plays an important role in tumorigenesis [7]. As cancer progresses, alterations of surrounding tissue stroma develop rapidly. A key role of any non-transformed tissue stroma is to maintain a homeostatic response to shelter the immune system, the vascular system, and connective tissue components. Cancer hijacks the physiological responses to build a tumor microenvironment beneficial for cancer progression [7]. The pancreatic microenvironment includes the surrounding desmoplastic stroma, such as the epithelial-mesenchymal transition (EMT), and immunosuppressive pathways [7]. Evidence reveals that anesthetics or analgesics might alter the tumor microenvironment and the progression of the cancer by affecting perioperative inflammatory or immune responses during PC surgery [8,9]. Soliz et al. reported that propofol anesthesia was associated with no or low-grade complication compared with desflurane anesthesia in PC surgery [10]. In addition, in a retrospective study, we found that desflurane anesthesia was associated with poorer survival than propofol anesthesia in PC surgery [11]. Zhang et al. demonstrated that intraoperative intravenous lidocaine infusion increased survival in PC surgery [12]. Therefore, anesthesiologists may improve clinical outcomes by using preferential anesthetics. This review summarizes an overview of current knowledge of implications of anesthesia in the pancreatic microenvironment, and provides future anesthetic strategies for improving PC survival.
2. Patient Factors: Hyperglycemia and Obesity
2.1. Hyperglycemia
Diabetes mellitus (DM) and PC are intimately related, as high blood glucose levels promote PC proliferation, invasion, EMT, and metastasis [13,14]. In addition, insulin resistance, hyperinsulinemia, hyperglycemia, and chronic inflammation are the mechanisms of type-2-DM-associated PC [15].
2.1.1. Laboratory Studies
Recently, Otto et al. attributed a role to the type-2-DM-related hyperglycemic inflammatory micromilieu in the acquisition of malignancy-associated alterations in premalignant pancreatic ductal epithelial cells, thus providing new insights into how hyperglycemia might promote PC initiation [16]. It is well-known that EMT of pancreatic ductal epithelial cells develops in correlation with hyperglycemia or macrophages [17,18]. Moreover, hyperglycemia aggravates microenvironment hypoxia, accelerates EMT, and then promotes the metastatic ability of PC. PC is generally hypoxic due to its avascular morphology, and PC cells express high levels of HIF-1α and MMP-9 for promoting tumor growth, invasion and metastasis in a hypoxic environment [19]. In addition, the accumulation of HIF-1α induced by hyperglycemia might promote pancreatic glycolysis to facilitate cancer progression [20]. Zhou et al. reported that the high-glucose microenvironment accelerated PC growth [21]. With regard to the VAs, Guo et al. reported that isoflurane promoted glucose metabolism through upregulation of miR-21 and suppressed mitochondrial oxidative phosphorylation in ovarian cancer cells [22]. Dong et al. reported that dezocine, an opioid analgesic, promoted glucose metabolism and impaired the proliferation of lung cancer cells [23]. However, Codd et al. reported that opioid agonists did not elevate blood glucose and lacked an insulin-reducing effect [24]. Han et al. reported that indometacin, an inhibitor of cyclooxygenase (COX)-2, ameliorated high-glucose-induced proliferation and invasion via upregulation of E-cadherin in PC cells [25]. Current laboratory data on the effect of anesthesia on glucose metabolism in PC are limited, and further investigation is required.
2.1.2. Clinical Studies
Insulin resistance, hyperinsulinemia, hyperglycemia, and chronic inflammation are the mechanisms of type-2-DM-associated PC [15]. Recently, type 2 DM was shown to reduce the likelihood of cancer survival, and was significantly correlated with comorbidity and poor prognosis in patients undergoing PC surgery [15]. In addition, metformin may lower the probability of PC. By contrast, insulin therapy may amplify the probability of PC [15]. In another study, approximately 85% of PC patients exhibited impaired glucose tolerance associated with DM and had a reduced overall survival rate [26]. Elderly patients with new-onset DM are at higher risk of developing PC than the general population [26]. Therefore, new-onset DM and hyperglycemia serve as important screening tools to diagnose asymptomatic PC and improve PC survival [26]. Sandini et al. reported that preoperative blood glucose ≥ 140 mg/dL was associated with poor long-term outcomes in patients undergoing resection for PC [27]. Conti et al. reported that anti-diabetic drugs represented a significant protective factor against mortality among older adults with metastatic PC [28]. However, in a recent meta-analysis study, blood glucose, fasting blood glucose, and glycated hemoglobin (HbA1c) levels were not associated with the survival of patients with PC [29].
Liu et al. reported that the blood glucose levels of the DM patients in the propofol group were significantly lower than those in the sevoflurane group during gastric cancer surgery. This result indicated that the effect of propofol on glucose metabolism under surgical stimulation was less than that of sevoflurane [30]. Epidural blockade with bupivacaine attenuated the hyperglycemic response to surgery by modifying glucose production in colorectal surgery [31]. Current clinical data on the effect of anesthesia on glucose metabolism in PC are limited. Further investigation is required to determine the effects of anesthetics and analgesics on glucose metabolism in PC (Figure 1).
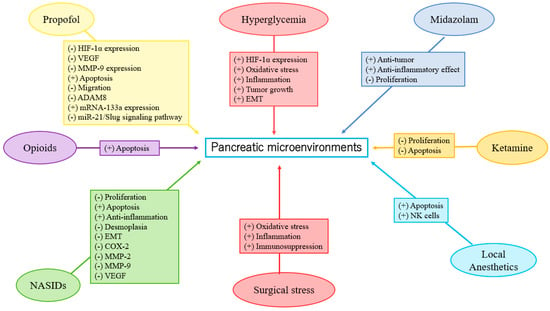
Figure 1.
Anesthesia in pancreatic microenvironments.
2.2. Obesity
Obesity-associated adipose tissue inflammation may play a central role in the development of PC and the promotion of PC growth [32]. Chronic inflammation, hormonal effects, circulating adipokines, and adipocyte-mediated inflammatory and immunosuppressive microenvironments are involved in the association of obesity with PC [33]. The tumor-promoting effects of obesity occur at the local level via adipose inflammation and associated alterations in the microenvironment, as well as systemically via circulating metabolic and inflammatory mediators associated with adipose inflammation [34].
In a review article, Heil et al. reported that anesthetics with the effect of inhibiting obesity-induced inflammation may improve postoperative outcomes [35]. Eley et al. concluded that VAs, ketamine, opioids, propofol, and regional anesthesia have been shown to modulate parts of the immune system in patients with obesity [36].
2.2.1. Laboratory Study
Incio et al. reported that obesity-induced inflammation and desmoplasia promoted PC progression and resistance to chemotherapy [37]. Until now, there have been no laboratory studies on the effects of anesthetics in obesity-induced inflammation and PC progression, and further investigation is necessary.
2.2.2. Clinical Studies
Recently, Zorbas et al. showed that obesity was significantly associated with higher risk of postoperative complications and mortality in patients with body mass index ≥ 40 after pancreatoduodenectomy [38]. Li et al. reported that the lean body-weight-based dosing of propofol had more potent antioxidant and anti-inflammatory effects on morbidly obese patients than the total body-weight-based dosing during anesthesia induction [39]. Until now, there have been no clinical studies on the effects of anesthetics in obesity-induced inflammation and PC progression, and further investigation is necessary.
3. Tumor Factors: EMT, Hypoxia-Inducible Factor-1α (HIF-1α), Matrix Metalloproteinases (MMP)-9 Expression, Inflammation, Apoptosis, Autophagy, and Oxidative Stress
3.1. EMT
The development of EMT originates in the conversion of epithelial cells to motile mesenchymal stem cells [40], which is based on many essential processes involving embryonic progression, tissue formation/fibrosis, and wound repairing [40]. Moreover, the initiation of EMT contributes to tumor growth, therapy resistance, and tumor spreading [40]. In the case of high EMT expression in tumors, deterioration of overall outcomes and metastases is inevitable. [40,41,42,43]. However, research on the direct effects of specific anesthetics on EMT of PC is currently lacking, and further investigation is required.
3.1.1. Laboratory Studies
Anesthesia and analgesia may affect EMT [25,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61]. Studies have reported that propofol suppressed EMT in esophageal cancer, choriocarcinoma, breast cancer, thyroid cancer, lung cancer, gastric cancer, hepatocellular carcinoma (HCC), renal cell carcinoma (RCC), prostate cancer, and oral squamous cell carcinoma cells [45,46,47,48,49,50,51,52,53,54]. By contrast, Ren et al. reported that desflurane induced EMT and metastasis in colorectal cancer through deregulation of the miR-34a/LOXL3 axis [44]. Opioids promoted EMT in breast and lung cancers via mu- or delta-opioid receptors [55,56]. Zhang et al. showed morphine-induced EMT in esophageal carcinoma cells [57]. However, sufentanil inhibited EMT by acting on NF-κB and Snail signaling pathways to inhibit proliferation and metastasis of esophageal cancer [58]. Lidocaine suppressed EMT in ovarian cancer cells [59]. However, high concentrations of levobupivacaine significantly increased EMT in the A549 lung cancer cell line, and enhanced metastasis in mice [60]. COX-2 inhibitors may suppress EMT in oral squamous cell carcinoma [61]. Han et al. reported that indometacin reduced the expression levels of MMP-2, MMP-9, and vascular endothelial growth factor (VEGF) by upregulation of E-cadherin, inhibiting proliferation and invasion of PC [25]. Zheng et al. observed the benefit of EMT inhibition due to the use of chemotherapy in PC treatment [62]. To the best of our knowledge, NSAIDs may inhibit EMT expression in PC. Propofol may inhibit EMT, but VAs may promote EMT in different cancers. On the other hand, opioids and LAs may induce uncertain effects (both positive and negative) on EMT. Laboratory research on the direct effects of specific anesthetics on EMT in PC is currently lacking. Further investigation is needed (see existing studies in Table 1 and Figure 1).

Table 1.
The existing studies on the effects of anesthetics/analgesics on clinical outcomes and pancreatic microenvironments.
3.1.2. Clinical Studies
3.2. HIF-1α
A review article showed that HIF-1α expression enhanced PC cell proliferation through multiple mechanisms by inducing neoplastic features and mediating tumorigenic crosstalk between tumor and stromal cells [91].
3.2.1. Laboratory Studies
Propofol could attenuate PC cells’ malignant potential by inhibiting HIF-1α and VEGF expression [73]. VAs enhance angiogenesis through HIF-1α activity in prostate and lung cancers [92]. Isoflurane upregulated the levels of HIF-1α and exerted a protumorigenic effect on a human RCC cell line [93]. However, in the neuroglioma cell line, sevoflurane decreased HIF-1α expression via miR-210, while desflurane downregulated HIF1-α and MMP-9 expressions via miR-138 and miR-335, respectively [94]. Opioids were shown to promote tumor angiogenesis in a breast cancer cell by stimulation of δ-opioid receptors in breast cancer cells, leading to activation of HIF-1α and expression of COX-2 via PI3K/Akt stimulation [95]. However, Koodie et al. reported that morphine suppressed tumor angiogenesis by inhibiting HIF-1α expression in mouse Lewis lung carcinoma cells [96]. Okamoto et al. showed that HIF-1α activation conferred resistance to lidocaine-induced cell death in the RCC cell line [97]. Zhou et al. revealed that inhibition of HIF-1α by meloxicam (a selective COX-2 inhibitor) could suppress angiogenesis and enhance apoptosis of HCC cells [98]. To the best of our knowledge, propofol may reduce HIF-1α expression in PC. Based on the limited data, further investigation is required and encouraged to determine the effects of VAs, LAs, and NSAIDs on HIF-1α expression in PC (Table 1 and Figure 1).
Recently, Yue et al. demonstrated that HIF-1α positively regulated miR-212 expression and resulted in pancreatic ductal adenocarcinoma progression [99]. Propofol inhibited ovarian cancer cells growth and glycolysis by elevating miR-212-5p expression [100]. Higher miR-212-5p expression showed a neuroprotective effect in rats with isoflurane-induced cognitive dysfunction by inhibiting neuroinflammation [101]. He et al. reported that δ-opioid receptor activation modified miR-212 expression in the rat kidney under prolonged hypoxia [102]. Until now, there have been no laboratory studies on the effects of anesthetics on miR-212 expression and PC progression; further investigation is necessary.
3.2.2. Clinical Studies
In a systemic review and meta-analysis, Raji et al. found that miR-212 could be a novel potential biomarker in cancer diagnosis and prognosis [103]. High levels of miR-212 indicated poor prognosis in PC, and low levels of miR-212 indicated poor prognosis in other cancers [103]. Until now, there have been no clinical studies on the effects of anesthetics on HIF-1α or miR-212 expression and PC progression; further investigation is necessary.
3.3. MMP-9
MMPs are part of the zinc-dependent proteolytic metalloenzyme family that may play a role in the early diagnosis and prognosis of PC. The higher expression of particular MMPs may also correlate with metastatic disease and/or poorer prognosis [104,105,106,107]. MMP-9, well-known as one of the most investigated MMPs, corrupts the extracellular matrix components, resulting in pathophysiologic alterations [108]. Impairment of MMP-9 expression and regulation affects various dysfunctions, including tumorigenesis, and MMP-9 suppression can be targeted in anticancer therapeutics [108]. Anesthesia may affect MMP-9 expression [74,94,109,110,111,112,113,114,115].
3.3.1. Laboratory Studies
Yu et al. reported that propofol inhibits PC growth by suppressing MMP-9 expression [74]. Sevoflurane and desflurane inhibited glioma cell proliferation and migration via downregulation of MMP-9 [94]. Sevoflurane and desflurane reduced the invasion of colorectal and neuroglioma cancer cells through downregulation of MMP-9 [94,110]. Moreover, sevoflurane inhibited the proliferation and invasion of HCC cells through downregulation of MMP-9 [111]. Zhang et al. showed that fentanyl inhibited tumor growth and cell invasion in colorectal cancer by downregulation of miR-182 and MMP-9 expression [112]. In addition, the antitumor effects of morphine are associated with a reduction in the level of MMP-9 [113]. Both lidocaine and ropivacaine inhibited TNFα-induced invasion of lung adenocarcinoma cells in vitro by blocking MMP-9 expression [114]. Based on the limited data, further investigation is needed to clarify the effects of anesthetics and analgesics on MMP-9 expression in PC (Table 1 and Figure 1).
3.3.2. Clinical Studies
Wang et al. reported that MMP-9 in the propofol group was significantly lower than in the sevoflurane group in lung cancer patients who received surgery [109]. In breast cancer patients, Kashefi et al. reported that novel NSAIDs may reduce MMP-2 and MMP-9 expression, which promotes angiogenesis and metastasis [115]. In summary, propofol may reduce MMP-9 expression in PC. Based on the limited data, further investigation is required to determine the effects of anesthetics and analgesics on MMP-9 expression in PC (Table 1 and Figure 1).
3.4. Inflammation, and the Immune System
Inflammation, apoptosis, and autophagy can provide cellular defense, and impairments of these processes (rendering them deficient or overactivated) lead to pathological effects. Inflammation induces secretion of various cytokines and chemokines, and recruits various immune cells in reaction to oxidative stress or infection sites. Reflexively, enhancement of reactive oxygen species (ROS)-generation via inflammatory immune cells provokes oxidative stress and tissue injury. In addition, chronic inflammation not only produces high numbers of inflammatory mediators but also gives rise to oxidative stress [116]. Inflammatory processes have emerged as key elements in PC development and progression [117,118]. The relationship of chronic inflammation and cancer, as revealed in the pioneering work of Rudolf Virchow, has been observed for more than 150 years, especially in PC progression [118]. However, even in malignancy without preceding inflammation, cancer-induced inflammation, secretions of inflammatory factors, and immune cell infiltration are main characters in tumor initiation and advanced metastasis [118]. Anesthesia and analgesia may impact cellular immunity and inflammation during surgery, and thus affect cancer outcomes [119,120,121,122,123,124,125].
3.4.1. Laboratory Studies
A recent laboratory study has shown that propofol enhances anti-inflammatory reactions and stimulatory effects on immune responses, which may be a potential benefit in the prevention of tumor recurrence. However, clinical evidence of the tumor suppression effects is inconclusive. [126]. Opioids influence the nervous system indirectly, as well as release biological amines that potentially impair innate immunity by suppressing natural killer (NK) cell cytotoxicity. [127]. However, a mu-opioid receptor (MOR) partial agonist, buprenorphine, intercepted the inhibition of NK cell cytotoxicity and progression caused by surgery in a rat mammary adenocarcinoma cell line [128]. Additionally, neoplasm is related to inflammation, and anti-inflammatory properties are identified in LAs. LAs may be able to reduce metastasis risk, but the molecular mechanism is not fully understood. [129]. With regard to NSAIDs, aspirin was associated with a decreased expression of markers for progression, inflammation, and desmoplasia in PC cell lines [82]. NSAIDs also reduced inflammation and induced apoptosis in rat osteosarcoma cells in vitro [130]. Thus, NSAIDs may attenuate inflammation in PC. Further laboratory research is necessary (see extant research in Table 1 and Figure 1).
3.4.2. Clinical Studies
The surgical treatment of PC is complicated by the prolonged nature of the surgery, the magnitude of the surgical stress, inflammatory response, immunosuppression, anesthesia-/epidural-induced hypotension, and blood loss, all of which cause oxidative stress [92,131]. In a retrospective study based on clinical pathological analysis, Huang et al. showed that the survival probability was reduced in patients with TNM stage III to IV, lymph node metastasis, higher CD4+IL-17+ level, and lower CD8+ expression, which implied that the tumor immune microenvironment may affect the outcome of PC [132]. Recently, Li et al. reported that high systemic immune-inflammation index levels were regarded as negative with regard to PC overall survival and cancer-specific survival [133]. Yamaguchi et al. demonstrated that propofol reduced the number of CD8+ T cells, whereas sevoflurane augmented the percentage of regulatory T cells in lung-cancer surgery patients [121]. Sevoflurane was revealed to devastate multiple pulmonary functions by releasing a series of inflammatory secretions in lung cancer patients undergoing perioperative one-lung ventilation [134]. However, another clinical study reported that sevoflurane inhibited pulmonary inflammatory cytokines [135]. Propofol combined with epidural anesthesia and epidural analgesia demonstrated less interference with the immune system (compared to propofol with intravenous analgesia) and led to fast recovery in patients undergoing radical resection of pulmonary carcinoma [125]. However, in a clinical study, Fant et al. reported that thoracic epidural analgesia with bupivacaine inhibits the neurohormonal but not the acute inflammatory stress response after radical retropubic prostatectomy [136]. Based on the published data, further investigation is required to determine the effects of anesthetics and analgesics on inflammation and cellular immunity in PC progression (Table 1 and Figure 1).
3.5. Apoptosis
Apoptosis, also known as programmed cell death, is an important mechanism in maintaining the stability of the tissue environment. It is activated by various vital signal transduction cascades [137]. Recent studies reported that autophagy and apoptosis are key mechanisms to fight PC [137,138].
3.5.1. Laboratory Studies
Evidence has shown that anesthesia may affect apoptosis [75,76,86,87,139,140,141,142,143]. Wang et al. reported that propofol inhibited migration, induced apoptosis of PC cells, and inhibited cell migration in PC cells in vitro by promoting miR-34a-dependent LOC 285194 and E-cadherin upregulation [75]. Propofol also induced apoptosis and increased gemcitabine sensitivity in PC cells via the nuclear factor-κB signaling pathway [76]. Wei et al. reported that isoflurane suppressed proliferation and increased apoptosis and autophagy by activating the AMPK/mTOR pathway in cervical carcinoma, both in vitro and in vivo [139]. In contrast, promotion of bladder tumor cell proliferation, invasion, and migration was reported to be induced by isoflurane instead of apoptosis inhibition [141]. Sevoflurane can suppress colon cancer cell proliferation and invasion, provoke apoptosis and autophagy, and regulate EMT, actions that may result from the sevoflurane-induced inhibition of the ERK signaling pathway [140]. Celik et al. showed that fentanyl prescription reduced the numbers of tumor cells and tumor stem cells, diminished the stem cell gene expression of markers, and enhanced apoptosis-related gene expression in PC cells [86]. However, the fact that opioids increased PC cell death was not entirely due to alterations in apoptotic or necrotic pathways [142]. Bundscherer et al. showed that ropivacaine, bupivacaine, and sufentanil did not change the PC apoptosis rate and cell cycle distribution in clinical concentration [87]. Lin et al. showed that aspirin inhibited the proliferation and promoted the apoptosis of PC cells [143]. In summary, propofol and NSAIDs may induce apoptosis. However, VAs, opioids, and LAs may induce uncertain effects on apoptosis in PC. Based on the published laboratory data, further investigation is required to determine the effects of anesthetics and analgesics on apoptosis and progression in PC.
3.5.2. Clinical Studies
To the best of our knowledge, clinical research on anesthetics/analgesics and apoptosis in PC progression is still lacking; further research is needed.
3.6. Autophagy
Autophagy occurs in response to various stresses, inducing a series of intracellular degradation processes that involve presentations of organelle damage, abnormal protein expression, and nutrient deprivation [144]. PC cells respond to metabolic stress, nutrient starvation, hypoxia, and chemotherapy with the aid of autophagy. Consequently, autophagy repression may impede PC tumorigenesis [117]. In addition, inflammation and autophagy dysregulation are prevailing features of pancreatitis and PC [117]. Recently, Luo et al. reported that tendencies in PC toward invasion and resistance to standardized therapy derive from the obstruction of autophagy and apoptosis [137]. Therefore, it can be concluded that autophagy exerts biphasic effects on PC inhibition and facilitation [117,144].
3.6.1. Laboratory Studies
Tumor cells depend on autophagy for tumor survival to a greater degree than normal cells, relying on it for their fast growth rate, for metabolic alteration, and to adapt to nutrient deprivation [145]. Autophagy enables cancer cells to respond to changes in nutrition supply by degenerating and recycling non-essential intracellular contents. Restriction of autophagy coupled with nutrient deprivation is an effective therapeutic strategy for cancer [146]. In addition, autophagy may improve cancer cell growth and survival in an unfavorable environment, such as that induced by the administration of cytostatic drugs; however, autophagy also constitutes an alternative mode of cell death [147]. Wang et al. reported that autophagy inhibitors combined with chemotherapeutic drugs showed promising results in PC treatments. Thus, autophagy may play a vital role in inhibiting PC progression [148].
Recent research shows that anesthesia may affect autophagy [140,149,150,151,152,153,154]. Wang et al. reported that propofol inhibited the proliferation, apoptosis, and cell cycle of HCC by inducing autophagy in vivo and in vitro [149]. Chen et al. showed that propofol exerted antitumor effects in cervical carcinoma cells by promoting autophagosome accumulation via inhibition of autophagy flux [150]. By contrast, sevoflurane-induced apoptosis and autophagy inhibited the proliferation and invasion of colon cancer cells [140]. Jiang et al. demonstrated that sufentanil impaired autophagic degradation and inhibited cell migration in lung cancer cells in vitro [151]. However, fentanyl induced autophagy via activation of the ROS/MAPK pathway, and reduced the sensitivity of cisplatin in lung cancer cells [152]. Izdebska et al. reported that lidocaine induced protective autophagy and cell cycle arrest in rat glioma cell lines [147]. Ropivacaine and ropivacaine-loaded liposomes impaired autophagy and suppressed cancer growth in B16 mouse melanoma lines and human cervical cancer cell lines [146]. Aspirin inhibited mTOR signaling, activated AMPK, and induced autophagy in colorectal cancer cells [153]. Palumbo et al. also reported that COX-2 inhibitor induced autophagy and reduced growth rate in human glioblastoma cell lines [154]. Laboratory research on the effects of anesthetics and analgesics on PC autophagy is lacking. Further investigation is required and encouraged.
3.6.2. Clinical Studies
Until now, clinical research on the effects of anesthetics/analgesics on PC autophagy is lacking. Further investigation is needed.
3.7. Oxidative Stress
Oxidative damage is induced through the excessive production and accumulation of free radicals, such as ROS, in mitochondria, leading to the impairment of lipids, proteins, and DNA [155]. Furthermore, fatty-acid peroxidation is influenced by oxidative stress, accompanied by mutagenic metabolites [155]. In addition, ROS and pro-inflammatory cytokines are considered to be important factors in the pathogenesis of PC [156]. Oxidative stress is involved in aging, inflammation, cancer, degenerative diseases, and can be induced by exposure to xenobiotics and drugs, such as anesthetics [131,157]. With the accumulation of evidence indicating a correlation between increased oxidative stress and worse postoperative outcomes, it is very important to choose anesthetics that minimize oxidative stress [131,157]. Anesthesiologists may improve clinical outcomes and reduce postoperative complications by selecting anesthetics that reduce perioperative oxidative stress.
3.7.1. Laboratory Studies
Zhang et al. demonstrated that propofol reduced oxidative stress in the human neuroblastoma cell line [158]. With regard to VAs, Wei et al. showed that oxidative stress was triggered by isoflurane, which elevated ROS levels and lowered the ratio of NAD+/NADH and ATP levels in cervical cancer cells [139]. In addition, there have been some indications in animal studies that sevoflurane may be neurotoxic in the developing brain, in part due to increased oxidative stress [159,160,161]. Regarding opioids, Almeida et al. stated that oxidative stress was ameliorated in glioma cell lines following treatment with therapeutic concentrations of morphine [162]. In contrast, Zhang et al. showed that morphine induced activation of the AMPK pathway and magnified oxidative stress in esophageal tumor cells [57]. Lv et al. demonstrated that ropivacaine alleviated high-glucose-induced brain microvascular endothelial injury through the downregulation of MMPs and the attenuation of oxidative stress [163]. In breast cancer cells, aspirin-modified metabolites were involved in suppressing lipogenesis, oxidative stress, and neoplastic formation [164]. On the other hand, Kacprzak and Pawliczak reported that aspirin induced oxidative stress in cells, a condition also supported by the inflammatory milieu [165]. In summary, propofol, VAs, opioids, LAs, and NSAIDs may induce uncertain effects on oxidative stress in different cancer processes. In the literature, laboratory research on anesthesia in relation to oxidative stress in PC progression is still limited, and further investigation is needed.
3.7.2. Clinical Studies
In clinical practice, propofol has been proven to have antioxidant capability, and this amelioration of oxidative stress correlates with its enhancement of postoperative prognoses and its association with faster recovery, which is why it is regarded as an ideal anesthetic [157,166]. Ucar et al. reported no significant plasma malondialdehyde changes in 29 liver donors with the use of propofol anesthesia before and after surgery [167]. However, isoflurane and sevoflurane have no influence on oxidative stress, inflammation, and DNA damage in patients undergoing minor surgeries [116]. Purdy et al. reported that the rectus sheath block with levobupivacaine did not significantly affect oxidative stress [168]. To the best of our knowledge, the relationship between anesthesia and oxidative stress on PC progress is still unclear, and further investigation is required.
4. The Effects of Anesthetics on PC Progression: From Laboratory to Clinical Studies
4.1. Laboratory Studies
4.1.1. Propofol and PC Progression
Several laboratory studies revealed that propofol inhibited PC progression via different pathways [73,74,75,76,77,78,79,80,81]. Chen et al. reported that propofol attenuated PC malignant potential via the inhibition of NMDA receptors [73]. Wang et al. showed that propofol inhibited migration and induced apoptosis of PC cells through miR-34a-mediated E-cadherin and LOC285194 signals [75]. In addition, an in vitro experiment by Du et al. demonstrated that propofol suppressed nuclear factor-κB activity and consequently resulted in apoptosis and augmentation of gemcitabine sensitivity in PC cells [76]. Propofol also suppressed PC proliferation and metastasis by means of miR-328 upregulation and ADAM8 downregulation. [77] Following induction of ADAM8 downregulation, propofol inhibited PC proliferation and migration [74]. Furthermore, propofol repressed ADAM8 both in a hypoxic environment and via SP1 to reduce PC progression. [78,79]. In addition, Wang et al. revealed that propofol depressed PC proliferation and invasion by microRNA-133a upregulation [80]. Liu et al. reported that propofol reduced PC growth and invasion via miR-21/Slug signaling regulation [81]. (Table 1, Figure 1 and Figure 2).
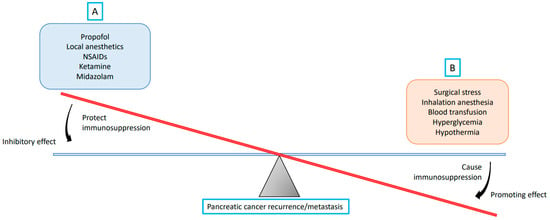
Figure 2.
A theory on the balance between recurrence/metastasis-promoting and -inhibiting factors during pancreatic cancer surgery. The strength of the promoting effect relies on the extent of the pancreatic cancer surgery, and the strength of the inhibitory effect originates in the inhibiting factors selected. (A) Propofol, local anesthetics, non-steroidal anti-inflammatory drugs (NSAIDs), ketamine, and midazolam reduce pancreatic cancer recurrence/metastasis by protecting against immunosuppression; (B) Surgical stress, inhalation anesthesia, blood transfusion, hyperglycemia, and hypothermia promote pancreatic cancer recurrence/metastasis by causing immunosuppression.
4.1.2. VAs and PC Progression
To the best of our knowledge, there is no laboratory study on the relationship between VAs and PC progression, and further research is needed.
4.1.3. Opioids and PC Progression
4.1.4. LAs and PC Progression
4.1.5. NSAIDs and PC Progression
Indometacin ameliorates high-glucose-induced proliferation and invasion by upregulating E-cadherin (EMT) in PC cells [25]. Aspirin counteracts PC stem cell features, desmoplasia, and gemcitabine resistance [82]. In preclinical models of PC, Zhang et al. showed that COX-2 inhibition potentiated the efficacy of VEGF blockade and promoted an immune-stimulatory microenvironment [83]. Perugini et al. demonstrated that sodium salicylate inhibited proliferation and induced G1 cell cycle arrest in human PC cell lines [84]. Indometacin inhibited the proliferation and activation of human pancreatic stellate cells through the downregulation of COX-2 [85] (Table 1, Figure 1 and Figure 2).
4.1.6. Midazolam and PC Progression
The antitumorigenic effects of midazolam are partly related to the peripheral benzodiazepine receptor [169]. Midazolam inhibited cell migrations of human lung carcinoma and neuroglioma, possessed properties of apoptotic induction through the intrinsic mitochondrial pathway, potentially caused mitochondrial membrane decrement, and led to improvement in ROS expression in vitro, which might be attributed to peripheral benzodiazepine receptor activation [169]. In addition, midazolam significantly suppressed proliferation of lung carcinoma in xenograft mice [169]. Oshima et al. reported that midazolam conferred antitumorigenic effects against PC neoplastic growth and achieved local infiltration of tumor-associated neutrophils, macrophages, and polymorphonuclear myeloid-derived suppressor cells [88] (Table 1, Figure 1 and Figure 2).
4.1.7. Ketamine and PC Progression
4.1.8. Tramadol and PC Progression
In a recent study, the antitumor effects of tramadol appeared to involve inhibition of proliferation, induction of apoptosis, and effects on 5-HT2B receptors and TRPV-1 in breast cancer cells [170]. In a xenograft mouse model, Kim et al. showed that a clinical dose of tramadol had antitumor effects on MCF-7-cell-derived breast cancer [171]. In addition, tramadol may regulate EMT and exert cytotoxic effects in breast cancer cells [172]. However, literature on tramadol in PC progression is lacking, and further laboratory studies are required.
4.1.9. Dexmedetomidine (DEX) and PC Progression
In gastrointestinal cancers, DEX promoted the progression of hepatocellular carcinoma through hepatic stellate cell activation [173], but DEX suppressed growth and metastasis while facilitating the apoptosis of esophageal cancer cells by upregulating the abundance of miR-143-3p and reducing the level of EPS8 in vivo and in vitro [174]. To date, laboratory research on DEX in PC progression is lacking, and further investigation is necessary.
4.2. Clinical Studies
Recent clinical studies reported that anesthesia may affect cancer outcomes [11,70,175,176]. Data also showed that anesthesia may inhibit PC proliferation and metastasis. Here, we review the clinical effects of anesthetics on PC progression.
4.2.1. Propofol and PC Progression
In a retrospective propensity score matched cohort, Soliz et al. showed that propofol anesthesia involved risk of low-grade (grade 1 or 2) complications, but carried risk of recurrence, metastasis, or mortality, compared with desflurane anesthesia in PC surgery [10]. Our recent study showed that propofol anesthesia was correlated with enhanced survival (hazard ratio (HR), 0.65; 95% confidence interval (CI), 0.42–0.99; P = 0.047) in the matched analysis by comparison with desflurane anesthesia. The subgroup analyses also revealed significant improvement in cancer-specific survival (HR, 0.63; 95% CI, 0.40–0.97; P = 0.037) in PC patients undergoing propofol anesthesia. Additionally, fewer postoperative recurrences were noticed in the propofol group than in the desflurane group (HR, 0.55; 95% CI, 0.34–0.90; P = 0.028) in the matched analysis [11]. In summary, propofol may inhibit PC progression. Further prospective studies are needed to confirm the effects of propofol on PC progression (Table 1, Figure 1 and Figure 2).
4.2.2. VAs and PC Progression
As mentioned above, desflurane was inferior to propofol anesthesia on patient outcomes after PC surgery [10,11]. The few available studies suggest that VAs may be associated with worse PC progression compared with propofol anesthesia. Further studies are needed to confirm the effects of VAs on PC progression (Table 1, Figure 1 and Figure 2).
4.2.3. Opioids and PC Progression
Steele et al. reported that high opioid use was associated with decreased survival (adjusted HR = 2.76; 95% CI: 1.39–5.48) in newly diagnosed stage IV PC [66]. Abdel-Rahman et al. also reported that opioid use was associated with worse overall survival (HR, 1.245; 95% CI, 1.063–1.459; P = 0.007) in patients with PC [67]. Call et al. showed that intraoperative opioid use was not associated with decreased survival in PC surgery [68]. Paradoxically, Zylberberg et al. reported that opioid prescription was associated with increased survival in older adult patients with PC; this might be due to the impact of cancer-related pain [69]. Accordingly, opioids may induce uncertain effects in PC progression. Further investigation is required to determine the effects of opioids on PC progression (Table 1, Figure 1 and Figure 2).
4.2.4. LAs and PC Progression
Cata et al. reported that lidocaine showed a major stimulatory activity on the function of NK cells, and concluded that perioperative lidocaine may diminish the effects of surgery by increasing the cytolytic activity of NK cells [71]. Zhang et al. investigated that significantly higher rates of 1-year and 3-year survival were found in the lidocaine group than in the non-lidocaine group (68.0% vs. 62.6%, P < 0.001; 34.1% vs. 27.2%, P = 0.011). The multivariable analysis showed that intraoperative administration of lidocaine improved overall survival (HR = 0.616; 95% CI, 0.290–0.783; P = 0.013) in patients undergoing pancreatectomy [12]. A clinical study reported that peridural anesthesia with ropivacaine may improve the oncological outcome of PC patients [72]. Chen et al. also reported that intraoperative epidural infusion with a high concentration of ropivacaine was associated with improved overall survival in PC patients undergoing pancreatectomy [70]. However, Lin et al. also showed no significant associations between epidural analgesia with bupivacaine and cancer recurrence and overall survival after curative surgery for PC [177]. Accordingly, LAs in epidural anesthesia (but not analgesia) as well as intravenous lidocaine infusion may induce positive effects on PC progression (Table 1, Figure 1 and Figure 2).
4.2.5. NSAIDs and PC Progression
A meta-analysis study of the research conducted from 2002 to 2017 revealed no significant association between aspirin use and mortality risk in PC [63]. In addition, Risch et al. reported that aspirin use reduced the risk of PC [64]. Recently, Pretzsch et al. demonstrated that aspirin intake proved to be independently associated with improved overall survival, disease-free survival, and hematogenous metastasis-free survival in PC surgery [65]. Accordingly, it can be theorized that NSAIDs may induce positive effects on PC progression. Further investigation is required to verify the effects of different kinds and dosages of NSAIDs on PC progression (Table 1, Figure 1 and Figure 2).
4.2.6. Midazolam and PC Progression
4.2.7. Ketamine and PC Progression
There are no clinical studies in the literature regarding the relationship between ketamine and PC progression.
4.2.8. Tramadol and PC Progression
Clinicians may prescribe tramadol for pain management in PC patients [178]. Tramadol promotes or preserves immunity, including NK cell activity, which is important in anticancer defenses [179]. Patients who received tramadol had a decreased risk of postoperative recurrence and mortality following breast cancer surgery [170]. However, the literature on tramadol use in PC is lacking, and further investigation is required to verify its effects on PC progression.
4.2.9. Dexmedetomidine (DEX) and PC Progression
DEX infusion may negatively affect lung cancer surgery outcome [180]. However, DEX may not affect survival in the context of cytoreductive surgery with hyperthermic intraperitoneal chemotherapy for peritoneal carcinomatosis [181]. DEX may induce uncertain effects in the progression of different cancers. The clinical data regarding the effects of DEX on PC are limited.
5. Perioperative Anesthesia Management
5.1. Enhanced Recovery after Surgery
Agarwal et al. reported that higher compliance with enhanced recovery after surgery (ERAS) protocols significantly reduces the occurrence of major complications, mortality, and postoperative hospital stays in pancreatic cancer resections [182]. Therefore, the implementation of depth of anesthesia monitoring (such as bispectral index), goal-directed fluid therapy with invasive hemodynamic monitoring (such as cardiac output or stroke volume variation), and postoperative nausea and vomiting prophylaxis with propofol use, in accordance with the recommendations of ERAS, were suggested for improving postoperative outcomes [183,184,185]. Using multimodal analgesia with lidocaine infusion, regional nerve blockade, ketamine, and NSAIDs to reduce intraoperative and postoperative opioid consumption is also suggested [183].
5.2. Blood Transfusion
Perioperative blood transfusion is common in pancreatic surgery. A meta-analysis study reported that patients receiving perioperative blood transfusion had significantly lower 5-year survival after PC surgery [186]. In addition, Kim et al. showed that intraoperative blood transfusion could be considered an independent prognostic factor in resected PC [187]. However, a recent systematic review revealed a weak association between perioperative blood transfusion in patients undergoing pancreatectomy for PC and worsened survival [188]. Accordingly, it can be stated that a perioperative blood transfusion may induce negative effects on PC progression (Figure 2).
5.3. Body Temperature
To the best of our knowledge, the effects of temperature on the PC outcome have not been studied. However, hypothermia has long been considered to correlate with major adverse outcomes in different pathophysiological conditions, such as inflammation and cancer. Therefore, active warming should be applied intraoperatively to maintain the patient’s temperature above 36 °C (Figure 2) [183].
5.4. Glucose Control
Despite the fact that the importance of the optimal glycemic target during the perioperative period is still controversial, blood glucose levels should be maintained as close as possible to the normal range for patient safety [183]. Perioperative hyperglycemia may increase the risk of surgical site infections in general surgery patients [189]. Perioperative prevention of insulin resistance and hypoglycemia is also recommended [183]. Therefore, we believe that controlled fasting and the maintenance of perioperative blood glucose levels may affect the outcome of PC [183].
5.5. Obesity
Recently, Zorbas et al. showed that obesity was significantly associated with higher risk of postoperative complications and mortality in patients with body mass index ≥ 40 after pancreatoduodenectomy [38]. Obesity-associated adipose tissue inflammation may play a central role in the development of PC and the promotion of PC growth [32]. Thus, anesthetics with the effect of inhibiting obesity-induced inflammation may improve postoperative outcomes [35]. VAs, ketamine, opioids, propofol, and regional anesthesia may modulate parts of the immune system in patients with obesity [36]. However, there are no studies on the relationship between anesthetics and obesity-induced inflammation in PC progression. Further investigation is necessary.
6. Conclusions
PC is a lethal malignancy associated with high mortality, a statistic related to late diagnosis, surgical resection complications, and a shortage of effective therapies. Surgery remains a key component in long-term PC survival. During surgery, anesthesia may alter the tumor microenvironment and even affect cancer progression. Herein, we endeavored to summarize the role of anesthesia in the PC microenvironment and in PC progression. The scarce evidence currently available suggests that propofol, NASIDS, midazolam, ketamine, and LAs may have a positive impact. While the effects of propofol, NASIDS, and LAs have been examined in PC patients, findings regarding midazolam and ketamine are based on cell or animal data, and have not yet been validated in humans. As yet, very little evidence exists to recommend specific anesthetics or analgesic techniques for PC surgery for optimal risk-reduction with regard to tumor recurrence or metastasis. Therefore, additional in-depth research and clinical trials are necessary to explore the molecular mechanisms involved in the relationship between anesthesia and PC microenvironments and progression.
Author Contributions
Conceptualization, H.-C.L. and Z.-F.W.; methodology, Y.-W.K.; software, Y.-W.K.; validation, Y.-H.H., S.-M.C. and K.-I.C.; formal analysis, Y.-H.H. and S.-M.C.; investigation, H.-C.L.; resources, Z.-F.W.; data curation, Y.-H.H. and S.-M.C.; writing—original draft preparation, H.-C.L.; writing—review and editing, Z.-F.W.; visualization, K.-I.C.; supervision, Z.-F.W.; project administration, H.-C.L.; funding acquisition, none. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no competing interest.
References
- Mizrahi, J.D.; Surana, R.; Valle, J.W.; Shroff, R.T. Pancreatic cancer. Lancet 2020, 395, 2008–2020. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2018. CA Cancer. J. Clin. 2018, 68, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Kleeff, J.; Korc, M.; Apte, M.; La Vecchia, C.; Johnson, C.D.; Biankin, A.V.; Neale, R.E.; Tempero, M.; Tuveson, D.A.; Hruban, R.H.; et al. Pancreatic cancer. Nat. Rev. Dis. Prime. 2016, 2, 16022. [Google Scholar] [CrossRef] [PubMed]
- Deplanque, G.; Demartines, N. Pancreatic cancer: Are more chemotherapy and surgery needed? Lancet 2017, 389, 985–986. [Google Scholar] [CrossRef]
- Ryan, D.P.; Hong, T.S.; Bardeesy, N. Pancreatic adenocarcinoma. N. Engl. J. Med. 2014, 371, 1039–1049. [Google Scholar] [CrossRef]
- Vincent, A.; Herman, J.; Schulick, R.; Hruban, R.H.; Goggins, M. Pancreatic cancer. Lancet 2011, 378, 607–620. [Google Scholar] [CrossRef]
- Ho, W.J.; Jaffee, E.M.; Zheng, L. The tumour microenvironment in pancreatic cancer—Clinical challenges and opportunities. Nat. Rev. Clin. Oncol. 2020, 17, 527–540. [Google Scholar] [CrossRef]
- Ramirez, M.F.; Gorur, A.; Cata, J.P. Opioids and cancer prognosis: A summary of the clinical evidence. Neurosci. Lett. 2021, 746, 135661. [Google Scholar] [CrossRef]
- Tat, T.; Jurj, A.; Selicean, C.; Pasca, S.; Ionescu, D. Antiproliferative effects of propofol and lidocaine on the colon adenocarcinoma microenvironment. J. Buon 2019, 24, 106–115. [Google Scholar]
- Soliz, J.M.; Ifeanyi, I.C.; Katz, M.H.; Wilks, J.; Cata, J.P.; McHugh, T.; Fleming, J.B.; Feng, L.; Rahlfs, T.; Bruno, M.; et al. Comparing postoperative complications and inflammatory markers using total intravenous anesthesia versus volatile gas anesthesia for pancreatic cancer surgery. Anesthesiol. Pain Med. 2017, 7, e13879. [Google Scholar] [CrossRef]
- Lai, H.C.; Lee, M.S.; Liu, Y.T.; Lin, K.T.; Hung, K.C.; Chen, J.Y.; Wu, Z.F. Propofol-based intravenous anesthesia is associated with better survival than desflurane anesthesia in pancreatic cancer surgery. PLoS ONE 2020, 15, e0233598. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Yang, L.; Zhu, X.; Zhu, M.; Sun, Z.; Cata, J.P.; Chen, W.; Miao, C. Association between intraoperative intravenous lidocaine infusion and survival in patients undergoing pancreatectomy for pancreatic cancer: A retrospective study. Br. J. Anaesth. 2020, 125, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Zhang, L.; Chen, X.; Jiang, Z.; Zong, L.; Ma, Q. Hyperglycemia promotes the epithelial-mesenchymal transition of pancreatic cancer via hydrogen peroxide. Oxid. Med. Cell Longev. 2016, 2016, 5190314. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Ma, J.; Han, L.; Xu, Q.; Lei, J.; Duan, W.; Li, W.; Wang, F.; Wu, E.; Ma, Q.; et al. Hyperglycemic tumor microenvironment induces perineural invasion in pancreatic cancer. Cancer Biol. Ther. 2015, 16, 912–921. [Google Scholar] [CrossRef]
- Li, Y.; Bian, X.; Wei, S.; He, M.; Yang, Y. The relationship between pancreatic cancer and type 2 diabetes: Cause and consequence. Cancer Manag. Res. 2019, 11, 8257–8268. [Google Scholar] [CrossRef]
- Otto, L.; Rahn, S.; Daunke, T.; Walter, F.; Winter, E.; Möller, J.L.; Rose-John, S.; Wesch, D.; Schäfer, H.; Sebens, S. Initiation of pancreatic cancer: The interplay of hyperglycemia and macrophages promotes the acquisition of malignancy-associated properties in pancreatic ductal epithelial cells. Int. J. Mol. Sci. 2021, 22, 5086. [Google Scholar] [CrossRef]
- Helm, O.; Held-Feindt, J.; Grage-Griebenow, E.; Reiling, N.; Ungefroren, H.; Vogel, I.; Krüger, U.; Becker, T.; Ebsen, M.; Röcken, C.; et al. Tumor-associated macrophages exhibit pro- and anti-inflammatory properties by which they impact on pancreatic tumorigenesis. Int. J. Cancer. 2014, 135, 843–861. [Google Scholar] [CrossRef]
- Helm, O.; Mennrich, R.; Petrick, D.; Goebel, L.; Freitag-Wolf, S.; Röder, C.; Kalthoff, H.; Röcken, C.; Sipos, B.; Kabelitz, D.; et al. Comparative characterization of stroma cells and ductal epithelium in chronic pancreatitis and pancreatic ductal adenocarcinoma. PLoS ONE 2014, 9, e94357. [Google Scholar] [CrossRef]
- Li, W.; Liu, H.; Qian, W.; Cheng, L.; Yan, B.; Han, L.; Xu, Q.; Ma, Q.; Ma, J. Hyperglycemia aggravates microenvironment hypoxia and promotes the metastatic ability of pancreatic cancer. Comput. Struct. Biotechnol. J. 2018, 16, 479–487. [Google Scholar] [CrossRef]
- Cheng, L.; Qin, T.; Ma, J.; Duan, W.; Xu, Q.; Li, X.; Han, L.; Li, W.; Wang, Z.; Zhang, D.; et al. Hypoxia-inducible factor-1α mediates hyperglycemia-induced pancreatic cancer glycolysis. Anticancer Agents Med. Chem. 2019, 19, 1503–1512. [Google Scholar] [CrossRef]
- Zhou, C.; Qian, W.; Li, J.; Ma, J.; Chen, X.; Jiang, Z.; Cheng, L.; Duan, W.; Wang, Z.; Wu, Z.; et al. High glucose microenvironment accelerates tumor growth via SREBP1-autophagy axis in pancreatic cancer. J. Exp. Clin. Cancer Res. 2019, 38, 302. [Google Scholar] [CrossRef] [PubMed]
- Guo, N.L.; Zhang, J.X.; Wu, J.P.; Xu, Y.H. Isoflurane promotes glucose metabolism through up-regulation of miR-21 and suppresses mitochondrial oxidative phosphorylation in ovarian cancer cells. Biosci. Rep. 2017, 37, BSR20170818. [Google Scholar] [CrossRef] [PubMed]
- Dong, W.; Zhang, D.; Zhu, A.; Hu, Y.; Li, W. High concentration of Dezocine induces immune escape of lung cancer and promotes glucose metabolism through up-regulating PD-L1 and activating NF-κB pathway. Curr. Mol. Med. 2021; Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Codd, E.E.; Baker, J.; Brandt, M.R.; Bryant, S.; Cai, C.; Carson, J.R.; Chevalier, K.M.; Colburn, R.W.; Coogan, T.P.; Dax, S.L.; et al. Diabetogenic effect of a series of tricyclic delta opioid agonists structurally related to cyproheptadine. Toxicol. Sci. 2010, 117, 493–504. [Google Scholar] [CrossRef]
- Han, L.; Peng, B.; Ma, Q.; Ma, J.; Li, J.; Li, W.; Duan, W.; Chen, C.; Liu, J.; Xu, Q.; et al. Indometacin ameliorates high glucose-induced proliferation and invasion via modulation of e-cadherin in pancreatic cancer cells. Curr. Med. Chem. 2013, 20, 4142–4152. [Google Scholar] [CrossRef] [PubMed]
- Khadka, R.; Tian, W.; Hao, X.; Koirala, R. Risk factor, early diagnosis and overall survival on outcome of association between pancreatic cancer and diabetes mellitus: Changes and advances, a review. Int. J. Surg. 2018, 52, 342–346. [Google Scholar] [CrossRef]
- Sandini, M.; Strobel, O.; Hank, T.; Lewosinska, M.; Nießen, A.; Hackert, T.; Büchler, M.W.; Schimmack, S. Pre-operative dysglycemia is associated with decreased survival in patients with pancreatic neuroendocrine neoplasms. Surgery 2020, 167, 575–580. [Google Scholar] [CrossRef]
- Conti, C.; Pamoukdjian, F.; Aparicio, T.; Mebarki, S.; Poisson, J.; Manceau, G.; Taieb, J.; Rance, B.; Katsahian, S.; Charles-Nelson, A.; et al. Overall survival and prognostic factors among older patients with metastatic pancreatic cancer: A retrospective analysis using a hospital database. Cancers 2022, 14, 1105. [Google Scholar] [CrossRef]
- Wang, X.; Xu, W.; Hu, X.; Yang, X.; Zhang, M. The prognostic role of glycemia in patients with pancreatic carcinoma: A systematic review and meta-analysis. Front. Oncol. 2022, 12, 780909. [Google Scholar] [CrossRef]
- Liu, J.; Yang, L. Effects of propofol and sevoflurane on blood glucose, hemodynamics, and inflammatory factors of patients with type 2 diabetes mellitus and gastric cancer. Oncol. Lett. 2020, 19, 1187–1194. [Google Scholar] [CrossRef]
- Lattermann, R.; Carli, F.; Wykes, L.; Schricker, T. Epidural blockade modifies perioperative glucose production without affecting protein catabolism. Anesthesiology 2002, 97, 374–381. [Google Scholar] [CrossRef] [PubMed]
- Eibl, G.; Rozengurt, E. Obesity and pancreatic cancer: Insight into mechanisms. Cancers 2021, 13, 5067. [Google Scholar] [CrossRef] [PubMed]
- Zhou, B.; Wu, D.; Liu, H.; Du, L.T.; Wang, Y.S.; Xu, J.W.; Qiu, F.B.; Hu, S.Y.; Zhan, H.X. Obesity and pancreatic cancer: An update of epidemiological evidence and molecular mechanisms. Pancreatology 2019, 19, 941–950. [Google Scholar] [CrossRef] [PubMed]
- Iyengar, N.M.; Gucalp, A.; Dannenberg, A.J.; Hudis, C.A. Obesity and cancer mechanisms: Tumor microenvironment and inflammation. J. Clin. Oncol. 2016, 34, 4270–4276. [Google Scholar] [CrossRef]
- Heil, L.B.B.; Silva, P.L.; Pelosi, P.; Rocco, P.R.M. Immunomodulatory effects of anesthetics in obese patients. World J. Crit. Care Med. 2017, 6, 140–152. [Google Scholar] [CrossRef]
- Eley, V.A.; Thuzar, M.; Navarro, S.; Dodd, B.R.; van Zundert, A.A. Obesity, metabolic syndrome, and inflammation: An update for anaesthetists caring for patients with obesity. Anaesth. Crit. Care Pain Med. 2021, 40, 100947. [Google Scholar] [CrossRef]
- Incio, J.; Liu, H.; Suboj, P.; Chin, S.M.; Chen, I.X.; Pinter, M.; Ng, M.R.; Nia, H.T.; Grahovac, J.; Kao, S.; et al. Obesity-induced inflammation and desmoplasia promote pancreatic cancer progression and resistance to chemotherapy. Cancer Discov. 2016, 6, 852–869. [Google Scholar] [CrossRef]
- Zorbas, K.; Wu, J.; Reddy, S.; Esnaola, N.; Karachristos, A. Obesity affects outcomes of pancreatoduodenectomy. Pancreatology 2021, 21, 824–832. [Google Scholar] [CrossRef]
- Li, J.; Li, J.Y.; Wu, Z.; Peng, X. Reduced antioxidant and anti-inflammatory effects of propofol at high-dose on morbidly obese patients. Pak. J. Pharm. Sci. 2021, 34, 561–565. [Google Scholar]
- Babaei, G.; Aziz, S.G.; Jaghi, N.Z.Z. EMT, cancer stem cells and autophagy; The three main axes of metastasis. Biomed. Pharmacother. 2021, 133, 110909. [Google Scholar] [CrossRef]
- Brown, M.S.; Muller, K.E.; Pattabiraman, D.R. Quantifying the epithelial-to-mesenchymal transition (EMT) from bench to bedside. Cancers 2022, 14, 1138. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, A.J.; Marengo, M.S.; Oltean, S.; Kemeny, G.; Bitting, R.L.; Turnbull, J.D.; Herold, C.I.; Marcom, P.K.; George, D.J.; Garcia-Blanco, M.A. Circulating tumor cells from patients with advanced prostate and breast cancer display both epithelial and mesenchymal markers. Mol. Cancer Res. 2011, 9, 997–1007. [Google Scholar] [CrossRef] [PubMed]
- Markiewicz, A.; Topa, J.; Nagel, A.; Skokowski, J.; Seroczynska, B.; Stokowy, T.; Welnicka-Jaskiewicz, M.; Zaczek, A.J. Spectrum of Epithelial-Mesenchymal Transition Phenotypes in Circulating Tumour Cells from Early Breast Cancer Patients. Cancers 2019, 11, 59. [Google Scholar] [CrossRef] [PubMed]
- Ren, J.; Wang, X.; Wei, G.; Meng, Y. Exposure to desflurane anesthesia confers colorectal cancer cells metastatic capacity through deregulation of miR-34a/LOXL3. Eur. J. Cancer Prev. 2021, 30, 143–153. [Google Scholar] [CrossRef]
- Guo, R.; Lu, X.; Xu, G.; Luo, S. Propofol suppresses hypoxia-induced esophageal cancer cell migration, invasion, and EMT through regulating lncRNA TMPO-AS1/miR-498 axis. Thorac. Cancer 2020, 11, 2398–2405. [Google Scholar] [CrossRef]
- Sun, H.; Wang, Y.; Zhang, W. Propofol inhibits proliferation and metastasis by up-regulation of miR-495 in JEG-3 choriocarcinoma cells. Artif. Cells Nanomed. Biotechnol. 2019, 47, 1738–1745. [Google Scholar] [CrossRef]
- Du, Q.; Zhang, X.; Zhang, X.; Wei, M.; Xu, H.; Wang, S. Propofol inhibits proliferation and epithelial-mesenchymal transition of MCF-7 cells by suppressing miR-21 expression. Artif. Cells Nanomed. Biotechnol. 2019, 47, 1265–1271. [Google Scholar] [CrossRef]
- Li, Y.; Zeng, Q.G.; Qiu, J.L.; Pang, T.; Wang, H.; Zhang, X.X. Propofol suppresses migration, invasion, and epithelial-mesenchymal transition in papillary thyroid carcinoma cells by regulating miR-122 expression. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 5101–5110. [Google Scholar]
- Liu, W.Z.; Liu, N. Propofol inhibits lung cancer A549 Cell growth and epithelial-mesenchymal transition process by upregulation of microRNA-1284. Oncol. Res. 2018, 27, 1–8. [Google Scholar] [CrossRef]
- Liu, F.; Qiu, F.; Fu, M.; Chen, H.; Wang, H. Propofol reduces epithelial to mesenchymal transition, invasion and migration of gastric cancer cells through the microRNA-195-5p/Snail axis. Med. Sci. Monit. 2020, 26, e920981. [Google Scholar] [CrossRef]
- Liu, Y.; Wang, X.; Li, H.; Guan, E.; Luo, K. Propofol ameliorates the proliferation and epithelial-mesenchymal transition of hepatoma carcinoma cells via non-coding RNA activated by DNA damage (NORAD)/microRNA (miR)-556-3p/migration and invasion enhancer 1 (MIEN1) axis. J. Environ. Pathol. Toxicol. Oncol. 2021, 40, 87–97. [Google Scholar] [CrossRef]
- Shi, H.; Yan, C.; Chen, Y.; Wang, Z.; Guo, J.; Pei, H. Propofol inhibits the proliferation, migration, invasion and epithelial to mesenchymal transition of renal cell carcinoma cells by regulating microRNA-363/Snail1. Am. J. Transl. Res. 2021, 13, 2256–2269. [Google Scholar] [PubMed]
- Qian, J.; Shen, S.; Chen, W.; Chen, N. Propofol reversed hypoxia-induced docetaxel resistance in prostate cancer cells by preventing epithelial-mesenchymal transition by inhibiting hypoxia-inducible factor 1α. Biomed. Res. Int. 2018, 2018, 4174232. [Google Scholar] [CrossRef] [PubMed]
- Cao, C.; Zhang, X.; Xu, Y. Propofol prevents the aggressive progression of oral squamous cell carcinoma via regulating circ_0005623/miR-195-5p/HOXB7 axis. Biotechnol. Appl. Biochem. 2021; Epub ahead of print. [Google Scholar] [CrossRef]
- Tripolt, S.; Neubauer, H.A.; Knab, V.M.; Elmer, D.P.; Aberger, F.; Moriggl, R.; Fux, D.A. Opioids drive breast cancer metastasis through the δ-opioid receptor and oncogenic STAT3. Neoplasia 2021, 23, 270–279. [Google Scholar] [CrossRef] [PubMed]
- Lennon, F.E.; Mirzapoiazova, T.; Mambetsariev, B.; Poroyko, V.A.; Salgia, R.; Moss, J.; Singleton, P.A. The Mu opioid receptor promotes opioid and growth factor-induced proliferation, migration and epithelial mesenchymal transition (EMT) in human lung cancer. PLoS ONE 2014, 9, e91577. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Yao, N.; Tian, S. Morphine stimulates migration and growth and alleviates the effects of chemo drugs via AMPK-dependent induction of epithelial-mesenchymal transition in esophageal carcinoma cells. Biol. Pharm. Bull. 2020, 43, 774–781. [Google Scholar] [CrossRef]
- Tang, H.; Li, C.; Wang, Y.; Deng, L. Sufentanil inhibits the proliferation and metastasis of esophageal cancer by inhibiting the NF-κB and snail signaling Pathways. J. Oncol. 2021, 2021, 7586100. [Google Scholar] [CrossRef]
- Liu, C.; Yu, M.; Li, Y.; Wang, H.; Xu, C.; Zhang, X.; Li, M.; Guo, H.; Ma, D.; Guo, X. Lidocaine inhibits the metastatic potential of ovarian cancer by blocking NaV 1.5-mediated EMT and FAK/Paxillin signaling pathway. Cancer Med. 2021, 10, 337–349. [Google Scholar] [CrossRef]
- Chan, S.M.; Lin, B.F.; Wong, C.S.; Chuang, W.T.; Chou, Y.T.; Wu, Z.F. Levobuipivacaine-induced dissemination of A549 lung cancer cells. Sci. Rep. 2017, 7, 8646. [Google Scholar] [CrossRef]
- Santoro, A.; Bufo, P.; Russo, G.; Cagiano, S.; Papagerakis, S.; Bucci, P.; Aquino, G.; Longo, F.; Feola, A.; Giordano, A.; et al. Expression and clinical implication of cyclooxygenase-2 and E-cadherin in oral squamous cell carcinomas. Cancer Biol Ther. 2020, 21, 667–674. [Google Scholar] [CrossRef] [PubMed]
- Zheng, X.; Carstens, J.L.; Kim, J.; Scheible, M.; Kaye, J.; Sugimoto, H.; Wu, C.C.; LeBleu, V.S.; Kalluri, R. Epithelial-to-mesenchymal transition is dispensable for metastasis but induces chemoresistance in pancreatic cancer. Nature 2015, 527, 525–530. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Li, Y.; Liu, L.; Jiang, Z.; Liu, G. Aspirin use and pancreatic cancer risk: A systematic review of observational studies. Medicine 2019, 98, e18033. [Google Scholar] [CrossRef] [PubMed]
- Risch, H.A.; Lu, L.; Streicher, S.A.; Wang, J.; Zhang, W.; Ni, Q.; Kidd, M.S.; Yu, H.; Gao, Y.T. Aspirin use and reduced risk of pancreatic cancer. Cancer Epidemiol. Biomark. Prev. 2017, 26, 68–74. [Google Scholar] [CrossRef]
- Pretzsch, E.; D’Haese, J.G.; Renz, B.; Ilmer, M.; Schiergens, T.; Miksch, R.C.; Albertsmeier, M.; Guba, M.; Angele, M.K.; Werner, J.; et al. Effect of platelet inhibition with perioperative aspirin on survival in patients undergoing curative resection for pancreatic cancer: A propensity score matched analysis. BMC Surg. 2021, 21, 98. [Google Scholar] [CrossRef]
- Steele, G.L.; Dudek, A.Z.; Gilmore, G.E.; Richter, S.A.; Olson, D.A.; Eklund, J.P.; Zylla, D.M. Impact of pain, opioids, and the mu-opioid receptor on progression and survival in patients with newly diagnosed stage IV pancreatic cancer. Am. J. Clin. Oncol. 2020, 43, 591–597. [Google Scholar] [CrossRef]
- Abdel-Rahman, O.; Karachiwala, H.; Easaw, J.C. Outcomes of patients with advanced gastrointestinal cancer in relationship to opioid use: Findings from eight clinical trials. J. Natl. Compr. Cancer Netw. 2020, 18, 575–581. [Google Scholar] [CrossRef]
- Call, T.R.; Pace, N.L.; Thorup, D.B.; Maxfield, D.; Chortkoff, B.; Christensen, J.; Mulvihill, S.J. Factors associated with improved survival after resection of pancreatic adenocarcinoma: A multivariable model. Anesthesiology 2015, 122, 317–324. [Google Scholar] [CrossRef]
- Zylberberg, H.M.; Woodrell, C.; Rustgi, S.D.; Aronson, A.; Kessel, E.; Amin, S.; Lucas, A.L. Opioid prescription is associated with increased survival in older adult patients with pancreatic cancer in the United States: A propensity score analysis. JCO Oncol. Pract. 2022, 18, e659–e668. [Google Scholar] [CrossRef]
- Chen, W.; Xu, Y.; Zhang, Y.; Lou, W.; Han, X. Positive impact of intraoperative epidural ropivacaine infusion on oncologic outcomes in pancreatic cancer patients undergoing pancreatectomy: A retrospective cohort study. J. Cancer 2021, 12, 4513–4521. [Google Scholar] [CrossRef]
- Cata, J.P.; Ramirez, M.F.; Velasquez, J.F.; Di, A.I.; Popat, K.U.; Gottumukkala, V.; Black, D.M.; Lewis, V.O.; Vauthey, J.N. Lidocaine stimulates the function of natural killer cells in different experimental settings. Anticancer Res. 2017, 37, 4727–4732. [Google Scholar] [PubMed]
- Alexander, A.; Lehwald-Tywuschik, N.; Rehders, A.; Rabenalt, S.; Verde, P.E.; Eisenberger, C.F.; Picker, N.; Knoefel, W.T.; Kienbaum, P. Peridural anesthesia and cancer-related survival after surgery for pancreatic cancer-A retrospective cohort study. Clin. Pract. 2021, 11, 532–542. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Wu, Q.; You, L.; Chen, S.; Zhu, M.; Miao, C. Propofol attenuates pancreatic cancer malignant potential via inhibition of NMDA receptor. Eur. J. Pharmacol. 2017, 795, 150–159. [Google Scholar] [CrossRef] [PubMed]
- Yu, X.; Shi, J.; Wang, X.; Zhang, F. Propofol affects the growth and metastasis of pancreatic cancer via ADAM8. Pharmacol. Rep. 2020, 72, 418–426. [Google Scholar] [CrossRef]
- Wang, H.; Jiao, H.; Jiang, Z.; Chen, R. Propofol inhibits migration and induces apoptosis of pancreatic cancer PANC-1 cells through miR-34a-mediated E-cadherin and LOC285194 signals. Bioengineered 2020, 11, 510–521. [Google Scholar] [CrossRef]
- Du, Q.H.; Xu, Y.B.; Zhang, M.Y.; Yun, P.; He, C.Y. Propofol induces apoptosis and increases gemcitabine sensitivity in pancreatic cancer cells in vitro by inhibition of nuclear factor-κB activity. World J. Gastroenterol. 2013, 19, 5485–5492. [Google Scholar] [CrossRef]
- Yu, X.; Gao, Y.; Zhang, F. Propofol inhibits pancreatic cancer proliferation and metastasis by up-regulating miR-328 and down-regulating ADAM8. Basic Clin. Pharmacol. Toxicol. 2019, 125, 271–278. [Google Scholar] [CrossRef]
- Gao, Y.; Yu, X.; Zhang, F.; Dai, J. Propofol inhibits pancreatic cancer progress under hypoxia via ADAM8. J. Hepatobiliary Pancreat Sci. 2019, 26, 219–226. [Google Scholar] [CrossRef]
- Gao, Y.; Zhou, Y.; Wang, C.; Sample, K.M.; Yu, X.; Ben-David, Y. Propofol mediates pancreatic cancer cell activity through the repression of ADAM8 via SP1. Oncol. Rep. 2021, 46, 249. [Google Scholar] [CrossRef]
- Wang, Z.T.; Gong, H.Y.; Zheng, F.; Liu, D.J.; Dong, T.L. Propofol suppresses proliferation and invasion of pancreatic cancer cells by upregulating microRNA-133a expression. Genet. Mol. Res. 2015, 14, 7529–7537. [Google Scholar] [CrossRef]
- Liu, Z.; Zhang, J.; Hong, G.; Quan, J.; Zhang, L.; Yu, M. Propofol inhibits growth and invasion of pancreatic cancer cells through regulation of the miR-21/Slug signaling pathway. Am. J. Transl. Res. 2016, 8, 4120–4133. [Google Scholar] [PubMed]
- Zhang, Y.; Liu, L.; Fan, P.; Bauer, N.; Gladkich, J.; Ryschich, E.; Bazhin, A.V.; Giese, N.A.; Strobel, O.; Hackert, T.; et al. Aspirin counteracts cancer stem cell features, desmoplasia and gemcitabine resistance in pancreatic cancer. Oncotarget 2015, 6, 9999–10015. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Kirane, A.; Huang, H.; Sorrelle, N.B.; Burrows, F.J.; Dellinger, M.T.; Brekken, R.A. Cyclooxygenase-2 inhibition potentiates the efficacy of vascular endothelial growth factor blockade and promotes an immune stimulatory microenvironment in preclinical models of pancreatic cancer. Mol. Cancer Res. 2019, 17, 348–355. [Google Scholar] [CrossRef] [PubMed]
- Perugini, R.A.; McDade, T.P.; Vittimberga, F.J., Jr.; Duffy, A.J.; Callery, M.P. Sodium salicylate inhibits proliferation and induces G1 cell cycle arrest in human pancreatic cancer cell lines. J. Gastrointest. Surg. 2000, 4, 24–32. [Google Scholar] [CrossRef]
- Sun, L.; Chen, K.; Jiang, Z.; Chen, X.; Ma, J.; Ma, Q.; Duan, W. Indometacin inhibits the proliferation and activation of human pancreatic stellate cells through the downregulation of COX-2. Oncol. Rep. 2018, 39, 2243–2251. [Google Scholar] [CrossRef] [PubMed]
- Celik, F.; Duran, T. Effects of fentanyl on pancreatic cancer cell proliferation and cancer stem cell differentiation. Cell Mol. Biol. 2019, 65, 21–25. [Google Scholar] [CrossRef]
- Bundscherer, A.; Malsy, M.; Gebhardt, K.; Metterlein, T.; Plank, C.; Wiese, C.H.; Gruber, M.; Graf, B.M. Effects of ropivacaine, bupivacaine and sufentanil in colon and pancreatic cancer cells in vitro. Pharmacol. Res. 2015, 95, 126–131. [Google Scholar] [CrossRef]
- Oshima, Y.; Sano, M.; Kajiwara, I.; Ichimaru, Y.; Itaya, T.; Kuramochi, T.; Hayashi, E.; Kim, J.; Kitajima, O.; Masugi, Y.; et al. Midazolam exhibits antitumour and anti-inflammatory effects in a mouse model of pancreatic ductal adenocarcinoma. Br. J. Anaesth. 2022, 128, 679–690. [Google Scholar] [CrossRef]
- Malsy, M.; Graf, B.; Bundscherer, A. The effects of analgesics and local anesthetics on gene transcription mediated by NFATc2 and Sp1 in pancreatic carcinoma. Anticancer Res. 2019, 39, 4721–4728. [Google Scholar] [CrossRef]
- Malsy, M.; Gebhardt, K.; Gruber, M.; Wiese, C.; Graf, B.; Bundscherer, A. Effects of ketamine, s-ketamine, and MK 801 on proliferation, apoptosis, and necrosis in pancreatic cancer cells. BMC Anesthesiol. 2015, 15, 111. [Google Scholar] [CrossRef]
- Jin, X.; Dai, L.; Ma, Y.; Wang, J.; Liu, Z. Implications of HIF-1α in the tumorigenesis and progression of pancreatic cancer. Cancer Cell Int. 2020, 20, 273. [Google Scholar] [CrossRef] [PubMed]
- Kim, R. Effects of surgery and anesthetic choice on immunosuppression and cancer recurrence. J. Transl. Med. 2018, 16, 8. [Google Scholar] [CrossRef] [PubMed]
- Benzonana, L.L.; Perry, N.J.; Watts, H.R.; Yang, B.; Perry, I.A.; Coombes, C.; Takata, M.; Ma, D. Isoflurane, a commonly used volatile anesthetic, enhances renal cancer growth and malignant potential via the hypoxia-inducible factor cellular signaling pathway in vitro. Anesthesiology 2013, 119, 593–605. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, M.; Iwasaki, M.; Zhao, H.; Saito, J.; Hu, C.; Sun, Q.; Sakamoto, A.; Ma, D. Inhalational anesthetics inhibit neuroglioma cell proliferation and migration via miR-138, -210 and -335. Int. J. Mol. Sci. 2021, 22, 4355. [Google Scholar] [CrossRef] [PubMed]
- Schoos, A.; Gabriel, C.; Knab, V.M.; Fux, D.A. Activation of HIF-1α by δ-opioid receptors induces COX-2 expression in breast cancer cells and leads to paracrine activation of vascular endothelial cells. J. Pharmacol. Exp. Ther. 2019, 370, 480–489. [Google Scholar] [CrossRef]
- Koodie, L.; Ramakrishnan, S.; Roy, S. Morphine suppresses tumor angiogenesis through a HIF-1alpha/p38MAPK pathway. Am. J. Pathol. 2010, 177, 984–997. [Google Scholar] [CrossRef]
- Okamoto, A.; Sumi, C.; Tanaka, H.; Kusunoki, M.; Iwai, T.; Nishi, K.; Matsuo, Y.; Harada, H.; Takenaga, K.; Bono, H.; et al. HIF-1-mediated suppression of mitochondria electron transport chain function confers resistance to lidocaine-induced cell death. Sci. Rep. 2017, 7, 3816. [Google Scholar] [CrossRef]
- Zhou, Y.; Dong, X.; Xiu, P.; Wang, X.; Yang, J.; Li, L.; Li, Z.; Sun, P.; Shi, X.; Zhong, J. Meloxicam, a selective COX-2 inhibitor, mediates hypoxia-inducible factor- (HIF-) 1α signaling in hepatocellular carcinoma. Oxid. Med. Cell Longev. 2020, 2020, 7079308. [Google Scholar] [CrossRef]
- Yue, H.; Liu, L.; Song, Z. miR-212 regulated by HIF-1α promotes the progression of pancreatic cancer. Exp. Ther. Med. 2019, 17, 2359–2365. [Google Scholar] [CrossRef]
- Qu, D.; Zou, X.; Liu, Z. Propofol modulates glycolysis reprogramming of ovarian tumor via restraining circular RNA-zinc finger RNA-binding protein/microRNA-212-5p/superoxide dismutase 2 axis. Bioengineered 2022, 13, 11881–11892. [Google Scholar] [CrossRef]
- Si, J.; Jin, Y.; Cui, M.; Yao, Q.; Li, R.; Li, X. Neuroprotective effect of miR-212-5p on isoflurane-induced cognitive dysfunction by inhibiting neuroinflammation. Toxicol. Mech. Methods 2021, 31, 501–506. [Google Scholar] [CrossRef] [PubMed]
- He, X.; Yang, Y.; Zhi, F.; Moore, M.L.; Kang, X.; Chao, D.; Wang, R.; Balboni, G.; Salvadori, S.; Kim, D.H.; et al. δ-Opioid receptor activation modified microRNA expression in the rat kidney under prolonged hypoxia. PLoS ONE 2013, 8, e61080. [Google Scholar] [CrossRef] [PubMed]
- Raji, S.; Sahranavard, M.; Mottaghi, M.; Sahebkar, A. MiR-212 value in prognosis and diagnosis of cancer and its association with patient characteristics: A systematic review and meta-analysis. Cancer Cell Int. 2022, 22, 163. [Google Scholar] [CrossRef] [PubMed]
- Xie, J.; Zhou, X.; Wang, R.; Zhao, J.; Tang, J.; Zhang, Q.; Du, Y.; Pang, Y. Identification of potential diagnostic biomarkers in MMPs for pancreatic carcinoma. Medicine 2021, 100, e26135. [Google Scholar] [CrossRef]
- Bramhall, S.R.; Neoptolemos, J.P.; Stamp, G.W.; Lemoine, N.R. Imbalance of expression of matrix metalloproteinases (MMPs) and tissue inhibitors of the matrix metalloproteinases (TIMPs) in human pancreatic carcinoma. J. Pathol. 1997, 182, 347–355. [Google Scholar] [CrossRef]
- Jones, L.E.; Humphreys, M.J.; Campbell, F.; Neoptolemos, J.P.; Boyd, M.T. Comprehensive analysis of matrix metalloproteinase and tissue inhibitor expression in pancreatic cancer: Increased expression of matrix metalloproteinase-7 predicts poor survival. Clin. Cancer Res. 2004, 10, 2832–2845. [Google Scholar] [CrossRef] [PubMed]
- Matsuyama, Y.; Takao, S.; Aikou, T. Comparison of matrix metalloproteinase expression between primary tumors with or without liver metastasis in pancreatic and colorectal carcinomas. J. Surg. Oncol. 2002, 80, 105–110. [Google Scholar] [CrossRef]
- Mondal, S.; Adhikari, N.; Banerjee, S.; Amin, S.A.; Jha, T. Matrix metalloproteinase-9 (MMP-9) and its inhibitors in cancer: A minireview. Eur. J. Med. Chem. 2020, 194, 112260. [Google Scholar] [CrossRef]
- Wang, G.; Liu, J.; Gao, J.; Zheng, X. Comparison of the effects of sevoflurane and propofol anesthesia on pulmonary function, MMP-9 and postoperative cognition in patients receiving lung cancer resection. Oncol. Lett. 2019, 17, 3399–3405. [Google Scholar] [CrossRef]
- Müller-Edenborn, B.; Roth-Zʼgraggen, B.; Bartnicka, K.; Borgeat, A.; Hoos, A.; Borsig, L.; Beck-Schimmer, B. Volatile anesthetics reduce invasion of colorectal cancer cells through down-regulation of matrix metalloproteinase-9. Anesthesiology 2012, 117, 293–301. [Google Scholar] [CrossRef]
- Cao, Y.; Lv, W.; Ding, W.; Li, J. Sevoflurane inhibits the proliferation and invasion of hepatocellular carcinoma cells through regulating the PTEN/Akt/GSK-3β/β-catenin signaling pathway by downregulating miR-25-3p. Int. J. Mol. Med. 2020, 46, 97–106. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.L.; Chen, M.L.; Zhou, S.L. Fentanyl inhibits proliferation and invasion of colorectal cancer via β-catenin. Int. J. Clin. Exp. Pathol. 2015, 8, 227–235. [Google Scholar] [PubMed]
- Afsharimani, B.; Baran, J.; Watanabe, S.; Lindner, D.; Cabot, P.J.; Parat, M.O. Morphine and breast tumor metastasis: The role of matrix-degrading enzymes. Clin. Exp. Metastasis 2014, 31, 149–158. [Google Scholar] [CrossRef] [PubMed]
- Piegeler, T.; Schläpfer, M.; Dull, R.O.; Schwartz, D.E.; Borgeat, A.; Minshall, R.D.; Beck-Schimmer, B. Clinically relevant concentrations of lidocaine and ropivacaine inhibit TNFα-induced invasion of lung adenocarcinoma cells in vitro by blocking the activation of Akt and focal adhesion kinase. Br. J. Anaesth. 2015, 115, 784–791. [Google Scholar] [CrossRef] [PubMed]
- Kashefi, S.; Ahmadi, H.; Omranipour, R.; Mahmoodzadeh, H.; Jafarnezhad-Ansariha, F.; Tofighi Zavareh, F.; Mirshafiey, A. The anti-tumoral effect of β-D-mannuronic acid (M2000) as a novel NSAID on Treg cells frequency and MMP-2, MMP-9, CCL22 and TGFβ1 gene expression in pre-surgical breast cancer patients. Iran. J. Allergy Asthma Immunol. 2019, 18, 80–90. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.M.; Song, B.C.; Yeum, K.J. Impact of volatile anesthetics on oxidative stress and inflammation. Biomed. Res. Int. 2015, 2015, 242709. [Google Scholar] [CrossRef] [PubMed]
- Gukovsky, I.; Li, N.; Todoric, J.; Gukovskaya, A.; Karin, M. Inflammation, autophagy, and obesity: Common features in the pathogenesis of pancreatitis and pancreatic cancer. Gastroenterology 2013, 144, 1199–1209. [Google Scholar] [CrossRef]
- Shadhu, K.; Xi, C. Inflammation and pancreatic cancer: An updated review. Saudi J. Gastroenterol. 2019, 25, 3–13. [Google Scholar] [CrossRef]
- Wall, T.; Sherwin, A.; Ma, D.; Buggy, D.J. Influence of perioperative anaesthetic and analgesic interventions on oncological outcomes: A narrative review. Br. J. Anaesth. 2019, 123, 135–150. [Google Scholar] [CrossRef]
- Ackerman, R.S.; Luddy, K.A.; Icard, B.E.; Piñeiro Fernández, J.; Gatenby, R.A.; Muncey, A.R. The effects of anesthetics and perioperative medications on immune function: A narrative review. Anesth. Analg. 2021, 133, 676–689. [Google Scholar] [CrossRef]
- Yamaguchi, A.; Kawagoe, I.; Inoue, S.; Kochiyama, T.; Fukuda, M.; Saito, M.; Hayashida, M. Propofol decreases CD8+ T cells and sevoflurane increases regulatory T cells after lung cancer resection: A randomized controlled trial. J. Thorac. Dis. 2021, 13, 5430–5438. [Google Scholar] [CrossRef] [PubMed]
- Zhu, R.; Xiang, J.; Tan, M. Effects of different anesthesia and analgesia on cellular immunity and cognitive function of patients after surgery for esophageal cancer. Minerva Chir. 2020, 75, 449–456. [Google Scholar] [CrossRef] [PubMed]
- Zhou, M.; Liu, W.; Peng, J.; Wang, Y. Impact of propofol epidural anesthesia on immune function and inflammatory factors in patients undergoing gastric cancer surgery. Am. J. Transl. Res. 2021, 13, 3064–3073. [Google Scholar] [PubMed]
- Xu, Q.; Shi, N.J.; Zhang, H.; Zhu, Y.M. Effects of combined general-epidural anesthesia and total intravenous anesthesia on cellular immunity and prognosis in patients with non-small cell lung cancer: A comparative study. Mol. Med. Rep. 2017, 16, 4445–4454. [Google Scholar] [CrossRef]
- Chen, J.; Luo, F.; Lei, M.; Chen, Z. A study on cellular immune function of patients treated with radical resection of pulmonary carcinoma with two different methods of anesthesia and analgesia. J. Buon 2017, 22, 1416–1421. [Google Scholar] [PubMed]
- Jiang, S.; Liu, Y.; Huang, L.; Zhang, F.; Kang, R. Effects of propofol on cancer development and chemotherapy: Potential mechanisms. Eur. J. Pharmacol. 2018, 831, 46–51. [Google Scholar] [CrossRef]
- Boland, J.W.; Pockley, A.G. Influence of opioids on immune function in patients with cancer pain: From bench to bedside. Br. J. Pharmacol. 2018, 175, 2726–2736. [Google Scholar] [CrossRef]
- Franchi, S.; Panerai, A.E.; Sacerdote, P. Buprenorphine ameliorates the effect of surgery on hypothalamus-pituitary-adrenal axis, natural killer cell activity and metastatic colonization in rats in comparison with morphine or fentanyl treatment. Brain Behav. Immun. 2007, 21, 767–774. [Google Scholar] [CrossRef]
- Votta-Velis, E.G.; Piegeler, T.; Minshall, R.D.; Aguirre, J.; Beck-Schimmer, B.; Schwartz, D.E.; Borgeat, A. Regional anaesthesia and cancer metastases: The implication of local anaesthetics. Acta Anaesthesiol. Scand. 2013, 57, 1211–1229. [Google Scholar] [CrossRef]
- Zuckerman, L.M.; Frames, W.L.; Elsissy, J.G.; Shields, T.G.; de Necochea-Campion, R.; Mirshahidi, H.R.; Williams, N.L.; Mirshahidi, S. The effect of non-steroidal anti-inflammatory drugs on osteosarcoma cells. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 2681–2690. [Google Scholar]
- Kundović, S.A.; Rašić, D.; Popović, L.; Peraica, M.; Črnjar, K. Oxidative stress under general intravenous and inhalation anaesthesia. Arh. Hig. Rada Toksikol. 2020, 71, 169–177. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.; Sun, J.; Li, Z.; Zhang, X.; Li, Z.; Zhu, H.; Yu, X. Impact of the tumor immune microenvironment on the outcome of pancreatic cancer: A retrospective study based on clinical pathological analysis. Gland Surg. 2022, 11, 472–482. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Lin, H.; Ouyang, R.; Yang, Y.; Peng, J. Prognostic significance of the systemic immune-inflammation index in pancreatic carcinoma patients: A meta-analysis. Biosci. Rep. 2021, 41, BSR20204401. [Google Scholar] [CrossRef] [PubMed]
- Jin, Y.; Zhao, X.; Li, H.; Wang, Z.; Wang, D. Effects of sevoflurane and propofol on the inflammatory response and pulmonary function of perioperative patients with one-lung ventilation. Exp. Ther. Med. 2013, 6, 781–785. [Google Scholar] [CrossRef] [PubMed]
- Schilling, T.; Kozian, A.; Senturk, M.; Huth, C.; Reinhold, A.; Hedenstierna, G.; Hachenberg, T. Effects of volatile and intravenous anesthesia on the alveolar and systemic inflammatory response in thoracic surgical patients. Anesthesiology 2011, 115, 65–74. [Google Scholar] [CrossRef]
- Fant, F.; Tina, E.; Sandblom, D.; Andersson, S.O.; Magnuson, A.; Hultgren-Hörnkvist, E.; Axelsson, K.; Gupta, A. Thoracic epidural analgesia inhibits the neuro-hormonal but not the acute inflammatory stress response after radical retropubic prostatectomy. Br. J. Anaesth. 2013, 110, 747–757. [Google Scholar] [CrossRef]
- Luo, W.; Zheng, L.; Zhang, T.T. Novel therapeutic strategies and perspectives for pancreatic cancer: Autophagy and apoptosis are key mechanisms to fight pancreatic cancer. Med. Oncol. 2021, 38, 74. [Google Scholar] [CrossRef]
- Pfeifer, E.; Burchell, J.M.; Dazzi, F.; Sarker, D.; Beatson, R. Apoptosis in the pancreatic cancer tumor microenvironment-the double-edged sword of cancer-associated fibroblasts. Cells 2021, 10, 1653. [Google Scholar] [CrossRef]
- Wei, H.; Sun, T.; Liu, J.; Wang, X.; Zhao, G.; Shi, J.; Chen, Y. Isoflurane activates AMP-activated protein kinase to inhibit proliferation, and promote apoptosis and autophagy in cervical carcinoma both in vitro and in vivo. J. Recept. Signal Transduct Res. 2021, 41, 538–545. [Google Scholar] [CrossRef]
- Yang, X.; Zheng, Y.T.; Rong, W. Sevoflurane induces apoptosis and inhibits the growth and motility of colon cancer in vitro and in vivo via inactivating Ras/Raf/MEK/ERK signaling. Life Sci. 2019, 239, 116916. [Google Scholar] [CrossRef]
- Lu, N.; Piao, M.H.; Feng, C.S.; Yuan, Y. Isoflurane promotes epithelial-to-mesenchymal transition and metastasis of bladder cancer cells through HIF-1α-β-catenin/Notch1 pathways. Life Sci. 2020, 258, 118154. [Google Scholar] [CrossRef] [PubMed]
- Zagon, I.S.; McLaughlin, P.J. Opioids and the apoptotic pathway in human cancer cells. Neuropeptides 2003, 37, 79–88. [Google Scholar] [CrossRef]
- Lin, S.; Pan, Y.; Xu, C. Effects of aspirin on pancreatic cancer cells PANC-1 and its potential molecular mechanism. J. Buon 2020, 25, 2449–2455. [Google Scholar] [PubMed]
- Yun, C.W.; Lee, S.H. The roles of autophagy in cancer. Int. J. Mol. Sci. 2018, 19, 3466. [Google Scholar] [CrossRef] [PubMed]
- Mowers, E.E.; Sharifi, M.N.; Macleod, K.F. Functions of autophagy in the tumor microenvironment and cancer metastasis. FEBS J. 2018, 285, 1751–1766. [Google Scholar] [CrossRef]
- Zhang, J.; Zhu, S.; Tan, Q.; Cheng, D.; Dai, Q.; Yang, Z.; Zhang, L.; Li, F.; Zuo, Y.; Dai, W.; et al. Combination therapy with ropivacaine-loaded liposomes and nutrient deprivation for simultaneous cancer therapy and cancer pain relief. Theranostics 2020, 10, 4885–4899. [Google Scholar] [CrossRef]
- Izdebska, M.; Hałas-Wiśniewska, M.; Zielińska, W.; Klimaszewska-Wiśniewska, A.; Grzanka, D.; Gagat, M. Lidocaine induces protective autophagy in rat C6 glioma cell line. Int. J. Oncol. 2019, 54, 1099–1111. [Google Scholar] [CrossRef]
- Wang, Y.; Qin, C.; Yang, G.; Zhao, B.; Wang, W. The role of autophagy in pancreatic cancer progression. Biochim. Biophys Acta Rev. Cancer 2021, 1876, 188592. [Google Scholar] [CrossRef]
- Wang, Y.; Xu, B.; Zhou, J.; Wu, X. Propofol activates AMPK to inhibit the growth of HepG2 cells in vitro and hepatocarcinogenesis in xenograft mouse tumor models by inducing autophagy. J. Gastrointest. Oncol. 2020, 11, 1322–1332. [Google Scholar] [CrossRef]
- Chen, X.; Li, K.; Zhao, G. Propofol inhibits HeLa cells by impairing autophagic flux via AMP-activated protein kinase (AMPK) activation and endoplasmic reticulum stress regulated by calcium. Med. Sci. Monit. 2018, 24, 2339–2349. [Google Scholar] [CrossRef]
- Jiang, H.; Wang, H.; Zou, W.; Hu, Y.; Chen, C.; Wang, C. Sufentanil impairs autophagic degradation and inhibits cell migration in NCI-H460 in vitro. Oncol. Lett. 2019, 18, 6829–6835. [Google Scholar] [CrossRef] [PubMed]
- Yao, J.; Ma, C.; Gao, W.; Liang, J.; Liu, C.; Yang, H.; Yan, Q.; Wen, Q. Fentanyl induces autophagy via activation of the ROS/MAPK pathway and reduces the sensitivity of cisplatin in lung cancer cells. Oncol. Rep. 2016, 36, 3363–3370. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Din, F.V.; Valanciute, A.; Houde, V.P.; Zibrova, D.; Green, K.A.; Sakamoto, K.; Alessi, D.R.; Dunlop, M.G. Aspirin inhibits mTOR signaling, activates AMP-activated protein kinase, and induces autophagy in colorectal cancer cells. Gastroenterology 2012, 142, 1504–1515.e3. [Google Scholar] [CrossRef] [PubMed]
- Palumbo, P.; Lombardi, F.; Augello, F.R.; Giusti, I.; Dolo, V.; Leocata, P.; Cifone, M.G.; Cinque, B. Biological effects of selective COX-2 inhibitor NS398 on human glioblastoma cell lines. Cancer Cell Int. 2020, 20, 167. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Useros, J.; Li, W.; Cabeza-Morales, M.; Garcia-Foncillas, J. Oxidative Stress: A new target for pancreatic cancer prognosis and treatment. J. Clin. Med. 2017, 6, 29. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.H.; Kim, H. Oxidative stress and cytokines in the pathogenesis of pancreatic cancer. J. Cancer Prev. 2014, 19, 97–102. [Google Scholar] [CrossRef]
- Senoner, T.; Velik-Salchner, C.; Luckner, G.; Tauber, H. Anesthesia-induced oxidative stress: Are there differences between intravenous and inhaled anesthetics? Oxid. Med. Cell Longev. 2021, 2021, 8782387. [Google Scholar] [CrossRef]
- Zhang, Y.; Zuo, Y.; Li, B.; Xie, J.; Ma, Z.; Thirupathi, A.; Yu, P.; Gao, G.; Shi, M.; Zhou, C.; et al. Propofol prevents oxidative stress and apoptosis by regulating iron homeostasis and targeting JAK/STAT3 signaling in SH-SY5Y cells. Brain Res. Bull. 2019, 153, 191–201. [Google Scholar] [CrossRef]
- Sanchez, V.; Feinstein, S.D.; Lunardi, N.; Joksovic, P.M.; Boscolo, A.; Todorovic, S.M.; Jevtovic-Todorovic, V. General anesthesia causes long-term impairment of mitochondrial morphogenesis and synaptic transmission in developing rat brain. Anesthesiology 2011, 115, 992–1002. [Google Scholar] [CrossRef]
- Jevtovic-Todorovic, V.; Hartman, R.E.; Izumi, Y.; Benshoff, N.D.; Dikranian, K.; Zorumski, C.F.; Olney, J.W.; Wozniak, D.F. Early exposure to common anesthetic agents causes widespread neurodegeneration in the developing rat brain and persistent learning deficits. J. Neurosci. 2003, 23, 876–882. [Google Scholar] [CrossRef]
- Jevtovic-Todorovic, V.; Absalom, A.R.; Blomgren, K.; Brambrink, A.; Crosby, G.; Culley, D.J.; Fiskum, G.; Giffard, R.G.; Herold, K.F.; Loepke, A.W.; et al. Anaesthetic neurotoxicity and neuroplasticity: An expert group report and statement based on the BJA Salzburg Seminar. Br. J. Anaesth. 2013, 111, 143–151. [Google Scholar] [CrossRef] [PubMed]
- Almeida, M.B.; Costa-Malaquias, A.; Nascimento, J.L.; Oliveira, K.R.; Herculano, A.M.; Crespo-López, M.E. Therapeutic concentration of morphine reduces oxidative stress in glioma cell line. Braz J. Med. Biol Res. 2014, 47, 398–402. [Google Scholar] [CrossRef] [PubMed]
- Lv, H.; Cheng, Q.; Li, Y.; Zhang, Y.; Chen, J.; Chen, W. The Protective effects of ropivacaine against high glucose-induced brain microvascular endothelial injury by reducing MMPs and alleviating oxidative stress. Neurotox. Res. 2021, 39, 851–859. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, C.C.; Chiu, H.H.; Wang, C.H.; Kuo, C.H. Aspirin modifies inflammatory mediators and metabolomic profiles and contributes to the suppression of obesity-associated breast cancer cell growth. Int. J. Mol. Sci. 2020, 21, 4652. [Google Scholar] [CrossRef] [PubMed]
- Kacprzak, D.; Pawliczak, R. Does aspirin-induced oxidative stress cause asthma exacerbation? Arch. Med. Sci. 2015, 11, 494–504. [Google Scholar] [CrossRef]
- Senoner, T.; Schindler, S.; Stättner, S.; Öfner, D.; Troppmair, J.; Primavesi, F. Associations of oxidative stress and postoperative outcome in liver surgery with an outlook to future potential therapeutic options. Oxid. Med. Cell Longev. 2019, 2019, 3950818. [Google Scholar] [CrossRef]
- Ucar, M.; Ozgül, U.; Polat, A.; Toprak, H.I.; Erdogan, M.A.; Aydogan, M.S.; Durmus, M.; Ersoy, M.O. Comparison of antioxidant effects of isoflurane and propofol in patients undergoing donor hepatectomy. Transplant Proc. 2015, 47, 469–472. [Google Scholar] [CrossRef]
- Purdy, M.; Kärkkäinen, J.; Kokki, M.; Anttila, M.; Aspinen, S.; Juvonen, P.; Kokki, H.; Pulkki, K.; Rantanen, T.; Eskelinen, M. Does rectus sheath block analgesia alter levels of the oxidative stress biomarker glutathione peroxidase: A randomised trial of patients with cancer and benign disease. Anticancer Res. 2017, 37, 897–902. [Google Scholar] [CrossRef][Green Version]
- Wang, C.; Datoo, T.; Zhao, H.; Wu, L.; Date, A.; Jiang, C.; Sanders, R.D.; Wang, G.; Bevan, C.; Ma, D. Midazolam and dexmedetomidine affect neuroglioma and lung carcinoma cell biology in vitro and in vivo. Anesthesiology 2018, 129, 1000–1014. [Google Scholar] [CrossRef]
- Kim, M.H.; Oh, J.E.; Park, S.; Kim, J.H.; Lee, K.Y.; Bai, S.J.; Song, H.; Hwang, H.J.; Kim, D.W.; Yoo, Y.C. Tramadol use is associated with enhanced postoperative outcomes in breast cancer patients: A retrospective clinical study with in vitro confirmation. Br. J. Anaesth. 2019, 123, 865–876. [Google Scholar] [CrossRef]
- Kim, M.H.; Lee, J.R.; Kim, K.J.; Jun, J.H.; Hwang, H.J.; Lee, W.; Nam, S.H.; Oh, J.E.; Yoo, Y.C. Identification for antitumor effects of tramadol in a xenograft mouse model using orthotopic breast cancer cells. Sci. Rep. 2021, 11, 22113. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.H.; Sue, S.H.; Wu, Z.S.; Huang, S.M.; Lee, S.Y.; Wu, Z.F. Antitumorigenic effect of tramadol and synergistic effect with doxorubicin in human breast cancer cells. Front. Oncol. 2022, 12, 811716. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.; Luo, X.; Dai, G.; Jiang, Y.; Luo, Y.; Peng, S.; Wang, H.; Xie, P.; Qu, C.; Lin, W.; et al. Dexmedetomidine promotes the progression of hepatocellular carcinoma through hepatic stellate cell activation. Exp. Mol. Med. 2020, 52, 1062–1074. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.; He, H.; Bai, Y.; Liu, W.; Huang, L. Dexmedetomidine suppresses the progression of esophageal cancer via miR-143-3p/epidermal growth factor receptor pathway substrate 8 axis. Anticancer Drugs 2020, 31, 693–701. [Google Scholar] [CrossRef]
- Huang, Y.H.; Wu, Z.F.; Lee, M.S.; Lou, Y.S.; Wu, K.L.; Cheng, K.I.; Lai, H.C. Propofol-based total intravenous anesthesia is associated with better survival than desflurane anesthesia in glioblastoma surgery. PLoS ONE 2021, 16, e0255627. [Google Scholar] [CrossRef]
- Tseng, W.C.; Lee, M.S.; Lin, Y.C.; Lai, H.C.; Yu, M.H.; Wu, K.L.; Wu, Z.F. Propofol-based total intravenous anesthesia is associated with better survival than desflurane anesthesia in epithelial ovarian cancer surgery: A retrospective cohort study. Front. Pharmacol. 2021, 12, 685265. [Google Scholar] [CrossRef]
- Lin, K.J.; Hsu, F.K.; Shyr, Y.M.; Ni, Y.W.; Tsou, M.Y.; Chang, K.Y. Effect of epidural analgesia on long-term outcomes after curative surgery for pancreatic cancer: A single-center cohort study in Taiwan. J. Chin. Med. Assoc. 2022, 85, 124–128. [Google Scholar] [CrossRef]
- Hameed, M.; Hameed, H.; Erdek, M. Pain management in pancreatic cancer. Cancers 2010, 3, 43–60. [Google Scholar] [CrossRef]
- Saeed, I.; La Caze, A.; Hollmann, M.W.; Shaw, P.N.; Parat, M.O. New insights on tramadol and immunomodulation. Curr. Oncol. Rep. 2021, 23, 123. [Google Scholar] [CrossRef]
- Cata, J.P.; Singh, V.; Lee, B.M.; Villarreal, J.; Mehran, J.R.; Yu, J.; Gottumukkala, V.; Lavon, H.; Ben-Eliyahu, S. Intraoperative use of dexmedetomidine is associated with decreased overall survival after lung cancer surgery. J. Anaesthesiol. Clin. Pharmacol. 2017, 33, 317–323. [Google Scholar] [CrossRef]
- Owusu-Agyemang, P.; Cata, J.P.; Kapoor, R.; Zavala, A.M.; Williams, U.U.; Van Meter, A.; Tsai, J.Y.; Zhang, W.H.; Feng, L.; Hayes-Jordan, A. An analysis of the survival impact of dexmedetomidine in children undergoing cytoreductive surgery with hyperthermic intraperitoneal chemotherapy. Int. J. Hyperth. 2018, 35, 435–440. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, V.; Thomas, M.J.; Joshi, R.; Chaudhari, V.; Bhandare, M.; Mitra, A.; deSouza, A.; Ambulkar, R.; Shrikhande, S.V. Improved outcomes in 394 pancreatic cancer resections: The impact of enhanced recovery pathway. J. Gastrointest. Surg. 2018, 22, 1732–1742. [Google Scholar] [CrossRef] [PubMed]
- Melloul, E.; Lassen, K.; Roulin, D.; Grass, F.; Perinel, J.; Adham, M.; Wellge, E.B.; Kunzler, F.; Besselink, M.G.; Asbun, H.; et al. Guidelines for perioperative care for pancreatoduodenectomy: Enhanced Recovery After Surgery (ERAS) Recommendations 2019. World J. Surg. 2020, 44, 2056–2084. [Google Scholar] [CrossRef] [PubMed]
- Lima, M.F.; Mondadori, L.A.; Chibana, A.Y.; Gilio, D.B.; Giroud Joaquim, E.H.; Michard, F. Outcome impact of hemodynamic and depth of anesthesia monitoring during major cancer surgery: A before-after study. J. Clin. Monit. Comput. 2019, 33, 365–371. [Google Scholar] [CrossRef]
- Lai, H.C.; Huang, Y.H.; Chen, J.Y.; Wong, C.S.; Cheng, K.I.; Shen, C.H.; Wu, Z.F. Safe Practice of total intravenous anesthesia with target-controlled infusion in Taiwan: A recommendation. Asian J. Anesthesiol. 2021, 59, 123–134. [Google Scholar]
- Mavros, M.N.; Xu, L.; Maqsood, H.; Gani, F.; Ejaz, A.; Spolverato, G.; Al-Refaie, W.B.; Frank, S.M.; Pawlik, T.M. Perioperative blood transfusion and the prognosis of pancreatic cancer surgery: Systematic review and meta-analysis. Ann. Surg. Oncol. 2015, 22, 4382–4391. [Google Scholar] [CrossRef]
- Kim, S.Y.; Choi, M.; Hwang, H.K.; Rho, S.Y.; Lee, W.J.; Kang, C.M. Intraoperative transfusion is independently associated with a worse prognosis in resected pancreatic cancer-a retrospective cohort analysis. J. Clin. Med. 2020, 9, 689. [Google Scholar] [CrossRef]
- Ye, L.; Livingston, E.H.; Myers, B.; Hines, O.J. The effect of perioperative blood transfusion on long-term survival outcomes after surgery for pancreatic ductal adenocarcinoma: A systematic review. Pancreas 2021, 50, 648–656. [Google Scholar] [CrossRef]
- Takesue, Y.; Tsuchida, T. Strict glycemic control to prevent surgical site infections in gastroenterological surgery. Ann. Gastroenterol. Surg. 2017, 1, 52–59. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).