Simple Summary
Several available medications are involved in the treatment of metastatic castration-resistant prostate cancer (mCRPC). In this Taiwanese mCRPC cohort receiving enzalutamide patients with high tumor burden (HTB) were defined as those with either appendicular bony metastasis or visceral metastasis. A high tumor burden reduced the PSA response rate, radiological response rate, and progression-free survival duration. In addition, patients’ comorbidities and laboratory data—such as ALP, LDH, ALT, and hemoglobin—were correlated with the treatment efficacy of enzalutamide. Our study revealed a tumor burden before the use of enzalutamide was associated with treatment outcomes. The physician can use this information to estimate the response rate of enzalutamide and help formulate a personalized treatment plan for mCRPC patients.
Abstract
To assess the predictive value of tumor burden on the biochemical response, and radiological response in Taiwanese metastatic castration-resistant prostate cancer (mCRPC) patients receiving enzalutamide. The mCRPC patients treated with enzalutamide were recruited from three hospitals. High tumor burden (HTB) was classified as metastases at either appendicular bone or visceral organ. Good prostate-specific antigen (PSA) response was defined as PSA reduction of 80%. In this cohort, there were 104 (54.2%) HTB patients and 88 (45.8%) with low tumor burden (LTB). Compared to LTB patients, fewer HTB patients had good PSA response (odds ratio: 0.43, range: 0.22–0.87, p = 0.019) and fewer radiological response (complete and partial remission) (odds ratio: 0.78, range: 0.36–1.68, p = 0.52) to enzalutamide. The disease control rate which also contained stable disease, was still lower in HTB (76.0%) than LTB group (92.9%, OR: 0.24, range: 0.07–0.77, p = 0.016) in the multivariable model. In addition, HTB patients had significantly shorter progression–free survival duration than did LTB patients (median: 8.3 vs. 21.6 months, log-rank test p = 0.003) in the univariable analysis. The tumor burden before the use of enzalutamide was associated with treatment outcomes. HTB reduced PSA response rate, radiological response rate and progression-free survival duration.
1. Introduction
The incidence and mortality of prostate cancer are rising in several Asian countries [1]. In Taiwan, the incidence of prostate cancer is also increasing and is now more than 30 cases per 100,000 person-years [2]. In Taiwan among newly-diagnosed prostate cancer cases, over 25% have metastatic disease [2]. Although most prostate cancer patients do not die from their prostate cancer, in the case of those with metastatic prostate cancer (mPC), death is cancer-related and their median overall survival is between 33 months and 45 months [3,4]. In addition, the sites of prostate cancer metastases have a significant impact on mPC patients’ outcomes. An Asian study series also reported that cases of mPC with high volume disease had poorer overall and cancer-specific survival [3].
The chemohormonal androgen ablation randomized (CHAARTED) trial effectively highlighted the impact of the mPC disease burden and demonstrated that the upfront use of docetaxel only benefited the metastatic castration-naive prostate cancer (mCNPC) patients with high volume disease (HVD), but not those with low volume disease (LVD) [5,6]. Furthermore, the LATITUDE and STAMPEDE trials also proved the upfront use of abiraterone helps improve progression-free and overall survival in mCNPC patients with a high tumor burden [7,8]. Therefore, in patients with mCNPC, the tumor burden is an important clinical factor in deciding on an appropriate treatment strategy.
Nevertheless, information is lacking regarding the impact of the tumor burden on the treatment response in those mPC patients who are already refractory to androgen deprivation therapy (ADT). Based on the current treatment guidelines, enzalutamide is one of the preferred first line medications for metastatic castration refractory prostate cancer (mCRPC) [9]. Enzalutamide was shown to increase mCRPC patients’ median overall survival duration to 2.2 months in the pre-docetaxel (PREVAIL) trial and to 4.8 months in the post-docetaxel (AFFIRM) trial [10,11]. However, these two pivotal studies did not analyze the influence of tumor volume on the response and survival outcomes.
The goal of the present study was to assess the predictive and prognostic role of the tumor burden in mCRPC patients receiving enzalutamide. To do so, we used a collaborated cohort study from three hospitals to investigate the impact of tumor burden on the PSA response, the radiological response rate, and progression-free survival duration in mCRPC patients.
2. Materials and Methods
2.1. Patient Population and Selection Criteria
Between February 2020 and October 2020, consecutive patients with mCRPC who received new hormonal agents, such as enzalutamide and abiraterone, at the National Taiwan University Hospital, the Taipei Medical University-Shuang Ho Hospital, and the Cardinal Tien Hospital, were enrolled in this study. The patients who ever used abiraterone prior to enzalutamide was excluded. The subjects without complete information for the outcomes and were excluded as well. (Figure 1) The study was reviewed and approved by the local institutional review board (201305059RINC, NTUH; N20201013 TMU; CTH-109-3-5-051).
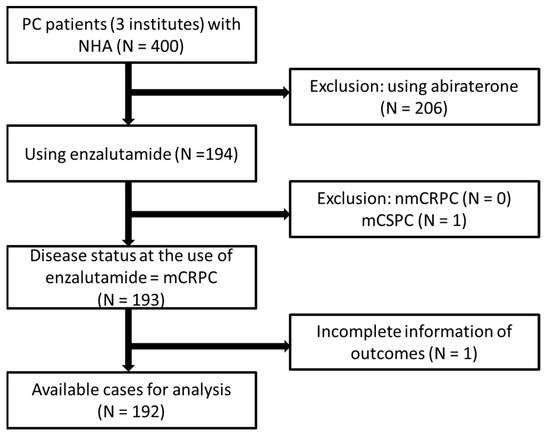
Figure 1.
Patient selection flow diagram PC = prostate cancer; NHA = new hormonal agents including abiraterone acetate and enzalutamide; mCRPC = metastatic castration resistant prostate cancer; nmCRPC = non-mCRPC; mCSPC = metastatic castration sensitive prostate cancer.
2.2. Definition of Tumor Burden
Tumor burden was defined by the existence of appendicular bony metastasis and visceral metastasis prior to the administration of enzalutamide. Patients with a high tumor burden (HTB) were defined as those with either appendicular bony metastasis or visceral metastasis [12]. The poor outcome of the patients with appendicular bony metastasis has been validated [13]. The remaining patients were considered to be in the low tumor burden (LTB) group.
2.3. Clinical Information Collection and Outcome Measurement
Clinical information was obtained from medical records using a standardized questionnaire (by YTH) and critically reviewed (by CHC). Data included: date of diagnosis, diagnosis age, initial symptoms, Gleason score, clinical stages, initial and all sequential treatments, date of castration, mPC and mCRPC treatment dates, and date of (and reasons for) death. In addition, Eastern Cooperative Oncology Group performance status, laboratory data, skeletal-related events, and tumor burden before the use of enzalutamide were obtained. We investigated three different important outcomes to evaluate the impact of enzalutamide on tumor burden. They were as follows: (1) The PSA response was defined as the maximal fall in PSA percentage after the use of enzalutamide. A PSA drop greater than 80% was designated as a good PSA response. (2) The radiological response was determined using the response evaluation criteria in solid tumors (RECIST) to assess changes in tumor burden. (3) Progression-free survival duration was defined as the duration between the start date of enzalutamide treatment and the date of PSA or radiological progression. PSA progression was determined based on the following criteria: (1) the PSA increased by ≥25% and ≥5 ng/mL in cases where the PSA did not decrease after the use of enzalutamide; (2) PSA increased ≥25% and ≥5 ng/mL in cases where the PSA decreased ≤50% after the use of enzalutamide; (3) PSA increased ≥50% and ≥5 ng/mL in cases where the PSA decreased ≥50% after the use of enzalutamide [14].
2.4. Statistical Analysis
All statistical analyses were tabulated and analyzed by Stata/MP version 16. The Chi-square test was used to evaluate the association between categorical variables and the Mann–Whitney U test was applied to compare the continuous variables. The Kaplan–Meier method with log-rank test and Cox proportional hazard models were utilized to compare progression–free survival duration among the patient groups. The logistic regression models were used to compare PSA and radiological response among the patient groups. All the above models were based on the patients with available information on outcomes, such as progression-free survival duration (N = 192), PSA response (N = 146), and radiological response (N = 131). The factors with statistical significance (p < 0.1 in univariable analysis) were selected for the multivariable model. All tests were two-sided with p < 0.05 considered statistically significant. The missing value would not be included in the Cox proportional analysis.
3. Results
3.1. Patient Demographics
A total of 192 mCRPC patients were enrolled in this study (Table 1). The median age at commencement of enzalutamide was 72 years (range, 46–94 years). HTB diseases were identified in 104 (54.2%) patients, and the remaining 88 (45.8%) patients were classified as having LTB disease. The patients with HTB were younger (median: 71 (range, 46–90) vs. 74 (range, 51–94) years, p = 0.065) and had higher PSA values at diagnosis (median: 256.6 (range, 3.2–16,410) vs. 63.4 (range, 3.3–9424.7) ng/mL, p < 0.001) than did those with LTB. The HTB patients had a significantly higher proportion of bone pain (21.2% vs. 6.8%), skeletal-related events (18.3% vs. 6.8%), and prior chemotherapy history (41.4% vs. 21.6%) compared to the LTB patients. The PSA value of more than 50 ng/mL before enzalutamide usage was significantly more frequently noted in HTB than in LTB patients (33.7% vs. 15.9%, p = 0.004). The chemotherapeutic agent used prior to enzalutamide was docetaxel in Taiwan. None of our patients received cabazitaxel before the administration of enzalutamide. Other demographic factors—including Gleason sum, ECOG performance status, and so on—were similar between the groups.

Table 1.
Demographics of prostate cancer patients stratified by tumor burden.
3.2. PSA Response
We considered a good PSA response to be the reduction in PSA value of greater than 80% after the use of enzalutamide. The HTB patients had fewer good PSA response rates than did the LTB patients (odds ratio (OR) for HTB: 0.43; range, 0.22–0.87, p = 0.019). Among the HTB patients, 53%, 16%, and 17% had a PSA reduction of ≥80%, ≥50%, and <50%, respectively. By contrast, 72%, 15%, and 11% of LTB patients experienced PSA reductions of ≥80%, ≥50%, and <50%, respectively (Figure 2). In the univariable analysis for good PSA response, initial presentation with both abnormal PSA and DRE (OR: 2.48, range, 1.11–5.58, p = 0.028), hypertension (OR: 2.1, range: 1.06–4.18, p = 0.033), and LDH value (OR: 0.2, range, 0.04–0.94, p = 0.041) were statistically significant factors. The multivariable analysis consisted of significant factors in the univariable analysis (p < 0.1), and revealed that hypertension (OR: 3.0, range, 0.31–6.84, p = 0.05) and a hemoglobin value of more than 12 mg/dL (OR: 2.7, range, 1.07–6.8, p = 0.035) significantly increased a good PSA response rate. In addition, tumor burden was also a statistically significant factor for predicting PSA responses. The LTB patients had more good PSA response rates than the patients with HTB (OR: 0.44, range, 0.19–1.0, p = 0.05) (Table 2).
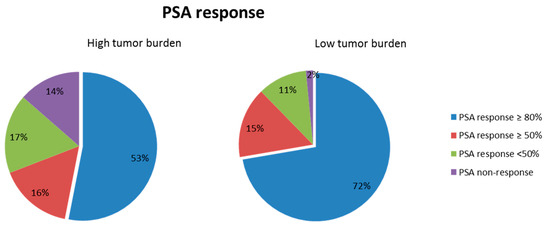
Figure 2.
PSA response in the patients stratified tumor burden. PSA response defined the maximal PSA drop percentage after the use of enzalutamide. PSA drop more than 80% was referred as the good PSA response.

Table 2.
Univariable and multivariable analyses of PSA response to enzalutamide in metastatic castration-resistant prostate cancer patients.
3.3. Radiological Response
The HTB patients had significantly fewer rates of partial radiological response and stable disease than did the LTB patients (Figure 3). The disease control rate, including the combination of complete response, partial response, and stable disease, was significantly lower in the HTB (76.0%) than LTB group (92.9%, OR: 0.24, range, 0.07–0.77, p = 0.016). The multivariable analysis for the disease control showed that HTB (OR: 0.21, range, 0.06–0.77, p = 0.018) predicted a poor response, whereas a higher hemoglobin (OR: 4.14, range, 1.0–1.0, p = 0.043) reflected good disease control using enzalutamide (Table 3).
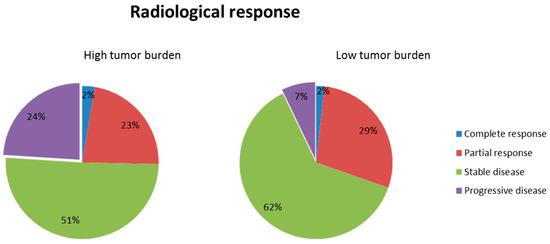
Figure 3.
Radiological response in the patients stratified tumor burden.

Table 3.
Univariable and multivariable analyses of radiological response to enzalutamide in metastatic castration-resistant prostate cancer patient.
3.4. Progression-Free Survival Duration
The HTB patients had a significantly shorter progression–free survival duration than did the LTB patients (median: 8.3 months, 95% confidence interval (CI): 5.8–10.8 vs. 21.6 months, 95% CI: 12.1–31.2) (log-rank test, p = 0.003) (Figure 4). In addition to tumor burden, several characteristics, including the duration from mPC to mCRPC, PSA value before using enzalutamide, ECOG performance status, prior chemotherapy history, skeletal-related events, and some laboratory data (hemoglobin, percent of segment neutrophil, platelets count, alanine aminotransferase (ALT), alkaline phosphatase (ALP), lactic dehydrogenase (LDH), and calcium) were associated with progression-free survival in the univariable analysis. The multivariable analysis revealed higher PSA value before using enzalutamide (hazard ratio (HR): 2.43 for PSA ≥50 ng/mL vs. PSA < 10 ng/mL; p = 0.008), prior chemotherapy history (HR: 2.23, p = 0.021), higher percent of segmental neutrophil (HR: 2.18, p = 0.033), higher ALT (HR: 0.53, p = 0.023), higher ALP (HR: 2.18, p = 0.051), and higher LDH (HR: 7.46, p < 0.001) significantly reduced progression-free survival duration. However, tumor burden lost its significance in predicting progression-free survival duration in the multivariable analysis (HR: 1.40, p = 0.221) (Table 4).
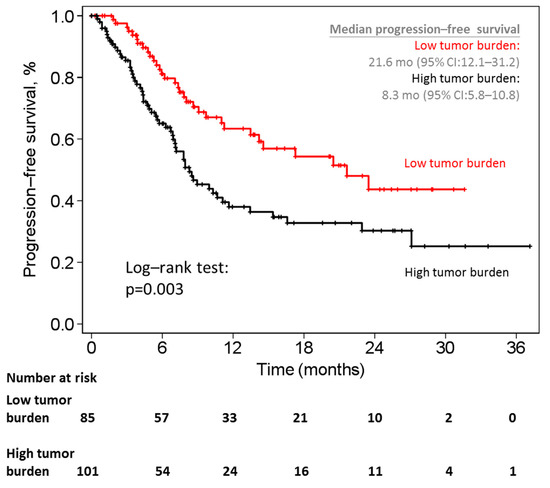
Figure 4.
Kaplan–Meier curves of progression-free survival between patients with high tumor burden and low tumor burden. mo = months; CI = confidence interval.

Table 4.
Univariable and multivariable analyses of progression-free survival duration to enzalutamide in metastatic castration-resistant prostate cancer patients.
4. Discussion
In this mCRPC cohort receiving enzalutamide, we identified tumor burden as a significant factor in predicting the effect of treatment, including the PSA response and the radiological response. The physician can use this finding to estimate the response rate of enzalutamide and help formulate a personalized treatment plan for mCRPC patients.
In several clinical trials, the extensiveness of tumors has been typically (and logically) regarded as a prognostic factor and treated as a stratified criterion. For example, the CHAARTED trial defined high volume disease as the presence of visceral metastases and/or ≥4 bone lesions with ≥1 lesion beyond the vertebral bodies and pelvis. This study revealed the survival benefit of the upfront use of docetaxel only existed in mPC patients with high volume disease but not in those with low volume disease [5]. In an Asian series of metastatic castration-sensitive prostate cancer patients, the tumor volume was significantly associated with overall survival (OS) and cancer-specific survival (CSS) [3]. Although the LATTITUDE study used a somewhat different definition of tumor burden, it still showed the value of tumor burden in selecting those cases who would receive a survival benefit with the early use of abiraterone [8,15]. In our study, in addition to being a stratified factor in clinical trials, tumor burden was noted to be a significant factor in predicting treatment response.
The PSA value is a direct indicator of treatment response and is correlated with OS and progression-free survival [16]. The CHAARTED trial revealed that patients whose PSA nadir was less than 0.2 ng/mL had a significantly longer OS duration than did those with a PSA nadir >4 ng/mL. In addition, more patients who were treated with ADT plus docetaxel had PSA nadir <0.2 ng/mL compared to those managed with ADT alone [5]. The analyses from the COU-AA-301 and COU-AA-302 trials also showed that PSA kinetics, including PSA nadir, PSA response, PSA doubling time, and time-to-PSA progression, were highly correlated with OS [17,18]. Moreover, early PSA response was noticed to be significantly associated with good survival outcomes in mCRPC patients treated with either abiraterone, enzalutamide, or ketoconazole [19]. All pivotal clinical trials, such as the ARCHES, ENZAMET, and LATTITUDE trials, lacked a detailed description of PSA response between HVD and LVD [8,20,21]. Our study provided this missing element by showing that a higher PSA response rate was noted in those mCRPC patients with LTB compared to those with HTB.
A post-hoc analysis of the Asian PREVAIL trial indicated that, in Japanese, Korean, and East Asian mCRPC patients treated with enzalutamide, the percentage of patients who achieved a PSA reduction of ≥50% from baseline was 60.7%, 70.0%, and 68.5%, respectively [22,23,24]. The treatment effects of enzalutamide in terms of radiographic progression-free survival, OS, and time-to-PSA progression were consistent with those observed in the overall study population of the PREVAIL trial [25]. Our study of Taiwanese mCRPC patients revealed the rate of PSA reduction ≥50% from baseline was slightly higher (77.4%) than that in PREVAIL and Asian PREVAIL trials. A possible reason was that our cohort had mildly lower Gleason scores and pretreatment PSA values than those patients in the PREVAIL and Asian PREVAIL trials.
Several laboratory biomarkers have been shown to be associated with the outcomes of mCRPC patients treated with either enzalutamide or abiraterone [26]. In the AFFIRM trial, pretreatment ALP and LDH levels were correlated with PSA value [27]. Moreover, ALP level prior to enzalutamide treatment has been proven to be a strong predictor of progression-free survival in a real-world cohort [28]. Furthermore, it has been observed in several mCRPC series that the higher the LDH value before treatment with enzalutamide or abiraterone, the poorer the progression-free survival [29,30,31]. Our findings regarding ALP and LDH in our Taiwanese cohort were consistent with those of other internationally previously published series.
Enzalutamide has been approved as a standard first-line therapeutic agent for mCRPC by the FDA, but some patients have not benefited from it due to tumor heterogeneity, genetic background, ethnicity, and/or other reasons [32]. In addition, most studies have compared outcomes between therapeutic agents, and few have focused on the comparison of a single drug in different types of patients. Our study identified a relationship between tumor burden and prostate cancer patients treated with enzalutamide in a Taiwanese cohort. Additionally, we derived some useful findings, such as that the duration of time from mPC to mCRPC and prior chemotherapy could predict progression-free survival duration. Further research may establish a useful model to develop optimal therapeutic decisions.
Our study has several limitations. Firstly, the case number was not enough to assess all clinical parameters in the multivariable analysis. Nevertheless, ours was the largest comparable cohort in Taiwan studied thus far, and it served to prove our hypothesis. Secondly, this was a retrospective analysis; however, selection bias may have been partially mitigated by recruiting consecutive mPC patients. Thirdly, the variety of treatments used in different institutions may interfere with study analysis; however, most of the patients in our cohort received enzalutamide reimbursed by the national health system, which would review the related medical records in advance. Therefore, there would be minimal variation of treatment plan. Finally, the administration of enzalutamide was reimbursed and should follow the regulation of the national health system in Taiwan. The patients who had duration of less than 12 months from mPC to mCRPC were suggested to have chemotherapy instead of enzalutamide. Therefore, the regulation limited us to enroll patients and analyze the effect of tumor burden for the patients with poor response to initial hormonal therapy.
5. Conclusions
In conclusion, our study revealed a tumor burden before the use of enzalutamide was associated with treatment outcomes. A high tumor burden reduced the PSA response rate, radiological response rate, and progression-free survival duration. In addition, patients’ comorbidities and laboratory data—such as ALP, LDH, ALT, and hemoglobin—were correlated with the treatment efficacy of enzalutamide.
Author Contributions
Y.-T.H. participated in study conception and design, acquisition, interpretation and analysis of data, and drafting of the manuscript. B.-J.C., C.-C.W., C.-H.L. and C.-D.L. participated in study acquisition and critical revision of the manuscript for important intellectual content. C.-H.C. participated in study conception and design, interpretation of data, critical revision of the manuscript for intellectual content and supervised the study. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was reviewed and approved by the local institutional review board (201305059RINC, NTUH; N20201013 TMU; CTH-109-3-5-051).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data available on request due to restrictions of privacy consideration of our institutions. The data presented in this study are available on request from the corresponding author. The data are not publicly available due to the consideration of patients’ privacy.
Acknowledgments
We thank all of the collaborators who participated in the Prostate Cancer clinic data collection. Provide our patient list and help us to solve some problems in the data collection.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Chung, B.H.; Horie, S.; Chiong, E. The incidence, mortality, and risk factors of prostate cancer in Asian men. Prostate Int. 2019, 7, 1–8. [Google Scholar] [CrossRef]
- Taiwan Health and Welfare Report 2019. Available online: http://www.cdway.com.tw/gov/mhw2/book108/book01e/index.html (accessed on 15 December 2020).
- Cheng, Y.-T.; Hong, J.-H.; Lu, Y.-C.; Pu, Y.-S.; Huang, C.-Y.; Huang, K.-H.; Liu, S.P.; Chen, C.-H. Impact of high-volume disease in Asian population with newly diagnosed metastatic prostate cancer. Urol. Sci. 2018, 29, 136. [Google Scholar] [CrossRef]
- Chen, C.-H.; Tzai, T.-S.; Huang, S.-P.; Wu, H.-C.; Tai, H.-C.; Chang, Y.-H.; Pu, Y.-S. Clinical outcome of Taiwanese men with metastatic prostate cancer compared with other ethnic groups. Urology 2008, 72, 1287–1292. [Google Scholar] [CrossRef]
- Sweeney, C.J.; Chen, Y.-H.; Carducci, M.; Liu, G.; Jarrard, D.F.; Eisenberger, M.; Wong, Y.-N.; Hahn, N.; Kohli, M.; Cooney, M.M. Chemohormonal therapy in metastatic hormone-sensitive prostate cancer. N. Engl. J. Med. 2015, 373, 737–746. [Google Scholar] [CrossRef] [PubMed]
- Kyriakopoulos, C.E.; Chen, Y.-H.; Carducci, M.A.; Liu, G.; Jarrard, D.F.; Hahn, N.M.; Shevrin, D.H.; Dreicer, R.; Hussain, M.; Eisenberger, M. Chemohormonal therapy in metastatic hormone-sensitive prostate cancer: Long-term survival analysis of the randomized phase III E3805 CHAARTED trial. J. Clin. Oncol. 2018, 36, 1080. [Google Scholar] [CrossRef] [Green Version]
- James, N.D.; Sydes, M.R.; Clarke, N.W.; Mason, M.D.; Dearnaley, D.P.; Spears, M.R.; Ritchie, A.W.; Parker, C.C.; Russell, J.M.; Attard, G. Addition of docetaxel, zoledronic acid, or both to first-line long-term hormone therapy in prostate cancer (STAMPEDE): Survival results from an adaptive, multiarm, multistage, platform randomised controlled trial. Lancet 2016, 387, 1163–1177. [Google Scholar] [CrossRef] [Green Version]
- Fizazi, K.; Tran, N.; Fein, L.; Matsubara, N.; Rodriguez-Antolin, A.; Alekseev, B.Y.; Özgüroğlu, M.; Ye, D.; Feyerabend, S.; Protheroe, A. Abiraterone acetate plus prednisone in patients with newly diagnosed high-risk metastatic castration-sensitive prostate cancer (LATITUDE): Final overall survival analysis of a randomised, double-blind, phase 3 trial. Lancet Oncol. 2019, 20, 686–700. [Google Scholar] [CrossRef]
- National Comprehensive Cancer Network. Prostate Cancer (Version 2.2021). Available online: https://www.nccn.org/professionals/physician_gls/default.aspx-prostate (accessed on 15 April 2021).
- Beer, T.M.; Armstrong, A.J.; Rathkopf, D.E.; Loriot, Y.; Sternberg, C.N.; Higano, C.S.; Iversen, P.; Bhattacharya, S.; Carles, J.; Chowdhury, S. Enzalutamide in metastatic prostate cancer before chemotherapy. N. Engl. J. Med. 2014, 371, 424–433. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scher, H.I.; Fizazi, K.; Saad, F.; Taplin, M.-E.; Sternberg, C.N.; Miller, K.; de Wit, R.; Mulders, P.; Chi, K.N.; Shore, N.D. Increased survival with enzalutamide in prostate cancer after chemotherapy. N. Engl. J. Med. 2012, 367, 1187–1197. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eisenberger, M.A.; Blumenstein, B.A.; Crawford, E.D.; Miller, G.; McLeod, D.G.; Loehrer, P.J.; Wilding, G.; Sears, K.; Culkin, D.J.; Thompson, I.M., Jr. Bilateral orchiectomy with or without flutamide for metastatic prostate cancer. N. Engl. J. Med. 1998, 339, 1036–1042. [Google Scholar] [CrossRef] [Green Version]
- Hussain, M.; Goldman, B.; Tangen, C.; Higano, C.S.; Petrylak, D.P.; Wilding, G.; Akdas, A.M.; Small, E.J.; Donnelly, B.J.; Sundram, S.K. Prostate-specific antigen progression predicts overall survival in patients with metastatic prostate cancer: Data from Southwest Oncology Group Trials 9346 (Intergroup Study 0162) and 9916. J. Clin. Oncol. 2009, 27, 2450. [Google Scholar] [CrossRef] [PubMed]
- Rigaud, J.; Tiguert, R.; Le Normand, L.; Karam, G.; Glemain, P.; Buzelin, J.-M.; Bouchot, O. Prognostic value of bone scan in patients with metastatic prostate cancer treated initially with androgen deprivation therapy. J. Urol. 2002, 168 Pt 1, 1423–1426. [Google Scholar] [CrossRef]
- Buelens, S.; Poelaert, F.; Dhondt, B.; Fonteyne, V.; De Visschere, P.; Ost, P.; Verbeke, S.; Villeirs, G.; De Man, K.; Rottey, S. Metastatic Burden in Newly Diagnosed Hormone-Naive Metastatic Prostate Cancer: Comparing dEfinitions of CHAARTED and LATITUDE Trial; Urologic Oncology: Seminars and Original Investigations; Elsevier: Amsterdam, The Netherlands, 2018; pp. 158.e13–158.e20. [Google Scholar]
- Alhanafy, A.M.; Zanaty, F.; Ibrahem, R.; Omar, S. Prognostic factors for hormone sensitive metastatic prostate cancer: Impact of disease volume. Asian Pac. J. Cancer Prev. APJCP 2018, 19, 1113. [Google Scholar] [PubMed]
- Xu, X.S.; Ryan, C.J.; Stuyckens, K.; Smith, M.R.; Saad, F.; Griffin, T.W.; Park, Y.C.; Margaret, K.Y.; Vermeulen, A.; Poggesi, I. Correlation between Prostate-Specific Antigen Kinetics and Overall Survival in Abiraterone Acetate–Treated Castration-Resistant Prostate Cancer Patients. Clin. Cancer Res. 2015, 21, 3170–3177. [Google Scholar] [CrossRef] [Green Version]
- De Velasco, G.; Lora, D.; Lorente, D.; Choueiri, T.K.; Sweeney, C.; Castellano, D.E. Impact of statins on outcomes in patients (pts) with metastatic castration resistant prostate cancer (mCRPC): Post-hoc analysis of data from COU-AA-301 and COU-AA-302 trials. Am. Soc. Clin. Oncol. 2018, 36, 230–230. [Google Scholar] [CrossRef]
- Fuerea, A.; Baciarello, G.; Patrikidou, A.; Albigès, L.; Massard, C.; Di Palma, M.; Escudier, B.; Fizazi, K.; Loriot, Y. Early PSA response is an independent prognostic factor in patients with metastatic castration-resistant prostate cancer treated with next-generation androgen pathway inhibitors. Eur. J. Cancer 2016, 61, 44–51. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, A.J.; Szmulewitz, R.Z.; Petrylak, D.P.; Holzbeierlein, J.; Villers, A.; Azad, A.; Alcaraz, A.; Alekseev, B.; Iguchi, T.; Shore, N.D. ARCHES: A randomized, phase III study of androgen deprivation therapy with enzalutamide or placebo in men with metastatic hormone-sensitive prostate cancer. J. Clin. Oncol. 2019, 37, 2974–2986. [Google Scholar] [CrossRef] [PubMed]
- Davis, I.D.; Martin, A.J.; Stockler, M.R.; Begbie, S.; Chi, K.N.; Chowdhury, S.; Coskinas, X.; Frydenberg, M.; Hague, W.E.; Horvath, L.G. Enzalutamide with standard first-line therapy in metastatic prostate cancer. N. Engl. J. Med. 2019, 381, 121–131. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.-S.; Theeuwes, A.; Kwon, D.D.; Choi, Y.D.; Chung, B.H.; Lee, H.M.; Lee, K.H.; Lee, S.E. The PREVAIL trial of enzalutamide in men with chemotherapy-naïve, metastatic castration-resistant prostate cancer: Post hoc analysis of Korean patients. Investig. Clin. Urol. 2016, 57, 174–183. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, C.S.; Choi, Y.D.; Lee, S.E.; Lee, H.M.; Ueda, T.; Yonese, J.; Fukagai, T.; Chiong, E.; Lau, W.; Abhyankar, S. Post hoc analyses of East Asian patients from the randomized placebo-controlled PREVAIL trial of enzalutamide in patients with chemotherapy-naïve, metastatic castration-resistant prostate cancer. Medicine 2017, 96, e7223. [Google Scholar] [CrossRef]
- Kimura, G.; Yonese, J.; Fukagai, T.; Kamba, T.; Nishimura, K.; Nozawa, M.; Mansbach, H.; Theeuwes, A.; Beer, T.M.; Tombal, B. Enzalutamide in Japanese patients with chemotherapy-naïve, metastatic castration-resistant prostate cancer: A post-hoc analysis of the placebo-controlled PREVAIL trial. Int. J. Urol. 2016, 23, 395–403. [Google Scholar] [CrossRef] [PubMed]
- Evans, C.P.; Higano, C.S.; Keane, T.; Andriole, G.; Saad, F.; Iversen, P.; Miller, K.; Kim, C.-S.; Kimura, G.; Armstrong, A.J. The PREVAIL study: Primary outcomes by site and extent of baseline disease for enzalutamide-treated men with chemotherapy-naive metastatic castration-resistant prostate cancer. Eur. Urol. 2016, 70, 675–683. [Google Scholar] [CrossRef] [PubMed]
- Chi, K.; Hotte, S.; Joshua, A.; North, S.; Wyatt, A.; Collins, L.; Saad, F. Treatment of mCRPC in the AR-axis-targeted therapy-resistant state. Ann. Oncol. 2015, 26, 2044–2056. [Google Scholar] [CrossRef] [Green Version]
- Saad, F.; de Bono, J.; Shore, N.; Fizazi, K.; Loriot, Y.; Hirmand, M.; Franks, B.; Haas, G.P.; Scher, H.I. Efficacy outcomes by baseline prostate-specific antigen quartile in the AFFIRM trial. Eur. Urol. 2015, 67, 223–230. [Google Scholar] [CrossRef]
- Poon, D.M.; Wong, K.C.; Chan, T.; Law, K.; Chan, K.; Lee, E.K.; Lee, C.; Chan, M.; Hong Kong Society of Uro-Oncology (HKSUO). Survival outcomes, prostate-specific antigen response, and tolerance in first and later lines of enzalutamide treatment for metastatic castration-resistant prostate cancer: A real-world experience in Hong Kong. Clin. Genitourin. Cancer 2018, 16, 402–412.e1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mori, K.; Kimura, T.; Onuma, H.; Kimura, S.; Yamamoto, T.; Sasaki, H.; Miki, J.; Miki, K.; Egawa, S. Lactate dehydrogenase predicts combined progression-free survival after sequential therapy with abiraterone and enzalutamide for patients with castration-resistant prostate cancer. Prostate 2017, 77, 1144–1150. [Google Scholar] [CrossRef] [PubMed]
- Chi, K.N.; Kheoh, T.; Ryan, C.J.; Molina, A.; Bellmunt, J.; Vogelzang, N.J.; Rathkopf, D.E.; Fizazi, K.; Kantoff, P.W.; Li, J. A prognostic index model for predicting overall survival in patients with metastatic castration-resistant prostate cancer treated with abiraterone acetate after docetaxel. Ann. Oncol. 2016, 27, 454–460. [Google Scholar] [CrossRef]
- Templeton, A.J.; Pezaro, C.; Omlin, A.; McNamara, M.G.; Leibowitz-Amit, R.; Vera-Badillo, F.E.; Attard, G.; De Bono, J.S.; Tannock, I.F.; Amir, E. Simple prognostic score for metastatic castration-resistant prostate cancer with incorporation of neutrophil-to-lymphocyte ratio. Cancer 2014, 120, 3346–3352. [Google Scholar] [CrossRef]
- Linder, S.; van der Poel, H.G.; Bergman, A.M.; Zwart, W.; Prekovic, S. Enzalutamide therapy for advanced prostate cancer: Efficacy, resistance and beyond. Endocr. Relat. Cancer 2019, 26, R31–R52. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).