Abstract
Snakebite envenomation (SBE)-induced immunity refers to individuals who have been previously bitten by a snake and developed a protective immune response against subsequent envenomations. The notion stems from observations of individuals, including in the indigenous population, who present only mild signs and symptoms after surviving multiple SBEs. Indeed, these observations have engendered scientific interest and prompted inquiries into the potential development of a protective immunity from exposure to snake toxins. This review explores the evidence of a protective immune response developing following SBE. Studies suggest that natural exposure to snake toxins can trigger protection from the severity of SBEs, mediated by specific antibodies. However, the evaluation of the immune memory response in SBE patients remains challenging. Further research is needed to elucidate the immune response dynamics and identify potential targets for therapeutic interventions. Furthermore, the estimation of the effect of previous exposures on SBE epidemiology in hyperendemic areas, such as in the indigenous villages of the Amazon region (e.g., the Yanomami population) is a matter of debate.
Key Contribution:
Snake toxins induce antibody production, but understanding SBE immune memory is complex. Previous snakebite exposure in hyperendemic areas like the Amazon is notable, especially among Yanomami. And, inoculation with snake toxins can prevent lesions in vaccinated individuals exposed to venom.
1. Introduction
In Brazil, approximately 30,000 snakebites are reported each year [1], presenting high morbidity and mortality rates within the Brazilian Amazon region [2]. Snake venoms are composed of a protein cocktail of high complexity and diversity [3], triggering a variety of biochemical and toxicological effects on victims, which influences several clinical manifestations [4] ranging from mild to severe outcomes, including hospitalization for long periods, surgical procedures, and follow-up for rehabilitation [5]. Indeed, snakebite after-effects depend on several factors, including the species, region of the bite, quantity of venom injected, and influence of ecology and evolution in driving inter- and intra-specific venom variations, in addition to the health condition of the victim [6,7].
Antivenom (i.e., horse-derived polyvalent antibodies) has been the primary and single specific snakebite treatment for more than a century. Although lifesaving, antivenoms still have therapeutic limitations [8,9], presenting limited efficacy against some effects of envenoming, such as local tissue damage [4,10].
Based on that, vaccines targeting snakebites were raised as a possibility to induce protection to those at risk for death by snakebite [11]. Knowing that many snake venom-derived toxins are immunogenic, different experimental approaches and studies have demonstrated that vaccine-elicited antibodies can neutralize venoms and protect from envenomation injury [12,13,14,15]. In humans, the ability of venom to induce neutralizing antibodies has also been demonstrated [16]. This article will review evidence of human antibodies targeting snake venoms and inducing protection for the victims, aiming to understand the memory immune response.
2. Snakebites in the Yanomami Indigenous Community of the Brazilian Amazon
The Yanomamis are a hunter–horticulturist indigenous population from the interfluvial tropical forest of the western Guiana massif, who inhabit the borders between Venezuela (upper Orinoco and Cassiquiare) and Brazil (upper Rio Branco, left bank of Rio Negro). They constitute a cultural and linguistic set composed of four territorially adjacent subgroups that speak mutually intelligible languages: the Yanomami (approximately 56% of the ethnic group), the Yanomam (25%), the Sanumá (14%), and the Ninam (5%) [17].
On the Brazil side, the Yanomami Indigenous Land (YIL) was demarcated in 1992, occupying 96,560 km2 in the west of the state of Roraima and north of the state of Amazonas (Figure 1), where around 21,600 indigenous people live in 260 communities [18].
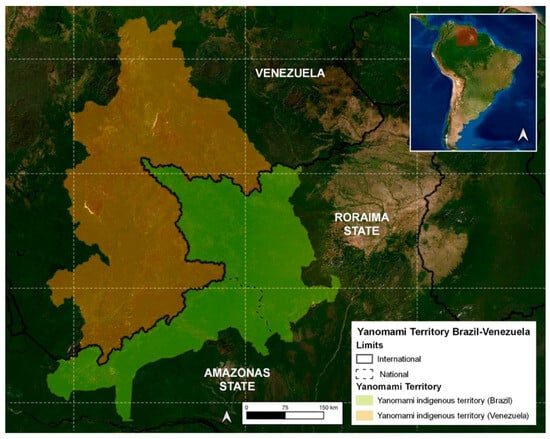
Figure 1.
Map of the Yanomami indigenous land.
Hence, the Yanomami people’s way of life, deeply intertwined with the Urihi (Forest-Earth, as it is referred to in Yanomami language), renders them particularly susceptible to snake-related accidents. Their homes (called Xapono in the Yanomami language) lack walls that would provide insulation from the surrounding forest. Additionally, their swidden agriculture is carried out in dense forest, and they frequently visit collection sites to gather roots and other plant materials essential to their daily lives. Moreover, their hunting and fishing grounds, crucial for sustenance, expose them to further potential encounters with snakes.
Since the Yanomamis are a closed indigenous community, there is no road to access the YIL, resulting in communities with difficult access (remote), which are marked by frequent snakebite envenomings due to the typical humid tropical Amazon Forest environment. Although highly prevalent, snakebites in YIL are commonly treated in situ, with the victim’s care mainly performed by local healers and health professionals working in the area [19]. In cases of severe envenomings with no improvement following local therapy, the indigenous victims can be transferred by air to main hospitals in cities [20,21]. Although snakebites are considered one of the main diseases in the YIL, there is a lack of studies in the region compared with other regions in the Amazon such as the state of Pará [22,23,24,25] and the Central Amazon [26,27].
As the Yanomamis live in places with difficult access, different causes have been shown to be responsible for the negligence of snakebite care, including the delay in therapy and difficulty in removing patients from the isolated areas, resulting in a higher lethality rate and sequelae than in other parts of Brazil [22].
In addition, recent studies [18,28,29] corroborate the fact that the Yanomamis have a mythological relationship with snakes, which can be considered as an “evil” for their population. Thus, they believe that being attacked by a snake may be a kind of punishment by the gods for some act performed. As a result, many Yanomamis do not seek medical assistance following snakebites, which, consequently, may result in the worsening of the envenomation. On the other hand, many Yanomamis that do not seek any care following a snakebite based on punishment beliefs testify that they had recovered from the envenoming without any kind of treatment, raising the possibility of a memory immune response. Nevertheless, the memory response targeting snakebites in the Yanomamis has not yet been studied or demonstrated. Nevertheless, it is undeniable that coexistence between the Yanomamis and snakes has persisted for several generations of this ethnic group.
Detailed clinical-epidemiological data obtained from the Yanomami and Ye’kuana Indigenous Special Health District (DSEI-YY) from 2017 to 2022, conducted in accordance with the Declaration of Helsinki (protocol approved by the Research Ethic Committee of the Federal University of Roraima under number CAAE 53970721.4.0000.5016), performed by the research group and presented for the first time here, demonstrated that:
- (i)
- In the YIL, men are mainly affected by snakebites at an average of 61.3%, which is statistically different in comparison to women (paired t-test, p = 0.034). However, compared with other studies [30,31], the percentage of Yanomami women (38.7%) who were affected by snakebites is 4.85 times higher than the national average (8%), probably due to the women-related activities in the community, as they also work in the field and harvest firewood, food, and medicinal products in the forest.
- (ii)
- Most snakebites occur in the age group of 20 to 39 years old (35.2%), followed by 15 to 19 (17.6%), 10 to 14 (16.9%), 40 to 59 (16.0%), 5 to 9 (10.4%), 60 to 79 years (2.1%), up to 4 years old (1.3% of cases), and over 80 years old (0.5% of cases), similarly to the results obtained by the pioneering Vital Brazil studies [30] and others [31,32,33].
- (iii)
- Regarding seasonality, the month with the highest snakebite incidence was May (mean of 19.8) and the one with the lowest incidence was December (mean of 9.5) (Figure 2). This is a different result compared to a previous study that marked July as the month with the highest occurrence of snakebites and October as the one with the lowest occurrence.
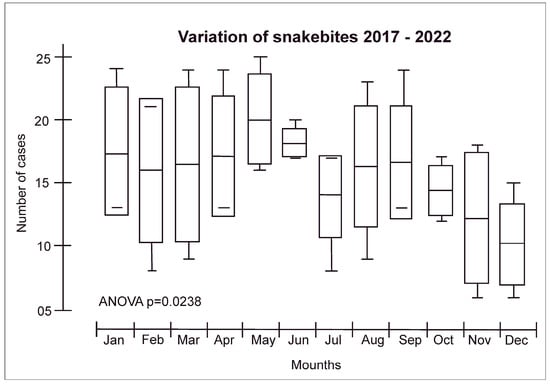 Figure 2. Snakebite distribution according to seasonality in the Yanomami Indigenous Land. The seasonality in Roraima is represented by a rainy period (from April to September) and a dry period (from October to March).
Figure 2. Snakebite distribution according to seasonality in the Yanomami Indigenous Land. The seasonality in Roraima is represented by a rainy period (from April to September) and a dry period (from October to March). - (iv)
- The highest number of snakebites were reported in the municipality of Alto Alegre in the Roraima States/Brazil (50.5%), which was expected since the region includes the Serra dos Surucucus, located in the westernmost portion of this municipality, in the border region with Venezuela, known to be inhabited by snake-rich fauna [31].
Snakebites can be life-threatening and reach a lethality of 2.75% in the YIL, which is five times higher than the lethality rate in Brazil (0.6%) [33]. Concerning the snakebite prevalence per 100,000 people, the prevalence of snakebites in the YIL is 69.7/100,000, which is much higher than the Brazilian prevalence of 1.2/100,000 inhabitants. Thus, we can determine the relative risk for the Yanomami compared to the Brazilian population as follows:
Brazilian lethality rate: 0.6% (0.006)
Brazilian snakebite prevalence: 1.2 per 100,000 (0.0012)
Yanomami lethality rate: 2.75% (0.0275)
Yanomami snakebite prevalence: 69.7 per 100,000 (0.0697)
This means that the Yanomami population has a risk of death from snakebites that is approximately 12.7 times higher than the risk for the Brazilian population. Despite the Yanomami having a higher lethality rate, due to the higher incidence of snakebites (58 times higher), we expected that proportionally the lethality should be even higher, especially due to the lack of health assistance, but the lower death rate than expected lead to the question of whether they may have developed some form of mechanism to control snake venom in their bodies. Notwithstanding, the severity and long-last disabilities in the Yanomami population have also been documented [21], indicating that snakebites have a significantly greater impact on the Yanomami population compared to other groups.
The Yanomami people are particularly noteworthy as they have had recent contact with external societies. The Fundação Nacional dos Povos Indígenas (FUNAI) defines “recent contact” indigenous groups as those who maintain both permanent and/or temporary connections with segments of the national society. Regardless of the duration of contact, these groups exhibit distinct characteristics in their relationship with the national society, displaying selectivity and autonomy in their incorporation of goods and services. As a result, they preserve their unique social structures and collective dynamics, and exercise a high degree of autonomy in defining their interactions with the state and national society [34].
3. The Immunological Response Targeting Snake Venoms
After a snakebite and the subsequent introduction of venom, the immune system is initiated in accordance with a well-established pattern, leading to the activation of both innate and adaptive immune responses. It is worth emphasizing that this immune mechanism is applicable to any other external or extracellular antigen (Figure 3) [35]. Briefly, antigen-presenting cells (APCs) are recruited to the bite site, where they recognize and process venom-derived toxins into small peptides. These peptides are then presented on the cell membrane by the major histocompatibility complex (MHC). Stimulated by the cytokines produced during the establishment of the innate immune response, the APCs migrate to the regional lymph nodes, where naive T CD8+ and T CD4+ cells recognize the antigen-MHC complex. Upon lymphocyte activation, they differentiate into effector lymphocytes. Simultaneously, naive B cells located in the lymph nodes recognize the toxin-derived components of the venom, known as antigenic epitopes. The B cells present it again on the cell membrane bound to MHC class II molecules. The subsequent interaction between the antigen-MHC class II complex on the B cell membrane and the activated helper T cell generates a second activating signal within the B cell. This signal triggers their proliferation and subsequent differentiation into plasma cells and memory cells leading to the production of specific antibodies targeting venom-derived toxins [36,37]. Memory B cells are predominantly localized in secondary lymphoid organs, such as lymph nodes and spleen. The role of memory B cells is to provide a rapid and enhanced immune response upon re-exposure to a previously encountered antigen. They are responsible for the long-term maintenance of immunological memory. Short-lived plasma cells are predominantly localized in the medullary cords of lymph nodes and the red pulp of the spleen and play a crucial role in the early immune response by producing high levels of IgM and IgG antibodies, which are important for the initial control of infections. On the other hand, long-lived plasma cells primarily reside in the bone marrow. They are responsible for maintaining a sustained production of IgG antibodies over a prolonged period [37].
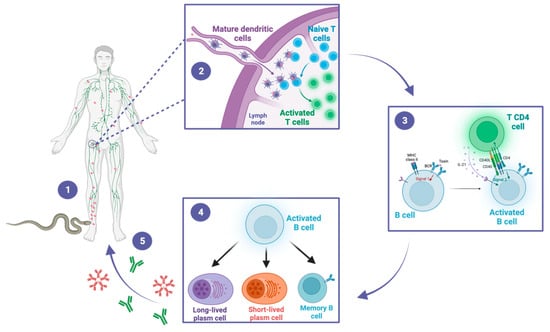
Figure 3.
A snakebite inducing antivenom antibodies. This figure illustrates the sequential steps of the immune response to snakebite, highlighting the crucial roles of dendritic cells, T cells, and B cells in the generation of protective antibodies. (1) The snake bites the victim and inoculates the venom, composed of a cocktail of toxins. The toxins are distributed locally and systemically throughout the body. Dendritic cells recognize and process the venom-derived toxins and migrate to the draining lymph nodes. (2) In the lymph nodes, dendritic cells present toxin-derived peptides to naïve CD4+ T cells, leading to their activation. (3) Activated CD4+ T cells in turn activate B cells through a T-dependent pathway. (4) Activated B cells differentiate into memory B cells, as well as into short-lived or long-lived plasma cells. (5) Short-lived plasma cells generate early IgM and IgG antibodies, while long-lived plasma cells sustain the production of IgG antibodies for long-term immunity. These antibodies could contribute to the protective immunity of snakebite victims during subsequent exposures.
To date, the only strategy available for assessing the memory response to snakebites is by measuring the humoral response through the quantification of venom-specific antibodies in serum. This approach involves determining the levels of venom-specific IgM and IgG antibodies using techniques such as enzyme-linked immunosorbent assay (ELISA). By measuring the antibody titers in the serum, valuable information can be obtained regarding the presence and magnitude of the immune memory generated after a snakebite. However, assessing other aspects of the memory response, such as the presence and functionality of memory cells (e.g., effector memory cells) and the dynamics of long-lived and short-lived plasma cells, poses challenges due to technical limitations and the complexity of accessing these cell populations in living human subjects [38].
4. Evidence of Humoral Memory Response following Snakebite Envenomings
Despite in vivo evidence demonstrating the capacity of humoral adaptive immunity to neutralize myotoxins and other compounds responsible for local and systemic venom symptoms [39,40,41], the delayed timeframe between venom inoculation and the production of sufficient quantities of antibodies for toxin neutralization poses a limitation for an immediate beneficial effect of the humoral response following snakebite envenomation. In fact, venom effects initiate immediately after the snakebite and are subsequently intensified by the body’s inflammatory response, resulting in significant symptoms within a few hours and potentially leading to fatality. On the other hand, the entire duration, from the snakebite incident to the immune activation, and the final production of specific antibodies against the toxins, takes a minimum of 5 to 7 days (Figure 4) [37].
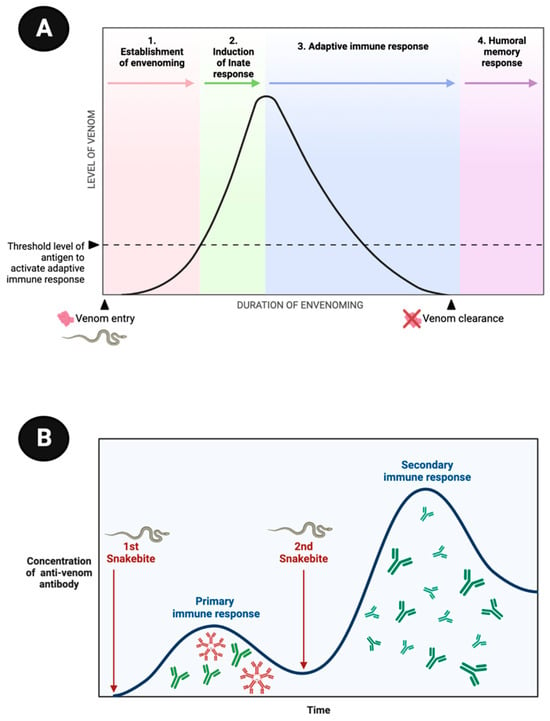
Figure 4.
Stages of the humoral memory response following a snakebite. (A) Venom-derived toxins (antigens) are rapidly distributed throughout the victim’s body (1) and trigger an immediate innate immune response following the snakebite (2). Conversely, the adaptive immune response takes several days to activate, leading to the production of a humoral response, including specific antibodies, typically occurring 5 to 7 days after the bite (4). (B) Initially, the concentration of specific antibodies targeting the venom is low (first episode), consisting primarily of IgM and IgG antibodies. However, upon a subsequent exposure (second episode), the antibody titers increase significantly, with predominantly high levels of IgGs. This enhanced immune response during re-exposure is indicative of a memory response, demonstrating the ability of the immune system to perform a stronger and more rapid defense against the venom. The figures are based on well-established immunological mechanisms [37].
In 1977, Theakston, Lloyd-Jones, and Reid, from the Liverpool School of Tropical Medicine, identified high levels of antibodies against the venoms of Echis carinatus, Bitis arietans, Causus maculatusan in rabbits, using as their method an enzyme-linked immunosorbent assay (ELISA) test [42]. After the initial study, the English research group started to analyze the immune response in two different populations: Waorani indigenous people from Ecuador and Nigerians from Bambur in the Benue Valley. First, the researchers analyzed the immune response of 223 indigenous people and revealed a high incidence (79% of the sample) of victims exhibiting antibodies against snake venom, with most individuals displaying reactivity against multiple species. In the second study, 347 subjects with alluding exposure to snakebite were tested for antibodies against the most important local species, with 37% displaying venom antibodies [16].
Subsequently, a follow-up study was conducted using sera with antibodies identified from seven indigenous Waorani people. In samples with high antibody concentrations, the researchers explored the potential for those antibodies to neutralize the effects of a second exposure, using animals. They observed that rodent groups exposed to both immunoglobulin-rich serum and a lethal dose of venom exhibited a higher survival rate compared to those exposed to sera with lower antibody concentrations or the control group [43]. These findings suggested that humoral memory could confer protective benefits in cases of subsequent snakebite accidents caused by the same species/genus, although the existing laboratory evidence in humans remains limited.
Subsequent studies have investigated the dynamic development of the adaptive humoral immune response following envenomation. These investigations have involved the meticulous measurement of isolated or prospective serum samples obtained from individuals who have experienced snakebites (Table 1). Consistently, these studies have revealed the production of diverse classes of immunoglobulins in response to venom exposure. Among these immunoglobulins, the initial one identified is IgM, which can be detected using the ELISA method as early as the third day post-exposure. However, IgM production gradually declines over the subsequent weeks. The kinetics of IgM production are relatively short-lived, resulting in lower levels compared to IgG, the latter being detectable and capable of persisting for several decades in certain individuals following venom exposure. Remarkably, individuals with a history of previous envenomation display earlier detectable IgG levels, characterized by higher concentrations and a more pronounced peak of production when compared to patients without prior exposure [44,45,46].

Table 1.
Studies demonstrating specific antibody production against snake venoms in snakebite victims.
Patients who have not been bitten by snakes can also develop an immune response against snake venom. For instance, in 1987, Wadeen and Rabson demonstrated the production of high titers of IgE and IgG antibodies, following exposure (whether through dermatological or inhalation contact) to Hemachatus haemachatus, in a snake farm worker [50]. This finding indicates an induced immune response that can occur after any type of exposure [55,56].
Furthermore, it has been observed that the production and maintenance of the venom-specific antibody pool can be influenced by various factors. For instance, the administered venom dose has been shown to impact the magnitude and kinetics of the humoral immune response [45,46]. Additionally, the administration of antivenom and the presence of uremia have been found to affect the production and sustainability of the antibody response [46]. However, it is important to note that conflicting evidence exists regarding the influence of the volume of antivenom administered on the evolution of the humoral response against venom. Further research is needed to elucidate the complex interplay between these factors and their specific impact on the dynamics and effectiveness of the humoral immune response in the context of snake envenomation. Such knowledge would contribute to improving the understanding of the immune mechanisms involved, and aid in the development of more effective therapeutic strategies for snakebite management.
5. Vaccine Approaches for Populations Living in Areas of Snakebite Risk
The optimal preventive measure against snakebites is to avoid encounters with snakes. Nevertheless, accidental encounters still occur in most situations, leading to envenomation and necessitating the best approach for overcoming it, which is treatment with antivenom. In 1877, Sewall conducted the first investigation on a prophylaxis for snakebite envenomation, subcutaneously inoculating rattlesnake venom into pigeons repeatedly. The observed signs and symptoms in the animals ranged from paw paralysis to death, occurring 3 to 20 h after injection. However, the study demonstrated that when animals received repeated venom injections they evolved to a “resistance” to the venom’s harmful effects, recovering quickly from the venom’s effects, even when exposed to lethal or higher doses, although the resistance lasted no longer than five months, as observed in one of the tested animals [57].
Later, Wallis and Wallis (2005) described the vaccination of dogs against rattlesnake venoms, showing that the dogs’ produced antibodies were able to bind and neutralize the venom effects of Crotalus atrox in vitro and in vivo [12]. Based on this information, a vaccine specifically designed for C. atrox has been developed and is currently available through Red Rock Biologics (http://redrockbiologics.com, accessed on 28 August 2023) for both dogs and horses. However, a study conducted by Leonard, Bresee, and Cruikshank (2014) suggests that there was no discernible difference in terms of morbidity and mortality rates between dogs that were vaccinated and those that were not [58]. Another study reports the vaccination of cattle with Bothrops asper venom, showing that the systemic effects that occur during moderate envenoming were prevented, and coagulopathies were delayed, in relation to non-vaccinated animals; however, the infusion of antivenom was still required [59].
Active immunization was tested not only with venoms, but also with isolated toxins derived from venoms. A study using α-cobratoxin from Naja kaouthia observed that the animals that were immunized with the toxin and later challenged with it survived, avoiding lethality [11]. Similarly, mice immunization with α-bungarotoxin peptides from Bungarus multicinctus led to a protective effect, even using high doses of the toxin [60].
These studies are not restricted to snake venoms, but also are conducted on toxins from other animal venoms. Costa et al. (2020) produced monoclonal antibodies able to recognize metalloprotease of Loxosceles spp. spider venom, through the immunization of mice with a recombinant multiepitopic protein derived from loxoscelic toxin (rMEPLox), and observed that the monoclonal antibodies produced were also able to neutralize the fibrinogenolytic activity of L. intermedia spider venom [61]. Moreover, Cerni et al. (2023) reported that the immunization of mice with Ts5, a toxin from Tityus serrulatus, was able to trigger the production of antibodies capable of inhibiting the pain caused during the scorpion envenomation [62].
In the context of human immunization against snake venoms, significant observations have been made. Haast and Winer (1955) conducted a study on a man who deliberately self-immunized using Elapidae venoms and managed to survive a snakebite incident. The individual described his symptoms from the time of the bite until his arrival at the hospital. Surprisingly, by the third day following the accident, he had fully recovered and was able to resume work the next day [63]. Another case study presented by Watt, Parrish, and Pollard (1956) involved a herpetologist who, over a period of 12 years, was bitten by ten venomous snakes and, remarkably, survived each encounter [64]. Building upon this line of research, Parrish and Pollard (1959) examined North American pit viper bites in 14 patients who had experienced multiple bites. Contrary to expectations, the study found that these repeated bites did not induce permanent immunity. In fact, some cases resulted in hypersensitivity reactions, which could potentially lead to fatal outcomes [65].
Flowers (1963) documented the immunization process of an individual who received 17 injections of Naja naja venom over a period of five months. After the immunization period, the individual’s antibodies were used in neutralization assays in mice, where 1 mL of his serum was able to neutralize 0.244 mg of venom [66]. Interestingly, despite having received 17 doses of venom, the individual continued to receive monthly injections of 5 mg of venom. However, during the study, approximately two weeks after the 24th venom injection, an accidental snakebite occurred. The snake responsible for the bite was identified as N. naja. Despite being admitted to the hospital 15 min after the bite, the individual did not receive antivenom therapy as he had already received venom doses for his immunization. Notably, he presented only mild symptoms of envenomation, and experienced only pain, swelling, and necrosis in the affected finger [67]. These human studies, involving repeated venom injections, have provided valuable insights that allow us to conclude that individuals can develop immunity to venom, rendering them protected against future bites [68].
However, it could be argued that the largest and most noteworthy study was the exceptional immunization campaign of the Amami and Okinawa Islands (Japan) performed over a period of three years (1957–1960), involving over 40,000 volunteers, aiming to immunize against Trimeresurus flavoviridis venom. This pioneering study evaluated the effectiveness of the immunization protocol in preventing local lesions caused by the venom. Meticulous data collection and analysis revealed that the immunization successfully prevented the occurrence of local lesions in vaccinated individuals exposed to the venom, highlighting the success of large-scale efforts in addressing the devastating impacts of snakebite envenomation and providing valuable insights for future research and the development of effective immunization strategies [69].
Despite the partial effectiveness observed in these human studies, it is important to highlight the cost-effectiveness of vaccines. In Brazil, snakebite care costs USD 78.15 per patient daily, including the price of the antivenom and the indirect care [70]. On the other hand, in sub-Saharan Africa the average cost of an antivenom vial is approximately USD 124 [71], which, although expensive, is relatively more affordable compared to vaccine production in low-income countries [72]. Thus, while previous studies have explored vaccination strategies, it is essential to acknowledge that these approaches have many limitations for effectively mitigating the risks associated with snakebites. The incidence of snakebites is comparatively lower than that of other epidemic diseases. Moreover, developing snakebite-specific vaccination strategies for various venomous snake species can be cost-prohibitive and may lack cost-effectiveness. Furthermore, snakebites can result from numerous snake species, each with distinct venom compositions, which should reveal the financial constraints associated with the development of multiple snake-specific vaccines and the challenges in providing widespread coverage for a relatively rare event like a snakebite.
6. Snakebite Immunity: A Fact Lacking Precise Assessment
According to the scientific evidence discussed in this study, the concept of snakebite-induced immunity is clear but very complex. While some studies suggest that individuals with a history of snakebites may exhibit partial or complete protection, or reduced severity of symptoms upon subsequent envenomation, the extent and duration of this immunity remain unclear.
Factors such as the snake species, venom composition, individual immune response, and time elapsed since the previous bite can greatly influence the outcomes. Indeed, it is worth noting that while snakes may share similar classes of toxins, we cannot assume that immunity to the venom of one species extends to another, even within the same genus and species, due to the venom variability [73]. Moreover, a previous encounter with a venomous snake does not necessarily indicate the activation of humoral immunity, particularly when there are no symptoms of envenomation, suggesting the possibility of a dry bite [74].
One of the challenges in assessing snakebite-induced immunity is the lack of standardized protocols and controlled studies. Many of the reported cases are anecdotal, making it difficult to draw definitive conclusions. Furthermore, snake venoms are highly diverse, with variations in their composition even within the same species. This complexity adds to the intricacy of understanding the immune response and the potential for developing immunity against different snake venoms.
7. Conclusions
In conclusion, the concept of snakebite-induced immunity continues to be a subject of scientific interest and investigation. While there is evidence of protection or altered immune responses in individuals with a history of snakebites, especially in indigenous communities, further research is needed to fully understand the detailed mechanisms and implications of such an immunity. Until then, the primary focus should remain on prevention, prompt medical intervention, and the availability of effective antivenom therapies to mitigate the devastating effects of snakebite envenomation.
Author Contributions
S.R.J., T.A.d.A.M. and M.B.P. conceived the main idea of this work and drafted the manuscript. I.S.d.O., I.G.F., F.A.C., M.A.S., J.d.A.G.S., A.M.R., A.S.d.F., G.M.-d.-S., E.T.M.F. and W.M.M. wrote parts of the review. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP, São Paulo Research Foundation, scholarships to ISO n. 2020/13176-3 and n. 2022/08964-8), Conselho Nacional de Desenvolvimento Científico e Tecnolόgico (CNPq, The National Council for Scientific and Technological Development, scholarship to MBP n. 307184/2020-0, WMM n. 309207/2020-7, JAGS n. 311434/2021-5), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES, Coordination for the Improvement of Higher Education Personnel, scholarship to SRJ n. 5809252), Fundação do Instituto de Biociências (FUNDIBIO, scholarship to ETMF n. 017/22), and Fundação de Amparo a Pesquisa do Estado do Amazonas (FAPEAM, scholarship to FAC n. 01.02.016301.01070/2023-13). This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES) – Finance Code 001.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of Federal University of Roraima (protocol code CAAE 53970721.4.0000.5016 and approved on 4 March 2022).
Informed Consent Statement
Since the study only present secondary data, informed consent statement was not necessary.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Ministério da Saúde Acidente Por Animais Peçonhentos—Notificações Registradas No Sistema de Informação de Agravos de Notificação—Brasil. Available online: http://tabnet.datasus.gov.br/cgi/tabcgi.exe?sinannet/cnv/animaisbr.def (accessed on 28 February 2023).
- Sampaio, V.S.; Gomes, A.A.; Silva, I.M.; Sachett, J.; Ferreira, L.C.L.; Oliveira, S.; Sabidò, M.; Chalkidis, H.; Barbosa Guerra, M.G.V.; Salinas, J.L.; et al. Low Health System Performance, Indigenous Status and Antivenom Underdosage Correlate with Spider Envenoming Severity in the Remote Brazilian Amazon. PLoS ONE 2016, 11, e0156386. [Google Scholar] [CrossRef][Green Version]
- Calvete, J.J. Proteomic Tools against the Neglected Pathology of Snake Bite Envenoming. Expert. Rev. Proteom. 2011, 8, 739–758. [Google Scholar] [CrossRef]
- Gutiérrez, J.M.; Calvete, J.J.; Habib, A.G.; Harrison, R.A.; Williams, D.J.; Warrell, D.A. Snakebite Envenoming. Nat. Rev. Dis. Primers 2017, 3, 17063. [Google Scholar] [CrossRef]
- Burki, T. Resolution on Snakebite Envenoming Adopted at the WHA. Lancet 2018, 391, 2311. [Google Scholar] [CrossRef] [PubMed]
- Gold, B.S.; Dart, R.C.; Barish, R.A. Bites of Venomous Snakes. N. Engl. J. Med. 2002, 347, 347–356. [Google Scholar] [CrossRef] [PubMed]
- Kaur, N.; Iyer, A.; Sunagar, K. Evolution Bites—Timeworn Inefficacious Snakebite Therapy in the Era of Recombinant Vaccines. Indian. Pediatr. 2021, 58, 219–223. [Google Scholar] [CrossRef] [PubMed]
- Harrison, R.A.; Cook, D.A.; Renjifo, C.; Casewell, N.R.; Currier, R.B.; Wagstaff, S.C. Research Strategies to Improve Snakebite Treatment: Challenges and Progress. J. Proteom. 2011, 74, 1768–1780. [Google Scholar] [CrossRef]
- Harrison, R.; Gutiérrez, J. Priority Actions and Progress to Substantially and Sustainably Reduce the Mortality, Morbidity and Socioeconomic Burden of Tropical Snakebite. Toxins 2016, 8, 351. [Google Scholar] [CrossRef]
- Laustsen, A.H.; María Gutiérrez, J.; Knudsen, C.; Johansen, K.H.; Bermúdez-Méndez, E.; Cerni, F.A.; Jürgensen, J.A.; Ledsgaard, L.; Martos-Esteban, A.; Øhlenschlæger, M.; et al. Pros and Cons of Different Therapeutic Antibody Formats for Recombinant Antivenom Development. Toxicon 2018, 146, 151–175. [Google Scholar] [CrossRef]
- Pergolizzi, R.G.; Dragos, R.; Ropper, A.E.; Menez, A.; Crystal, R.G. Protective Immunity against α-Cobratoxin Following a Single Administration of a Genetic Vaccine Encoding a Non-Toxic Cobratoxin Variant. Hum. Gene Ther. 2005, 16, 292–298. [Google Scholar]
- Wallis, D.; Wallis, J. Rattlesnake Vaccine to Prevent Envenomation Toxicity in Dogs. In Proceedings of the Western Veterinary Conference, Las Vegas, NV, USA, 1 January 2005; Volume SIS1. [Google Scholar]
- Ayala, M.S.; Arevalo, B.; Vanegas, V. Design of a Therapeutic Vaccine against Snake Venom Disintegrins, 2015. [CrossRef]
- Freitas, T.; Diniz, C.; Frézard, F. The Use of Liposomes as Snake Venom Vehicles. Application in Protective Immunization. J. Toxicol. Toxin Rev. 1998, 17, 441–466. [Google Scholar] [CrossRef]
- de Melo, P.D.V.; Lima, S.d.A.; Araújo, P.; Santos, R.M.; Gonzalez, E.; Belo, A.A.; Machado-De-Ávila, R.A.; Costal-Oliveira, F.; Soccol, V.T.; Guerra-Duarte, C.; et al. Immunoprotection against Lethal Effects of Crotalus durissus Snake Venom Elicited by Synthetic Epitopes Trapped in Liposomes. Int. J. Biol. Macromol. 2020, 161, 299–307. [Google Scholar] [CrossRef]
- Theakston, R.D.; Reid, H.A.; Larrick, J.W.; Kaplan, J.; Yost, J.A. Snake Venom Antibodies in Ecuadorian Indians. J. Trop. Med. Hyg. 1981, 84, 199–202. [Google Scholar]
- Albert, B. URIHI: Terra, Economia e Saûde Yanomami; Universidade de Brasília: Brasília, Brazil, 1991. [Google Scholar]
- Kopenawa, D. A Queda do Céu: Palavras de um Xamã Yanomami; Companhia das Letras: São Paulo, Brazil, 2015; ISBN 978-85-359-2620-0. [Google Scholar]
- Freitas, F.P.d.P.; Luna, W.F.; Bastos, L.O.d.A.; Ávila, B.T. Experiências de Médicos Brasileiros Em Seus Primeiros Meses Na Atenção Primária à Saúde Na Terra Indígena Yanomami. Interface 2021, 25, e200212. [Google Scholar] [CrossRef]
- Cristino, J.S.; Salazar, G.M.; Machado, V.A.; Honorato, E.; Farias, A.S.; Vissoci, J.R.N.; Silva Neto, A.V.; Lacerda, M.; Wen, F.H.; Monteiro, W.M.; et al. A Painful Journey to Antivenom: The Therapeutic Itinerary of Snakebite Patients in the Brazilian Amazon (The QUALISnake Study). PLoS Negl. Trop. Dis. 2021, 15, e0009245. [Google Scholar] [CrossRef]
- Oliveira, I.S.; Ananias, C.B.; Medeiros, J.M.; Franco, M.V.S.; Ferreira, I.G.; Cerni, F.A.; Sandri, E.A.; Monteiro, W.M.; Pucca, M.B. Medical Management after Lancehead Snakebite in North Amazon: A Case Report of Long-Term Disability. Toxins 2022, 14, 494. [Google Scholar] [CrossRef]
- da Cunha, O.R.; Nascimento, F.P. Do Ofídios da Amazônia: As Cobras da Região Leste do Pará; Museu Emílio Goeldi: Belém, Brazil, 1993; Volume 9. [Google Scholar]
- da Frota, J.G.; dos Santos, A.P., Jr.; de Chalkidis, H.M.; Guedes, A.G. As Serpentes Da Regiao Do Baixo Rio Amazonas, Oeste Do Estado Do Pará, Brasil (Squamata). Biociências 2005, 13, 211–220. [Google Scholar]
- da Prudente, A.L.C.; Sarmento, J.F.M.; Avila-Pires, T.C.S.; Maschio, G.; Sturaro, M.J. How Much Do We Know about the Diversity of Squamata (Reptilia) in the Most Degraded Region of Amazonia? S. Am. J. Herpetol. 2018, 13, 117. [Google Scholar] [CrossRef]
- Prudente, A.L.; Ramos, L.; Silva, T.; Sarmento, J.; Dourado, A.; Silva, F.; Almeida, P.; Santos, C.; Sousa, M. Dataset from the Snakes (Serpentes, Reptiles) Collection of the Museu Paraense Emílio Goeldi, Pará, Brazil. Biodivers. Data J. 2019, 7, e34013. [Google Scholar] [CrossRef]
- de Fraga, R.; Stow, A.J.; Magnusson, W.E.; Lima, A.P. The Costs of Evaluating Species Densities and Composition of Snakes to Assess Development Impacts in Amazonia. PLoS ONE 2014, 9, e105453. [Google Scholar] [CrossRef]
- Martins, M.; Oliveira, M. Natural History of Snakes in Forests of the Manaus Region, Central Amazonia, Brazil. Herpetol. Nat. Hist. 1998, 6, 78–150. [Google Scholar]
- Kawaguchi, D. Lições de Um Xamã Yanomami Para a Construção de Uma Identidade Pós-Antropocêntrica. Rev. Abordagem Gestáltica Phenomenol. Stud. 2021, 27, 328–338. [Google Scholar] [CrossRef]
- Hata, L. A Potência Do Falso: A Cosmogonia Yanomami Na Obra de Claudia Andujar. Esferas 2021, 16, 16–31. [Google Scholar] [CrossRef]
- Brazil, I.V. A Defesa Contra o Ofidismo; Pocai & Weiss: São Paulo, Brazil, 1911. [Google Scholar]
- Nascimento, S.P. do Aspectos epidemiológicos dos acidentes ofídicos ocorridos no Estado de Roraima, Brasil, entre 1992 e 1998. Cad. Saúde Pública 2000, 16, 271–276. [Google Scholar] [CrossRef] [PubMed]
- Cunha, L.E.R. DSEI YANOMAMI e os Acidentes Ofídicos No Norte do Brasil: Do Perfil Epidemiológico à Avaliação da Termoestabilidade dos Soros Antiofídicos como Estratégia de Saúde Pública; Doutorado em Medicina Tropical, Fundação Oswaldo Cruz; Instituto Oswaldo Cruz: Rio de Janeiro, Brazil, 2020. [Google Scholar]
- Jati, S.R.; Sousa, F.; Sant’Ana, A.C.; Mello, G.T.; Ferreira, D.E.S.; Gama, H.F.; Jati, N.S. Epidemiology of Accidents by Snakes in the Yanomami Indigenous Lands, in Roraima. In VenoRaima Abstract Book; Journal of Venomous Animals Including Tropical Diseases: Boa Vista, Brazil, 2022; Volume 28, p. 100. [Google Scholar]
- FUNAI Povos de Recente Contato. Available online: https://www.gov.br/funai/pt-br/atuacao/povos-indigenas/povos-indigenas-isolados-e-de-recente-contato-2/povos-de-recente-contato-1 (accessed on 21 May 2023).
- Leon, G.; Sanchez, L.; Hernandez, A.; Villalta, M.; Herrera, M.; Segura, A.; Estrada, R.; Maria Gutierrez, J. Immune Response towards Snake Venoms. Inflamm. Allergy-Drug Targets 2011, 10, 381–398. [Google Scholar] [CrossRef] [PubMed]
- Ryan, R.Y.M.; Seymour, J.; Loukas, A.; Lopez, J.A.; Ikonomopoulou, M.P.; Miles, J.J. Immunological Responses to Envenomation. Front. Immunol. 2021, 12, 661082. [Google Scholar]
- Abbas, A.K.; Lichtman, A.H.; Pillai, S.; Baker, D.L.; Baker, A. Cellular and Molecular Immunology, 9th ed.; Elsevier: Philadelphia, PA, USA, 2018; ISBN 978-0-323-47978-3. [Google Scholar]
- Chen, W.; Ghobrial, R.M.; Li, X.C. The Evolving Roles of Memory Immune Cells in Transplantation. Transplantation 2015, 99, 2029–2037. [Google Scholar] [CrossRef]
- Lomonte, B.; Kahan, L. Production and Partial Characterization of Monoclonal Antibodies to Bothrops Asper (Terciopelo) Myotoxin. Toxicon 1988, 26, 675–689. [Google Scholar] [CrossRef]
- Lomonte, B.; Gutiérrez, J.M.; Moreno, E.; Cerdas, L. Antibody Neutralization of a Myotoxin from the Venom of Bothrops Asper (Terciopelo). Toxicon 1987, 25, 443–449. [Google Scholar] [CrossRef]
- Garcia Denegri, M.E.; Maruñak, S.; Todaro, J.S.; Ponce-Soto, L.A.; Acosta, O.; Leiva, L. Neutralisation of the Pharmacological Activities of Bothrops Alternatus Venom by Anti-PLA2 IgGs. Toxicon 2014, 86, 89–95. [Google Scholar] [CrossRef]
- Theakston, R.D.; Lloyd-Jones, M.J.; Reid, H.A. Micro-ELISA for Detecting and Assaying Snake Venom and Venom-Antibody. Lancet 1977, 2, 639–641. [Google Scholar] [CrossRef]
- Theakston, R.D.G.; Reid, H.A.; Iddon, D.; Larrick, J.W. Protective Effect of Snake Venom Antibodies in Sera of Previous Snake Bite Victims. Ann. Trop. Med. Parasitol. 1983, 77, 311–314. [Google Scholar] [CrossRef] [PubMed]
- Barraviera, B.; Sartori, A.; Pereira Da Silva, M.F.; Kaneno, R.; Peraçoli, M.T.S. Use of an Elisa assay to evaluate venom, antivenom, igg and igm human antibody levels in serum and cerebrospinal fluid from patients bitten by Crotalus durissus terrificus in Brazil. J. Venom. Anim. Toxins 1996, 2, 14–27. [Google Scholar] [CrossRef]
- Domingos, M.O.; Cardoso, J.L.; da Silva, A.M.; Mota, I. The Humoral Immune Responses of Patients Bitten by the Snake Bothrops Jararaca (Jararaca). Toxicon 1990, 28, 723–726. [Google Scholar] [CrossRef]
- Pe, T.; Myint, A. Humoral Response Following Russell’s Viper (Daboia russelli siamensis) Bites in Myanmar. Toxicon 1995, 33, 373–377. [Google Scholar] [CrossRef]
- Theakston, R.D.; Pugh, R.N.; Reid, H.A. Enzyme-Linked Immunosorbent Assay of Venom-Antibodies in Human Victims of Snake Bite. J. Trop. Med. Hyg. 1981, 84, 109–112. [Google Scholar]
- Theakston, R.D.; Wyatt, G.B. Venom Antibody Levels in a Patient Bitten by a Young Puff Adder (Bitis arietans) during a World Record Attempt. Ann. Trop. Med. Parasitol. 1985, 79, 305–307. [Google Scholar] [CrossRef] [PubMed]
- Chippaux, J.P.; Theakston, R.D. Epidemiological Studies of Snake Bite in French Guiana. Ann. Trop. Med. Parasitol. 1987, 81, 301–304. [Google Scholar] [CrossRef]
- Wadee, A.A.; Rabson, A.R. Development of Specific IgE Antibodies after Repeated Exposure to Snake Venom. J. Allergy Clin. Immunol. 1987, 80, 695–698. [Google Scholar] [CrossRef]
- Ameno, S.; Ameno, K.; Fuke, C.; Kiryu, T.; Ijiri, I. IgG Subclass Distributions of Anti-Horse Serum Antibodies and Natural Venom-Antibodies Produced in Response to Antivenom Injection or Snake Bite in Humans. Toxicon 1990, 28, 347–350. [Google Scholar] [CrossRef]
- Sells, P.G.; Theakston, R.D.; Warrell, D.A. Development of Alpha-Neurotoxin Antibodies in Patients Envenomed by the Monocellate Thai Cobra (Naja kaouthia). Toxicon 1994, 32, 1667–1671. [Google Scholar] [CrossRef]
- Pe, T.; Myint, A.A.; Warrell, D.; Myint, T. King Cobra (Ophiophagus hannah) Bites in Myanmar: Venom Antigen Levels and Development of Venom Antibodies. Toxicon 1995, 33, 379–382. [Google Scholar] [CrossRef]
- Morais, V.; Berasain, P.; Ifrán, S.; Carreira, S.; Tortorella, M.N.; Negrín, A.; Massaldi, H. Humoral Immune Responses to Venom and Antivenom of Patients Bitten by Bothrops Snakes. Toxicon 2012, 59, 315–319. [Google Scholar] [CrossRef] [PubMed]
- de Medeiros, C.R.; Barbaro, K.C.; Lira, M.S.; França, F.O.S.; Zaher, V.L.; Kokron, C.M.; Kalil, J.; Castro, F.F.M. Predictors of Bothrops jararaca Venom Allergy in Snake Handlers and Snake Venom Handlers. Toxicon 2008, 51, 672–680. [Google Scholar] [CrossRef] [PubMed]
- Swiontek, K.; Planchon, S.; Ollert, M.; Eyer, F.; Fischer, J.; Hilger, C. Phospholipase A2 Triggers Anaphylaxis to Snake Venom by Repeated Skin Sensitization: A Case Report. J. Investig. Allergol. Clin. Immunol. 2021, 31, 175–177. [Google Scholar] [CrossRef] [PubMed]
- Sewall, H. Experiments on the Preventive Inoculation of Rattlesnake Venom. J. Physiol. 1887, 8, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Leonard, M.; Bresee, C.; Cruikshank, A. Effects of the Canine Rattlesnake Vaccine in Moderate to Severe Cases of Canine Crotalid Envenomation. Veter. Med. Res. Rep. 2014, 5, 153–158. [Google Scholar] [CrossRef]
- Herrera, M.; González, K.; Rodríguez, C.; Gómez, A.; Segura, Á.; Vargas, M.; Villalta, M.; Estrada, R.; León, G. Active Immunization of Cattle with a Bothropic Toxoid Does Not Abrogate Envenomation by Bothrops asper. Venom, but Increases the Likelihood of Survival. Biologicals 2017, 46, 1–5. [Google Scholar] [CrossRef]
- Dolimbek, B.Z.; Zouhair Atassi, M. Protection against α-Bungarotoxin Poisoning by Immunization with Synthetic Toxin Peptides. Mol. Immunol. 1996, 33, 681–689. [Google Scholar] [CrossRef]
- Costa, T.G.F.; Costal-Oliveira, F.; de Assis, T.C.S.; Lima, S.A.; Martins, C.A.; Finco, A.B.; Veiga, S.S.; Soccol, V.T.; Machado-de-Ávila, R.A.; Figueiredo, L.F.M.; et al. Engineered Antigen Containing Epitopes from Loxosceles spp. Spider Toxins Induces a Monoclonal Antibody (Lox-mAb3) against Astacin-like Metalloproteases. Int. J. Biol. Macromol. 2020, 162, 490–500. [Google Scholar] [CrossRef]
- Cerni, F.; Oliveira, I.; Cordeiro, F.; Bordon, K.; Ferreira, I.; Monteiro, W.; Arantes, E.; Cunha, T.; Pucca, M. The Nociceptive Response Induced by Different Classes of Tityus serrulatus Neurotoxins: The Important Role of Ts5 in Venom-Induced Nociception. PLoS Neglected Trop. Dis. 2023, 17, e0011057. [Google Scholar] [CrossRef]
- Haast, W.E.; Winer, M.L. Complete and Spontaneous Recovery from the Bite of a Blue Krait Snake (Bungarus caeruleiis). Am. J. Trop. Med. Hyg. 1955, 4, 1135–1137. [Google Scholar] [CrossRef] [PubMed]
- Watt, H.F.; Parrish, H.M.; Pollard, C.B. Repeated Poisonous Snakebites in the Same Patient: An Unusual Case Report. North Carol. Med. J. 1956, 17, 174–179. [Google Scholar]
- Parrish, H.M.; Pollard, C.B. Effects of Repeated Poisonous Snakebites in Man. Am. J. Med. Sci. 1959, 237, 277–286. [Google Scholar] [CrossRef] [PubMed]
- Flowers, H.H. Active immunization of a human being against cobra (Naja naja) venom. Nature 1963, 200, 1017–1018. [Google Scholar] [CrossRef] [PubMed]
- Canan, E.D.; Flowers, H.H. Cobra Bite Following Immunization against Cobra Venom. JAMA 1965, 193, 625–626. [Google Scholar] [CrossRef]
- Repeated Poisonous Snakebites in Man. Am. J. Public Health Nations Health 1959, 49, 946. [CrossRef]
- Sawai, Y.; Kawamura, Y.; Fukuyama, T.; Okonogi, T.; Ebisawa, I. Studies on the Improvement of Treatment of Habu (Trimeresurus flavoviridis) Bites. 8. A Field Trial of Prophylactic Inoculation of the Habu Venom Toxoid. Jap. J. Expo Med. 1969, 39, 197–203. [Google Scholar]
- Magalhães, S.F.V.; Peixoto, H.M.; De Almeida Gonçalves Sachett, J.; Oliveira, S.S.; Alves, E.C.; Dos Santos Ibiapina, H.N.; Monteiro, W.M.; De Oliveira, M.R.F. Snakebite Envenomation in the Brazilian Amazon: A Cost-of-Illness Study. Trans. R. Soc. Trop. Med. Hyg. 2020, 114, 642–649. [Google Scholar] [CrossRef]
- Brown, N.I. Consequences of Neglect: Analysis of the Sub-Saharan African Snake Antivenom Market and the Global Context. PLoS Neglected Trop. Dis. 2012, 6, e1670. [Google Scholar] [CrossRef]
- Habib, A.G.; Lamorde, M.; Dalhat, M.M.; Habib, Z.G.; Kuznik, A. Cost-Effectiveness of Antivenoms for Snakebite Envenoming in Nigeria. PLoS Neglected Trop. Dis. 2015, 9, e3381. [Google Scholar] [CrossRef]
- de Oliveira, I.S.; Cardoso, I.A.; de Bordon, K.C.F.; Carone, S.E.I.; Boldrini-França, J.; Pucca, M.B.; Zoccal, K.F.; Faccioli, L.H.; Sampaio, S.V.; Rosa, J.C.; et al. Global Proteomic and Functional Analysis of Crotalus durissus collilineatus Individual Venom Variation and Its Impact on Envenoming. J. Proteom. 2019, 191, 153–165. [Google Scholar] [CrossRef] [PubMed]
- Pucca, M.B.; Knudsen, C.; Oliveira, I.S.; Rimbault, C.; Cerni, F.A.; Wen, F.H.; Sachett, J.; Sartim, M.A.; Laustsen, A.H.; Monteiro, W.M. Current Knowledge on Snake Dry Bites. Toxins 2020, 12, 668. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).