Abstract
Background/Objectives: Prospective cohort studies are useful for studying how biomolecular status affects risk of adverse health outcomes. Less well known is that the longer the follow-up time, the lower the association (or “apparent effect”) due to “regression dilution”. Here, we evaluate how follow-up interval from baseline to “event” affects the relationship between baseline serum 25-hydroxyvitamin D [25(OH)D] concentration and the later incidence of stroke and major cardiovascular events (MACEs). Methods: Findings for the relative risk (RR) of stroke and MACEs with respect to serum 25(OH)D concentrations at baseline from prospective cohort studies were plotted against mean follow-up time. Fifteen studies from mainly European countries and the United States were used for stroke and nine studies for MACEs. Linear regression analyses were used to study data for follow-up periods of up to 10 years and for more than 10 years. Results: For stroke, the linear regression fit for 1–10 years is RR = 0.34 + (0.065 × follow-up [years]), r = 0.84, adjusted r2 = 0.67, p < 0.001. No significant variations in association were found for studies with follow-up periods of 10–20 years. For MACEs, the linear fit for 1–8.1 years is RR = 0.61 + (0.055 × follow-up [years]), r = 0.81, adjusted r2 = 0.59, p = 0.03. Discussion: The shorter the follow-up period, the greater the apparent effect of better vitamin D status in reducing risk of stroke and MACEs. In addition, the apparent effect of higher 25(OH)D concentration found for the shortest follow-up time is more than twice as great as the estimate based on average follow-up intervals for all studies. Mechanisms have been found to explain how higher serum 25(OH)D concentrations could reduce risk of stroke and MACEs. Randomized controlled trials have not shown that vitamin D supplementation significantly reduces risk of either stroke or MACEs, probably because risk of both outcomes increases rapidly below 15 ng/mL (38 nmol/L) and it is difficult in Western developed countries to enroll enough participants with concentrations that low. Nonetheless, vitamin D’s role in reducing risk of stroke and MACEs could be considered causal on the basis of an evaluation of the evidence using Hill’s criteria for causality in a biological system. Conclusions: Serum 25(OH)D concentrations above 20 ng/mL are associated with significantly reduced risk of stroke and MACEs prospectively and in an apparent causal manner. Raising serum 25(OH)D concentrations to >20 ng/mL should, therefore, be recommended for everyone likely to be at risk for stroke or MACEs and indeed in the general population.
1. Introduction
The prospective cohort study is a type of observational study commonly used to assess how dietary and lifestyle factors and biological variables affect health outcomes. Participants are recruited and enrolled, information relevant to the study is obtained from each participant, and participants are followed up for a period during which various health outcomes of interest are recorded. Afterward, health outcome rates are analyzed statistically in relation to data assessed at baseline during enrollment. Most such studies do not remeasure any variables assessed during the follow-up period. Therefore, an underestimation of risk associations due to “regression dilution” generally occurs in long-term follow-up in prospective studies, as outlined by Clarke and colleagues in 1999 [1], who reported repeated measurements over 25 years for systolic and diastolic blood pressure and blood cholesterol for participants in the Framingham Study: their findings showed that the range of associations from high to low for the first and fifth quantile shrank by 65%, 75%, and 57%, respectively. Although the article had 897 citations by 31 August 2024, according to Google Scholar, that finding seems not to have had much effect on the conduct of prospective cohort studies or, more importantly, on meta-analyses made using such studies though the concentration of 25-hydroxyvitamin D [25(OH)D] in serum changes over time. For example, a study in Norway reported that the correlation coefficient, r, for serum 25(OH)D concentrations measured in 2668 participants in 1994 and again in 2008 and adjusted for season of measurement was 0.42 [2], indicating low-to-moderate correlation. In comparison, the correlation coefficients for systolic blood pressure, diastolic blood pressure, pulse, body mass index (kilograms per square meter of body surface area), serum total cholesterol, and triglycerides between 1994 and 2008 were 0.47, 0.42, 0.46, 0.83, 0.37, and 0.49, respectively, again indicating only moderate correlation. The significant effect of follow-up period on the associations of serum 25(OH)D with health outcome has been known for cancer since 2011 [3] and for all-cause mortality rate since 2012 [4], yet that phenomenon was overlooked in a highly cited meta-analysis of risk of colorectal cancer with respect to serum 25(OH)D concentration in 2019 [5], as Muñoz and Grant pointed out in 2022 [6]. By ignoring this factor, the beneficial effects of higher serum 25(OH)D concentration are underestimated, making them less likely to be used to guide research or public health policies.
Recently, researchers showed that the same effect (of changes in vitamin D status over time reducing its associations with health outcomes) is found for the risk of cognitive impairment, dementia, and Alzheimer’s disease. A 2024 meta-analyses included 15 prospective studies regarding dementia and/or Alzheimer’s disease and 9 regarding cognitive impairment [7]. As shown in plots of risk ratio for low versus high 25(OH)D concentration with different follow-up periods, linear decreases emerged in the regression fit to the data from near 2.0 for the shortest follow-up periods (near 4–5 years) to near 1.0 for follow-up periods near 13 years [8].
Stroke is an important cause of disability and death. In 2016, an estimated 13.7 million new incident strokes occurred globally, of which about 87% were ischemic strokes [9]. In 2017, an estimated 1.12 million incident strokes occurred in the European Union, with 9.53 million stroke survivors and 7.06 million disability-adjusted life years lost because of stroke [10]. A prospective study of 418,329 participants in the European Prospective Investigation into Cancer and Nutrition (EPIC) included an analysis of dietary risk factors for stroke [11]. Risk of ischemic stroke was inversely associated with consumption of fruit and vegetables, dietary fiber, and dairy foods, whereas risk of hemorrhagic stroke was positively associated with egg consumption. In the USA in 2021, it was estimated that there were 932 thousand deaths from cardiovascular disease (CVD), 696 thousand from heart disease, and 163 thousand from stroke [12].
A 2021 meta-analysis of prospective cohort studies of risk of stroke with respect to serum 25(OH)D by Su and colleagues [13] suggested to us that a reanalysis of stroke and MACE data should be made allowing for intervals from baseline to event, as in a recent meta-analysis of relevance by Xiong and colleagues [14]. There was also the meta-analysis of incidence of major cardiovascular events (MACEs) by Zhang and colleagues [15], suggesting that a similar analysis of the effect of follow-up time on the incidence of MACEs be conducted. The goal of this review, therefore, is to assess how follow-up period affects the associations found between baseline serum 25(OH)D concentrations and incidence rates of stroke and MACEs.
2. Materials and Methods
The data used here are from the prospective cohort studies examined by both Su and colleagues [13] and Xiong and colleagues [14]. Table 1 and Table 2 list the studies in ascending order of follow-up interval. Table 2 includes the adjusted odds ratio/relative risk (OR/RR) for each study reported by Su and colleagues [13] and by Xiong and colleagues [14] and is verified by inspection of the studies, and it gives the follow-up period and 25(OH)D concentration association [correlation rate] reported in each article. Each study listed the variables included in adjusting the OR/RR. For example, Anderson and colleagues [16] included hypertension, hyperlipidemia, diabetes mellitus (DM), and peripheral vascular disease. Judd and colleagues [17] adjusted for socio-demographic factors, co-morbidities, and laboratory values including parathyroid hormone.

Table 1.
Baseline data for stroke studies listed in Su and colleagues [13] and Xiong and colleagues [14] used in this study and listed by increasing follow-up period.

Table 2.
Findings for stroke studies from data for stroke studies listed in Su and colleagues [13] and Xiong and colleagues [14]. They are listed in order of increasing follow-up period.
We excluded four studies from the analysis: two did not have enough information on follow-up period or on how 25(OH)D concentrations were compared, and two because they were based on dietary vitamin D intake.
Table 3, Table 4 and Table 5 list information from eight studies used to investigate the effect of follow-up period on risk of incidence of MACEs. The tables do not include studies regarding cardiovascular disease (CVD) mortality rate because mortality can be significantly affected by treatment, thereby obscuring the effect of serum 25(OH)D concentration. MACE incidence can also be lowered through intervention. For example, lowering blood pressure pharmacologically by 5 mmHg can lower incidence of MACEs by 5–15% depending on baseline blood pressure [35].

Table 3.
Participant information for MACEs in prospective cohort studies from studies in Zhang and colleagues [15] used in this study, listed in order of increasing follow-up period.

Table 4.
Patient characteristics and type of MACE for studies in Zhang and colleagues [15] used in this study, listed in order of increasing follow-up period.

Table 5.
Findings for MACE rates in prospective cohort studies in Zhang and colleagues [15], listed in order of increasing follow-up period.
Data were analyzed using SigmaStat 4.0 (Grafiti, Palo Alto, CA, USA). Data plots were made using KaleidaGraph 4.5.4 (Synergy Software, Reading, PA, USA).
3. Results
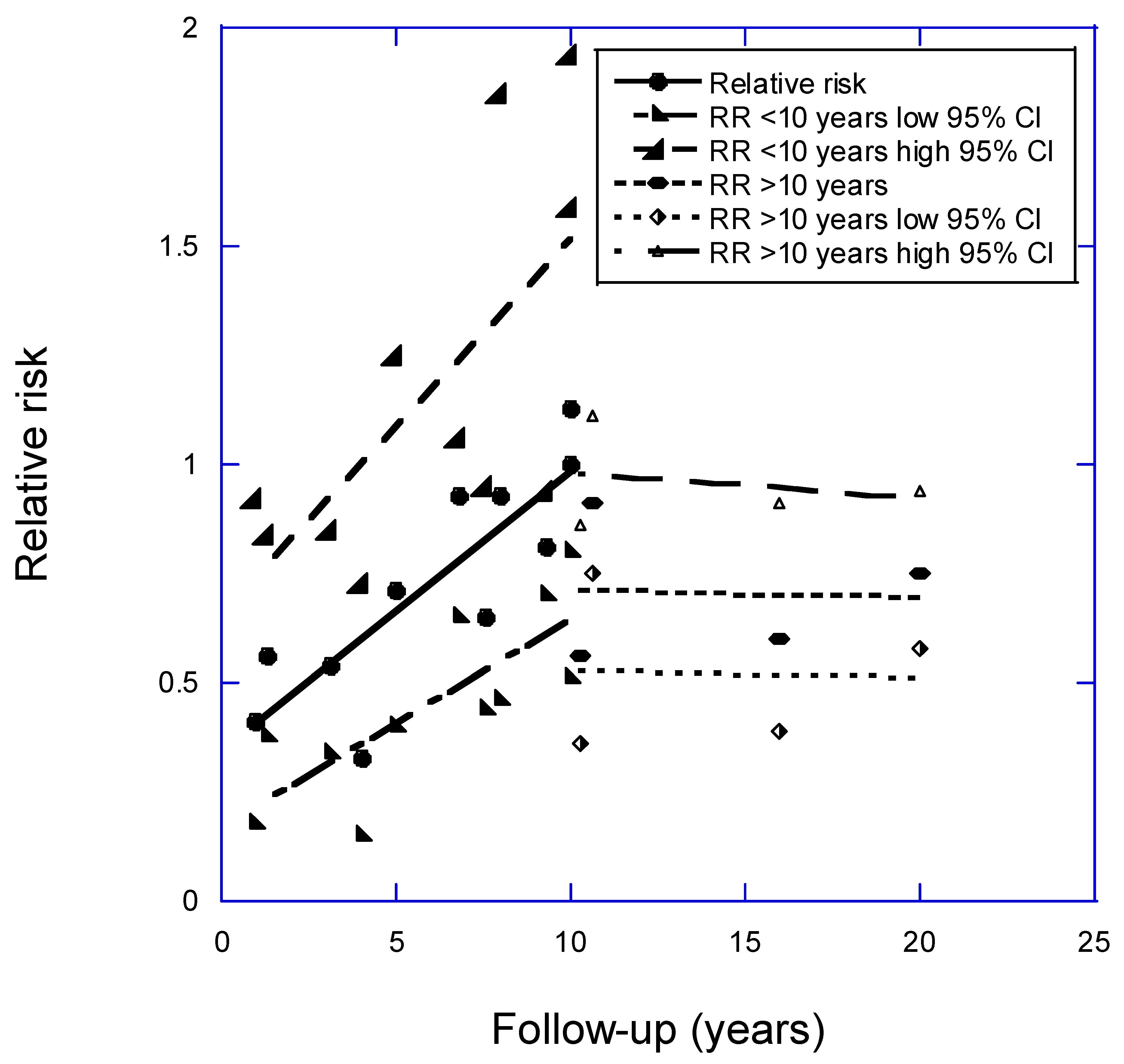
Figure 1 shows a plot of the data from Table 1. The data were analyzed after division into two groups of 1–10-year or >10-year follow-up periods between baseline vitamin D and determination of the incident events. The determination of the dividing year was made by inspecting the data plot. The graph shows a good linear fit to the data for follow-up periods of 1–10 years: RR = 0.34 + (0.065 × follow-up [years]), r = 0.84, adjusted r2 = 0.67, p < 0.001. The regression coefficients for the data were reported for the shortest interval to events post-baseline, one year, =−0.41 (95% CI, 0.22–0.75), but regression coefficients for the data on follow-up intervals >10 years showed no significant change with increasing follow-up interval. In addition, the 95% confidence interval (95% CI) values are smaller for the regression coefficients for the shorter follow-up intervals, though this finding may simply reflect the higher events rates in the studies with shorter follow-up periods. Although most studies gave results for all strokes (hemorrhagic and ischemic), ischemic strokes are much more frequent than hemorrhagic strokes in the countries studied [9]. Some reports included in the present study, however, showed that hemorrhagic strokes had weaker associations with baseline serum 25(OH)D concentrations than did ischemic stokes [17,28].
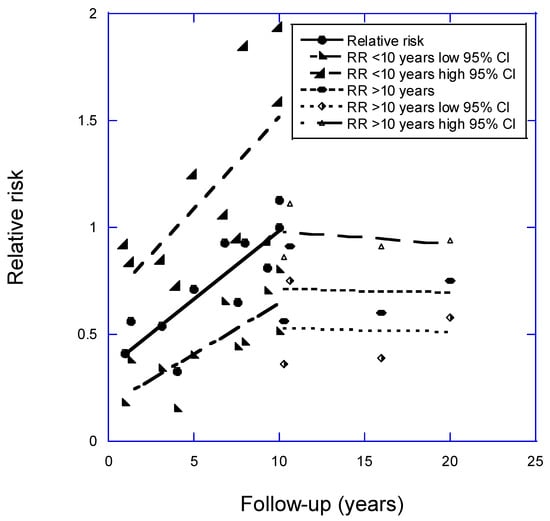
Figure 1.
Plot of relative risk for stroke versus years of follow-up with respect to high vs. low 25(OH)D concentration, with regression fits to studies of less than 10 years and for those carried out over more than 10 years; 95% CI, 95% confidence interval. Equation for regression fit to RR for follow-up period < 10 years is RR = 0.34 + (0.065 × follow-up [years]), r = 0.84, adjusted r2 = 0.67, p < 0.001.
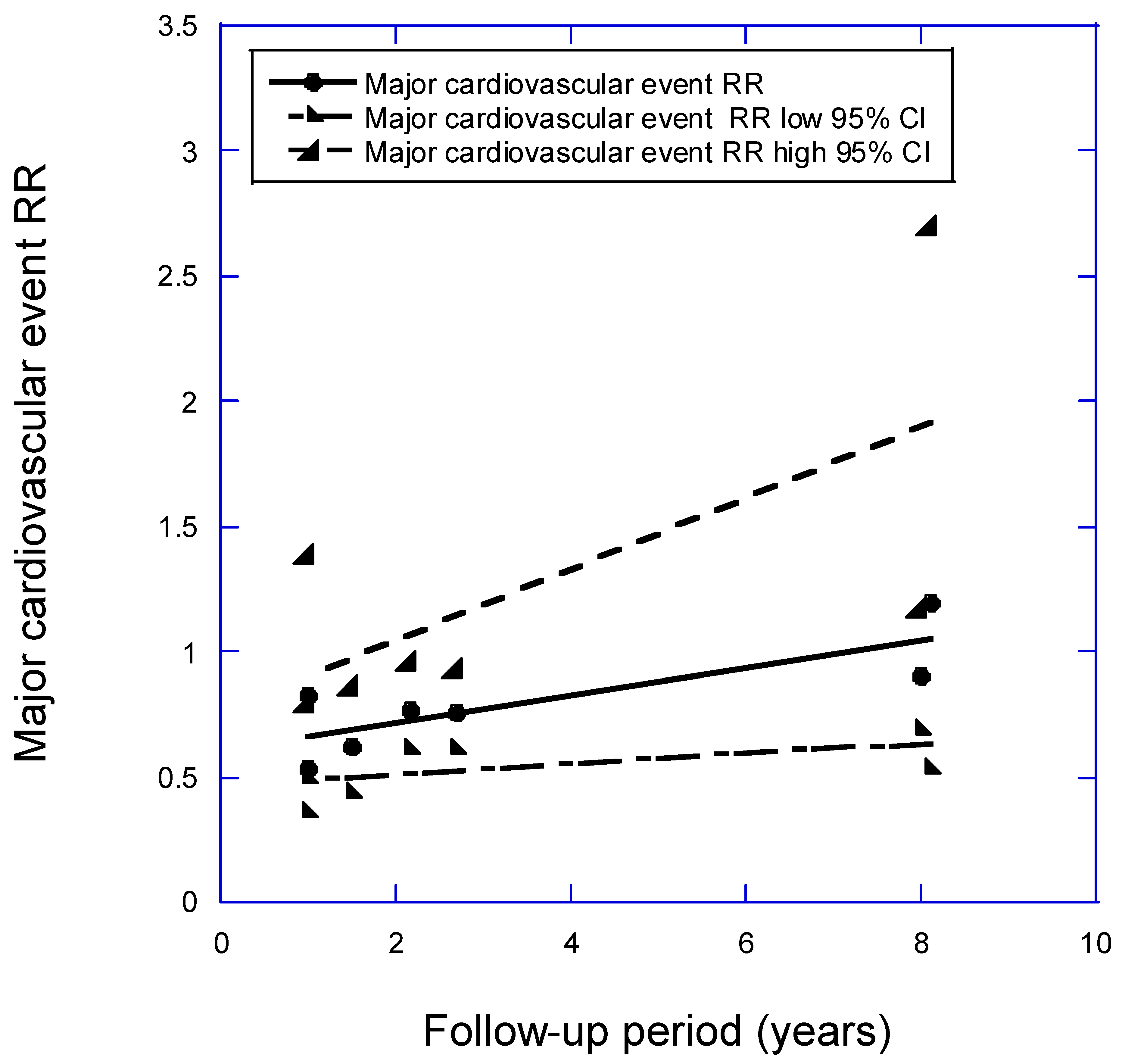
Figure 2 shows a plot of the data from Table 2 for MACE vs. follow-up period. The equation for the regression fit to the RR for high versus low 25(OH)D concentration for a follow-up period <10 years is RR = 0.61 + (0.055 × follow-up [years]), r = 0.81, adjusted r2 = 0.59, p = 0.03. The regression fit to the data for the shortest follow-up period, one year, is RR = 0.66 (95% CI, 0.48–0.91). This is a lower reduction than that found for stroke, which for one year for low versus high baseline 25(OH)D concentration is RR = 0.41 (95% CI, 0.22–0.75).
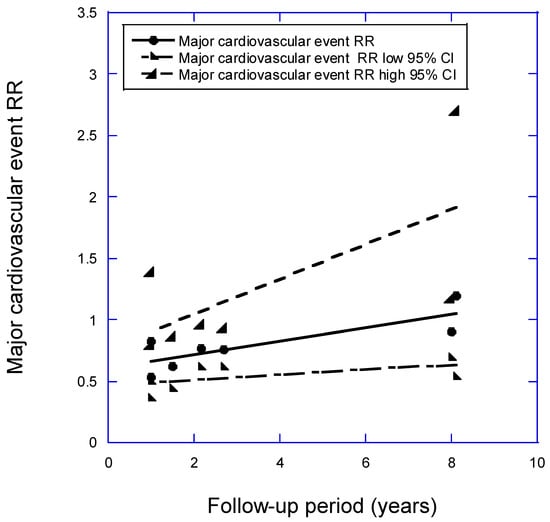
Figure 2.
Plot of relative risk of a major cardiovascular event (MACE) versus mean follow-up period for high versus low 25(OH)D concentration. Equation for regression fitted to RRs over follow-up periods <10 years is RR = 0.61 + (0.055 × follow-up [years]), r = 0.81, adjusted r2 = 0.59, p = 0.03.
4. Discussion
This study found that mean follow-up period significantly affects the determination of relative risk for stroke and MACEs in relation to 25(OH)D concentration measured at time of enrollment. The effect was much stronger for stroke incidence than for MACEs. A search for “stroke” in the MACE studies used in this analysis found that the four longest follow-up studies did not include stroke, while three of the four reporting MACE rates per se mention stroke. Only Beska 2019 [37] mentioned stroke, noting that very few stroke events were observed. Thus, it seems that the MACE findings are independent of stroke. The tentative conclusion is that the risk of stroke for low serum 25(OH)D concentration is much stronger than for other CVD events.
The meta-analysis of RRs calculated for stroke rates in relation to baseline serum 25(OH)D concentration, based on 21 prospective observational studies by Su and colleagues [13], reported an average value of 0.78 (95% CI, 0.70–0.86), whereas that by Xiong and colleagues [14], based on 21 slightly different prospective observational studies, showed an average value of 0.78 (95% CI, 0.70–0.87). Those values are approximately half the reduction seen for the 1-year follow-up period and 44% of the regression found for a “zero” follow-up period in the present study. That finding offers more evidence to support the suggestion that failure to consider the effect of follow-up period in meta-analyses of observational studies with long follow-up times can lead to considerable underestimates of the effect of the baseline variable studied. As a result, public policy recommendations are likely to be less strong than they should be.
In a 2020 article, Shi and colleagues [42] calculated the dose–response relationship for 25(OH)D concentration and stroke risk by using mostly the same observational studies as Su and colleagues [13]. The result, shown in Figure 2 in Ref. [42], was that risk decreased by ~20% with increasing vitamin D status between zero and ~20 ng/mL, with no further risk reduction between 20 and 40 ng/mL. However, as a result of not having accounted for variation in follow-up period, that analysis underestimates the reduction actually achievable with better vitamin D status. By contrast, the study does show that the main risk reduction occurs with increases in serum 25(OH)D up to 15 ng/mL. Very few randomized controlled trials (RCTs) could enroll participants with mean 25(OH)D concentrations that low, for ethical reasons, unless conducted in a country where such low 25(OH)D concentrations commonly persist. For example, many Middle Eastern countries have diets low in animal products, and their peoples often wear clothing that covers most of the body and stay indoors during the hot summers [43]. Results of a stratified randomized field trial of vitamin D supplementation in pregnant women in Iran reported that the mean baseline 25(OH)D concentration was 11 ng/mL [44]. By supplementing the women at one hospital with enough vitamin D to raise 25(OH)D concentrations to above 20 ng/mL, significant reductions occurred for gestational diabetes, pre-eclampsia, and preterm birth in comparison with outcomes in a comparable hospital where pregnant women were not supplemented.
Two factors might help explain why the results for MACEs with respect to 25(OH)D concentration were weaker than those for stroke: since mortality was an important component of MACEs in several of the studies, the participants were very likely to be treated in a variety of ways, thereby reducing the impact of 25(OH)D concentration; also, the individual MACE components may have different 25(OH)D concentration–health outcome relationships.
Comparing the differences in outcomes for stroke, CVD, and cancer is insightful. Cancer incidence and mortality rates used to have very large geographic variations in the United States [6], but stroke and CVD have not shown similar geographical variations. However, they do have more pronounced seasonal variations in mortality rates than cancer, with 20% higher mortality rates in winter than in summer in northern hemisphere countries [45]. The seasonal variation is due in part to the seasonal variations in serum 25(OH)D concentrations related to solar UVB doses [46,47]. Cancers have large geographical variations in midlatitude counties such as the United States [48] because serum 25(OH)D concentrations greater than 50 ng/mL reduce risk in comparison with lower concentrations, as shown for colorectal cancer [49] and breast cancer [50]. The differences in the 25(OH)D concentration–risk relationship also explain why the VITAL study—with a mean 25(OH)D concentration of 31 ng/mL for the participants in the vitamin D treatment arm whose serum 25(OH)D was measured—showed significantly reduced all-cancer incidence rates for participants with BMI < 25 kg/m2 and reduced all-cancer mortality rates for the entire treatment group, but no significant effects for cardiovascular disease [51]. In that RCT, MACEs occurred in 3.1% of the vitamin D treatment arm and in 3.2% of the placebo arm, whereas strokes occurred in 1.1% of the vitamin D treatment arm and 1.2% of the placebo arm.
An important question is how rapidly vitamin D might reduce risk of adverse brain and other health outcomes. As discussed in the analysis of follow-up period for cognitive function, one RCT has shown significant beneficial effects in improving cognitive function during 1 year of vitamin D supplementation [52]. To examine that question further, we searched Google Scholar for representative RCTs that reported a beneficial effect on brain health in less than 1 year (Table 6), and significant benefits were found for depression and cognitive function within one year; those studies also showed that raising serum 25(OH)D concentrations can lead to significant improvements in brain health within a year. Three of those papers dealt with studies from China, India, and/or Iran, where serum 25(OH)D concentrations are generally low, a situation that means that RCTs in those communities are more likely to be able to show health benefits from supplementation than studies conducted in countries where their populations have much higher mean 25(OH)D concentrations.

Table 6.
Results of short-term vitamin D supplementation on brain health.
For many reasons, serum 25(OH)D concentrations change over time scales from months to years (Table 7).

Table 7.
Why 25(OH)D concentrations may change over time.
Several mechanisms have been identified that help explain how higher 25(OH)D concentrations can reduce the risk of stroke. For example, a 2014 review [68] stated that vitamin D influences neuronal function by binding to vitamin D receptors that can act as transcription factors and regulate gene expression [69]. Particularly in the nervous system, vitamin D’s biological effects appear to arise from stimulation of neurotrophic factors, quenching of oxidative hyperactivity, and regulation of autoimmune responses [70]. Increasing 25(OH)D concentrations through vitamin D supplementation causes more genes to be expressed (or, more rarely, fewer). Thirty healthy adults were randomized to receive 600, 4000, or 10,000 IU/day of vitamin D3 for 6 months. The study showed a dose-dependent 25(OH)D alteration in broad gene expression with 162, 320, and 1289 genes, respectively, upregulated or downregulated in white blood cells [71].
Evidence also exists that vitamin D supplementation in vitamin D-deficient subjects can reduce serum concentrations of matrix metalloproteinases MMP-2 and MMP-9, as well as of their inhibitor, TIMP-1, and of C-reactive protein [72]. That finding is relevant because people who develop MACEs have raised MMP-9 concentrations, and MMP-9 is an important risk factor for vulnerable atherosclerotic plaque [73].
Hypertension is a risk factor for stroke. A dose–response meta-analysis showed that higher adherence to antihypertension medications reduced the risk of hemorrhagic stroke by 45% (RR = 0.55 [95% CI, 0.42–0.72]) and of ischemic stroke by 26% (RR = 0.74 [95% CI, 0.69–0.79]) [74]. A meta-analysis of serum 25(OH)D concentration on risk of hypertension in the general population based on cohort studies reported a significant increase of 38% (RR = 1.38 [95% CI = 1.14–1.64]) as 25(OH)D concentrations decreased from 75 to 15 nmol/L [75]. The same paper showed no effect of vitamin D supplementation on systolic or diastolic blood pressure on the basis of 27 studies. However, three supplementation studies reported significant or near-significant reductions in systolic blood pressure [76,77,78]. Also, an open-label study in Canada in which participants took enough vitamin D3 to increase serum 25(OH)D concentrations above 40 ng/mL reported significant reductions in the prevalence of hypertension [79]. Thus, there is some evidence that does show that vitamin D repletion can lower blood pressure and reduce the risk of established hypertension.
Table 8 lists more mechanisms by which vitamin D can reduce risk of stroke and MACEs.

Table 8.
Mechanisms by which vitamin D can reduce risk of stroke and MACEs.
RCTs have not supported the role of better vitamin D provision in reducing risk of stroke. A 2020 systematic review and meta-analysis of vitamin D supplementation and incidence of stroke included 13 RCTs [90]. The mean age was 66 years, and the mean follow-up time was 3.1 years. The mean baseline 25(OH)D concentration for studies that reported values was 19.4 ng/mL (range, 8.8–25.4 ng/mL). The percentage of participants in those 13 trials who experienced a stroke was 2.1% in both the treatment and control arms, resulting in an RR for stroke of 1.00 (95% CI, 0.91–1.10). Inspecting the baseline characteristics of participants in those trials (in Table 1 in Nudy 2021 [90]) shows that participants were being studied for various adverse health effects, including arthritis index pain, asthma exacerbations, progression to type 2 DM, falls and fractures, insulin sensitivity, and renal function. In other words, none of the trials was established specifically to evaluate the role of vitamin D supplementation, in deficiency, on the risk of stroke incidence.
A 2024 review included a different group of five vitamin D RCTs to assess the risk of ischemic strokes [91]. Mean baseline 25(OH)D concentrations were from 66 ± 23 to 77 ± 25 ng/mL in four trials and 38 ± 16 ng/mL in one trial. Follow-up duration ranged from 3.3 to 5.3 years. All those trials had CVD outcome as a primary outcome. Again, no significant difference in stroke risk was found between the vitamin D treatment and control arms, as could have been predicted from the baseline vitamin D status.
Even if the trials had been set up to test for stroke incidence, they probably would not have shown a beneficial effect for several reasons. First, nearly all vitamin D RCTs have been based on guidelines for pharmaceutical drugs. In such trials, the control arm does not receive the drug. That is not the case for vitamin D trials because vitamin D is a naturally occurring substance required for life and supplement use is often permitted in controls and it is considered unethical not to give the control group a minimal vitamin D3 supplement [92]. In 2014, Heaney outlined guidelines for trials of nutrient provision [93].
The main steps appropriate for vitamin D [94] are as follows:
- Measure 25(OH)D concentrations and include participants with low concentrations appropriate for the outcome of interest.
- Give a vitamin D dose large enough to raise 25(OH)D concentrations to levels at which beneficial effects are normally observed.
- Measure achieved 25(OH)D concentrations and adjust vitamin D dosage to maintain adequate achieved levels.
- Analyze results with respect to achieved vitamin D concentrations.
Another major reason for failure of vitamin D RCTs is the enrollment of people with relatively high 25(OH)D concentrations. Other reasons include giving relatively low doses, i.e., too small to correct deficiency, and permitting participants in the control and sometimes also the treatment arms to continue taking moderate vitamin D supplements. Analyzing results by intention to treat rather than by initial and achieved vitamin D status is another common mistake in vitamin D RCT analysis. Those common failures have been discussed in two 2022 reviews [95,96].
Risk rates for the incidence of stroke and other CVD events increase rapidly as serum 25(OH)D concentrations fall below 20 ng/mL [23,97]. Thus, for example, the large VITAL study [51], which enrolled participants whose mean baseline 25(OH)D concentration was 31 ng/mL in the vitamin D treatment arm, had no chance of finding any significant reduction in CVD from supplementation at 2000 IU/day of vitamin D3, The failure to recruit participants with deficiency and permitting those in the placebo arm to take up to 600 or, for those over 70 years, 800 IU/day of vitamin D, also reduced the possibility of any significant findings being able to emerge from the VITAL trial.
A stratified randomized field trial of vitamin D supplementation for pregnant women in Iran [44] shows how to design and carry out any trial of vitamin D RCT more appropriately [though in that instance for pregnancy complications rather than for stroke]. Firstly, participants had mean 25(OH)D concentrations of about 11 ng/mL. Second, serum 25(OH)D concentrations for the vitamin D treatment arm were measured during the trial and used to adjust vitamin D doses so as to ensure that 25(OH)D concentrations greater than 20 ng/mL were achieved and maintained throughout the trial, as confirmed by follow-up 25(OH)D values, while participants in the control arm received no vitamin D supplements. Outcomes for gestational diabetes, pre-eclampsia, and preterm delivery were then evaluated with respect to achieved 25(OH)D concentrations, and highly significant reductions in those outcomes were found. Adverse pregnancy outcomes, including pre-eclampsia, gestational diabetes mellitus, and preterm delivery, were decreased by 60% (OR = 0.4 [95% CI, 0.3–0.6]), 50% (OR = 0.5 [95% CI, 0.3–0.9]), and 40% (OR = 0.6 [95% CI, 0.4–0.8]), respectively, in the screening site. Those findings were in contrast with results from the standard vitamin D RCTs for pregnant women that were used to prepare a recent Cochrane review [98]. It reported, “The evidence is very uncertain about the effect of supplementation with vitamin D during pregnancy compared to placebo or no intervention on pre-eclampsia (risk ratio (RR) 0.53, 95% confidence interval (CI) 0.21 to 1.33; 1 study, 165 women), gestational diabetes (RR 0.53, 95% CI 0.03 to 8.28; 1 study, 165 women), preterm birth (<37 weeks) (RR 0.76, 95% CI 0.25 to 2.33; 3 studies, 1368 women)”.
The mainstream medical system relies on RCTs to show effectiveness and to ensure limited adverse effects before approving pharmaceutical drugs for general use, but, as discussed, vitamin D RCTs based on guidelines for pharmaceutical drugs are not appropriate. In addition, Hill in 1965 proposed another way to examine causality in a biological system [99]. The criteria appropriate for vitamin D included strength of association, consistent findings in different populations, temporality, biological gradient, plausibility (e.g., mechanisms known), coherence with known science of the day, experiment, and analogy. Necessary adjustment for confounding factors and bias were added later [100]. A 2024 review discussed how those considerations have influenced epidemiologic methods [101]. For vitamin D, examination of Hill’s criteria for causality of inadequate vitamin D provision for various health outcomes (diseases) [96], including cardiovascular disease [102], suggested that the criteria were generally satisfied. Ironically, the main limitation to using Hill’s criteria of causation was in finding reliable evidence from experimentation owing to the problems with RCTs, as discussed above and as recently reviewed [87].
It is notable that when results from RCTs are not available, observational studies have been used to evaluate and establish causal relationships. This was performed, for example, for smoking as a primary cause of lung cancer by Doll and Hill [103,104]. Table 9 uses Hill’s criteria to briefly outline the evidence that vitamin D reduces risk of stroke. While most of the criteria appear to be satisfied, experimental verification has not been satisfied. Again, the most likely reason is that RCTs have not found that vitamin D reduces risk of stroke or MACEs, again because they have been based on guidelines for pharmaceutical drugs rather than nutrients [93,95,96]; in addition, no RCTs have enrolled sufficient numbers of participants low 25(OH)D concentrations, i.e., at less than 15 ng/mL. As Hill noted, not all criteria have to be satisfied for causality to be likely, though the more that are, the stronger the claim [99].

Table 9.
Evaluation of findings relating serum 25(OH)D concentration to the risk of stroke and of major cardiovascular disease events using Hill’s criteria for causality in a biological system [99].
Strengths and Weaknesses
Strengths include using several cohort studies in analysis and analyzing the meta-analysis results in terms of the follow-up periods used.
One limitation is that the analyses are based on observational studies. Another is that the findings relating vitamin D status to stroke risks are not supported by RCTs. A third is that nearly all of the studies are from Western developed countries. As a result, they may not be applicable to developing countries. Also, most CVD events are in part related to Western dietary patterns, although this has not been investigated in this work.
5. Conclusions
From our findings, the risks of stroke and of acute cardiovascular events are likely to be minimized by ensuring population serum 25(OH)D concentrations are maintained at or above 20–30 ng/mL. In normal-weight people, that level can be achieved with supplementation of at least 1000 IU/day of vitamin D3, though 2000 IU/day would be more reliable [107]. Obese people, however, should take 2–3 times higher doses, and overweight individuals should take 1.5 times as much [108].
Author Contributions
Writing—original draft preparation, W.B.G. Writing the final article and final editing, W.B.G. and B.J.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Data Availability Statement
The original contributions presented in the study are included in the article or in the references provided. Further inquiries can be directed to the corresponding author.
Conflicts of Interest
W.B.G. had funding in prior years from Bio-Tech Pharmacal Inc. (Fayetteville, AR, USA). The funder had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results. B.J.B. has no conflicts of interest to declare.
References
- Clarke, R.; Shipley, M.; Lewington, S.; Youngman, L.; Collins, R.; Marmot, M.; Peto, R. Underestimation of risk associations due to regression dilution in long-term follow-up of prospective studies. Am. J. Epidemiol. 1999, 150, 341–353. [Google Scholar] [CrossRef] [PubMed]
- Jorde, R.; Sneve, M.; Hutchinson, M.; Emaus, N.; Figenschau, Y.; Grimnes, G. Tracking of serum 25-hydroxyvitamin D levels during 14 years in a population-based study and during 12 months in an intervention study. Am. J. Epidemiol. 2010, 171, 903–908. [Google Scholar] [CrossRef] [PubMed]
- Grant, W.B. Effect of interval between serum draw and follow-up period on relative risk of cancer incidence with respect to 25-hydroxyvitamin D level: Implications for meta-analyses and setting vitamin D guidelines. Dermatoendocrinol 2011, 3, 199–204. [Google Scholar] [CrossRef] [PubMed]
- Grant, W.B. Effect of follow-up time on the relation between prediagnostic serum 25-hydroxyvitamin D and all-cause mortality rate. Dermatoendocrinol 2012, 4, 198–202. [Google Scholar] [CrossRef] [PubMed]
- McCullough, M.L.; Zoltick, E.S.; Weinstein, S.J.; Fedirko, V.; Wang, M.; Cook, N.R.; Eliassen, A.H.; Zeleniuch-Jacquotte, A.; Agnoli, C.; Albanes, D.; et al. Circulating Vitamin D and Colorectal Cancer Risk: An International Pooling Project of 17 Cohorts. J. Natl. Cancer Inst. 2019, 111, 158–169. [Google Scholar] [CrossRef] [PubMed]
- Munoz, A.; Grant, W.B. Vitamin D and Cancer: An Historical Overview of the Epidemiology and Mechanisms. Nutrients 2022, 14, 1448. [Google Scholar] [CrossRef]
- Zhang, X.X.; Wang, H.R.; Meng, W.; Hu, Y.Z.; Sun, H.M.; Feng, Y.X.; Jia, J.J. Association of Vitamin D Levels with Risk of Cognitive Impairment and Dementia: A Systematic Review and Meta-Analysis of Prospective Studies. J. Alzheimers Dis. 2024, 98, 373–385. [Google Scholar] [CrossRef]
- Grant, W.B. Follow-up period affects the association between serum 25-hydroxyvitamin D concentration and incidence of dementia, Alzheimer’s disease, and cognitive impairment. Nutrients 2024, 16, 3211. [Google Scholar] [CrossRef]
- Saini, V.; Guada, L.; Yavagal, D.R. Global Epidemiology of Stroke and Access to Acute Ischemic Stroke Interventions. Neurology 2021, 97, S6–S16. [Google Scholar] [CrossRef]
- Wafa, H.A.; Wolfe, C.D.A.; Emmett, E.; Roth, G.A.; Johnson, C.O.; Wang, Y. Burden of Stroke in Europe: Thirty-Year Projections of Incidence, Prevalence, Deaths, and Disability-Adjusted Life Years. Stroke 2020, 51, 2418–2427. [Google Scholar] [CrossRef]
- Tong, T.Y.N.; Appleby, P.N.; Key, T.J.; Dahm, C.C.; Overvad, K.; Olsen, A.; Tjonneland, A.; Katzke, V.; Kuhn, T.; Boeing, H.; et al. The associations of major foods and fibre with risks of ischaemic and haemorrhagic stroke: A prospective study of 418 329 participants in the EPIC cohort across nine European countries. Eur. Heart J. 2020, 41, 2632–2640. [Google Scholar] [CrossRef] [PubMed]
- Martin, S.S.; Aday, A.W.; Almarzooq, Z.I.; Anderson, C.A.M.; Arora, P.; Avery, C.L.; Baker-Smith, C.M.; Barone Gibbs, B.; Beaton, A.Z.; Boehme, A.K.; et al. 2024 Heart Disease and Stroke Statistics: A Report of US and Global Data From the American Heart Association. Circulation 2024, 149, e347–e913. [Google Scholar] [CrossRef] [PubMed]
- Su, C.; Jin, B.; Xia, H.; Zhao, K. Association between Vitamin D and Risk of Stroke: A PRISMA-Compliant Systematic Review and Meta-Analysis. Eur. Neurol. 2021, 84, 399–408. [Google Scholar] [CrossRef] [PubMed]
- Xiong, J.; Zhao, C.; Li, J.; Li, Y. A systematic review and meta-analysis of the linkage between low vitamin D and the risk as well as the prognosis of stroke. Brain Behav. 2024, 14, e3577. [Google Scholar] [CrossRef]
- Zhang, H.; Wang, P.; Jie, Y.; Sun, Y.; Wang, X.; Fan, Y. Predictive value of 25-hydroxyvitamin D level in patients with coronary artery disease: A meta-analysis. Front. Nutr. 2022, 9, 984487. [Google Scholar] [CrossRef]
- Anderson, J.L.; May, H.T.; Horne, B.D.; Bair, T.L.; Hall, N.L.; Carlquist, J.F.; Lappe, D.L.; Muhlestein, J.B.; Intermountain Heart Collaborative (IHC) Study Group. Relation of vitamin D deficiency to cardiovascular risk factors, disease status, and incident events in a general healthcare population. Am. J. Cardiol. 2010, 106, 963–968. [Google Scholar] [CrossRef]
- Judd, S.E.; Morgan, C.J.; Panwar, B.; Howard, V.J.; Wadley, V.G.; Jenny, N.S.; Kissela, B.M.; Gutierrez, O.M. Vitamin D deficiency and incident stroke risk in community-living black and white adults. Int. J. Stroke 2016, 11, 93–102. [Google Scholar] [CrossRef]
- Zittermann, A.; Morshuis, M.; Kuhn, J.; Pilz, S.; Ernst, J.B.; Oezpeker, C.; Dreier, J.; Knabbe, C.; Gummert, J.F.; Milting, H. Vitamin D metabolites and fibroblast growth factor-23 in patients with left ventricular assist device implants: Association with stroke and mortality risk. Eur. J. Nutr. 2016, 55, 305–313. [Google Scholar] [CrossRef]
- Drechsler, C.; Pilz, S.; Obermayer-Pietsch, B.; Verduijn, M.; Tomaschitz, A.; Krane, V.; Espe, K.; Dekker, F.; Brandenburg, V.; Marz, W.; et al. Vitamin D deficiency is associated with sudden cardiac death, combined cardiovascular events, and mortality in haemodialysis patients. Eur. Heart J. 2010, 31, 2253–2261. [Google Scholar] [CrossRef]
- Bolland, M.J.; Bacon, C.J.; Horne, A.M.; Mason, B.H.; Ames, R.W.; Wang, T.K.; Grey, A.B.; Gamble, G.D.; Reid, I.R. Vitamin D insufficiency and health outcomes over 5 y in older women. Am. J. Clin. Nutr. 2010, 91, 82–89. [Google Scholar] [CrossRef]
- Perna, L.; Schottker, B.; Holleczek, B.; Brenner, H. Serum 25-hydroxyvitamin D and incidence of fatal and nonfatal cardiovascular events: A prospective study with repeated measurements. J. Clin. Endocrinol. Metab. 2013, 98, 4908–4915. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, T.; Kaaks, R.; Teucher, B.; Hirche, F.; Dierkes, J.; Weikert, C.; Katzke, V.; Boeing, H.; Stangl, G.I.; Buijsse, B. Plasma 25-hydroxyvitamin D and its genetic determinants in relation to incident myocardial infarction and stroke in the European prospective investigation into cancer and nutrition (EPIC)-Germany study. PLoS ONE 2013, 8, e69080. [Google Scholar] [CrossRef] [PubMed]
- Welles, C.C.; Whooley, M.A.; Karumanchi, S.A.; Hod, T.; Thadhani, R.; Berg, A.H.; Ix, J.H.; Mukamal, K.J. Vitamin D deficiency and cardiovascular events in patients with coronary heart disease: Data from the Heart and Soul Study. Am. J. Epidemiol. 2014, 179, 1279–1287. [Google Scholar] [CrossRef] [PubMed]
- Afzal, S.; Nordestgaard, B.G. Vitamin D, Hypertension, and Ischemic Stroke in 116 655 Individuals From the General Population: A Genetic Study. Hypertension 2017, 70, 499–507. [Google Scholar] [CrossRef] [PubMed]
- Marniemi, J.; Alanen, E.; Impivaara, O.; Seppanen, R.; Hakala, P.; Rajala, T.; Ronnemaa, T. Dietary and serum vitamins and minerals as predictors of myocardial infarction and stroke in elderly subjects. Nutr. Metab. Cardiovasc. Dis. 2005, 15, 188–197. [Google Scholar] [CrossRef]
- Skaaby, T.; Husemoen, L.L.; Pisinger, C.; Jorgensen, T.; Thuesen, B.H.; Fenger, M.; Linneberg, A. Vitamin D status and incident cardiovascular disease and all-cause mortality: A general population study. Endocrine 2013, 43, 618–625. [Google Scholar] [CrossRef]
- Leung, R.Y.; Han, Y.; Sing, C.W.; Cheung, B.M.; Wong, I.C.; Tan, K.C.; Kung, A.W.; Cheung, C.L. Serum 25-hydroxyvitamin D and the risk of stroke in Hong Kong Chinese. Thromb. Haemost. 2017, 117, 158–163. [Google Scholar] [CrossRef]
- Berghout, B.P.; Fani, L.; Heshmatollah, A.; Koudstaal, P.J.; Ikram, M.A.; Zillikens, M.C.; Ikram, M.K. Vitamin D Status and Risk of Stroke: The Rotterdam Study. Stroke 2019, 50, 2293–2298. [Google Scholar] [CrossRef]
- Schierbeck, L.L.; Rejnmark, L.; Tofteng, C.L.; Stilgren, L.; Eiken, P.; Mosekilde, L.; Kober, L.; Jensen, J.E. Vitamin D deficiency in postmenopausal, healthy women predicts increased cardiovascular events: A 16-year follow-up study. Eur. J. Endocrinol. 2012, 167, 553–560. [Google Scholar] [CrossRef]
- Schneider, A.L.; Lutsey, P.L.; Selvin, E.; Mosley, T.H.; Sharrett, A.R.; Carson, K.A.; Post, W.S.; Pankow, J.S.; Folsom, A.R.; Gottesman, R.F.; et al. Vitamin D, vitamin D binding protein gene polymorphisms, race and risk of incident stroke: The Atherosclerosis Risk in Communities (ARIC) study. Eur. J. Neurol. 2015, 22, 1220–1227. [Google Scholar] [CrossRef]
- Guo, J.; Cockcroft, J.R.; Elwood, P.C.; Pickering, J.E.; Lovegrove, J.A.; Givens, D.I. Vitamin D intake and risk of CVD and all-cause mortality: Evidence from the Caerphilly Prospective Cohort Study. Public Health Nutr. 2017, 20, 2744–2753. [Google Scholar] [CrossRef]
- Leu Agelii, M.; Lehtinen-Jacks, S.; Zetterberg, H.; Sundh, V.; Bjorkelund, C.; Lissner, L. Low vitamin D status in relation to cardiovascular disease and mortality in Swedish women—Effect of extended follow-up. Nutr. Metab. Cardiovasc. Dis. 2017, 27, 1143–1151. [Google Scholar] [CrossRef] [PubMed]
- Sheerah, H.A.; Eshak, E.S.; Cui, R.; Imano, H.; Iso, H.; Tamakoshi, A.; Japan Collaborative Cohort Study Group. Relationship Between Dietary Vitamin D and Deaths From Stroke and Coronary Heart Disease: The Japan Collaborative Cohort Study. Stroke 2018, 49, 454–457. [Google Scholar] [CrossRef] [PubMed]
- Kojima, G.; Bell, C.; Abbott, R.D.; Launer, L.; Chen, R.; Motonaga, H.; Ross, G.W.; Curb, J.D.; Masaki, K. Low dietary vitamin D predicts 34-year incident stroke: The Honolulu Heart Program. Stroke 2012, 43, 2163–2167. [Google Scholar] [CrossRef] [PubMed]
- The Blood Pressure Lowering Treatment Trialists’ Collaboration. Pharmacological blood pressure lowering for primary and secondary prevention of cardiovascular disease across different levels of blood pressure: An individual participant-level data meta-analysis. Lancet 2021, 397, 1625–1636. [Google Scholar] [CrossRef] [PubMed]
- De Metrio, M.; Milazzo, V.; Rubino, M.; Cabiati, A.; Moltrasio, M.; Marana, I.; Campodonico, J.; Cosentino, N.; Veglia, F.; Bonomi, A.; et al. Vitamin D plasma levels and in-hospital and 1-year outcomes in acute coronary syndromes: A prospective study. Medicine 2015, 94, e857. [Google Scholar] [CrossRef]
- Beska, B.; Chan, D.; Gu, S.; Qiu, W.; Mossop, H.; Neely, D.; Kunadian, V. The association between vitamin D status and clinical events in high-risk older patients with non-ST elevation acute coronary syndrome undergoing invasive management. PLoS ONE 2019, 14, e0217476. [Google Scholar] [CrossRef]
- Ng, L.L.; Sandhu, J.K.; Squire, I.B.; Davies, J.E.; Jones, D.J. Vitamin D and prognosis in acute myocardial infarction. Int. J. Cardiol. 2013, 168, 2341–2346. [Google Scholar] [CrossRef]
- Aleksova, A.; Ferro, F.; Gagno, G.; Padoan, L.; Saro, R.; Santon, D.; Stenner, E.; Barbati, G.; Cappelletto, C.; Rossi, M.; et al. Diabetes Mellitus and Vitamin D Deficiency:Comparable Effect on Survival and a DeadlyAssociation after a Myocardial Infarction. J. Clin. Med. 2020, 9, 2127. [Google Scholar] [CrossRef]
- Verdoia, M.; Nardin, M.; Rolla, R.; Negro, F.; Gioscia, R.; Afifeh, A.M.S.; Viglione, F.; Suryapranata, H.; Marcolongo, M.; De Luca, G.; et al. Prognostic impact of Vitamin D deficiency in patients with coronary artery disease undergoing percutaneous coronary intervention. Eur. J. Intern. Med. 2021, 83, 62–67. [Google Scholar] [CrossRef]
- Grandi, N.C.; Breitling, L.P.; Vossen, C.Y.; Hahmann, H.; Wusten, B.; Marz, W.; Rothenbacher, D.; Brenner, H. Serum vitamin D and risk of secondary cardiovascular disease events in patients with stable coronary heart disease. Am. Heart J. 2010, 159, 1044–1051. [Google Scholar] [CrossRef] [PubMed]
- Shi, H.; Chen, H.; Zhang, Y.; Li, J.; Fu, K.; Xue, W.; Teng, W.; Tian, L. 25-Hydroxyvitamin D level, vitamin D intake, and risk of stroke: A dose-response meta-analysis. Clin. Nutr. 2020, 39, 2025–2034. [Google Scholar] [CrossRef] [PubMed]
- Grant, W.B.; Fakhoury, H.M.A.; Karras, S.N.; Al Anouti, F.; Bhattoa, H.P. Variations in 25-Hydroxyvitamin D in Countries from the Middle East and Europe: The Roles of UVB Exposure and Diet. Nutrients 2019, 11, 2065. [Google Scholar] [CrossRef] [PubMed]
- Rostami, M.; Tehrani, F.R.; Simbar, M.; Bidhendi Yarandi, R.; Minooee, S.; Hollis, B.W.; Hosseinpanah, F. Effectiveness of Prenatal Vitamin D Deficiency Screening and Treatment Program: A Stratified Randomized Field Trial. J. Clin. Endocrinol. Metab. 2018, 103, 2936–2948. [Google Scholar] [CrossRef]
- Marti-Soler, H.; Gonseth, S.; Gubelmann, C.; Stringhini, S.; Bovet, P.; Chen, P.C.; Wojtyniak, B.; Paccaud, F.; Tsai, D.H.; Zdrojewski, T.; et al. Seasonal variation of overall and cardiovascular mortality: A study in 19 countries from different geographic locations. PLoS ONE 2014, 9, e113500. [Google Scholar] [CrossRef]
- Hypponen, E.; Power, C. Hypovitaminosis D in British adults at age 45 y: Nationwide cohort study of dietary and lifestyle predictors. Am. J. Clin. Nutr. 2007, 85, 860–868. [Google Scholar] [CrossRef]
- Kroll, M.H.; Bi, C.; Garber, C.C.; Kaufman, H.W.; Liu, D.; Caston-Balderrama, A.; Zhang, K.; Clarke, N.; Xie, M.; Reitz, R.E.; et al. Temporal relationship between vitamin D status and parathyroid hormone in the United States. PLoS ONE 2015, 10, e0118108. [Google Scholar] [CrossRef]
- Grant, W.B.; Garland, C.F. The association of solar ultraviolet B (UVB) with reducing risk of cancer: Multifactorial ecologic analysis of geographic variation in age-adjusted cancer mortality rates. Anticancer Res. 2006, 26, 2687–2699. [Google Scholar]
- Garland, C.F.; Gorham, E.D. Dose-response of serum 25-hydroxyvitamin D in association with risk of colorectal cancer: A meta-analysis. J. Steroid Biochem. Mol. Biol. 2017, 168, 1–8. [Google Scholar] [CrossRef]
- McDonnell, S.L.; Baggerly, C.A.; French, C.B.; Baggerly, L.L.; Garland, C.F.; Gorham, E.D.; Hollis, B.W.; Trump, D.L.; Lappe, J.M. Breast cancer risk markedly lower with serum 25-hydroxyvitamin D concentrations >/=60 vs. <20 ng/ml (150 vs. 50 nmol/L): Pooled analysis of two randomized trials and a prospective cohort. PLoS ONE 2018, 13, e0199265. [Google Scholar] [CrossRef]
- Manson, J.E.; Cook, N.R.; Lee, I.M.; Christen, W.; Bassuk, S.S.; Mora, S.; Gibson, H.; Gordon, D.; Copeland, T.; D’Agostino, D.; et al. Vitamin D Supplements and Prevention of Cancer and Cardiovascular Disease. N. Engl. J. Med. 2019, 380, 33–44. [Google Scholar] [CrossRef] [PubMed]
- Jia, J.; Hu, J.; Huo, X.; Miao, R.; Zhang, Y.; Ma, F. Effects of vitamin D supplementation on cognitive function and blood Abeta-related biomarkers in older adults with Alzheimer’s disease: A randomised, double-blind, placebo-controlled trial. J. Neurol. Neurosurg. Psychiatry 2019, 90, 1347–1352. [Google Scholar] [CrossRef] [PubMed]
- Jamilian, H.; Amirani, E.; Milajerdi, A.; Kolahdooz, F.; Mirzaei, H.; Zaroudi, M.; Ghaderi, A.; Asemi, Z. The effects of vitamin D supplementation on mental health, and biomarkers of inflammation and oxidative stress in patients with psychiatric disorders: A systematic review and meta-analysis of randomized controlled trials. Prog. Neuropsychopharmacol. Biol. Psychiatry 2019, 94, 109651. [Google Scholar] [CrossRef] [PubMed]
- Vellekkatt, F.; Menon, V.; Rajappa, M.; Sahoo, J. Effect of adjunctive single dose parenteral Vitamin D supplementation in major depressive disorder with concurrent vitamin D deficiency: A double-blind randomized placebo-controlled trial. J. Psychiatr. Res. 2020, 129, 250–256. [Google Scholar] [CrossRef]
- Ghaderi, A.; Rasouli-Azad, M.; Farhadi, M.H.; Mirhosseini, N.; Motmaen, M.; Pishyareh, E.; Omidi, A.; Asemi, Z. Exploring the Effects of Vitamin D Supplementation on Cognitive Functions and Mental Health Status in Subjects Under Methadone Maintenance Treatment. J. Addict. Med. 2020, 14, 18–25. [Google Scholar] [CrossRef]
- Castle, M.; Fiedler, N.; Pop, L.C.; Schneider, S.J.; Schlussel, Y.; Sukumar, D.; Hao, L.; Shapses, S.A. Three Doses of Vitamin D and Cognitive Outcomes in Older Women: A Double-Blind Randomized Controlled Trial. J. Gerontol. A Biol. Sci. Med. Sci. 2020, 75, 835–842. [Google Scholar] [CrossRef] [PubMed]
- Rooney, M.R.; Harnack, L.; Michos, E.D.; Ogilvie, R.P.; Sempos, C.T.; Lutsey, P.L. Trends in Use of High-Dose Vitamin D Supplements Exceeding 1000 or 4000 International Units Daily, 1999–2014. JAMA 2017, 317, 2448–2450. [Google Scholar] [CrossRef]
- Alhabeeb, H.; Kord-Varkaneh, H.; Tan, S.C.; Gaman, M.A.; Otayf, B.Y.; Qadri, A.A.; Alomar, O.; Salem, H.; Al-Badawi, I.A.; Abu-Zaid, A. The influence of omega-3 supplementation on vitamin D levels in humans: A systematic review and dose-response meta-analysis of randomized controlled trials. Crit. Rev. Food Sci. Nutr. 2022, 62, 3116–3123. [Google Scholar] [CrossRef]
- Perez-Lopez, F.R.; Chedraui, P.; Pilz, S. Vitamin D supplementation after the menopause. Ther. Adv. Endocrinol. Metab. 2020, 11, 2042018820931291. [Google Scholar] [CrossRef]
- Aspell, N.; Laird, E.; Healy, M.; Shannon, T.; Lawlor, B.; O’Sullivan, M. The Prevalence and Determinants of Vitamin D Status in Community-Dwelling Older Adults: Results from the English Longitudinal Study of Ageing (ELSA). Nutrients 2019, 11, 1253. [Google Scholar] [CrossRef]
- Engelsen, O. The relationship between ultraviolet radiation exposure and vitamin D status. Nutrients 2010, 2, 482–495. [Google Scholar] [CrossRef]
- Chalcraft, J.R.; Cardinal, L.M.; Wechsler, P.J.; Hollis, B.W.; Gerow, K.G.; Alexander, B.M.; Keith, J.F.; Larson-Meyer, D.E. Vitamin D Synthesis Following a Single Bout of Sun Exposure in Older and Younger Men and Women. Nutrients 2020, 12, 2237. [Google Scholar] [CrossRef] [PubMed]
- Crowe, F.L.; Steur, M.; Allen, N.E.; Appleby, P.N.; Travis, R.C.; Key, T.J. Plasma concentrations of 25-hydroxyvitamin D in meat eaters, fish eaters, vegetarians and vegans: Results from the EPIC-Oxford study. Public Health Nutr. 2011, 14, 340–346. [Google Scholar] [CrossRef] [PubMed]
- Jorde, R.; Sneve, M.; Emaus, N.; Figenschau, Y.; Grimnes, G. Cross-sectional and longitudinal relation between serum 25-hydroxyvitamin D and body mass index: The Tromso study. Eur. J. Nutr. 2010, 49, 401–407. [Google Scholar] [CrossRef] [PubMed]
- Maghfour, J.; Boothby-Shoemaker, W.; Lim, H.W. Evaluating the USA population’s interest in sunscreen: A Google Trends analysis. Clin. Exp. Dermatol. 2022, 47, 757–759. [Google Scholar] [CrossRef] [PubMed]
- Ngoc, L.T.N.; Tan, V.V.; Moon, J.Y.; Chae, M.; Park, D.; Lee, Y.-C. Recent Trends of Sunscreen Cosmetic: An Update Review. Cosmetics 2019, 6, 64. [Google Scholar] [CrossRef]
- Okan, F.; Okan, S.; Zincir, H. Effect of Sunlight Exposure on Vitamin D Status of Individuals Living in a Nursing Home and Their Own Homes. J. Clin. Densitom. 2020, 23, 21–28. [Google Scholar] [CrossRef]
- Makariou, S.E.; Michel, P.; Tzoufi, M.S.; Challa, A.; Milionis, H.J. Vitamin D and stroke: Promise for prevention and better outcome. Curr. Vasc. Pharmacol. 2014, 12, 117–124. [Google Scholar] [CrossRef]
- Haussler, M.R.; Haussler, C.A.; Jurutka, P.W.; Thompson, P.D.; Hsieh, J.C.; Remus, L.S.; Selznick, S.H.; Whitfield, G.K. The vitamin D hormone and its nuclear receptor: Molecular actions and disease states. J. Endocrinol. 1997, 154, S57–S73. [Google Scholar]
- Kiraly, S.J.; Kiraly, M.A.; Hawe, R.D.; Makhani, N. Vitamin D as a neuroactive substance: Review. Sci. World J. 2006, 6, 125–139. [Google Scholar] [CrossRef]
- Shirvani, A.; Kalajian, T.A.; Song, A.; Holick, M.F. Disassociation of Vitamin D’s Calcemic Activity and Non-calcemic Genomic Activity and Individual Responsiveness: A Randomized Controlled Double-Blind Clinical Trial. Sci. Rep. 2019, 9, 17685. [Google Scholar] [CrossRef] [PubMed]
- Timms, P.M.; Mannan, N.; Hitman, G.A.; Noonan, K.; Mills, P.G.; Syndercombe-Court, D.; Aganna, E.; Price, C.P.; Boucher, B.J. Circulating MMP9, vitamin D and variation in the TIMP-1 response with VDR genotype: Mechanisms for inflammatory damage in chronic disorders? QJM 2002, 95, 787–796. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Li, X.; Feng, Y.; Dong, G.; Wang, Y.; Yang, J. The Role of Matrix Metalloproteinase-9 in Atherosclerotic Plaque Instability. Mediat. Inflamm. 2020, 2020, 3872367. [Google Scholar] [CrossRef]
- Xu, T.; Yu, X.; Ou, S.; Liu, X.; Yuan, J.; Tan, X.; Chen, Y. Adherence to Antihypertensive Medications and Stroke Risk: A Dose-Response Meta-Analysis. J. Am. Heart Assoc. 2017, 6, 7. [Google Scholar] [CrossRef]
- Zhang, Y.; Tan, H.; Tang, J.; Li, J.; Chong, W.; Hai, Y.; Feng, Y.; Lunsford, L.D.; Xu, P.; Jia, D.; et al. Effects of Vitamin D Supplementation on Prevention of Type 2 Diabetes in Patients With Prediabetes: A Systematic Review and Meta-analysis. Diabetes Care 2020, 43, 1650–1658. [Google Scholar] [CrossRef] [PubMed]
- Pfeifer, M.; Begerow, B.; Minne, H.W.; Nachtigall, D.; Hansen, C. Effects of a short-term vitamin D(3) and calcium supplementation on blood pressure and parathyroid hormone levels in elderly women. J. Clin. Endocrinol. Metab. 2001, 86, 1633–1637. [Google Scholar] [CrossRef][Green Version]
- Forman, J.P.; Scott, J.B.; Ng, K.; Drake, B.F.; Suarez, E.G.; Hayden, D.L.; Bennett, G.G.; Chandler, P.D.; Hollis, B.W.; Emmons, K.M.; et al. Effect of vitamin D supplementation on blood pressure in blacks. Hypertension 2013, 61, 779–785. [Google Scholar] [CrossRef] [PubMed]
- Sluyter, J.D.; Camargo, C.A., Jr.; Stewart, A.W.; Waayer, D.; Lawes, C.M.M.; Toop, L.; Khaw, K.T.; Thom, S.A.M.; Hametner, B.; Wassertheurer, S.; et al. Effect of Monthly, High-Dose, Long-Term Vitamin D Supplementation on Central Blood Pressure Parameters: A Randomized Controlled Trial Substudy. J. Am. Heart Assoc. 2017, 6, 10. [Google Scholar] [CrossRef]
- Mirhosseini, N.; Vatanparast, H.; Kimball, S.M. The Association between Serum 25(OH)D Status and Blood Pressure in Participants of a Community-Based Program Taking Vitamin D Supplements. Nutrients 2017, 9, 1244. [Google Scholar] [CrossRef]
- Latic, N.; Erben, R.G. Vitamin D and Cardiovascular Disease, with Emphasis on Hypertension, Atherosclerosis, and Heart Failure. Int. J. Mol. Sci. 2020, 21, 6483. [Google Scholar] [CrossRef]
- Della Nera, G.; Sabatino, L.; Gaggini, M.; Gorini, F.; Vassalle, C. Vitamin D Determinants, Status, and Antioxidant/Anti-inflammatory-Related Effects in Cardiovascular Risk and Disease: Not the Last Word in the Controversy. Antioxidants 2023, 12, 948. [Google Scholar] [CrossRef]
- Marek, K.; Cichon, N.; Saluk-Bijak, J.; Bijak, M.; Miller, E. The Role of Vitamin D in Stroke Prevention and the Effects of Its Supplementation for Post-Stroke Rehabilitation: A Narrative Review. Nutrients 2022, 14, 2761. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.H.; Meza, C.A.; Clarke, H.; Kim, J.S.; Hickner, R.C. Vitamin D and Endothelial Function. Nutrients 2020, 12, 575. [Google Scholar] [CrossRef]
- Contreras-Bolivar, V.; Garcia-Fontana, B.; Garcia-Fontana, C.; Munoz-Torres, M. Mechanisms Involved in the Relationship between Vitamin D and Insulin Resistance: Impact on Clinical Practice. Nutrients 2021, 13, 3491. [Google Scholar] [CrossRef] [PubMed]
- Surdu, A.M.; Pinzariu, O.; Ciobanu, D.M.; Negru, A.G.; Cainap, S.S.; Lazea, C.; Iacob, D.; Saraci, G.; Tirinescu, D.; Borda, I.M.; et al. Vitamin D and Its Role in the Lipid Metabolism and the Development of Atherosclerosis. Biomedicines 2021, 9, 172. [Google Scholar] [CrossRef]
- Yarlagadda, K.; Ma, N.; Dore, S. Vitamin D and Stroke: Effects on Incidence, Severity, and Outcome and the Potential Benefits of Supplementation. Front. Neurol. 2020, 11, 384. [Google Scholar] [CrossRef]
- Legarth, C.; Grimm, D.; Kruger, M.; Infanger, M.; Wehland, M. Potential Beneficial Effects of Vitamin D in Coronary Artery Disease. Nutrients 2019, 12, 99. [Google Scholar] [CrossRef]
- de la Guia-Galipienso, F.; Martinez-Ferran, M.; Vallecillo, N.; Lavie, C.J.; Sanchis-Gomar, F.; Pareja-Galeano, H. Vitamin D and cardiovascular health. Clin. Nutr. 2021, 40, 2946–2957. [Google Scholar] [CrossRef] [PubMed]
- Dawson-Hughes, B.; Staten, M.A.; Knowler, W.C.; Nelson, J.; Vickery, E.M.; LeBlanc, E.S.; Neff, L.M.; Park, J.; Pittas, A.G.; Group, D.d.R. Intratrial Exposure to Vitamin D and New-Onset Diabetes Among Adults With Prediabetes: A Secondary Analysis From the Vitamin D and Type 2 Diabetes (D2d) Study. Diabetes Care 2020, 43, 2916–2922. [Google Scholar] [CrossRef]
- Nudy, M.; Krakowski, G.; Ghahramani, M.; Ruzieh, M.; Foy, A.J. Vitamin D supplementation, cardiac events and stroke: A systematic review and meta-regression analysis. Int. J. Cardiol. Heart Vasc. 2020, 28, 100537. [Google Scholar] [CrossRef]
- Cui, P.; Hou, H.; Song, B.; Xia, Z.; Xu, Y. Vitamin D and ischemic stroke—Association, mechanisms, and therapeutics. Ageing Res. Rev. 2024, 96, 102244. [Google Scholar] [CrossRef]
- Boucher, B.J. Why do so many trials of vitamin D supplementation fail? Endocr. Connect. 2020, 9, R195–R206. [Google Scholar] [CrossRef]
- Heaney, R.P. Guidelines for optimizing design and analysis of clinical studies of nutrient effects. Nutr. Rev. 2014, 72, 48–54. [Google Scholar] [CrossRef]
- Grant, W.B.; Boucher, B.J.; Bhattoa, H.P.; Lahore, H. Why vitamin D clinical trials should be based on 25-hydroxyvitamin D concentrations. J. Steroid Biochem. Mol. Biol. 2018, 177, 266–269. [Google Scholar] [CrossRef]
- Pilz, S.; Trummer, C.; Theiler-Schwetz, V.; Grubler, M.R.; Verheyen, N.D.; Odler, B.; Karras, S.N.; Zittermann, A.; Marz, W. Critical Appraisal of Large Vitamin D Randomized Controlled Trials. Nutrients 2022, 14, 303. [Google Scholar] [CrossRef]
- Grant, W.B.; Boucher, B.J.; Al Anouti, F.; Pilz, S. Comparing the Evidence from Observational Studies and Randomized Controlled Trials for Nonskeletal Health Effects of Vitamin D. Nutrients 2022, 14, 3811. [Google Scholar] [CrossRef]
- Wang, L.; Song, Y.; Manson, J.E.; Pilz, S.; Marz, W.; Michaelsson, K.; Lundqvist, A.; Jassal, S.K.; Barrett-Connor, E.; Zhang, C.; et al. Circulating 25-hydroxy-vitamin D and risk of cardiovascular disease: A meta-analysis of prospective studies. Circ. Cardiovasc. Qual. Outcomes 2012, 5, 819–829. [Google Scholar] [CrossRef]
- Palacios, C.; Kostiuk, L.L.; Cuthbert, A.; Weeks, J. Vitamin D supplementation for women during pregnancy. Cochrane Database Syst. Rev. 2024, 7, CD008873. [Google Scholar] [CrossRef]
- Hill, A.B. The Environment and Disease: Association or Causation? Proc. R. Soc. Med. 1965, 58, 295–300. [Google Scholar] [CrossRef]
- Potischman, N.; Weed, D.L. Causal criteria in nutritional epidemiology. Am. J. Clin. Nutr. 1999, 69, 1309S–1314S. [Google Scholar] [CrossRef]
- Lesko, C.R.; Fox, M.P. An evolved interpretation of Austin Bradford Hill’s causal viewpoints and their influence on epidemiologic methods. Am. J. Epidemiol. 2024, kwae367. [Google Scholar] [CrossRef] [PubMed]
- Weyland, P.G.; Grant, W.B.; Howie-Esquivel, J. Does sufficient evidence exist to support a causal association between vitamin D status and cardiovascular disease risk? An assessment using Hill’s criteria for causality. Nutrients 2014, 6, 3403–3430. [Google Scholar] [CrossRef]
- Doll, R.; Hill, A.B. Smoking and carcinoma of the lung; preliminary report. Br. Med. J. 1950, 2, 739–748. [Google Scholar] [CrossRef]
- Doll, R.; Hill, A.B. Lung cancer and other causes of death in relation to smoking; a second report on the mortality of British doctors. Br. Med. J. 1956, 2, 1071–1081. [Google Scholar] [CrossRef] [PubMed]
- Barbarawi, M.; Kheiri, B.; Zayed, Y.; Barbarawi, O.; Dhillon, H.; Swaid, B.; Yelangi, A.; Sundus, S.; Bachuwa, G.; Alkotob, M.L.; et al. Vitamin D Supplementation and Cardiovascular Disease Risks in More Than 83000 Individuals in 21 Randomized Clinical Trials: A Meta-analysis. JAMA Cardiol. 2019, 4, 765–776. [Google Scholar] [CrossRef]
- Quan, Q.L.; Yoon, K.N.; Lee, J.S.; Kim, E.J.; Lee, D.H. Impact of ultraviolet radiation on cardiovascular and metabolic disorders: The role of nitric oxide and vitamin D. Photodermatol. Photoimmunol. Photomed. 2023, 39, 573–581. [Google Scholar] [CrossRef] [PubMed]
- Pludowski, P.; Kos-Kudla, B.; Walczak, M.; Fal, A.; Zozulinska-Ziolkiewicz, D.; Sieroszewski, P.; Peregud-Pogorzelski, J.; Lauterbach, R.; Targowski, T.; Lewinski, A.; et al. Guidelines for Preventing and Treating Vitamin D Deficiency: A 2023 Update in Poland. Nutrients 2023, 15, 695. [Google Scholar] [CrossRef]
- Ekwaru, J.P.; Zwicker, J.D.; Holick, M.F.; Giovannucci, E.; Veugelers, P.J. The importance of body weight for the dose response relationship of oral vitamin D supplementation and serum 25-hydroxyvitamin D in healthy volunteers. PLoS ONE 2014, 9, e111265. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).