Perceived Quality of Life Is Related to a Healthy Lifestyle and Related Outcomes in Spanish Children and Adolescents: The Physical Activity, Sedentarism, and Obesity in Spanish Study
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. Participants, Recruitment, Randomization, Data Collection, and Ethics
2.3. HRQoL in Children and Adolescents
2.4. Weight Status Assessment
2.5. Healthy Behaviour Assessment
2.6. Physical Fitness
2.7. Statistics
3. Results
4. Discussion
Strengths and Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Wallander, J.L.; Koot, H.M. Quality of life in children: A critical examination of concepts, approaches, issues, and future directions. Clin. Psychol. Rev. 2016, 45, 131–143. [Google Scholar] [CrossRef] [PubMed]
- Remington, P.L.; Catlin, B.B.; Gennuso, K.P. The County Health Rankings: Rationale and methods. Popul. Health Metr. 2015, 13, 11. [Google Scholar] [CrossRef] [PubMed]
- Short, S.E.; Mollborn, S. Social Determinants and Health Behaviors: Conceptual Frames and Empirical Advances. Curr. Opin. Psychol. 2015, 5, 78–84. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. WHOQOL—Measuring Quality of Life The World Health Organization [Internet]. Available online: https://www.who.int/tools/whoqol (accessed on 12 September 2023).
- Vajdi, M.; Farhangi, M.A. A systematic review of the association between dietary patterns and health-related quality of life. Health Qual. Life Outcomes 2020, 18, 337. [Google Scholar] [CrossRef] [PubMed]
- Pastor, R.; Bouzas, C.; Albertos, I.; García, C.; García, Á.; Prieto, T.; Velázquez, J.; Sánchez-Jiménez, E.; Rodríguez, R.; Martín, F.J.; et al. Health-related quality of life in Spanish schoolchildren and its association with the fitness status and adherence to the Mediterranean Diet. Nutrients 2022, 14, 2322. [Google Scholar] [CrossRef] [PubMed]
- Evaristo, O.S.; Moreira, C.; Lopes, L.; Abreu, S.; Agostinis-Sobrinho, C.; Oliveira-Santos, J.; Póvoas, S.; Oliveira, A.; Santos, R.; Mota, J. Associations between physical fitness and adherence to the Mediterranean diet with health-related quality of life in adolescents: Results from the LabMed Physical Activity Study. Eur. J. Public Health 2018, 28, 631–635. [Google Scholar] [CrossRef]
- Alfaro-González, S.; Garrido-Miguel, M.; Martínez-Vizcaíno, V.; López-Gil, J.F. Mediterranean Dietary Pattern and Psychosocial Health Problems in Spanish Adolescents: The EHDLA Study. Nutrients 2023, 15, 2905. [Google Scholar] [CrossRef]
- George, E.S.; Gavrili, S.; Itsiopoulos, C.; Manios, Y.; Moschonis, G. Poor adherence to the Mediterranean diet is associated with increased likelihood of metabolic syndrome components in children: The Healthy Growth Study. Public Health Nutr. 2021, 24, 2823–2833. [Google Scholar] [CrossRef]
- Dinu, M.; Pagliai, G.; Casini, A.; Sofi, F. Mediterranean diet and multiple health outcomes: An umbrella review of meta-analyses of observational studies and randomised trials. Eur. J. Clin. Nutr. 2018, 72, 30–43. [Google Scholar] [CrossRef]
- Wärnberg, J.; Pérez-Farinós, N.; Benavente-Marín, J.C.; Gómez, S.F.; Labayen, I.; Zapico, A.G.; Gusi, N.; Aznar, S.; Alcaraz, P.E.; González-Valeiro, M.; et al. Screen Time and Parents’ Education Level Are Associated with Poor Adherence to the Mediterranean Diet in Spanish Children and Adolescents: The PASOS Study. J. Clin. Med. 2021, 10, 795. [Google Scholar] [CrossRef]
- Sampasa-Kanyinga, H.; Colman, I.; Goldfield, G.S.; Janssen, I.; Wang, J.; Podinic, I.; Tremblay, M.S.; Saunders, T.J.; Sampson, M.; Chaput, J.-P. Combinations of physical activity, sedentary time, and sleep duration and their associations with depressive symptoms and other mental health problems in children and adolescents: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 72. [Google Scholar] [CrossRef] [PubMed]
- Martin, A.; Booth, J.N.; Laird, Y.; Sproule, J.; Reilly, J.J.; Saunders, D.H. Physical activity, diet and other behavioural interventions for improving cognition and school achievement in children and adolescents with obesity or overweight. Cochrane Database Syst. Rev. 2018, 3, CD009728. [Google Scholar] [PubMed]
- Hosker, D.K.; Elkins, R.M.; Potter, M.P. Promoting Mental Health and Wellness in Youth Through Physical Activity, Nutrition, and Sleep. Child Adolesc. Psychiatr. Clin. N. Am. 2019, 28, 171–193. [Google Scholar] [CrossRef] [PubMed]
- Zapico, A.G.; Aparicio-Ugarriza, R.; Quesada-González, C.; Gómez, S.F.; Wärnberg, J.; Medrano, M.; Gusi, N.; Aznar, S.; Marín-Cascales, E.; González-Valeiro, M.A.; et al. Lifestyle behaviors clusters in a nationwide sample of Spanish children and adolescents: PASOS study. Pediatr. Res. 2023, 94, 2077–2084. [Google Scholar] [CrossRef] [PubMed]
- Zhuang, Z.; Gao, M.; Yang, R.; Li, N.; Liu, Z.; Cao, W.; Huang, T. Association of physical activity, sedentary behaviours and sleep duration with cardiovascular diseases and lipid profiles: A Mendelian randomization analysis. Lipids Health Dis. 2020, 19, 86. [Google Scholar] [CrossRef] [PubMed]
- LaVigne, T.; Hoza, B.; Smith, A.L.; Shoulberg, E.K.; Bukowski, W. Associations between Physical Fitness and Children’s Psychological Well-Being. J. Clin. Sport Psychol. 2016, 10, 32–47. [Google Scholar] [CrossRef]
- Ortega, F.B.; Ruiz, J.R.; Castillo, M.J.; Sjöström, M. Physical fitness in childhood and adolescence: A powerful marker of health. Int. J. Obes. 2008, 32, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Lema-Gómez, L.; Arango-Paternina, C.M.; Eusse-López, C.; Petro, J.; Petro-Petro, J.; López-Sánchez, M.; Watts-Fernández, W.; Perea-Velásquez, F. Family aspects, physical fitness, and physical activity associated with mental-health indicators in adolescents. BMC Public Health 2021, 21, 2324. [Google Scholar] [CrossRef]
- Aragón-Martín, R.; Gómez-Sánchez, M.d.M.; Martínez-Nieto, J.M.; Novalbos-Ruiz, J.P.; Segundo-Iglesias, C.; Santi-Cano, M.J.; Castro-Piñero, J.; Lineros-González, C.; Hernán-García, M.; Schwarz-Rodríguez, M.; et al. Independent and Combined Association of Lifestyle Behaviours and Physical Fitness with Body Weight Status in Schoolchildren. Nutrients 2022, 14, 1208. [Google Scholar] [CrossRef]
- Orkaby, A.R.; Forman, D.E. Physical activity and CVD in older adults: An expert’s perspective. Expert Rev. Cardiovasc. Ther. 2018, 16, 1–10. [Google Scholar] [CrossRef]
- Muros, J.J.; Salvador Pérez, F.; Zurita Ortega, F.; Gámez Sánchez, V.M.; Knox, E. The association between healthy lifestyle behaviors and health-related quality of life among adolescents. J. Pediatr. (Rio J.) 2017, 93, 406–412. [Google Scholar] [CrossRef] [PubMed]
- Esteban-Gonzalo, L.; Turner, A.I.; Torres, S.J.; Esteban-Cornejo, I.; Castro-Piñero, J.; Delgado-Alfonso, Á.; Marcos, A.; Gómez-Martínez, S.; Veiga, Ó.L. Diet quality and well-being in children and adolescents: The UP&DOWN longitudinal study. Br. J. Nutr. 2019, 121, 221–231. [Google Scholar] [CrossRef] [PubMed]
- Juton, C.; Berruezo, P.; Rajmil, L.; Lerin, C.; Fíto, M.; Homs, C.; Según, G.; Gómez, S.F.; Schröder, H. Prospective Association between Adherence to the Mediterranean Diet and Health-Related Quality of Life in Spanish Children. Nutrients 2022, 14, 5304. [Google Scholar] [CrossRef] [PubMed]
- Moravejolahkami, A.R.; Paknahad, Z.; Chitsaz, A. Association of dietary patterns with systemic inflammation, quality of life, disease severity, relapse rate, severity of fatigue and anthropometric measurements in MS patients. Nutr. Neurosci. 2020, 23, 920–930. [Google Scholar] [CrossRef] [PubMed]
- Marques, A.; Mota, J.; Gaspar, T.; de Matos, M.G. Associations between self-reported fitness and self-rated health, life-satisfaction and health-related quality of life among adolescents. J. Exerc. Sci. Fit. 2017, 15, 8–11. [Google Scholar] [CrossRef]
- Mozzillo, E.; Zito, E.; Calcaterra, V.; Corciulo, N.; Di Pietro, M.; Di Sessa, A.; Franceschi, R.; Licenziati, M.R.; Maltoni, G.; Morino, G.; et al. Poor Health Related Quality of Life and Unhealthy Lifestyle Habits in Weight-Loss Treatment-Seeking Youth. Int. J. Environ. Res. Public Health 2021, 18, 9355. [Google Scholar] [CrossRef]
- Redondo-Tébar, A.; Ruíz-Hermosa, A.; Martínez-Vizcaíno, V.; Cobo-Cuenca, A.I.; Bermejo-Cantarero, A.; Cavero-Redondo, I.; Sánchez-López, M. Associations between health-related quality of life and physical fitness in 4–7-year-old Spanish children: The MOVIKIDS study. Qual. Life Res. 2019, 28, 1751–1759. [Google Scholar] [CrossRef]
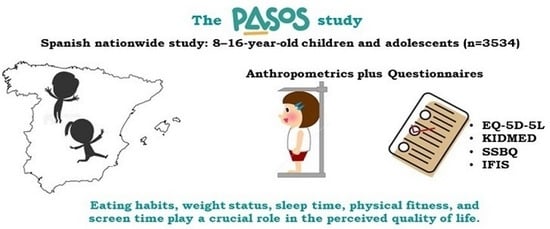
- Gómez, S.F.; Homs, C.; Wärnberg, J.; Medrano, M.; Gonzalez-Gross, M.; Gusi, N.; Aznar, S.; Cascales, E.M.; González-Valeiro, M.; Serra-Majem, L.; et al. Study protocol of a population-based cohort investigating Physical Activity, Sedentarism, lifestyles and Obesity in Spanish youth: The PASOS study. BMJ Open 2020, 10, e036210. [Google Scholar] [CrossRef]
- The EuroQol Group. EuroQol-a new facility for the measurement of health-related quality of life. Health Policy 1990, 16, 199–208. [Google Scholar] [CrossRef]
- Hernandez, G.; Garin, O.; Pardo, Y.; Vilagut, G.; Pont, À.; Suárez, M.; Neira, M.; Rajmil, L.; Gorostiza, I.; Ramallo-Fariña, Y.; et al. Validity of the EQ–5D–5L and reference norms for the Spanish population. Qual. Life Res. 2018, 27, 2337–2348. [Google Scholar] [CrossRef]
- Oppe, M.; Devlin, N.J.; van Hout, B.; Krabbe, P.F.; de Charro, F. A Program of Methodological Research to Arrive at the New International EQ-5D-5L Valuation Protocol. Value Health 2014, 17, 445–453. [Google Scholar] [CrossRef] [PubMed]
- Herdman, M.; Gudex, C.; Lloyd, A.; Janssen, M.; Kind, P.; Parkin, D.; Bonsel, G.; Badia, X. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual. Life Res. 2011, 20, 1727–1736. [Google Scholar] [CrossRef] [PubMed]
- Devlin, N.; Roudijk, B.; Ludwig, K. (Eds.) . Value Sets for EQ-5D-5L: A Compendium, Comparative Review & User Guide [Internet]; Springer: Cham, Switzerland, 2022. [Google Scholar]
- World Health Organization. WHO Child Growth Standards: Training Course on Child Growth Assessment. Cours de formation sur l’évaluation de la croissance de l’enfant : Normes OMS de croissance de l’enfant; World Health Organization: Geneva, Switzerland, 2008; p. 10. [Google Scholar]
- Fernández, C.; Lorenzo, H.; Vrotsou, K.; Aresti, U.; Rica, I.; Sánchez, E. Curvas y Tablas de Crecimiento (Estudio Transversal). 2011. Available online: https://www.fundacionorbegozo.com/wp-content/uploads/pdf/estudios_2011.pdf (accessed on 12 September 2023).
- Taylor, R.W.; Williams, S.M.; Grant, A.M.; Taylor, B.J.; Goulding, A. Predictive ability of waist-to-height in relation to adiposity in children is not improved with age and sex-specific values. Obesity 2011, 19, 1062–1068. [Google Scholar] [CrossRef] [PubMed]
- Serra, L.; Aranceta, J. Alimentación Infantil y Juvenil; Estudio enKid Barcelona: Masson, SA, USA, 2002. [Google Scholar]
- Serra-Majem, L.; Ribas, L.; Ngo, J.; Ortega, R.M.; García, A.; Pérez-Rodrigo, C.; Aranceta, J. Food, youth and the Mediterranean diet in Spain. Development of KIDMED, Mediterranean Diet Quality Index in children and adolescents. Public Health Nutr. 2004, 7, 931–935. [Google Scholar] [CrossRef] [PubMed]
- Štefan, L.; Prosoli, R.; Juranko, D.; Čule, M.; Milinović, I.; Novak, D.; Sporiš, G. The Reliability of the Mediterranean Diet Quality Index (KIDMED) Questionnaire. Nutrients 2017, 9, 419. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Farinós, N.; Villar-Villalba, C.; Sobaler, A.M.L.; Saavedra, M.Á.D.R.; Aparicio, A.; Sanz, S.S.; de Dios, T.R.; Castrodeza-Sanz, J.J.; Anta, R.M.O. The relationship between hours of sleep, screen time and frequency of food and drink consumption in Spain in the 2011 and 2013 ALADINO: A cross-sectional study. BMC Public Health 2017, 17, 33. [Google Scholar] [CrossRef]
- The Organisation for Economic Co-operation and Development (OECD). OECD Health Statistics 2018—Definitions, Sources and Methods—Consumption of Vegetables and Fruits, Daily—Survey Data. 2018. Available online: http://stats.oecd.org/wbos/fileview2.aspx?IDFile=5b61fb4c-1d39-42ef-93c2-b126609edd23 (accessed on 14 November 2023).
- Huang, P.; O’keeffe, M.; Elia, C.; Karamanos, A.; Goff, L.M.; Maynard, M.; Cruickshank, J.K.; Harding, S. Fruit and vegetable consumption and mental health across adolescence: Evidence from a diverse urban British cohort study. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 19. [Google Scholar] [CrossRef]
- Wallace, T.C.; Bailey, R.L.; Blumberg, J.B.; Burton-Freeman, B.; Chen, C.-Y.O.; Crowe-White, K.M.; Drewnowski, A.; Hooshmand, S.; Johnson, E.; Lewis, R.; et al. Fruits, vegetables, and health: A comprehensive narrative, umbrella review of the science and recommendations for enhanced public policy to improve intake. Crit. Rev. Food Sci. Nutr. 2020, 60, 2174–2211. [Google Scholar] [CrossRef]
- Wolfson, A.R.; Carskadon, M.A.; Acebo, C.; Seifer, R.; Fallone, G.; Labyak, S.E.; Martin, J.L. Evidence for the validity of a sleep habits survey for adolescents. Sleep 2003, 26, 213–216. [Google Scholar] [CrossRef]
- National Sleep Foundation. Better Sleep for a Better You. Available online: https://www.sleepfoundation.org/ (accessed on 12 December 2023).
- Rey-López, J.P.; Ruiz, J.R.; Ortega, F.B.; Verloigne, M.; Vicente-Rodriguez, G.; Gracia-Marco, L.; Gottrand, F.; Molnar, D.; Widhalm, K.; Zaccaria, M.; et al. Reliability and validity of a screen time-based sedentary behaviour questionnaire for adolescents: The HELENA study. Eur. J. Public Health 2012, 22, 373–377. [Google Scholar] [CrossRef]
- American Academy of Pediatrics. Committee on Public Education. American Academy of Pediatrics: Children, adolescents, and television. Pediatrics 2001, 107, 423–426. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-López, M.; Martínez-Vizcaíno, V.; García-Hermoso, A.; Jiménez-Pavón, D.; Ortega, F.B. Construct validity and test–retest reliability of the International Fitness Scale (IFIS) in Spanish children aged 9–12 years. Scand. J. Med. Sci. Sports 2015, 25, 543–551. [Google Scholar] [CrossRef] [PubMed]
- Regan, C.; Walltott, H.; Kjellenberg, K.; Nyberg, G.; Helgadóttir, B. Investigation of the Associations between Diet Quality and Health-Related Quality of Life in a Sample of Swedish Adolescents. Nutrients 2022, 14, 2489. [Google Scholar] [CrossRef] [PubMed]
- Ilhan, N.; Peker, K.; Yildirim, G.; Baykut, G.; Bayraktar, M.; Yildirim, H. Relationship between healthy lifestyle behaviors and health related quality of life in turkish school-going adolescents. Niger. J. Clin. Pract. 2019, 22, 1742–1751. [Google Scholar] [CrossRef] [PubMed]
- Costarelli, V.; Koretsi, E.; Georgitsogianni, E. Health-related quality of life of Greek adolescents: The role of the Mediterranean diet. Qual. Life Res. 2013, 22, 951–956. [Google Scholar] [CrossRef]
- Diamantis, D.V.; Katsas, K.; Kalogiannis, D.; Kouvari, M.; Linos, A. Health-Related Quality of Life in Childhood and Adolescence: The Interrelation with Level of Adherence to Mediterranean Diet and Dietary Trajectories: Highlights from the DIATROFI Program (2021–2022). Nutrients 2023, 15, 1829. [Google Scholar] [CrossRef]
- Mitri, R.N.; Boulos, C.; Ziade, F. Mediterranean diet adherence amongst adolescents in North Lebanon: The role of skipping meals, meals with the family, physical activity and physical well-being. Br. J. Nutr. 2022, 128, 1349–1356. [Google Scholar] [CrossRef]
- Bolton, K.A.; Jacka, F.; Allender, S.; Kremer, P.; Gibbs, L.; Waters, E.; de Silva, A. The association between self-reported diet quality and health-related quality of life in rural and urban Australian adolescents. Aust. J. Rural. Health 2016, 24, 317–325. [Google Scholar] [CrossRef]
- Sanchez-Aguadero, N.; MARK Group; Alonso-Dominguez, R.; Garcia-Ortiz, L.; Agudo-Conde, C.; Rodriguez-Martin, C.; de Cabo-Laso, A.; Sanchez-Salgado, B.; Ramos, R.; Maderuelo-Fernandez, J.A.; et al. Diet and physical activity in people with intermediate cardiovascular risk and their relationship with the health-related quality of life: Results from the MARK study. Health Qual. Life Outcomes 2016, 14, 169. [Google Scholar] [CrossRef]
- Sundell, A.L.; Angelhoff, C. Sleep and its relation to health-related quality of life in 3–10-year-old children. BMC Public Health 2021, 21, 1043. [Google Scholar] [CrossRef]
- Xiao, Q.; Chaput, J.-P.; Olds, T.; Fogelholm, M.; Hu, G.; Lambert, E.V.; Maher, C.; Maia, J.; Onywera, V.; Sarmiento, O.L.; et al. Sleep characteristics and health-related quality of life in 9- to 11-year-old children from 12 countries. Sleep Health 2020, 6, 4–14. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.K.H.; Wong, R.S.; Cheung, J.P.Y.; Tung, K.T.S.; Yam, J.C.S.; Rich, M.; Fu, K.-W.; Cheung, P.W.H.; Luo, N.; Au, C.H.; et al. Impact of sleep duration, physical activity, and screen time on health-related quality of life in children and adolescents. Health Qual. Life Outcomes 2021, 19, 145. [Google Scholar] [CrossRef] [PubMed]
- Motamed-Gorji, N.; Qorbani, M.; Nikkho, F.; Asadi, M.; Motlagh, M.E.; Safari, O.; Arefirad, T.; Asayesh, H.; Mohammadi, R.; Mansourian, M.; et al. Association of screen time and physical activity with health-related quality of life in Iranian children and adolescents. Health Qual. Life Outcomes 2019, 17, 2. [Google Scholar] [CrossRef] [PubMed]
- Xiang, H.; Lin, L.; Chen, W.; Li, C.; Liu, X.; Li, J.; Ren, Y.; Guo, V.Y. Associations of excessive screen time and early screen exposure with health-related quality of life and behavioral problems among children attending preschools. BMC Public Health 2022, 22, 2440. [Google Scholar] [CrossRef] [PubMed]
- del Pozo-Cruz, B.; Perales, F.; Parker, P.; Lonsdale, C.; Noetel, M.; Hesketh, K.D.; Sanders, T. Joint physical-activity/screen-time trajectories during early childhood: Socio-demographic predictors and consequences on health-related quality-of-life and socio-emotional outcomes. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 55. [Google Scholar] [CrossRef] [PubMed]
- de Lucena, J.M.S.; Loch, M.R.; Silva, E.C.d.C.; Júnior, J.C.d.F. Sedentary behavior and health-related quality of life in adolescents. Ciência Saúde Coletiva 2022, 27, 2143–2152. [Google Scholar] [CrossRef] [PubMed]
- Evaristo, S.; Moreira, C.; Lopes, L.; Oliveira, A.; Abreu, S.; Agostinis-Sobrinho, C.; Oliveira-Santos, J.; Póvoas, S.; Santos, R.; Mota, J. Muscular fitness and cardiorespiratory fitness are associated with health-related quality of life: Results from labmed physical activity study. J. Exerc. Sci. Fit. 2019, 17, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Bermejo-Cantarero, A.; Álvarez-Bueno, C.; Martínez-Vizcaino, V.; Redondo-Tébar, A.; Pozuelo-Carrascosa, D.P.; Sánchez-López, M. Relationship between both cardiorespiratory and muscular fitness and health-related quality of life in children and adolescents: A systematic review and meta-analysis of observational studies. Health Qual. Life Outcomes 2021, 19, 127. [Google Scholar] [CrossRef]
- Al-Akour, N.A.; Khader, Y.S.; Khassawneh, M.Y.; Bawadi, H. Health-related quality of life of adolescents with overweight or obesity in the north of Jordan. Child Care Health Dev. 2012, 38, 237–243. [Google Scholar] [CrossRef]
- Parvin, P.; Amiri, P.; Mansouri-Tehrani, M.M.; Cheraghi, L.; Shab-Khaneh, A.Z.; Azizi, F. Developmental trajectories of body mass index since childhood and health-related quality of life in young adulthood: Tehran Lipid and Glucose Study. Qual. Life Res. 2022, 31, 2093–2106. [Google Scholar] [CrossRef]
- Hoedjes, M.; Makkes, S.; Halberstadt, J.; Noordam, H.; Renders, C.M.; Bosmans, J.E.; van der Baan-Slootweg, O.H.; Seidell, J.C. Health-Related Quality of Life in Children and Adolescents with Severe Obesity after Intensive Lifestyle Treatment and at 1-Year Follow-Up. Obes. Facts 2018, 11, 116–128. [Google Scholar] [CrossRef] [PubMed]
- Kesztyüs, D.; Schreiber, A.; Kobel, S.; Wartha, O.; Kesztyüs, T.; Kilian, R.; Steinacker, J.M. Illness and determinants of health-related quality of life in a cross-sectional sample of schoolchildren in different weight categories. GMS Ger. Med. Sci. 2014, 12, Doc04. [Google Scholar] [CrossRef] [PubMed]
- Kesztyüs, D.; The “Komm mit in das gesunde Boot—Grundschule”—Research Group; Wirt, T.; Kobel, S.; Schreiber, A.; Kettner, S.; Dreyhaupt, J.; Kilian, R.; Steinacker, J.M. Is central obesity associated with poorer health and health-related quality of life in primary school children? Cross-sectional results from the Baden-Württemberg Study. BMC Public Health 2013, 13, 260. [Google Scholar] [CrossRef] [PubMed]
- Delgado-Floody, P.; Gómez-López, M.; Caamaño-Navarrete, F.; Valdés-Badilla, P.; Jerez-Mayorga, D. The Mediating Role of the Muscle Quality Index in the Relation of Screen Time and Abdominal Obesity with Health-Related Quality of Life in Chilean Schoolchildren. Nutrients 2023, 15, 714. [Google Scholar] [CrossRef]
- Gätjens, I.; Hasler, M.; di Giuseppe, R.; Bosy-Westphal, A.; Plachta-Danielzik, S. Family and Lifestyle Factors Mediate the Relationship between Socioeconomic Status and Fat Mass in Children and Adolescents. Obes. Facts 2020, 13, 596–607. [Google Scholar] [CrossRef]

| Low HRQoL § (n = 1775) | High HRQoL § (n = 1759) | p-Value ‡ | |
|---|---|---|---|
| Children age (years) * | 13.00 (2.36) | 12.14 (2.28) | <0.001 |
| Parent age (years) * | 45.01 (6.08) | 44.10 (6.06) | <0.001 |
| Gender | 0.008 | ||
| Male (n; %) | 816 (46.0) | 888 (50.5) | |
| Female (n; %) | 958 (54.0) | 871 (49.5) | |
| Children weight status | <0.001 | ||
| Undernutrition (n; %) | 18 (1.0) | 27 (1.5) | |
| Underweight (n; %) | 98 (5.5) | 110 (6.3) | |
| Normal weight (n; %) | 1124 (63.3) | 1266 (72.0) | |
| Overweight (n; %) | 405 (22.8) | 285 (16.2) | |
| Obesity (n; %) | 114 (6.4) | 59 (3.4) | |
| Children abdominal obesity | <0.001 | ||
| No (n; %) | 1271 (71.6) | 1427 (81.1) | |
| Yes (n; %) | 488 (27.5) | 320 (18.2) | |
| Kid BMI (kg/m2) * | 21.02 (4.21) | 19.68 (3.64) | <0.001 |
| Parent BMI (kg/m2) * | 25.56 (4.64) | 25.19 (4.28) | 0.022 |
| High HRQoL § (n = 1759) | Low HRQoL § (n = 1775) | ||
|---|---|---|---|
| Low adherence MedDiet | Crude OR | 1.00 (ref.) | 2.03 (1.62–2.55) ** |
| Adjusted OR | 1.00 (ref.) | 2.00 (1.58–2.53) ** | |
| Medium adherence MedDiet | Crude OR | 1.00 (ref.) | 1.32 (1.15–1.50) ** |
| Adjusted OR | 1.00 (ref.) | 1.26 (1.10–1.44) ** | |
| High adherence MedDiet | Crude OR | 1.00 (ref.) | 0.57 (0.50–0.65) ** |
| Adjusted OR | 1.00 (ref.) | 0.60 (0.52–0.69) ** | |
| Achieve recommendations of fruits and vegetables | Crude OR | 1.00 (ref.) | 0.49 (0.40–0.59) ** |
| Adjusted OR | 1.00 (ref.) | 0.50 (0.42–0.61) ** | |
| Achieve daily sleep recommendation (Weekdays) | Crude OR | 1.00 (ref.) | 0.66 (0.58–0.76) ** |
| Adjusted OR | 1.00 (ref.) | 0.77 (0.67–0.89) ** | |
| Achieve daily sleep recommendation (Weekend) | Crude OR | 1.00 (ref.) | 0.97 (0.85–1.11) |
| Adjusted OR | 1.00 (ref.) | 0.93 (0.81–1.07) | |
| ScreenTime recommendation Weekdays | Crude OR | 1.00 (ref.) | 0.55 (0.48–0.63) ** |
| Adjusted OR | 1.00 (ref.) | 0.70 (0.60–0.81) ** | |
| ScreenTime recommendation Weekend | Crude OR | 1.00 (ref.) | 0.50 (0.42–0.59) ** |
| Adjusted OR | 1.00 (ref.) | 0.62 (0.51–0.74) ** | |
| High HRQoL § (n = 1759) | Low HRQoL § (n = 1775) | ||
|---|---|---|---|
| Weight status | |||
| Undernutrition | Crude OR | 1.00 (ref.) | 0.66 (0.36–1.20) |
| Adjusted OR | 1.00 (ref.) | 2.59 (0.68–9.93) | |
| Underweight | Crude OR | 1.00 (ref.) | 0.87 (0.66–1.16) |
| Adjusted OR | 1.00 (ref.) | 1.20 (0.81–1.79) | |
| Normal weight | Crude OR | 1.00 (ref.) | 0.67 (0.58–0.77) ** |
| Adjusted OR | 1.00 (ref.) | 0.80 (0.67–0.95) * | |
| Overweight | Crude OR | 1.00 (ref.) | 1.53 (1.29–1.81) ** |
| Adjusted OR | 1.00 (ref.) | 1.22 (1.00–1.50) * | |
| Obesity | Crude OR | 1.00 (ref.) | 1.98 (1.43–2.73) ** |
| Adjusted OR | 1.00 (ref.) | 1.89 (0.49–7.28) | |
| Abdominal obesity | Crude OR | 1.00 (ref.) | 1.71 (1.45–2.00) ** |
| Adjusted OR | 1.00 (ref.) | 1.49 (1.15–1.94) * | |
| High HRQoL § (n = 1759) | Low HRQoL § (n = 1775) | ||
|---|---|---|---|
| General fitness status | Crude OR | 1.00 (ref.) | 0.29 (0.25–0.34) ** |
| Adjusted OR | 1.00 (ref.) | 0.34 (0.29–0.40) ** | |
| Cardiorespiratory physical condition | Crude OR | 1.00 (ref.) | 0.29 (0.25–0.34) ** |
| Adjusted OR | 1.00 (ref.) | 0.34 (0.29–0.39) ** | |
| Muscle strength | Crude OR | 1.00 (ref.) | 0.42 (0.35–0.49) ** |
| Adjusted OR | 1.00 (ref.) | 0.45 (0.38–0.54) ** | |
| Speed and agility | Crude OR | 1.00 (ref.) | 0.44 (0.38–0.51) ** |
| Adjusted OR | 1.00 (ref.) | 0.53 (0.45–0.62) ** | |
| Flexibility | Crude OR | 1.00 (ref.) | 0.55 (0.46–0.66) ** |
| Adjusted OR | 1.00 (ref.) | 0.63 (0.52–0.76) ** | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ródenas-Munar, M.; Monserrat-Mesquida, M.; Gómez, S.F.; Wärnberg, J.; Medrano, M.; González-Gross, M.; Gusi, N.; Aznar, S.; Marín-Cascales, E.; González-Valeiro, M.A.; et al. Perceived Quality of Life Is Related to a Healthy Lifestyle and Related Outcomes in Spanish Children and Adolescents: The Physical Activity, Sedentarism, and Obesity in Spanish Study. Nutrients 2023, 15, 5125. https://doi.org/10.3390/nu15245125
Ródenas-Munar M, Monserrat-Mesquida M, Gómez SF, Wärnberg J, Medrano M, González-Gross M, Gusi N, Aznar S, Marín-Cascales E, González-Valeiro MA, et al. Perceived Quality of Life Is Related to a Healthy Lifestyle and Related Outcomes in Spanish Children and Adolescents: The Physical Activity, Sedentarism, and Obesity in Spanish Study. Nutrients. 2023; 15(24):5125. https://doi.org/10.3390/nu15245125
Chicago/Turabian StyleRódenas-Munar, Marina, Margalida Monserrat-Mesquida, Santiago F. Gómez, Julia Wärnberg, María Medrano, Marcela González-Gross, Narcís Gusi, Susana Aznar, Elena Marín-Cascales, Miguel A. González-Valeiro, and et al. 2023. "Perceived Quality of Life Is Related to a Healthy Lifestyle and Related Outcomes in Spanish Children and Adolescents: The Physical Activity, Sedentarism, and Obesity in Spanish Study" Nutrients 15, no. 24: 5125. https://doi.org/10.3390/nu15245125
APA StyleRódenas-Munar, M., Monserrat-Mesquida, M., Gómez, S. F., Wärnberg, J., Medrano, M., González-Gross, M., Gusi, N., Aznar, S., Marín-Cascales, E., González-Valeiro, M. A., Serra-Majem, L., Pulgar, S., Segu, M., Fitó, M., Torres, S., Benavente-Marín, J. C., Labayen, I., Zapico, A. G., Sánchez-Gómez, J., ... Tur, J. A. (2023). Perceived Quality of Life Is Related to a Healthy Lifestyle and Related Outcomes in Spanish Children and Adolescents: The Physical Activity, Sedentarism, and Obesity in Spanish Study. Nutrients, 15(24), 5125. https://doi.org/10.3390/nu15245125